User login
Melatonin as a sleep aid: Are you prescribing it correctly?
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
New international consensus document on treating OSA
The Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has issued a new international consensus document (ICD) on obstructive sleep apnea (OSA). The objective is to improve the diagnosis and treatment of one of the most prevalent sleep disorders.
It provides a series of clinical guidelines to help health care professionals make the best decisions for adult patients with OSA. Notably, the authors propose changing the name from sleep apnea syndrome. In recommending the term OSA, they reintroduce the term “obstructive” – to differentiate the disorder from central sleep apnea – and remove the outdated word “syndrome.”
“The definition has also been changed, as it was a bit vague and difficult to understand. And there are significant changes to the treatment and to the diagnostic algorithms – one for primary care and another for sleep units,” Olga Mediano, MD, said in an interview. She is a SEPAR pulmonologist, first author of the ICD, and the coordinator of SEPAR 2022 Year of Intermediate Respiratory Care Units.
Diagnosis in primary care
The ICD indicates that all levels of care must be involved in the management of OSA, a condition in which complete or partial upper airway blockage occurs during sleep, causing the individual to stop breathing for a few seconds. These pauses, which produce hypoxia and sleep fragmentation, increase the risk of workplace and traffic accidents, affect cardiovascular health, and contribute to uncontrolled or resistant hypertension.
The recommendations in the ICD aim at increasing the role of primary care physicians so as to reduce underdiagnosis of OSA in primary care. “The vast majority of patients with OSA haven’t been diagnosed. In fact, those whom we have diagnosed are the patients with the most severe cases – in other words, patients who present with the most symptoms,” said Dr. Mediano. She explained that many patients with OSA don’t consider it a medical condition, so they do not go to the doctor.
“The other big problem is that, before, there was a preconceived notion of the typical OSA patient: A middle-aged obese man who’s fallen asleep in the waiting room. However, there are many other profiles: thin build, women. ... Sleep has a heterogeneous profile, and all profiles need to be known,” said Dr. Mediano. The difficulties in carrying out a sleep study with the various patients are an added problem that the new consensus document also seeks to resolve. “The step we’ve taken is to involve the primary care physician in super-simplified studies to reach more people,” she said. For this, the primary care site must work in coordination with a sleep unit.
“In the super-simplified study, the patient is given a machine to use at home; they hook themselves up to it when they go to sleep. This machine records the number of apnea episodes the patient experiences during the night, as well as the oxygen level. The next day, the patient returns the machine. The data are downloaded to a computer. The software analyzes the breathing pauses that the patient had during the night and automatically gives a series of values that, if very pronounced, as the document indicates, would lead to a diagnosis of OSA. Once diagnosed by a primary care physician, the patient is referred to a sleep unit where treatment can then be assessed,” explained Dr. Mediano.
Different treatments
The new ICD’s approach incorporates therapeutic alternatives as well. Until now, many consensus documents and clinical guidelines have focused on continuous positive airway pressure therapy, in which a machine delivers continuous airflow to help keep the patient’s airway open and unobstructed during sleep. Some guidelines recommend its use, and others do not. “However, in this new document, management of the patient is much more multidisciplinary. What changes, with respect to the treatment, is the philosophy. It’s not one single type of treatment; rather, other therapeutic options are kept in mind,” said Dr. Mediano.
First, treatment of reversible causes of OSA must be offered. The conditions that lead to OSA and that can be reversed are addressed. These include overweight and obesity; heavy drinking; tonsillar hypertrophy, or severe dental or facial alterations, for which surgery can be considered; and gastroesophageal reflux or hypothyroidism, both of which can be treated. “For example, the leading cause of sleep apnea is obesity. If we can get the patient to lose weight, that can end up making the OSA go away. What does the document say? Well, you have to try to implement intensive strategies regarding diet, exercise, etc. And if that’s not enough, you need to consider using drugs or even bariatric surgery,” said Dr. Mediano.
“If there’s no one definitive treatment, we highly recommend that all patients implement hygienic-dietary measures and then assess all the therapeutic options. In some cases, several can be in place at the same time,” she said. Various medical specialists can play a role in the treatment of OSA, said Dr. Mediano. They include otolaryngologists, maxillofacial surgeons, dentists, cardiologists, and neurophysiologists, to mention a few.
A website has been created to explain the ICD. There, visitors will be able to find the most up-to-date version of the ICD as well as related information, news, and materials.
A version of this article appeared on Medscape.com. This article was translated from Univadis Spain.
The Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has issued a new international consensus document (ICD) on obstructive sleep apnea (OSA). The objective is to improve the diagnosis and treatment of one of the most prevalent sleep disorders.
It provides a series of clinical guidelines to help health care professionals make the best decisions for adult patients with OSA. Notably, the authors propose changing the name from sleep apnea syndrome. In recommending the term OSA, they reintroduce the term “obstructive” – to differentiate the disorder from central sleep apnea – and remove the outdated word “syndrome.”
“The definition has also been changed, as it was a bit vague and difficult to understand. And there are significant changes to the treatment and to the diagnostic algorithms – one for primary care and another for sleep units,” Olga Mediano, MD, said in an interview. She is a SEPAR pulmonologist, first author of the ICD, and the coordinator of SEPAR 2022 Year of Intermediate Respiratory Care Units.
Diagnosis in primary care
The ICD indicates that all levels of care must be involved in the management of OSA, a condition in which complete or partial upper airway blockage occurs during sleep, causing the individual to stop breathing for a few seconds. These pauses, which produce hypoxia and sleep fragmentation, increase the risk of workplace and traffic accidents, affect cardiovascular health, and contribute to uncontrolled or resistant hypertension.
The recommendations in the ICD aim at increasing the role of primary care physicians so as to reduce underdiagnosis of OSA in primary care. “The vast majority of patients with OSA haven’t been diagnosed. In fact, those whom we have diagnosed are the patients with the most severe cases – in other words, patients who present with the most symptoms,” said Dr. Mediano. She explained that many patients with OSA don’t consider it a medical condition, so they do not go to the doctor.
“The other big problem is that, before, there was a preconceived notion of the typical OSA patient: A middle-aged obese man who’s fallen asleep in the waiting room. However, there are many other profiles: thin build, women. ... Sleep has a heterogeneous profile, and all profiles need to be known,” said Dr. Mediano. The difficulties in carrying out a sleep study with the various patients are an added problem that the new consensus document also seeks to resolve. “The step we’ve taken is to involve the primary care physician in super-simplified studies to reach more people,” she said. For this, the primary care site must work in coordination with a sleep unit.
“In the super-simplified study, the patient is given a machine to use at home; they hook themselves up to it when they go to sleep. This machine records the number of apnea episodes the patient experiences during the night, as well as the oxygen level. The next day, the patient returns the machine. The data are downloaded to a computer. The software analyzes the breathing pauses that the patient had during the night and automatically gives a series of values that, if very pronounced, as the document indicates, would lead to a diagnosis of OSA. Once diagnosed by a primary care physician, the patient is referred to a sleep unit where treatment can then be assessed,” explained Dr. Mediano.
Different treatments
The new ICD’s approach incorporates therapeutic alternatives as well. Until now, many consensus documents and clinical guidelines have focused on continuous positive airway pressure therapy, in which a machine delivers continuous airflow to help keep the patient’s airway open and unobstructed during sleep. Some guidelines recommend its use, and others do not. “However, in this new document, management of the patient is much more multidisciplinary. What changes, with respect to the treatment, is the philosophy. It’s not one single type of treatment; rather, other therapeutic options are kept in mind,” said Dr. Mediano.
First, treatment of reversible causes of OSA must be offered. The conditions that lead to OSA and that can be reversed are addressed. These include overweight and obesity; heavy drinking; tonsillar hypertrophy, or severe dental or facial alterations, for which surgery can be considered; and gastroesophageal reflux or hypothyroidism, both of which can be treated. “For example, the leading cause of sleep apnea is obesity. If we can get the patient to lose weight, that can end up making the OSA go away. What does the document say? Well, you have to try to implement intensive strategies regarding diet, exercise, etc. And if that’s not enough, you need to consider using drugs or even bariatric surgery,” said Dr. Mediano.
“If there’s no one definitive treatment, we highly recommend that all patients implement hygienic-dietary measures and then assess all the therapeutic options. In some cases, several can be in place at the same time,” she said. Various medical specialists can play a role in the treatment of OSA, said Dr. Mediano. They include otolaryngologists, maxillofacial surgeons, dentists, cardiologists, and neurophysiologists, to mention a few.
A website has been created to explain the ICD. There, visitors will be able to find the most up-to-date version of the ICD as well as related information, news, and materials.
A version of this article appeared on Medscape.com. This article was translated from Univadis Spain.
The Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has issued a new international consensus document (ICD) on obstructive sleep apnea (OSA). The objective is to improve the diagnosis and treatment of one of the most prevalent sleep disorders.
It provides a series of clinical guidelines to help health care professionals make the best decisions for adult patients with OSA. Notably, the authors propose changing the name from sleep apnea syndrome. In recommending the term OSA, they reintroduce the term “obstructive” – to differentiate the disorder from central sleep apnea – and remove the outdated word “syndrome.”
“The definition has also been changed, as it was a bit vague and difficult to understand. And there are significant changes to the treatment and to the diagnostic algorithms – one for primary care and another for sleep units,” Olga Mediano, MD, said in an interview. She is a SEPAR pulmonologist, first author of the ICD, and the coordinator of SEPAR 2022 Year of Intermediate Respiratory Care Units.
Diagnosis in primary care
The ICD indicates that all levels of care must be involved in the management of OSA, a condition in which complete or partial upper airway blockage occurs during sleep, causing the individual to stop breathing for a few seconds. These pauses, which produce hypoxia and sleep fragmentation, increase the risk of workplace and traffic accidents, affect cardiovascular health, and contribute to uncontrolled or resistant hypertension.
The recommendations in the ICD aim at increasing the role of primary care physicians so as to reduce underdiagnosis of OSA in primary care. “The vast majority of patients with OSA haven’t been diagnosed. In fact, those whom we have diagnosed are the patients with the most severe cases – in other words, patients who present with the most symptoms,” said Dr. Mediano. She explained that many patients with OSA don’t consider it a medical condition, so they do not go to the doctor.
“The other big problem is that, before, there was a preconceived notion of the typical OSA patient: A middle-aged obese man who’s fallen asleep in the waiting room. However, there are many other profiles: thin build, women. ... Sleep has a heterogeneous profile, and all profiles need to be known,” said Dr. Mediano. The difficulties in carrying out a sleep study with the various patients are an added problem that the new consensus document also seeks to resolve. “The step we’ve taken is to involve the primary care physician in super-simplified studies to reach more people,” she said. For this, the primary care site must work in coordination with a sleep unit.
“In the super-simplified study, the patient is given a machine to use at home; they hook themselves up to it when they go to sleep. This machine records the number of apnea episodes the patient experiences during the night, as well as the oxygen level. The next day, the patient returns the machine. The data are downloaded to a computer. The software analyzes the breathing pauses that the patient had during the night and automatically gives a series of values that, if very pronounced, as the document indicates, would lead to a diagnosis of OSA. Once diagnosed by a primary care physician, the patient is referred to a sleep unit where treatment can then be assessed,” explained Dr. Mediano.
Different treatments
The new ICD’s approach incorporates therapeutic alternatives as well. Until now, many consensus documents and clinical guidelines have focused on continuous positive airway pressure therapy, in which a machine delivers continuous airflow to help keep the patient’s airway open and unobstructed during sleep. Some guidelines recommend its use, and others do not. “However, in this new document, management of the patient is much more multidisciplinary. What changes, with respect to the treatment, is the philosophy. It’s not one single type of treatment; rather, other therapeutic options are kept in mind,” said Dr. Mediano.
First, treatment of reversible causes of OSA must be offered. The conditions that lead to OSA and that can be reversed are addressed. These include overweight and obesity; heavy drinking; tonsillar hypertrophy, or severe dental or facial alterations, for which surgery can be considered; and gastroesophageal reflux or hypothyroidism, both of which can be treated. “For example, the leading cause of sleep apnea is obesity. If we can get the patient to lose weight, that can end up making the OSA go away. What does the document say? Well, you have to try to implement intensive strategies regarding diet, exercise, etc. And if that’s not enough, you need to consider using drugs or even bariatric surgery,” said Dr. Mediano.
“If there’s no one definitive treatment, we highly recommend that all patients implement hygienic-dietary measures and then assess all the therapeutic options. In some cases, several can be in place at the same time,” she said. Various medical specialists can play a role in the treatment of OSA, said Dr. Mediano. They include otolaryngologists, maxillofacial surgeons, dentists, cardiologists, and neurophysiologists, to mention a few.
A website has been created to explain the ICD. There, visitors will be able to find the most up-to-date version of the ICD as well as related information, news, and materials.
A version of this article appeared on Medscape.com. This article was translated from Univadis Spain.
How does not getting enough sleep affect the developing brain?
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
FROM THE LANCET CHILD & ADOLESCENT HEALTH
Poor sleep raises risk for fatty liver disease
Sleep behaviors, both individually and combined, are associated with an increased risk of developing metabolic dysfunction–associated fatty liver disease (MAFLD), according to a Chinese analysis that suggests the effect may be independent of obesity.
Yan Liu, PhD, from the School of Public Health at Sun Yat-sen University in Guangzhou, China, and colleagues studied data on over 5,000 individuals who self-reported sleep behaviors and underwent liver ultrasound.
, increasing the risk by 37%, 59%, and 17%, respectively, whereas people with both poor nighttime sleep and prolonged daytime napping had the “highest risk for developing fatty liver disease,” said Dr. Liu in a press release.
In contrast, having any of six healthy sleep behaviors decreased the risk by 16% each, and even a “moderate improvement in sleep quality was related to a 29% reduction in the risk for fatty liver disease,” he added.
The research, published online in the Journal of Clinical Endocrinology & Metabolism, also indicated that obesity accounted for only one fifth of the effect of sleep quality on MAFLD risk.
Rise in unhealthy lifestyles leads to increase in MALFD
The authors write that MAFLD is the “leading chronic liver disease worldwide,” affecting around a quarter of the adult population, and may lead to end-stage liver diseases and extrahepatic complications, thus “posing a major health and economic burden.”
Moreover, the disease prevalence is “soaring at an unanticipated rate,” increasing from 18% to 29% in China over the past decade, because of a “rapid rise in unhealthy lifestyles,” the authors note.
Sleep disturbance is increasingly prevalent, “and an emerging contributor to multiple metabolic disorders,” with insomnia and habitual snoring, for example, positively correlated with hypertension, impaired glucose metabolism, and dyslipidemia, report the authors.
However, whether sleep quality, which includes “several metabolic-related sleep behaviors,” constitutes an independent risk for MAFLD “over and above” the effect of obesity remains unclear.
To investigate further, the researchers examined data from the baseline survey of the community-based, prospective South China Cohort study, which was conducted in four regions of Southern China and involved 5,430 individuals aged 30-79 years.
Between March 2018 and October 2019, the participants self-reported sleep behaviors on the Pittsburgh Sleep Quality Index questionnaire and underwent ultrasound examination of the liver.
MAFLD was diagnosed in those with hepatic steatosis and one of the following:
- Overweight/obesity, defined by this study as a body mass index greater than or equal to 23 kg/m2.
- Presence of diabetes.
- Evidence of metabolic dysregulation.
After excluding patients with insufficient data, and those with a history of liver cirrhosis, hepatectomy, or liver cancer, among others, the team included 5,011 individuals with an average age of 64 years and a mean body mass index of 24.31 kg/m2. Forty percent were male.
Obesity was present in 13% of participants, whereas 15% had diabetes, 58% hypertension, and 35% metabolic syndrome.
MAFLD was diagnosed in 28% of the study population. They were older, more likely to be female with a higher education, and had a higher prevalence of preexisting metabolic disorders and worse metabolic profiles, than those without the disease.
Turning to the associations between sleep and the risk of MAFLD, the researchers say that “in contrast to previous reports, neither shorter nor longer sleep duration was found to be associated with the risk for MAFLD.”
However, after adjusting for demographics, lifestyles, medication, and preexisting metabolic comorbidities including hypertension, diabetes, and obesity, they found that the risk of MAFLD was significantly associated with late bedtime (defined as after 10 p.m.), at an odds ratio of 1.37 (P < .05).
MAFLD was also linked to snoring, at an odds ratio of 1.59, and to daytime napping for longer than 30 minutes, at an odds ratio of 1.17 (P < .05 for both).
When the team compared low-risk and high-risk sleep factors, they found that participants who had an early bedtime, slept 7-8 hours per night, never or rarely had insomnia or snoring, had infrequent daytime sleepiness, and daytime napping of half-hour or less had an odds ratio for MAFLD vs. other participants of 0.64 (P < .05).
Combining those factors into a healthy sleep score, the team found that each additional increase of healthy sleep score was associated with a fully adjusted odds ratio for MAFLD of 0.84 (P < .05).
In contrast, individuals with poor nocturnal sleep patterns and prolonged daytime napping had a higher risk for developing MAFLD, compared with those with a healthy nocturnal sleep pattern and daytime napping of half-hour or less, at an odds ratio of 2.38 (P < .05).
Further analysis indicated that individuals with a sedentary lifestyle and central obesity had a higher risk of MAFLD, but that the presence of obesity accounted for only 20.8% of the total effect of sleep quality on the risk of MAFLD.
“Taken together, our results suggests that obesity only partially mediates the effect of overall sleep quality on MAFLD,” the authors write.
“Given that large proportions of subjects suffering from poor sleep quality are underdiagnosed and undertreated, our study calls for more research into this field and strategies to improve sleep quality,” Dr. Liu said.
The study was supported by the “National Key R&D Program” of China, the Fundamental Research Funds for the Central Universities (Sun Yat-sen University), Natural Science Foundation of Guangdong Province, the Key Project of Medicine Discipline of Guangzhou, and Basic Research Project of Key Laboratory of Guangzhou.
The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sleep behaviors, both individually and combined, are associated with an increased risk of developing metabolic dysfunction–associated fatty liver disease (MAFLD), according to a Chinese analysis that suggests the effect may be independent of obesity.
Yan Liu, PhD, from the School of Public Health at Sun Yat-sen University in Guangzhou, China, and colleagues studied data on over 5,000 individuals who self-reported sleep behaviors and underwent liver ultrasound.
, increasing the risk by 37%, 59%, and 17%, respectively, whereas people with both poor nighttime sleep and prolonged daytime napping had the “highest risk for developing fatty liver disease,” said Dr. Liu in a press release.
In contrast, having any of six healthy sleep behaviors decreased the risk by 16% each, and even a “moderate improvement in sleep quality was related to a 29% reduction in the risk for fatty liver disease,” he added.
The research, published online in the Journal of Clinical Endocrinology & Metabolism, also indicated that obesity accounted for only one fifth of the effect of sleep quality on MAFLD risk.
Rise in unhealthy lifestyles leads to increase in MALFD
The authors write that MAFLD is the “leading chronic liver disease worldwide,” affecting around a quarter of the adult population, and may lead to end-stage liver diseases and extrahepatic complications, thus “posing a major health and economic burden.”
Moreover, the disease prevalence is “soaring at an unanticipated rate,” increasing from 18% to 29% in China over the past decade, because of a “rapid rise in unhealthy lifestyles,” the authors note.
Sleep disturbance is increasingly prevalent, “and an emerging contributor to multiple metabolic disorders,” with insomnia and habitual snoring, for example, positively correlated with hypertension, impaired glucose metabolism, and dyslipidemia, report the authors.
However, whether sleep quality, which includes “several metabolic-related sleep behaviors,” constitutes an independent risk for MAFLD “over and above” the effect of obesity remains unclear.
To investigate further, the researchers examined data from the baseline survey of the community-based, prospective South China Cohort study, which was conducted in four regions of Southern China and involved 5,430 individuals aged 30-79 years.
Between March 2018 and October 2019, the participants self-reported sleep behaviors on the Pittsburgh Sleep Quality Index questionnaire and underwent ultrasound examination of the liver.
MAFLD was diagnosed in those with hepatic steatosis and one of the following:
- Overweight/obesity, defined by this study as a body mass index greater than or equal to 23 kg/m2.
- Presence of diabetes.
- Evidence of metabolic dysregulation.
After excluding patients with insufficient data, and those with a history of liver cirrhosis, hepatectomy, or liver cancer, among others, the team included 5,011 individuals with an average age of 64 years and a mean body mass index of 24.31 kg/m2. Forty percent were male.
Obesity was present in 13% of participants, whereas 15% had diabetes, 58% hypertension, and 35% metabolic syndrome.
MAFLD was diagnosed in 28% of the study population. They were older, more likely to be female with a higher education, and had a higher prevalence of preexisting metabolic disorders and worse metabolic profiles, than those without the disease.
Turning to the associations between sleep and the risk of MAFLD, the researchers say that “in contrast to previous reports, neither shorter nor longer sleep duration was found to be associated with the risk for MAFLD.”
However, after adjusting for demographics, lifestyles, medication, and preexisting metabolic comorbidities including hypertension, diabetes, and obesity, they found that the risk of MAFLD was significantly associated with late bedtime (defined as after 10 p.m.), at an odds ratio of 1.37 (P < .05).
MAFLD was also linked to snoring, at an odds ratio of 1.59, and to daytime napping for longer than 30 minutes, at an odds ratio of 1.17 (P < .05 for both).
When the team compared low-risk and high-risk sleep factors, they found that participants who had an early bedtime, slept 7-8 hours per night, never or rarely had insomnia or snoring, had infrequent daytime sleepiness, and daytime napping of half-hour or less had an odds ratio for MAFLD vs. other participants of 0.64 (P < .05).
Combining those factors into a healthy sleep score, the team found that each additional increase of healthy sleep score was associated with a fully adjusted odds ratio for MAFLD of 0.84 (P < .05).
In contrast, individuals with poor nocturnal sleep patterns and prolonged daytime napping had a higher risk for developing MAFLD, compared with those with a healthy nocturnal sleep pattern and daytime napping of half-hour or less, at an odds ratio of 2.38 (P < .05).
Further analysis indicated that individuals with a sedentary lifestyle and central obesity had a higher risk of MAFLD, but that the presence of obesity accounted for only 20.8% of the total effect of sleep quality on the risk of MAFLD.
“Taken together, our results suggests that obesity only partially mediates the effect of overall sleep quality on MAFLD,” the authors write.
“Given that large proportions of subjects suffering from poor sleep quality are underdiagnosed and undertreated, our study calls for more research into this field and strategies to improve sleep quality,” Dr. Liu said.
The study was supported by the “National Key R&D Program” of China, the Fundamental Research Funds for the Central Universities (Sun Yat-sen University), Natural Science Foundation of Guangdong Province, the Key Project of Medicine Discipline of Guangzhou, and Basic Research Project of Key Laboratory of Guangzhou.
The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sleep behaviors, both individually and combined, are associated with an increased risk of developing metabolic dysfunction–associated fatty liver disease (MAFLD), according to a Chinese analysis that suggests the effect may be independent of obesity.
Yan Liu, PhD, from the School of Public Health at Sun Yat-sen University in Guangzhou, China, and colleagues studied data on over 5,000 individuals who self-reported sleep behaviors and underwent liver ultrasound.
, increasing the risk by 37%, 59%, and 17%, respectively, whereas people with both poor nighttime sleep and prolonged daytime napping had the “highest risk for developing fatty liver disease,” said Dr. Liu in a press release.
In contrast, having any of six healthy sleep behaviors decreased the risk by 16% each, and even a “moderate improvement in sleep quality was related to a 29% reduction in the risk for fatty liver disease,” he added.
The research, published online in the Journal of Clinical Endocrinology & Metabolism, also indicated that obesity accounted for only one fifth of the effect of sleep quality on MAFLD risk.
Rise in unhealthy lifestyles leads to increase in MALFD
The authors write that MAFLD is the “leading chronic liver disease worldwide,” affecting around a quarter of the adult population, and may lead to end-stage liver diseases and extrahepatic complications, thus “posing a major health and economic burden.”
Moreover, the disease prevalence is “soaring at an unanticipated rate,” increasing from 18% to 29% in China over the past decade, because of a “rapid rise in unhealthy lifestyles,” the authors note.
Sleep disturbance is increasingly prevalent, “and an emerging contributor to multiple metabolic disorders,” with insomnia and habitual snoring, for example, positively correlated with hypertension, impaired glucose metabolism, and dyslipidemia, report the authors.
However, whether sleep quality, which includes “several metabolic-related sleep behaviors,” constitutes an independent risk for MAFLD “over and above” the effect of obesity remains unclear.
To investigate further, the researchers examined data from the baseline survey of the community-based, prospective South China Cohort study, which was conducted in four regions of Southern China and involved 5,430 individuals aged 30-79 years.
Between March 2018 and October 2019, the participants self-reported sleep behaviors on the Pittsburgh Sleep Quality Index questionnaire and underwent ultrasound examination of the liver.
MAFLD was diagnosed in those with hepatic steatosis and one of the following:
- Overweight/obesity, defined by this study as a body mass index greater than or equal to 23 kg/m2.
- Presence of diabetes.
- Evidence of metabolic dysregulation.
After excluding patients with insufficient data, and those with a history of liver cirrhosis, hepatectomy, or liver cancer, among others, the team included 5,011 individuals with an average age of 64 years and a mean body mass index of 24.31 kg/m2. Forty percent were male.
Obesity was present in 13% of participants, whereas 15% had diabetes, 58% hypertension, and 35% metabolic syndrome.
MAFLD was diagnosed in 28% of the study population. They were older, more likely to be female with a higher education, and had a higher prevalence of preexisting metabolic disorders and worse metabolic profiles, than those without the disease.
Turning to the associations between sleep and the risk of MAFLD, the researchers say that “in contrast to previous reports, neither shorter nor longer sleep duration was found to be associated with the risk for MAFLD.”
However, after adjusting for demographics, lifestyles, medication, and preexisting metabolic comorbidities including hypertension, diabetes, and obesity, they found that the risk of MAFLD was significantly associated with late bedtime (defined as after 10 p.m.), at an odds ratio of 1.37 (P < .05).
MAFLD was also linked to snoring, at an odds ratio of 1.59, and to daytime napping for longer than 30 minutes, at an odds ratio of 1.17 (P < .05 for both).
When the team compared low-risk and high-risk sleep factors, they found that participants who had an early bedtime, slept 7-8 hours per night, never or rarely had insomnia or snoring, had infrequent daytime sleepiness, and daytime napping of half-hour or less had an odds ratio for MAFLD vs. other participants of 0.64 (P < .05).
Combining those factors into a healthy sleep score, the team found that each additional increase of healthy sleep score was associated with a fully adjusted odds ratio for MAFLD of 0.84 (P < .05).
In contrast, individuals with poor nocturnal sleep patterns and prolonged daytime napping had a higher risk for developing MAFLD, compared with those with a healthy nocturnal sleep pattern and daytime napping of half-hour or less, at an odds ratio of 2.38 (P < .05).
Further analysis indicated that individuals with a sedentary lifestyle and central obesity had a higher risk of MAFLD, but that the presence of obesity accounted for only 20.8% of the total effect of sleep quality on the risk of MAFLD.
“Taken together, our results suggests that obesity only partially mediates the effect of overall sleep quality on MAFLD,” the authors write.
“Given that large proportions of subjects suffering from poor sleep quality are underdiagnosed and undertreated, our study calls for more research into this field and strategies to improve sleep quality,” Dr. Liu said.
The study was supported by the “National Key R&D Program” of China, the Fundamental Research Funds for the Central Universities (Sun Yat-sen University), Natural Science Foundation of Guangdong Province, the Key Project of Medicine Discipline of Guangzhou, and Basic Research Project of Key Laboratory of Guangzhou.
The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Growing pains? ... Rubbish
I’m pretty sure my ancestors came from Europe. And, as far as I know, I have no relatives in Australia. But, I must have some cosmic relationship with the Land Down Under because as I review articles for these columns I have an uncanny attraction to those coming out of Australia. Most of them are about sleep, one of my obsessions, and in general they address simple questions that no one has thought to ask.
My most recent Australia-based nugget appeared in the August edition of Pediatrics.
The researchers in Sidney were seeking to define “growing pains” by embarking on an extensive review of the medical literature. Beginning with thousands of articles, they winnowed these down to 145 studies. They found “there was extremely poor consensus between studies.” The most consistent components were the lower limb, bilaterality, evening onset, a normal physical assessment, and an episodic or recurrent course. However, all of these factors were mentioned in 50% or less of the articles they reviewed. The investigators wisely concluded that clinicians “should be wary of relying on the diagnosis to direct treatment decisions.”
This may seem like one small step for pediatrics. You may have reassured parents that none of your patients ever died of “growing pains” and the condition would eventually resolve. Hopefully, you were correct and that your case rate fatality is zero. But I suspect it wouldn’t take too long to unearth a wealth of malpractices cases in which another pediatrician’s patient died with an illness whose eventual discovery was tragically delayed by a period of false reassurance and diagnosis that the child merely had growing pains.
I can’t remember which of my sage instructors told me to never use “growing pains” as a diagnosis. It may have just been something I stumbled upon as my clinical experience grew. While holding firm to my commitment to never use it as a diagnosis, it became abundantly clear that I was seeing a large group of children (toddlers to early adolescents) who were experiencing lower leg pains in the early evening, often bad enough to wake them.
It took a bit longer to discover that most often these painful episodes occurred in children who were acutely or chronically sleep deprived. Occasionally, the pain would come on days in which the child had been unusually physically active. However, in most cases there was little correlation with lower limb activity.
I will admit that my observations were colored by my growing obsession that sleep deprivation is the root of many evils, including the phenomenon known as attention-deficit/hyperactivity disorder. I was even bold enough to include it in my one of the books I have written (Is My Child Overtired? Simon & Schuster, 2001). Nonetheless, I am still convinced that every investigation of a child with evening leg pains should include a thorough history of the child’s sleep history.
The bottom line is that these Australian researchers have done us a great favor with their research. However, I think they should have made a bolder statement in their conclusion. It is clear to me that “growing pains” should be removed as a diagnosis and no longer be reimbursed by third-party payers.
The void created by that action should spur some research into a better-defined diagnosis of the condition. If you want to use my tack and label it “nocturnal leg pains of childhood” and suggest better sleep hygiene, I will be flattered. But more importantly, take the time to take a good history, do a thorough exam, and then follow up, follow up, follow up, until the problem resolves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I’m pretty sure my ancestors came from Europe. And, as far as I know, I have no relatives in Australia. But, I must have some cosmic relationship with the Land Down Under because as I review articles for these columns I have an uncanny attraction to those coming out of Australia. Most of them are about sleep, one of my obsessions, and in general they address simple questions that no one has thought to ask.
My most recent Australia-based nugget appeared in the August edition of Pediatrics.
The researchers in Sidney were seeking to define “growing pains” by embarking on an extensive review of the medical literature. Beginning with thousands of articles, they winnowed these down to 145 studies. They found “there was extremely poor consensus between studies.” The most consistent components were the lower limb, bilaterality, evening onset, a normal physical assessment, and an episodic or recurrent course. However, all of these factors were mentioned in 50% or less of the articles they reviewed. The investigators wisely concluded that clinicians “should be wary of relying on the diagnosis to direct treatment decisions.”
This may seem like one small step for pediatrics. You may have reassured parents that none of your patients ever died of “growing pains” and the condition would eventually resolve. Hopefully, you were correct and that your case rate fatality is zero. But I suspect it wouldn’t take too long to unearth a wealth of malpractices cases in which another pediatrician’s patient died with an illness whose eventual discovery was tragically delayed by a period of false reassurance and diagnosis that the child merely had growing pains.
I can’t remember which of my sage instructors told me to never use “growing pains” as a diagnosis. It may have just been something I stumbled upon as my clinical experience grew. While holding firm to my commitment to never use it as a diagnosis, it became abundantly clear that I was seeing a large group of children (toddlers to early adolescents) who were experiencing lower leg pains in the early evening, often bad enough to wake them.
It took a bit longer to discover that most often these painful episodes occurred in children who were acutely or chronically sleep deprived. Occasionally, the pain would come on days in which the child had been unusually physically active. However, in most cases there was little correlation with lower limb activity.
I will admit that my observations were colored by my growing obsession that sleep deprivation is the root of many evils, including the phenomenon known as attention-deficit/hyperactivity disorder. I was even bold enough to include it in my one of the books I have written (Is My Child Overtired? Simon & Schuster, 2001). Nonetheless, I am still convinced that every investigation of a child with evening leg pains should include a thorough history of the child’s sleep history.
The bottom line is that these Australian researchers have done us a great favor with their research. However, I think they should have made a bolder statement in their conclusion. It is clear to me that “growing pains” should be removed as a diagnosis and no longer be reimbursed by third-party payers.
The void created by that action should spur some research into a better-defined diagnosis of the condition. If you want to use my tack and label it “nocturnal leg pains of childhood” and suggest better sleep hygiene, I will be flattered. But more importantly, take the time to take a good history, do a thorough exam, and then follow up, follow up, follow up, until the problem resolves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I’m pretty sure my ancestors came from Europe. And, as far as I know, I have no relatives in Australia. But, I must have some cosmic relationship with the Land Down Under because as I review articles for these columns I have an uncanny attraction to those coming out of Australia. Most of them are about sleep, one of my obsessions, and in general they address simple questions that no one has thought to ask.
My most recent Australia-based nugget appeared in the August edition of Pediatrics.
The researchers in Sidney were seeking to define “growing pains” by embarking on an extensive review of the medical literature. Beginning with thousands of articles, they winnowed these down to 145 studies. They found “there was extremely poor consensus between studies.” The most consistent components were the lower limb, bilaterality, evening onset, a normal physical assessment, and an episodic or recurrent course. However, all of these factors were mentioned in 50% or less of the articles they reviewed. The investigators wisely concluded that clinicians “should be wary of relying on the diagnosis to direct treatment decisions.”
This may seem like one small step for pediatrics. You may have reassured parents that none of your patients ever died of “growing pains” and the condition would eventually resolve. Hopefully, you were correct and that your case rate fatality is zero. But I suspect it wouldn’t take too long to unearth a wealth of malpractices cases in which another pediatrician’s patient died with an illness whose eventual discovery was tragically delayed by a period of false reassurance and diagnosis that the child merely had growing pains.
I can’t remember which of my sage instructors told me to never use “growing pains” as a diagnosis. It may have just been something I stumbled upon as my clinical experience grew. While holding firm to my commitment to never use it as a diagnosis, it became abundantly clear that I was seeing a large group of children (toddlers to early adolescents) who were experiencing lower leg pains in the early evening, often bad enough to wake them.
It took a bit longer to discover that most often these painful episodes occurred in children who were acutely or chronically sleep deprived. Occasionally, the pain would come on days in which the child had been unusually physically active. However, in most cases there was little correlation with lower limb activity.
I will admit that my observations were colored by my growing obsession that sleep deprivation is the root of many evils, including the phenomenon known as attention-deficit/hyperactivity disorder. I was even bold enough to include it in my one of the books I have written (Is My Child Overtired? Simon & Schuster, 2001). Nonetheless, I am still convinced that every investigation of a child with evening leg pains should include a thorough history of the child’s sleep history.
The bottom line is that these Australian researchers have done us a great favor with their research. However, I think they should have made a bolder statement in their conclusion. It is clear to me that “growing pains” should be removed as a diagnosis and no longer be reimbursed by third-party payers.
The void created by that action should spur some research into a better-defined diagnosis of the condition. If you want to use my tack and label it “nocturnal leg pains of childhood” and suggest better sleep hygiene, I will be flattered. But more importantly, take the time to take a good history, do a thorough exam, and then follow up, follow up, follow up, until the problem resolves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Reassessing benzodiazepines: What role should this medication class play in psychiatry?
Many psychiatrists have had the grim experience of a newly referred patient explaining that her (and it is most often “her”) primary care doctor has been prescribing lorazepam 8 mg per day or alprazolam 6 mg per day and is sending her to you for help with ongoing anxiety. For conscientious psychiatrists, this means the beginning of a long tapering process along with a great deal of reassuring of a patient who is terrified of feeling overwhelmed with anxiety. The same problem occurs with patients taking large doses of sedatives who are still unable to sleep.
Mark Olfson and coauthors quantified benzodiazepine use in the United States in 2008 using a large prescription database, and found that 5.2% of adults between 18 and 80 years old were taking these drugs.1 The percentage increased with age, to 8.7% of those 65-80 years, in whom 31% received long-term prescriptions from a psychiatrist. Benzodiazepine use was twice as prevalent in women, compared with men. This occurs despite peer-reviewed publications and articles in the popular press regarding the risks of long-term benzodiazepine use in the elderly. Fang-Yu Lin and coauthors documented a 2.23-fold higher risk of hip fracture in zolpidem users that increased with age; elderly users had a 21-fold higher incidence of fracture, compared with younger users, and were twice as likely to sustain a fracture than elderly nonusers.2
Rashona Thomas and Edid Ramos-Rivas reviewed the risks of benzodiazepines in older patients with insomnia and document the increase in serious adverse events such as falls, fractures, and cognitive and behavioral changes.3 Many patients have ongoing prescriptions that make discontinuation difficult, given the potential for withdrawal agitation, seizures, insomnia, nightmares and even psychosis.
Greta Bushnell and coauthors pointed to the problem of simultaneous prescribing of a new antidepressant with a benzodiazepine by 10% of doctors initiating antidepressants.4 Over 12% of this group of patients continued benzodiazepines long term, even though there was no difference in the response to antidepressant treatment at 6 months. Those with long-term benzodiazepine use were also more likely to have recent prescriptions for opiates.
A Finnish research team found that 34% of middle-aged and 55% of elderly people developed long-term use of benzodiazepines after an initial prescription.5 Those who became long-term users were more often older male receivers of social benefits, with psychiatric comorbidities and substance abuse histories.
Kevin Xu and coauthors reviewed a National Health and Nutrition Examination Survey dataset from 1999 to 2015 with follow-up on over 5,000 individuals in that period.6 They found doubling of all-cause mortality in users of benzodiazepines with or without accompanying use of opiates, a statistically significant increase.
Perhaps most alarming is the increased risk for Alzheimer’s dementia diagnosis in users of benzodiazepines. Two separate studies (Billoti de Gage and colleagues and Ettcheto and colleagues7,8) provided reviews of evidence for the relationship between use of benzodiazepines and development of dementia, and repeated warnings about close monitoring of patients and the need for alternative treatments for anxiety and insomnia in the elderly.
Be alert to underlying issues
Overburdened primary practitioners faced with complaints about sleep and anxiety understandably turn to medication rather than taking time to discuss the reasons for these problems or to describe nonmedication approaches to relief of symptoms. Even insured patients may have very limited options for “covered” psychiatric consultation, as many competent psychiatrists have moved to a cash-only system. It is easier to renew prescriptions than to counsel patients or refer them, and many primary care practitioners have limited experience with diagnosing causes of anxiety and insomnia, much less alternative medication approaches.
Psychiatrists should be aware of the frequency of underlying mood disorders that include sleep and anxiety as prominent symptoms; in fact, these symptoms are often what motivates patients to pursue treatment. It is critical to obtain not only a personal history of symptoms beginning in childhood up to the present, but also a family history of mood and anxiety problems. Mood dysregulation disorders are highly hereditary and a family history of mania or psychosis should raise concern about the cause of symptoms in one’s patient. A strong personal and/or family history of alcohol abuse and dependence may cover underlying undiagnosed mood dysregulation. Primary care physicians may not recognize mood dysregulation unless a patient is clearly manic or psychotic.
There is a cohort of patients who do well on antidepressant medication, but anorgasmia, fatigue, and emotional blunting are common side effects that affect compliance. When patients have unexpected responses to SSRI medications such as euphoria, agitation, anxiety, insomnia, and more prominent mood swings, primary care physicians may add a benzodiazepine, expecting the problem to abate with time. Unfortunately, this often leads to ongoing use of benzodiazepines, since attempts to stop them causes withdrawal effects that are indistinguishable from the original anxiety symptoms.
Most psychiatrists are aware that some patients need mood stabilization rather than mood elevation to maintain an adequate baseline mood. Lithium, anticonvulsants, and second-generation antipsychotics may be effective without adding antidepressant medication. Managing dosing and side effects requires time for follow-up visits with patients after initiating treatment but leads to more stability and better outcomes.
Benzodiazepines are appropriate and helpful in situations that cause transient anxiety and with patients who have done poorly with other options. Intermittent use is key to avoiding tolerance and inevitable dose increases. Some individuals can take low daily doses that are harmless, though these likely only prevent withdrawal rather than preventing anxiety. The placebo effect of taking a pill is powerful. And some patients take more doses than they admit to. Most practitioners have heard stories about the alprazolam that was accidentally spilled into the sink or the prescription bottle of diazepam that was lost or the lorazepam supply that was stolen by the babysitter.
These concepts are illustrated in case examples below.
Case one
Ms. A, a 55-year-old married female business administrator, admitted to using zolpidem at 40 mg per night for the past several months. She began with the typical dose of 10 mg at bedtime prescribed by her internist, but after several weeks, needed an additional 10 mg at 2 a.m. to stay asleep. As weeks passed, she found that she needed an additional 20 mg when she awoke at 2 a.m. Within months, she needed 20 mg to initiate sleep and 20 mg to maintain sleep. She obtained extra zolpidem from her gynecologist and came for consultation when refill requests were refused.
Ms. A had a family history of high anxiety in her mother and depressed mood in multiple paternal relatives, including her father. She had trouble sleeping beginning in adolescence, significant premenstrual dysphoria, and postpartum depression that led to a prescription for sertraline. Instead of feeling better, Ms. A remembers being agitated and unable to sleep, so she stopped it. Ms. A was now perimenopausal, and insomnia was worse. She had gradually increased wine consumption to a bottle of wine each night after work to “settle down.” This allowed her to fall asleep, but she inevitably awoke within 4 hours. Her internist noted an elevation in ALT and asked Ms. A about alcohol consumption. She was alarmed and cut back to one glass of wine per night but again couldn’t sleep. Her internist started zolpidem at that point.
The psychiatrist explained the concepts of tolerance and addiction and a plan to slowly taper off zolpidem while using quetiapine for sleep. She decreased to 20 mg of zolpidem at bedtime with quetiapine 50 mg and was able to stay asleep. After 3 weeks, Ms. A took zolpidem 10 mg at bedtime with quetiapine 75 mg and again, was able to fall asleep and stay asleep. After another 3 weeks, she increased quetiapine to 100 mg and stopped zolpidem without difficulty. This dose of quetiapine has continued to work well without significant side effects.
Case two
Ms. B, a 70-year-old married housewife, was referred for help with longstanding anxiety when her primary care doctor recognized that lorazepam, initially helpful at 1 mg twice daily, had required titration to 2 mg three times daily. Ms. B was preoccupied with having lorazepam on hand and never missed a dose. She had little interest in activities beyond her home, rarely socialized, and had fallen twice. She napped for 2 hours each afternoon, and sometimes had trouble staying asleep through the night.
Ms. B was reluctant to talk about her childhood history of hostility and undermining by her mother, who clearly preferred her older brother and was competitive with Ms. B. Her father traveled for work during the week and had little time for her. Ms. B had always seen herself as stupid and unlovable, which interfered with making friends. She attended college for 1 year but dropped out to marry her husband. He was also anxious and had difficulty socializing, but they found reassurance in each other. Their only child, a son in his 40s, was estranged from them, having married a woman who disliked Ms. B. Ms. B felt hopeless about developing a relationship with her grandchildren who were rarely allowed to visit. Despite her initial shame in talking about these painful problems, Ms. B realized that she felt better and scheduled monthly visits to check in.
Ms. B understood the risks of using lorazepam and wanted to stop it but was terrified of becoming anxious again. We set up a very slow tapering schedule that lowered her total dose by 0.5 mg every 2 weeks. At the same time, she began escitalopram which was effective at 20 mg. Ms. B noted that she no longer felt anxious upon awakening but was still afraid to miss a dose of lorazepam. As she felt more confident and alert, Ms. B joined a painting class at a local community center and was gratified to find that she was good at working with watercolors. She invited her neighbors to come for dinner and was surprised at how friendly and open they were. Once she had tapered to 1 mg twice daily, Ms. B began walking for exercise as she now had enough energy that it felt good to move around. After 6 months, she was completely off lorazepam, and very grateful to have discovered her capacity to improve her pleasure in life.
Case three
Ms. C, a 48-year-old attorney was referred for help with anxiety and distress in the face of separation from her husband who had admitted to an affair after she heard him talking to his girlfriend from their basement. She was unsure whether she wanted to save the marriage or end it and was horrified at the thought of dating. She had never felt especially anxious or depressed and had a supportive circle of close friends. She was uncharacteristically unable to concentrate long enough to consider her options because of anxiety.
A dose of clonazepam 0.5 mg allowed her to stay alert but calm enough to reflect on her feelings. She used it intermittently over several months and maintained regular individual psychotherapy sessions that allowed her to review the situation thoroughly. On her psychiatrist’s recommendation, she contacted a colleague to represent her if she decided to initiate divorce proceedings. She attempted to engage her husband in marital therapy, and his reluctance made it clear to her that she could no longer trust him. Ms. C offered him the option of a dissolution if he was willing to cooperate, or to sue for divorce if not. Once Ms. C regained her confidence and recognized that she would survive this emotionally fraught situation, she no longer needed clonazepam.
Summary
The risks, which include cognitive slowing, falls and fractures, and withdrawal phenomena when abruptly stopped, make this class dangerous for all patients but particularly the elderly. Benzodiazepines are nonetheless useful medications for patients able to use them intermittently, whether on an alternating basis with other medications (for example, quetiapine alternating with clonazepam for chronic insomnia) or because symptoms of anxiety are intermittent. Psychiatrists treating tolerant patients should be familiar with the approach of tapering slowly while introducing more appropriate medications at adequate doses to manage symptoms.
Dr. Kaplan is training and supervising psychoanalyst at the Cincinnati Psychoanalytic Institute and volunteer professor of clinical psychiatry at the University of Cincinnati. The author reported no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Olfson M et al. JAMA Psychiatry. 2015 Feb;72(2):136-42. doi: 10.1001/jamapsychiatry.2014.1763.
2. Lin FY et al. Sleep. 2014 Apr 1;37(4):673-9. doi: 10.5665/sleep.3566.
3. Thomas R and Ramos-Rivas E. Psychiatr Ann. 2018;48(6):266-70. doi: 10.3928/00485713-20180513-01.
4. Bushnell GA et al. JAMA Psychiatry. 2017 Jul 1;74(7):747-55. doi: 10.1001/jamapsychiatry.2017.1273.
5. Taipale H et al. JAMA Netw Open. 2020;3(10):e2019029. doi: 10.1001/jamanetworkopen.2020.19029.
6. Xu KY et al. JAMA Netw Open. 2020;3(12):e2028557. doi: 10.1001/jamanetworkopen.2020.28557.
7. Billioti de Gage S et al. BMJ. 2014;349:g5205. doi: 10.1136/bmj.g5205.
8. Ettcheto M et al. Front Aging Neurosci. 2020 Jan 8;11:344. doi: 10.3389/fnagi.2019.00344.
Many psychiatrists have had the grim experience of a newly referred patient explaining that her (and it is most often “her”) primary care doctor has been prescribing lorazepam 8 mg per day or alprazolam 6 mg per day and is sending her to you for help with ongoing anxiety. For conscientious psychiatrists, this means the beginning of a long tapering process along with a great deal of reassuring of a patient who is terrified of feeling overwhelmed with anxiety. The same problem occurs with patients taking large doses of sedatives who are still unable to sleep.
Mark Olfson and coauthors quantified benzodiazepine use in the United States in 2008 using a large prescription database, and found that 5.2% of adults between 18 and 80 years old were taking these drugs.1 The percentage increased with age, to 8.7% of those 65-80 years, in whom 31% received long-term prescriptions from a psychiatrist. Benzodiazepine use was twice as prevalent in women, compared with men. This occurs despite peer-reviewed publications and articles in the popular press regarding the risks of long-term benzodiazepine use in the elderly. Fang-Yu Lin and coauthors documented a 2.23-fold higher risk of hip fracture in zolpidem users that increased with age; elderly users had a 21-fold higher incidence of fracture, compared with younger users, and were twice as likely to sustain a fracture than elderly nonusers.2
Rashona Thomas and Edid Ramos-Rivas reviewed the risks of benzodiazepines in older patients with insomnia and document the increase in serious adverse events such as falls, fractures, and cognitive and behavioral changes.3 Many patients have ongoing prescriptions that make discontinuation difficult, given the potential for withdrawal agitation, seizures, insomnia, nightmares and even psychosis.
Greta Bushnell and coauthors pointed to the problem of simultaneous prescribing of a new antidepressant with a benzodiazepine by 10% of doctors initiating antidepressants.4 Over 12% of this group of patients continued benzodiazepines long term, even though there was no difference in the response to antidepressant treatment at 6 months. Those with long-term benzodiazepine use were also more likely to have recent prescriptions for opiates.
A Finnish research team found that 34% of middle-aged and 55% of elderly people developed long-term use of benzodiazepines after an initial prescription.5 Those who became long-term users were more often older male receivers of social benefits, with psychiatric comorbidities and substance abuse histories.
Kevin Xu and coauthors reviewed a National Health and Nutrition Examination Survey dataset from 1999 to 2015 with follow-up on over 5,000 individuals in that period.6 They found doubling of all-cause mortality in users of benzodiazepines with or without accompanying use of opiates, a statistically significant increase.
Perhaps most alarming is the increased risk for Alzheimer’s dementia diagnosis in users of benzodiazepines. Two separate studies (Billoti de Gage and colleagues and Ettcheto and colleagues7,8) provided reviews of evidence for the relationship between use of benzodiazepines and development of dementia, and repeated warnings about close monitoring of patients and the need for alternative treatments for anxiety and insomnia in the elderly.
Be alert to underlying issues
Overburdened primary practitioners faced with complaints about sleep and anxiety understandably turn to medication rather than taking time to discuss the reasons for these problems or to describe nonmedication approaches to relief of symptoms. Even insured patients may have very limited options for “covered” psychiatric consultation, as many competent psychiatrists have moved to a cash-only system. It is easier to renew prescriptions than to counsel patients or refer them, and many primary care practitioners have limited experience with diagnosing causes of anxiety and insomnia, much less alternative medication approaches.
Psychiatrists should be aware of the frequency of underlying mood disorders that include sleep and anxiety as prominent symptoms; in fact, these symptoms are often what motivates patients to pursue treatment. It is critical to obtain not only a personal history of symptoms beginning in childhood up to the present, but also a family history of mood and anxiety problems. Mood dysregulation disorders are highly hereditary and a family history of mania or psychosis should raise concern about the cause of symptoms in one’s patient. A strong personal and/or family history of alcohol abuse and dependence may cover underlying undiagnosed mood dysregulation. Primary care physicians may not recognize mood dysregulation unless a patient is clearly manic or psychotic.
There is a cohort of patients who do well on antidepressant medication, but anorgasmia, fatigue, and emotional blunting are common side effects that affect compliance. When patients have unexpected responses to SSRI medications such as euphoria, agitation, anxiety, insomnia, and more prominent mood swings, primary care physicians may add a benzodiazepine, expecting the problem to abate with time. Unfortunately, this often leads to ongoing use of benzodiazepines, since attempts to stop them causes withdrawal effects that are indistinguishable from the original anxiety symptoms.
Most psychiatrists are aware that some patients need mood stabilization rather than mood elevation to maintain an adequate baseline mood. Lithium, anticonvulsants, and second-generation antipsychotics may be effective without adding antidepressant medication. Managing dosing and side effects requires time for follow-up visits with patients after initiating treatment but leads to more stability and better outcomes.
Benzodiazepines are appropriate and helpful in situations that cause transient anxiety and with patients who have done poorly with other options. Intermittent use is key to avoiding tolerance and inevitable dose increases. Some individuals can take low daily doses that are harmless, though these likely only prevent withdrawal rather than preventing anxiety. The placebo effect of taking a pill is powerful. And some patients take more doses than they admit to. Most practitioners have heard stories about the alprazolam that was accidentally spilled into the sink or the prescription bottle of diazepam that was lost or the lorazepam supply that was stolen by the babysitter.
These concepts are illustrated in case examples below.
Case one
Ms. A, a 55-year-old married female business administrator, admitted to using zolpidem at 40 mg per night for the past several months. She began with the typical dose of 10 mg at bedtime prescribed by her internist, but after several weeks, needed an additional 10 mg at 2 a.m. to stay asleep. As weeks passed, she found that she needed an additional 20 mg when she awoke at 2 a.m. Within months, she needed 20 mg to initiate sleep and 20 mg to maintain sleep. She obtained extra zolpidem from her gynecologist and came for consultation when refill requests were refused.
Ms. A had a family history of high anxiety in her mother and depressed mood in multiple paternal relatives, including her father. She had trouble sleeping beginning in adolescence, significant premenstrual dysphoria, and postpartum depression that led to a prescription for sertraline. Instead of feeling better, Ms. A remembers being agitated and unable to sleep, so she stopped it. Ms. A was now perimenopausal, and insomnia was worse. She had gradually increased wine consumption to a bottle of wine each night after work to “settle down.” This allowed her to fall asleep, but she inevitably awoke within 4 hours. Her internist noted an elevation in ALT and asked Ms. A about alcohol consumption. She was alarmed and cut back to one glass of wine per night but again couldn’t sleep. Her internist started zolpidem at that point.
The psychiatrist explained the concepts of tolerance and addiction and a plan to slowly taper off zolpidem while using quetiapine for sleep. She decreased to 20 mg of zolpidem at bedtime with quetiapine 50 mg and was able to stay asleep. After 3 weeks, Ms. A took zolpidem 10 mg at bedtime with quetiapine 75 mg and again, was able to fall asleep and stay asleep. After another 3 weeks, she increased quetiapine to 100 mg and stopped zolpidem without difficulty. This dose of quetiapine has continued to work well without significant side effects.
Case two
Ms. B, a 70-year-old married housewife, was referred for help with longstanding anxiety when her primary care doctor recognized that lorazepam, initially helpful at 1 mg twice daily, had required titration to 2 mg three times daily. Ms. B was preoccupied with having lorazepam on hand and never missed a dose. She had little interest in activities beyond her home, rarely socialized, and had fallen twice. She napped for 2 hours each afternoon, and sometimes had trouble staying asleep through the night.
Ms. B was reluctant to talk about her childhood history of hostility and undermining by her mother, who clearly preferred her older brother and was competitive with Ms. B. Her father traveled for work during the week and had little time for her. Ms. B had always seen herself as stupid and unlovable, which interfered with making friends. She attended college for 1 year but dropped out to marry her husband. He was also anxious and had difficulty socializing, but they found reassurance in each other. Their only child, a son in his 40s, was estranged from them, having married a woman who disliked Ms. B. Ms. B felt hopeless about developing a relationship with her grandchildren who were rarely allowed to visit. Despite her initial shame in talking about these painful problems, Ms. B realized that she felt better and scheduled monthly visits to check in.
Ms. B understood the risks of using lorazepam and wanted to stop it but was terrified of becoming anxious again. We set up a very slow tapering schedule that lowered her total dose by 0.5 mg every 2 weeks. At the same time, she began escitalopram which was effective at 20 mg. Ms. B noted that she no longer felt anxious upon awakening but was still afraid to miss a dose of lorazepam. As she felt more confident and alert, Ms. B joined a painting class at a local community center and was gratified to find that she was good at working with watercolors. She invited her neighbors to come for dinner and was surprised at how friendly and open they were. Once she had tapered to 1 mg twice daily, Ms. B began walking for exercise as she now had enough energy that it felt good to move around. After 6 months, she was completely off lorazepam, and very grateful to have discovered her capacity to improve her pleasure in life.
Case three
Ms. C, a 48-year-old attorney was referred for help with anxiety and distress in the face of separation from her husband who had admitted to an affair after she heard him talking to his girlfriend from their basement. She was unsure whether she wanted to save the marriage or end it and was horrified at the thought of dating. She had never felt especially anxious or depressed and had a supportive circle of close friends. She was uncharacteristically unable to concentrate long enough to consider her options because of anxiety.
A dose of clonazepam 0.5 mg allowed her to stay alert but calm enough to reflect on her feelings. She used it intermittently over several months and maintained regular individual psychotherapy sessions that allowed her to review the situation thoroughly. On her psychiatrist’s recommendation, she contacted a colleague to represent her if she decided to initiate divorce proceedings. She attempted to engage her husband in marital therapy, and his reluctance made it clear to her that she could no longer trust him. Ms. C offered him the option of a dissolution if he was willing to cooperate, or to sue for divorce if not. Once Ms. C regained her confidence and recognized that she would survive this emotionally fraught situation, she no longer needed clonazepam.
Summary
The risks, which include cognitive slowing, falls and fractures, and withdrawal phenomena when abruptly stopped, make this class dangerous for all patients but particularly the elderly. Benzodiazepines are nonetheless useful medications for patients able to use them intermittently, whether on an alternating basis with other medications (for example, quetiapine alternating with clonazepam for chronic insomnia) or because symptoms of anxiety are intermittent. Psychiatrists treating tolerant patients should be familiar with the approach of tapering slowly while introducing more appropriate medications at adequate doses to manage symptoms.
Dr. Kaplan is training and supervising psychoanalyst at the Cincinnati Psychoanalytic Institute and volunteer professor of clinical psychiatry at the University of Cincinnati. The author reported no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Olfson M et al. JAMA Psychiatry. 2015 Feb;72(2):136-42. doi: 10.1001/jamapsychiatry.2014.1763.
2. Lin FY et al. Sleep. 2014 Apr 1;37(4):673-9. doi: 10.5665/sleep.3566.
3. Thomas R and Ramos-Rivas E. Psychiatr Ann. 2018;48(6):266-70. doi: 10.3928/00485713-20180513-01.
4. Bushnell GA et al. JAMA Psychiatry. 2017 Jul 1;74(7):747-55. doi: 10.1001/jamapsychiatry.2017.1273.
5. Taipale H et al. JAMA Netw Open. 2020;3(10):e2019029. doi: 10.1001/jamanetworkopen.2020.19029.
6. Xu KY et al. JAMA Netw Open. 2020;3(12):e2028557. doi: 10.1001/jamanetworkopen.2020.28557.
7. Billioti de Gage S et al. BMJ. 2014;349:g5205. doi: 10.1136/bmj.g5205.
8. Ettcheto M et al. Front Aging Neurosci. 2020 Jan 8;11:344. doi: 10.3389/fnagi.2019.00344.
Many psychiatrists have had the grim experience of a newly referred patient explaining that her (and it is most often “her”) primary care doctor has been prescribing lorazepam 8 mg per day or alprazolam 6 mg per day and is sending her to you for help with ongoing anxiety. For conscientious psychiatrists, this means the beginning of a long tapering process along with a great deal of reassuring of a patient who is terrified of feeling overwhelmed with anxiety. The same problem occurs with patients taking large doses of sedatives who are still unable to sleep.
Mark Olfson and coauthors quantified benzodiazepine use in the United States in 2008 using a large prescription database, and found that 5.2% of adults between 18 and 80 years old were taking these drugs.1 The percentage increased with age, to 8.7% of those 65-80 years, in whom 31% received long-term prescriptions from a psychiatrist. Benzodiazepine use was twice as prevalent in women, compared with men. This occurs despite peer-reviewed publications and articles in the popular press regarding the risks of long-term benzodiazepine use in the elderly. Fang-Yu Lin and coauthors documented a 2.23-fold higher risk of hip fracture in zolpidem users that increased with age; elderly users had a 21-fold higher incidence of fracture, compared with younger users, and were twice as likely to sustain a fracture than elderly nonusers.2
Rashona Thomas and Edid Ramos-Rivas reviewed the risks of benzodiazepines in older patients with insomnia and document the increase in serious adverse events such as falls, fractures, and cognitive and behavioral changes.3 Many patients have ongoing prescriptions that make discontinuation difficult, given the potential for withdrawal agitation, seizures, insomnia, nightmares and even psychosis.
Greta Bushnell and coauthors pointed to the problem of simultaneous prescribing of a new antidepressant with a benzodiazepine by 10% of doctors initiating antidepressants.4 Over 12% of this group of patients continued benzodiazepines long term, even though there was no difference in the response to antidepressant treatment at 6 months. Those with long-term benzodiazepine use were also more likely to have recent prescriptions for opiates.
A Finnish research team found that 34% of middle-aged and 55% of elderly people developed long-term use of benzodiazepines after an initial prescription.5 Those who became long-term users were more often older male receivers of social benefits, with psychiatric comorbidities and substance abuse histories.
Kevin Xu and coauthors reviewed a National Health and Nutrition Examination Survey dataset from 1999 to 2015 with follow-up on over 5,000 individuals in that period.6 They found doubling of all-cause mortality in users of benzodiazepines with or without accompanying use of opiates, a statistically significant increase.
Perhaps most alarming is the increased risk for Alzheimer’s dementia diagnosis in users of benzodiazepines. Two separate studies (Billoti de Gage and colleagues and Ettcheto and colleagues7,8) provided reviews of evidence for the relationship between use of benzodiazepines and development of dementia, and repeated warnings about close monitoring of patients and the need for alternative treatments for anxiety and insomnia in the elderly.
Be alert to underlying issues
Overburdened primary practitioners faced with complaints about sleep and anxiety understandably turn to medication rather than taking time to discuss the reasons for these problems or to describe nonmedication approaches to relief of symptoms. Even insured patients may have very limited options for “covered” psychiatric consultation, as many competent psychiatrists have moved to a cash-only system. It is easier to renew prescriptions than to counsel patients or refer them, and many primary care practitioners have limited experience with diagnosing causes of anxiety and insomnia, much less alternative medication approaches.
Psychiatrists should be aware of the frequency of underlying mood disorders that include sleep and anxiety as prominent symptoms; in fact, these symptoms are often what motivates patients to pursue treatment. It is critical to obtain not only a personal history of symptoms beginning in childhood up to the present, but also a family history of mood and anxiety problems. Mood dysregulation disorders are highly hereditary and a family history of mania or psychosis should raise concern about the cause of symptoms in one’s patient. A strong personal and/or family history of alcohol abuse and dependence may cover underlying undiagnosed mood dysregulation. Primary care physicians may not recognize mood dysregulation unless a patient is clearly manic or psychotic.
There is a cohort of patients who do well on antidepressant medication, but anorgasmia, fatigue, and emotional blunting are common side effects that affect compliance. When patients have unexpected responses to SSRI medications such as euphoria, agitation, anxiety, insomnia, and more prominent mood swings, primary care physicians may add a benzodiazepine, expecting the problem to abate with time. Unfortunately, this often leads to ongoing use of benzodiazepines, since attempts to stop them causes withdrawal effects that are indistinguishable from the original anxiety symptoms.
Most psychiatrists are aware that some patients need mood stabilization rather than mood elevation to maintain an adequate baseline mood. Lithium, anticonvulsants, and second-generation antipsychotics may be effective without adding antidepressant medication. Managing dosing and side effects requires time for follow-up visits with patients after initiating treatment but leads to more stability and better outcomes.
Benzodiazepines are appropriate and helpful in situations that cause transient anxiety and with patients who have done poorly with other options. Intermittent use is key to avoiding tolerance and inevitable dose increases. Some individuals can take low daily doses that are harmless, though these likely only prevent withdrawal rather than preventing anxiety. The placebo effect of taking a pill is powerful. And some patients take more doses than they admit to. Most practitioners have heard stories about the alprazolam that was accidentally spilled into the sink or the prescription bottle of diazepam that was lost or the lorazepam supply that was stolen by the babysitter.
These concepts are illustrated in case examples below.
Case one
Ms. A, a 55-year-old married female business administrator, admitted to using zolpidem at 40 mg per night for the past several months. She began with the typical dose of 10 mg at bedtime prescribed by her internist, but after several weeks, needed an additional 10 mg at 2 a.m. to stay asleep. As weeks passed, she found that she needed an additional 20 mg when she awoke at 2 a.m. Within months, she needed 20 mg to initiate sleep and 20 mg to maintain sleep. She obtained extra zolpidem from her gynecologist and came for consultation when refill requests were refused.
Ms. A had a family history of high anxiety in her mother and depressed mood in multiple paternal relatives, including her father. She had trouble sleeping beginning in adolescence, significant premenstrual dysphoria, and postpartum depression that led to a prescription for sertraline. Instead of feeling better, Ms. A remembers being agitated and unable to sleep, so she stopped it. Ms. A was now perimenopausal, and insomnia was worse. She had gradually increased wine consumption to a bottle of wine each night after work to “settle down.” This allowed her to fall asleep, but she inevitably awoke within 4 hours. Her internist noted an elevation in ALT and asked Ms. A about alcohol consumption. She was alarmed and cut back to one glass of wine per night but again couldn’t sleep. Her internist started zolpidem at that point.
The psychiatrist explained the concepts of tolerance and addiction and a plan to slowly taper off zolpidem while using quetiapine for sleep. She decreased to 20 mg of zolpidem at bedtime with quetiapine 50 mg and was able to stay asleep. After 3 weeks, Ms. A took zolpidem 10 mg at bedtime with quetiapine 75 mg and again, was able to fall asleep and stay asleep. After another 3 weeks, she increased quetiapine to 100 mg and stopped zolpidem without difficulty. This dose of quetiapine has continued to work well without significant side effects.
Case two
Ms. B, a 70-year-old married housewife, was referred for help with longstanding anxiety when her primary care doctor recognized that lorazepam, initially helpful at 1 mg twice daily, had required titration to 2 mg three times daily. Ms. B was preoccupied with having lorazepam on hand and never missed a dose. She had little interest in activities beyond her home, rarely socialized, and had fallen twice. She napped for 2 hours each afternoon, and sometimes had trouble staying asleep through the night.
Ms. B was reluctant to talk about her childhood history of hostility and undermining by her mother, who clearly preferred her older brother and was competitive with Ms. B. Her father traveled for work during the week and had little time for her. Ms. B had always seen herself as stupid and unlovable, which interfered with making friends. She attended college for 1 year but dropped out to marry her husband. He was also anxious and had difficulty socializing, but they found reassurance in each other. Their only child, a son in his 40s, was estranged from them, having married a woman who disliked Ms. B. Ms. B felt hopeless about developing a relationship with her grandchildren who were rarely allowed to visit. Despite her initial shame in talking about these painful problems, Ms. B realized that she felt better and scheduled monthly visits to check in.
Ms. B understood the risks of using lorazepam and wanted to stop it but was terrified of becoming anxious again. We set up a very slow tapering schedule that lowered her total dose by 0.5 mg every 2 weeks. At the same time, she began escitalopram which was effective at 20 mg. Ms. B noted that she no longer felt anxious upon awakening but was still afraid to miss a dose of lorazepam. As she felt more confident and alert, Ms. B joined a painting class at a local community center and was gratified to find that she was good at working with watercolors. She invited her neighbors to come for dinner and was surprised at how friendly and open they were. Once she had tapered to 1 mg twice daily, Ms. B began walking for exercise as she now had enough energy that it felt good to move around. After 6 months, she was completely off lorazepam, and very grateful to have discovered her capacity to improve her pleasure in life.
Case three
Ms. C, a 48-year-old attorney was referred for help with anxiety and distress in the face of separation from her husband who had admitted to an affair after she heard him talking to his girlfriend from their basement. She was unsure whether she wanted to save the marriage or end it and was horrified at the thought of dating. She had never felt especially anxious or depressed and had a supportive circle of close friends. She was uncharacteristically unable to concentrate long enough to consider her options because of anxiety.
A dose of clonazepam 0.5 mg allowed her to stay alert but calm enough to reflect on her feelings. She used it intermittently over several months and maintained regular individual psychotherapy sessions that allowed her to review the situation thoroughly. On her psychiatrist’s recommendation, she contacted a colleague to represent her if she decided to initiate divorce proceedings. She attempted to engage her husband in marital therapy, and his reluctance made it clear to her that she could no longer trust him. Ms. C offered him the option of a dissolution if he was willing to cooperate, or to sue for divorce if not. Once Ms. C regained her confidence and recognized that she would survive this emotionally fraught situation, she no longer needed clonazepam.
Summary
The risks, which include cognitive slowing, falls and fractures, and withdrawal phenomena when abruptly stopped, make this class dangerous for all patients but particularly the elderly. Benzodiazepines are nonetheless useful medications for patients able to use them intermittently, whether on an alternating basis with other medications (for example, quetiapine alternating with clonazepam for chronic insomnia) or because symptoms of anxiety are intermittent. Psychiatrists treating tolerant patients should be familiar with the approach of tapering slowly while introducing more appropriate medications at adequate doses to manage symptoms.
Dr. Kaplan is training and supervising psychoanalyst at the Cincinnati Psychoanalytic Institute and volunteer professor of clinical psychiatry at the University of Cincinnati. The author reported no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Olfson M et al. JAMA Psychiatry. 2015 Feb;72(2):136-42. doi: 10.1001/jamapsychiatry.2014.1763.
2. Lin FY et al. Sleep. 2014 Apr 1;37(4):673-9. doi: 10.5665/sleep.3566.
3. Thomas R and Ramos-Rivas E. Psychiatr Ann. 2018;48(6):266-70. doi: 10.3928/00485713-20180513-01.
4. Bushnell GA et al. JAMA Psychiatry. 2017 Jul 1;74(7):747-55. doi: 10.1001/jamapsychiatry.2017.1273.
5. Taipale H et al. JAMA Netw Open. 2020;3(10):e2019029. doi: 10.1001/jamanetworkopen.2020.19029.
6. Xu KY et al. JAMA Netw Open. 2020;3(12):e2028557. doi: 10.1001/jamanetworkopen.2020.28557.
7. Billioti de Gage S et al. BMJ. 2014;349:g5205. doi: 10.1136/bmj.g5205.
8. Ettcheto M et al. Front Aging Neurosci. 2020 Jan 8;11:344. doi: 10.3389/fnagi.2019.00344.
Waking up at night could be your brain boosting your memory
We tend to think a good night’s sleep should be uninterrupted, but surprising new research from the University of Copenhagen suggests just the opposite:
The study, done on mice, found that the stress transmitter noradrenaline wakes up the brain many times a night. These “microarousals” were linked to memory consolidation, meaning they help you remember the previous day’s events. In fact, the more “awake” you are during a microarousal, the better the memory boost, suggests the research, which was published in Nature Neuroscience.
“Every time I wake up in the middle of the night now, I think – ah, nice, I probably just had great memory-boosting sleep,” said study author Celia Kjaerby, PhD, an assistant professor at the university’s Center for Translational Neuromedicine.
The findings add insight to what happens in the brain during sleep and may help pave the way for new treatments for those who have sleep disorders.
Waves of noradrenaline
Previous research has suggested that noradrenaline – a hormone that increases during stress but also helps you stay focused – is inactive during sleep. So, the researchers were surprised to see high levels of it in the brains of the sleeping rodents.
“I still remember seeing the first traces showing the brain activity of the norepinephrine stress system during sleep. We could not believe our eyes,” Dr. Kjaerby said. “Everyone had thought the system would be quiet. And now we have found out that it completely controls the microarchitecture of sleep.”
Those noradrenaline levels rise and fall like waves every 30 seconds during non-REM (NREM) sleep. At each “peak” the brain is briefly awake, and at each “valley” it is asleep. Typically, these awakenings are so brief that the sleeping subject does not notice. But the higher the rise, the longer the awakening – and the more likely the sleeper may notice.
During the valleys, or when norepinephrine drops, so-called sleep spindles occur.
“These are short oscillatory bursts of brain activity linked to memory consolidation,” Dr. Kjaerby said. Occasionally there is a “deep valley,” lasting 3-5 minutes, leading to more sleep spindles. The mice with the most deep valleys also had the best memories, the researchers noted.
“We have shown that the amount of these super-boosts of sleep spindles, and not REM sleep, defines how well you remember the experiences you had prior to going to sleep,” said Dr. Kjaerby.
Deep valleys were followed by longer awakenings, the researchers observed. So, the longer the valley, the longer the awakening – and the better the memory boost. This means that, though restless sleep is not good, waking up briefly may be a natural part of memory-related sleep phases and may even mean you’ve slept well.
What happens in our brains when we sleep: Piecing it together
The findings fit with previous clinical data that shows we wake up roughly 100-plus times a night, mostly during NREM sleep stage 2 (the spindle-rich sleep stage), Dr. Kjaerby said.
Still, more research on these small awakenings is needed, Dr. Kjaerby said, noting that professor Maiken Nedergaard, MD, another author of this study, has found that the brain cleans up waste products through a rinsing fluid system.
“It remains a puzzle why the fluid system is so active when we sleep,” Dr. Kjaerby said. “We believe these short awakenings could potentially be the key to answering this question.”
A version of this article first appeared on WebMD.com.
We tend to think a good night’s sleep should be uninterrupted, but surprising new research from the University of Copenhagen suggests just the opposite:
The study, done on mice, found that the stress transmitter noradrenaline wakes up the brain many times a night. These “microarousals” were linked to memory consolidation, meaning they help you remember the previous day’s events. In fact, the more “awake” you are during a microarousal, the better the memory boost, suggests the research, which was published in Nature Neuroscience.
“Every time I wake up in the middle of the night now, I think – ah, nice, I probably just had great memory-boosting sleep,” said study author Celia Kjaerby, PhD, an assistant professor at the university’s Center for Translational Neuromedicine.
The findings add insight to what happens in the brain during sleep and may help pave the way for new treatments for those who have sleep disorders.
Waves of noradrenaline
Previous research has suggested that noradrenaline – a hormone that increases during stress but also helps you stay focused – is inactive during sleep. So, the researchers were surprised to see high levels of it in the brains of the sleeping rodents.
“I still remember seeing the first traces showing the brain activity of the norepinephrine stress system during sleep. We could not believe our eyes,” Dr. Kjaerby said. “Everyone had thought the system would be quiet. And now we have found out that it completely controls the microarchitecture of sleep.”
Those noradrenaline levels rise and fall like waves every 30 seconds during non-REM (NREM) sleep. At each “peak” the brain is briefly awake, and at each “valley” it is asleep. Typically, these awakenings are so brief that the sleeping subject does not notice. But the higher the rise, the longer the awakening – and the more likely the sleeper may notice.
During the valleys, or when norepinephrine drops, so-called sleep spindles occur.
“These are short oscillatory bursts of brain activity linked to memory consolidation,” Dr. Kjaerby said. Occasionally there is a “deep valley,” lasting 3-5 minutes, leading to more sleep spindles. The mice with the most deep valleys also had the best memories, the researchers noted.
“We have shown that the amount of these super-boosts of sleep spindles, and not REM sleep, defines how well you remember the experiences you had prior to going to sleep,” said Dr. Kjaerby.
Deep valleys were followed by longer awakenings, the researchers observed. So, the longer the valley, the longer the awakening – and the better the memory boost. This means that, though restless sleep is not good, waking up briefly may be a natural part of memory-related sleep phases and may even mean you’ve slept well.
What happens in our brains when we sleep: Piecing it together
The findings fit with previous clinical data that shows we wake up roughly 100-plus times a night, mostly during NREM sleep stage 2 (the spindle-rich sleep stage), Dr. Kjaerby said.
Still, more research on these small awakenings is needed, Dr. Kjaerby said, noting that professor Maiken Nedergaard, MD, another author of this study, has found that the brain cleans up waste products through a rinsing fluid system.
“It remains a puzzle why the fluid system is so active when we sleep,” Dr. Kjaerby said. “We believe these short awakenings could potentially be the key to answering this question.”
A version of this article first appeared on WebMD.com.
We tend to think a good night’s sleep should be uninterrupted, but surprising new research from the University of Copenhagen suggests just the opposite:
The study, done on mice, found that the stress transmitter noradrenaline wakes up the brain many times a night. These “microarousals” were linked to memory consolidation, meaning they help you remember the previous day’s events. In fact, the more “awake” you are during a microarousal, the better the memory boost, suggests the research, which was published in Nature Neuroscience.
“Every time I wake up in the middle of the night now, I think – ah, nice, I probably just had great memory-boosting sleep,” said study author Celia Kjaerby, PhD, an assistant professor at the university’s Center for Translational Neuromedicine.
The findings add insight to what happens in the brain during sleep and may help pave the way for new treatments for those who have sleep disorders.
Waves of noradrenaline
Previous research has suggested that noradrenaline – a hormone that increases during stress but also helps you stay focused – is inactive during sleep. So, the researchers were surprised to see high levels of it in the brains of the sleeping rodents.
“I still remember seeing the first traces showing the brain activity of the norepinephrine stress system during sleep. We could not believe our eyes,” Dr. Kjaerby said. “Everyone had thought the system would be quiet. And now we have found out that it completely controls the microarchitecture of sleep.”
Those noradrenaline levels rise and fall like waves every 30 seconds during non-REM (NREM) sleep. At each “peak” the brain is briefly awake, and at each “valley” it is asleep. Typically, these awakenings are so brief that the sleeping subject does not notice. But the higher the rise, the longer the awakening – and the more likely the sleeper may notice.
During the valleys, or when norepinephrine drops, so-called sleep spindles occur.
“These are short oscillatory bursts of brain activity linked to memory consolidation,” Dr. Kjaerby said. Occasionally there is a “deep valley,” lasting 3-5 minutes, leading to more sleep spindles. The mice with the most deep valleys also had the best memories, the researchers noted.
“We have shown that the amount of these super-boosts of sleep spindles, and not REM sleep, defines how well you remember the experiences you had prior to going to sleep,” said Dr. Kjaerby.
Deep valleys were followed by longer awakenings, the researchers observed. So, the longer the valley, the longer the awakening – and the better the memory boost. This means that, though restless sleep is not good, waking up briefly may be a natural part of memory-related sleep phases and may even mean you’ve slept well.
What happens in our brains when we sleep: Piecing it together
The findings fit with previous clinical data that shows we wake up roughly 100-plus times a night, mostly during NREM sleep stage 2 (the spindle-rich sleep stage), Dr. Kjaerby said.
Still, more research on these small awakenings is needed, Dr. Kjaerby said, noting that professor Maiken Nedergaard, MD, another author of this study, has found that the brain cleans up waste products through a rinsing fluid system.
“It remains a puzzle why the fluid system is so active when we sleep,” Dr. Kjaerby said. “We believe these short awakenings could potentially be the key to answering this question.”
A version of this article first appeared on WebMD.com.
FROM NATURE NEUROSCIENCE
Charcoal could be the cure for the common high-fat diet
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Steroids no cure for obstructive sleep apnea in children
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM CHEST
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).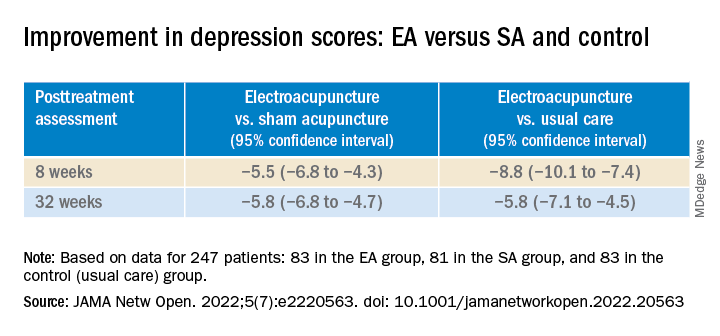
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).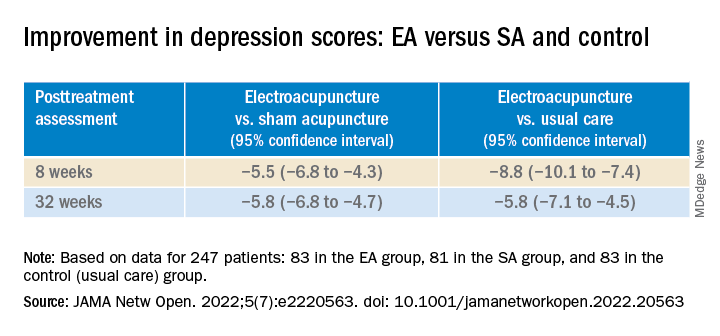
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).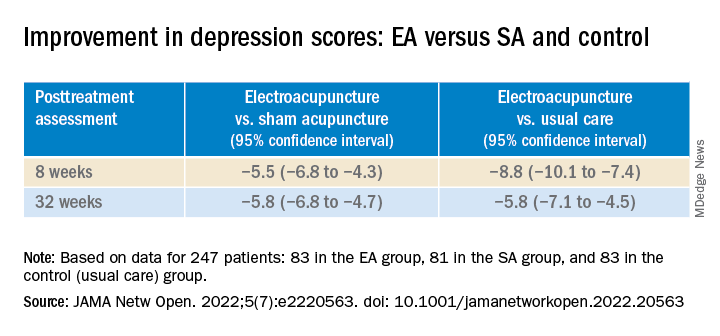
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN