User login
ED visits up for acute pancreatitis linked to younger age, alcohol, chronic disease
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
Predicting early outcomes in DLBCL
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
Fracture risk linked to mortality in women with myeloma
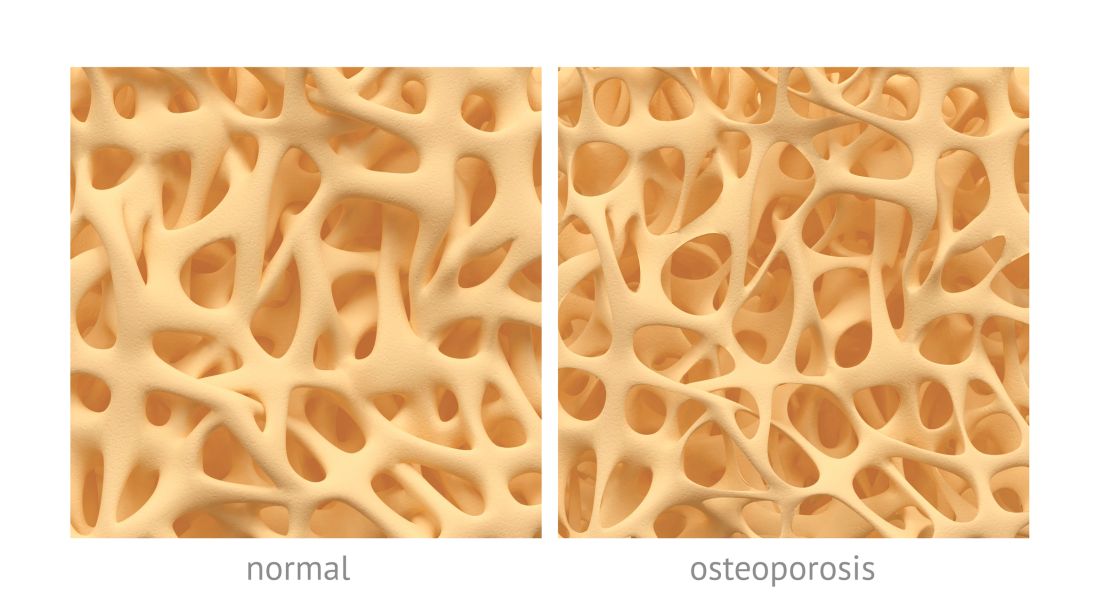
Preexisting osteoporosis is an important risk factor for mortality risk in cancer-free postmenopausal women who go on to develop multiple myeloma, results of a recent analysis suggest.
High fracture risk was associated with an increased risk of death, independent of other clinical risk factors, in this analysis of postmenopausal women in the Women’s Health Initiative (WHI) data set.
The findings help define osteoporosis as an important prognostic factor associated with mortality in postmenopausal women who develop myeloma, according to study author Ashley E. Rosko, MD, of Ohio State University, Columbus, and her colleagues.
“Osteoporosis is highly prevalent in aging adults, and very little is known on how this comorbid condition contributes to outcomes in individuals who develop myeloma,” wrote Dr. Rosko and her coauthors. Their report is in the journal Clinical Lymphoma, Myeloma and Leukemia.
The analysis involved 362 women in the WHI data set who developed myeloma and had no history of any cancer at baseline. Women in the WHI were between 50 and 79 years of age and postmenopausal at baseline when originally recruited at 40 U.S. centers between 1993 and 1998.
Dr. Rosko and her colleagues calculated bone health for women in the data set using the Fracture Risk Assessment Tool (FRAX), a web-based tool that calculates 10-year probability of hip and other major osteoporotic fractures.
Of the 362 women who developed myeloma, 98 were classified as having high FRAX scores, defined as a 10-year probability of 3% or greater for hip fracture, or 20% or greater for other major osteoporosis-related fractures.
With a median follow-up of 10.5 years, the adjusted risk of death was elevated in women with high FRAX scores, according to investigators, with a covariate-adjusted hazard ratio of 1.51 (95% confidence interval, 1.01-2.25; P = .044) versus women with low FRAX scores.
Of the 362 patients who developed myeloma, 226 died during the follow-up period. That included 71 women with high FRAX scores, or 72% of that subset; and 155 women with low FRAX scores, or 59% of that subset, investigators reported.
These findings suggest osteoporosis is an “important comorbidity” in women who develop multiple myeloma, Dr. Rosko and her coauthors said in a discussion of the study results.
“Recognizing osteoporosis as a risk factor associated with multiple myeloma mortality is an important prognostic factor in postmenopausal women,” they said.
This investigation was supported in part by the National Cancer Institute. The researchers reported having no relevant financial disclosures.
SOURCE: Rosko AE et al. Clin Lymphoma Myeloma Leuk. 2018 Sep;18(9):597-602.e1.
Preexisting osteoporosis is an important risk factor for mortality risk in cancer-free postmenopausal women who go on to develop multiple myeloma, results of a recent analysis suggest.
High fracture risk was associated with an increased risk of death, independent of other clinical risk factors, in this analysis of postmenopausal women in the Women’s Health Initiative (WHI) data set.
The findings help define osteoporosis as an important prognostic factor associated with mortality in postmenopausal women who develop myeloma, according to study author Ashley E. Rosko, MD, of Ohio State University, Columbus, and her colleagues.
“Osteoporosis is highly prevalent in aging adults, and very little is known on how this comorbid condition contributes to outcomes in individuals who develop myeloma,” wrote Dr. Rosko and her coauthors. Their report is in the journal Clinical Lymphoma, Myeloma and Leukemia.
The analysis involved 362 women in the WHI data set who developed myeloma and had no history of any cancer at baseline. Women in the WHI were between 50 and 79 years of age and postmenopausal at baseline when originally recruited at 40 U.S. centers between 1993 and 1998.
Dr. Rosko and her colleagues calculated bone health for women in the data set using the Fracture Risk Assessment Tool (FRAX), a web-based tool that calculates 10-year probability of hip and other major osteoporotic fractures.
Of the 362 women who developed myeloma, 98 were classified as having high FRAX scores, defined as a 10-year probability of 3% or greater for hip fracture, or 20% or greater for other major osteoporosis-related fractures.
With a median follow-up of 10.5 years, the adjusted risk of death was elevated in women with high FRAX scores, according to investigators, with a covariate-adjusted hazard ratio of 1.51 (95% confidence interval, 1.01-2.25; P = .044) versus women with low FRAX scores.
Of the 362 patients who developed myeloma, 226 died during the follow-up period. That included 71 women with high FRAX scores, or 72% of that subset; and 155 women with low FRAX scores, or 59% of that subset, investigators reported.
These findings suggest osteoporosis is an “important comorbidity” in women who develop multiple myeloma, Dr. Rosko and her coauthors said in a discussion of the study results.
“Recognizing osteoporosis as a risk factor associated with multiple myeloma mortality is an important prognostic factor in postmenopausal women,” they said.
This investigation was supported in part by the National Cancer Institute. The researchers reported having no relevant financial disclosures.
SOURCE: Rosko AE et al. Clin Lymphoma Myeloma Leuk. 2018 Sep;18(9):597-602.e1.
Preexisting osteoporosis is an important risk factor for mortality risk in cancer-free postmenopausal women who go on to develop multiple myeloma, results of a recent analysis suggest.
High fracture risk was associated with an increased risk of death, independent of other clinical risk factors, in this analysis of postmenopausal women in the Women’s Health Initiative (WHI) data set.
The findings help define osteoporosis as an important prognostic factor associated with mortality in postmenopausal women who develop myeloma, according to study author Ashley E. Rosko, MD, of Ohio State University, Columbus, and her colleagues.
“Osteoporosis is highly prevalent in aging adults, and very little is known on how this comorbid condition contributes to outcomes in individuals who develop myeloma,” wrote Dr. Rosko and her coauthors. Their report is in the journal Clinical Lymphoma, Myeloma and Leukemia.
The analysis involved 362 women in the WHI data set who developed myeloma and had no history of any cancer at baseline. Women in the WHI were between 50 and 79 years of age and postmenopausal at baseline when originally recruited at 40 U.S. centers between 1993 and 1998.
Dr. Rosko and her colleagues calculated bone health for women in the data set using the Fracture Risk Assessment Tool (FRAX), a web-based tool that calculates 10-year probability of hip and other major osteoporotic fractures.
Of the 362 women who developed myeloma, 98 were classified as having high FRAX scores, defined as a 10-year probability of 3% or greater for hip fracture, or 20% or greater for other major osteoporosis-related fractures.
With a median follow-up of 10.5 years, the adjusted risk of death was elevated in women with high FRAX scores, according to investigators, with a covariate-adjusted hazard ratio of 1.51 (95% confidence interval, 1.01-2.25; P = .044) versus women with low FRAX scores.
Of the 362 patients who developed myeloma, 226 died during the follow-up period. That included 71 women with high FRAX scores, or 72% of that subset; and 155 women with low FRAX scores, or 59% of that subset, investigators reported.
These findings suggest osteoporosis is an “important comorbidity” in women who develop multiple myeloma, Dr. Rosko and her coauthors said in a discussion of the study results.
“Recognizing osteoporosis as a risk factor associated with multiple myeloma mortality is an important prognostic factor in postmenopausal women,” they said.
This investigation was supported in part by the National Cancer Institute. The researchers reported having no relevant financial disclosures.
SOURCE: Rosko AE et al. Clin Lymphoma Myeloma Leuk. 2018 Sep;18(9):597-602.e1.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Key clinical point:
Major finding: Risk of death was elevated in women at high risk of fracture (covariate-adjusted hazard ratio, 1.51; 95% confidence interval, 1.01-2.25; P = .044) versus women with low fracture risk.
Study details: Retrospective analysis of the Women’s Health Initiative data set including 362 postmenopausal women who were cancer free at baseline and developed myeloma over the course of study follow-up.
Disclosures: The analysis was supported in part by the National Cancer Institute. The researchers reported having no relevant financial disclosures.
Source: Rosko AE et al. Clin Lymphoma Myeloma Leuk. 2018 Sep;18(9):597-602.e1.
Declining lung function linked to heart failure, stroke
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Rapid declines in spirometric measures of lung function were associated with higher risks of heart failure, among other adverse cardiovascular outcomes.
Major finding: Rapid decline in forced expiratory volume in 1 second was associated with higher risk of incident heart failure (HR, 1.17; 95% CI, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01).
Study details: An analysis including a total of 10,351 participants in a large, prospective cohort study with a mean follow-up of 17 years.
Disclosures: The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
Source: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
ctDNA predicts early outcomes in DLBCL
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to authors of a recent prospective study.
Pretreatment ctDNA levels predicted 24-month event-free survival – an important disease milestone in DLBCL – as well as overall survival in the study, which included more than 200 patients at six institutions in North America and Europe.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy, according to corresponding author Ash A. Alizadeh, MD, PhD, of Stanford (Calif.) University and his coinvestigators.
“Our data suggest that both pretreatment and dynamic assessments of ctDNA are feasible and can add to established risk factors,” Dr. Alizadeh and his coauthors reported in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, they wrote in the report.
In an evaluation of pretreatment ctDNA levels, investigators found a 2.5 log haploid genome equivalents per milliliter (hGE/mL) threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P = .007) for frontline treatment and 2.9 (P = 0.01) for salvage.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy, according to investigators. An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P = .0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P less than .001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival, according to investigators.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index (IPI) and interim PET/CT studies, results of multivariable analysis showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, and conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
SOURCE: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Early molecular response (a 2-log decrease in ctDNA levels after one treatment cycle) was associated with a 24-month event-free survival of 83% versus 50% for no early molecular response (P = .0015).
Study details: Prospective analysis of pretreatment and dynamic on-treatment ctDNA levels in patients with DLBCL who received standard immunochemotherapy.
Disclosures: Study authors reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, among others.
Source: Kurtz DM et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.78.5246.
Nivolumab plus ipilimumab effective in melanoma brain metastases
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
These data show that checkpoint inhibitors can be similarly effective in CNS metastases as they can be in extracranial metastases related to melanoma, according to Samra Turajlic, MD, PhD, and James Larkin, FRCP, PhD, of the Renal and Skin Units at the Royal Marsden National Health Service Foundation Trust in London.
Based on the study results, larger trials are warranted, including patients with CNS metastases from melanoma, kidney, lung, and other cancers where checkpoint inhibitors have demonstrated efficacy, Dr. Turajlic, who is also with the Translational Cancer Therapeutics Laboratory at the Francis Crick Institute in London, and Dr. Larkin wrote in an editorial.
“Such patients should no longer generally be excluded from clinical trials,” they wrote.
While the study by Dr. Tawbi and his colleagues was small, they added, its results are relevant to clinical practice because of the high rate of response, rapid response time, and side effect profile, which was manageable.
In fact, the nivolumab plus ipilimumab regimen described in this study should be considered first-line therapy for all patients who meet the study’s inclusion criteria, they asserted.
However, the results should “absolutely not” be extrapolated to higher-risk patients, such as those with leptomeningeal disease or with low performance status, which investigators excluded from the present study.
“There are good data showing that patients with cerebral metastases can be stratified into groups that have very different survival and morbidity,” Dr. Turajlic and Dr. Larkin wrote. “Caution is necessary until we have data across all the groups.”
These comment are based on an editorial in the New England Journal of Medicine (doi: 10.1056/NEJMe1807752) . Dr. Turajlic reported patents pending for an indel biomarker (PCT/GB2018/051893) and an indel therapeutic (PCT/GB2018/051892). Dr. Larkin reported disclosures related to Bristol-Myers Squibb, Novartis, Genentech, Pierre-Fabre, Incyte, and AstraZeneca.
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
Treatment with nivolumab plus ipilimumab resulted in clinically meaningful efficacy for melanoma patients with asymptomatic, previously untreated brain metastases, results of an open-label, multicenter, phase 2 study have shown.
The combination of these two immune checkpoint inhibitors produced intracranial responses in more than half of the patients treated, and perhaps more importantly, according to the study investigators, the combination treatment prevented intracranial progression for more than 6 months in 64% of the study population.
“These results are relevant in a population in whom progression can quickly result in substantial neurologic symptoms, functional impairment, and the need for glucocorticoid therapy,” the study investigators wrote in the New England Journal of Medicine.
The investigators, led by Hussein A. Tawbi, MD, PhD, of the University of Texas MD Anderson Cancer, Houston, initially enrolled 101 patients with histologically confirmed melanoma and metastases to the brain that were asymptomatic. All patients had an Eastern Cooperative Oncology Group performance status of 0-1 and had not received systemic glucocorticoid therapy within 10 days of study treatment.
The primary endpoint of the study was the rate of intracranial benefit, defined as the percentage of patients with complete response, partial response, or stable disease for at least 6 months after starting treatment.
For 94 patients with at least 6 months of follow-up at the time of analysis (median follow-up, 14 months), the rate of intracranial benefit was 57%, including complete responses in 26%, partial responses in 30%, and stable disease in 2%, the investigators reported. The rate of extracranial benefit was similar, at 56%.
The 6-month rate of progression-free survival was 64.2% for intracranial assessments, while the 6-month overall survival rate was 92.3%, according to results of an initial assessment.
Grade 3 or 4 adverse events thought to be related to treatment occurred in 55% of patients and led to treatment discontinuation in 20%; the most common were increased levels of ALT and AST.
Dr. Tawbi and his colleagues said that, while cross-trial comparisons have inherent limitations, the rate of intracranial response seen in this trial is similar to what was seen in the COMBI-MB study of dabrafenib plus trametinib in patients with BRAF-mutant melanoma and brain metastases. However, in that study, published in 2017 in the Lancet, the combination of a BRAF inhibitor and MEK inhibitor had rates of intracranial response and progression-free survival that were “substantially shorter” than the rates of extracranial response and progression-free survival.
“In our study, the use of immunotherapy seemed capable of inducing intracranial responses that were very similar to extracranial responses in character, depth, and duration,” they wrote.
Dr. Tawbi and his coinvestigators enrolled an additional 20 symptomatic patients with brain metastases following a study protocol amendment; however, results from that cohort are not being reported yet because of inadequate follow-up length, they said.
The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. Dr. Tawbi reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, and Novartis. His coauthors reported additional disclosures related to MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, and Eisai, among others.
SOURCE: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Nivolumab plus ipilimumab resulted in clinically meaningful responses and progression-free survival for melanoma patients with asymptomatic, previously untreated brain metastases.
Major finding: The reported rate of intracranial benefit was 57% of patients, including complete responses in 26%, partial responses in 30%, and stable disease for at least 6 months in 2%.
Study details: An open-label, multicenter, phase 2 study initially enrolling 101 patients with histologically confirmed melanoma and metastases to the brain.
Disclosures: The study was supported by Bristol-Myers Squibb and a grant from the National Cancer Institute. The study authors reported disclosures related to Bristol-Myers Squibb, Merck, Genentech, Novartis, MedImmune, AstraZeneca, Dynavax Technologies, Genoptix, Exelixis, Acceleron Pharma, Eisai, and others.
Source: Tawbi HA et al. N Engl J Med. 2018 Aug 23. doi: 10.1056/NEJMoa1805453.
Sunitinib alone not inferior to nephrectomy-sunitinib in metastatic RCC
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
The finding of the CARMENA trial that sunitinib was not inferior to nephrectomy should not lead to the abandonment of nephrectomy, according to Robert J. Motzer, MD, and Paul Russo, MD.
Instead, the results emphasize the importance of carefully selecting patients for nephrectomy based on published risk models, Dr. Motzer and Dr. Russo wrote in an editorial.
“We think that nephrectomy in properly chosen patients with metastatic renal cell carcinoma remains an essential component of care,” they said.
It is not surprising that the CARMENA study met its noninferiority endpoint, as it was “heavily weighted” toward poor-risk patients, they added.
Over an 8-year period, 79 European centers enrolled 450 patients out of 576 patients planned, or just 0.7 patients per site per year.
“This slow and incomplete enrollment raises the possibility that many centers saw few patients with stage IV disease, or that when surgeons saw patients with intermediate-risk disease who were likely to benefit from combination therapy, they were unwilling for them to undergo randomization and instead treated them outside the trial,” they wrote.
Over the same time frame at Dr. Motzer’s and Dr. Russo’s center, there were 189 patients with stage IV disease, or about 24 patients each year.
“We took care to avoid operating on poor-risk patients with extensive metastatic disease, instead focusing on intermediate-risk patients,” they explained in their editorial.
Dr. Motzer and Dr. Russo are with Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College in New York. These comments come from their editorial in the New England Journal of Medicine. Dr. Russo had nothing to disclose. Dr. Motzer reported disclosures related to Genentech/Roche, Pfizer, Novartis, Exelixis, Eisai, Bristol-Myers Squibb, and Merck outside the submitted work.
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
Sunitinib alone was not inferior to nephrectomy followed by sunitinib in patients with metastatic, clear cell renal cell carcinoma (RCC), according to results of the randomized, phase 3 CARMENA trial.
Overall survival was not inferior in the sunitinib arm of the trial, which comprised 450 patients who were suitable candidates for nephrectomy and had MSKCC intermediate or poor risk disease.
These findings contrast with those of previous retrospective studies suggesting patients undergoing nephrectomy who were treated with targeted therapies had an overall survival benefit, according to Bernard Escudier, MD, of Gustave Roussy Institute, Villejuif, France, and his coauthors.
“Given the many approved options for systemic targeted therapy that are now available, the reassessment of the role of surgery in disease management is important,” Dr. Escudier and his colleagues noted. The report is in the New England Journal of Medicine.
The CARMENA trial enrolled 450 out of a planned 576 patients in 79 European centers between September 2009 and September 2017. A total of 226 were randomized to sunitinib alone and 224 to nephrectomy and sunitinib.
With a median follow-up of 50.9 months and 326 deaths, the hazard ratio for death was 0.89 (95% confidence interval, 0.71-1.10). The upper boundary of the 95% CI for noninferiority was 1.20, according to the report.
Median overall survival was 18.4 months for the sunitinib alone arm, and 13.9 months for the nephrectomy-plus-sunitinib arm. While the study was statistically underpowered because of incomplete enrollment, that “trend in longer overall survival” supports the findings favoring sunitinib alone in this noninferiority trial, the authors noted.
Safety results were as expected based on previous trial results, according to the investigators. Grade 3/4 adverse events occurred in 91 patients (42.7%) in the sunitinib group, and 61 (32.8%) in the nephrectomy-sunitinib group, they reported. Nine patients in the sunitinib group had grade 3/4 renal or urinary tract disorders, versus 1 in the nephrectomy-sunitinib group (P = .051).
These findings confirm current clinical practice guidelines on the use of systemic targeted therapy in patients with poor-risk metastatic RCC, according to the authors.
However, targeted therapy in this setting has evolved considerably since the CARMENA trial was designed.
Sunitinib remains one of the most commonly used treatments in patients with good or intermediate prognosis metastatic RCC; however, recent randomized trials show the superiority of the c-MET inhibitor cabozantinib and the immune checkpoint inhibitor combination of nivolumab plus ipilimumab over sunitinib.
Those newer agents will likely become initial treatment options for intermediate- and poor-risk groups, according to the authors.
Both cabozantinib and nivolumab plus ipilimumab are listed as first-line treatment options for intermediate- and poor-risk patients in the most recent clinical practice guidelines from the National Comprehensive Cancer Network.
Nephrectomy may have a role for symptom control in some patients with metastatic RCC, based on results of previous retrospective studies suggesting benefit.
“There is no ‘one size fits all’ approach,” Dr. Escudier and his coauthors wrote. “The multimodal approach of individualized treatment provides appropriate management of metastatic renal-cell carcinoma.”
Dr. Escudier reported personal fees from Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche outside the submitted work. Coauthors reported disclosures with Bayer, MSD, Janssen, Astellas, Bouchara, Ferring, and others.
SOURCE: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Sunitinib alone was not inferior to nephrectomy plus sunitinib in patients with MSKCC intermediate- or poor-risk metastatic, clear cell renal cell carcinoma (RCC) who were suitable candidates for nephrectomy.
Major finding: Overall survival was not inferior in the sunitinib arm of the trial.
Study details: A randomized phase 3 trial involving 450 patients with metastatic clear-cell RCC who were suitable candidates for nephrectomy.
Disclosures: The authors reported disclosures related to Bristol-Myers Squibb, EUSA Pharma, Ipsen, Novartis, Pfizer, and Roche, among others.
Source: Méjean A et al. N Engl J Med. 2018 Aug 2. doi: 10.1056/NEJMoa1803675.
High-sensitivity cardiac troponin levels linked to cardiovascular outcomes in COPD patients
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
The current study data are “robust” and suggest a strong association between high-sensitivity cardiac troponin values and cardiovascular event risk in these COPD patients, according to authors of an editorial.
The study also showed that a change in high-sensitivity cardiac troponin at 3 months is associated with increased risk, noted editorial authors Allan S. Jaffe, MD, and H. Ari Jaffe, MD.
“Most of these events probably represent acceleration of atherosclerosis, given the effects of smoking on atherosclerotic disease and its progression,” the authors said in the Journal of the American College of Cardiology.
However, study authors could have more extensively addressed how to use that information to improve the care of COPD patients at elevated cardiovascular event risk, they added.
A “pilot algorithm” that could be used to apply this biomarker analysis in clinical practice was proposed in an editorial accompanying the research report.
They suggest repeating high-sensitivity cardiac troponin measurements to reduce variability, as well as repeating samples at 3 months to detect changes that could signal increased risk.
“In addition, one should avoid decisions based on small differences,” they wrote.
Allan S. Jaffe, MD, is with the department of cardiovascular medicine and the department of laboratory medicine and pathology at the Mayo Clinic in Rochester, Minn. He reported serving as a consultant for Beckman, Abbott, Siemens, ET Healthcare, Sphingotec, Becton Dickinson, Quindel, and Novartis. H. Ari Jaffe, MD, is with the department of medicine, pulmonary division at University of Illinois at Chicago, Jesse Brown VA Medicine Center, Chicago. He reported he has no relationships to disclose relevant to the contents of the editorial.
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
, according to a post-hoc analysis of a clinical trial.
An increased risk of cardiovascular adverse events and cardiovascular death was seen in COPD patients in the highest quintile of plasma cardiac troponin concentrations at baseline, results of the analysis show.
The findings highlight the potential utility of high-sensitivity cardiac troponin in both clinical trials and clinical practice, according to researcher Nicholas L. Mills, MD, PhD, BHF/University Centre for Cardiovascular Science, The University of Edinburgh, Scotland, and co-investigators.
“Recognizing the risk associated with increased troponin concentrations might encourage clinicians to address cardiovascular risk due to lifestyle choices, and make patients more likely to engage with these recommendations,” Dr. Mills and co-authors wrote in the Journal of the American College of Cardiology.
Improved risk stratification may also help clinicians more appropriately target the use of preventive medications in COPD patients, they added in the report.
The analysis by Dr. Mills and colleagues was based on assessment of cardiac troponin I concentrations for patients in SUMMIT, a randomized trial assessing inhaled corticosteroids and long-acting beta agonists in COPD patients with ele-vated cardiovascular risk.
A total of 1,599 patients in the SUMMIT trial had a baseline cardiac troponin I assessment, and 1,258 had a follow-up assessment at 3 months following randomization.
Compared with those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event, even after adjusting for confounding variables (hazard ratio, 3.67; 95% confidence interval, 1.33-10.13; P = .012)..
Increased risk of cardiovascular death was also seen in the highest quintile as compared with the lowest quintile (HR, 20.06; 95% CI, 2.44-165.15; P = .005), investigators said.
There was no difference in risk of COPD exacerbations between the highest and lowest quintiles, they added.
At 3 months, there were no differences in troponin concentrations related to COPD treatment, consistent with previous observations in the SUMMIT trial that treatment did not impact the cardiovascular composite endpoint, investigators said.
However, patients with a plasma troponin of 5 ng/L or greater recorded at either the baseline or 3-month assessment had an increased rate of the composite cardiovascular endpoint and a “markedly increased” risk of cardiovascular death, they wrote.
The research was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship received by Dr. Mills. Disclosures reported by Dr. Mills included consultancy, research grants, and speaker fees from Abbott Diagnostics, Roche, and Singulex. Study co-authors reported disclosures related to GlaxoSmithKline, Veramed Limited, AstraZeneca, Zambon, Bayer, Novartis, and others.
SOURCE: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: In patients with COPD and heightened cardiovascular risk, high levels of high-sensitivity cardiac troponin were strongly associated with risk of cardiovascular outcomes.
Major finding: Compared to those in the lowest quintile, patients in the highest quintile of baseline plasma cardiac troponin concentrations had an increased risk of a cardiovascular composite event (hazard ratio, 3.67; 95% CI, 1.33-10.13; P = 0.012).
Study details: Post-hoc analysis of 1,599 patients in the SUMMIT trial who had a baseline cardiac troponin I assessment and 1,258 who had a 3-month follow-up assessment.
Disclosures: The study was supported by GlaxoSmithKline and a Butler British Heart Foundation Senior Clinical Research Fellowship. Authors reported disclosures related to GlaxoSmithKline, Veramed Limited, Abbott Diagnostics, Roche, Singulex, AstraZeneca, Zambon, Bayer, Novartis, and others.
Source: Adamson PD et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1126-37.
Adding checkpoint inhibitors to radiotherapy requires particular caution in this one scenario
Among scenarios where immune checkpoint inhibitors (ICIs) might be combined, particular caution is needed in the setting of brain metastases, according to authors of a recent clinical review.
While evidence to date is mixed, some studies do suggest that adding ICIs to high-dose stereotactic intracranial radiotherapy for brain metastases might increase the risk of treatment-related brain necrosis, the authors said.
By contrast, the balance of evidence suggests ICIs can be safely combined with palliative radiotherapy without site-specific increases in adverse events, they added.
Likewise, in patients with non–small-cell lung cancer, ICIs do not appear to increase incidence of grade 3 or greater pneumonitis when given after definitive chemoradiotherapy, in both retrospective and prospective investigations.
Nevertheless, the addition of ICIs to radiotherapy requires careful further study because of the potential for increased type or severity of toxicities, including the immune-related adverse events associated with ICIs, wrote corresponding author Jay S. Loeffler, MD, of Massachusetts General Hospital, Boston, and his colleagues.
“Caution is warranted when combining radiotherapy and ICI, especially with intracranial radiotherapy,” the researchers wrote. Their report is in Nature Reviews Clinical Oncology.
Some studies have indicated a higher rate of treatment-associated brain necrosis when ICIs are combined with intracranial radiotherapy, while others have shown no such trend, the authors said.
In one single-institution experience involving 180 patients with brain metastases undergoing stereotactic radiotherapy, incidence of treatment-associated brain necrosis was significantly higher in patients receiving an ICI, with an odds ratio of 2.4 (95% confidence interval, 1.06-5.44; P = .03).
Similarly, a retrospective single institution 480-patient study showed an incidence of treatment-associated brain necrosis of 20% for ICIs plus stereotactic radiotherapy versus 7% for radiotherapy alone (P less than .001), but substantial differences in baseline characteristics between groups limited the strength of the study’s conclusions, according to the researchers.
Increased risk is primarily in the form of asymptomatic or minimally symptomatic episodes in some series, the authors noted. A retrospective, 54-patient report showed a rate of treatment-associated brain necrosis of 30% when ICIs were combined with stereotactic radiotherapy, versus 21% for radiotherapy alone (P = .08), but the incidence of symptomatic cases was 15% in both groups, they noted.
“Intriguingly, the findings of several studies have demonstrated an association between [treatment-associated brain necrosis] and improved survival outcomes in patients with melanoma brain metastases that is similar to the independent observations of an analogous relationship between risk of [immune-related adverse events] in general and responsiveness to ICI,” the researchers wrote.
Most of the Food and Drug Administration–approved indications for ICIs are in the metastatic setting, where palliative radiotherapy is frequently important, the authors noted.
In two retrospective studies of patients with metastatic cancers receiving palliative radiotherapy with ICIs, there was a lack of clear association between the irradiated site and specific immune-related adverse events; that lack of association suggests that any toxicities arising from interactions between palliative radiotherapy and ICIs are mainly systemic, rather than local, the authors wrote.
Several retrospective series in advanced-stage melanoma patients have suggested that palliative radiotherapy plus ICIs is safe and does not significantly increase incidence of immune-related adverse events. However, findings from one series showed a correlation between both the ICI and radiotherapy dose given and the incidence of immune-related adverse events.
Prospective studies will be essential to optimize the balance between disease control and risk of morbidity associated with ICIs and radiotherapy combinations, the authors concluded.
The researchers declared no competing interests related to their review article.
SOURCE: Hwang WL, et al. Nat Rev Clin Oncol. 2018 Aug;15(8):477-494.
Among scenarios where immune checkpoint inhibitors (ICIs) might be combined, particular caution is needed in the setting of brain metastases, according to authors of a recent clinical review.
While evidence to date is mixed, some studies do suggest that adding ICIs to high-dose stereotactic intracranial radiotherapy for brain metastases might increase the risk of treatment-related brain necrosis, the authors said.
By contrast, the balance of evidence suggests ICIs can be safely combined with palliative radiotherapy without site-specific increases in adverse events, they added.
Likewise, in patients with non–small-cell lung cancer, ICIs do not appear to increase incidence of grade 3 or greater pneumonitis when given after definitive chemoradiotherapy, in both retrospective and prospective investigations.
Nevertheless, the addition of ICIs to radiotherapy requires careful further study because of the potential for increased type or severity of toxicities, including the immune-related adverse events associated with ICIs, wrote corresponding author Jay S. Loeffler, MD, of Massachusetts General Hospital, Boston, and his colleagues.
“Caution is warranted when combining radiotherapy and ICI, especially with intracranial radiotherapy,” the researchers wrote. Their report is in Nature Reviews Clinical Oncology.
Some studies have indicated a higher rate of treatment-associated brain necrosis when ICIs are combined with intracranial radiotherapy, while others have shown no such trend, the authors said.
In one single-institution experience involving 180 patients with brain metastases undergoing stereotactic radiotherapy, incidence of treatment-associated brain necrosis was significantly higher in patients receiving an ICI, with an odds ratio of 2.4 (95% confidence interval, 1.06-5.44; P = .03).
Similarly, a retrospective single institution 480-patient study showed an incidence of treatment-associated brain necrosis of 20% for ICIs plus stereotactic radiotherapy versus 7% for radiotherapy alone (P less than .001), but substantial differences in baseline characteristics between groups limited the strength of the study’s conclusions, according to the researchers.
Increased risk is primarily in the form of asymptomatic or minimally symptomatic episodes in some series, the authors noted. A retrospective, 54-patient report showed a rate of treatment-associated brain necrosis of 30% when ICIs were combined with stereotactic radiotherapy, versus 21% for radiotherapy alone (P = .08), but the incidence of symptomatic cases was 15% in both groups, they noted.
“Intriguingly, the findings of several studies have demonstrated an association between [treatment-associated brain necrosis] and improved survival outcomes in patients with melanoma brain metastases that is similar to the independent observations of an analogous relationship between risk of [immune-related adverse events] in general and responsiveness to ICI,” the researchers wrote.
Most of the Food and Drug Administration–approved indications for ICIs are in the metastatic setting, where palliative radiotherapy is frequently important, the authors noted.
In two retrospective studies of patients with metastatic cancers receiving palliative radiotherapy with ICIs, there was a lack of clear association between the irradiated site and specific immune-related adverse events; that lack of association suggests that any toxicities arising from interactions between palliative radiotherapy and ICIs are mainly systemic, rather than local, the authors wrote.
Several retrospective series in advanced-stage melanoma patients have suggested that palliative radiotherapy plus ICIs is safe and does not significantly increase incidence of immune-related adverse events. However, findings from one series showed a correlation between both the ICI and radiotherapy dose given and the incidence of immune-related adverse events.
Prospective studies will be essential to optimize the balance between disease control and risk of morbidity associated with ICIs and radiotherapy combinations, the authors concluded.
The researchers declared no competing interests related to their review article.
SOURCE: Hwang WL, et al. Nat Rev Clin Oncol. 2018 Aug;15(8):477-494.
Among scenarios where immune checkpoint inhibitors (ICIs) might be combined, particular caution is needed in the setting of brain metastases, according to authors of a recent clinical review.
While evidence to date is mixed, some studies do suggest that adding ICIs to high-dose stereotactic intracranial radiotherapy for brain metastases might increase the risk of treatment-related brain necrosis, the authors said.
By contrast, the balance of evidence suggests ICIs can be safely combined with palliative radiotherapy without site-specific increases in adverse events, they added.
Likewise, in patients with non–small-cell lung cancer, ICIs do not appear to increase incidence of grade 3 or greater pneumonitis when given after definitive chemoradiotherapy, in both retrospective and prospective investigations.
Nevertheless, the addition of ICIs to radiotherapy requires careful further study because of the potential for increased type or severity of toxicities, including the immune-related adverse events associated with ICIs, wrote corresponding author Jay S. Loeffler, MD, of Massachusetts General Hospital, Boston, and his colleagues.
“Caution is warranted when combining radiotherapy and ICI, especially with intracranial radiotherapy,” the researchers wrote. Their report is in Nature Reviews Clinical Oncology.
Some studies have indicated a higher rate of treatment-associated brain necrosis when ICIs are combined with intracranial radiotherapy, while others have shown no such trend, the authors said.
In one single-institution experience involving 180 patients with brain metastases undergoing stereotactic radiotherapy, incidence of treatment-associated brain necrosis was significantly higher in patients receiving an ICI, with an odds ratio of 2.4 (95% confidence interval, 1.06-5.44; P = .03).
Similarly, a retrospective single institution 480-patient study showed an incidence of treatment-associated brain necrosis of 20% for ICIs plus stereotactic radiotherapy versus 7% for radiotherapy alone (P less than .001), but substantial differences in baseline characteristics between groups limited the strength of the study’s conclusions, according to the researchers.
Increased risk is primarily in the form of asymptomatic or minimally symptomatic episodes in some series, the authors noted. A retrospective, 54-patient report showed a rate of treatment-associated brain necrosis of 30% when ICIs were combined with stereotactic radiotherapy, versus 21% for radiotherapy alone (P = .08), but the incidence of symptomatic cases was 15% in both groups, they noted.
“Intriguingly, the findings of several studies have demonstrated an association between [treatment-associated brain necrosis] and improved survival outcomes in patients with melanoma brain metastases that is similar to the independent observations of an analogous relationship between risk of [immune-related adverse events] in general and responsiveness to ICI,” the researchers wrote.
Most of the Food and Drug Administration–approved indications for ICIs are in the metastatic setting, where palliative radiotherapy is frequently important, the authors noted.
In two retrospective studies of patients with metastatic cancers receiving palliative radiotherapy with ICIs, there was a lack of clear association between the irradiated site and specific immune-related adverse events; that lack of association suggests that any toxicities arising from interactions between palliative radiotherapy and ICIs are mainly systemic, rather than local, the authors wrote.
Several retrospective series in advanced-stage melanoma patients have suggested that palliative radiotherapy plus ICIs is safe and does not significantly increase incidence of immune-related adverse events. However, findings from one series showed a correlation between both the ICI and radiotherapy dose given and the incidence of immune-related adverse events.
Prospective studies will be essential to optimize the balance between disease control and risk of morbidity associated with ICIs and radiotherapy combinations, the authors concluded.
The researchers declared no competing interests related to their review article.
SOURCE: Hwang WL, et al. Nat Rev Clin Oncol. 2018 Aug;15(8):477-494.
FROM NATURE REVIEWS CLINICAL ONCOLOGY
Key clinical point: Some studies suggest that adding ICIs to high-dose stereotactic intracranial radiotherapy for brain metastases might increase the risk of treatment-related brain necrosis.
Major finding: The balance of evidence suggests ICIs can be safely combined with palliative radiotherapy.
Study details: A literature review.
Disclosures: The researchers declared no competing interests related to their review article.
Source: Hwang WL et al. Nat Rev Clin Oncol. 2018 Aug;15(8):477-94.
Live attenuated flu vaccine gets ACIP nod for 2018-2019 season
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
FROM MMWR