User login
Most TKR Patients Return to Life, Work Following Surgery
Obesity Alone May Not Affect TKR Outcome or Increase Complication Risk
THR May Reduce Mortality, Heart Failure, and Have Other Benefits
CHICAGO—In addition to improving life quality and diminishing pain, total hip replacement (THR) is associated with reduced mortality, heart failure, depression, and diabetes rates in Medicare patients with osteoarthritis, according to a new study presented at the conference. The procedure is cost effective, with the 7-year costs of total hip arthroplasty only $6,366 higher than the cost of treating an osteoarthritis patient for hip pain without THR.
"The study has demonstrated that THR confers a potential long-term benefit in terms of prolonged lifespan and reduced burden of disease in Medicare patients with osteoarthritis of the hip," said lead study author Scott Lovald, PhD, a researcher at Exponent Inc. While the short-term benefits of THR are well known and documented, less information exists on the long-term effects, cost and value of the surgery.
Using Medicare codes, the researchers identified more than 43,000 patients with osteoarthritis of the hip from 1998 to 2009. These patients were divided into those receiving THR and those who did not. The investigators followed all of the patients for at least 1 year, and nearly 24,000 patients for 7 years. They collected data on annual Medicare payments, mortality, and new diagnoses of congestive heart failure, ischemic heart disease, artherosclerosis, diabetes, and depression. The data was adjusted for age, sex, race, buy-in status, region, and Charlson comorbidity score.
Overall, Lovald and colleagues found that THR patients had a consistently lower mortality risk, less than 52% of that in the non-THR group. Heart failure was similar between groups in the first year, but there was a consistent reduced risk—between 0.85 and 0.92 of the risk for the non-THR group—at 3-to-7 years following surgery. THR patients had a reduced risk of diabetes at 1 and 3 years, and THR patients had a reduced rate of depression beginning 3 years post-THR surgery.
The THR patients in the study did have an increased risk of ischemic heart disease and atherosclerosis at 1 year, and an increased risk of "cardiovascular disease unspecified" over all time points.
The 7-year cumulative average Medicare payment for all medical care was $82,788 for non-THR patients and $89,154 for THR patients, a difference of $6,366. The actual average per-patient THR cost is expected to be much less than $6,366 when differences in costs incurred due to prescription pain medications are taken into account.
"Joint [replacement] has been proposed as possibly costsaving in the management of disability related to arthritis," said Lovald. "This study provides supporting data to evaluate the cost-effectiveness of THR."
The "Canoe" Technique to Insert Lumbar Pedicle Screws: Consistent, Safe, and Simple
Bisphosphonates associated with improved hip, knee implant survival
BIRMINGHAM, ENGLAND – Long-term bisphosphonate use reduced the risk for joint implant failure and subsequent hip or knee revision survey in 40% of patients in a large, retrospective, observational study.
The rate for revision surgery at a median of 2.6 years’ follow-up was 1.88% in the 1,911 participants who had taken bisphosphonates for at least 6 months, compared with 4.36% in the 10,755 nonbisphosphonate users (hazard ratio, 0.62).
"The observed effect size is stronger in patients with higher therapy duration and adherence," Dr. Daniel Prieto-Alhambra reported at the annual meeting of the British Society for Rheumatology.
"This association does not differ by age, gender, joint replaced, or fracture history," added Dr. Prieto-Alhambra, senior clinical research fellow from the Nuffield department of orthopaedics, rheumatology, and musculoskeletal sciences at the University of Oxford, England.
Osteolysis and aseptic loosening are the most common causes of revision surgery, the researcher noted, adding that bisphosphonates have antiosteoclast activity that may have potential benefits on implant survival.
"Patients need to be on treatment for at least 6 months for the drug to be effective," Dr. Prieto-Alhambra emphasized. He later said after his presentation that data from a sub-analysis suggest that patients benefit further if they started therapy in the weeks following surgery.*
Data used in the study were obtained from Danish nationwide health registries on more than 80,000 patients aged 40 years or older who had total hip arthroplasty (THA) or total knee arthroplasty (TKA) in Denmark between 1998 and 2007. Patients were excluded if they had experienced a prior hip fracture; had inflammatory arthritis or used disease-modifying antirheumatic drugs; or had Paget’s disease, bone cancer, or metastasis. Baseline characteristics of those who did and those who did not use bisphosphonates were comparable except for calcium and vitamin D supplementation, which was higher in the bisphosphonate-treated group (9.9% vs. 4.8%).
The longer the duration of treatment, the less chance there was for implant failure: 5 implants failed in 352 (1.4%) patients treated with bisphosphonates for more than 2 years (HR, 0.53); 16 (1.6%) in 1,006 patients treated for 1-2 years (HR, 0.52); and 15 (2.7%) in 553 patients treated for 6-12 months (HR, 1.31).
Adherence was assessed using a medication possession ratio (MPR), with lower MPR values indicating poorer adherence. Failure rates were 3%, 2.9%, and 1.5% for MPRs of less than 0.5 (HR, 0.93), 0.5-0.79 (HR, 0.48), and 0.8 or greater (HR, 0.56), respectively.
The study’s findings support those of a recent U.K. population-based, retrospective cohort study (BMJ 2011 [doi:10.1136/bmj.d7222]) that involved more than 41,000 primary THA/TKA patients.
The U.K. data showed that fewer surgical revisions occurred at 5 years in bisphosphonate users (0.93% vs. 1.96% in nonusers), and that there was a 46% decrease in the risk of revision surgery (HR for implant survival of 0.54; P = .047). It was also estimated, however, that at least 107 patients would need to be treated with bisphosphonates to avoid one revision surgery.
Osteoarthritis accounts for more than 90% of THAs and TKAs performed in the United Kingdom, with 1 in 75 patients experiencing implant failure and revision surgery within 3 years of the index surgery. Such surgery is associated with a worse clinical outcome than the primary procedure, and it is also associated with greater health care costs (PLoS Med. 2008;5:e179). Bisphosphonates could potentially offer a simple and hopefully cost-effective solution to reducing the likelihood of such surgery.
"Confirmation in a randomized controlled trial is needed to test the efficacy of bisphosphonates to improve implant survival, Dr. Prieto-Alhambra said.
A 40% reduction in the risk of aseptic loosening of the prosthesis is potentially very good news for patients, observed Dr. Ken Poole, a clinical lecturer at the University of Cambridge, England. Randomized trial data would be welcomed and warranted, he added.
Dr. Poole, who was chairing the session at which these data were presented, highlighted that this was another "good news" story for bisphosphonates, adding to recent evidence that they increased survival after hip fracture and have also been associated with reductions in the incidence of certain cancers.
"Many of my patients are well versed in the potential harms of bisphosphonate treatments for osteoporosis, often because of enthusiastic media coverage of the ‘bad news’ aspect," he said in an interview.
"The upshot is that ‘at-risk’ patients are increasingly reluctant to commence therapy; indeed, it is easy to find out about rare and frightening side effects like osteonecrosis of the jaw and atraumatic fractures of the femur from a few clicks on the Internet," Dr. Poole commented.
Although serious adverse events should be borne in mind when considering treatment choice, Dr. Poole noted that bisphosphonates were effective for osteoporosis in the right patients, and that Dr. Prieto-Alhambra’s study was one of several identifying additional health benefits in patients undergoing total hip or knee replacement.
A poor public perception of bisphosphonates could influence adherence, and there is recent evidence that only 30% of women actually take their prescriptions to the pharmacist (Osteoporos. Int. 2013 [doi:10.1007/s00198-013-2326-5]). Concern over calcium supplementation causing heart attacks and stroke might also be a factor, as this, together with vitamin D, goes along with bisphosphonate use. Indeed, a study of 233 women taking bisphosphonates for osteoporosis also presented at the British Society for Rheumatology meeting found that a lack of concomitant calcium and vitamin D supplementation was predictive of poor adherence (Rheumatology 2013;52[Suppl. 1]:i116-7; abstract 163). Other predictive factors were older age and the use of sleeping tablets.
Dr. Prieto-Alhambra and Dr. Poole had no conflicts of interests.
* Revised, 5/1/13
BIRMINGHAM, ENGLAND – Long-term bisphosphonate use reduced the risk for joint implant failure and subsequent hip or knee revision survey in 40% of patients in a large, retrospective, observational study.
The rate for revision surgery at a median of 2.6 years’ follow-up was 1.88% in the 1,911 participants who had taken bisphosphonates for at least 6 months, compared with 4.36% in the 10,755 nonbisphosphonate users (hazard ratio, 0.62).
"The observed effect size is stronger in patients with higher therapy duration and adherence," Dr. Daniel Prieto-Alhambra reported at the annual meeting of the British Society for Rheumatology.
"This association does not differ by age, gender, joint replaced, or fracture history," added Dr. Prieto-Alhambra, senior clinical research fellow from the Nuffield department of orthopaedics, rheumatology, and musculoskeletal sciences at the University of Oxford, England.
Osteolysis and aseptic loosening are the most common causes of revision surgery, the researcher noted, adding that bisphosphonates have antiosteoclast activity that may have potential benefits on implant survival.
"Patients need to be on treatment for at least 6 months for the drug to be effective," Dr. Prieto-Alhambra emphasized. He later said after his presentation that data from a sub-analysis suggest that patients benefit further if they started therapy in the weeks following surgery.*
Data used in the study were obtained from Danish nationwide health registries on more than 80,000 patients aged 40 years or older who had total hip arthroplasty (THA) or total knee arthroplasty (TKA) in Denmark between 1998 and 2007. Patients were excluded if they had experienced a prior hip fracture; had inflammatory arthritis or used disease-modifying antirheumatic drugs; or had Paget’s disease, bone cancer, or metastasis. Baseline characteristics of those who did and those who did not use bisphosphonates were comparable except for calcium and vitamin D supplementation, which was higher in the bisphosphonate-treated group (9.9% vs. 4.8%).
The longer the duration of treatment, the less chance there was for implant failure: 5 implants failed in 352 (1.4%) patients treated with bisphosphonates for more than 2 years (HR, 0.53); 16 (1.6%) in 1,006 patients treated for 1-2 years (HR, 0.52); and 15 (2.7%) in 553 patients treated for 6-12 months (HR, 1.31).
Adherence was assessed using a medication possession ratio (MPR), with lower MPR values indicating poorer adherence. Failure rates were 3%, 2.9%, and 1.5% for MPRs of less than 0.5 (HR, 0.93), 0.5-0.79 (HR, 0.48), and 0.8 or greater (HR, 0.56), respectively.
The study’s findings support those of a recent U.K. population-based, retrospective cohort study (BMJ 2011 [doi:10.1136/bmj.d7222]) that involved more than 41,000 primary THA/TKA patients.
The U.K. data showed that fewer surgical revisions occurred at 5 years in bisphosphonate users (0.93% vs. 1.96% in nonusers), and that there was a 46% decrease in the risk of revision surgery (HR for implant survival of 0.54; P = .047). It was also estimated, however, that at least 107 patients would need to be treated with bisphosphonates to avoid one revision surgery.
Osteoarthritis accounts for more than 90% of THAs and TKAs performed in the United Kingdom, with 1 in 75 patients experiencing implant failure and revision surgery within 3 years of the index surgery. Such surgery is associated with a worse clinical outcome than the primary procedure, and it is also associated with greater health care costs (PLoS Med. 2008;5:e179). Bisphosphonates could potentially offer a simple and hopefully cost-effective solution to reducing the likelihood of such surgery.
"Confirmation in a randomized controlled trial is needed to test the efficacy of bisphosphonates to improve implant survival, Dr. Prieto-Alhambra said.
A 40% reduction in the risk of aseptic loosening of the prosthesis is potentially very good news for patients, observed Dr. Ken Poole, a clinical lecturer at the University of Cambridge, England. Randomized trial data would be welcomed and warranted, he added.
Dr. Poole, who was chairing the session at which these data were presented, highlighted that this was another "good news" story for bisphosphonates, adding to recent evidence that they increased survival after hip fracture and have also been associated with reductions in the incidence of certain cancers.
"Many of my patients are well versed in the potential harms of bisphosphonate treatments for osteoporosis, often because of enthusiastic media coverage of the ‘bad news’ aspect," he said in an interview.
"The upshot is that ‘at-risk’ patients are increasingly reluctant to commence therapy; indeed, it is easy to find out about rare and frightening side effects like osteonecrosis of the jaw and atraumatic fractures of the femur from a few clicks on the Internet," Dr. Poole commented.
Although serious adverse events should be borne in mind when considering treatment choice, Dr. Poole noted that bisphosphonates were effective for osteoporosis in the right patients, and that Dr. Prieto-Alhambra’s study was one of several identifying additional health benefits in patients undergoing total hip or knee replacement.
A poor public perception of bisphosphonates could influence adherence, and there is recent evidence that only 30% of women actually take their prescriptions to the pharmacist (Osteoporos. Int. 2013 [doi:10.1007/s00198-013-2326-5]). Concern over calcium supplementation causing heart attacks and stroke might also be a factor, as this, together with vitamin D, goes along with bisphosphonate use. Indeed, a study of 233 women taking bisphosphonates for osteoporosis also presented at the British Society for Rheumatology meeting found that a lack of concomitant calcium and vitamin D supplementation was predictive of poor adherence (Rheumatology 2013;52[Suppl. 1]:i116-7; abstract 163). Other predictive factors were older age and the use of sleeping tablets.
Dr. Prieto-Alhambra and Dr. Poole had no conflicts of interests.
* Revised, 5/1/13
BIRMINGHAM, ENGLAND – Long-term bisphosphonate use reduced the risk for joint implant failure and subsequent hip or knee revision survey in 40% of patients in a large, retrospective, observational study.
The rate for revision surgery at a median of 2.6 years’ follow-up was 1.88% in the 1,911 participants who had taken bisphosphonates for at least 6 months, compared with 4.36% in the 10,755 nonbisphosphonate users (hazard ratio, 0.62).
"The observed effect size is stronger in patients with higher therapy duration and adherence," Dr. Daniel Prieto-Alhambra reported at the annual meeting of the British Society for Rheumatology.
"This association does not differ by age, gender, joint replaced, or fracture history," added Dr. Prieto-Alhambra, senior clinical research fellow from the Nuffield department of orthopaedics, rheumatology, and musculoskeletal sciences at the University of Oxford, England.
Osteolysis and aseptic loosening are the most common causes of revision surgery, the researcher noted, adding that bisphosphonates have antiosteoclast activity that may have potential benefits on implant survival.
"Patients need to be on treatment for at least 6 months for the drug to be effective," Dr. Prieto-Alhambra emphasized. He later said after his presentation that data from a sub-analysis suggest that patients benefit further if they started therapy in the weeks following surgery.*
Data used in the study were obtained from Danish nationwide health registries on more than 80,000 patients aged 40 years or older who had total hip arthroplasty (THA) or total knee arthroplasty (TKA) in Denmark between 1998 and 2007. Patients were excluded if they had experienced a prior hip fracture; had inflammatory arthritis or used disease-modifying antirheumatic drugs; or had Paget’s disease, bone cancer, or metastasis. Baseline characteristics of those who did and those who did not use bisphosphonates were comparable except for calcium and vitamin D supplementation, which was higher in the bisphosphonate-treated group (9.9% vs. 4.8%).
The longer the duration of treatment, the less chance there was for implant failure: 5 implants failed in 352 (1.4%) patients treated with bisphosphonates for more than 2 years (HR, 0.53); 16 (1.6%) in 1,006 patients treated for 1-2 years (HR, 0.52); and 15 (2.7%) in 553 patients treated for 6-12 months (HR, 1.31).
Adherence was assessed using a medication possession ratio (MPR), with lower MPR values indicating poorer adherence. Failure rates were 3%, 2.9%, and 1.5% for MPRs of less than 0.5 (HR, 0.93), 0.5-0.79 (HR, 0.48), and 0.8 or greater (HR, 0.56), respectively.
The study’s findings support those of a recent U.K. population-based, retrospective cohort study (BMJ 2011 [doi:10.1136/bmj.d7222]) that involved more than 41,000 primary THA/TKA patients.
The U.K. data showed that fewer surgical revisions occurred at 5 years in bisphosphonate users (0.93% vs. 1.96% in nonusers), and that there was a 46% decrease in the risk of revision surgery (HR for implant survival of 0.54; P = .047). It was also estimated, however, that at least 107 patients would need to be treated with bisphosphonates to avoid one revision surgery.
Osteoarthritis accounts for more than 90% of THAs and TKAs performed in the United Kingdom, with 1 in 75 patients experiencing implant failure and revision surgery within 3 years of the index surgery. Such surgery is associated with a worse clinical outcome than the primary procedure, and it is also associated with greater health care costs (PLoS Med. 2008;5:e179). Bisphosphonates could potentially offer a simple and hopefully cost-effective solution to reducing the likelihood of such surgery.
"Confirmation in a randomized controlled trial is needed to test the efficacy of bisphosphonates to improve implant survival, Dr. Prieto-Alhambra said.
A 40% reduction in the risk of aseptic loosening of the prosthesis is potentially very good news for patients, observed Dr. Ken Poole, a clinical lecturer at the University of Cambridge, England. Randomized trial data would be welcomed and warranted, he added.
Dr. Poole, who was chairing the session at which these data were presented, highlighted that this was another "good news" story for bisphosphonates, adding to recent evidence that they increased survival after hip fracture and have also been associated with reductions in the incidence of certain cancers.
"Many of my patients are well versed in the potential harms of bisphosphonate treatments for osteoporosis, often because of enthusiastic media coverage of the ‘bad news’ aspect," he said in an interview.
"The upshot is that ‘at-risk’ patients are increasingly reluctant to commence therapy; indeed, it is easy to find out about rare and frightening side effects like osteonecrosis of the jaw and atraumatic fractures of the femur from a few clicks on the Internet," Dr. Poole commented.
Although serious adverse events should be borne in mind when considering treatment choice, Dr. Poole noted that bisphosphonates were effective for osteoporosis in the right patients, and that Dr. Prieto-Alhambra’s study was one of several identifying additional health benefits in patients undergoing total hip or knee replacement.
A poor public perception of bisphosphonates could influence adherence, and there is recent evidence that only 30% of women actually take their prescriptions to the pharmacist (Osteoporos. Int. 2013 [doi:10.1007/s00198-013-2326-5]). Concern over calcium supplementation causing heart attacks and stroke might also be a factor, as this, together with vitamin D, goes along with bisphosphonate use. Indeed, a study of 233 women taking bisphosphonates for osteoporosis also presented at the British Society for Rheumatology meeting found that a lack of concomitant calcium and vitamin D supplementation was predictive of poor adherence (Rheumatology 2013;52[Suppl. 1]:i116-7; abstract 163). Other predictive factors were older age and the use of sleeping tablets.
Dr. Prieto-Alhambra and Dr. Poole had no conflicts of interests.
* Revised, 5/1/13
AT THE ANNUAL MEETING OF THE BRITISH SOCIETY FOR RHEUMATOLOGY
Major finding: Revision surgery rates were 1.88% in bisphosphonate users vs. 4.36% in nonusers (HR, 0.62).
Data source: Retrospective, observational, cohort study of primary total hip or knee arthroplasty patients who did (n = 1,911) or did not (n = 10,755) receive 6 months’ bisphosphonate therapy.
Disclosures: Dr. Prieto-Alhambra and Dr. Poole had no conflicts of interests.
Providing an Alternative Treatment Modality for Veterans: Establishing and Evaluating an Acupuncture Clinic in a VA Medical Center
Man, 57, With Dyspnea After Chiropractic Manipulation
A 57-year-old man presented to the emergency department (ED) with a two-day history of worsening shortness of breath, light-headedness, and back pain. The patient, who had a history of ankylosing spondylitis, had been receiving weekly therapy from a chiropractor for about 10 years. One week before presenting to the ED, he had begun to undergo daily manipulations under anesthesia (MUA)—an aggressive chiropractic procedure that is administered while the patient is under monitored, procedural sedation. After the second day of treatment, the patient began to experience worsening back pain and progressive light-headedness and shortness of breath.
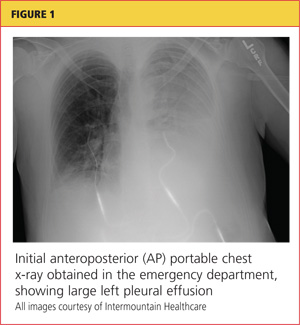
At a follow-up visit with his chiropractor, he was found to have decreased O2 saturation and was directed to go to the hospital for evaluation. On arrival at the ED, the patient was awake and alert. He had intact motor strength in all extremities, no sensory abnormalities, intact symmetric reflexes, and no bladder or bowel dysfunction, with a negative Babinski sign. His O2 saturation was 92% on 5 L of oxygen. An absence of breath sounds was noted on the left side.
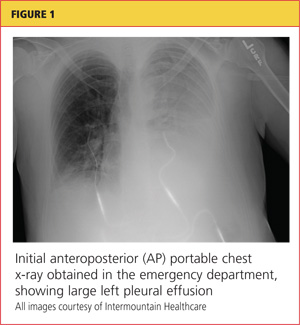
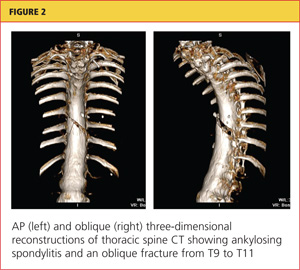
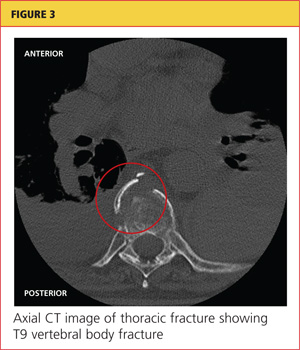
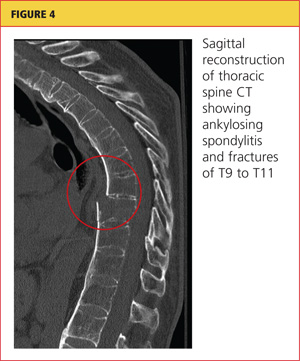
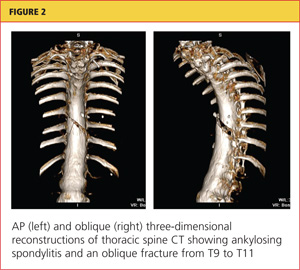
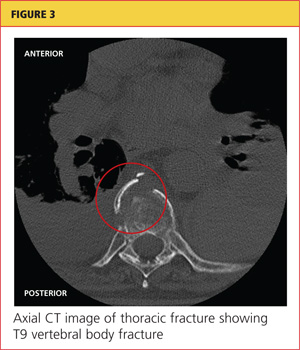
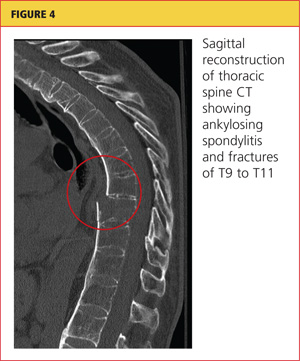
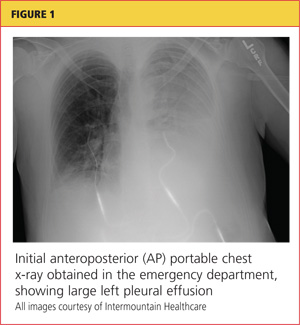
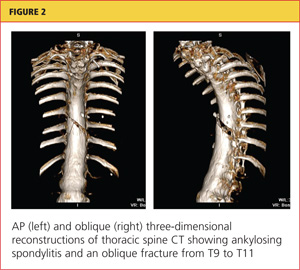
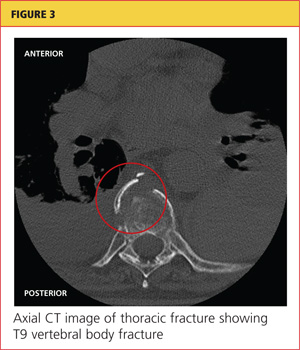
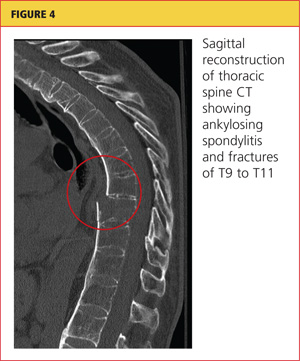
Chest x-ray (see Figure 1) was performed, which demonstrated complete opacification of the left hemithorax, consistent with a large pleural effusion or hemothorax. CT scan of the thoracic spine showed diffuse ankylosis. A complex oblique coronal and transversely oriented fracture with 7 mm of displacement was identified, beginning at the right anterior inferior lateral margin of the T8 vertebral body and extending centrally and inferiorly to the left and right into the T9 vertebral body. The fracture continued through the right T9-10 neural foramen and what was probably the right fused T9-10 facet joint. The fracture exited through the left superior and lateral margin of the T10 vertebral body and the left T10-11 neural foramen (see Figures 2, 3, and 4).
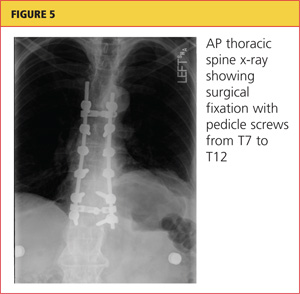
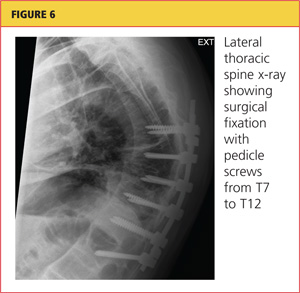
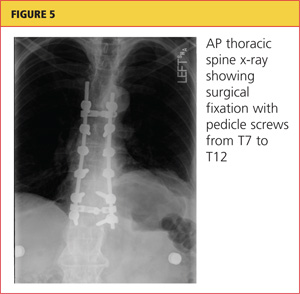
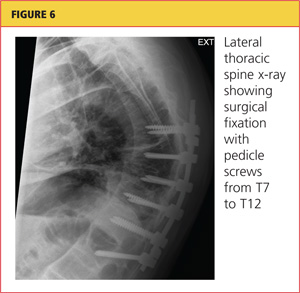
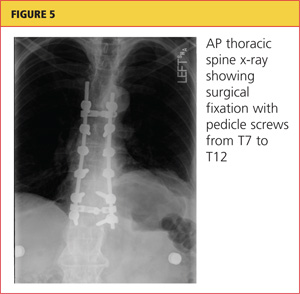
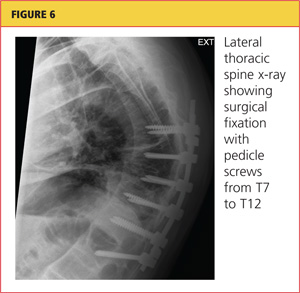
A chest tube was inserted in the ED, and 1,600 mL of old blood was immediately drained. The patient was admitted to the ICU on the trauma service. He was taken to surgery for open reduction and internal fixation of his unstable thoracic spine fracture on day 3 of hospitalization, after his pulmonary condition stabilized. Pedicle screws were placed from T7 through T12 during the spinal fusion. Good reduction of the fracture was observed following the spine surgery (see Figures 5 and 6). At the conclusion of surgery, an epidural catheter was placed in the thoracic spine to administer pain control.
After the spine portion of the procedure, the patient was repositioned and underwent video-assisted thoracoscopic surgery of the left hemithorax for evacuation of retained hemothorax. The patient tolerated the procedure well and was taken to the ICU for recovery.
On postoperative day 2, the patient complained of chest pain and experienced hypoxemia with activity. CT angiography of the chest demonstrated bilateral segmental and subsegmental pulmonary emboli. The epidural catheter was discontinued. Six hours later, a heparin drip was started, and the patient was transitioned to therapeutic enoxaparin and warfarin. When methicillin-sensitive Staphylococcus aureus (MSSA) was detected in his hemothorax fluid, he was treated with a course of nafcillin.
The patient was discharged to home on postoperative day 12. He has remained neurologically intact and has returned to his former work activities. He is not taking narcotic pain medications.
Discussion
Chiropractic care is a popular alternative health care modality in the United States. Researchers for the 2007 National Health Interview Study1 reported an annual use of chiropractic manipulation of 8.6%, while the Medical Expenditure Panel Survey2 data yielded an estimate of 12.6 million adults using chiropractic manipulation in 2006—translating to a prevalence of 5.6%. Despite the popularity of chiropractic medicine, few well-designed studies have been conducted to support its use.3,4 Because of its designation as an alternative therapy, however, chiropractic manipulation has not been subjected to rigorous efficacy and safety evaluations.5
Given the inconsistency of the evidence to support chiropractic manipulation, the practice's safety profile is a concern. The risks associated with spinal manipulation are generally described in case reports and small series. Most serious adverse events described in the literature are cerebrovascular in nature and tend to occur after cervical manipulation.6,7 Fractures after spine manipulation are exceedingly rare, and published literature on this topic consists of a few isolated case reports, with all fractures occurring in the cervical spine in patients with an underlying pathologic condition.8-10
In 2009, Gouveia et al5 reviewed the published literature regarding all adverse events resulting from chiropractic manipulation. The authors found one randomized controlled trial, two case-control studies, six prospective studies, 12 surveys, three retrospective studies, and 100 case reports. The spectrum of complications identified ranged from benign and transient, such as local discomfort, to far more serious: stroke, myelopathy, radiculopathy, subdural hematoma, spinal fluid leakage, cauda equina syndrome, herniated disc, diaphragmatic palsy, and vertebral fractures. The authors were unable to perform a true meta-analysis because of the heterogeneity of the data, but they concluded that complications associated with chiropractic procedures are "frequent."5
Manipulations Under Anesthesia
MUA is a procedure that combines chiropractic adjustments and manipulations with general anesthesia or procedural sedation.11 The theory behind this strategy is that the anesthesia or sedation reduces pain and muscle spasm that may hinder the manipulation, allowing the practitioner to more effectively break up joint adhesions and reduce segmental dysfunction than if the patient had not undergone anesthesia.11
MUA is generally indicated in patients who have not responded to a 4- to 8-week trial of traditional manipulation therapy.12 It is also considered in patients who have "painful and restricting muscular guarding [that] interferes with the performance of spinal adjustments, mobilizations, and soft tissue release techniques."13
In the chiropractic literature, between 3% and 10% of patients are estimated to be candidates for MUA.12,14 It is not completely clear, however, what diagnoses are most likely to be treated successfully with this technique. Contraindications to MUA are generally the same as those for manipulation in conscious patients. A published list of contraindications from the Committee for Manipulation under Anesthesia (2003)15 included malignancy with bony metastasis, tuberculosis of the bone, recent fracture, acute arthritis, acute gout, diabetic neuropathy, syphilitic articular lesions, excessive spinal osteoporosis, disk fragmentation, direct nerve root impingement, and evidence of cord or caudal compression by tumor, ankylosis, or other space-occupying lesions.
MUA generally begins with deep procedural sedation, managed by an anesthesiologist. Once an adequate level of sedation is achieved, the manipulations are performed. Both high- and low-velocity thrusts are used, but it is recommended that the force exerted should be much less, and the manipulations performed with more caution, than in patients who are not anesthetized.12
For the thoracic spine, the patient is manipulated in the supine position with the arms crossed over the chest. The practitioner places one hand in a fist under the spine with the other hand on the patient's crossed arms, then delivers an anterior-to-posterior thrust. This is repeated until all affected segments have been treated.11,12
Literature to support the use of MUA for various indications is largely anecdotal. The largest published series13 is of 177 patients with chronic spinal pain who each underwent three MUA sessions followed by four to six weeks of traditional manipulations. The authors found that pain, as measured by visual analog scale, was reduced by 62% in patients with cervical spine pain, and by 60% in patients with lumbar pain. No adverse events were reported in the study.
Kohlbeck and Haldeman12 reviewed the reported complications of MUA across all published literature. They found that in 17 published papers, the overall complication rate was 0.7%, mainly represented by transitory increased pain. No spinal fractures were reported.
This case demonstrates a rare but serious complication of chiropractic MUA. It is unclear exactly what mechanism of injury led to an unstable thoracic spine fracture with massive hemothorax, and the precise cause will probably never be known. The clinicians who treated the case patient find it curious that the reported rate of adverse events following this procedure is so low, but they suspect an element of reporting bias in the chiropractic literature.
Conclusion
Iatrogenic injury after chiropractic manipulation is uncommon, but it can be devastating. Few serious complications of chiropractic MUA have been reported, but the literature is lacking in well-designed research studies. Despite the dearth of clinical trials to support its safety and efficacy, use of MUA has continued in the chiropractic community. This case demonstrates that serious adverse outcomes can occur, and more rigorous studies are needed to delineate the true benefits and risks of this set of chiropractic procedures.
References
1. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-9.
2. Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2009;45:748-761.
3. Canadian Chiropractic Association; Canadian Federation of Chiropractic Regulatory Boards; Clinical Practice Guidelines Development Initiative; Guidelines Development Committee. Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc. 2005;49:417-421.
4.
Hurwitz EL, Aker PD, Adams AH, et al. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine (Phila Pa 1976). 1996;21:1746-1760.
5.Gouveia LO, Castanho P, Ferreira JJ. Safety of chiropractic interventions: a systematic review. Spine (Phila Pa 1976). 2009;34:E405-E413.
6. Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79:50-65.
7. Nadareishvili Z, Norris JW. Stroke from traumatic arterial dissection. Lancet. 1999;354:159-160.
8. Austin RT. Pathological vertebral fractures after spinal manipulation. Br Med J (Clin Res Ed). 1985;291:1114-1115.
9. Ea HK, Weber AJ, Yon F, Lioté F. Osteoporotic fracture of the dens revealed by cervical manipulation. Joint Bone Spine. 2004;71:246-250.
10. Schmitz A, Lutterbey G, von Engelhardt L, et al. Pathological cervical fracture after spinal manipulation in a pregnant patient. J Manipulative Physiol Ther. 2005;28:633-636.
11. Cremata E, Collins S, Clauson W, et al. Manipulation under anesthesia: a report of four cases. J Manipulative Physiol Ther. 2005;28:526-533.
12. Kohlbeck FJ, Haldeman S. Medication-assisted spinal manipulation. Spine J. 2002;2:288-302.
13. West DT, Mathews RS, Miller MR, Kent GM. Effective management of spinal pain in one hundred seventy-seven patients evaluated for manipulation under anesthesia. J Manipulative Physiol Ther. 1999;22:299-308.
14. Morey LW Jr. Osteopathic manipulation under general anesthesia. J Am Osteopath Assoc. 1973;73:116-127.
15. Tain L, Gunderson C, Cremata E, et al; Committee for Manipulation Under Anesthesia. Recommendations to the Industrial Medical Council Work Group of California for manipulation under anesthesia use for injured workers. Sacramento, CA: Industrial Medical Council; 2003.
A 57-year-old man presented to the emergency department (ED) with a two-day history of worsening shortness of breath, light-headedness, and back pain. The patient, who had a history of ankylosing spondylitis, had been receiving weekly therapy from a chiropractor for about 10 years. One week before presenting to the ED, he had begun to undergo daily manipulations under anesthesia (MUA)—an aggressive chiropractic procedure that is administered while the patient is under monitored, procedural sedation. After the second day of treatment, the patient began to experience worsening back pain and progressive light-headedness and shortness of breath.
At a follow-up visit with his chiropractor, he was found to have decreased O2 saturation and was directed to go to the hospital for evaluation. On arrival at the ED, the patient was awake and alert. He had intact motor strength in all extremities, no sensory abnormalities, intact symmetric reflexes, and no bladder or bowel dysfunction, with a negative Babinski sign. His O2 saturation was 92% on 5 L of oxygen. An absence of breath sounds was noted on the left side.
Chest x-ray (see Figure 1) was performed, which demonstrated complete opacification of the left hemithorax, consistent with a large pleural effusion or hemothorax. CT scan of the thoracic spine showed diffuse ankylosis. A complex oblique coronal and transversely oriented fracture with 7 mm of displacement was identified, beginning at the right anterior inferior lateral margin of the T8 vertebral body and extending centrally and inferiorly to the left and right into the T9 vertebral body. The fracture continued through the right T9-10 neural foramen and what was probably the right fused T9-10 facet joint. The fracture exited through the left superior and lateral margin of the T10 vertebral body and the left T10-11 neural foramen (see Figures 2, 3, and 4).
A chest tube was inserted in the ED, and 1,600 mL of old blood was immediately drained. The patient was admitted to the ICU on the trauma service. He was taken to surgery for open reduction and internal fixation of his unstable thoracic spine fracture on day 3 of hospitalization, after his pulmonary condition stabilized. Pedicle screws were placed from T7 through T12 during the spinal fusion. Good reduction of the fracture was observed following the spine surgery (see Figures 5 and 6). At the conclusion of surgery, an epidural catheter was placed in the thoracic spine to administer pain control.
After the spine portion of the procedure, the patient was repositioned and underwent video-assisted thoracoscopic surgery of the left hemithorax for evacuation of retained hemothorax. The patient tolerated the procedure well and was taken to the ICU for recovery.
On postoperative day 2, the patient complained of chest pain and experienced hypoxemia with activity. CT angiography of the chest demonstrated bilateral segmental and subsegmental pulmonary emboli. The epidural catheter was discontinued. Six hours later, a heparin drip was started, and the patient was transitioned to therapeutic enoxaparin and warfarin. When methicillin-sensitive Staphylococcus aureus (MSSA) was detected in his hemothorax fluid, he was treated with a course of nafcillin.
The patient was discharged to home on postoperative day 12. He has remained neurologically intact and has returned to his former work activities. He is not taking narcotic pain medications.
Discussion
Chiropractic care is a popular alternative health care modality in the United States. Researchers for the 2007 National Health Interview Study1 reported an annual use of chiropractic manipulation of 8.6%, while the Medical Expenditure Panel Survey2 data yielded an estimate of 12.6 million adults using chiropractic manipulation in 2006—translating to a prevalence of 5.6%. Despite the popularity of chiropractic medicine, few well-designed studies have been conducted to support its use.3,4 Because of its designation as an alternative therapy, however, chiropractic manipulation has not been subjected to rigorous efficacy and safety evaluations.5
Given the inconsistency of the evidence to support chiropractic manipulation, the practice's safety profile is a concern. The risks associated with spinal manipulation are generally described in case reports and small series. Most serious adverse events described in the literature are cerebrovascular in nature and tend to occur after cervical manipulation.6,7 Fractures after spine manipulation are exceedingly rare, and published literature on this topic consists of a few isolated case reports, with all fractures occurring in the cervical spine in patients with an underlying pathologic condition.8-10
In 2009, Gouveia et al5 reviewed the published literature regarding all adverse events resulting from chiropractic manipulation. The authors found one randomized controlled trial, two case-control studies, six prospective studies, 12 surveys, three retrospective studies, and 100 case reports. The spectrum of complications identified ranged from benign and transient, such as local discomfort, to far more serious: stroke, myelopathy, radiculopathy, subdural hematoma, spinal fluid leakage, cauda equina syndrome, herniated disc, diaphragmatic palsy, and vertebral fractures. The authors were unable to perform a true meta-analysis because of the heterogeneity of the data, but they concluded that complications associated with chiropractic procedures are "frequent."5
Manipulations Under Anesthesia
MUA is a procedure that combines chiropractic adjustments and manipulations with general anesthesia or procedural sedation.11 The theory behind this strategy is that the anesthesia or sedation reduces pain and muscle spasm that may hinder the manipulation, allowing the practitioner to more effectively break up joint adhesions and reduce segmental dysfunction than if the patient had not undergone anesthesia.11
MUA is generally indicated in patients who have not responded to a 4- to 8-week trial of traditional manipulation therapy.12 It is also considered in patients who have "painful and restricting muscular guarding [that] interferes with the performance of spinal adjustments, mobilizations, and soft tissue release techniques."13
In the chiropractic literature, between 3% and 10% of patients are estimated to be candidates for MUA.12,14 It is not completely clear, however, what diagnoses are most likely to be treated successfully with this technique. Contraindications to MUA are generally the same as those for manipulation in conscious patients. A published list of contraindications from the Committee for Manipulation under Anesthesia (2003)15 included malignancy with bony metastasis, tuberculosis of the bone, recent fracture, acute arthritis, acute gout, diabetic neuropathy, syphilitic articular lesions, excessive spinal osteoporosis, disk fragmentation, direct nerve root impingement, and evidence of cord or caudal compression by tumor, ankylosis, or other space-occupying lesions.
MUA generally begins with deep procedural sedation, managed by an anesthesiologist. Once an adequate level of sedation is achieved, the manipulations are performed. Both high- and low-velocity thrusts are used, but it is recommended that the force exerted should be much less, and the manipulations performed with more caution, than in patients who are not anesthetized.12
For the thoracic spine, the patient is manipulated in the supine position with the arms crossed over the chest. The practitioner places one hand in a fist under the spine with the other hand on the patient's crossed arms, then delivers an anterior-to-posterior thrust. This is repeated until all affected segments have been treated.11,12
Literature to support the use of MUA for various indications is largely anecdotal. The largest published series13 is of 177 patients with chronic spinal pain who each underwent three MUA sessions followed by four to six weeks of traditional manipulations. The authors found that pain, as measured by visual analog scale, was reduced by 62% in patients with cervical spine pain, and by 60% in patients with lumbar pain. No adverse events were reported in the study.
Kohlbeck and Haldeman12 reviewed the reported complications of MUA across all published literature. They found that in 17 published papers, the overall complication rate was 0.7%, mainly represented by transitory increased pain. No spinal fractures were reported.
This case demonstrates a rare but serious complication of chiropractic MUA. It is unclear exactly what mechanism of injury led to an unstable thoracic spine fracture with massive hemothorax, and the precise cause will probably never be known. The clinicians who treated the case patient find it curious that the reported rate of adverse events following this procedure is so low, but they suspect an element of reporting bias in the chiropractic literature.
Conclusion
Iatrogenic injury after chiropractic manipulation is uncommon, but it can be devastating. Few serious complications of chiropractic MUA have been reported, but the literature is lacking in well-designed research studies. Despite the dearth of clinical trials to support its safety and efficacy, use of MUA has continued in the chiropractic community. This case demonstrates that serious adverse outcomes can occur, and more rigorous studies are needed to delineate the true benefits and risks of this set of chiropractic procedures.
References
1. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-9.
2. Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2009;45:748-761.
3. Canadian Chiropractic Association; Canadian Federation of Chiropractic Regulatory Boards; Clinical Practice Guidelines Development Initiative; Guidelines Development Committee. Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc. 2005;49:417-421.
4.
Hurwitz EL, Aker PD, Adams AH, et al. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine (Phila Pa 1976). 1996;21:1746-1760.
5.Gouveia LO, Castanho P, Ferreira JJ. Safety of chiropractic interventions: a systematic review. Spine (Phila Pa 1976). 2009;34:E405-E413.
6. Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79:50-65.
7. Nadareishvili Z, Norris JW. Stroke from traumatic arterial dissection. Lancet. 1999;354:159-160.
8. Austin RT. Pathological vertebral fractures after spinal manipulation. Br Med J (Clin Res Ed). 1985;291:1114-1115.
9. Ea HK, Weber AJ, Yon F, Lioté F. Osteoporotic fracture of the dens revealed by cervical manipulation. Joint Bone Spine. 2004;71:246-250.
10. Schmitz A, Lutterbey G, von Engelhardt L, et al. Pathological cervical fracture after spinal manipulation in a pregnant patient. J Manipulative Physiol Ther. 2005;28:633-636.
11. Cremata E, Collins S, Clauson W, et al. Manipulation under anesthesia: a report of four cases. J Manipulative Physiol Ther. 2005;28:526-533.
12. Kohlbeck FJ, Haldeman S. Medication-assisted spinal manipulation. Spine J. 2002;2:288-302.
13. West DT, Mathews RS, Miller MR, Kent GM. Effective management of spinal pain in one hundred seventy-seven patients evaluated for manipulation under anesthesia. J Manipulative Physiol Ther. 1999;22:299-308.
14. Morey LW Jr. Osteopathic manipulation under general anesthesia. J Am Osteopath Assoc. 1973;73:116-127.
15. Tain L, Gunderson C, Cremata E, et al; Committee for Manipulation Under Anesthesia. Recommendations to the Industrial Medical Council Work Group of California for manipulation under anesthesia use for injured workers. Sacramento, CA: Industrial Medical Council; 2003.
A 57-year-old man presented to the emergency department (ED) with a two-day history of worsening shortness of breath, light-headedness, and back pain. The patient, who had a history of ankylosing spondylitis, had been receiving weekly therapy from a chiropractor for about 10 years. One week before presenting to the ED, he had begun to undergo daily manipulations under anesthesia (MUA)—an aggressive chiropractic procedure that is administered while the patient is under monitored, procedural sedation. After the second day of treatment, the patient began to experience worsening back pain and progressive light-headedness and shortness of breath.
At a follow-up visit with his chiropractor, he was found to have decreased O2 saturation and was directed to go to the hospital for evaluation. On arrival at the ED, the patient was awake and alert. He had intact motor strength in all extremities, no sensory abnormalities, intact symmetric reflexes, and no bladder or bowel dysfunction, with a negative Babinski sign. His O2 saturation was 92% on 5 L of oxygen. An absence of breath sounds was noted on the left side.
Chest x-ray (see Figure 1) was performed, which demonstrated complete opacification of the left hemithorax, consistent with a large pleural effusion or hemothorax. CT scan of the thoracic spine showed diffuse ankylosis. A complex oblique coronal and transversely oriented fracture with 7 mm of displacement was identified, beginning at the right anterior inferior lateral margin of the T8 vertebral body and extending centrally and inferiorly to the left and right into the T9 vertebral body. The fracture continued through the right T9-10 neural foramen and what was probably the right fused T9-10 facet joint. The fracture exited through the left superior and lateral margin of the T10 vertebral body and the left T10-11 neural foramen (see Figures 2, 3, and 4).
A chest tube was inserted in the ED, and 1,600 mL of old blood was immediately drained. The patient was admitted to the ICU on the trauma service. He was taken to surgery for open reduction and internal fixation of his unstable thoracic spine fracture on day 3 of hospitalization, after his pulmonary condition stabilized. Pedicle screws were placed from T7 through T12 during the spinal fusion. Good reduction of the fracture was observed following the spine surgery (see Figures 5 and 6). At the conclusion of surgery, an epidural catheter was placed in the thoracic spine to administer pain control.
After the spine portion of the procedure, the patient was repositioned and underwent video-assisted thoracoscopic surgery of the left hemithorax for evacuation of retained hemothorax. The patient tolerated the procedure well and was taken to the ICU for recovery.
On postoperative day 2, the patient complained of chest pain and experienced hypoxemia with activity. CT angiography of the chest demonstrated bilateral segmental and subsegmental pulmonary emboli. The epidural catheter was discontinued. Six hours later, a heparin drip was started, and the patient was transitioned to therapeutic enoxaparin and warfarin. When methicillin-sensitive Staphylococcus aureus (MSSA) was detected in his hemothorax fluid, he was treated with a course of nafcillin.
The patient was discharged to home on postoperative day 12. He has remained neurologically intact and has returned to his former work activities. He is not taking narcotic pain medications.
Discussion
Chiropractic care is a popular alternative health care modality in the United States. Researchers for the 2007 National Health Interview Study1 reported an annual use of chiropractic manipulation of 8.6%, while the Medical Expenditure Panel Survey2 data yielded an estimate of 12.6 million adults using chiropractic manipulation in 2006—translating to a prevalence of 5.6%. Despite the popularity of chiropractic medicine, few well-designed studies have been conducted to support its use.3,4 Because of its designation as an alternative therapy, however, chiropractic manipulation has not been subjected to rigorous efficacy and safety evaluations.5
Given the inconsistency of the evidence to support chiropractic manipulation, the practice's safety profile is a concern. The risks associated with spinal manipulation are generally described in case reports and small series. Most serious adverse events described in the literature are cerebrovascular in nature and tend to occur after cervical manipulation.6,7 Fractures after spine manipulation are exceedingly rare, and published literature on this topic consists of a few isolated case reports, with all fractures occurring in the cervical spine in patients with an underlying pathologic condition.8-10
In 2009, Gouveia et al5 reviewed the published literature regarding all adverse events resulting from chiropractic manipulation. The authors found one randomized controlled trial, two case-control studies, six prospective studies, 12 surveys, three retrospective studies, and 100 case reports. The spectrum of complications identified ranged from benign and transient, such as local discomfort, to far more serious: stroke, myelopathy, radiculopathy, subdural hematoma, spinal fluid leakage, cauda equina syndrome, herniated disc, diaphragmatic palsy, and vertebral fractures. The authors were unable to perform a true meta-analysis because of the heterogeneity of the data, but they concluded that complications associated with chiropractic procedures are "frequent."5
Manipulations Under Anesthesia
MUA is a procedure that combines chiropractic adjustments and manipulations with general anesthesia or procedural sedation.11 The theory behind this strategy is that the anesthesia or sedation reduces pain and muscle spasm that may hinder the manipulation, allowing the practitioner to more effectively break up joint adhesions and reduce segmental dysfunction than if the patient had not undergone anesthesia.11
MUA is generally indicated in patients who have not responded to a 4- to 8-week trial of traditional manipulation therapy.12 It is also considered in patients who have "painful and restricting muscular guarding [that] interferes with the performance of spinal adjustments, mobilizations, and soft tissue release techniques."13
In the chiropractic literature, between 3% and 10% of patients are estimated to be candidates for MUA.12,14 It is not completely clear, however, what diagnoses are most likely to be treated successfully with this technique. Contraindications to MUA are generally the same as those for manipulation in conscious patients. A published list of contraindications from the Committee for Manipulation under Anesthesia (2003)15 included malignancy with bony metastasis, tuberculosis of the bone, recent fracture, acute arthritis, acute gout, diabetic neuropathy, syphilitic articular lesions, excessive spinal osteoporosis, disk fragmentation, direct nerve root impingement, and evidence of cord or caudal compression by tumor, ankylosis, or other space-occupying lesions.
MUA generally begins with deep procedural sedation, managed by an anesthesiologist. Once an adequate level of sedation is achieved, the manipulations are performed. Both high- and low-velocity thrusts are used, but it is recommended that the force exerted should be much less, and the manipulations performed with more caution, than in patients who are not anesthetized.12
For the thoracic spine, the patient is manipulated in the supine position with the arms crossed over the chest. The practitioner places one hand in a fist under the spine with the other hand on the patient's crossed arms, then delivers an anterior-to-posterior thrust. This is repeated until all affected segments have been treated.11,12
Literature to support the use of MUA for various indications is largely anecdotal. The largest published series13 is of 177 patients with chronic spinal pain who each underwent three MUA sessions followed by four to six weeks of traditional manipulations. The authors found that pain, as measured by visual analog scale, was reduced by 62% in patients with cervical spine pain, and by 60% in patients with lumbar pain. No adverse events were reported in the study.
Kohlbeck and Haldeman12 reviewed the reported complications of MUA across all published literature. They found that in 17 published papers, the overall complication rate was 0.7%, mainly represented by transitory increased pain. No spinal fractures were reported.
This case demonstrates a rare but serious complication of chiropractic MUA. It is unclear exactly what mechanism of injury led to an unstable thoracic spine fracture with massive hemothorax, and the precise cause will probably never be known. The clinicians who treated the case patient find it curious that the reported rate of adverse events following this procedure is so low, but they suspect an element of reporting bias in the chiropractic literature.
Conclusion
Iatrogenic injury after chiropractic manipulation is uncommon, but it can be devastating. Few serious complications of chiropractic MUA have been reported, but the literature is lacking in well-designed research studies. Despite the dearth of clinical trials to support its safety and efficacy, use of MUA has continued in the chiropractic community. This case demonstrates that serious adverse outcomes can occur, and more rigorous studies are needed to delineate the true benefits and risks of this set of chiropractic procedures.
References
1. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-9.
2. Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2009;45:748-761.
3. Canadian Chiropractic Association; Canadian Federation of Chiropractic Regulatory Boards; Clinical Practice Guidelines Development Initiative; Guidelines Development Committee. Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc. 2005;49:417-421.
4.
Hurwitz EL, Aker PD, Adams AH, et al. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine (Phila Pa 1976). 1996;21:1746-1760.
5.Gouveia LO, Castanho P, Ferreira JJ. Safety of chiropractic interventions: a systematic review. Spine (Phila Pa 1976). 2009;34:E405-E413.
6. Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79:50-65.
7. Nadareishvili Z, Norris JW. Stroke from traumatic arterial dissection. Lancet. 1999;354:159-160.
8. Austin RT. Pathological vertebral fractures after spinal manipulation. Br Med J (Clin Res Ed). 1985;291:1114-1115.
9. Ea HK, Weber AJ, Yon F, Lioté F. Osteoporotic fracture of the dens revealed by cervical manipulation. Joint Bone Spine. 2004;71:246-250.
10. Schmitz A, Lutterbey G, von Engelhardt L, et al. Pathological cervical fracture after spinal manipulation in a pregnant patient. J Manipulative Physiol Ther. 2005;28:633-636.
11. Cremata E, Collins S, Clauson W, et al. Manipulation under anesthesia: a report of four cases. J Manipulative Physiol Ther. 2005;28:526-533.
12. Kohlbeck FJ, Haldeman S. Medication-assisted spinal manipulation. Spine J. 2002;2:288-302.
13. West DT, Mathews RS, Miller MR, Kent GM. Effective management of spinal pain in one hundred seventy-seven patients evaluated for manipulation under anesthesia. J Manipulative Physiol Ther. 1999;22:299-308.
14. Morey LW Jr. Osteopathic manipulation under general anesthesia. J Am Osteopath Assoc. 1973;73:116-127.
15. Tain L, Gunderson C, Cremata E, et al; Committee for Manipulation Under Anesthesia. Recommendations to the Industrial Medical Council Work Group of California for manipulation under anesthesia use for injured workers. Sacramento, CA: Industrial Medical Council; 2003.