User login
The Pop That Stopped the Soccer Game
ANSWER
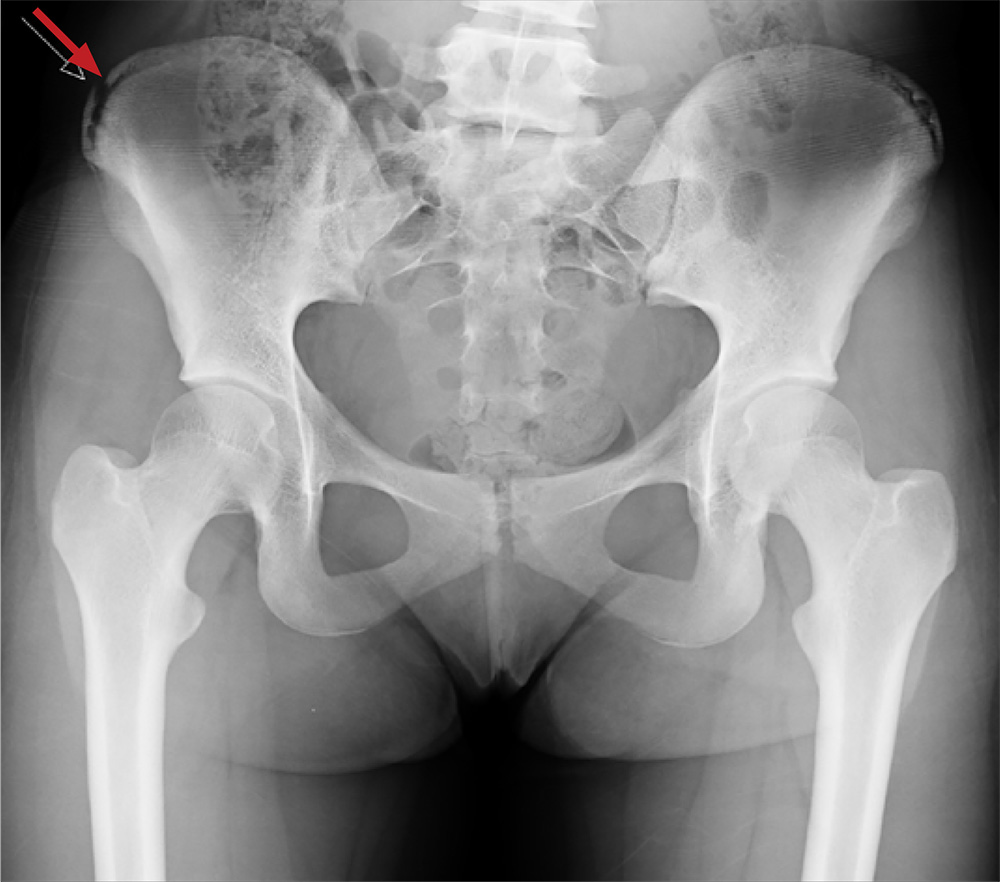
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.
ANSWER
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.
ANSWER
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.

A 13-year-old girl presents with her mother for evaluation of right hip pain following a soccer game two days ago. The patient says she felt a “pop” in her right hip while running and kicking the ball. She was escorted off the field, unable to finish the game.
Since then, she has had pain over the right superior pelvic region. She rates the pain as a 1/10 at rest but 7/10 with ambulation. She is unwilling to bear weight secondary to discomfort and has been using crutches provided by her trainer. She has been using ice and ibuprofen without relief. Her medical history is unremarkable.
On physical exam, you note a well-developed, well-nourished female in no acute distress. No ecchymosis, erythema, or abrasions can be seen on skin exam. The patient has point tenderness over the right iliac crest. She has mild pain and weakness with hip flexion and significant pain with abduction. The extremity is neurovascularly intact.
A pelvic radiograph is obtained. What is your impression?
Concussion in sport
Concussion has become an increasing concern over the past several years because of evidence that it can have long-term deleterious effects on the human brain. In November 2012, the American Medical Society for Sports Medicine (AMSSM) published its position statement on concussion in sport. The National Trainer’s Athletic Association and the American College of Sports Medicine have endorsed the guideline.
Diagnosis
The AMSSM defines a concussion as "a traumatically induced transient disturbance of brain function ... caused by a complex pathophysiological process." The signs and symptoms of concussion are varied and usually overlap with other vague symptoms of illness. By far the most common symptom is headache. Other common symptoms are nausea, dizziness, photophobia, balance problems, and feeling mentally foggy. In 80%-90% of cases of concussion in athletes, symptoms resolve within 7 days, although dizziness, migraine headaches, and cognitive symptoms such as fogginess and mental slowing all suggest a longer recovery period.
Several factors increase a patient’s risk for sustaining a concussion. The most common predictor is a previous concussion, which increases a person’s risk of having a concussion by 2-5.8 times the average risk. Females sustain more concussions, experience/report more symptoms, and have longer recovery times than do males who play the same sport. Younger athletes are more susceptible to prolonged recovery and catastrophic injury likely due to differences between developing and mature brains.
Mood disorders do not increase an athlete’s risk for concussion, but depression and anxiety may be increased as a consequence of concussion. Preexisting learning disorders may increase recovery times, but do not increase the risk for concussion. Preexisting migraines may increase the concussion risk, but the evidence is mixed whether this increases the recovery period. Developing migraine symptoms after a concussion can lengthen the recovery period.
Treatment
The primary treatment for concussion is physical and mental rest. Therapies should be tailored to specific symptoms although little evidence exists in support of medications to alleviate symptoms. Acetaminophen offers the lowest risk profile for headache. Nonsteroidal anti-inflammatory drugs as well as aspirin are usually avoided because of a theoretical risk of bleeding. There is no evidence to support the use of stimulants or sleep aids in the management of postconcussive symptoms nor should antidepressants be started in the first 6-12 weeks after a concussion. Changes in mood may occur. If symptoms persist for more than 6-12 weeks, then further workup for an underlying mood disorder should be considered. Balance disturbance that persists may benefit from vestibular therapy.
There are no current standardized return-to-school recommendations. Each student should be evaluated individually and a custom return-to-school plan should be devised. Students with symptoms that are exacerbated with cognitive stress may need limitations such as a decreased work load, extended testing time, half days off or full days off. Athletes should be able to tolerate full school days without symptom recurrence prior to being released for a return-to-play protocol.
Each athlete’s return to play should be individualized. The return-to-play program should be started only when the athlete’s symptoms are resolved. The return-to-play protocol should be gradual and incremental with slow increases in physical activity, then sport-specific activities, then sport-specific physical contact. For example, a wrestler might, once symptom free, be told to start with light aerobic training, then if remaining symptom free, proceed to weight training, then movements on the mat, then light training with other wrestlers, then practice matches, and finally full competition. Going from one level to the next in the return-to-play protocol should only happen if the athlete remains asymptomatic. With any reoccurring symptoms, the athlete should be returned to the preceding step. The return-to-play progression may be as few as 4-5 days and as long as a couple of months. The final return-to-play determination should come from a "licensed health care provider trained in the evaluation and management of concussion," according to the statement.
Computerized neuropsychiatric testing has been shown to have a moderate sensitivity in detecting postconcussive deficits. These deficits have been shown to persist even past symptom resolution although it is unknown if baseline and postinjury testing alter the short- and long-term risk associated with concussion. There is no consensus on specific recommendations for use of computerized, neuropsychiatric testing other than that it can be used as part of a "comprehensive concussion management strategy" and should not be used alone.
Most concussions do not need advanced neuroimaging. CT and MRI should be reserved for those patients whose symptoms worsen and/or whose ability to process information declines.
There are no current guidelines for disqualification of an athlete from sport. Some experts recommend considering disqualification if any of the following are present: "structural abnormality on neuroimaging, multiple lifetime concussions, persistent diminished academic or workplace performance, persistent postconcussive symptoms, prolonged recovery courses, and perceived reduced threshold of sustaining recurrent concussions."
The bottom line
Concussion is an increasingly diagnosed injury that has short-term consequences and can have long-term complications. The current literature supports individualized treatment of patients with concussion, and it supports the idea that no athlete should be returned to play the same day or while symptomatic.
Reference:
– American Medical Society for Sports Medicine position statement: concussion in sport, Br. J. Sports Med. 2013;47:15-26.
Dr. Skolnik is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Chrusch is an assistant director in the family medicine residency program at the hospital.
Concussion has become an increasing concern over the past several years because of evidence that it can have long-term deleterious effects on the human brain. In November 2012, the American Medical Society for Sports Medicine (AMSSM) published its position statement on concussion in sport. The National Trainer’s Athletic Association and the American College of Sports Medicine have endorsed the guideline.
Diagnosis
The AMSSM defines a concussion as "a traumatically induced transient disturbance of brain function ... caused by a complex pathophysiological process." The signs and symptoms of concussion are varied and usually overlap with other vague symptoms of illness. By far the most common symptom is headache. Other common symptoms are nausea, dizziness, photophobia, balance problems, and feeling mentally foggy. In 80%-90% of cases of concussion in athletes, symptoms resolve within 7 days, although dizziness, migraine headaches, and cognitive symptoms such as fogginess and mental slowing all suggest a longer recovery period.
Several factors increase a patient’s risk for sustaining a concussion. The most common predictor is a previous concussion, which increases a person’s risk of having a concussion by 2-5.8 times the average risk. Females sustain more concussions, experience/report more symptoms, and have longer recovery times than do males who play the same sport. Younger athletes are more susceptible to prolonged recovery and catastrophic injury likely due to differences between developing and mature brains.
Mood disorders do not increase an athlete’s risk for concussion, but depression and anxiety may be increased as a consequence of concussion. Preexisting learning disorders may increase recovery times, but do not increase the risk for concussion. Preexisting migraines may increase the concussion risk, but the evidence is mixed whether this increases the recovery period. Developing migraine symptoms after a concussion can lengthen the recovery period.
Treatment
The primary treatment for concussion is physical and mental rest. Therapies should be tailored to specific symptoms although little evidence exists in support of medications to alleviate symptoms. Acetaminophen offers the lowest risk profile for headache. Nonsteroidal anti-inflammatory drugs as well as aspirin are usually avoided because of a theoretical risk of bleeding. There is no evidence to support the use of stimulants or sleep aids in the management of postconcussive symptoms nor should antidepressants be started in the first 6-12 weeks after a concussion. Changes in mood may occur. If symptoms persist for more than 6-12 weeks, then further workup for an underlying mood disorder should be considered. Balance disturbance that persists may benefit from vestibular therapy.
There are no current standardized return-to-school recommendations. Each student should be evaluated individually and a custom return-to-school plan should be devised. Students with symptoms that are exacerbated with cognitive stress may need limitations such as a decreased work load, extended testing time, half days off or full days off. Athletes should be able to tolerate full school days without symptom recurrence prior to being released for a return-to-play protocol.
Each athlete’s return to play should be individualized. The return-to-play program should be started only when the athlete’s symptoms are resolved. The return-to-play protocol should be gradual and incremental with slow increases in physical activity, then sport-specific activities, then sport-specific physical contact. For example, a wrestler might, once symptom free, be told to start with light aerobic training, then if remaining symptom free, proceed to weight training, then movements on the mat, then light training with other wrestlers, then practice matches, and finally full competition. Going from one level to the next in the return-to-play protocol should only happen if the athlete remains asymptomatic. With any reoccurring symptoms, the athlete should be returned to the preceding step. The return-to-play progression may be as few as 4-5 days and as long as a couple of months. The final return-to-play determination should come from a "licensed health care provider trained in the evaluation and management of concussion," according to the statement.
Computerized neuropsychiatric testing has been shown to have a moderate sensitivity in detecting postconcussive deficits. These deficits have been shown to persist even past symptom resolution although it is unknown if baseline and postinjury testing alter the short- and long-term risk associated with concussion. There is no consensus on specific recommendations for use of computerized, neuropsychiatric testing other than that it can be used as part of a "comprehensive concussion management strategy" and should not be used alone.
Most concussions do not need advanced neuroimaging. CT and MRI should be reserved for those patients whose symptoms worsen and/or whose ability to process information declines.
There are no current guidelines for disqualification of an athlete from sport. Some experts recommend considering disqualification if any of the following are present: "structural abnormality on neuroimaging, multiple lifetime concussions, persistent diminished academic or workplace performance, persistent postconcussive symptoms, prolonged recovery courses, and perceived reduced threshold of sustaining recurrent concussions."
The bottom line
Concussion is an increasingly diagnosed injury that has short-term consequences and can have long-term complications. The current literature supports individualized treatment of patients with concussion, and it supports the idea that no athlete should be returned to play the same day or while symptomatic.
Reference:
– American Medical Society for Sports Medicine position statement: concussion in sport, Br. J. Sports Med. 2013;47:15-26.
Dr. Skolnik is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Chrusch is an assistant director in the family medicine residency program at the hospital.
Concussion has become an increasing concern over the past several years because of evidence that it can have long-term deleterious effects on the human brain. In November 2012, the American Medical Society for Sports Medicine (AMSSM) published its position statement on concussion in sport. The National Trainer’s Athletic Association and the American College of Sports Medicine have endorsed the guideline.
Diagnosis
The AMSSM defines a concussion as "a traumatically induced transient disturbance of brain function ... caused by a complex pathophysiological process." The signs and symptoms of concussion are varied and usually overlap with other vague symptoms of illness. By far the most common symptom is headache. Other common symptoms are nausea, dizziness, photophobia, balance problems, and feeling mentally foggy. In 80%-90% of cases of concussion in athletes, symptoms resolve within 7 days, although dizziness, migraine headaches, and cognitive symptoms such as fogginess and mental slowing all suggest a longer recovery period.
Several factors increase a patient’s risk for sustaining a concussion. The most common predictor is a previous concussion, which increases a person’s risk of having a concussion by 2-5.8 times the average risk. Females sustain more concussions, experience/report more symptoms, and have longer recovery times than do males who play the same sport. Younger athletes are more susceptible to prolonged recovery and catastrophic injury likely due to differences between developing and mature brains.
Mood disorders do not increase an athlete’s risk for concussion, but depression and anxiety may be increased as a consequence of concussion. Preexisting learning disorders may increase recovery times, but do not increase the risk for concussion. Preexisting migraines may increase the concussion risk, but the evidence is mixed whether this increases the recovery period. Developing migraine symptoms after a concussion can lengthen the recovery period.
Treatment
The primary treatment for concussion is physical and mental rest. Therapies should be tailored to specific symptoms although little evidence exists in support of medications to alleviate symptoms. Acetaminophen offers the lowest risk profile for headache. Nonsteroidal anti-inflammatory drugs as well as aspirin are usually avoided because of a theoretical risk of bleeding. There is no evidence to support the use of stimulants or sleep aids in the management of postconcussive symptoms nor should antidepressants be started in the first 6-12 weeks after a concussion. Changes in mood may occur. If symptoms persist for more than 6-12 weeks, then further workup for an underlying mood disorder should be considered. Balance disturbance that persists may benefit from vestibular therapy.
There are no current standardized return-to-school recommendations. Each student should be evaluated individually and a custom return-to-school plan should be devised. Students with symptoms that are exacerbated with cognitive stress may need limitations such as a decreased work load, extended testing time, half days off or full days off. Athletes should be able to tolerate full school days without symptom recurrence prior to being released for a return-to-play protocol.
Each athlete’s return to play should be individualized. The return-to-play program should be started only when the athlete’s symptoms are resolved. The return-to-play protocol should be gradual and incremental with slow increases in physical activity, then sport-specific activities, then sport-specific physical contact. For example, a wrestler might, once symptom free, be told to start with light aerobic training, then if remaining symptom free, proceed to weight training, then movements on the mat, then light training with other wrestlers, then practice matches, and finally full competition. Going from one level to the next in the return-to-play protocol should only happen if the athlete remains asymptomatic. With any reoccurring symptoms, the athlete should be returned to the preceding step. The return-to-play progression may be as few as 4-5 days and as long as a couple of months. The final return-to-play determination should come from a "licensed health care provider trained in the evaluation and management of concussion," according to the statement.
Computerized neuropsychiatric testing has been shown to have a moderate sensitivity in detecting postconcussive deficits. These deficits have been shown to persist even past symptom resolution although it is unknown if baseline and postinjury testing alter the short- and long-term risk associated with concussion. There is no consensus on specific recommendations for use of computerized, neuropsychiatric testing other than that it can be used as part of a "comprehensive concussion management strategy" and should not be used alone.
Most concussions do not need advanced neuroimaging. CT and MRI should be reserved for those patients whose symptoms worsen and/or whose ability to process information declines.
There are no current guidelines for disqualification of an athlete from sport. Some experts recommend considering disqualification if any of the following are present: "structural abnormality on neuroimaging, multiple lifetime concussions, persistent diminished academic or workplace performance, persistent postconcussive symptoms, prolonged recovery courses, and perceived reduced threshold of sustaining recurrent concussions."
The bottom line
Concussion is an increasingly diagnosed injury that has short-term consequences and can have long-term complications. The current literature supports individualized treatment of patients with concussion, and it supports the idea that no athlete should be returned to play the same day or while symptomatic.
Reference:
– American Medical Society for Sports Medicine position statement: concussion in sport, Br. J. Sports Med. 2013;47:15-26.
Dr. Skolnik is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Chrusch is an assistant director in the family medicine residency program at the hospital.


