User login
Anticoagulation Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving treatment options for preventing stroke, acute coronary events, deep vein thrombosis, and pulmonary embolism in at-risk patients. The Anticoagulation Hub is powered by Frontline Medical Communications.
FDA approves betrixaban for VTE prophylaxis
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
FFR stumbles in revascularization deferral decisions for ACS
Paris – One-year outcomes were significantly worse in patients with acute coronary syndrome whose revascularization was deferred based upon the results of fractional flow reserve than with instantaneous wave-free ratio, in the largest-ever study of patients whose revascularization decision was guided by physiologic measurements obtained via a pressure guidewire.
“The hypothesis that some authors have put forth – that in an ACS the hyperemic response of the myocardium is blunted by the ACS, and that this will affect the FFR hyperemic index – is now strengthened,” Javier Escaned, MD, said in presenting the study results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The study was a pooled, patient-level meta-analysis of the 4,529 participants with angiographically determined intermediate-risk stenoses in the previously reported randomized DEFINE FLAIR (N Engl J Med. 2017 May 11;376[19]:1824-34) and iFR SWEDEHEART (N Engl J Med. 2017 May 11;376[19]:1813-23) studies. The primary endpoint was the composite of death, nonfatal MI, or unplanned coronary revascularization within 12 months. And while the analysis brought unwelcome news for proponents of FFR with regard to the subset of patients with ACS, such patients comprised only 17% of the total study population.
“I think that overall these results are very reassuring. The big finding is that we have dramatically improved the safety of deferral of revascularization using pressure guidewires. If you look at the MACE [major adverse cardiovascular event] rate in the deferred ACS group, it was about 6%, which is much less than the event rate at 1 year with deferral in patients with stable coronary disease in the pivotal DEFER trial [Circulation. 2001 Jun 19;103(24):2928-34], which was our former standard,” observed Dr. Escaned, an interventional cardiologist at San Carlos Hospital in Madrid and a DEFER coinvestigator.
He attributed these greatly improved outcomes of physiologically guided revascularization during the past 15 years to vastly improved stent technology and more effective optimal medical management.
Among the key findings of the combined analysis of DEFINE FLAIR and iFR SWEDEHEART:
• More patients were deferred from PCI when iFR was used for decision-making: 50%, compared with 45% in the FFR arm. Yet 1-year outcomes were as good in the deferred iFR group as in the FFR group overall, and better than with FFR in the deferred ACS patients.
• Event rates were significantly higher in deferred ACS patients overall than in deferred patients with stable coronary disease: 5.9% versus 3.6%. But the deferral tool made a difference: When iFR was utilized, the 1-year event rate was 5.4% in deferred ACS patients, not significantly different from the 3.8% rate in deferred patients with stable coronary disease. In contrast, the event rate in ACS patients with FFR-based deferral was 6.4%, significantly higher than the 3.4% rate in FFR-deferred patients with stable coronary disease.
Dr. Escaned noted that this finding is consistent with the cautionary results of several recent studies, including one, albeit tenfold smaller, in which ACS patients in whom revascularization was deferred based on FFR had a 25% rate of major adverse cardiovascular events at 3.4 years, compared with a 12% rate in patients with stable coronary disease (J Am Coll Cardiol. 2016 Sep 13;68[11]:1181-91).
Discussant Peter Jüni, MD, professor of medicine at the University of Toronto, said “the main results of your study show in a completely waterproof fashion that there is no signal of harm with the experimental strategy” of deferred revascularization based on physiologic measurements, at least in patients with stable ischemic coronary disease.
The results, however, also raise the question of whether physiology-based revascularization decision-making in ACS patients is the best strategy.
“Considering that the event rate in the deferred ACS group was nearly twice as high compared with stable patients, my question to you is: Should we ignore any functional testing in ACS patients and just say, ‘Let’s move forward with revascularization because this clinical presentation is a very good clinical characteristic for risk stratification?’ ”
Dr. Escaned rejected that option. He noted that both the European and U.S. guidelines now state that it’s inappropriate to base a revascularization decision solely on a coronary vessel’s angiographic appearance, because that has been shown to result in unnecessary treatment, which causes harm. Adoption of pressure guidewires to assist in revascularization decision making, whether by FFR or iFR, is still limited in interventional cardiology. The priority in the field now should be to encourage more widespread use of this technology, regardless of which method is selected, he argued.
“The biggest room in the world is the room for improvement,” the cardiologist mused.
“I think one of the real problems that’s impeding adoption of physiologic testing is that many physicians are still afraid of leaving a stenosis without treatment,” he continued. “It’s strange: If you perform angioplasty and it wasn’t indicated and there is a complication, physicians seem to have some type of peace of mind that they did their best and they were trying to help the patient. That’s why it’s so important to establish that deferring revascularization – not treating when it is not needed – is safe.”
The DEFINE FLAIR and iFR SWEDEHEART studies were funded by unrestricted grants from Philips Volcano. Dr. Escaned reported serving as a consultant to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, and Philips Healthcare.
Paris – One-year outcomes were significantly worse in patients with acute coronary syndrome whose revascularization was deferred based upon the results of fractional flow reserve than with instantaneous wave-free ratio, in the largest-ever study of patients whose revascularization decision was guided by physiologic measurements obtained via a pressure guidewire.
“The hypothesis that some authors have put forth – that in an ACS the hyperemic response of the myocardium is blunted by the ACS, and that this will affect the FFR hyperemic index – is now strengthened,” Javier Escaned, MD, said in presenting the study results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The study was a pooled, patient-level meta-analysis of the 4,529 participants with angiographically determined intermediate-risk stenoses in the previously reported randomized DEFINE FLAIR (N Engl J Med. 2017 May 11;376[19]:1824-34) and iFR SWEDEHEART (N Engl J Med. 2017 May 11;376[19]:1813-23) studies. The primary endpoint was the composite of death, nonfatal MI, or unplanned coronary revascularization within 12 months. And while the analysis brought unwelcome news for proponents of FFR with regard to the subset of patients with ACS, such patients comprised only 17% of the total study population.
“I think that overall these results are very reassuring. The big finding is that we have dramatically improved the safety of deferral of revascularization using pressure guidewires. If you look at the MACE [major adverse cardiovascular event] rate in the deferred ACS group, it was about 6%, which is much less than the event rate at 1 year with deferral in patients with stable coronary disease in the pivotal DEFER trial [Circulation. 2001 Jun 19;103(24):2928-34], which was our former standard,” observed Dr. Escaned, an interventional cardiologist at San Carlos Hospital in Madrid and a DEFER coinvestigator.
He attributed these greatly improved outcomes of physiologically guided revascularization during the past 15 years to vastly improved stent technology and more effective optimal medical management.
Among the key findings of the combined analysis of DEFINE FLAIR and iFR SWEDEHEART:
• More patients were deferred from PCI when iFR was used for decision-making: 50%, compared with 45% in the FFR arm. Yet 1-year outcomes were as good in the deferred iFR group as in the FFR group overall, and better than with FFR in the deferred ACS patients.
• Event rates were significantly higher in deferred ACS patients overall than in deferred patients with stable coronary disease: 5.9% versus 3.6%. But the deferral tool made a difference: When iFR was utilized, the 1-year event rate was 5.4% in deferred ACS patients, not significantly different from the 3.8% rate in deferred patients with stable coronary disease. In contrast, the event rate in ACS patients with FFR-based deferral was 6.4%, significantly higher than the 3.4% rate in FFR-deferred patients with stable coronary disease.
Dr. Escaned noted that this finding is consistent with the cautionary results of several recent studies, including one, albeit tenfold smaller, in which ACS patients in whom revascularization was deferred based on FFR had a 25% rate of major adverse cardiovascular events at 3.4 years, compared with a 12% rate in patients with stable coronary disease (J Am Coll Cardiol. 2016 Sep 13;68[11]:1181-91).
Discussant Peter Jüni, MD, professor of medicine at the University of Toronto, said “the main results of your study show in a completely waterproof fashion that there is no signal of harm with the experimental strategy” of deferred revascularization based on physiologic measurements, at least in patients with stable ischemic coronary disease.
The results, however, also raise the question of whether physiology-based revascularization decision-making in ACS patients is the best strategy.
“Considering that the event rate in the deferred ACS group was nearly twice as high compared with stable patients, my question to you is: Should we ignore any functional testing in ACS patients and just say, ‘Let’s move forward with revascularization because this clinical presentation is a very good clinical characteristic for risk stratification?’ ”
Dr. Escaned rejected that option. He noted that both the European and U.S. guidelines now state that it’s inappropriate to base a revascularization decision solely on a coronary vessel’s angiographic appearance, because that has been shown to result in unnecessary treatment, which causes harm. Adoption of pressure guidewires to assist in revascularization decision making, whether by FFR or iFR, is still limited in interventional cardiology. The priority in the field now should be to encourage more widespread use of this technology, regardless of which method is selected, he argued.
“The biggest room in the world is the room for improvement,” the cardiologist mused.
“I think one of the real problems that’s impeding adoption of physiologic testing is that many physicians are still afraid of leaving a stenosis without treatment,” he continued. “It’s strange: If you perform angioplasty and it wasn’t indicated and there is a complication, physicians seem to have some type of peace of mind that they did their best and they were trying to help the patient. That’s why it’s so important to establish that deferring revascularization – not treating when it is not needed – is safe.”
The DEFINE FLAIR and iFR SWEDEHEART studies were funded by unrestricted grants from Philips Volcano. Dr. Escaned reported serving as a consultant to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, and Philips Healthcare.
Paris – One-year outcomes were significantly worse in patients with acute coronary syndrome whose revascularization was deferred based upon the results of fractional flow reserve than with instantaneous wave-free ratio, in the largest-ever study of patients whose revascularization decision was guided by physiologic measurements obtained via a pressure guidewire.
“The hypothesis that some authors have put forth – that in an ACS the hyperemic response of the myocardium is blunted by the ACS, and that this will affect the FFR hyperemic index – is now strengthened,” Javier Escaned, MD, said in presenting the study results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The study was a pooled, patient-level meta-analysis of the 4,529 participants with angiographically determined intermediate-risk stenoses in the previously reported randomized DEFINE FLAIR (N Engl J Med. 2017 May 11;376[19]:1824-34) and iFR SWEDEHEART (N Engl J Med. 2017 May 11;376[19]:1813-23) studies. The primary endpoint was the composite of death, nonfatal MI, or unplanned coronary revascularization within 12 months. And while the analysis brought unwelcome news for proponents of FFR with regard to the subset of patients with ACS, such patients comprised only 17% of the total study population.
“I think that overall these results are very reassuring. The big finding is that we have dramatically improved the safety of deferral of revascularization using pressure guidewires. If you look at the MACE [major adverse cardiovascular event] rate in the deferred ACS group, it was about 6%, which is much less than the event rate at 1 year with deferral in patients with stable coronary disease in the pivotal DEFER trial [Circulation. 2001 Jun 19;103(24):2928-34], which was our former standard,” observed Dr. Escaned, an interventional cardiologist at San Carlos Hospital in Madrid and a DEFER coinvestigator.
He attributed these greatly improved outcomes of physiologically guided revascularization during the past 15 years to vastly improved stent technology and more effective optimal medical management.
Among the key findings of the combined analysis of DEFINE FLAIR and iFR SWEDEHEART:
• More patients were deferred from PCI when iFR was used for decision-making: 50%, compared with 45% in the FFR arm. Yet 1-year outcomes were as good in the deferred iFR group as in the FFR group overall, and better than with FFR in the deferred ACS patients.
• Event rates were significantly higher in deferred ACS patients overall than in deferred patients with stable coronary disease: 5.9% versus 3.6%. But the deferral tool made a difference: When iFR was utilized, the 1-year event rate was 5.4% in deferred ACS patients, not significantly different from the 3.8% rate in deferred patients with stable coronary disease. In contrast, the event rate in ACS patients with FFR-based deferral was 6.4%, significantly higher than the 3.4% rate in FFR-deferred patients with stable coronary disease.
Dr. Escaned noted that this finding is consistent with the cautionary results of several recent studies, including one, albeit tenfold smaller, in which ACS patients in whom revascularization was deferred based on FFR had a 25% rate of major adverse cardiovascular events at 3.4 years, compared with a 12% rate in patients with stable coronary disease (J Am Coll Cardiol. 2016 Sep 13;68[11]:1181-91).
Discussant Peter Jüni, MD, professor of medicine at the University of Toronto, said “the main results of your study show in a completely waterproof fashion that there is no signal of harm with the experimental strategy” of deferred revascularization based on physiologic measurements, at least in patients with stable ischemic coronary disease.
The results, however, also raise the question of whether physiology-based revascularization decision-making in ACS patients is the best strategy.
“Considering that the event rate in the deferred ACS group was nearly twice as high compared with stable patients, my question to you is: Should we ignore any functional testing in ACS patients and just say, ‘Let’s move forward with revascularization because this clinical presentation is a very good clinical characteristic for risk stratification?’ ”
Dr. Escaned rejected that option. He noted that both the European and U.S. guidelines now state that it’s inappropriate to base a revascularization decision solely on a coronary vessel’s angiographic appearance, because that has been shown to result in unnecessary treatment, which causes harm. Adoption of pressure guidewires to assist in revascularization decision making, whether by FFR or iFR, is still limited in interventional cardiology. The priority in the field now should be to encourage more widespread use of this technology, regardless of which method is selected, he argued.
“The biggest room in the world is the room for improvement,” the cardiologist mused.
“I think one of the real problems that’s impeding adoption of physiologic testing is that many physicians are still afraid of leaving a stenosis without treatment,” he continued. “It’s strange: If you perform angioplasty and it wasn’t indicated and there is a complication, physicians seem to have some type of peace of mind that they did their best and they were trying to help the patient. That’s why it’s so important to establish that deferring revascularization – not treating when it is not needed – is safe.”
The DEFINE FLAIR and iFR SWEDEHEART studies were funded by unrestricted grants from Philips Volcano. Dr. Escaned reported serving as a consultant to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, and Philips Healthcare.
AT EUROPCR
Key clinical point:
Major finding: In patients with acute coronary syndrome, the 1-year adverse event rate in patients with FFR-based deferral was 6.4%, significantly higher than the 3.4% rate in patients with FFR-based deferral with stable coronary disease.
Data source: A pooled patient-level meta-analysis of the 4,529 participants with angiographically intermediate-risk stenoses in two previously reported randomized trials of physiologic assessment of lesions by fractional flow reserve or instantaneous wave-free ratio.
Disclosures: The DEFINE FLAIR and iFR SWEDEHEART studies were funded by unrestricted grants from Philips Volcano. The presenter reported serving as a consultant to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, and Philips Healthcare.
Aspirin triples major bleeding risk after age 75 years
Older adults who take aspirin daily are at greater risk for serious bleeding than previously thought, based on data from roughly 3,000 patients.
“The risk of upper gastrointestinal bleeding on antiplatelet treatment increases with age, but it is uncertain whether older age alone is a sufficient indicator of high risk to justify routine coprescription of PPIs [proton pump inhibitors],” wrote Linxin Li, DPhil, of the University of Oxford (England) and her colleagues.
To assess the rate of bleeding among older adults on long-term aspirin therapy, Dr. Li and her colleagues reviewed data from the Oxford Vascular Study, a prospective population-based study of 3,166 patients. Of those, 1,584 were younger than 75 years, with an average age of 61 years, and 1,582 were at least 75 years old, with average age of 83 years. Patients were followed at 30 days, 6 months, and 1, 5, and 10 years to determine bleeding, recurrent ischemic events, and disability (Lancet. 2017. doi: 10.1016/S0140-6736[17]30770-5).
In addition, more than twice the major upper GI bleeds were disabling or fatal in adults aged 75 years and older than in the younger patients (62% vs. 25%).
Only a third of the patients in the study were taking proton pump inhibitors (PPIs), partly because current clinical guidelines don’t specifically recommend their use and partly in the absence of an accepted definition of which patients are at high risk for upper GI bleeding, the researchers said. They estimated that the number needed to treat with PPIs to prevent a major GI bleed after 5 years decreased with age: “80 for patients younger than 65 years, 75 for patients aged 65-74 years, 23 for patients aged 75-84 years, and 21 for patients aged 85 years or older.” In addition, the number needed to treat with PPIs to prevent a disabling or fatal upper GI bleed after 5 years was 338 for patients younger than 65 years but dropped to 25 for patients aged 85 years and older.
The findings were limited by the observational nature of the study and inability to show that increased risk of bleeding was caused by aspirin alone, the researchers said. However, based on the data, “age 75 years would be an appropriate threshold to start a PPI both in patients newly initiated on antiplatelet drugs and in patients on established treatment,” they wrote.
The study data were taken from the Oxford Vascular Study, which was funded by the National Institute of Health Research and several other research institutions. Corresponding author Peter Rothwell, MD, disclosed financial relationships with Bayer.
In patients with stroke with a cardiac source of embolism who qualify for oral anticoagulation, we obsess about the association between benefit and bleeding risk. Specific risk scores were developed to assess the bleeding risk for patients with atrial fibrillation who qualified for anticoagulation. However, similar risk scores are not applied for patients who undergo long-term prevention with antiplatelet therapy.
On the basis of this study’s results, the benefit-risk association in long-term antiplatelet therapy should be evaluated every 3-5 years in patients older than 75 years, and PPIs should be used in patients on antiplatelet therapy who are at least 75 years old or in patients with a history of gastrointestinal bleeds.
Hans-Christoph Diener, MD, of the department of neurology at the University Duisburg-Essen in Essen, Germany, made these remarks in an accompanying editorial (Lancet. 2017 Jun 13. doi: 10.1016/S0140-6736[17]31507-6). He disclosed relationships with multiple companies, including AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Merck, and Novartis.
In patients with stroke with a cardiac source of embolism who qualify for oral anticoagulation, we obsess about the association between benefit and bleeding risk. Specific risk scores were developed to assess the bleeding risk for patients with atrial fibrillation who qualified for anticoagulation. However, similar risk scores are not applied for patients who undergo long-term prevention with antiplatelet therapy.
On the basis of this study’s results, the benefit-risk association in long-term antiplatelet therapy should be evaluated every 3-5 years in patients older than 75 years, and PPIs should be used in patients on antiplatelet therapy who are at least 75 years old or in patients with a history of gastrointestinal bleeds.
Hans-Christoph Diener, MD, of the department of neurology at the University Duisburg-Essen in Essen, Germany, made these remarks in an accompanying editorial (Lancet. 2017 Jun 13. doi: 10.1016/S0140-6736[17]31507-6). He disclosed relationships with multiple companies, including AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Merck, and Novartis.
In patients with stroke with a cardiac source of embolism who qualify for oral anticoagulation, we obsess about the association between benefit and bleeding risk. Specific risk scores were developed to assess the bleeding risk for patients with atrial fibrillation who qualified for anticoagulation. However, similar risk scores are not applied for patients who undergo long-term prevention with antiplatelet therapy.
On the basis of this study’s results, the benefit-risk association in long-term antiplatelet therapy should be evaluated every 3-5 years in patients older than 75 years, and PPIs should be used in patients on antiplatelet therapy who are at least 75 years old or in patients with a history of gastrointestinal bleeds.
Hans-Christoph Diener, MD, of the department of neurology at the University Duisburg-Essen in Essen, Germany, made these remarks in an accompanying editorial (Lancet. 2017 Jun 13. doi: 10.1016/S0140-6736[17]31507-6). He disclosed relationships with multiple companies, including AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Merck, and Novartis.
Older adults who take aspirin daily are at greater risk for serious bleeding than previously thought, based on data from roughly 3,000 patients.
“The risk of upper gastrointestinal bleeding on antiplatelet treatment increases with age, but it is uncertain whether older age alone is a sufficient indicator of high risk to justify routine coprescription of PPIs [proton pump inhibitors],” wrote Linxin Li, DPhil, of the University of Oxford (England) and her colleagues.
To assess the rate of bleeding among older adults on long-term aspirin therapy, Dr. Li and her colleagues reviewed data from the Oxford Vascular Study, a prospective population-based study of 3,166 patients. Of those, 1,584 were younger than 75 years, with an average age of 61 years, and 1,582 were at least 75 years old, with average age of 83 years. Patients were followed at 30 days, 6 months, and 1, 5, and 10 years to determine bleeding, recurrent ischemic events, and disability (Lancet. 2017. doi: 10.1016/S0140-6736[17]30770-5).
In addition, more than twice the major upper GI bleeds were disabling or fatal in adults aged 75 years and older than in the younger patients (62% vs. 25%).
Only a third of the patients in the study were taking proton pump inhibitors (PPIs), partly because current clinical guidelines don’t specifically recommend their use and partly in the absence of an accepted definition of which patients are at high risk for upper GI bleeding, the researchers said. They estimated that the number needed to treat with PPIs to prevent a major GI bleed after 5 years decreased with age: “80 for patients younger than 65 years, 75 for patients aged 65-74 years, 23 for patients aged 75-84 years, and 21 for patients aged 85 years or older.” In addition, the number needed to treat with PPIs to prevent a disabling or fatal upper GI bleed after 5 years was 338 for patients younger than 65 years but dropped to 25 for patients aged 85 years and older.
The findings were limited by the observational nature of the study and inability to show that increased risk of bleeding was caused by aspirin alone, the researchers said. However, based on the data, “age 75 years would be an appropriate threshold to start a PPI both in patients newly initiated on antiplatelet drugs and in patients on established treatment,” they wrote.
The study data were taken from the Oxford Vascular Study, which was funded by the National Institute of Health Research and several other research institutions. Corresponding author Peter Rothwell, MD, disclosed financial relationships with Bayer.
Older adults who take aspirin daily are at greater risk for serious bleeding than previously thought, based on data from roughly 3,000 patients.
“The risk of upper gastrointestinal bleeding on antiplatelet treatment increases with age, but it is uncertain whether older age alone is a sufficient indicator of high risk to justify routine coprescription of PPIs [proton pump inhibitors],” wrote Linxin Li, DPhil, of the University of Oxford (England) and her colleagues.
To assess the rate of bleeding among older adults on long-term aspirin therapy, Dr. Li and her colleagues reviewed data from the Oxford Vascular Study, a prospective population-based study of 3,166 patients. Of those, 1,584 were younger than 75 years, with an average age of 61 years, and 1,582 were at least 75 years old, with average age of 83 years. Patients were followed at 30 days, 6 months, and 1, 5, and 10 years to determine bleeding, recurrent ischemic events, and disability (Lancet. 2017. doi: 10.1016/S0140-6736[17]30770-5).
In addition, more than twice the major upper GI bleeds were disabling or fatal in adults aged 75 years and older than in the younger patients (62% vs. 25%).
Only a third of the patients in the study were taking proton pump inhibitors (PPIs), partly because current clinical guidelines don’t specifically recommend their use and partly in the absence of an accepted definition of which patients are at high risk for upper GI bleeding, the researchers said. They estimated that the number needed to treat with PPIs to prevent a major GI bleed after 5 years decreased with age: “80 for patients younger than 65 years, 75 for patients aged 65-74 years, 23 for patients aged 75-84 years, and 21 for patients aged 85 years or older.” In addition, the number needed to treat with PPIs to prevent a disabling or fatal upper GI bleed after 5 years was 338 for patients younger than 65 years but dropped to 25 for patients aged 85 years and older.
The findings were limited by the observational nature of the study and inability to show that increased risk of bleeding was caused by aspirin alone, the researchers said. However, based on the data, “age 75 years would be an appropriate threshold to start a PPI both in patients newly initiated on antiplatelet drugs and in patients on established treatment,” they wrote.
The study data were taken from the Oxford Vascular Study, which was funded by the National Institute of Health Research and several other research institutions. Corresponding author Peter Rothwell, MD, disclosed financial relationships with Bayer.
FROM THE LANCET
Key clinical point:
Major finding: The annual rate of life-threatening or fatal bleeding episodes was less than 0.5% for patients younger than 65 years but rose to 1.5% in those aged 75-84 years and 2.5% in those aged 85 years and older.
Data source: A prospective, population-based cohort study of 3,166 adults who had one transient ischemic attack, ischemic stroke, or MI and who were treated with antiplatelet drugs.
Disclosures: The study data were taken from the Oxford Vascular Study, which was funded by the Wellcome Trust, Wolfson Foundation, British Heart Foundation, Dunhill Medical Trust, the National Institute of Health Research (NIHR), and the NIHR Oxford Biomedical Research Centre. Corresponding author Peter Rothwell, MD, disclosed financial relationships with Bayer.
Low-dose aspirin bests dual-antiplatelet therapy in TAVR
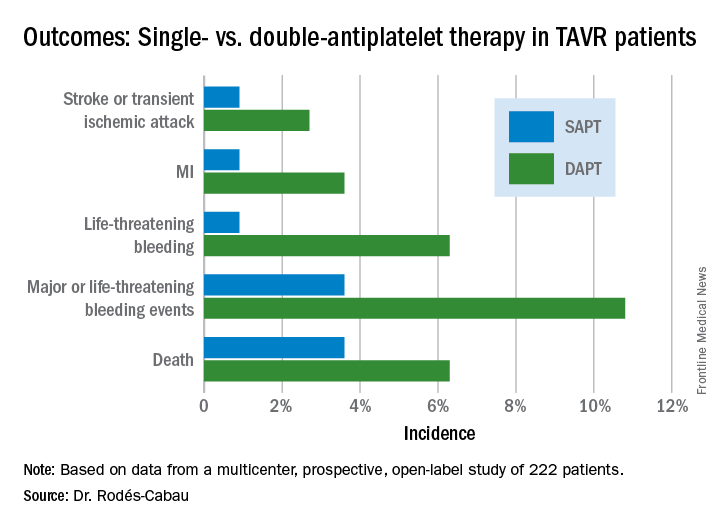
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
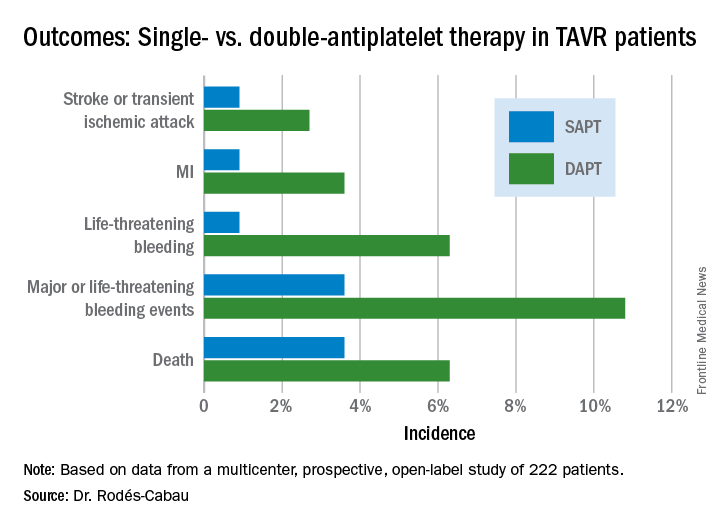
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
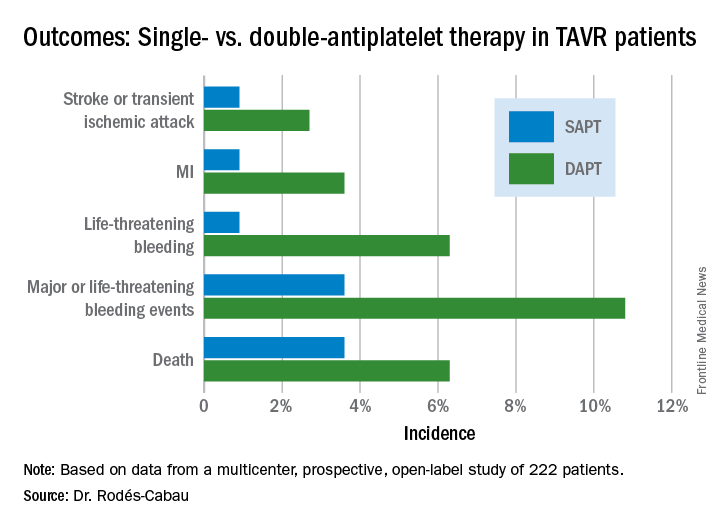
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
AT EUROPCR
Key clinical point:
Major finding: The 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack occurred in 15.3% of TAVR patients randomized to DAPT with low-dose aspirin plus clopidogrel, compared with 7.2% on aspirin only.
Data source: A randomized, multicenter, international, prospective open-label trial in 222 TAVR patients.
Disclosures: The presenter reported receiving research grants from Edwards Lifesciences and the Quebec Heart and Lung Institute, which supported the ARTE trial.
Transradial PCI in acute coronary syndrome causes less kidney damage
PARIS – Transradial-access percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) results in a significantly lower risk of acute kidney injury (AKI), compared with the transfemoral approach, according to a new analysis from the large randomized MATRIX trial.
The results of this prespecified secondary subgroup analysis of MATRIX suggest it’s time to update the classic “five golden rules” for reduction of contrast medium–induced AKI by adding a sixth. “Use a transradial approach,” Bernardo Cortese, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He reported on 8,210 participants in the MATRIX trial (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) who were randomized to transradial- or transfemoral-access PCI for non–ST-elevation MI or ST-elevation MI.
The primary results of the 78-site, four-country European study, previously published, showed that transradial PCI reduced the composite risk of death, MI, stroke, or major bleeding by 17%, compared with transfemoral PCI, a benefit mainly driven by a marked reduction in clinically important bleeding (Lancet. 2015 Jun 20;385[9986]:2465-76).
Left unanswered by the primary analysis was the question of whether transradial PCI in ACS patients also reduced AKI risk, as had previously been suggested by a meta-analysis of observational studies (Int J Cardiol. 2015 Jan 20;179:309-11). In designing the MATRIX trial, Dr. Cortese and the other investigators decided to address that issue separately in a prespecified secondary analysis known as AKI-MATRIX. For this purpose, AKI was defined as either a post-PCI in-hospital increase in serum creatinine level of more than 25%, compared with the preangiography baseline, or an absolute increase in serum creatinine of greater than 0.5 mg/dL.
AKI occurred in 15.4% of ACS patients who underwent PCI with transradial access and 17.3% of those randomized to transfemoral access, for a significant 13% relative risk reduction. This was accomplished without any increase in the volume of contrast media required. The average was 200 mL in both study groups.
The reduction in AKI achieved with transradial-access PCI was seen in all patient subgroups, including those at increased AKI risk because of an estimated glomerular filtration rate below 60 mL/min, age 75 or older, Killup class III or IV, or a Mehran score greater than 10.
Dr. Cortese proposed several possible mechanisms for the observed reduction in AKI seen with transradial-access PCI. The major factor in his view is that the transradial approach entails less bleeding, as earlier demonstrated in the primary analysis – and bleeding has been associated with impaired renal perfusion in several prior studies. Also, it’s plausible that the passage of the catheter across the renal arteries during the transfemoral approach dislodges atherosclerotic debris, which then travels down the renal vessels.
The five golden rules for preventing contrast media–induced AKI, he noted, are
1. Discontinue nephrotoxic drugs before the procedure.
2. Identify high-risk patients.
3. Hydrate them.
4. Choose an ideal contrast medium.
5. Adapt the dose of contrast medium to the patient’s specific situation.
Discussant Jacek Legutko, MD, PhD, of Jagiellonian University in Krakow, Poland, said the primary results of the MATRIX trial published in 2015 have had a major impact on Polish interventional cardiology, where transradial PCI is now used in 80% of PCIs. The AKI study results will reinforce this trend, he added.
“You have shown something opposite to what we’ve thought in the past, that maybe, with a radial approach, we would use more contrast medium, which is a risk factor for AKI. In your study – at least in ACS with very experienced transradial operators – there was no increase in contrast volume, and the risk of AKI decreased,” Dr. Legutko said.
Asked about the possibility that transradial PCI might be associated with an increased risk of embolization to the brain, much as the transfemoral approach might cause embolization to the kidneys, Dr. Cortese said there was no significant difference between the two AKI-MATRIX study arms in rates of transient ischemic attack or stroke.
“I did my first transradial PCI in 2003, and I haven’t seen any increase in these events or later dementia,” he added.
The prespecified secondary analysis of the MATRIX trial was conducted without commercial support. The presenter reported serving as a consultant to Abbott, AstraZeneca, Daiichi Sankyo, Eli Lilly, and Stentys.
Simultaneous with his presentation in Paris, the AKI-MATRIX study was published online at www.sciencedirect.com/science/article/pii/S0735109717368973.
PARIS – Transradial-access percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) results in a significantly lower risk of acute kidney injury (AKI), compared with the transfemoral approach, according to a new analysis from the large randomized MATRIX trial.
The results of this prespecified secondary subgroup analysis of MATRIX suggest it’s time to update the classic “five golden rules” for reduction of contrast medium–induced AKI by adding a sixth. “Use a transradial approach,” Bernardo Cortese, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He reported on 8,210 participants in the MATRIX trial (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) who were randomized to transradial- or transfemoral-access PCI for non–ST-elevation MI or ST-elevation MI.
The primary results of the 78-site, four-country European study, previously published, showed that transradial PCI reduced the composite risk of death, MI, stroke, or major bleeding by 17%, compared with transfemoral PCI, a benefit mainly driven by a marked reduction in clinically important bleeding (Lancet. 2015 Jun 20;385[9986]:2465-76).
Left unanswered by the primary analysis was the question of whether transradial PCI in ACS patients also reduced AKI risk, as had previously been suggested by a meta-analysis of observational studies (Int J Cardiol. 2015 Jan 20;179:309-11). In designing the MATRIX trial, Dr. Cortese and the other investigators decided to address that issue separately in a prespecified secondary analysis known as AKI-MATRIX. For this purpose, AKI was defined as either a post-PCI in-hospital increase in serum creatinine level of more than 25%, compared with the preangiography baseline, or an absolute increase in serum creatinine of greater than 0.5 mg/dL.
AKI occurred in 15.4% of ACS patients who underwent PCI with transradial access and 17.3% of those randomized to transfemoral access, for a significant 13% relative risk reduction. This was accomplished without any increase in the volume of contrast media required. The average was 200 mL in both study groups.
The reduction in AKI achieved with transradial-access PCI was seen in all patient subgroups, including those at increased AKI risk because of an estimated glomerular filtration rate below 60 mL/min, age 75 or older, Killup class III or IV, or a Mehran score greater than 10.
Dr. Cortese proposed several possible mechanisms for the observed reduction in AKI seen with transradial-access PCI. The major factor in his view is that the transradial approach entails less bleeding, as earlier demonstrated in the primary analysis – and bleeding has been associated with impaired renal perfusion in several prior studies. Also, it’s plausible that the passage of the catheter across the renal arteries during the transfemoral approach dislodges atherosclerotic debris, which then travels down the renal vessels.
The five golden rules for preventing contrast media–induced AKI, he noted, are
1. Discontinue nephrotoxic drugs before the procedure.
2. Identify high-risk patients.
3. Hydrate them.
4. Choose an ideal contrast medium.
5. Adapt the dose of contrast medium to the patient’s specific situation.
Discussant Jacek Legutko, MD, PhD, of Jagiellonian University in Krakow, Poland, said the primary results of the MATRIX trial published in 2015 have had a major impact on Polish interventional cardiology, where transradial PCI is now used in 80% of PCIs. The AKI study results will reinforce this trend, he added.
“You have shown something opposite to what we’ve thought in the past, that maybe, with a radial approach, we would use more contrast medium, which is a risk factor for AKI. In your study – at least in ACS with very experienced transradial operators – there was no increase in contrast volume, and the risk of AKI decreased,” Dr. Legutko said.
Asked about the possibility that transradial PCI might be associated with an increased risk of embolization to the brain, much as the transfemoral approach might cause embolization to the kidneys, Dr. Cortese said there was no significant difference between the two AKI-MATRIX study arms in rates of transient ischemic attack or stroke.
“I did my first transradial PCI in 2003, and I haven’t seen any increase in these events or later dementia,” he added.
The prespecified secondary analysis of the MATRIX trial was conducted without commercial support. The presenter reported serving as a consultant to Abbott, AstraZeneca, Daiichi Sankyo, Eli Lilly, and Stentys.
Simultaneous with his presentation in Paris, the AKI-MATRIX study was published online at www.sciencedirect.com/science/article/pii/S0735109717368973.
PARIS – Transradial-access percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) results in a significantly lower risk of acute kidney injury (AKI), compared with the transfemoral approach, according to a new analysis from the large randomized MATRIX trial.
The results of this prespecified secondary subgroup analysis of MATRIX suggest it’s time to update the classic “five golden rules” for reduction of contrast medium–induced AKI by adding a sixth. “Use a transradial approach,” Bernardo Cortese, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He reported on 8,210 participants in the MATRIX trial (Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) who were randomized to transradial- or transfemoral-access PCI for non–ST-elevation MI or ST-elevation MI.
The primary results of the 78-site, four-country European study, previously published, showed that transradial PCI reduced the composite risk of death, MI, stroke, or major bleeding by 17%, compared with transfemoral PCI, a benefit mainly driven by a marked reduction in clinically important bleeding (Lancet. 2015 Jun 20;385[9986]:2465-76).
Left unanswered by the primary analysis was the question of whether transradial PCI in ACS patients also reduced AKI risk, as had previously been suggested by a meta-analysis of observational studies (Int J Cardiol. 2015 Jan 20;179:309-11). In designing the MATRIX trial, Dr. Cortese and the other investigators decided to address that issue separately in a prespecified secondary analysis known as AKI-MATRIX. For this purpose, AKI was defined as either a post-PCI in-hospital increase in serum creatinine level of more than 25%, compared with the preangiography baseline, or an absolute increase in serum creatinine of greater than 0.5 mg/dL.
AKI occurred in 15.4% of ACS patients who underwent PCI with transradial access and 17.3% of those randomized to transfemoral access, for a significant 13% relative risk reduction. This was accomplished without any increase in the volume of contrast media required. The average was 200 mL in both study groups.
The reduction in AKI achieved with transradial-access PCI was seen in all patient subgroups, including those at increased AKI risk because of an estimated glomerular filtration rate below 60 mL/min, age 75 or older, Killup class III or IV, or a Mehran score greater than 10.
Dr. Cortese proposed several possible mechanisms for the observed reduction in AKI seen with transradial-access PCI. The major factor in his view is that the transradial approach entails less bleeding, as earlier demonstrated in the primary analysis – and bleeding has been associated with impaired renal perfusion in several prior studies. Also, it’s plausible that the passage of the catheter across the renal arteries during the transfemoral approach dislodges atherosclerotic debris, which then travels down the renal vessels.
The five golden rules for preventing contrast media–induced AKI, he noted, are
1. Discontinue nephrotoxic drugs before the procedure.
2. Identify high-risk patients.
3. Hydrate them.
4. Choose an ideal contrast medium.
5. Adapt the dose of contrast medium to the patient’s specific situation.
Discussant Jacek Legutko, MD, PhD, of Jagiellonian University in Krakow, Poland, said the primary results of the MATRIX trial published in 2015 have had a major impact on Polish interventional cardiology, where transradial PCI is now used in 80% of PCIs. The AKI study results will reinforce this trend, he added.
“You have shown something opposite to what we’ve thought in the past, that maybe, with a radial approach, we would use more contrast medium, which is a risk factor for AKI. In your study – at least in ACS with very experienced transradial operators – there was no increase in contrast volume, and the risk of AKI decreased,” Dr. Legutko said.
Asked about the possibility that transradial PCI might be associated with an increased risk of embolization to the brain, much as the transfemoral approach might cause embolization to the kidneys, Dr. Cortese said there was no significant difference between the two AKI-MATRIX study arms in rates of transient ischemic attack or stroke.
“I did my first transradial PCI in 2003, and I haven’t seen any increase in these events or later dementia,” he added.
The prespecified secondary analysis of the MATRIX trial was conducted without commercial support. The presenter reported serving as a consultant to Abbott, AstraZeneca, Daiichi Sankyo, Eli Lilly, and Stentys.
Simultaneous with his presentation in Paris, the AKI-MATRIX study was published online at www.sciencedirect.com/science/article/pii/S0735109717368973.
AT EUROPCR
Key clinical point:
Major finding: Transradial-access PCI for ACS resulted in a 13% lower risk of acute kidney injury than the transfemoral approach.
Data source: A four-country European randomized trial of transradial- vs. transfemoral-access PCI in more than 8,200 patients with ACS.
Disclosures: This prespecified secondary analysis of the MATRIX trial was conducted without commercial support. The presenter reported serving as a consultant to Abbott, AstraZeneca, Daiichi Sankyo, Eli Lilly, and Stentys.
Infections up the risk for pregnancy-associated stroke in preeclampsia
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
FROM STROKE
Key clinical point:
Major finding: Independent risk factors for pregnancy-associated stroke were severe preeclampsia or eclampsia (OR, 7.2), infections (OR, 3.0), prothrombotic states (OR, 3.5), coagulopathies (OR, 3.1), or chronic hypertension (OR, 3.2).
Data source: A matched, case-control study of 788 women from a New York inpatient database who were hospitalized for preeclampsia.
Disclosures: The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
Novel Lotus valve outperforms CoreValve in REPRISE III
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
[email protected]
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
[email protected]
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
[email protected]
AT EUROPCR
Key clinical point:
Major finding: The rate of the 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak was 17% in patients randomized to the investigational Lotus transcatheter aortic valve replacement system, compared with 29% in recipients of the CoreValve.
Data source: REPRISE III, a prospective, multicenter, international clinical trial randomized 912 patients with severe aortic stenosis who were at high surgical risk to TAVR with the investigational Lotus valve or a commercially available CoreValve.
Disclosures: REPRISE III was sponsored by Boston Scientific. The study presenter reported serving as a consultant to that company as well as for Abbott and Edwards Lifesciences. He has also received institutional research grants from those companies.
Consider switch to clopidogrel for DAPT early post ACS
PARIS – A strategy of switching from prasugrel or ticagrelor to clopidogrel 1 month after percutaneous coronary intervention for acute coronary syndrome is superior to the guideline-recommended full 12 months of dual-antiplatelet therapy with either of the newer P2Y12 inhibitors, according to Thomas Cuisset, MD.
In the randomized TOPIC (Timing of Platelet Inhibition After Acute Coronary Syndrome) trial, this switch strategy resulted in a marked reduction in bleeding without an increased risk of ischemic events, compared with a full 12 months of standard dual-antiplatelet therapy (DAPT) using prasugrel (Effient) or ticagrelor (Brilinta).
He added that the cost savings of this switch strategy would be enormous, since generic clopidogrel is vastly less expensive than prasugrel or ticagrelor.
Twelve months of DAPT with aspirin plus either prasugrel or ticagrelor is the guideline-recommended DAPT regimen following PCI for ACS on the strength of the TRITON and PLATO trials, respectively, which showed that those agents were more effective than clopidogrel for the prevention of thrombotic events. But Dr. Cuisset and his coinvestigators noted that the risk of ischemic events was highest in the first month or so following ACS, while the risk of DAPT-related serious bleeding increased after the first month and continued for the duration.
“We need to use the new drugs, and we need to go for 1 year with DAPT. But does that mean we need to go for 1 year with the new drugs?” he asked.
This question was the impetus for TOPIC, an open-label, single-center randomized trial that included 646 ACS patients who were free of major adverse cardiovascular events during their first month on DAPT with prasugrel or ticagrelor. At that point they were randomized to remain on their standard regimen or switch to aspirin at 75 mg/day plus clopidogrel at 75 mg/day for months 2-12. The switch strategy is similar to the way pulmonary embolism is managed: an early phase of high-intensity therapy followed by a backing off to a less intensive regimen, said Dr. Cuisset, a cardiologist at Aix-Marseille University, Provence, France.
The primary endpoint in TOPIC was the cumulative 1-year rate of a composite of all-cause mortality, stroke, urgent revascularization, or clinically significant bleeding as reflected in a Bleeding Academic Research Consortium (BARC) grade 2 or greater bleeding. The primary endpoint occurred in 13.4% of the switch group, a 52% relative risk reduction, compared with the 26.3% cumulative incidence with standard DAPT.
This difference wasn’t due to any between-group disparity in ischemic events, but rather to a 70% reduction in the risk of BARC grade 2 or greater bleeding in the switch group: 4.0% vs. 14.9%.
Some physicians have already been switching to clopidogrel for DAPT after ACS, either because of safety or cost concerns. Now their practice is evidence based, Dr. Cuisset noted.
Asked why TOPIC didn’t use the more stringent bleeding endpoint of BARC grade 3-5 bleeding, the cardiologist replied that it would have required a larger trial to show a significant difference. Besides, he added, BARC grade 2 bleeding is clinically important because it has a negative impact on quality of life and can cause patients to discontinue DAPT, thereby increasing their risk of thrombosis.
The TOPIC protocol didn’t utilize a loading dose of clopidogrel when making the switch. Investigators started clopidogrel the day after stopping prasugrel and at least 12 hours after the final dose of ticagrelor.
Ideally, the novel TOPIC findings should be confirmed in a much larger, randomized, double-blind clinical trial capable of detecting any small differences in stent thrombosis or MI rates before physicians adopt a change in practice, but discussant Chaim Lotan, MD, director of the Heart Institute at Hadassah Medical Center in Jerusalem, dismissed that prospect as unlikely.
“I tried myself to do a similar study and found I got a lot of opposition from the pharma companies as well as from physicians who said, ‘How can you go against the guidelines?’ ” he said.
“I want to congratulate your team because I think this is a groundbreaking study that is going to dictate a changing of the guidelines,” he told Dr. Cuisset.
Dr. Cuisset reported having no financial conflicts regarding this investigator-driven study funded without commercial support.
Simultaneous with his presentation in Paris, the TOPIC findings were published online (Eur Heart J. 2017 May 16. doi: 10.1093/eurheartj/ehx175).
Dr. Cuisset reported no financial conflicts regarding this investigator-driven study funded without commercial support.
[email protected]
PARIS – A strategy of switching from prasugrel or ticagrelor to clopidogrel 1 month after percutaneous coronary intervention for acute coronary syndrome is superior to the guideline-recommended full 12 months of dual-antiplatelet therapy with either of the newer P2Y12 inhibitors, according to Thomas Cuisset, MD.
In the randomized TOPIC (Timing of Platelet Inhibition After Acute Coronary Syndrome) trial, this switch strategy resulted in a marked reduction in bleeding without an increased risk of ischemic events, compared with a full 12 months of standard dual-antiplatelet therapy (DAPT) using prasugrel (Effient) or ticagrelor (Brilinta).
He added that the cost savings of this switch strategy would be enormous, since generic clopidogrel is vastly less expensive than prasugrel or ticagrelor.
Twelve months of DAPT with aspirin plus either prasugrel or ticagrelor is the guideline-recommended DAPT regimen following PCI for ACS on the strength of the TRITON and PLATO trials, respectively, which showed that those agents were more effective than clopidogrel for the prevention of thrombotic events. But Dr. Cuisset and his coinvestigators noted that the risk of ischemic events was highest in the first month or so following ACS, while the risk of DAPT-related serious bleeding increased after the first month and continued for the duration.
“We need to use the new drugs, and we need to go for 1 year with DAPT. But does that mean we need to go for 1 year with the new drugs?” he asked.
This question was the impetus for TOPIC, an open-label, single-center randomized trial that included 646 ACS patients who were free of major adverse cardiovascular events during their first month on DAPT with prasugrel or ticagrelor. At that point they were randomized to remain on their standard regimen or switch to aspirin at 75 mg/day plus clopidogrel at 75 mg/day for months 2-12. The switch strategy is similar to the way pulmonary embolism is managed: an early phase of high-intensity therapy followed by a backing off to a less intensive regimen, said Dr. Cuisset, a cardiologist at Aix-Marseille University, Provence, France.
The primary endpoint in TOPIC was the cumulative 1-year rate of a composite of all-cause mortality, stroke, urgent revascularization, or clinically significant bleeding as reflected in a Bleeding Academic Research Consortium (BARC) grade 2 or greater bleeding. The primary endpoint occurred in 13.4% of the switch group, a 52% relative risk reduction, compared with the 26.3% cumulative incidence with standard DAPT.
This difference wasn’t due to any between-group disparity in ischemic events, but rather to a 70% reduction in the risk of BARC grade 2 or greater bleeding in the switch group: 4.0% vs. 14.9%.
Some physicians have already been switching to clopidogrel for DAPT after ACS, either because of safety or cost concerns. Now their practice is evidence based, Dr. Cuisset noted.
Asked why TOPIC didn’t use the more stringent bleeding endpoint of BARC grade 3-5 bleeding, the cardiologist replied that it would have required a larger trial to show a significant difference. Besides, he added, BARC grade 2 bleeding is clinically important because it has a negative impact on quality of life and can cause patients to discontinue DAPT, thereby increasing their risk of thrombosis.
The TOPIC protocol didn’t utilize a loading dose of clopidogrel when making the switch. Investigators started clopidogrel the day after stopping prasugrel and at least 12 hours after the final dose of ticagrelor.
Ideally, the novel TOPIC findings should be confirmed in a much larger, randomized, double-blind clinical trial capable of detecting any small differences in stent thrombosis or MI rates before physicians adopt a change in practice, but discussant Chaim Lotan, MD, director of the Heart Institute at Hadassah Medical Center in Jerusalem, dismissed that prospect as unlikely.
“I tried myself to do a similar study and found I got a lot of opposition from the pharma companies as well as from physicians who said, ‘How can you go against the guidelines?’ ” he said.
“I want to congratulate your team because I think this is a groundbreaking study that is going to dictate a changing of the guidelines,” he told Dr. Cuisset.
Dr. Cuisset reported having no financial conflicts regarding this investigator-driven study funded without commercial support.
Simultaneous with his presentation in Paris, the TOPIC findings were published online (Eur Heart J. 2017 May 16. doi: 10.1093/eurheartj/ehx175).
Dr. Cuisset reported no financial conflicts regarding this investigator-driven study funded without commercial support.
[email protected]
PARIS – A strategy of switching from prasugrel or ticagrelor to clopidogrel 1 month after percutaneous coronary intervention for acute coronary syndrome is superior to the guideline-recommended full 12 months of dual-antiplatelet therapy with either of the newer P2Y12 inhibitors, according to Thomas Cuisset, MD.
In the randomized TOPIC (Timing of Platelet Inhibition After Acute Coronary Syndrome) trial, this switch strategy resulted in a marked reduction in bleeding without an increased risk of ischemic events, compared with a full 12 months of standard dual-antiplatelet therapy (DAPT) using prasugrel (Effient) or ticagrelor (Brilinta).
He added that the cost savings of this switch strategy would be enormous, since generic clopidogrel is vastly less expensive than prasugrel or ticagrelor.
Twelve months of DAPT with aspirin plus either prasugrel or ticagrelor is the guideline-recommended DAPT regimen following PCI for ACS on the strength of the TRITON and PLATO trials, respectively, which showed that those agents were more effective than clopidogrel for the prevention of thrombotic events. But Dr. Cuisset and his coinvestigators noted that the risk of ischemic events was highest in the first month or so following ACS, while the risk of DAPT-related serious bleeding increased after the first month and continued for the duration.
“We need to use the new drugs, and we need to go for 1 year with DAPT. But does that mean we need to go for 1 year with the new drugs?” he asked.
This question was the impetus for TOPIC, an open-label, single-center randomized trial that included 646 ACS patients who were free of major adverse cardiovascular events during their first month on DAPT with prasugrel or ticagrelor. At that point they were randomized to remain on their standard regimen or switch to aspirin at 75 mg/day plus clopidogrel at 75 mg/day for months 2-12. The switch strategy is similar to the way pulmonary embolism is managed: an early phase of high-intensity therapy followed by a backing off to a less intensive regimen, said Dr. Cuisset, a cardiologist at Aix-Marseille University, Provence, France.
The primary endpoint in TOPIC was the cumulative 1-year rate of a composite of all-cause mortality, stroke, urgent revascularization, or clinically significant bleeding as reflected in a Bleeding Academic Research Consortium (BARC) grade 2 or greater bleeding. The primary endpoint occurred in 13.4% of the switch group, a 52% relative risk reduction, compared with the 26.3% cumulative incidence with standard DAPT.
This difference wasn’t due to any between-group disparity in ischemic events, but rather to a 70% reduction in the risk of BARC grade 2 or greater bleeding in the switch group: 4.0% vs. 14.9%.
Some physicians have already been switching to clopidogrel for DAPT after ACS, either because of safety or cost concerns. Now their practice is evidence based, Dr. Cuisset noted.
Asked why TOPIC didn’t use the more stringent bleeding endpoint of BARC grade 3-5 bleeding, the cardiologist replied that it would have required a larger trial to show a significant difference. Besides, he added, BARC grade 2 bleeding is clinically important because it has a negative impact on quality of life and can cause patients to discontinue DAPT, thereby increasing their risk of thrombosis.
The TOPIC protocol didn’t utilize a loading dose of clopidogrel when making the switch. Investigators started clopidogrel the day after stopping prasugrel and at least 12 hours after the final dose of ticagrelor.
Ideally, the novel TOPIC findings should be confirmed in a much larger, randomized, double-blind clinical trial capable of detecting any small differences in stent thrombosis or MI rates before physicians adopt a change in practice, but discussant Chaim Lotan, MD, director of the Heart Institute at Hadassah Medical Center in Jerusalem, dismissed that prospect as unlikely.
“I tried myself to do a similar study and found I got a lot of opposition from the pharma companies as well as from physicians who said, ‘How can you go against the guidelines?’ ” he said.
“I want to congratulate your team because I think this is a groundbreaking study that is going to dictate a changing of the guidelines,” he told Dr. Cuisset.
Dr. Cuisset reported having no financial conflicts regarding this investigator-driven study funded without commercial support.
Simultaneous with his presentation in Paris, the TOPIC findings were published online (Eur Heart J. 2017 May 16. doi: 10.1093/eurheartj/ehx175).
Dr. Cuisset reported no financial conflicts regarding this investigator-driven study funded without commercial support.
[email protected]
AT EuroPCR
Key clinical point:
Major finding: The cumulative 1-year incidence of all-cause mortality, stroke, urgent revascularization, or clinically significant bleeding was 13.4% in acute coronary syndrome patients who switched to clopidogrel after 1 month on prasugrel or ticagrelor for dual-antiplatelet therapy, compared with 26.3% in those who didn’t switch.
Data source: An open-label, single-center, randomized trial including 646 ACS patients.
Disclosures: The presenter reported no financial conflicts regarding this investigator-driven study funded without commercial support.
Game over: VTE is a risk in obese, sedentary teens
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
FROM ASPHO 2017
Key clinical point: Obesity and a sedentary lifestyle are risk factors for venous thromboembolic events in teens, as well as adults.
Major finding: Teen boys who were obese and spent much of their day playing video games presented with VTE.
Data source: Retrospective review and case series.
Disclosures: The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
Antithrombotics no deterrent for emergent lap appendectomy
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Emergent laparoscopic appendectomy poses no significant risk for patients on irreversible antithrombotic therapy.
Major finding: Average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% vs. 1%, respectively.
Data source: A retrospective study of 390 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014.
Disclosures: Dr. Pearcy reported having no financial disclosures.