User login
FDA Warns of Seizure Risk With Cefepime
The Food and Drug Administration has reported cases of a specific type of seizure called nonconvulsive status epilepticus that is associated with the use of the antibacterial drug cefepime in patients with renal impairment.
The seizures have been seen primarily in patients with renal impairment who did not receive appropriate dosage adjustments of cefepime, although in several cases patients received "dosage adjustment appropriate for their degree of renal impairment," according to the agency. The FDA is working to revise the "Warnings and Precautions" and "Adverse Reactions" sections of the cefepime label to highlight this risk.
The FDA advises health care professionals to adjust the dosage of cefepime in patients with a creatinine clearance of 60 mL/min or less in order to minimize the risk of seizures. If seizures associated with cefepime therapy occur, physicians should consider discontinuing cefepime or making appropriate dosage adjustments in patients with renal impairment.
Nonconvulsive status epilepticus associated with cefepime occurred in 59 patients from 1996 through February 2012. The cases were identified through the FDA’s Adverse Event Reporting System (AERS) database. The majority of seizures were reversible, and resolved after discontinuation of cefepime and/or after hemodialysis.
Cefepime is a cephalosporin antibacterial drug used to treat pneumonia, urinary tract, skin, and intra-abdominal infections.
*This article was updated on 7/3/2012*
The Food and Drug Administration has reported cases of a specific type of seizure called nonconvulsive status epilepticus that is associated with the use of the antibacterial drug cefepime in patients with renal impairment.
The seizures have been seen primarily in patients with renal impairment who did not receive appropriate dosage adjustments of cefepime, although in several cases patients received "dosage adjustment appropriate for their degree of renal impairment," according to the agency. The FDA is working to revise the "Warnings and Precautions" and "Adverse Reactions" sections of the cefepime label to highlight this risk.
The FDA advises health care professionals to adjust the dosage of cefepime in patients with a creatinine clearance of 60 mL/min or less in order to minimize the risk of seizures. If seizures associated with cefepime therapy occur, physicians should consider discontinuing cefepime or making appropriate dosage adjustments in patients with renal impairment.
Nonconvulsive status epilepticus associated with cefepime occurred in 59 patients from 1996 through February 2012. The cases were identified through the FDA’s Adverse Event Reporting System (AERS) database. The majority of seizures were reversible, and resolved after discontinuation of cefepime and/or after hemodialysis.
Cefepime is a cephalosporin antibacterial drug used to treat pneumonia, urinary tract, skin, and intra-abdominal infections.
*This article was updated on 7/3/2012*
The Food and Drug Administration has reported cases of a specific type of seizure called nonconvulsive status epilepticus that is associated with the use of the antibacterial drug cefepime in patients with renal impairment.
The seizures have been seen primarily in patients with renal impairment who did not receive appropriate dosage adjustments of cefepime, although in several cases patients received "dosage adjustment appropriate for their degree of renal impairment," according to the agency. The FDA is working to revise the "Warnings and Precautions" and "Adverse Reactions" sections of the cefepime label to highlight this risk.
The FDA advises health care professionals to adjust the dosage of cefepime in patients with a creatinine clearance of 60 mL/min or less in order to minimize the risk of seizures. If seizures associated with cefepime therapy occur, physicians should consider discontinuing cefepime or making appropriate dosage adjustments in patients with renal impairment.
Nonconvulsive status epilepticus associated with cefepime occurred in 59 patients from 1996 through February 2012. The cases were identified through the FDA’s Adverse Event Reporting System (AERS) database. The majority of seizures were reversible, and resolved after discontinuation of cefepime and/or after hemodialysis.
Cefepime is a cephalosporin antibacterial drug used to treat pneumonia, urinary tract, skin, and intra-abdominal infections.
*This article was updated on 7/3/2012*
Tool Boosts Power to Predict Delirium in Adult ICU
A recently developed tool could help doctors stay ahead of the game in preventing delirium in intensive care patients.
Dutch researchers say their delirium prediction model, known as PRE-DELIRIC, was significantly more successful than doctors and nurses at predicting delirium in hospitalized adults.
Preventive measures for delirium can limit its incidence, severity, and duration. While several assessment tools exist for other segments of hospitalized patients, "no evidence-based prediction model for general intensive care patients is available," Mark van den Boogaard, Ph.D., of Radboud University Nijmegen (Netherlands) Medical Centre and his colleagues said (BMJ 2012;344:e420 [doi: 10.1136/bmj.e420]).
General preventive measures in all ICU patients are time consuming, and may expose many patients to unnecessary risks such as adverse events related to drug prophylaxis, the researchers explained.
For PRE-DELIRIC (Prediction of Delirium in ICU Patients), Dr. van den Boogaard and his colleagues defined 10 risk factors that can be easily assessed within 24 hours of admission to the ICU: age, APACHE II (Acute Physiology and Chronic Health Evaluation II) score, admission category, coma, infection, metabolic acidosis, morphine use, sedative use, urea concentration, and urgent admission.
"The use of the PRE-DELERIC model to identify and consequently preventively treat high-risk patients could offer an important contribution to intensive care practice and ensure efficient use of research resources to study only high-risk patients," the researchers said.
Clinically, the model may improve the use of nondrug measures to prevent delirium in high-risk patients, the researchers added. Such measures include improvement of orientation, cognitive stimulation, early mobilization, and listening to music, they said.
In noncritical patients, nondrug preventive measures have been shown to reduce delirium incidence and duration, and haloperidol treatment has lessened severity, duration, and associated length of stay. But for ICU patients, data are hard to come by. PRE-DELIRIC could inform the choice to use prophylactic haloperidol in these patients, the authors said. Existing research (Lancet 2009;373:1874-82) does show that "early mobilisation of mechanically ventilated patients in intensive care, besides other significant effects, resulted in a reduced duration of delirium," Dr. van den Boogaard and his coauthors wrote.
After testing their model for temporal validation, the researchers conducted an external validation study of data from intensive care patients admitted to four Dutch hospitals between Jan. 1 and Sept. 1, 2009. The pooled data included information from 3,056 patients aged 18 years and older, yielding an area under the receiver operating characteristics curve (AUROC) of 0.85. The patients were divided into four risk groups: low, moderate, high, and very high. The sensitivity and specificity were, respectively, 81% and 75% for the group with low-risk group; 62% and 89% for the moderate-risk group; 46% and 95% for the high-risk group; and 30% and 98% for the group with very high risk.
The researchers compared the predictions of patient delirium made by their model to predictions made by doctors and nurses in the hospital, using a convenience sample of 124 patients.
The AUROC for the PRE-DELIRIC model (0.87) was significantly higher than that of the doctors and nurses (0.59).
No significant differences appeared in the predictions of intensive care nurses compared with student intensive care nurses or among intensivists, fellow-intensivists, and residents, the researchers said.
The PRE-DELIRIC model is being used in daily practice in the hospital where the model was developed, the researchers said. "Intensive care patients with a high risk of delirium (at least a 50% PRE-DELIRIC score), and patients with dementia or alcohol misuse, receive preventive measures. The optimal cut-off point of the PRE-DELIRIC model and the most effective delirium preventive interventions for intensive care patients need to be studied in the near future."
The findings were limited by the static nature of the model, which does not account for changes in health status that might affect the odds of developing delirium, the researchers noted.
The researchers reported having no financial conflicts of interest.
haloperidol treatment,
A recently developed tool could help doctors stay ahead of the game in preventing delirium in intensive care patients.
Dutch researchers say their delirium prediction model, known as PRE-DELIRIC, was significantly more successful than doctors and nurses at predicting delirium in hospitalized adults.
Preventive measures for delirium can limit its incidence, severity, and duration. While several assessment tools exist for other segments of hospitalized patients, "no evidence-based prediction model for general intensive care patients is available," Mark van den Boogaard, Ph.D., of Radboud University Nijmegen (Netherlands) Medical Centre and his colleagues said (BMJ 2012;344:e420 [doi: 10.1136/bmj.e420]).
General preventive measures in all ICU patients are time consuming, and may expose many patients to unnecessary risks such as adverse events related to drug prophylaxis, the researchers explained.
For PRE-DELIRIC (Prediction of Delirium in ICU Patients), Dr. van den Boogaard and his colleagues defined 10 risk factors that can be easily assessed within 24 hours of admission to the ICU: age, APACHE II (Acute Physiology and Chronic Health Evaluation II) score, admission category, coma, infection, metabolic acidosis, morphine use, sedative use, urea concentration, and urgent admission.
"The use of the PRE-DELERIC model to identify and consequently preventively treat high-risk patients could offer an important contribution to intensive care practice and ensure efficient use of research resources to study only high-risk patients," the researchers said.
Clinically, the model may improve the use of nondrug measures to prevent delirium in high-risk patients, the researchers added. Such measures include improvement of orientation, cognitive stimulation, early mobilization, and listening to music, they said.
In noncritical patients, nondrug preventive measures have been shown to reduce delirium incidence and duration, and haloperidol treatment has lessened severity, duration, and associated length of stay. But for ICU patients, data are hard to come by. PRE-DELIRIC could inform the choice to use prophylactic haloperidol in these patients, the authors said. Existing research (Lancet 2009;373:1874-82) does show that "early mobilisation of mechanically ventilated patients in intensive care, besides other significant effects, resulted in a reduced duration of delirium," Dr. van den Boogaard and his coauthors wrote.
After testing their model for temporal validation, the researchers conducted an external validation study of data from intensive care patients admitted to four Dutch hospitals between Jan. 1 and Sept. 1, 2009. The pooled data included information from 3,056 patients aged 18 years and older, yielding an area under the receiver operating characteristics curve (AUROC) of 0.85. The patients were divided into four risk groups: low, moderate, high, and very high. The sensitivity and specificity were, respectively, 81% and 75% for the group with low-risk group; 62% and 89% for the moderate-risk group; 46% and 95% for the high-risk group; and 30% and 98% for the group with very high risk.
The researchers compared the predictions of patient delirium made by their model to predictions made by doctors and nurses in the hospital, using a convenience sample of 124 patients.
The AUROC for the PRE-DELIRIC model (0.87) was significantly higher than that of the doctors and nurses (0.59).
No significant differences appeared in the predictions of intensive care nurses compared with student intensive care nurses or among intensivists, fellow-intensivists, and residents, the researchers said.
The PRE-DELIRIC model is being used in daily practice in the hospital where the model was developed, the researchers said. "Intensive care patients with a high risk of delirium (at least a 50% PRE-DELIRIC score), and patients with dementia or alcohol misuse, receive preventive measures. The optimal cut-off point of the PRE-DELIRIC model and the most effective delirium preventive interventions for intensive care patients need to be studied in the near future."
The findings were limited by the static nature of the model, which does not account for changes in health status that might affect the odds of developing delirium, the researchers noted.
The researchers reported having no financial conflicts of interest.
A recently developed tool could help doctors stay ahead of the game in preventing delirium in intensive care patients.
Dutch researchers say their delirium prediction model, known as PRE-DELIRIC, was significantly more successful than doctors and nurses at predicting delirium in hospitalized adults.
Preventive measures for delirium can limit its incidence, severity, and duration. While several assessment tools exist for other segments of hospitalized patients, "no evidence-based prediction model for general intensive care patients is available," Mark van den Boogaard, Ph.D., of Radboud University Nijmegen (Netherlands) Medical Centre and his colleagues said (BMJ 2012;344:e420 [doi: 10.1136/bmj.e420]).
General preventive measures in all ICU patients are time consuming, and may expose many patients to unnecessary risks such as adverse events related to drug prophylaxis, the researchers explained.
For PRE-DELIRIC (Prediction of Delirium in ICU Patients), Dr. van den Boogaard and his colleagues defined 10 risk factors that can be easily assessed within 24 hours of admission to the ICU: age, APACHE II (Acute Physiology and Chronic Health Evaluation II) score, admission category, coma, infection, metabolic acidosis, morphine use, sedative use, urea concentration, and urgent admission.
"The use of the PRE-DELERIC model to identify and consequently preventively treat high-risk patients could offer an important contribution to intensive care practice and ensure efficient use of research resources to study only high-risk patients," the researchers said.
Clinically, the model may improve the use of nondrug measures to prevent delirium in high-risk patients, the researchers added. Such measures include improvement of orientation, cognitive stimulation, early mobilization, and listening to music, they said.
In noncritical patients, nondrug preventive measures have been shown to reduce delirium incidence and duration, and haloperidol treatment has lessened severity, duration, and associated length of stay. But for ICU patients, data are hard to come by. PRE-DELIRIC could inform the choice to use prophylactic haloperidol in these patients, the authors said. Existing research (Lancet 2009;373:1874-82) does show that "early mobilisation of mechanically ventilated patients in intensive care, besides other significant effects, resulted in a reduced duration of delirium," Dr. van den Boogaard and his coauthors wrote.
After testing their model for temporal validation, the researchers conducted an external validation study of data from intensive care patients admitted to four Dutch hospitals between Jan. 1 and Sept. 1, 2009. The pooled data included information from 3,056 patients aged 18 years and older, yielding an area under the receiver operating characteristics curve (AUROC) of 0.85. The patients were divided into four risk groups: low, moderate, high, and very high. The sensitivity and specificity were, respectively, 81% and 75% for the group with low-risk group; 62% and 89% for the moderate-risk group; 46% and 95% for the high-risk group; and 30% and 98% for the group with very high risk.
The researchers compared the predictions of patient delirium made by their model to predictions made by doctors and nurses in the hospital, using a convenience sample of 124 patients.
The AUROC for the PRE-DELIRIC model (0.87) was significantly higher than that of the doctors and nurses (0.59).
No significant differences appeared in the predictions of intensive care nurses compared with student intensive care nurses or among intensivists, fellow-intensivists, and residents, the researchers said.
The PRE-DELIRIC model is being used in daily practice in the hospital where the model was developed, the researchers said. "Intensive care patients with a high risk of delirium (at least a 50% PRE-DELIRIC score), and patients with dementia or alcohol misuse, receive preventive measures. The optimal cut-off point of the PRE-DELIRIC model and the most effective delirium preventive interventions for intensive care patients need to be studied in the near future."
The findings were limited by the static nature of the model, which does not account for changes in health status that might affect the odds of developing delirium, the researchers noted.
The researchers reported having no financial conflicts of interest.
haloperidol treatment,
haloperidol treatment,
FROM THE BRITISH MEDICAL JOURNAL
Some Antidepressants Increased Risk of Death in ICU
SAN FRANCISCO – Patients on selective serotonin reuptake inhibitors or serotonin norepinephrine reuptake inhibitors when they were admitted to an intensive care unit were 73% more likely to die in the hospital, compared with ICU patients who were not on these antidepressants, a retrospective study found.
Dr. Katherine M. Berg and her associates analyzed electronic records from admissions to four ICUs in 2001-2008 to compare outcomes for 1,876 patients who were on a selective serotonin reuptake inhibitor (SSRI) or serotonin norepinephrine reuptake inhibitor (SNRI) and 8,692 control patients who were not taking an SSRI or SNRI before admission.
The mortality risk remained elevated at 1,000 days after ICU admission, she reported in a late-breaking poster presentation and discussion session at an international conference of the American Thoracic Society.
Certain subgroups were at even greater risk of dying in the hospital if they were on an SSRI or SNRI when admitted to the ICU. Patients who had acute coronary syndrome or had undergone cardiac surgery were more than twice as likely to die if they were on an SSRI/SNRI when entering the ICU, compared with controls, said Dr. Berg, a pulmonary/critical care fellow at Massachusetts General Hospital and Harvard University, Boston.
The increased mortality risk appeared to be associated mainly with medications that have higher degrees of serotonin reuptake inhibition. "Citalopram, which is a lower-potency drug, by itself did not incur a higher mortality risk, but sertraline, which is one of the more potent drugs, did. Even comparing the two drugs to each other, if you were on sertraline, your mortality risk was higher" than if you were on citalopram, Dr. Berg said in an interview.
Fluoxetine, paroxetine, and sertraline were associated with significantly higher mortality, but no significant mortality differences were seen between patients on citalopram or escitalopram and control patients.
Of the 8,692 control patients, 7% died in the hospital, compared with in-hospital death rates of 10% in 286 patients on fluoxetine, 13% in 320 patients on paroxetine, and 15% in 426 patients on sertraline at the time of ICU admission. The remaining 844 patients were on other antidepressants.
The study adjusted for the effects of each patient’s age, Simplified Acute Physiology Score, and combined Elixhauser comorbidity score on in-hospital mortality risk.
Slight but statistically significant differences in the characteristics of the two groups included a greater proportion of women in the SSRI/SNRI group, compared with controls (57% vs. 40%), and a higher prevalence of diabetes (21% vs. 17%) or chronic obstructive pulmonary disease (11% vs. 7%) in patients on an SSRI/SNRI, compared with controls. Patients in the SSRI/SNRI group were more likely to have an infection than were controls (11% vs. 8%), but less likely to have acute coronary syndrome (8% vs. 10%) or cardiovascular disease (67% vs. 70%).
Further studies are needed to ascertain if this is a causal relationship or just an association between SSRI/SNRI use and mortality in ICU patients, she said. The findings are limited by the retrospective nature of the study, which also was unable to control for the effects of potentially important confounders such as smoking status or the presence of depression.
The data came from the Multiparameter Intelligent Monitoring in Intensive Care II database, a public collection of data with patient identifiers removed.
Antidepressants were the most commonly prescribed medication class in the United States in 2011, and SSRIs were the most common type of antidepressant, she said. SSRI use has been associated with increased risk of bleeding, falls, bradycardia, and stroke in previous studies, which also suggest a possible protective effect of SSRIs in patients with coronary artery disease.
Dr. Berg reported having no financial disclosures.
Dr. Katherine M. Berg, SSRI, or serotonin norepinephrine reuptake inhibitor, SNRI, American Thoracic Society, acute coronary syndrome, Citalopram, sertraline, Fluoxetine, paroxetine, escitalopram,
SAN FRANCISCO – Patients on selective serotonin reuptake inhibitors or serotonin norepinephrine reuptake inhibitors when they were admitted to an intensive care unit were 73% more likely to die in the hospital, compared with ICU patients who were not on these antidepressants, a retrospective study found.
Dr. Katherine M. Berg and her associates analyzed electronic records from admissions to four ICUs in 2001-2008 to compare outcomes for 1,876 patients who were on a selective serotonin reuptake inhibitor (SSRI) or serotonin norepinephrine reuptake inhibitor (SNRI) and 8,692 control patients who were not taking an SSRI or SNRI before admission.
The mortality risk remained elevated at 1,000 days after ICU admission, she reported in a late-breaking poster presentation and discussion session at an international conference of the American Thoracic Society.
Certain subgroups were at even greater risk of dying in the hospital if they were on an SSRI or SNRI when admitted to the ICU. Patients who had acute coronary syndrome or had undergone cardiac surgery were more than twice as likely to die if they were on an SSRI/SNRI when entering the ICU, compared with controls, said Dr. Berg, a pulmonary/critical care fellow at Massachusetts General Hospital and Harvard University, Boston.
The increased mortality risk appeared to be associated mainly with medications that have higher degrees of serotonin reuptake inhibition. "Citalopram, which is a lower-potency drug, by itself did not incur a higher mortality risk, but sertraline, which is one of the more potent drugs, did. Even comparing the two drugs to each other, if you were on sertraline, your mortality risk was higher" than if you were on citalopram, Dr. Berg said in an interview.
Fluoxetine, paroxetine, and sertraline were associated with significantly higher mortality, but no significant mortality differences were seen between patients on citalopram or escitalopram and control patients.
Of the 8,692 control patients, 7% died in the hospital, compared with in-hospital death rates of 10% in 286 patients on fluoxetine, 13% in 320 patients on paroxetine, and 15% in 426 patients on sertraline at the time of ICU admission. The remaining 844 patients were on other antidepressants.
The study adjusted for the effects of each patient’s age, Simplified Acute Physiology Score, and combined Elixhauser comorbidity score on in-hospital mortality risk.
Slight but statistically significant differences in the characteristics of the two groups included a greater proportion of women in the SSRI/SNRI group, compared with controls (57% vs. 40%), and a higher prevalence of diabetes (21% vs. 17%) or chronic obstructive pulmonary disease (11% vs. 7%) in patients on an SSRI/SNRI, compared with controls. Patients in the SSRI/SNRI group were more likely to have an infection than were controls (11% vs. 8%), but less likely to have acute coronary syndrome (8% vs. 10%) or cardiovascular disease (67% vs. 70%).
Further studies are needed to ascertain if this is a causal relationship or just an association between SSRI/SNRI use and mortality in ICU patients, she said. The findings are limited by the retrospective nature of the study, which also was unable to control for the effects of potentially important confounders such as smoking status or the presence of depression.
The data came from the Multiparameter Intelligent Monitoring in Intensive Care II database, a public collection of data with patient identifiers removed.
Antidepressants were the most commonly prescribed medication class in the United States in 2011, and SSRIs were the most common type of antidepressant, she said. SSRI use has been associated with increased risk of bleeding, falls, bradycardia, and stroke in previous studies, which also suggest a possible protective effect of SSRIs in patients with coronary artery disease.
Dr. Berg reported having no financial disclosures.
SAN FRANCISCO – Patients on selective serotonin reuptake inhibitors or serotonin norepinephrine reuptake inhibitors when they were admitted to an intensive care unit were 73% more likely to die in the hospital, compared with ICU patients who were not on these antidepressants, a retrospective study found.
Dr. Katherine M. Berg and her associates analyzed electronic records from admissions to four ICUs in 2001-2008 to compare outcomes for 1,876 patients who were on a selective serotonin reuptake inhibitor (SSRI) or serotonin norepinephrine reuptake inhibitor (SNRI) and 8,692 control patients who were not taking an SSRI or SNRI before admission.
The mortality risk remained elevated at 1,000 days after ICU admission, she reported in a late-breaking poster presentation and discussion session at an international conference of the American Thoracic Society.
Certain subgroups were at even greater risk of dying in the hospital if they were on an SSRI or SNRI when admitted to the ICU. Patients who had acute coronary syndrome or had undergone cardiac surgery were more than twice as likely to die if they were on an SSRI/SNRI when entering the ICU, compared with controls, said Dr. Berg, a pulmonary/critical care fellow at Massachusetts General Hospital and Harvard University, Boston.
The increased mortality risk appeared to be associated mainly with medications that have higher degrees of serotonin reuptake inhibition. "Citalopram, which is a lower-potency drug, by itself did not incur a higher mortality risk, but sertraline, which is one of the more potent drugs, did. Even comparing the two drugs to each other, if you were on sertraline, your mortality risk was higher" than if you were on citalopram, Dr. Berg said in an interview.
Fluoxetine, paroxetine, and sertraline were associated with significantly higher mortality, but no significant mortality differences were seen between patients on citalopram or escitalopram and control patients.
Of the 8,692 control patients, 7% died in the hospital, compared with in-hospital death rates of 10% in 286 patients on fluoxetine, 13% in 320 patients on paroxetine, and 15% in 426 patients on sertraline at the time of ICU admission. The remaining 844 patients were on other antidepressants.
The study adjusted for the effects of each patient’s age, Simplified Acute Physiology Score, and combined Elixhauser comorbidity score on in-hospital mortality risk.
Slight but statistically significant differences in the characteristics of the two groups included a greater proportion of women in the SSRI/SNRI group, compared with controls (57% vs. 40%), and a higher prevalence of diabetes (21% vs. 17%) or chronic obstructive pulmonary disease (11% vs. 7%) in patients on an SSRI/SNRI, compared with controls. Patients in the SSRI/SNRI group were more likely to have an infection than were controls (11% vs. 8%), but less likely to have acute coronary syndrome (8% vs. 10%) or cardiovascular disease (67% vs. 70%).
Further studies are needed to ascertain if this is a causal relationship or just an association between SSRI/SNRI use and mortality in ICU patients, she said. The findings are limited by the retrospective nature of the study, which also was unable to control for the effects of potentially important confounders such as smoking status or the presence of depression.
The data came from the Multiparameter Intelligent Monitoring in Intensive Care II database, a public collection of data with patient identifiers removed.
Antidepressants were the most commonly prescribed medication class in the United States in 2011, and SSRIs were the most common type of antidepressant, she said. SSRI use has been associated with increased risk of bleeding, falls, bradycardia, and stroke in previous studies, which also suggest a possible protective effect of SSRIs in patients with coronary artery disease.
Dr. Berg reported having no financial disclosures.
Dr. Katherine M. Berg, SSRI, or serotonin norepinephrine reuptake inhibitor, SNRI, American Thoracic Society, acute coronary syndrome, Citalopram, sertraline, Fluoxetine, paroxetine, escitalopram,
Dr. Katherine M. Berg, SSRI, or serotonin norepinephrine reuptake inhibitor, SNRI, American Thoracic Society, acute coronary syndrome, Citalopram, sertraline, Fluoxetine, paroxetine, escitalopram,
AT AN INTERNATIONAL CONFERENCE OF THE AMERICAN THORACIC SOCIETY
Tips on Cardiovascular Testing Before Cancer Surgery
MIAMI BEACH – When you are called to assess a patient before cancer surgery, how do you know when noninvasive cardiovascular testing is warranted?
Start by asking patients to describe their functional status before they started any treatment to combat their cancer, Dr. Sunil K. Sahai said.
Also assess for any ischemia preoperatively, because its presence might direct a surgeon to prescribe a less cardiotoxic postoperative treatment for your patient, Dr. Sahai said at a meeting on perioperative medicine sponsored by the University of Miami. Occult ischemia might be found if a patient reports shortness of breath during prior chemotherapy administration, he added.
"Everything you’ve heard about perioperative medicine is true for cancer patients, but they are also unique," Dr. Sahai said. The physiologic burden of cancer and its treatment makes preoperative evaluation challenging, but it’s worth doing right to ensure the patient receives the optimal therapy. Also, in some cases, either the patient or surgeon will decide not to proceed with surgery based on your risk assessment, said Dr. Sahai, medical director of the Internal Medicine Perioperative Assessment Center at the University of Texas M.D. Anderson Cancer Center in Houston.
To illustrate some of the challenges, Dr. Sahai described an actual patient, a 60-year-old man referred for preoperative assessment 1 week before a scheduled neck dissection and total laryngectomy. He presented with dysphagia and sore throat. A biopsy revealed postcricoid squamous cell carcinoma. He was otherwise healthy, except for psoriasis and benign prostatic hyperplasia. He had undergone surgery and radiation for nasopharyngeal cancer 15 years earlier. The current physical examination was unremarkable, except for bilateral carotid bruits. Doppler ultrasound findings led to a diagnosis of radiation-induced carotid stenosis with diffuse, bilateral atherosclerosis and greater than 70% stenosis.
Head and neck cancer patients can have double the risk of transient ischemic attack or cerebrovascular accident, compared with a patient with normal pathologic narrowing of the carotid arteries, Dr. Sahai said. This is a controversial area because "data are not clear on what to do."
"We postponed and all discussed with all the providers involved," Dr. Sahai said. A stent was placed in the patient’s right internal carotid artery, and cancer surgery was delayed for 1 month while the patient took clopidogrel and aspirin. "He then went to the operating room on aspirin, and he did well."
Another case, a 70-year-old woman scheduled for a 6-hour cystectomy for bladder cancer, raised issues around preoperative cardiovascular assessment. "She reports fatigue and shortness of breath with exertion on her evening walks," Dr. Sahai said. "Before chemotherapy, she was able to walk eight blocks and up two flights of stairs without stopping. Now she can walk only four blocks and stops to rest between flights." She does not describe typical angina symptoms, he added.
The patient is obese, has diabetes mellitus, and is taking a statin for hyperlipidemia. She does not report any angina symptoms. Her history includes a myocardial infarction 5 years earlier addressed with medical management only.
Cancer can sap a patient’s energy, but the precise etiology in this case was unclear, Dr. Sahai said. Was her shortness of breath related to coronary artery disease, heart failure, pulmonary hypertension, or treatment with cardiotoxic chemotherapy? Should the patient be tested, for example, with an echocardiogram for heart function, stress test for ischemia, or both?
"Because this patient had received cardiotoxic chemotherapy ... we would do a stress echo on this patient," Dr. Sahai said. "In addition, BNP [B-type natriuretic peptide] levels may be helpful to detect cardiomyopathy. I would also optimize cardiac function and heart rate and send her to the operating room with the statin on board."
Patients with no cardiovascular symptoms can generally go to the operating room. If a patient is symptomatic, however, especially if the symptoms are new since cancer therapy was begun, Dr. Sahai said he generally considers further testing and work-up.
Dr. Sahai had no relevant financial disclosures.
MIAMI BEACH – When you are called to assess a patient before cancer surgery, how do you know when noninvasive cardiovascular testing is warranted?
Start by asking patients to describe their functional status before they started any treatment to combat their cancer, Dr. Sunil K. Sahai said.
Also assess for any ischemia preoperatively, because its presence might direct a surgeon to prescribe a less cardiotoxic postoperative treatment for your patient, Dr. Sahai said at a meeting on perioperative medicine sponsored by the University of Miami. Occult ischemia might be found if a patient reports shortness of breath during prior chemotherapy administration, he added.
"Everything you’ve heard about perioperative medicine is true for cancer patients, but they are also unique," Dr. Sahai said. The physiologic burden of cancer and its treatment makes preoperative evaluation challenging, but it’s worth doing right to ensure the patient receives the optimal therapy. Also, in some cases, either the patient or surgeon will decide not to proceed with surgery based on your risk assessment, said Dr. Sahai, medical director of the Internal Medicine Perioperative Assessment Center at the University of Texas M.D. Anderson Cancer Center in Houston.
To illustrate some of the challenges, Dr. Sahai described an actual patient, a 60-year-old man referred for preoperative assessment 1 week before a scheduled neck dissection and total laryngectomy. He presented with dysphagia and sore throat. A biopsy revealed postcricoid squamous cell carcinoma. He was otherwise healthy, except for psoriasis and benign prostatic hyperplasia. He had undergone surgery and radiation for nasopharyngeal cancer 15 years earlier. The current physical examination was unremarkable, except for bilateral carotid bruits. Doppler ultrasound findings led to a diagnosis of radiation-induced carotid stenosis with diffuse, bilateral atherosclerosis and greater than 70% stenosis.
Head and neck cancer patients can have double the risk of transient ischemic attack or cerebrovascular accident, compared with a patient with normal pathologic narrowing of the carotid arteries, Dr. Sahai said. This is a controversial area because "data are not clear on what to do."
"We postponed and all discussed with all the providers involved," Dr. Sahai said. A stent was placed in the patient’s right internal carotid artery, and cancer surgery was delayed for 1 month while the patient took clopidogrel and aspirin. "He then went to the operating room on aspirin, and he did well."
Another case, a 70-year-old woman scheduled for a 6-hour cystectomy for bladder cancer, raised issues around preoperative cardiovascular assessment. "She reports fatigue and shortness of breath with exertion on her evening walks," Dr. Sahai said. "Before chemotherapy, she was able to walk eight blocks and up two flights of stairs without stopping. Now she can walk only four blocks and stops to rest between flights." She does not describe typical angina symptoms, he added.
The patient is obese, has diabetes mellitus, and is taking a statin for hyperlipidemia. She does not report any angina symptoms. Her history includes a myocardial infarction 5 years earlier addressed with medical management only.
Cancer can sap a patient’s energy, but the precise etiology in this case was unclear, Dr. Sahai said. Was her shortness of breath related to coronary artery disease, heart failure, pulmonary hypertension, or treatment with cardiotoxic chemotherapy? Should the patient be tested, for example, with an echocardiogram for heart function, stress test for ischemia, or both?
"Because this patient had received cardiotoxic chemotherapy ... we would do a stress echo on this patient," Dr. Sahai said. "In addition, BNP [B-type natriuretic peptide] levels may be helpful to detect cardiomyopathy. I would also optimize cardiac function and heart rate and send her to the operating room with the statin on board."
Patients with no cardiovascular symptoms can generally go to the operating room. If a patient is symptomatic, however, especially if the symptoms are new since cancer therapy was begun, Dr. Sahai said he generally considers further testing and work-up.
Dr. Sahai had no relevant financial disclosures.
MIAMI BEACH – When you are called to assess a patient before cancer surgery, how do you know when noninvasive cardiovascular testing is warranted?
Start by asking patients to describe their functional status before they started any treatment to combat their cancer, Dr. Sunil K. Sahai said.
Also assess for any ischemia preoperatively, because its presence might direct a surgeon to prescribe a less cardiotoxic postoperative treatment for your patient, Dr. Sahai said at a meeting on perioperative medicine sponsored by the University of Miami. Occult ischemia might be found if a patient reports shortness of breath during prior chemotherapy administration, he added.
"Everything you’ve heard about perioperative medicine is true for cancer patients, but they are also unique," Dr. Sahai said. The physiologic burden of cancer and its treatment makes preoperative evaluation challenging, but it’s worth doing right to ensure the patient receives the optimal therapy. Also, in some cases, either the patient or surgeon will decide not to proceed with surgery based on your risk assessment, said Dr. Sahai, medical director of the Internal Medicine Perioperative Assessment Center at the University of Texas M.D. Anderson Cancer Center in Houston.
To illustrate some of the challenges, Dr. Sahai described an actual patient, a 60-year-old man referred for preoperative assessment 1 week before a scheduled neck dissection and total laryngectomy. He presented with dysphagia and sore throat. A biopsy revealed postcricoid squamous cell carcinoma. He was otherwise healthy, except for psoriasis and benign prostatic hyperplasia. He had undergone surgery and radiation for nasopharyngeal cancer 15 years earlier. The current physical examination was unremarkable, except for bilateral carotid bruits. Doppler ultrasound findings led to a diagnosis of radiation-induced carotid stenosis with diffuse, bilateral atherosclerosis and greater than 70% stenosis.
Head and neck cancer patients can have double the risk of transient ischemic attack or cerebrovascular accident, compared with a patient with normal pathologic narrowing of the carotid arteries, Dr. Sahai said. This is a controversial area because "data are not clear on what to do."
"We postponed and all discussed with all the providers involved," Dr. Sahai said. A stent was placed in the patient’s right internal carotid artery, and cancer surgery was delayed for 1 month while the patient took clopidogrel and aspirin. "He then went to the operating room on aspirin, and he did well."
Another case, a 70-year-old woman scheduled for a 6-hour cystectomy for bladder cancer, raised issues around preoperative cardiovascular assessment. "She reports fatigue and shortness of breath with exertion on her evening walks," Dr. Sahai said. "Before chemotherapy, she was able to walk eight blocks and up two flights of stairs without stopping. Now she can walk only four blocks and stops to rest between flights." She does not describe typical angina symptoms, he added.
The patient is obese, has diabetes mellitus, and is taking a statin for hyperlipidemia. She does not report any angina symptoms. Her history includes a myocardial infarction 5 years earlier addressed with medical management only.
Cancer can sap a patient’s energy, but the precise etiology in this case was unclear, Dr. Sahai said. Was her shortness of breath related to coronary artery disease, heart failure, pulmonary hypertension, or treatment with cardiotoxic chemotherapy? Should the patient be tested, for example, with an echocardiogram for heart function, stress test for ischemia, or both?
"Because this patient had received cardiotoxic chemotherapy ... we would do a stress echo on this patient," Dr. Sahai said. "In addition, BNP [B-type natriuretic peptide] levels may be helpful to detect cardiomyopathy. I would also optimize cardiac function and heart rate and send her to the operating room with the statin on board."
Patients with no cardiovascular symptoms can generally go to the operating room. If a patient is symptomatic, however, especially if the symptoms are new since cancer therapy was begun, Dr. Sahai said he generally considers further testing and work-up.
Dr. Sahai had no relevant financial disclosures.
EXPERT ANALYSIS FROM A MEETING ON PERIOPERATIVE MEDICINE SPONSORED BY THE UNIVERSITY OF MIAMI
Ventral Hernia Repair Incurs Overall Financial Losses
SAN DIEGO – Ventral hernia repair is associated with overall financial losses reaching the thousands of dollars in some cases, a single-center study demonstrated.
"These financial losses are just simply not sustainable," Dr. Drew Reynolds said in an interview prior to the annual Digestive Disease Week, where the study was presented.
In what is believed to be the first study of its kind, he and his associates set out to systematically evaluate hospital finances with respect to open ventral incisional hernia repair in the tertiary care environment.
"There is limited cost data currently available in the literature," he said. "These patients are complex and often require management in tertiary referral centers. Biologic meshes have a legitimate role in certain clinical scenarios, especially in those encountered in the tertiary care environment. Reimbursement strategies need to be reevaluated with more appropriate adjustment for preoperative risk factors and operative complexity."
Hospital costs associated with complex hernia repairs include direct costs (mesh materials, supplies, and non–surgeon labor), and indirect costs (facility fees, equipment depreciation, and unallocated labor), said Dr. Reynolds, a fellow in minimally invasive surgery at the University of Kentucky, Lexington. "Operative supplies including mesh represent a significant component of direct costs, especially in an era of proprietary synthetic meshes and biologic grafts," the researchers wrote in their abstract.
Dr. Reynolds and his associates evaluated cost data on 415 consecutive open ventral hernia repairs performed at the university’s hospital between July 1, 2008, and May 31, 2011, using CPT codes 49560, 49561, 49565, and 49566. They analyzed data based on hospital status (inpatient vs. outpatient) and whether the hernia repair was a primary or secondary procedure. The primary end points were hospital revenue and costs. Revenue calculations were adjusted for comorbid conditions/diagnosis-related groups, and readmission costs were not included.
Of the 415 patients, 353 were inpatients and 62 were outpatients. Among the 353 inpatients, ventral hernia repair was the primary procedure performed on 173 patients and was the secondary procedure for 180 patients. The median net revenue was significantly greater for those who underwent hernia repair as a secondary procedure compared with those who had hernia repair as a primary procedure ($17,310 vs. $10,360, P less than .01), as were net losses ($3,340 vs. $1,700, P less than .01).
Among the inpatient primary ventral hernia repairs, 46 were repaired without mesh, 79 were repaired with synthetic mesh, and 48 were repaired with biologic mesh, for median direct costs of $5,432, $7,590, and $16,970, respectively (P less than .01).
Dr. Reynolds also reported that among all inpatient ventral hernia repairs, the median net losses for repairs without mesh were $500, while synthetic mesh–based repairs yielded a median net profit of $60. The median contribution margin for cases involving biologic mesh was –$4,560, and the median net financial loss was $8,370.
Among patients who underwent outpatient ventral hernia repairs, median net losses among those performed with and without synthetic mesh reached $1,560 and $230, respectively.
"It was surprising to note that the vast majority of open ventral incisional hernia repairs are performed at an overall financial loss for the hospital," Dr. Reynolds said. "Further, it was surprising to note that inpatient biologic mesh–based ventral hernia repairs resulted in such a sizable negative median contribution margin ($4,560), and the striking median net financial loss of $8,370."
He acknowledged certain limitations of the study, including the fact that data used in the analysis were retrieved by CPT code search. "Hospital readmission costs were not included, which leads to underestimation of the costs," he added.
Dr. Reynolds said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Ventral hernia repair is associated with overall financial losses reaching the thousands of dollars in some cases, a single-center study demonstrated.
"These financial losses are just simply not sustainable," Dr. Drew Reynolds said in an interview prior to the annual Digestive Disease Week, where the study was presented.
In what is believed to be the first study of its kind, he and his associates set out to systematically evaluate hospital finances with respect to open ventral incisional hernia repair in the tertiary care environment.
"There is limited cost data currently available in the literature," he said. "These patients are complex and often require management in tertiary referral centers. Biologic meshes have a legitimate role in certain clinical scenarios, especially in those encountered in the tertiary care environment. Reimbursement strategies need to be reevaluated with more appropriate adjustment for preoperative risk factors and operative complexity."
Hospital costs associated with complex hernia repairs include direct costs (mesh materials, supplies, and non–surgeon labor), and indirect costs (facility fees, equipment depreciation, and unallocated labor), said Dr. Reynolds, a fellow in minimally invasive surgery at the University of Kentucky, Lexington. "Operative supplies including mesh represent a significant component of direct costs, especially in an era of proprietary synthetic meshes and biologic grafts," the researchers wrote in their abstract.
Dr. Reynolds and his associates evaluated cost data on 415 consecutive open ventral hernia repairs performed at the university’s hospital between July 1, 2008, and May 31, 2011, using CPT codes 49560, 49561, 49565, and 49566. They analyzed data based on hospital status (inpatient vs. outpatient) and whether the hernia repair was a primary or secondary procedure. The primary end points were hospital revenue and costs. Revenue calculations were adjusted for comorbid conditions/diagnosis-related groups, and readmission costs were not included.
Of the 415 patients, 353 were inpatients and 62 were outpatients. Among the 353 inpatients, ventral hernia repair was the primary procedure performed on 173 patients and was the secondary procedure for 180 patients. The median net revenue was significantly greater for those who underwent hernia repair as a secondary procedure compared with those who had hernia repair as a primary procedure ($17,310 vs. $10,360, P less than .01), as were net losses ($3,340 vs. $1,700, P less than .01).
Among the inpatient primary ventral hernia repairs, 46 were repaired without mesh, 79 were repaired with synthetic mesh, and 48 were repaired with biologic mesh, for median direct costs of $5,432, $7,590, and $16,970, respectively (P less than .01).
Dr. Reynolds also reported that among all inpatient ventral hernia repairs, the median net losses for repairs without mesh were $500, while synthetic mesh–based repairs yielded a median net profit of $60. The median contribution margin for cases involving biologic mesh was –$4,560, and the median net financial loss was $8,370.
Among patients who underwent outpatient ventral hernia repairs, median net losses among those performed with and without synthetic mesh reached $1,560 and $230, respectively.
"It was surprising to note that the vast majority of open ventral incisional hernia repairs are performed at an overall financial loss for the hospital," Dr. Reynolds said. "Further, it was surprising to note that inpatient biologic mesh–based ventral hernia repairs resulted in such a sizable negative median contribution margin ($4,560), and the striking median net financial loss of $8,370."
He acknowledged certain limitations of the study, including the fact that data used in the analysis were retrieved by CPT code search. "Hospital readmission costs were not included, which leads to underestimation of the costs," he added.
Dr. Reynolds said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Ventral hernia repair is associated with overall financial losses reaching the thousands of dollars in some cases, a single-center study demonstrated.
"These financial losses are just simply not sustainable," Dr. Drew Reynolds said in an interview prior to the annual Digestive Disease Week, where the study was presented.
In what is believed to be the first study of its kind, he and his associates set out to systematically evaluate hospital finances with respect to open ventral incisional hernia repair in the tertiary care environment.
"There is limited cost data currently available in the literature," he said. "These patients are complex and often require management in tertiary referral centers. Biologic meshes have a legitimate role in certain clinical scenarios, especially in those encountered in the tertiary care environment. Reimbursement strategies need to be reevaluated with more appropriate adjustment for preoperative risk factors and operative complexity."
Hospital costs associated with complex hernia repairs include direct costs (mesh materials, supplies, and non–surgeon labor), and indirect costs (facility fees, equipment depreciation, and unallocated labor), said Dr. Reynolds, a fellow in minimally invasive surgery at the University of Kentucky, Lexington. "Operative supplies including mesh represent a significant component of direct costs, especially in an era of proprietary synthetic meshes and biologic grafts," the researchers wrote in their abstract.
Dr. Reynolds and his associates evaluated cost data on 415 consecutive open ventral hernia repairs performed at the university’s hospital between July 1, 2008, and May 31, 2011, using CPT codes 49560, 49561, 49565, and 49566. They analyzed data based on hospital status (inpatient vs. outpatient) and whether the hernia repair was a primary or secondary procedure. The primary end points were hospital revenue and costs. Revenue calculations were adjusted for comorbid conditions/diagnosis-related groups, and readmission costs were not included.
Of the 415 patients, 353 were inpatients and 62 were outpatients. Among the 353 inpatients, ventral hernia repair was the primary procedure performed on 173 patients and was the secondary procedure for 180 patients. The median net revenue was significantly greater for those who underwent hernia repair as a secondary procedure compared with those who had hernia repair as a primary procedure ($17,310 vs. $10,360, P less than .01), as were net losses ($3,340 vs. $1,700, P less than .01).
Among the inpatient primary ventral hernia repairs, 46 were repaired without mesh, 79 were repaired with synthetic mesh, and 48 were repaired with biologic mesh, for median direct costs of $5,432, $7,590, and $16,970, respectively (P less than .01).
Dr. Reynolds also reported that among all inpatient ventral hernia repairs, the median net losses for repairs without mesh were $500, while synthetic mesh–based repairs yielded a median net profit of $60. The median contribution margin for cases involving biologic mesh was –$4,560, and the median net financial loss was $8,370.
Among patients who underwent outpatient ventral hernia repairs, median net losses among those performed with and without synthetic mesh reached $1,560 and $230, respectively.
"It was surprising to note that the vast majority of open ventral incisional hernia repairs are performed at an overall financial loss for the hospital," Dr. Reynolds said. "Further, it was surprising to note that inpatient biologic mesh–based ventral hernia repairs resulted in such a sizable negative median contribution margin ($4,560), and the striking median net financial loss of $8,370."
He acknowledged certain limitations of the study, including the fact that data used in the analysis were retrieved by CPT code search. "Hospital readmission costs were not included, which leads to underestimation of the costs," he added.
Dr. Reynolds said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL DIGESTIVE DISEASE WEEK
MRSA Nasal Colonization Predicts MRSA Site Infection in GI Surgery
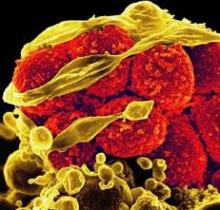
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
SAN DIEGO – Nasal colonization of methicillin-resistant Staphylococcus aureus was linked to an increase in surgical site infections and longer hospital stays in patients undergoing major gastrointestinal surgery in a large retrospective study, a finding that surprised investigators who had hypothesized that nasal colonization of the organism, which is not routinely found or colonized in the GI tract, would have little impact on outcome measures.
"Gastrointestinal operations are different from other surgeries in that infectious pathogens are typically organisms found in the gut, not bacteria that colonize in the skin, which is why we didn’t expect to find a correlation," lead investigator Dr. Harry T. Papaconstantinou said during a teleconference reporting the results, which he presented on Sunday, May 20, at the annual Digestive Disease Week conference.
While it’s unlikely that nasal colonization of MRSA necessarily increases the risk of developing a surgical site infection following GI surgery, "it is possible that it might be an indicator of the type of organism that is involved in the infection." For example, in the current analysis, wound culture data were available for 92 patients. In patients who tested positive for MRSA, 70% of the wound infections stemmed from MRSA, compared with only 8.5% in of those who tested negative, he said.
To evaluate the relationship between MRSA nasal colonization and surgical site infection, wound cultures, hospital length of stay, and mortality, Dr. Papaconstantinou, chief of colorectal surgery at Scott and White Memorial Hospital in Temple, Tex., and his colleagues examined the records of patients who underwent major GI surgery at the hospital between December 2007 and August 2009. The patients, who also had nasal swab tests within 24-48 hours after admission, were divided into one of three categories: MRSA-swab positive, methicillin-sensitive Staphylococcus aureus (MSSA)–swab positive, or negative for both.
Of the 1,137 patients, mean age 59.5 years, 73 (6.4%) were MRSA-swab positive, 167 (14.7%) were MSSA-swab positive, and 897 (78.9%) were negative, Dr. Papaconstantinou reported. Surgical site infection was identified in 101 patients (8.9%), and the rate of infection was highest, at 14%, in the MRSA-swab positive patients, compared with 4% and 9%, respectively, in the MSSA-swab positive and negative patients, he said. "When we controlled for other confounding factors, we didn’t find nasal swab to be an independent predictor of surgical site infection, but what we did find was a strong relationship between MRSA-positive nasal colonization and type of organism involved [in the surgical site infection]."
Regarding mean hospital length of stay, the respective durations for the MRSA-swab positive, MSSA-swab positive, and the negative groups overall were 12.5 days, 7.6 days, and 8.8 days, representing a significant increase, said Dr. Papaconstantinou. "By multiregression analysis, we found a MRSA-positive swab to be an independent risk factor for extended length of stay." However, when looking specifically at patients with surgical site infections, the presence of which increased hospital length of stay significantly from 6.2 days to 15.7 days, "there was no between group differences based on nasal swab," he said. Similarly, the 45 deaths in the study population wee distributed evenly across the nasal swab groups.
Based on the findings, Dr. Papaconstantinou said in an interview, "we can conclude that a positive MRSA nasal swab test for colonization is a strong predictor that MRSA-associated surgical site infections will occur in patients undergoing major GI surgery." As such, "we propose the possibility that it might be beneficial to preoperatively screen and decolonize these patients in an effort to reduce the incidence of these infections and improve patient outcomes following surgery." Toward this end, he and his colleagues are anticipating performing such a study and plan on including a cost-benefit analysis to determine whether screening is economically beneficial, he said.
Dr. Papaconstantinou disclosed a financial relationship with Covidien.
NEWS FROM DIGESTIVE DISEASE WEEK
Major Finding: The surgical site infection rate following major gastrointestinal surgery was 13.7% among patients with positive nasal swab results for MRSA, compared with 4.2% for patients testing positive for MSSA and 9.4% for patients with negative swabs. In patients with for whom wound culture data was available, the rate of MRSA-positive cultures was significantly higher, at 70%, in the MRSA-swab positive group, compared with 8.5% in noncolonized patients.
Data Source: Data were taken from retrospective analysis of medical records for 1,137 patients who underwent major gastrointestinal surgery and had nasal swab tests at Scott and White Memorial Hospital between December 2007 and August 2009. Wound culture data were available for 92 patients.
Disclosures: Dr. Papaconstantinou disclosed a financial relationship with Covidien.
Preop Antihypertensive Medication Should Not Be Skipped
MIAMI BEACH – "Green suit hypertension" can result in cancellation of procedures on the scheduled day of surgery, according to researchers who retrospectively studied 9,543 preoperative patients at the VA Nebraska – Western Iowa Health System.
And about half of these cases of preoperative hypertension result from withholding or missing antihypertensive medications on the morning of surgery, Dr. Joleen Fixley said at a meeting on perioperative medicine sponsored by the University of Miami.
Dr. Fixley and her colleagues found that 2,947 – or 31% of the total cohort of presurgical patients seen between 2004 and 2009 – had significant increases in blood pressure readings (blood pressure over 140 mmHg/90 mmHg) on the day of their procedure. This so-called green suit hypertension has been attributed to patients seeing their surgeons in green scrubs on the day of their operation. The group included 1,389 patients with previously controlled hypertension.
Those with green suit hypertension had a statistically significant average increase of 16 mmHg systolic and 23 mmHg diastolic over their baseline blood pressure measures as compared with other patients at the VA Nebraska – Western Iowa Health System, where Dr. Fixley is an attending in the department of internal medicine and medical director of the preoperative clinic.
Preoperative hypertension resulted in surgical cancellations for 73 patients overall, including 38 patients with green suit hypertension. These 38 patients had an average blood pressure increase from baseline of 47 mmHg systolic and 27 mmHg diastolic just before surgery.
"Holding or missing antihypertensive medications on the morning of surgery was responsible for almost half [45%] of our cancellations due to preoperative hypertension," Dr. Fixley said. This included 22% who skipped their diuretics, 15% who skipped their ACE inhibitors, and 8% who skipped both.
"Patient adherence to antihypertensive medication regimen is a factor in the perioperative period. The controversial practice of holding diuretics and ACE-inhibitors should cease," Dr. Fixley said.
Use of baseline blood pressure readings taken anywhere within their institution within 90 days of surgery was a potential limitation of the study, Dr. Fixley said. In addition, the study included a predominantly male population (94% were men; the average age was 63 years).
Future trials that assess intraoperative beta blockade therapy could include a cohort of patients with green suit hypertension to determine any beneficial effect, Dr. Fixley said.
Dr. Fixley said that she had no relevant financial disclosures.
MIAMI BEACH – "Green suit hypertension" can result in cancellation of procedures on the scheduled day of surgery, according to researchers who retrospectively studied 9,543 preoperative patients at the VA Nebraska – Western Iowa Health System.
And about half of these cases of preoperative hypertension result from withholding or missing antihypertensive medications on the morning of surgery, Dr. Joleen Fixley said at a meeting on perioperative medicine sponsored by the University of Miami.
Dr. Fixley and her colleagues found that 2,947 – or 31% of the total cohort of presurgical patients seen between 2004 and 2009 – had significant increases in blood pressure readings (blood pressure over 140 mmHg/90 mmHg) on the day of their procedure. This so-called green suit hypertension has been attributed to patients seeing their surgeons in green scrubs on the day of their operation. The group included 1,389 patients with previously controlled hypertension.
Those with green suit hypertension had a statistically significant average increase of 16 mmHg systolic and 23 mmHg diastolic over their baseline blood pressure measures as compared with other patients at the VA Nebraska – Western Iowa Health System, where Dr. Fixley is an attending in the department of internal medicine and medical director of the preoperative clinic.
Preoperative hypertension resulted in surgical cancellations for 73 patients overall, including 38 patients with green suit hypertension. These 38 patients had an average blood pressure increase from baseline of 47 mmHg systolic and 27 mmHg diastolic just before surgery.
"Holding or missing antihypertensive medications on the morning of surgery was responsible for almost half [45%] of our cancellations due to preoperative hypertension," Dr. Fixley said. This included 22% who skipped their diuretics, 15% who skipped their ACE inhibitors, and 8% who skipped both.
"Patient adherence to antihypertensive medication regimen is a factor in the perioperative period. The controversial practice of holding diuretics and ACE-inhibitors should cease," Dr. Fixley said.
Use of baseline blood pressure readings taken anywhere within their institution within 90 days of surgery was a potential limitation of the study, Dr. Fixley said. In addition, the study included a predominantly male population (94% were men; the average age was 63 years).
Future trials that assess intraoperative beta blockade therapy could include a cohort of patients with green suit hypertension to determine any beneficial effect, Dr. Fixley said.
Dr. Fixley said that she had no relevant financial disclosures.
MIAMI BEACH – "Green suit hypertension" can result in cancellation of procedures on the scheduled day of surgery, according to researchers who retrospectively studied 9,543 preoperative patients at the VA Nebraska – Western Iowa Health System.
And about half of these cases of preoperative hypertension result from withholding or missing antihypertensive medications on the morning of surgery, Dr. Joleen Fixley said at a meeting on perioperative medicine sponsored by the University of Miami.
Dr. Fixley and her colleagues found that 2,947 – or 31% of the total cohort of presurgical patients seen between 2004 and 2009 – had significant increases in blood pressure readings (blood pressure over 140 mmHg/90 mmHg) on the day of their procedure. This so-called green suit hypertension has been attributed to patients seeing their surgeons in green scrubs on the day of their operation. The group included 1,389 patients with previously controlled hypertension.
Those with green suit hypertension had a statistically significant average increase of 16 mmHg systolic and 23 mmHg diastolic over their baseline blood pressure measures as compared with other patients at the VA Nebraska – Western Iowa Health System, where Dr. Fixley is an attending in the department of internal medicine and medical director of the preoperative clinic.
Preoperative hypertension resulted in surgical cancellations for 73 patients overall, including 38 patients with green suit hypertension. These 38 patients had an average blood pressure increase from baseline of 47 mmHg systolic and 27 mmHg diastolic just before surgery.
"Holding or missing antihypertensive medications on the morning of surgery was responsible for almost half [45%] of our cancellations due to preoperative hypertension," Dr. Fixley said. This included 22% who skipped their diuretics, 15% who skipped their ACE inhibitors, and 8% who skipped both.
"Patient adherence to antihypertensive medication regimen is a factor in the perioperative period. The controversial practice of holding diuretics and ACE-inhibitors should cease," Dr. Fixley said.
Use of baseline blood pressure readings taken anywhere within their institution within 90 days of surgery was a potential limitation of the study, Dr. Fixley said. In addition, the study included a predominantly male population (94% were men; the average age was 63 years).
Future trials that assess intraoperative beta blockade therapy could include a cohort of patients with green suit hypertension to determine any beneficial effect, Dr. Fixley said.
Dr. Fixley said that she had no relevant financial disclosures.
FROM A MEETING ON PERIOPERATIVE MEDICINE SPONSORED BY THE UNIVERSITY OF MIAMI
Major Finding: Preoperative hypertension resulted in surgical cancellations for 73 patients overall, including 38 patients with green suit hypertension.
Data Source: A retrospective study of 9,543 surgical patients from 2004 to 2009 with baseline and day of surgery blood pressure readings.
Disclosures: Dr. Fixley reported having no financial disclosures.
Obesity Increases Surgical Site Infection Risk
LONDON – Being obese increased the risk of surgical site infection nearly fourfold among patients who underwent operations in the United Kingdom from 2006 through 2010.
The findings pose questions such as whether preoperative dosing of antibiotics might be adjusted upward or whether preoperative weight loss should be advocated, said Dr. Simon Thelwall of the Health Protection Agency, London.
The analysis was done using nationwide data from the UK’s Health Protection Agency (HPA) Surgical Site Infection Surveillance Service, comprising data submitted from all 212 of the National Health Service hospitals in England on a cumulative total of 326,880 adult patients who underwent one of five operations: abdominal hysterectomy, coronary artery bypass graft (CABG), hip replacement, knee replacement, and large bowel surgery.
Of those, surgical site infections (SSIs) were detected in inpatients and at readmission for 4,453, and body mass index (BMI) data were available for 43%. Of these 112,048 (79.3%) were overweight or obese, said Dr. Thelwall.
The rates of SSIs didn’t differ among those with and without available body mass index data except among CABG patients, for whom the rate of SSIs was double among those with and without BMI data (5.17% vs. 2.71%). The CABG patients with BMI data were also significantly more likely to have received implants (85% vs. 61%), to have undergone emergency operations (1.29% vs. 0.76%), and to have had significantly longer operations (205 vs. 220 minutes).
Thus, "CABG patients with BMI data are more likely to have risk factors predisposing them to SSI," Dr. Thelwall noted.
Obesity significantly increased the risk for SSI in all surgical groups except for abdominal hysterectomy, with risk ratios ranging from 1.62 for knee replacement to 1.87 for large bowel surgery. Obesity still increased the SSI risk among abdominal hysterectomy patients with a risk ratio of 1.81, but that did not reach statistical significance, he said.
Overall, the SSI risk increased with increasing BMI. In multivariate analysis adjusting for a variety of potential confounders including age, trauma, category of surgery, implant, and emergency surgery, the odds ratios for SSI increased from 1.44 among the overweight patients to 1.89 for those with BMIs of 30-34.99 kg/m2, to 2.94 for BMIs of 35-39.99 kg/m2, and to 3.73 for BMIs greater than 40 kg/m2. In the highest BMI category, even the SSI rate for abdominal hysterectomy became significantly greater, compared with that of patients of normal weight (risk ratio, 3.90), Dr. Thelwall said.
Among the morbidly obese (BMI greater than 40 kg/m2), between 65% and 78% of the risk for SSI was attributable to being very obese. And in that group of morbidly obese patients, the risk of SSI among abdominal hysterectomy patients became significantly elevated three- to fivefold, compared with that of women of normal weight, he noted.
Dr. Thelwall declared that he had no disclosures.
LONDON – Being obese increased the risk of surgical site infection nearly fourfold among patients who underwent operations in the United Kingdom from 2006 through 2010.
The findings pose questions such as whether preoperative dosing of antibiotics might be adjusted upward or whether preoperative weight loss should be advocated, said Dr. Simon Thelwall of the Health Protection Agency, London.
The analysis was done using nationwide data from the UK’s Health Protection Agency (HPA) Surgical Site Infection Surveillance Service, comprising data submitted from all 212 of the National Health Service hospitals in England on a cumulative total of 326,880 adult patients who underwent one of five operations: abdominal hysterectomy, coronary artery bypass graft (CABG), hip replacement, knee replacement, and large bowel surgery.
Of those, surgical site infections (SSIs) were detected in inpatients and at readmission for 4,453, and body mass index (BMI) data were available for 43%. Of these 112,048 (79.3%) were overweight or obese, said Dr. Thelwall.
The rates of SSIs didn’t differ among those with and without available body mass index data except among CABG patients, for whom the rate of SSIs was double among those with and without BMI data (5.17% vs. 2.71%). The CABG patients with BMI data were also significantly more likely to have received implants (85% vs. 61%), to have undergone emergency operations (1.29% vs. 0.76%), and to have had significantly longer operations (205 vs. 220 minutes).
Thus, "CABG patients with BMI data are more likely to have risk factors predisposing them to SSI," Dr. Thelwall noted.
Obesity significantly increased the risk for SSI in all surgical groups except for abdominal hysterectomy, with risk ratios ranging from 1.62 for knee replacement to 1.87 for large bowel surgery. Obesity still increased the SSI risk among abdominal hysterectomy patients with a risk ratio of 1.81, but that did not reach statistical significance, he said.
Overall, the SSI risk increased with increasing BMI. In multivariate analysis adjusting for a variety of potential confounders including age, trauma, category of surgery, implant, and emergency surgery, the odds ratios for SSI increased from 1.44 among the overweight patients to 1.89 for those with BMIs of 30-34.99 kg/m2, to 2.94 for BMIs of 35-39.99 kg/m2, and to 3.73 for BMIs greater than 40 kg/m2. In the highest BMI category, even the SSI rate for abdominal hysterectomy became significantly greater, compared with that of patients of normal weight (risk ratio, 3.90), Dr. Thelwall said.
Among the morbidly obese (BMI greater than 40 kg/m2), between 65% and 78% of the risk for SSI was attributable to being very obese. And in that group of morbidly obese patients, the risk of SSI among abdominal hysterectomy patients became significantly elevated three- to fivefold, compared with that of women of normal weight, he noted.
Dr. Thelwall declared that he had no disclosures.
LONDON – Being obese increased the risk of surgical site infection nearly fourfold among patients who underwent operations in the United Kingdom from 2006 through 2010.
The findings pose questions such as whether preoperative dosing of antibiotics might be adjusted upward or whether preoperative weight loss should be advocated, said Dr. Simon Thelwall of the Health Protection Agency, London.
The analysis was done using nationwide data from the UK’s Health Protection Agency (HPA) Surgical Site Infection Surveillance Service, comprising data submitted from all 212 of the National Health Service hospitals in England on a cumulative total of 326,880 adult patients who underwent one of five operations: abdominal hysterectomy, coronary artery bypass graft (CABG), hip replacement, knee replacement, and large bowel surgery.
Of those, surgical site infections (SSIs) were detected in inpatients and at readmission for 4,453, and body mass index (BMI) data were available for 43%. Of these 112,048 (79.3%) were overweight or obese, said Dr. Thelwall.
The rates of SSIs didn’t differ among those with and without available body mass index data except among CABG patients, for whom the rate of SSIs was double among those with and without BMI data (5.17% vs. 2.71%). The CABG patients with BMI data were also significantly more likely to have received implants (85% vs. 61%), to have undergone emergency operations (1.29% vs. 0.76%), and to have had significantly longer operations (205 vs. 220 minutes).
Thus, "CABG patients with BMI data are more likely to have risk factors predisposing them to SSI," Dr. Thelwall noted.
Obesity significantly increased the risk for SSI in all surgical groups except for abdominal hysterectomy, with risk ratios ranging from 1.62 for knee replacement to 1.87 for large bowel surgery. Obesity still increased the SSI risk among abdominal hysterectomy patients with a risk ratio of 1.81, but that did not reach statistical significance, he said.
Overall, the SSI risk increased with increasing BMI. In multivariate analysis adjusting for a variety of potential confounders including age, trauma, category of surgery, implant, and emergency surgery, the odds ratios for SSI increased from 1.44 among the overweight patients to 1.89 for those with BMIs of 30-34.99 kg/m2, to 2.94 for BMIs of 35-39.99 kg/m2, and to 3.73 for BMIs greater than 40 kg/m2. In the highest BMI category, even the SSI rate for abdominal hysterectomy became significantly greater, compared with that of patients of normal weight (risk ratio, 3.90), Dr. Thelwall said.
Among the morbidly obese (BMI greater than 40 kg/m2), between 65% and 78% of the risk for SSI was attributable to being very obese. And in that group of morbidly obese patients, the risk of SSI among abdominal hysterectomy patients became significantly elevated three- to fivefold, compared with that of women of normal weight, he noted.
Dr. Thelwall declared that he had no disclosures.
FROM THE EUROPEAN CONGRESS OF CLINICAL MICROBIOLOGY AND INFECTIOUS DISEASES
Major Finding: Obesity significantly increased the risk for surgical site infection in all surgical groups except for abdominal hysterectomy, with risk ratios ranging from 1.62 for knee replacement to 1.87 for large bowel surgery.
Data Source: This data analysis was based on data from the UK’s Health Protection Agency Surgical Site Infection Surveillance, which included 326,880 adult patients who underwent abdominal hysterectomy, coronary artery bypass graft, hip replacement, knee replacement, or large bowel surgery.
Disclosures: Dr. Thelwall is employed by the UK’s Health Protection Agency and has no financial disclosures.
Empowerment's Price Tag: Shared Decision-Making May Be Costly
SAN DIEGO – Inpatients who most strongly preferred to leave medical decisions to their doctors were discharged a third of a day sooner with $970 lower mean costs per patient, compared with patients who strongly disagreed about leaving decisions to their physicians, a study of data on 20,213 patients found.
The findings throw a wrinkle into the idea that empowering patients for shared decision making is always the best approach, Hyo Jung Tak, Ph.D. said at the annual meeting of the Society of Hospital Medicine.
Administrative and patient interview data on patients in the general medicine service at the University of Chicago Medical Center from 2003-2011 included responses of to the statement, "I prefer to leave decisions about my medical care up to my doctor." Patients responded with "definitely agree" (37% of patients), "somewhat agree" (34%), "somewhat disagree" (15%), or "definitely disagree" (14%).
Although 96% of patients said that they prefer to be informed by their doctors about treatment options and to be asked their opinions, 71% of patients strongly or somewhat agreed that they prefer to leave decisions about medical care to their doctors.
Dr. Tak compared responses to data on patients’ health care utilization, length of stay, and mean total costs.
Length of stay averaged 5.3 days for the entire cohort, but patients who "definitely agreed" with letting doctors make decisions left the hospital 0.31 days sooner than did those who "definitely disagreed," reported Dr. Tak and her associate in the study, Dr. David Meltzer, both of the University.
Total costs averaged $14,500 for the entire cohort, but costs for patients who "definitely agreed" with leaving decision to doctors averaged $970 less than for patients who "definitely disagreed" with that approach.
The differences between groups in length of stay and cost were statistically significant, Dr. Tak said. The analysis controlled for the possible effects of age, gender, educational category, health status, 10 most frequent diagnoses, Charlson index, weekend admission, transfer from another institution, and attending physicians.
The results raise a provocative question, she said: "Will patient empowerment efforts in a shared-decision model increase costs" in an era in which cost-control is one of the most pressing health policy issues?
Patients who definitely agreed to leave medical decisions to their doctors were significantly more likely to have no more than a high school education and to have public or no insurance, compared with patients who definitely disagreed about leaving medical decisions to their doctors.
Shared decision making between doctors and patients has emerged as the preferred approach for medical decisions, but patient preference for this approach has not been well characterized, and the effects of this approach on medical resource utilization rarely have been studied, Dr. Tak said.
The study was limited by its reliance on data from a single institution and by a lack of information on physicians’ preferences for shared decision making and the decision-making mechanisms.
The investigators plan further studies on how preferences for shared decision making affect health outcomes and on associations between socioeconomic status and preferences about decision-making. "At least in our study, it was patients with higher education and with more generous health insurance who preferred to participate" in decision-making, she said.
Dr. Tak reported having no financial disclosures.
SAN DIEGO – Inpatients who most strongly preferred to leave medical decisions to their doctors were discharged a third of a day sooner with $970 lower mean costs per patient, compared with patients who strongly disagreed about leaving decisions to their physicians, a study of data on 20,213 patients found.
The findings throw a wrinkle into the idea that empowering patients for shared decision making is always the best approach, Hyo Jung Tak, Ph.D. said at the annual meeting of the Society of Hospital Medicine.
Administrative and patient interview data on patients in the general medicine service at the University of Chicago Medical Center from 2003-2011 included responses of to the statement, "I prefer to leave decisions about my medical care up to my doctor." Patients responded with "definitely agree" (37% of patients), "somewhat agree" (34%), "somewhat disagree" (15%), or "definitely disagree" (14%).
Although 96% of patients said that they prefer to be informed by their doctors about treatment options and to be asked their opinions, 71% of patients strongly or somewhat agreed that they prefer to leave decisions about medical care to their doctors.
Dr. Tak compared responses to data on patients’ health care utilization, length of stay, and mean total costs.
Length of stay averaged 5.3 days for the entire cohort, but patients who "definitely agreed" with letting doctors make decisions left the hospital 0.31 days sooner than did those who "definitely disagreed," reported Dr. Tak and her associate in the study, Dr. David Meltzer, both of the University.
Total costs averaged $14,500 for the entire cohort, but costs for patients who "definitely agreed" with leaving decision to doctors averaged $970 less than for patients who "definitely disagreed" with that approach.
The differences between groups in length of stay and cost were statistically significant, Dr. Tak said. The analysis controlled for the possible effects of age, gender, educational category, health status, 10 most frequent diagnoses, Charlson index, weekend admission, transfer from another institution, and attending physicians.
The results raise a provocative question, she said: "Will patient empowerment efforts in a shared-decision model increase costs" in an era in which cost-control is one of the most pressing health policy issues?
Patients who definitely agreed to leave medical decisions to their doctors were significantly more likely to have no more than a high school education and to have public or no insurance, compared with patients who definitely disagreed about leaving medical decisions to their doctors.
Shared decision making between doctors and patients has emerged as the preferred approach for medical decisions, but patient preference for this approach has not been well characterized, and the effects of this approach on medical resource utilization rarely have been studied, Dr. Tak said.
The study was limited by its reliance on data from a single institution and by a lack of information on physicians’ preferences for shared decision making and the decision-making mechanisms.
The investigators plan further studies on how preferences for shared decision making affect health outcomes and on associations between socioeconomic status and preferences about decision-making. "At least in our study, it was patients with higher education and with more generous health insurance who preferred to participate" in decision-making, she said.
Dr. Tak reported having no financial disclosures.
SAN DIEGO – Inpatients who most strongly preferred to leave medical decisions to their doctors were discharged a third of a day sooner with $970 lower mean costs per patient, compared with patients who strongly disagreed about leaving decisions to their physicians, a study of data on 20,213 patients found.
The findings throw a wrinkle into the idea that empowering patients for shared decision making is always the best approach, Hyo Jung Tak, Ph.D. said at the annual meeting of the Society of Hospital Medicine.
Administrative and patient interview data on patients in the general medicine service at the University of Chicago Medical Center from 2003-2011 included responses of to the statement, "I prefer to leave decisions about my medical care up to my doctor." Patients responded with "definitely agree" (37% of patients), "somewhat agree" (34%), "somewhat disagree" (15%), or "definitely disagree" (14%).
Although 96% of patients said that they prefer to be informed by their doctors about treatment options and to be asked their opinions, 71% of patients strongly or somewhat agreed that they prefer to leave decisions about medical care to their doctors.
Dr. Tak compared responses to data on patients’ health care utilization, length of stay, and mean total costs.
Length of stay averaged 5.3 days for the entire cohort, but patients who "definitely agreed" with letting doctors make decisions left the hospital 0.31 days sooner than did those who "definitely disagreed," reported Dr. Tak and her associate in the study, Dr. David Meltzer, both of the University.
Total costs averaged $14,500 for the entire cohort, but costs for patients who "definitely agreed" with leaving decision to doctors averaged $970 less than for patients who "definitely disagreed" with that approach.
The differences between groups in length of stay and cost were statistically significant, Dr. Tak said. The analysis controlled for the possible effects of age, gender, educational category, health status, 10 most frequent diagnoses, Charlson index, weekend admission, transfer from another institution, and attending physicians.
The results raise a provocative question, she said: "Will patient empowerment efforts in a shared-decision model increase costs" in an era in which cost-control is one of the most pressing health policy issues?
Patients who definitely agreed to leave medical decisions to their doctors were significantly more likely to have no more than a high school education and to have public or no insurance, compared with patients who definitely disagreed about leaving medical decisions to their doctors.
Shared decision making between doctors and patients has emerged as the preferred approach for medical decisions, but patient preference for this approach has not been well characterized, and the effects of this approach on medical resource utilization rarely have been studied, Dr. Tak said.
The study was limited by its reliance on data from a single institution and by a lack of information on physicians’ preferences for shared decision making and the decision-making mechanisms.
The investigators plan further studies on how preferences for shared decision making affect health outcomes and on associations between socioeconomic status and preferences about decision-making. "At least in our study, it was patients with higher education and with more generous health insurance who preferred to participate" in decision-making, she said.
Dr. Tak reported having no financial disclosures.
FROM THE ANNUAL MEETING OF THE SOCIETY OF HOSPITAL MEDICINE
Major Finding: Inpatients who most strongly preferred to leave medical decisions to their [physicians were discharged 0.31 days sooner and paid $970 lower mean costs per patient, compared with those who strongly disagreed with doing so.
Data Source: Data on 20,213 inpatients on general medicine services at one center during 2003-2011 were analyzed retrospectively.
Disclosures: Dr. Tak did not report any financial disclosures.
In Case You Missed 'Em: Prominent Studies Published in Past Year
MIAMI BEACH – What do the timing of smoking cessation prior to surgery, reliable prediction of postoperative respiratory failure, and biomarkers that point to elevated postoperative myocardial infarction risk have in common? They emerged as some of the most prominent findings published in the past year, according to three experts in hospital medicine.
Dr. Gerald W. Smetana, Dr. Steven L. Cohn, and Dr. Paul J. Grant each selected studies of particular relevance to hospitalists and explained why during a panel presentation at a meeting on perioperative medicine sponsored by the University of Miami:
• Preoperative Smoking Cessation. When a patient stops smoking up to 8 weeks before noncardiac surgery, it does not significantly change the total or pulmonary complication rates, according to a systematic literature review (Arch. Intern. Med. 2011;171:983-9).
"Many patients who quit smoking report they feel worse before they feel better," said Dr. Smetana, an attending in the general medicine division at Beth Israel Deaconess Medical Center, Boston.
Increased cough and sputum production are common right after quitting, he said. "This could be a plausible mechanism to explain why recent quitters might be at increased risk for postoperative pulmonary complications."
However, there was no statistically significant difference in total complications (relative risk of 0.78 for recent quitters, compared with a reference value of 1.0 for current smokers) in the nine eligible studies with 889 participants. Five of the trials assessed pulmonary complications, and found that recent quitters had a nonsignificant increased risk (RR, 1.18) compared with patients who continued to smoke.
Until there is consensus based on large randomized trials, stopping smoking before surgery can be considered safe, said Dr. Smetana, who is also on the medicine faculty at Harvard Medical School. In addition, longer periods of cessation are likely better than shorter ones. He added that despite the lack of a significant finding, it is still worthwhile to counsel patients because any time before surgery is a still a teachable moment for smoking cessation.
• Predicting Postoperative Pulmonary Failure. Type of procedure, emergency surgery, poor dependent functional status, sepsis, and higher American Society of Anesthesiologists classification were the five independent preoperative factors that significantly predicted postoperative respiratory failure in a multicenter database study (Chest 2011;140:1207-15).
The study included 211,410 participants undergoing all types of surgery. Mortality was 26% among those with postoperative respiratory failure, compared with 1% for unaffected patients. "This shows how important pulmonary complications can be," Dr. Smetana said.
The researchers incorporated these five predictors into a surgical risk calculator that is downloadable for free.
Dr. Smetana said, "It is a nice tool that ... helps to stratify patients. It makes a difference in identifying which patients for which you will pull out all the stops."
• Preoperative Peptide Gauges Risk. Although multiple researchers have looked at preoperative B-type natriuretic peptide (BNP) as a predictor of postoperative cardiac events or death, there remain "a lot of unknowns for BNP at this point," said Dr. Cohn, director of the University of Miami Hospital Medical Consultation Service and professor of medicine at the University of Miami.
A recent meta-analysis may shed some light on the predictive value of BNP (J. Am. Coll. Cardiol. 2011;58:522-9). Investigators assessed five BNP studies with 632 patients to determine cutoff values for screening (high sensitivity) and diagnosis (high specificity), and an optimal value that combines both.
The researchers found that patients with BNP above the optimal cutoff point of 116 pg/mL had a significantly elevated risk for the composite outcome of nonfatal myocardial infarction or cardiovascular death (unadjusted odds ratio, 7.36). Compared with use of the Revised Cardiac Risk Index, the optimal BNP cutoff classification improved risk prediction by 58%. This means some patients moved to a more accurate ranking among the low-, intermediate- and high-risk categories, Dr. Cohn said.
• Troponin and Postoperative MI Risk. Myocardial infarction is the most common major, perioperative vascular complication, so investigators continue to search for an accurate way to identify high-risk patients. Some propose elevated serum levels of the protein troponin as a predictor, Dr. Cohn said, but the question remains: Would it change patient management and improve outcomes?
Researchers found that increased troponin after noncardiac surgery did in fact independently predict postoperative MI mortality in a meta-analysis (Anesthesiology 2011;114:796-806).
Elevated levels significantly predicted increased risk in the 14 studies with 3,318 patients overall (OR, 3.4). However, prediction within the first year was higher (OR, 6.7) compared with studies that measured troponin more than 12 months out (OR, 1.8).
These findings could have implications for practice, because the majority of perioperative MIs are asymptomatic, Dr. Cohn said. "Maybe we should, as the authors suggest, recommend routine troponins after high-risk surgery."
More frequent vital-sign monitoring; transfer to a unit with additional monitoring; and/or screening for hypoxia and anemia could be implemented in patients identified as high risk, Dr. Cohn said. Optimization of intravascular volume and initiation of cardiac medications are additional strategies. Also, closely monitored patients who experience an MI potentially could be transferred for cardiac catheterization or revascularization more quickly.
"It is thought provoking that we can change the management," Dr. Cohn said.
• HF, AF, and Cardiovascular Risk. Heart failure and atrial fibrillation should factor more prominently into cardiovascular risk stratification prior to noncardiac surgery, according to a population-based cohort study of more than 38,000 consecutive patients (Circulation 2011:124:289-96).
"There are many cardiovascular risk stratification tools available with quite a bit of variation. Coronary artery disease [CAD] is typically weighted heavily on most models," said Dr. Grant, director of perioperative and consultative medicine and member of the medicine faculty at the University of Michigan in Ann Arbor.
However, researchers found that ischemic and nonischemic heart failure and atrial fibrillation were more commonly associated with 30-day mortality and readmission rates than CAD in this large cohort, Dr. Grant said. The authors concluded that these risk factors are likely underestimated in current prediction models.
• Liberal vs. Conservative Blood Transfusion. "The hemoglobin level at which we decide to transfuse patients after surgery is controversial," Dr. Grant said, "and has not been adequately studied to date. Great variations in practice exist."
A randomized controlled trial of 2,016 hip fracture surgery patients found no significant difference between liberal and conservative postoperative blood transfusion policies in terms of mortality or ability to walk independently at 60 days for patients at high cardiovascular risk (N. Engl. J. Med. 2011;365:2453-62).
The liberal policy allowed transfusions to maintain hemoglobin at 10 g/dL. In contrast, patients randomized to a conservative approach could only be transfused if they had symptoms of anemia or at the physician’s discretion once hemoglobin was below 8 g/dL.
"Implications for practice, from my point of view, include some more evidence that maybe using more of a restrictive transfusion practice may be reasonable, including for higher-risk populations," Dr. Grant said. However, "red-cell transfusion practices still need to be individualized for your perioperative patient."
Dr. Smetana, Dr. Cohn, and Dr. Grant had no relevant financial disclosures.
MIAMI BEACH – What do the timing of smoking cessation prior to surgery, reliable prediction of postoperative respiratory failure, and biomarkers that point to elevated postoperative myocardial infarction risk have in common? They emerged as some of the most prominent findings published in the past year, according to three experts in hospital medicine.
Dr. Gerald W. Smetana, Dr. Steven L. Cohn, and Dr. Paul J. Grant each selected studies of particular relevance to hospitalists and explained why during a panel presentation at a meeting on perioperative medicine sponsored by the University of Miami:
• Preoperative Smoking Cessation. When a patient stops smoking up to 8 weeks before noncardiac surgery, it does not significantly change the total or pulmonary complication rates, according to a systematic literature review (Arch. Intern. Med. 2011;171:983-9).
"Many patients who quit smoking report they feel worse before they feel better," said Dr. Smetana, an attending in the general medicine division at Beth Israel Deaconess Medical Center, Boston.
Increased cough and sputum production are common right after quitting, he said. "This could be a plausible mechanism to explain why recent quitters might be at increased risk for postoperative pulmonary complications."
However, there was no statistically significant difference in total complications (relative risk of 0.78 for recent quitters, compared with a reference value of 1.0 for current smokers) in the nine eligible studies with 889 participants. Five of the trials assessed pulmonary complications, and found that recent quitters had a nonsignificant increased risk (RR, 1.18) compared with patients who continued to smoke.
Until there is consensus based on large randomized trials, stopping smoking before surgery can be considered safe, said Dr. Smetana, who is also on the medicine faculty at Harvard Medical School. In addition, longer periods of cessation are likely better than shorter ones. He added that despite the lack of a significant finding, it is still worthwhile to counsel patients because any time before surgery is a still a teachable moment for smoking cessation.
• Predicting Postoperative Pulmonary Failure. Type of procedure, emergency surgery, poor dependent functional status, sepsis, and higher American Society of Anesthesiologists classification were the five independent preoperative factors that significantly predicted postoperative respiratory failure in a multicenter database study (Chest 2011;140:1207-15).
The study included 211,410 participants undergoing all types of surgery. Mortality was 26% among those with postoperative respiratory failure, compared with 1% for unaffected patients. "This shows how important pulmonary complications can be," Dr. Smetana said.
The researchers incorporated these five predictors into a surgical risk calculator that is downloadable for free.
Dr. Smetana said, "It is a nice tool that ... helps to stratify patients. It makes a difference in identifying which patients for which you will pull out all the stops."
• Preoperative Peptide Gauges Risk. Although multiple researchers have looked at preoperative B-type natriuretic peptide (BNP) as a predictor of postoperative cardiac events or death, there remain "a lot of unknowns for BNP at this point," said Dr. Cohn, director of the University of Miami Hospital Medical Consultation Service and professor of medicine at the University of Miami.
A recent meta-analysis may shed some light on the predictive value of BNP (J. Am. Coll. Cardiol. 2011;58:522-9). Investigators assessed five BNP studies with 632 patients to determine cutoff values for screening (high sensitivity) and diagnosis (high specificity), and an optimal value that combines both.
The researchers found that patients with BNP above the optimal cutoff point of 116 pg/mL had a significantly elevated risk for the composite outcome of nonfatal myocardial infarction or cardiovascular death (unadjusted odds ratio, 7.36). Compared with use of the Revised Cardiac Risk Index, the optimal BNP cutoff classification improved risk prediction by 58%. This means some patients moved to a more accurate ranking among the low-, intermediate- and high-risk categories, Dr. Cohn said.
• Troponin and Postoperative MI Risk. Myocardial infarction is the most common major, perioperative vascular complication, so investigators continue to search for an accurate way to identify high-risk patients. Some propose elevated serum levels of the protein troponin as a predictor, Dr. Cohn said, but the question remains: Would it change patient management and improve outcomes?
Researchers found that increased troponin after noncardiac surgery did in fact independently predict postoperative MI mortality in a meta-analysis (Anesthesiology 2011;114:796-806).
Elevated levels significantly predicted increased risk in the 14 studies with 3,318 patients overall (OR, 3.4). However, prediction within the first year was higher (OR, 6.7) compared with studies that measured troponin more than 12 months out (OR, 1.8).
These findings could have implications for practice, because the majority of perioperative MIs are asymptomatic, Dr. Cohn said. "Maybe we should, as the authors suggest, recommend routine troponins after high-risk surgery."
More frequent vital-sign monitoring; transfer to a unit with additional monitoring; and/or screening for hypoxia and anemia could be implemented in patients identified as high risk, Dr. Cohn said. Optimization of intravascular volume and initiation of cardiac medications are additional strategies. Also, closely monitored patients who experience an MI potentially could be transferred for cardiac catheterization or revascularization more quickly.
"It is thought provoking that we can change the management," Dr. Cohn said.
• HF, AF, and Cardiovascular Risk. Heart failure and atrial fibrillation should factor more prominently into cardiovascular risk stratification prior to noncardiac surgery, according to a population-based cohort study of more than 38,000 consecutive patients (Circulation 2011:124:289-96).
"There are many cardiovascular risk stratification tools available with quite a bit of variation. Coronary artery disease [CAD] is typically weighted heavily on most models," said Dr. Grant, director of perioperative and consultative medicine and member of the medicine faculty at the University of Michigan in Ann Arbor.
However, researchers found that ischemic and nonischemic heart failure and atrial fibrillation were more commonly associated with 30-day mortality and readmission rates than CAD in this large cohort, Dr. Grant said. The authors concluded that these risk factors are likely underestimated in current prediction models.
• Liberal vs. Conservative Blood Transfusion. "The hemoglobin level at which we decide to transfuse patients after surgery is controversial," Dr. Grant said, "and has not been adequately studied to date. Great variations in practice exist."
A randomized controlled trial of 2,016 hip fracture surgery patients found no significant difference between liberal and conservative postoperative blood transfusion policies in terms of mortality or ability to walk independently at 60 days for patients at high cardiovascular risk (N. Engl. J. Med. 2011;365:2453-62).
The liberal policy allowed transfusions to maintain hemoglobin at 10 g/dL. In contrast, patients randomized to a conservative approach could only be transfused if they had symptoms of anemia or at the physician’s discretion once hemoglobin was below 8 g/dL.
"Implications for practice, from my point of view, include some more evidence that maybe using more of a restrictive transfusion practice may be reasonable, including for higher-risk populations," Dr. Grant said. However, "red-cell transfusion practices still need to be individualized for your perioperative patient."
Dr. Smetana, Dr. Cohn, and Dr. Grant had no relevant financial disclosures.
MIAMI BEACH – What do the timing of smoking cessation prior to surgery, reliable prediction of postoperative respiratory failure, and biomarkers that point to elevated postoperative myocardial infarction risk have in common? They emerged as some of the most prominent findings published in the past year, according to three experts in hospital medicine.
Dr. Gerald W. Smetana, Dr. Steven L. Cohn, and Dr. Paul J. Grant each selected studies of particular relevance to hospitalists and explained why during a panel presentation at a meeting on perioperative medicine sponsored by the University of Miami:
• Preoperative Smoking Cessation. When a patient stops smoking up to 8 weeks before noncardiac surgery, it does not significantly change the total or pulmonary complication rates, according to a systematic literature review (Arch. Intern. Med. 2011;171:983-9).
"Many patients who quit smoking report they feel worse before they feel better," said Dr. Smetana, an attending in the general medicine division at Beth Israel Deaconess Medical Center, Boston.
Increased cough and sputum production are common right after quitting, he said. "This could be a plausible mechanism to explain why recent quitters might be at increased risk for postoperative pulmonary complications."
However, there was no statistically significant difference in total complications (relative risk of 0.78 for recent quitters, compared with a reference value of 1.0 for current smokers) in the nine eligible studies with 889 participants. Five of the trials assessed pulmonary complications, and found that recent quitters had a nonsignificant increased risk (RR, 1.18) compared with patients who continued to smoke.
Until there is consensus based on large randomized trials, stopping smoking before surgery can be considered safe, said Dr. Smetana, who is also on the medicine faculty at Harvard Medical School. In addition, longer periods of cessation are likely better than shorter ones. He added that despite the lack of a significant finding, it is still worthwhile to counsel patients because any time before surgery is a still a teachable moment for smoking cessation.
• Predicting Postoperative Pulmonary Failure. Type of procedure, emergency surgery, poor dependent functional status, sepsis, and higher American Society of Anesthesiologists classification were the five independent preoperative factors that significantly predicted postoperative respiratory failure in a multicenter database study (Chest 2011;140:1207-15).
The study included 211,410 participants undergoing all types of surgery. Mortality was 26% among those with postoperative respiratory failure, compared with 1% for unaffected patients. "This shows how important pulmonary complications can be," Dr. Smetana said.
The researchers incorporated these five predictors into a surgical risk calculator that is downloadable for free.
Dr. Smetana said, "It is a nice tool that ... helps to stratify patients. It makes a difference in identifying which patients for which you will pull out all the stops."
• Preoperative Peptide Gauges Risk. Although multiple researchers have looked at preoperative B-type natriuretic peptide (BNP) as a predictor of postoperative cardiac events or death, there remain "a lot of unknowns for BNP at this point," said Dr. Cohn, director of the University of Miami Hospital Medical Consultation Service and professor of medicine at the University of Miami.
A recent meta-analysis may shed some light on the predictive value of BNP (J. Am. Coll. Cardiol. 2011;58:522-9). Investigators assessed five BNP studies with 632 patients to determine cutoff values for screening (high sensitivity) and diagnosis (high specificity), and an optimal value that combines both.
The researchers found that patients with BNP above the optimal cutoff point of 116 pg/mL had a significantly elevated risk for the composite outcome of nonfatal myocardial infarction or cardiovascular death (unadjusted odds ratio, 7.36). Compared with use of the Revised Cardiac Risk Index, the optimal BNP cutoff classification improved risk prediction by 58%. This means some patients moved to a more accurate ranking among the low-, intermediate- and high-risk categories, Dr. Cohn said.
• Troponin and Postoperative MI Risk. Myocardial infarction is the most common major, perioperative vascular complication, so investigators continue to search for an accurate way to identify high-risk patients. Some propose elevated serum levels of the protein troponin as a predictor, Dr. Cohn said, but the question remains: Would it change patient management and improve outcomes?
Researchers found that increased troponin after noncardiac surgery did in fact independently predict postoperative MI mortality in a meta-analysis (Anesthesiology 2011;114:796-806).
Elevated levels significantly predicted increased risk in the 14 studies with 3,318 patients overall (OR, 3.4). However, prediction within the first year was higher (OR, 6.7) compared with studies that measured troponin more than 12 months out (OR, 1.8).
These findings could have implications for practice, because the majority of perioperative MIs are asymptomatic, Dr. Cohn said. "Maybe we should, as the authors suggest, recommend routine troponins after high-risk surgery."
More frequent vital-sign monitoring; transfer to a unit with additional monitoring; and/or screening for hypoxia and anemia could be implemented in patients identified as high risk, Dr. Cohn said. Optimization of intravascular volume and initiation of cardiac medications are additional strategies. Also, closely monitored patients who experience an MI potentially could be transferred for cardiac catheterization or revascularization more quickly.
"It is thought provoking that we can change the management," Dr. Cohn said.
• HF, AF, and Cardiovascular Risk. Heart failure and atrial fibrillation should factor more prominently into cardiovascular risk stratification prior to noncardiac surgery, according to a population-based cohort study of more than 38,000 consecutive patients (Circulation 2011:124:289-96).
"There are many cardiovascular risk stratification tools available with quite a bit of variation. Coronary artery disease [CAD] is typically weighted heavily on most models," said Dr. Grant, director of perioperative and consultative medicine and member of the medicine faculty at the University of Michigan in Ann Arbor.
However, researchers found that ischemic and nonischemic heart failure and atrial fibrillation were more commonly associated with 30-day mortality and readmission rates than CAD in this large cohort, Dr. Grant said. The authors concluded that these risk factors are likely underestimated in current prediction models.
• Liberal vs. Conservative Blood Transfusion. "The hemoglobin level at which we decide to transfuse patients after surgery is controversial," Dr. Grant said, "and has not been adequately studied to date. Great variations in practice exist."
A randomized controlled trial of 2,016 hip fracture surgery patients found no significant difference between liberal and conservative postoperative blood transfusion policies in terms of mortality or ability to walk independently at 60 days for patients at high cardiovascular risk (N. Engl. J. Med. 2011;365:2453-62).
The liberal policy allowed transfusions to maintain hemoglobin at 10 g/dL. In contrast, patients randomized to a conservative approach could only be transfused if they had symptoms of anemia or at the physician’s discretion once hemoglobin was below 8 g/dL.
"Implications for practice, from my point of view, include some more evidence that maybe using more of a restrictive transfusion practice may be reasonable, including for higher-risk populations," Dr. Grant said. However, "red-cell transfusion practices still need to be individualized for your perioperative patient."
Dr. Smetana, Dr. Cohn, and Dr. Grant had no relevant financial disclosures.
EXPERT ANALYSIS FROM A MEETING ON PERIOPERATIVE MEDICINE SPONSORED BY THE UNIVERSITY OF MIAMI