User login
Official Newspaper of the American College of Surgeons
Investigators recover nearly $755 million in health fraud
Government investigators recovered nearly $755 million in criminal and civil health fraud actions in 2015, according to new figures from the Health & Human Services Office of Inspector General (OIG).
The recoveries were made by Medicaid Fraud Control Units that operate in every state and consist of nearly 2,000 staff members.
This interactive OIG map shows the distribution of recoveries by state.
On Twitter @legal_med
Government investigators recovered nearly $755 million in criminal and civil health fraud actions in 2015, according to new figures from the Health & Human Services Office of Inspector General (OIG).
The recoveries were made by Medicaid Fraud Control Units that operate in every state and consist of nearly 2,000 staff members.
This interactive OIG map shows the distribution of recoveries by state.
On Twitter @legal_med
Government investigators recovered nearly $755 million in criminal and civil health fraud actions in 2015, according to new figures from the Health & Human Services Office of Inspector General (OIG).
The recoveries were made by Medicaid Fraud Control Units that operate in every state and consist of nearly 2,000 staff members.
This interactive OIG map shows the distribution of recoveries by state.
On Twitter @legal_med
Prepared surgery patients less likely to boomerang
JACKSONVILLE, FLA. – Patients who report receiving and using materials to help them prepare for surgery and its aftermath are less likely to be readmitted, according to results of a large surgical patient survey.
Readmissions after surgery have become anathema to doctors and hospitals as government and commercial payers ratchet up penalties, but a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress has found that giving patients written instructions, handouts, and videos and directing them to multimedia and online sources can reduce the risk of readmission after surgery by about two-thirds.
Dr. Luke Martin, a general surgery resident at the University of Utah, Salt Lake City, presented results from a nationwide online survey of 1,917 people who either had surgery in the past year or were relatives or caregivers of someone who did.
“We found a direct relationship between the quantity of resources used and the patient-reported feelings of preparedness,” Dr. Martin said. “We found that feeling unprepared or using no resources was associated with an increased 30-day risk of readmission.”
The study analyzed respondents’ feelings of preparedness before surgery and after surgery but before discharge. Those who felt prepared before surgery had a 30-day readmission rate of 8% vs. 23% for those who did not feel prepared. Rates were similar for those who felt prepared after surgery and those who felt unprepared: 9% vs. 23%. The overall readmission rate of 10% “is in line with expected results,” Dr. Martin said. “Using any resource was associated with a 10% rate of readmission, whereas using no resources was associated with a 31% rate of 30-day readmission,” Dr. Martin said.
“The bottom line is that health information resources have not been well studied in surgical patients, and no matter what types of resources we provide patients, sometimes they go out and find their own health information resources and supplements,” Dr. Martin said.
Overall, 64% of respondents said they felt very prepared before and after surgery and before leaving the hospital; 8% felt very unprepared before their operations, and 4% felt that way before leaving the hospital.
Patients who felt prepared were most likely to report being given multiple health information resources before surgery (97% vs. 79%, P less than .001) and before leaving the hospital (91% vs. 85%, P = .02). Resources included face-to-face meetings, written instructions, Internet sites, videos, and smartphone applications.
Patients who reported receiving one or more resources before surgery had rates of feeling prepared exceeding 90%. Those who said they had received three or more resources had almost universal rates of feeling prepared. On the other hand, only about 60% of patients who claimed they did not receive resources before their operations felt prepared.
The researchers also looked at whether survey respondents reported that they actually utilized the resources they were given before their operations or if they sought out resources on their own.
“We found that the very commonly provided written instructions are used by patients less than half the time, 41%, vs. a 90% rate of having them provided,” Dr. Martin said. The converse was true of utilization of Internet resources; only 17% of respondents said they were provided with Internet resources, but 45% said they utilized them.
“We should as providers ensure access to more resources because patients who use more resources or are provided with more resources feel more prepared to transition after surgical procedures, and perhaps we should personalize resources to patients’ preferences, learning styles, and levels of health literacy so that we can ensure they feel prepared to transition before and after their surgical procedure,” Dr. Martin said.
During the discussion, Dr. Dawn Elfenbein of the University of California, Irvine, cautioned against using quantity of information as the only measure. “We give our patients written instructions and websites, and they say they actually don’t use the information because we give them too much and it needs to be better organized,” she said. ”Sometimes accessibility is part of the issue, and quality is also important.”
Dr. Matthew Corriere of Wake Forest University, Winston-Salem, N.C., had another take on patient preparation for surgery. “I think those patients who do not have Internet access are a real goldmine for readmission,” he said.
Dr. Martin and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who report receiving and using materials to help them prepare for surgery and its aftermath are less likely to be readmitted, according to results of a large surgical patient survey.
Readmissions after surgery have become anathema to doctors and hospitals as government and commercial payers ratchet up penalties, but a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress has found that giving patients written instructions, handouts, and videos and directing them to multimedia and online sources can reduce the risk of readmission after surgery by about two-thirds.
Dr. Luke Martin, a general surgery resident at the University of Utah, Salt Lake City, presented results from a nationwide online survey of 1,917 people who either had surgery in the past year or were relatives or caregivers of someone who did.
“We found a direct relationship between the quantity of resources used and the patient-reported feelings of preparedness,” Dr. Martin said. “We found that feeling unprepared or using no resources was associated with an increased 30-day risk of readmission.”
The study analyzed respondents’ feelings of preparedness before surgery and after surgery but before discharge. Those who felt prepared before surgery had a 30-day readmission rate of 8% vs. 23% for those who did not feel prepared. Rates were similar for those who felt prepared after surgery and those who felt unprepared: 9% vs. 23%. The overall readmission rate of 10% “is in line with expected results,” Dr. Martin said. “Using any resource was associated with a 10% rate of readmission, whereas using no resources was associated with a 31% rate of 30-day readmission,” Dr. Martin said.
“The bottom line is that health information resources have not been well studied in surgical patients, and no matter what types of resources we provide patients, sometimes they go out and find their own health information resources and supplements,” Dr. Martin said.
Overall, 64% of respondents said they felt very prepared before and after surgery and before leaving the hospital; 8% felt very unprepared before their operations, and 4% felt that way before leaving the hospital.
Patients who felt prepared were most likely to report being given multiple health information resources before surgery (97% vs. 79%, P less than .001) and before leaving the hospital (91% vs. 85%, P = .02). Resources included face-to-face meetings, written instructions, Internet sites, videos, and smartphone applications.
Patients who reported receiving one or more resources before surgery had rates of feeling prepared exceeding 90%. Those who said they had received three or more resources had almost universal rates of feeling prepared. On the other hand, only about 60% of patients who claimed they did not receive resources before their operations felt prepared.
The researchers also looked at whether survey respondents reported that they actually utilized the resources they were given before their operations or if they sought out resources on their own.
“We found that the very commonly provided written instructions are used by patients less than half the time, 41%, vs. a 90% rate of having them provided,” Dr. Martin said. The converse was true of utilization of Internet resources; only 17% of respondents said they were provided with Internet resources, but 45% said they utilized them.
“We should as providers ensure access to more resources because patients who use more resources or are provided with more resources feel more prepared to transition after surgical procedures, and perhaps we should personalize resources to patients’ preferences, learning styles, and levels of health literacy so that we can ensure they feel prepared to transition before and after their surgical procedure,” Dr. Martin said.
During the discussion, Dr. Dawn Elfenbein of the University of California, Irvine, cautioned against using quantity of information as the only measure. “We give our patients written instructions and websites, and they say they actually don’t use the information because we give them too much and it needs to be better organized,” she said. ”Sometimes accessibility is part of the issue, and quality is also important.”
Dr. Matthew Corriere of Wake Forest University, Winston-Salem, N.C., had another take on patient preparation for surgery. “I think those patients who do not have Internet access are a real goldmine for readmission,” he said.
Dr. Martin and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Patients who report receiving and using materials to help them prepare for surgery and its aftermath are less likely to be readmitted, according to results of a large surgical patient survey.
Readmissions after surgery have become anathema to doctors and hospitals as government and commercial payers ratchet up penalties, but a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress has found that giving patients written instructions, handouts, and videos and directing them to multimedia and online sources can reduce the risk of readmission after surgery by about two-thirds.
Dr. Luke Martin, a general surgery resident at the University of Utah, Salt Lake City, presented results from a nationwide online survey of 1,917 people who either had surgery in the past year or were relatives or caregivers of someone who did.
“We found a direct relationship between the quantity of resources used and the patient-reported feelings of preparedness,” Dr. Martin said. “We found that feeling unprepared or using no resources was associated with an increased 30-day risk of readmission.”
The study analyzed respondents’ feelings of preparedness before surgery and after surgery but before discharge. Those who felt prepared before surgery had a 30-day readmission rate of 8% vs. 23% for those who did not feel prepared. Rates were similar for those who felt prepared after surgery and those who felt unprepared: 9% vs. 23%. The overall readmission rate of 10% “is in line with expected results,” Dr. Martin said. “Using any resource was associated with a 10% rate of readmission, whereas using no resources was associated with a 31% rate of 30-day readmission,” Dr. Martin said.
“The bottom line is that health information resources have not been well studied in surgical patients, and no matter what types of resources we provide patients, sometimes they go out and find their own health information resources and supplements,” Dr. Martin said.
Overall, 64% of respondents said they felt very prepared before and after surgery and before leaving the hospital; 8% felt very unprepared before their operations, and 4% felt that way before leaving the hospital.
Patients who felt prepared were most likely to report being given multiple health information resources before surgery (97% vs. 79%, P less than .001) and before leaving the hospital (91% vs. 85%, P = .02). Resources included face-to-face meetings, written instructions, Internet sites, videos, and smartphone applications.
Patients who reported receiving one or more resources before surgery had rates of feeling prepared exceeding 90%. Those who said they had received three or more resources had almost universal rates of feeling prepared. On the other hand, only about 60% of patients who claimed they did not receive resources before their operations felt prepared.
The researchers also looked at whether survey respondents reported that they actually utilized the resources they were given before their operations or if they sought out resources on their own.
“We found that the very commonly provided written instructions are used by patients less than half the time, 41%, vs. a 90% rate of having them provided,” Dr. Martin said. The converse was true of utilization of Internet resources; only 17% of respondents said they were provided with Internet resources, but 45% said they utilized them.
“We should as providers ensure access to more resources because patients who use more resources or are provided with more resources feel more prepared to transition after surgical procedures, and perhaps we should personalize resources to patients’ preferences, learning styles, and levels of health literacy so that we can ensure they feel prepared to transition before and after their surgical procedure,” Dr. Martin said.
During the discussion, Dr. Dawn Elfenbein of the University of California, Irvine, cautioned against using quantity of information as the only measure. “We give our patients written instructions and websites, and they say they actually don’t use the information because we give them too much and it needs to be better organized,” she said. ”Sometimes accessibility is part of the issue, and quality is also important.”
Dr. Matthew Corriere of Wake Forest University, Winston-Salem, N.C., had another take on patient preparation for surgery. “I think those patients who do not have Internet access are a real goldmine for readmission,” he said.
Dr. Martin and coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: The amount and quality of information patients report receiving before an operation and discharge are correlated to how likely patients are to be readmitted after surgery.
Major finding: Patients who felt prepared before surgery had a 30-day readmission rate of 8% vs. 23% for those who did not feel prepared.
Data source: A nationwide online survey of 1,917 people who either had surgery in the past year or were relatives or caregivers of someone who did.
Disclosures: The study authors reported having no relevant financial disclosures.
Stanford program takes aim at resident burnout
JACKSONVILLE, FLA. – When an admired surgical resident from Stanford (Calif.) University took his own life during his fellowship within 4 months of completing his residency, it sent a wake-up call to the residency program directors that burnout of surgical and medical residents was real and that something had to be done about it.
So Stanford launched a programmed approach to address resident burnout that includes group counseling, retreats, and even a fully stocked refrigerator accessible 24 hours a day, and found that after 3 years residents reported feeling more “in balance” than they did before the program started, said Dr. Claudia Mueller, a pediatric surgeon at Stanford, who presented a poster on the program at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The surgery department at Stanford has charted the progress of the program to address burnout among surgical residents. The effort started with the creation of a committee at the behest of Dr. Ralph Greco, former Stanford residency program director and study coauthor. “This group was intentionally resident driven so that we could figure out how best to look at four concepts of wellness – psychological, physical, social, and professional – from the resident perspective, because all four areas are necessary,” Dr. Mueller said.
Components of the program include outside group activities, group sessions on a 4- to 6-week schedule with a psychologist who is also available for individual sessions, and wellness visits to doctors.
To evaluate the program, the study authors had the surgical residents complete two different surveys, the Life Balance survey and the Causes of Stress survey, at separate times during 2013-2015. In the first assessment, only 5 of 25 residents surveyed achieved scores indicating their lives were in balance. “We knew that something was off,” Dr. Mueller said.
First-year residents were more likely to report feeling in balance than were more senior colleagues, Dr. Mueller said. “After about 3 years, we looked at how residents were doing in terms of balance, and what we found is that there have been some improvements, although not as many as we would like,” she said. “Junior residents in particular seemed to have shown some improvements in their overall balance.”
The concept is reproducible at other institutions, Dr. Mueller said. Dr. Ellen Morrow, a former Stanford resident, has started a similar program at the University of Utah, and other residency managers have approached Stanford for advice. Dr. Mueller said she believes that one key to the program is the involvement of residents. “It has to be what the residents want, not what we think they want,” she said.
“Our program came out of a very tragic event,” Dr. Mueller said. “We’re trying obviously not only to prevent a tragedy like that from happening again, but to also improve the lives of residents overall. The burnout is everywhere.”
Dr. Mueller said she had no financial relationships to disclose.
JACKSONVILLE, FLA. – When an admired surgical resident from Stanford (Calif.) University took his own life during his fellowship within 4 months of completing his residency, it sent a wake-up call to the residency program directors that burnout of surgical and medical residents was real and that something had to be done about it.
So Stanford launched a programmed approach to address resident burnout that includes group counseling, retreats, and even a fully stocked refrigerator accessible 24 hours a day, and found that after 3 years residents reported feeling more “in balance” than they did before the program started, said Dr. Claudia Mueller, a pediatric surgeon at Stanford, who presented a poster on the program at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The surgery department at Stanford has charted the progress of the program to address burnout among surgical residents. The effort started with the creation of a committee at the behest of Dr. Ralph Greco, former Stanford residency program director and study coauthor. “This group was intentionally resident driven so that we could figure out how best to look at four concepts of wellness – psychological, physical, social, and professional – from the resident perspective, because all four areas are necessary,” Dr. Mueller said.
Components of the program include outside group activities, group sessions on a 4- to 6-week schedule with a psychologist who is also available for individual sessions, and wellness visits to doctors.
To evaluate the program, the study authors had the surgical residents complete two different surveys, the Life Balance survey and the Causes of Stress survey, at separate times during 2013-2015. In the first assessment, only 5 of 25 residents surveyed achieved scores indicating their lives were in balance. “We knew that something was off,” Dr. Mueller said.
First-year residents were more likely to report feeling in balance than were more senior colleagues, Dr. Mueller said. “After about 3 years, we looked at how residents were doing in terms of balance, and what we found is that there have been some improvements, although not as many as we would like,” she said. “Junior residents in particular seemed to have shown some improvements in their overall balance.”
The concept is reproducible at other institutions, Dr. Mueller said. Dr. Ellen Morrow, a former Stanford resident, has started a similar program at the University of Utah, and other residency managers have approached Stanford for advice. Dr. Mueller said she believes that one key to the program is the involvement of residents. “It has to be what the residents want, not what we think they want,” she said.
“Our program came out of a very tragic event,” Dr. Mueller said. “We’re trying obviously not only to prevent a tragedy like that from happening again, but to also improve the lives of residents overall. The burnout is everywhere.”
Dr. Mueller said she had no financial relationships to disclose.
JACKSONVILLE, FLA. – When an admired surgical resident from Stanford (Calif.) University took his own life during his fellowship within 4 months of completing his residency, it sent a wake-up call to the residency program directors that burnout of surgical and medical residents was real and that something had to be done about it.
So Stanford launched a programmed approach to address resident burnout that includes group counseling, retreats, and even a fully stocked refrigerator accessible 24 hours a day, and found that after 3 years residents reported feeling more “in balance” than they did before the program started, said Dr. Claudia Mueller, a pediatric surgeon at Stanford, who presented a poster on the program at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The surgery department at Stanford has charted the progress of the program to address burnout among surgical residents. The effort started with the creation of a committee at the behest of Dr. Ralph Greco, former Stanford residency program director and study coauthor. “This group was intentionally resident driven so that we could figure out how best to look at four concepts of wellness – psychological, physical, social, and professional – from the resident perspective, because all four areas are necessary,” Dr. Mueller said.
Components of the program include outside group activities, group sessions on a 4- to 6-week schedule with a psychologist who is also available for individual sessions, and wellness visits to doctors.
To evaluate the program, the study authors had the surgical residents complete two different surveys, the Life Balance survey and the Causes of Stress survey, at separate times during 2013-2015. In the first assessment, only 5 of 25 residents surveyed achieved scores indicating their lives were in balance. “We knew that something was off,” Dr. Mueller said.
First-year residents were more likely to report feeling in balance than were more senior colleagues, Dr. Mueller said. “After about 3 years, we looked at how residents were doing in terms of balance, and what we found is that there have been some improvements, although not as many as we would like,” she said. “Junior residents in particular seemed to have shown some improvements in their overall balance.”
The concept is reproducible at other institutions, Dr. Mueller said. Dr. Ellen Morrow, a former Stanford resident, has started a similar program at the University of Utah, and other residency managers have approached Stanford for advice. Dr. Mueller said she believes that one key to the program is the involvement of residents. “It has to be what the residents want, not what we think they want,” she said.
“Our program came out of a very tragic event,” Dr. Mueller said. “We’re trying obviously not only to prevent a tragedy like that from happening again, but to also improve the lives of residents overall. The burnout is everywhere.”
Dr. Mueller said she had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Emergency hernia surgery risk predicted by access, age, and race
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Disparities among patients more likely to get emergency rather than elective ventral hernia repair include race, insurance status, and advanced age.
Major finding: Among demographic groups with a significantly higher likelihood of undergoing emergency ventral hernia repair were blacks (odds ratio, 1.64), Hispanics (OR, 1.44), and people over age 85 (OR, 2.23).
Data source: Nationwide Inpatient Sample of 453,000 adults who had inpatient ventral hernia repair from 2003 to 2011.
Disclosures: The study authors reported having no relevant financial disclosures.
STS: Minimizing LVAD pump thrombosis poses new challenges
PHOENIX – Cardiothoracic surgeons who implant left ventricular assist devices in patients with failing hearts remain at a loss to fully explain why they started seeing a sharp increase in thrombus clogging in these devices in 2012, but nevertheless they are gaining a better sense of how to minimize the risk.
Three key principles for minimizing thrombosis risk are selecting the right patients to receive left ventricular assist devices (LVAD), applying optimal management strategies once patients receive a LVAD, and maintaining adequate flow of blood through the pump, Dr. Francis D. Pagani said in a talk at a session devoted to pump thrombosis at the annual meeting of the Society of Thoracic Surgeons.
Other critical aspects include optimal implantation technique, quick work-up of patients to rule out reversible LVAD inflow or outflow problems once pump thrombosis is suspected, and ceasing medical therapy of the thrombosis if it proves ineffective and instead progress to surgical pump exchange, pump explantation, or heart transplant when necessary, said Dr. Ahmet Kilic, a cardiothoracic surgeon at the Ohio State University, Columbus.
Another key issue is that, now that the pump thrombosis incidence is averaging about 10% of LVAD recipients, with an incidence rate during 2-year follow-up as high as 24% reported from one series, surgeons and physicians who care for LVAD patients must have a high index of suspicion and routinely screen LVAD recipients for early signs of pump thrombosis. The best way to catch pump thrombosis early seems to be by regularly measuring patients’ serum level of lactate dehydrogenase (LDH), said Dr. Robert L. Kormos, professor of surgery and director of the artificial heart program at the University of Pittsburgh.
“We measure LDH on most clinic visits, whether or not the patient has an indication of pump thrombosis. We need to screen [LDH levels] much more routinely than we used to,” he said during the session. “Elevated LDH is probably the first and most reliable early sign, but you need to also assess LDH isoenzymes because we’ve had patients with an elevation but no sign of pump thrombosis, and their isoenzymes showed that the increased LDH was coming from their liver,” Dr. Kormos said in an interview.
Although serial measurements and isoenzyme analysis can establish a sharp rise in heart-specific LDH in an individual patient, a report at the meeting documented that in a series of 53 patients with pump thrombosis treated at either of two U.S. centers, an LDH level of at least 1,155 IU/L flagged pump thrombosis with a fairly high sensitivity and specificity. This LDH level is roughly five times the upper limit of normal, noted Dr. Pagani, professor of surgery and surgical director of adult heart transplantation at the University of Michigan, Ann Arbor, and a senior author on this report.
But prior to this report Dr. Kormos said that he regarded a LDH level of 600-800 IU/L as enough of an elevation above normal to prompt concern and investigation. And he criticized some LVAD programs that allow LDH levels to rise much higher.
“I know of clinicians who see a LDH of 1,500-2,000 IU/L but the patient seems okay and they wonder if they should change out the pump. For me, it’s a no brainer. Others try to list a patient like this for a heart transplant so they can avoid doing a pump exchange. I think that’s dangerous; it risks liver failure or renal failure. I would not sit on any LVAD that is starting to produce signs of hemolysis syndrome, but some places do this,” Dr. Kormos said in an interview.
“Pump thrombosis probably did not get addressed in as timely a fashion as it should have been” when it was first seen on the rise in 2012, noted Dr. James K. Kirklin, professor of surgery and director of cardiothoracic surgery at the University of Alabama, Birmingham. “It is now being addressed, and we realize that this is not just a pump problem but also involves patient factors and management factors that we need to learn more about. We are quite ignorant of the patient factors and understanding their contributions to bleeding and thrombosis,” said Dr. Kirklin. He also acknowledged that whatever role the current generation of LVAD pumps play in causing thrombosis will not quickly resolve.
“I’m looking forward to a new generation of pumps, but the pumps we have today will probably remain for another 3-5 years.”
The issue of LVAD pump thrombosis first came into clear focus with publication at the start of 2014 of a report that tracked its incidence from 2004 to mid-2013 at three U.S. centers that had placed a total of 895 LVADs in 837 patients. The annual rate of new episodes of pump thrombosis jumped from about 1%-2% of LVAD recipients throughout the first part of the study period through the end of 2011, to an annual rate of about 10% by mid 2013 (N Engl J Med. 2014 Jan 2;370[1]:33-40).
“The inflection occurred in about 2012,” noted Dr. Nicholas G. Smedira, a cardiothoracic surgeon at the Cleveland Clinic. “No one has figured out why” the incidence suddenly spiked starting in 2012 and intensified in 2013, he said. This epidemic of pump thrombosis has produced “devastating complications” that have led to multiple readmissions and reduced cost-effectiveness of LVADs and has affected how the heart transplant community allocates hearts, Dr. Smedira said during his talk at the session. He noted that once the surge in pump thrombosis started, the timing of the appearance of significant thrombus shifted earlier, often occurring within 2-3 months after LVAD placement. There now is “increasing device-related pessimism” and increasing demoralization among clinicians because of this recurring complication, he said.
More recent data show the trend toward increasingly higher rates of pump thrombosis continuing through the end of 2013, with the situation during 2014 a bit less clear. Late last year, data from 9,808 U.S. patients who received an LVAD and entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed that the incidence of pump thrombosis during the first 6 months following an implant rose from 1% in 2008 to 2% in 2009 and in 2010, 4% in 2011, 7% in 2012, 8% in 2013, and then eased back to 5% in the first half of 2014 (J Heart Lung Transplant. 2015 Dec;34[12]:1515-26). The annual rate rose from 2% in 2008 to a peak of 11% in 2013, with 12-month data from 2014 not yet available at the time of this report.
“The modest reduction of observed pump thrombosis at 6 months during 2014 has occurred in a milieu of heightened intensity of anti-coagulation management, greater surgical awareness of optimal pump implantation and positioning and pump speed management. Thus, one may speculate that current thrombosis risk-mitigation strategies have contributed to reducing but not eliminating the increased thrombosis risk observed since 2011,” concluded the authors of the report.
Surgeons and cardiologists must now have a high index of suspicion for pump thrombosis in LVAD recipients, and be especially on the lookout for four key flags of a problem, said Dr. Kormos. The first is a rising LDH level, but additional flags include an isolated power elevation that doesn’t correlate with anything else, evidence of hemolysis, and new-onset heart failure symptoms. These can occur individually or in some combination. He recommended following a diagnostic algorithm first presented in 2013 that remains very valid today (J Heart Lung Transplant. 2013 July;32[7]:667-70).
Dr. Kormos also highlighted that the presentation of pump thrombosis can differ between the two LVADs most commonly used in U.S. practice, the HeartMate II and the HeartWare devices. A LDH elevation is primarily an indicator for HeartMate II, while both that model and the HeartWare device show sustained, isolated power elevations when thrombosis occurs.
Dr. Pagani, Dr. Kirklin, and Dr. Smedira had no disclosures. Dr. Kormos has received travel support from HeartWare. Dr. Kilic has been a consultant to Thoratec and a speaker on behalf of Baxter International.
On Twitter @mitchelzoler
Dr. Hossein Almassi, FCCP, comments: With improvements in technology and development of rotary pumps, there has been a significant growth in the use of mechanical circulatory support (MCS) for treatment of end stage heart failure with a parallel improvement in patients’ survival and the quality of life.

|
| Dr. Hossein Almassi |
The authors of this report presented at the 2016 annual meeting of the STS, are authorities in the field of MCS outlining the observed increase in pump thrombosis noted in 2012. The sharp increase in the thrombosis rate is different from the lower incidence seen in the preapproval stage of the pump trial.
It should be noted that the report is related mainly to the HeatMate II left ventricular assist device (LVAD) and not the more recently implanted HeartWare device.
The diagnostic algorithm outlined in the accompanying reference (J Heart Lung Transplant. 2013 July;32[7]:667-70) regarding the diagnosis and management of suspected pump thrombosis is worth reading with the main criteria heralding a potential pump thrombosis being 1)sustained pump power elevation, 2) elevation of cardiac LDH or plasma-free hemoglobin, 3) hemolysis, and 4) symptoms of heart failure.
With further refinements in technology, the field of MCS is awaiting the development of newer LVAD devices that would mitigate the serious problem of pump thrombosis.
Dr. Hossein Almassi, FCCP, comments: With improvements in technology and development of rotary pumps, there has been a significant growth in the use of mechanical circulatory support (MCS) for treatment of end stage heart failure with a parallel improvement in patients’ survival and the quality of life.

|
| Dr. Hossein Almassi |
The authors of this report presented at the 2016 annual meeting of the STS, are authorities in the field of MCS outlining the observed increase in pump thrombosis noted in 2012. The sharp increase in the thrombosis rate is different from the lower incidence seen in the preapproval stage of the pump trial.
It should be noted that the report is related mainly to the HeatMate II left ventricular assist device (LVAD) and not the more recently implanted HeartWare device.
The diagnostic algorithm outlined in the accompanying reference (J Heart Lung Transplant. 2013 July;32[7]:667-70) regarding the diagnosis and management of suspected pump thrombosis is worth reading with the main criteria heralding a potential pump thrombosis being 1)sustained pump power elevation, 2) elevation of cardiac LDH or plasma-free hemoglobin, 3) hemolysis, and 4) symptoms of heart failure.
With further refinements in technology, the field of MCS is awaiting the development of newer LVAD devices that would mitigate the serious problem of pump thrombosis.
Dr. Hossein Almassi, FCCP, comments: With improvements in technology and development of rotary pumps, there has been a significant growth in the use of mechanical circulatory support (MCS) for treatment of end stage heart failure with a parallel improvement in patients’ survival and the quality of life.

|
| Dr. Hossein Almassi |
The authors of this report presented at the 2016 annual meeting of the STS, are authorities in the field of MCS outlining the observed increase in pump thrombosis noted in 2012. The sharp increase in the thrombosis rate is different from the lower incidence seen in the preapproval stage of the pump trial.
It should be noted that the report is related mainly to the HeatMate II left ventricular assist device (LVAD) and not the more recently implanted HeartWare device.
The diagnostic algorithm outlined in the accompanying reference (J Heart Lung Transplant. 2013 July;32[7]:667-70) regarding the diagnosis and management of suspected pump thrombosis is worth reading with the main criteria heralding a potential pump thrombosis being 1)sustained pump power elevation, 2) elevation of cardiac LDH or plasma-free hemoglobin, 3) hemolysis, and 4) symptoms of heart failure.
With further refinements in technology, the field of MCS is awaiting the development of newer LVAD devices that would mitigate the serious problem of pump thrombosis.
PHOENIX – Cardiothoracic surgeons who implant left ventricular assist devices in patients with failing hearts remain at a loss to fully explain why they started seeing a sharp increase in thrombus clogging in these devices in 2012, but nevertheless they are gaining a better sense of how to minimize the risk.
Three key principles for minimizing thrombosis risk are selecting the right patients to receive left ventricular assist devices (LVAD), applying optimal management strategies once patients receive a LVAD, and maintaining adequate flow of blood through the pump, Dr. Francis D. Pagani said in a talk at a session devoted to pump thrombosis at the annual meeting of the Society of Thoracic Surgeons.
Other critical aspects include optimal implantation technique, quick work-up of patients to rule out reversible LVAD inflow or outflow problems once pump thrombosis is suspected, and ceasing medical therapy of the thrombosis if it proves ineffective and instead progress to surgical pump exchange, pump explantation, or heart transplant when necessary, said Dr. Ahmet Kilic, a cardiothoracic surgeon at the Ohio State University, Columbus.
Another key issue is that, now that the pump thrombosis incidence is averaging about 10% of LVAD recipients, with an incidence rate during 2-year follow-up as high as 24% reported from one series, surgeons and physicians who care for LVAD patients must have a high index of suspicion and routinely screen LVAD recipients for early signs of pump thrombosis. The best way to catch pump thrombosis early seems to be by regularly measuring patients’ serum level of lactate dehydrogenase (LDH), said Dr. Robert L. Kormos, professor of surgery and director of the artificial heart program at the University of Pittsburgh.
“We measure LDH on most clinic visits, whether or not the patient has an indication of pump thrombosis. We need to screen [LDH levels] much more routinely than we used to,” he said during the session. “Elevated LDH is probably the first and most reliable early sign, but you need to also assess LDH isoenzymes because we’ve had patients with an elevation but no sign of pump thrombosis, and their isoenzymes showed that the increased LDH was coming from their liver,” Dr. Kormos said in an interview.
Although serial measurements and isoenzyme analysis can establish a sharp rise in heart-specific LDH in an individual patient, a report at the meeting documented that in a series of 53 patients with pump thrombosis treated at either of two U.S. centers, an LDH level of at least 1,155 IU/L flagged pump thrombosis with a fairly high sensitivity and specificity. This LDH level is roughly five times the upper limit of normal, noted Dr. Pagani, professor of surgery and surgical director of adult heart transplantation at the University of Michigan, Ann Arbor, and a senior author on this report.
But prior to this report Dr. Kormos said that he regarded a LDH level of 600-800 IU/L as enough of an elevation above normal to prompt concern and investigation. And he criticized some LVAD programs that allow LDH levels to rise much higher.
“I know of clinicians who see a LDH of 1,500-2,000 IU/L but the patient seems okay and they wonder if they should change out the pump. For me, it’s a no brainer. Others try to list a patient like this for a heart transplant so they can avoid doing a pump exchange. I think that’s dangerous; it risks liver failure or renal failure. I would not sit on any LVAD that is starting to produce signs of hemolysis syndrome, but some places do this,” Dr. Kormos said in an interview.
“Pump thrombosis probably did not get addressed in as timely a fashion as it should have been” when it was first seen on the rise in 2012, noted Dr. James K. Kirklin, professor of surgery and director of cardiothoracic surgery at the University of Alabama, Birmingham. “It is now being addressed, and we realize that this is not just a pump problem but also involves patient factors and management factors that we need to learn more about. We are quite ignorant of the patient factors and understanding their contributions to bleeding and thrombosis,” said Dr. Kirklin. He also acknowledged that whatever role the current generation of LVAD pumps play in causing thrombosis will not quickly resolve.
“I’m looking forward to a new generation of pumps, but the pumps we have today will probably remain for another 3-5 years.”
The issue of LVAD pump thrombosis first came into clear focus with publication at the start of 2014 of a report that tracked its incidence from 2004 to mid-2013 at three U.S. centers that had placed a total of 895 LVADs in 837 patients. The annual rate of new episodes of pump thrombosis jumped from about 1%-2% of LVAD recipients throughout the first part of the study period through the end of 2011, to an annual rate of about 10% by mid 2013 (N Engl J Med. 2014 Jan 2;370[1]:33-40).
“The inflection occurred in about 2012,” noted Dr. Nicholas G. Smedira, a cardiothoracic surgeon at the Cleveland Clinic. “No one has figured out why” the incidence suddenly spiked starting in 2012 and intensified in 2013, he said. This epidemic of pump thrombosis has produced “devastating complications” that have led to multiple readmissions and reduced cost-effectiveness of LVADs and has affected how the heart transplant community allocates hearts, Dr. Smedira said during his talk at the session. He noted that once the surge in pump thrombosis started, the timing of the appearance of significant thrombus shifted earlier, often occurring within 2-3 months after LVAD placement. There now is “increasing device-related pessimism” and increasing demoralization among clinicians because of this recurring complication, he said.
More recent data show the trend toward increasingly higher rates of pump thrombosis continuing through the end of 2013, with the situation during 2014 a bit less clear. Late last year, data from 9,808 U.S. patients who received an LVAD and entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed that the incidence of pump thrombosis during the first 6 months following an implant rose from 1% in 2008 to 2% in 2009 and in 2010, 4% in 2011, 7% in 2012, 8% in 2013, and then eased back to 5% in the first half of 2014 (J Heart Lung Transplant. 2015 Dec;34[12]:1515-26). The annual rate rose from 2% in 2008 to a peak of 11% in 2013, with 12-month data from 2014 not yet available at the time of this report.
“The modest reduction of observed pump thrombosis at 6 months during 2014 has occurred in a milieu of heightened intensity of anti-coagulation management, greater surgical awareness of optimal pump implantation and positioning and pump speed management. Thus, one may speculate that current thrombosis risk-mitigation strategies have contributed to reducing but not eliminating the increased thrombosis risk observed since 2011,” concluded the authors of the report.
Surgeons and cardiologists must now have a high index of suspicion for pump thrombosis in LVAD recipients, and be especially on the lookout for four key flags of a problem, said Dr. Kormos. The first is a rising LDH level, but additional flags include an isolated power elevation that doesn’t correlate with anything else, evidence of hemolysis, and new-onset heart failure symptoms. These can occur individually or in some combination. He recommended following a diagnostic algorithm first presented in 2013 that remains very valid today (J Heart Lung Transplant. 2013 July;32[7]:667-70).
Dr. Kormos also highlighted that the presentation of pump thrombosis can differ between the two LVADs most commonly used in U.S. practice, the HeartMate II and the HeartWare devices. A LDH elevation is primarily an indicator for HeartMate II, while both that model and the HeartWare device show sustained, isolated power elevations when thrombosis occurs.
Dr. Pagani, Dr. Kirklin, and Dr. Smedira had no disclosures. Dr. Kormos has received travel support from HeartWare. Dr. Kilic has been a consultant to Thoratec and a speaker on behalf of Baxter International.
On Twitter @mitchelzoler
PHOENIX – Cardiothoracic surgeons who implant left ventricular assist devices in patients with failing hearts remain at a loss to fully explain why they started seeing a sharp increase in thrombus clogging in these devices in 2012, but nevertheless they are gaining a better sense of how to minimize the risk.
Three key principles for minimizing thrombosis risk are selecting the right patients to receive left ventricular assist devices (LVAD), applying optimal management strategies once patients receive a LVAD, and maintaining adequate flow of blood through the pump, Dr. Francis D. Pagani said in a talk at a session devoted to pump thrombosis at the annual meeting of the Society of Thoracic Surgeons.
Other critical aspects include optimal implantation technique, quick work-up of patients to rule out reversible LVAD inflow or outflow problems once pump thrombosis is suspected, and ceasing medical therapy of the thrombosis if it proves ineffective and instead progress to surgical pump exchange, pump explantation, or heart transplant when necessary, said Dr. Ahmet Kilic, a cardiothoracic surgeon at the Ohio State University, Columbus.
Another key issue is that, now that the pump thrombosis incidence is averaging about 10% of LVAD recipients, with an incidence rate during 2-year follow-up as high as 24% reported from one series, surgeons and physicians who care for LVAD patients must have a high index of suspicion and routinely screen LVAD recipients for early signs of pump thrombosis. The best way to catch pump thrombosis early seems to be by regularly measuring patients’ serum level of lactate dehydrogenase (LDH), said Dr. Robert L. Kormos, professor of surgery and director of the artificial heart program at the University of Pittsburgh.
“We measure LDH on most clinic visits, whether or not the patient has an indication of pump thrombosis. We need to screen [LDH levels] much more routinely than we used to,” he said during the session. “Elevated LDH is probably the first and most reliable early sign, but you need to also assess LDH isoenzymes because we’ve had patients with an elevation but no sign of pump thrombosis, and their isoenzymes showed that the increased LDH was coming from their liver,” Dr. Kormos said in an interview.
Although serial measurements and isoenzyme analysis can establish a sharp rise in heart-specific LDH in an individual patient, a report at the meeting documented that in a series of 53 patients with pump thrombosis treated at either of two U.S. centers, an LDH level of at least 1,155 IU/L flagged pump thrombosis with a fairly high sensitivity and specificity. This LDH level is roughly five times the upper limit of normal, noted Dr. Pagani, professor of surgery and surgical director of adult heart transplantation at the University of Michigan, Ann Arbor, and a senior author on this report.
But prior to this report Dr. Kormos said that he regarded a LDH level of 600-800 IU/L as enough of an elevation above normal to prompt concern and investigation. And he criticized some LVAD programs that allow LDH levels to rise much higher.
“I know of clinicians who see a LDH of 1,500-2,000 IU/L but the patient seems okay and they wonder if they should change out the pump. For me, it’s a no brainer. Others try to list a patient like this for a heart transplant so they can avoid doing a pump exchange. I think that’s dangerous; it risks liver failure or renal failure. I would not sit on any LVAD that is starting to produce signs of hemolysis syndrome, but some places do this,” Dr. Kormos said in an interview.
“Pump thrombosis probably did not get addressed in as timely a fashion as it should have been” when it was first seen on the rise in 2012, noted Dr. James K. Kirklin, professor of surgery and director of cardiothoracic surgery at the University of Alabama, Birmingham. “It is now being addressed, and we realize that this is not just a pump problem but also involves patient factors and management factors that we need to learn more about. We are quite ignorant of the patient factors and understanding their contributions to bleeding and thrombosis,” said Dr. Kirklin. He also acknowledged that whatever role the current generation of LVAD pumps play in causing thrombosis will not quickly resolve.
“I’m looking forward to a new generation of pumps, but the pumps we have today will probably remain for another 3-5 years.”
The issue of LVAD pump thrombosis first came into clear focus with publication at the start of 2014 of a report that tracked its incidence from 2004 to mid-2013 at three U.S. centers that had placed a total of 895 LVADs in 837 patients. The annual rate of new episodes of pump thrombosis jumped from about 1%-2% of LVAD recipients throughout the first part of the study period through the end of 2011, to an annual rate of about 10% by mid 2013 (N Engl J Med. 2014 Jan 2;370[1]:33-40).
“The inflection occurred in about 2012,” noted Dr. Nicholas G. Smedira, a cardiothoracic surgeon at the Cleveland Clinic. “No one has figured out why” the incidence suddenly spiked starting in 2012 and intensified in 2013, he said. This epidemic of pump thrombosis has produced “devastating complications” that have led to multiple readmissions and reduced cost-effectiveness of LVADs and has affected how the heart transplant community allocates hearts, Dr. Smedira said during his talk at the session. He noted that once the surge in pump thrombosis started, the timing of the appearance of significant thrombus shifted earlier, often occurring within 2-3 months after LVAD placement. There now is “increasing device-related pessimism” and increasing demoralization among clinicians because of this recurring complication, he said.
More recent data show the trend toward increasingly higher rates of pump thrombosis continuing through the end of 2013, with the situation during 2014 a bit less clear. Late last year, data from 9,808 U.S. patients who received an LVAD and entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed that the incidence of pump thrombosis during the first 6 months following an implant rose from 1% in 2008 to 2% in 2009 and in 2010, 4% in 2011, 7% in 2012, 8% in 2013, and then eased back to 5% in the first half of 2014 (J Heart Lung Transplant. 2015 Dec;34[12]:1515-26). The annual rate rose from 2% in 2008 to a peak of 11% in 2013, with 12-month data from 2014 not yet available at the time of this report.
“The modest reduction of observed pump thrombosis at 6 months during 2014 has occurred in a milieu of heightened intensity of anti-coagulation management, greater surgical awareness of optimal pump implantation and positioning and pump speed management. Thus, one may speculate that current thrombosis risk-mitigation strategies have contributed to reducing but not eliminating the increased thrombosis risk observed since 2011,” concluded the authors of the report.
Surgeons and cardiologists must now have a high index of suspicion for pump thrombosis in LVAD recipients, and be especially on the lookout for four key flags of a problem, said Dr. Kormos. The first is a rising LDH level, but additional flags include an isolated power elevation that doesn’t correlate with anything else, evidence of hemolysis, and new-onset heart failure symptoms. These can occur individually or in some combination. He recommended following a diagnostic algorithm first presented in 2013 that remains very valid today (J Heart Lung Transplant. 2013 July;32[7]:667-70).
Dr. Kormos also highlighted that the presentation of pump thrombosis can differ between the two LVADs most commonly used in U.S. practice, the HeartMate II and the HeartWare devices. A LDH elevation is primarily an indicator for HeartMate II, while both that model and the HeartWare device show sustained, isolated power elevations when thrombosis occurs.
Dr. Pagani, Dr. Kirklin, and Dr. Smedira had no disclosures. Dr. Kormos has received travel support from HeartWare. Dr. Kilic has been a consultant to Thoratec and a speaker on behalf of Baxter International.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
Supreme Court: Fate of health care cases uncertain after Scalia death
The fate of several high-profile health care cases remains uncertain after the death of U.S. Supreme Court Justice Antonin Scalia.
The eight remaining justices will hear oral arguments on and weigh in on a range of cases this term. Justice Scalia’s death however, means the possibility of a tie vote in some cases, which could lead to conflicting case law across states.
“Most Supreme Court decisions are not decided on a 5-to-4 split, so presumably regular business will continue as to most of the cases they are deciding,” said Timothy S. Jost, health law professor at Washington and Lee University in Lexington, Va. “However, for some of the most important cases in health care – like the abortion decision or the contraceptive decision – it was likely there was going to be a 5-to-4 split. Of those cases, the justices can either hold them over or vote, in which case there [could] be a 4-to-4 split.”
If the court divides equally on a case, the lower court’s decision is affirmed. But the case would not have a Supreme Court precedent, meaning the lower ruling would apply only in the circuit court’s jurisdiction, said Eric J. Segall, a professor of law at Georgia State University, Atlanta.
In Whole Woman’s Health v. Cole, also known as Whole Woman’s Health v. Hellerstedt, for instance, a split would uphold an appellate decision that allowed abortion restrictions in Texas to go forward. In that case, the state is battling health providers over a mandate that abortion providers must have admitting privileges at a hospital within 30 miles and that abortion clinics must meet the same requirements as those of ambulatory surgical centers (ASCs). The 5th U.S. Circuit Court of Appeals ruled that the regulations do not impose an undue burden on a patient’s right to get an abortion.
“If a 5-4 [Supreme Court decision] upheld those restrictions, that would be national law for the whole country, and it would be a huge deal,” Mr. Segall said in an interview. “If it’s a 4-4 tie, than in Texas and two other states, the Texas decision would still be good law, but it would have no effect outside that circuit.”
In the case of Zubik v. Burwell however, a split vote would mean nationwide differences in how the Affordable Care Act’s contraceptive mandate is applied, said Ilya Shapiro, a senior fellow in constitutional studies at the Cato Institute. The Zubik case centers on whether the ACA contraceptive-coverage mandate and its “accommodation” violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuits.
Because of the conflicting lower court opinions, if the Zubik case were decided 4-4, “the regulation [would be] in place in parts of the country and not in others,” Mr. Shapiro said in an interview. “That seems untenable. Cases like that especially, the court would likely delay the arguments that are currently scheduled until the next term.”
Justices can decide whether to vote or rehear cases that were already heard with Justice Scalia in attendance, but are not yet decided. They can also dismiss or wait to address cases next term. Decisions that were made with Justice Scalia’s vote, but were not yet published, will be void, Mr. Shapiro said. As for Justice Scalia’s replacement, Mr. Shapiro noted that even if President Obama makes a nomination and it is confirmed by the Senate, it would be too late to consider cases this term.
Mr. Segall stressed that it’s too early to tell how Justice Scalia’s death will impact ongoing and future cases and the court as a whole.
“We don’t really have a precedent for this,” he said. “We’ve had vacancies before, but we’ve never had a vacancy in an election year where [the Court comprised] four conservative Republicans and four liberal Democrats. I think we should all step back. There are so many imponderables.”
Supreme Court analysts predict the eight justices will announce their decisions – or lack thereof – during the last week of June.
Justice Scalia was known as the high court’s most vocal conservative and was the longest-serving current justice on the court, hearing cases for 29 years.
What’s on the docket?
The Supreme Court is set to decide a number of significant health law cases this term. Here are some of the most pressing ones and the issues at stake.
Argument date: March 23, 2016
The court will decide whether an accommodation under the ACA contraceptive mandate violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs, when the government has not proved that this compulsion is the least restrictive means of advancing a compelling interest. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches. The plaintiffs argue the process serves as a trigger that enables contraceptive use and makes the groups complicit. The government argues the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
Argument date: March 2, 2016
Justices will weigh whether two Texas regulations place an undue burden on a woman’s right to access an abortion. The regulations mandate that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as those of ambulatory surgical centers (ASCs). The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services states the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The case is sometimes cited as Whole Woman’s Health v. Hellerstedt.
Universal Health Services v. United States ex rel. Escobar
Argument date: To be determined
In question is whether the legal theory used by the federal government to bring False Claims Act (FCA) lawsuits is valid. The case centers on a patient who died after receiving care by Universal Health Services Inc. (UHS) in Lawrence, Mass. The patient’s parents sued UHS under both the federal and state False Claims Act laws alleging that UHS providers were improperly licensed and made fraudulent government claims. The Supreme Court will answer whether the implied certification test for determining when claims “sufficiently plead falsity” under the FCA is constitutional and if so, if the relevant statute needs to explicitly state the conditions of payment with which the defendant allegedly failed to comply. Physician associations are concerned that a ruling for the plaintiff will expand the FCA’s reach and increase false claim lawsuits against health providers.
Gobeille v. Liberty Mutual Insurance Company
Argument date: Dec. 2, 2015
The Supreme Court will decide whether a self-funded insurer must share certain information, such as claims and member data, with Vermont’s all-payer database. The state argues the information is needed to improve the cost and effectiveness of health care and that an adverse ruling would chill reform efforts in other states with similar databases. Liberty Mutual, which maintains a self-insured health plan for its employees, argues that the Employee Retirement Income Security Act of 1973 (ERISA) preempts state statutes that provide for “all payer” health care databases, and that it does not have to supply the information. Analysts say the case will ultimately decide to what extent federal law can facilitate the centralized management of health care.
On Twitter @legal_med
The fate of several high-profile health care cases remains uncertain after the death of U.S. Supreme Court Justice Antonin Scalia.
The eight remaining justices will hear oral arguments on and weigh in on a range of cases this term. Justice Scalia’s death however, means the possibility of a tie vote in some cases, which could lead to conflicting case law across states.
“Most Supreme Court decisions are not decided on a 5-to-4 split, so presumably regular business will continue as to most of the cases they are deciding,” said Timothy S. Jost, health law professor at Washington and Lee University in Lexington, Va. “However, for some of the most important cases in health care – like the abortion decision or the contraceptive decision – it was likely there was going to be a 5-to-4 split. Of those cases, the justices can either hold them over or vote, in which case there [could] be a 4-to-4 split.”
If the court divides equally on a case, the lower court’s decision is affirmed. But the case would not have a Supreme Court precedent, meaning the lower ruling would apply only in the circuit court’s jurisdiction, said Eric J. Segall, a professor of law at Georgia State University, Atlanta.
In Whole Woman’s Health v. Cole, also known as Whole Woman’s Health v. Hellerstedt, for instance, a split would uphold an appellate decision that allowed abortion restrictions in Texas to go forward. In that case, the state is battling health providers over a mandate that abortion providers must have admitting privileges at a hospital within 30 miles and that abortion clinics must meet the same requirements as those of ambulatory surgical centers (ASCs). The 5th U.S. Circuit Court of Appeals ruled that the regulations do not impose an undue burden on a patient’s right to get an abortion.
“If a 5-4 [Supreme Court decision] upheld those restrictions, that would be national law for the whole country, and it would be a huge deal,” Mr. Segall said in an interview. “If it’s a 4-4 tie, than in Texas and two other states, the Texas decision would still be good law, but it would have no effect outside that circuit.”
In the case of Zubik v. Burwell however, a split vote would mean nationwide differences in how the Affordable Care Act’s contraceptive mandate is applied, said Ilya Shapiro, a senior fellow in constitutional studies at the Cato Institute. The Zubik case centers on whether the ACA contraceptive-coverage mandate and its “accommodation” violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuits.
Because of the conflicting lower court opinions, if the Zubik case were decided 4-4, “the regulation [would be] in place in parts of the country and not in others,” Mr. Shapiro said in an interview. “That seems untenable. Cases like that especially, the court would likely delay the arguments that are currently scheduled until the next term.”
Justices can decide whether to vote or rehear cases that were already heard with Justice Scalia in attendance, but are not yet decided. They can also dismiss or wait to address cases next term. Decisions that were made with Justice Scalia’s vote, but were not yet published, will be void, Mr. Shapiro said. As for Justice Scalia’s replacement, Mr. Shapiro noted that even if President Obama makes a nomination and it is confirmed by the Senate, it would be too late to consider cases this term.
Mr. Segall stressed that it’s too early to tell how Justice Scalia’s death will impact ongoing and future cases and the court as a whole.
“We don’t really have a precedent for this,” he said. “We’ve had vacancies before, but we’ve never had a vacancy in an election year where [the Court comprised] four conservative Republicans and four liberal Democrats. I think we should all step back. There are so many imponderables.”
Supreme Court analysts predict the eight justices will announce their decisions – or lack thereof – during the last week of June.
Justice Scalia was known as the high court’s most vocal conservative and was the longest-serving current justice on the court, hearing cases for 29 years.
What’s on the docket?
The Supreme Court is set to decide a number of significant health law cases this term. Here are some of the most pressing ones and the issues at stake.
Argument date: March 23, 2016
The court will decide whether an accommodation under the ACA contraceptive mandate violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs, when the government has not proved that this compulsion is the least restrictive means of advancing a compelling interest. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches. The plaintiffs argue the process serves as a trigger that enables contraceptive use and makes the groups complicit. The government argues the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
Argument date: March 2, 2016
Justices will weigh whether two Texas regulations place an undue burden on a woman’s right to access an abortion. The regulations mandate that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as those of ambulatory surgical centers (ASCs). The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services states the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The case is sometimes cited as Whole Woman’s Health v. Hellerstedt.
Universal Health Services v. United States ex rel. Escobar
Argument date: To be determined
In question is whether the legal theory used by the federal government to bring False Claims Act (FCA) lawsuits is valid. The case centers on a patient who died after receiving care by Universal Health Services Inc. (UHS) in Lawrence, Mass. The patient’s parents sued UHS under both the federal and state False Claims Act laws alleging that UHS providers were improperly licensed and made fraudulent government claims. The Supreme Court will answer whether the implied certification test for determining when claims “sufficiently plead falsity” under the FCA is constitutional and if so, if the relevant statute needs to explicitly state the conditions of payment with which the defendant allegedly failed to comply. Physician associations are concerned that a ruling for the plaintiff will expand the FCA’s reach and increase false claim lawsuits against health providers.
Gobeille v. Liberty Mutual Insurance Company
Argument date: Dec. 2, 2015
The Supreme Court will decide whether a self-funded insurer must share certain information, such as claims and member data, with Vermont’s all-payer database. The state argues the information is needed to improve the cost and effectiveness of health care and that an adverse ruling would chill reform efforts in other states with similar databases. Liberty Mutual, which maintains a self-insured health plan for its employees, argues that the Employee Retirement Income Security Act of 1973 (ERISA) preempts state statutes that provide for “all payer” health care databases, and that it does not have to supply the information. Analysts say the case will ultimately decide to what extent federal law can facilitate the centralized management of health care.
On Twitter @legal_med
The fate of several high-profile health care cases remains uncertain after the death of U.S. Supreme Court Justice Antonin Scalia.
The eight remaining justices will hear oral arguments on and weigh in on a range of cases this term. Justice Scalia’s death however, means the possibility of a tie vote in some cases, which could lead to conflicting case law across states.
“Most Supreme Court decisions are not decided on a 5-to-4 split, so presumably regular business will continue as to most of the cases they are deciding,” said Timothy S. Jost, health law professor at Washington and Lee University in Lexington, Va. “However, for some of the most important cases in health care – like the abortion decision or the contraceptive decision – it was likely there was going to be a 5-to-4 split. Of those cases, the justices can either hold them over or vote, in which case there [could] be a 4-to-4 split.”
If the court divides equally on a case, the lower court’s decision is affirmed. But the case would not have a Supreme Court precedent, meaning the lower ruling would apply only in the circuit court’s jurisdiction, said Eric J. Segall, a professor of law at Georgia State University, Atlanta.
In Whole Woman’s Health v. Cole, also known as Whole Woman’s Health v. Hellerstedt, for instance, a split would uphold an appellate decision that allowed abortion restrictions in Texas to go forward. In that case, the state is battling health providers over a mandate that abortion providers must have admitting privileges at a hospital within 30 miles and that abortion clinics must meet the same requirements as those of ambulatory surgical centers (ASCs). The 5th U.S. Circuit Court of Appeals ruled that the regulations do not impose an undue burden on a patient’s right to get an abortion.
“If a 5-4 [Supreme Court decision] upheld those restrictions, that would be national law for the whole country, and it would be a huge deal,” Mr. Segall said in an interview. “If it’s a 4-4 tie, than in Texas and two other states, the Texas decision would still be good law, but it would have no effect outside that circuit.”
In the case of Zubik v. Burwell however, a split vote would mean nationwide differences in how the Affordable Care Act’s contraceptive mandate is applied, said Ilya Shapiro, a senior fellow in constitutional studies at the Cato Institute. The Zubik case centers on whether the ACA contraceptive-coverage mandate and its “accommodation” violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuits.
Because of the conflicting lower court opinions, if the Zubik case were decided 4-4, “the regulation [would be] in place in parts of the country and not in others,” Mr. Shapiro said in an interview. “That seems untenable. Cases like that especially, the court would likely delay the arguments that are currently scheduled until the next term.”
Justices can decide whether to vote or rehear cases that were already heard with Justice Scalia in attendance, but are not yet decided. They can also dismiss or wait to address cases next term. Decisions that were made with Justice Scalia’s vote, but were not yet published, will be void, Mr. Shapiro said. As for Justice Scalia’s replacement, Mr. Shapiro noted that even if President Obama makes a nomination and it is confirmed by the Senate, it would be too late to consider cases this term.
Mr. Segall stressed that it’s too early to tell how Justice Scalia’s death will impact ongoing and future cases and the court as a whole.
“We don’t really have a precedent for this,” he said. “We’ve had vacancies before, but we’ve never had a vacancy in an election year where [the Court comprised] four conservative Republicans and four liberal Democrats. I think we should all step back. There are so many imponderables.”
Supreme Court analysts predict the eight justices will announce their decisions – or lack thereof – during the last week of June.
Justice Scalia was known as the high court’s most vocal conservative and was the longest-serving current justice on the court, hearing cases for 29 years.
What’s on the docket?
The Supreme Court is set to decide a number of significant health law cases this term. Here are some of the most pressing ones and the issues at stake.
Argument date: March 23, 2016
The court will decide whether an accommodation under the ACA contraceptive mandate violates the Religious Freedom Restoration Act by forcing religious nonprofits to act in violation of their beliefs, when the government has not proved that this compulsion is the least restrictive means of advancing a compelling interest. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches. The plaintiffs argue the process serves as a trigger that enables contraceptive use and makes the groups complicit. The government argues the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
Argument date: March 2, 2016
Justices will weigh whether two Texas regulations place an undue burden on a woman’s right to access an abortion. The regulations mandate that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as those of ambulatory surgical centers (ASCs). The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services states the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The case is sometimes cited as Whole Woman’s Health v. Hellerstedt.
Universal Health Services v. United States ex rel. Escobar
Argument date: To be determined
In question is whether the legal theory used by the federal government to bring False Claims Act (FCA) lawsuits is valid. The case centers on a patient who died after receiving care by Universal Health Services Inc. (UHS) in Lawrence, Mass. The patient’s parents sued UHS under both the federal and state False Claims Act laws alleging that UHS providers were improperly licensed and made fraudulent government claims. The Supreme Court will answer whether the implied certification test for determining when claims “sufficiently plead falsity” under the FCA is constitutional and if so, if the relevant statute needs to explicitly state the conditions of payment with which the defendant allegedly failed to comply. Physician associations are concerned that a ruling for the plaintiff will expand the FCA’s reach and increase false claim lawsuits against health providers.
Gobeille v. Liberty Mutual Insurance Company
Argument date: Dec. 2, 2015
The Supreme Court will decide whether a self-funded insurer must share certain information, such as claims and member data, with Vermont’s all-payer database. The state argues the information is needed to improve the cost and effectiveness of health care and that an adverse ruling would chill reform efforts in other states with similar databases. Liberty Mutual, which maintains a self-insured health plan for its employees, argues that the Employee Retirement Income Security Act of 1973 (ERISA) preempts state statutes that provide for “all payer” health care databases, and that it does not have to supply the information. Analysts say the case will ultimately decide to what extent federal law can facilitate the centralized management of health care.
On Twitter @legal_med
Study validates cholecystectomy safe in obese
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
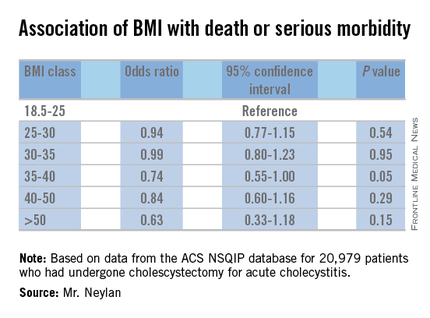
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
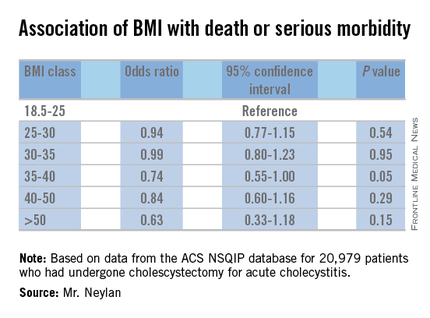
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
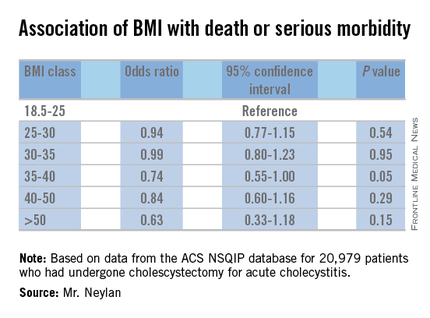
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Cholecystectomy for acute cholecystitis has been found to have a similar safety profile in obese and normal-weight patients.
Major finding: Rates of death/serious morbidity ranged from 6% to 9% across six different weight classes ranging from normal weight to morbidly obese.
Data source: Retrospective analysis of 20,979 patients who had cholecystectomy for cholecystitis from 2008 to 2015 drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database.
Disclosures: The study authors reported having no financial disclosures.
Show your FACS pride
The Division of Member Services strives to educate surgical patients about what it means to be treated by a surgeon who is a Fellow of the American College of Surgeons (FACS). As part of this campaign, the College has created a poster of the Fellowship Pledge that is suitable for display in waiting areas, exam rooms, and offices, and is available for purchase or free download. The Fellowship Pledge poster—available in seven languages: English, Arabic, Chinese (both Simplified and Traditional), Japanese, German, Portuguese and Spanish—may be displayed only by surgeons with the FACS designation.
ACS Fellows are committed to providing their patients with the highest standards of surgical care and pledge to protect the welfare and rights of their patients, to respect each patient’s autonomy and individuality, and to advance their knowledge and skills throughout their careers. The Fellowship Pledge poster is available for purchase for $10.00 including standard shipping, or can be downloaded for free. Visit the ACS Online Store at https://goo.gl/sCKiUc to download your poster. Two PDF versions are available; a 22” x 32” poster that may be printed by a professional print shop, or an 11” x 17” version that may be printed on a personal color printer.
The Division of Member Services strives to educate surgical patients about what it means to be treated by a surgeon who is a Fellow of the American College of Surgeons (FACS). As part of this campaign, the College has created a poster of the Fellowship Pledge that is suitable for display in waiting areas, exam rooms, and offices, and is available for purchase or free download. The Fellowship Pledge poster—available in seven languages: English, Arabic, Chinese (both Simplified and Traditional), Japanese, German, Portuguese and Spanish—may be displayed only by surgeons with the FACS designation.
ACS Fellows are committed to providing their patients with the highest standards of surgical care and pledge to protect the welfare and rights of their patients, to respect each patient’s autonomy and individuality, and to advance their knowledge and skills throughout their careers. The Fellowship Pledge poster is available for purchase for $10.00 including standard shipping, or can be downloaded for free. Visit the ACS Online Store at https://goo.gl/sCKiUc to download your poster. Two PDF versions are available; a 22” x 32” poster that may be printed by a professional print shop, or an 11” x 17” version that may be printed on a personal color printer.
The Division of Member Services strives to educate surgical patients about what it means to be treated by a surgeon who is a Fellow of the American College of Surgeons (FACS). As part of this campaign, the College has created a poster of the Fellowship Pledge that is suitable for display in waiting areas, exam rooms, and offices, and is available for purchase or free download. The Fellowship Pledge poster—available in seven languages: English, Arabic, Chinese (both Simplified and Traditional), Japanese, German, Portuguese and Spanish—may be displayed only by surgeons with the FACS designation.
ACS Fellows are committed to providing their patients with the highest standards of surgical care and pledge to protect the welfare and rights of their patients, to respect each patient’s autonomy and individuality, and to advance their knowledge and skills throughout their careers. The Fellowship Pledge poster is available for purchase for $10.00 including standard shipping, or can be downloaded for free. Visit the ACS Online Store at https://goo.gl/sCKiUc to download your poster. Two PDF versions are available; a 22” x 32” poster that may be printed by a professional print shop, or an 11” x 17” version that may be printed on a personal color printer.
Registration opens for 2016 Leadership & Advocacy Summit
Registration is now open for the fifth annual American College of Surgeons (ACS) 2016 Leadership & Advocacy Summit, April 9–12, at the JW Marriott, Washington, DC. The Summit is a dual meeting that offers volunteer leaders and advocates educational sessions fon effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2016 Leadership Summit
(https://www.facs.org/advocacy/participate/summit-2016) will commence the evening of Saturday, April 9, with a Welcome Reception and continue the morning of April 12 with presentations on conflict management, managing difficult or “courageous” conversations, and emotional intelligence. In addition, Adil Haider, MD, MPH, FACS, director, Kessler Center for Surgery and Public Health (CSPH), a joint initiative of Brigham and Women’s Hospital, Harvard Medical School, and the Harvard T.H. Chan School of Public Health, Boston, MA, will discuss unconscious bias and cultural competency in surgical care. During lunch, attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 10, with a keynote address by MSNBC Hardball host, Chris Matthews, who is also a frequent commentator and expert analyst on NBC’s TODAY Show. Monday, April 11, attendees will hear from speakers examining the political environment in Washington, DC, and across the nation, and vital health care issues.
Tuesday morning, attendees will use the knowledge gathered at the Summit when they meet with their senators and representative and/or congressional staff. Tuesday’s meetings provide an opportunity to rally surgery’s collective grassroots advocacy voice on vital issues.
For more information or to register for the 2016 Leadership & Advocacy Summit, go to the ACS website. (https://www.facs.org/advocacy/participate/summit-2016 ) The conference hotel reservation deadline is Friday, March 4.
Registration is now open for the fifth annual American College of Surgeons (ACS) 2016 Leadership & Advocacy Summit, April 9–12, at the JW Marriott, Washington, DC. The Summit is a dual meeting that offers volunteer leaders and advocates educational sessions fon effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2016 Leadership Summit
(https://www.facs.org/advocacy/participate/summit-2016) will commence the evening of Saturday, April 9, with a Welcome Reception and continue the morning of April 12 with presentations on conflict management, managing difficult or “courageous” conversations, and emotional intelligence. In addition, Adil Haider, MD, MPH, FACS, director, Kessler Center for Surgery and Public Health (CSPH), a joint initiative of Brigham and Women’s Hospital, Harvard Medical School, and the Harvard T.H. Chan School of Public Health, Boston, MA, will discuss unconscious bias and cultural competency in surgical care. During lunch, attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 10, with a keynote address by MSNBC Hardball host, Chris Matthews, who is also a frequent commentator and expert analyst on NBC’s TODAY Show. Monday, April 11, attendees will hear from speakers examining the political environment in Washington, DC, and across the nation, and vital health care issues.
Tuesday morning, attendees will use the knowledge gathered at the Summit when they meet with their senators and representative and/or congressional staff. Tuesday’s meetings provide an opportunity to rally surgery’s collective grassroots advocacy voice on vital issues.
For more information or to register for the 2016 Leadership & Advocacy Summit, go to the ACS website. (https://www.facs.org/advocacy/participate/summit-2016 ) The conference hotel reservation deadline is Friday, March 4.
Registration is now open for the fifth annual American College of Surgeons (ACS) 2016 Leadership & Advocacy Summit, April 9–12, at the JW Marriott, Washington, DC. The Summit is a dual meeting that offers volunteer leaders and advocates educational sessions fon effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2016 Leadership Summit
(https://www.facs.org/advocacy/participate/summit-2016) will commence the evening of Saturday, April 9, with a Welcome Reception and continue the morning of April 12 with presentations on conflict management, managing difficult or “courageous” conversations, and emotional intelligence. In addition, Adil Haider, MD, MPH, FACS, director, Kessler Center for Surgery and Public Health (CSPH), a joint initiative of Brigham and Women’s Hospital, Harvard Medical School, and the Harvard T.H. Chan School of Public Health, Boston, MA, will discuss unconscious bias and cultural competency in surgical care. During lunch, attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 10, with a keynote address by MSNBC Hardball host, Chris Matthews, who is also a frequent commentator and expert analyst on NBC’s TODAY Show. Monday, April 11, attendees will hear from speakers examining the political environment in Washington, DC, and across the nation, and vital health care issues.
Tuesday morning, attendees will use the knowledge gathered at the Summit when they meet with their senators and representative and/or congressional staff. Tuesday’s meetings provide an opportunity to rally surgery’s collective grassroots advocacy voice on vital issues.
For more information or to register for the 2016 Leadership & Advocacy Summit, go to the ACS website. (https://www.facs.org/advocacy/participate/summit-2016 ) The conference hotel reservation deadline is Friday, March 4.
Apply by April 1 to ACS Clinical Scholars in Residence Program
The application process for the American College of Surgeons (ACS) Clinical Scholars in Residence Program, a two-year on-site fellowship in surgical outcomes research, health services research, and health care policy, opened January 1. The deadline for submitting applications is April 1, 2016.
The fellowship, which will start July 1, 2017, will be performed at ACS headquarters in Chicago, IL, with additional funds provided for the scholar to complete a master’s program at Northwestern University in Chicago. Applicants must be U.S. citizens who have completed two years of clinical training and are able to obtain two years of program funding from their home institution or other granting agency. Applicants must be ACS members in good standing. The ACS will continue to seek external funding for the position, and candidates will be notified should funding become available.
The Clinical Scholar will work in multiple areas within the ACS Division of Research and Optimal Patient Care to advance the quality improvement initiatives of the ACS and to perform research relevant to ongoing projects. The Clinical Scholar will receive strong mentorship in clinical, statistical, and health services research. ACS Clinical Scholars in Residence have had excellent, productive experiences that have launched successful careers in this field.
Important Dates:
Interview notification: May 2, 2016
Interview process: May 2−31, 2016
Notification of appointment: June 10, 2016
Find more information on the ACS website. [https://www.facs.org/quality-programs/about/clinical-scholars-program] If you have additional questions, contact the ACS Clinical Scholars in Residence Program at [email protected].
The application process for the American College of Surgeons (ACS) Clinical Scholars in Residence Program, a two-year on-site fellowship in surgical outcomes research, health services research, and health care policy, opened January 1. The deadline for submitting applications is April 1, 2016.
The fellowship, which will start July 1, 2017, will be performed at ACS headquarters in Chicago, IL, with additional funds provided for the scholar to complete a master’s program at Northwestern University in Chicago. Applicants must be U.S. citizens who have completed two years of clinical training and are able to obtain two years of program funding from their home institution or other granting agency. Applicants must be ACS members in good standing. The ACS will continue to seek external funding for the position, and candidates will be notified should funding become available.
The Clinical Scholar will work in multiple areas within the ACS Division of Research and Optimal Patient Care to advance the quality improvement initiatives of the ACS and to perform research relevant to ongoing projects. The Clinical Scholar will receive strong mentorship in clinical, statistical, and health services research. ACS Clinical Scholars in Residence have had excellent, productive experiences that have launched successful careers in this field.
Important Dates:
Interview notification: May 2, 2016
Interview process: May 2−31, 2016
Notification of appointment: June 10, 2016
Find more information on the ACS website. [https://www.facs.org/quality-programs/about/clinical-scholars-program] If you have additional questions, contact the ACS Clinical Scholars in Residence Program at [email protected].
The application process for the American College of Surgeons (ACS) Clinical Scholars in Residence Program, a two-year on-site fellowship in surgical outcomes research, health services research, and health care policy, opened January 1. The deadline for submitting applications is April 1, 2016.
The fellowship, which will start July 1, 2017, will be performed at ACS headquarters in Chicago, IL, with additional funds provided for the scholar to complete a master’s program at Northwestern University in Chicago. Applicants must be U.S. citizens who have completed two years of clinical training and are able to obtain two years of program funding from their home institution or other granting agency. Applicants must be ACS members in good standing. The ACS will continue to seek external funding for the position, and candidates will be notified should funding become available.
The Clinical Scholar will work in multiple areas within the ACS Division of Research and Optimal Patient Care to advance the quality improvement initiatives of the ACS and to perform research relevant to ongoing projects. The Clinical Scholar will receive strong mentorship in clinical, statistical, and health services research. ACS Clinical Scholars in Residence have had excellent, productive experiences that have launched successful careers in this field.
Important Dates:
Interview notification: May 2, 2016
Interview process: May 2−31, 2016
Notification of appointment: June 10, 2016
Find more information on the ACS website. [https://www.facs.org/quality-programs/about/clinical-scholars-program] If you have additional questions, contact the ACS Clinical Scholars in Residence Program at [email protected].















