User login
Military Deployment Raises Respiratory Disease Risk
Individuals who served in Iraq or Afghanistan had significantly higher rates of new-onset respiratory diseases after deployment compared to non-deployed control peers, based on data from more than 48,000 veterans. The findings were presented at the American College of Allergy, Asthma, and Immunology (ACAAI) 2025 Annual Meeting.
“Veterans deployed to Iraq and Afghanistan were often exposed to airborne hazards such as burn pits and dust storms,” said Patrick Gleeson, MD, an allergist at the University of Pennsylvania Perelman School of Medicine, Philadelphia, in a press release.
“We found that these exposures may have long-term health impacts, particularly for respiratory diseases that can affect quality of life for years after service,” said Gleeson, who presented the results at the meeting.
Gleeson and colleagues used data from the Veterans Affairs Corporate Data Warehouse and Observational Medical Outcomes Partnership to identify veterans with a single deployment as part of Operation Iraqi Freedom or Operation Enduring Freedom. Participants had at least one outpatient visit prior to deployment with no baseline history of asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis. The mean age of the participants at deployment was 26.7 years, 84% were male, 75% were White, and 11% were Hispanic or Latino. Each was matched with a similar non-deployed veteran control.
The primary outcome was outpatient diagnoses or problem list entries for asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis.
Compared to non-deployed peers, deployed veterans had a 55% increased risk of asthma, a 48% increased risk of nasal polyposis, a 41% increased risk of chronic rhinitis, and a 27% increased risk of chronic rhinosinusitis, based on Cox proportional hazards models (P < .0005 for all).
The findings were limited by the retrospective design. However, “Recognizing the link between deployment and respiratory disease can help guide medical support, policy, and preventive strategies for those affected,” Gleeson said in the press release.
The study received no outside funding. The researchers disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Individuals who served in Iraq or Afghanistan had significantly higher rates of new-onset respiratory diseases after deployment compared to non-deployed control peers, based on data from more than 48,000 veterans. The findings were presented at the American College of Allergy, Asthma, and Immunology (ACAAI) 2025 Annual Meeting.
“Veterans deployed to Iraq and Afghanistan were often exposed to airborne hazards such as burn pits and dust storms,” said Patrick Gleeson, MD, an allergist at the University of Pennsylvania Perelman School of Medicine, Philadelphia, in a press release.
“We found that these exposures may have long-term health impacts, particularly for respiratory diseases that can affect quality of life for years after service,” said Gleeson, who presented the results at the meeting.
Gleeson and colleagues used data from the Veterans Affairs Corporate Data Warehouse and Observational Medical Outcomes Partnership to identify veterans with a single deployment as part of Operation Iraqi Freedom or Operation Enduring Freedom. Participants had at least one outpatient visit prior to deployment with no baseline history of asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis. The mean age of the participants at deployment was 26.7 years, 84% were male, 75% were White, and 11% were Hispanic or Latino. Each was matched with a similar non-deployed veteran control.
The primary outcome was outpatient diagnoses or problem list entries for asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis.
Compared to non-deployed peers, deployed veterans had a 55% increased risk of asthma, a 48% increased risk of nasal polyposis, a 41% increased risk of chronic rhinitis, and a 27% increased risk of chronic rhinosinusitis, based on Cox proportional hazards models (P < .0005 for all).
The findings were limited by the retrospective design. However, “Recognizing the link between deployment and respiratory disease can help guide medical support, policy, and preventive strategies for those affected,” Gleeson said in the press release.
The study received no outside funding. The researchers disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Individuals who served in Iraq or Afghanistan had significantly higher rates of new-onset respiratory diseases after deployment compared to non-deployed control peers, based on data from more than 48,000 veterans. The findings were presented at the American College of Allergy, Asthma, and Immunology (ACAAI) 2025 Annual Meeting.
“Veterans deployed to Iraq and Afghanistan were often exposed to airborne hazards such as burn pits and dust storms,” said Patrick Gleeson, MD, an allergist at the University of Pennsylvania Perelman School of Medicine, Philadelphia, in a press release.
“We found that these exposures may have long-term health impacts, particularly for respiratory diseases that can affect quality of life for years after service,” said Gleeson, who presented the results at the meeting.
Gleeson and colleagues used data from the Veterans Affairs Corporate Data Warehouse and Observational Medical Outcomes Partnership to identify veterans with a single deployment as part of Operation Iraqi Freedom or Operation Enduring Freedom. Participants had at least one outpatient visit prior to deployment with no baseline history of asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis. The mean age of the participants at deployment was 26.7 years, 84% were male, 75% were White, and 11% were Hispanic or Latino. Each was matched with a similar non-deployed veteran control.
The primary outcome was outpatient diagnoses or problem list entries for asthma, chronic rhinitis, chronic rhinosinusitis, or nasal polyposis.
Compared to non-deployed peers, deployed veterans had a 55% increased risk of asthma, a 48% increased risk of nasal polyposis, a 41% increased risk of chronic rhinitis, and a 27% increased risk of chronic rhinosinusitis, based on Cox proportional hazards models (P < .0005 for all).
The findings were limited by the retrospective design. However, “Recognizing the link between deployment and respiratory disease can help guide medical support, policy, and preventive strategies for those affected,” Gleeson said in the press release.
The study received no outside funding. The researchers disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM ACAAI 2025
Approach to Weight Management in GI Practice
Introduction
The majority of patients in the United States are now overweight or obese, and as gastroenterologists we treat a number of conditions that are caused or worsened by obesity.1 Cirrhosis related to metabolic associated fatty liver disease (MAFLD) is now a leading indication for liver transplantation in the US2 and obesity is a clear risk factor for all major malignancies of the GI tract, including esophageal, gastric cardia, pancreatic, liver, gallbladder, colon, and rectum.3 Obesity is associated with dysbiosis and impacts barrier function: increasing permeability, abnormal gut bacterial translocation, and inflammation.4 It is more common than malnutrition in our patients with inflammatory bowel disease (IBD), where it impacts response to biologic drugs, increases the technical difficulty of surgeries, such as IPAA, and is associated with worse surgical outcomes.5 Furthermore, patients with obesity may be less likely to undergo preventative cancer screenings and are at increased risk related to sedation for endoscopic procedures.6 With over 40% of Americans suffering from obesity, and increasingly effective treatments available,
Understanding the Mechanisms of Obesity
There are complex orexigenic and anorexigenic brain pathways in the hypothalamus which control global energy balance.7 Obesity results when energy intake exceeds energy expenditure. While overeating and a sedentary lifestyle are commonly blamed, there are a number of elements that contribute, including genetics, medical conditions, medications, psychosocial factors, and environmental components. For example, sleep loss contributes to weight gain by several mechanisms including increasing ghrelin and decreasing leptin levels, thereby increasing hunger and appetite, as well as by decreasing insulin sensitivity and increasing cortisol. Subjects exposed to sleep deprivation in research settings take in 550 kcal more the following day.8 Medications used commonly in GI practice including corticosteroids, antihistamines, propranolol, and amitriptyline, are obesogenic9 and cannabis can impact hypothalamic pathways to stimulate hunger.10
When patients diet or exercise to lose weight, as we have traditionally advised, there are strong hormonal changes and metabolic adaptations that occur to preserve the defended fat mass or “set point.” Loss of adipose tissue results in decreased production of leptin, a hormone that stimulates satiety pathways and inhibits orexigenic pathways, greatly increasing hunger and cravings. Increases in ghrelin production by the stomach decreases perceptions of fullness. With weight loss, energy requirements decrease, and muscles become more efficient, meaning fewer kcal are needed to maintain bodily processes.11 Eventually a plateau is reached, while motivation to diet and restraint around food wane, and hedonistic (reward) pathways are activated. These powerful factors result in the regain of lost weight within one year in the majority of patients.
Implementing Weight Management into GI Practice
Given the stigma and bias around obesity, patients often feel shame and vulnerability around the condition. It is important to have empathy in your approach, asking permission to discuss weight and using patient-first language (e.g. “patient with obesity” not “obese patient”). While BMI is predictive of health outcomes, it does not measure body fat percentage and may be misleading, such as in muscular individuals. Other measures of adiposity including waist circumference and body composition testing, such as with DEXA, may provide additional data. A BMI of 30 or above defines obesity, though newer definitions incorporate related symptoms, organ disfunction, and metabolic abnormalities into the term “clinical obesity.”12 Asian patients experience metabolic complications at a lower BMI, and therefore the definition of obese is 27.5kg/m2 in this population.
Begin by taking a weight history. Has this been a lifelong struggle or is there a particular life circumstance, such as working a third shift or recent pregnancy which precipitated weight gain? Patients should be asked about binge eating or eating late into the evening or waking at night to eat, as these disordered eating behaviors are managed with specific medications and behavioral therapies. Inquire about sleep duration and quality and refer for a sleep study if there is suspicion for obstructive sleep apnea. Other weight-related comorbidities including hyperlipidemia, type 2 diabetes mellitus (T2DM), and MAFLD should be considered and merit a more aggressive approach, as does more severe obesity (class III, BMI ≥40). Questions about marijuana and alcohol use as well as review of the medication list for obesogenic medications can provide further insight into modifiable contributing factors.
Pillars of Weight Management
The internet is awash with trendy diet recommendations, and widespread misconceptions about obesity management are even ingrained into how physicians approach the disease. It is critical to remember that this is not a consequence of bad choices or lack of self-control. Exercise alone is insufficient to result in significant weight loss.13 Furthermore, whether it is through low fat, low carb, or intermittent fasting, weight loss will occur with calorie deficit.14 Evidence-based diet and lifestyle recommendations to lay the groundwork for success should be discussed at each visit (see Table 1). The Mediterranean diet is recommended for weight loss as well as for several GI disorders (i.e., MAFLD and IBD) and is the optimal eating strategy for cardiovascular health.15 Patients should be advised to engage in 150 minutes of moderate exercise per week, such as brisk walking, and should incorporate resistance training to build muscle and maintain bone density.
Anti-obesity Medications
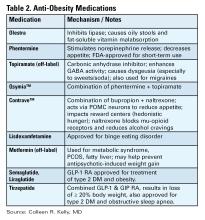
There are a number of medications, either FDA approved or used off label, for treatment of obesity (see Table 2).16 All are indicated for patients with a BMI of ≥ 30 kg/m2 or for those with a BMI between 27-29 kg/m2 with weight-related comorbidities and should be used in combination with diet and lifestyle interventions. None are approved or safe in pregnancy. Mechanisms of action vary by type and include decreased appetite, increased energy expenditure, improved insulin sensitivity, and interfere with absorption.
The newest and most effective anti-obesity medications (AOM), the glucagon-like peptide-1 receptor agonists (GLP-1 RA) are derived from gut hormones secreted in the distal small bowel and colon in response to a meal, which function to delay gastric emptying, increase insulin release from the pancreas, and reduce hepatic gluconeogenesis. Central nervous system effects are not yet entirely understood, but function to decrease appetite and increase satiety. Initially developed for treatment of T2DM, observed weight reduction in patients treated with GLP-1 RA led to clinical trials for treatment of obesity. Semaglutide treatment resulted in weight reduction of 16.9% of total body weight (TBW), and one third of subjects lost ≥ 20% of TBW.17 Tirzepatide combines GLP-1 RA and a gastric inhibitory polypeptide (GIP) receptor agonist, which also has an incretin effect and functions to slow gastric emptying. In the pivotal SURMOUNT trial, approximately 58% of patients achieved ≥20% loss of TBW18 with 15mg weekly dosing of tirzepatide. This class of drugs is a logical choice in patients with T2DM and obesity. Long-term treatment appears necessary, as patients typically regain two-thirds of lost weight within a year after GLP-1 RA are stopped.
Based on tumors observed in rodents, GLP-1 RA are contraindicated in patients with a personal or family history of multiple endocrine neoplasia type 2 (MEN II) or medullary thyroid cancer. These tumors have not been observed in humans treated with GLP-1 RA. They should be used with caution in patients with history of pancreatitis, gastroparesis, or diabetic retinopathy, though a recent systematic review and meta-analysis suggests showed little to no increased risk for biliary events from GLP-1 RA.19 Side effects are most commonly gastrointestinal in nature (nausea, reflux, constipation or diarrhea) and are typically most severe with initiation of the drug and with dose escalation. Side effects can be mitigated by initiating these drugs at lowest doses and gradually titrating up (every four weeks) based on effectiveness and tolerability. Antisecretory, antiemetic, and laxative medications can also be used to help manage GLP-1 RA related side effects.
There is no reason to escalate to highest doses if patients are experiencing weight loss and reduction in food cravings at lower doses. Both semaglutide and tirzepatide are administered subcutaneously every seven days. Once patients have reached goal weight, they can either continue maintenance therapy at that same dose/interval, or if motivated to do so, may gradually reduce the weekly dose in a stepwise approach to determine the minimally effective dose to maintain weight loss. There are not yet published maintenance studies to guide this process. Currently the price of GLP-1 RA and inconsistent insurance coverage make them inaccessible to many patients. The manufacturers of both semaglutide and tirzepatide offer direct to consumer pricing and home delivery.
Bariatric Surgery
In patients with higher BMI (≥35kg/m2) or those with BMI ≥30kg/m2 and obesity-related metabolic disease and the desire to avoid lifelong medications or who fail or are intolerant of AOM, bariatric options should be considered.20 Sleeve gastrectomy has become the most performed surgery for treatment of obesity. It is a restrictive procedure, removing 80% of the stomach, but a drop in circulating levels of ghrelin afterwards also leads to decreased feelings of hunger. It results in weight loss of 25-30% TBW loss. It is not a good choice for patients who suffer from severe GERD, as this typically worsens afterwards; furthermore, de novo Barrett’s has been observed in nearly 6% of patients who undergo sleeve gastrectomy.21
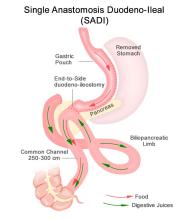
Roux-en-Y gastric bypass is a restrictive and malabsorptive procedure, resulting in 30-35% TBW loss. It has beneficial and immediate metabolic effects, including increased release of endogenous GLP-1, which leads to improvements in weight-related T2DM. The newer single anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) starts with a sleeve gastrectomy, making a smaller tube-shaped stomach. The duodenum is divided just after the stomach and then a loop of ileum is brought up and connected to the stomach (see Figure 1). This procedure is highly effective, with patients losing 75-95% of excess body weight and is becoming a preferred option for patients with greater BMI (≥50kg/m2). It is also an option for patients who have already had a sleeve gastrectomy and are seeking further weight loss. Because there is only one anastomosis, perioperative complications, such as anastomotic leaks, are reduced. The risk of micronutrient deficiencies is present with all malabsorptive procedures, and these patients must supplement with multivitamins, iron, vitamin D, and calcium.
Endoscopic Therapies
Endoscopic bariatric and metabolic therapies (EBMTs) have been increasingly studied and utilized, and this less invasive option may be more appropriate for or attractive to many patients. Intragastric balloons, which reduce meal volume and delay gastric emptying, can be used short term only (six months) resulting in loss of about 6.9% of total body weight (TBW) greater than lifestyle modification (LM) alone, and may be considered in limited situations, such as need for pre-operative weight loss to reduce risks in very obese individuals.22
Endoscopic gastric remodeling (EGR), also known as endoscopic sleeve gastrectomy (ESG), is a purely restrictive procedure in which the stomach is cinched to resize and reshape using an endoscopic suturing device (see Figure 2).23 It is an option for patients with class 1 or 2 obesity, with data from a randomized controlled trial in this population demonstrating mean percentage of TBW loss of 13.6% at 52 weeks compared to 0.8% in those treated with LM alone.24 A recent meta-analysis of 21 observational studies, including patients with higher BMIs (32.5 to 49.9 kg/m2) showed pooled average weight loss of 17.3% TBW at 12 months with EGR.22 This procedure has potential advantages of fewer complications, quicker recovery, and much less new-onset GERD compared to laparoscopic sleeve gastrectomy. Furthermore, it may be utilized in combination with AOMs to achieve optimum weight loss and metabolic outcomes.25,26 Potential adverse events include abdominal pain, nausea and vomiting (which may be severe), as well as rare instances of intra/extra luminal bleeding or abdominal abscess requiring drainage.22
Recent joint American/European Gastrointestinal Endoscopy guidelines suggest the use of EBMTs plus lifestyle modification in patients with a BMI of ≥ 30 kg/m2, or with a BMI of 27.0-29.9 kg/m2 with at least 1 obesity-related comorbidity.22 Small bowel interventions including duodenal-jejunal bypass liner and duodenal mucosal resurfacing are being investigated for patients with obesity and type 2 diabetes but not yet commercially available.
Conclusion
Given the overlap of obesity with many GI disorders, it is entirely appropriate for gastroenterologists to consider it worthy of aggressive treatment, particularly in patients with MAFLD and other serious weight related comorbidities. With a compassionate and empathetic approach, and a number of highly effective medical, endoscopic, and surgical therapies now available, weight management has the potential to be extremely rewarding when implemented in GI practice.
Dr. Kelly is based in the Department of Medicine, Division of Gastroenterology, Brigham and Women’s Hospital, and Harvard Medical School, both in Boston, Massachusetts. She serves on the clinical advisory board for OpenBiome (unpaid) and has served on an advisory board for Eli Lilly and Company.
References
1. Hales CM, et al. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS Data Brief 2020 Feb:(360):1–8.
2. Pais R, et al. NAFLD and liver transplantation: Current burden and expected challenges. J Hepatol. 2016 Dec. doi: 10.1016/j.jhep.2016.07.033.
3. Lauby-Secretan B, et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med. 2016 Aug. doi: 10.1056/NEJMsr1606602.
4. Kim A. Dysbiosis: A Review Highlighting Obesity and Inflammatory Bowel Disease. J Clin Gastroenterol. 2015 Nov-Dec. doi: 10.1097/MCG.0000000000000356.
5. Singh S, et al. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017 Feb. doi: 10.1038/nrgastro.2016.181.
6. Sundararaman L, Goudra B. Sedation for GI Endoscopy in the Morbidly Obese: Challenges and Possible Solutions. J Clin Med. 2024 Aug. doi: 10.3390/jcm13164635.
7. Bombassaro B, et al. The hypothalamus as the central regulator of energy balance and its impact on current and future obesity treatments. Arch Endocrinol Metab. 2024 Nov. doi: 10.20945/2359-4292-2024-0082.
8. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011 Jul. doi: 10.1097/MCO.0b013e3283479109.
9. Desalermos A, et al. Effect of Obesogenic Medications on Weight-Loss Outcomes in a Behavioral Weight-Management Program. Obesity (Silver Spring). 2019 May. doi: 10.1002/oby.22444.
10. Lord MN, Noble EE. Hypothalamic cannabinoid signaling: Consequences for eating behavior. Pharmacol Res Perspect. 2024 Oct. doi: 10.1002/prp2.1251.
11. Farhana A, Rehman A. Metabolic Consequences of Weight Reduction. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572145/.
12. Rubino F, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025 Mar. doi: 10.1016/S2213-8587(24)00316-4.
13. Cox CE. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017 Aug. doi: 10.2337/ds17-0013.
14. Chaput JP, et al. Widespread misconceptions about obesity. Can Fam Physician. 2014 Nov. PMID: 25392431.
15. Muscogiuri G, et al. Mediterranean Diet and Obesity-related Disorders: What is the Evidence? Curr Obes Rep. 2022 Dec. doi: 10.1007/s13679-022-00481-1.
16. Gudzune KA, Kushner RF. Medications for Obesity: A Review. JAMA. 2024 Aug. doi: 10.1001/jama.2024.10816.
17. Wilding JPH, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Feb. doi: 10.1056/NEJMoa2032183.
18. Jastreboff AM, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jun. doi: 10.1056/NEJMoa2206038.
19. Chiang CH, et al. Glucagon-Like Peptide-1 Receptor Agonists and Gastrointestinal Adverse Events: A Systematic Review and Meta-Analysis. Gastroenterology. 2025 Nov. doi: 10.1053/j.gastro.2025.06.003.
20. Aderinto N, et al. Recent advances in bariatric surgery: a narrative review of weight loss procedures. Ann Med Surg (Lond). 2023 Nov. doi: 10.1097/MS9.0000000000001472.
21. Chandan S, et al. Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis of Studies With Long-Term Follow-Up. Clin Gastroenterol Hepatol. 2025 Jan. doi: 10.1016/j.cgh.2024.06.041.
22. Jirapinyo P, et al. American Society for Gastrointestinal Endoscopy-European Society of Gastrointestinal Endoscopy guideline on primary endoscopic bariatric and metabolic therapies for adults with obesity. Gastrointest Endosc. 2024 Jun. doi: 10.1016/j.gie.2023.12.004.
23. Nduma BN, et al. Endoscopic Gastric Sleeve: A Review of Literature. Cureus. 2023 Mar. doi: 10.7759/cureus.36353.
24. Abu Dayyeh BK, et al. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet. 2022 Aug. doi: 10.1016/S0140-6736(22)01280-6.
25. Gala K, et al. Outcomes of concomitant antiobesity medication use with endoscopic sleeve gastroplasty in clinical US settings. Obes Pillars. 2024 May. doi: 10.1016/j.obpill.2024.100112.
26. Chung CS, et al. Endoscopic sleeve gastroplasty combined with anti-obesity medication for better control of weight and diabetes. Clin Endosc. 2025 May. doi: 10.5946/ce.2024.274.
Introduction
The majority of patients in the United States are now overweight or obese, and as gastroenterologists we treat a number of conditions that are caused or worsened by obesity.1 Cirrhosis related to metabolic associated fatty liver disease (MAFLD) is now a leading indication for liver transplantation in the US2 and obesity is a clear risk factor for all major malignancies of the GI tract, including esophageal, gastric cardia, pancreatic, liver, gallbladder, colon, and rectum.3 Obesity is associated with dysbiosis and impacts barrier function: increasing permeability, abnormal gut bacterial translocation, and inflammation.4 It is more common than malnutrition in our patients with inflammatory bowel disease (IBD), where it impacts response to biologic drugs, increases the technical difficulty of surgeries, such as IPAA, and is associated with worse surgical outcomes.5 Furthermore, patients with obesity may be less likely to undergo preventative cancer screenings and are at increased risk related to sedation for endoscopic procedures.6 With over 40% of Americans suffering from obesity, and increasingly effective treatments available,
Understanding the Mechanisms of Obesity
There are complex orexigenic and anorexigenic brain pathways in the hypothalamus which control global energy balance.7 Obesity results when energy intake exceeds energy expenditure. While overeating and a sedentary lifestyle are commonly blamed, there are a number of elements that contribute, including genetics, medical conditions, medications, psychosocial factors, and environmental components. For example, sleep loss contributes to weight gain by several mechanisms including increasing ghrelin and decreasing leptin levels, thereby increasing hunger and appetite, as well as by decreasing insulin sensitivity and increasing cortisol. Subjects exposed to sleep deprivation in research settings take in 550 kcal more the following day.8 Medications used commonly in GI practice including corticosteroids, antihistamines, propranolol, and amitriptyline, are obesogenic9 and cannabis can impact hypothalamic pathways to stimulate hunger.10
When patients diet or exercise to lose weight, as we have traditionally advised, there are strong hormonal changes and metabolic adaptations that occur to preserve the defended fat mass or “set point.” Loss of adipose tissue results in decreased production of leptin, a hormone that stimulates satiety pathways and inhibits orexigenic pathways, greatly increasing hunger and cravings. Increases in ghrelin production by the stomach decreases perceptions of fullness. With weight loss, energy requirements decrease, and muscles become more efficient, meaning fewer kcal are needed to maintain bodily processes.11 Eventually a plateau is reached, while motivation to diet and restraint around food wane, and hedonistic (reward) pathways are activated. These powerful factors result in the regain of lost weight within one year in the majority of patients.
Implementing Weight Management into GI Practice
Given the stigma and bias around obesity, patients often feel shame and vulnerability around the condition. It is important to have empathy in your approach, asking permission to discuss weight and using patient-first language (e.g. “patient with obesity” not “obese patient”). While BMI is predictive of health outcomes, it does not measure body fat percentage and may be misleading, such as in muscular individuals. Other measures of adiposity including waist circumference and body composition testing, such as with DEXA, may provide additional data. A BMI of 30 or above defines obesity, though newer definitions incorporate related symptoms, organ disfunction, and metabolic abnormalities into the term “clinical obesity.”12 Asian patients experience metabolic complications at a lower BMI, and therefore the definition of obese is 27.5kg/m2 in this population.
Begin by taking a weight history. Has this been a lifelong struggle or is there a particular life circumstance, such as working a third shift or recent pregnancy which precipitated weight gain? Patients should be asked about binge eating or eating late into the evening or waking at night to eat, as these disordered eating behaviors are managed with specific medications and behavioral therapies. Inquire about sleep duration and quality and refer for a sleep study if there is suspicion for obstructive sleep apnea. Other weight-related comorbidities including hyperlipidemia, type 2 diabetes mellitus (T2DM), and MAFLD should be considered and merit a more aggressive approach, as does more severe obesity (class III, BMI ≥40). Questions about marijuana and alcohol use as well as review of the medication list for obesogenic medications can provide further insight into modifiable contributing factors.
Pillars of Weight Management
The internet is awash with trendy diet recommendations, and widespread misconceptions about obesity management are even ingrained into how physicians approach the disease. It is critical to remember that this is not a consequence of bad choices or lack of self-control. Exercise alone is insufficient to result in significant weight loss.13 Furthermore, whether it is through low fat, low carb, or intermittent fasting, weight loss will occur with calorie deficit.14 Evidence-based diet and lifestyle recommendations to lay the groundwork for success should be discussed at each visit (see Table 1). The Mediterranean diet is recommended for weight loss as well as for several GI disorders (i.e., MAFLD and IBD) and is the optimal eating strategy for cardiovascular health.15 Patients should be advised to engage in 150 minutes of moderate exercise per week, such as brisk walking, and should incorporate resistance training to build muscle and maintain bone density.
Anti-obesity Medications
There are a number of medications, either FDA approved or used off label, for treatment of obesity (see Table 2).16 All are indicated for patients with a BMI of ≥ 30 kg/m2 or for those with a BMI between 27-29 kg/m2 with weight-related comorbidities and should be used in combination with diet and lifestyle interventions. None are approved or safe in pregnancy. Mechanisms of action vary by type and include decreased appetite, increased energy expenditure, improved insulin sensitivity, and interfere with absorption.
The newest and most effective anti-obesity medications (AOM), the glucagon-like peptide-1 receptor agonists (GLP-1 RA) are derived from gut hormones secreted in the distal small bowel and colon in response to a meal, which function to delay gastric emptying, increase insulin release from the pancreas, and reduce hepatic gluconeogenesis. Central nervous system effects are not yet entirely understood, but function to decrease appetite and increase satiety. Initially developed for treatment of T2DM, observed weight reduction in patients treated with GLP-1 RA led to clinical trials for treatment of obesity. Semaglutide treatment resulted in weight reduction of 16.9% of total body weight (TBW), and one third of subjects lost ≥ 20% of TBW.17 Tirzepatide combines GLP-1 RA and a gastric inhibitory polypeptide (GIP) receptor agonist, which also has an incretin effect and functions to slow gastric emptying. In the pivotal SURMOUNT trial, approximately 58% of patients achieved ≥20% loss of TBW18 with 15mg weekly dosing of tirzepatide. This class of drugs is a logical choice in patients with T2DM and obesity. Long-term treatment appears necessary, as patients typically regain two-thirds of lost weight within a year after GLP-1 RA are stopped.
Based on tumors observed in rodents, GLP-1 RA are contraindicated in patients with a personal or family history of multiple endocrine neoplasia type 2 (MEN II) or medullary thyroid cancer. These tumors have not been observed in humans treated with GLP-1 RA. They should be used with caution in patients with history of pancreatitis, gastroparesis, or diabetic retinopathy, though a recent systematic review and meta-analysis suggests showed little to no increased risk for biliary events from GLP-1 RA.19 Side effects are most commonly gastrointestinal in nature (nausea, reflux, constipation or diarrhea) and are typically most severe with initiation of the drug and with dose escalation. Side effects can be mitigated by initiating these drugs at lowest doses and gradually titrating up (every four weeks) based on effectiveness and tolerability. Antisecretory, antiemetic, and laxative medications can also be used to help manage GLP-1 RA related side effects.
There is no reason to escalate to highest doses if patients are experiencing weight loss and reduction in food cravings at lower doses. Both semaglutide and tirzepatide are administered subcutaneously every seven days. Once patients have reached goal weight, they can either continue maintenance therapy at that same dose/interval, or if motivated to do so, may gradually reduce the weekly dose in a stepwise approach to determine the minimally effective dose to maintain weight loss. There are not yet published maintenance studies to guide this process. Currently the price of GLP-1 RA and inconsistent insurance coverage make them inaccessible to many patients. The manufacturers of both semaglutide and tirzepatide offer direct to consumer pricing and home delivery.
Bariatric Surgery
In patients with higher BMI (≥35kg/m2) or those with BMI ≥30kg/m2 and obesity-related metabolic disease and the desire to avoid lifelong medications or who fail or are intolerant of AOM, bariatric options should be considered.20 Sleeve gastrectomy has become the most performed surgery for treatment of obesity. It is a restrictive procedure, removing 80% of the stomach, but a drop in circulating levels of ghrelin afterwards also leads to decreased feelings of hunger. It results in weight loss of 25-30% TBW loss. It is not a good choice for patients who suffer from severe GERD, as this typically worsens afterwards; furthermore, de novo Barrett’s has been observed in nearly 6% of patients who undergo sleeve gastrectomy.21
Roux-en-Y gastric bypass is a restrictive and malabsorptive procedure, resulting in 30-35% TBW loss. It has beneficial and immediate metabolic effects, including increased release of endogenous GLP-1, which leads to improvements in weight-related T2DM. The newer single anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) starts with a sleeve gastrectomy, making a smaller tube-shaped stomach. The duodenum is divided just after the stomach and then a loop of ileum is brought up and connected to the stomach (see Figure 1). This procedure is highly effective, with patients losing 75-95% of excess body weight and is becoming a preferred option for patients with greater BMI (≥50kg/m2). It is also an option for patients who have already had a sleeve gastrectomy and are seeking further weight loss. Because there is only one anastomosis, perioperative complications, such as anastomotic leaks, are reduced. The risk of micronutrient deficiencies is present with all malabsorptive procedures, and these patients must supplement with multivitamins, iron, vitamin D, and calcium.
Endoscopic Therapies
Endoscopic bariatric and metabolic therapies (EBMTs) have been increasingly studied and utilized, and this less invasive option may be more appropriate for or attractive to many patients. Intragastric balloons, which reduce meal volume and delay gastric emptying, can be used short term only (six months) resulting in loss of about 6.9% of total body weight (TBW) greater than lifestyle modification (LM) alone, and may be considered in limited situations, such as need for pre-operative weight loss to reduce risks in very obese individuals.22
Endoscopic gastric remodeling (EGR), also known as endoscopic sleeve gastrectomy (ESG), is a purely restrictive procedure in which the stomach is cinched to resize and reshape using an endoscopic suturing device (see Figure 2).23 It is an option for patients with class 1 or 2 obesity, with data from a randomized controlled trial in this population demonstrating mean percentage of TBW loss of 13.6% at 52 weeks compared to 0.8% in those treated with LM alone.24 A recent meta-analysis of 21 observational studies, including patients with higher BMIs (32.5 to 49.9 kg/m2) showed pooled average weight loss of 17.3% TBW at 12 months with EGR.22 This procedure has potential advantages of fewer complications, quicker recovery, and much less new-onset GERD compared to laparoscopic sleeve gastrectomy. Furthermore, it may be utilized in combination with AOMs to achieve optimum weight loss and metabolic outcomes.25,26 Potential adverse events include abdominal pain, nausea and vomiting (which may be severe), as well as rare instances of intra/extra luminal bleeding or abdominal abscess requiring drainage.22
Recent joint American/European Gastrointestinal Endoscopy guidelines suggest the use of EBMTs plus lifestyle modification in patients with a BMI of ≥ 30 kg/m2, or with a BMI of 27.0-29.9 kg/m2 with at least 1 obesity-related comorbidity.22 Small bowel interventions including duodenal-jejunal bypass liner and duodenal mucosal resurfacing are being investigated for patients with obesity and type 2 diabetes but not yet commercially available.
Conclusion
Given the overlap of obesity with many GI disorders, it is entirely appropriate for gastroenterologists to consider it worthy of aggressive treatment, particularly in patients with MAFLD and other serious weight related comorbidities. With a compassionate and empathetic approach, and a number of highly effective medical, endoscopic, and surgical therapies now available, weight management has the potential to be extremely rewarding when implemented in GI practice.
Dr. Kelly is based in the Department of Medicine, Division of Gastroenterology, Brigham and Women’s Hospital, and Harvard Medical School, both in Boston, Massachusetts. She serves on the clinical advisory board for OpenBiome (unpaid) and has served on an advisory board for Eli Lilly and Company.
References
1. Hales CM, et al. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS Data Brief 2020 Feb:(360):1–8.
2. Pais R, et al. NAFLD and liver transplantation: Current burden and expected challenges. J Hepatol. 2016 Dec. doi: 10.1016/j.jhep.2016.07.033.
3. Lauby-Secretan B, et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med. 2016 Aug. doi: 10.1056/NEJMsr1606602.
4. Kim A. Dysbiosis: A Review Highlighting Obesity and Inflammatory Bowel Disease. J Clin Gastroenterol. 2015 Nov-Dec. doi: 10.1097/MCG.0000000000000356.
5. Singh S, et al. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017 Feb. doi: 10.1038/nrgastro.2016.181.
6. Sundararaman L, Goudra B. Sedation for GI Endoscopy in the Morbidly Obese: Challenges and Possible Solutions. J Clin Med. 2024 Aug. doi: 10.3390/jcm13164635.
7. Bombassaro B, et al. The hypothalamus as the central regulator of energy balance and its impact on current and future obesity treatments. Arch Endocrinol Metab. 2024 Nov. doi: 10.20945/2359-4292-2024-0082.
8. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011 Jul. doi: 10.1097/MCO.0b013e3283479109.
9. Desalermos A, et al. Effect of Obesogenic Medications on Weight-Loss Outcomes in a Behavioral Weight-Management Program. Obesity (Silver Spring). 2019 May. doi: 10.1002/oby.22444.
10. Lord MN, Noble EE. Hypothalamic cannabinoid signaling: Consequences for eating behavior. Pharmacol Res Perspect. 2024 Oct. doi: 10.1002/prp2.1251.
11. Farhana A, Rehman A. Metabolic Consequences of Weight Reduction. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572145/.
12. Rubino F, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025 Mar. doi: 10.1016/S2213-8587(24)00316-4.
13. Cox CE. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017 Aug. doi: 10.2337/ds17-0013.
14. Chaput JP, et al. Widespread misconceptions about obesity. Can Fam Physician. 2014 Nov. PMID: 25392431.
15. Muscogiuri G, et al. Mediterranean Diet and Obesity-related Disorders: What is the Evidence? Curr Obes Rep. 2022 Dec. doi: 10.1007/s13679-022-00481-1.
16. Gudzune KA, Kushner RF. Medications for Obesity: A Review. JAMA. 2024 Aug. doi: 10.1001/jama.2024.10816.
17. Wilding JPH, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Feb. doi: 10.1056/NEJMoa2032183.
18. Jastreboff AM, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jun. doi: 10.1056/NEJMoa2206038.
19. Chiang CH, et al. Glucagon-Like Peptide-1 Receptor Agonists and Gastrointestinal Adverse Events: A Systematic Review and Meta-Analysis. Gastroenterology. 2025 Nov. doi: 10.1053/j.gastro.2025.06.003.
20. Aderinto N, et al. Recent advances in bariatric surgery: a narrative review of weight loss procedures. Ann Med Surg (Lond). 2023 Nov. doi: 10.1097/MS9.0000000000001472.
21. Chandan S, et al. Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis of Studies With Long-Term Follow-Up. Clin Gastroenterol Hepatol. 2025 Jan. doi: 10.1016/j.cgh.2024.06.041.
22. Jirapinyo P, et al. American Society for Gastrointestinal Endoscopy-European Society of Gastrointestinal Endoscopy guideline on primary endoscopic bariatric and metabolic therapies for adults with obesity. Gastrointest Endosc. 2024 Jun. doi: 10.1016/j.gie.2023.12.004.
23. Nduma BN, et al. Endoscopic Gastric Sleeve: A Review of Literature. Cureus. 2023 Mar. doi: 10.7759/cureus.36353.
24. Abu Dayyeh BK, et al. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet. 2022 Aug. doi: 10.1016/S0140-6736(22)01280-6.
25. Gala K, et al. Outcomes of concomitant antiobesity medication use with endoscopic sleeve gastroplasty in clinical US settings. Obes Pillars. 2024 May. doi: 10.1016/j.obpill.2024.100112.
26. Chung CS, et al. Endoscopic sleeve gastroplasty combined with anti-obesity medication for better control of weight and diabetes. Clin Endosc. 2025 May. doi: 10.5946/ce.2024.274.
Introduction
The majority of patients in the United States are now overweight or obese, and as gastroenterologists we treat a number of conditions that are caused or worsened by obesity.1 Cirrhosis related to metabolic associated fatty liver disease (MAFLD) is now a leading indication for liver transplantation in the US2 and obesity is a clear risk factor for all major malignancies of the GI tract, including esophageal, gastric cardia, pancreatic, liver, gallbladder, colon, and rectum.3 Obesity is associated with dysbiosis and impacts barrier function: increasing permeability, abnormal gut bacterial translocation, and inflammation.4 It is more common than malnutrition in our patients with inflammatory bowel disease (IBD), where it impacts response to biologic drugs, increases the technical difficulty of surgeries, such as IPAA, and is associated with worse surgical outcomes.5 Furthermore, patients with obesity may be less likely to undergo preventative cancer screenings and are at increased risk related to sedation for endoscopic procedures.6 With over 40% of Americans suffering from obesity, and increasingly effective treatments available,
Understanding the Mechanisms of Obesity
There are complex orexigenic and anorexigenic brain pathways in the hypothalamus which control global energy balance.7 Obesity results when energy intake exceeds energy expenditure. While overeating and a sedentary lifestyle are commonly blamed, there are a number of elements that contribute, including genetics, medical conditions, medications, psychosocial factors, and environmental components. For example, sleep loss contributes to weight gain by several mechanisms including increasing ghrelin and decreasing leptin levels, thereby increasing hunger and appetite, as well as by decreasing insulin sensitivity and increasing cortisol. Subjects exposed to sleep deprivation in research settings take in 550 kcal more the following day.8 Medications used commonly in GI practice including corticosteroids, antihistamines, propranolol, and amitriptyline, are obesogenic9 and cannabis can impact hypothalamic pathways to stimulate hunger.10
When patients diet or exercise to lose weight, as we have traditionally advised, there are strong hormonal changes and metabolic adaptations that occur to preserve the defended fat mass or “set point.” Loss of adipose tissue results in decreased production of leptin, a hormone that stimulates satiety pathways and inhibits orexigenic pathways, greatly increasing hunger and cravings. Increases in ghrelin production by the stomach decreases perceptions of fullness. With weight loss, energy requirements decrease, and muscles become more efficient, meaning fewer kcal are needed to maintain bodily processes.11 Eventually a plateau is reached, while motivation to diet and restraint around food wane, and hedonistic (reward) pathways are activated. These powerful factors result in the regain of lost weight within one year in the majority of patients.
Implementing Weight Management into GI Practice
Given the stigma and bias around obesity, patients often feel shame and vulnerability around the condition. It is important to have empathy in your approach, asking permission to discuss weight and using patient-first language (e.g. “patient with obesity” not “obese patient”). While BMI is predictive of health outcomes, it does not measure body fat percentage and may be misleading, such as in muscular individuals. Other measures of adiposity including waist circumference and body composition testing, such as with DEXA, may provide additional data. A BMI of 30 or above defines obesity, though newer definitions incorporate related symptoms, organ disfunction, and metabolic abnormalities into the term “clinical obesity.”12 Asian patients experience metabolic complications at a lower BMI, and therefore the definition of obese is 27.5kg/m2 in this population.
Begin by taking a weight history. Has this been a lifelong struggle or is there a particular life circumstance, such as working a third shift or recent pregnancy which precipitated weight gain? Patients should be asked about binge eating or eating late into the evening or waking at night to eat, as these disordered eating behaviors are managed with specific medications and behavioral therapies. Inquire about sleep duration and quality and refer for a sleep study if there is suspicion for obstructive sleep apnea. Other weight-related comorbidities including hyperlipidemia, type 2 diabetes mellitus (T2DM), and MAFLD should be considered and merit a more aggressive approach, as does more severe obesity (class III, BMI ≥40). Questions about marijuana and alcohol use as well as review of the medication list for obesogenic medications can provide further insight into modifiable contributing factors.
Pillars of Weight Management
The internet is awash with trendy diet recommendations, and widespread misconceptions about obesity management are even ingrained into how physicians approach the disease. It is critical to remember that this is not a consequence of bad choices or lack of self-control. Exercise alone is insufficient to result in significant weight loss.13 Furthermore, whether it is through low fat, low carb, or intermittent fasting, weight loss will occur with calorie deficit.14 Evidence-based diet and lifestyle recommendations to lay the groundwork for success should be discussed at each visit (see Table 1). The Mediterranean diet is recommended for weight loss as well as for several GI disorders (i.e., MAFLD and IBD) and is the optimal eating strategy for cardiovascular health.15 Patients should be advised to engage in 150 minutes of moderate exercise per week, such as brisk walking, and should incorporate resistance training to build muscle and maintain bone density.
Anti-obesity Medications
There are a number of medications, either FDA approved or used off label, for treatment of obesity (see Table 2).16 All are indicated for patients with a BMI of ≥ 30 kg/m2 or for those with a BMI between 27-29 kg/m2 with weight-related comorbidities and should be used in combination with diet and lifestyle interventions. None are approved or safe in pregnancy. Mechanisms of action vary by type and include decreased appetite, increased energy expenditure, improved insulin sensitivity, and interfere with absorption.
The newest and most effective anti-obesity medications (AOM), the glucagon-like peptide-1 receptor agonists (GLP-1 RA) are derived from gut hormones secreted in the distal small bowel and colon in response to a meal, which function to delay gastric emptying, increase insulin release from the pancreas, and reduce hepatic gluconeogenesis. Central nervous system effects are not yet entirely understood, but function to decrease appetite and increase satiety. Initially developed for treatment of T2DM, observed weight reduction in patients treated with GLP-1 RA led to clinical trials for treatment of obesity. Semaglutide treatment resulted in weight reduction of 16.9% of total body weight (TBW), and one third of subjects lost ≥ 20% of TBW.17 Tirzepatide combines GLP-1 RA and a gastric inhibitory polypeptide (GIP) receptor agonist, which also has an incretin effect and functions to slow gastric emptying. In the pivotal SURMOUNT trial, approximately 58% of patients achieved ≥20% loss of TBW18 with 15mg weekly dosing of tirzepatide. This class of drugs is a logical choice in patients with T2DM and obesity. Long-term treatment appears necessary, as patients typically regain two-thirds of lost weight within a year after GLP-1 RA are stopped.
Based on tumors observed in rodents, GLP-1 RA are contraindicated in patients with a personal or family history of multiple endocrine neoplasia type 2 (MEN II) or medullary thyroid cancer. These tumors have not been observed in humans treated with GLP-1 RA. They should be used with caution in patients with history of pancreatitis, gastroparesis, or diabetic retinopathy, though a recent systematic review and meta-analysis suggests showed little to no increased risk for biliary events from GLP-1 RA.19 Side effects are most commonly gastrointestinal in nature (nausea, reflux, constipation or diarrhea) and are typically most severe with initiation of the drug and with dose escalation. Side effects can be mitigated by initiating these drugs at lowest doses and gradually titrating up (every four weeks) based on effectiveness and tolerability. Antisecretory, antiemetic, and laxative medications can also be used to help manage GLP-1 RA related side effects.
There is no reason to escalate to highest doses if patients are experiencing weight loss and reduction in food cravings at lower doses. Both semaglutide and tirzepatide are administered subcutaneously every seven days. Once patients have reached goal weight, they can either continue maintenance therapy at that same dose/interval, or if motivated to do so, may gradually reduce the weekly dose in a stepwise approach to determine the minimally effective dose to maintain weight loss. There are not yet published maintenance studies to guide this process. Currently the price of GLP-1 RA and inconsistent insurance coverage make them inaccessible to many patients. The manufacturers of both semaglutide and tirzepatide offer direct to consumer pricing and home delivery.
Bariatric Surgery
In patients with higher BMI (≥35kg/m2) or those with BMI ≥30kg/m2 and obesity-related metabolic disease and the desire to avoid lifelong medications or who fail or are intolerant of AOM, bariatric options should be considered.20 Sleeve gastrectomy has become the most performed surgery for treatment of obesity. It is a restrictive procedure, removing 80% of the stomach, but a drop in circulating levels of ghrelin afterwards also leads to decreased feelings of hunger. It results in weight loss of 25-30% TBW loss. It is not a good choice for patients who suffer from severe GERD, as this typically worsens afterwards; furthermore, de novo Barrett’s has been observed in nearly 6% of patients who undergo sleeve gastrectomy.21
Roux-en-Y gastric bypass is a restrictive and malabsorptive procedure, resulting in 30-35% TBW loss. It has beneficial and immediate metabolic effects, including increased release of endogenous GLP-1, which leads to improvements in weight-related T2DM. The newer single anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) starts with a sleeve gastrectomy, making a smaller tube-shaped stomach. The duodenum is divided just after the stomach and then a loop of ileum is brought up and connected to the stomach (see Figure 1). This procedure is highly effective, with patients losing 75-95% of excess body weight and is becoming a preferred option for patients with greater BMI (≥50kg/m2). It is also an option for patients who have already had a sleeve gastrectomy and are seeking further weight loss. Because there is only one anastomosis, perioperative complications, such as anastomotic leaks, are reduced. The risk of micronutrient deficiencies is present with all malabsorptive procedures, and these patients must supplement with multivitamins, iron, vitamin D, and calcium.
Endoscopic Therapies
Endoscopic bariatric and metabolic therapies (EBMTs) have been increasingly studied and utilized, and this less invasive option may be more appropriate for or attractive to many patients. Intragastric balloons, which reduce meal volume and delay gastric emptying, can be used short term only (six months) resulting in loss of about 6.9% of total body weight (TBW) greater than lifestyle modification (LM) alone, and may be considered in limited situations, such as need for pre-operative weight loss to reduce risks in very obese individuals.22
Endoscopic gastric remodeling (EGR), also known as endoscopic sleeve gastrectomy (ESG), is a purely restrictive procedure in which the stomach is cinched to resize and reshape using an endoscopic suturing device (see Figure 2).23 It is an option for patients with class 1 or 2 obesity, with data from a randomized controlled trial in this population demonstrating mean percentage of TBW loss of 13.6% at 52 weeks compared to 0.8% in those treated with LM alone.24 A recent meta-analysis of 21 observational studies, including patients with higher BMIs (32.5 to 49.9 kg/m2) showed pooled average weight loss of 17.3% TBW at 12 months with EGR.22 This procedure has potential advantages of fewer complications, quicker recovery, and much less new-onset GERD compared to laparoscopic sleeve gastrectomy. Furthermore, it may be utilized in combination with AOMs to achieve optimum weight loss and metabolic outcomes.25,26 Potential adverse events include abdominal pain, nausea and vomiting (which may be severe), as well as rare instances of intra/extra luminal bleeding or abdominal abscess requiring drainage.22
Recent joint American/European Gastrointestinal Endoscopy guidelines suggest the use of EBMTs plus lifestyle modification in patients with a BMI of ≥ 30 kg/m2, or with a BMI of 27.0-29.9 kg/m2 with at least 1 obesity-related comorbidity.22 Small bowel interventions including duodenal-jejunal bypass liner and duodenal mucosal resurfacing are being investigated for patients with obesity and type 2 diabetes but not yet commercially available.
Conclusion
Given the overlap of obesity with many GI disorders, it is entirely appropriate for gastroenterologists to consider it worthy of aggressive treatment, particularly in patients with MAFLD and other serious weight related comorbidities. With a compassionate and empathetic approach, and a number of highly effective medical, endoscopic, and surgical therapies now available, weight management has the potential to be extremely rewarding when implemented in GI practice.
Dr. Kelly is based in the Department of Medicine, Division of Gastroenterology, Brigham and Women’s Hospital, and Harvard Medical School, both in Boston, Massachusetts. She serves on the clinical advisory board for OpenBiome (unpaid) and has served on an advisory board for Eli Lilly and Company.
References
1. Hales CM, et al. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS Data Brief 2020 Feb:(360):1–8.
2. Pais R, et al. NAFLD and liver transplantation: Current burden and expected challenges. J Hepatol. 2016 Dec. doi: 10.1016/j.jhep.2016.07.033.
3. Lauby-Secretan B, et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med. 2016 Aug. doi: 10.1056/NEJMsr1606602.
4. Kim A. Dysbiosis: A Review Highlighting Obesity and Inflammatory Bowel Disease. J Clin Gastroenterol. 2015 Nov-Dec. doi: 10.1097/MCG.0000000000000356.
5. Singh S, et al. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017 Feb. doi: 10.1038/nrgastro.2016.181.
6. Sundararaman L, Goudra B. Sedation for GI Endoscopy in the Morbidly Obese: Challenges and Possible Solutions. J Clin Med. 2024 Aug. doi: 10.3390/jcm13164635.
7. Bombassaro B, et al. The hypothalamus as the central regulator of energy balance and its impact on current and future obesity treatments. Arch Endocrinol Metab. 2024 Nov. doi: 10.20945/2359-4292-2024-0082.
8. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011 Jul. doi: 10.1097/MCO.0b013e3283479109.
9. Desalermos A, et al. Effect of Obesogenic Medications on Weight-Loss Outcomes in a Behavioral Weight-Management Program. Obesity (Silver Spring). 2019 May. doi: 10.1002/oby.22444.
10. Lord MN, Noble EE. Hypothalamic cannabinoid signaling: Consequences for eating behavior. Pharmacol Res Perspect. 2024 Oct. doi: 10.1002/prp2.1251.
11. Farhana A, Rehman A. Metabolic Consequences of Weight Reduction. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572145/.
12. Rubino F, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025 Mar. doi: 10.1016/S2213-8587(24)00316-4.
13. Cox CE. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017 Aug. doi: 10.2337/ds17-0013.
14. Chaput JP, et al. Widespread misconceptions about obesity. Can Fam Physician. 2014 Nov. PMID: 25392431.
15. Muscogiuri G, et al. Mediterranean Diet and Obesity-related Disorders: What is the Evidence? Curr Obes Rep. 2022 Dec. doi: 10.1007/s13679-022-00481-1.
16. Gudzune KA, Kushner RF. Medications for Obesity: A Review. JAMA. 2024 Aug. doi: 10.1001/jama.2024.10816.
17. Wilding JPH, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Feb. doi: 10.1056/NEJMoa2032183.
18. Jastreboff AM, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jun. doi: 10.1056/NEJMoa2206038.
19. Chiang CH, et al. Glucagon-Like Peptide-1 Receptor Agonists and Gastrointestinal Adverse Events: A Systematic Review and Meta-Analysis. Gastroenterology. 2025 Nov. doi: 10.1053/j.gastro.2025.06.003.
20. Aderinto N, et al. Recent advances in bariatric surgery: a narrative review of weight loss procedures. Ann Med Surg (Lond). 2023 Nov. doi: 10.1097/MS9.0000000000001472.
21. Chandan S, et al. Risk of De Novo Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis of Studies With Long-Term Follow-Up. Clin Gastroenterol Hepatol. 2025 Jan. doi: 10.1016/j.cgh.2024.06.041.
22. Jirapinyo P, et al. American Society for Gastrointestinal Endoscopy-European Society of Gastrointestinal Endoscopy guideline on primary endoscopic bariatric and metabolic therapies for adults with obesity. Gastrointest Endosc. 2024 Jun. doi: 10.1016/j.gie.2023.12.004.
23. Nduma BN, et al. Endoscopic Gastric Sleeve: A Review of Literature. Cureus. 2023 Mar. doi: 10.7759/cureus.36353.
24. Abu Dayyeh BK, et al. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet. 2022 Aug. doi: 10.1016/S0140-6736(22)01280-6.
25. Gala K, et al. Outcomes of concomitant antiobesity medication use with endoscopic sleeve gastroplasty in clinical US settings. Obes Pillars. 2024 May. doi: 10.1016/j.obpill.2024.100112.
26. Chung CS, et al. Endoscopic sleeve gastroplasty combined with anti-obesity medication for better control of weight and diabetes. Clin Endosc. 2025 May. doi: 10.5946/ce.2024.274.
Why Your Support Matters Now
Federal research funding is uncertain, but discovery can’t wait.
As an AGA member, you can help the AGA Research Foundation ensure that critical digestive health research continues, regardless of the circumstances. With your donation, you will help fuel the next breakthroughs in digestive health by backing bold ideas and early-career investigators when federal dollars fall short.
By donating today, you become a vital part of the solution, helping to provide the necessary funding to foster scientific discovery and enhance patient care for those affected by digestive diseases.
Your support will transform lives and accelerate medical breakthroughs.
Donate by December 31 to receive a tax-credit in 2025. Make your gift by visiting www.foundation.gastro.org.
Federal research funding is uncertain, but discovery can’t wait.
As an AGA member, you can help the AGA Research Foundation ensure that critical digestive health research continues, regardless of the circumstances. With your donation, you will help fuel the next breakthroughs in digestive health by backing bold ideas and early-career investigators when federal dollars fall short.
By donating today, you become a vital part of the solution, helping to provide the necessary funding to foster scientific discovery and enhance patient care for those affected by digestive diseases.
Your support will transform lives and accelerate medical breakthroughs.
Donate by December 31 to receive a tax-credit in 2025. Make your gift by visiting www.foundation.gastro.org.
Federal research funding is uncertain, but discovery can’t wait.
As an AGA member, you can help the AGA Research Foundation ensure that critical digestive health research continues, regardless of the circumstances. With your donation, you will help fuel the next breakthroughs in digestive health by backing bold ideas and early-career investigators when federal dollars fall short.
By donating today, you become a vital part of the solution, helping to provide the necessary funding to foster scientific discovery and enhance patient care for those affected by digestive diseases.
Your support will transform lives and accelerate medical breakthroughs.
Donate by December 31 to receive a tax-credit in 2025. Make your gift by visiting www.foundation.gastro.org.
Resmetirom Reduces Liver Stiffness in MASH Cirrhosis
PHOENIX — according to the results of a new study.
As well as showing sustained reduction in liver stiffness on vibration-controlled transient elastography (VCTE) after 2 years of treatment with resmetirom, the study suggested that up to 35% of patients could “potentially reverse their cirrhosis,” said lead author Naim Alkhouri, MD, chief medical officer and director of the steatotic liver program at Arizona Liver Health in Phoenix.
Alkhouri presented data on patients with compensated cirrhosis from a 1-year open-label extension of the already-completed MAESTRO-NAFLD-1 study at American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
The FDA approved resmetirom (Rezdiffra, Madrigal Pharmaceuticals) in 2024 for MASH and moderate-to-advanced liver fibrosis (consistent with stage F2 and F3 disease), to be used in conjunction with diet and exercise. The agency granted the once-daily, oral thyroid hormone receptor beta-selective agonist breakthrough therapy designation and priority review.
According to the American Liver Foundation, about 5% of adults in the US have MASH — one of the leading causes of liver transplantation in the country. There is currently no FDA-approved therapy for compensated cirrhosis caused by MASH, said Alkhouri. Patients with MASH cirrhosis with clinically significant portal hypertension (CSPH) experience major adverse liver outcomes.
In an analysis of 122 patients with Child Pugh A MASH cirrhosis who completed both a year in an open-label arm of MAESTRO-NAFLD-1 and a 1-year extension, 113 (93%) completed 2 years of treatment with resmetirom (80 mg). Of the 122 patients, only 114 received MRI proton density fat fraction (MRI-PDFF) testing — 93 (82%) had a baseline of > 5% indicating cirrhosis, while 21 (18%) had an MRI-PDFF of < 5%.
Patients were assessed for baseline portal hypertension (Baveno VII) with FibroScan VCTE and platelet count, which was confirmed using magnetic resonance elastography (MRE). Noninvasive biomarkers and imaging were analyzed at baseline and out to 2 years.
At baseline, 63% of patients were categorized as probable/definitive CSPH (Baveno VII). At 1 year of treatment with resmetirom, 20% of patients who were CSPH positive no longer met the criteria, and at 2 years this number had increased to 28%.
After 2 years of treatment, more than half of the patients had a sustained reduction in liver stiffness of more than 25%, as measured by VCTE; and 35% of patients with confirmed F4 at baseline (liver biopsy F4 and/or platelets < 140/MRE ≥ 5 with VCTE ≥ 15) had a conversion to F3.
Patients taking resmetirom also had significant improvements in MRI-PDFF and MRE at 2 years. Almost a third of those with a baseline MRI-PDFF > 5% improved, while 43% of those with a baseline of < 5% improved.
Although 113 patients had an adverse event — primarily gastrointestinal — the observed events were consistent with previous studies. Twenty-seven patients had a serious adverse event, but none were related to the study drug, said Alkhouri. The researchers reported that only 8% of patients discontinued the medication.
Changing the Treatment Landscape for MASH-Related Cirrhosis
When asked to comment by GI & Hepatology News, Hazem Ayesh, MD, an endocrinologist at Deaconess Health System, Evansville, Indiana, said that “reversal of cirrhosis from F4 to F3 and reduction of portal hypertension are quite surprising, since cirrhosis typically progresses slowly.”
Ayesh said it was notable that the researchers had used imaging to confirm both functional and hemodynamic improvements in liver architecture not just biochemical changes. Given the results, “clinicians may reasonably consider off-label use in selected compensated patients until more outcome data become available,” he said.
A phase 3 study is underway to examine those outcomes, MAESTRO-NASH OUTCOMES, with 845 patients with MASH cirrhosis, and should be completed in 2027.
“Resmetirom could change the treatment landscape for MASH-related cirrhosis,” said Ayesh, adding, “this drug offers a chance to target the disease process itself,” while other therapies focus on preventing complications.
“For patients without access to liver transplant, a therapy that can slow or reverse disease progression could be transformative,” he told GI & Hepatology News.
Alkhouri disclosed that he is a consultant and speaker for Madrigal Pharmaceuticals. Three coauthors are Madrigal employees and own stock options in the company. Two coauthors are Madrigal consultants and advisers. Ayesh reported no conflicts.
A version of this article appeared on Medscape.com.
PHOENIX — according to the results of a new study.
As well as showing sustained reduction in liver stiffness on vibration-controlled transient elastography (VCTE) after 2 years of treatment with resmetirom, the study suggested that up to 35% of patients could “potentially reverse their cirrhosis,” said lead author Naim Alkhouri, MD, chief medical officer and director of the steatotic liver program at Arizona Liver Health in Phoenix.
Alkhouri presented data on patients with compensated cirrhosis from a 1-year open-label extension of the already-completed MAESTRO-NAFLD-1 study at American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
The FDA approved resmetirom (Rezdiffra, Madrigal Pharmaceuticals) in 2024 for MASH and moderate-to-advanced liver fibrosis (consistent with stage F2 and F3 disease), to be used in conjunction with diet and exercise. The agency granted the once-daily, oral thyroid hormone receptor beta-selective agonist breakthrough therapy designation and priority review.
According to the American Liver Foundation, about 5% of adults in the US have MASH — one of the leading causes of liver transplantation in the country. There is currently no FDA-approved therapy for compensated cirrhosis caused by MASH, said Alkhouri. Patients with MASH cirrhosis with clinically significant portal hypertension (CSPH) experience major adverse liver outcomes.
In an analysis of 122 patients with Child Pugh A MASH cirrhosis who completed both a year in an open-label arm of MAESTRO-NAFLD-1 and a 1-year extension, 113 (93%) completed 2 years of treatment with resmetirom (80 mg). Of the 122 patients, only 114 received MRI proton density fat fraction (MRI-PDFF) testing — 93 (82%) had a baseline of > 5% indicating cirrhosis, while 21 (18%) had an MRI-PDFF of < 5%.
Patients were assessed for baseline portal hypertension (Baveno VII) with FibroScan VCTE and platelet count, which was confirmed using magnetic resonance elastography (MRE). Noninvasive biomarkers and imaging were analyzed at baseline and out to 2 years.
At baseline, 63% of patients were categorized as probable/definitive CSPH (Baveno VII). At 1 year of treatment with resmetirom, 20% of patients who were CSPH positive no longer met the criteria, and at 2 years this number had increased to 28%.
After 2 years of treatment, more than half of the patients had a sustained reduction in liver stiffness of more than 25%, as measured by VCTE; and 35% of patients with confirmed F4 at baseline (liver biopsy F4 and/or platelets < 140/MRE ≥ 5 with VCTE ≥ 15) had a conversion to F3.
Patients taking resmetirom also had significant improvements in MRI-PDFF and MRE at 2 years. Almost a third of those with a baseline MRI-PDFF > 5% improved, while 43% of those with a baseline of < 5% improved.
Although 113 patients had an adverse event — primarily gastrointestinal — the observed events were consistent with previous studies. Twenty-seven patients had a serious adverse event, but none were related to the study drug, said Alkhouri. The researchers reported that only 8% of patients discontinued the medication.
Changing the Treatment Landscape for MASH-Related Cirrhosis
When asked to comment by GI & Hepatology News, Hazem Ayesh, MD, an endocrinologist at Deaconess Health System, Evansville, Indiana, said that “reversal of cirrhosis from F4 to F3 and reduction of portal hypertension are quite surprising, since cirrhosis typically progresses slowly.”
Ayesh said it was notable that the researchers had used imaging to confirm both functional and hemodynamic improvements in liver architecture not just biochemical changes. Given the results, “clinicians may reasonably consider off-label use in selected compensated patients until more outcome data become available,” he said.
A phase 3 study is underway to examine those outcomes, MAESTRO-NASH OUTCOMES, with 845 patients with MASH cirrhosis, and should be completed in 2027.
“Resmetirom could change the treatment landscape for MASH-related cirrhosis,” said Ayesh, adding, “this drug offers a chance to target the disease process itself,” while other therapies focus on preventing complications.
“For patients without access to liver transplant, a therapy that can slow or reverse disease progression could be transformative,” he told GI & Hepatology News.
Alkhouri disclosed that he is a consultant and speaker for Madrigal Pharmaceuticals. Three coauthors are Madrigal employees and own stock options in the company. Two coauthors are Madrigal consultants and advisers. Ayesh reported no conflicts.
A version of this article appeared on Medscape.com.
PHOENIX — according to the results of a new study.
As well as showing sustained reduction in liver stiffness on vibration-controlled transient elastography (VCTE) after 2 years of treatment with resmetirom, the study suggested that up to 35% of patients could “potentially reverse their cirrhosis,” said lead author Naim Alkhouri, MD, chief medical officer and director of the steatotic liver program at Arizona Liver Health in Phoenix.
Alkhouri presented data on patients with compensated cirrhosis from a 1-year open-label extension of the already-completed MAESTRO-NAFLD-1 study at American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
The FDA approved resmetirom (Rezdiffra, Madrigal Pharmaceuticals) in 2024 for MASH and moderate-to-advanced liver fibrosis (consistent with stage F2 and F3 disease), to be used in conjunction with diet and exercise. The agency granted the once-daily, oral thyroid hormone receptor beta-selective agonist breakthrough therapy designation and priority review.
According to the American Liver Foundation, about 5% of adults in the US have MASH — one of the leading causes of liver transplantation in the country. There is currently no FDA-approved therapy for compensated cirrhosis caused by MASH, said Alkhouri. Patients with MASH cirrhosis with clinically significant portal hypertension (CSPH) experience major adverse liver outcomes.
In an analysis of 122 patients with Child Pugh A MASH cirrhosis who completed both a year in an open-label arm of MAESTRO-NAFLD-1 and a 1-year extension, 113 (93%) completed 2 years of treatment with resmetirom (80 mg). Of the 122 patients, only 114 received MRI proton density fat fraction (MRI-PDFF) testing — 93 (82%) had a baseline of > 5% indicating cirrhosis, while 21 (18%) had an MRI-PDFF of < 5%.
Patients were assessed for baseline portal hypertension (Baveno VII) with FibroScan VCTE and platelet count, which was confirmed using magnetic resonance elastography (MRE). Noninvasive biomarkers and imaging were analyzed at baseline and out to 2 years.
At baseline, 63% of patients were categorized as probable/definitive CSPH (Baveno VII). At 1 year of treatment with resmetirom, 20% of patients who were CSPH positive no longer met the criteria, and at 2 years this number had increased to 28%.
After 2 years of treatment, more than half of the patients had a sustained reduction in liver stiffness of more than 25%, as measured by VCTE; and 35% of patients with confirmed F4 at baseline (liver biopsy F4 and/or platelets < 140/MRE ≥ 5 with VCTE ≥ 15) had a conversion to F3.
Patients taking resmetirom also had significant improvements in MRI-PDFF and MRE at 2 years. Almost a third of those with a baseline MRI-PDFF > 5% improved, while 43% of those with a baseline of < 5% improved.
Although 113 patients had an adverse event — primarily gastrointestinal — the observed events were consistent with previous studies. Twenty-seven patients had a serious adverse event, but none were related to the study drug, said Alkhouri. The researchers reported that only 8% of patients discontinued the medication.
Changing the Treatment Landscape for MASH-Related Cirrhosis
When asked to comment by GI & Hepatology News, Hazem Ayesh, MD, an endocrinologist at Deaconess Health System, Evansville, Indiana, said that “reversal of cirrhosis from F4 to F3 and reduction of portal hypertension are quite surprising, since cirrhosis typically progresses slowly.”
Ayesh said it was notable that the researchers had used imaging to confirm both functional and hemodynamic improvements in liver architecture not just biochemical changes. Given the results, “clinicians may reasonably consider off-label use in selected compensated patients until more outcome data become available,” he said.
A phase 3 study is underway to examine those outcomes, MAESTRO-NASH OUTCOMES, with 845 patients with MASH cirrhosis, and should be completed in 2027.
“Resmetirom could change the treatment landscape for MASH-related cirrhosis,” said Ayesh, adding, “this drug offers a chance to target the disease process itself,” while other therapies focus on preventing complications.
“For patients without access to liver transplant, a therapy that can slow or reverse disease progression could be transformative,” he told GI & Hepatology News.
Alkhouri disclosed that he is a consultant and speaker for Madrigal Pharmaceuticals. Three coauthors are Madrigal employees and own stock options in the company. Two coauthors are Madrigal consultants and advisers. Ayesh reported no conflicts.
A version of this article appeared on Medscape.com.
FROM ACG 2025
Patients With a Positive FIT Fail to Get Follow-Up Colonoscopies
PHOENIX — Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
“In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy,” said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
“ and colorectal cancer, regardless of polypectomy history,” Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, because of the higher risk.
Reasons patients may instead turn to FIT may include cost or other factors, she said.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2024.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the non-polypectomy group).
Among the FIT screenings, results were positive in 17.2% of post-polypectomy patients and 14.1% of patients with no prior polypectomy, indicating a history of polypectomy to be predictive of a positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result — and having a previous polypectomy should add further urgency to the matter — the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the non-polypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the post-colonoscopy interval FIT.
The findings underscore that “positive results carried a high risk of advanced neoplasia or cancer, irrespective of prior polypectomy history,” Wilson said.
Clinicians Must ‘Do a Better Job’
Commenting on the study, William D. Chey, MD, AGAF, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, noted that the study “addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy.”
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
“Other data suggests that the rate might even be significantly higher — at 70%-80%, depending upon the population and the test,” Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies “should raise questions about whether there might be a role for FIT testing in addition to colonoscopy.” However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is “how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy,” he said.
“I think a lot of this is going to come down to how it’s done at the primary care level.”
Chey added that in that, and any other setting, “the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it’s positive, a follow-up colonoscopy must be performed.”
“Otherwise, the stool-based test is of no value.”
Wilson had no disclosures to report. Chey’s disclosures included consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestlé, Phathom, Redhill, Salix/Valeant, Takeda, and Vibrant.
A version of this article appeared on Medscape.com .
PHOENIX — Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
“In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy,” said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
“ and colorectal cancer, regardless of polypectomy history,” Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, because of the higher risk.
Reasons patients may instead turn to FIT may include cost or other factors, she said.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2024.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the non-polypectomy group).
Among the FIT screenings, results were positive in 17.2% of post-polypectomy patients and 14.1% of patients with no prior polypectomy, indicating a history of polypectomy to be predictive of a positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result — and having a previous polypectomy should add further urgency to the matter — the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the non-polypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the post-colonoscopy interval FIT.
The findings underscore that “positive results carried a high risk of advanced neoplasia or cancer, irrespective of prior polypectomy history,” Wilson said.
Clinicians Must ‘Do a Better Job’
Commenting on the study, William D. Chey, MD, AGAF, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, noted that the study “addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy.”
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
“Other data suggests that the rate might even be significantly higher — at 70%-80%, depending upon the population and the test,” Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies “should raise questions about whether there might be a role for FIT testing in addition to colonoscopy.” However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is “how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy,” he said.
“I think a lot of this is going to come down to how it’s done at the primary care level.”
Chey added that in that, and any other setting, “the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it’s positive, a follow-up colonoscopy must be performed.”
“Otherwise, the stool-based test is of no value.”
Wilson had no disclosures to report. Chey’s disclosures included consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestlé, Phathom, Redhill, Salix/Valeant, Takeda, and Vibrant.
A version of this article appeared on Medscape.com .
PHOENIX — Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
“In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy,” said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
“ and colorectal cancer, regardless of polypectomy history,” Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, because of the higher risk.
Reasons patients may instead turn to FIT may include cost or other factors, she said.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2024.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the non-polypectomy group).
Among the FIT screenings, results were positive in 17.2% of post-polypectomy patients and 14.1% of patients with no prior polypectomy, indicating a history of polypectomy to be predictive of a positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result — and having a previous polypectomy should add further urgency to the matter — the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the non-polypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the post-colonoscopy interval FIT.
The findings underscore that “positive results carried a high risk of advanced neoplasia or cancer, irrespective of prior polypectomy history,” Wilson said.
Clinicians Must ‘Do a Better Job’
Commenting on the study, William D. Chey, MD, AGAF, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, noted that the study “addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy.”
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
“Other data suggests that the rate might even be significantly higher — at 70%-80%, depending upon the population and the test,” Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies “should raise questions about whether there might be a role for FIT testing in addition to colonoscopy.” However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is “how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy,” he said.
“I think a lot of this is going to come down to how it’s done at the primary care level.”
Chey added that in that, and any other setting, “the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it’s positive, a follow-up colonoscopy must be performed.”
“Otherwise, the stool-based test is of no value.”
Wilson had no disclosures to report. Chey’s disclosures included consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestlé, Phathom, Redhill, Salix/Valeant, Takeda, and Vibrant.
A version of this article appeared on Medscape.com .
FROM ACG 2025
Needle-Knife Fistulotomy is Safe During ERCP, Even for Trainees
, based on results of a randomized trial.
Across procedures conducted predominantly by trainees, safety outcomes were similar between NKF and standard cannulation, and all patients were successfully cannulated, suggesting this is a broadly accessible technique, reported lead author Aleksey Novikov, MD, of the University of Florida College of Medicine, Gainesville, and colleagues, reported.
Writing in Techniques and Innovations in Gastrointestinal Endoscopy, the investigators noted that standard cannulation fails in 5-20% of cases, which has led to development of various alternative techniques, including NKF. To perform the technique, the endoscopist makes a small incision in the intraduodenal biliary segment 3-6mm above the papillary orifice, with cephalad extension until bili-ary access is achieved.
To date, four prospective studies have evaluated NKF in the hands of expert advanced endoscopists.
“These studies showed that NKF is a safe and useful technique that significantly reduces the risk of PEP in the hands of expert advanced endoscopists,” the investigators wrote. ‘The suggestion that NKF should be restricted to expert advanced endoscopists likely limits widespread use.”
To determine whether NKF is a suitable technique for less experienced endoscopists, the investigators conducted the present single-center, prospective randomized controlled trial at Thomas Jefferson University Hospital in Philadelphia.
Adults undergoing ERCP for biliary indications were randomly assigned in a 1:1 ratio to undergo primary cannulation via NKF or standard cannulation. Patients with prior sphincterotomy, ampullectomy, or unfavorable anatomy were excluded.
A total of 186 patients were randomized, with 137 ultimately included in the per-protocol analysis after exclusions for anatomic factors. Most procedures (72.3%) were performed by advanced endoscopy trainees under direct supervision, 26 procedures (19.0%) were performed by attending endoscopists without substantive prior NKF experience, and 12 (8.8%) by an attending endoscopist with NKF expertise.
“It is important to note that the majority of procedures performed in the context of this study were performed by an advanced endoscopy trainee with no NKF experience or an attending advanced endoscopist with minimal NKF experience,” the investigators wrote.
All patients received prophylactic rectal indomethacin, and cannulation attempts were capped at 20 minutes before crossover to another technique was permitted.
The primary endpoint was incidence of post-ERCP pancreatitis. Secondary endpoints included successful biliary access, time to access, and rates of bleeding and perforation.
Post-ERCP pancreatitis occurred at similar rate across groups: 6 cases (8.2%) in the standard cannulation arm and 5 cases (7.8%) in the NKF arm (P = .93). Rates of bleeding and perforation were also similar for both techniques.
Within the initial 20-minute window, biliary access rates were comparable between groups, at 75.3% and 82.2% for standard cannulation and NKF, respectively (P = .89). Allowing additional attempts or crossover, overall success rose to 100% in both arms.
Mean time to access was longer with NKF, averaging 380 seconds compared with 268 seconds for standard cannulation (P less than .05).
“NKF was essentially equivalent to standard cannulation in many aspects,” the investigators wrote, calling the two techniques “complementary.”
They also suggested that the relative equivalence between techniques “carries more weight” after considering the low level of NKF experience among participating endoscopists.
“Overall, our data support teaching advanced endoscopy trainees NKF as a primary method of biliary access in patients with favorable anatomy,” the investigators concluded.
The investigators disclosed relationships with Medtronic, Boston Scientific, and Olympus.
, based on results of a randomized trial.
Across procedures conducted predominantly by trainees, safety outcomes were similar between NKF and standard cannulation, and all patients were successfully cannulated, suggesting this is a broadly accessible technique, reported lead author Aleksey Novikov, MD, of the University of Florida College of Medicine, Gainesville, and colleagues, reported.
Writing in Techniques and Innovations in Gastrointestinal Endoscopy, the investigators noted that standard cannulation fails in 5-20% of cases, which has led to development of various alternative techniques, including NKF. To perform the technique, the endoscopist makes a small incision in the intraduodenal biliary segment 3-6mm above the papillary orifice, with cephalad extension until bili-ary access is achieved.
To date, four prospective studies have evaluated NKF in the hands of expert advanced endoscopists.
“These studies showed that NKF is a safe and useful technique that significantly reduces the risk of PEP in the hands of expert advanced endoscopists,” the investigators wrote. ‘The suggestion that NKF should be restricted to expert advanced endoscopists likely limits widespread use.”
To determine whether NKF is a suitable technique for less experienced endoscopists, the investigators conducted the present single-center, prospective randomized controlled trial at Thomas Jefferson University Hospital in Philadelphia.
Adults undergoing ERCP for biliary indications were randomly assigned in a 1:1 ratio to undergo primary cannulation via NKF or standard cannulation. Patients with prior sphincterotomy, ampullectomy, or unfavorable anatomy were excluded.
A total of 186 patients were randomized, with 137 ultimately included in the per-protocol analysis after exclusions for anatomic factors. Most procedures (72.3%) were performed by advanced endoscopy trainees under direct supervision, 26 procedures (19.0%) were performed by attending endoscopists without substantive prior NKF experience, and 12 (8.8%) by an attending endoscopist with NKF expertise.
“It is important to note that the majority of procedures performed in the context of this study were performed by an advanced endoscopy trainee with no NKF experience or an attending advanced endoscopist with minimal NKF experience,” the investigators wrote.
All patients received prophylactic rectal indomethacin, and cannulation attempts were capped at 20 minutes before crossover to another technique was permitted.
The primary endpoint was incidence of post-ERCP pancreatitis. Secondary endpoints included successful biliary access, time to access, and rates of bleeding and perforation.
Post-ERCP pancreatitis occurred at similar rate across groups: 6 cases (8.2%) in the standard cannulation arm and 5 cases (7.8%) in the NKF arm (P = .93). Rates of bleeding and perforation were also similar for both techniques.
Within the initial 20-minute window, biliary access rates were comparable between groups, at 75.3% and 82.2% for standard cannulation and NKF, respectively (P = .89). Allowing additional attempts or crossover, overall success rose to 100% in both arms.
Mean time to access was longer with NKF, averaging 380 seconds compared with 268 seconds for standard cannulation (P less than .05).
“NKF was essentially equivalent to standard cannulation in many aspects,” the investigators wrote, calling the two techniques “complementary.”
They also suggested that the relative equivalence between techniques “carries more weight” after considering the low level of NKF experience among participating endoscopists.
“Overall, our data support teaching advanced endoscopy trainees NKF as a primary method of biliary access in patients with favorable anatomy,” the investigators concluded.
The investigators disclosed relationships with Medtronic, Boston Scientific, and Olympus.
, based on results of a randomized trial.
Across procedures conducted predominantly by trainees, safety outcomes were similar between NKF and standard cannulation, and all patients were successfully cannulated, suggesting this is a broadly accessible technique, reported lead author Aleksey Novikov, MD, of the University of Florida College of Medicine, Gainesville, and colleagues, reported.
Writing in Techniques and Innovations in Gastrointestinal Endoscopy, the investigators noted that standard cannulation fails in 5-20% of cases, which has led to development of various alternative techniques, including NKF. To perform the technique, the endoscopist makes a small incision in the intraduodenal biliary segment 3-6mm above the papillary orifice, with cephalad extension until bili-ary access is achieved.
To date, four prospective studies have evaluated NKF in the hands of expert advanced endoscopists.
“These studies showed that NKF is a safe and useful technique that significantly reduces the risk of PEP in the hands of expert advanced endoscopists,” the investigators wrote. ‘The suggestion that NKF should be restricted to expert advanced endoscopists likely limits widespread use.”
To determine whether NKF is a suitable technique for less experienced endoscopists, the investigators conducted the present single-center, prospective randomized controlled trial at Thomas Jefferson University Hospital in Philadelphia.
Adults undergoing ERCP for biliary indications were randomly assigned in a 1:1 ratio to undergo primary cannulation via NKF or standard cannulation. Patients with prior sphincterotomy, ampullectomy, or unfavorable anatomy were excluded.
A total of 186 patients were randomized, with 137 ultimately included in the per-protocol analysis after exclusions for anatomic factors. Most procedures (72.3%) were performed by advanced endoscopy trainees under direct supervision, 26 procedures (19.0%) were performed by attending endoscopists without substantive prior NKF experience, and 12 (8.8%) by an attending endoscopist with NKF expertise.
“It is important to note that the majority of procedures performed in the context of this study were performed by an advanced endoscopy trainee with no NKF experience or an attending advanced endoscopist with minimal NKF experience,” the investigators wrote.
All patients received prophylactic rectal indomethacin, and cannulation attempts were capped at 20 minutes before crossover to another technique was permitted.
The primary endpoint was incidence of post-ERCP pancreatitis. Secondary endpoints included successful biliary access, time to access, and rates of bleeding and perforation.
Post-ERCP pancreatitis occurred at similar rate across groups: 6 cases (8.2%) in the standard cannulation arm and 5 cases (7.8%) in the NKF arm (P = .93). Rates of bleeding and perforation were also similar for both techniques.
Within the initial 20-minute window, biliary access rates were comparable between groups, at 75.3% and 82.2% for standard cannulation and NKF, respectively (P = .89). Allowing additional attempts or crossover, overall success rose to 100% in both arms.
Mean time to access was longer with NKF, averaging 380 seconds compared with 268 seconds for standard cannulation (P less than .05).
“NKF was essentially equivalent to standard cannulation in many aspects,” the investigators wrote, calling the two techniques “complementary.”
They also suggested that the relative equivalence between techniques “carries more weight” after considering the low level of NKF experience among participating endoscopists.
“Overall, our data support teaching advanced endoscopy trainees NKF as a primary method of biliary access in patients with favorable anatomy,” the investigators concluded.
The investigators disclosed relationships with Medtronic, Boston Scientific, and Olympus.
FROM TECHNIQUES AND INNOVATIONS IN GASTROINTESTINAL ENDOSCOPY
VA Performs Its First ‘Bloodless’ Stem Cell Transplant
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
Head and Neck Cancer: VA Dietitian Advocates Whole Foods Over Supplements
PHOENIX — Patients with head and neck cancer face high rates of malnutrition during treatment, and oral supplements are often recommended. But they are not the entire answer, a dietician told colleagues at the Association of Veterans Affairs (VA) Hematology/Oncology annual meeting.
“Patients should consume the most liberal diet possible throughout treatment,” said advanced practice oncology dietician Brittany Leneweaver, RD, CSO, CES, at the VA Washington DC Healthcare System. “This means not solely relying on oral nutrition supplements like Ensure if possible.”
While Leneweaver said many patients will need supplements, she stressed these products “are meant to supplement the diet and not be the sole source of nutrition, ideally.” Encouraging the intake of whole foods “is really key to make the transition back to solid foods after they’re done with treatment. This makes it so much easier when they’re already swallowing those thicker textures, rather than just liquid the entire time.”
Malnutrition: Common and Damaging
As Leneweaver noted, malnutrition is common in patients with head and neck cancer, and can lead to “increased treatment toxicity, increased risk of infection, decreased survival, increased surgical complication, delayed healing, decreased physical function, and decreased quality of life.”
Malnutrition data in patients with head and neck cancer in the US is sparse. However, a 2024 study found malnutrition in 20% of patients undergoing head and neck cancer surgery and linked the condition to increased length of stay (β, 5.20 additional days), higher costs (β, $15,722) higher odds of potentially preventable complications (adjusted odds ratio [aOR], 2.04), and lower odds of discharge to home (aOR, 0.34).
Leneweaver said her role involves addressing “nutrition impact symptoms” that reduce veteran food intake such as difficulty swallowing, taste disorders, dry mouth, and inflammation of the mucus membranes.
“I can’t tell you how much time I spend just talking to the patient about their medication regimens, making sure they have antiemetics on board, letting the radiation oncologist know, ‘Hey, it’s probably time for medicine,’” she said. “We’re constantly looking at side effects and addressing to alert the team as quickly as possible so that we can prevent further weight loss.”
Better Diets Lead to Better Outcomes
Leneweaver noted that “many times, patients will continue to rely on oral supplements as their primary source of nutrition over the long term. They may be missing out on several health benefits as a result.”
Research shows that high-quality diets matter in this patient group, she said. They’re associated with “decreased symptoms during treatment, reduced head and neck cancer risk, and reduced risk of those chronic nutrition impact symptoms,” Leneweaver said.
Diets before and after cancer diagnosis can make a difference. A 2019 study examined patient diets prior to diagnosis of head and neck cancer. It found that patients with better diet quality were less likely to experience overall nutrition impact symptoms (OR 0.45). However, “studies have found that the majority of our patients with head and neck cancer have an inadequate diet prior to diagnosis,” Leneweaver said.
As for postdiagnosis nutrition, a 2022 study linked healthier diets in patients with head and neck cancer to 93% lower 3-year risk of all-cause mortality and 85% lower risk of cancer-specific mortality.
What’s in a High-Quality Diet?
Regarding specific food recommendations, Leneweaver prefers the American Institute for Cancer Research (AICR) nutrition guidelines over the US Department of Agriculture’s Dietary Guidelines for Americans. The AICR “more clearly recommends plant-based diet with at least two-thirds of each meal coming from a variety of plant sources” and recommends avoiding alcohol entirely and limiting red meat, she said.
Leneweaver said she recognizes that dietary change can be gradual.
“It’s not going to happen overnight,” she said. “We know that lifestyle change takes a lot of work.”
Basic interventions can be effective, she said: “This can be just as simple as recommending a plant-based diet to your patient or recommending they eat the rainbow. And I don’t mean Skittles, I mean actual plants. If you just mention these couple of things to the patients, this can really go a long way, especially if they’re hearing that consistent messaging.”
Team-Based Follow-Up Is Key
Leneweaver emphasized the importance of following up over time even if patients do not initially accept referrals to nutritional services. Dieticians ideally see patients before or during initial treatment and then weekly during radiation therapy. Posttreatment follow-up continues “until they’re nutritionally stable. This can be anywhere from weekly to monthly.”
Leneweaver emphasized collaborating with other team members. For example, she works with a speech pathologist at joint visits, either weekly or monthly, “so that they can get off of that feeding tube or get back to a solid consistency diet, typically before that 3-month PET scan.”
It is also important to understand barriers to healthy eating in the veteran population, including transportation challenges and poor access to healthy food, Leneweaver said.
“Make sure you’re utilizing your social worker, your psychologist, other resources, and food pantries, if you have them.”
Even when the most ideal choices are not available, she said, “if they only have access to canned vegetables, I’d much rather them eat that than have nothing.”
No disclosures for Leneweaver were provided.
PHOENIX — Patients with head and neck cancer face high rates of malnutrition during treatment, and oral supplements are often recommended. But they are not the entire answer, a dietician told colleagues at the Association of Veterans Affairs (VA) Hematology/Oncology annual meeting.
“Patients should consume the most liberal diet possible throughout treatment,” said advanced practice oncology dietician Brittany Leneweaver, RD, CSO, CES, at the VA Washington DC Healthcare System. “This means not solely relying on oral nutrition supplements like Ensure if possible.”
While Leneweaver said many patients will need supplements, she stressed these products “are meant to supplement the diet and not be the sole source of nutrition, ideally.” Encouraging the intake of whole foods “is really key to make the transition back to solid foods after they’re done with treatment. This makes it so much easier when they’re already swallowing those thicker textures, rather than just liquid the entire time.”
Malnutrition: Common and Damaging
As Leneweaver noted, malnutrition is common in patients with head and neck cancer, and can lead to “increased treatment toxicity, increased risk of infection, decreased survival, increased surgical complication, delayed healing, decreased physical function, and decreased quality of life.”
Malnutrition data in patients with head and neck cancer in the US is sparse. However, a 2024 study found malnutrition in 20% of patients undergoing head and neck cancer surgery and linked the condition to increased length of stay (β, 5.20 additional days), higher costs (β, $15,722) higher odds of potentially preventable complications (adjusted odds ratio [aOR], 2.04), and lower odds of discharge to home (aOR, 0.34).
Leneweaver said her role involves addressing “nutrition impact symptoms” that reduce veteran food intake such as difficulty swallowing, taste disorders, dry mouth, and inflammation of the mucus membranes.
“I can’t tell you how much time I spend just talking to the patient about their medication regimens, making sure they have antiemetics on board, letting the radiation oncologist know, ‘Hey, it’s probably time for medicine,’” she said. “We’re constantly looking at side effects and addressing to alert the team as quickly as possible so that we can prevent further weight loss.”
Better Diets Lead to Better Outcomes
Leneweaver noted that “many times, patients will continue to rely on oral supplements as their primary source of nutrition over the long term. They may be missing out on several health benefits as a result.”
Research shows that high-quality diets matter in this patient group, she said. They’re associated with “decreased symptoms during treatment, reduced head and neck cancer risk, and reduced risk of those chronic nutrition impact symptoms,” Leneweaver said.
Diets before and after cancer diagnosis can make a difference. A 2019 study examined patient diets prior to diagnosis of head and neck cancer. It found that patients with better diet quality were less likely to experience overall nutrition impact symptoms (OR 0.45). However, “studies have found that the majority of our patients with head and neck cancer have an inadequate diet prior to diagnosis,” Leneweaver said.
As for postdiagnosis nutrition, a 2022 study linked healthier diets in patients with head and neck cancer to 93% lower 3-year risk of all-cause mortality and 85% lower risk of cancer-specific mortality.
What’s in a High-Quality Diet?
Regarding specific food recommendations, Leneweaver prefers the American Institute for Cancer Research (AICR) nutrition guidelines over the US Department of Agriculture’s Dietary Guidelines for Americans. The AICR “more clearly recommends plant-based diet with at least two-thirds of each meal coming from a variety of plant sources” and recommends avoiding alcohol entirely and limiting red meat, she said.
Leneweaver said she recognizes that dietary change can be gradual.
“It’s not going to happen overnight,” she said. “We know that lifestyle change takes a lot of work.”
Basic interventions can be effective, she said: “This can be just as simple as recommending a plant-based diet to your patient or recommending they eat the rainbow. And I don’t mean Skittles, I mean actual plants. If you just mention these couple of things to the patients, this can really go a long way, especially if they’re hearing that consistent messaging.”
Team-Based Follow-Up Is Key
Leneweaver emphasized the importance of following up over time even if patients do not initially accept referrals to nutritional services. Dieticians ideally see patients before or during initial treatment and then weekly during radiation therapy. Posttreatment follow-up continues “until they’re nutritionally stable. This can be anywhere from weekly to monthly.”
Leneweaver emphasized collaborating with other team members. For example, she works with a speech pathologist at joint visits, either weekly or monthly, “so that they can get off of that feeding tube or get back to a solid consistency diet, typically before that 3-month PET scan.”
It is also important to understand barriers to healthy eating in the veteran population, including transportation challenges and poor access to healthy food, Leneweaver said.
“Make sure you’re utilizing your social worker, your psychologist, other resources, and food pantries, if you have them.”
Even when the most ideal choices are not available, she said, “if they only have access to canned vegetables, I’d much rather them eat that than have nothing.”
No disclosures for Leneweaver were provided.
PHOENIX — Patients with head and neck cancer face high rates of malnutrition during treatment, and oral supplements are often recommended. But they are not the entire answer, a dietician told colleagues at the Association of Veterans Affairs (VA) Hematology/Oncology annual meeting.
“Patients should consume the most liberal diet possible throughout treatment,” said advanced practice oncology dietician Brittany Leneweaver, RD, CSO, CES, at the VA Washington DC Healthcare System. “This means not solely relying on oral nutrition supplements like Ensure if possible.”
While Leneweaver said many patients will need supplements, she stressed these products “are meant to supplement the diet and not be the sole source of nutrition, ideally.” Encouraging the intake of whole foods “is really key to make the transition back to solid foods after they’re done with treatment. This makes it so much easier when they’re already swallowing those thicker textures, rather than just liquid the entire time.”
Malnutrition: Common and Damaging
As Leneweaver noted, malnutrition is common in patients with head and neck cancer, and can lead to “increased treatment toxicity, increased risk of infection, decreased survival, increased surgical complication, delayed healing, decreased physical function, and decreased quality of life.”
Malnutrition data in patients with head and neck cancer in the US is sparse. However, a 2024 study found malnutrition in 20% of patients undergoing head and neck cancer surgery and linked the condition to increased length of stay (β, 5.20 additional days), higher costs (β, $15,722) higher odds of potentially preventable complications (adjusted odds ratio [aOR], 2.04), and lower odds of discharge to home (aOR, 0.34).
Leneweaver said her role involves addressing “nutrition impact symptoms” that reduce veteran food intake such as difficulty swallowing, taste disorders, dry mouth, and inflammation of the mucus membranes.
“I can’t tell you how much time I spend just talking to the patient about their medication regimens, making sure they have antiemetics on board, letting the radiation oncologist know, ‘Hey, it’s probably time for medicine,’” she said. “We’re constantly looking at side effects and addressing to alert the team as quickly as possible so that we can prevent further weight loss.”
Better Diets Lead to Better Outcomes
Leneweaver noted that “many times, patients will continue to rely on oral supplements as their primary source of nutrition over the long term. They may be missing out on several health benefits as a result.”
Research shows that high-quality diets matter in this patient group, she said. They’re associated with “decreased symptoms during treatment, reduced head and neck cancer risk, and reduced risk of those chronic nutrition impact symptoms,” Leneweaver said.
Diets before and after cancer diagnosis can make a difference. A 2019 study examined patient diets prior to diagnosis of head and neck cancer. It found that patients with better diet quality were less likely to experience overall nutrition impact symptoms (OR 0.45). However, “studies have found that the majority of our patients with head and neck cancer have an inadequate diet prior to diagnosis,” Leneweaver said.
As for postdiagnosis nutrition, a 2022 study linked healthier diets in patients with head and neck cancer to 93% lower 3-year risk of all-cause mortality and 85% lower risk of cancer-specific mortality.
What’s in a High-Quality Diet?
Regarding specific food recommendations, Leneweaver prefers the American Institute for Cancer Research (AICR) nutrition guidelines over the US Department of Agriculture’s Dietary Guidelines for Americans. The AICR “more clearly recommends plant-based diet with at least two-thirds of each meal coming from a variety of plant sources” and recommends avoiding alcohol entirely and limiting red meat, she said.
Leneweaver said she recognizes that dietary change can be gradual.
“It’s not going to happen overnight,” she said. “We know that lifestyle change takes a lot of work.”
Basic interventions can be effective, she said: “This can be just as simple as recommending a plant-based diet to your patient or recommending they eat the rainbow. And I don’t mean Skittles, I mean actual plants. If you just mention these couple of things to the patients, this can really go a long way, especially if they’re hearing that consistent messaging.”
Team-Based Follow-Up Is Key
Leneweaver emphasized the importance of following up over time even if patients do not initially accept referrals to nutritional services. Dieticians ideally see patients before or during initial treatment and then weekly during radiation therapy. Posttreatment follow-up continues “until they’re nutritionally stable. This can be anywhere from weekly to monthly.”
Leneweaver emphasized collaborating with other team members. For example, she works with a speech pathologist at joint visits, either weekly or monthly, “so that they can get off of that feeding tube or get back to a solid consistency diet, typically before that 3-month PET scan.”
It is also important to understand barriers to healthy eating in the veteran population, including transportation challenges and poor access to healthy food, Leneweaver said.
“Make sure you’re utilizing your social worker, your psychologist, other resources, and food pantries, if you have them.”
Even when the most ideal choices are not available, she said, “if they only have access to canned vegetables, I’d much rather them eat that than have nothing.”
No disclosures for Leneweaver were provided.
Polypectomy Best Practices Not Routinely Followed in US
, an analysis of more than 1.8 million colonoscopies found.
“We expected to find some variations in polypectomy technique, but the results were surprising; overall, cold snare usage was much lower than expected, given that this is the recommended method for removing most small polyps,” Seth Crockett, MD, MPH, AGAF, professor of medicine, Division of Gastroenterology and Hepatology, Oregon Health & Science University, Portland, told GI & Hepatology News.
The study was published in the October issue of The American Journal of Gastroenterology.
Using Gastroenterology Quality Improvement Consortium Registry data, Crockett and colleagues analyzed more than 1.8 million colonoscopies performed by 4601 endoscopists between 2019 and 2022 across 702 sites. All colonoscopies involved removal of polyps < 1 cm; lesions of this size are commonly found in screening colonoscopies, and detection is crucial to early cancer prevention.
The researchers found striking variation in polypectomy technique. Guideline-based cold snare polypectomy (CSP) was used in only 58% of cases (and as a single device in only 51%), whereas cold forceps polypectomy (CFP) accounted for 35% and hot snare polypectomy (HSP) for 11%.
The fact that CSP was used in fewer than 60% of cases represents “an important quality gap,” the authors wrote, adding that the fact that more than 10% of colonoscopies used HSP suggests that “some patients harboring low-risk lesions may be exposed to excess risk related to these practice variations.”
And while recommendations around the use of CFP are more nuanced (based largely on forceps type and polyp size), the “high frequency of CFP also suggests nonadherence to best practices,” they noted.
Gastroenterologists More Apt to Follow Guidance
Polypectomy technique varied by polyp type. CFP was more common in cases where only hyperplastic polyps were removed compared with cases with tubular adenomas (45% vs 30%, respectively). CSP use was highest in cases where only sessile serrated lesions were removed (66%) compared with cases with only tubular adenomas (61%) or hyperplastic polyps (37%).
There was also considerable variation by provider specialty.
Gastroenterologists (compared with non-GI specialists) used HSP less (4% vs 8%) and CSP more (40% vs 34%). Colonoscopies performed with GI fellows were more likely to use CFP (31% vs 21%) and less likely to use HSP (1% vs 5%) compared with colonoscopies without fellows.
“It was somewhat reassuring that colonoscopies performed by gastroenterologists were more likely to adhere to guideline recommendations, which suggests that dedicated endoscopy training is likely an important factor driving high-quality colonoscopy,” Crockett told GI & Hepatology News.
“Unexpectedly,” polypectomy technique also differed dramatically by geographic region, he said. CFP was used more than twice as often in the Northeast (31%) as in the Midwest (14%), whereas CSP was used more frequently in the Midwest (52%) than in the Northeast (32%).
“We suspect that much of the variation is related to differences in training, preferences, habits, and evolution of colonoscopy practice over time,” Crockett said. “More research is needed on the underlying drivers of this variation, and how differences in polypectomy technique impact both the safety and efficacy of colonoscopy to prevent colorectal cancer,” he said.
“As a specialty, we need to continue to work on disseminating guideline recommendations regarding colonoscopy quality, monitoring adherence to evidence-based practices, and working to address gaps in quality where they exist,” he added.
‘Concerning, Surprising, and Disappointing’
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School and Old Dominion University in Norfolk, called the results “concerning, surprising, and disappointing” and not consistent with the most current quality recommendations that advocate cold snare for most polyps less than 1 cm in size.
“Cold snare polypectomy has been shown not only to be more effective but also takes less time to perform, relative to cold biopsy,” said Johnson, who wasn’t involved in the study.
Johnson told GI & Hepatology News, “Inadequate lesion resection and variation in resection quality are major issues for colonoscopy quality. Those who perform colonoscopies need to be up-to-date with evidence-based quality standards — as well as held accountable if [there is] discordant practice — if we are to optimize the cancer prevention benefits of quality colonoscopy.”
Limitations of the current analysis include lack of extensive patient information and inability to further stratify polyps < 1 cm by size.
The study had no commercial funding. Crockett had no disclosures. Johnson disclosed serving as a director, officer, partner, employee, advisor, consultant, or trustee for ISOThrive.
A version of this article appeared on Medscape.com.
, an analysis of more than 1.8 million colonoscopies found.
“We expected to find some variations in polypectomy technique, but the results were surprising; overall, cold snare usage was much lower than expected, given that this is the recommended method for removing most small polyps,” Seth Crockett, MD, MPH, AGAF, professor of medicine, Division of Gastroenterology and Hepatology, Oregon Health & Science University, Portland, told GI & Hepatology News.
The study was published in the October issue of The American Journal of Gastroenterology.
Using Gastroenterology Quality Improvement Consortium Registry data, Crockett and colleagues analyzed more than 1.8 million colonoscopies performed by 4601 endoscopists between 2019 and 2022 across 702 sites. All colonoscopies involved removal of polyps < 1 cm; lesions of this size are commonly found in screening colonoscopies, and detection is crucial to early cancer prevention.
The researchers found striking variation in polypectomy technique. Guideline-based cold snare polypectomy (CSP) was used in only 58% of cases (and as a single device in only 51%), whereas cold forceps polypectomy (CFP) accounted for 35% and hot snare polypectomy (HSP) for 11%.
The fact that CSP was used in fewer than 60% of cases represents “an important quality gap,” the authors wrote, adding that the fact that more than 10% of colonoscopies used HSP suggests that “some patients harboring low-risk lesions may be exposed to excess risk related to these practice variations.”
And while recommendations around the use of CFP are more nuanced (based largely on forceps type and polyp size), the “high frequency of CFP also suggests nonadherence to best practices,” they noted.
Gastroenterologists More Apt to Follow Guidance
Polypectomy technique varied by polyp type. CFP was more common in cases where only hyperplastic polyps were removed compared with cases with tubular adenomas (45% vs 30%, respectively). CSP use was highest in cases where only sessile serrated lesions were removed (66%) compared with cases with only tubular adenomas (61%) or hyperplastic polyps (37%).
There was also considerable variation by provider specialty.
Gastroenterologists (compared with non-GI specialists) used HSP less (4% vs 8%) and CSP more (40% vs 34%). Colonoscopies performed with GI fellows were more likely to use CFP (31% vs 21%) and less likely to use HSP (1% vs 5%) compared with colonoscopies without fellows.
“It was somewhat reassuring that colonoscopies performed by gastroenterologists were more likely to adhere to guideline recommendations, which suggests that dedicated endoscopy training is likely an important factor driving high-quality colonoscopy,” Crockett told GI & Hepatology News.
“Unexpectedly,” polypectomy technique also differed dramatically by geographic region, he said. CFP was used more than twice as often in the Northeast (31%) as in the Midwest (14%), whereas CSP was used more frequently in the Midwest (52%) than in the Northeast (32%).
“We suspect that much of the variation is related to differences in training, preferences, habits, and evolution of colonoscopy practice over time,” Crockett said. “More research is needed on the underlying drivers of this variation, and how differences in polypectomy technique impact both the safety and efficacy of colonoscopy to prevent colorectal cancer,” he said.
“As a specialty, we need to continue to work on disseminating guideline recommendations regarding colonoscopy quality, monitoring adherence to evidence-based practices, and working to address gaps in quality where they exist,” he added.
‘Concerning, Surprising, and Disappointing’
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School and Old Dominion University in Norfolk, called the results “concerning, surprising, and disappointing” and not consistent with the most current quality recommendations that advocate cold snare for most polyps less than 1 cm in size.
“Cold snare polypectomy has been shown not only to be more effective but also takes less time to perform, relative to cold biopsy,” said Johnson, who wasn’t involved in the study.
Johnson told GI & Hepatology News, “Inadequate lesion resection and variation in resection quality are major issues for colonoscopy quality. Those who perform colonoscopies need to be up-to-date with evidence-based quality standards — as well as held accountable if [there is] discordant practice — if we are to optimize the cancer prevention benefits of quality colonoscopy.”
Limitations of the current analysis include lack of extensive patient information and inability to further stratify polyps < 1 cm by size.
The study had no commercial funding. Crockett had no disclosures. Johnson disclosed serving as a director, officer, partner, employee, advisor, consultant, or trustee for ISOThrive.
A version of this article appeared on Medscape.com.
, an analysis of more than 1.8 million colonoscopies found.
“We expected to find some variations in polypectomy technique, but the results were surprising; overall, cold snare usage was much lower than expected, given that this is the recommended method for removing most small polyps,” Seth Crockett, MD, MPH, AGAF, professor of medicine, Division of Gastroenterology and Hepatology, Oregon Health & Science University, Portland, told GI & Hepatology News.
The study was published in the October issue of The American Journal of Gastroenterology.
Using Gastroenterology Quality Improvement Consortium Registry data, Crockett and colleagues analyzed more than 1.8 million colonoscopies performed by 4601 endoscopists between 2019 and 2022 across 702 sites. All colonoscopies involved removal of polyps < 1 cm; lesions of this size are commonly found in screening colonoscopies, and detection is crucial to early cancer prevention.
The researchers found striking variation in polypectomy technique. Guideline-based cold snare polypectomy (CSP) was used in only 58% of cases (and as a single device in only 51%), whereas cold forceps polypectomy (CFP) accounted for 35% and hot snare polypectomy (HSP) for 11%.
The fact that CSP was used in fewer than 60% of cases represents “an important quality gap,” the authors wrote, adding that the fact that more than 10% of colonoscopies used HSP suggests that “some patients harboring low-risk lesions may be exposed to excess risk related to these practice variations.”
And while recommendations around the use of CFP are more nuanced (based largely on forceps type and polyp size), the “high frequency of CFP also suggests nonadherence to best practices,” they noted.
Gastroenterologists More Apt to Follow Guidance
Polypectomy technique varied by polyp type. CFP was more common in cases where only hyperplastic polyps were removed compared with cases with tubular adenomas (45% vs 30%, respectively). CSP use was highest in cases where only sessile serrated lesions were removed (66%) compared with cases with only tubular adenomas (61%) or hyperplastic polyps (37%).
There was also considerable variation by provider specialty.
Gastroenterologists (compared with non-GI specialists) used HSP less (4% vs 8%) and CSP more (40% vs 34%). Colonoscopies performed with GI fellows were more likely to use CFP (31% vs 21%) and less likely to use HSP (1% vs 5%) compared with colonoscopies without fellows.
“It was somewhat reassuring that colonoscopies performed by gastroenterologists were more likely to adhere to guideline recommendations, which suggests that dedicated endoscopy training is likely an important factor driving high-quality colonoscopy,” Crockett told GI & Hepatology News.
“Unexpectedly,” polypectomy technique also differed dramatically by geographic region, he said. CFP was used more than twice as often in the Northeast (31%) as in the Midwest (14%), whereas CSP was used more frequently in the Midwest (52%) than in the Northeast (32%).
“We suspect that much of the variation is related to differences in training, preferences, habits, and evolution of colonoscopy practice over time,” Crockett said. “More research is needed on the underlying drivers of this variation, and how differences in polypectomy technique impact both the safety and efficacy of colonoscopy to prevent colorectal cancer,” he said.
“As a specialty, we need to continue to work on disseminating guideline recommendations regarding colonoscopy quality, monitoring adherence to evidence-based practices, and working to address gaps in quality where they exist,” he added.
‘Concerning, Surprising, and Disappointing’
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School and Old Dominion University in Norfolk, called the results “concerning, surprising, and disappointing” and not consistent with the most current quality recommendations that advocate cold snare for most polyps less than 1 cm in size.
“Cold snare polypectomy has been shown not only to be more effective but also takes less time to perform, relative to cold biopsy,” said Johnson, who wasn’t involved in the study.
Johnson told GI & Hepatology News, “Inadequate lesion resection and variation in resection quality are major issues for colonoscopy quality. Those who perform colonoscopies need to be up-to-date with evidence-based quality standards — as well as held accountable if [there is] discordant practice — if we are to optimize the cancer prevention benefits of quality colonoscopy.”
Limitations of the current analysis include lack of extensive patient information and inability to further stratify polyps < 1 cm by size.
The study had no commercial funding. Crockett had no disclosures. Johnson disclosed serving as a director, officer, partner, employee, advisor, consultant, or trustee for ISOThrive.
A version of this article appeared on Medscape.com.
Colon Cleanses: How to Discourage Patients
Social media is rife with content promoting colon cleansing as a way to shed toxins and fix everything from chronic fatigue and overweight to weak immunity and skin problems.
Even doctors who aren’t hip to the latest TikTok trends may not be able to avoid the hype. That’s because patients are bringing up colon cleansing during their office visit.
“Patients often raise questions about colonics or detox teas, especially when these gain traction on social media platforms like TikTok,” said Tauseef Ali, MD, AGAF, medical executive director of SSM Health Digestive Care at St. Anthony Hospital in Oklahoma City. “Interest typically comes in waves, closely tied to the latest online trends.”
That means . And it’s not just patients who are asking.
“Sometimes we’ll get a message from primary care,” Mohammad Bilal, MD, associate professor of medicine and director of Bariatric and Third Space Endoscopy at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, told GI & Hepatology News. They’re getting the same questions from patients, and they want to know if colon cleansing that’s not connected with a colonoscopy exam has any benefits for overall health or specific health conditions.
The answer is no, and patients are more likely to believe that when physicians explain it using good information. Here is how Ali, Bilal, and professional organizations advise doctors to approach the issue.
What Exactly Is a Colon Cleanse?
Colon cleanses come in a variety of forms. Colonic irrigation, also called colon hydrotherapy, involves inserting a tube into the rectum and flushing out the colon with a large amount of fluid. Enemas do the same but use a small amount of liquid, and some product instructions tell the user to “hold it” for a designated amount of time before expelling colon contents.
Other cleanses, often called detoxing cleanses, are laxatives or herbal teas that users drink — and then stay close to the bathroom. Detox regimens and diets also are mentioned as a way to remove toxins from the body, improve health, and promote well-being.
Why Do Patients Use Them?
“Many patients describe a desire for ‘cleanliness,’ ‘detoxification,’ or to ‘feel lighter,’” Ali told GI & Hepatology News.
The claims on social media promote all of this and more — and well-known influencers make it all sound even more attractive.
“These motivations are often rooted in the cultural belief that the colon accumulates harmful toxins that must be flushed out,” Ali said. “This idea is not supported by scientific evidence. The body’s natural detox systems, primarily the liver and kidneys, already perform this function effectively.”
Bilal said that in recent years, he has noticed more awareness in general about the importance of gut health. “When there’s awareness, people often go to the other extreme,” he said.
Where Is the Evidence?
The National Center for Complementary and Integrative Health (NCCIH), part of the National Institutes of Health, warns on an information page that both cleansing and detox programs can be unsafe and falsely advertised.
While searches of medical literature turn up few studies, the NCCIH information points to a 2014 review that concluded that there is no compelling research to support the use of detox diets for managing weight or eliminating toxins. A 2017 review found juicing and detox regimens can cause weight loss initially but then lead to weight gain once a normal diet is resumed.
A systematic review of research on the safety and effectiveness of self-administered coffee enemas found nine case reports describing adverse events: seven reported colitis after the enema, and two reported more critical adverse events. All nine reports warned against the procedure. The researchers found no study reporting the effectiveness of coffee enemas.
The NCCIH information also notes that there is “limited clinical evidence validating colonic irrigation and insufficient evidence for its prescribed uses.”
Are Cleanses Regulated?
Some over-the-counter colon cleansing products are viewed as dietary supplements, giving the FDA authority to regulate them and take action under the Dietary Supplement Health and Education Act of 1994.
Certain products promoted as colon cleanses, such as laxatives, are regulated by the FDA as over-the-counter drugs and must meet safety and other requirements.
Colonic irrigation systems meant for cleansing before radiologic or endoscopic exams are class II devices — subject to 510(k) premarket notification requirements before marketing — whereas systems intended for other uses, such as routine colon cleansing for general well-being, are regarded as class III devices — subject to premarket approval requirements — according to an FDA spokesperson. To date, the FDA has not approved any colonic irrigation devices for the latter use, the spokesperson said.
For instance, the FDA warned consumers not to use a product promoted for colon cleansing after finding it contained tadalafil, the active ingredient in an FDA-approved drug for erectile dysfunction. The FDA has also issued numerous warning letters to the makers of colon cleansing devices, as they are not approved for this purpose.
The Federal Trade Commission can also take action specifically if the claims about the benefits and safety of products — including supplements, foods, over-the-counter drugs, or health equipment — are false, misleading, or not supported by science.
What Are the Dangers?
Cleanse and detox products come with many risks, including electrolyte imbalances, dehydration, and infections, Ali said. With colonic irrigation, there is a risk for rectal perforation. Products also may disrupt the gut microbiome, and some can interact with medications or worsen underlying health conditions, he added.
“It’s important for patients to be aware of these risks before considering nonmedical ‘cleaning’ methods,” he said.
At worst, patients risk fatality, Ali noted. He recalled a young patient who began using a vegetable enema as a detox. As it was being administered, the colon ruptured. The patient was admitted as a medical emergency and required surgery. Fortunately, the patient survived, but the incident could have proven fatal, Ali said.
Educating Patients
Because patients often don’t think of herbal cleanses, detox teas, and over-the-counter powders as supplements, Ali said it’s important to ask them about everything they take.
One way to frame this question is to ask if they are consuming any over-the-counter supplements or any other remedies, he said, and perhaps ask directly about any cleanses they are doing.
When patients ask him about colon cleanses, Ali explains the difference between evidence-based colonoscopy preparation and unregulated “cleanses.” Most patients respond to that approach, he said. Indeed, AGA and other GI societies updated their recommendations on optimizing bowel preparation quality for colonoscopy.
“Still, the appeal of quick fixes of social media trends can sometimes outweigh medical advice,” Ali said. He depends on building trusted relationships and reinforcing the message over time and finds that helps patients make informed and healthier choices.
Bilal, too, explains to patients that cleanses are unnecessary and educates them about what to do instead:
- Eat a containing the recommended amount of (22-34 g, depending on age and gender).
- For , follow a bowel regimen advised by your doctor.
- If gastrointestinal issues persist, get a medical checkup.
- Get any unexplained constipation or checked out by a doctor.
Taking a careful history can pay off, Ali has found. He questioned a patient complaining of abdominal discomfort whose testing found unexpectedly elevated liver enzymes and found she had been using an herbal “cleanse tea” found online. Within 4 weeks of stopping it, her liver enzymes normalized. “Thankfully, she made a full recovery — and she never touched those remedies again,” he said.
Ali had no relevant disclosures. Bilal reported consulting for Boston Scientific, Cook Medical, and Steris.
A version of this article appeared on Medscape.com.
Social media is rife with content promoting colon cleansing as a way to shed toxins and fix everything from chronic fatigue and overweight to weak immunity and skin problems.
Even doctors who aren’t hip to the latest TikTok trends may not be able to avoid the hype. That’s because patients are bringing up colon cleansing during their office visit.
“Patients often raise questions about colonics or detox teas, especially when these gain traction on social media platforms like TikTok,” said Tauseef Ali, MD, AGAF, medical executive director of SSM Health Digestive Care at St. Anthony Hospital in Oklahoma City. “Interest typically comes in waves, closely tied to the latest online trends.”
That means . And it’s not just patients who are asking.
“Sometimes we’ll get a message from primary care,” Mohammad Bilal, MD, associate professor of medicine and director of Bariatric and Third Space Endoscopy at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, told GI & Hepatology News. They’re getting the same questions from patients, and they want to know if colon cleansing that’s not connected with a colonoscopy exam has any benefits for overall health or specific health conditions.
The answer is no, and patients are more likely to believe that when physicians explain it using good information. Here is how Ali, Bilal, and professional organizations advise doctors to approach the issue.
What Exactly Is a Colon Cleanse?
Colon cleanses come in a variety of forms. Colonic irrigation, also called colon hydrotherapy, involves inserting a tube into the rectum and flushing out the colon with a large amount of fluid. Enemas do the same but use a small amount of liquid, and some product instructions tell the user to “hold it” for a designated amount of time before expelling colon contents.
Other cleanses, often called detoxing cleanses, are laxatives or herbal teas that users drink — and then stay close to the bathroom. Detox regimens and diets also are mentioned as a way to remove toxins from the body, improve health, and promote well-being.
Why Do Patients Use Them?
“Many patients describe a desire for ‘cleanliness,’ ‘detoxification,’ or to ‘feel lighter,’” Ali told GI & Hepatology News.
The claims on social media promote all of this and more — and well-known influencers make it all sound even more attractive.
“These motivations are often rooted in the cultural belief that the colon accumulates harmful toxins that must be flushed out,” Ali said. “This idea is not supported by scientific evidence. The body’s natural detox systems, primarily the liver and kidneys, already perform this function effectively.”
Bilal said that in recent years, he has noticed more awareness in general about the importance of gut health. “When there’s awareness, people often go to the other extreme,” he said.
Where Is the Evidence?
The National Center for Complementary and Integrative Health (NCCIH), part of the National Institutes of Health, warns on an information page that both cleansing and detox programs can be unsafe and falsely advertised.
While searches of medical literature turn up few studies, the NCCIH information points to a 2014 review that concluded that there is no compelling research to support the use of detox diets for managing weight or eliminating toxins. A 2017 review found juicing and detox regimens can cause weight loss initially but then lead to weight gain once a normal diet is resumed.
A systematic review of research on the safety and effectiveness of self-administered coffee enemas found nine case reports describing adverse events: seven reported colitis after the enema, and two reported more critical adverse events. All nine reports warned against the procedure. The researchers found no study reporting the effectiveness of coffee enemas.
The NCCIH information also notes that there is “limited clinical evidence validating colonic irrigation and insufficient evidence for its prescribed uses.”
Are Cleanses Regulated?
Some over-the-counter colon cleansing products are viewed as dietary supplements, giving the FDA authority to regulate them and take action under the Dietary Supplement Health and Education Act of 1994.
Certain products promoted as colon cleanses, such as laxatives, are regulated by the FDA as over-the-counter drugs and must meet safety and other requirements.
Colonic irrigation systems meant for cleansing before radiologic or endoscopic exams are class II devices — subject to 510(k) premarket notification requirements before marketing — whereas systems intended for other uses, such as routine colon cleansing for general well-being, are regarded as class III devices — subject to premarket approval requirements — according to an FDA spokesperson. To date, the FDA has not approved any colonic irrigation devices for the latter use, the spokesperson said.
For instance, the FDA warned consumers not to use a product promoted for colon cleansing after finding it contained tadalafil, the active ingredient in an FDA-approved drug for erectile dysfunction. The FDA has also issued numerous warning letters to the makers of colon cleansing devices, as they are not approved for this purpose.
The Federal Trade Commission can also take action specifically if the claims about the benefits and safety of products — including supplements, foods, over-the-counter drugs, or health equipment — are false, misleading, or not supported by science.
What Are the Dangers?
Cleanse and detox products come with many risks, including electrolyte imbalances, dehydration, and infections, Ali said. With colonic irrigation, there is a risk for rectal perforation. Products also may disrupt the gut microbiome, and some can interact with medications or worsen underlying health conditions, he added.
“It’s important for patients to be aware of these risks before considering nonmedical ‘cleaning’ methods,” he said.
At worst, patients risk fatality, Ali noted. He recalled a young patient who began using a vegetable enema as a detox. As it was being administered, the colon ruptured. The patient was admitted as a medical emergency and required surgery. Fortunately, the patient survived, but the incident could have proven fatal, Ali said.
Educating Patients
Because patients often don’t think of herbal cleanses, detox teas, and over-the-counter powders as supplements, Ali said it’s important to ask them about everything they take.
One way to frame this question is to ask if they are consuming any over-the-counter supplements or any other remedies, he said, and perhaps ask directly about any cleanses they are doing.
When patients ask him about colon cleanses, Ali explains the difference between evidence-based colonoscopy preparation and unregulated “cleanses.” Most patients respond to that approach, he said. Indeed, AGA and other GI societies updated their recommendations on optimizing bowel preparation quality for colonoscopy.
“Still, the appeal of quick fixes of social media trends can sometimes outweigh medical advice,” Ali said. He depends on building trusted relationships and reinforcing the message over time and finds that helps patients make informed and healthier choices.
Bilal, too, explains to patients that cleanses are unnecessary and educates them about what to do instead:
- Eat a containing the recommended amount of (22-34 g, depending on age and gender).
- For , follow a bowel regimen advised by your doctor.
- If gastrointestinal issues persist, get a medical checkup.
- Get any unexplained constipation or checked out by a doctor.
Taking a careful history can pay off, Ali has found. He questioned a patient complaining of abdominal discomfort whose testing found unexpectedly elevated liver enzymes and found she had been using an herbal “cleanse tea” found online. Within 4 weeks of stopping it, her liver enzymes normalized. “Thankfully, she made a full recovery — and she never touched those remedies again,” he said.
Ali had no relevant disclosures. Bilal reported consulting for Boston Scientific, Cook Medical, and Steris.
A version of this article appeared on Medscape.com.
Social media is rife with content promoting colon cleansing as a way to shed toxins and fix everything from chronic fatigue and overweight to weak immunity and skin problems.
Even doctors who aren’t hip to the latest TikTok trends may not be able to avoid the hype. That’s because patients are bringing up colon cleansing during their office visit.
“Patients often raise questions about colonics or detox teas, especially when these gain traction on social media platforms like TikTok,” said Tauseef Ali, MD, AGAF, medical executive director of SSM Health Digestive Care at St. Anthony Hospital in Oklahoma City. “Interest typically comes in waves, closely tied to the latest online trends.”
That means . And it’s not just patients who are asking.
“Sometimes we’ll get a message from primary care,” Mohammad Bilal, MD, associate professor of medicine and director of Bariatric and Third Space Endoscopy at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, told GI & Hepatology News. They’re getting the same questions from patients, and they want to know if colon cleansing that’s not connected with a colonoscopy exam has any benefits for overall health or specific health conditions.
The answer is no, and patients are more likely to believe that when physicians explain it using good information. Here is how Ali, Bilal, and professional organizations advise doctors to approach the issue.
What Exactly Is a Colon Cleanse?
Colon cleanses come in a variety of forms. Colonic irrigation, also called colon hydrotherapy, involves inserting a tube into the rectum and flushing out the colon with a large amount of fluid. Enemas do the same but use a small amount of liquid, and some product instructions tell the user to “hold it” for a designated amount of time before expelling colon contents.
Other cleanses, often called detoxing cleanses, are laxatives or herbal teas that users drink — and then stay close to the bathroom. Detox regimens and diets also are mentioned as a way to remove toxins from the body, improve health, and promote well-being.
Why Do Patients Use Them?
“Many patients describe a desire for ‘cleanliness,’ ‘detoxification,’ or to ‘feel lighter,’” Ali told GI & Hepatology News.
The claims on social media promote all of this and more — and well-known influencers make it all sound even more attractive.
“These motivations are often rooted in the cultural belief that the colon accumulates harmful toxins that must be flushed out,” Ali said. “This idea is not supported by scientific evidence. The body’s natural detox systems, primarily the liver and kidneys, already perform this function effectively.”
Bilal said that in recent years, he has noticed more awareness in general about the importance of gut health. “When there’s awareness, people often go to the other extreme,” he said.
Where Is the Evidence?
The National Center for Complementary and Integrative Health (NCCIH), part of the National Institutes of Health, warns on an information page that both cleansing and detox programs can be unsafe and falsely advertised.
While searches of medical literature turn up few studies, the NCCIH information points to a 2014 review that concluded that there is no compelling research to support the use of detox diets for managing weight or eliminating toxins. A 2017 review found juicing and detox regimens can cause weight loss initially but then lead to weight gain once a normal diet is resumed.
A systematic review of research on the safety and effectiveness of self-administered coffee enemas found nine case reports describing adverse events: seven reported colitis after the enema, and two reported more critical adverse events. All nine reports warned against the procedure. The researchers found no study reporting the effectiveness of coffee enemas.
The NCCIH information also notes that there is “limited clinical evidence validating colonic irrigation and insufficient evidence for its prescribed uses.”
Are Cleanses Regulated?
Some over-the-counter colon cleansing products are viewed as dietary supplements, giving the FDA authority to regulate them and take action under the Dietary Supplement Health and Education Act of 1994.
Certain products promoted as colon cleanses, such as laxatives, are regulated by the FDA as over-the-counter drugs and must meet safety and other requirements.
Colonic irrigation systems meant for cleansing before radiologic or endoscopic exams are class II devices — subject to 510(k) premarket notification requirements before marketing — whereas systems intended for other uses, such as routine colon cleansing for general well-being, are regarded as class III devices — subject to premarket approval requirements — according to an FDA spokesperson. To date, the FDA has not approved any colonic irrigation devices for the latter use, the spokesperson said.
For instance, the FDA warned consumers not to use a product promoted for colon cleansing after finding it contained tadalafil, the active ingredient in an FDA-approved drug for erectile dysfunction. The FDA has also issued numerous warning letters to the makers of colon cleansing devices, as they are not approved for this purpose.
The Federal Trade Commission can also take action specifically if the claims about the benefits and safety of products — including supplements, foods, over-the-counter drugs, or health equipment — are false, misleading, or not supported by science.
What Are the Dangers?
Cleanse and detox products come with many risks, including electrolyte imbalances, dehydration, and infections, Ali said. With colonic irrigation, there is a risk for rectal perforation. Products also may disrupt the gut microbiome, and some can interact with medications or worsen underlying health conditions, he added.
“It’s important for patients to be aware of these risks before considering nonmedical ‘cleaning’ methods,” he said.
At worst, patients risk fatality, Ali noted. He recalled a young patient who began using a vegetable enema as a detox. As it was being administered, the colon ruptured. The patient was admitted as a medical emergency and required surgery. Fortunately, the patient survived, but the incident could have proven fatal, Ali said.
Educating Patients
Because patients often don’t think of herbal cleanses, detox teas, and over-the-counter powders as supplements, Ali said it’s important to ask them about everything they take.
One way to frame this question is to ask if they are consuming any over-the-counter supplements or any other remedies, he said, and perhaps ask directly about any cleanses they are doing.
When patients ask him about colon cleanses, Ali explains the difference between evidence-based colonoscopy preparation and unregulated “cleanses.” Most patients respond to that approach, he said. Indeed, AGA and other GI societies updated their recommendations on optimizing bowel preparation quality for colonoscopy.
“Still, the appeal of quick fixes of social media trends can sometimes outweigh medical advice,” Ali said. He depends on building trusted relationships and reinforcing the message over time and finds that helps patients make informed and healthier choices.
Bilal, too, explains to patients that cleanses are unnecessary and educates them about what to do instead:
- Eat a containing the recommended amount of (22-34 g, depending on age and gender).
- For , follow a bowel regimen advised by your doctor.
- If gastrointestinal issues persist, get a medical checkup.
- Get any unexplained constipation or checked out by a doctor.
Taking a careful history can pay off, Ali has found. He questioned a patient complaining of abdominal discomfort whose testing found unexpectedly elevated liver enzymes and found she had been using an herbal “cleanse tea” found online. Within 4 weeks of stopping it, her liver enzymes normalized. “Thankfully, she made a full recovery — and she never touched those remedies again,” he said.
Ali had no relevant disclosures. Bilal reported consulting for Boston Scientific, Cook Medical, and Steris.
A version of this article appeared on Medscape.com.