User login
Hospitalists Encouraged to Join the Future of Hospital Conversation
This month, hospitalists can play a role in crowdsourcing the future of the community hospital. And one hospitalist is helping to shape the game.
On Jan. 8, the Institute for the Future launched its Future of Hospital foresight game (www.futureofhospital.org). The game will tap the wisdom of healthcare experts, urban planners, technologists, sociologists, local community leaders, social entrepreneurs, and citizens interested in engaging in a thoughtful discussion about future possibilities for community hospitals.
Hospitalist Jason Stein, MD, SFHM, is working with the Institute for the Future to help judge the responses and participation in the online, crowd-sourced game. As an advisor to the Centers for Medicare & Medicaid Services Innovation Center, Dr. Stein is no stranger to new ideas for hospitals. He was one of the co-architects of SHM’s Implementation Guides, which create step-wise approaches for system-level change. He also has been recognized nationally for his work redesigning traditional medical wards into accountable-care units, each featuring unit-based physician teams that conduct structured interdisciplinary bedside rounds (SIBRs).
“This is an exciting way for hospitalists to join a dynamic conversation about how hospitals—and their staff—provide the best care possible to their patients in 21st-century, American healthcare,” Dr. Stein says.
The Future of the Hospital is a game that anyone can play; all that is required is ideas. If others build on those ideas, contributors win points and create award-winning chains of innovation, linking people and their ideas from all over the world.
“Hospitalists have been on the cutting edge of some of the best ideas in healthcare for the last two decades,” Dr. Stein says. “This is an exciting and innovative way for all of us to contribute ideas and leverage our collective experience for the good of our hospitals and patients.”
This month, hospitalists can play a role in crowdsourcing the future of the community hospital. And one hospitalist is helping to shape the game.
On Jan. 8, the Institute for the Future launched its Future of Hospital foresight game (www.futureofhospital.org). The game will tap the wisdom of healthcare experts, urban planners, technologists, sociologists, local community leaders, social entrepreneurs, and citizens interested in engaging in a thoughtful discussion about future possibilities for community hospitals.
Hospitalist Jason Stein, MD, SFHM, is working with the Institute for the Future to help judge the responses and participation in the online, crowd-sourced game. As an advisor to the Centers for Medicare & Medicaid Services Innovation Center, Dr. Stein is no stranger to new ideas for hospitals. He was one of the co-architects of SHM’s Implementation Guides, which create step-wise approaches for system-level change. He also has been recognized nationally for his work redesigning traditional medical wards into accountable-care units, each featuring unit-based physician teams that conduct structured interdisciplinary bedside rounds (SIBRs).
“This is an exciting way for hospitalists to join a dynamic conversation about how hospitals—and their staff—provide the best care possible to their patients in 21st-century, American healthcare,” Dr. Stein says.
The Future of the Hospital is a game that anyone can play; all that is required is ideas. If others build on those ideas, contributors win points and create award-winning chains of innovation, linking people and their ideas from all over the world.
“Hospitalists have been on the cutting edge of some of the best ideas in healthcare for the last two decades,” Dr. Stein says. “This is an exciting and innovative way for all of us to contribute ideas and leverage our collective experience for the good of our hospitals and patients.”
This month, hospitalists can play a role in crowdsourcing the future of the community hospital. And one hospitalist is helping to shape the game.
On Jan. 8, the Institute for the Future launched its Future of Hospital foresight game (www.futureofhospital.org). The game will tap the wisdom of healthcare experts, urban planners, technologists, sociologists, local community leaders, social entrepreneurs, and citizens interested in engaging in a thoughtful discussion about future possibilities for community hospitals.
Hospitalist Jason Stein, MD, SFHM, is working with the Institute for the Future to help judge the responses and participation in the online, crowd-sourced game. As an advisor to the Centers for Medicare & Medicaid Services Innovation Center, Dr. Stein is no stranger to new ideas for hospitals. He was one of the co-architects of SHM’s Implementation Guides, which create step-wise approaches for system-level change. He also has been recognized nationally for his work redesigning traditional medical wards into accountable-care units, each featuring unit-based physician teams that conduct structured interdisciplinary bedside rounds (SIBRs).
“This is an exciting way for hospitalists to join a dynamic conversation about how hospitals—and their staff—provide the best care possible to their patients in 21st-century, American healthcare,” Dr. Stein says.
The Future of the Hospital is a game that anyone can play; all that is required is ideas. If others build on those ideas, contributors win points and create award-winning chains of innovation, linking people and their ideas from all over the world.
“Hospitalists have been on the cutting edge of some of the best ideas in healthcare for the last two decades,” Dr. Stein says. “This is an exciting and innovative way for all of us to contribute ideas and leverage our collective experience for the good of our hospitals and patients.”
Medicaid Payments for Some Primary-Care Services Reach Parity with Medicare Levels
On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulation implementing increased Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
Covered Medicaid services include evaluation and management codes between 99201 and 99499 when used by physicians with a specialty designation of family medicine, general internal medicine, or pediatric medicine. CMS also finalized a policy to qualify services provided by subspecialists related to the designated primary-care specialists board-certified by the American Board of Medical Specialties, American Osteopathic Association, and the American Board of Physician Specialties. Advanced-practice clinicians also qualify for the increased payment when services are furnished under a physician’s personal supervision.
In commenting on the proposed rule, SHM stated that hospitalists should qualify for purposes of the increased payment because they are an important part of the “team” of clinicians required to treat many common conditions within the Medicaid population, and that hospitalists often provide the first contact and facilitate an entry point into the comprehensive care network.
CMS agreed.
The codes included in the pay increase will be limited to traditional primary care but also will include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services.
Hospitalists will qualify for the enhanced payment, but it remains somewhat unclear how individual states will handle the increase. State Medicaid agencies could pay physicians based on their self-attestation alone or in conjunction with any other provider enrollment requirements that currently exist in the state. Further, inclusion of a code does not require a state to pay for the service if it is not already covered under the state’s Medicaid program. All other state coverage and payment policy rules related to the services also remain in effect.
Timing of the pay increase also remains unclear. The statute requires that states make higher payments for services provided on or after Jan. 1, 2013, but for many physicians, the higher payment might be longer in coming despite being retroactive to the January deadline. States must submit a State Plan Amendment (SPA) to reflect the fee schedule rate increases by March 31, 2013, and CMS may then take up to 90 days to review and approve the SPA. Therefore, it could be six months or longer before eligible physicians and practitioners receive any of the payment increase.
States will receive an estimated $5.8 billion in 2013 and $6.1 billion in 2014 in federal funds to meet this two-year requirement, unless Congress acts to extend or fund the provision permanently. In response to an SHM suggestion on the potential to extend the increase, CMS will be collecting relevant data on the impact of the pay increase on Medicaid patients.
Even with the remaining uncertainty and timing issues, this is a change in payment policy that presents an important shift in the valuation of primary-care services, including some services provided by hospitalists. Medicaid services are notoriously undervalued, and this increase to providers will certainly have a positive impact on the accessibility of care for patients.
Josh Boswell is SHM’s interim senior manager of government relations.
On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulation implementing increased Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
Covered Medicaid services include evaluation and management codes between 99201 and 99499 when used by physicians with a specialty designation of family medicine, general internal medicine, or pediatric medicine. CMS also finalized a policy to qualify services provided by subspecialists related to the designated primary-care specialists board-certified by the American Board of Medical Specialties, American Osteopathic Association, and the American Board of Physician Specialties. Advanced-practice clinicians also qualify for the increased payment when services are furnished under a physician’s personal supervision.
In commenting on the proposed rule, SHM stated that hospitalists should qualify for purposes of the increased payment because they are an important part of the “team” of clinicians required to treat many common conditions within the Medicaid population, and that hospitalists often provide the first contact and facilitate an entry point into the comprehensive care network.
CMS agreed.
The codes included in the pay increase will be limited to traditional primary care but also will include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services.
Hospitalists will qualify for the enhanced payment, but it remains somewhat unclear how individual states will handle the increase. State Medicaid agencies could pay physicians based on their self-attestation alone or in conjunction with any other provider enrollment requirements that currently exist in the state. Further, inclusion of a code does not require a state to pay for the service if it is not already covered under the state’s Medicaid program. All other state coverage and payment policy rules related to the services also remain in effect.
Timing of the pay increase also remains unclear. The statute requires that states make higher payments for services provided on or after Jan. 1, 2013, but for many physicians, the higher payment might be longer in coming despite being retroactive to the January deadline. States must submit a State Plan Amendment (SPA) to reflect the fee schedule rate increases by March 31, 2013, and CMS may then take up to 90 days to review and approve the SPA. Therefore, it could be six months or longer before eligible physicians and practitioners receive any of the payment increase.
States will receive an estimated $5.8 billion in 2013 and $6.1 billion in 2014 in federal funds to meet this two-year requirement, unless Congress acts to extend or fund the provision permanently. In response to an SHM suggestion on the potential to extend the increase, CMS will be collecting relevant data on the impact of the pay increase on Medicaid patients.
Even with the remaining uncertainty and timing issues, this is a change in payment policy that presents an important shift in the valuation of primary-care services, including some services provided by hospitalists. Medicaid services are notoriously undervalued, and this increase to providers will certainly have a positive impact on the accessibility of care for patients.
Josh Boswell is SHM’s interim senior manager of government relations.
On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulation implementing increased Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
Covered Medicaid services include evaluation and management codes between 99201 and 99499 when used by physicians with a specialty designation of family medicine, general internal medicine, or pediatric medicine. CMS also finalized a policy to qualify services provided by subspecialists related to the designated primary-care specialists board-certified by the American Board of Medical Specialties, American Osteopathic Association, and the American Board of Physician Specialties. Advanced-practice clinicians also qualify for the increased payment when services are furnished under a physician’s personal supervision.
In commenting on the proposed rule, SHM stated that hospitalists should qualify for purposes of the increased payment because they are an important part of the “team” of clinicians required to treat many common conditions within the Medicaid population, and that hospitalists often provide the first contact and facilitate an entry point into the comprehensive care network.
CMS agreed.
The codes included in the pay increase will be limited to traditional primary care but also will include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services.
Hospitalists will qualify for the enhanced payment, but it remains somewhat unclear how individual states will handle the increase. State Medicaid agencies could pay physicians based on their self-attestation alone or in conjunction with any other provider enrollment requirements that currently exist in the state. Further, inclusion of a code does not require a state to pay for the service if it is not already covered under the state’s Medicaid program. All other state coverage and payment policy rules related to the services also remain in effect.
Timing of the pay increase also remains unclear. The statute requires that states make higher payments for services provided on or after Jan. 1, 2013, but for many physicians, the higher payment might be longer in coming despite being retroactive to the January deadline. States must submit a State Plan Amendment (SPA) to reflect the fee schedule rate increases by March 31, 2013, and CMS may then take up to 90 days to review and approve the SPA. Therefore, it could be six months or longer before eligible physicians and practitioners receive any of the payment increase.
States will receive an estimated $5.8 billion in 2013 and $6.1 billion in 2014 in federal funds to meet this two-year requirement, unless Congress acts to extend or fund the provision permanently. In response to an SHM suggestion on the potential to extend the increase, CMS will be collecting relevant data on the impact of the pay increase on Medicaid patients.
Even with the remaining uncertainty and timing issues, this is a change in payment policy that presents an important shift in the valuation of primary-care services, including some services provided by hospitalists. Medicaid services are notoriously undervalued, and this increase to providers will certainly have a positive impact on the accessibility of care for patients.
Josh Boswell is SHM’s interim senior manager of government relations.
Shaun Frost: Call for Transparency in Healthcare Performance Results to Impact Hospitalists
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Bipartisan Proposal to Repeal SGR Plan Likely to be Reintroduced
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
Society of Hospital Medicine Joins Fight to Delay Medicare Cuts that Reduce Pay for Hospitalists
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
Physician Value-Based Payment Initiative Would Change Medicare Reimbursement
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
Win Whitcomb: Hospital Readmissions Penalties Start Now
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
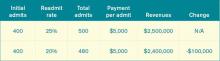
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
CMS Rule on Use of Electronic Health Records Gets Mixed Reviews
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
Hospitalists Play Integral Roles in HHS-Funded Innovation Projects
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
Established Performance Metrics Help CMS Expand Its Value-Based Purchasing Program

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.