User login
Risk scale predicts mortality after gastric cancer surgery
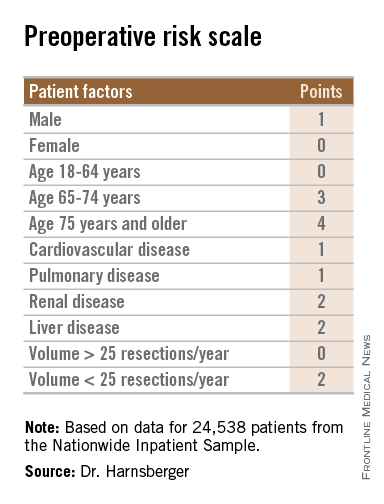
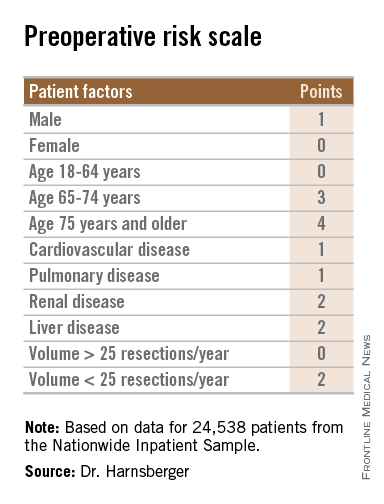
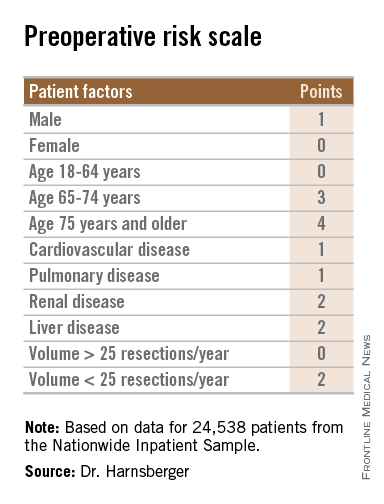
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
AT SSO 2015
Key clinical point: The bedside risk scale can be used in patient counseling prior to surgery for gastric malignancies.
Major finding: Patients with scores of 0-5 had perioperative death rates of 1.3%-4.5%. Patients with higher scores had death rates ranging from 6.0% to 23.1%.
Data source: Review of retrospective data on 24,538 adults who underwent partial or total gastric resection for malignancies.
Disclosures: The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
Laparoscopic ‘noninferior’ to open approach for rectal cancer
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Key clinical point: Laparoscopic resection is noninferior to open surgery in preventing locoregional recurrence of rectal cancer and improving survival.
Major finding: At 3-year follow-up, the rate of locoregional recurrence was identical between the laparoscopic- and the open-surgery groups, at 5% each.
Data source: An industry-sponsored multicenter open-label noninferiority trial comparing laparoscopic to open resection of rectal cancer in 1,044 patients followed for 3 years.
Disclosures: The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Study found two-way link between IBD and cervical cancer
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Inflammatory bowel disease – particularly Crohn’s disease – might increase risk of cervical cancer.
Major finding: Women with Crohn’s disease had an estimated 53% increase in risk of developing cervical cancer, compared with controls.
Data source: Population-based cohort study of 27,408 women with inflammatory bowel disease and 1,508,334 controls.
Disclosures: The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
Physician-patient communication, terminology play important role in CPM decisions
BIRMINGHAM, ALA. – The perception that one’s physician had recommended contralateral prophylactic mastectomy was a particularly important factor in the decision to undergo the procedure among BRCA1/2 mutation noncarriers with newly diagnosed breast cancer in a prospective study.
Of 90 BRCA noncarriers with newly diagnosed breast cancer, a “sizable minority” (24.4%) chose to undergo contralateral prophylactic mastectomy (CPM) after learning their mutation status, Jada G. Hamilton, Ph.D., reported at the annual meeting of the American Society of Preventive Oncology.
By comparison, 88% of eight BRCA1/2 carriers who participated in the study chose to undergo CPM, and neither of two women with a BRCA1/2 variant of undetermined significance chose to undergo CPM.
On multivariate analysis, the perception that one’s physician had recommended CPM was most strongly associated with the decision to undergo the procedure (odds ratio, 11.1), said Dr. Hamilton of Memorial Sloan-Kettering Cancer Center, New York.
Other factors associated with the decision were a perception of greater risk for contralateral breast cancer (OR, 6.46) and a perception of greater pros of CPM (OR, 1.37), she said, noting that those who indicated they would feel good about having CPM and those who indicated they might feel regret if they didn’t have CPM were most likely to elect CPM.
Age, Ashkenazi Jewish ethnicity, breast cancer–related distress, perceived cons of CPM (such as disfigurement and concerns regarding a negative impact on one’s sex life), and decisional conflict regarding CPM were not significantly associated with the decision.
Presurgical genetic testing provides valuable information to women with newly diagnosed breast cancer as they begin to make decisions about treatment, Dr. Hamilton said. Although BRCA1/2 mutation noncarriers have a low (3%-10%) risk, compared with carriers (27%-37%), studies suggest that about 18% nevertheless choose to undergo CPM.
The psychosocial factors that may affect the decision are not well understood, Dr. Hamilton said.
For the current analysis, participants who were part of a larger prospective study on presurgical BRCA1/2 testing completed a questionnaire, and the frequency and psychosocial correlates of the decision to undergo a CPM were assessed. The participants were adult women with a median age of 43 years (range of 29-59 years).
The findings raise interesting questions for future work, Dr. Hamilton said.
“I think it’s really critical for future studies to dig in to what’s happening in terms of physician-patient communication around CPM,” she said, noting that it will be important to explore how such communication interacts with a woman’s past experiences, emotions, and beliefs to shape her cancer prevention decisions.
Further, the women who undergo CPM should be followed to assess their long-term outcomes with respect to factors such as quality of life, satisfaction, and decisional regret, she concluded.
The decision to undergo CPM and the effects of physician-patient communication on that decision were also addressed in another study presented at the meeting.
In that study – a mixed methods pilot study looking mainly at factors affecting informed decision making in women who had ductal carcinoma in situ (DCIS) or who were considered to be at increased risk of invasive breast cancer risk because of a diagnosis of lobular carcinoma in situ (LCIS), BRCA positivity, or 20% or greater calculated lifetime risk – anxiety about cancer recurrence was the top reason for pursuing CPM.
Despite a lack of survival benefit, an increasing number of women with DCIS are undergoing CPM, but little is known about the decision-making process, said Jessica Valente of Emory University, Atlanta.
She and her colleagues sought to identify factors impacting risk comprehension and decision making. Of 68 women with DCIS or who were at high risk for development of invasive breast cancer, 33 considered CPM and 11 underwent the procedure.
The choice to undergo CPM was significantly associated with plastic surgery consultation, increased 10-year breast cancer risk, genetic counseling, genetic testing, and higher income, she said.
The study also highlighted a lack of health literacy and understanding of related terminology.
Most participants (nearly 84%) stated that DCIS qualified as breast cancer, but only about 40% correctly defined DCIS, Ms. Valente said.
When asked what they would recommend as a treatment strategy for a friend with DCIS, 35% thought surgery would be best. A similar percentage would recommend surgery for LCIS.
“When we looked at ductal hyperplasia, fewer people thought that that qualified as cancer, and they were more likely to recommend observation,” she said.
Further, when asked to interpret the phrase “indolent lesion of epithelial origin,” which is a phrase that has been promoted as a replacement for “DCIS” in light of concerns that women are increasingly electing CPM for DCIS because of fear of the word “carcinoma” despite a 99% survival rate, only 28% of patients believed it referred to cancer.
Observation was one of the highly recommended interventions for “indolent lesion of epithelial origin,” followed by biopsy, she said, noting that only 13% recommended surgery when this phrase was used.
“Interestingly, 7.4% said an oral or topical medication [should be used for “indolent lesion of epithelial origin]” – a finding likely explained by the fact that some women interpreted the word “lesion” to mean a wound or sore on the skin, she said.
Additionally, few women were able to define contralateral prophylactic mastectomy.
Overall, despite the study population being very well educated and from a higher socioeconomic status, they had low scores for understanding terminology (8.21 out of 20), Ms. Valente noted.
The findings demonstrate that decision making in the context of DCIS remains complex and underscore the importance of recognizing patients’ knowledge of risk communication and terminology for supporting shared and informed surgical decision making, she said.
The findings also demonstrate that while fewer women felt that surgery was appropriate when the term “indolent lesion of epithelial origin” was used instead of “DCIS,” the proposed new terminology doesn’t necessarily provide the desired clarity, she noted.
“They still came up with such a broad range of interpretations that we really might be introducing a new set of conflicts and confusion when we think about changing to that terminology when we talk to patients,” she concluded.
Dr. Hamilton and Ms. Valente each reported having no disclosures.
BIRMINGHAM, ALA. – The perception that one’s physician had recommended contralateral prophylactic mastectomy was a particularly important factor in the decision to undergo the procedure among BRCA1/2 mutation noncarriers with newly diagnosed breast cancer in a prospective study.
Of 90 BRCA noncarriers with newly diagnosed breast cancer, a “sizable minority” (24.4%) chose to undergo contralateral prophylactic mastectomy (CPM) after learning their mutation status, Jada G. Hamilton, Ph.D., reported at the annual meeting of the American Society of Preventive Oncology.
By comparison, 88% of eight BRCA1/2 carriers who participated in the study chose to undergo CPM, and neither of two women with a BRCA1/2 variant of undetermined significance chose to undergo CPM.
On multivariate analysis, the perception that one’s physician had recommended CPM was most strongly associated with the decision to undergo the procedure (odds ratio, 11.1), said Dr. Hamilton of Memorial Sloan-Kettering Cancer Center, New York.
Other factors associated with the decision were a perception of greater risk for contralateral breast cancer (OR, 6.46) and a perception of greater pros of CPM (OR, 1.37), she said, noting that those who indicated they would feel good about having CPM and those who indicated they might feel regret if they didn’t have CPM were most likely to elect CPM.
Age, Ashkenazi Jewish ethnicity, breast cancer–related distress, perceived cons of CPM (such as disfigurement and concerns regarding a negative impact on one’s sex life), and decisional conflict regarding CPM were not significantly associated with the decision.
Presurgical genetic testing provides valuable information to women with newly diagnosed breast cancer as they begin to make decisions about treatment, Dr. Hamilton said. Although BRCA1/2 mutation noncarriers have a low (3%-10%) risk, compared with carriers (27%-37%), studies suggest that about 18% nevertheless choose to undergo CPM.
The psychosocial factors that may affect the decision are not well understood, Dr. Hamilton said.
For the current analysis, participants who were part of a larger prospective study on presurgical BRCA1/2 testing completed a questionnaire, and the frequency and psychosocial correlates of the decision to undergo a CPM were assessed. The participants were adult women with a median age of 43 years (range of 29-59 years).
The findings raise interesting questions for future work, Dr. Hamilton said.
“I think it’s really critical for future studies to dig in to what’s happening in terms of physician-patient communication around CPM,” she said, noting that it will be important to explore how such communication interacts with a woman’s past experiences, emotions, and beliefs to shape her cancer prevention decisions.
Further, the women who undergo CPM should be followed to assess their long-term outcomes with respect to factors such as quality of life, satisfaction, and decisional regret, she concluded.
The decision to undergo CPM and the effects of physician-patient communication on that decision were also addressed in another study presented at the meeting.
In that study – a mixed methods pilot study looking mainly at factors affecting informed decision making in women who had ductal carcinoma in situ (DCIS) or who were considered to be at increased risk of invasive breast cancer risk because of a diagnosis of lobular carcinoma in situ (LCIS), BRCA positivity, or 20% or greater calculated lifetime risk – anxiety about cancer recurrence was the top reason for pursuing CPM.
Despite a lack of survival benefit, an increasing number of women with DCIS are undergoing CPM, but little is known about the decision-making process, said Jessica Valente of Emory University, Atlanta.
She and her colleagues sought to identify factors impacting risk comprehension and decision making. Of 68 women with DCIS or who were at high risk for development of invasive breast cancer, 33 considered CPM and 11 underwent the procedure.
The choice to undergo CPM was significantly associated with plastic surgery consultation, increased 10-year breast cancer risk, genetic counseling, genetic testing, and higher income, she said.
The study also highlighted a lack of health literacy and understanding of related terminology.
Most participants (nearly 84%) stated that DCIS qualified as breast cancer, but only about 40% correctly defined DCIS, Ms. Valente said.
When asked what they would recommend as a treatment strategy for a friend with DCIS, 35% thought surgery would be best. A similar percentage would recommend surgery for LCIS.
“When we looked at ductal hyperplasia, fewer people thought that that qualified as cancer, and they were more likely to recommend observation,” she said.
Further, when asked to interpret the phrase “indolent lesion of epithelial origin,” which is a phrase that has been promoted as a replacement for “DCIS” in light of concerns that women are increasingly electing CPM for DCIS because of fear of the word “carcinoma” despite a 99% survival rate, only 28% of patients believed it referred to cancer.
Observation was one of the highly recommended interventions for “indolent lesion of epithelial origin,” followed by biopsy, she said, noting that only 13% recommended surgery when this phrase was used.
“Interestingly, 7.4% said an oral or topical medication [should be used for “indolent lesion of epithelial origin]” – a finding likely explained by the fact that some women interpreted the word “lesion” to mean a wound or sore on the skin, she said.
Additionally, few women were able to define contralateral prophylactic mastectomy.
Overall, despite the study population being very well educated and from a higher socioeconomic status, they had low scores for understanding terminology (8.21 out of 20), Ms. Valente noted.
The findings demonstrate that decision making in the context of DCIS remains complex and underscore the importance of recognizing patients’ knowledge of risk communication and terminology for supporting shared and informed surgical decision making, she said.
The findings also demonstrate that while fewer women felt that surgery was appropriate when the term “indolent lesion of epithelial origin” was used instead of “DCIS,” the proposed new terminology doesn’t necessarily provide the desired clarity, she noted.
“They still came up with such a broad range of interpretations that we really might be introducing a new set of conflicts and confusion when we think about changing to that terminology when we talk to patients,” she concluded.
Dr. Hamilton and Ms. Valente each reported having no disclosures.
BIRMINGHAM, ALA. – The perception that one’s physician had recommended contralateral prophylactic mastectomy was a particularly important factor in the decision to undergo the procedure among BRCA1/2 mutation noncarriers with newly diagnosed breast cancer in a prospective study.
Of 90 BRCA noncarriers with newly diagnosed breast cancer, a “sizable minority” (24.4%) chose to undergo contralateral prophylactic mastectomy (CPM) after learning their mutation status, Jada G. Hamilton, Ph.D., reported at the annual meeting of the American Society of Preventive Oncology.
By comparison, 88% of eight BRCA1/2 carriers who participated in the study chose to undergo CPM, and neither of two women with a BRCA1/2 variant of undetermined significance chose to undergo CPM.
On multivariate analysis, the perception that one’s physician had recommended CPM was most strongly associated with the decision to undergo the procedure (odds ratio, 11.1), said Dr. Hamilton of Memorial Sloan-Kettering Cancer Center, New York.
Other factors associated with the decision were a perception of greater risk for contralateral breast cancer (OR, 6.46) and a perception of greater pros of CPM (OR, 1.37), she said, noting that those who indicated they would feel good about having CPM and those who indicated they might feel regret if they didn’t have CPM were most likely to elect CPM.
Age, Ashkenazi Jewish ethnicity, breast cancer–related distress, perceived cons of CPM (such as disfigurement and concerns regarding a negative impact on one’s sex life), and decisional conflict regarding CPM were not significantly associated with the decision.
Presurgical genetic testing provides valuable information to women with newly diagnosed breast cancer as they begin to make decisions about treatment, Dr. Hamilton said. Although BRCA1/2 mutation noncarriers have a low (3%-10%) risk, compared with carriers (27%-37%), studies suggest that about 18% nevertheless choose to undergo CPM.
The psychosocial factors that may affect the decision are not well understood, Dr. Hamilton said.
For the current analysis, participants who were part of a larger prospective study on presurgical BRCA1/2 testing completed a questionnaire, and the frequency and psychosocial correlates of the decision to undergo a CPM were assessed. The participants were adult women with a median age of 43 years (range of 29-59 years).
The findings raise interesting questions for future work, Dr. Hamilton said.
“I think it’s really critical for future studies to dig in to what’s happening in terms of physician-patient communication around CPM,” she said, noting that it will be important to explore how such communication interacts with a woman’s past experiences, emotions, and beliefs to shape her cancer prevention decisions.
Further, the women who undergo CPM should be followed to assess their long-term outcomes with respect to factors such as quality of life, satisfaction, and decisional regret, she concluded.
The decision to undergo CPM and the effects of physician-patient communication on that decision were also addressed in another study presented at the meeting.
In that study – a mixed methods pilot study looking mainly at factors affecting informed decision making in women who had ductal carcinoma in situ (DCIS) or who were considered to be at increased risk of invasive breast cancer risk because of a diagnosis of lobular carcinoma in situ (LCIS), BRCA positivity, or 20% or greater calculated lifetime risk – anxiety about cancer recurrence was the top reason for pursuing CPM.
Despite a lack of survival benefit, an increasing number of women with DCIS are undergoing CPM, but little is known about the decision-making process, said Jessica Valente of Emory University, Atlanta.
She and her colleagues sought to identify factors impacting risk comprehension and decision making. Of 68 women with DCIS or who were at high risk for development of invasive breast cancer, 33 considered CPM and 11 underwent the procedure.
The choice to undergo CPM was significantly associated with plastic surgery consultation, increased 10-year breast cancer risk, genetic counseling, genetic testing, and higher income, she said.
The study also highlighted a lack of health literacy and understanding of related terminology.
Most participants (nearly 84%) stated that DCIS qualified as breast cancer, but only about 40% correctly defined DCIS, Ms. Valente said.
When asked what they would recommend as a treatment strategy for a friend with DCIS, 35% thought surgery would be best. A similar percentage would recommend surgery for LCIS.
“When we looked at ductal hyperplasia, fewer people thought that that qualified as cancer, and they were more likely to recommend observation,” she said.
Further, when asked to interpret the phrase “indolent lesion of epithelial origin,” which is a phrase that has been promoted as a replacement for “DCIS” in light of concerns that women are increasingly electing CPM for DCIS because of fear of the word “carcinoma” despite a 99% survival rate, only 28% of patients believed it referred to cancer.
Observation was one of the highly recommended interventions for “indolent lesion of epithelial origin,” followed by biopsy, she said, noting that only 13% recommended surgery when this phrase was used.
“Interestingly, 7.4% said an oral or topical medication [should be used for “indolent lesion of epithelial origin]” – a finding likely explained by the fact that some women interpreted the word “lesion” to mean a wound or sore on the skin, she said.
Additionally, few women were able to define contralateral prophylactic mastectomy.
Overall, despite the study population being very well educated and from a higher socioeconomic status, they had low scores for understanding terminology (8.21 out of 20), Ms. Valente noted.
The findings demonstrate that decision making in the context of DCIS remains complex and underscore the importance of recognizing patients’ knowledge of risk communication and terminology for supporting shared and informed surgical decision making, she said.
The findings also demonstrate that while fewer women felt that surgery was appropriate when the term “indolent lesion of epithelial origin” was used instead of “DCIS,” the proposed new terminology doesn’t necessarily provide the desired clarity, she noted.
“They still came up with such a broad range of interpretations that we really might be introducing a new set of conflicts and confusion when we think about changing to that terminology when we talk to patients,” she concluded.
Dr. Hamilton and Ms. Valente each reported having no disclosures.
AT THE ASPO ANNUAL MEETING
Key clinical point: Physician-patient communication plays an important role in a woman’s decision to undergo CPM.
Major finding: Of 90 women with invasive breast cancer and without BRCA mutations, 24% chose to undergo CPM; of 68 women with DCIS, 33 considered CPM and 11 underwent the procedure.The choice to undergo CPM was significantly associated with the perception that one’s physician had recommended CPM in the first study, and with a plastic surgery consultation, increased 10-year breast cancer risk, genetic counseling, genetic testing, and higher income in the DCIS study.
Data source: A prospective study of 90 patients with invasive breast cancer and a mixed methods pilot study of 68 patients with DCIS.
Disclosures: Dr. Hamilton and Ms. Valente each reported having no disclosures.
Indocyanine green technique detects sentinel nodes in breast cancers
Indocyanine green dye caused no major side effects and was almost 99% concordant with radioisotope technetium for sentinel lymph node detection in early-stage breast cancer, according to researchers.
The results extend promising findings from an earlier meta-analysis of the tracer in a variety of tumor types, said Dr. Domenico Samorani of Santarcangelo di Romagna Hospital, Rimini, Italy.
“The method seems reproducible, safe, eliminates exposure to ionizing radiation, and is potentially cost-saving, despite requiring specialist training. [Also,] it could be an option for breast cancer centers with no nuclear medicine supply,” wrote Dr. Samorani and colleagues.
Sentinel lymph node biopsy has largely replaced axillary lymph node dissection for staging breast cancer, as it causes much less morbidity and is associated with similar rates of survival and locoregional recurrence. Vital blue dyes and radioisotope technetium (99mTc) are the most commonly used enhancers, but the blue dyes can cause allergic reactions and skin necrosis, and 99mTc is costly and requires special logistics and handling because of its radioactivity, the investigators noted. For these reasons, there has been renewed interest in indocyanine green dye (ICG) as an alternative, they said (Eur. J. Surg. Oncol. 2015;41:64-70).
For the study, the investigators evaluated 589 lymph nodes from 301 patients with clinically node-negative, invasive or microinvasive early breast cancer confirmed by core biopsy. All patients underwent 99mTc-guided sentinel node detection, which served as the gold standard for comparison. To perform ICG-guided detection, the researchers diluted 25 mg of ICG PULSION with 5 mL distilled water and then injected empirical doses of 0.4 to 1.2 mL of the solution subcutaneously above the tumor site for unicentric cancers, or around the areola for multicentric disease. Then the researchers used an infrared-emitting camera (Photodynamic Eye, Hamamatsu Photonics, Hamamatsu, Japan) to visualize the lymphatic drainage pathway and localize sentinel nodes for removal.
Overall, 98.7% of sentinel nodes that were 99mTc positive also were ICG positive (95% confidence interval, 97.1%-99.5%), a high degree of concordance that reflected past study results, the investigators said. Notably, the ICG-guided technique identified at least one sentinel node for 297 patients (98.7%), compared with 287 patients (95.4%) for the 99mTc method (P < .05). Thus, the use of ICG prevented removal of the entire axilla for 10 patients, the researchers wrote.
For six patients, the ICG method identified a metastatic node that 99mTc failed to identify. Therefore, ICG provided an advantage for 16 cases (5.3%). No patients experienced allergic reactions, 3.2% developed seromas, and 2.5% developed paresthesia, the researchers added.
Use of ICG instead of 99mTc for sentinel lymph node detection has several advantages: It does not require involving a nuclear medicine department, uses less radioactive material, minimizes issues around waste disposal, and can be performed in the operating room immediately after the induction of general anesthesia, said the researchers. And if combined with radio-guided occult lesion localization (ROLL), it avoids placing two radioactive tracings at the injection site, thereby facilitating tumor detection, the researchers noted.
Clinicians who are implementing ICG-guided sentinel node detection should consider combining it with 99mTc to avoid missing nodes during the learning process, the researchers emphasized.
They reported no funding sources and no conflicts of interest.
Indocyanine green dye caused no major side effects and was almost 99% concordant with radioisotope technetium for sentinel lymph node detection in early-stage breast cancer, according to researchers.
The results extend promising findings from an earlier meta-analysis of the tracer in a variety of tumor types, said Dr. Domenico Samorani of Santarcangelo di Romagna Hospital, Rimini, Italy.
“The method seems reproducible, safe, eliminates exposure to ionizing radiation, and is potentially cost-saving, despite requiring specialist training. [Also,] it could be an option for breast cancer centers with no nuclear medicine supply,” wrote Dr. Samorani and colleagues.
Sentinel lymph node biopsy has largely replaced axillary lymph node dissection for staging breast cancer, as it causes much less morbidity and is associated with similar rates of survival and locoregional recurrence. Vital blue dyes and radioisotope technetium (99mTc) are the most commonly used enhancers, but the blue dyes can cause allergic reactions and skin necrosis, and 99mTc is costly and requires special logistics and handling because of its radioactivity, the investigators noted. For these reasons, there has been renewed interest in indocyanine green dye (ICG) as an alternative, they said (Eur. J. Surg. Oncol. 2015;41:64-70).
For the study, the investigators evaluated 589 lymph nodes from 301 patients with clinically node-negative, invasive or microinvasive early breast cancer confirmed by core biopsy. All patients underwent 99mTc-guided sentinel node detection, which served as the gold standard for comparison. To perform ICG-guided detection, the researchers diluted 25 mg of ICG PULSION with 5 mL distilled water and then injected empirical doses of 0.4 to 1.2 mL of the solution subcutaneously above the tumor site for unicentric cancers, or around the areola for multicentric disease. Then the researchers used an infrared-emitting camera (Photodynamic Eye, Hamamatsu Photonics, Hamamatsu, Japan) to visualize the lymphatic drainage pathway and localize sentinel nodes for removal.
Overall, 98.7% of sentinel nodes that were 99mTc positive also were ICG positive (95% confidence interval, 97.1%-99.5%), a high degree of concordance that reflected past study results, the investigators said. Notably, the ICG-guided technique identified at least one sentinel node for 297 patients (98.7%), compared with 287 patients (95.4%) for the 99mTc method (P < .05). Thus, the use of ICG prevented removal of the entire axilla for 10 patients, the researchers wrote.
For six patients, the ICG method identified a metastatic node that 99mTc failed to identify. Therefore, ICG provided an advantage for 16 cases (5.3%). No patients experienced allergic reactions, 3.2% developed seromas, and 2.5% developed paresthesia, the researchers added.
Use of ICG instead of 99mTc for sentinel lymph node detection has several advantages: It does not require involving a nuclear medicine department, uses less radioactive material, minimizes issues around waste disposal, and can be performed in the operating room immediately after the induction of general anesthesia, said the researchers. And if combined with radio-guided occult lesion localization (ROLL), it avoids placing two radioactive tracings at the injection site, thereby facilitating tumor detection, the researchers noted.
Clinicians who are implementing ICG-guided sentinel node detection should consider combining it with 99mTc to avoid missing nodes during the learning process, the researchers emphasized.
They reported no funding sources and no conflicts of interest.
Indocyanine green dye caused no major side effects and was almost 99% concordant with radioisotope technetium for sentinel lymph node detection in early-stage breast cancer, according to researchers.
The results extend promising findings from an earlier meta-analysis of the tracer in a variety of tumor types, said Dr. Domenico Samorani of Santarcangelo di Romagna Hospital, Rimini, Italy.
“The method seems reproducible, safe, eliminates exposure to ionizing radiation, and is potentially cost-saving, despite requiring specialist training. [Also,] it could be an option for breast cancer centers with no nuclear medicine supply,” wrote Dr. Samorani and colleagues.
Sentinel lymph node biopsy has largely replaced axillary lymph node dissection for staging breast cancer, as it causes much less morbidity and is associated with similar rates of survival and locoregional recurrence. Vital blue dyes and radioisotope technetium (99mTc) are the most commonly used enhancers, but the blue dyes can cause allergic reactions and skin necrosis, and 99mTc is costly and requires special logistics and handling because of its radioactivity, the investigators noted. For these reasons, there has been renewed interest in indocyanine green dye (ICG) as an alternative, they said (Eur. J. Surg. Oncol. 2015;41:64-70).
For the study, the investigators evaluated 589 lymph nodes from 301 patients with clinically node-negative, invasive or microinvasive early breast cancer confirmed by core biopsy. All patients underwent 99mTc-guided sentinel node detection, which served as the gold standard for comparison. To perform ICG-guided detection, the researchers diluted 25 mg of ICG PULSION with 5 mL distilled water and then injected empirical doses of 0.4 to 1.2 mL of the solution subcutaneously above the tumor site for unicentric cancers, or around the areola for multicentric disease. Then the researchers used an infrared-emitting camera (Photodynamic Eye, Hamamatsu Photonics, Hamamatsu, Japan) to visualize the lymphatic drainage pathway and localize sentinel nodes for removal.
Overall, 98.7% of sentinel nodes that were 99mTc positive also were ICG positive (95% confidence interval, 97.1%-99.5%), a high degree of concordance that reflected past study results, the investigators said. Notably, the ICG-guided technique identified at least one sentinel node for 297 patients (98.7%), compared with 287 patients (95.4%) for the 99mTc method (P < .05). Thus, the use of ICG prevented removal of the entire axilla for 10 patients, the researchers wrote.
For six patients, the ICG method identified a metastatic node that 99mTc failed to identify. Therefore, ICG provided an advantage for 16 cases (5.3%). No patients experienced allergic reactions, 3.2% developed seromas, and 2.5% developed paresthesia, the researchers added.
Use of ICG instead of 99mTc for sentinel lymph node detection has several advantages: It does not require involving a nuclear medicine department, uses less radioactive material, minimizes issues around waste disposal, and can be performed in the operating room immediately after the induction of general anesthesia, said the researchers. And if combined with radio-guided occult lesion localization (ROLL), it avoids placing two radioactive tracings at the injection site, thereby facilitating tumor detection, the researchers noted.
Clinicians who are implementing ICG-guided sentinel node detection should consider combining it with 99mTc to avoid missing nodes during the learning process, the researchers emphasized.
They reported no funding sources and no conflicts of interest.
FROM THE EUROPEAN JOURNAL OF SURGICAL ONCOLOGY
Key clinical point: The fluorescent dye indocyanine green tracer showed promise in detecting sentinel lymph nodes in early-stage breast cancer.
Major finding: The dye caused no major side effects and was almost 99% concordant with radioisotope technetium.
Data source: Prospective validation trial evaluating 589 lymph nodes from 301 patients with clinically node-negative, invasive early breast cancer.
Disclosures: The investigators reported no funding sources and no conflicts of interest.
Study: No value in sending hernia sac specimens for routine pathology
Pathologic evaluations of hernia sac specimens from adult patients did not alter clinical management, and cost a medical center more than $75,000 over 4 years, according to a study published online in the American Journal of Surgery.
“The results from our study indicate that ‘routine’ evaluation of hernia sac specimens is likely neither indicated nor cost effective,” said Dr. Patrick Chesley of Madigan Army Medical Center, Fort Lewis, Wash., and his associates. “The rarity of changes in diagnosis and treatment from routine pathologic examination of a hernia sac does not justify this practice, and indicates that it may be omitted except in unique circumstances.”
The practice of sending hernia sac specimens for pathologic evaluation dates to 1926, when the American College of Surgeons Minimum Standard for Hospitals stated that all tissues removed during surgery should be examined and the results reported. The Joint Commission reiterated that recommendation in 1998, stating in its Comprehensive Accreditation Manual for Pathology and Clinical Laboratory Services that ‘‘specimens removed during surgery need to be evaluated for gross and microscopic abnormalities before a final diagnosis can be made.”
But the literature offers little support for the recommendation regarding hernia sac specimens, and institutions are starting to question the practice, Dr. Chesley and his associates wrote (Am. J. Surg. 2015 Feb. 12 [doi: 10.1016/j.amjsurg.2014.12.019]).
In one study, for example, pathologists reviewed 1,020 hernia sac specimens and found that only one had yielded an unexpected result – an atypical lipoma that did not affect patient management. Another study reviewed more than 2,000 hernia repairs and found that only 34% cases underwent pathologic review, with no resulting changes in treatment or management of any case.
For their study, Dr. Chesley and his coinvestigators retrospectively reviewed operative reports and medical records for 1,216 inguinal, incisional, umbilical, and ventral hernia repairs, all of which occurred at a single medical center between 2007 and 2011. More than half (55.4%) of cases were inguinal hernia repairs, 21.5% were umbilical, 11.4% were incisional, and 11.7% were ventral. In 20% of cases, surgeons sent hernia sac specimens for pathologic evaluation. Of these, 96% were selected for routine examination and 4% were selected because of concerns about possible gross abnormalities, the researchers said. Regardless of the reason for pathologic evaluation, none of the 246 examinations produced findings that reportedly altered clinical management, they said. Furthermore, pathologic evaluations cost patients about $300 to $350 each, for a total bill of more than $75,000 during the course of the study.
“These data reflect previous results from the pediatric surgical literature, and support the notion that routine pathologic evaluation of hernia sac specimens is not indicated,” the researchers concluded. But the recommendation should only apply to routine pathologic examinations, and surgeons should continue to treat abnormal intraoperative findings during hernia repair as indications for pathologic evaluation at their own discretion, they said.
Because the study was retrospective, the researchers could not ensure completeness of the data, they said. They also lacked a standardized method for reporting the reasons for specimen collection.
They reported no funding sources and declared no conflicts of interest.
Pathologic evaluations of hernia sac specimens from adult patients did not alter clinical management, and cost a medical center more than $75,000 over 4 years, according to a study published online in the American Journal of Surgery.
“The results from our study indicate that ‘routine’ evaluation of hernia sac specimens is likely neither indicated nor cost effective,” said Dr. Patrick Chesley of Madigan Army Medical Center, Fort Lewis, Wash., and his associates. “The rarity of changes in diagnosis and treatment from routine pathologic examination of a hernia sac does not justify this practice, and indicates that it may be omitted except in unique circumstances.”
The practice of sending hernia sac specimens for pathologic evaluation dates to 1926, when the American College of Surgeons Minimum Standard for Hospitals stated that all tissues removed during surgery should be examined and the results reported. The Joint Commission reiterated that recommendation in 1998, stating in its Comprehensive Accreditation Manual for Pathology and Clinical Laboratory Services that ‘‘specimens removed during surgery need to be evaluated for gross and microscopic abnormalities before a final diagnosis can be made.”
But the literature offers little support for the recommendation regarding hernia sac specimens, and institutions are starting to question the practice, Dr. Chesley and his associates wrote (Am. J. Surg. 2015 Feb. 12 [doi: 10.1016/j.amjsurg.2014.12.019]).
In one study, for example, pathologists reviewed 1,020 hernia sac specimens and found that only one had yielded an unexpected result – an atypical lipoma that did not affect patient management. Another study reviewed more than 2,000 hernia repairs and found that only 34% cases underwent pathologic review, with no resulting changes in treatment or management of any case.
For their study, Dr. Chesley and his coinvestigators retrospectively reviewed operative reports and medical records for 1,216 inguinal, incisional, umbilical, and ventral hernia repairs, all of which occurred at a single medical center between 2007 and 2011. More than half (55.4%) of cases were inguinal hernia repairs, 21.5% were umbilical, 11.4% were incisional, and 11.7% were ventral. In 20% of cases, surgeons sent hernia sac specimens for pathologic evaluation. Of these, 96% were selected for routine examination and 4% were selected because of concerns about possible gross abnormalities, the researchers said. Regardless of the reason for pathologic evaluation, none of the 246 examinations produced findings that reportedly altered clinical management, they said. Furthermore, pathologic evaluations cost patients about $300 to $350 each, for a total bill of more than $75,000 during the course of the study.
“These data reflect previous results from the pediatric surgical literature, and support the notion that routine pathologic evaluation of hernia sac specimens is not indicated,” the researchers concluded. But the recommendation should only apply to routine pathologic examinations, and surgeons should continue to treat abnormal intraoperative findings during hernia repair as indications for pathologic evaluation at their own discretion, they said.
Because the study was retrospective, the researchers could not ensure completeness of the data, they said. They also lacked a standardized method for reporting the reasons for specimen collection.
They reported no funding sources and declared no conflicts of interest.
Pathologic evaluations of hernia sac specimens from adult patients did not alter clinical management, and cost a medical center more than $75,000 over 4 years, according to a study published online in the American Journal of Surgery.
“The results from our study indicate that ‘routine’ evaluation of hernia sac specimens is likely neither indicated nor cost effective,” said Dr. Patrick Chesley of Madigan Army Medical Center, Fort Lewis, Wash., and his associates. “The rarity of changes in diagnosis and treatment from routine pathologic examination of a hernia sac does not justify this practice, and indicates that it may be omitted except in unique circumstances.”
The practice of sending hernia sac specimens for pathologic evaluation dates to 1926, when the American College of Surgeons Minimum Standard for Hospitals stated that all tissues removed during surgery should be examined and the results reported. The Joint Commission reiterated that recommendation in 1998, stating in its Comprehensive Accreditation Manual for Pathology and Clinical Laboratory Services that ‘‘specimens removed during surgery need to be evaluated for gross and microscopic abnormalities before a final diagnosis can be made.”
But the literature offers little support for the recommendation regarding hernia sac specimens, and institutions are starting to question the practice, Dr. Chesley and his associates wrote (Am. J. Surg. 2015 Feb. 12 [doi: 10.1016/j.amjsurg.2014.12.019]).
In one study, for example, pathologists reviewed 1,020 hernia sac specimens and found that only one had yielded an unexpected result – an atypical lipoma that did not affect patient management. Another study reviewed more than 2,000 hernia repairs and found that only 34% cases underwent pathologic review, with no resulting changes in treatment or management of any case.
For their study, Dr. Chesley and his coinvestigators retrospectively reviewed operative reports and medical records for 1,216 inguinal, incisional, umbilical, and ventral hernia repairs, all of which occurred at a single medical center between 2007 and 2011. More than half (55.4%) of cases were inguinal hernia repairs, 21.5% were umbilical, 11.4% were incisional, and 11.7% were ventral. In 20% of cases, surgeons sent hernia sac specimens for pathologic evaluation. Of these, 96% were selected for routine examination and 4% were selected because of concerns about possible gross abnormalities, the researchers said. Regardless of the reason for pathologic evaluation, none of the 246 examinations produced findings that reportedly altered clinical management, they said. Furthermore, pathologic evaluations cost patients about $300 to $350 each, for a total bill of more than $75,000 during the course of the study.
“These data reflect previous results from the pediatric surgical literature, and support the notion that routine pathologic evaluation of hernia sac specimens is not indicated,” the researchers concluded. But the recommendation should only apply to routine pathologic examinations, and surgeons should continue to treat abnormal intraoperative findings during hernia repair as indications for pathologic evaluation at their own discretion, they said.
Because the study was retrospective, the researchers could not ensure completeness of the data, they said. They also lacked a standardized method for reporting the reasons for specimen collection.
They reported no funding sources and declared no conflicts of interest.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Pathologic examination of hernia sac specimens can be omitted except in unique cases.
Major finding: Pathologic evaluation yielded no information that changed clinical management.
Data source: Four-year, single-center retrospective analysis of hernia sac specimens from 246 adults.
Disclosures: The investigators reported no funding sources and declared no conflicts of interest.
Perioperative treatment with diuretic linked with lower lung cancer recurrence
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Key clinical point: After surgical removal of tumors, lung cancer patients treated with atrial natriuretic peptide had a significantly lower recurrence rate than did patients who had not received atrial natriuretic peptide.
Major finding: Patients treated with atrial natriuretic peptide had significantly greater 2-year relapse-free survival than did untreated patients (91% vs. 75%, P = .018).
Data source: The retrospective study included 390 patients who were not treated with atrial natriuretic peptide and 77 patients who were.
Disclosures: Dr. Nojiri and two other authors have filed a patent related to atrial natriuretic peptide treatment for cancer metastasis with Daiichi-Sankyo Pharmaceutical Inc.
Stem cell divisions help dictate cancer risk
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
FROM SCIENCE
Key clinical point: Only a third of the variation in cancer risk among tissues is because of the environment or inheritance, and this has implications with regard to prevention and detection.
Major finding: The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells.
Data source: Researchers performed a literature review to correlate cancer incidence in a variety of tissues with the nature, number, and hierarchical division patterns of the tissue’s stem cells.
Disclosures: The researchers reported no relevant disclosures.
Greater surgeon experience linked to better long-term survival in NSCLC
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:Insufficient lymph-node sampling by less-experienced surgeons may be a reason why patients with stage I NSCLC had better long-term survival if operated on by moderate- and high-experience surgeons.
Major finding: Short-term outcomes in pathologic stage I NSCLC were not affected by surgeon experience, but 5-year survival was significantly lower for the low-experience compared to the moderate-experience surgeons (76.9% vs. 67.5%).
Data source: An institutional database analysis was conducted of 800 operations on stage I NSCLC patients performed from 2000 to 2012.
Disclosures: The authors reported having no conflicts of interest.
Heparin, warfarin tied to similar VTE rates after radical cystectomy
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
FROM THE JOURNAL OF UROLOGY
Key clinical point: Heparin and warfarin were linked to similar rates of postcystectomy venous thromboembolism.
Major finding: Symptomatic VTE affected 4.7% of patients in the overall cohort, compared with 6.4% of those treated with the modern, heparin-based protocol (P = .089).
Data source: A single-center retrospective cohort study of 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection.
Disclosures: Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.




