User login
Robotic surgery technologies have unique learning curves for trainees
Training surgeons to use robotic technology involves learning curves, and a study has found that robotic technologies have unique learning curve profiles that have implications for the time and number of procedures needed to achieve competence.
Giorgio Mazzon, MD, of the Institute of Urology at University College Hospital, London, and his colleagues reviewed the literature on training surgeons in the use of a variety of technologies for urological procedures. They analyzed learning curves for virtual reality robotic simulators, robot-assisted laparoscopic radical prostatectomy (RALP), robot-assisted radical cystectomy (RARC), and robot-assisted partial nephrectomy (RAPN) (Curr Urol Rep. 2017 Sep 23;18:89).
RARC learning curves are more rapid than RALP, but this may be due to the fact that most surgeons practice RALP before learning RARC. It is estimated that it takes 21 procedures for operating time to plateau and 30 patients for proper lymph node yield and positive surgical margins of less than 5% to occur (Eur Urol. 2010 Aug;58[2]:197-202).Safety and competence in RAPN is usually defined by operating times, warm ischemic time, positive surgical margin, and complication rates. It has been reported that RAPN can be safely performed with completion of 25-30 cases (Eur Urol. 2010 Jul;58[1]:127-32).The results of the review “should inform trainers and trainees on what outcomes are expected at a given stage of training,” according to the investigators.
They reported no relevant financial disclosures.
Training surgeons to use robotic technology involves learning curves, and a study has found that robotic technologies have unique learning curve profiles that have implications for the time and number of procedures needed to achieve competence.
Giorgio Mazzon, MD, of the Institute of Urology at University College Hospital, London, and his colleagues reviewed the literature on training surgeons in the use of a variety of technologies for urological procedures. They analyzed learning curves for virtual reality robotic simulators, robot-assisted laparoscopic radical prostatectomy (RALP), robot-assisted radical cystectomy (RARC), and robot-assisted partial nephrectomy (RAPN) (Curr Urol Rep. 2017 Sep 23;18:89).
RARC learning curves are more rapid than RALP, but this may be due to the fact that most surgeons practice RALP before learning RARC. It is estimated that it takes 21 procedures for operating time to plateau and 30 patients for proper lymph node yield and positive surgical margins of less than 5% to occur (Eur Urol. 2010 Aug;58[2]:197-202).Safety and competence in RAPN is usually defined by operating times, warm ischemic time, positive surgical margin, and complication rates. It has been reported that RAPN can be safely performed with completion of 25-30 cases (Eur Urol. 2010 Jul;58[1]:127-32).The results of the review “should inform trainers and trainees on what outcomes are expected at a given stage of training,” according to the investigators.
They reported no relevant financial disclosures.
Training surgeons to use robotic technology involves learning curves, and a study has found that robotic technologies have unique learning curve profiles that have implications for the time and number of procedures needed to achieve competence.
Giorgio Mazzon, MD, of the Institute of Urology at University College Hospital, London, and his colleagues reviewed the literature on training surgeons in the use of a variety of technologies for urological procedures. They analyzed learning curves for virtual reality robotic simulators, robot-assisted laparoscopic radical prostatectomy (RALP), robot-assisted radical cystectomy (RARC), and robot-assisted partial nephrectomy (RAPN) (Curr Urol Rep. 2017 Sep 23;18:89).
RARC learning curves are more rapid than RALP, but this may be due to the fact that most surgeons practice RALP before learning RARC. It is estimated that it takes 21 procedures for operating time to plateau and 30 patients for proper lymph node yield and positive surgical margins of less than 5% to occur (Eur Urol. 2010 Aug;58[2]:197-202).Safety and competence in RAPN is usually defined by operating times, warm ischemic time, positive surgical margin, and complication rates. It has been reported that RAPN can be safely performed with completion of 25-30 cases (Eur Urol. 2010 Jul;58[1]:127-32).The results of the review “should inform trainers and trainees on what outcomes are expected at a given stage of training,” according to the investigators.
They reported no relevant financial disclosures.
FROM CURRENT UROLOGY REPORTS
Key clinical point:
Major finding: For virtual reality training programs, recommendations for achieving safety and competence is between 4 and 12 hours of training in a simulator.
Data source: Review of studies of learning curves in robotic urological surgery.
Disclosures: The researchers reported no financial disclosures.
Robot-assisted prostatectomy providing better outcomes
Robot-assisted radical prostatectomy shows better early postoperative outcomes than does laparoscopic radical prostatectomy, but the differences between the two surgical approaches disappeared by the 6-month follow-up.
Dr. Hiroyuki Koike and his colleagues at Wakayama (Japan) Medical University Hospital conducted a study of two groups of patients treated for localized prostate cancer. One group of 229 patients underwent laparoscopic radical prostatectomy (LRP) between July 2007 and July 2013. The other group of 115 patients had robot-assisted radical prostatectomy (RARP) between December 2012 and August 2014 (J Robot Surg. 2017;11[3]:325-31).
The patients were given health-related quality of life self-assessment surveys prior to surgery and at 3, 6, and 12 months post surgery. In addition, a generic questionnaire, the eight-item Short-Form Health Survey, was used to assess a physical component summary (PCS) and a mental component summary (MCS). The Expanded Prostate Cancer Index of Prostate, which covers four domains – urinary, sexual, bowel, and hormonal – was used as a disease-specific measure, and the response rates for both LRP and RARP at each follow-up interval were over 80%.
“The RARP group showed significantly better scores in urinary summary and all urinary subscales at postoperative 3-month follow-up. However, these differences disappeared at postoperative 6 and 12-month follow-up,” the investigators wrote. For the urinary summary score, LRP significantly underperformed, compared with RARP, with scores of 63.3 vs. 75.8, respectively, after 3 months. In addition, the bowel function score was superior for RARP, compared with LRP, at 96.9 vs. 92.9, respectively. Sexual function results were similar, with RARP and LRP scores of 2.8 vs. 0.
The general measures of the PCS and MCS also favored RARP. At the 3-month follow-up, PCS (51.3 vs. 48.1) and MCS (50 vs. 47.8) scores were higher for RARP, compared with LRP.
“It is unclear why our superiority of urinary function in RARP was observed only in early period. However, we can speculate several reasons for better urinary function in RARP group. First, we were able to treat the apex area more delicately with RARP. Second, some of the new techniques which we employed after the introduction of RARP could influence the urinary continence recovery,” the investigators wrote.
The authors had no relevant financial disclosures.
Robot-assisted radical prostatectomy shows better early postoperative outcomes than does laparoscopic radical prostatectomy, but the differences between the two surgical approaches disappeared by the 6-month follow-up.
Dr. Hiroyuki Koike and his colleagues at Wakayama (Japan) Medical University Hospital conducted a study of two groups of patients treated for localized prostate cancer. One group of 229 patients underwent laparoscopic radical prostatectomy (LRP) between July 2007 and July 2013. The other group of 115 patients had robot-assisted radical prostatectomy (RARP) between December 2012 and August 2014 (J Robot Surg. 2017;11[3]:325-31).
The patients were given health-related quality of life self-assessment surveys prior to surgery and at 3, 6, and 12 months post surgery. In addition, a generic questionnaire, the eight-item Short-Form Health Survey, was used to assess a physical component summary (PCS) and a mental component summary (MCS). The Expanded Prostate Cancer Index of Prostate, which covers four domains – urinary, sexual, bowel, and hormonal – was used as a disease-specific measure, and the response rates for both LRP and RARP at each follow-up interval were over 80%.
“The RARP group showed significantly better scores in urinary summary and all urinary subscales at postoperative 3-month follow-up. However, these differences disappeared at postoperative 6 and 12-month follow-up,” the investigators wrote. For the urinary summary score, LRP significantly underperformed, compared with RARP, with scores of 63.3 vs. 75.8, respectively, after 3 months. In addition, the bowel function score was superior for RARP, compared with LRP, at 96.9 vs. 92.9, respectively. Sexual function results were similar, with RARP and LRP scores of 2.8 vs. 0.
The general measures of the PCS and MCS also favored RARP. At the 3-month follow-up, PCS (51.3 vs. 48.1) and MCS (50 vs. 47.8) scores were higher for RARP, compared with LRP.
“It is unclear why our superiority of urinary function in RARP was observed only in early period. However, we can speculate several reasons for better urinary function in RARP group. First, we were able to treat the apex area more delicately with RARP. Second, some of the new techniques which we employed after the introduction of RARP could influence the urinary continence recovery,” the investigators wrote.
The authors had no relevant financial disclosures.
Robot-assisted radical prostatectomy shows better early postoperative outcomes than does laparoscopic radical prostatectomy, but the differences between the two surgical approaches disappeared by the 6-month follow-up.
Dr. Hiroyuki Koike and his colleagues at Wakayama (Japan) Medical University Hospital conducted a study of two groups of patients treated for localized prostate cancer. One group of 229 patients underwent laparoscopic radical prostatectomy (LRP) between July 2007 and July 2013. The other group of 115 patients had robot-assisted radical prostatectomy (RARP) between December 2012 and August 2014 (J Robot Surg. 2017;11[3]:325-31).
The patients were given health-related quality of life self-assessment surveys prior to surgery and at 3, 6, and 12 months post surgery. In addition, a generic questionnaire, the eight-item Short-Form Health Survey, was used to assess a physical component summary (PCS) and a mental component summary (MCS). The Expanded Prostate Cancer Index of Prostate, which covers four domains – urinary, sexual, bowel, and hormonal – was used as a disease-specific measure, and the response rates for both LRP and RARP at each follow-up interval were over 80%.
“The RARP group showed significantly better scores in urinary summary and all urinary subscales at postoperative 3-month follow-up. However, these differences disappeared at postoperative 6 and 12-month follow-up,” the investigators wrote. For the urinary summary score, LRP significantly underperformed, compared with RARP, with scores of 63.3 vs. 75.8, respectively, after 3 months. In addition, the bowel function score was superior for RARP, compared with LRP, at 96.9 vs. 92.9, respectively. Sexual function results were similar, with RARP and LRP scores of 2.8 vs. 0.
The general measures of the PCS and MCS also favored RARP. At the 3-month follow-up, PCS (51.3 vs. 48.1) and MCS (50 vs. 47.8) scores were higher for RARP, compared with LRP.
“It is unclear why our superiority of urinary function in RARP was observed only in early period. However, we can speculate several reasons for better urinary function in RARP group. First, we were able to treat the apex area more delicately with RARP. Second, some of the new techniques which we employed after the introduction of RARP could influence the urinary continence recovery,” the investigators wrote.
The authors had no relevant financial disclosures.
FROM JOURNAL OF ROBOTIC SURGERY
Key clinical point:
Major finding: Quality-of-life score for robotic-assisted radical prostatectomy was higher in all urinary categories after 3 months.
Data source: Postop survey results from patients with localized prostate cancer who underwent laparoscopic radical prostatectomy (n = 229) or robot-assisted radical prostatectomy (n = 115).
Disclosures: The investigators had no financial disclosures to report.
Peer-to-peer learning about robotic surgery is happening on social media
Social media is now being used by surgeons for interaction among peers, informal learning, exchange of technical information, and diffusion of ideas.
A study has examined posting and membership data from a closed Facebook page, the “Robotic Surgery Collaboration,” created by surgeons who practice robotic-assisted procedures. Overall, the findings show exponential growth in membership in January 2015 through August 2016, some signs of stagnating engagement, and use of the platform for peer-to-peer learning and discussion.
“The growth in this group over time suggests that surgeons found it useful for engaging in informal interactions and learning vicariously from one another, but also reveals that not all users were actively engaged in these interactions each month and that growth in active membership differed from growth in overall group membership (as evident in the stagnating growth of active members, despite continued growth in total members),” the investigators concluded. Read the full study at Ann Surg. 2017 Aug 29. doi: 10.1097/SLA.0000000000002479. (Epub ahead of print).
Social media is now being used by surgeons for interaction among peers, informal learning, exchange of technical information, and diffusion of ideas.
A study has examined posting and membership data from a closed Facebook page, the “Robotic Surgery Collaboration,” created by surgeons who practice robotic-assisted procedures. Overall, the findings show exponential growth in membership in January 2015 through August 2016, some signs of stagnating engagement, and use of the platform for peer-to-peer learning and discussion.
“The growth in this group over time suggests that surgeons found it useful for engaging in informal interactions and learning vicariously from one another, but also reveals that not all users were actively engaged in these interactions each month and that growth in active membership differed from growth in overall group membership (as evident in the stagnating growth of active members, despite continued growth in total members),” the investigators concluded. Read the full study at Ann Surg. 2017 Aug 29. doi: 10.1097/SLA.0000000000002479. (Epub ahead of print).
Social media is now being used by surgeons for interaction among peers, informal learning, exchange of technical information, and diffusion of ideas.
A study has examined posting and membership data from a closed Facebook page, the “Robotic Surgery Collaboration,” created by surgeons who practice robotic-assisted procedures. Overall, the findings show exponential growth in membership in January 2015 through August 2016, some signs of stagnating engagement, and use of the platform for peer-to-peer learning and discussion.
“The growth in this group over time suggests that surgeons found it useful for engaging in informal interactions and learning vicariously from one another, but also reveals that not all users were actively engaged in these interactions each month and that growth in active membership differed from growth in overall group membership (as evident in the stagnating growth of active members, despite continued growth in total members),” the investigators concluded. Read the full study at Ann Surg. 2017 Aug 29. doi: 10.1097/SLA.0000000000002479. (Epub ahead of print).
Adoption of robotic-assisted surgery uneven across specialties
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).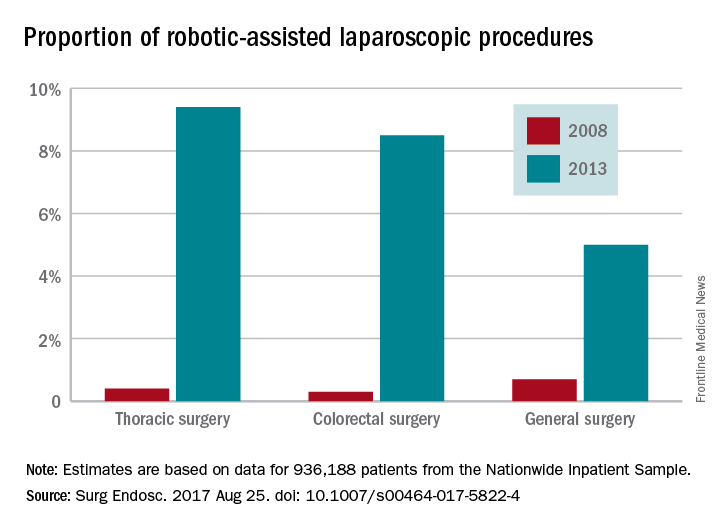
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).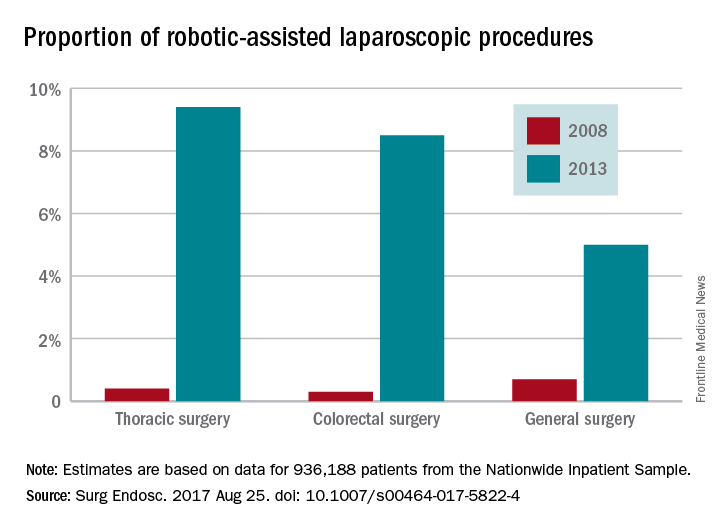
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).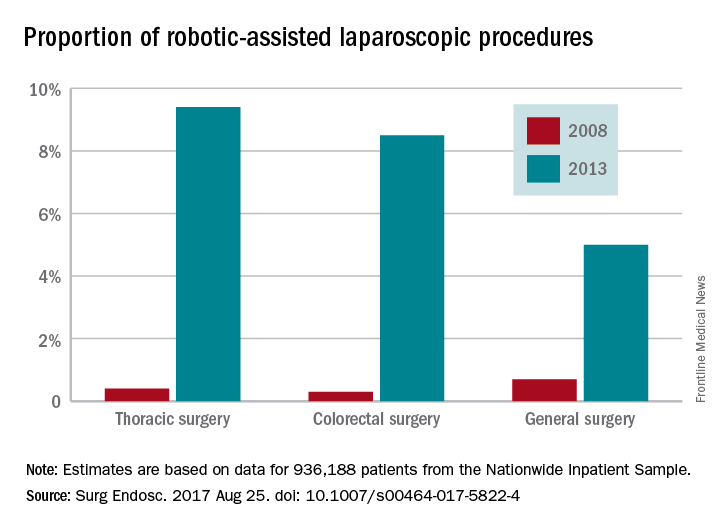
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
FROM SURGICAL ENDOSCOPY
Key clinical point:
Major finding: Procedures performed with robotic assistance increased from 6.8% to 17% over a 5-year period.
Data source: Analysis of data from 936,188 patients from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database.
Disclosures: Investigators reported no conflicts of interest.
Clinical trial: Sinai Robotic Surgery Trial in HPVOPC
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
Clinical trial: Use of robotics for cholecystectomy
The Use of Robotics for Cholecystectomy study is a retrospective review currently recruiting patients who underwent robotic-assisted laparoscopic cholecystectomy from June 2004 through May 2015.
Several methods are considered standard of care for the surgical treatment of cholecystitis, including open surgery, laparoscopic, and robotic-assisted laparoscopic surgery. This study, a retrospective analysis of charts, operating room notes, and operating room documentation of procedures, will review intraoperative and postoperative clinical outcomes of robotic-assisted laparoscopic cholecystectomy.
The intent of the study is to establish the role of robotics in laparoscopic surgery and to assess the learning curve for surgeons. Primary outcomes will be to compare hernia rates between multiport and single-port approaches, and to compare multiport against single-port approaches through the standard of care model of normal postsurgery follow-ups, along with additional follow-ups if complications are seen.
Recruitment for the study ends in May 2019. About 500 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Use of Robotics for Cholecystectomy study is a retrospective review currently recruiting patients who underwent robotic-assisted laparoscopic cholecystectomy from June 2004 through May 2015.
Several methods are considered standard of care for the surgical treatment of cholecystitis, including open surgery, laparoscopic, and robotic-assisted laparoscopic surgery. This study, a retrospective analysis of charts, operating room notes, and operating room documentation of procedures, will review intraoperative and postoperative clinical outcomes of robotic-assisted laparoscopic cholecystectomy.
The intent of the study is to establish the role of robotics in laparoscopic surgery and to assess the learning curve for surgeons. Primary outcomes will be to compare hernia rates between multiport and single-port approaches, and to compare multiport against single-port approaches through the standard of care model of normal postsurgery follow-ups, along with additional follow-ups if complications are seen.
Recruitment for the study ends in May 2019. About 500 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Use of Robotics for Cholecystectomy study is a retrospective review currently recruiting patients who underwent robotic-assisted laparoscopic cholecystectomy from June 2004 through May 2015.
Several methods are considered standard of care for the surgical treatment of cholecystitis, including open surgery, laparoscopic, and robotic-assisted laparoscopic surgery. This study, a retrospective analysis of charts, operating room notes, and operating room documentation of procedures, will review intraoperative and postoperative clinical outcomes of robotic-assisted laparoscopic cholecystectomy.
The intent of the study is to establish the role of robotics in laparoscopic surgery and to assess the learning curve for surgeons. Primary outcomes will be to compare hernia rates between multiport and single-port approaches, and to compare multiport against single-port approaches through the standard of care model of normal postsurgery follow-ups, along with additional follow-ups if complications are seen.
Recruitment for the study ends in May 2019. About 500 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
SUMMARY FROM CLINICALTRIALS.GOV
Robotic-assisted IHR causes fewer complications in obese patients
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
FROM SURGICAL ENDOSCOPY
Predicting extraction of an intact uterus in robotic-assisted laparoscopic hysterectomy
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The sensitivity of the scoring system was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Data source: Single-center review of 367 robotic total laparoscopic hysterectomies during 2012-2015.
Disclosures: There was no external funding for the work, and the investigators reported having no relevant financial disclosures.
Confirmatory blood typing unnecessary for closed prolapse repairs
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: Given the 0.4% risk of transfusion reactions in unscreened women, the risk of serious transfusion reactions was 1 in 50,000 women with closed apical prolapse repairs.
Data source: A review of more than 600 cases of apical prolapse surgery at a single center.
Disclosures: There was no industry funding, and the investigators reported having no relevant financial disclosures.
Robot-assisted surgery can be a pain
It’s early days for research on the physical impact of robot-assisted surgery on operators. But a study of surgeons who regularly do this kind of work suggests that surgical robots can be the cause of workplace injuries, despite their reputation for good ergonomic design and low stress on surgeon hands, wrists, backs, and necks
More than half (236) of 432 surveyed surgeons with at least 10 robotic surgeries annually reported physical discomfort associated with robotics consoles, according to a study out of Johns Hopkins University, Baltimore.
Most participants were male (71%) and averaged 48 years of age; their specialties comprised gynecology (68%), urology (20%), general surgery (8%), and others (3%).
Of the 432 participants, they reported physical discomfort in the following areas: fingers, 78%; necks, 74%; upper backs, 53%; and 43%, 34%, and 33% in the lower backs, eyes, and wrists, respectively.
Most of those who responded to the survey (80.8%) performed surgery with the da Vinci Si as their primary robotic system, with the rest using a different iteration of the da Vinci system.
Dr. Lee and his colleagues estimate the high rates of reported discomfort in fingers and necks are because of the structure of the robotics console.
“Due to the absence of tactile feedback at the master controller of the surgeon console, some robotic surgeons might close their fingers excessively when holding objects with instruments,” researchers said. “During the performance of suturing and knot-tying tasks, surgeons must squeeze their grip to hold a needle in place because there is no locking mechanism, which is present with open and laparoscopic needle holders.”
Researchers credit high rates of neck pain to the console as well, which “requires [surgeons] to maintain their neck position in a fixed place for extended period of time.”
While the rate of physical discomfort was 56%, participants rated the ergonomic functions of the console an average of 4 out of 5, with 5 being the highest score.
In contrast, surgeons gave low ratings to the communications systems used by the surgeon and the in-room supporting OR staff – an average of 2.87 out of 5 – noting an urgency for system updates.
Overall, researchers found that surgeons with high confidence in their ergonomic console settings were more likely to feel confident in the use of robotics in their surgical procedures and less likely to report physical discomfort. This finding led researchers to conclude the importance of surgeons new to robot-assisted surgery to receive education in ergonomic settings.
“Formal robotic surgery training programs should include this crucially important knowledge about optimal ergonomic guidelines so that any surgeon starting their training in robotic surgery would have the knowledge to maintain sound body posture and to minimize any physical strains while acquiring the best skill set,” according to Dr. Lee and his associates.
This study was limited by the self-reported data, which could create possible reporting bias, as well as by a small sample size. Since surgeons conducted more than one type of surgery annually, researchers found it difficult to identify what had caused the physical symptoms with complete confidence.
Researchers declared no relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
It’s early days for research on the physical impact of robot-assisted surgery on operators. But a study of surgeons who regularly do this kind of work suggests that surgical robots can be the cause of workplace injuries, despite their reputation for good ergonomic design and low stress on surgeon hands, wrists, backs, and necks
More than half (236) of 432 surveyed surgeons with at least 10 robotic surgeries annually reported physical discomfort associated with robotics consoles, according to a study out of Johns Hopkins University, Baltimore.
Most participants were male (71%) and averaged 48 years of age; their specialties comprised gynecology (68%), urology (20%), general surgery (8%), and others (3%).
Of the 432 participants, they reported physical discomfort in the following areas: fingers, 78%; necks, 74%; upper backs, 53%; and 43%, 34%, and 33% in the lower backs, eyes, and wrists, respectively.
Most of those who responded to the survey (80.8%) performed surgery with the da Vinci Si as their primary robotic system, with the rest using a different iteration of the da Vinci system.
Dr. Lee and his colleagues estimate the high rates of reported discomfort in fingers and necks are because of the structure of the robotics console.
“Due to the absence of tactile feedback at the master controller of the surgeon console, some robotic surgeons might close their fingers excessively when holding objects with instruments,” researchers said. “During the performance of suturing and knot-tying tasks, surgeons must squeeze their grip to hold a needle in place because there is no locking mechanism, which is present with open and laparoscopic needle holders.”
Researchers credit high rates of neck pain to the console as well, which “requires [surgeons] to maintain their neck position in a fixed place for extended period of time.”
While the rate of physical discomfort was 56%, participants rated the ergonomic functions of the console an average of 4 out of 5, with 5 being the highest score.
In contrast, surgeons gave low ratings to the communications systems used by the surgeon and the in-room supporting OR staff – an average of 2.87 out of 5 – noting an urgency for system updates.
Overall, researchers found that surgeons with high confidence in their ergonomic console settings were more likely to feel confident in the use of robotics in their surgical procedures and less likely to report physical discomfort. This finding led researchers to conclude the importance of surgeons new to robot-assisted surgery to receive education in ergonomic settings.
“Formal robotic surgery training programs should include this crucially important knowledge about optimal ergonomic guidelines so that any surgeon starting their training in robotic surgery would have the knowledge to maintain sound body posture and to minimize any physical strains while acquiring the best skill set,” according to Dr. Lee and his associates.
This study was limited by the self-reported data, which could create possible reporting bias, as well as by a small sample size. Since surgeons conducted more than one type of surgery annually, researchers found it difficult to identify what had caused the physical symptoms with complete confidence.
Researchers declared no relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
It’s early days for research on the physical impact of robot-assisted surgery on operators. But a study of surgeons who regularly do this kind of work suggests that surgical robots can be the cause of workplace injuries, despite their reputation for good ergonomic design and low stress on surgeon hands, wrists, backs, and necks
More than half (236) of 432 surveyed surgeons with at least 10 robotic surgeries annually reported physical discomfort associated with robotics consoles, according to a study out of Johns Hopkins University, Baltimore.
Most participants were male (71%) and averaged 48 years of age; their specialties comprised gynecology (68%), urology (20%), general surgery (8%), and others (3%).
Of the 432 participants, they reported physical discomfort in the following areas: fingers, 78%; necks, 74%; upper backs, 53%; and 43%, 34%, and 33% in the lower backs, eyes, and wrists, respectively.
Most of those who responded to the survey (80.8%) performed surgery with the da Vinci Si as their primary robotic system, with the rest using a different iteration of the da Vinci system.
Dr. Lee and his colleagues estimate the high rates of reported discomfort in fingers and necks are because of the structure of the robotics console.
“Due to the absence of tactile feedback at the master controller of the surgeon console, some robotic surgeons might close their fingers excessively when holding objects with instruments,” researchers said. “During the performance of suturing and knot-tying tasks, surgeons must squeeze their grip to hold a needle in place because there is no locking mechanism, which is present with open and laparoscopic needle holders.”
Researchers credit high rates of neck pain to the console as well, which “requires [surgeons] to maintain their neck position in a fixed place for extended period of time.”
While the rate of physical discomfort was 56%, participants rated the ergonomic functions of the console an average of 4 out of 5, with 5 being the highest score.
In contrast, surgeons gave low ratings to the communications systems used by the surgeon and the in-room supporting OR staff – an average of 2.87 out of 5 – noting an urgency for system updates.
Overall, researchers found that surgeons with high confidence in their ergonomic console settings were more likely to feel confident in the use of robotics in their surgical procedures and less likely to report physical discomfort. This finding led researchers to conclude the importance of surgeons new to robot-assisted surgery to receive education in ergonomic settings.
“Formal robotic surgery training programs should include this crucially important knowledge about optimal ergonomic guidelines so that any surgeon starting their training in robotic surgery would have the knowledge to maintain sound body posture and to minimize any physical strains while acquiring the best skill set,” according to Dr. Lee and his associates.
This study was limited by the self-reported data, which could create possible reporting bias, as well as by a small sample size. Since surgeons conducted more than one type of surgery annually, researchers found it difficult to identify what had caused the physical symptoms with complete confidence.
Researchers declared no relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
Key clinical point:
Major finding: Of 432 participating surgeons, 236 (56.1%) reported having physical discomfort during or after using the surgical robot.
Data source: A 20-question, self-reporting survey disseminated to surgeons via email, analyzed using logistic regression.
Disclosures: Researchers declared no relevant financial disclosures.









