User login
Thirteen Steps Advised to Prevent Delirium in Hospitalized Patients
Delirium is common but underrecognized in hospitalized patients, "a neglected condition relative to its frequency and serious consequences," and approximately one-third of cases are preventable, according to a report in the June 7 Annals of Internal Medicine.
The United Kingdom’s National Institute for Health and Clinical Excellence (NICE) has released a new clinical guideline for preventing delirium, which lists 13 recommendations that "could probably be easily accommodated in current care without incurring high costs." On the contrary, preventing delirium in hospitalized patients is expected to markedly cut health care costs, as well as to improve quality-adjusted life-year gains, compared with usual care, said Rachel O’Mahony, Ph.D., of the National Clinical Guideline Centre at the Royal College of Physicians, London, and her associates.
A multidisciplinary group of experts, including physicians, psychiatrists, specialist nurses, a home care manager, and patient representatives, reviewed the literature to find which prevention strategies were effective to compile the guidelines.
No single intervention was identified that significantly reduced hospital stay, placement in long-term care facilities, mortality, or duration or severity of delirium. Instead, multicomponent interventions provided the strongest evidence of improving these factors.
The recommendations include:
- Avoid changes in patient surroundings to prevent confusion and disorientation. This includes avoiding unnecessary room changes as well as changes in the personnel who provide care.
"Several moves within an acute care hospital are now common ... [from] emergency department to assessment unit to acute care ward and sometimes to post-acute care ward.
"Moving could make it difficult for a sick person on the brink of a delirium episode to maintain his or her orientation and contact with reality," Dr. O’Mahony and her colleagues said (Ann. Intern. Med. 2011;154:746-51).
- Provide appropriate lighting, clear signage, an easily visible 24-hour clock (to distinguish day from night in rooms without windows), and a calendar to help patients stay oriented to time and place.
- Reorient patients by explaining where they are and what your role is.
- Provide cognitively stimulating activities, such as encouraging patients to reminisce and facilitating visits from family and friends.
- Address dehydration and constipation, with intravenous fluids, if necessary, and manage fluid balance in patients with relevant comorbidities such as heart failure or kidney disease.
- Assess for hypoxia and optimize oxygen saturation.
- Actively assess for infection and treat it; employ infection-control procedures; and avoid unnecessary catheterization.
The presence of a bladder catheter is a known risk factor for delirium, the researchers noted.
- Address immobility by encouraging patients to walk as soon as possible, providing appropriate walking aids and ensuring they are available at all times, and encouraging range-of-motion exercises.
- Assess for pain, attending to nonverbal signs of pain, and manage it.
Although some clinicians are leery of inducing confusion by providing painkillers, pain itself is an independent risk factor for delirium, the investigators said.
- Review both the type and the number of medications.
- Address poor nutrition, and make sure that dentures fit properly in patients who have them.
- Address sensory impairment and resolve any reversible causes such as impacted ear wax or need for visual or hearing aids. Ensure such aids are in good working order.
- Promote good sleep patterns by avoiding procedures and minimizing ambient noise during sleeping hours.
"Some of these components are provided to some patients some of the time, but prevention of delirium requires that we do all of these things all the time to all of the patients who are at risk," Dr. O’Mahony and her associates said.
"It makes sense" to target these interventions to patients at highest risk of developing delirium. There are four such easy-to-identify groups, each with a greater than fivefold increase in risk for delirium: patients aged 65 [years] and older, patients with preexisting cognitive impairment, patients with severe illness, and patients with hip fracture, they noted.
"This enhanced approach goes beyond well-trained and prepared staff. It requires a health care system ... that supports comprehensive and reliable delivery of specific tasks," they researchers added.
The guideline was supported by the National Clinical Guideline Centre at the Royal College of Physicians; the U.K. Cochrane Centre and KSG-Trans; and the Bradford Institute for Health Research. None of the authors reported having any relevant conflicts of interest.
The full version of the guideline, including details about the methods used in its development, is available online. A synopsis is available at Annals of Internal Medicine.
Clinical guidelines should bring order to the dizzying array of diagnostic and therapeutic options facing physicians, but too often, the thousands of such guidelines published by "hundreds of groups in dozens of countries" instead can make the "chaos" even worse, according to Dr. Christine Laine, Dr. Darren B. Taichman, and Dr. Cynthia Mulrow.
The American College of Physicians has always presented summaries of the high-quality guidelines compiled by themselves and by the U.S. Preventive Services Task Force, and the organization now seeks "to publish thoughtful synopses of guidelines initially released in other venues but whose topics are highly relevant to the practice of internal medicine and its subspecialties.
"As the first example of this new venture," the ACP presents a synopsis of the NICE guideline for preventing delirium, because the methods for developing it came so close to meeting the Institute of Medicine’s "rigorous definition of trustworthy."
"We urge readers to gain familiarity with the IOM standards and consider them as they use guidelines to navigate the maze of available clinical choices," the editors noted.
Christine Laine, M.D., is editor in chief of the Annals of Internal Medicine, senior vice president of the American College of Physicians, and an internist at Jefferson Medical College, all in Philadelphia. Darren B. Taichman, M.D., Ph.D., is executive deputy editor of the Annals and director of the medical ICU at the University of Pennsylvania Medical Center, Philadelphia. Cynthia Mulrow, M.D., is senior deputy editor of the Annals. These remarks were taken from their editorial accompanying the NICE guideline (Ann. Intern. Med. 2011;154:774-5). No potential conflicts of interest were disclosed.
Clinical guidelines should bring order to the dizzying array of diagnostic and therapeutic options facing physicians, but too often, the thousands of such guidelines published by "hundreds of groups in dozens of countries" instead can make the "chaos" even worse, according to Dr. Christine Laine, Dr. Darren B. Taichman, and Dr. Cynthia Mulrow.
The American College of Physicians has always presented summaries of the high-quality guidelines compiled by themselves and by the U.S. Preventive Services Task Force, and the organization now seeks "to publish thoughtful synopses of guidelines initially released in other venues but whose topics are highly relevant to the practice of internal medicine and its subspecialties.
"As the first example of this new venture," the ACP presents a synopsis of the NICE guideline for preventing delirium, because the methods for developing it came so close to meeting the Institute of Medicine’s "rigorous definition of trustworthy."
"We urge readers to gain familiarity with the IOM standards and consider them as they use guidelines to navigate the maze of available clinical choices," the editors noted.
Christine Laine, M.D., is editor in chief of the Annals of Internal Medicine, senior vice president of the American College of Physicians, and an internist at Jefferson Medical College, all in Philadelphia. Darren B. Taichman, M.D., Ph.D., is executive deputy editor of the Annals and director of the medical ICU at the University of Pennsylvania Medical Center, Philadelphia. Cynthia Mulrow, M.D., is senior deputy editor of the Annals. These remarks were taken from their editorial accompanying the NICE guideline (Ann. Intern. Med. 2011;154:774-5). No potential conflicts of interest were disclosed.
Clinical guidelines should bring order to the dizzying array of diagnostic and therapeutic options facing physicians, but too often, the thousands of such guidelines published by "hundreds of groups in dozens of countries" instead can make the "chaos" even worse, according to Dr. Christine Laine, Dr. Darren B. Taichman, and Dr. Cynthia Mulrow.
The American College of Physicians has always presented summaries of the high-quality guidelines compiled by themselves and by the U.S. Preventive Services Task Force, and the organization now seeks "to publish thoughtful synopses of guidelines initially released in other venues but whose topics are highly relevant to the practice of internal medicine and its subspecialties.
"As the first example of this new venture," the ACP presents a synopsis of the NICE guideline for preventing delirium, because the methods for developing it came so close to meeting the Institute of Medicine’s "rigorous definition of trustworthy."
"We urge readers to gain familiarity with the IOM standards and consider them as they use guidelines to navigate the maze of available clinical choices," the editors noted.
Christine Laine, M.D., is editor in chief of the Annals of Internal Medicine, senior vice president of the American College of Physicians, and an internist at Jefferson Medical College, all in Philadelphia. Darren B. Taichman, M.D., Ph.D., is executive deputy editor of the Annals and director of the medical ICU at the University of Pennsylvania Medical Center, Philadelphia. Cynthia Mulrow, M.D., is senior deputy editor of the Annals. These remarks were taken from their editorial accompanying the NICE guideline (Ann. Intern. Med. 2011;154:774-5). No potential conflicts of interest were disclosed.
Delirium is common but underrecognized in hospitalized patients, "a neglected condition relative to its frequency and serious consequences," and approximately one-third of cases are preventable, according to a report in the June 7 Annals of Internal Medicine.
The United Kingdom’s National Institute for Health and Clinical Excellence (NICE) has released a new clinical guideline for preventing delirium, which lists 13 recommendations that "could probably be easily accommodated in current care without incurring high costs." On the contrary, preventing delirium in hospitalized patients is expected to markedly cut health care costs, as well as to improve quality-adjusted life-year gains, compared with usual care, said Rachel O’Mahony, Ph.D., of the National Clinical Guideline Centre at the Royal College of Physicians, London, and her associates.
A multidisciplinary group of experts, including physicians, psychiatrists, specialist nurses, a home care manager, and patient representatives, reviewed the literature to find which prevention strategies were effective to compile the guidelines.
No single intervention was identified that significantly reduced hospital stay, placement in long-term care facilities, mortality, or duration or severity of delirium. Instead, multicomponent interventions provided the strongest evidence of improving these factors.
The recommendations include:
- Avoid changes in patient surroundings to prevent confusion and disorientation. This includes avoiding unnecessary room changes as well as changes in the personnel who provide care.
"Several moves within an acute care hospital are now common ... [from] emergency department to assessment unit to acute care ward and sometimes to post-acute care ward.
"Moving could make it difficult for a sick person on the brink of a delirium episode to maintain his or her orientation and contact with reality," Dr. O’Mahony and her colleagues said (Ann. Intern. Med. 2011;154:746-51).
- Provide appropriate lighting, clear signage, an easily visible 24-hour clock (to distinguish day from night in rooms without windows), and a calendar to help patients stay oriented to time and place.
- Reorient patients by explaining where they are and what your role is.
- Provide cognitively stimulating activities, such as encouraging patients to reminisce and facilitating visits from family and friends.
- Address dehydration and constipation, with intravenous fluids, if necessary, and manage fluid balance in patients with relevant comorbidities such as heart failure or kidney disease.
- Assess for hypoxia and optimize oxygen saturation.
- Actively assess for infection and treat it; employ infection-control procedures; and avoid unnecessary catheterization.
The presence of a bladder catheter is a known risk factor for delirium, the researchers noted.
- Address immobility by encouraging patients to walk as soon as possible, providing appropriate walking aids and ensuring they are available at all times, and encouraging range-of-motion exercises.
- Assess for pain, attending to nonverbal signs of pain, and manage it.
Although some clinicians are leery of inducing confusion by providing painkillers, pain itself is an independent risk factor for delirium, the investigators said.
- Review both the type and the number of medications.
- Address poor nutrition, and make sure that dentures fit properly in patients who have them.
- Address sensory impairment and resolve any reversible causes such as impacted ear wax or need for visual or hearing aids. Ensure such aids are in good working order.
- Promote good sleep patterns by avoiding procedures and minimizing ambient noise during sleeping hours.
"Some of these components are provided to some patients some of the time, but prevention of delirium requires that we do all of these things all the time to all of the patients who are at risk," Dr. O’Mahony and her associates said.
"It makes sense" to target these interventions to patients at highest risk of developing delirium. There are four such easy-to-identify groups, each with a greater than fivefold increase in risk for delirium: patients aged 65 [years] and older, patients with preexisting cognitive impairment, patients with severe illness, and patients with hip fracture, they noted.
"This enhanced approach goes beyond well-trained and prepared staff. It requires a health care system ... that supports comprehensive and reliable delivery of specific tasks," they researchers added.
The guideline was supported by the National Clinical Guideline Centre at the Royal College of Physicians; the U.K. Cochrane Centre and KSG-Trans; and the Bradford Institute for Health Research. None of the authors reported having any relevant conflicts of interest.
The full version of the guideline, including details about the methods used in its development, is available online. A synopsis is available at Annals of Internal Medicine.
Delirium is common but underrecognized in hospitalized patients, "a neglected condition relative to its frequency and serious consequences," and approximately one-third of cases are preventable, according to a report in the June 7 Annals of Internal Medicine.
The United Kingdom’s National Institute for Health and Clinical Excellence (NICE) has released a new clinical guideline for preventing delirium, which lists 13 recommendations that "could probably be easily accommodated in current care without incurring high costs." On the contrary, preventing delirium in hospitalized patients is expected to markedly cut health care costs, as well as to improve quality-adjusted life-year gains, compared with usual care, said Rachel O’Mahony, Ph.D., of the National Clinical Guideline Centre at the Royal College of Physicians, London, and her associates.
A multidisciplinary group of experts, including physicians, psychiatrists, specialist nurses, a home care manager, and patient representatives, reviewed the literature to find which prevention strategies were effective to compile the guidelines.
No single intervention was identified that significantly reduced hospital stay, placement in long-term care facilities, mortality, or duration or severity of delirium. Instead, multicomponent interventions provided the strongest evidence of improving these factors.
The recommendations include:
- Avoid changes in patient surroundings to prevent confusion and disorientation. This includes avoiding unnecessary room changes as well as changes in the personnel who provide care.
"Several moves within an acute care hospital are now common ... [from] emergency department to assessment unit to acute care ward and sometimes to post-acute care ward.
"Moving could make it difficult for a sick person on the brink of a delirium episode to maintain his or her orientation and contact with reality," Dr. O’Mahony and her colleagues said (Ann. Intern. Med. 2011;154:746-51).
- Provide appropriate lighting, clear signage, an easily visible 24-hour clock (to distinguish day from night in rooms without windows), and a calendar to help patients stay oriented to time and place.
- Reorient patients by explaining where they are and what your role is.
- Provide cognitively stimulating activities, such as encouraging patients to reminisce and facilitating visits from family and friends.
- Address dehydration and constipation, with intravenous fluids, if necessary, and manage fluid balance in patients with relevant comorbidities such as heart failure or kidney disease.
- Assess for hypoxia and optimize oxygen saturation.
- Actively assess for infection and treat it; employ infection-control procedures; and avoid unnecessary catheterization.
The presence of a bladder catheter is a known risk factor for delirium, the researchers noted.
- Address immobility by encouraging patients to walk as soon as possible, providing appropriate walking aids and ensuring they are available at all times, and encouraging range-of-motion exercises.
- Assess for pain, attending to nonverbal signs of pain, and manage it.
Although some clinicians are leery of inducing confusion by providing painkillers, pain itself is an independent risk factor for delirium, the investigators said.
- Review both the type and the number of medications.
- Address poor nutrition, and make sure that dentures fit properly in patients who have them.
- Address sensory impairment and resolve any reversible causes such as impacted ear wax or need for visual or hearing aids. Ensure such aids are in good working order.
- Promote good sleep patterns by avoiding procedures and minimizing ambient noise during sleeping hours.
"Some of these components are provided to some patients some of the time, but prevention of delirium requires that we do all of these things all the time to all of the patients who are at risk," Dr. O’Mahony and her associates said.
"It makes sense" to target these interventions to patients at highest risk of developing delirium. There are four such easy-to-identify groups, each with a greater than fivefold increase in risk for delirium: patients aged 65 [years] and older, patients with preexisting cognitive impairment, patients with severe illness, and patients with hip fracture, they noted.
"This enhanced approach goes beyond well-trained and prepared staff. It requires a health care system ... that supports comprehensive and reliable delivery of specific tasks," they researchers added.
The guideline was supported by the National Clinical Guideline Centre at the Royal College of Physicians; the U.K. Cochrane Centre and KSG-Trans; and the Bradford Institute for Health Research. None of the authors reported having any relevant conflicts of interest.
The full version of the guideline, including details about the methods used in its development, is available online. A synopsis is available at Annals of Internal Medicine.
FROM THE ANNALS OF INTERNAL MEDICINE
Data Analysis Favors Laparoscopic Abdominal Wall Hernia Repair
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The 0.18% mortality rate in the group having laparoscopic abdominal wall hernia repair was roughly half the 0.33% mortality rate in patients undergoing open repair. Complication and morbidity rates were also lower in the laparoscopic group.
Data Source: Database analysis of 71,026 patients.
Disclosures: Dr. Mason declared having no financial conflicts.
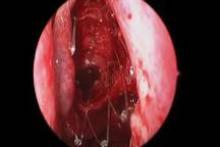
Intranasal Postop Steroids Same as Saline in Select Patients
CHICAGO – Intranasal steroids were as good as saline alone as postoperative care in a randomized, double-blinded study of patients with chronic rhinosinusitis and Samter’s triad.
There was no difference in disease recurrence rate, complications, or quality of life at 6 months and 1-year postoperative using intranasal saline, saline plus budesonide, or saline and budesonide combined.
The surprising finding runs contrary to general practice and has several implications including how best to counsel patients for postoperative care, lead author Dr. Brian Rotenberg said at the Combined Otolaryngology Spring Meetings.
"If nasal steroids as done in this population don’t confer any additional benefit postoperatively, should we still prescribe them?" he asked. "Should we be prescribing something different or perhaps nothing at all? Is there a potential plus side here in terms of health-care cost savings?"
During a discussion of the study, an attendee expressed concern that insurers would interpret the results too broadly and deny coverage of postoperative nasal steroids for all patients with rhinosinusitis and polyposis, and not just those with Samter’s triad, a condition consisting of asthma, aspirin sensitivity, and nasal polyposis.
Another attendee agreed that nasal steroids are not potent enough in this population and said a pulse course of oral steroids 60 mg for 4 days can knock down symptoms in 80% of those with recurrence and be maintained with topical steroids. In the absence of a federally approved product for nasal use, he also suggested that dexamethasone eye drops can be effective.
Dr. Rotenberg replied that all patients received 3 weeks of postoperative oral prednisone, but that pulse-dosing of steroids was limited to one patient with early recurrence.
The 60 patients in the analysis had failed medical management for chronic rhinosinusitis with nasal polyposis and had a minimum preoperative Lund-Kennedy score of 8 out of 12. Nineteen patients were randomized to saline, 21 to saline plus budesonide, and 20 to saline/budesonide combination. Their mean Lund-Mackay scores were 20.6, 19.9, and 20.5, respectively.
Exclusion criteria included revision functional endoscopic sinus surgery, use of corticosteroids for other medical conditions, smoking, and concurrent disease with steroid contraindication.
At 6 months postoperatively, there were no significant differences between the saline, saline plus budesonide, and saline/budesonide combination groups with regard to Lund-Kennedy scores (1.5, 0.9, and 1.2, respectively), adrenocorticotropic hormone (ACTH) ranges (all normal), and intraocular pressure (12.4, 12.9, and 13.9 mm Hg, respectively), said Dr. Rotenberg of the University of Western Ontario in London, Ontario. Quality of life as assessed using the 21-item Sino-Nasal Outcome Test (SNOT-21) was also similar at a mean of 29.7, 27.4 and 28.2, respectively.
At 1 year of follow-up, once again there were no significant differences between the saline, saline plus budesonide, and saline/budesonide groups in Lund-Kennedy scores (3.7, 4.4, and 4.1, respectively), Lund-Mackay scores (11.8, 12.7, and 13.4, respectively), SNOT-21 scores (42.5, 47.9, and 42.2, respectively), intraocular pressure (13.1, 13.4,and 12.9 mm Hg, respectively). ACTH ranges were all normal.
A within-group analysis showed a significant improvement in all outcomes from baseline to 6 months, and a general worsening of outcomes at 1 year compared with the first 6 months, although they were still improved over baseline, Dr. Rotenberg said.
He pointed out that the literature is lacking in evidence guiding the postoperative management of patients with chronic rhinosinusitis with nasal polyps undergoing surgery. One study reported that steroid nasal spray did not influence polyp recurrence rate after surgery (Clin. Exp. Allergy. 2004;34:1395-400), while another showed that normal and buffered hypertonic saline nasal sprays had no beneficial effect on postoperative symptoms compared with no treatment (Am. J. Rhinol. 2006;20:191-6).
Dr. Rotenberg reported no relevant financial disclosures.
Session moderator Dr. Brent A. Senior said in an interview that the study was well designed and sufficiently powered, but would have been strengthened by the inclusion of a nontreatment group and more information on oral medications, as they can have a significant impact on disease. Follow-up to 18 months also would be useful, as the endoscopic appearance of the nasal cavity at 18 months has been shown to be predictive of how patients will do years after surgery.
"This is a good study, but not a game changer," he said, adding that additional work is needed to confirm the findings.
Dr. Senior is chief of rhinology, allergy and sinus surgery at the University of North Carolina at Chapel Hill.
rhinosinusitis and polyposis, dexamethasone eye drops,
Session moderator Dr. Brent A. Senior said in an interview that the study was well designed and sufficiently powered, but would have been strengthened by the inclusion of a nontreatment group and more information on oral medications, as they can have a significant impact on disease. Follow-up to 18 months also would be useful, as the endoscopic appearance of the nasal cavity at 18 months has been shown to be predictive of how patients will do years after surgery.
"This is a good study, but not a game changer," he said, adding that additional work is needed to confirm the findings.
Dr. Senior is chief of rhinology, allergy and sinus surgery at the University of North Carolina at Chapel Hill.
Session moderator Dr. Brent A. Senior said in an interview that the study was well designed and sufficiently powered, but would have been strengthened by the inclusion of a nontreatment group and more information on oral medications, as they can have a significant impact on disease. Follow-up to 18 months also would be useful, as the endoscopic appearance of the nasal cavity at 18 months has been shown to be predictive of how patients will do years after surgery.
"This is a good study, but not a game changer," he said, adding that additional work is needed to confirm the findings.
Dr. Senior is chief of rhinology, allergy and sinus surgery at the University of North Carolina at Chapel Hill.
CHICAGO – Intranasal steroids were as good as saline alone as postoperative care in a randomized, double-blinded study of patients with chronic rhinosinusitis and Samter’s triad.
There was no difference in disease recurrence rate, complications, or quality of life at 6 months and 1-year postoperative using intranasal saline, saline plus budesonide, or saline and budesonide combined.
The surprising finding runs contrary to general practice and has several implications including how best to counsel patients for postoperative care, lead author Dr. Brian Rotenberg said at the Combined Otolaryngology Spring Meetings.
"If nasal steroids as done in this population don’t confer any additional benefit postoperatively, should we still prescribe them?" he asked. "Should we be prescribing something different or perhaps nothing at all? Is there a potential plus side here in terms of health-care cost savings?"
During a discussion of the study, an attendee expressed concern that insurers would interpret the results too broadly and deny coverage of postoperative nasal steroids for all patients with rhinosinusitis and polyposis, and not just those with Samter’s triad, a condition consisting of asthma, aspirin sensitivity, and nasal polyposis.
Another attendee agreed that nasal steroids are not potent enough in this population and said a pulse course of oral steroids 60 mg for 4 days can knock down symptoms in 80% of those with recurrence and be maintained with topical steroids. In the absence of a federally approved product for nasal use, he also suggested that dexamethasone eye drops can be effective.
Dr. Rotenberg replied that all patients received 3 weeks of postoperative oral prednisone, but that pulse-dosing of steroids was limited to one patient with early recurrence.
The 60 patients in the analysis had failed medical management for chronic rhinosinusitis with nasal polyposis and had a minimum preoperative Lund-Kennedy score of 8 out of 12. Nineteen patients were randomized to saline, 21 to saline plus budesonide, and 20 to saline/budesonide combination. Their mean Lund-Mackay scores were 20.6, 19.9, and 20.5, respectively.
Exclusion criteria included revision functional endoscopic sinus surgery, use of corticosteroids for other medical conditions, smoking, and concurrent disease with steroid contraindication.
At 6 months postoperatively, there were no significant differences between the saline, saline plus budesonide, and saline/budesonide combination groups with regard to Lund-Kennedy scores (1.5, 0.9, and 1.2, respectively), adrenocorticotropic hormone (ACTH) ranges (all normal), and intraocular pressure (12.4, 12.9, and 13.9 mm Hg, respectively), said Dr. Rotenberg of the University of Western Ontario in London, Ontario. Quality of life as assessed using the 21-item Sino-Nasal Outcome Test (SNOT-21) was also similar at a mean of 29.7, 27.4 and 28.2, respectively.
At 1 year of follow-up, once again there were no significant differences between the saline, saline plus budesonide, and saline/budesonide groups in Lund-Kennedy scores (3.7, 4.4, and 4.1, respectively), Lund-Mackay scores (11.8, 12.7, and 13.4, respectively), SNOT-21 scores (42.5, 47.9, and 42.2, respectively), intraocular pressure (13.1, 13.4,and 12.9 mm Hg, respectively). ACTH ranges were all normal.
A within-group analysis showed a significant improvement in all outcomes from baseline to 6 months, and a general worsening of outcomes at 1 year compared with the first 6 months, although they were still improved over baseline, Dr. Rotenberg said.
He pointed out that the literature is lacking in evidence guiding the postoperative management of patients with chronic rhinosinusitis with nasal polyps undergoing surgery. One study reported that steroid nasal spray did not influence polyp recurrence rate after surgery (Clin. Exp. Allergy. 2004;34:1395-400), while another showed that normal and buffered hypertonic saline nasal sprays had no beneficial effect on postoperative symptoms compared with no treatment (Am. J. Rhinol. 2006;20:191-6).
Dr. Rotenberg reported no relevant financial disclosures.
CHICAGO – Intranasal steroids were as good as saline alone as postoperative care in a randomized, double-blinded study of patients with chronic rhinosinusitis and Samter’s triad.
There was no difference in disease recurrence rate, complications, or quality of life at 6 months and 1-year postoperative using intranasal saline, saline plus budesonide, or saline and budesonide combined.
The surprising finding runs contrary to general practice and has several implications including how best to counsel patients for postoperative care, lead author Dr. Brian Rotenberg said at the Combined Otolaryngology Spring Meetings.
"If nasal steroids as done in this population don’t confer any additional benefit postoperatively, should we still prescribe them?" he asked. "Should we be prescribing something different or perhaps nothing at all? Is there a potential plus side here in terms of health-care cost savings?"
During a discussion of the study, an attendee expressed concern that insurers would interpret the results too broadly and deny coverage of postoperative nasal steroids for all patients with rhinosinusitis and polyposis, and not just those with Samter’s triad, a condition consisting of asthma, aspirin sensitivity, and nasal polyposis.
Another attendee agreed that nasal steroids are not potent enough in this population and said a pulse course of oral steroids 60 mg for 4 days can knock down symptoms in 80% of those with recurrence and be maintained with topical steroids. In the absence of a federally approved product for nasal use, he also suggested that dexamethasone eye drops can be effective.
Dr. Rotenberg replied that all patients received 3 weeks of postoperative oral prednisone, but that pulse-dosing of steroids was limited to one patient with early recurrence.
The 60 patients in the analysis had failed medical management for chronic rhinosinusitis with nasal polyposis and had a minimum preoperative Lund-Kennedy score of 8 out of 12. Nineteen patients were randomized to saline, 21 to saline plus budesonide, and 20 to saline/budesonide combination. Their mean Lund-Mackay scores were 20.6, 19.9, and 20.5, respectively.
Exclusion criteria included revision functional endoscopic sinus surgery, use of corticosteroids for other medical conditions, smoking, and concurrent disease with steroid contraindication.
At 6 months postoperatively, there were no significant differences between the saline, saline plus budesonide, and saline/budesonide combination groups with regard to Lund-Kennedy scores (1.5, 0.9, and 1.2, respectively), adrenocorticotropic hormone (ACTH) ranges (all normal), and intraocular pressure (12.4, 12.9, and 13.9 mm Hg, respectively), said Dr. Rotenberg of the University of Western Ontario in London, Ontario. Quality of life as assessed using the 21-item Sino-Nasal Outcome Test (SNOT-21) was also similar at a mean of 29.7, 27.4 and 28.2, respectively.
At 1 year of follow-up, once again there were no significant differences between the saline, saline plus budesonide, and saline/budesonide groups in Lund-Kennedy scores (3.7, 4.4, and 4.1, respectively), Lund-Mackay scores (11.8, 12.7, and 13.4, respectively), SNOT-21 scores (42.5, 47.9, and 42.2, respectively), intraocular pressure (13.1, 13.4,and 12.9 mm Hg, respectively). ACTH ranges were all normal.
A within-group analysis showed a significant improvement in all outcomes from baseline to 6 months, and a general worsening of outcomes at 1 year compared with the first 6 months, although they were still improved over baseline, Dr. Rotenberg said.
He pointed out that the literature is lacking in evidence guiding the postoperative management of patients with chronic rhinosinusitis with nasal polyps undergoing surgery. One study reported that steroid nasal spray did not influence polyp recurrence rate after surgery (Clin. Exp. Allergy. 2004;34:1395-400), while another showed that normal and buffered hypertonic saline nasal sprays had no beneficial effect on postoperative symptoms compared with no treatment (Am. J. Rhinol. 2006;20:191-6).
Dr. Rotenberg reported no relevant financial disclosures.
rhinosinusitis and polyposis, dexamethasone eye drops,
rhinosinusitis and polyposis, dexamethasone eye drops,
FROM THE COMBINED OTOLARYNGOLOGY SPRING MEETINGS
Bariatric Surgery Risk Scoring Tool May Predict Serious Complications
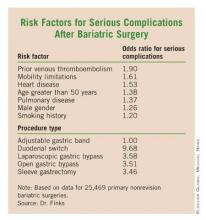
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
NSQIP Found Highly Cost Effective for Participating Hospitals
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
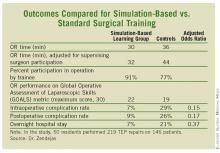
Simulator Tops Standard Training for Laparoscopic Hernia Repair
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: General surgery residents who learned laparoscopic totally extraperitoneal inguinal herniorrhaphy through a novel simulation-based training program significantly outperformed those trained in standard fashion.
Data Source: Randomized trial with 50 residents.
Disclosures: Dr. Zendejas reported having no financial conflicts.
Steroid-Eluting Sinus Stent May Minimize Postop Events
CHICAGO – A bioabsorbable steroid-eluting stent preserved sinus patency following endoscopic sinus surgery in 50 patients with chronic rhinosinusitis in a prospective, multicenter study.
The stent was associated with low rates of polyp formation, inflammation, and adhesions, despite a challenging patient population and withholding of postoperative oral and topical steroids for 30 days, lead author Dr. Keith D. Forwith said at the Combined Otolaryngology Spring Meetings.
The results were consistent across different patient populations and consistent with the pilot study in 43 patients (Int. Forum Allergy Rhinol. 2011;1:23-32).
"I think with any kind of new technique or device, the ultimate thing is how the surgeon feels about it and his or her results," he said. "What I noticed most of all when we stopped doing the study is that I missed using this device. Patients I had used it in during the study had very clean results, very easy debridements. ... We’re very pleased with the results and think it’s a promising technology."
Study sponsor Intersect ENT Inc. has submitted the investigational stent for federal review and hopes to market the device within 6-9 months.
The springlike stent maintains patency by propping open the sinus cavity and releasing mometasone furoate into the sinus lining over 30 days before being resorbed. If approved, it could provide patients with an alternative to space-filling packing materials and silicone stents, and reduce the use of systemic steroids.
The current study involved 50 adults from seven centers with chronic rhinosinusitis for at least 8 consecutive weeks that was confirmed by CT scan (mean CT stage, 11.2). Antibiotics could be prescribed per physician standard of care, and saline irrigation was permitted postoperatively as needed. Polyps were present in 66% of patients, and 28% had undergone a prior sinus procedure. Their mean age was 44 years, and 52% were male.
Ethmoidectomy and maxillary antrostomy were performed in all 50 patients, with 28 also undergoing frontal sinusotomy and 31 sphenoidotomy. Stents were placed unilaterally in 10 patients and bilaterally in 40 patients. Device placement was successful in 100% of sinuses treated, and the implants were resorbed as predicted, Dr. Forwith said. At postoperative day 30, 15% of the material remained and 0.2% remained at day 60.
Endoscopic follow-up at 1 month revealed polypoid edema in 10% of patients, significant adhesion formation in 1%, and middle turbinate lateralization in only 4.4%, said Dr. Forwith, who is in private practice in Louisville, Ky.
When patients were asked about the procedure, their mean score on the 22-question Sino-Nasal Outcome Test improved significantly from baseline through 6 months. The same was true using the Rhinosinusitis Disability Index. "We were pretty pleased that our patients liked the results of the intervention," he said.
No clinically significant changes from baseline occurred in lens opacities or intraocular pressure, which was a theoretical concern given the close proximity of the device. The patients’ mean intraocular pressure was 15 mm Hg at baseline and 14.3 mm Hg at day 30.
One patient experienced headache with sinus pressure/irritation at day 21 that was determined to be related primarily to the surgery and was exacerbated in intensity by the presence of crust on the device. The device was removed and the event resolved without sequelae by day 28.
When asked during a discussion of the study whether the drug-eluting stent resulted in any systemic complications or adrenal corticol suppression, Dr. Forwith replied that they did not specifically look at adrenal suppression, but added that the 370-mcg dose of mometasone furoate is lower than the dose patients receive with most b.i.d. nasal spray administration.
Stent maker Intersect ENT provided funding, administrative support, and materials for the study. Dr. Forwith reported no conflicts of interest.
CHICAGO – A bioabsorbable steroid-eluting stent preserved sinus patency following endoscopic sinus surgery in 50 patients with chronic rhinosinusitis in a prospective, multicenter study.
The stent was associated with low rates of polyp formation, inflammation, and adhesions, despite a challenging patient population and withholding of postoperative oral and topical steroids for 30 days, lead author Dr. Keith D. Forwith said at the Combined Otolaryngology Spring Meetings.
The results were consistent across different patient populations and consistent with the pilot study in 43 patients (Int. Forum Allergy Rhinol. 2011;1:23-32).
"I think with any kind of new technique or device, the ultimate thing is how the surgeon feels about it and his or her results," he said. "What I noticed most of all when we stopped doing the study is that I missed using this device. Patients I had used it in during the study had very clean results, very easy debridements. ... We’re very pleased with the results and think it’s a promising technology."
Study sponsor Intersect ENT Inc. has submitted the investigational stent for federal review and hopes to market the device within 6-9 months.
The springlike stent maintains patency by propping open the sinus cavity and releasing mometasone furoate into the sinus lining over 30 days before being resorbed. If approved, it could provide patients with an alternative to space-filling packing materials and silicone stents, and reduce the use of systemic steroids.
The current study involved 50 adults from seven centers with chronic rhinosinusitis for at least 8 consecutive weeks that was confirmed by CT scan (mean CT stage, 11.2). Antibiotics could be prescribed per physician standard of care, and saline irrigation was permitted postoperatively as needed. Polyps were present in 66% of patients, and 28% had undergone a prior sinus procedure. Their mean age was 44 years, and 52% were male.
Ethmoidectomy and maxillary antrostomy were performed in all 50 patients, with 28 also undergoing frontal sinusotomy and 31 sphenoidotomy. Stents were placed unilaterally in 10 patients and bilaterally in 40 patients. Device placement was successful in 100% of sinuses treated, and the implants were resorbed as predicted, Dr. Forwith said. At postoperative day 30, 15% of the material remained and 0.2% remained at day 60.
Endoscopic follow-up at 1 month revealed polypoid edema in 10% of patients, significant adhesion formation in 1%, and middle turbinate lateralization in only 4.4%, said Dr. Forwith, who is in private practice in Louisville, Ky.
When patients were asked about the procedure, their mean score on the 22-question Sino-Nasal Outcome Test improved significantly from baseline through 6 months. The same was true using the Rhinosinusitis Disability Index. "We were pretty pleased that our patients liked the results of the intervention," he said.
No clinically significant changes from baseline occurred in lens opacities or intraocular pressure, which was a theoretical concern given the close proximity of the device. The patients’ mean intraocular pressure was 15 mm Hg at baseline and 14.3 mm Hg at day 30.
One patient experienced headache with sinus pressure/irritation at day 21 that was determined to be related primarily to the surgery and was exacerbated in intensity by the presence of crust on the device. The device was removed and the event resolved without sequelae by day 28.
When asked during a discussion of the study whether the drug-eluting stent resulted in any systemic complications or adrenal corticol suppression, Dr. Forwith replied that they did not specifically look at adrenal suppression, but added that the 370-mcg dose of mometasone furoate is lower than the dose patients receive with most b.i.d. nasal spray administration.
Stent maker Intersect ENT provided funding, administrative support, and materials for the study. Dr. Forwith reported no conflicts of interest.
CHICAGO – A bioabsorbable steroid-eluting stent preserved sinus patency following endoscopic sinus surgery in 50 patients with chronic rhinosinusitis in a prospective, multicenter study.
The stent was associated with low rates of polyp formation, inflammation, and adhesions, despite a challenging patient population and withholding of postoperative oral and topical steroids for 30 days, lead author Dr. Keith D. Forwith said at the Combined Otolaryngology Spring Meetings.
The results were consistent across different patient populations and consistent with the pilot study in 43 patients (Int. Forum Allergy Rhinol. 2011;1:23-32).
"I think with any kind of new technique or device, the ultimate thing is how the surgeon feels about it and his or her results," he said. "What I noticed most of all when we stopped doing the study is that I missed using this device. Patients I had used it in during the study had very clean results, very easy debridements. ... We’re very pleased with the results and think it’s a promising technology."
Study sponsor Intersect ENT Inc. has submitted the investigational stent for federal review and hopes to market the device within 6-9 months.
The springlike stent maintains patency by propping open the sinus cavity and releasing mometasone furoate into the sinus lining over 30 days before being resorbed. If approved, it could provide patients with an alternative to space-filling packing materials and silicone stents, and reduce the use of systemic steroids.
The current study involved 50 adults from seven centers with chronic rhinosinusitis for at least 8 consecutive weeks that was confirmed by CT scan (mean CT stage, 11.2). Antibiotics could be prescribed per physician standard of care, and saline irrigation was permitted postoperatively as needed. Polyps were present in 66% of patients, and 28% had undergone a prior sinus procedure. Their mean age was 44 years, and 52% were male.
Ethmoidectomy and maxillary antrostomy were performed in all 50 patients, with 28 also undergoing frontal sinusotomy and 31 sphenoidotomy. Stents were placed unilaterally in 10 patients and bilaterally in 40 patients. Device placement was successful in 100% of sinuses treated, and the implants were resorbed as predicted, Dr. Forwith said. At postoperative day 30, 15% of the material remained and 0.2% remained at day 60.
Endoscopic follow-up at 1 month revealed polypoid edema in 10% of patients, significant adhesion formation in 1%, and middle turbinate lateralization in only 4.4%, said Dr. Forwith, who is in private practice in Louisville, Ky.
When patients were asked about the procedure, their mean score on the 22-question Sino-Nasal Outcome Test improved significantly from baseline through 6 months. The same was true using the Rhinosinusitis Disability Index. "We were pretty pleased that our patients liked the results of the intervention," he said.
No clinically significant changes from baseline occurred in lens opacities or intraocular pressure, which was a theoretical concern given the close proximity of the device. The patients’ mean intraocular pressure was 15 mm Hg at baseline and 14.3 mm Hg at day 30.
One patient experienced headache with sinus pressure/irritation at day 21 that was determined to be related primarily to the surgery and was exacerbated in intensity by the presence of crust on the device. The device was removed and the event resolved without sequelae by day 28.
When asked during a discussion of the study whether the drug-eluting stent resulted in any systemic complications or adrenal corticol suppression, Dr. Forwith replied that they did not specifically look at adrenal suppression, but added that the 370-mcg dose of mometasone furoate is lower than the dose patients receive with most b.i.d. nasal spray administration.
Stent maker Intersect ENT provided funding, administrative support, and materials for the study. Dr. Forwith reported no conflicts of interest.
FROM THE COMBINED OTOLARYNGOLOGY SPRING MEETINGS
Repair of Uncomplicated Diaphragmatic Hernia Can Avoid Worse Outcomes
PHILADELPHIA – Current clinical practice is to repair symptomatic diaphragmatic hernias to avoid complications such as obstruction or gangrene. However, practice patterns are based largely on limited data from institutional case series, according to Dr. Subroto Paul and his colleagues at Cornell University in New York.
Mortality was significantly higher in patients with uncomplicated hernia who went on to readmission with obstruction or gangrene, Dr. Paul said at the annual meeting of the American Association for Thoracic Surgery, where he presented an analysis of the National Inpatient Sample (NIS) database.
Over a 10-year-period, 193,554 patient admissions were identified for the primary diagnosis of diaphragmatic hernia of any type. An uncomplicated diaphragmatic hernia was the diagnosis in 161,777 (83.6%) admissions. Of these, 38,764 (24.0%) patients underwent an elective repair of their hernia as the principal procedure for their admission.
A diagnosis of diaphragmatic hernia with obstruction or gangrene was the reason for admission in 31,127 (16.1%) and 651 (0.3%) patients, respectively. Mortality was significantly higher in patients who were admitted with obstruction or gangrene (4.5% vs. 27.5%, respectively), compared with patients who were admitted for an elective hernia repair (1%).
Morbidity from pneumonia and sepsis was also significantly higher in patients who were admitted for obstruction or gangrene. Symptomatic admission was associated with more intensive hospitalization, as evidenced by significantly increasing length of stay – 6 days (uncomplicated) vs. 9 days (obstruction) vs. 17.5 days (gangrene) – and the need for mechanical ventilation (3.6% vs. 9.7 vs. 41.3%, respectively).
Based on their mortality data, the authors also performed a lifetime risk analysis that suggested that elective repair is associated with a favorable risk-benefit profile for patients in their 50s, 60s, and perhaps early 70s.
"In this large national database study, the prevalence of diaphragmatic hernia per hospital admission is 1:2,000. Admissions resulting from gangrene or obstruction are not uncommon and are associated with worse outcomes than [is repair] in uncomplicated hernias.
"This analysis suggests the practice of repair of uncomplicated diaphragmatic hernia may avoid the morbidity and mortality associated with either obstruction or gangrene," he concluded.
Dr. Paul reported that he had no relevant disclosures.
PHILADELPHIA – Current clinical practice is to repair symptomatic diaphragmatic hernias to avoid complications such as obstruction or gangrene. However, practice patterns are based largely on limited data from institutional case series, according to Dr. Subroto Paul and his colleagues at Cornell University in New York.
Mortality was significantly higher in patients with uncomplicated hernia who went on to readmission with obstruction or gangrene, Dr. Paul said at the annual meeting of the American Association for Thoracic Surgery, where he presented an analysis of the National Inpatient Sample (NIS) database.
Over a 10-year-period, 193,554 patient admissions were identified for the primary diagnosis of diaphragmatic hernia of any type. An uncomplicated diaphragmatic hernia was the diagnosis in 161,777 (83.6%) admissions. Of these, 38,764 (24.0%) patients underwent an elective repair of their hernia as the principal procedure for their admission.
A diagnosis of diaphragmatic hernia with obstruction or gangrene was the reason for admission in 31,127 (16.1%) and 651 (0.3%) patients, respectively. Mortality was significantly higher in patients who were admitted with obstruction or gangrene (4.5% vs. 27.5%, respectively), compared with patients who were admitted for an elective hernia repair (1%).
Morbidity from pneumonia and sepsis was also significantly higher in patients who were admitted for obstruction or gangrene. Symptomatic admission was associated with more intensive hospitalization, as evidenced by significantly increasing length of stay – 6 days (uncomplicated) vs. 9 days (obstruction) vs. 17.5 days (gangrene) – and the need for mechanical ventilation (3.6% vs. 9.7 vs. 41.3%, respectively).
Based on their mortality data, the authors also performed a lifetime risk analysis that suggested that elective repair is associated with a favorable risk-benefit profile for patients in their 50s, 60s, and perhaps early 70s.
"In this large national database study, the prevalence of diaphragmatic hernia per hospital admission is 1:2,000. Admissions resulting from gangrene or obstruction are not uncommon and are associated with worse outcomes than [is repair] in uncomplicated hernias.
"This analysis suggests the practice of repair of uncomplicated diaphragmatic hernia may avoid the morbidity and mortality associated with either obstruction or gangrene," he concluded.
Dr. Paul reported that he had no relevant disclosures.
PHILADELPHIA – Current clinical practice is to repair symptomatic diaphragmatic hernias to avoid complications such as obstruction or gangrene. However, practice patterns are based largely on limited data from institutional case series, according to Dr. Subroto Paul and his colleagues at Cornell University in New York.
Mortality was significantly higher in patients with uncomplicated hernia who went on to readmission with obstruction or gangrene, Dr. Paul said at the annual meeting of the American Association for Thoracic Surgery, where he presented an analysis of the National Inpatient Sample (NIS) database.
Over a 10-year-period, 193,554 patient admissions were identified for the primary diagnosis of diaphragmatic hernia of any type. An uncomplicated diaphragmatic hernia was the diagnosis in 161,777 (83.6%) admissions. Of these, 38,764 (24.0%) patients underwent an elective repair of their hernia as the principal procedure for their admission.
A diagnosis of diaphragmatic hernia with obstruction or gangrene was the reason for admission in 31,127 (16.1%) and 651 (0.3%) patients, respectively. Mortality was significantly higher in patients who were admitted with obstruction or gangrene (4.5% vs. 27.5%, respectively), compared with patients who were admitted for an elective hernia repair (1%).
Morbidity from pneumonia and sepsis was also significantly higher in patients who were admitted for obstruction or gangrene. Symptomatic admission was associated with more intensive hospitalization, as evidenced by significantly increasing length of stay – 6 days (uncomplicated) vs. 9 days (obstruction) vs. 17.5 days (gangrene) – and the need for mechanical ventilation (3.6% vs. 9.7 vs. 41.3%, respectively).
Based on their mortality data, the authors also performed a lifetime risk analysis that suggested that elective repair is associated with a favorable risk-benefit profile for patients in their 50s, 60s, and perhaps early 70s.
"In this large national database study, the prevalence of diaphragmatic hernia per hospital admission is 1:2,000. Admissions resulting from gangrene or obstruction are not uncommon and are associated with worse outcomes than [is repair] in uncomplicated hernias.
"This analysis suggests the practice of repair of uncomplicated diaphragmatic hernia may avoid the morbidity and mortality associated with either obstruction or gangrene," he concluded.
Dr. Paul reported that he had no relevant disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: Compared with patients who were admitted for an elective repair of uncomplicated diaphragmatic hernia, mortality was significantly higher in patients who were admitted with obstruction or gangrene (1% vs. 4.5% vs. 27.5%, respectively).
Data Source: A National Inpatient Sample database analysis of 161,777 patients who were diagnosed with diaphragmatic hernia.
Disclosures: Dr. Paul reported that he had no relevant disclosures.
Cryolipolysis Side Effects Mostly Mild and Transient, "Severe Pain" Rare
GRAPEVINE, TEX. – Risks associated with cryolipolysis for fat reduction are mostly transient and generally mild, according to a recent analysis.
"Severe pain" was reported in approximately 0.05% of all treated patients, said Dr. Nazanin Saedi of the University of California, Irvine.
Reports of severe pain emerged in postmarket surveillance, which traditionally allows for the detection of rare side effects not seen in clinical trials. Of more than 60,000 cryolipolysis treatments between June 2009 and December 2010, there were 23 reports of "severe pain" associated with the Zeltiq system. The determination that a report was of "severe" pain rather than the known potential discomfort following treatment depended on symptoms. Of the reports, 11 were described as "severe," 8 as "sensitive to touch," 6 as "stabbing," and 6 as "deep/severe burning." (Patients could report more than one symptom). The incidence was calculated based on a denominator of 50,000, giving a rate of 0.00046, or 0.05%.
Zeltiq evaluated the "severe pain" to understand its etiology. The pain does not appear to be associated with the increasing number of larger applicators, because 10 of the 23 of patients reporting "severe pain" underwent treatment with the smaller applicator, Dr. Saedi noted.
Most severe pain involved the abdomen (21 of the 23 patients), arising at a mean of 3.4 days (range, 1-7) following the procedure. The mean time to resolution was 13.9 days (range, 7-28). Just one patient had severe pain lasting for 28 days, while in the majority (16 of the 23), pain had resolved by 2 weeks. Six patients reported that the pain worsened before getting better, peaking at about a week.
Two of the patients had known connective tissue disease, while the etiology was unknown for the rest. Exaggerated panniculitis is one possibility. The pain might also be of focal neuropathic origin, including allodynia, hyperneuralgia, or nerve inflammation arising from cytokine-mediated irritation of nerve fibers during the onset of inflammation following the procedure, said Dr. Saedi. It is likely that there are multiple etiologies.
A variety of therapeutic measures were used to treat the severe pain, but only the topical lidocaine patch was consistently reported as being helpful. Compression garments, lidocaine/tetracaine cream, and Vicodin (hydrocodone bitartrate and acetaminophen) were reported to have some effect, while ibuprofen, Percocet (oxycodone HCl and acetaminophen), Tylenol (acetaminophen) with codeine, ice, and heating pads had little or no effect, Dr. Saedi said.
Hyperpigmentation associated with a first- or second-degree burn of the dermis was another rare adverse event that arose in postmarketing surveillance. A total of four cases were reported, or less than 0.01% of treated patients. Three of the four were deemed to have been a result of operator error. All cases resolved.
Cryolipolysis technology uses controlled cold exposure to reduce subcutaneous fat. Adipocytes are selectively damaged via control and modulation of the cold exposure, while avoiding damage to the overlying epidermis and dermis. The decrease in fat thickness occurs gradually over the subsequent 3 months, and is most pronounced in patients with limited, discrete fatty bulges. The novel technology is among the noninvasive mechanisms for fat reduction that are becoming increasingly popular commercially, she noted.
Since the reports, there have been changes to the user manual as well as revisions in user training, user interface, and procedure monitoring , which make the likelihood of burn injury or subsequent hyperpigmentation more unlikely, even in the event of misuse. In fact, there have been no further reports of burn injury or hyperpigmentation during the last 30,000 procedure cycles, she noted.
"Further postmarket surveillance is needed to identify and better understand rare events," Dr. Saedi concluded.
Dr. Saedi said that she had no relevant financial disclosures. However, her coinvestigators are on Zeltiq’s advisory board and have received educational and research support and honoraria from the company.
GRAPEVINE, TEX. – Risks associated with cryolipolysis for fat reduction are mostly transient and generally mild, according to a recent analysis.
"Severe pain" was reported in approximately 0.05% of all treated patients, said Dr. Nazanin Saedi of the University of California, Irvine.
Reports of severe pain emerged in postmarket surveillance, which traditionally allows for the detection of rare side effects not seen in clinical trials. Of more than 60,000 cryolipolysis treatments between June 2009 and December 2010, there were 23 reports of "severe pain" associated with the Zeltiq system. The determination that a report was of "severe" pain rather than the known potential discomfort following treatment depended on symptoms. Of the reports, 11 were described as "severe," 8 as "sensitive to touch," 6 as "stabbing," and 6 as "deep/severe burning." (Patients could report more than one symptom). The incidence was calculated based on a denominator of 50,000, giving a rate of 0.00046, or 0.05%.
Zeltiq evaluated the "severe pain" to understand its etiology. The pain does not appear to be associated with the increasing number of larger applicators, because 10 of the 23 of patients reporting "severe pain" underwent treatment with the smaller applicator, Dr. Saedi noted.
Most severe pain involved the abdomen (21 of the 23 patients), arising at a mean of 3.4 days (range, 1-7) following the procedure. The mean time to resolution was 13.9 days (range, 7-28). Just one patient had severe pain lasting for 28 days, while in the majority (16 of the 23), pain had resolved by 2 weeks. Six patients reported that the pain worsened before getting better, peaking at about a week.
Two of the patients had known connective tissue disease, while the etiology was unknown for the rest. Exaggerated panniculitis is one possibility. The pain might also be of focal neuropathic origin, including allodynia, hyperneuralgia, or nerve inflammation arising from cytokine-mediated irritation of nerve fibers during the onset of inflammation following the procedure, said Dr. Saedi. It is likely that there are multiple etiologies.
A variety of therapeutic measures were used to treat the severe pain, but only the topical lidocaine patch was consistently reported as being helpful. Compression garments, lidocaine/tetracaine cream, and Vicodin (hydrocodone bitartrate and acetaminophen) were reported to have some effect, while ibuprofen, Percocet (oxycodone HCl and acetaminophen), Tylenol (acetaminophen) with codeine, ice, and heating pads had little or no effect, Dr. Saedi said.
Hyperpigmentation associated with a first- or second-degree burn of the dermis was another rare adverse event that arose in postmarketing surveillance. A total of four cases were reported, or less than 0.01% of treated patients. Three of the four were deemed to have been a result of operator error. All cases resolved.
Cryolipolysis technology uses controlled cold exposure to reduce subcutaneous fat. Adipocytes are selectively damaged via control and modulation of the cold exposure, while avoiding damage to the overlying epidermis and dermis. The decrease in fat thickness occurs gradually over the subsequent 3 months, and is most pronounced in patients with limited, discrete fatty bulges. The novel technology is among the noninvasive mechanisms for fat reduction that are becoming increasingly popular commercially, she noted.
Since the reports, there have been changes to the user manual as well as revisions in user training, user interface, and procedure monitoring , which make the likelihood of burn injury or subsequent hyperpigmentation more unlikely, even in the event of misuse. In fact, there have been no further reports of burn injury or hyperpigmentation during the last 30,000 procedure cycles, she noted.
"Further postmarket surveillance is needed to identify and better understand rare events," Dr. Saedi concluded.
Dr. Saedi said that she had no relevant financial disclosures. However, her coinvestigators are on Zeltiq’s advisory board and have received educational and research support and honoraria from the company.
GRAPEVINE, TEX. – Risks associated with cryolipolysis for fat reduction are mostly transient and generally mild, according to a recent analysis.
"Severe pain" was reported in approximately 0.05% of all treated patients, said Dr. Nazanin Saedi of the University of California, Irvine.
Reports of severe pain emerged in postmarket surveillance, which traditionally allows for the detection of rare side effects not seen in clinical trials. Of more than 60,000 cryolipolysis treatments between June 2009 and December 2010, there were 23 reports of "severe pain" associated with the Zeltiq system. The determination that a report was of "severe" pain rather than the known potential discomfort following treatment depended on symptoms. Of the reports, 11 were described as "severe," 8 as "sensitive to touch," 6 as "stabbing," and 6 as "deep/severe burning." (Patients could report more than one symptom). The incidence was calculated based on a denominator of 50,000, giving a rate of 0.00046, or 0.05%.
Zeltiq evaluated the "severe pain" to understand its etiology. The pain does not appear to be associated with the increasing number of larger applicators, because 10 of the 23 of patients reporting "severe pain" underwent treatment with the smaller applicator, Dr. Saedi noted.
Most severe pain involved the abdomen (21 of the 23 patients), arising at a mean of 3.4 days (range, 1-7) following the procedure. The mean time to resolution was 13.9 days (range, 7-28). Just one patient had severe pain lasting for 28 days, while in the majority (16 of the 23), pain had resolved by 2 weeks. Six patients reported that the pain worsened before getting better, peaking at about a week.
Two of the patients had known connective tissue disease, while the etiology was unknown for the rest. Exaggerated panniculitis is one possibility. The pain might also be of focal neuropathic origin, including allodynia, hyperneuralgia, or nerve inflammation arising from cytokine-mediated irritation of nerve fibers during the onset of inflammation following the procedure, said Dr. Saedi. It is likely that there are multiple etiologies.
A variety of therapeutic measures were used to treat the severe pain, but only the topical lidocaine patch was consistently reported as being helpful. Compression garments, lidocaine/tetracaine cream, and Vicodin (hydrocodone bitartrate and acetaminophen) were reported to have some effect, while ibuprofen, Percocet (oxycodone HCl and acetaminophen), Tylenol (acetaminophen) with codeine, ice, and heating pads had little or no effect, Dr. Saedi said.
Hyperpigmentation associated with a first- or second-degree burn of the dermis was another rare adverse event that arose in postmarketing surveillance. A total of four cases were reported, or less than 0.01% of treated patients. Three of the four were deemed to have been a result of operator error. All cases resolved.
Cryolipolysis technology uses controlled cold exposure to reduce subcutaneous fat. Adipocytes are selectively damaged via control and modulation of the cold exposure, while avoiding damage to the overlying epidermis and dermis. The decrease in fat thickness occurs gradually over the subsequent 3 months, and is most pronounced in patients with limited, discrete fatty bulges. The novel technology is among the noninvasive mechanisms for fat reduction that are becoming increasingly popular commercially, she noted.
Since the reports, there have been changes to the user manual as well as revisions in user training, user interface, and procedure monitoring , which make the likelihood of burn injury or subsequent hyperpigmentation more unlikely, even in the event of misuse. In fact, there have been no further reports of burn injury or hyperpigmentation during the last 30,000 procedure cycles, she noted.
"Further postmarket surveillance is needed to identify and better understand rare events," Dr. Saedi concluded.
Dr. Saedi said that she had no relevant financial disclosures. However, her coinvestigators are on Zeltiq’s advisory board and have received educational and research support and honoraria from the company.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR LASER MEDICINE AND SURGERY
Preoperative Hyponatremia Points to Dismal Outcomes After Cardiac Surgery
NEW ORLEANS – Preoperative hyponatremia was common in patients undergoing cardiac surgery and associated with a dramatic increase in the risk of death and surgical complications in a large retrospective analysis.
Of the 4,370 patients who underwent cardiac surgery between 2002 and 2009 at the Ohio State Medical Center in Columbus, 931 (21%) had hyponatremia, defined as serum sodium less than 135 mEq/L on at least one of three sodium tests obtained before surgery.
In unadjusted analysis, hyponatremic patients had significantly higher rates than did those without hyponatremia of early mortality (9% vs. 4%), late mortality (24% vs. 15.6%), longer mean hospital length of stay (12.6 days vs. 8.2 days), and operative complications (13% vs. 7%), Dr. Juan Crestanello and his colleagues reported in a poster at the annual meeting of the American College of Cardiology.
This isn’t all that surprising since hyponatremic patients were sicker at baseline, but the poor outcomes remained, even after adjustment for a slew of baseline clinical and operative variables.
In multivariable logistic regression analysis, preoperative hyponatremia was independently associated with a 31% increase in overall mortality, a 52% increase in early mortality, and a 56% increase in late mortality, said Dr. Crestanello, a thoracic surgeon at the medical center.
Hyponatremia also significantly increased the risk of operative complications by 30%, pulmonary complications by 73%, renal failure requiring dialysis by 64%, and hospital length of stay by 26%. Infectious and neurologic complications were not independently associated with preoperative hyponatremia.
"Hyponatremia identifies a group of patients at higher risk for cardiac surgery," Dr. Crestanello said in an interview. "It constitutes another tool to risk-stratify these patients and will help surgeons advise patients of their risk associated with surgery."
At baseline, patients with hyponatremia had a significantly lower mean ejection fraction than did patients without hyponatremia (39% vs. 46%), higher mean pulmonary artery pressure (32 mmHg vs. 28 mmHg), and higher incidence of comorbidities, including diabetes (47% vs. 34%), chronic obstructive pulmonary disease (24.5% vs. 18%), and history of a previous MI (44.5% vs. 35.6%).
Hyponatremic patients also had significantly higher New York Heart Association functional class, higher surgical risk as predicted by the European System for Cardiac Operative Risk Evaluation (19% vs. 9%) and underwent more complex surgical procedures including coronary artery bypass surgery with valve replacement and ventricular-assist device placement.
Their mean age was 62 years, 66.5% were male, and the mean sodium level was 134 mEq/L.
Sodium levels are one of the most common laboratory values measured and are routinely obtained preoperatively.
"In spite of being widely available, they are often overlooked," Dr. Crestanello said.
Data on other factors that may have influenced serum sodium like medications, glucose levels, and fluid use were not accounted for in the study because of its retrospective nature, he noted.
When asked to speculate on the mechanism behind the association between hyponatremia and poor outcomes, Dr. Crestanello said they are not well understood. "Obviously, hyponatremia is a marker for high-risk patients, but at the same time it is likely that it has pathophysiological effects on its own ... hyponatremia is also associated with changes in the neurohormonal milieu that, by itself, can have deleterious effects."
The analysis was based on data from electronic medical records, the Society of Thoracic Surgery database, and Social Security Death Index. Mean follow-up was 2.2 years.
The authors plan to analyze the effects that correcting preoperative hyponatremia has on outcomes of cardiac surgery. The current study was supported by a grant from Biogen Inc.
NEW ORLEANS – Preoperative hyponatremia was common in patients undergoing cardiac surgery and associated with a dramatic increase in the risk of death and surgical complications in a large retrospective analysis.
Of the 4,370 patients who underwent cardiac surgery between 2002 and 2009 at the Ohio State Medical Center in Columbus, 931 (21%) had hyponatremia, defined as serum sodium less than 135 mEq/L on at least one of three sodium tests obtained before surgery.
In unadjusted analysis, hyponatremic patients had significantly higher rates than did those without hyponatremia of early mortality (9% vs. 4%), late mortality (24% vs. 15.6%), longer mean hospital length of stay (12.6 days vs. 8.2 days), and operative complications (13% vs. 7%), Dr. Juan Crestanello and his colleagues reported in a poster at the annual meeting of the American College of Cardiology.
This isn’t all that surprising since hyponatremic patients were sicker at baseline, but the poor outcomes remained, even after adjustment for a slew of baseline clinical and operative variables.
In multivariable logistic regression analysis, preoperative hyponatremia was independently associated with a 31% increase in overall mortality, a 52% increase in early mortality, and a 56% increase in late mortality, said Dr. Crestanello, a thoracic surgeon at the medical center.
Hyponatremia also significantly increased the risk of operative complications by 30%, pulmonary complications by 73%, renal failure requiring dialysis by 64%, and hospital length of stay by 26%. Infectious and neurologic complications were not independently associated with preoperative hyponatremia.
"Hyponatremia identifies a group of patients at higher risk for cardiac surgery," Dr. Crestanello said in an interview. "It constitutes another tool to risk-stratify these patients and will help surgeons advise patients of their risk associated with surgery."
At baseline, patients with hyponatremia had a significantly lower mean ejection fraction than did patients without hyponatremia (39% vs. 46%), higher mean pulmonary artery pressure (32 mmHg vs. 28 mmHg), and higher incidence of comorbidities, including diabetes (47% vs. 34%), chronic obstructive pulmonary disease (24.5% vs. 18%), and history of a previous MI (44.5% vs. 35.6%).
Hyponatremic patients also had significantly higher New York Heart Association functional class, higher surgical risk as predicted by the European System for Cardiac Operative Risk Evaluation (19% vs. 9%) and underwent more complex surgical procedures including coronary artery bypass surgery with valve replacement and ventricular-assist device placement.
Their mean age was 62 years, 66.5% were male, and the mean sodium level was 134 mEq/L.
Sodium levels are one of the most common laboratory values measured and are routinely obtained preoperatively.
"In spite of being widely available, they are often overlooked," Dr. Crestanello said.
Data on other factors that may have influenced serum sodium like medications, glucose levels, and fluid use were not accounted for in the study because of its retrospective nature, he noted.
When asked to speculate on the mechanism behind the association between hyponatremia and poor outcomes, Dr. Crestanello said they are not well understood. "Obviously, hyponatremia is a marker for high-risk patients, but at the same time it is likely that it has pathophysiological effects on its own ... hyponatremia is also associated with changes in the neurohormonal milieu that, by itself, can have deleterious effects."
The analysis was based on data from electronic medical records, the Society of Thoracic Surgery database, and Social Security Death Index. Mean follow-up was 2.2 years.
The authors plan to analyze the effects that correcting preoperative hyponatremia has on outcomes of cardiac surgery. The current study was supported by a grant from Biogen Inc.
NEW ORLEANS – Preoperative hyponatremia was common in patients undergoing cardiac surgery and associated with a dramatic increase in the risk of death and surgical complications in a large retrospective analysis.
Of the 4,370 patients who underwent cardiac surgery between 2002 and 2009 at the Ohio State Medical Center in Columbus, 931 (21%) had hyponatremia, defined as serum sodium less than 135 mEq/L on at least one of three sodium tests obtained before surgery.
In unadjusted analysis, hyponatremic patients had significantly higher rates than did those without hyponatremia of early mortality (9% vs. 4%), late mortality (24% vs. 15.6%), longer mean hospital length of stay (12.6 days vs. 8.2 days), and operative complications (13% vs. 7%), Dr. Juan Crestanello and his colleagues reported in a poster at the annual meeting of the American College of Cardiology.
This isn’t all that surprising since hyponatremic patients were sicker at baseline, but the poor outcomes remained, even after adjustment for a slew of baseline clinical and operative variables.
In multivariable logistic regression analysis, preoperative hyponatremia was independently associated with a 31% increase in overall mortality, a 52% increase in early mortality, and a 56% increase in late mortality, said Dr. Crestanello, a thoracic surgeon at the medical center.
Hyponatremia also significantly increased the risk of operative complications by 30%, pulmonary complications by 73%, renal failure requiring dialysis by 64%, and hospital length of stay by 26%. Infectious and neurologic complications were not independently associated with preoperative hyponatremia.
"Hyponatremia identifies a group of patients at higher risk for cardiac surgery," Dr. Crestanello said in an interview. "It constitutes another tool to risk-stratify these patients and will help surgeons advise patients of their risk associated with surgery."
At baseline, patients with hyponatremia had a significantly lower mean ejection fraction than did patients without hyponatremia (39% vs. 46%), higher mean pulmonary artery pressure (32 mmHg vs. 28 mmHg), and higher incidence of comorbidities, including diabetes (47% vs. 34%), chronic obstructive pulmonary disease (24.5% vs. 18%), and history of a previous MI (44.5% vs. 35.6%).
Hyponatremic patients also had significantly higher New York Heart Association functional class, higher surgical risk as predicted by the European System for Cardiac Operative Risk Evaluation (19% vs. 9%) and underwent more complex surgical procedures including coronary artery bypass surgery with valve replacement and ventricular-assist device placement.
Their mean age was 62 years, 66.5% were male, and the mean sodium level was 134 mEq/L.
Sodium levels are one of the most common laboratory values measured and are routinely obtained preoperatively.
"In spite of being widely available, they are often overlooked," Dr. Crestanello said.
Data on other factors that may have influenced serum sodium like medications, glucose levels, and fluid use were not accounted for in the study because of its retrospective nature, he noted.
When asked to speculate on the mechanism behind the association between hyponatremia and poor outcomes, Dr. Crestanello said they are not well understood. "Obviously, hyponatremia is a marker for high-risk patients, but at the same time it is likely that it has pathophysiological effects on its own ... hyponatremia is also associated with changes in the neurohormonal milieu that, by itself, can have deleterious effects."
The analysis was based on data from electronic medical records, the Society of Thoracic Surgery database, and Social Security Death Index. Mean follow-up was 2.2 years.
The authors plan to analyze the effects that correcting preoperative hyponatremia has on outcomes of cardiac surgery. The current study was supported by a grant from Biogen Inc.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF CARDIOLOGY