User login
Delaying surgery for 11 weeks after RCT does not increase pCR rates for rectal cancer
Among patients with rectal cancer, delaying surgery for 11 weeks after the end of radiochemotherapy does not improve pathologic complete response rates, investigators reported.
Previously, the Lyon trial, the only randomized controlled study to investigate the effects of delaying surgery following the end of radiochemotherapy (RCT), found that compared with a 2-week delay, a 6-week delay significantly increased the number of patients who experienced complete response (53.1% vs. 71.7%, P = .007). The purpose of the current study was to evaluate the effect of a longer interval between RCT and surgery on pathologic complete response (pCR) rates.
For the phase III, multicenter, randomized trial, 265 patients with mid or lower rectal cancer were randomized to receive surgery at 7 weeks (n = 133) or 11 weeks (n = 132) following the end of RCT.
Baseline tumor characteristics and patient demographics were similar between the two study arms; the majority of patients had stage cT3 rectal cancer (82%).
There was no significant difference in pathologic complete response rate between the study arms (15% for 7-week group vs. 17.4% for 11-week group, P = .5983), reported Jeremie Lefevre, MD, of Hopital Saint-Antoine, Paris, and his associates (J Clin Oncol. 2016 July. doi: 10.1200/JCO.2016.67.6049).
Overall morbidity was significantly increased in the 11-week group (44.5% v 32%; P = .04), primarily explained by an increase in medical complications (32.8% vs. 19.2%; P = .01), the investigators wrote.
The French Ministry of Health funded the study. Dr. Lefevre and seven of his associates reported serving in advisory roles, receiving financial compensation, or participating in the speakers bureau for multiple companies.
On Twitter @jessnicolecraig
Among patients with rectal cancer, delaying surgery for 11 weeks after the end of radiochemotherapy does not improve pathologic complete response rates, investigators reported.
Previously, the Lyon trial, the only randomized controlled study to investigate the effects of delaying surgery following the end of radiochemotherapy (RCT), found that compared with a 2-week delay, a 6-week delay significantly increased the number of patients who experienced complete response (53.1% vs. 71.7%, P = .007). The purpose of the current study was to evaluate the effect of a longer interval between RCT and surgery on pathologic complete response (pCR) rates.
For the phase III, multicenter, randomized trial, 265 patients with mid or lower rectal cancer were randomized to receive surgery at 7 weeks (n = 133) or 11 weeks (n = 132) following the end of RCT.
Baseline tumor characteristics and patient demographics were similar between the two study arms; the majority of patients had stage cT3 rectal cancer (82%).
There was no significant difference in pathologic complete response rate between the study arms (15% for 7-week group vs. 17.4% for 11-week group, P = .5983), reported Jeremie Lefevre, MD, of Hopital Saint-Antoine, Paris, and his associates (J Clin Oncol. 2016 July. doi: 10.1200/JCO.2016.67.6049).
Overall morbidity was significantly increased in the 11-week group (44.5% v 32%; P = .04), primarily explained by an increase in medical complications (32.8% vs. 19.2%; P = .01), the investigators wrote.
The French Ministry of Health funded the study. Dr. Lefevre and seven of his associates reported serving in advisory roles, receiving financial compensation, or participating in the speakers bureau for multiple companies.
On Twitter @jessnicolecraig
Among patients with rectal cancer, delaying surgery for 11 weeks after the end of radiochemotherapy does not improve pathologic complete response rates, investigators reported.
Previously, the Lyon trial, the only randomized controlled study to investigate the effects of delaying surgery following the end of radiochemotherapy (RCT), found that compared with a 2-week delay, a 6-week delay significantly increased the number of patients who experienced complete response (53.1% vs. 71.7%, P = .007). The purpose of the current study was to evaluate the effect of a longer interval between RCT and surgery on pathologic complete response (pCR) rates.
For the phase III, multicenter, randomized trial, 265 patients with mid or lower rectal cancer were randomized to receive surgery at 7 weeks (n = 133) or 11 weeks (n = 132) following the end of RCT.
Baseline tumor characteristics and patient demographics were similar between the two study arms; the majority of patients had stage cT3 rectal cancer (82%).
There was no significant difference in pathologic complete response rate between the study arms (15% for 7-week group vs. 17.4% for 11-week group, P = .5983), reported Jeremie Lefevre, MD, of Hopital Saint-Antoine, Paris, and his associates (J Clin Oncol. 2016 July. doi: 10.1200/JCO.2016.67.6049).
Overall morbidity was significantly increased in the 11-week group (44.5% v 32%; P = .04), primarily explained by an increase in medical complications (32.8% vs. 19.2%; P = .01), the investigators wrote.
The French Ministry of Health funded the study. Dr. Lefevre and seven of his associates reported serving in advisory roles, receiving financial compensation, or participating in the speakers bureau for multiple companies.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Delaying surgery for 11 weeks after the end of radiochemotherapy does not improve pathologic complete response rates in patients with rectal cancer, compared with a delay of 7 weeks.
Major finding: There was no significant difference in pathologic complete response rate between the study arms (15% for 7-week group vs. 17.4% for 11-week group, P = .5983).
Data source: A phase III, multicenter, randomized trial involving 265 patients with varying stages of rectal cancer.
Disclosures: The French Ministry of Health funded the study. Dr. Lefevre and seven of his associates reported serving in advisory roles, receiving financial compensation, or participating in the speakers bureau for multiple companies.
Study identifies important predictors for PC/PGL
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
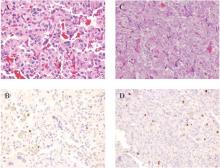
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: SDHB mutation and tumor size may be better predictors of outcomes in patients with pheochromocytoma and abdominal paraganglioma than are other previously identified predictors.
Major finding: The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation.
Data source: Retrospective analysis of 84 patients with PC/PGL evaluated by the Surgical Endocrine Oncology branch at George Washington University Hospital from 1998-2015.
Disclosures: The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors reported having no financial disclosures.
Safety of sentinel node dissection alone holds up a decade out
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: In women with clinical early-stage breast cancer who have a positive sentinel node and undergo breast-conserving therapy, skipping ALND does not compromise outcomes.
Major finding: Women treated with and without ALND were statistically indistinguishable with respect to 10-year rates of locoregional recurrence (6.2% and 5.3%), disease-free survival (78.2% and 80.2%), and overall survival (83.6% and 86.3%).
Data source: A randomized phase III trial among 891 women with clinical T1-2,N0,M0 breast cancer and positive sentinel nodes treated with breast-conserving therapy and usually adjuvant systemic therapy (ACOSOG Z0011).
Disclosures: Dr. Giuliano disclosed that he had no relevant conflicts of interest.
Oophorectomy cost-effective at 4% lifetime ovarian cancer risk
Premenopausal risk-reducing salpingo-oophorectomy becomes cost-effective in women who have a 4% or greater lifetime risk of ovarian cancer, according to a modeling study published online in the Journal of Medical Genetics.
The procedure, which is usually undertaken in women aged over 35 years who have completed their families, is available in the United Kingdom to women with a greater than 10% lifetime risk of ovarian cancer. However, the researchers, led by Dr. Ranjit Manchanda of Barts Cancer Institute at Queen Mary University of London, suggested that this threshold has not been tested for cost-effectiveness.
The decision analysis model evaluated lifetime costs as well as the effects of risk-reducing salpingo-oophorectomy in 40-year-old premenopausal women by comparing it with no procedure in women whose lifetime ovarian cancer risk ranged from 2%-10%. The final outcomes were development of breast cancer, ovarian cancer, and excess deaths from coronary heart disease, while cost-effectiveness was judged against the National Institute for Health and Care Excellence threshold of £20,000-£30,000 per quality-adjusted life-years (QALY).
Researchers found that premenopausal risk-reducing salpingo-oophorectomy was cost-effective in women with a 4% or greater lifetime risk of ovarian cancer, largely because of the reduction in their risk of breast cancer. At this level of risk, surgery gained 42.7 days of life-expectancy, with an incremental cost-effectiveness ratio of £19,536($26,186)/QALY.
Premenopausal risk-reducing salpingo-oophorectomy was not cost-effective at the baseline risk rate of 2%, with an incremental cost-effectiveness ratio of £46,480($62,267)/QALY and 19.9 days gain in life expectancy (J Med Genetics 2016 June 27. doi: 10.1136/jmedgenet-2016-103800).
The cost-effectiveness was predicated on the assumption of at least an 80% compliance rate with hormone therapy (HT) in women who underwent the procedure; without HT, the cost-effectiveness threshold increased to a lifetime risk of over 8.2%.
“Our results are of major significance for clinical practice and risk management in view of declining genetic testing costs and the improvements in estimating an individual’s OC risk,” the authors wrote.
“With routine clinical testing for certain moderate penetrance genes around the corner and lack of an effective OC screening programme, these findings are timely as it provides evidence supporting a surgical prevention strategy for ‘lower-risk’ (lifetime risk less than 10%) individuals,” noted Dr. Manchanda and colleagues.
They stressed that symptom levels after salpingo-oophorectomy, particularly for sexual function, were still higher even in women taking HT compared to those who hadn’t undergone salpingo-oophorectomy.
“This limitation needs to be discussed as part of informed consent for the surgical procedure and incorporated into [the risk-reducing salpingo-oophorectomy] decision-making process,” they wrote.
One author declared a financial interest in Abcodia, which has an interest in ovarian cancer screening and biomarkers for screening and risk prediction. No other conflicts of interest were declared.
Premenopausal risk-reducing salpingo-oophorectomy becomes cost-effective in women who have a 4% or greater lifetime risk of ovarian cancer, according to a modeling study published online in the Journal of Medical Genetics.
The procedure, which is usually undertaken in women aged over 35 years who have completed their families, is available in the United Kingdom to women with a greater than 10% lifetime risk of ovarian cancer. However, the researchers, led by Dr. Ranjit Manchanda of Barts Cancer Institute at Queen Mary University of London, suggested that this threshold has not been tested for cost-effectiveness.
The decision analysis model evaluated lifetime costs as well as the effects of risk-reducing salpingo-oophorectomy in 40-year-old premenopausal women by comparing it with no procedure in women whose lifetime ovarian cancer risk ranged from 2%-10%. The final outcomes were development of breast cancer, ovarian cancer, and excess deaths from coronary heart disease, while cost-effectiveness was judged against the National Institute for Health and Care Excellence threshold of £20,000-£30,000 per quality-adjusted life-years (QALY).
Researchers found that premenopausal risk-reducing salpingo-oophorectomy was cost-effective in women with a 4% or greater lifetime risk of ovarian cancer, largely because of the reduction in their risk of breast cancer. At this level of risk, surgery gained 42.7 days of life-expectancy, with an incremental cost-effectiveness ratio of £19,536($26,186)/QALY.
Premenopausal risk-reducing salpingo-oophorectomy was not cost-effective at the baseline risk rate of 2%, with an incremental cost-effectiveness ratio of £46,480($62,267)/QALY and 19.9 days gain in life expectancy (J Med Genetics 2016 June 27. doi: 10.1136/jmedgenet-2016-103800).
The cost-effectiveness was predicated on the assumption of at least an 80% compliance rate with hormone therapy (HT) in women who underwent the procedure; without HT, the cost-effectiveness threshold increased to a lifetime risk of over 8.2%.
“Our results are of major significance for clinical practice and risk management in view of declining genetic testing costs and the improvements in estimating an individual’s OC risk,” the authors wrote.
“With routine clinical testing for certain moderate penetrance genes around the corner and lack of an effective OC screening programme, these findings are timely as it provides evidence supporting a surgical prevention strategy for ‘lower-risk’ (lifetime risk less than 10%) individuals,” noted Dr. Manchanda and colleagues.
They stressed that symptom levels after salpingo-oophorectomy, particularly for sexual function, were still higher even in women taking HT compared to those who hadn’t undergone salpingo-oophorectomy.
“This limitation needs to be discussed as part of informed consent for the surgical procedure and incorporated into [the risk-reducing salpingo-oophorectomy] decision-making process,” they wrote.
One author declared a financial interest in Abcodia, which has an interest in ovarian cancer screening and biomarkers for screening and risk prediction. No other conflicts of interest were declared.
Premenopausal risk-reducing salpingo-oophorectomy becomes cost-effective in women who have a 4% or greater lifetime risk of ovarian cancer, according to a modeling study published online in the Journal of Medical Genetics.
The procedure, which is usually undertaken in women aged over 35 years who have completed their families, is available in the United Kingdom to women with a greater than 10% lifetime risk of ovarian cancer. However, the researchers, led by Dr. Ranjit Manchanda of Barts Cancer Institute at Queen Mary University of London, suggested that this threshold has not been tested for cost-effectiveness.
The decision analysis model evaluated lifetime costs as well as the effects of risk-reducing salpingo-oophorectomy in 40-year-old premenopausal women by comparing it with no procedure in women whose lifetime ovarian cancer risk ranged from 2%-10%. The final outcomes were development of breast cancer, ovarian cancer, and excess deaths from coronary heart disease, while cost-effectiveness was judged against the National Institute for Health and Care Excellence threshold of £20,000-£30,000 per quality-adjusted life-years (QALY).
Researchers found that premenopausal risk-reducing salpingo-oophorectomy was cost-effective in women with a 4% or greater lifetime risk of ovarian cancer, largely because of the reduction in their risk of breast cancer. At this level of risk, surgery gained 42.7 days of life-expectancy, with an incremental cost-effectiveness ratio of £19,536($26,186)/QALY.
Premenopausal risk-reducing salpingo-oophorectomy was not cost-effective at the baseline risk rate of 2%, with an incremental cost-effectiveness ratio of £46,480($62,267)/QALY and 19.9 days gain in life expectancy (J Med Genetics 2016 June 27. doi: 10.1136/jmedgenet-2016-103800).
The cost-effectiveness was predicated on the assumption of at least an 80% compliance rate with hormone therapy (HT) in women who underwent the procedure; without HT, the cost-effectiveness threshold increased to a lifetime risk of over 8.2%.
“Our results are of major significance for clinical practice and risk management in view of declining genetic testing costs and the improvements in estimating an individual’s OC risk,” the authors wrote.
“With routine clinical testing for certain moderate penetrance genes around the corner and lack of an effective OC screening programme, these findings are timely as it provides evidence supporting a surgical prevention strategy for ‘lower-risk’ (lifetime risk less than 10%) individuals,” noted Dr. Manchanda and colleagues.
They stressed that symptom levels after salpingo-oophorectomy, particularly for sexual function, were still higher even in women taking HT compared to those who hadn’t undergone salpingo-oophorectomy.
“This limitation needs to be discussed as part of informed consent for the surgical procedure and incorporated into [the risk-reducing salpingo-oophorectomy] decision-making process,” they wrote.
One author declared a financial interest in Abcodia, which has an interest in ovarian cancer screening and biomarkers for screening and risk prediction. No other conflicts of interest were declared.
FROM THE JOURNAL OF MEDICAL GENETICS
Key clinical point: Premenopausal risk-reducing salpingo-oophorectomy becomes cost-effective in women who have a 4% or greater lifetime risk of ovarian cancer.
Major finding: Premenopausal risk-reducing salpingo-oophorectomy in women with a 4% or greater lifetime risk of ovarian cancer gained 42.7 days of life expectancy, with an incremental cost-effectiveness ratio of £19,536($26,186)/QALY.
Data source: Decision analysis model.
Disclosures: One author declared a financial interest in Abcodia, which has an interest in ovarian cancer screening and biomarkers for screening and risk prediction. No other conflicts of interest were declared.
Point/Counterpoint: Should breast MRI be used routinely in the preoperative evaluation of breast cancer?
Yes: MRI should be considered in the preoperative setting for specific clinical indications.
MRI, like any technology, has its strengths and weaknesses, with high sensitivity but low specificity. Importantly, MRI provides excellent soft tissue contrast with anatomic 3-D detail, and is not impeded by high breast density.
Admittedly, MRI only incrementally increases cancer detection rates in either the ipsilateral or contralateral breasts of all patients, and when used in the preoperative setting does not affect short-term surgical outcomes for all patients. Therefore, MRI should not be used for routine screening or routine preoperative screening.
That said, there are specific clinical situations where preoperative MRI may provide surgeons with valuable information. These include patients who have:
• Invasive lobular carcinoma.
• Neoadjuvant chemotherapy.
• Occult primaries in extremely dense breasts.
Invasive lobular carcinomas are more likely to be multi-centric, multi-focal, and/or bilateral than other breast cancer types, and they are more difficult to diagnose because they infiltrate into tissue, making it extremely difficult to determine the extent of disease. In this setting, MRI can more accurately determine tumor size than mammography. Mammography underestimates the tumor size significantly more frequently than does MRI. In addition, among women with this cancer subtype, MRI can significantly reduce the rate of excision (Breast Cancer Res Treat. 2010;119;415-22).
We know that women at risk for systemic recurrence will not be cured with surgery alone. Neoadjuvant therapies give us the opportunity to refine local therapy options, better understand the patient’s response to therapy and prognosis, and accelerate targeted drug development to improve outcomes. To accomplish all of these goals, we need a noninvasive way to assess tumors before, during, and after neoadjuvant treatment. MRI is unsurpassed for evaluating the extent of tumors, showing in larger tumors, for example, the complexity of tumor and stroma.
MRI is also a biomarker for response to therapy and has been shown to be an independent predictor of event-free survival. In addition, MRI is more accurate than either clinical exam, mammography, or ultrasound for determining residual tumor size following neoadjuvant chemotherapy (Radiology. 2012;263:663-72).
Lastly, for patients with an occult primary (by imaging) breast cancer or primary presentation of axillary node involvement, MRI has been found to have an approximately 90% sensitivity for identifying a primary tumor, and a 95% accuracy at locating the tumor in patients who undergo surgical excision. Mammography cannot distinguish a tumor mass that is dense relative to surrounding tissue. However, MRI can distinguish a tumor which is obscured by dense breast tissue because tumors are visualized on MRI by rapid contrast uptake and washout.
MRI is a catalyst for change, but you have to use it and all technology wisely: At the time of diagnosis for select patients, for screening only those patients with very breast dense tissue and very high risk for developing breast cancer, and, perhaps most importantly, for postcancer surveillance only in women at very high risk of recurrence where standard tools such as mammography are expected to have lower performance (for example, very dense breast tissue). Overuse of MRI will increase false positives, anxiety, and cost. However, used appropriately, MRI can be used to help usher in a change in practice through the evaluation of response to neoadjuvant therapy and novel therapeutic approaches to both invasive and in situ lesions.
With improvements in technology and techniques such as diffusion-weighted imaging, the value of MRI in the preoperative setting can only continue to grow. We can also expect greater performance for presurgical staging with more refined technologies for breast imaging, localization, and biopsy, but the costs have to come down. Breast-dedicated MRI technologies may address this need.
Laura Esserman, MD, is a professor of surgery and radiology at the University of California, San Francisco, and Director of the Carol Franc Buck Breast Care Center at the UCSF Mount Zion campus.
No: MRI leads to unnecessary surgeries and does not improve short-term surgical outcomes.
The key word in this debate is “routinely.” I agree that preoperative MRI may have a role in about 5% of all cases – namely in women with occult primaries and those who undergo neoadjuvant chemotherapy. But for the vast majority of patients, the 95%, I would argue that preoperative MRI has the potential to do more harm than good.
Thirty years of experience providing breast conserving therapies without MRI has taught us several important lessons:
• Selection of patients for breast-conserving therapy is not a big problem.
• The incidences of local recurrence and contralateral breast cancers have decreased over time, antedating the use of MRI.
• Surgical excision of all microscopic subclinical disease is not necessary to achieve good long-term outcomes.
In National Surgical Adjuvant Breast and Bowel Project studies from the 1990s, in the era before the use of aromatase inhibitors or HER-2 blockade, the 10-year incidence of ipsilateral breast tumor recurrence ranged from 3.5% to 6.5% in the breast cancer population at large.
In addition, the incidence of contralateral breast cancers has been declining at a rate of approximately 3% per year, thanks to the use of adjuvant systemic therapies.
We have known since the 1960s, thanks to our colleagues in pathology, that somewhere between 30% and 60% of breast cancers that appear to be localized have microscopic subclinical disease which is treated with breast irradiation. More recently, we have recognized that we can leave behind cancer in the axilla in anywhere from 13% to 27% of patients who are not receiving direct axillary radiation, and see failure rates of 1% or less.
In the context, then, of our current understanding of breast cancer biology, what outcomes could MRI be expected to improve, since the purpose of a test is to improve patient outcomes?
We know that MRI will not improve survival, because 30 years ago randomized trials showed us that survival was equal between breast conservation and mastectomy.
MRI has no apparent effect on reducing local recurrences either, as shown in an analysis of data on 3,180 patients published in 2014 (J Clin Oncol. 2014;32:292).
Regarding contralateral breast cancer, a 2007 study (N Engl J Med. 2007;356:1295-303) showed that among 969 women, MRI found unsuspected cancer in the contralateral breast within 1 year of diagnosis in 3.1%, a finding used to support the argument that all women with breast cancer should have an MRI. But a second study using Surveillance, Epidemiology and End Results (SEER) data on 339,790 women with 2.5 million person-years of follow-up found that the 10-year rate of contralateral cancers was 2%-3% of women with estrogen-receptor–positive tumors, and in 5%-6% of those with estrogen-receptor–negative tumors, strongly suggesting that MRI leads to detection and treatment of disease that would never become clinically evident.
Finally, I would point to evidence that MRI does not improve short-term surgical outcomes, as shown in a meta-analysis my colleagues and I conducted of two randomized controlled trials and seven cohort studies, involving a total of 3,112 patients (Ann Surg. 2013;257:249-55).
We found that after adjustment for age, having an MRI was associated with a three-fold greater chance of having a mastectomy, and MRI did not significantly reduce either the need for re-excision or unexpected conversion to mastectomy. We also performed a subanalysis of infiltrating lobular cancers, and found that there was no statistically significant benefit for MRI in these patients.
The overall rate of mastectomy was 25.5% among patients who had an MRI, vs. 18.2% for those who did not.
So to summarize: MRI finds two to three times more cancer than observed rates of local recurrence, leading to unnecessary mastectomies and does not improve short-term surgical outcomes, and there is no evidence indicating that MRI decreases local recurrence.
Monica Morrow, MD, FACS, is chief of the breast service in the department of surgery and holds the Anne Burnett Windfohr Chair of Clinical Oncology at Memorial Sloan Kettering Cancer Center in New York.
Yes: MRI should be considered in the preoperative setting for specific clinical indications.
MRI, like any technology, has its strengths and weaknesses, with high sensitivity but low specificity. Importantly, MRI provides excellent soft tissue contrast with anatomic 3-D detail, and is not impeded by high breast density.
Admittedly, MRI only incrementally increases cancer detection rates in either the ipsilateral or contralateral breasts of all patients, and when used in the preoperative setting does not affect short-term surgical outcomes for all patients. Therefore, MRI should not be used for routine screening or routine preoperative screening.
That said, there are specific clinical situations where preoperative MRI may provide surgeons with valuable information. These include patients who have:
• Invasive lobular carcinoma.
• Neoadjuvant chemotherapy.
• Occult primaries in extremely dense breasts.
Invasive lobular carcinomas are more likely to be multi-centric, multi-focal, and/or bilateral than other breast cancer types, and they are more difficult to diagnose because they infiltrate into tissue, making it extremely difficult to determine the extent of disease. In this setting, MRI can more accurately determine tumor size than mammography. Mammography underestimates the tumor size significantly more frequently than does MRI. In addition, among women with this cancer subtype, MRI can significantly reduce the rate of excision (Breast Cancer Res Treat. 2010;119;415-22).
We know that women at risk for systemic recurrence will not be cured with surgery alone. Neoadjuvant therapies give us the opportunity to refine local therapy options, better understand the patient’s response to therapy and prognosis, and accelerate targeted drug development to improve outcomes. To accomplish all of these goals, we need a noninvasive way to assess tumors before, during, and after neoadjuvant treatment. MRI is unsurpassed for evaluating the extent of tumors, showing in larger tumors, for example, the complexity of tumor and stroma.
MRI is also a biomarker for response to therapy and has been shown to be an independent predictor of event-free survival. In addition, MRI is more accurate than either clinical exam, mammography, or ultrasound for determining residual tumor size following neoadjuvant chemotherapy (Radiology. 2012;263:663-72).
Lastly, for patients with an occult primary (by imaging) breast cancer or primary presentation of axillary node involvement, MRI has been found to have an approximately 90% sensitivity for identifying a primary tumor, and a 95% accuracy at locating the tumor in patients who undergo surgical excision. Mammography cannot distinguish a tumor mass that is dense relative to surrounding tissue. However, MRI can distinguish a tumor which is obscured by dense breast tissue because tumors are visualized on MRI by rapid contrast uptake and washout.
MRI is a catalyst for change, but you have to use it and all technology wisely: At the time of diagnosis for select patients, for screening only those patients with very breast dense tissue and very high risk for developing breast cancer, and, perhaps most importantly, for postcancer surveillance only in women at very high risk of recurrence where standard tools such as mammography are expected to have lower performance (for example, very dense breast tissue). Overuse of MRI will increase false positives, anxiety, and cost. However, used appropriately, MRI can be used to help usher in a change in practice through the evaluation of response to neoadjuvant therapy and novel therapeutic approaches to both invasive and in situ lesions.
With improvements in technology and techniques such as diffusion-weighted imaging, the value of MRI in the preoperative setting can only continue to grow. We can also expect greater performance for presurgical staging with more refined technologies for breast imaging, localization, and biopsy, but the costs have to come down. Breast-dedicated MRI technologies may address this need.
Laura Esserman, MD, is a professor of surgery and radiology at the University of California, San Francisco, and Director of the Carol Franc Buck Breast Care Center at the UCSF Mount Zion campus.
No: MRI leads to unnecessary surgeries and does not improve short-term surgical outcomes.
The key word in this debate is “routinely.” I agree that preoperative MRI may have a role in about 5% of all cases – namely in women with occult primaries and those who undergo neoadjuvant chemotherapy. But for the vast majority of patients, the 95%, I would argue that preoperative MRI has the potential to do more harm than good.
Thirty years of experience providing breast conserving therapies without MRI has taught us several important lessons:
• Selection of patients for breast-conserving therapy is not a big problem.
• The incidences of local recurrence and contralateral breast cancers have decreased over time, antedating the use of MRI.
• Surgical excision of all microscopic subclinical disease is not necessary to achieve good long-term outcomes.
In National Surgical Adjuvant Breast and Bowel Project studies from the 1990s, in the era before the use of aromatase inhibitors or HER-2 blockade, the 10-year incidence of ipsilateral breast tumor recurrence ranged from 3.5% to 6.5% in the breast cancer population at large.
In addition, the incidence of contralateral breast cancers has been declining at a rate of approximately 3% per year, thanks to the use of adjuvant systemic therapies.
We have known since the 1960s, thanks to our colleagues in pathology, that somewhere between 30% and 60% of breast cancers that appear to be localized have microscopic subclinical disease which is treated with breast irradiation. More recently, we have recognized that we can leave behind cancer in the axilla in anywhere from 13% to 27% of patients who are not receiving direct axillary radiation, and see failure rates of 1% or less.
In the context, then, of our current understanding of breast cancer biology, what outcomes could MRI be expected to improve, since the purpose of a test is to improve patient outcomes?
We know that MRI will not improve survival, because 30 years ago randomized trials showed us that survival was equal between breast conservation and mastectomy.
MRI has no apparent effect on reducing local recurrences either, as shown in an analysis of data on 3,180 patients published in 2014 (J Clin Oncol. 2014;32:292).
Regarding contralateral breast cancer, a 2007 study (N Engl J Med. 2007;356:1295-303) showed that among 969 women, MRI found unsuspected cancer in the contralateral breast within 1 year of diagnosis in 3.1%, a finding used to support the argument that all women with breast cancer should have an MRI. But a second study using Surveillance, Epidemiology and End Results (SEER) data on 339,790 women with 2.5 million person-years of follow-up found that the 10-year rate of contralateral cancers was 2%-3% of women with estrogen-receptor–positive tumors, and in 5%-6% of those with estrogen-receptor–negative tumors, strongly suggesting that MRI leads to detection and treatment of disease that would never become clinically evident.
Finally, I would point to evidence that MRI does not improve short-term surgical outcomes, as shown in a meta-analysis my colleagues and I conducted of two randomized controlled trials and seven cohort studies, involving a total of 3,112 patients (Ann Surg. 2013;257:249-55).
We found that after adjustment for age, having an MRI was associated with a three-fold greater chance of having a mastectomy, and MRI did not significantly reduce either the need for re-excision or unexpected conversion to mastectomy. We also performed a subanalysis of infiltrating lobular cancers, and found that there was no statistically significant benefit for MRI in these patients.
The overall rate of mastectomy was 25.5% among patients who had an MRI, vs. 18.2% for those who did not.
So to summarize: MRI finds two to three times more cancer than observed rates of local recurrence, leading to unnecessary mastectomies and does not improve short-term surgical outcomes, and there is no evidence indicating that MRI decreases local recurrence.
Monica Morrow, MD, FACS, is chief of the breast service in the department of surgery and holds the Anne Burnett Windfohr Chair of Clinical Oncology at Memorial Sloan Kettering Cancer Center in New York.
Yes: MRI should be considered in the preoperative setting for specific clinical indications.
MRI, like any technology, has its strengths and weaknesses, with high sensitivity but low specificity. Importantly, MRI provides excellent soft tissue contrast with anatomic 3-D detail, and is not impeded by high breast density.
Admittedly, MRI only incrementally increases cancer detection rates in either the ipsilateral or contralateral breasts of all patients, and when used in the preoperative setting does not affect short-term surgical outcomes for all patients. Therefore, MRI should not be used for routine screening or routine preoperative screening.
That said, there are specific clinical situations where preoperative MRI may provide surgeons with valuable information. These include patients who have:
• Invasive lobular carcinoma.
• Neoadjuvant chemotherapy.
• Occult primaries in extremely dense breasts.
Invasive lobular carcinomas are more likely to be multi-centric, multi-focal, and/or bilateral than other breast cancer types, and they are more difficult to diagnose because they infiltrate into tissue, making it extremely difficult to determine the extent of disease. In this setting, MRI can more accurately determine tumor size than mammography. Mammography underestimates the tumor size significantly more frequently than does MRI. In addition, among women with this cancer subtype, MRI can significantly reduce the rate of excision (Breast Cancer Res Treat. 2010;119;415-22).
We know that women at risk for systemic recurrence will not be cured with surgery alone. Neoadjuvant therapies give us the opportunity to refine local therapy options, better understand the patient’s response to therapy and prognosis, and accelerate targeted drug development to improve outcomes. To accomplish all of these goals, we need a noninvasive way to assess tumors before, during, and after neoadjuvant treatment. MRI is unsurpassed for evaluating the extent of tumors, showing in larger tumors, for example, the complexity of tumor and stroma.
MRI is also a biomarker for response to therapy and has been shown to be an independent predictor of event-free survival. In addition, MRI is more accurate than either clinical exam, mammography, or ultrasound for determining residual tumor size following neoadjuvant chemotherapy (Radiology. 2012;263:663-72).
Lastly, for patients with an occult primary (by imaging) breast cancer or primary presentation of axillary node involvement, MRI has been found to have an approximately 90% sensitivity for identifying a primary tumor, and a 95% accuracy at locating the tumor in patients who undergo surgical excision. Mammography cannot distinguish a tumor mass that is dense relative to surrounding tissue. However, MRI can distinguish a tumor which is obscured by dense breast tissue because tumors are visualized on MRI by rapid contrast uptake and washout.
MRI is a catalyst for change, but you have to use it and all technology wisely: At the time of diagnosis for select patients, for screening only those patients with very breast dense tissue and very high risk for developing breast cancer, and, perhaps most importantly, for postcancer surveillance only in women at very high risk of recurrence where standard tools such as mammography are expected to have lower performance (for example, very dense breast tissue). Overuse of MRI will increase false positives, anxiety, and cost. However, used appropriately, MRI can be used to help usher in a change in practice through the evaluation of response to neoadjuvant therapy and novel therapeutic approaches to both invasive and in situ lesions.
With improvements in technology and techniques such as diffusion-weighted imaging, the value of MRI in the preoperative setting can only continue to grow. We can also expect greater performance for presurgical staging with more refined technologies for breast imaging, localization, and biopsy, but the costs have to come down. Breast-dedicated MRI technologies may address this need.
Laura Esserman, MD, is a professor of surgery and radiology at the University of California, San Francisco, and Director of the Carol Franc Buck Breast Care Center at the UCSF Mount Zion campus.
No: MRI leads to unnecessary surgeries and does not improve short-term surgical outcomes.
The key word in this debate is “routinely.” I agree that preoperative MRI may have a role in about 5% of all cases – namely in women with occult primaries and those who undergo neoadjuvant chemotherapy. But for the vast majority of patients, the 95%, I would argue that preoperative MRI has the potential to do more harm than good.
Thirty years of experience providing breast conserving therapies without MRI has taught us several important lessons:
• Selection of patients for breast-conserving therapy is not a big problem.
• The incidences of local recurrence and contralateral breast cancers have decreased over time, antedating the use of MRI.
• Surgical excision of all microscopic subclinical disease is not necessary to achieve good long-term outcomes.
In National Surgical Adjuvant Breast and Bowel Project studies from the 1990s, in the era before the use of aromatase inhibitors or HER-2 blockade, the 10-year incidence of ipsilateral breast tumor recurrence ranged from 3.5% to 6.5% in the breast cancer population at large.
In addition, the incidence of contralateral breast cancers has been declining at a rate of approximately 3% per year, thanks to the use of adjuvant systemic therapies.
We have known since the 1960s, thanks to our colleagues in pathology, that somewhere between 30% and 60% of breast cancers that appear to be localized have microscopic subclinical disease which is treated with breast irradiation. More recently, we have recognized that we can leave behind cancer in the axilla in anywhere from 13% to 27% of patients who are not receiving direct axillary radiation, and see failure rates of 1% or less.
In the context, then, of our current understanding of breast cancer biology, what outcomes could MRI be expected to improve, since the purpose of a test is to improve patient outcomes?
We know that MRI will not improve survival, because 30 years ago randomized trials showed us that survival was equal between breast conservation and mastectomy.
MRI has no apparent effect on reducing local recurrences either, as shown in an analysis of data on 3,180 patients published in 2014 (J Clin Oncol. 2014;32:292).
Regarding contralateral breast cancer, a 2007 study (N Engl J Med. 2007;356:1295-303) showed that among 969 women, MRI found unsuspected cancer in the contralateral breast within 1 year of diagnosis in 3.1%, a finding used to support the argument that all women with breast cancer should have an MRI. But a second study using Surveillance, Epidemiology and End Results (SEER) data on 339,790 women with 2.5 million person-years of follow-up found that the 10-year rate of contralateral cancers was 2%-3% of women with estrogen-receptor–positive tumors, and in 5%-6% of those with estrogen-receptor–negative tumors, strongly suggesting that MRI leads to detection and treatment of disease that would never become clinically evident.
Finally, I would point to evidence that MRI does not improve short-term surgical outcomes, as shown in a meta-analysis my colleagues and I conducted of two randomized controlled trials and seven cohort studies, involving a total of 3,112 patients (Ann Surg. 2013;257:249-55).
We found that after adjustment for age, having an MRI was associated with a three-fold greater chance of having a mastectomy, and MRI did not significantly reduce either the need for re-excision or unexpected conversion to mastectomy. We also performed a subanalysis of infiltrating lobular cancers, and found that there was no statistically significant benefit for MRI in these patients.
The overall rate of mastectomy was 25.5% among patients who had an MRI, vs. 18.2% for those who did not.
So to summarize: MRI finds two to three times more cancer than observed rates of local recurrence, leading to unnecessary mastectomies and does not improve short-term surgical outcomes, and there is no evidence indicating that MRI decreases local recurrence.
Monica Morrow, MD, FACS, is chief of the breast service in the department of surgery and holds the Anne Burnett Windfohr Chair of Clinical Oncology at Memorial Sloan Kettering Cancer Center in New York.
Wedge resection showed improved survival over SBRT for early-stage NSCLC
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Wedge resection outperformed SBRT in terms of mortality for early-stage NSCLC.
Major finding: In matched groups, SBRT was associated with significantly lower 5-year overall survival than was wedge resection (32% vs. 50%).
Data source: The study assessed more than 8.000 patients with early stage NSCLC who had either wedge resection or SBRT from the National Cancer Database from 2003 to 2011.
Disclosures: Dr. Yerokun had no relevant disclosures.
IASLC lung cancer staging project proposes changes for new TNM classification
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
FROM THE JOURNAL OF THORACIC ONCOLOGY
Key clinical point: New lung cancer classification to become effective January 2017.
Major finding: Size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed dividing stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm.
Data source: The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer.
Disclosures: The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
‘Meticulous’ surgical procedure best defense against rectal cancer recurrence
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
EXPERT ANALYSIS AT THE ASCRS ANNUAL MEETING
Web app boosts lung cancer survival
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: A Web-based app improves survival for advanced lung cancer patients.
Major finding: Survival improved by 26% for web-app patients vs. controls.
Data source: Multicenter, prospective, phase III, randomized trial of 121 patients.
Disclosures: Dr. Denis has received honoraria and expenses from several pharmaceutical companies and has received institutional research funding from Sivan. Dr. Patricia Ganz reported stock and other ownership interest in Abbott Laboratories, GlaxoSmithKline, Johnson & Johnson, Merck, Novartis, Pfizer, and Teva.
Preoperative chemotherapy improves survival in patients with large anorectal GIST
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
AT THE ASCRS ANNUAL MEETING
Key clinical point: Anorectal gastrointestinal stroma tumors greater than 5 cm in size were associated with worse survival.
Major finding: Anorectal gastrointestinal stroma tumors greater than 5 cm in size were associated with increased mortality (HR 2.48; P = .004).
Data source: A review of National Cancer Database records to identify 333 cases of anorectal GIST from 1998 through 2012.
Disclosures: Dr. Hawkins reported having no relevant financial disclosures.