User login
Your medical conference is canceled. Now what?
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Khadija Hafidh, MD, was already booked on a 14-hour, direct flight from Dubai to Los Angeles, when the American College of Physicians (ACP) announced it was canceling its internal medicine meeting scheduled for April.
Canceling her hotel reservation was not a problem, and she was assured a refund for the conference fee, but her airline ticket was another matter, said Dr. Hafidh, an internist and diabetologist with the Dubai Health Authority.
“The airline I booked my ticket with is willing to waive the change fees, but will deduct a cancellation fee if I choose not to take the trip,” Dr. Hafidh said in an interview. “The cancellation fees is $300. A bit steep I must admit.”
Dr. Hafidh now faces a dilemma: Lose the $300 and cancel, or change her flight dates to June for the American Diabetes Association meeting in Chicago.
“But then again, we aren’t sure if that meeting will take place,” Dr. Hafidh said. “A few weeks ago I thought this whole thing was just a storm in a tea cup. However when it was declared a pandemic yesterday, it brought about another dimension.”
More than 25 medical meetings and conferences across the globe have been canceled or postponed because of COVID-19 concerns. The sudden cancellations have caused reservation woes and travel headaches for thousands of physicians who planned to attend the meetings. Some societies are considering the idea of virtual conferences, while other associations have scrapped their meetings until next year.
For physicians facing a canceled conference, the most likely question is, what now? Read on for tips and suggestions.
Reservation refunds vary
Refunds on airfare because of conference cancellations differ, depending on the airline and where you were traveling. Some airlines, such as United Airlines, have waived all change fees for tickets issued March 3, 2020, through March 31, 2020, and passengers can change their dates for up to 12 months after the ticket was issued.
Full refunds often depend on whether your ticket was nonrefundable when purchased. Many airlines, such as Delta, are providing full refunds if the airline canceled your flight. JetBlue is waiving all change and cancellation fees for customers scheduled to travel March 10, 2020, through April 30, 2020.
Las Vegas–based dermatologist H.L. Greenberg, MD, was satisfied with the credit he received from Southwest Airlines after the American Academy of Dermatology (AAD) canceled its Denver meeting. He and his staff were looking forward to the gathering, but he noted that the meeting would likely have been limited, even if it had take place as scheduled.
“I am disappointed that I won’t be able to meet with colleagues and industry to explore what the latest advances and interests are in dermatology,” he said. “Because many academic institutions were forbidding their faculty from traveling, the content of the meeting was going to be severely diminished. It’s just a rough time for everyone.”
Meanwhile, Asa Radix, MD, PhD, a New York–based internist, received a full refund for his Amtrak ticket to Boston when the Conference on Retroviruses and Opportunistic Infections (CROI) scheduled for early March was converted to a virtual meeting. Dr. Radix, senior director of research and education at the Callen-Lorde Community Health Center in New York, left another meeting in Brazil early to get to the Boston conference, he said.
“I was packed, but really that was a minor inconvenience,” he said in an interview. “I appreciate that they prioritized health concerns and changed to a virtual meeting. I received full refunds, no issues whatsoever. [It was] really great since I had no travel insurance.”
Check with your individual airline or train line for information about ticket refunds and credits. Many airlines are currently making special accommodations because of COVID-19. If your flight was covered by trip insurance, also called travel assistance, you are generally protected against unforeseen financial losses such as cancellations. The U.S. Department of Transportation provides this general online resource about airline refunds.
Hotel refunds probable
Most meeting organizations who have made the decision to cancel or postpone a conference also have canceled block hotel reservations reserved for the meeting. Medical associations are not directly refunding the hotel costs, but the majority of hotels are refunding reservations with no questions asked. Physicians interviewed for this story all reported no trouble getting refunds for their hotel reservations. However, attendees who did not book a hotel in official housing blocks should contact the hotel directly to cancel.
What about registration fees?
In response to COVID-19 cancellations, most conference leaders are refunding registration fees in full for both attendees and exhibitors. The refund may not be automatic, some associations such as ACP and the American College of Obstetricians and Gynecologists state it may take up to 45 days for the funds to be credited, depending on the payment used.
If the conference you planned to attend was postponed, the registration fee may be assigned to the new meeting dates and the money may not be refunded. Registration fees for the Minimally Invasive Surgery Symposium, for example, delayed until an unconfirmed date, and for the European Association of Urology (EAU) meeting, postponed until July, will be automatically credited to the rescheduled meeting, according to the websites. If attendees cannot attend the rescheduled EAU meeting, the association will not provide a refund and the registration will not apply to the 2021 meeting, according to its website. However, the group is providing registrants with a free access code for the EAU20 Resource Centre, which contains websites of sessions and scientific content.
A number of physicians have expressed disappointment with the EAU’s postponement on social media. On Twitter, some doctors wrote that the rescheduled dates were bad timing, while others lamented the refund refusal.
The EAU said it regrets that some delegates will experience financial losses, but that the organization has already experienced a significant outlay that cannot be recovered including venue, logistics, travel, and accommodation costs.
"We are doing what we can to absorb costs, but we need to be realistic about what is affordable; should the organization have to refund all or even most registrations, it would significantly jeopardize the viability of the organization," the EAU said in a statement. "These are difficult times, not only for the EAU, but on a global scale. Where there are specific cases of hardship or very extenuating financial circumstances, we will be willing to review individual cases. So far, we believe that we have done what we can do to meet the conflicting demands presented by the postponement of the congress, but this is a situation which changes from day to day, and we need to continuously evaluate what might be the best course of action." *
Contact your medical association directly for details on postponements.
What if I’m a presenter?
In an attempt to save the hard work and time that planners and presenters have invested into now-canceled meetings, some conferences are moving to a digital format. The Conference on Retroviruses and Opportunistic Infections (CROI) was the first to convert its in-person conference to a virtual meeting, held from March 8 to 11, 2020. At-home attendees logged onto CROI’s digital platform to hear plenaries, oral abstracts, themed discussion sessions, and symposia.
Dr. Radix was one of many CROI speakers who changed his presentation on HIV prevalence among transgender men to a virtual format.
“We were provided with detailed instructions from CROI about how to do this,” said Dr. Radix, who tweeted about the experience. “For my presentation, I used the video option in PowerPoint; it seemed the most straightforward and didn’t require buying additional software. It was fairly easy to follow the instructions to create the video but it was disappointing to present to an empty room.”
Matthew Spinelli, MD, an HIV researcher with the University of California, San Francisco, who also presented virtually, said it was remarkable that CROI leaders were able to put together the virtual program in such a short time. He delivered his presentation on the accuracy of a real-time urine tenofovir test using PowerPoint and a podcast microphone.
“It seemed to work pretty well,” he said in an interview. “It’s not the same as being there in person, there’s a lot of networking and chance conversations that happen when you’re all in the same place, but it was the right decision to cancel. If I have to be at home or at work doing social distancing, this was the best possible way of doing it.”
Following in CROI’s footsteps, the National Kidney Foundation’s spring conference has moved to a live virtual conference. The 2020 Healthcare Information and Management Systems Society (HIMSS) global health conference also will move to a digital format. Other societies are considering similar virtual options. Check with your meeting website for more details on digital options and attendee access.
*The article was updated on 03/16/2020.
Supreme Court to rule on Louisiana abortion rules by end of summer
The U.S. Supreme Court will likely decide by the end of the summer whether a controversial Louisiana abortion law that imposes restrictions on physicians can stand.
Justices heard oral arguments March 4, 2020, in June Medicare Services v. Russo, which centers on a Louisiana law requiring physicians who perform abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, while clinics that violate the law can have their licenses revoked, according to the state law, originally passed in 2014. In 2016, the Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, the justices struck down the measure as unconstitutional.
During oral arguments, Julie Rikelman an attorney representing June Medical Services, said that the Louisiana law is identical to the abortion law in Texas, and she argued that justices should reach the same conclusion.
“The district court found this law would leave Louisiana with just one clinic in one state to serve about 10,000 people per year,” Ms. Rikelman said during oral arguments. “That would mean that hundreds of thousands of women would now live more than 150 miles from the closest provider. And the burdens were actually more severe than this court found in Whole Woman’s Health.”
Elizabeth Murrill, solicitor general of Louisiana, argued that the Louisiana law was justified, and that the 5th U.S. Circuit Court of Appeals was correct when it reversed a district court decision and upheld the law.
“The 5th Circuit correctly held that the plaintiffs in this case failed to carry their burden – their heavy burden of proof that is required to facially invalidate a state law,” Ms. Murrill said during oral arguments. “Louisiana’s decision to require abortion providers to have admitting privileges was justified by abundant evidence of life-threatening health and safety violations, malpractice, noncompliance with professional licensing rules, legislative testimony from postabortive women, [and] testimony from doctors who took care of abortion providers’ abandoned patients.”
During arguments, Justice Ruth Bader Ginsburg questioned the reasoning behind the 30-mile privileges rule, expressing doubt at the state’s justification for the requirement. “What sense does the 30-mile limit make, considering that – certainly for medication abortions and for the overwhelming number of other abortions ... if the woman has a problem, it will be her local hospital that ... she will need to go to for the care, not something 30 miles from the clinic.”
Ms. Murrill responded that the Louisiana regulation is consistent with surgery and ambulatory surgery regulations and aligns with the state’s regulatory structure.
“We had evidence in the record of women who did require transfers,” Ms. Murrill said. “[An abortion provider] testified unambiguously that he had to transfer four patients who had punctured uteruses and were hemorrhaging.”
Whether the plaintiffs have standing to sue is a key question. As a general rule, a plaintiff can only sue to protect their own rights, unless the plaintiff has a close relationship with a third party and there are barriers that prevent the third party from suing. Attorneys for Louisiana contend that the plaintiffs – the medical clinic and several physicians – have no right to sue because their rights are not at stake, and that there is no obstacle to patients suing over the law.
Since the Louisiana law is intended to protect women from “unscrupulous and incompetent abortion providers,” the state argues also that there is a conflict of interest between the physicians and the patients on whose behalf they are suing.
During arguments, Justice Samuel Alito Jr. repeatedly questioned Ms. Rikelman on the plaintiffs’ right to sue, conveying doubt that the plaintiffs were on solid legal ground.
“Would you agree with the general proposition that a party should not be able to sue ostensibly to protect the rights of other people, if there is a real conflict of interest between the party who is suing and those whose rights the party claims to be attempting to defend?” Associate Justice Alito asked during oral arguments.
The hearing ended with no clear picture of how some justices were leaning. Justice Clarence Thomas and Justice Neil Gorsuch remained silent during arguments and asked no questions. Chief Justice John Roberts Jr., and Justice Brett Kavanaugh questioned whether all admitting privileges laws were unconstitutional or if a state-by-state analysis is required. Near the end of the hearing, Justice Stephen Breyer stressed that more research and fact-finding is necessary before the court can reach a decision.
“We’re not going to solve this at oral argument,” he said.
A decision by the Supreme Court is expected by August 2020.
The U.S. Supreme Court will likely decide by the end of the summer whether a controversial Louisiana abortion law that imposes restrictions on physicians can stand.
Justices heard oral arguments March 4, 2020, in June Medicare Services v. Russo, which centers on a Louisiana law requiring physicians who perform abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, while clinics that violate the law can have their licenses revoked, according to the state law, originally passed in 2014. In 2016, the Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, the justices struck down the measure as unconstitutional.
During oral arguments, Julie Rikelman an attorney representing June Medical Services, said that the Louisiana law is identical to the abortion law in Texas, and she argued that justices should reach the same conclusion.
“The district court found this law would leave Louisiana with just one clinic in one state to serve about 10,000 people per year,” Ms. Rikelman said during oral arguments. “That would mean that hundreds of thousands of women would now live more than 150 miles from the closest provider. And the burdens were actually more severe than this court found in Whole Woman’s Health.”
Elizabeth Murrill, solicitor general of Louisiana, argued that the Louisiana law was justified, and that the 5th U.S. Circuit Court of Appeals was correct when it reversed a district court decision and upheld the law.
“The 5th Circuit correctly held that the plaintiffs in this case failed to carry their burden – their heavy burden of proof that is required to facially invalidate a state law,” Ms. Murrill said during oral arguments. “Louisiana’s decision to require abortion providers to have admitting privileges was justified by abundant evidence of life-threatening health and safety violations, malpractice, noncompliance with professional licensing rules, legislative testimony from postabortive women, [and] testimony from doctors who took care of abortion providers’ abandoned patients.”
During arguments, Justice Ruth Bader Ginsburg questioned the reasoning behind the 30-mile privileges rule, expressing doubt at the state’s justification for the requirement. “What sense does the 30-mile limit make, considering that – certainly for medication abortions and for the overwhelming number of other abortions ... if the woman has a problem, it will be her local hospital that ... she will need to go to for the care, not something 30 miles from the clinic.”
Ms. Murrill responded that the Louisiana regulation is consistent with surgery and ambulatory surgery regulations and aligns with the state’s regulatory structure.
“We had evidence in the record of women who did require transfers,” Ms. Murrill said. “[An abortion provider] testified unambiguously that he had to transfer four patients who had punctured uteruses and were hemorrhaging.”
Whether the plaintiffs have standing to sue is a key question. As a general rule, a plaintiff can only sue to protect their own rights, unless the plaintiff has a close relationship with a third party and there are barriers that prevent the third party from suing. Attorneys for Louisiana contend that the plaintiffs – the medical clinic and several physicians – have no right to sue because their rights are not at stake, and that there is no obstacle to patients suing over the law.
Since the Louisiana law is intended to protect women from “unscrupulous and incompetent abortion providers,” the state argues also that there is a conflict of interest between the physicians and the patients on whose behalf they are suing.
During arguments, Justice Samuel Alito Jr. repeatedly questioned Ms. Rikelman on the plaintiffs’ right to sue, conveying doubt that the plaintiffs were on solid legal ground.
“Would you agree with the general proposition that a party should not be able to sue ostensibly to protect the rights of other people, if there is a real conflict of interest between the party who is suing and those whose rights the party claims to be attempting to defend?” Associate Justice Alito asked during oral arguments.
The hearing ended with no clear picture of how some justices were leaning. Justice Clarence Thomas and Justice Neil Gorsuch remained silent during arguments and asked no questions. Chief Justice John Roberts Jr., and Justice Brett Kavanaugh questioned whether all admitting privileges laws were unconstitutional or if a state-by-state analysis is required. Near the end of the hearing, Justice Stephen Breyer stressed that more research and fact-finding is necessary before the court can reach a decision.
“We’re not going to solve this at oral argument,” he said.
A decision by the Supreme Court is expected by August 2020.
The U.S. Supreme Court will likely decide by the end of the summer whether a controversial Louisiana abortion law that imposes restrictions on physicians can stand.
Justices heard oral arguments March 4, 2020, in June Medicare Services v. Russo, which centers on a Louisiana law requiring physicians who perform abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, while clinics that violate the law can have their licenses revoked, according to the state law, originally passed in 2014. In 2016, the Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, the justices struck down the measure as unconstitutional.
During oral arguments, Julie Rikelman an attorney representing June Medical Services, said that the Louisiana law is identical to the abortion law in Texas, and she argued that justices should reach the same conclusion.
“The district court found this law would leave Louisiana with just one clinic in one state to serve about 10,000 people per year,” Ms. Rikelman said during oral arguments. “That would mean that hundreds of thousands of women would now live more than 150 miles from the closest provider. And the burdens were actually more severe than this court found in Whole Woman’s Health.”
Elizabeth Murrill, solicitor general of Louisiana, argued that the Louisiana law was justified, and that the 5th U.S. Circuit Court of Appeals was correct when it reversed a district court decision and upheld the law.
“The 5th Circuit correctly held that the plaintiffs in this case failed to carry their burden – their heavy burden of proof that is required to facially invalidate a state law,” Ms. Murrill said during oral arguments. “Louisiana’s decision to require abortion providers to have admitting privileges was justified by abundant evidence of life-threatening health and safety violations, malpractice, noncompliance with professional licensing rules, legislative testimony from postabortive women, [and] testimony from doctors who took care of abortion providers’ abandoned patients.”
During arguments, Justice Ruth Bader Ginsburg questioned the reasoning behind the 30-mile privileges rule, expressing doubt at the state’s justification for the requirement. “What sense does the 30-mile limit make, considering that – certainly for medication abortions and for the overwhelming number of other abortions ... if the woman has a problem, it will be her local hospital that ... she will need to go to for the care, not something 30 miles from the clinic.”
Ms. Murrill responded that the Louisiana regulation is consistent with surgery and ambulatory surgery regulations and aligns with the state’s regulatory structure.
“We had evidence in the record of women who did require transfers,” Ms. Murrill said. “[An abortion provider] testified unambiguously that he had to transfer four patients who had punctured uteruses and were hemorrhaging.”
Whether the plaintiffs have standing to sue is a key question. As a general rule, a plaintiff can only sue to protect their own rights, unless the plaintiff has a close relationship with a third party and there are barriers that prevent the third party from suing. Attorneys for Louisiana contend that the plaintiffs – the medical clinic and several physicians – have no right to sue because their rights are not at stake, and that there is no obstacle to patients suing over the law.
Since the Louisiana law is intended to protect women from “unscrupulous and incompetent abortion providers,” the state argues also that there is a conflict of interest between the physicians and the patients on whose behalf they are suing.
During arguments, Justice Samuel Alito Jr. repeatedly questioned Ms. Rikelman on the plaintiffs’ right to sue, conveying doubt that the plaintiffs were on solid legal ground.
“Would you agree with the general proposition that a party should not be able to sue ostensibly to protect the rights of other people, if there is a real conflict of interest between the party who is suing and those whose rights the party claims to be attempting to defend?” Associate Justice Alito asked during oral arguments.
The hearing ended with no clear picture of how some justices were leaning. Justice Clarence Thomas and Justice Neil Gorsuch remained silent during arguments and asked no questions. Chief Justice John Roberts Jr., and Justice Brett Kavanaugh questioned whether all admitting privileges laws were unconstitutional or if a state-by-state analysis is required. Near the end of the hearing, Justice Stephen Breyer stressed that more research and fact-finding is necessary before the court can reach a decision.
“We’re not going to solve this at oral argument,” he said.
A decision by the Supreme Court is expected by August 2020.
The fate of the ACA now rests with the U.S. Supreme Court
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
Supreme Court roundup: Latest health care decisions
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
Medical malpractice insurance premiums likely to rise in 2020
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
Private equity firms acquiring more physician group practices
Lead author Jane M. Zhu, MD, of Oregon Health & Science University, Portland, and colleagues examined physician group practice acquisitions by private equity firms using the Irving Levin Associates Health Care M&A data set, which includes manually collected and verified transactional information on health care mergers and acquisitions. Investigators linked acquisitions to the SK&A data set, a commercial data set of verified physicians and practice-level characteristics of U.S. office-based practices.
Of about 18,000 unique group medical practices, private equity firms acquired 355 physician practice acquisitions from 2013 to 2016, a trend that rose from 59 practices in 2013 to 136 practices in 2016, Dr. Zhu and colleagues reported on Feb. 18 , 2020, in a research letter published in JAMA.
Acquired practices had a mean of four sites, 16 physicians in each practice, and 6 physicians affiliated with each site, the data found. Overall, 81% of these medical practices reported accepting new patients, 83% accepted Medicare, and 60% accepted Medicaid. The majority of acquired practices were in the South (44%).
Anesthesiology (19%) and multispecialty (19%) were the most commonly represented medical groups in the acquisitions, followed by emergency medicine (12%), family practice (11%), and dermatology (10%). In addition, from 2015 to 2016, the number of acquired cardiology, ophthalmology, radiology, and ob.gyn. practices increased. Within acquired practices, anesthesiologists represented the majority of all physicians, followed by emergency medicine specialists, family physicians, and dermatologists.
Dr. Zhu and colleagues cited a key limitation: Because the data are based on transactions that have been publicly announced, the acquisition of smaller practices might have been underestimated.
Still, the findings demonstrate that private equity acquisitions of physician medical groups are accelerating across multiple specialties, Dr. Zhu said in an interview.
“From our data, acquired medical groups seem to have relatively large footprints with multiple office sites and multiple physicians, which mirrors a typical investment strategy for these firms,” she said.
Dr. Zhu said that more research is needed about how these purchases affect practice patterns, delivery of care, and clinician behavior. Private equity firms expect greater than 20% annual returns, and such financial incentives may conflict with the need for longer-term investments in practice stability, physician recruitment, quality, and safety, according to the study.
“In theory, there may be greater efficiencies introduced from private equity investment – for example, through administrative and billing efficiencies, reorganizing practice structures, or strengthening technology supports,” Dr. Zhu said. “But because of private equity firms’ emphasis on return on investment, there may be unintended consequences of these purchases on practice stability and patient care. We don’t yet know what these effects will be, and we need robust, longitudinal data to investigate this question.”
Dr. Zhu and colleagues reported that they had no disclosures.
SOURCE: Zhu JM et al. JAMA. 2020 Feb 18;323(17):663-5.
Lead author Jane M. Zhu, MD, of Oregon Health & Science University, Portland, and colleagues examined physician group practice acquisitions by private equity firms using the Irving Levin Associates Health Care M&A data set, which includes manually collected and verified transactional information on health care mergers and acquisitions. Investigators linked acquisitions to the SK&A data set, a commercial data set of verified physicians and practice-level characteristics of U.S. office-based practices.
Of about 18,000 unique group medical practices, private equity firms acquired 355 physician practice acquisitions from 2013 to 2016, a trend that rose from 59 practices in 2013 to 136 practices in 2016, Dr. Zhu and colleagues reported on Feb. 18 , 2020, in a research letter published in JAMA.
Acquired practices had a mean of four sites, 16 physicians in each practice, and 6 physicians affiliated with each site, the data found. Overall, 81% of these medical practices reported accepting new patients, 83% accepted Medicare, and 60% accepted Medicaid. The majority of acquired practices were in the South (44%).
Anesthesiology (19%) and multispecialty (19%) were the most commonly represented medical groups in the acquisitions, followed by emergency medicine (12%), family practice (11%), and dermatology (10%). In addition, from 2015 to 2016, the number of acquired cardiology, ophthalmology, radiology, and ob.gyn. practices increased. Within acquired practices, anesthesiologists represented the majority of all physicians, followed by emergency medicine specialists, family physicians, and dermatologists.
Dr. Zhu and colleagues cited a key limitation: Because the data are based on transactions that have been publicly announced, the acquisition of smaller practices might have been underestimated.
Still, the findings demonstrate that private equity acquisitions of physician medical groups are accelerating across multiple specialties, Dr. Zhu said in an interview.
“From our data, acquired medical groups seem to have relatively large footprints with multiple office sites and multiple physicians, which mirrors a typical investment strategy for these firms,” she said.
Dr. Zhu said that more research is needed about how these purchases affect practice patterns, delivery of care, and clinician behavior. Private equity firms expect greater than 20% annual returns, and such financial incentives may conflict with the need for longer-term investments in practice stability, physician recruitment, quality, and safety, according to the study.
“In theory, there may be greater efficiencies introduced from private equity investment – for example, through administrative and billing efficiencies, reorganizing practice structures, or strengthening technology supports,” Dr. Zhu said. “But because of private equity firms’ emphasis on return on investment, there may be unintended consequences of these purchases on practice stability and patient care. We don’t yet know what these effects will be, and we need robust, longitudinal data to investigate this question.”
Dr. Zhu and colleagues reported that they had no disclosures.
SOURCE: Zhu JM et al. JAMA. 2020 Feb 18;323(17):663-5.
Lead author Jane M. Zhu, MD, of Oregon Health & Science University, Portland, and colleagues examined physician group practice acquisitions by private equity firms using the Irving Levin Associates Health Care M&A data set, which includes manually collected and verified transactional information on health care mergers and acquisitions. Investigators linked acquisitions to the SK&A data set, a commercial data set of verified physicians and practice-level characteristics of U.S. office-based practices.
Of about 18,000 unique group medical practices, private equity firms acquired 355 physician practice acquisitions from 2013 to 2016, a trend that rose from 59 practices in 2013 to 136 practices in 2016, Dr. Zhu and colleagues reported on Feb. 18 , 2020, in a research letter published in JAMA.
Acquired practices had a mean of four sites, 16 physicians in each practice, and 6 physicians affiliated with each site, the data found. Overall, 81% of these medical practices reported accepting new patients, 83% accepted Medicare, and 60% accepted Medicaid. The majority of acquired practices were in the South (44%).
Anesthesiology (19%) and multispecialty (19%) were the most commonly represented medical groups in the acquisitions, followed by emergency medicine (12%), family practice (11%), and dermatology (10%). In addition, from 2015 to 2016, the number of acquired cardiology, ophthalmology, radiology, and ob.gyn. practices increased. Within acquired practices, anesthesiologists represented the majority of all physicians, followed by emergency medicine specialists, family physicians, and dermatologists.
Dr. Zhu and colleagues cited a key limitation: Because the data are based on transactions that have been publicly announced, the acquisition of smaller practices might have been underestimated.
Still, the findings demonstrate that private equity acquisitions of physician medical groups are accelerating across multiple specialties, Dr. Zhu said in an interview.
“From our data, acquired medical groups seem to have relatively large footprints with multiple office sites and multiple physicians, which mirrors a typical investment strategy for these firms,” she said.
Dr. Zhu said that more research is needed about how these purchases affect practice patterns, delivery of care, and clinician behavior. Private equity firms expect greater than 20% annual returns, and such financial incentives may conflict with the need for longer-term investments in practice stability, physician recruitment, quality, and safety, according to the study.
“In theory, there may be greater efficiencies introduced from private equity investment – for example, through administrative and billing efficiencies, reorganizing practice structures, or strengthening technology supports,” Dr. Zhu said. “But because of private equity firms’ emphasis on return on investment, there may be unintended consequences of these purchases on practice stability and patient care. We don’t yet know what these effects will be, and we need robust, longitudinal data to investigate this question.”
Dr. Zhu and colleagues reported that they had no disclosures.
SOURCE: Zhu JM et al. JAMA. 2020 Feb 18;323(17):663-5.
FROM JAMA
WHO declares public health emergency for novel coronavirus
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
HHS: Coronavirus risk low in U.S., vaccine development underway
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
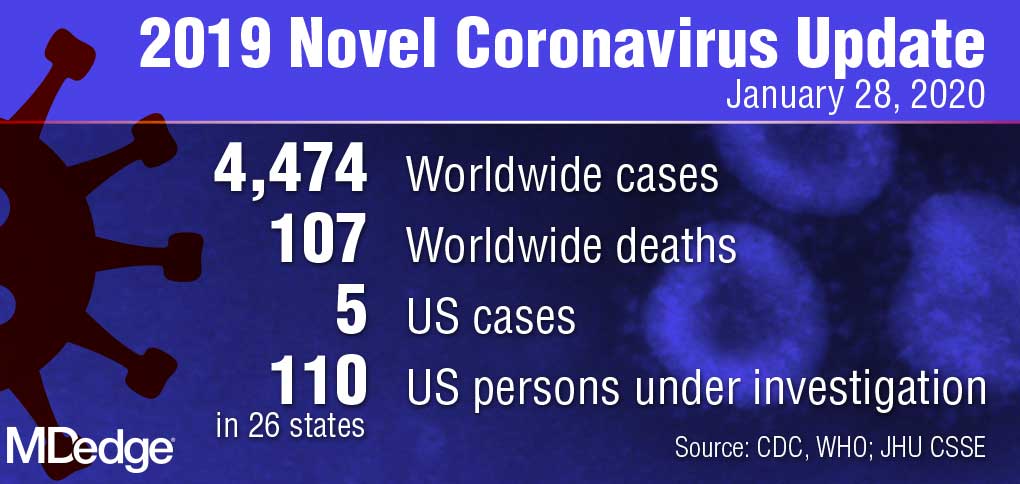
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
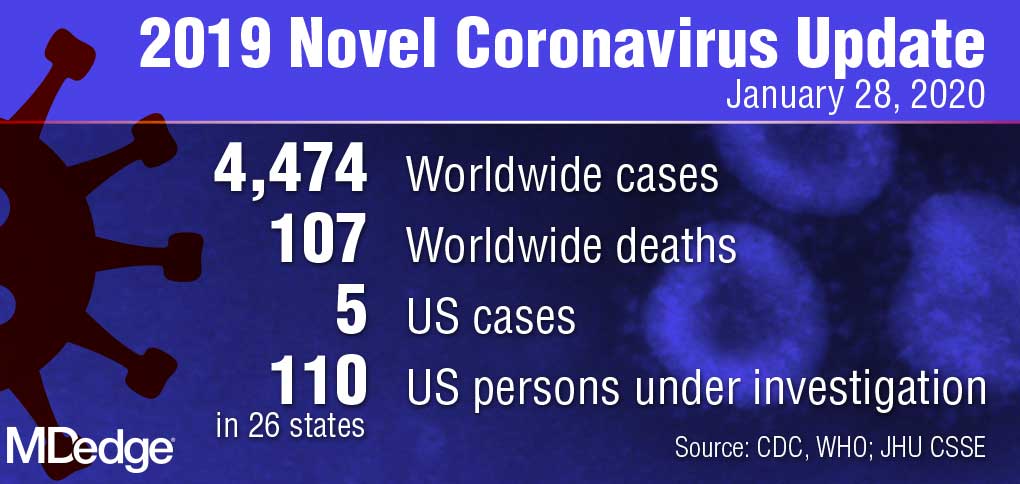
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
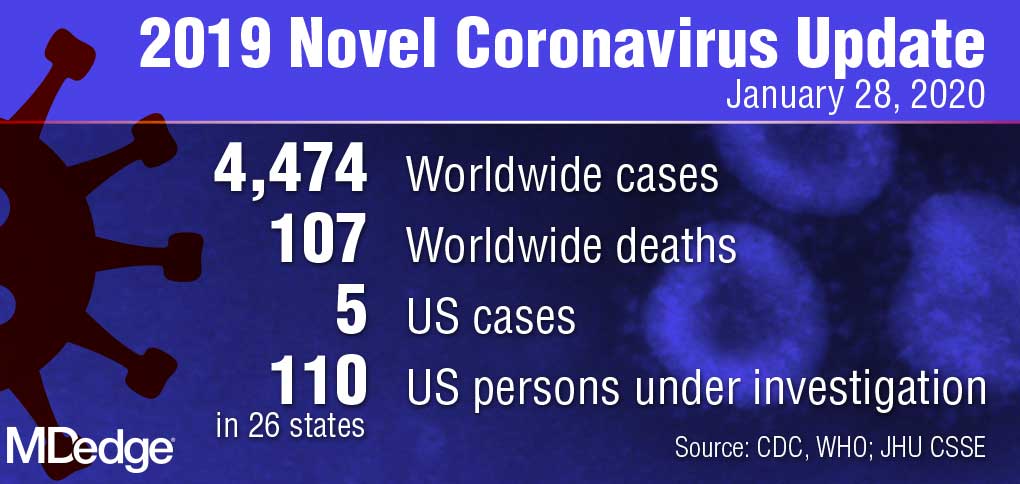
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.
Doctor wins $4.75 million award in defamation suit against hospital
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Your colleague appears depressed. Now what?
Encountering a colleague who appears depressed or suicidal can be challenging, but experts say the worst thing you can do is turn away.
, professor of clinical psychiatry at State University of New York, Brooklyn. “Don’t leave it to ‘the other guy.’ ”
Below, Dr. Myers and other experts offer advice on how to approach a fellow physician who seems depressed or might be in need of professional help.
1. Reach out to the colleague, and find a private, quiet space to talk.
2. Let them know you’re there for them, and do not pass judgment.
3. Share a short list of reasons for your concerns. For example, “It seems you have lost some weight,” or “You seem sad a lot of the time.”
4. Encourage them to accept help. Refrain from giving them a list of names for professional help. Instead, make the phone call for them or set up the appointment, if necessary.
5. Ask specifically about suicidal ideation. For instance, “Are you having thoughts of hurting yourself?” or “Are you having thoughts of ending your life?” People who are suicidal often want someone to ask and help.
6. Stay with the colleague until he or she has worked out a plan of safety – for example, returned to family/loved ones, visited a physician or mental health professional, gone to an emergency department, or called for an ambulance or other assistance.
7. Accompany the colleague to the emergency department or call 911.
8. Remember these two goals: Inquire about safety/danger. Ensure safety of the individual.
Sources: Dr. Myers, Dr. Zisook, and Dr. Yellowlees.
For more information, contact the American Foundation for Suicide Prevention (www.afsp.org), and the 24-hour crisis line: 1-800-273-TALK (8255). Late last year, the Federal Communications Commission approved plans to designate 988 as a suicide prevention hotline number. Implementation of the proposal is expected to take several months.
Encountering a colleague who appears depressed or suicidal can be challenging, but experts say the worst thing you can do is turn away.
, professor of clinical psychiatry at State University of New York, Brooklyn. “Don’t leave it to ‘the other guy.’ ”
Below, Dr. Myers and other experts offer advice on how to approach a fellow physician who seems depressed or might be in need of professional help.
1. Reach out to the colleague, and find a private, quiet space to talk.
2. Let them know you’re there for them, and do not pass judgment.
3. Share a short list of reasons for your concerns. For example, “It seems you have lost some weight,” or “You seem sad a lot of the time.”
4. Encourage them to accept help. Refrain from giving them a list of names for professional help. Instead, make the phone call for them or set up the appointment, if necessary.
5. Ask specifically about suicidal ideation. For instance, “Are you having thoughts of hurting yourself?” or “Are you having thoughts of ending your life?” People who are suicidal often want someone to ask and help.
6. Stay with the colleague until he or she has worked out a plan of safety – for example, returned to family/loved ones, visited a physician or mental health professional, gone to an emergency department, or called for an ambulance or other assistance.
7. Accompany the colleague to the emergency department or call 911.
8. Remember these two goals: Inquire about safety/danger. Ensure safety of the individual.
Sources: Dr. Myers, Dr. Zisook, and Dr. Yellowlees.
For more information, contact the American Foundation for Suicide Prevention (www.afsp.org), and the 24-hour crisis line: 1-800-273-TALK (8255). Late last year, the Federal Communications Commission approved plans to designate 988 as a suicide prevention hotline number. Implementation of the proposal is expected to take several months.
Encountering a colleague who appears depressed or suicidal can be challenging, but experts say the worst thing you can do is turn away.
, professor of clinical psychiatry at State University of New York, Brooklyn. “Don’t leave it to ‘the other guy.’ ”
Below, Dr. Myers and other experts offer advice on how to approach a fellow physician who seems depressed or might be in need of professional help.
1. Reach out to the colleague, and find a private, quiet space to talk.
2. Let them know you’re there for them, and do not pass judgment.
3. Share a short list of reasons for your concerns. For example, “It seems you have lost some weight,” or “You seem sad a lot of the time.”
4. Encourage them to accept help. Refrain from giving them a list of names for professional help. Instead, make the phone call for them or set up the appointment, if necessary.
5. Ask specifically about suicidal ideation. For instance, “Are you having thoughts of hurting yourself?” or “Are you having thoughts of ending your life?” People who are suicidal often want someone to ask and help.
6. Stay with the colleague until he or she has worked out a plan of safety – for example, returned to family/loved ones, visited a physician or mental health professional, gone to an emergency department, or called for an ambulance or other assistance.
7. Accompany the colleague to the emergency department or call 911.
8. Remember these two goals: Inquire about safety/danger. Ensure safety of the individual.
Sources: Dr. Myers, Dr. Zisook, and Dr. Yellowlees.
For more information, contact the American Foundation for Suicide Prevention (www.afsp.org), and the 24-hour crisis line: 1-800-273-TALK (8255). Late last year, the Federal Communications Commission approved plans to designate 988 as a suicide prevention hotline number. Implementation of the proposal is expected to take several months.