User login
Serum Creatinine Elevations: Red Flag After Noncardiac Surgery
SAN DIEGO – Patients who have minor elevations in serum creatinine after noncardiac surgery may be more likely to require a longer postoperative hospital stay and face a twofold increased risk of dying during that stay, preliminary data from a German study have shown.
"This is a big problem, because minor kidney dysfunction may not be noticed postoperatively," Dr. Felix Kork said in an interview during a poster session at Kidney Week 2012 "About 2% of people in general have a small increase in serum creatinine. They are at a greater risk of dying and staying longer in the hospital. Therapeutic options are needed to prevent this minor kidney dysfunction perioperatively."
Dr. Kork of the department of anesthesiology and intensive care medicine at Charité Hospital in Berlin and his associates retrospectively studied the records of 27,616 patients who underwent noncardiac surgery at Charité between 2006 and 2012. The researchers evaluated perioperative renal function by serum creatinine level.
After doing a multivariate analysis that adjusted for age, comorbidities, renal function, high-risk surgery, and postoperative admission to the ICU, the researchers observed that minor elevations in serum creatinine (defined as a range from 0.25 to 0.50 mg/dL) were independently associated with a prolonged hospital length of stay (HR for early discharge, 0.81) and a twofold increased risk of death during the postoperative hospital stay (OR, 1.99) compared with patients without an increase in serum creatinine level. Both findings were statistically significant.
"While adjusting for covariates, we also found that having received radio contrast agent before surgery is independently associated with a greater risk of mortality and hospital length of stay, whether there was kidney dysfunction after the radio contrast agent or not," Dr. Kork added. "We’re still looking into that [association]. It could be that those patients were sicker."
He acknowledged that the study’s retrospective design is a limitation. Because of this "we can only show the association between the serum creatinine increase and the outcome," he said. "We are planning a prospective study right now." Dr. Kork explained that the current study has been submitted for publication in an undisclosed journal, which will contain more detail about these findings.
Dr. Kork said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who have minor elevations in serum creatinine after noncardiac surgery may be more likely to require a longer postoperative hospital stay and face a twofold increased risk of dying during that stay, preliminary data from a German study have shown.
"This is a big problem, because minor kidney dysfunction may not be noticed postoperatively," Dr. Felix Kork said in an interview during a poster session at Kidney Week 2012 "About 2% of people in general have a small increase in serum creatinine. They are at a greater risk of dying and staying longer in the hospital. Therapeutic options are needed to prevent this minor kidney dysfunction perioperatively."
Dr. Kork of the department of anesthesiology and intensive care medicine at Charité Hospital in Berlin and his associates retrospectively studied the records of 27,616 patients who underwent noncardiac surgery at Charité between 2006 and 2012. The researchers evaluated perioperative renal function by serum creatinine level.
After doing a multivariate analysis that adjusted for age, comorbidities, renal function, high-risk surgery, and postoperative admission to the ICU, the researchers observed that minor elevations in serum creatinine (defined as a range from 0.25 to 0.50 mg/dL) were independently associated with a prolonged hospital length of stay (HR for early discharge, 0.81) and a twofold increased risk of death during the postoperative hospital stay (OR, 1.99) compared with patients without an increase in serum creatinine level. Both findings were statistically significant.
"While adjusting for covariates, we also found that having received radio contrast agent before surgery is independently associated with a greater risk of mortality and hospital length of stay, whether there was kidney dysfunction after the radio contrast agent or not," Dr. Kork added. "We’re still looking into that [association]. It could be that those patients were sicker."
He acknowledged that the study’s retrospective design is a limitation. Because of this "we can only show the association between the serum creatinine increase and the outcome," he said. "We are planning a prospective study right now." Dr. Kork explained that the current study has been submitted for publication in an undisclosed journal, which will contain more detail about these findings.
Dr. Kork said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who have minor elevations in serum creatinine after noncardiac surgery may be more likely to require a longer postoperative hospital stay and face a twofold increased risk of dying during that stay, preliminary data from a German study have shown.
"This is a big problem, because minor kidney dysfunction may not be noticed postoperatively," Dr. Felix Kork said in an interview during a poster session at Kidney Week 2012 "About 2% of people in general have a small increase in serum creatinine. They are at a greater risk of dying and staying longer in the hospital. Therapeutic options are needed to prevent this minor kidney dysfunction perioperatively."
Dr. Kork of the department of anesthesiology and intensive care medicine at Charité Hospital in Berlin and his associates retrospectively studied the records of 27,616 patients who underwent noncardiac surgery at Charité between 2006 and 2012. The researchers evaluated perioperative renal function by serum creatinine level.
After doing a multivariate analysis that adjusted for age, comorbidities, renal function, high-risk surgery, and postoperative admission to the ICU, the researchers observed that minor elevations in serum creatinine (defined as a range from 0.25 to 0.50 mg/dL) were independently associated with a prolonged hospital length of stay (HR for early discharge, 0.81) and a twofold increased risk of death during the postoperative hospital stay (OR, 1.99) compared with patients without an increase in serum creatinine level. Both findings were statistically significant.
"While adjusting for covariates, we also found that having received radio contrast agent before surgery is independently associated with a greater risk of mortality and hospital length of stay, whether there was kidney dysfunction after the radio contrast agent or not," Dr. Kork added. "We’re still looking into that [association]. It could be that those patients were sicker."
He acknowledged that the study’s retrospective design is a limitation. Because of this "we can only show the association between the serum creatinine increase and the outcome," he said. "We are planning a prospective study right now." Dr. Kork explained that the current study has been submitted for publication in an undisclosed journal, which will contain more detail about these findings.
Dr. Kork said that he had no relevant financial conflicts to disclose.
AT KIDNEY WEEK 2012
Major Finding: Patients who experienced minor elevations in serum creatinine after noncardiac surgery had an increased risk of a prolonged hospital length of stay (HR for early discharge, 0.81; P less than .01) and a twofold increased risk of death during the postoperative hospital stay (OR, 1.99; P less than .01).
Data Source: A study of 27,616 patients who underwent noncardiac surgery at Charité Hospital in Berlin between 2006 and 2012.
Disclosures: Dr. Kork said he had no relevant financial conflicts to disclose.
Recent Evidence Challenges Four Inpatient Management Habits
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Rivaroxaban Now Approved for DVT, PE Treatment
The oral anticoagulant rivaroxaban has been approved for the treatment of deep vein thrombosis or pulmonary embolism and for reducing the recurrence of DVT and PE after initial treatment, the Food and Drug Administration announced Nov. 5.
The expanded approval was based on the results of three studies of almost 9,500 patients with a DVT or PE which found that treatment with rivaroxaban was as effective as the combination of the low molecular weight heparin enoxaparin and a vitamin K antagonist in treating DVT and PE. In one of the studies, continued treatment with rivaroxaban reduced the risk of recurrent DVT and PE, according to an FDA statement.
Rivaroxaban, a factor Xa inhibitor, was initially approved in July 2011 for prophylaxis of DVT or PE in patients undergoing hip replacement or knee-replacement surgery, at a dose of 10 mg orally once a day. Marketed as Xarelto by Janssen Pharmaceuticals, it received in November 2011 a second indication for reducing the risk of stroke in patients with nonvalvular atrial fibrillation.
The FDA is currently reviewing the company’s applications to approve rivaroxaban for reducing the risk of stent thrombosis in patients with acute coronary syndrome and for reducing the risk of secondary cardiovascular events in patients with ACS, according to Janssen.
The oral anticoagulant rivaroxaban has been approved for the treatment of deep vein thrombosis or pulmonary embolism and for reducing the recurrence of DVT and PE after initial treatment, the Food and Drug Administration announced Nov. 5.
The expanded approval was based on the results of three studies of almost 9,500 patients with a DVT or PE which found that treatment with rivaroxaban was as effective as the combination of the low molecular weight heparin enoxaparin and a vitamin K antagonist in treating DVT and PE. In one of the studies, continued treatment with rivaroxaban reduced the risk of recurrent DVT and PE, according to an FDA statement.
Rivaroxaban, a factor Xa inhibitor, was initially approved in July 2011 for prophylaxis of DVT or PE in patients undergoing hip replacement or knee-replacement surgery, at a dose of 10 mg orally once a day. Marketed as Xarelto by Janssen Pharmaceuticals, it received in November 2011 a second indication for reducing the risk of stroke in patients with nonvalvular atrial fibrillation.
The FDA is currently reviewing the company’s applications to approve rivaroxaban for reducing the risk of stent thrombosis in patients with acute coronary syndrome and for reducing the risk of secondary cardiovascular events in patients with ACS, according to Janssen.
The oral anticoagulant rivaroxaban has been approved for the treatment of deep vein thrombosis or pulmonary embolism and for reducing the recurrence of DVT and PE after initial treatment, the Food and Drug Administration announced Nov. 5.
The expanded approval was based on the results of three studies of almost 9,500 patients with a DVT or PE which found that treatment with rivaroxaban was as effective as the combination of the low molecular weight heparin enoxaparin and a vitamin K antagonist in treating DVT and PE. In one of the studies, continued treatment with rivaroxaban reduced the risk of recurrent DVT and PE, according to an FDA statement.
Rivaroxaban, a factor Xa inhibitor, was initially approved in July 2011 for prophylaxis of DVT or PE in patients undergoing hip replacement or knee-replacement surgery, at a dose of 10 mg orally once a day. Marketed as Xarelto by Janssen Pharmaceuticals, it received in November 2011 a second indication for reducing the risk of stroke in patients with nonvalvular atrial fibrillation.
The FDA is currently reviewing the company’s applications to approve rivaroxaban for reducing the risk of stent thrombosis in patients with acute coronary syndrome and for reducing the risk of secondary cardiovascular events in patients with ACS, according to Janssen.
Pneumonia Prevalence Highest of Health Care-Associated Infections
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
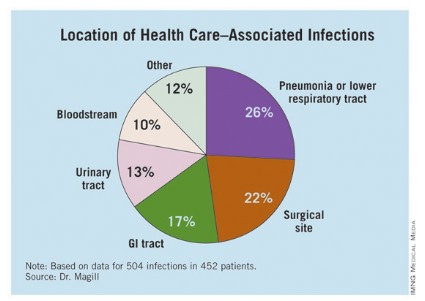
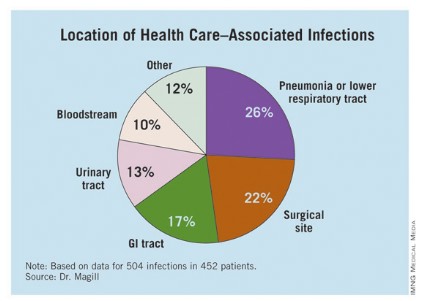
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
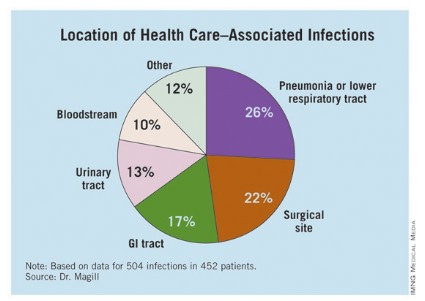
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
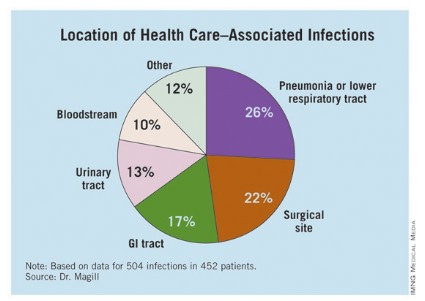
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
AT IDWEEK 2012
Major Finding: The overall prevalence of health care–associated infections among hospitalized patients nationwide was 4%.
Data Source: Preliminary results were obtained from a 2011 survey of 11,282 inpatients at 183 hospitals located in 10 states.
Disclosures: The study was conducted by the Centers for Disease Control and Prevention. Dr. Magill said she had no relevant financial conflicts to disclose.
Stewardship Team Caught Drug Errors in Hospitalized HIV Patients
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
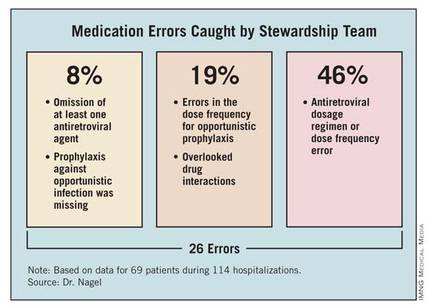
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
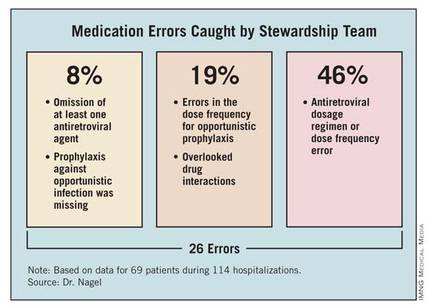
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
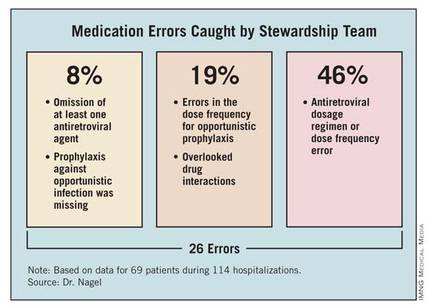
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: An antimicrobial stewardship team identified 26 errors associated with HIV-associated medications in 69 hospitalized patients with HIV over a 9-month period.
Data Source: This was a prospective study using a team for daily evaluation of drug regimens in HIV-infected patients at one institution from March to December 2011.
Disclosures: Dr. Nagel reported having no financial disclosures.
Hospital Complexity Mitigates Mortality
CHICAGO – Surgical patients receiving care at the least complex hospitals had a 50% increased risk of death compared with those treated at more complex hospitals, based on data from more than 400,000 patients.
Data from previous research suggest that the characteristics of individual hospitals predict surgical outcomes, but the relationship between hospital complexity and surgical mortality has not been well studied, Dr. Marta McCrum said at the annual clinical congress of the American College of Surgeons.
She and her colleagues reviewed Medicare administrative claims data from 2008-2009 and information on hospital characteristics from the American Hospital Association Survey 2009 on 2,695 hospitals. The hospitals were divided into quintiles based on complexity, which for purposes of this study was defined as the number of unique diagnoses and procedures performed at each facility.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals."
"Hospitals that see a wide variety of conditions (common problems but also very rare or complicated diagnoses) would be equipped with the wide range of services and resources needed to support them – that is, they would be complex. Similarly, hospitals that perform the widest range of unique procedures would also have the greatest diversity of services and technology," Dr. McCrum of Harvard University, Boston, explained in an interview.
"We therefore ranked the hospitals separately based on the number of unique diagnoses and procedures they saw, and then summed the ranks to assign a numeric value to the complexity of that hospital in comparison to the others. For the analysis, we separated the hospitals into quintiles based on this value."
Not surprisingly, low-complexity hospitals tended to be smaller, more rural, and located in lower-income areas, and the more complex hospitals tended to be larger, urban, and in higher-income areas, she said.
"Of note, the surgical mortality rate of the highest-complexity hospitals was 7.3%, versus 12.6% at the lowest-complexity hospitals," for an absolute risk reduction of 5.3%, she said.
The researchers controlled for hospital and population characteristics, including total number of hospital discharges, public/private ownership, percentage of Medicare patients, urban location, and county income. Hospital complexity remained a significant predictor of mortality between each quintile compared with the highest-complexity quintile.
"The average aggregate mortality rate at the lowest-complexity hospitals is 46% higher than that of the highest-complexity hospitals," said Dr. McCrum.
Overall, the research model explained 28% of the variability in mortality rates, and within the model, hospital complexity explained the greatest proportion of variability in mortality rates. Although hospital volume was a statistically significant predictor of mortality, the effect was small, she noted.
The study was limited by the fact that approximately two-thirds of the variability remained unexplained, likely due to a combination of patient factors and hospital factors, she said. Additional limitations included the lack of an existing metric to measure hospital complexity, and the limitations of using administrative claims data.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals," Dr. McCrum said in an interview. "This might be due in part to the expanded capabilities and systems of care present at these centers. By identifying these lifesaving elements that are cultivated in complex centers, and making them available in lower-complexity hospitals, we can ensure that all surgical procedures take place in facilities with the appropriate systems to support them," she said.
Dr. McCrum had no financial conflicts to disclose.
CHICAGO – Surgical patients receiving care at the least complex hospitals had a 50% increased risk of death compared with those treated at more complex hospitals, based on data from more than 400,000 patients.
Data from previous research suggest that the characteristics of individual hospitals predict surgical outcomes, but the relationship between hospital complexity and surgical mortality has not been well studied, Dr. Marta McCrum said at the annual clinical congress of the American College of Surgeons.
She and her colleagues reviewed Medicare administrative claims data from 2008-2009 and information on hospital characteristics from the American Hospital Association Survey 2009 on 2,695 hospitals. The hospitals were divided into quintiles based on complexity, which for purposes of this study was defined as the number of unique diagnoses and procedures performed at each facility.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals."
"Hospitals that see a wide variety of conditions (common problems but also very rare or complicated diagnoses) would be equipped with the wide range of services and resources needed to support them – that is, they would be complex. Similarly, hospitals that perform the widest range of unique procedures would also have the greatest diversity of services and technology," Dr. McCrum of Harvard University, Boston, explained in an interview.
"We therefore ranked the hospitals separately based on the number of unique diagnoses and procedures they saw, and then summed the ranks to assign a numeric value to the complexity of that hospital in comparison to the others. For the analysis, we separated the hospitals into quintiles based on this value."
Not surprisingly, low-complexity hospitals tended to be smaller, more rural, and located in lower-income areas, and the more complex hospitals tended to be larger, urban, and in higher-income areas, she said.
"Of note, the surgical mortality rate of the highest-complexity hospitals was 7.3%, versus 12.6% at the lowest-complexity hospitals," for an absolute risk reduction of 5.3%, she said.
The researchers controlled for hospital and population characteristics, including total number of hospital discharges, public/private ownership, percentage of Medicare patients, urban location, and county income. Hospital complexity remained a significant predictor of mortality between each quintile compared with the highest-complexity quintile.
"The average aggregate mortality rate at the lowest-complexity hospitals is 46% higher than that of the highest-complexity hospitals," said Dr. McCrum.
Overall, the research model explained 28% of the variability in mortality rates, and within the model, hospital complexity explained the greatest proportion of variability in mortality rates. Although hospital volume was a statistically significant predictor of mortality, the effect was small, she noted.
The study was limited by the fact that approximately two-thirds of the variability remained unexplained, likely due to a combination of patient factors and hospital factors, she said. Additional limitations included the lack of an existing metric to measure hospital complexity, and the limitations of using administrative claims data.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals," Dr. McCrum said in an interview. "This might be due in part to the expanded capabilities and systems of care present at these centers. By identifying these lifesaving elements that are cultivated in complex centers, and making them available in lower-complexity hospitals, we can ensure that all surgical procedures take place in facilities with the appropriate systems to support them," she said.
Dr. McCrum had no financial conflicts to disclose.
CHICAGO – Surgical patients receiving care at the least complex hospitals had a 50% increased risk of death compared with those treated at more complex hospitals, based on data from more than 400,000 patients.
Data from previous research suggest that the characteristics of individual hospitals predict surgical outcomes, but the relationship between hospital complexity and surgical mortality has not been well studied, Dr. Marta McCrum said at the annual clinical congress of the American College of Surgeons.
She and her colleagues reviewed Medicare administrative claims data from 2008-2009 and information on hospital characteristics from the American Hospital Association Survey 2009 on 2,695 hospitals. The hospitals were divided into quintiles based on complexity, which for purposes of this study was defined as the number of unique diagnoses and procedures performed at each facility.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals."
"Hospitals that see a wide variety of conditions (common problems but also very rare or complicated diagnoses) would be equipped with the wide range of services and resources needed to support them – that is, they would be complex. Similarly, hospitals that perform the widest range of unique procedures would also have the greatest diversity of services and technology," Dr. McCrum of Harvard University, Boston, explained in an interview.
"We therefore ranked the hospitals separately based on the number of unique diagnoses and procedures they saw, and then summed the ranks to assign a numeric value to the complexity of that hospital in comparison to the others. For the analysis, we separated the hospitals into quintiles based on this value."
Not surprisingly, low-complexity hospitals tended to be smaller, more rural, and located in lower-income areas, and the more complex hospitals tended to be larger, urban, and in higher-income areas, she said.
"Of note, the surgical mortality rate of the highest-complexity hospitals was 7.3%, versus 12.6% at the lowest-complexity hospitals," for an absolute risk reduction of 5.3%, she said.
The researchers controlled for hospital and population characteristics, including total number of hospital discharges, public/private ownership, percentage of Medicare patients, urban location, and county income. Hospital complexity remained a significant predictor of mortality between each quintile compared with the highest-complexity quintile.
"The average aggregate mortality rate at the lowest-complexity hospitals is 46% higher than that of the highest-complexity hospitals," said Dr. McCrum.
Overall, the research model explained 28% of the variability in mortality rates, and within the model, hospital complexity explained the greatest proportion of variability in mortality rates. Although hospital volume was a statistically significant predictor of mortality, the effect was small, she noted.
The study was limited by the fact that approximately two-thirds of the variability remained unexplained, likely due to a combination of patient factors and hospital factors, she said. Additional limitations included the lack of an existing metric to measure hospital complexity, and the limitations of using administrative claims data.
"Our research suggests that outcomes for certain surgical procedures are better at more complex hospitals," Dr. McCrum said in an interview. "This might be due in part to the expanded capabilities and systems of care present at these centers. By identifying these lifesaving elements that are cultivated in complex centers, and making them available in lower-complexity hospitals, we can ensure that all surgical procedures take place in facilities with the appropriate systems to support them," she said.
Dr. McCrum had no financial conflicts to disclose.
FROM THE ANNUAL CLINICAL CONGRESS OF THE AMERICAN COLLEGE OF SURGEONS
Major Finding: Hospitals in the highest quintile of complexity were associated with a 5% absolute risk reduction in surgical mortality rates compared with hospitals in the lowest quintile of complexity.
Data Source: The data come from a review of Medicare administrative claims data from 2008-2009 and information from the American Hospital Association Survey 2009 on 2,695 U.S. hospitals.
Disclosures: Dr. McCrum had no financial conflicts to disclose.
Sternal SSIs, Mediastinitis Plummet Under Preop Decolonization Program
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
AT IDWEEK 2012
Major Finding: Following initiation of a preoperative S. aureus decolonization program, the rate of postoperative sternal SSIs following coronary artery bypass grafting dropped by 65%, and the rate of mediastinitis cases dropped by 75%.
Data Source: A single-center study of 580 cardiothoracic surgery patients who were screened from April 2010 through March 2012.
Disclosures: The researchers reported having no relevant financial conflicts.
Early Oral Feeding Benefits Bowel Surgery Patients
CHICAGO – A total of 80% of bowel resection patients tolerated early fluids one day after surgery, based on data from 100 patients.
"Early oral feeding is an important part of fast-track surgery, which enhances recovery after surgery," but feeding in patients undergoing emergency bowel resection is often delayed until the resolution of ileus, Dr. Mohamed E. Shams of Suez Canal University in Ismailia, Egypt, said at the annual clinical congress of the American College of Surgeons.
Dr. Shams and colleagues randomized 100 adults who underwent small or large bowel resection into two groups. The early group comprised 50 patients who received fluid oral feedings on the first day after surgery. The late group comprised 50 patients who received oral feedings after the resolution of ileus.
Overall, 80% of patients in the early group tolerated the early oral feeding. In addition, patients in the early group averaged a significantly shorter time than did the late group to the passage of flatus (3.2 days vs. 0.8 days, respectively), and stool (4.4 days vs. 1.2 days, respectively).
Postoperative monitoring showed that the chest infections occurred in four patients in the early feeding group compared with 10 patients in the late feeding group, while wound infections occurred in 12 patients in the early group and 15 patients in the late group, Dr. Shams said. No incidents of a burst abdomen occurred in the early group, and three incidents occurred in the late group.
"Early oral feeding after emergency intestinal surgery is safe and well tolerated by the majority of patients, without an increase in mortality and morbidity risk," said Dr. Shams. "It also has a positive impact on reduction in hospital stay," he said.
The findings were limited by the small number of patients, but the results suggest that a majority of patients undergoing emergency intestinal surgery can benefit from early feeding, Dr. Shams noted.
Dr. Shams had no financial conflicts to disclose.
CHICAGO – A total of 80% of bowel resection patients tolerated early fluids one day after surgery, based on data from 100 patients.
"Early oral feeding is an important part of fast-track surgery, which enhances recovery after surgery," but feeding in patients undergoing emergency bowel resection is often delayed until the resolution of ileus, Dr. Mohamed E. Shams of Suez Canal University in Ismailia, Egypt, said at the annual clinical congress of the American College of Surgeons.
Dr. Shams and colleagues randomized 100 adults who underwent small or large bowel resection into two groups. The early group comprised 50 patients who received fluid oral feedings on the first day after surgery. The late group comprised 50 patients who received oral feedings after the resolution of ileus.
Overall, 80% of patients in the early group tolerated the early oral feeding. In addition, patients in the early group averaged a significantly shorter time than did the late group to the passage of flatus (3.2 days vs. 0.8 days, respectively), and stool (4.4 days vs. 1.2 days, respectively).
Postoperative monitoring showed that the chest infections occurred in four patients in the early feeding group compared with 10 patients in the late feeding group, while wound infections occurred in 12 patients in the early group and 15 patients in the late group, Dr. Shams said. No incidents of a burst abdomen occurred in the early group, and three incidents occurred in the late group.
"Early oral feeding after emergency intestinal surgery is safe and well tolerated by the majority of patients, without an increase in mortality and morbidity risk," said Dr. Shams. "It also has a positive impact on reduction in hospital stay," he said.
The findings were limited by the small number of patients, but the results suggest that a majority of patients undergoing emergency intestinal surgery can benefit from early feeding, Dr. Shams noted.
Dr. Shams had no financial conflicts to disclose.
CHICAGO – A total of 80% of bowel resection patients tolerated early fluids one day after surgery, based on data from 100 patients.
"Early oral feeding is an important part of fast-track surgery, which enhances recovery after surgery," but feeding in patients undergoing emergency bowel resection is often delayed until the resolution of ileus, Dr. Mohamed E. Shams of Suez Canal University in Ismailia, Egypt, said at the annual clinical congress of the American College of Surgeons.
Dr. Shams and colleagues randomized 100 adults who underwent small or large bowel resection into two groups. The early group comprised 50 patients who received fluid oral feedings on the first day after surgery. The late group comprised 50 patients who received oral feedings after the resolution of ileus.
Overall, 80% of patients in the early group tolerated the early oral feeding. In addition, patients in the early group averaged a significantly shorter time than did the late group to the passage of flatus (3.2 days vs. 0.8 days, respectively), and stool (4.4 days vs. 1.2 days, respectively).
Postoperative monitoring showed that the chest infections occurred in four patients in the early feeding group compared with 10 patients in the late feeding group, while wound infections occurred in 12 patients in the early group and 15 patients in the late group, Dr. Shams said. No incidents of a burst abdomen occurred in the early group, and three incidents occurred in the late group.
"Early oral feeding after emergency intestinal surgery is safe and well tolerated by the majority of patients, without an increase in mortality and morbidity risk," said Dr. Shams. "It also has a positive impact on reduction in hospital stay," he said.
The findings were limited by the small number of patients, but the results suggest that a majority of patients undergoing emergency intestinal surgery can benefit from early feeding, Dr. Shams noted.
Dr. Shams had no financial conflicts to disclose.
FROM THE ANNUAL CLINICAL CONGRESS OF THE AMERICAN COLLEGE OF SURGEONS
Major Finding: Eighty percent of patients who received oral fluids on the first day after surgery vs. delayed feeding had significantly shorter time to the passage of flatus (3.2 days vs. 0.8 days, respectively), and stool (4.4 days vs. 1.2 days, respectively).
Data Source: The data come from a randomized trial of 100 adults who underwent bowel resection.
Disclosures: Dr. Shams reported having no financial conflicts.
Blood Cultures Can Miss Invasive Candidiasis
SAN FRANCISCO – Every patient should get antifungal therapy following surgical treatment of intra-abdominal candidiasis, according to researchers at the University of Pittsburgh.
Not all do; 38% of 199 patients there (76) who had surgical drainage received no antifungals, at least initially; infections persisted in half (38) and 20% (15) died.
"Clinicians could not reliably identify patients who were cured with surgical drainage alone, showing that all patients require antifungal therapy in addition to drainage. A lot of people don’t get treatment, and it’s a problem," said lead investigator Dr. M. Hong Nguyen, director of both the transplant infectious diseases and the antimicrobial management programs at the university.
An overreliance on blood cultures to screen for invasive candidiasis – either before or after surgery – could be to blame; blood cultures aren’t that good at picking it up, she said at the meeting, which was sponsored by the American Society for Microbiology
Even so, they are the go-to screening option in many places because blood stream infections (candidemia) are thought to be the most common manifestations of invasive candidiasis.
That wasn’t true in Pittsburgh. Among the 199 invasive candidiasis patients Dr. Nguyen and her team investigated, intra-abdominal candidiasis (IAC) – mostly abscesses and peritonitis without candidemia – accounted for 53% (105) of cases, and candidemia just 28% (56). Intra-abdominal candidiasis "is much more of a problem than candidemia," Dr. Nguyen said.
Other cases were a blend of both, or infections at another site. Candida albicans was the most implicated organism.
Dr. Nguyen and her colleagues concluded that blood cultures aren’t the right screening tool for invasive candidiasis because they can be negative even when patients have serious disease. "We need some kind of blood diagnostic to help us," she said.
They’ve found that Candida polymerase chain reaction and Fungitell 1,3-Beta-D-glucan (BDG) blood tests seem to be better options, especially helpful when used with blood cultures (Clin. Infect. Dis. 2012;54:1240-8).
The team also concluded that "IAC is more common than recognized ... more common than candidemia, [and] associated with significant morbidity and mortality," she said.
Dr. Nguyen reported having no disclosures.
SAN FRANCISCO – Every patient should get antifungal therapy following surgical treatment of intra-abdominal candidiasis, according to researchers at the University of Pittsburgh.
Not all do; 38% of 199 patients there (76) who had surgical drainage received no antifungals, at least initially; infections persisted in half (38) and 20% (15) died.
"Clinicians could not reliably identify patients who were cured with surgical drainage alone, showing that all patients require antifungal therapy in addition to drainage. A lot of people don’t get treatment, and it’s a problem," said lead investigator Dr. M. Hong Nguyen, director of both the transplant infectious diseases and the antimicrobial management programs at the university.
An overreliance on blood cultures to screen for invasive candidiasis – either before or after surgery – could be to blame; blood cultures aren’t that good at picking it up, she said at the meeting, which was sponsored by the American Society for Microbiology
Even so, they are the go-to screening option in many places because blood stream infections (candidemia) are thought to be the most common manifestations of invasive candidiasis.
That wasn’t true in Pittsburgh. Among the 199 invasive candidiasis patients Dr. Nguyen and her team investigated, intra-abdominal candidiasis (IAC) – mostly abscesses and peritonitis without candidemia – accounted for 53% (105) of cases, and candidemia just 28% (56). Intra-abdominal candidiasis "is much more of a problem than candidemia," Dr. Nguyen said.
Other cases were a blend of both, or infections at another site. Candida albicans was the most implicated organism.
Dr. Nguyen and her colleagues concluded that blood cultures aren’t the right screening tool for invasive candidiasis because they can be negative even when patients have serious disease. "We need some kind of blood diagnostic to help us," she said.
They’ve found that Candida polymerase chain reaction and Fungitell 1,3-Beta-D-glucan (BDG) blood tests seem to be better options, especially helpful when used with blood cultures (Clin. Infect. Dis. 2012;54:1240-8).
The team also concluded that "IAC is more common than recognized ... more common than candidemia, [and] associated with significant morbidity and mortality," she said.
Dr. Nguyen reported having no disclosures.
SAN FRANCISCO – Every patient should get antifungal therapy following surgical treatment of intra-abdominal candidiasis, according to researchers at the University of Pittsburgh.
Not all do; 38% of 199 patients there (76) who had surgical drainage received no antifungals, at least initially; infections persisted in half (38) and 20% (15) died.
"Clinicians could not reliably identify patients who were cured with surgical drainage alone, showing that all patients require antifungal therapy in addition to drainage. A lot of people don’t get treatment, and it’s a problem," said lead investigator Dr. M. Hong Nguyen, director of both the transplant infectious diseases and the antimicrobial management programs at the university.
An overreliance on blood cultures to screen for invasive candidiasis – either before or after surgery – could be to blame; blood cultures aren’t that good at picking it up, she said at the meeting, which was sponsored by the American Society for Microbiology
Even so, they are the go-to screening option in many places because blood stream infections (candidemia) are thought to be the most common manifestations of invasive candidiasis.
That wasn’t true in Pittsburgh. Among the 199 invasive candidiasis patients Dr. Nguyen and her team investigated, intra-abdominal candidiasis (IAC) – mostly abscesses and peritonitis without candidemia – accounted for 53% (105) of cases, and candidemia just 28% (56). Intra-abdominal candidiasis "is much more of a problem than candidemia," Dr. Nguyen said.
Other cases were a blend of both, or infections at another site. Candida albicans was the most implicated organism.
Dr. Nguyen and her colleagues concluded that blood cultures aren’t the right screening tool for invasive candidiasis because they can be negative even when patients have serious disease. "We need some kind of blood diagnostic to help us," she said.
They’ve found that Candida polymerase chain reaction and Fungitell 1,3-Beta-D-glucan (BDG) blood tests seem to be better options, especially helpful when used with blood cultures (Clin. Infect. Dis. 2012;54:1240-8).
The team also concluded that "IAC is more common than recognized ... more common than candidemia, [and] associated with significant morbidity and mortality," she said.
Dr. Nguyen reported having no disclosures.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Based on blood culture results, 38% of patients who had surgical drainage received no antifungals, at least initially; infections persisted in half, and 20% died.
Data Source: Observational study of 199 patients with invasive candidiasis.
Disclosures: The investigator reported having no relevant disclosures.
Male Gender, Length of Stay Raise Readmission Risk
CHICAGO – Approximately half of hospital readmissions are surgery related and one-third of these are due to infections, data from nearly 3,000 Medicare patients indicated.
Risk factors for readmission included male gender, higher ASA (American Society of Anesthesiologists) class, and longer hospital stay, Dr. Shanu N. Kothari said at the annual clinical congress of the American College of Surgeons.
Recent health care reform initiatives include a proposal to reduce reimbursement for certain 30-day hospital readmissions among Medicare patients, he noted.
Dr. Kothari of Gundersen Lutheran Health System in La Crosse, Wis., and his colleagues reviewed data from 2,865 Medicare patients who had surgery at their institution between Jan. 1, 2010, and May 16, 2011. A readmission was defined as any patient who was readmitted within 30 days of initial surgery. Patients with incomplete follow-up data and those who died within 30 days were excluded.
The overall 30-day readmission rate was 7%. Readmitted patients were significantly more likely to be male compared with nonreadmitted patients (54% vs. 44%) and significantly more likely to have an ASA class of 3 or greater (84% vs. 66%). There were no significant differences in age or body mass index between readmitted and nonreadmitted patients.
In addition, the average length of stay and operative times were significantly longer for readmitted patients vs. nonreadmitted patients (4.8 days vs. 2.8 days and 123 minutes vs. 98 minutes).
A majority of the procedures were general and orthopedic, and 77% were elective.
Of the readmitted patients, "84% had at least one chronic condition, and patients with cardiac disease, renal disease, and diabetes had higher readmission rates," Dr. Kothari said.
The reasons for readmission were divided into four categories: surgery related (53%), not related to the surgical procedure (35%), planned (7%), and patient related (5%).
The most common surgery-related reasons for readmission were infections (32%), medication side effects (12%), or pulmonary complications (9%), Dr. Kothari noted.
Most of the readmissions unrelated to the index surgical procedure were exacerbations of underlying conditions, such as renal failure or heart failure. Patient-related reasons for readmission included noncompliance with discharge instructions or medications, as well as psychological issues.
"Further study is needed to address reasons for readmission on a multicenter level," said Dr. Kothari. "Decreased reimbursement should be discouraged for readmissions directly related to patient noncompliance."
Dr. Kothari said he had no relevant financial disclosures.
CHICAGO – Approximately half of hospital readmissions are surgery related and one-third of these are due to infections, data from nearly 3,000 Medicare patients indicated.
Risk factors for readmission included male gender, higher ASA (American Society of Anesthesiologists) class, and longer hospital stay, Dr. Shanu N. Kothari said at the annual clinical congress of the American College of Surgeons.
Recent health care reform initiatives include a proposal to reduce reimbursement for certain 30-day hospital readmissions among Medicare patients, he noted.
Dr. Kothari of Gundersen Lutheran Health System in La Crosse, Wis., and his colleagues reviewed data from 2,865 Medicare patients who had surgery at their institution between Jan. 1, 2010, and May 16, 2011. A readmission was defined as any patient who was readmitted within 30 days of initial surgery. Patients with incomplete follow-up data and those who died within 30 days were excluded.
The overall 30-day readmission rate was 7%. Readmitted patients were significantly more likely to be male compared with nonreadmitted patients (54% vs. 44%) and significantly more likely to have an ASA class of 3 or greater (84% vs. 66%). There were no significant differences in age or body mass index between readmitted and nonreadmitted patients.
In addition, the average length of stay and operative times were significantly longer for readmitted patients vs. nonreadmitted patients (4.8 days vs. 2.8 days and 123 minutes vs. 98 minutes).
A majority of the procedures were general and orthopedic, and 77% were elective.
Of the readmitted patients, "84% had at least one chronic condition, and patients with cardiac disease, renal disease, and diabetes had higher readmission rates," Dr. Kothari said.
The reasons for readmission were divided into four categories: surgery related (53%), not related to the surgical procedure (35%), planned (7%), and patient related (5%).
The most common surgery-related reasons for readmission were infections (32%), medication side effects (12%), or pulmonary complications (9%), Dr. Kothari noted.
Most of the readmissions unrelated to the index surgical procedure were exacerbations of underlying conditions, such as renal failure or heart failure. Patient-related reasons for readmission included noncompliance with discharge instructions or medications, as well as psychological issues.
"Further study is needed to address reasons for readmission on a multicenter level," said Dr. Kothari. "Decreased reimbursement should be discouraged for readmissions directly related to patient noncompliance."
Dr. Kothari said he had no relevant financial disclosures.
CHICAGO – Approximately half of hospital readmissions are surgery related and one-third of these are due to infections, data from nearly 3,000 Medicare patients indicated.
Risk factors for readmission included male gender, higher ASA (American Society of Anesthesiologists) class, and longer hospital stay, Dr. Shanu N. Kothari said at the annual clinical congress of the American College of Surgeons.
Recent health care reform initiatives include a proposal to reduce reimbursement for certain 30-day hospital readmissions among Medicare patients, he noted.
Dr. Kothari of Gundersen Lutheran Health System in La Crosse, Wis., and his colleagues reviewed data from 2,865 Medicare patients who had surgery at their institution between Jan. 1, 2010, and May 16, 2011. A readmission was defined as any patient who was readmitted within 30 days of initial surgery. Patients with incomplete follow-up data and those who died within 30 days were excluded.
The overall 30-day readmission rate was 7%. Readmitted patients were significantly more likely to be male compared with nonreadmitted patients (54% vs. 44%) and significantly more likely to have an ASA class of 3 or greater (84% vs. 66%). There were no significant differences in age or body mass index between readmitted and nonreadmitted patients.
In addition, the average length of stay and operative times were significantly longer for readmitted patients vs. nonreadmitted patients (4.8 days vs. 2.8 days and 123 minutes vs. 98 minutes).
A majority of the procedures were general and orthopedic, and 77% were elective.
Of the readmitted patients, "84% had at least one chronic condition, and patients with cardiac disease, renal disease, and diabetes had higher readmission rates," Dr. Kothari said.
The reasons for readmission were divided into four categories: surgery related (53%), not related to the surgical procedure (35%), planned (7%), and patient related (5%).
The most common surgery-related reasons for readmission were infections (32%), medication side effects (12%), or pulmonary complications (9%), Dr. Kothari noted.
Most of the readmissions unrelated to the index surgical procedure were exacerbations of underlying conditions, such as renal failure or heart failure. Patient-related reasons for readmission included noncompliance with discharge instructions or medications, as well as psychological issues.
"Further study is needed to address reasons for readmission on a multicenter level," said Dr. Kothari. "Decreased reimbursement should be discouraged for readmissions directly related to patient noncompliance."
Dr. Kothari said he had no relevant financial disclosures.
AT THE ANNUAL CLINICAL CONGRESS OF THE AMERICAN COLLEGE OF SURGEONS
Major Finding: A total of 53% of 30-day readmissions at a single institution were surgically related, and 32% of these were due to infections.
Data Source: The data come from a retrospective study of 2,865 Medicare patients who underwent surgery at a single institution between Jan. 1, 2010, and May 16, 2011.
Disclosures: Dr. Kothari said he had no relevant financial disclosures.