User login
Ultraprocessed Foods Linked to Faster Biological Aging
TOPLINE:
and factors other than poor nutritional content may be to blame.
METHODOLOGY:
- Previous studies have reported an association between high consumption of UPFs and some measures of early biological aging, such as shorter telomere length, cognitive decline, and frailty, but the relationship is largely unexplored so far, including exactly how UPFs may harm health.
- To examine the association between UPF consumption and biological aging, researchers conducted a cross-sectional analysis of 22,495 participants (mean chronological age, 55.6 years; 52% women) from the Moli-sani Study in Italy, who were recruited between 2005 and 2010.
- Food intake was assessed with a food frequency questionnaire that covered 188 different food items, each of which was categorized into one of four groups based on the extent of processing, ranging from minimally processed foods, such as fruits, vegetables, meat and fish, to UPFs.
- UPF intake was determined by weight, using the ratio of UPFs to the total weight of food and beverages (g/d), and participants were categorized into sex-specific fifths according to the proportion of UPFs in their total food intake. Diet quality was also evaluated using the Mediterranean Diet Score.
- Biological age was computed using a deep neural network approach based on 36 circulating blood biomarkers, and the mean difference between the mean biological and chronological ages was analyzed.
TAKEAWAY:
- The mean difference between biological and chronological ages of the participants was –0.70 years.
- Higher intake of UPFs was associated with accelerated biological aging compared with the lowest intake (regression coefficient, 0.34; 95% CI, 0.08-0.61), with a mean difference between the biological and chronological ages of −4.1 years and 1.6 years in those with the lowest and highest intakes, respectively.
- The association between UPF consumption and biological aging was nonlinear (P = .049 for nonlinearity). The association tended to be stronger in men than in women, but this was not statistically significant.
- Including the Mediterranean Diet Score in the model slightly attenuated the association by 9.1%, indicating that poor nutritional content was likely to explain a small part of the underlying mechanism.
IN PRACTICE:
“Our results showed that the UPFs–biological aging association was weakly explained by the poor nutritional composition of these highly processed foods, suggesting that biological aging could be mainly influenced by non-nutrient food characteristics, which include altered food matrix, contact materials and neo-formed compounds,” the authors wrote.
SOURCE:
The study was led by Simona Esposito, Research Unit of Epidemiology and Prevention, IRCCS Neuromed, Isernia, Italy. It was published online in The American Journal of Clinical Nutrition.
LIMITATIONS:
The cross-sectional design of the study limited the ability to determine the temporal directionality of the association, and the observational nature of the study limited the ability to establish the causality between UPF consumption and biological aging. The use of self-reported dietary data may have introduced recall bias. The study population was limited to adults from Central-Southern Italy, which may affect the generalizability of the findings.
DISCLOSURES:
The study was developed within the project funded by the Next Generation European Union “Age-It — Ageing well in an ageing society” project, National Recovery and Resilience Plan. The analyses were partially supported by the Italian Ministry of Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
and factors other than poor nutritional content may be to blame.
METHODOLOGY:
- Previous studies have reported an association between high consumption of UPFs and some measures of early biological aging, such as shorter telomere length, cognitive decline, and frailty, but the relationship is largely unexplored so far, including exactly how UPFs may harm health.
- To examine the association between UPF consumption and biological aging, researchers conducted a cross-sectional analysis of 22,495 participants (mean chronological age, 55.6 years; 52% women) from the Moli-sani Study in Italy, who were recruited between 2005 and 2010.
- Food intake was assessed with a food frequency questionnaire that covered 188 different food items, each of which was categorized into one of four groups based on the extent of processing, ranging from minimally processed foods, such as fruits, vegetables, meat and fish, to UPFs.
- UPF intake was determined by weight, using the ratio of UPFs to the total weight of food and beverages (g/d), and participants were categorized into sex-specific fifths according to the proportion of UPFs in their total food intake. Diet quality was also evaluated using the Mediterranean Diet Score.
- Biological age was computed using a deep neural network approach based on 36 circulating blood biomarkers, and the mean difference between the mean biological and chronological ages was analyzed.
TAKEAWAY:
- The mean difference between biological and chronological ages of the participants was –0.70 years.
- Higher intake of UPFs was associated with accelerated biological aging compared with the lowest intake (regression coefficient, 0.34; 95% CI, 0.08-0.61), with a mean difference between the biological and chronological ages of −4.1 years and 1.6 years in those with the lowest and highest intakes, respectively.
- The association between UPF consumption and biological aging was nonlinear (P = .049 for nonlinearity). The association tended to be stronger in men than in women, but this was not statistically significant.
- Including the Mediterranean Diet Score in the model slightly attenuated the association by 9.1%, indicating that poor nutritional content was likely to explain a small part of the underlying mechanism.
IN PRACTICE:
“Our results showed that the UPFs–biological aging association was weakly explained by the poor nutritional composition of these highly processed foods, suggesting that biological aging could be mainly influenced by non-nutrient food characteristics, which include altered food matrix, contact materials and neo-formed compounds,” the authors wrote.
SOURCE:
The study was led by Simona Esposito, Research Unit of Epidemiology and Prevention, IRCCS Neuromed, Isernia, Italy. It was published online in The American Journal of Clinical Nutrition.
LIMITATIONS:
The cross-sectional design of the study limited the ability to determine the temporal directionality of the association, and the observational nature of the study limited the ability to establish the causality between UPF consumption and biological aging. The use of self-reported dietary data may have introduced recall bias. The study population was limited to adults from Central-Southern Italy, which may affect the generalizability of the findings.
DISCLOSURES:
The study was developed within the project funded by the Next Generation European Union “Age-It — Ageing well in an ageing society” project, National Recovery and Resilience Plan. The analyses were partially supported by the Italian Ministry of Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
and factors other than poor nutritional content may be to blame.
METHODOLOGY:
- Previous studies have reported an association between high consumption of UPFs and some measures of early biological aging, such as shorter telomere length, cognitive decline, and frailty, but the relationship is largely unexplored so far, including exactly how UPFs may harm health.
- To examine the association between UPF consumption and biological aging, researchers conducted a cross-sectional analysis of 22,495 participants (mean chronological age, 55.6 years; 52% women) from the Moli-sani Study in Italy, who were recruited between 2005 and 2010.
- Food intake was assessed with a food frequency questionnaire that covered 188 different food items, each of which was categorized into one of four groups based on the extent of processing, ranging from minimally processed foods, such as fruits, vegetables, meat and fish, to UPFs.
- UPF intake was determined by weight, using the ratio of UPFs to the total weight of food and beverages (g/d), and participants were categorized into sex-specific fifths according to the proportion of UPFs in their total food intake. Diet quality was also evaluated using the Mediterranean Diet Score.
- Biological age was computed using a deep neural network approach based on 36 circulating blood biomarkers, and the mean difference between the mean biological and chronological ages was analyzed.
TAKEAWAY:
- The mean difference between biological and chronological ages of the participants was –0.70 years.
- Higher intake of UPFs was associated with accelerated biological aging compared with the lowest intake (regression coefficient, 0.34; 95% CI, 0.08-0.61), with a mean difference between the biological and chronological ages of −4.1 years and 1.6 years in those with the lowest and highest intakes, respectively.
- The association between UPF consumption and biological aging was nonlinear (P = .049 for nonlinearity). The association tended to be stronger in men than in women, but this was not statistically significant.
- Including the Mediterranean Diet Score in the model slightly attenuated the association by 9.1%, indicating that poor nutritional content was likely to explain a small part of the underlying mechanism.
IN PRACTICE:
“Our results showed that the UPFs–biological aging association was weakly explained by the poor nutritional composition of these highly processed foods, suggesting that biological aging could be mainly influenced by non-nutrient food characteristics, which include altered food matrix, contact materials and neo-formed compounds,” the authors wrote.
SOURCE:
The study was led by Simona Esposito, Research Unit of Epidemiology and Prevention, IRCCS Neuromed, Isernia, Italy. It was published online in The American Journal of Clinical Nutrition.
LIMITATIONS:
The cross-sectional design of the study limited the ability to determine the temporal directionality of the association, and the observational nature of the study limited the ability to establish the causality between UPF consumption and biological aging. The use of self-reported dietary data may have introduced recall bias. The study population was limited to adults from Central-Southern Italy, which may affect the generalizability of the findings.
DISCLOSURES:
The study was developed within the project funded by the Next Generation European Union “Age-It — Ageing well in an ageing society” project, National Recovery and Resilience Plan. The analyses were partially supported by the Italian Ministry of Health. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Oral Semaglutide 25-mg Dose May Provide Most Benefit
SAN ANTONIO — Oral semaglutide 25 mg appears to be just as effective in promoting weight loss and other beneficial outcomes as are the investigational 50-mg oral dose and the injectable 2.4-mg dose (Wegovy), in new research.
Data from Novo Nordisk’s OASIS 4 trial suggest that “oral semaglutide 25 mg may represent an efficacious option for the treatment of overweight and obesity, particularly in patients who prefer oral administration,” W. Timothy Garvey, MD, professor in the Department of Nutrition Sciences at the University of Alabama at Birmingham (UAB), said at the Obesity Society’s Obesity Week 2024 meeting.
In an interview, Garvey, who is also senior scientist at the UAB Nutrition Obesity Research Center, added: “There’s a principle in medicine that you always use the lowest dose that has highest efficacy, and for oral semaglutide for obesity, that appears to be the 25-mg dose. We need oral medicines to offer as an option for patients that could lead to a longer persistence in adherence to obesity medications, which is a big problem. Less than half the people maintain their adherence after a year.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said that OASIS 4 was “extremely well done, especially given that we’re all concerned about the high prevalence of people stopping these medications at a year. ... I love the idea of trying to find these lower doses and increasing options for people.”
(The oral semaglutide approved for treating type 2 diabetes [Rybelsus] is sold in 7-mg and 14-mg doses.)
With Oral Semaglutide, Lower May Be Better
OASIS 4 was a double-blind, randomized, placebo-controlled 64-week multicenter trial involving a total of 307 participants with overweight/obesity randomized 2:1 to oral semaglutide 25 mg or placebo. Of those, 167 in the semaglutide 25 mg and 76 in the placebo groups completed the trial.
For the co–primary endpoint change in body weight at week 64 (including 52-week maintenance and 7-week follow-up periods), there was a drop of 13.6% with oral semaglutide vs just 2.2% with placebo (P < .0001), based on in-trial observation regardless of adherence. For the analysis including just the on-treatment period, those reductions were 16.6% and 2.7%, respectively (P < .0001).
For the other co–primary endpoint, 79.2% semaglutide vs 31.1% placebo lost at least 5% of their body weight, 63.0% vs 14.4% lost ≥ 10%, 50.0% vs 5.6% lost ≥ 15%, and 29.7% vs 3.3% lost ≥ 20%. All were statistically significant differences, at P < .0001.
On the Impact of Weight on Quality of Life-Lite Clinical Trials Version, change from baseline scores were 16.2 with oral semaglutide vs 8.4 for placebo (P = .0006) and the proportion of participants achieving clinically meaningful increases in those scores (≥ 14.6 points) were 55.3% vs 34.8% (P = .0022).
Waist circumference was also significantly reduced from baseline with oral semaglutide, by 12.2 cm vs 2.8 cm (P < .0001). Both systolic and diastolic blood pressure dropped more with semaglutide than placebo, but not significantly. However, the inflammatory marker C-reactive protein dropped from baseline by 46.4% vs just 4.2% with placebo, a significant difference (P < .0001).
Hemoglobin A1c dropped by 0.29 percentage points vs just 0.06 with placebo (P = .0012) and fasting plasma glucose by 6.6 mg/dL, while rising by 0.4 mg/dL in the placebo group (P = .0012). Lipid levels also improved more with oral semaglutide.
Overall adverse events occurred in 93.1% on oral semaglutide and 85.3% with placebo, and gastrointestinal adverse events in 74% and 42.2%, respectively. Other types of adverse events didn’t differ between the groups. The proportions experiencing severe adverse events were less in the semaglutide group (3.9% vs 8.8%), although adverse events leading to permanent treatment discontinuation were slightly higher with oral semaglutide (6.9% vs 5.9%). There were no deaths.
The estimated treatment difference from placebo in body weight change of −11.4% in OASIS 4 (P < .0001) was similar to the –12.7% (P < .0001) seen with the 50-mg oral semaglutide dose studied in OASIS 1 and the –12.4% (P < .0001) difference with subcutaneous semaglutide 2.4 mg in the STEP 1 trial. “All had pretty comparable efficacy,” Garvey noted.
The side-effect profiles, including frequency of gastrointestinal side effects, were also similar across the three trials. However, Garvey added, “the mean duration of nausea in those patients that experienced nausea was shorter in patients on a 25-mg dose, 13 days, whereas the mean duration of nausea was greater, 19 days, in those in OASIS 1 taking 50 mg a day.”
Garvey has consulted for Boehringer Ingelheim, Carmot Therapeutics/Roche, Eli Lilly, Fractyl Laboratories, Inogen, Lilly, Merck, Novo Nordisk, and Zealand Pharma; has ownership interest (stock, stock options in a publicly owned company) for Bristol-Myers Squibb, Isis, Lilly, and Novartis; serves as site principal investigator for Carmot Therapeutics/Roche, Eli Lilly, Epitomee Medical, Lilly, Neurovalens, Novo Nordisk, and Zealand Pharmaceuticals; and as a data monitoring committee member for Boehringer Ingelheim and Eli Lilly. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Oral semaglutide 25 mg appears to be just as effective in promoting weight loss and other beneficial outcomes as are the investigational 50-mg oral dose and the injectable 2.4-mg dose (Wegovy), in new research.
Data from Novo Nordisk’s OASIS 4 trial suggest that “oral semaglutide 25 mg may represent an efficacious option for the treatment of overweight and obesity, particularly in patients who prefer oral administration,” W. Timothy Garvey, MD, professor in the Department of Nutrition Sciences at the University of Alabama at Birmingham (UAB), said at the Obesity Society’s Obesity Week 2024 meeting.
In an interview, Garvey, who is also senior scientist at the UAB Nutrition Obesity Research Center, added: “There’s a principle in medicine that you always use the lowest dose that has highest efficacy, and for oral semaglutide for obesity, that appears to be the 25-mg dose. We need oral medicines to offer as an option for patients that could lead to a longer persistence in adherence to obesity medications, which is a big problem. Less than half the people maintain their adherence after a year.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said that OASIS 4 was “extremely well done, especially given that we’re all concerned about the high prevalence of people stopping these medications at a year. ... I love the idea of trying to find these lower doses and increasing options for people.”
(The oral semaglutide approved for treating type 2 diabetes [Rybelsus] is sold in 7-mg and 14-mg doses.)
With Oral Semaglutide, Lower May Be Better
OASIS 4 was a double-blind, randomized, placebo-controlled 64-week multicenter trial involving a total of 307 participants with overweight/obesity randomized 2:1 to oral semaglutide 25 mg or placebo. Of those, 167 in the semaglutide 25 mg and 76 in the placebo groups completed the trial.
For the co–primary endpoint change in body weight at week 64 (including 52-week maintenance and 7-week follow-up periods), there was a drop of 13.6% with oral semaglutide vs just 2.2% with placebo (P < .0001), based on in-trial observation regardless of adherence. For the analysis including just the on-treatment period, those reductions were 16.6% and 2.7%, respectively (P < .0001).
For the other co–primary endpoint, 79.2% semaglutide vs 31.1% placebo lost at least 5% of their body weight, 63.0% vs 14.4% lost ≥ 10%, 50.0% vs 5.6% lost ≥ 15%, and 29.7% vs 3.3% lost ≥ 20%. All were statistically significant differences, at P < .0001.
On the Impact of Weight on Quality of Life-Lite Clinical Trials Version, change from baseline scores were 16.2 with oral semaglutide vs 8.4 for placebo (P = .0006) and the proportion of participants achieving clinically meaningful increases in those scores (≥ 14.6 points) were 55.3% vs 34.8% (P = .0022).
Waist circumference was also significantly reduced from baseline with oral semaglutide, by 12.2 cm vs 2.8 cm (P < .0001). Both systolic and diastolic blood pressure dropped more with semaglutide than placebo, but not significantly. However, the inflammatory marker C-reactive protein dropped from baseline by 46.4% vs just 4.2% with placebo, a significant difference (P < .0001).
Hemoglobin A1c dropped by 0.29 percentage points vs just 0.06 with placebo (P = .0012) and fasting plasma glucose by 6.6 mg/dL, while rising by 0.4 mg/dL in the placebo group (P = .0012). Lipid levels also improved more with oral semaglutide.
Overall adverse events occurred in 93.1% on oral semaglutide and 85.3% with placebo, and gastrointestinal adverse events in 74% and 42.2%, respectively. Other types of adverse events didn’t differ between the groups. The proportions experiencing severe adverse events were less in the semaglutide group (3.9% vs 8.8%), although adverse events leading to permanent treatment discontinuation were slightly higher with oral semaglutide (6.9% vs 5.9%). There were no deaths.
The estimated treatment difference from placebo in body weight change of −11.4% in OASIS 4 (P < .0001) was similar to the –12.7% (P < .0001) seen with the 50-mg oral semaglutide dose studied in OASIS 1 and the –12.4% (P < .0001) difference with subcutaneous semaglutide 2.4 mg in the STEP 1 trial. “All had pretty comparable efficacy,” Garvey noted.
The side-effect profiles, including frequency of gastrointestinal side effects, were also similar across the three trials. However, Garvey added, “the mean duration of nausea in those patients that experienced nausea was shorter in patients on a 25-mg dose, 13 days, whereas the mean duration of nausea was greater, 19 days, in those in OASIS 1 taking 50 mg a day.”
Garvey has consulted for Boehringer Ingelheim, Carmot Therapeutics/Roche, Eli Lilly, Fractyl Laboratories, Inogen, Lilly, Merck, Novo Nordisk, and Zealand Pharma; has ownership interest (stock, stock options in a publicly owned company) for Bristol-Myers Squibb, Isis, Lilly, and Novartis; serves as site principal investigator for Carmot Therapeutics/Roche, Eli Lilly, Epitomee Medical, Lilly, Neurovalens, Novo Nordisk, and Zealand Pharmaceuticals; and as a data monitoring committee member for Boehringer Ingelheim and Eli Lilly. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Oral semaglutide 25 mg appears to be just as effective in promoting weight loss and other beneficial outcomes as are the investigational 50-mg oral dose and the injectable 2.4-mg dose (Wegovy), in new research.
Data from Novo Nordisk’s OASIS 4 trial suggest that “oral semaglutide 25 mg may represent an efficacious option for the treatment of overweight and obesity, particularly in patients who prefer oral administration,” W. Timothy Garvey, MD, professor in the Department of Nutrition Sciences at the University of Alabama at Birmingham (UAB), said at the Obesity Society’s Obesity Week 2024 meeting.
In an interview, Garvey, who is also senior scientist at the UAB Nutrition Obesity Research Center, added: “There’s a principle in medicine that you always use the lowest dose that has highest efficacy, and for oral semaglutide for obesity, that appears to be the 25-mg dose. We need oral medicines to offer as an option for patients that could lead to a longer persistence in adherence to obesity medications, which is a big problem. Less than half the people maintain their adherence after a year.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said that OASIS 4 was “extremely well done, especially given that we’re all concerned about the high prevalence of people stopping these medications at a year. ... I love the idea of trying to find these lower doses and increasing options for people.”
(The oral semaglutide approved for treating type 2 diabetes [Rybelsus] is sold in 7-mg and 14-mg doses.)
With Oral Semaglutide, Lower May Be Better
OASIS 4 was a double-blind, randomized, placebo-controlled 64-week multicenter trial involving a total of 307 participants with overweight/obesity randomized 2:1 to oral semaglutide 25 mg or placebo. Of those, 167 in the semaglutide 25 mg and 76 in the placebo groups completed the trial.
For the co–primary endpoint change in body weight at week 64 (including 52-week maintenance and 7-week follow-up periods), there was a drop of 13.6% with oral semaglutide vs just 2.2% with placebo (P < .0001), based on in-trial observation regardless of adherence. For the analysis including just the on-treatment period, those reductions were 16.6% and 2.7%, respectively (P < .0001).
For the other co–primary endpoint, 79.2% semaglutide vs 31.1% placebo lost at least 5% of their body weight, 63.0% vs 14.4% lost ≥ 10%, 50.0% vs 5.6% lost ≥ 15%, and 29.7% vs 3.3% lost ≥ 20%. All were statistically significant differences, at P < .0001.
On the Impact of Weight on Quality of Life-Lite Clinical Trials Version, change from baseline scores were 16.2 with oral semaglutide vs 8.4 for placebo (P = .0006) and the proportion of participants achieving clinically meaningful increases in those scores (≥ 14.6 points) were 55.3% vs 34.8% (P = .0022).
Waist circumference was also significantly reduced from baseline with oral semaglutide, by 12.2 cm vs 2.8 cm (P < .0001). Both systolic and diastolic blood pressure dropped more with semaglutide than placebo, but not significantly. However, the inflammatory marker C-reactive protein dropped from baseline by 46.4% vs just 4.2% with placebo, a significant difference (P < .0001).
Hemoglobin A1c dropped by 0.29 percentage points vs just 0.06 with placebo (P = .0012) and fasting plasma glucose by 6.6 mg/dL, while rising by 0.4 mg/dL in the placebo group (P = .0012). Lipid levels also improved more with oral semaglutide.
Overall adverse events occurred in 93.1% on oral semaglutide and 85.3% with placebo, and gastrointestinal adverse events in 74% and 42.2%, respectively. Other types of adverse events didn’t differ between the groups. The proportions experiencing severe adverse events were less in the semaglutide group (3.9% vs 8.8%), although adverse events leading to permanent treatment discontinuation were slightly higher with oral semaglutide (6.9% vs 5.9%). There were no deaths.
The estimated treatment difference from placebo in body weight change of −11.4% in OASIS 4 (P < .0001) was similar to the –12.7% (P < .0001) seen with the 50-mg oral semaglutide dose studied in OASIS 1 and the –12.4% (P < .0001) difference with subcutaneous semaglutide 2.4 mg in the STEP 1 trial. “All had pretty comparable efficacy,” Garvey noted.
The side-effect profiles, including frequency of gastrointestinal side effects, were also similar across the three trials. However, Garvey added, “the mean duration of nausea in those patients that experienced nausea was shorter in patients on a 25-mg dose, 13 days, whereas the mean duration of nausea was greater, 19 days, in those in OASIS 1 taking 50 mg a day.”
Garvey has consulted for Boehringer Ingelheim, Carmot Therapeutics/Roche, Eli Lilly, Fractyl Laboratories, Inogen, Lilly, Merck, Novo Nordisk, and Zealand Pharma; has ownership interest (stock, stock options in a publicly owned company) for Bristol-Myers Squibb, Isis, Lilly, and Novartis; serves as site principal investigator for Carmot Therapeutics/Roche, Eli Lilly, Epitomee Medical, Lilly, Neurovalens, Novo Nordisk, and Zealand Pharmaceuticals; and as a data monitoring committee member for Boehringer Ingelheim and Eli Lilly. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article first appeared on Medscape.com.
FROM OBESITY WEEK 2024
8 New GI Studies With Practice-Shifting Implications
I’m just back from the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting in Philadelphia, Pennsylvania.
In part 2 of this series, I’m offering my highlights from this year’s meeting. (Part 1 is available here.) They are not presented in any particular order, but instead I am sharing what I found to be the most exciting among the thousands of abstracts and presentations.
Performing Capsule Endoscopy in Patients Taking GLP-1s
We’ve heard a lot about glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and the possibility that they might contribute to an increased risk for retained gastric contents and aspiration during endoscopy.
In the first study I’d like to highlight, researchers from the Mayo Clinic in Jacksonville, Florida, investigated video capsule endoscopy in patients with diabetes who were taking GLP-1 RAs vs a control group with diabetes not taking GLP-1 Ras. Patients in this retrospective matched cohort study were well balanced for demographics and diabetes-related characteristics.
Researchers found that in 7% of the 68 patients in the GLP-1 RA cohort, the video capsule endoscopy actually failed to pass through the stomach, whereas it passed successfully in all 68 patients in the control group (P =.06). The GLP-1 RA cohort had a longer transit time by a factor of almost four times (P <.001).
Multivariate analysis also showed that gastric transit time was approximately 80 minutes longer in the GLP-1 RA cohort (P <.001). Interestingly, 23.5% (16 of 68 patients) in the GLP-1 RA group experienced incomplete passage of the video capsule endoscopy through the small intestine, which was significantly higher than the proportion observed in the control group (4.4%; P <.01).
We need to look at potential strategies to mitigate these effects. Be aware of these results as you perform capsule endoscopy in patients taking GLP-1 RAs.
Barrett Esophagus On the Rise in the Young
The second study that caught my eye revealed the increasing incidence of young-onset Barrett esophagus (BE).
This population-based study used data obtained from TriNetX, a multi-institutional national database that offers a composite of health records from 88 healthcare organizations. Eligible patients had to have a negative upper esophagogastroduodenoscopy for BE prior to subsequently developing BE. Researchers stratified patients as to whether they were younger (< 50 years) or older (≥ 50 years), with further age ranges analyzed within those groups.
Young-onset BE accounted for 20% of all incident cases. The majority (94%) had nondysplastic BE. The incidence rate was not significantly different depending on whether patients were in the 45- to 49-year or 50- to 54-year age group.
Regression analysis revealed that there was a significantly increased trend for young-onset BE with hiatal hernia (odds ratio [OR], 2.6), smoking (OR, 2.3), White race (OR, 2.3), obstructive sleep apnea (OR, 2.2), male gender (OR, 2.0), and — at relatively lower risk levels — gastroesophageal reflux disease symptoms (OR, 1.2) and body mass index (OR, 1.1). The researchers did not analyze patients based on the presence of obesity, which is one of the risk factors for BE mentioned in national guidelines.
Results also showed that 6% of those with young-onset BE had BE-related neoplasia.
ACG guidelines recommend screening for BE beginning at age 50 in those with some of the risk factors noted in this study, including the presence of chronic gastroesophageal reflux disease symptoms. However, doing so may not capture the growing number of patients with young-onset BE.
We’ve seen a similar rise in rates of young-onset colorectal cancer, which has caused us to reevaluate our screening methods. Maybe we should do this for BE as well, specifically for patients presenting with these risk factors.
There’s a caveat to be aware of, which comes from my personal experience. I was biopsied for short-segment BE, and because it came up on my health record, it increased my life insurance premiums. This was because I was identified as having the risk profile of, essentially, an otherwise healthy smoker.
Dr Nicholas J. Shaheen and colleagues published a study several years ago showing that many insurance companies would not certify young, otherwise healthy people once diagnosed with BE. This is something to be aware of when you start to screen for BE, especially among younger patients.
A Novel Biologic for Eosinophilic Esophagitis
The next study presented results from a randomized, placebo-controlled, phase 3 study of cendakimab, a biologic agent in development for the treatment of eosinophilic esophagitis (EoE).
Dupilumab, which is an anti–interleukin (IL)-4 antibody, is the first treatment approved by the US Food and Drug Administration (FDA) for the treatment of EoE. Cendakimab, in turn, is a monoclonal antibody that neutralizes IL-13, a cytokine that plays a key role in EoE.
The study was led by Dr Evan Dellon from the University of North Carolina at Chapel Hill. Dellon and colleagues analyzed two different dosing regimens of cendakimab — 360 mg once weekly for 48 weeks, or 360 mg once weekly for 24 weeks followed by 360 mg every other week for 24 weeks — vs placebo for 48 weeks.
There was a significant effect for both cendakimab regimens in terms of symptom improvement and histologic response. There wasn’t much difference between participants that maintained once-weekly dosing and those who switched over to receive cendakimab every other week at 24 weeks. Only a minimal number of serious adverse events leading to discontinuation were noted in the study, with no notable difference between the treatment groups.
I think we’ll probably see this drug become available to us soon after it goes through the FDA review process, at which point it will add to our ability to use formative biologics in patients with EoE.
No Clear Benefit to Adding Bezlotoxumab to Fecal Microbiota Transplantation
Next was a very interesting study, and I think a clinically relevant one, about using fecal microbiota transplantation (FMT) alone or in combination with bezlotoxumab in patients with inflammatory bowel disease (IBD) with recurrent Clostridioides difficile infection.
Bezlotoxumab is a fully human monoclonal antibody that binds to C difficile toxin B. This drug has been studied and is approved for use, but it’s also extremely expensive, at a cost of approximately $4000 per dose.
Patients with IBD were eligible for inclusion if they had had two or more episodes of C difficile infection. They were then randomized in a 1:1 ration to receive either a single infusion of bezlotoxumab or placebo prior to FMT. The primary endpoint was C difficile infection recurrence within 8 weeks, which was defined as diarrhea plus a positive enzyme immunoassay toxin test. The secondary outcome was C difficile decolonization following treatment.
Researchers observed no statistically significant difference between the two cohorts. Steroid use prior to FMT significantly increased the risk for ongoing C difficile colonization (P =.03).
In summary, this is a case where it doesn’t seem that more is better. Bezlotoxumab didn’t add much, which calls into question the justification for its combined use with FMT.
Additional Positive Data for Seladelpar in Primary Biliary Cholangitis and Cirrhosis
Reassuring findings were presented on seladelpar, which was granted accelerated approval by the FDA in August.
Seladelpar is a selective peroxisome proliferator–activated receptor delta agonist that works in biliary cholangitis by regulating the genes involved in blocking biliary bile acid synthesis and controlling inflammation and fibrosis.
Results from the phase 3 RESPONSE trial were published in The New England Journal of Medicine in February reporting on the use of seladelpar in primary biliary cholangitis.
Whereas the RESPONSE trial removed decompensated patients, the ongoing phase 3 ASSURE trial results presented at this year’s meeting included patients with compensated cirrhosis. Approximately 94% of the patients in this study had Child-Pugh class A and 6% had class B cirrhosis. Eligibility required that patients had an inadequate response or were intolerant to ursodeoxycholic acid. Patients were administered open-label seladelpar 10 mg orally daily and followed for up to 1 year.
The good news is that there were no safety signals, which is reassuring news for our patients with compensated cirrhosis.
Advantages to Respiratory Syncytial Virus Vaccination in IBD
Another study that offered results certainly worthy of attention dealt with vaccination recommendations in patients with IBD.
Vaccination for respiratory syncytial virus (RSV) is now available in the United States. Its use was recommended for patients with IBD as early as 2021 per the Canadian Association of Gastroenterology’s clinical practice guideline, which discusses both live and nonlive vaccines. We should be aggressive in recommending this vaccine to our patients with IBD, but we haven’t really had one until recently.
Researchers behind this retrospective cohort study used the TriNetX database, which includes over 100 million unique patient charts. They identified patients with IBD, who were then divided into two groups according to whether they received the RSV vaccine or not.
Although this analysis was conducted in patients > 60 years of age, the US Centers for Disease Control and Prevention recommends RSV vaccination for all those over the age of 75 years, as well as for those 60-74 years old based on severity of risk.
For the primary endpoint of risk for RSV pneumonia, the OR was dramatically better in those who were vaccinated, with an approximately 80% risk reduction. Additionally, vaccinated patients experienced risk reductions of approximately 60% for acute respiratory failure, 50% for hospital inpatient admission, and 70% for requiring intensive care unit services.
This is a strong study showing not only that RSV vaccine did not exacerbate IBD but also that it improved outcomes in these patients. There’s a live-attenuated RSV vaccination that’s administered intranasally, which wouldn’t be used in your biologic or immunosuppressed patients with IBD, but the intramuscularly administered RSV vaccine doesn’t have any risk.
I think we can immediately begin recommending the RSV vaccine for our patients with IBD, particularly in those 60 years of age or older.
The Impact of Palliative Care Consultations in Decompensated Cirrhosis
The next study I’d like to highlight offers important data on the impact of palliative care consultation on 30- and 90-day readmission in patients with decompensated cirrhosis, which is a major cause of morbidity and mortality.
Researchers queried the National Readmissions Database over a 10-year period (2010-2019) to determine whether patients received a palliative care consult during index admission. They drew on a population of over 1.6 million patients admitted with decompensated cirrhosis.
Of this group, only 7.4% received a palliative care consultation at the index admission. But if they had this consultation, it was associated with a dramatic effect on readmission at 30 and 90 days. There was statistically significant risk reduction of approximately 70% for both 30- and 90-day readmission compared with those who didn’t receive the palliative consult (P <.001).
The take-home message here is to get a palliative care consult with these patients when they come in. Your hospital will unquestionably experience value in this reduction in readmission, especially considering that readmission within 30 days may not even be covered. Look at these results and start to take advantage of this valuable consultation.
Auxora: A Novel Treatment for Acute Pancreatitis
The last study for discussion offered very interesting data related to a drug called Auxora, a calcium release–activated calcium-channel inhibitor.
There is growing data that overactive calcium release–activated calcium channels aggravate acute pancreatitis and accelerate systemic inflammatory response syndrome (SIRS).
Acute pancreatitis with necrosis encompasses both local and systemic inflammation and is associated with significant mortality and morbidity. It is estimated that among patients with acute pancreatitis, 20%-30% have pancreatic necrosis, 30% develop infection, and 25% develop organ failure.
The presence of SIRS seems to herald the activation of these complex inflammatory pathways, which then leads to organ failure and necrosis, which can potentially be stemmed through this calcium channel inhibitor. Phase 2 studies of Auxora found that its use was associated with significant reduction in the risk for progression.
This subsequent phase 3 study looked at patients with acute pancreatitis and accompanying grade ≥ 2 SIRS criteria. They were randomized to receive placebo or Auxora at doses of 2 mg/kg, 1 mg/kg, or 0.5 mg/kg, which was administered intravenously over 4 hours for 3 consecutive days.
The primary endpoint was time to solid food tolerance, which was defined as eating ≥ 50% of a ≥ 500-calorie low-fat solid meal without increased abdominal pain or emesis, which is an important target because we always aim for enteral nutrition in patients with acute pancreatitis. The key secondary endpoint was severe respiratory failure, which was defined as invasive mechanical ventilation or ≥ 48 hours of either high-flow nasal cannula or noninvasive mechanical ventilation.
The primary endpoint was dramatically improved among those receiving Auxora, who achieved early onset of refeed. It appears that the high-dose 2 mg/kg may be the most beneficial in achieving improvement.
There were no patients with suspected or unexpected adverse events in the study population. Additionally, no patients receiving Auxora at any dose level went on to develop respiratory failure.
The present results show that Auxora decreases the time for solid food tolerance, as well as the rates of respiratory failure and necrotizing pancreatitis in patients presenting with two or more SIRS criteria. We’ll certainly look forward to more data, but it provides hope for a new treatment for acute pancreatitis.
Some of the take-home messages I presented are actionable now, whereas for others, we’ll have to wait and see what the final data show as well as the results of ongoing FDA approval before applying them.
Dr Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Virginia, and a past president of the American College of Gastroenterology. He reported serving in an advisory position with ISOTHRIVE. This transcript has been edited for clarity.
A version of this article first appeared on Medscape.com.
I’m just back from the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting in Philadelphia, Pennsylvania.
In part 2 of this series, I’m offering my highlights from this year’s meeting. (Part 1 is available here.) They are not presented in any particular order, but instead I am sharing what I found to be the most exciting among the thousands of abstracts and presentations.
Performing Capsule Endoscopy in Patients Taking GLP-1s
We’ve heard a lot about glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and the possibility that they might contribute to an increased risk for retained gastric contents and aspiration during endoscopy.
In the first study I’d like to highlight, researchers from the Mayo Clinic in Jacksonville, Florida, investigated video capsule endoscopy in patients with diabetes who were taking GLP-1 RAs vs a control group with diabetes not taking GLP-1 Ras. Patients in this retrospective matched cohort study were well balanced for demographics and diabetes-related characteristics.
Researchers found that in 7% of the 68 patients in the GLP-1 RA cohort, the video capsule endoscopy actually failed to pass through the stomach, whereas it passed successfully in all 68 patients in the control group (P =.06). The GLP-1 RA cohort had a longer transit time by a factor of almost four times (P <.001).
Multivariate analysis also showed that gastric transit time was approximately 80 minutes longer in the GLP-1 RA cohort (P <.001). Interestingly, 23.5% (16 of 68 patients) in the GLP-1 RA group experienced incomplete passage of the video capsule endoscopy through the small intestine, which was significantly higher than the proportion observed in the control group (4.4%; P <.01).
We need to look at potential strategies to mitigate these effects. Be aware of these results as you perform capsule endoscopy in patients taking GLP-1 RAs.
Barrett Esophagus On the Rise in the Young
The second study that caught my eye revealed the increasing incidence of young-onset Barrett esophagus (BE).
This population-based study used data obtained from TriNetX, a multi-institutional national database that offers a composite of health records from 88 healthcare organizations. Eligible patients had to have a negative upper esophagogastroduodenoscopy for BE prior to subsequently developing BE. Researchers stratified patients as to whether they were younger (< 50 years) or older (≥ 50 years), with further age ranges analyzed within those groups.
Young-onset BE accounted for 20% of all incident cases. The majority (94%) had nondysplastic BE. The incidence rate was not significantly different depending on whether patients were in the 45- to 49-year or 50- to 54-year age group.
Regression analysis revealed that there was a significantly increased trend for young-onset BE with hiatal hernia (odds ratio [OR], 2.6), smoking (OR, 2.3), White race (OR, 2.3), obstructive sleep apnea (OR, 2.2), male gender (OR, 2.0), and — at relatively lower risk levels — gastroesophageal reflux disease symptoms (OR, 1.2) and body mass index (OR, 1.1). The researchers did not analyze patients based on the presence of obesity, which is one of the risk factors for BE mentioned in national guidelines.
Results also showed that 6% of those with young-onset BE had BE-related neoplasia.
ACG guidelines recommend screening for BE beginning at age 50 in those with some of the risk factors noted in this study, including the presence of chronic gastroesophageal reflux disease symptoms. However, doing so may not capture the growing number of patients with young-onset BE.
We’ve seen a similar rise in rates of young-onset colorectal cancer, which has caused us to reevaluate our screening methods. Maybe we should do this for BE as well, specifically for patients presenting with these risk factors.
There’s a caveat to be aware of, which comes from my personal experience. I was biopsied for short-segment BE, and because it came up on my health record, it increased my life insurance premiums. This was because I was identified as having the risk profile of, essentially, an otherwise healthy smoker.
Dr Nicholas J. Shaheen and colleagues published a study several years ago showing that many insurance companies would not certify young, otherwise healthy people once diagnosed with BE. This is something to be aware of when you start to screen for BE, especially among younger patients.
A Novel Biologic for Eosinophilic Esophagitis
The next study presented results from a randomized, placebo-controlled, phase 3 study of cendakimab, a biologic agent in development for the treatment of eosinophilic esophagitis (EoE).
Dupilumab, which is an anti–interleukin (IL)-4 antibody, is the first treatment approved by the US Food and Drug Administration (FDA) for the treatment of EoE. Cendakimab, in turn, is a monoclonal antibody that neutralizes IL-13, a cytokine that plays a key role in EoE.
The study was led by Dr Evan Dellon from the University of North Carolina at Chapel Hill. Dellon and colleagues analyzed two different dosing regimens of cendakimab — 360 mg once weekly for 48 weeks, or 360 mg once weekly for 24 weeks followed by 360 mg every other week for 24 weeks — vs placebo for 48 weeks.
There was a significant effect for both cendakimab regimens in terms of symptom improvement and histologic response. There wasn’t much difference between participants that maintained once-weekly dosing and those who switched over to receive cendakimab every other week at 24 weeks. Only a minimal number of serious adverse events leading to discontinuation were noted in the study, with no notable difference between the treatment groups.
I think we’ll probably see this drug become available to us soon after it goes through the FDA review process, at which point it will add to our ability to use formative biologics in patients with EoE.
No Clear Benefit to Adding Bezlotoxumab to Fecal Microbiota Transplantation
Next was a very interesting study, and I think a clinically relevant one, about using fecal microbiota transplantation (FMT) alone or in combination with bezlotoxumab in patients with inflammatory bowel disease (IBD) with recurrent Clostridioides difficile infection.
Bezlotoxumab is a fully human monoclonal antibody that binds to C difficile toxin B. This drug has been studied and is approved for use, but it’s also extremely expensive, at a cost of approximately $4000 per dose.
Patients with IBD were eligible for inclusion if they had had two or more episodes of C difficile infection. They were then randomized in a 1:1 ration to receive either a single infusion of bezlotoxumab or placebo prior to FMT. The primary endpoint was C difficile infection recurrence within 8 weeks, which was defined as diarrhea plus a positive enzyme immunoassay toxin test. The secondary outcome was C difficile decolonization following treatment.
Researchers observed no statistically significant difference between the two cohorts. Steroid use prior to FMT significantly increased the risk for ongoing C difficile colonization (P =.03).
In summary, this is a case where it doesn’t seem that more is better. Bezlotoxumab didn’t add much, which calls into question the justification for its combined use with FMT.
Additional Positive Data for Seladelpar in Primary Biliary Cholangitis and Cirrhosis
Reassuring findings were presented on seladelpar, which was granted accelerated approval by the FDA in August.
Seladelpar is a selective peroxisome proliferator–activated receptor delta agonist that works in biliary cholangitis by regulating the genes involved in blocking biliary bile acid synthesis and controlling inflammation and fibrosis.
Results from the phase 3 RESPONSE trial were published in The New England Journal of Medicine in February reporting on the use of seladelpar in primary biliary cholangitis.
Whereas the RESPONSE trial removed decompensated patients, the ongoing phase 3 ASSURE trial results presented at this year’s meeting included patients with compensated cirrhosis. Approximately 94% of the patients in this study had Child-Pugh class A and 6% had class B cirrhosis. Eligibility required that patients had an inadequate response or were intolerant to ursodeoxycholic acid. Patients were administered open-label seladelpar 10 mg orally daily and followed for up to 1 year.
The good news is that there were no safety signals, which is reassuring news for our patients with compensated cirrhosis.
Advantages to Respiratory Syncytial Virus Vaccination in IBD
Another study that offered results certainly worthy of attention dealt with vaccination recommendations in patients with IBD.
Vaccination for respiratory syncytial virus (RSV) is now available in the United States. Its use was recommended for patients with IBD as early as 2021 per the Canadian Association of Gastroenterology’s clinical practice guideline, which discusses both live and nonlive vaccines. We should be aggressive in recommending this vaccine to our patients with IBD, but we haven’t really had one until recently.
Researchers behind this retrospective cohort study used the TriNetX database, which includes over 100 million unique patient charts. They identified patients with IBD, who were then divided into two groups according to whether they received the RSV vaccine or not.
Although this analysis was conducted in patients > 60 years of age, the US Centers for Disease Control and Prevention recommends RSV vaccination for all those over the age of 75 years, as well as for those 60-74 years old based on severity of risk.
For the primary endpoint of risk for RSV pneumonia, the OR was dramatically better in those who were vaccinated, with an approximately 80% risk reduction. Additionally, vaccinated patients experienced risk reductions of approximately 60% for acute respiratory failure, 50% for hospital inpatient admission, and 70% for requiring intensive care unit services.
This is a strong study showing not only that RSV vaccine did not exacerbate IBD but also that it improved outcomes in these patients. There’s a live-attenuated RSV vaccination that’s administered intranasally, which wouldn’t be used in your biologic or immunosuppressed patients with IBD, but the intramuscularly administered RSV vaccine doesn’t have any risk.
I think we can immediately begin recommending the RSV vaccine for our patients with IBD, particularly in those 60 years of age or older.
The Impact of Palliative Care Consultations in Decompensated Cirrhosis
The next study I’d like to highlight offers important data on the impact of palliative care consultation on 30- and 90-day readmission in patients with decompensated cirrhosis, which is a major cause of morbidity and mortality.
Researchers queried the National Readmissions Database over a 10-year period (2010-2019) to determine whether patients received a palliative care consult during index admission. They drew on a population of over 1.6 million patients admitted with decompensated cirrhosis.
Of this group, only 7.4% received a palliative care consultation at the index admission. But if they had this consultation, it was associated with a dramatic effect on readmission at 30 and 90 days. There was statistically significant risk reduction of approximately 70% for both 30- and 90-day readmission compared with those who didn’t receive the palliative consult (P <.001).
The take-home message here is to get a palliative care consult with these patients when they come in. Your hospital will unquestionably experience value in this reduction in readmission, especially considering that readmission within 30 days may not even be covered. Look at these results and start to take advantage of this valuable consultation.
Auxora: A Novel Treatment for Acute Pancreatitis
The last study for discussion offered very interesting data related to a drug called Auxora, a calcium release–activated calcium-channel inhibitor.
There is growing data that overactive calcium release–activated calcium channels aggravate acute pancreatitis and accelerate systemic inflammatory response syndrome (SIRS).
Acute pancreatitis with necrosis encompasses both local and systemic inflammation and is associated with significant mortality and morbidity. It is estimated that among patients with acute pancreatitis, 20%-30% have pancreatic necrosis, 30% develop infection, and 25% develop organ failure.
The presence of SIRS seems to herald the activation of these complex inflammatory pathways, which then leads to organ failure and necrosis, which can potentially be stemmed through this calcium channel inhibitor. Phase 2 studies of Auxora found that its use was associated with significant reduction in the risk for progression.
This subsequent phase 3 study looked at patients with acute pancreatitis and accompanying grade ≥ 2 SIRS criteria. They were randomized to receive placebo or Auxora at doses of 2 mg/kg, 1 mg/kg, or 0.5 mg/kg, which was administered intravenously over 4 hours for 3 consecutive days.
The primary endpoint was time to solid food tolerance, which was defined as eating ≥ 50% of a ≥ 500-calorie low-fat solid meal without increased abdominal pain or emesis, which is an important target because we always aim for enteral nutrition in patients with acute pancreatitis. The key secondary endpoint was severe respiratory failure, which was defined as invasive mechanical ventilation or ≥ 48 hours of either high-flow nasal cannula or noninvasive mechanical ventilation.
The primary endpoint was dramatically improved among those receiving Auxora, who achieved early onset of refeed. It appears that the high-dose 2 mg/kg may be the most beneficial in achieving improvement.
There were no patients with suspected or unexpected adverse events in the study population. Additionally, no patients receiving Auxora at any dose level went on to develop respiratory failure.
The present results show that Auxora decreases the time for solid food tolerance, as well as the rates of respiratory failure and necrotizing pancreatitis in patients presenting with two or more SIRS criteria. We’ll certainly look forward to more data, but it provides hope for a new treatment for acute pancreatitis.
Some of the take-home messages I presented are actionable now, whereas for others, we’ll have to wait and see what the final data show as well as the results of ongoing FDA approval before applying them.
Dr Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Virginia, and a past president of the American College of Gastroenterology. He reported serving in an advisory position with ISOTHRIVE. This transcript has been edited for clarity.
A version of this article first appeared on Medscape.com.
I’m just back from the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting in Philadelphia, Pennsylvania.
In part 2 of this series, I’m offering my highlights from this year’s meeting. (Part 1 is available here.) They are not presented in any particular order, but instead I am sharing what I found to be the most exciting among the thousands of abstracts and presentations.
Performing Capsule Endoscopy in Patients Taking GLP-1s
We’ve heard a lot about glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and the possibility that they might contribute to an increased risk for retained gastric contents and aspiration during endoscopy.
In the first study I’d like to highlight, researchers from the Mayo Clinic in Jacksonville, Florida, investigated video capsule endoscopy in patients with diabetes who were taking GLP-1 RAs vs a control group with diabetes not taking GLP-1 Ras. Patients in this retrospective matched cohort study were well balanced for demographics and diabetes-related characteristics.
Researchers found that in 7% of the 68 patients in the GLP-1 RA cohort, the video capsule endoscopy actually failed to pass through the stomach, whereas it passed successfully in all 68 patients in the control group (P =.06). The GLP-1 RA cohort had a longer transit time by a factor of almost four times (P <.001).
Multivariate analysis also showed that gastric transit time was approximately 80 minutes longer in the GLP-1 RA cohort (P <.001). Interestingly, 23.5% (16 of 68 patients) in the GLP-1 RA group experienced incomplete passage of the video capsule endoscopy through the small intestine, which was significantly higher than the proportion observed in the control group (4.4%; P <.01).
We need to look at potential strategies to mitigate these effects. Be aware of these results as you perform capsule endoscopy in patients taking GLP-1 RAs.
Barrett Esophagus On the Rise in the Young
The second study that caught my eye revealed the increasing incidence of young-onset Barrett esophagus (BE).
This population-based study used data obtained from TriNetX, a multi-institutional national database that offers a composite of health records from 88 healthcare organizations. Eligible patients had to have a negative upper esophagogastroduodenoscopy for BE prior to subsequently developing BE. Researchers stratified patients as to whether they were younger (< 50 years) or older (≥ 50 years), with further age ranges analyzed within those groups.
Young-onset BE accounted for 20% of all incident cases. The majority (94%) had nondysplastic BE. The incidence rate was not significantly different depending on whether patients were in the 45- to 49-year or 50- to 54-year age group.
Regression analysis revealed that there was a significantly increased trend for young-onset BE with hiatal hernia (odds ratio [OR], 2.6), smoking (OR, 2.3), White race (OR, 2.3), obstructive sleep apnea (OR, 2.2), male gender (OR, 2.0), and — at relatively lower risk levels — gastroesophageal reflux disease symptoms (OR, 1.2) and body mass index (OR, 1.1). The researchers did not analyze patients based on the presence of obesity, which is one of the risk factors for BE mentioned in national guidelines.
Results also showed that 6% of those with young-onset BE had BE-related neoplasia.
ACG guidelines recommend screening for BE beginning at age 50 in those with some of the risk factors noted in this study, including the presence of chronic gastroesophageal reflux disease symptoms. However, doing so may not capture the growing number of patients with young-onset BE.
We’ve seen a similar rise in rates of young-onset colorectal cancer, which has caused us to reevaluate our screening methods. Maybe we should do this for BE as well, specifically for patients presenting with these risk factors.
There’s a caveat to be aware of, which comes from my personal experience. I was biopsied for short-segment BE, and because it came up on my health record, it increased my life insurance premiums. This was because I was identified as having the risk profile of, essentially, an otherwise healthy smoker.
Dr Nicholas J. Shaheen and colleagues published a study several years ago showing that many insurance companies would not certify young, otherwise healthy people once diagnosed with BE. This is something to be aware of when you start to screen for BE, especially among younger patients.
A Novel Biologic for Eosinophilic Esophagitis
The next study presented results from a randomized, placebo-controlled, phase 3 study of cendakimab, a biologic agent in development for the treatment of eosinophilic esophagitis (EoE).
Dupilumab, which is an anti–interleukin (IL)-4 antibody, is the first treatment approved by the US Food and Drug Administration (FDA) for the treatment of EoE. Cendakimab, in turn, is a monoclonal antibody that neutralizes IL-13, a cytokine that plays a key role in EoE.
The study was led by Dr Evan Dellon from the University of North Carolina at Chapel Hill. Dellon and colleagues analyzed two different dosing regimens of cendakimab — 360 mg once weekly for 48 weeks, or 360 mg once weekly for 24 weeks followed by 360 mg every other week for 24 weeks — vs placebo for 48 weeks.
There was a significant effect for both cendakimab regimens in terms of symptom improvement and histologic response. There wasn’t much difference between participants that maintained once-weekly dosing and those who switched over to receive cendakimab every other week at 24 weeks. Only a minimal number of serious adverse events leading to discontinuation were noted in the study, with no notable difference between the treatment groups.
I think we’ll probably see this drug become available to us soon after it goes through the FDA review process, at which point it will add to our ability to use formative biologics in patients with EoE.
No Clear Benefit to Adding Bezlotoxumab to Fecal Microbiota Transplantation
Next was a very interesting study, and I think a clinically relevant one, about using fecal microbiota transplantation (FMT) alone or in combination with bezlotoxumab in patients with inflammatory bowel disease (IBD) with recurrent Clostridioides difficile infection.
Bezlotoxumab is a fully human monoclonal antibody that binds to C difficile toxin B. This drug has been studied and is approved for use, but it’s also extremely expensive, at a cost of approximately $4000 per dose.
Patients with IBD were eligible for inclusion if they had had two or more episodes of C difficile infection. They were then randomized in a 1:1 ration to receive either a single infusion of bezlotoxumab or placebo prior to FMT. The primary endpoint was C difficile infection recurrence within 8 weeks, which was defined as diarrhea plus a positive enzyme immunoassay toxin test. The secondary outcome was C difficile decolonization following treatment.
Researchers observed no statistically significant difference between the two cohorts. Steroid use prior to FMT significantly increased the risk for ongoing C difficile colonization (P =.03).
In summary, this is a case where it doesn’t seem that more is better. Bezlotoxumab didn’t add much, which calls into question the justification for its combined use with FMT.
Additional Positive Data for Seladelpar in Primary Biliary Cholangitis and Cirrhosis
Reassuring findings were presented on seladelpar, which was granted accelerated approval by the FDA in August.
Seladelpar is a selective peroxisome proliferator–activated receptor delta agonist that works in biliary cholangitis by regulating the genes involved in blocking biliary bile acid synthesis and controlling inflammation and fibrosis.
Results from the phase 3 RESPONSE trial were published in The New England Journal of Medicine in February reporting on the use of seladelpar in primary biliary cholangitis.
Whereas the RESPONSE trial removed decompensated patients, the ongoing phase 3 ASSURE trial results presented at this year’s meeting included patients with compensated cirrhosis. Approximately 94% of the patients in this study had Child-Pugh class A and 6% had class B cirrhosis. Eligibility required that patients had an inadequate response or were intolerant to ursodeoxycholic acid. Patients were administered open-label seladelpar 10 mg orally daily and followed for up to 1 year.
The good news is that there were no safety signals, which is reassuring news for our patients with compensated cirrhosis.
Advantages to Respiratory Syncytial Virus Vaccination in IBD
Another study that offered results certainly worthy of attention dealt with vaccination recommendations in patients with IBD.
Vaccination for respiratory syncytial virus (RSV) is now available in the United States. Its use was recommended for patients with IBD as early as 2021 per the Canadian Association of Gastroenterology’s clinical practice guideline, which discusses both live and nonlive vaccines. We should be aggressive in recommending this vaccine to our patients with IBD, but we haven’t really had one until recently.
Researchers behind this retrospective cohort study used the TriNetX database, which includes over 100 million unique patient charts. They identified patients with IBD, who were then divided into two groups according to whether they received the RSV vaccine or not.
Although this analysis was conducted in patients > 60 years of age, the US Centers for Disease Control and Prevention recommends RSV vaccination for all those over the age of 75 years, as well as for those 60-74 years old based on severity of risk.
For the primary endpoint of risk for RSV pneumonia, the OR was dramatically better in those who were vaccinated, with an approximately 80% risk reduction. Additionally, vaccinated patients experienced risk reductions of approximately 60% for acute respiratory failure, 50% for hospital inpatient admission, and 70% for requiring intensive care unit services.
This is a strong study showing not only that RSV vaccine did not exacerbate IBD but also that it improved outcomes in these patients. There’s a live-attenuated RSV vaccination that’s administered intranasally, which wouldn’t be used in your biologic or immunosuppressed patients with IBD, but the intramuscularly administered RSV vaccine doesn’t have any risk.
I think we can immediately begin recommending the RSV vaccine for our patients with IBD, particularly in those 60 years of age or older.
The Impact of Palliative Care Consultations in Decompensated Cirrhosis
The next study I’d like to highlight offers important data on the impact of palliative care consultation on 30- and 90-day readmission in patients with decompensated cirrhosis, which is a major cause of morbidity and mortality.
Researchers queried the National Readmissions Database over a 10-year period (2010-2019) to determine whether patients received a palliative care consult during index admission. They drew on a population of over 1.6 million patients admitted with decompensated cirrhosis.
Of this group, only 7.4% received a palliative care consultation at the index admission. But if they had this consultation, it was associated with a dramatic effect on readmission at 30 and 90 days. There was statistically significant risk reduction of approximately 70% for both 30- and 90-day readmission compared with those who didn’t receive the palliative consult (P <.001).
The take-home message here is to get a palliative care consult with these patients when they come in. Your hospital will unquestionably experience value in this reduction in readmission, especially considering that readmission within 30 days may not even be covered. Look at these results and start to take advantage of this valuable consultation.
Auxora: A Novel Treatment for Acute Pancreatitis
The last study for discussion offered very interesting data related to a drug called Auxora, a calcium release–activated calcium-channel inhibitor.
There is growing data that overactive calcium release–activated calcium channels aggravate acute pancreatitis and accelerate systemic inflammatory response syndrome (SIRS).
Acute pancreatitis with necrosis encompasses both local and systemic inflammation and is associated with significant mortality and morbidity. It is estimated that among patients with acute pancreatitis, 20%-30% have pancreatic necrosis, 30% develop infection, and 25% develop organ failure.
The presence of SIRS seems to herald the activation of these complex inflammatory pathways, which then leads to organ failure and necrosis, which can potentially be stemmed through this calcium channel inhibitor. Phase 2 studies of Auxora found that its use was associated with significant reduction in the risk for progression.
This subsequent phase 3 study looked at patients with acute pancreatitis and accompanying grade ≥ 2 SIRS criteria. They were randomized to receive placebo or Auxora at doses of 2 mg/kg, 1 mg/kg, or 0.5 mg/kg, which was administered intravenously over 4 hours for 3 consecutive days.
The primary endpoint was time to solid food tolerance, which was defined as eating ≥ 50% of a ≥ 500-calorie low-fat solid meal without increased abdominal pain or emesis, which is an important target because we always aim for enteral nutrition in patients with acute pancreatitis. The key secondary endpoint was severe respiratory failure, which was defined as invasive mechanical ventilation or ≥ 48 hours of either high-flow nasal cannula or noninvasive mechanical ventilation.
The primary endpoint was dramatically improved among those receiving Auxora, who achieved early onset of refeed. It appears that the high-dose 2 mg/kg may be the most beneficial in achieving improvement.
There were no patients with suspected or unexpected adverse events in the study population. Additionally, no patients receiving Auxora at any dose level went on to develop respiratory failure.
The present results show that Auxora decreases the time for solid food tolerance, as well as the rates of respiratory failure and necrotizing pancreatitis in patients presenting with two or more SIRS criteria. We’ll certainly look forward to more data, but it provides hope for a new treatment for acute pancreatitis.
Some of the take-home messages I presented are actionable now, whereas for others, we’ll have to wait and see what the final data show as well as the results of ongoing FDA approval before applying them.
Dr Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Virginia, and a past president of the American College of Gastroenterology. He reported serving in an advisory position with ISOTHRIVE. This transcript has been edited for clarity.
A version of this article first appeared on Medscape.com.
Weight Loss Treatments Beyond the Reach of Many in Need
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
FROM OBESITY WEEK 2024
Endoscopic Sleeve Gastroplasty Yields Durable Weight Loss at 10 Years
PHILADELPHIA —
“The procedure is dependable and safe and should be considered among individuals who have not attained their desired results through lifestyle medications and those who are not eligible for or choose not to undergo bariatric procedures,” said Ali Lahooti, with the Department of Gastroenterology and Hepatology, Weill Cornell Medical College, New York City. He presented his research at the annual meeting of the American College of Gastroenterology (ACG).
Obesity is a growing global health challenge. Lifestyle modification as a standalone therapy has limited effectiveness achieving weight loss. Pharmacotherapies are more efficacious, but they’re also associated with higher costs of and risk for side effects, leading to lower rates of compliance, Lahooti explained.
Bariatric surgery remains the most effective therapy for management of obesity and improvement of comorbid conditions, yet < 1% of candidates undergo a surgical intervention either because of access, cost, or fear of the procedure.
“Endoscopic treatments for obesity, such as ESG, can potentially fill this gap by combining durable weight loss with lower risk and costs,” Lahooti said.
He and his colleagues assessed outcomes out to 10 years in 404 patients (mean age, 45 years; 76% women; mean body mass index, 37.3) who underwent ESG between 2013 and 2024 at a single large tertiary hospital.
Out of the 404 patients, 397, 335, 249, and 110 patients were eligible for 1-, 3-, 5-, and 10-year follow-up, with complete follow-up rates of 85%, 66%, 79%, and 62%, respectively.
The primary outcome was weight loss at 10 years after ESG reported at percent total body weight loss (%TBWL).
At 10 years, mean %TBWL (the primary outcome) was 10.5% — with 53% of patients maintaining at least 5% TBWL and 42% maintaining at least 10% weight loss, Lahooti reported.
ESG had a favorable safety profile; 20% of patients experienced mild abdominal pain, constipation, heartburn, and nausea after the procedure that typically resolved within 2 weeks of the procedure.
“There were a total of three moderate adverse events — two perigastric leaks, one repaired endoscopically, and another that only required antibiotics,” Lahooti reported. There were no severe or fatal adverse events.
About 11% of patients had endoscopic revision via retightening or resuturing at 10 years, the study team noted in their conference abstract.
Bariatric Surgery Remains Gold Standard
Lahooti shared that in his experience, some patients will need a revision at “about 40 months,” but at the same time, he’s seen some patients at 10 years “and their sutures are still in place.”
Session comoderator Shivangi Kothari, MD, with the Center for Advanced Therapeutic Endoscopy, University of Rochester Medical Center in New York, congratulated Lahooti for providing “robust” long-term data on ESG and said, “there is a need for more studies like this.”
In an interview, Ann M. Rogers, MD, president of the American Society for Metabolic and Bariatric Surgery, noted that bariatric surgery remains the “gold standard for weight loss and metabolic improvements,” with studies showing “around 30%” TWBL at 10 years, compared with about 10% at 10 years in this study.
Another key caveat, said Rogers, is that there are practical barriers to ESG; insurance typically does not cover the procedure because they view it as “cosmetic.”
The study had no commercial funding. Lahooti and Rogers had no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA —
“The procedure is dependable and safe and should be considered among individuals who have not attained their desired results through lifestyle medications and those who are not eligible for or choose not to undergo bariatric procedures,” said Ali Lahooti, with the Department of Gastroenterology and Hepatology, Weill Cornell Medical College, New York City. He presented his research at the annual meeting of the American College of Gastroenterology (ACG).
Obesity is a growing global health challenge. Lifestyle modification as a standalone therapy has limited effectiveness achieving weight loss. Pharmacotherapies are more efficacious, but they’re also associated with higher costs of and risk for side effects, leading to lower rates of compliance, Lahooti explained.
Bariatric surgery remains the most effective therapy for management of obesity and improvement of comorbid conditions, yet < 1% of candidates undergo a surgical intervention either because of access, cost, or fear of the procedure.
“Endoscopic treatments for obesity, such as ESG, can potentially fill this gap by combining durable weight loss with lower risk and costs,” Lahooti said.
He and his colleagues assessed outcomes out to 10 years in 404 patients (mean age, 45 years; 76% women; mean body mass index, 37.3) who underwent ESG between 2013 and 2024 at a single large tertiary hospital.
Out of the 404 patients, 397, 335, 249, and 110 patients were eligible for 1-, 3-, 5-, and 10-year follow-up, with complete follow-up rates of 85%, 66%, 79%, and 62%, respectively.
The primary outcome was weight loss at 10 years after ESG reported at percent total body weight loss (%TBWL).
At 10 years, mean %TBWL (the primary outcome) was 10.5% — with 53% of patients maintaining at least 5% TBWL and 42% maintaining at least 10% weight loss, Lahooti reported.
ESG had a favorable safety profile; 20% of patients experienced mild abdominal pain, constipation, heartburn, and nausea after the procedure that typically resolved within 2 weeks of the procedure.
“There were a total of three moderate adverse events — two perigastric leaks, one repaired endoscopically, and another that only required antibiotics,” Lahooti reported. There were no severe or fatal adverse events.
About 11% of patients had endoscopic revision via retightening or resuturing at 10 years, the study team noted in their conference abstract.
Bariatric Surgery Remains Gold Standard
Lahooti shared that in his experience, some patients will need a revision at “about 40 months,” but at the same time, he’s seen some patients at 10 years “and their sutures are still in place.”
Session comoderator Shivangi Kothari, MD, with the Center for Advanced Therapeutic Endoscopy, University of Rochester Medical Center in New York, congratulated Lahooti for providing “robust” long-term data on ESG and said, “there is a need for more studies like this.”
In an interview, Ann M. Rogers, MD, president of the American Society for Metabolic and Bariatric Surgery, noted that bariatric surgery remains the “gold standard for weight loss and metabolic improvements,” with studies showing “around 30%” TWBL at 10 years, compared with about 10% at 10 years in this study.
Another key caveat, said Rogers, is that there are practical barriers to ESG; insurance typically does not cover the procedure because they view it as “cosmetic.”
The study had no commercial funding. Lahooti and Rogers had no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA —
“The procedure is dependable and safe and should be considered among individuals who have not attained their desired results through lifestyle medications and those who are not eligible for or choose not to undergo bariatric procedures,” said Ali Lahooti, with the Department of Gastroenterology and Hepatology, Weill Cornell Medical College, New York City. He presented his research at the annual meeting of the American College of Gastroenterology (ACG).
Obesity is a growing global health challenge. Lifestyle modification as a standalone therapy has limited effectiveness achieving weight loss. Pharmacotherapies are more efficacious, but they’re also associated with higher costs of and risk for side effects, leading to lower rates of compliance, Lahooti explained.
Bariatric surgery remains the most effective therapy for management of obesity and improvement of comorbid conditions, yet < 1% of candidates undergo a surgical intervention either because of access, cost, or fear of the procedure.
“Endoscopic treatments for obesity, such as ESG, can potentially fill this gap by combining durable weight loss with lower risk and costs,” Lahooti said.
He and his colleagues assessed outcomes out to 10 years in 404 patients (mean age, 45 years; 76% women; mean body mass index, 37.3) who underwent ESG between 2013 and 2024 at a single large tertiary hospital.
Out of the 404 patients, 397, 335, 249, and 110 patients were eligible for 1-, 3-, 5-, and 10-year follow-up, with complete follow-up rates of 85%, 66%, 79%, and 62%, respectively.
The primary outcome was weight loss at 10 years after ESG reported at percent total body weight loss (%TBWL).
At 10 years, mean %TBWL (the primary outcome) was 10.5% — with 53% of patients maintaining at least 5% TBWL and 42% maintaining at least 10% weight loss, Lahooti reported.
ESG had a favorable safety profile; 20% of patients experienced mild abdominal pain, constipation, heartburn, and nausea after the procedure that typically resolved within 2 weeks of the procedure.
“There were a total of three moderate adverse events — two perigastric leaks, one repaired endoscopically, and another that only required antibiotics,” Lahooti reported. There were no severe or fatal adverse events.
About 11% of patients had endoscopic revision via retightening or resuturing at 10 years, the study team noted in their conference abstract.
Bariatric Surgery Remains Gold Standard
Lahooti shared that in his experience, some patients will need a revision at “about 40 months,” but at the same time, he’s seen some patients at 10 years “and their sutures are still in place.”
Session comoderator Shivangi Kothari, MD, with the Center for Advanced Therapeutic Endoscopy, University of Rochester Medical Center in New York, congratulated Lahooti for providing “robust” long-term data on ESG and said, “there is a need for more studies like this.”
In an interview, Ann M. Rogers, MD, president of the American Society for Metabolic and Bariatric Surgery, noted that bariatric surgery remains the “gold standard for weight loss and metabolic improvements,” with studies showing “around 30%” TWBL at 10 years, compared with about 10% at 10 years in this study.
Another key caveat, said Rogers, is that there are practical barriers to ESG; insurance typically does not cover the procedure because they view it as “cosmetic.”
The study had no commercial funding. Lahooti and Rogers had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ACG 2024
GLP-1 Prescribing Decisions: Compounded or Brand-Name?
Both Eli Lilly and Novo Nordisk have asked the Food and Drug Administration (FDA) to place their GLP-1 medications, tirzepatide and semaglutide, on its Demonstrable Difficulties for Compounding or DDC Lists, which would prohibit compounding the medications. Lawsuits are another issue. The Outsourcing Facility Association, a trade group, filed a lawsuit against the FDA, calling on it to restore tirzepatide to the shortage list after the FDA removed it on October 2, despite pharmacies still experiencing shortages, according to the association. The FDA is reevaluating the decision and won’t take action against compounders in the interim, with a joint status report scheduled for November 21.
In the midst of the lawsuits and pending decisions, healthcare providers are taking a variety of approaches when they need to decide between compounded vs brand-name GLP-1s for obesity treatment. The Alliance for Pharmacy Compounding, another trade group, offers a number of suggestions for doctors faced with compound or brand-name decisions and has a website tool to be sure a compounding pharmacy meets standards.
According to the FDA, a drug may be compounded for a patient who can’t be treated with an FDA-approved medication, such as a patient who has an allergy to a certain ingredient and needs medication to be made without it, or for a medication that appears on the FDA Drug Shortages List.
Here’s how five healthcare providers make the decision.
Physicians Weigh in
Hard pass: “I have no experience with compounded formulations by choice,” said W. Timothy Garvey, MD, MACE, an obesity specialist and the Charles E. Butterworth Jr professor and university professor at the University of Alabama at Birmingham. “I think our patients deserve better.”
However, he acknowledged: “This is a difficult situation when there is a lack of access to medications patients need.” Even so, “online prescriptions [for compounded medications] are often done without an evaluation for obesity complications and related diseases and ongoing active management, making a complications-centric approach to care impossible.”
That’s not the optimal approach to treating obesity or other chronic diseases, he said in an interview.
Rather than prescribe compounded GLP-1s for weight loss, he said, other options exist. Among them: Prescribe Ozempic off label for obesity.
“Plus, we have a good first-generation obesity medication — phentermine/topiramate — that gets close to 10% weight loss on average in clinical trials that is available and less expensive.”
Other options, he said, are to switch to lower doses of the brand name that may be available until the treatment dose needed is out of shortage status or, the less desirable option, wait for availability, which means the patient may be off the medication for a month or more.
He acknowledged none of these options solves “the problem of high costs [for brand-name drugs] and lack of insurance coverage.”
In agreement is Caroline Apovian, MD, codirector of the Center for Weight Management and Wellness at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
“Doctors who are obesity medicine specialists like myself in academic centers do not prescribe compounded semaglutide or tirzepatide,” she said.
Many of the compounded prescriptions, she said, come from telehealth virtual–only companies interested in profits.
Brand names preferred: “Brand-name versions as far as I’m concerned are always preferred,” said Sarah Stombaugh, MD, an obesity medicine and family medicine physician in Charlottesville, Virginia. She terms it irresponsible for a prescriber to give a patient a compounded GLP-1 if the patient has prescription coverage and the brand name is available.
Her approach: She first checks the patients’ coverage. Do they have coverage for these medications for obesity? If so, she said, she will do a prior authorization to get the brand name approved. If a brand name is available but not covered, she explores other options. One is the cash pay option for Zepbound in vials. It’s more affordable than the typical $1000 cash price for the brand name GLP-1s but still pricey, at about $400-$549 for lower doses.
She looks at drug makers’ discount coupons, or whether a patient with a history of cardiovascular issues might qualify for coverage on Wegovy. Another option is to give the patient a prescription for Mounjaro or Ozempic to fill from a Canadian pharmacy for about $400 a month.
“I think a lot of people jump quickly to compounding,” she said.
She views it as a last resort and reminds other healthcare providers that the compounded medications aren’t cheap, either, typically costing $100-$500 a month depending on dosage. And, she said, “we have many who get the brand name for $25 a month [by using discount cards and insurance coverage].”
When prescribing a compounded medication is necessary, it’s important for healthcare providers to know that the quality of the compounding pharmacies varies greatly, Stombaugh said. A prescriber needs to pick the compounding pharmacy, not the patient, and needs to vet it, she said, asking about protocols it follows for sterility and for chemical analysis, for instance.
Stombaugh is hopeful that several new medications under study and now in phase 3 trials will soon provide enough competition to drive down the price of the current brand-name GLP-1s.
History of mistrust: Robert Dubin, MD, associate professor of research at the Pennington Biomedical Research Center at Louisiana State University, Baton Rouge, and program director for its obesity medicine fellowship, sees a role for compounding and has for several years, but acknowledged that many in his community are against it.
He estimates that about 75% of his colleagues in the Baton Rouge area are opposed to prescribing compounded GLP-1s. He chalks it up to a “track record of distrust,” based on reports of infractions called out by the FDA for some compounding pharmacies as well as physicians not being familiar with the process.
Dubin said he will prescribe a compounded medication if the brand name isn’t available. Cost is also a consideration. “If there’s not a problem with availability and there’s not a problem with cost, then why compound?”
For anyone considering prescribing compounded GLP-1s, he said, “The first step, I believe, is having a relationship with the compounding pharmacy. If you don’t have that, it could be very difficult. We don’t want to send people to a black hole, and we aren’t sure what is going to happen.” He urges colleagues to educate themselves about compounding pharmacies.
Official shortage list vs real world: “The official shortage list doesn’t always reflect the real world,” said Amanda Guarniere, NP, a nurse practitioner with a self-pay telehealth and in-person practice and director of growth for Collaborating Docs, a service based in Arlington, Virginia, that pairs nurse practitioners with supervising physicians.
“When Zepbound and Mounjaro came off the [FDA] shortage list a few weeks ago, patients were still calling around and couldn’t find it in their county.”
It’s important to vet compounding pharmacies before dealing with them, she said.
“I have accounts with two compounding pharmacies who I trust,” she said. She’s researched their quality control provided and is comfortable with their standards. When appropriate, the cost savings of compounded GLP-1s over brand name is “pretty significant,” with compounded medicine costs about 20% of brand-name costs.
When the brand name is back, how might a prescriber still write a prescription for a compounded version? “Compounded versions are typically compounded with something else,” Guarniere said.
For instance, compounded tirzepatide often includes vitamin B12 and other B vitamins, which may help with the side effect of nausea. So a prescriber might decide that the compounded prescription is more appropriate and justified because the patient would benefit from the additive, she said.
What Else to Know: Alliance Views
On November 7, the Alliance for Pharmacy Compounding, a trade group, responded to Lilly’s request to put tirzepatide on the “demonstrably difficult to compound (DDC)” list, asking the FDA to deny it. The group also took issue with criticism of compounded GLP-1s from the Novo Nordisk CEO.
The alliance offers perspective and a number of suggestions for doctors faced with compound or brand-name decisions, including using its website tool called “Is It Legit?” to be sure a compounding pharmacy meets standards.
“When these [GLP-1] drugs came out, I don’t think anybody anticipated them to be such blockbusters,” said Tenille Davis, PharmD, a board-certified sterile compounding pharmacist and chief advocacy officer for the Alliance for Pharmacy Compounding. Shortages have plagued the GLP-1s since their approvals, with Wegovy approved on June 4, 2021, and Eli Lilly’s Zepbound on November 8, 2023.
The proposed “Demonstrably Difficult to Compound (DDC)” rule, published in March 2024, aims to finalize the six criteria for a medication to land on that list, she said. No drugs are currently on this list, Davis said.
For now, she said, prescribers faced with a compound vs brand-name decision should be aware of the pending lawsuit concerning tirzepatide and that the FDA has said it will cease most enforcement action until 2 weeks after it reviews the decision to remove the medication from the shortage list and issues a new determination.
Davis suggests prescribers have conversations now with their patients about their options and to tell them it may be necessary to transition from the compounded medicines to brand name. “This may require insurance prior authorizations, so if they are going to transition from compounded tirzepatide to Zepbound and Mounjaro, it’s good to start the process sooner rather than later so there isn’t an interruption in care.”
Earlier in 2024, the three leading obesity organizations issued a statement, advising patients that they do not recommend the use of compounded GLP-1s.
Garvey is a consultant on advisory boards for Eli Lilly, Novo Nordisk, and several other pharmaceutical companies. Apovian had no relevant disclosures. Stombaugh, Dubin, and Guarniere had no disclosures.
A version of this article appeared on Medscape.com.
Both Eli Lilly and Novo Nordisk have asked the Food and Drug Administration (FDA) to place their GLP-1 medications, tirzepatide and semaglutide, on its Demonstrable Difficulties for Compounding or DDC Lists, which would prohibit compounding the medications. Lawsuits are another issue. The Outsourcing Facility Association, a trade group, filed a lawsuit against the FDA, calling on it to restore tirzepatide to the shortage list after the FDA removed it on October 2, despite pharmacies still experiencing shortages, according to the association. The FDA is reevaluating the decision and won’t take action against compounders in the interim, with a joint status report scheduled for November 21.
In the midst of the lawsuits and pending decisions, healthcare providers are taking a variety of approaches when they need to decide between compounded vs brand-name GLP-1s for obesity treatment. The Alliance for Pharmacy Compounding, another trade group, offers a number of suggestions for doctors faced with compound or brand-name decisions and has a website tool to be sure a compounding pharmacy meets standards.
According to the FDA, a drug may be compounded for a patient who can’t be treated with an FDA-approved medication, such as a patient who has an allergy to a certain ingredient and needs medication to be made without it, or for a medication that appears on the FDA Drug Shortages List.
Here’s how five healthcare providers make the decision.
Physicians Weigh in
Hard pass: “I have no experience with compounded formulations by choice,” said W. Timothy Garvey, MD, MACE, an obesity specialist and the Charles E. Butterworth Jr professor and university professor at the University of Alabama at Birmingham. “I think our patients deserve better.”
However, he acknowledged: “This is a difficult situation when there is a lack of access to medications patients need.” Even so, “online prescriptions [for compounded medications] are often done without an evaluation for obesity complications and related diseases and ongoing active management, making a complications-centric approach to care impossible.”
That’s not the optimal approach to treating obesity or other chronic diseases, he said in an interview.
Rather than prescribe compounded GLP-1s for weight loss, he said, other options exist. Among them: Prescribe Ozempic off label for obesity.
“Plus, we have a good first-generation obesity medication — phentermine/topiramate — that gets close to 10% weight loss on average in clinical trials that is available and less expensive.”
Other options, he said, are to switch to lower doses of the brand name that may be available until the treatment dose needed is out of shortage status or, the less desirable option, wait for availability, which means the patient may be off the medication for a month or more.
He acknowledged none of these options solves “the problem of high costs [for brand-name drugs] and lack of insurance coverage.”
In agreement is Caroline Apovian, MD, codirector of the Center for Weight Management and Wellness at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
“Doctors who are obesity medicine specialists like myself in academic centers do not prescribe compounded semaglutide or tirzepatide,” she said.
Many of the compounded prescriptions, she said, come from telehealth virtual–only companies interested in profits.
Brand names preferred: “Brand-name versions as far as I’m concerned are always preferred,” said Sarah Stombaugh, MD, an obesity medicine and family medicine physician in Charlottesville, Virginia. She terms it irresponsible for a prescriber to give a patient a compounded GLP-1 if the patient has prescription coverage and the brand name is available.
Her approach: She first checks the patients’ coverage. Do they have coverage for these medications for obesity? If so, she said, she will do a prior authorization to get the brand name approved. If a brand name is available but not covered, she explores other options. One is the cash pay option for Zepbound in vials. It’s more affordable than the typical $1000 cash price for the brand name GLP-1s but still pricey, at about $400-$549 for lower doses.
She looks at drug makers’ discount coupons, or whether a patient with a history of cardiovascular issues might qualify for coverage on Wegovy. Another option is to give the patient a prescription for Mounjaro or Ozempic to fill from a Canadian pharmacy for about $400 a month.
“I think a lot of people jump quickly to compounding,” she said.
She views it as a last resort and reminds other healthcare providers that the compounded medications aren’t cheap, either, typically costing $100-$500 a month depending on dosage. And, she said, “we have many who get the brand name for $25 a month [by using discount cards and insurance coverage].”
When prescribing a compounded medication is necessary, it’s important for healthcare providers to know that the quality of the compounding pharmacies varies greatly, Stombaugh said. A prescriber needs to pick the compounding pharmacy, not the patient, and needs to vet it, she said, asking about protocols it follows for sterility and for chemical analysis, for instance.
Stombaugh is hopeful that several new medications under study and now in phase 3 trials will soon provide enough competition to drive down the price of the current brand-name GLP-1s.
History of mistrust: Robert Dubin, MD, associate professor of research at the Pennington Biomedical Research Center at Louisiana State University, Baton Rouge, and program director for its obesity medicine fellowship, sees a role for compounding and has for several years, but acknowledged that many in his community are against it.
He estimates that about 75% of his colleagues in the Baton Rouge area are opposed to prescribing compounded GLP-1s. He chalks it up to a “track record of distrust,” based on reports of infractions called out by the FDA for some compounding pharmacies as well as physicians not being familiar with the process.
Dubin said he will prescribe a compounded medication if the brand name isn’t available. Cost is also a consideration. “If there’s not a problem with availability and there’s not a problem with cost, then why compound?”
For anyone considering prescribing compounded GLP-1s, he said, “The first step, I believe, is having a relationship with the compounding pharmacy. If you don’t have that, it could be very difficult. We don’t want to send people to a black hole, and we aren’t sure what is going to happen.” He urges colleagues to educate themselves about compounding pharmacies.
Official shortage list vs real world: “The official shortage list doesn’t always reflect the real world,” said Amanda Guarniere, NP, a nurse practitioner with a self-pay telehealth and in-person practice and director of growth for Collaborating Docs, a service based in Arlington, Virginia, that pairs nurse practitioners with supervising physicians.
“When Zepbound and Mounjaro came off the [FDA] shortage list a few weeks ago, patients were still calling around and couldn’t find it in their county.”
It’s important to vet compounding pharmacies before dealing with them, she said.
“I have accounts with two compounding pharmacies who I trust,” she said. She’s researched their quality control provided and is comfortable with their standards. When appropriate, the cost savings of compounded GLP-1s over brand name is “pretty significant,” with compounded medicine costs about 20% of brand-name costs.
When the brand name is back, how might a prescriber still write a prescription for a compounded version? “Compounded versions are typically compounded with something else,” Guarniere said.
For instance, compounded tirzepatide often includes vitamin B12 and other B vitamins, which may help with the side effect of nausea. So a prescriber might decide that the compounded prescription is more appropriate and justified because the patient would benefit from the additive, she said.
What Else to Know: Alliance Views
On November 7, the Alliance for Pharmacy Compounding, a trade group, responded to Lilly’s request to put tirzepatide on the “demonstrably difficult to compound (DDC)” list, asking the FDA to deny it. The group also took issue with criticism of compounded GLP-1s from the Novo Nordisk CEO.
The alliance offers perspective and a number of suggestions for doctors faced with compound or brand-name decisions, including using its website tool called “Is It Legit?” to be sure a compounding pharmacy meets standards.
“When these [GLP-1] drugs came out, I don’t think anybody anticipated them to be such blockbusters,” said Tenille Davis, PharmD, a board-certified sterile compounding pharmacist and chief advocacy officer for the Alliance for Pharmacy Compounding. Shortages have plagued the GLP-1s since their approvals, with Wegovy approved on June 4, 2021, and Eli Lilly’s Zepbound on November 8, 2023.
The proposed “Demonstrably Difficult to Compound (DDC)” rule, published in March 2024, aims to finalize the six criteria for a medication to land on that list, she said. No drugs are currently on this list, Davis said.
For now, she said, prescribers faced with a compound vs brand-name decision should be aware of the pending lawsuit concerning tirzepatide and that the FDA has said it will cease most enforcement action until 2 weeks after it reviews the decision to remove the medication from the shortage list and issues a new determination.
Davis suggests prescribers have conversations now with their patients about their options and to tell them it may be necessary to transition from the compounded medicines to brand name. “This may require insurance prior authorizations, so if they are going to transition from compounded tirzepatide to Zepbound and Mounjaro, it’s good to start the process sooner rather than later so there isn’t an interruption in care.”
Earlier in 2024, the three leading obesity organizations issued a statement, advising patients that they do not recommend the use of compounded GLP-1s.
Garvey is a consultant on advisory boards for Eli Lilly, Novo Nordisk, and several other pharmaceutical companies. Apovian had no relevant disclosures. Stombaugh, Dubin, and Guarniere had no disclosures.
A version of this article appeared on Medscape.com.
Both Eli Lilly and Novo Nordisk have asked the Food and Drug Administration (FDA) to place their GLP-1 medications, tirzepatide and semaglutide, on its Demonstrable Difficulties for Compounding or DDC Lists, which would prohibit compounding the medications. Lawsuits are another issue. The Outsourcing Facility Association, a trade group, filed a lawsuit against the FDA, calling on it to restore tirzepatide to the shortage list after the FDA removed it on October 2, despite pharmacies still experiencing shortages, according to the association. The FDA is reevaluating the decision and won’t take action against compounders in the interim, with a joint status report scheduled for November 21.
In the midst of the lawsuits and pending decisions, healthcare providers are taking a variety of approaches when they need to decide between compounded vs brand-name GLP-1s for obesity treatment. The Alliance for Pharmacy Compounding, another trade group, offers a number of suggestions for doctors faced with compound or brand-name decisions and has a website tool to be sure a compounding pharmacy meets standards.
According to the FDA, a drug may be compounded for a patient who can’t be treated with an FDA-approved medication, such as a patient who has an allergy to a certain ingredient and needs medication to be made without it, or for a medication that appears on the FDA Drug Shortages List.
Here’s how five healthcare providers make the decision.
Physicians Weigh in
Hard pass: “I have no experience with compounded formulations by choice,” said W. Timothy Garvey, MD, MACE, an obesity specialist and the Charles E. Butterworth Jr professor and university professor at the University of Alabama at Birmingham. “I think our patients deserve better.”
However, he acknowledged: “This is a difficult situation when there is a lack of access to medications patients need.” Even so, “online prescriptions [for compounded medications] are often done without an evaluation for obesity complications and related diseases and ongoing active management, making a complications-centric approach to care impossible.”
That’s not the optimal approach to treating obesity or other chronic diseases, he said in an interview.
Rather than prescribe compounded GLP-1s for weight loss, he said, other options exist. Among them: Prescribe Ozempic off label for obesity.
“Plus, we have a good first-generation obesity medication — phentermine/topiramate — that gets close to 10% weight loss on average in clinical trials that is available and less expensive.”
Other options, he said, are to switch to lower doses of the brand name that may be available until the treatment dose needed is out of shortage status or, the less desirable option, wait for availability, which means the patient may be off the medication for a month or more.
He acknowledged none of these options solves “the problem of high costs [for brand-name drugs] and lack of insurance coverage.”
In agreement is Caroline Apovian, MD, codirector of the Center for Weight Management and Wellness at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
“Doctors who are obesity medicine specialists like myself in academic centers do not prescribe compounded semaglutide or tirzepatide,” she said.
Many of the compounded prescriptions, she said, come from telehealth virtual–only companies interested in profits.
Brand names preferred: “Brand-name versions as far as I’m concerned are always preferred,” said Sarah Stombaugh, MD, an obesity medicine and family medicine physician in Charlottesville, Virginia. She terms it irresponsible for a prescriber to give a patient a compounded GLP-1 if the patient has prescription coverage and the brand name is available.
Her approach: She first checks the patients’ coverage. Do they have coverage for these medications for obesity? If so, she said, she will do a prior authorization to get the brand name approved. If a brand name is available but not covered, she explores other options. One is the cash pay option for Zepbound in vials. It’s more affordable than the typical $1000 cash price for the brand name GLP-1s but still pricey, at about $400-$549 for lower doses.
She looks at drug makers’ discount coupons, or whether a patient with a history of cardiovascular issues might qualify for coverage on Wegovy. Another option is to give the patient a prescription for Mounjaro or Ozempic to fill from a Canadian pharmacy for about $400 a month.
“I think a lot of people jump quickly to compounding,” she said.
She views it as a last resort and reminds other healthcare providers that the compounded medications aren’t cheap, either, typically costing $100-$500 a month depending on dosage. And, she said, “we have many who get the brand name for $25 a month [by using discount cards and insurance coverage].”
When prescribing a compounded medication is necessary, it’s important for healthcare providers to know that the quality of the compounding pharmacies varies greatly, Stombaugh said. A prescriber needs to pick the compounding pharmacy, not the patient, and needs to vet it, she said, asking about protocols it follows for sterility and for chemical analysis, for instance.
Stombaugh is hopeful that several new medications under study and now in phase 3 trials will soon provide enough competition to drive down the price of the current brand-name GLP-1s.
History of mistrust: Robert Dubin, MD, associate professor of research at the Pennington Biomedical Research Center at Louisiana State University, Baton Rouge, and program director for its obesity medicine fellowship, sees a role for compounding and has for several years, but acknowledged that many in his community are against it.
He estimates that about 75% of his colleagues in the Baton Rouge area are opposed to prescribing compounded GLP-1s. He chalks it up to a “track record of distrust,” based on reports of infractions called out by the FDA for some compounding pharmacies as well as physicians not being familiar with the process.
Dubin said he will prescribe a compounded medication if the brand name isn’t available. Cost is also a consideration. “If there’s not a problem with availability and there’s not a problem with cost, then why compound?”
For anyone considering prescribing compounded GLP-1s, he said, “The first step, I believe, is having a relationship with the compounding pharmacy. If you don’t have that, it could be very difficult. We don’t want to send people to a black hole, and we aren’t sure what is going to happen.” He urges colleagues to educate themselves about compounding pharmacies.
Official shortage list vs real world: “The official shortage list doesn’t always reflect the real world,” said Amanda Guarniere, NP, a nurse practitioner with a self-pay telehealth and in-person practice and director of growth for Collaborating Docs, a service based in Arlington, Virginia, that pairs nurse practitioners with supervising physicians.
“When Zepbound and Mounjaro came off the [FDA] shortage list a few weeks ago, patients were still calling around and couldn’t find it in their county.”
It’s important to vet compounding pharmacies before dealing with them, she said.
“I have accounts with two compounding pharmacies who I trust,” she said. She’s researched their quality control provided and is comfortable with their standards. When appropriate, the cost savings of compounded GLP-1s over brand name is “pretty significant,” with compounded medicine costs about 20% of brand-name costs.
When the brand name is back, how might a prescriber still write a prescription for a compounded version? “Compounded versions are typically compounded with something else,” Guarniere said.
For instance, compounded tirzepatide often includes vitamin B12 and other B vitamins, which may help with the side effect of nausea. So a prescriber might decide that the compounded prescription is more appropriate and justified because the patient would benefit from the additive, she said.
What Else to Know: Alliance Views
On November 7, the Alliance for Pharmacy Compounding, a trade group, responded to Lilly’s request to put tirzepatide on the “demonstrably difficult to compound (DDC)” list, asking the FDA to deny it. The group also took issue with criticism of compounded GLP-1s from the Novo Nordisk CEO.
The alliance offers perspective and a number of suggestions for doctors faced with compound or brand-name decisions, including using its website tool called “Is It Legit?” to be sure a compounding pharmacy meets standards.
“When these [GLP-1] drugs came out, I don’t think anybody anticipated them to be such blockbusters,” said Tenille Davis, PharmD, a board-certified sterile compounding pharmacist and chief advocacy officer for the Alliance for Pharmacy Compounding. Shortages have plagued the GLP-1s since their approvals, with Wegovy approved on June 4, 2021, and Eli Lilly’s Zepbound on November 8, 2023.
The proposed “Demonstrably Difficult to Compound (DDC)” rule, published in March 2024, aims to finalize the six criteria for a medication to land on that list, she said. No drugs are currently on this list, Davis said.
For now, she said, prescribers faced with a compound vs brand-name decision should be aware of the pending lawsuit concerning tirzepatide and that the FDA has said it will cease most enforcement action until 2 weeks after it reviews the decision to remove the medication from the shortage list and issues a new determination.
Davis suggests prescribers have conversations now with their patients about their options and to tell them it may be necessary to transition from the compounded medicines to brand name. “This may require insurance prior authorizations, so if they are going to transition from compounded tirzepatide to Zepbound and Mounjaro, it’s good to start the process sooner rather than later so there isn’t an interruption in care.”
Earlier in 2024, the three leading obesity organizations issued a statement, advising patients that they do not recommend the use of compounded GLP-1s.
Garvey is a consultant on advisory boards for Eli Lilly, Novo Nordisk, and several other pharmaceutical companies. Apovian had no relevant disclosures. Stombaugh, Dubin, and Guarniere had no disclosures.
A version of this article appeared on Medscape.com.
How to Manage Patients on GLP-1s Before Surgery
, as does the US Food and Drug Administration’s (FDA’s) labeling for the drugs. The changes can be challenging to keep up with, and endocrinologists seem to be making their own decisions based on clinical experience and their interpretations of the potential impact and value of the emerging information.
The latest FDA label change warns about the risk for pulmonary aspiration but notes “insufficient” data to inform recommendations to mitigate the risk in vulnerable patients. Yet, the latest multi-society guidance, led by the American Society of Anesthesiologists (ASA) and based on consensus, not evidence, has nuanced advice for managing patients at risk.
Does the FDA’s label change make a difference regarding the multi-society guidance, which was published earlier? “The answer is no,” Girish Joshi, MD, vice chair, ASA Committee on Practice Parameters, told this news organization. “The concern of increased pulmonary aspiration in patients who are on GLP-1 receptor agonists has been known, and that concern still exists. So, we started with not an assumption but the premise that patients on GLP-1 receptor agonists are at a higher risk of aspiration during sedation, analgesia, and/or general anesthesia. The FDA basically confirms what we say in the guidance.”
Joshi, professor in the Anesthesiology and Pain Management Department at UT Southwestern Medical Center, Dallas, aimed to make the guidance, which was published simultaneously in several society journals, more implementable with a letter to the editor of Anesthesiology. The key, he said, is to identify patients at higher risk for aspiration; all others would follow treatment as usual.
The letter highlights three overarching recommendations and then expands upon them: Standardized preoperative assessment for risk for delayed gastric emptying (yes/no); selective preoperative care plan based on delayed gastric emptying assessment and shared decision-making; and on the day of the procedure, reassess for delayed gastric emptying and mitigate risk if there is clinical concern.
But it seems as though, for now, endocrinologists are managing these patients as they see fit, within the parameters of any institutional guidance requirements. Here is what they said about their practice:
Amy E. Rothberg, MD, DABOM, director of the Weight Management Program & Rewind at the University of Michigan, Ann Arbor, Michigan, said, “I think it makes sense to inform our patients of the labeling and rare but potential adverse effects if they intend to undergo anesthesia for a scheduled procedure/surgery. There is never no risk of aspiration during anesthesia.”
“I find it a bit curious that ASA implies that those who experience GI side effects are more likely than those who do not to have this potential risk. I doubt there is evidence that those without GI side effects are necessarily ‘safer’ and a study to determine that is unlikely to take be conducted.”
“My institution does require a 1-week pause on GLP-1s for those undergoing anesthesia for surgery,” she added. “That’s not evidence-based either, but probably reduces the risk of aspiration during anesthesia — but I don’t know what the actual denominator is for aspiration in those who continued vs those who took a pause from GLP-1s. Pausing does certainly (anecdotally) increase the traffic of communications between physicians and their patients about what to do in the interval.”
Anne Peters, MD, a professor of clinical medicine and a clinical scholar at the Keck School of Medicine of the University of Southern California, Los Angeles, said, “The FDA label change is a warning that really doesn’t say exactly who on GLP-1 RAs is at highest risk or what to do, and if any intervention has been shown to help. The ASA recommendations seem much more nuanced and practical, including point-of-care gastric ultrasound to see if there is retained food/fluid prior to surgery.”
“In my practice, I individualize what I say, depending on the person and the circumstance,” she said. “Mostly, I have people hold one dose before planned surgery, so they have been 10 days at least without a dose. But if worried about gastrointestinal symptoms or gastroparesis, I have them do a clear liquid diet for 24 hours presurgery. Or at least avoid heavy fat meals the day before.”
“There is a risk of aspiration with anything that slows gastric emptying — maybe even in patients with gastroparesis at baseline due to physiologic, not pharmacological, reasons — and anesthesiologists should be aware of the need to assess patients individually.”
Michael A. Weintraub, MD, of NYU Langone Health Diabetes & Endocrine Associates in New York City, observed, “The risk of a pulmonary aspiration event with GLP-1 medication is quite rare, but not zero. On the other hand, stopping the GLP-1 can cause hyperglycemia or rebound weight gain. Furthermore, it can become complicated to restart GLP1 dosing, particularly given the existing medication shortages.”
“In most cases, stopping a weekly GLP-1 medication 1 week prior to the procedure minimizes the risks of pulmonary aspiration and prevents any worsening hyperglycemia or weight gain,” he said. However, taking the drug 7 days prior to the procedure is optimal. “That way, they would be due for the next dose on the day of the procedure, and taking it the day following procedure minimizes disruption in their once-weekly regimen.”
Malini Gupta, MD, director of G2Endo Endocrinology & Metabolism, Memphis, Tennessee, advised that physicians weigh the risk of stopping the medication (which can cause a glycemic spike) vs risk for aspiration.
“In my opinion, all patients should follow a strict liquid diet or NPO status prior to a surgery to further decrease the risk of aspiration,” she said. “I generally hold the GLP-1 RA for a week before a surgery. If additional glycemic control is necessary, I will add to or adjust one of the patient’s other diabetes medications.”
Jaime Almandoz, MD, associate professor of medicine and medical director of the Weight Wellness Program in Dallas, said, “As endocrinologists, we typically rely on our anesthesia colleagues for guidance on perioperative management. In light of emerging guidelines for holding GLP-1 medications, we also recommend patients adopt a liquid diet 24 hours prior to surgery, along with the fasting protocol.”
“For those managing diabetes with GLP-1 therapies, it is crucial to establish a blood sugar management plan while off these medications, especially during fasting or postoperative periods, which can be further influenced by many factors, including nausea, pain medications, and antibiotics after the procedure.”
Joshi added that at Parkland Hospital in Dallas, “we do a huge number of cases using the same information. We identify patients who are at risk, and then we tell our proceduralists and our surgeons if they’re in the escalating phase of the dosing or if they have GI symptoms; don’t even schedule them as an elective case; wait till the escalation phase is over and then schedule them.”
“That way,” he said, “it becomes logistically easy to manage because the recommendation from the group is that patients who are at higher risk should receive a 24-hour liquid diet — the same as colonoscopy. But sometimes it can be challenging to do so.”
Joshi has received honoraria for consultation from Merck Sharp & Dohme, Vertex Pharmaceuticals, and Haisco-USA Pharmaceuticals. Gupta is on the speakers bureau for Amgen (Tepezza) and IBSA (Tirosint) and is a creative consultant for AbbVie. Almandoz serves on advisory boards for Novo Nordisk, Eli Lilly, and Boehringer Ingelheim. The other experts declared no relevant relationships.
A version of this article first appeared on Medscape.com.
, as does the US Food and Drug Administration’s (FDA’s) labeling for the drugs. The changes can be challenging to keep up with, and endocrinologists seem to be making their own decisions based on clinical experience and their interpretations of the potential impact and value of the emerging information.
The latest FDA label change warns about the risk for pulmonary aspiration but notes “insufficient” data to inform recommendations to mitigate the risk in vulnerable patients. Yet, the latest multi-society guidance, led by the American Society of Anesthesiologists (ASA) and based on consensus, not evidence, has nuanced advice for managing patients at risk.
Does the FDA’s label change make a difference regarding the multi-society guidance, which was published earlier? “The answer is no,” Girish Joshi, MD, vice chair, ASA Committee on Practice Parameters, told this news organization. “The concern of increased pulmonary aspiration in patients who are on GLP-1 receptor agonists has been known, and that concern still exists. So, we started with not an assumption but the premise that patients on GLP-1 receptor agonists are at a higher risk of aspiration during sedation, analgesia, and/or general anesthesia. The FDA basically confirms what we say in the guidance.”
Joshi, professor in the Anesthesiology and Pain Management Department at UT Southwestern Medical Center, Dallas, aimed to make the guidance, which was published simultaneously in several society journals, more implementable with a letter to the editor of Anesthesiology. The key, he said, is to identify patients at higher risk for aspiration; all others would follow treatment as usual.
The letter highlights three overarching recommendations and then expands upon them: Standardized preoperative assessment for risk for delayed gastric emptying (yes/no); selective preoperative care plan based on delayed gastric emptying assessment and shared decision-making; and on the day of the procedure, reassess for delayed gastric emptying and mitigate risk if there is clinical concern.
But it seems as though, for now, endocrinologists are managing these patients as they see fit, within the parameters of any institutional guidance requirements. Here is what they said about their practice:
Amy E. Rothberg, MD, DABOM, director of the Weight Management Program & Rewind at the University of Michigan, Ann Arbor, Michigan, said, “I think it makes sense to inform our patients of the labeling and rare but potential adverse effects if they intend to undergo anesthesia for a scheduled procedure/surgery. There is never no risk of aspiration during anesthesia.”
“I find it a bit curious that ASA implies that those who experience GI side effects are more likely than those who do not to have this potential risk. I doubt there is evidence that those without GI side effects are necessarily ‘safer’ and a study to determine that is unlikely to take be conducted.”
“My institution does require a 1-week pause on GLP-1s for those undergoing anesthesia for surgery,” she added. “That’s not evidence-based either, but probably reduces the risk of aspiration during anesthesia — but I don’t know what the actual denominator is for aspiration in those who continued vs those who took a pause from GLP-1s. Pausing does certainly (anecdotally) increase the traffic of communications between physicians and their patients about what to do in the interval.”
Anne Peters, MD, a professor of clinical medicine and a clinical scholar at the Keck School of Medicine of the University of Southern California, Los Angeles, said, “The FDA label change is a warning that really doesn’t say exactly who on GLP-1 RAs is at highest risk or what to do, and if any intervention has been shown to help. The ASA recommendations seem much more nuanced and practical, including point-of-care gastric ultrasound to see if there is retained food/fluid prior to surgery.”
“In my practice, I individualize what I say, depending on the person and the circumstance,” she said. “Mostly, I have people hold one dose before planned surgery, so they have been 10 days at least without a dose. But if worried about gastrointestinal symptoms or gastroparesis, I have them do a clear liquid diet for 24 hours presurgery. Or at least avoid heavy fat meals the day before.”
“There is a risk of aspiration with anything that slows gastric emptying — maybe even in patients with gastroparesis at baseline due to physiologic, not pharmacological, reasons — and anesthesiologists should be aware of the need to assess patients individually.”
Michael A. Weintraub, MD, of NYU Langone Health Diabetes & Endocrine Associates in New York City, observed, “The risk of a pulmonary aspiration event with GLP-1 medication is quite rare, but not zero. On the other hand, stopping the GLP-1 can cause hyperglycemia or rebound weight gain. Furthermore, it can become complicated to restart GLP1 dosing, particularly given the existing medication shortages.”
“In most cases, stopping a weekly GLP-1 medication 1 week prior to the procedure minimizes the risks of pulmonary aspiration and prevents any worsening hyperglycemia or weight gain,” he said. However, taking the drug 7 days prior to the procedure is optimal. “That way, they would be due for the next dose on the day of the procedure, and taking it the day following procedure minimizes disruption in their once-weekly regimen.”
Malini Gupta, MD, director of G2Endo Endocrinology & Metabolism, Memphis, Tennessee, advised that physicians weigh the risk of stopping the medication (which can cause a glycemic spike) vs risk for aspiration.
“In my opinion, all patients should follow a strict liquid diet or NPO status prior to a surgery to further decrease the risk of aspiration,” she said. “I generally hold the GLP-1 RA for a week before a surgery. If additional glycemic control is necessary, I will add to or adjust one of the patient’s other diabetes medications.”
Jaime Almandoz, MD, associate professor of medicine and medical director of the Weight Wellness Program in Dallas, said, “As endocrinologists, we typically rely on our anesthesia colleagues for guidance on perioperative management. In light of emerging guidelines for holding GLP-1 medications, we also recommend patients adopt a liquid diet 24 hours prior to surgery, along with the fasting protocol.”
“For those managing diabetes with GLP-1 therapies, it is crucial to establish a blood sugar management plan while off these medications, especially during fasting or postoperative periods, which can be further influenced by many factors, including nausea, pain medications, and antibiotics after the procedure.”
Joshi added that at Parkland Hospital in Dallas, “we do a huge number of cases using the same information. We identify patients who are at risk, and then we tell our proceduralists and our surgeons if they’re in the escalating phase of the dosing or if they have GI symptoms; don’t even schedule them as an elective case; wait till the escalation phase is over and then schedule them.”
“That way,” he said, “it becomes logistically easy to manage because the recommendation from the group is that patients who are at higher risk should receive a 24-hour liquid diet — the same as colonoscopy. But sometimes it can be challenging to do so.”
Joshi has received honoraria for consultation from Merck Sharp & Dohme, Vertex Pharmaceuticals, and Haisco-USA Pharmaceuticals. Gupta is on the speakers bureau for Amgen (Tepezza) and IBSA (Tirosint) and is a creative consultant for AbbVie. Almandoz serves on advisory boards for Novo Nordisk, Eli Lilly, and Boehringer Ingelheim. The other experts declared no relevant relationships.
A version of this article first appeared on Medscape.com.
, as does the US Food and Drug Administration’s (FDA’s) labeling for the drugs. The changes can be challenging to keep up with, and endocrinologists seem to be making their own decisions based on clinical experience and their interpretations of the potential impact and value of the emerging information.
The latest FDA label change warns about the risk for pulmonary aspiration but notes “insufficient” data to inform recommendations to mitigate the risk in vulnerable patients. Yet, the latest multi-society guidance, led by the American Society of Anesthesiologists (ASA) and based on consensus, not evidence, has nuanced advice for managing patients at risk.
Does the FDA’s label change make a difference regarding the multi-society guidance, which was published earlier? “The answer is no,” Girish Joshi, MD, vice chair, ASA Committee on Practice Parameters, told this news organization. “The concern of increased pulmonary aspiration in patients who are on GLP-1 receptor agonists has been known, and that concern still exists. So, we started with not an assumption but the premise that patients on GLP-1 receptor agonists are at a higher risk of aspiration during sedation, analgesia, and/or general anesthesia. The FDA basically confirms what we say in the guidance.”
Joshi, professor in the Anesthesiology and Pain Management Department at UT Southwestern Medical Center, Dallas, aimed to make the guidance, which was published simultaneously in several society journals, more implementable with a letter to the editor of Anesthesiology. The key, he said, is to identify patients at higher risk for aspiration; all others would follow treatment as usual.
The letter highlights three overarching recommendations and then expands upon them: Standardized preoperative assessment for risk for delayed gastric emptying (yes/no); selective preoperative care plan based on delayed gastric emptying assessment and shared decision-making; and on the day of the procedure, reassess for delayed gastric emptying and mitigate risk if there is clinical concern.
But it seems as though, for now, endocrinologists are managing these patients as they see fit, within the parameters of any institutional guidance requirements. Here is what they said about their practice:
Amy E. Rothberg, MD, DABOM, director of the Weight Management Program & Rewind at the University of Michigan, Ann Arbor, Michigan, said, “I think it makes sense to inform our patients of the labeling and rare but potential adverse effects if they intend to undergo anesthesia for a scheduled procedure/surgery. There is never no risk of aspiration during anesthesia.”
“I find it a bit curious that ASA implies that those who experience GI side effects are more likely than those who do not to have this potential risk. I doubt there is evidence that those without GI side effects are necessarily ‘safer’ and a study to determine that is unlikely to take be conducted.”
“My institution does require a 1-week pause on GLP-1s for those undergoing anesthesia for surgery,” she added. “That’s not evidence-based either, but probably reduces the risk of aspiration during anesthesia — but I don’t know what the actual denominator is for aspiration in those who continued vs those who took a pause from GLP-1s. Pausing does certainly (anecdotally) increase the traffic of communications between physicians and their patients about what to do in the interval.”
Anne Peters, MD, a professor of clinical medicine and a clinical scholar at the Keck School of Medicine of the University of Southern California, Los Angeles, said, “The FDA label change is a warning that really doesn’t say exactly who on GLP-1 RAs is at highest risk or what to do, and if any intervention has been shown to help. The ASA recommendations seem much more nuanced and practical, including point-of-care gastric ultrasound to see if there is retained food/fluid prior to surgery.”
“In my practice, I individualize what I say, depending on the person and the circumstance,” she said. “Mostly, I have people hold one dose before planned surgery, so they have been 10 days at least without a dose. But if worried about gastrointestinal symptoms or gastroparesis, I have them do a clear liquid diet for 24 hours presurgery. Or at least avoid heavy fat meals the day before.”
“There is a risk of aspiration with anything that slows gastric emptying — maybe even in patients with gastroparesis at baseline due to physiologic, not pharmacological, reasons — and anesthesiologists should be aware of the need to assess patients individually.”
Michael A. Weintraub, MD, of NYU Langone Health Diabetes & Endocrine Associates in New York City, observed, “The risk of a pulmonary aspiration event with GLP-1 medication is quite rare, but not zero. On the other hand, stopping the GLP-1 can cause hyperglycemia or rebound weight gain. Furthermore, it can become complicated to restart GLP1 dosing, particularly given the existing medication shortages.”
“In most cases, stopping a weekly GLP-1 medication 1 week prior to the procedure minimizes the risks of pulmonary aspiration and prevents any worsening hyperglycemia or weight gain,” he said. However, taking the drug 7 days prior to the procedure is optimal. “That way, they would be due for the next dose on the day of the procedure, and taking it the day following procedure minimizes disruption in their once-weekly regimen.”
Malini Gupta, MD, director of G2Endo Endocrinology & Metabolism, Memphis, Tennessee, advised that physicians weigh the risk of stopping the medication (which can cause a glycemic spike) vs risk for aspiration.
“In my opinion, all patients should follow a strict liquid diet or NPO status prior to a surgery to further decrease the risk of aspiration,” she said. “I generally hold the GLP-1 RA for a week before a surgery. If additional glycemic control is necessary, I will add to or adjust one of the patient’s other diabetes medications.”
Jaime Almandoz, MD, associate professor of medicine and medical director of the Weight Wellness Program in Dallas, said, “As endocrinologists, we typically rely on our anesthesia colleagues for guidance on perioperative management. In light of emerging guidelines for holding GLP-1 medications, we also recommend patients adopt a liquid diet 24 hours prior to surgery, along with the fasting protocol.”
“For those managing diabetes with GLP-1 therapies, it is crucial to establish a blood sugar management plan while off these medications, especially during fasting or postoperative periods, which can be further influenced by many factors, including nausea, pain medications, and antibiotics after the procedure.”
Joshi added that at Parkland Hospital in Dallas, “we do a huge number of cases using the same information. We identify patients who are at risk, and then we tell our proceduralists and our surgeons if they’re in the escalating phase of the dosing or if they have GI symptoms; don’t even schedule them as an elective case; wait till the escalation phase is over and then schedule them.”
“That way,” he said, “it becomes logistically easy to manage because the recommendation from the group is that patients who are at higher risk should receive a 24-hour liquid diet — the same as colonoscopy. But sometimes it can be challenging to do so.”
Joshi has received honoraria for consultation from Merck Sharp & Dohme, Vertex Pharmaceuticals, and Haisco-USA Pharmaceuticals. Gupta is on the speakers bureau for Amgen (Tepezza) and IBSA (Tirosint) and is a creative consultant for AbbVie. Almandoz serves on advisory boards for Novo Nordisk, Eli Lilly, and Boehringer Ingelheim. The other experts declared no relevant relationships.
A version of this article first appeared on Medscape.com.
Continuous Glucose Monitors for All? Opinions Remain Mixed
The recent US Food and Drug Administration (FDA) clearance of two over-the-counter (OTC) continuous glucose monitors (CGMs) — Dexcom’s Stelo and Abbott’s Lingo — has sparked interest in potentially expanding their use to those without diabetes or prediabetes.
There are several valid questions about how the general population might benefit from CGMs. Can they motivate those struggling with overweight to shed pounds? Would they prompt users to follow more healthful eating patterns? Can they act as a canary in the coal mine, alerting users to prediabetes?
The short answer to these questions is, we don’t know.
“Glucose levels fluctuate in everyone in response to meals, exercise, stress, etc, but there has been no credible research to support CGM use by most people who do not have diabetes,” Jill Crandall, MD, chief of endocrinology at Albert Einstein College of Medicine and Montefiore Health System in New York City, said in an interview.
“The utility of CGM for people without diabetes hasn’t been established and the drive to market CGM as an OTC device seems largely driven by financial considerations,” Crandall said. She advocates instead for a strategy directed at more meaningful objectives.
“For now, efforts should be focused on making CGMs available to patients who will clearly benefit — ie, people with diabetes, especially those who are using insulin and those who are struggling to achieve desired levels of glucose control.”
Nicole Spartano, PhD, assistant professor of medicine in endocrinology, diabetes, nutrition and weight management at Boston University’s Chobanian & Avedisian School of Medicine in Massachusetts, agreed with this assessment.
“It is definitely too early to make recommendations for patients without diabetes based on their CGM data,” said Spartano, who also serves as the director of the Glucose Monitoring Station at the Framingham Heart Study in Framingham, Massachusetts. “We simply do not have enough follow-up data to tell us which CGM metrics are associated with higher risk for disease.”
Spartano served as the lead author of a recent study showing time spent in various CGM ranges in a large cohort of individuals without diabetes using the Dexcom G6 Pro model. In the future, she said the data may be used to establish reference ranges for clinicians and individuals.
“We are working on another paper surveying diabetologists and CGM experts about how they interpret CGM reports from individuals without diabetes,” she said in an interview. Although the data are not yet published, Spartano said, “we are finding that clinicians are currently very discordant in how they interpret these reports.”
Potential Benefits Right Now
Satish Garg, MD, director of the Adult Clinic at the Barbara Davis Center for Diabetes at the University of Colorado Anschutz Medical Campus, Aurora, and editor-in-chief of Diabetes Technology & Therapeutics, is convinced that glucose should be considered another vital sign, like blood pressure, pulse rate, respiration rate, and body temperature. Therefore, he sees the use of a CGM in people without diabetes as a way to build awareness and perhaps prompt behavior modification.
“Someone with an A1c of 4.9 on a normal day may notice that they’ve gained a little bit of weight, and if they use an OTC CGM and start seeing changes, it might help them to modulate their diet themselves, whether they see a dietitian or not,” Garg said.
He gave the example of “a natural behavioral change” occurring when someone using a CGM declines to eat a post-meal dessert after seeing their blood glucose had already risen to 170.
Wearing a CGM also has the potential to alert the user to high blood glucose, leading them to an earlier diagnosis of prediabetes or diabetes, Shichun Bao, MD, PhD, Diabetes Technology Program Leader at the Vanderbilt Eskind Diabetes Clinic of Vanderbilt University in Nashville, Tennessee, said in an interview. She has had cases where a family member of someone with diabetes used the patient’s fingerstick meter, found that their glucose was 280, and self-diagnosed with diabetes.
“It’s the same thing with the CGM,” she said. “If they somehow did not know they have diabetes and they wear a CGM and it shows their sugar is high, that will help them to know to see their provider to get a diagnosis, get treated, and track progression.”
Given the shortage of endocrinologists and long waits for appointments in the United States and elsewhere, it is very likely that primary care physicians will be the ones fielding questions from individuals without diabetes interested in purchasing an OTC CGM. Internist Douglas Paauw, MD, a professor at the University of Washington School of Medicine, Seattle, said in an interview that, for his practice, “the benefits outweigh some of the limitations.”
“I don’t really think somebody who doesn’t have diabetes needs to be using a CGM all the time or long term,” he said. “But I have used it in a few people without diabetes, and I think if someone can afford to use it for 2-4 weeks, especially if they’ve been gaining weight, then they can really recognize what happens to their bodies when they eat certain foods.”
Paauw added that CGMs are a more effective means of teaching his patients than them receiving a lecture from him on healthy eating. “There’s nothing like immediate feedback on what happens to your body to change behavior.”
Similarly, William Golden, medical director at Arkansas Medicaid and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview that “it is difficult to justify coverage for CGMs on demand — but if people want to invest in their own devices and the technology motivates them to eat better and/or lose weight, then there are benefits to be had.”
Potential Downsides
Although it may seem simple to use an OTC CGM to measure blood glucose on the fly, in the real world it can take patients time to understand these devices, “especially the first day or so, when users are going to get false lows,” Bao said. “Clinicians need to tell them if you don’t feel like your sugar is low and the device says it’s low, whether they do or don’t have diabetes, they should do a fingerstick glucose test to confirm the low before rushing to take in sugar. On the other hand, if they drink a lot of juice, their sugar will go high. So, it can create problems and false results either way.”
Many factors affect glucose, she said. “When you’re sick, glucose can go high, and when you’re very sick, in the ICU, sometimes it can be low. It depends on the situation.” Bao noted that certain vitamins and drugs can also interfere with readings.
Bao doesn’t see value in having people without diabetes monitor their glucose continuously. “If they want to see what foods or exercise do to their body, they will probably benefit from a short trial to gain some insight; otherwise, they’re wasting money,” she said.
Another potential downside is that there’s no head-to-head comparison data with the approved devices, Garg said. “But it’s clear to us that Stelo’s range is very narrow, 70 to 200, whereas the Lingo ranges are pretty much full, from 40 to 400 or 55 to 400. So, we don’t know the accuracy of these sensors.”
Golden observed that for certain patients, CGMs may lead to psychological distress rather than providing a sense of control over their blood glucose levels.
“I have had a nondiabetic patient or two that obsessed about their blood sugars and a device would only magnify their anxiety/neurosis,” he said. “The bottom line is that it’s a tool for a balanced approach to health management, but the daily results must be kept in perspective!”
Educate Patients, Primary Care Physicians
To maximize potential benefits for patients without diabetes, clinicians need to be well trained in the use and interpretation of results from the devices, Bao said. They can then better educate their patients, including discussing with them possible pitfalls surrounding their use.
“For example, a patient may see that their blood glucose, as measured by a fingerstick, is 95, whereas the CGM says 140, and ask, ‘Which one do I trust?’ ”
This is where the patient can be educated about the difference between interstitial glucose, as measured by the CGM, and blood glucose, as measured by the fingerstick. Because it takes about 15 minutes for blood glucose to get to the interstitial tissue, there’s lag time, and the two measurements will differ.
“A discrepancy of 20% is totally acceptable for that reason,” Bao said.
She has also seen several examples where patients were misled by their CGM when its censor became dislodged.
“Sometimes when a sensor has moved, the patient may push it back in because they don’t want to throw it away. But it doesn’t work that way, and they end up with inaccurate readings.”
At a minimum, Bao added, clinicians and patients should read the package insert but also be aware that it doesn’t list everything that might go wrong or interfere with the device’s accuracy.
Manufacturers of OTC devices should be training primary care and family practice doctors in their use, given the expected “huge” influx of patients wanting to use them, according to Garg.
“If you are expecting endos or diabetes specialists to see these people, that’s never going to happen,” he said. “We have a big shortage of these specialists, so industry has to train these doctors. Patients will bring their doctor’s data, and the clinicians need to learn the basics of how to interpret the glucose values they see. Then they can treat these patients rather than shipping all of them to endos who likely are not available.”
Paauw agreed that CGM training should be directed largely toward primary care professionals, who can help their under-resourced endocrinologist colleagues from seeing an uptick in “the worried well.”
“The bottom line is that primary care professionals do need to understand the CGM,” he said. “They do need to get comfortable with it. They do need to come up with opinions on how to use it. The public’s going to be using it, and we need to be competent in it and use our subspecialists appropriately.”
Spartano received funding for an investigator-initiated research grant from Novo Nordisk unrelated to the cited CGM studies. Garg , Bao, Paauw, Golden, and Crandall declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The recent US Food and Drug Administration (FDA) clearance of two over-the-counter (OTC) continuous glucose monitors (CGMs) — Dexcom’s Stelo and Abbott’s Lingo — has sparked interest in potentially expanding their use to those without diabetes or prediabetes.
There are several valid questions about how the general population might benefit from CGMs. Can they motivate those struggling with overweight to shed pounds? Would they prompt users to follow more healthful eating patterns? Can they act as a canary in the coal mine, alerting users to prediabetes?
The short answer to these questions is, we don’t know.
“Glucose levels fluctuate in everyone in response to meals, exercise, stress, etc, but there has been no credible research to support CGM use by most people who do not have diabetes,” Jill Crandall, MD, chief of endocrinology at Albert Einstein College of Medicine and Montefiore Health System in New York City, said in an interview.
“The utility of CGM for people without diabetes hasn’t been established and the drive to market CGM as an OTC device seems largely driven by financial considerations,” Crandall said. She advocates instead for a strategy directed at more meaningful objectives.
“For now, efforts should be focused on making CGMs available to patients who will clearly benefit — ie, people with diabetes, especially those who are using insulin and those who are struggling to achieve desired levels of glucose control.”
Nicole Spartano, PhD, assistant professor of medicine in endocrinology, diabetes, nutrition and weight management at Boston University’s Chobanian & Avedisian School of Medicine in Massachusetts, agreed with this assessment.
“It is definitely too early to make recommendations for patients without diabetes based on their CGM data,” said Spartano, who also serves as the director of the Glucose Monitoring Station at the Framingham Heart Study in Framingham, Massachusetts. “We simply do not have enough follow-up data to tell us which CGM metrics are associated with higher risk for disease.”
Spartano served as the lead author of a recent study showing time spent in various CGM ranges in a large cohort of individuals without diabetes using the Dexcom G6 Pro model. In the future, she said the data may be used to establish reference ranges for clinicians and individuals.
“We are working on another paper surveying diabetologists and CGM experts about how they interpret CGM reports from individuals without diabetes,” she said in an interview. Although the data are not yet published, Spartano said, “we are finding that clinicians are currently very discordant in how they interpret these reports.”
Potential Benefits Right Now
Satish Garg, MD, director of the Adult Clinic at the Barbara Davis Center for Diabetes at the University of Colorado Anschutz Medical Campus, Aurora, and editor-in-chief of Diabetes Technology & Therapeutics, is convinced that glucose should be considered another vital sign, like blood pressure, pulse rate, respiration rate, and body temperature. Therefore, he sees the use of a CGM in people without diabetes as a way to build awareness and perhaps prompt behavior modification.
“Someone with an A1c of 4.9 on a normal day may notice that they’ve gained a little bit of weight, and if they use an OTC CGM and start seeing changes, it might help them to modulate their diet themselves, whether they see a dietitian or not,” Garg said.
He gave the example of “a natural behavioral change” occurring when someone using a CGM declines to eat a post-meal dessert after seeing their blood glucose had already risen to 170.
Wearing a CGM also has the potential to alert the user to high blood glucose, leading them to an earlier diagnosis of prediabetes or diabetes, Shichun Bao, MD, PhD, Diabetes Technology Program Leader at the Vanderbilt Eskind Diabetes Clinic of Vanderbilt University in Nashville, Tennessee, said in an interview. She has had cases where a family member of someone with diabetes used the patient’s fingerstick meter, found that their glucose was 280, and self-diagnosed with diabetes.
“It’s the same thing with the CGM,” she said. “If they somehow did not know they have diabetes and they wear a CGM and it shows their sugar is high, that will help them to know to see their provider to get a diagnosis, get treated, and track progression.”
Given the shortage of endocrinologists and long waits for appointments in the United States and elsewhere, it is very likely that primary care physicians will be the ones fielding questions from individuals without diabetes interested in purchasing an OTC CGM. Internist Douglas Paauw, MD, a professor at the University of Washington School of Medicine, Seattle, said in an interview that, for his practice, “the benefits outweigh some of the limitations.”
“I don’t really think somebody who doesn’t have diabetes needs to be using a CGM all the time or long term,” he said. “But I have used it in a few people without diabetes, and I think if someone can afford to use it for 2-4 weeks, especially if they’ve been gaining weight, then they can really recognize what happens to their bodies when they eat certain foods.”
Paauw added that CGMs are a more effective means of teaching his patients than them receiving a lecture from him on healthy eating. “There’s nothing like immediate feedback on what happens to your body to change behavior.”
Similarly, William Golden, medical director at Arkansas Medicaid and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview that “it is difficult to justify coverage for CGMs on demand — but if people want to invest in their own devices and the technology motivates them to eat better and/or lose weight, then there are benefits to be had.”
Potential Downsides
Although it may seem simple to use an OTC CGM to measure blood glucose on the fly, in the real world it can take patients time to understand these devices, “especially the first day or so, when users are going to get false lows,” Bao said. “Clinicians need to tell them if you don’t feel like your sugar is low and the device says it’s low, whether they do or don’t have diabetes, they should do a fingerstick glucose test to confirm the low before rushing to take in sugar. On the other hand, if they drink a lot of juice, their sugar will go high. So, it can create problems and false results either way.”
Many factors affect glucose, she said. “When you’re sick, glucose can go high, and when you’re very sick, in the ICU, sometimes it can be low. It depends on the situation.” Bao noted that certain vitamins and drugs can also interfere with readings.
Bao doesn’t see value in having people without diabetes monitor their glucose continuously. “If they want to see what foods or exercise do to their body, they will probably benefit from a short trial to gain some insight; otherwise, they’re wasting money,” she said.
Another potential downside is that there’s no head-to-head comparison data with the approved devices, Garg said. “But it’s clear to us that Stelo’s range is very narrow, 70 to 200, whereas the Lingo ranges are pretty much full, from 40 to 400 or 55 to 400. So, we don’t know the accuracy of these sensors.”
Golden observed that for certain patients, CGMs may lead to psychological distress rather than providing a sense of control over their blood glucose levels.
“I have had a nondiabetic patient or two that obsessed about their blood sugars and a device would only magnify their anxiety/neurosis,” he said. “The bottom line is that it’s a tool for a balanced approach to health management, but the daily results must be kept in perspective!”
Educate Patients, Primary Care Physicians
To maximize potential benefits for patients without diabetes, clinicians need to be well trained in the use and interpretation of results from the devices, Bao said. They can then better educate their patients, including discussing with them possible pitfalls surrounding their use.
“For example, a patient may see that their blood glucose, as measured by a fingerstick, is 95, whereas the CGM says 140, and ask, ‘Which one do I trust?’ ”
This is where the patient can be educated about the difference between interstitial glucose, as measured by the CGM, and blood glucose, as measured by the fingerstick. Because it takes about 15 minutes for blood glucose to get to the interstitial tissue, there’s lag time, and the two measurements will differ.
“A discrepancy of 20% is totally acceptable for that reason,” Bao said.
She has also seen several examples where patients were misled by their CGM when its censor became dislodged.
“Sometimes when a sensor has moved, the patient may push it back in because they don’t want to throw it away. But it doesn’t work that way, and they end up with inaccurate readings.”
At a minimum, Bao added, clinicians and patients should read the package insert but also be aware that it doesn’t list everything that might go wrong or interfere with the device’s accuracy.
Manufacturers of OTC devices should be training primary care and family practice doctors in their use, given the expected “huge” influx of patients wanting to use them, according to Garg.
“If you are expecting endos or diabetes specialists to see these people, that’s never going to happen,” he said. “We have a big shortage of these specialists, so industry has to train these doctors. Patients will bring their doctor’s data, and the clinicians need to learn the basics of how to interpret the glucose values they see. Then they can treat these patients rather than shipping all of them to endos who likely are not available.”
Paauw agreed that CGM training should be directed largely toward primary care professionals, who can help their under-resourced endocrinologist colleagues from seeing an uptick in “the worried well.”
“The bottom line is that primary care professionals do need to understand the CGM,” he said. “They do need to get comfortable with it. They do need to come up with opinions on how to use it. The public’s going to be using it, and we need to be competent in it and use our subspecialists appropriately.”
Spartano received funding for an investigator-initiated research grant from Novo Nordisk unrelated to the cited CGM studies. Garg , Bao, Paauw, Golden, and Crandall declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The recent US Food and Drug Administration (FDA) clearance of two over-the-counter (OTC) continuous glucose monitors (CGMs) — Dexcom’s Stelo and Abbott’s Lingo — has sparked interest in potentially expanding their use to those without diabetes or prediabetes.
There are several valid questions about how the general population might benefit from CGMs. Can they motivate those struggling with overweight to shed pounds? Would they prompt users to follow more healthful eating patterns? Can they act as a canary in the coal mine, alerting users to prediabetes?
The short answer to these questions is, we don’t know.
“Glucose levels fluctuate in everyone in response to meals, exercise, stress, etc, but there has been no credible research to support CGM use by most people who do not have diabetes,” Jill Crandall, MD, chief of endocrinology at Albert Einstein College of Medicine and Montefiore Health System in New York City, said in an interview.
“The utility of CGM for people without diabetes hasn’t been established and the drive to market CGM as an OTC device seems largely driven by financial considerations,” Crandall said. She advocates instead for a strategy directed at more meaningful objectives.
“For now, efforts should be focused on making CGMs available to patients who will clearly benefit — ie, people with diabetes, especially those who are using insulin and those who are struggling to achieve desired levels of glucose control.”
Nicole Spartano, PhD, assistant professor of medicine in endocrinology, diabetes, nutrition and weight management at Boston University’s Chobanian & Avedisian School of Medicine in Massachusetts, agreed with this assessment.
“It is definitely too early to make recommendations for patients without diabetes based on their CGM data,” said Spartano, who also serves as the director of the Glucose Monitoring Station at the Framingham Heart Study in Framingham, Massachusetts. “We simply do not have enough follow-up data to tell us which CGM metrics are associated with higher risk for disease.”
Spartano served as the lead author of a recent study showing time spent in various CGM ranges in a large cohort of individuals without diabetes using the Dexcom G6 Pro model. In the future, she said the data may be used to establish reference ranges for clinicians and individuals.
“We are working on another paper surveying diabetologists and CGM experts about how they interpret CGM reports from individuals without diabetes,” she said in an interview. Although the data are not yet published, Spartano said, “we are finding that clinicians are currently very discordant in how they interpret these reports.”
Potential Benefits Right Now
Satish Garg, MD, director of the Adult Clinic at the Barbara Davis Center for Diabetes at the University of Colorado Anschutz Medical Campus, Aurora, and editor-in-chief of Diabetes Technology & Therapeutics, is convinced that glucose should be considered another vital sign, like blood pressure, pulse rate, respiration rate, and body temperature. Therefore, he sees the use of a CGM in people without diabetes as a way to build awareness and perhaps prompt behavior modification.
“Someone with an A1c of 4.9 on a normal day may notice that they’ve gained a little bit of weight, and if they use an OTC CGM and start seeing changes, it might help them to modulate their diet themselves, whether they see a dietitian or not,” Garg said.
He gave the example of “a natural behavioral change” occurring when someone using a CGM declines to eat a post-meal dessert after seeing their blood glucose had already risen to 170.
Wearing a CGM also has the potential to alert the user to high blood glucose, leading them to an earlier diagnosis of prediabetes or diabetes, Shichun Bao, MD, PhD, Diabetes Technology Program Leader at the Vanderbilt Eskind Diabetes Clinic of Vanderbilt University in Nashville, Tennessee, said in an interview. She has had cases where a family member of someone with diabetes used the patient’s fingerstick meter, found that their glucose was 280, and self-diagnosed with diabetes.
“It’s the same thing with the CGM,” she said. “If they somehow did not know they have diabetes and they wear a CGM and it shows their sugar is high, that will help them to know to see their provider to get a diagnosis, get treated, and track progression.”
Given the shortage of endocrinologists and long waits for appointments in the United States and elsewhere, it is very likely that primary care physicians will be the ones fielding questions from individuals without diabetes interested in purchasing an OTC CGM. Internist Douglas Paauw, MD, a professor at the University of Washington School of Medicine, Seattle, said in an interview that, for his practice, “the benefits outweigh some of the limitations.”
“I don’t really think somebody who doesn’t have diabetes needs to be using a CGM all the time or long term,” he said. “But I have used it in a few people without diabetes, and I think if someone can afford to use it for 2-4 weeks, especially if they’ve been gaining weight, then they can really recognize what happens to their bodies when they eat certain foods.”
Paauw added that CGMs are a more effective means of teaching his patients than them receiving a lecture from him on healthy eating. “There’s nothing like immediate feedback on what happens to your body to change behavior.”
Similarly, William Golden, medical director at Arkansas Medicaid and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview that “it is difficult to justify coverage for CGMs on demand — but if people want to invest in their own devices and the technology motivates them to eat better and/or lose weight, then there are benefits to be had.”
Potential Downsides
Although it may seem simple to use an OTC CGM to measure blood glucose on the fly, in the real world it can take patients time to understand these devices, “especially the first day or so, when users are going to get false lows,” Bao said. “Clinicians need to tell them if you don’t feel like your sugar is low and the device says it’s low, whether they do or don’t have diabetes, they should do a fingerstick glucose test to confirm the low before rushing to take in sugar. On the other hand, if they drink a lot of juice, their sugar will go high. So, it can create problems and false results either way.”
Many factors affect glucose, she said. “When you’re sick, glucose can go high, and when you’re very sick, in the ICU, sometimes it can be low. It depends on the situation.” Bao noted that certain vitamins and drugs can also interfere with readings.
Bao doesn’t see value in having people without diabetes monitor their glucose continuously. “If they want to see what foods or exercise do to their body, they will probably benefit from a short trial to gain some insight; otherwise, they’re wasting money,” she said.
Another potential downside is that there’s no head-to-head comparison data with the approved devices, Garg said. “But it’s clear to us that Stelo’s range is very narrow, 70 to 200, whereas the Lingo ranges are pretty much full, from 40 to 400 or 55 to 400. So, we don’t know the accuracy of these sensors.”
Golden observed that for certain patients, CGMs may lead to psychological distress rather than providing a sense of control over their blood glucose levels.
“I have had a nondiabetic patient or two that obsessed about their blood sugars and a device would only magnify their anxiety/neurosis,” he said. “The bottom line is that it’s a tool for a balanced approach to health management, but the daily results must be kept in perspective!”
Educate Patients, Primary Care Physicians
To maximize potential benefits for patients without diabetes, clinicians need to be well trained in the use and interpretation of results from the devices, Bao said. They can then better educate their patients, including discussing with them possible pitfalls surrounding their use.
“For example, a patient may see that their blood glucose, as measured by a fingerstick, is 95, whereas the CGM says 140, and ask, ‘Which one do I trust?’ ”
This is where the patient can be educated about the difference between interstitial glucose, as measured by the CGM, and blood glucose, as measured by the fingerstick. Because it takes about 15 minutes for blood glucose to get to the interstitial tissue, there’s lag time, and the two measurements will differ.
“A discrepancy of 20% is totally acceptable for that reason,” Bao said.
She has also seen several examples where patients were misled by their CGM when its censor became dislodged.
“Sometimes when a sensor has moved, the patient may push it back in because they don’t want to throw it away. But it doesn’t work that way, and they end up with inaccurate readings.”
At a minimum, Bao added, clinicians and patients should read the package insert but also be aware that it doesn’t list everything that might go wrong or interfere with the device’s accuracy.
Manufacturers of OTC devices should be training primary care and family practice doctors in their use, given the expected “huge” influx of patients wanting to use them, according to Garg.
“If you are expecting endos or diabetes specialists to see these people, that’s never going to happen,” he said. “We have a big shortage of these specialists, so industry has to train these doctors. Patients will bring their doctor’s data, and the clinicians need to learn the basics of how to interpret the glucose values they see. Then they can treat these patients rather than shipping all of them to endos who likely are not available.”
Paauw agreed that CGM training should be directed largely toward primary care professionals, who can help their under-resourced endocrinologist colleagues from seeing an uptick in “the worried well.”
“The bottom line is that primary care professionals do need to understand the CGM,” he said. “They do need to get comfortable with it. They do need to come up with opinions on how to use it. The public’s going to be using it, and we need to be competent in it and use our subspecialists appropriately.”
Spartano received funding for an investigator-initiated research grant from Novo Nordisk unrelated to the cited CGM studies. Garg , Bao, Paauw, Golden, and Crandall declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Doctors Caution Over Weight Loss Drug Link to Nurse’s Death
Doctors have urged caution in linking the weight loss drug tirzepatide to the death of a 58-year-old nurse from Scotland.
Susan McGowan, from North Lanarkshire, took two low-dose injections of tirzepatide (Mounjaro) over the course of about 2 weeks before her death in September.
BBC News reported that multiple organ failure, septic shock, and pancreatitis were listed on her death certificate as the immediate cause of death, with “the use of prescribed tirzepatide” recorded as a contributing factor.
McGowan worked as a nurse at University Hospital Monklands in Airdrie. A family member said that, apart from carrying a “bit of extra weight,” she had been otherwise healthy and was not taking any other medication.
It is understood that McGowan had sought medical advice before purchasing a prescription for tirzepatide through a registered UK pharmacy. However, days after administering a second injection, she went to A&E at Monklands with severe stomach pain and sickness. She died on September 4.
Expert Insights
Commenting to the Science Media Centre (SMC), Amanda Adler, MD, PhD, professor of diabetic medicine and health policy at the University of Oxford, described the nurse’s death as “sad” but said that “whether or not it was related to tirzepatide may be difficult to prove.” While tirzepatide can be associated with uncommon problems such as acute pancreatitis, “one can develop acute pancreatitis for many other reasons as well,” she said.
Naveed Sattar, MD, PhD, professor of metabolic medicine at the University of Glasgow, noted that data from multiple trials of tirzepatide, involving around 10,000 people living with diabetes or obesity, “do not suggest a higher risk of pancreatitis.” Furthermore, “the data seem to show acceptable safety thus far and a range of benefits including sizable average weight loss (near 20%), strong diabetes prevention, and considerable benefits in people living with sleep apnea,” he told the SMC.
Approved Based on Extensive Assessment
Tirzepatide, a GLP-1 receptor agonist, was approved for use as a weight loss aid in the United Kingdom in November last year by the Medicines and Healthcare products Regulatory Agency (MHRA). It lists nausea, diarrhea, and vomiting as the most common side effects, as well as hypoglycemia for patients with diabetes.
Available figures under the Yellow Card scheme up to 19 May 2024 show that there were 208 adverse drug reactions reported about tirzepatide this year, including 31 serious reactions and one suspected death of a man in his 60s.
In a statement, a spokesperson for the drug’s manufacturer, Eli Lilly, said, “Patient safety is Lilly’s top priority. We are committed to continually monitoring, evaluating, and reporting safety information for all Lilly medicines.
“Mounjaro (tirzepatide) was approved based on extensive assessment of the benefits and risks of the medicine, and we provide information about the benefits and risks of all our medicines to regulators around the world to ensure the latest information is available for prescribers. If anyone is experiencing side effects when taking any Lilly medicine, they should talk to their doctor or other healthcare professional.”
In October, the NHS submitted plans to the National Institute for Health and Care Excellence (NICE) for a phased rollout of tirzepatide in England that would initially prioritize patients with the greatest clinical need. The first phase would see the drug available to people with a body mass index of more than 40 kg/m2 who also suffer from at least three of the main weight-related health problems: hypertension, dyslipidemia, obstructive sleep apnea, and cardiovascular disease.
“Our sincere sympathies are with the family of individual concerned,” said Alison Cave, MHRA Chief Safety Officer.
“Patient safety is our top priority and no medicine would be approved unless it met our expected standards of safety, quality, and effectiveness. Our role is to continually monitor the safety of medicines during their use, such as GLP-1 RAs. We have robust, safety monitoring and surveillance systems in place for all healthcare products.
“New medicines, such as tirzepatide, are more intensively monitored to ensure that any new safety issues are identified promptly. We strongly encourage the reporting of all suspected reactions to newer medicines, which are denoted by an inverted Black Triangle symbol.
“On the basis of the current evidence the benefits of GLP-1 RAs outweigh the potential risks when used for the licensed indications. The decision to start, continue, or stop treatments should be made jointly by patients and their doctor, based on full consideration of the benefits and risks.”
She encouraged patients and healthcare professionals to continue reporting suspected side effects to GLP-1 RAs, such as tirzepatide, through the Yellow Card Scheme. “When a safety issue is confirmed, we always act promptly to inform patients and healthcare professionals and take appropriate steps to mitigate any identified risk.”
The Department of Health and Social Care declined to comment.
Adler disclosed being involved as an unpaid investigator on an Eli Lilly–funded trial for a different drug. Sattar has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Doctors have urged caution in linking the weight loss drug tirzepatide to the death of a 58-year-old nurse from Scotland.
Susan McGowan, from North Lanarkshire, took two low-dose injections of tirzepatide (Mounjaro) over the course of about 2 weeks before her death in September.
BBC News reported that multiple organ failure, septic shock, and pancreatitis were listed on her death certificate as the immediate cause of death, with “the use of prescribed tirzepatide” recorded as a contributing factor.
McGowan worked as a nurse at University Hospital Monklands in Airdrie. A family member said that, apart from carrying a “bit of extra weight,” she had been otherwise healthy and was not taking any other medication.
It is understood that McGowan had sought medical advice before purchasing a prescription for tirzepatide through a registered UK pharmacy. However, days after administering a second injection, she went to A&E at Monklands with severe stomach pain and sickness. She died on September 4.
Expert Insights
Commenting to the Science Media Centre (SMC), Amanda Adler, MD, PhD, professor of diabetic medicine and health policy at the University of Oxford, described the nurse’s death as “sad” but said that “whether or not it was related to tirzepatide may be difficult to prove.” While tirzepatide can be associated with uncommon problems such as acute pancreatitis, “one can develop acute pancreatitis for many other reasons as well,” she said.
Naveed Sattar, MD, PhD, professor of metabolic medicine at the University of Glasgow, noted that data from multiple trials of tirzepatide, involving around 10,000 people living with diabetes or obesity, “do not suggest a higher risk of pancreatitis.” Furthermore, “the data seem to show acceptable safety thus far and a range of benefits including sizable average weight loss (near 20%), strong diabetes prevention, and considerable benefits in people living with sleep apnea,” he told the SMC.
Approved Based on Extensive Assessment
Tirzepatide, a GLP-1 receptor agonist, was approved for use as a weight loss aid in the United Kingdom in November last year by the Medicines and Healthcare products Regulatory Agency (MHRA). It lists nausea, diarrhea, and vomiting as the most common side effects, as well as hypoglycemia for patients with diabetes.
Available figures under the Yellow Card scheme up to 19 May 2024 show that there were 208 adverse drug reactions reported about tirzepatide this year, including 31 serious reactions and one suspected death of a man in his 60s.
In a statement, a spokesperson for the drug’s manufacturer, Eli Lilly, said, “Patient safety is Lilly’s top priority. We are committed to continually monitoring, evaluating, and reporting safety information for all Lilly medicines.
“Mounjaro (tirzepatide) was approved based on extensive assessment of the benefits and risks of the medicine, and we provide information about the benefits and risks of all our medicines to regulators around the world to ensure the latest information is available for prescribers. If anyone is experiencing side effects when taking any Lilly medicine, they should talk to their doctor or other healthcare professional.”
In October, the NHS submitted plans to the National Institute for Health and Care Excellence (NICE) for a phased rollout of tirzepatide in England that would initially prioritize patients with the greatest clinical need. The first phase would see the drug available to people with a body mass index of more than 40 kg/m2 who also suffer from at least three of the main weight-related health problems: hypertension, dyslipidemia, obstructive sleep apnea, and cardiovascular disease.
“Our sincere sympathies are with the family of individual concerned,” said Alison Cave, MHRA Chief Safety Officer.
“Patient safety is our top priority and no medicine would be approved unless it met our expected standards of safety, quality, and effectiveness. Our role is to continually monitor the safety of medicines during their use, such as GLP-1 RAs. We have robust, safety monitoring and surveillance systems in place for all healthcare products.
“New medicines, such as tirzepatide, are more intensively monitored to ensure that any new safety issues are identified promptly. We strongly encourage the reporting of all suspected reactions to newer medicines, which are denoted by an inverted Black Triangle symbol.
“On the basis of the current evidence the benefits of GLP-1 RAs outweigh the potential risks when used for the licensed indications. The decision to start, continue, or stop treatments should be made jointly by patients and their doctor, based on full consideration of the benefits and risks.”
She encouraged patients and healthcare professionals to continue reporting suspected side effects to GLP-1 RAs, such as tirzepatide, through the Yellow Card Scheme. “When a safety issue is confirmed, we always act promptly to inform patients and healthcare professionals and take appropriate steps to mitigate any identified risk.”
The Department of Health and Social Care declined to comment.
Adler disclosed being involved as an unpaid investigator on an Eli Lilly–funded trial for a different drug. Sattar has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Doctors have urged caution in linking the weight loss drug tirzepatide to the death of a 58-year-old nurse from Scotland.
Susan McGowan, from North Lanarkshire, took two low-dose injections of tirzepatide (Mounjaro) over the course of about 2 weeks before her death in September.
BBC News reported that multiple organ failure, septic shock, and pancreatitis were listed on her death certificate as the immediate cause of death, with “the use of prescribed tirzepatide” recorded as a contributing factor.
McGowan worked as a nurse at University Hospital Monklands in Airdrie. A family member said that, apart from carrying a “bit of extra weight,” she had been otherwise healthy and was not taking any other medication.
It is understood that McGowan had sought medical advice before purchasing a prescription for tirzepatide through a registered UK pharmacy. However, days after administering a second injection, she went to A&E at Monklands with severe stomach pain and sickness. She died on September 4.
Expert Insights
Commenting to the Science Media Centre (SMC), Amanda Adler, MD, PhD, professor of diabetic medicine and health policy at the University of Oxford, described the nurse’s death as “sad” but said that “whether or not it was related to tirzepatide may be difficult to prove.” While tirzepatide can be associated with uncommon problems such as acute pancreatitis, “one can develop acute pancreatitis for many other reasons as well,” she said.
Naveed Sattar, MD, PhD, professor of metabolic medicine at the University of Glasgow, noted that data from multiple trials of tirzepatide, involving around 10,000 people living with diabetes or obesity, “do not suggest a higher risk of pancreatitis.” Furthermore, “the data seem to show acceptable safety thus far and a range of benefits including sizable average weight loss (near 20%), strong diabetes prevention, and considerable benefits in people living with sleep apnea,” he told the SMC.
Approved Based on Extensive Assessment
Tirzepatide, a GLP-1 receptor agonist, was approved for use as a weight loss aid in the United Kingdom in November last year by the Medicines and Healthcare products Regulatory Agency (MHRA). It lists nausea, diarrhea, and vomiting as the most common side effects, as well as hypoglycemia for patients with diabetes.
Available figures under the Yellow Card scheme up to 19 May 2024 show that there were 208 adverse drug reactions reported about tirzepatide this year, including 31 serious reactions and one suspected death of a man in his 60s.
In a statement, a spokesperson for the drug’s manufacturer, Eli Lilly, said, “Patient safety is Lilly’s top priority. We are committed to continually monitoring, evaluating, and reporting safety information for all Lilly medicines.
“Mounjaro (tirzepatide) was approved based on extensive assessment of the benefits and risks of the medicine, and we provide information about the benefits and risks of all our medicines to regulators around the world to ensure the latest information is available for prescribers. If anyone is experiencing side effects when taking any Lilly medicine, they should talk to their doctor or other healthcare professional.”
In October, the NHS submitted plans to the National Institute for Health and Care Excellence (NICE) for a phased rollout of tirzepatide in England that would initially prioritize patients with the greatest clinical need. The first phase would see the drug available to people with a body mass index of more than 40 kg/m2 who also suffer from at least three of the main weight-related health problems: hypertension, dyslipidemia, obstructive sleep apnea, and cardiovascular disease.
“Our sincere sympathies are with the family of individual concerned,” said Alison Cave, MHRA Chief Safety Officer.
“Patient safety is our top priority and no medicine would be approved unless it met our expected standards of safety, quality, and effectiveness. Our role is to continually monitor the safety of medicines during their use, such as GLP-1 RAs. We have robust, safety monitoring and surveillance systems in place for all healthcare products.
“New medicines, such as tirzepatide, are more intensively monitored to ensure that any new safety issues are identified promptly. We strongly encourage the reporting of all suspected reactions to newer medicines, which are denoted by an inverted Black Triangle symbol.
“On the basis of the current evidence the benefits of GLP-1 RAs outweigh the potential risks when used for the licensed indications. The decision to start, continue, or stop treatments should be made jointly by patients and their doctor, based on full consideration of the benefits and risks.”
She encouraged patients and healthcare professionals to continue reporting suspected side effects to GLP-1 RAs, such as tirzepatide, through the Yellow Card Scheme. “When a safety issue is confirmed, we always act promptly to inform patients and healthcare professionals and take appropriate steps to mitigate any identified risk.”
The Department of Health and Social Care declined to comment.
Adler disclosed being involved as an unpaid investigator on an Eli Lilly–funded trial for a different drug. Sattar has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Round Face’: A Viral Term’s Real Diagnostic Implications
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
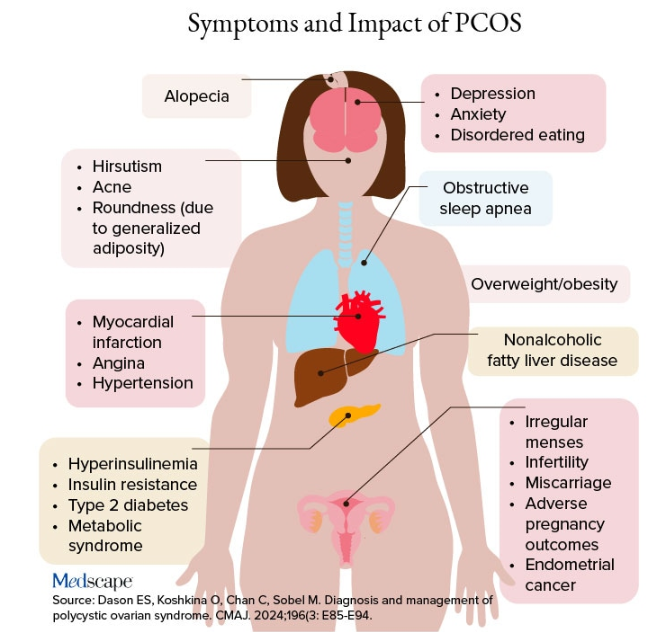
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
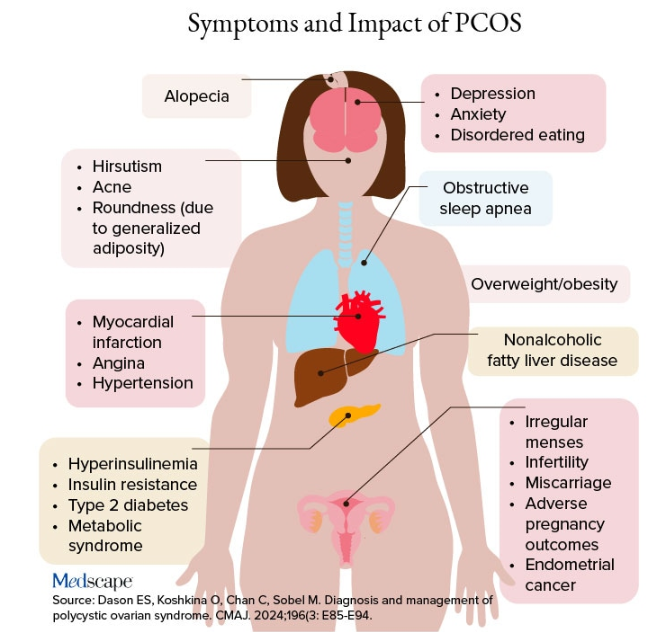
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
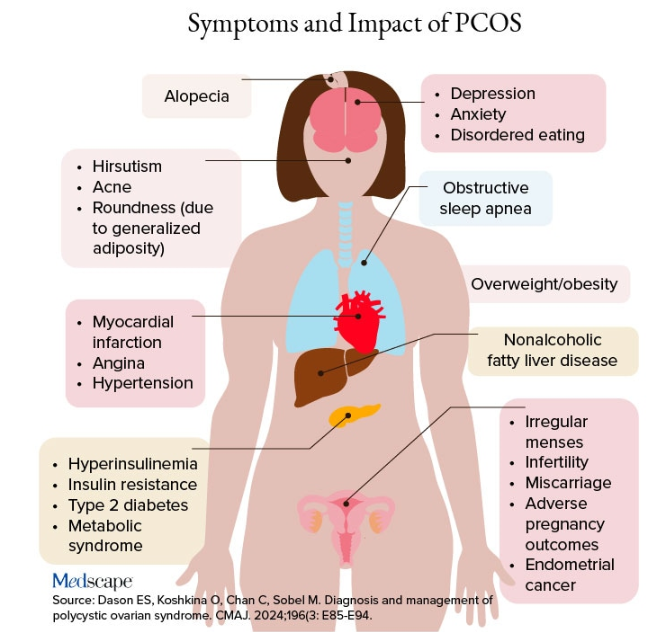
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.