User login
Soaring Medicare Costs for Unplanned Hospitalizations Underscore Need to Reduce Readmissions
- According to research published in the New England Journal of Medicine, about 1 in 5 hospitalized Medicare beneficiaries were readmitted within 30 days after discharge. Unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
- The Project BOOST toolkit has been downloaded more than 4,000 times.
- Project BOOST has been implemented at more than 150 sites nationwide.
- Early data from six sites that have implemented Project BOOST reveal a reduction in 30-day readmission rates to 11.2% from 14.2%, as well as a 21% reduction in 30-day, all-cause readmission rates.
Source: www.hospitalmedicine.org
- According to research published in the New England Journal of Medicine, about 1 in 5 hospitalized Medicare beneficiaries were readmitted within 30 days after discharge. Unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
- The Project BOOST toolkit has been downloaded more than 4,000 times.
- Project BOOST has been implemented at more than 150 sites nationwide.
- Early data from six sites that have implemented Project BOOST reveal a reduction in 30-day readmission rates to 11.2% from 14.2%, as well as a 21% reduction in 30-day, all-cause readmission rates.
Source: www.hospitalmedicine.org
- According to research published in the New England Journal of Medicine, about 1 in 5 hospitalized Medicare beneficiaries were readmitted within 30 days after discharge. Unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
- The Project BOOST toolkit has been downloaded more than 4,000 times.
- Project BOOST has been implemented at more than 150 sites nationwide.
- Early data from six sites that have implemented Project BOOST reveal a reduction in 30-day readmission rates to 11.2% from 14.2%, as well as a 21% reduction in 30-day, all-cause readmission rates.
Source: www.hospitalmedicine.org
Win Whitcomb: Hospital Value-Based Purchasing Program Adds Measure in Efficiency Domain
HVBP’s First Efficiency Measure
Move over, cost, LOS—make room for ‘Medicare spending per beneficiary’
The unwritten rule in hospitalist circles is that lower cost and length of stay (LOS) mean higher efficiency, with hospitalists (me included) often pointing to one or both of these as a yardstick of performance in the efficiency domain. But if we lower hospital length of stay and costs while shifting costs to post-hospital care, have we solved anything?
This very question was raised by Kuo and Goodwin’s observational study that revealed that decreased hospital costs and LOS were offset by higher utilization and costs after discharge under hospitalist care.1
Efficiency As a Domain of Quality
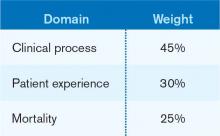
Using the Institute of Medicine’s (IOM) six domains of quality as a framework (see Table 1, right), the Centers for Medicare & Medicaid Services’ (CMS) Hospital Value-Based Purchasing (HVBP) program seeks to encourage enhanced quality in all of the IOM domains. For HVBP 2015, we see the addition of the first measure in the domain of efficiency.
You may be saying to yourself, “It’s only 2013. Why should I worry about HVBP 2015?” Here’s why: The measurement periods for HVBP 2015 are May to December 2011 (baseline) and May to December 2013 (performance). Hospitals can succeed under HVBP if they demonstrate improvement from baseline or attainment, which indicates maintenance of a high level of performance despite no substantial improvement from baseline. Medicare spending per beneficiary (MSPB) will make up 20% of the 2015 HVBP incentive pool for hospitals.
Medicare Spending Per Beneficiary Instead of Costs or LOS
Why did CMS choose to use MSPB as a measure and not simply hospital costs or length of stay? Measuring efficiency of hospital care has proven to be a sticky wicket. If one simply measures and rewards decreased hospital costs and/or length of stay (which you might legitimately argue is exactly what the current DRG system does by paying a case rate to the hospital), one runs the risk of shifting costs to settings beyond the four walls of the hospital, or even fueling higher rates of hospital readmissions. Also, physician costs and other costs (therapy, home care) are not accounted for; they are accounted for under MSPB (described below). Finally, hospital costs and LOS vary substantially across regions and by severity of illness of the patients being analyzed. This makes it difficult to compare, for example, LOS in California versus Massachusetts.
The MSPB is designed to be a comprehensive and equitable metric:
- It seeks to eliminate cost-shifting among settings by widening the time period from three days prior to 30 days post-inpatient-care episode;
- It looks at the full cost of care by including expenses from both Medicare Part A (hospital) and Part B (doctors, PT, OT, home health, others);
- It incorporates risk adjustment by taking into account differences in patient health status; and
- It seeks to level the playing field by using a price standardization methodology that factors in geographic payment differences in wages, practice costs, and payments for indirect medical education and disproportionate share hospitals (those that treat large numbers of the indigent population).
Driving High Performance in Medicare Spending Per Beneficiary
Hospitalists straddle the Part A and Part B elements of Medicare; they have one foot in the hospital and one foot in the physician practice world. They should be able to improve their hospitals’ performance under the MSPB yardstick. Since the performance measurement period starts in May, now is the time to sharpen your focus on MSPB.
Here are the top priorities for MSPB that I recommend for hospitalists:
Reduction of marginally beneficial resource utilization. This is a process of analyzing resource (e.g. pharmacy, radiology, laboratory, blood products) utilization for the purpose of minimizing costly practices that do not benefit the patient. This is an essential practice of a high-functioning hospitalist program. Through its participation in the Choosing Wisely campaign (see “Stop! Think Twice Before You Order,” p. 46), SHM has helped hospitalists have conversations about these practices with patients.
Hospital throughput. Work on “front end” throughput with the ED by having a process in place to quickly evaluate and facilitate potential admissions. Work with case management to assure timely (and early in the day) discharges.
Safe-discharge processes. We reviewed key elements of a safe discharge last month and provided a link to SHM’s Project BOOST (www.hospitalmedicine.org/boost). From the MSPB perspective: A safe discharge minimizes exorbitant spending after discharge.
Documentation integrity. Because MSPB is risk-adjusted, the more the record reflects patient severity of illness, the better your hospital will perform, all else being equal. Work collaboratively with your documentation integrity professionals!
Much of the success of the HM specialty has been built on the tenet that the hospitalist model delivers efficient inpatient care. In the coming years, the specialty’s contribution will increasingly be gauged by the MSPB measure.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
HVBP’s First Efficiency Measure
Move over, cost, LOS—make room for ‘Medicare spending per beneficiary’
The unwritten rule in hospitalist circles is that lower cost and length of stay (LOS) mean higher efficiency, with hospitalists (me included) often pointing to one or both of these as a yardstick of performance in the efficiency domain. But if we lower hospital length of stay and costs while shifting costs to post-hospital care, have we solved anything?
This very question was raised by Kuo and Goodwin’s observational study that revealed that decreased hospital costs and LOS were offset by higher utilization and costs after discharge under hospitalist care.1
Efficiency As a Domain of Quality
Using the Institute of Medicine’s (IOM) six domains of quality as a framework (see Table 1, right), the Centers for Medicare & Medicaid Services’ (CMS) Hospital Value-Based Purchasing (HVBP) program seeks to encourage enhanced quality in all of the IOM domains. For HVBP 2015, we see the addition of the first measure in the domain of efficiency.
You may be saying to yourself, “It’s only 2013. Why should I worry about HVBP 2015?” Here’s why: The measurement periods for HVBP 2015 are May to December 2011 (baseline) and May to December 2013 (performance). Hospitals can succeed under HVBP if they demonstrate improvement from baseline or attainment, which indicates maintenance of a high level of performance despite no substantial improvement from baseline. Medicare spending per beneficiary (MSPB) will make up 20% of the 2015 HVBP incentive pool for hospitals.
Medicare Spending Per Beneficiary Instead of Costs or LOS
Why did CMS choose to use MSPB as a measure and not simply hospital costs or length of stay? Measuring efficiency of hospital care has proven to be a sticky wicket. If one simply measures and rewards decreased hospital costs and/or length of stay (which you might legitimately argue is exactly what the current DRG system does by paying a case rate to the hospital), one runs the risk of shifting costs to settings beyond the four walls of the hospital, or even fueling higher rates of hospital readmissions. Also, physician costs and other costs (therapy, home care) are not accounted for; they are accounted for under MSPB (described below). Finally, hospital costs and LOS vary substantially across regions and by severity of illness of the patients being analyzed. This makes it difficult to compare, for example, LOS in California versus Massachusetts.
The MSPB is designed to be a comprehensive and equitable metric:
- It seeks to eliminate cost-shifting among settings by widening the time period from three days prior to 30 days post-inpatient-care episode;
- It looks at the full cost of care by including expenses from both Medicare Part A (hospital) and Part B (doctors, PT, OT, home health, others);
- It incorporates risk adjustment by taking into account differences in patient health status; and
- It seeks to level the playing field by using a price standardization methodology that factors in geographic payment differences in wages, practice costs, and payments for indirect medical education and disproportionate share hospitals (those that treat large numbers of the indigent population).
Driving High Performance in Medicare Spending Per Beneficiary
Hospitalists straddle the Part A and Part B elements of Medicare; they have one foot in the hospital and one foot in the physician practice world. They should be able to improve their hospitals’ performance under the MSPB yardstick. Since the performance measurement period starts in May, now is the time to sharpen your focus on MSPB.
Here are the top priorities for MSPB that I recommend for hospitalists:
Reduction of marginally beneficial resource utilization. This is a process of analyzing resource (e.g. pharmacy, radiology, laboratory, blood products) utilization for the purpose of minimizing costly practices that do not benefit the patient. This is an essential practice of a high-functioning hospitalist program. Through its participation in the Choosing Wisely campaign (see “Stop! Think Twice Before You Order,” p. 46), SHM has helped hospitalists have conversations about these practices with patients.
Hospital throughput. Work on “front end” throughput with the ED by having a process in place to quickly evaluate and facilitate potential admissions. Work with case management to assure timely (and early in the day) discharges.
Safe-discharge processes. We reviewed key elements of a safe discharge last month and provided a link to SHM’s Project BOOST (www.hospitalmedicine.org/boost). From the MSPB perspective: A safe discharge minimizes exorbitant spending after discharge.
Documentation integrity. Because MSPB is risk-adjusted, the more the record reflects patient severity of illness, the better your hospital will perform, all else being equal. Work collaboratively with your documentation integrity professionals!
Much of the success of the HM specialty has been built on the tenet that the hospitalist model delivers efficient inpatient care. In the coming years, the specialty’s contribution will increasingly be gauged by the MSPB measure.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
HVBP’s First Efficiency Measure
Move over, cost, LOS—make room for ‘Medicare spending per beneficiary’
The unwritten rule in hospitalist circles is that lower cost and length of stay (LOS) mean higher efficiency, with hospitalists (me included) often pointing to one or both of these as a yardstick of performance in the efficiency domain. But if we lower hospital length of stay and costs while shifting costs to post-hospital care, have we solved anything?
This very question was raised by Kuo and Goodwin’s observational study that revealed that decreased hospital costs and LOS were offset by higher utilization and costs after discharge under hospitalist care.1
Efficiency As a Domain of Quality
Using the Institute of Medicine’s (IOM) six domains of quality as a framework (see Table 1, right), the Centers for Medicare & Medicaid Services’ (CMS) Hospital Value-Based Purchasing (HVBP) program seeks to encourage enhanced quality in all of the IOM domains. For HVBP 2015, we see the addition of the first measure in the domain of efficiency.
You may be saying to yourself, “It’s only 2013. Why should I worry about HVBP 2015?” Here’s why: The measurement periods for HVBP 2015 are May to December 2011 (baseline) and May to December 2013 (performance). Hospitals can succeed under HVBP if they demonstrate improvement from baseline or attainment, which indicates maintenance of a high level of performance despite no substantial improvement from baseline. Medicare spending per beneficiary (MSPB) will make up 20% of the 2015 HVBP incentive pool for hospitals.
Medicare Spending Per Beneficiary Instead of Costs or LOS
Why did CMS choose to use MSPB as a measure and not simply hospital costs or length of stay? Measuring efficiency of hospital care has proven to be a sticky wicket. If one simply measures and rewards decreased hospital costs and/or length of stay (which you might legitimately argue is exactly what the current DRG system does by paying a case rate to the hospital), one runs the risk of shifting costs to settings beyond the four walls of the hospital, or even fueling higher rates of hospital readmissions. Also, physician costs and other costs (therapy, home care) are not accounted for; they are accounted for under MSPB (described below). Finally, hospital costs and LOS vary substantially across regions and by severity of illness of the patients being analyzed. This makes it difficult to compare, for example, LOS in California versus Massachusetts.
The MSPB is designed to be a comprehensive and equitable metric:
- It seeks to eliminate cost-shifting among settings by widening the time period from three days prior to 30 days post-inpatient-care episode;
- It looks at the full cost of care by including expenses from both Medicare Part A (hospital) and Part B (doctors, PT, OT, home health, others);
- It incorporates risk adjustment by taking into account differences in patient health status; and
- It seeks to level the playing field by using a price standardization methodology that factors in geographic payment differences in wages, practice costs, and payments for indirect medical education and disproportionate share hospitals (those that treat large numbers of the indigent population).
Driving High Performance in Medicare Spending Per Beneficiary
Hospitalists straddle the Part A and Part B elements of Medicare; they have one foot in the hospital and one foot in the physician practice world. They should be able to improve their hospitals’ performance under the MSPB yardstick. Since the performance measurement period starts in May, now is the time to sharpen your focus on MSPB.
Here are the top priorities for MSPB that I recommend for hospitalists:
Reduction of marginally beneficial resource utilization. This is a process of analyzing resource (e.g. pharmacy, radiology, laboratory, blood products) utilization for the purpose of minimizing costly practices that do not benefit the patient. This is an essential practice of a high-functioning hospitalist program. Through its participation in the Choosing Wisely campaign (see “Stop! Think Twice Before You Order,” p. 46), SHM has helped hospitalists have conversations about these practices with patients.
Hospital throughput. Work on “front end” throughput with the ED by having a process in place to quickly evaluate and facilitate potential admissions. Work with case management to assure timely (and early in the day) discharges.
Safe-discharge processes. We reviewed key elements of a safe discharge last month and provided a link to SHM’s Project BOOST (www.hospitalmedicine.org/boost). From the MSPB perspective: A safe discharge minimizes exorbitant spending after discharge.
Documentation integrity. Because MSPB is risk-adjusted, the more the record reflects patient severity of illness, the better your hospital will perform, all else being equal. Work collaboratively with your documentation integrity professionals!
Much of the success of the HM specialty has been built on the tenet that the hospitalist model delivers efficient inpatient care. In the coming years, the specialty’s contribution will increasingly be gauged by the MSPB measure.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Better Thinking by Hospitalists Key to Improving Healthcare Industry
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
Hospital Medicine Leaders Set to Converge for HM13
Every year, thousands of hospitalists gather to share their experiences, challenges, and energy with each other at SHM’s annual meeting. In 2013, hospitalists can do all of that while visiting the nation’s capital.
And make a real difference by advocating on Capitol Hill for quality improvement and safety in hospitals.
And enjoy all the amenities of a first-class hotel and conference center under one roof.
And get ahead of the curve on some of the most pressing topics in healthcare, such as the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely campaign.
But in order to do all of that, hospitalists have to register for HM13, and must do so quickly to save $50. The early registration deadline is March 19, earlier than in prior years. So don’t wait—sign up now at www.hospitalmedicine2013.org.
Choosing Wisely
Are you ready to make wise choices? HM13 provides unprecedented access to the hospitalist experts who developed the lists of recommendations for the Choosing Wisely campaign with two educational sessions and a pre-course.
Before HM13 kicks off, hospitalists John Bulger, DO, FACP, SFHM, and Ian Jenkins, MD, will direct a full-day Choosing Wisely pre-course on Thursday, May 16, featuring didactic sessions in the morning with national experts in QI on such topics as teambuilding and making the case for quality. The afternoon session will encompass highly interactive workgroups utilizing skills learned in the morning to develop a plan for how to “choose wisely.” Attendees will apply quality methodologies to frequently overutilized tests or procedures, resulting in an actual plan for embedding “avoids” or “never-dos” into their own practice in their own institutions.
On Saturday, May 18, Douglas Carlson, MD, and Ricardo Quinonez, MD, FAAP, FHM, will present “Addressing Overuse in Pediatric Hospital Medicine: The ABIM Choosing Wisely Campaign—PHM Recommendations,” and on Sunday, May 19, Drs. Bulger and Jenkins will present “Choosing Wisely: 5 Things Physicians and Patients Should Question.”
New Featured Speaker
Back by popular demand, hospitalist Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and the director of the Office of Clinical Standards and Quality Centers for the Centers for Medicare & Medicaid Services (CMS), will speak on the role hospitalists will play as change agents for healthcare reform and patient safety in the years to come. Dr. Conway replaces quality expert Peter Pronovost, MD, who had a scheduling conflict and will not be able to speak at HM13.
Get Your Conference In Hand
Hospitalists continue to be ahead of the curve, and the technology at HM13 is no exception. This year’s HM13 At Hand conference app for smartphones and tablets enables conference-goers to plan their schedule ahead of time, download meeting content, play a scavenger hunt for prizes, and socialize with other attendees.
The app’s scheduling feature offers attendees the chance to explore their options ahead of time or make changes on the fly to their HM13 experience.
For links to download the HM13 app, visit www.hospitalmedicine.org.
Every year, thousands of hospitalists gather to share their experiences, challenges, and energy with each other at SHM’s annual meeting. In 2013, hospitalists can do all of that while visiting the nation’s capital.
And make a real difference by advocating on Capitol Hill for quality improvement and safety in hospitals.
And enjoy all the amenities of a first-class hotel and conference center under one roof.
And get ahead of the curve on some of the most pressing topics in healthcare, such as the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely campaign.
But in order to do all of that, hospitalists have to register for HM13, and must do so quickly to save $50. The early registration deadline is March 19, earlier than in prior years. So don’t wait—sign up now at www.hospitalmedicine2013.org.
Choosing Wisely
Are you ready to make wise choices? HM13 provides unprecedented access to the hospitalist experts who developed the lists of recommendations for the Choosing Wisely campaign with two educational sessions and a pre-course.
Before HM13 kicks off, hospitalists John Bulger, DO, FACP, SFHM, and Ian Jenkins, MD, will direct a full-day Choosing Wisely pre-course on Thursday, May 16, featuring didactic sessions in the morning with national experts in QI on such topics as teambuilding and making the case for quality. The afternoon session will encompass highly interactive workgroups utilizing skills learned in the morning to develop a plan for how to “choose wisely.” Attendees will apply quality methodologies to frequently overutilized tests or procedures, resulting in an actual plan for embedding “avoids” or “never-dos” into their own practice in their own institutions.
On Saturday, May 18, Douglas Carlson, MD, and Ricardo Quinonez, MD, FAAP, FHM, will present “Addressing Overuse in Pediatric Hospital Medicine: The ABIM Choosing Wisely Campaign—PHM Recommendations,” and on Sunday, May 19, Drs. Bulger and Jenkins will present “Choosing Wisely: 5 Things Physicians and Patients Should Question.”
New Featured Speaker
Back by popular demand, hospitalist Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and the director of the Office of Clinical Standards and Quality Centers for the Centers for Medicare & Medicaid Services (CMS), will speak on the role hospitalists will play as change agents for healthcare reform and patient safety in the years to come. Dr. Conway replaces quality expert Peter Pronovost, MD, who had a scheduling conflict and will not be able to speak at HM13.
Get Your Conference In Hand
Hospitalists continue to be ahead of the curve, and the technology at HM13 is no exception. This year’s HM13 At Hand conference app for smartphones and tablets enables conference-goers to plan their schedule ahead of time, download meeting content, play a scavenger hunt for prizes, and socialize with other attendees.
The app’s scheduling feature offers attendees the chance to explore their options ahead of time or make changes on the fly to their HM13 experience.
For links to download the HM13 app, visit www.hospitalmedicine.org.
Every year, thousands of hospitalists gather to share their experiences, challenges, and energy with each other at SHM’s annual meeting. In 2013, hospitalists can do all of that while visiting the nation’s capital.
And make a real difference by advocating on Capitol Hill for quality improvement and safety in hospitals.
And enjoy all the amenities of a first-class hotel and conference center under one roof.
And get ahead of the curve on some of the most pressing topics in healthcare, such as the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely campaign.
But in order to do all of that, hospitalists have to register for HM13, and must do so quickly to save $50. The early registration deadline is March 19, earlier than in prior years. So don’t wait—sign up now at www.hospitalmedicine2013.org.
Choosing Wisely
Are you ready to make wise choices? HM13 provides unprecedented access to the hospitalist experts who developed the lists of recommendations for the Choosing Wisely campaign with two educational sessions and a pre-course.
Before HM13 kicks off, hospitalists John Bulger, DO, FACP, SFHM, and Ian Jenkins, MD, will direct a full-day Choosing Wisely pre-course on Thursday, May 16, featuring didactic sessions in the morning with national experts in QI on such topics as teambuilding and making the case for quality. The afternoon session will encompass highly interactive workgroups utilizing skills learned in the morning to develop a plan for how to “choose wisely.” Attendees will apply quality methodologies to frequently overutilized tests or procedures, resulting in an actual plan for embedding “avoids” or “never-dos” into their own practice in their own institutions.
On Saturday, May 18, Douglas Carlson, MD, and Ricardo Quinonez, MD, FAAP, FHM, will present “Addressing Overuse in Pediatric Hospital Medicine: The ABIM Choosing Wisely Campaign—PHM Recommendations,” and on Sunday, May 19, Drs. Bulger and Jenkins will present “Choosing Wisely: 5 Things Physicians and Patients Should Question.”
New Featured Speaker
Back by popular demand, hospitalist Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and the director of the Office of Clinical Standards and Quality Centers for the Centers for Medicare & Medicaid Services (CMS), will speak on the role hospitalists will play as change agents for healthcare reform and patient safety in the years to come. Dr. Conway replaces quality expert Peter Pronovost, MD, who had a scheduling conflict and will not be able to speak at HM13.
Get Your Conference In Hand
Hospitalists continue to be ahead of the curve, and the technology at HM13 is no exception. This year’s HM13 At Hand conference app for smartphones and tablets enables conference-goers to plan their schedule ahead of time, download meeting content, play a scavenger hunt for prizes, and socialize with other attendees.
The app’s scheduling feature offers attendees the chance to explore their options ahead of time or make changes on the fly to their HM13 experience.
For links to download the HM13 app, visit www.hospitalmedicine.org.
Medicare Billing Regulations for Nonphysician Providers Vary by State, Facility
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Affordable Care Act Provides Two-Year Increase in Medicaid Payments for Primary-Care Services
Some hospitalist groups can expect a bump in total revenue over the next two years, thanks to the Medicaid-to-Medicare parity regulation that was included in the Affordable Care Act. But whether the increase in reimbursement lasts beyond 2014 is anyone’s guess.
The regulation, which the Centers for Medicare & Medicaid Services (CMS) released in November and made effective Jan. 1, increases Medicaid payments for certain primary-care services to 100% of Medicare levels this year and next. States will receive an estimated $11 billion over the next two years to fund the program, according to the American Academy of Family Physicians (AAFP). Eligible providers include physicians, physician assistants (PAs), and nurse practitioners (NPs), who self-attest they are board-certified in family, pediatric, or general internal medicine; it also includes those doctors, PAs, or NPs who self-attest that at least 60% of all Medicaid services they bill or provide in a managed-care environment are for specific evaluation and management (E&M) and vaccine administration codes.1
The concept is to boost Medicaid participation by improving historically lagging reimbursement rates.2 To wit, CMS’ Office of the Actuary estimates the parity rule will add more than 10,000 new primary-care physicians (PCPs) to the Medicaid participation ranks.3
SHM Public Policy Committee member Brad Flansbaum, DO, MPH, SFHM, says that hospitalists who deal with Medicaid populations can expect at least some increase in their revenue over the next two years. For example, he says, take an HM group earning $100,000 a year in Medicaid revenue. Now consider Urban Institute figures that show, in 2012, Medicaid physician fees on average were 66% of Medicare physician fees (with wide state variations). The parity rule now pays that hypothetical HM group about $150,000.
“It’s simple math,” Dr. Flansbaum says. “I would emphasize that the bump in pay is going to be proportional to the percentage of Medicaid patients that you see. There are some doctors who see an awful lot of Medicaid patients in safety-net and public hospitals, and that money, when it comes back to departments and divisions, can be used for things that a lot of these places never had the means to do before. It could be salary, but it could also mean hiring more people, more resources. It makes a difference.”
Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says SHM advocated for the parity regulation, as Medicaid has historically paid for only about 70% of the healthcare delivered to patients. Although the parity issue has not gathered as much attention as other facets of the healthcare reform movement, having CMS recognize that delivery of primary care is not restricted to traditional offices is one he and SHM are particularly proud of.
“This is a correction long in coming,” Dr. Greeno says. “We’re happy hospitalists were included in the group of people that will achieve that parity.”
Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City, says few physicians are even aware of the provision, in part because of a widespread frustration with Medicaid’s historic reimbursements rates.
“It’s almost a foregone conclusion that Medicaid never pays, reimbursement always goes down, and the interactions with Medicaid are always increasingly difficult,” Dr. Flansbaum adds.
The question for physicians and policy wonks now is what happens to the parity regulation after its scheduled expiration Dec. 31, 2014. Several medical societies, including SHM and the American College of Physicians (ACP), lobbied Congress to make sure the parity regulation was not impacted by the “fiscal cliff” negotiations. The next step is to craft a permanent funding source to pay for it.
“Unless Congress acts to permanently extend and fund this provision, a sudden return to disparate and inadequate payment for primary services needed by Medicaid patients after only two years will again threaten to restrict their access to such needed services,” AAFP said in a statement after the rule was implemented. “It would once again shut out people who have come to know and depend on their primary care physicians. Only by extending Medicaid parity with Medicare can we ensure that these Americans continue to have uninterrupted medical care in the future.”

—Brad Flansbaum, DO, MPH, SFHM, Lenox Hill Hospital, New York City, SHM Public Policy Committee member
SHM recommended that CMS work with the states to facilitate timely data collection designed to determine the effects on the quality and efficiency of care being received under Medicaid as a result of the enhanced fees. CMS agreed with this recommendation and the resulting data, hopefully, will make the case for continuing the enhanced payment following 2014.
Dr. Flansbaum says SHM’s policy team will continue to work on the issue, but given the precarious state of federal budgets and political dysfunction in Washington, it’s too early to know whether a funding source will be identified to pay for parity in 2015 and beyond—especially as politicians have yet to craft long-term solutions to issues including the sustainable-growth rate formula and other specialists, including radiologists and obstetricians, lobby to be eligible for the parity pay. However, he is hopeful that physicians who see the added impact of parity pay in the next two years will lobby Congress to find a way to continue the higher reimbursement.
“I can’t tell you whether or not when you put on the scale of all the priorities whether it’s going to be a new Air Force bomber, another $50 billion into Medicare for physicians, or an educational system upgrade,” he says. “I don’t know where the government is going to assign its priorities. Will the money be there to extend both the two-year Medicaid and the reprieve? And if the answer is yes, will it be extended to other providers beyond just primary-care practitioners? It’s anyone’s guess.”
Richard Quinn is a freelance writer in New Jersey.
References
- FAQ: Medicaid/Medicare Parity Regulation. Society of Hospital Medicine website. Available at: http://www.hospitalmedicine.org/AM/Images/Advocacy_Image/pdf/Parity_FAQ_Final.pdf. Accessed Jan. 27, 2013.
- Centers for Medicare & Medicaid Services. Medicaid program; payments for services furnished by certain primary care physicians and charges for vaccine administration under the Vaccines for Children program. Federal Register website. Available at: http://www.gpo.gov/fdsys/pkg/FR-2012-11-06/pdf/2012-26507.pdf. Accessed Jan. 15, 2013.
- Bindman A. JAMA Forum: Warning: Dangerous physician payment cliffs ahead. Journal of the American Medical Association website. Available at: http://newsatjama.jama.com/2013/01/10/jama-forum-warning-dangerous-physician-payment-cliffs-ahead/.Accessed Jan. 15, 2013.
Some hospitalist groups can expect a bump in total revenue over the next two years, thanks to the Medicaid-to-Medicare parity regulation that was included in the Affordable Care Act. But whether the increase in reimbursement lasts beyond 2014 is anyone’s guess.
The regulation, which the Centers for Medicare & Medicaid Services (CMS) released in November and made effective Jan. 1, increases Medicaid payments for certain primary-care services to 100% of Medicare levels this year and next. States will receive an estimated $11 billion over the next two years to fund the program, according to the American Academy of Family Physicians (AAFP). Eligible providers include physicians, physician assistants (PAs), and nurse practitioners (NPs), who self-attest they are board-certified in family, pediatric, or general internal medicine; it also includes those doctors, PAs, or NPs who self-attest that at least 60% of all Medicaid services they bill or provide in a managed-care environment are for specific evaluation and management (E&M) and vaccine administration codes.1
The concept is to boost Medicaid participation by improving historically lagging reimbursement rates.2 To wit, CMS’ Office of the Actuary estimates the parity rule will add more than 10,000 new primary-care physicians (PCPs) to the Medicaid participation ranks.3
SHM Public Policy Committee member Brad Flansbaum, DO, MPH, SFHM, says that hospitalists who deal with Medicaid populations can expect at least some increase in their revenue over the next two years. For example, he says, take an HM group earning $100,000 a year in Medicaid revenue. Now consider Urban Institute figures that show, in 2012, Medicaid physician fees on average were 66% of Medicare physician fees (with wide state variations). The parity rule now pays that hypothetical HM group about $150,000.
“It’s simple math,” Dr. Flansbaum says. “I would emphasize that the bump in pay is going to be proportional to the percentage of Medicaid patients that you see. There are some doctors who see an awful lot of Medicaid patients in safety-net and public hospitals, and that money, when it comes back to departments and divisions, can be used for things that a lot of these places never had the means to do before. It could be salary, but it could also mean hiring more people, more resources. It makes a difference.”
Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says SHM advocated for the parity regulation, as Medicaid has historically paid for only about 70% of the healthcare delivered to patients. Although the parity issue has not gathered as much attention as other facets of the healthcare reform movement, having CMS recognize that delivery of primary care is not restricted to traditional offices is one he and SHM are particularly proud of.
“This is a correction long in coming,” Dr. Greeno says. “We’re happy hospitalists were included in the group of people that will achieve that parity.”
Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City, says few physicians are even aware of the provision, in part because of a widespread frustration with Medicaid’s historic reimbursements rates.
“It’s almost a foregone conclusion that Medicaid never pays, reimbursement always goes down, and the interactions with Medicaid are always increasingly difficult,” Dr. Flansbaum adds.
The question for physicians and policy wonks now is what happens to the parity regulation after its scheduled expiration Dec. 31, 2014. Several medical societies, including SHM and the American College of Physicians (ACP), lobbied Congress to make sure the parity regulation was not impacted by the “fiscal cliff” negotiations. The next step is to craft a permanent funding source to pay for it.
“Unless Congress acts to permanently extend and fund this provision, a sudden return to disparate and inadequate payment for primary services needed by Medicaid patients after only two years will again threaten to restrict their access to such needed services,” AAFP said in a statement after the rule was implemented. “It would once again shut out people who have come to know and depend on their primary care physicians. Only by extending Medicaid parity with Medicare can we ensure that these Americans continue to have uninterrupted medical care in the future.”

—Brad Flansbaum, DO, MPH, SFHM, Lenox Hill Hospital, New York City, SHM Public Policy Committee member
SHM recommended that CMS work with the states to facilitate timely data collection designed to determine the effects on the quality and efficiency of care being received under Medicaid as a result of the enhanced fees. CMS agreed with this recommendation and the resulting data, hopefully, will make the case for continuing the enhanced payment following 2014.
Dr. Flansbaum says SHM’s policy team will continue to work on the issue, but given the precarious state of federal budgets and political dysfunction in Washington, it’s too early to know whether a funding source will be identified to pay for parity in 2015 and beyond—especially as politicians have yet to craft long-term solutions to issues including the sustainable-growth rate formula and other specialists, including radiologists and obstetricians, lobby to be eligible for the parity pay. However, he is hopeful that physicians who see the added impact of parity pay in the next two years will lobby Congress to find a way to continue the higher reimbursement.
“I can’t tell you whether or not when you put on the scale of all the priorities whether it’s going to be a new Air Force bomber, another $50 billion into Medicare for physicians, or an educational system upgrade,” he says. “I don’t know where the government is going to assign its priorities. Will the money be there to extend both the two-year Medicaid and the reprieve? And if the answer is yes, will it be extended to other providers beyond just primary-care practitioners? It’s anyone’s guess.”
Richard Quinn is a freelance writer in New Jersey.
References
- FAQ: Medicaid/Medicare Parity Regulation. Society of Hospital Medicine website. Available at: http://www.hospitalmedicine.org/AM/Images/Advocacy_Image/pdf/Parity_FAQ_Final.pdf. Accessed Jan. 27, 2013.
- Centers for Medicare & Medicaid Services. Medicaid program; payments for services furnished by certain primary care physicians and charges for vaccine administration under the Vaccines for Children program. Federal Register website. Available at: http://www.gpo.gov/fdsys/pkg/FR-2012-11-06/pdf/2012-26507.pdf. Accessed Jan. 15, 2013.
- Bindman A. JAMA Forum: Warning: Dangerous physician payment cliffs ahead. Journal of the American Medical Association website. Available at: http://newsatjama.jama.com/2013/01/10/jama-forum-warning-dangerous-physician-payment-cliffs-ahead/.Accessed Jan. 15, 2013.
Some hospitalist groups can expect a bump in total revenue over the next two years, thanks to the Medicaid-to-Medicare parity regulation that was included in the Affordable Care Act. But whether the increase in reimbursement lasts beyond 2014 is anyone’s guess.
The regulation, which the Centers for Medicare & Medicaid Services (CMS) released in November and made effective Jan. 1, increases Medicaid payments for certain primary-care services to 100% of Medicare levels this year and next. States will receive an estimated $11 billion over the next two years to fund the program, according to the American Academy of Family Physicians (AAFP). Eligible providers include physicians, physician assistants (PAs), and nurse practitioners (NPs), who self-attest they are board-certified in family, pediatric, or general internal medicine; it also includes those doctors, PAs, or NPs who self-attest that at least 60% of all Medicaid services they bill or provide in a managed-care environment are for specific evaluation and management (E&M) and vaccine administration codes.1
The concept is to boost Medicaid participation by improving historically lagging reimbursement rates.2 To wit, CMS’ Office of the Actuary estimates the parity rule will add more than 10,000 new primary-care physicians (PCPs) to the Medicaid participation ranks.3
SHM Public Policy Committee member Brad Flansbaum, DO, MPH, SFHM, says that hospitalists who deal with Medicaid populations can expect at least some increase in their revenue over the next two years. For example, he says, take an HM group earning $100,000 a year in Medicaid revenue. Now consider Urban Institute figures that show, in 2012, Medicaid physician fees on average were 66% of Medicare physician fees (with wide state variations). The parity rule now pays that hypothetical HM group about $150,000.
“It’s simple math,” Dr. Flansbaum says. “I would emphasize that the bump in pay is going to be proportional to the percentage of Medicaid patients that you see. There are some doctors who see an awful lot of Medicaid patients in safety-net and public hospitals, and that money, when it comes back to departments and divisions, can be used for things that a lot of these places never had the means to do before. It could be salary, but it could also mean hiring more people, more resources. It makes a difference.”
Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says SHM advocated for the parity regulation, as Medicaid has historically paid for only about 70% of the healthcare delivered to patients. Although the parity issue has not gathered as much attention as other facets of the healthcare reform movement, having CMS recognize that delivery of primary care is not restricted to traditional offices is one he and SHM are particularly proud of.
“This is a correction long in coming,” Dr. Greeno says. “We’re happy hospitalists were included in the group of people that will achieve that parity.”
Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City, says few physicians are even aware of the provision, in part because of a widespread frustration with Medicaid’s historic reimbursements rates.
“It’s almost a foregone conclusion that Medicaid never pays, reimbursement always goes down, and the interactions with Medicaid are always increasingly difficult,” Dr. Flansbaum adds.
The question for physicians and policy wonks now is what happens to the parity regulation after its scheduled expiration Dec. 31, 2014. Several medical societies, including SHM and the American College of Physicians (ACP), lobbied Congress to make sure the parity regulation was not impacted by the “fiscal cliff” negotiations. The next step is to craft a permanent funding source to pay for it.
“Unless Congress acts to permanently extend and fund this provision, a sudden return to disparate and inadequate payment for primary services needed by Medicaid patients after only two years will again threaten to restrict their access to such needed services,” AAFP said in a statement after the rule was implemented. “It would once again shut out people who have come to know and depend on their primary care physicians. Only by extending Medicaid parity with Medicare can we ensure that these Americans continue to have uninterrupted medical care in the future.”

—Brad Flansbaum, DO, MPH, SFHM, Lenox Hill Hospital, New York City, SHM Public Policy Committee member
SHM recommended that CMS work with the states to facilitate timely data collection designed to determine the effects on the quality and efficiency of care being received under Medicaid as a result of the enhanced fees. CMS agreed with this recommendation and the resulting data, hopefully, will make the case for continuing the enhanced payment following 2014.
Dr. Flansbaum says SHM’s policy team will continue to work on the issue, but given the precarious state of federal budgets and political dysfunction in Washington, it’s too early to know whether a funding source will be identified to pay for parity in 2015 and beyond—especially as politicians have yet to craft long-term solutions to issues including the sustainable-growth rate formula and other specialists, including radiologists and obstetricians, lobby to be eligible for the parity pay. However, he is hopeful that physicians who see the added impact of parity pay in the next two years will lobby Congress to find a way to continue the higher reimbursement.
“I can’t tell you whether or not when you put on the scale of all the priorities whether it’s going to be a new Air Force bomber, another $50 billion into Medicare for physicians, or an educational system upgrade,” he says. “I don’t know where the government is going to assign its priorities. Will the money be there to extend both the two-year Medicaid and the reprieve? And if the answer is yes, will it be extended to other providers beyond just primary-care practitioners? It’s anyone’s guess.”
Richard Quinn is a freelance writer in New Jersey.
References
- FAQ: Medicaid/Medicare Parity Regulation. Society of Hospital Medicine website. Available at: http://www.hospitalmedicine.org/AM/Images/Advocacy_Image/pdf/Parity_FAQ_Final.pdf. Accessed Jan. 27, 2013.
- Centers for Medicare & Medicaid Services. Medicaid program; payments for services furnished by certain primary care physicians and charges for vaccine administration under the Vaccines for Children program. Federal Register website. Available at: http://www.gpo.gov/fdsys/pkg/FR-2012-11-06/pdf/2012-26507.pdf. Accessed Jan. 15, 2013.
- Bindman A. JAMA Forum: Warning: Dangerous physician payment cliffs ahead. Journal of the American Medical Association website. Available at: http://newsatjama.jama.com/2013/01/10/jama-forum-warning-dangerous-physician-payment-cliffs-ahead/.Accessed Jan. 15, 2013.
Medicare Funding May Become Enormous Burden for Generations of Future Taxpayers
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
Effect of Nonpayment on Nosocomial Infection Rates in U.S. Hospitals
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Win Whitcomb: Mortality Rates Become a Measuring Stick for Hospital Performance
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Multidisciplinary Palliative-Care Consults Help Reduce Hospital Readmissions
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.