User login
Combo extends PFS in previously treated MM

Photo courtesy of Janssen
Results of the phase 3 CASTOR trial suggest that adding daratumumab to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in patients with previously treated multiple myeloma (MM).
Compared to patients who received only bortezomib and dexamethasone, those who received daratumumab as well had a higher response rate and longer PFS, but they also had a higher incidence of grade 3/4 adverse events (AEs).
These results were recently published in NEJM. They were previously presented at the 2016 ASCO Annual Meeting. The CASTOR trial was funded by Janssen Research & Development.
The trial enrolled 498 patients with relapsed or relapsed and refractory MM. Patients were randomized to receive bortezomib (1.3 mg/m2) and dexamethasone (20 mg) alone (control arm) or in combination with daratumumab (16 mg/kg).
Baseline characteristics were well balanced between the treatment arms. Across both groups, the median patient age was 64 (range, 30 to 88), the median time since MM diagnosis was 3.8 years, and the patients had received a median of 2 (range, 1 to 10) previous lines of therapy.
Efficacy
The overall response rate was significantly higher in the daratumumab arm than the control arm—82.9% and 63.2%, respectively (P<0.001). The rate of complete response or better was higher in the daratumumab arm as well—19.2% and 9.0%, respectively (P=0.001).
After a median follow-up of 7.4 months, the median PFS was not reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio=0.39, P<0.001). The estimated 12-month PFS was 60.7% and 26.9%, respectively.
Overall survival was not reached in either treatment arm.
This trial was unblinded after meeting its primary endpoint of improved PFS in this interim analysis. Based on the recommendation of an independent data monitoring committee, patients in the control arm were offered the option to receive daratumumab following confirmed disease progression.
Safety
AEs occurred in 98.8% of patients in the daratumumab arm and 95.4% of patients in the control arm. Grade 3/4 AEs occurred in 76.1% and 62.4%, respectively.
There was a higher incidence of the following AEs in the daratumumab arm than the control arm—thrombocytopenia (58.8% vs 43.9%), neutropenia (17.7% vs 9.3%), lymphopenia (13.2% vs 3.8%), peripheral sensory neuropathy (47.3% vs 37.6%), bleeding events (7.0% vs 3.8%), and secondary primary cancers (2.5% vs 0.4%).
Infusion-related reactions associated with daratumumab were reported in 45.3% of patients. These reactions were mostly grade 1 or 2.
The percentage of patients who discontinued treatment because of at least 1 AE was similar between the daratumumab and control arms (7.4% and 9.3%, respectively). ![]()

Photo courtesy of Janssen
Results of the phase 3 CASTOR trial suggest that adding daratumumab to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in patients with previously treated multiple myeloma (MM).
Compared to patients who received only bortezomib and dexamethasone, those who received daratumumab as well had a higher response rate and longer PFS, but they also had a higher incidence of grade 3/4 adverse events (AEs).
These results were recently published in NEJM. They were previously presented at the 2016 ASCO Annual Meeting. The CASTOR trial was funded by Janssen Research & Development.
The trial enrolled 498 patients with relapsed or relapsed and refractory MM. Patients were randomized to receive bortezomib (1.3 mg/m2) and dexamethasone (20 mg) alone (control arm) or in combination with daratumumab (16 mg/kg).
Baseline characteristics were well balanced between the treatment arms. Across both groups, the median patient age was 64 (range, 30 to 88), the median time since MM diagnosis was 3.8 years, and the patients had received a median of 2 (range, 1 to 10) previous lines of therapy.
Efficacy
The overall response rate was significantly higher in the daratumumab arm than the control arm—82.9% and 63.2%, respectively (P<0.001). The rate of complete response or better was higher in the daratumumab arm as well—19.2% and 9.0%, respectively (P=0.001).
After a median follow-up of 7.4 months, the median PFS was not reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio=0.39, P<0.001). The estimated 12-month PFS was 60.7% and 26.9%, respectively.
Overall survival was not reached in either treatment arm.
This trial was unblinded after meeting its primary endpoint of improved PFS in this interim analysis. Based on the recommendation of an independent data monitoring committee, patients in the control arm were offered the option to receive daratumumab following confirmed disease progression.
Safety
AEs occurred in 98.8% of patients in the daratumumab arm and 95.4% of patients in the control arm. Grade 3/4 AEs occurred in 76.1% and 62.4%, respectively.
There was a higher incidence of the following AEs in the daratumumab arm than the control arm—thrombocytopenia (58.8% vs 43.9%), neutropenia (17.7% vs 9.3%), lymphopenia (13.2% vs 3.8%), peripheral sensory neuropathy (47.3% vs 37.6%), bleeding events (7.0% vs 3.8%), and secondary primary cancers (2.5% vs 0.4%).
Infusion-related reactions associated with daratumumab were reported in 45.3% of patients. These reactions were mostly grade 1 or 2.
The percentage of patients who discontinued treatment because of at least 1 AE was similar between the daratumumab and control arms (7.4% and 9.3%, respectively). ![]()

Photo courtesy of Janssen
Results of the phase 3 CASTOR trial suggest that adding daratumumab to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in patients with previously treated multiple myeloma (MM).
Compared to patients who received only bortezomib and dexamethasone, those who received daratumumab as well had a higher response rate and longer PFS, but they also had a higher incidence of grade 3/4 adverse events (AEs).
These results were recently published in NEJM. They were previously presented at the 2016 ASCO Annual Meeting. The CASTOR trial was funded by Janssen Research & Development.
The trial enrolled 498 patients with relapsed or relapsed and refractory MM. Patients were randomized to receive bortezomib (1.3 mg/m2) and dexamethasone (20 mg) alone (control arm) or in combination with daratumumab (16 mg/kg).
Baseline characteristics were well balanced between the treatment arms. Across both groups, the median patient age was 64 (range, 30 to 88), the median time since MM diagnosis was 3.8 years, and the patients had received a median of 2 (range, 1 to 10) previous lines of therapy.
Efficacy
The overall response rate was significantly higher in the daratumumab arm than the control arm—82.9% and 63.2%, respectively (P<0.001). The rate of complete response or better was higher in the daratumumab arm as well—19.2% and 9.0%, respectively (P=0.001).
After a median follow-up of 7.4 months, the median PFS was not reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio=0.39, P<0.001). The estimated 12-month PFS was 60.7% and 26.9%, respectively.
Overall survival was not reached in either treatment arm.
This trial was unblinded after meeting its primary endpoint of improved PFS in this interim analysis. Based on the recommendation of an independent data monitoring committee, patients in the control arm were offered the option to receive daratumumab following confirmed disease progression.
Safety
AEs occurred in 98.8% of patients in the daratumumab arm and 95.4% of patients in the control arm. Grade 3/4 AEs occurred in 76.1% and 62.4%, respectively.
There was a higher incidence of the following AEs in the daratumumab arm than the control arm—thrombocytopenia (58.8% vs 43.9%), neutropenia (17.7% vs 9.3%), lymphopenia (13.2% vs 3.8%), peripheral sensory neuropathy (47.3% vs 37.6%), bleeding events (7.0% vs 3.8%), and secondary primary cancers (2.5% vs 0.4%).
Infusion-related reactions associated with daratumumab were reported in 45.3% of patients. These reactions were mostly grade 1 or 2.
The percentage of patients who discontinued treatment because of at least 1 AE was similar between the daratumumab and control arms (7.4% and 9.3%, respectively). ![]()
CASTOR study shows daratumumab efficacy in myeloma
Daratumumab significantly improved survival when added to the current two-drug regimen for multiple myeloma, according to published data from a phase III study.
Patients treated with the anti-CD38 antibody in addition to the current standard treatment combination of bortezomib and dexamethasone had a 61% progression-free survival rate compared with a 27% rate seen in controls who received only bortezomib and dexamethasone.
The study results were presented initially at the annual meeting of the American Society of Hematology in 2015.
After an average follow-up of 7 months, 67 disease-progression events or deaths occurred in the daratumumab group, compared with 122 in the control group. Overall treatment response rates also were significantly higher in the daratumumab group compared with controls (83% vs. 63%), reported Antonio Palumbo, MD, of the University of Turin, Italy, and his associates in the CASTOR study.
The multicenter, randomized trial included 251 multiple myeloma patients in the daratumumab group 247 patients in the control group. Demographics were similar between the groups; the median patient age was 64 years.
Although more than 95% of patients in each group reported at least one adverse event, fewer than 10% of patients in each group discontinued treatment as a result. The most common adverse events associated with discontinuation were peripheral sensory neuropathy and pneumonia (N Engl J Med 2016;375:754-66).
The study was funded by Janssen Research and Development.
Daratumumab significantly improved survival when added to the current two-drug regimen for multiple myeloma, according to published data from a phase III study.
Patients treated with the anti-CD38 antibody in addition to the current standard treatment combination of bortezomib and dexamethasone had a 61% progression-free survival rate compared with a 27% rate seen in controls who received only bortezomib and dexamethasone.
The study results were presented initially at the annual meeting of the American Society of Hematology in 2015.
After an average follow-up of 7 months, 67 disease-progression events or deaths occurred in the daratumumab group, compared with 122 in the control group. Overall treatment response rates also were significantly higher in the daratumumab group compared with controls (83% vs. 63%), reported Antonio Palumbo, MD, of the University of Turin, Italy, and his associates in the CASTOR study.
The multicenter, randomized trial included 251 multiple myeloma patients in the daratumumab group 247 patients in the control group. Demographics were similar between the groups; the median patient age was 64 years.
Although more than 95% of patients in each group reported at least one adverse event, fewer than 10% of patients in each group discontinued treatment as a result. The most common adverse events associated with discontinuation were peripheral sensory neuropathy and pneumonia (N Engl J Med 2016;375:754-66).
The study was funded by Janssen Research and Development.
Daratumumab significantly improved survival when added to the current two-drug regimen for multiple myeloma, according to published data from a phase III study.
Patients treated with the anti-CD38 antibody in addition to the current standard treatment combination of bortezomib and dexamethasone had a 61% progression-free survival rate compared with a 27% rate seen in controls who received only bortezomib and dexamethasone.
The study results were presented initially at the annual meeting of the American Society of Hematology in 2015.
After an average follow-up of 7 months, 67 disease-progression events or deaths occurred in the daratumumab group, compared with 122 in the control group. Overall treatment response rates also were significantly higher in the daratumumab group compared with controls (83% vs. 63%), reported Antonio Palumbo, MD, of the University of Turin, Italy, and his associates in the CASTOR study.
The multicenter, randomized trial included 251 multiple myeloma patients in the daratumumab group 247 patients in the control group. Demographics were similar between the groups; the median patient age was 64 years.
Although more than 95% of patients in each group reported at least one adverse event, fewer than 10% of patients in each group discontinued treatment as a result. The most common adverse events associated with discontinuation were peripheral sensory neuropathy and pneumonia (N Engl J Med 2016;375:754-66).
The study was funded by Janssen Research and Development.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Treatment may allow HSCT without radiation, chemotherapy
A new therapy combining an anti-c-Kit monoclonal antibody with a CD47 blocker allowed hematopoietic stem cell engraftment in immunocompetent mice without the need for toxic preconditioning using radiation or chemotherapy, according to a report published in Science Translational Medicine.
Until now, hematopoietic stem cell transplantation has required rigorous conditioning regimens to clear out the host’s bone marrow, which can cause lifelong complications. So the procedure has been reserved for patients whose life-threatening disorders justified such toxicity. “Safer and more targeted conditioning protocols could both improve the safety of transplantation and extend the existing clinical utility of this powerful form of cell therapy,” said Akanksha Chhabra, PhD, of the department of blood and marrow transplantation, Stanford (Calif.) University, and her associates.
They assessed the new combined treatment in a series of laboratory and mouse studies. The opsonizing anti-c-Kit monoclonal antibodies induced robust depletion of functional hematopoietic stem cells in immunocompetent mice, which allowed donor stem cells to engraft in these hosts. Adding the T-cell–depleting CD47-antagonists further facilitated immune ablation of host stem cells and progenitor cells. Combined, the two agents eliminated more than 99% of host hematopoietic stem cells in the bone marrow and enabled strong engraftment of the donor stem cells, while avoiding radiation- and chemotherapy-related adverse effects.
The main toxicities that occurred in treated mice were, as expected, reductions in hematologic parameters, especially red blood cell indices. This may be related to a factor in mouse physiology that is not present in humans. But if such toxicities do develop in human subjects, they can be mitigated by careful monitoring and occasional supportive transfusions, Dr. Chhabra and her associates said (Sci Transl Med. 2016;8:351ra105).
These two types of antibodies are already being investigated separately in early-phase clinical trials. If the combined treatment proves effective and safe in humans – a question that awaits further clinical studies – hematopoietic stem cell transplantation might be extended to nonmalignant conditions such as inherited immunodeficiency, inborn errors of metabolism, and hemoglobinopathies. It might also be adapted for use in solid-organ transplants, the researchers added.
This work was supported by the Virginia and D.K. Ludwig Fund for Cancer Research and several other nonprofit organizations, the California Institute for Regenerative Medicine, and the National Institutes of Health. Dr. Chhabra is a coinventor on a patent described in this article, and her associates are cofounders of Forty Seven, the company that licensed the technology for radiation- and chemotherapy-free stem-cell transplantation. Two associates also serve as advisors for Alexo Therapeutics, which develops CD47-based treatments.
A new therapy combining an anti-c-Kit monoclonal antibody with a CD47 blocker allowed hematopoietic stem cell engraftment in immunocompetent mice without the need for toxic preconditioning using radiation or chemotherapy, according to a report published in Science Translational Medicine.
Until now, hematopoietic stem cell transplantation has required rigorous conditioning regimens to clear out the host’s bone marrow, which can cause lifelong complications. So the procedure has been reserved for patients whose life-threatening disorders justified such toxicity. “Safer and more targeted conditioning protocols could both improve the safety of transplantation and extend the existing clinical utility of this powerful form of cell therapy,” said Akanksha Chhabra, PhD, of the department of blood and marrow transplantation, Stanford (Calif.) University, and her associates.
They assessed the new combined treatment in a series of laboratory and mouse studies. The opsonizing anti-c-Kit monoclonal antibodies induced robust depletion of functional hematopoietic stem cells in immunocompetent mice, which allowed donor stem cells to engraft in these hosts. Adding the T-cell–depleting CD47-antagonists further facilitated immune ablation of host stem cells and progenitor cells. Combined, the two agents eliminated more than 99% of host hematopoietic stem cells in the bone marrow and enabled strong engraftment of the donor stem cells, while avoiding radiation- and chemotherapy-related adverse effects.
The main toxicities that occurred in treated mice were, as expected, reductions in hematologic parameters, especially red blood cell indices. This may be related to a factor in mouse physiology that is not present in humans. But if such toxicities do develop in human subjects, they can be mitigated by careful monitoring and occasional supportive transfusions, Dr. Chhabra and her associates said (Sci Transl Med. 2016;8:351ra105).
These two types of antibodies are already being investigated separately in early-phase clinical trials. If the combined treatment proves effective and safe in humans – a question that awaits further clinical studies – hematopoietic stem cell transplantation might be extended to nonmalignant conditions such as inherited immunodeficiency, inborn errors of metabolism, and hemoglobinopathies. It might also be adapted for use in solid-organ transplants, the researchers added.
This work was supported by the Virginia and D.K. Ludwig Fund for Cancer Research and several other nonprofit organizations, the California Institute for Regenerative Medicine, and the National Institutes of Health. Dr. Chhabra is a coinventor on a patent described in this article, and her associates are cofounders of Forty Seven, the company that licensed the technology for radiation- and chemotherapy-free stem-cell transplantation. Two associates also serve as advisors for Alexo Therapeutics, which develops CD47-based treatments.
A new therapy combining an anti-c-Kit monoclonal antibody with a CD47 blocker allowed hematopoietic stem cell engraftment in immunocompetent mice without the need for toxic preconditioning using radiation or chemotherapy, according to a report published in Science Translational Medicine.
Until now, hematopoietic stem cell transplantation has required rigorous conditioning regimens to clear out the host’s bone marrow, which can cause lifelong complications. So the procedure has been reserved for patients whose life-threatening disorders justified such toxicity. “Safer and more targeted conditioning protocols could both improve the safety of transplantation and extend the existing clinical utility of this powerful form of cell therapy,” said Akanksha Chhabra, PhD, of the department of blood and marrow transplantation, Stanford (Calif.) University, and her associates.
They assessed the new combined treatment in a series of laboratory and mouse studies. The opsonizing anti-c-Kit monoclonal antibodies induced robust depletion of functional hematopoietic stem cells in immunocompetent mice, which allowed donor stem cells to engraft in these hosts. Adding the T-cell–depleting CD47-antagonists further facilitated immune ablation of host stem cells and progenitor cells. Combined, the two agents eliminated more than 99% of host hematopoietic stem cells in the bone marrow and enabled strong engraftment of the donor stem cells, while avoiding radiation- and chemotherapy-related adverse effects.
The main toxicities that occurred in treated mice were, as expected, reductions in hematologic parameters, especially red blood cell indices. This may be related to a factor in mouse physiology that is not present in humans. But if such toxicities do develop in human subjects, they can be mitigated by careful monitoring and occasional supportive transfusions, Dr. Chhabra and her associates said (Sci Transl Med. 2016;8:351ra105).
These two types of antibodies are already being investigated separately in early-phase clinical trials. If the combined treatment proves effective and safe in humans – a question that awaits further clinical studies – hematopoietic stem cell transplantation might be extended to nonmalignant conditions such as inherited immunodeficiency, inborn errors of metabolism, and hemoglobinopathies. It might also be adapted for use in solid-organ transplants, the researchers added.
This work was supported by the Virginia and D.K. Ludwig Fund for Cancer Research and several other nonprofit organizations, the California Institute for Regenerative Medicine, and the National Institutes of Health. Dr. Chhabra is a coinventor on a patent described in this article, and her associates are cofounders of Forty Seven, the company that licensed the technology for radiation- and chemotherapy-free stem-cell transplantation. Two associates also serve as advisors for Alexo Therapeutics, which develops CD47-based treatments.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: A new treatment allowed hematopoietic stem cell engraftment in immunocompetent mice without the need for toxic preconditioning using radiation or chemotherapy.
Major finding: The combined therapy eliminated more than 99% of host hematopoietic stem cells.
Data source: A series of laboratory and mouse studies of combined treatment with anti-c-Kit monoclonal antibodies plus CD47 blockers.
Disclosures: This work was supported by the Virginia and D.K. Ludwig Fund for Cancer Research and several other nonprofit organizations, the California Institute for Regenerative Medicine, and the National Institutes of Health. Dr. Chhabra is a coinventor on a patent described in this article, and her associates are cofounders of Forty Seven, the company that licensed the technology for radiation- and chemotherapy-free stem-cell transplantation. Two associates also serve as advisors for Alexo Therapeutics, which develops CD47-based treatments.
Thymidine phosphorylase increases myeloma-induced bone lesions
Myeloma-induced osteolytic bone lesions were reduced by suppressing expression of thymidine phosphorylase (TP), according to Huan Liu of the University of Texas MD Anderson Cancer Center in Houston and associates.
In osteoblast progenitors, methylation of alpha-1/runt-related transcription factor 2 (RUNX2) and osterix was upregulated by TP, resulting in decreased bone formation. TP also upregulated methylation of interferon regulatory factor 8 (IRF8) and enhanced nuclear factor of activated T cells, cytoplasmic 1 protein (NFATc1), which increased bone resorption. Thymidine was catalyzed into thymine and 2-deoxy-d-ribose, which bound to integrins alphavbeta3 and alpha5beta1, activated PI3K/Akt signaling, and increased DNA methyltransferase 3A (DNMT3A) expression, the investigators found.
In an experiment, myeloma was established in severe combined immunodeficient mice, and the mice were injected with ARP-1 cells, which produce high levels of TP. The mice were then treated with 7-deazaxanthine or tipiracil hydrochloride, which reduced ARP-1-induced bone lesions, DNMT3A expression, and 2DDR levels in the serum of tumor-bearing mice.
“This model could facilitate the translation of these inhibitors into human studies of myeloma bone disease. Because TP is often expressed by other malignancies including breast, prostate, and lung cancer, these findings may also have broader implications for the genesis of bone metastasis caused by these and other tumors,” the investigators concluded.
Find the full study in Science Translational Medicine (doi:10.1126/scitranslmed.aad8949)
Myeloma-induced osteolytic bone lesions were reduced by suppressing expression of thymidine phosphorylase (TP), according to Huan Liu of the University of Texas MD Anderson Cancer Center in Houston and associates.
In osteoblast progenitors, methylation of alpha-1/runt-related transcription factor 2 (RUNX2) and osterix was upregulated by TP, resulting in decreased bone formation. TP also upregulated methylation of interferon regulatory factor 8 (IRF8) and enhanced nuclear factor of activated T cells, cytoplasmic 1 protein (NFATc1), which increased bone resorption. Thymidine was catalyzed into thymine and 2-deoxy-d-ribose, which bound to integrins alphavbeta3 and alpha5beta1, activated PI3K/Akt signaling, and increased DNA methyltransferase 3A (DNMT3A) expression, the investigators found.
In an experiment, myeloma was established in severe combined immunodeficient mice, and the mice were injected with ARP-1 cells, which produce high levels of TP. The mice were then treated with 7-deazaxanthine or tipiracil hydrochloride, which reduced ARP-1-induced bone lesions, DNMT3A expression, and 2DDR levels in the serum of tumor-bearing mice.
“This model could facilitate the translation of these inhibitors into human studies of myeloma bone disease. Because TP is often expressed by other malignancies including breast, prostate, and lung cancer, these findings may also have broader implications for the genesis of bone metastasis caused by these and other tumors,” the investigators concluded.
Find the full study in Science Translational Medicine (doi:10.1126/scitranslmed.aad8949)
Myeloma-induced osteolytic bone lesions were reduced by suppressing expression of thymidine phosphorylase (TP), according to Huan Liu of the University of Texas MD Anderson Cancer Center in Houston and associates.
In osteoblast progenitors, methylation of alpha-1/runt-related transcription factor 2 (RUNX2) and osterix was upregulated by TP, resulting in decreased bone formation. TP also upregulated methylation of interferon regulatory factor 8 (IRF8) and enhanced nuclear factor of activated T cells, cytoplasmic 1 protein (NFATc1), which increased bone resorption. Thymidine was catalyzed into thymine and 2-deoxy-d-ribose, which bound to integrins alphavbeta3 and alpha5beta1, activated PI3K/Akt signaling, and increased DNA methyltransferase 3A (DNMT3A) expression, the investigators found.
In an experiment, myeloma was established in severe combined immunodeficient mice, and the mice were injected with ARP-1 cells, which produce high levels of TP. The mice were then treated with 7-deazaxanthine or tipiracil hydrochloride, which reduced ARP-1-induced bone lesions, DNMT3A expression, and 2DDR levels in the serum of tumor-bearing mice.
“This model could facilitate the translation of these inhibitors into human studies of myeloma bone disease. Because TP is often expressed by other malignancies including breast, prostate, and lung cancer, these findings may also have broader implications for the genesis of bone metastasis caused by these and other tumors,” the investigators concluded.
Find the full study in Science Translational Medicine (doi:10.1126/scitranslmed.aad8949)
FROM SCIENCE TRANSLATIONAL MEDICINE
Can Serum Free Light Chains Be Used for the Early Diagnosis of Monoclonal Immunoglobulin-Secreting B-Cell and Plasma-Cell Diseases? (FULL)
Patients who are undergoing multiple myeloma screening with serum protein electrophoresis and immunofixation, especially those with renal failure, also should receive serum free light chain testing to increase specificity and reduce false-negatives.
Multiple myeloma (MM) is a devastating disease with an estimated 26,850 new cases in 2015 according to Surveillance, Epidemiology, and End Results data and no definitive chemotherapeutic cure.1 In 97% of cases, MM is defined by monoclonal hypergammaglobulinemia, in which a malignant plasma cell clone secretes a monoclonal globulin; the remaining cases are nonsecretors.2 Each pathologically produced clonal globulin contains 2 heavy chains attached by disulfide linkage and 2 light chains. Unchecked plasma cell production is what later causes the symptoms of renal failure, bone destruction, and anemia.
The rate of MM is disproportionately high in the veteran population, and the VA health care system provides care for many of these patients. The higher rate is likely secondary to the predominantly male population, which has higher MM rates, and has been linked to Agent Orange exposure in Vietnam. As MM is not easy to diagnose, any algorithm or testing method would be of great benefit to this population.
The gold standard for MM detection remains serum protein electrophoresis (SPEP) with immunofixation (IFE), but other detection methods have been emerging. The method of serum free light chain (SFLC) assay has become more readily available, and its incorporation into diagnostic guidelines has become more apparent but is not universal.3
In the case series reported in this article, SPEP/IFE and SFLC assays were used to test 207 patients from the VA New York Harbor Healthcare System (VANYHHS). All these patients had a clinical context for MM testing.
Methods
In this retrospective study, the authors reviewed the charts of VANYHHS patients who were being treated for conditions that prompted SPEP/IFE and λ and κ SFLC analysis between December 2013 and March 2014. The study was exempt from institutional review board approval.
The SPEP/IFE analysis was performed with an automated electrophoresis machine (Sebia Electrophoresis), and the SFLC analysis was performed with an automated SFLC assay (Freelite). Sensitivity, specificity, and positive and negative predictive values were calculated using SPEP/IFE as the gold standard and SFLC κ-to-λ ratio asthe test method. Patients with a positive κ-to-λ ratio but negative SPEP were considered false-positives. These patients’ SFLC analyses were further analyzed in an effort to evaluate use of the κ-to-λ ratio as an early tumor marker.
The κ reference range used was 3.3 to 19.4 mg/L, and the λ reference range used was 5.7 to 26.3 mg/L.4 The traditional reference range for the κ-to-λ ratio is 0.26 to 1.65.5
Results
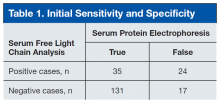
Of the 207 patients in this study, 205 were men. Mean age was 69 years (range, 28-97 years). Mean serum urea nitrogen level was 8.75 mmol/L (range, 2.86-38.21 mmol/L), and mean creatinine level was 140.59 μmol/L (range, 44.21-1503.14 μmol/L). Mean κ was 49.82 mg/L (range, 4.6-700.96 mg/L), and mean λ was 54.27 mg/L (range, 3-1,750 mg/L). Table 1 compares the SPEP and SFLC data. Sensitivity was 67%, specificity was 85%, positive predictive value was 58%, and negative predictive value was 89%. Concordance of the 2 methods was 80%. The false-positive group was followed up 16 months later to check for diagnosis of disease. Two of the 24 patients in this quadrant were later diagnosed with MM (Table 1).
One of the patients with MM was an 82-year-old African American man with a history of hypertension, diabetes, and prostate cancer (Gleason 4 + 4 = 8/10). He presented to VANYHHS after a fall in which he sustained a pathologic fracture of the left acromion. Recurrent prostate cancer was initially suspected, and nuclear bone scintigraphy revealed increased uptake in the left shoulder and the posterior ninth rib. Results of computed tomography-guided biopsy showed the rib lesion packed with plasma cells and consistent with MM. Immunohistochemical analysis was positive for CD138 and κ in the malignant plasma cells. Initial SPEP performed before the biopsy showed an acute phase reaction with hypogammaglobulinemia, and SPEP after the biopsy showed an increased α-2 band but no monoclonal gammaglobulinopathy. The initial κ of 42.18 mg/L (κ-to-λ ratio, 4.01) was up to 67.53 mg/L 4 months later.
The other patient with MM was a 91-year-old man who had coronary artery disease after undergoing coronary artery bypass grafting in 1993, sick sinus syndrome after pacemaker implantation, hypertension, and anemia. He initially presented to the geriatrics clinic with polyneuropathy, which prompted SPEP and SFLC analysis. SPEP results showed a normal electrophoretic pattern, but κ increased to 47.52 mg/L (κ-to-λ ratio, 2.63). The decision was made to monitor the patient in the hematology clinic. Subsequent κ chain analysis revealed an increase to 59.50 mg/L. A repeat SPEP, performed 1 year after the first SPEP, revealed monoclonal immunoglobulin A on IFE.
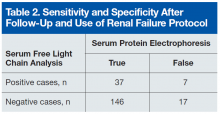
Of the 24 patients with false-positive results, 16 had moderate-to-severe kidney disease (stage IIIa-IV).6All patients in this quadrant were men; their mean age was 75 years, and their mean creatinine level was 182.15 μmol/L. Further laboratory data are listed in Table 2.
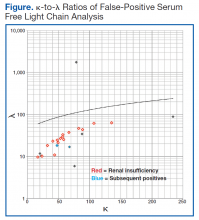
The patient whose biopsy results led to an MM diagnosis and the patient whose IFE led to a gammopathy diagnosis both maintained a glomerular filtration rate within normal limits. The Figure shows the κ-to-λ ratios of this quadrant logarithmically.
Discussion
Use of SFLC analysis as a supplement to serum and urine protein electrophoresis has been investigated and accepted in the recent literature.3,4,7,8 Use of light chains as a method of earlier or alternative detection has not been proved. In the present study of 207 patients, comparisons showed that more traditional MM detection methods and SFLC analysis are largely concordant. The 2 patients with MM and negative electrophoretic patterns provided a clear indication of the potential benefit of SFLC analysis in the diagnosis of secretory and nonsecretory myeloma.
In 2014, Kim and colleagues compared 2 SFLC assays (Freelite, N Latex) to each other and to SPEP in a 120-patient population.9 The Freelite results in their study correlated closely with VA population findings (κ-to-λ ratio sensitivity and specificity: 72.2% and 93.6%, respectively). N Latex, the newer SFLC assay, had lower sensitivity (64.6%) and higher specificity (100%). With application of the extended reference range (0.37-3.1) proposed by Hutchison and colleagues for use in patients with renal failure, SFLC becomes a more statistically powerful tool.5
The patients who tested false-positive had higher mean creatinine levels, and 16 had renal insufficiency. The 2 false-positive patients were later found to have clinical myeloma and were within the normal range of renal function. Of the 16 patients with an abnormal κ-to-λ ratio and renal failure, 15 would be within the revised normal reference range, leaving 9 false-positives, 2 of whom eventually were found to have disease. With the application of the extended light chain range (as per Hutchison) for those patients with renal failure, 15 of the original 24 false-positives became true-negatives. Two of the false-positives become true-positives after they were subsequently diagnosed. Therefore, SFLC analysis detected disease in 22% of the revised false-positives when SPEP could not.
Table 2 lists the revised data after follow-up and renal failure correction. The strongest aspect of SFLC analysis remains its 95% specificity; its 69% sensitivity remains relatively constant. The test’s positive predictive value is 84%, and its negative predictive value is 90%. In veteran and other at-risk populations, SFLC analysis proves to be a very powerful tool on its own.
Conclusion
Both patient cases described in this article demonstrate the usefulness of SFLC analysis as an adjunct to SPEP. The authors propose SFLC testing for all patients who are undergoing MM screening with SPEP/IFE. In patients with renal failure, the expanded reference range seems to reduce erroneous false-positive results. Patients who have abnormal ratios should be followed up in clinic with repeat MM testing. It seems clear that, at the very least, SFLC analysis is a necessary adjunct to SPEP testing. However, SFLC stands on its own merit as well.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
1. National Cancer Institute, Surveillance, Epidemiology, and End Results (SEER) Program. SEER website. http://seer.cancer.gov/statfacts/html/mulmy.html. Accessed July 11, 2016.
2. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33.
3. Dimopoulos M, Kyle R, Fermand JP, et al; International Myeloma Workshop Consensus Panel 3. Consensus recommendations for standard investigative workup: report of the International Myeloma Workshop Consensus Panel 3. Blood. 2011;117(18):4701-4705.
4. Katzmann JA, Clark RJ, Abraham RS, et al. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: relative sensitivity for detection of monoclonal light chains. Clin Chem. 2002;48(9):1437-1444.
5. Hutchison CA, Plant T, Drayson M, et al. Serum free light chain measurement
aids the diagnosis of myeloma in patients with severe renal failure.
BMC Nephrol. 2008;9:11.
6. Levey AS, Stevens LA, Schmid CH, et al; CKD-EPI (Chronic Kidney Disease
Epidemiology Collaboration). A new equation to estimate glomerular filtration
rate. Ann Intern Med. 2009;150(9):604-612.
7. McTaggart MP, Lindsay J, Kearney EM. Replacing urine protein electrophoresis
with serum free light chain analysis as a first-line test for detecting plasma
cell disorders offers increased diagnostic accuracy and potential health benefit
to patients. Am J Clin Pathol. 2013;140(6):890-897.
8. Abadie JM, Bankson DD. Assessment of serum free light chain assays for
plasma cell disorder screening in a Veterans Affairs population. Ann Clin Lab
Sci. 2006;36(2):157-162.
9. Kim HS, Kim HS, Shin KS, et al. Clinical comparisons of two free light chain
assays to immunofixation electrophoresis for detecting monoclonal gammopathy.
Biomed Res Int. 2014;2014:647238.
Note: Page numbers differ between the print issue and digital edition.
Patients who are undergoing multiple myeloma screening with serum protein electrophoresis and immunofixation, especially those with renal failure, also should receive serum free light chain testing to increase specificity and reduce false-negatives.
Multiple myeloma (MM) is a devastating disease with an estimated 26,850 new cases in 2015 according to Surveillance, Epidemiology, and End Results data and no definitive chemotherapeutic cure.1 In 97% of cases, MM is defined by monoclonal hypergammaglobulinemia, in which a malignant plasma cell clone secretes a monoclonal globulin; the remaining cases are nonsecretors.2 Each pathologically produced clonal globulin contains 2 heavy chains attached by disulfide linkage and 2 light chains. Unchecked plasma cell production is what later causes the symptoms of renal failure, bone destruction, and anemia.
The rate of MM is disproportionately high in the veteran population, and the VA health care system provides care for many of these patients. The higher rate is likely secondary to the predominantly male population, which has higher MM rates, and has been linked to Agent Orange exposure in Vietnam. As MM is not easy to diagnose, any algorithm or testing method would be of great benefit to this population.
The gold standard for MM detection remains serum protein electrophoresis (SPEP) with immunofixation (IFE), but other detection methods have been emerging. The method of serum free light chain (SFLC) assay has become more readily available, and its incorporation into diagnostic guidelines has become more apparent but is not universal.3
In the case series reported in this article, SPEP/IFE and SFLC assays were used to test 207 patients from the VA New York Harbor Healthcare System (VANYHHS). All these patients had a clinical context for MM testing.
Methods
In this retrospective study, the authors reviewed the charts of VANYHHS patients who were being treated for conditions that prompted SPEP/IFE and λ and κ SFLC analysis between December 2013 and March 2014. The study was exempt from institutional review board approval.
The SPEP/IFE analysis was performed with an automated electrophoresis machine (Sebia Electrophoresis), and the SFLC analysis was performed with an automated SFLC assay (Freelite). Sensitivity, specificity, and positive and negative predictive values were calculated using SPEP/IFE as the gold standard and SFLC κ-to-λ ratio asthe test method. Patients with a positive κ-to-λ ratio but negative SPEP were considered false-positives. These patients’ SFLC analyses were further analyzed in an effort to evaluate use of the κ-to-λ ratio as an early tumor marker.
The κ reference range used was 3.3 to 19.4 mg/L, and the λ reference range used was 5.7 to 26.3 mg/L.4 The traditional reference range for the κ-to-λ ratio is 0.26 to 1.65.5
Results
Of the 207 patients in this study, 205 were men. Mean age was 69 years (range, 28-97 years). Mean serum urea nitrogen level was 8.75 mmol/L (range, 2.86-38.21 mmol/L), and mean creatinine level was 140.59 μmol/L (range, 44.21-1503.14 μmol/L). Mean κ was 49.82 mg/L (range, 4.6-700.96 mg/L), and mean λ was 54.27 mg/L (range, 3-1,750 mg/L). Table 1 compares the SPEP and SFLC data. Sensitivity was 67%, specificity was 85%, positive predictive value was 58%, and negative predictive value was 89%. Concordance of the 2 methods was 80%. The false-positive group was followed up 16 months later to check for diagnosis of disease. Two of the 24 patients in this quadrant were later diagnosed with MM (Table 1).
One of the patients with MM was an 82-year-old African American man with a history of hypertension, diabetes, and prostate cancer (Gleason 4 + 4 = 8/10). He presented to VANYHHS after a fall in which he sustained a pathologic fracture of the left acromion. Recurrent prostate cancer was initially suspected, and nuclear bone scintigraphy revealed increased uptake in the left shoulder and the posterior ninth rib. Results of computed tomography-guided biopsy showed the rib lesion packed with plasma cells and consistent with MM. Immunohistochemical analysis was positive for CD138 and κ in the malignant plasma cells. Initial SPEP performed before the biopsy showed an acute phase reaction with hypogammaglobulinemia, and SPEP after the biopsy showed an increased α-2 band but no monoclonal gammaglobulinopathy. The initial κ of 42.18 mg/L (κ-to-λ ratio, 4.01) was up to 67.53 mg/L 4 months later.
The other patient with MM was a 91-year-old man who had coronary artery disease after undergoing coronary artery bypass grafting in 1993, sick sinus syndrome after pacemaker implantation, hypertension, and anemia. He initially presented to the geriatrics clinic with polyneuropathy, which prompted SPEP and SFLC analysis. SPEP results showed a normal electrophoretic pattern, but κ increased to 47.52 mg/L (κ-to-λ ratio, 2.63). The decision was made to monitor the patient in the hematology clinic. Subsequent κ chain analysis revealed an increase to 59.50 mg/L. A repeat SPEP, performed 1 year after the first SPEP, revealed monoclonal immunoglobulin A on IFE.
Of the 24 patients with false-positive results, 16 had moderate-to-severe kidney disease (stage IIIa-IV).6All patients in this quadrant were men; their mean age was 75 years, and their mean creatinine level was 182.15 μmol/L. Further laboratory data are listed in Table 2.
The patient whose biopsy results led to an MM diagnosis and the patient whose IFE led to a gammopathy diagnosis both maintained a glomerular filtration rate within normal limits. The Figure shows the κ-to-λ ratios of this quadrant logarithmically.
Discussion
Use of SFLC analysis as a supplement to serum and urine protein electrophoresis has been investigated and accepted in the recent literature.3,4,7,8 Use of light chains as a method of earlier or alternative detection has not been proved. In the present study of 207 patients, comparisons showed that more traditional MM detection methods and SFLC analysis are largely concordant. The 2 patients with MM and negative electrophoretic patterns provided a clear indication of the potential benefit of SFLC analysis in the diagnosis of secretory and nonsecretory myeloma.
In 2014, Kim and colleagues compared 2 SFLC assays (Freelite, N Latex) to each other and to SPEP in a 120-patient population.9 The Freelite results in their study correlated closely with VA population findings (κ-to-λ ratio sensitivity and specificity: 72.2% and 93.6%, respectively). N Latex, the newer SFLC assay, had lower sensitivity (64.6%) and higher specificity (100%). With application of the extended reference range (0.37-3.1) proposed by Hutchison and colleagues for use in patients with renal failure, SFLC becomes a more statistically powerful tool.5
The patients who tested false-positive had higher mean creatinine levels, and 16 had renal insufficiency. The 2 false-positive patients were later found to have clinical myeloma and were within the normal range of renal function. Of the 16 patients with an abnormal κ-to-λ ratio and renal failure, 15 would be within the revised normal reference range, leaving 9 false-positives, 2 of whom eventually were found to have disease. With the application of the extended light chain range (as per Hutchison) for those patients with renal failure, 15 of the original 24 false-positives became true-negatives. Two of the false-positives become true-positives after they were subsequently diagnosed. Therefore, SFLC analysis detected disease in 22% of the revised false-positives when SPEP could not.
Table 2 lists the revised data after follow-up and renal failure correction. The strongest aspect of SFLC analysis remains its 95% specificity; its 69% sensitivity remains relatively constant. The test’s positive predictive value is 84%, and its negative predictive value is 90%. In veteran and other at-risk populations, SFLC analysis proves to be a very powerful tool on its own.
Conclusion
Both patient cases described in this article demonstrate the usefulness of SFLC analysis as an adjunct to SPEP. The authors propose SFLC testing for all patients who are undergoing MM screening with SPEP/IFE. In patients with renal failure, the expanded reference range seems to reduce erroneous false-positive results. Patients who have abnormal ratios should be followed up in clinic with repeat MM testing. It seems clear that, at the very least, SFLC analysis is a necessary adjunct to SPEP testing. However, SFLC stands on its own merit as well.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
Patients who are undergoing multiple myeloma screening with serum protein electrophoresis and immunofixation, especially those with renal failure, also should receive serum free light chain testing to increase specificity and reduce false-negatives.
Multiple myeloma (MM) is a devastating disease with an estimated 26,850 new cases in 2015 according to Surveillance, Epidemiology, and End Results data and no definitive chemotherapeutic cure.1 In 97% of cases, MM is defined by monoclonal hypergammaglobulinemia, in which a malignant plasma cell clone secretes a monoclonal globulin; the remaining cases are nonsecretors.2 Each pathologically produced clonal globulin contains 2 heavy chains attached by disulfide linkage and 2 light chains. Unchecked plasma cell production is what later causes the symptoms of renal failure, bone destruction, and anemia.
The rate of MM is disproportionately high in the veteran population, and the VA health care system provides care for many of these patients. The higher rate is likely secondary to the predominantly male population, which has higher MM rates, and has been linked to Agent Orange exposure in Vietnam. As MM is not easy to diagnose, any algorithm or testing method would be of great benefit to this population.
The gold standard for MM detection remains serum protein electrophoresis (SPEP) with immunofixation (IFE), but other detection methods have been emerging. The method of serum free light chain (SFLC) assay has become more readily available, and its incorporation into diagnostic guidelines has become more apparent but is not universal.3
In the case series reported in this article, SPEP/IFE and SFLC assays were used to test 207 patients from the VA New York Harbor Healthcare System (VANYHHS). All these patients had a clinical context for MM testing.
Methods
In this retrospective study, the authors reviewed the charts of VANYHHS patients who were being treated for conditions that prompted SPEP/IFE and λ and κ SFLC analysis between December 2013 and March 2014. The study was exempt from institutional review board approval.
The SPEP/IFE analysis was performed with an automated electrophoresis machine (Sebia Electrophoresis), and the SFLC analysis was performed with an automated SFLC assay (Freelite). Sensitivity, specificity, and positive and negative predictive values were calculated using SPEP/IFE as the gold standard and SFLC κ-to-λ ratio asthe test method. Patients with a positive κ-to-λ ratio but negative SPEP were considered false-positives. These patients’ SFLC analyses were further analyzed in an effort to evaluate use of the κ-to-λ ratio as an early tumor marker.
The κ reference range used was 3.3 to 19.4 mg/L, and the λ reference range used was 5.7 to 26.3 mg/L.4 The traditional reference range for the κ-to-λ ratio is 0.26 to 1.65.5
Results
Of the 207 patients in this study, 205 were men. Mean age was 69 years (range, 28-97 years). Mean serum urea nitrogen level was 8.75 mmol/L (range, 2.86-38.21 mmol/L), and mean creatinine level was 140.59 μmol/L (range, 44.21-1503.14 μmol/L). Mean κ was 49.82 mg/L (range, 4.6-700.96 mg/L), and mean λ was 54.27 mg/L (range, 3-1,750 mg/L). Table 1 compares the SPEP and SFLC data. Sensitivity was 67%, specificity was 85%, positive predictive value was 58%, and negative predictive value was 89%. Concordance of the 2 methods was 80%. The false-positive group was followed up 16 months later to check for diagnosis of disease. Two of the 24 patients in this quadrant were later diagnosed with MM (Table 1).
One of the patients with MM was an 82-year-old African American man with a history of hypertension, diabetes, and prostate cancer (Gleason 4 + 4 = 8/10). He presented to VANYHHS after a fall in which he sustained a pathologic fracture of the left acromion. Recurrent prostate cancer was initially suspected, and nuclear bone scintigraphy revealed increased uptake in the left shoulder and the posterior ninth rib. Results of computed tomography-guided biopsy showed the rib lesion packed with plasma cells and consistent with MM. Immunohistochemical analysis was positive for CD138 and κ in the malignant plasma cells. Initial SPEP performed before the biopsy showed an acute phase reaction with hypogammaglobulinemia, and SPEP after the biopsy showed an increased α-2 band but no monoclonal gammaglobulinopathy. The initial κ of 42.18 mg/L (κ-to-λ ratio, 4.01) was up to 67.53 mg/L 4 months later.
The other patient with MM was a 91-year-old man who had coronary artery disease after undergoing coronary artery bypass grafting in 1993, sick sinus syndrome after pacemaker implantation, hypertension, and anemia. He initially presented to the geriatrics clinic with polyneuropathy, which prompted SPEP and SFLC analysis. SPEP results showed a normal electrophoretic pattern, but κ increased to 47.52 mg/L (κ-to-λ ratio, 2.63). The decision was made to monitor the patient in the hematology clinic. Subsequent κ chain analysis revealed an increase to 59.50 mg/L. A repeat SPEP, performed 1 year after the first SPEP, revealed monoclonal immunoglobulin A on IFE.
Of the 24 patients with false-positive results, 16 had moderate-to-severe kidney disease (stage IIIa-IV).6All patients in this quadrant were men; their mean age was 75 years, and their mean creatinine level was 182.15 μmol/L. Further laboratory data are listed in Table 2.
The patient whose biopsy results led to an MM diagnosis and the patient whose IFE led to a gammopathy diagnosis both maintained a glomerular filtration rate within normal limits. The Figure shows the κ-to-λ ratios of this quadrant logarithmically.
Discussion
Use of SFLC analysis as a supplement to serum and urine protein electrophoresis has been investigated and accepted in the recent literature.3,4,7,8 Use of light chains as a method of earlier or alternative detection has not been proved. In the present study of 207 patients, comparisons showed that more traditional MM detection methods and SFLC analysis are largely concordant. The 2 patients with MM and negative electrophoretic patterns provided a clear indication of the potential benefit of SFLC analysis in the diagnosis of secretory and nonsecretory myeloma.
In 2014, Kim and colleagues compared 2 SFLC assays (Freelite, N Latex) to each other and to SPEP in a 120-patient population.9 The Freelite results in their study correlated closely with VA population findings (κ-to-λ ratio sensitivity and specificity: 72.2% and 93.6%, respectively). N Latex, the newer SFLC assay, had lower sensitivity (64.6%) and higher specificity (100%). With application of the extended reference range (0.37-3.1) proposed by Hutchison and colleagues for use in patients with renal failure, SFLC becomes a more statistically powerful tool.5
The patients who tested false-positive had higher mean creatinine levels, and 16 had renal insufficiency. The 2 false-positive patients were later found to have clinical myeloma and were within the normal range of renal function. Of the 16 patients with an abnormal κ-to-λ ratio and renal failure, 15 would be within the revised normal reference range, leaving 9 false-positives, 2 of whom eventually were found to have disease. With the application of the extended light chain range (as per Hutchison) for those patients with renal failure, 15 of the original 24 false-positives became true-negatives. Two of the false-positives become true-positives after they were subsequently diagnosed. Therefore, SFLC analysis detected disease in 22% of the revised false-positives when SPEP could not.
Table 2 lists the revised data after follow-up and renal failure correction. The strongest aspect of SFLC analysis remains its 95% specificity; its 69% sensitivity remains relatively constant. The test’s positive predictive value is 84%, and its negative predictive value is 90%. In veteran and other at-risk populations, SFLC analysis proves to be a very powerful tool on its own.
Conclusion
Both patient cases described in this article demonstrate the usefulness of SFLC analysis as an adjunct to SPEP. The authors propose SFLC testing for all patients who are undergoing MM screening with SPEP/IFE. In patients with renal failure, the expanded reference range seems to reduce erroneous false-positive results. Patients who have abnormal ratios should be followed up in clinic with repeat MM testing. It seems clear that, at the very least, SFLC analysis is a necessary adjunct to SPEP testing. However, SFLC stands on its own merit as well.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to read the digital edition.
1. National Cancer Institute, Surveillance, Epidemiology, and End Results (SEER) Program. SEER website. http://seer.cancer.gov/statfacts/html/mulmy.html. Accessed July 11, 2016.
2. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33.
3. Dimopoulos M, Kyle R, Fermand JP, et al; International Myeloma Workshop Consensus Panel 3. Consensus recommendations for standard investigative workup: report of the International Myeloma Workshop Consensus Panel 3. Blood. 2011;117(18):4701-4705.
4. Katzmann JA, Clark RJ, Abraham RS, et al. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: relative sensitivity for detection of monoclonal light chains. Clin Chem. 2002;48(9):1437-1444.
5. Hutchison CA, Plant T, Drayson M, et al. Serum free light chain measurement
aids the diagnosis of myeloma in patients with severe renal failure.
BMC Nephrol. 2008;9:11.
6. Levey AS, Stevens LA, Schmid CH, et al; CKD-EPI (Chronic Kidney Disease
Epidemiology Collaboration). A new equation to estimate glomerular filtration
rate. Ann Intern Med. 2009;150(9):604-612.
7. McTaggart MP, Lindsay J, Kearney EM. Replacing urine protein electrophoresis
with serum free light chain analysis as a first-line test for detecting plasma
cell disorders offers increased diagnostic accuracy and potential health benefit
to patients. Am J Clin Pathol. 2013;140(6):890-897.
8. Abadie JM, Bankson DD. Assessment of serum free light chain assays for
plasma cell disorder screening in a Veterans Affairs population. Ann Clin Lab
Sci. 2006;36(2):157-162.
9. Kim HS, Kim HS, Shin KS, et al. Clinical comparisons of two free light chain
assays to immunofixation electrophoresis for detecting monoclonal gammopathy.
Biomed Res Int. 2014;2014:647238.
Note: Page numbers differ between the print issue and digital edition.
1. National Cancer Institute, Surveillance, Epidemiology, and End Results (SEER) Program. SEER website. http://seer.cancer.gov/statfacts/html/mulmy.html. Accessed July 11, 2016.
2. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33.
3. Dimopoulos M, Kyle R, Fermand JP, et al; International Myeloma Workshop Consensus Panel 3. Consensus recommendations for standard investigative workup: report of the International Myeloma Workshop Consensus Panel 3. Blood. 2011;117(18):4701-4705.
4. Katzmann JA, Clark RJ, Abraham RS, et al. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: relative sensitivity for detection of monoclonal light chains. Clin Chem. 2002;48(9):1437-1444.
5. Hutchison CA, Plant T, Drayson M, et al. Serum free light chain measurement
aids the diagnosis of myeloma in patients with severe renal failure.
BMC Nephrol. 2008;9:11.
6. Levey AS, Stevens LA, Schmid CH, et al; CKD-EPI (Chronic Kidney Disease
Epidemiology Collaboration). A new equation to estimate glomerular filtration
rate. Ann Intern Med. 2009;150(9):604-612.
7. McTaggart MP, Lindsay J, Kearney EM. Replacing urine protein electrophoresis
with serum free light chain analysis as a first-line test for detecting plasma
cell disorders offers increased diagnostic accuracy and potential health benefit
to patients. Am J Clin Pathol. 2013;140(6):890-897.
8. Abadie JM, Bankson DD. Assessment of serum free light chain assays for
plasma cell disorder screening in a Veterans Affairs population. Ann Clin Lab
Sci. 2006;36(2):157-162.
9. Kim HS, Kim HS, Shin KS, et al. Clinical comparisons of two free light chain
assays to immunofixation electrophoresis for detecting monoclonal gammopathy.
Biomed Res Int. 2014;2014:647238.
Note: Page numbers differ between the print issue and digital edition.
Excess weight linked to myeloma, other cancers

An analysis of more than 1000 studies suggests multiple myeloma (MM) and 12 other cancers are associated with excess weight.
The data suggest that limiting weight gain over time could help reduce a person’s risk of developing these cancers.
A working group convened by the International Agency for Research on Cancer (IARC) conducted this analysis and reported the results in NEJM.
“The burden of cancer due to being overweight or obese is more extensive than what has been assumed,” said Graham Colditz, MD, DrPH, who chaired the IARC working group.
“Many of the newly identified cancers linked to excess weight haven’t been on people’s radar screens as having a weight component.”
In 2002, an IARC working group reported finding sufficient evidence linking excess weight to higher risks of colon, esophageal, kidney, breast, and uterine cancers.
Now, another IARC working group has found evidence linking excess weight and additional cancers.
The group reviewed more than 1000 epidemiologic studies. Most of the studies provided cancer risk estimates for adult body mass index (BMI), although some provided estimates for BMI or body shape in childhood/adolescence, changes in BMI or weight over time, or other indicators of adiposity.
The IARC working group reported the relative risk (RR) of developing various cancers for the highest BMI category evaluated, versus a normal BMI.
The group said there was sufficient evidence linking excess weight to the following cancers: adenocarcinoma (RR=4.8), gastric cardia (RR=1.8), colon and rectal cancer (RR=1.3), liver cancer (RR=1.8), gallbladder cancer (RR=1.3), pancreatic cancer (RR=1.5), postmenopausal breast cancer (RR=1.1), corpus uteri (RR=7.1), ovarian cancer (RR=1.1), renal cell cancer (RR=1.8), meningioma (RR=1.5), thyroid cancer (RR=1.1), and MM (RR=1.5).
Looking more closely at MM, the RR was 1.2 for adults who were overweight (BMI 25-29.9), 1.2 for those with class 1 obesity (BMI 30-34.9), and 1.5 for those with class 2 or 3 obesity (BMI 35-40+).
For most of the cancers, there was positive dose-response relationship; in other words, the higher the BMI, the greater the cancer risk.
In addition, the cancer risks associated with excess weight were similar for men and women and were consistent across geographic regions—North America, Europe, Asia, and the Middle East—where data were available.
“Significant numbers of the US and the world’s population are overweight,” Dr Colditz noted. “This is another wake-up call. It’s time to take our health and our diets seriously.”
Dr Colditz conceded that losing weight can be difficult. Therefore, he recommended that people who struggle with weight loss should focus on avoiding weight gain to reduce their risk of developing certain cancers. ![]()

An analysis of more than 1000 studies suggests multiple myeloma (MM) and 12 other cancers are associated with excess weight.
The data suggest that limiting weight gain over time could help reduce a person’s risk of developing these cancers.
A working group convened by the International Agency for Research on Cancer (IARC) conducted this analysis and reported the results in NEJM.
“The burden of cancer due to being overweight or obese is more extensive than what has been assumed,” said Graham Colditz, MD, DrPH, who chaired the IARC working group.
“Many of the newly identified cancers linked to excess weight haven’t been on people’s radar screens as having a weight component.”
In 2002, an IARC working group reported finding sufficient evidence linking excess weight to higher risks of colon, esophageal, kidney, breast, and uterine cancers.
Now, another IARC working group has found evidence linking excess weight and additional cancers.
The group reviewed more than 1000 epidemiologic studies. Most of the studies provided cancer risk estimates for adult body mass index (BMI), although some provided estimates for BMI or body shape in childhood/adolescence, changes in BMI or weight over time, or other indicators of adiposity.
The IARC working group reported the relative risk (RR) of developing various cancers for the highest BMI category evaluated, versus a normal BMI.
The group said there was sufficient evidence linking excess weight to the following cancers: adenocarcinoma (RR=4.8), gastric cardia (RR=1.8), colon and rectal cancer (RR=1.3), liver cancer (RR=1.8), gallbladder cancer (RR=1.3), pancreatic cancer (RR=1.5), postmenopausal breast cancer (RR=1.1), corpus uteri (RR=7.1), ovarian cancer (RR=1.1), renal cell cancer (RR=1.8), meningioma (RR=1.5), thyroid cancer (RR=1.1), and MM (RR=1.5).
Looking more closely at MM, the RR was 1.2 for adults who were overweight (BMI 25-29.9), 1.2 for those with class 1 obesity (BMI 30-34.9), and 1.5 for those with class 2 or 3 obesity (BMI 35-40+).
For most of the cancers, there was positive dose-response relationship; in other words, the higher the BMI, the greater the cancer risk.
In addition, the cancer risks associated with excess weight were similar for men and women and were consistent across geographic regions—North America, Europe, Asia, and the Middle East—where data were available.
“Significant numbers of the US and the world’s population are overweight,” Dr Colditz noted. “This is another wake-up call. It’s time to take our health and our diets seriously.”
Dr Colditz conceded that losing weight can be difficult. Therefore, he recommended that people who struggle with weight loss should focus on avoiding weight gain to reduce their risk of developing certain cancers. ![]()

An analysis of more than 1000 studies suggests multiple myeloma (MM) and 12 other cancers are associated with excess weight.
The data suggest that limiting weight gain over time could help reduce a person’s risk of developing these cancers.
A working group convened by the International Agency for Research on Cancer (IARC) conducted this analysis and reported the results in NEJM.
“The burden of cancer due to being overweight or obese is more extensive than what has been assumed,” said Graham Colditz, MD, DrPH, who chaired the IARC working group.
“Many of the newly identified cancers linked to excess weight haven’t been on people’s radar screens as having a weight component.”
In 2002, an IARC working group reported finding sufficient evidence linking excess weight to higher risks of colon, esophageal, kidney, breast, and uterine cancers.
Now, another IARC working group has found evidence linking excess weight and additional cancers.
The group reviewed more than 1000 epidemiologic studies. Most of the studies provided cancer risk estimates for adult body mass index (BMI), although some provided estimates for BMI or body shape in childhood/adolescence, changes in BMI or weight over time, or other indicators of adiposity.
The IARC working group reported the relative risk (RR) of developing various cancers for the highest BMI category evaluated, versus a normal BMI.
The group said there was sufficient evidence linking excess weight to the following cancers: adenocarcinoma (RR=4.8), gastric cardia (RR=1.8), colon and rectal cancer (RR=1.3), liver cancer (RR=1.8), gallbladder cancer (RR=1.3), pancreatic cancer (RR=1.5), postmenopausal breast cancer (RR=1.1), corpus uteri (RR=7.1), ovarian cancer (RR=1.1), renal cell cancer (RR=1.8), meningioma (RR=1.5), thyroid cancer (RR=1.1), and MM (RR=1.5).
Looking more closely at MM, the RR was 1.2 for adults who were overweight (BMI 25-29.9), 1.2 for those with class 1 obesity (BMI 30-34.9), and 1.5 for those with class 2 or 3 obesity (BMI 35-40+).
For most of the cancers, there was positive dose-response relationship; in other words, the higher the BMI, the greater the cancer risk.
In addition, the cancer risks associated with excess weight were similar for men and women and were consistent across geographic regions—North America, Europe, Asia, and the Middle East—where data were available.
“Significant numbers of the US and the world’s population are overweight,” Dr Colditz noted. “This is another wake-up call. It’s time to take our health and our diets seriously.”
Dr Colditz conceded that losing weight can be difficult. Therefore, he recommended that people who struggle with weight loss should focus on avoiding weight gain to reduce their risk of developing certain cancers. ![]()
Ninlaro receives approval for use in Canada
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Massage therapy seems to benefit cancer patients

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()
Sociodemographic factors impact OS in MM

Photo courtesy of NCI
New research has revealed sociodemographic factors that appear to influence survival in younger patients with multiple myeloma (MM).
The study, which included more than 10,000 MM patients under the age of 65, suggested that marital status, insurance status, and county-level income all affect a patient’s chance of survival.
However, race/ethnicity and county-level educational achievement were not associated with overall survival (OS).
Luciano Costa, MD, PhD, of the University of Alabama at Birmingham, and his colleagues reported these findings in Cancer.
The researchers analyzed data on patients who were diagnosed with MM before the age of 65, between 2007 and 2012. There were 10,161 cases of MM, and the median follow-up was 27 months (range, 0-71 months).
The sociodemographic variables assessed were marital status, insurance status, median household income in the county of residence, and county-level educational achievement.
The researchers also looked at race/ethnicity, which was defined as a self-reported construct including Hispanic, non-Hispanic black, non-Hispanic white, and “other.”
The researchers found that patients had an increased risk of death if they were not married, did not have private insurance (were uninsured or on Medicaid), or lived in a low-income area (belonging to the lowest 2 income quartiles).
The 4-year estimated OS rate was 71.1% for patients who did not have any of these adverse sociodemographic factors, but it was 63.2% for patients with 1 factor, 53.4% for patients with 2 factors, and 46.5% for patients with all 3 factors (P<0.001).
The researchers did find that Hispanic and non-Hispanic black individuals had more adverse sociodemographic factors and worse OS than non-Hispanic whites and people belonging to the “other” category.
However, when the population was stratified by the cumulative number of sociodemographic factors and the researchers adjusted for confounders, there was no consistent association between race/ethnicity and OS.
The researchers said this suggests the apparent impact of race/ethnicity on OS may be due to the disparate distribution of sociodemographic factors observed among the different races/ethnicities rather than the race/ethnicity construct itself.
“This [study] strongly suggests that there is a huge disparity in outcomes that could potentially be overcome by improving access and affordability of treatments,” Dr Costa said.
“With the recent emphasis on comparative effectiveness in oncology, it also becomes crucial that all variables affecting outcomes—including sociodemographic factors—are accounted for when comparisons between different therapeutic approaches and healthcare systems are made.” ![]()

Photo courtesy of NCI
New research has revealed sociodemographic factors that appear to influence survival in younger patients with multiple myeloma (MM).
The study, which included more than 10,000 MM patients under the age of 65, suggested that marital status, insurance status, and county-level income all affect a patient’s chance of survival.
However, race/ethnicity and county-level educational achievement were not associated with overall survival (OS).
Luciano Costa, MD, PhD, of the University of Alabama at Birmingham, and his colleagues reported these findings in Cancer.
The researchers analyzed data on patients who were diagnosed with MM before the age of 65, between 2007 and 2012. There were 10,161 cases of MM, and the median follow-up was 27 months (range, 0-71 months).
The sociodemographic variables assessed were marital status, insurance status, median household income in the county of residence, and county-level educational achievement.
The researchers also looked at race/ethnicity, which was defined as a self-reported construct including Hispanic, non-Hispanic black, non-Hispanic white, and “other.”
The researchers found that patients had an increased risk of death if they were not married, did not have private insurance (were uninsured or on Medicaid), or lived in a low-income area (belonging to the lowest 2 income quartiles).
The 4-year estimated OS rate was 71.1% for patients who did not have any of these adverse sociodemographic factors, but it was 63.2% for patients with 1 factor, 53.4% for patients with 2 factors, and 46.5% for patients with all 3 factors (P<0.001).
The researchers did find that Hispanic and non-Hispanic black individuals had more adverse sociodemographic factors and worse OS than non-Hispanic whites and people belonging to the “other” category.
However, when the population was stratified by the cumulative number of sociodemographic factors and the researchers adjusted for confounders, there was no consistent association between race/ethnicity and OS.
The researchers said this suggests the apparent impact of race/ethnicity on OS may be due to the disparate distribution of sociodemographic factors observed among the different races/ethnicities rather than the race/ethnicity construct itself.
“This [study] strongly suggests that there is a huge disparity in outcomes that could potentially be overcome by improving access and affordability of treatments,” Dr Costa said.
“With the recent emphasis on comparative effectiveness in oncology, it also becomes crucial that all variables affecting outcomes—including sociodemographic factors—are accounted for when comparisons between different therapeutic approaches and healthcare systems are made.” ![]()

Photo courtesy of NCI
New research has revealed sociodemographic factors that appear to influence survival in younger patients with multiple myeloma (MM).
The study, which included more than 10,000 MM patients under the age of 65, suggested that marital status, insurance status, and county-level income all affect a patient’s chance of survival.
However, race/ethnicity and county-level educational achievement were not associated with overall survival (OS).
Luciano Costa, MD, PhD, of the University of Alabama at Birmingham, and his colleagues reported these findings in Cancer.
The researchers analyzed data on patients who were diagnosed with MM before the age of 65, between 2007 and 2012. There were 10,161 cases of MM, and the median follow-up was 27 months (range, 0-71 months).
The sociodemographic variables assessed were marital status, insurance status, median household income in the county of residence, and county-level educational achievement.
The researchers also looked at race/ethnicity, which was defined as a self-reported construct including Hispanic, non-Hispanic black, non-Hispanic white, and “other.”
The researchers found that patients had an increased risk of death if they were not married, did not have private insurance (were uninsured or on Medicaid), or lived in a low-income area (belonging to the lowest 2 income quartiles).
The 4-year estimated OS rate was 71.1% for patients who did not have any of these adverse sociodemographic factors, but it was 63.2% for patients with 1 factor, 53.4% for patients with 2 factors, and 46.5% for patients with all 3 factors (P<0.001).
The researchers did find that Hispanic and non-Hispanic black individuals had more adverse sociodemographic factors and worse OS than non-Hispanic whites and people belonging to the “other” category.
However, when the population was stratified by the cumulative number of sociodemographic factors and the researchers adjusted for confounders, there was no consistent association between race/ethnicity and OS.
The researchers said this suggests the apparent impact of race/ethnicity on OS may be due to the disparate distribution of sociodemographic factors observed among the different races/ethnicities rather than the race/ethnicity construct itself.
“This [study] strongly suggests that there is a huge disparity in outcomes that could potentially be overcome by improving access and affordability of treatments,” Dr Costa said.
“With the recent emphasis on comparative effectiveness in oncology, it also becomes crucial that all variables affecting outcomes—including sociodemographic factors—are accounted for when comparisons between different therapeutic approaches and healthcare systems are made.” ![]()
Cancer survivors have ‘normal’ sex lives, survey says

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()