User login
Higher lymph node harvest could improve right-side colon cancer outcomes
ORLANDO – The inferior outcomes associated with right-sided colon cancers might be mitigated if a higher lymph node harvest is obtained, a retrospective study suggested.
“These data may provide indirect evidence for complete mesocolic excision to obtain a higher lymph node harvest to improve survival,” said investigator Arman Erkan, MD, of the Center for Colon and Rectal Surgery at Florida Hospital Orlando, in an oral abstract presentation.
This study adds new perspective on recent studies that have also demonstrated worse outcomes for right-sided versus left-sided tumors, which may be related to differences in levels of vascular ligation and nodal harvest. In addition, many studies to date have been limited in their ability to evaluate that hypothesis because of small sample size or other factors, he said in his presentation.
Accordingly, Dr. Erkan and his colleagues queried the National Cancer Database for colectomies for nonmetastatic colon adenocarcinoma occurring between 2004 and 2014, evaluating a total of 504,958 patient records, of which 273,198 were for right-sided tumors. To minimize bias, they used propensity score matching, leaving 148,540 patients in each group for the primary analysis.
Right-sided tumors were associated with inferior 5-year survival for patients with stage II and III disease (P less than .001 for right vs. left in both analyses), the investigators found.
In multivariate analysis, they found a significant interaction between right-sided tumors and a lymph node harvest of greater than 22 nodes toward increased survival, with a hazard ratio of 0.87 (95% confidence interval, 0.84-0.90). “This indicates that survival after right-sided resections can be improved if more than 22 nodes are harvested during the surgery,” Dr. Erkan said.
The difference was most pronounced in stage III of the disease, he added.
Study coauthor Lawrence Lee, MD, a colorectal surgeon at McGill University, said in a related press release that the study findings might prompt surgeons to reevaluate the types of procedures they perform in patients with right-sided tumors. “These patients may need a more extensive resection than is considered to be standard for them.”
Dr. Erkan, Dr. Lee, and other coinvestigators reported no conflicts of interest related to their research.
ORLANDO – The inferior outcomes associated with right-sided colon cancers might be mitigated if a higher lymph node harvest is obtained, a retrospective study suggested.
“These data may provide indirect evidence for complete mesocolic excision to obtain a higher lymph node harvest to improve survival,” said investigator Arman Erkan, MD, of the Center for Colon and Rectal Surgery at Florida Hospital Orlando, in an oral abstract presentation.
This study adds new perspective on recent studies that have also demonstrated worse outcomes for right-sided versus left-sided tumors, which may be related to differences in levels of vascular ligation and nodal harvest. In addition, many studies to date have been limited in their ability to evaluate that hypothesis because of small sample size or other factors, he said in his presentation.
Accordingly, Dr. Erkan and his colleagues queried the National Cancer Database for colectomies for nonmetastatic colon adenocarcinoma occurring between 2004 and 2014, evaluating a total of 504,958 patient records, of which 273,198 were for right-sided tumors. To minimize bias, they used propensity score matching, leaving 148,540 patients in each group for the primary analysis.
Right-sided tumors were associated with inferior 5-year survival for patients with stage II and III disease (P less than .001 for right vs. left in both analyses), the investigators found.
In multivariate analysis, they found a significant interaction between right-sided tumors and a lymph node harvest of greater than 22 nodes toward increased survival, with a hazard ratio of 0.87 (95% confidence interval, 0.84-0.90). “This indicates that survival after right-sided resections can be improved if more than 22 nodes are harvested during the surgery,” Dr. Erkan said.
The difference was most pronounced in stage III of the disease, he added.
Study coauthor Lawrence Lee, MD, a colorectal surgeon at McGill University, said in a related press release that the study findings might prompt surgeons to reevaluate the types of procedures they perform in patients with right-sided tumors. “These patients may need a more extensive resection than is considered to be standard for them.”
Dr. Erkan, Dr. Lee, and other coinvestigators reported no conflicts of interest related to their research.
ORLANDO – The inferior outcomes associated with right-sided colon cancers might be mitigated if a higher lymph node harvest is obtained, a retrospective study suggested.
“These data may provide indirect evidence for complete mesocolic excision to obtain a higher lymph node harvest to improve survival,” said investigator Arman Erkan, MD, of the Center for Colon and Rectal Surgery at Florida Hospital Orlando, in an oral abstract presentation.
This study adds new perspective on recent studies that have also demonstrated worse outcomes for right-sided versus left-sided tumors, which may be related to differences in levels of vascular ligation and nodal harvest. In addition, many studies to date have been limited in their ability to evaluate that hypothesis because of small sample size or other factors, he said in his presentation.
Accordingly, Dr. Erkan and his colleagues queried the National Cancer Database for colectomies for nonmetastatic colon adenocarcinoma occurring between 2004 and 2014, evaluating a total of 504,958 patient records, of which 273,198 were for right-sided tumors. To minimize bias, they used propensity score matching, leaving 148,540 patients in each group for the primary analysis.
Right-sided tumors were associated with inferior 5-year survival for patients with stage II and III disease (P less than .001 for right vs. left in both analyses), the investigators found.
In multivariate analysis, they found a significant interaction between right-sided tumors and a lymph node harvest of greater than 22 nodes toward increased survival, with a hazard ratio of 0.87 (95% confidence interval, 0.84-0.90). “This indicates that survival after right-sided resections can be improved if more than 22 nodes are harvested during the surgery,” Dr. Erkan said.
The difference was most pronounced in stage III of the disease, he added.
Study coauthor Lawrence Lee, MD, a colorectal surgeon at McGill University, said in a related press release that the study findings might prompt surgeons to reevaluate the types of procedures they perform in patients with right-sided tumors. “These patients may need a more extensive resection than is considered to be standard for them.”
Dr. Erkan, Dr. Lee, and other coinvestigators reported no conflicts of interest related to their research.
REPORTING FROM ACSQSC 2018
Pediatric appendectomy fast track reduced LoS, narcotic use
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
REPORTING FROM ACSQSC 2018
Myeloma frailty index predicts survival based on biological age
A new index of frailty predicts survival in older patients with multiple myeloma based on accumulation of aging-associated deficits, rather than chronological age alone, investigators report. A 16% increased risk of death was seen for each 10% increase in the deficit-accumulation frailty index (DAFI), which includes 25 variables related health, function, and activities of daily living.
There was only a weak correlation between chronological age and increase in deficits tracked by the index, in contrast to a cohort without cancer, in which age and frailty were strongly correlated, the investigators reported in JCO Clinical Cancer Informatics.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health,” study author Tanya M. Wildes, MD, of Washington University, St. Louis, said in a news release from the American Society of Clinical Oncology.
Existing tools to assess frailty include an index proposed by the International Myeloma Working Group that looks at age plus other indexes related to comorbidities and activities of daily living, and the revised Myeloma Comorbidity Index that incorporates age with other prognostic factors.
“Although both tools provide prognostic information, chronological age automatically increases frailty without taking biologic or functional age into account,” Dr. Wildes and her coauthors wrote in their report.
By contrast, the DAFI is based on the concept of biologic age, in which the health status of an individual is measured based on the proportion of aging-associated deficits they have accumulated, according to the authors.
To create the DAFI, Dr. Wildes and her colleagues analyzed nearly 2.7 million records of noncancer patients aged 66 years or older in the SEER Medicare Health Outcomes Survey (MHOS) database. They identified 25 variables in the database representing chronic health conditions, activities of daily living, functioning, mental health, and general health.
An individual’s DAFI score was calculated as the sum of scores for each of the 25 variables as 0 for absent, 0.5 for limited, and 1 for present. Predicted DAFI means were calculated for each year of age and used to create age-specific cut points to determine whether an individual would be considered frail or not versus others of the same age.
“In other words, the same frailty score may qualify an 80-year-old individual as fit and a 70-year-old as frail, depending on the cutoff for their respective age group,” investigators explained in their report.
They applied the index to 305 patients with newly diagnosed myeloma in the SEER-MHOS database who were 66 years of age or older (median age, 76 years) and had completed the survey within 1 year of diagnosis.
The DAFI classified 52% of the myeloma patients as frail, and for that group, median overall survival was 26.8 months, versus 43.7 months for nonfrail patients (P = .015), according to the reported data. For each 10% increase in score, the risk of death increased by 16% (P less than .001).
Notably, advancing age was very weakly correlated with increased age-related deficits in the myeloma cohort (r2 = 0.15; P = .010), according to investigators, but very strongly correlated with deficits in the cohort of noncancer patients (r2 = 0.98; P less than .001).
“This suggests that, in patients with multiple myeloma, the prevalence of impairments across domains of function, chronic comorbidities, general health, and mental health are more related to the overall burden of myeloma rather than chronological age alone,” the investigators wrote.
The information used to calculate a DAFI score is easily obtainable during a clinic visit, according to the authors, who provided an overview of all 25 variables in the journal article.
Further development of a computerized program would further enhance usability in the clinic, allowing for real-time calculation during a patient visit, they said.
Survivorship expert Merry Jennifer Markham, MD, said in the ASCO news release that this frailty index is notable because it accounts for more than just chronological age. “Knowing this information can help oncologists have more informed discussions with patients about their prognosis, which in turn can empower patients and families as they weigh treatment options,” she said.
The research was supported by National Cancer Institute. Dr. Wildes reported honoraria from Carevive Systems and research funding from Janssen Oncology. Another coauthor reported honoraria from Celgene and Janssen, and a consulting or advisory role with Amgen and Takeda.
SOURCE: Mian HS et al. JCO Clin Cancer Inform. 2018 Jul 25. 2018 Jul 25. doi: 10.1200/CCI.18.00043.
A new index of frailty predicts survival in older patients with multiple myeloma based on accumulation of aging-associated deficits, rather than chronological age alone, investigators report. A 16% increased risk of death was seen for each 10% increase in the deficit-accumulation frailty index (DAFI), which includes 25 variables related health, function, and activities of daily living.
There was only a weak correlation between chronological age and increase in deficits tracked by the index, in contrast to a cohort without cancer, in which age and frailty were strongly correlated, the investigators reported in JCO Clinical Cancer Informatics.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health,” study author Tanya M. Wildes, MD, of Washington University, St. Louis, said in a news release from the American Society of Clinical Oncology.
Existing tools to assess frailty include an index proposed by the International Myeloma Working Group that looks at age plus other indexes related to comorbidities and activities of daily living, and the revised Myeloma Comorbidity Index that incorporates age with other prognostic factors.
“Although both tools provide prognostic information, chronological age automatically increases frailty without taking biologic or functional age into account,” Dr. Wildes and her coauthors wrote in their report.
By contrast, the DAFI is based on the concept of biologic age, in which the health status of an individual is measured based on the proportion of aging-associated deficits they have accumulated, according to the authors.
To create the DAFI, Dr. Wildes and her colleagues analyzed nearly 2.7 million records of noncancer patients aged 66 years or older in the SEER Medicare Health Outcomes Survey (MHOS) database. They identified 25 variables in the database representing chronic health conditions, activities of daily living, functioning, mental health, and general health.
An individual’s DAFI score was calculated as the sum of scores for each of the 25 variables as 0 for absent, 0.5 for limited, and 1 for present. Predicted DAFI means were calculated for each year of age and used to create age-specific cut points to determine whether an individual would be considered frail or not versus others of the same age.
“In other words, the same frailty score may qualify an 80-year-old individual as fit and a 70-year-old as frail, depending on the cutoff for their respective age group,” investigators explained in their report.
They applied the index to 305 patients with newly diagnosed myeloma in the SEER-MHOS database who were 66 years of age or older (median age, 76 years) and had completed the survey within 1 year of diagnosis.
The DAFI classified 52% of the myeloma patients as frail, and for that group, median overall survival was 26.8 months, versus 43.7 months for nonfrail patients (P = .015), according to the reported data. For each 10% increase in score, the risk of death increased by 16% (P less than .001).
Notably, advancing age was very weakly correlated with increased age-related deficits in the myeloma cohort (r2 = 0.15; P = .010), according to investigators, but very strongly correlated with deficits in the cohort of noncancer patients (r2 = 0.98; P less than .001).
“This suggests that, in patients with multiple myeloma, the prevalence of impairments across domains of function, chronic comorbidities, general health, and mental health are more related to the overall burden of myeloma rather than chronological age alone,” the investigators wrote.
The information used to calculate a DAFI score is easily obtainable during a clinic visit, according to the authors, who provided an overview of all 25 variables in the journal article.
Further development of a computerized program would further enhance usability in the clinic, allowing for real-time calculation during a patient visit, they said.
Survivorship expert Merry Jennifer Markham, MD, said in the ASCO news release that this frailty index is notable because it accounts for more than just chronological age. “Knowing this information can help oncologists have more informed discussions with patients about their prognosis, which in turn can empower patients and families as they weigh treatment options,” she said.
The research was supported by National Cancer Institute. Dr. Wildes reported honoraria from Carevive Systems and research funding from Janssen Oncology. Another coauthor reported honoraria from Celgene and Janssen, and a consulting or advisory role with Amgen and Takeda.
SOURCE: Mian HS et al. JCO Clin Cancer Inform. 2018 Jul 25. 2018 Jul 25. doi: 10.1200/CCI.18.00043.
A new index of frailty predicts survival in older patients with multiple myeloma based on accumulation of aging-associated deficits, rather than chronological age alone, investigators report. A 16% increased risk of death was seen for each 10% increase in the deficit-accumulation frailty index (DAFI), which includes 25 variables related health, function, and activities of daily living.
There was only a weak correlation between chronological age and increase in deficits tracked by the index, in contrast to a cohort without cancer, in which age and frailty were strongly correlated, the investigators reported in JCO Clinical Cancer Informatics.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health,” study author Tanya M. Wildes, MD, of Washington University, St. Louis, said in a news release from the American Society of Clinical Oncology.
Existing tools to assess frailty include an index proposed by the International Myeloma Working Group that looks at age plus other indexes related to comorbidities and activities of daily living, and the revised Myeloma Comorbidity Index that incorporates age with other prognostic factors.
“Although both tools provide prognostic information, chronological age automatically increases frailty without taking biologic or functional age into account,” Dr. Wildes and her coauthors wrote in their report.
By contrast, the DAFI is based on the concept of biologic age, in which the health status of an individual is measured based on the proportion of aging-associated deficits they have accumulated, according to the authors.
To create the DAFI, Dr. Wildes and her colleagues analyzed nearly 2.7 million records of noncancer patients aged 66 years or older in the SEER Medicare Health Outcomes Survey (MHOS) database. They identified 25 variables in the database representing chronic health conditions, activities of daily living, functioning, mental health, and general health.
An individual’s DAFI score was calculated as the sum of scores for each of the 25 variables as 0 for absent, 0.5 for limited, and 1 for present. Predicted DAFI means were calculated for each year of age and used to create age-specific cut points to determine whether an individual would be considered frail or not versus others of the same age.
“In other words, the same frailty score may qualify an 80-year-old individual as fit and a 70-year-old as frail, depending on the cutoff for their respective age group,” investigators explained in their report.
They applied the index to 305 patients with newly diagnosed myeloma in the SEER-MHOS database who were 66 years of age or older (median age, 76 years) and had completed the survey within 1 year of diagnosis.
The DAFI classified 52% of the myeloma patients as frail, and for that group, median overall survival was 26.8 months, versus 43.7 months for nonfrail patients (P = .015), according to the reported data. For each 10% increase in score, the risk of death increased by 16% (P less than .001).
Notably, advancing age was very weakly correlated with increased age-related deficits in the myeloma cohort (r2 = 0.15; P = .010), according to investigators, but very strongly correlated with deficits in the cohort of noncancer patients (r2 = 0.98; P less than .001).
“This suggests that, in patients with multiple myeloma, the prevalence of impairments across domains of function, chronic comorbidities, general health, and mental health are more related to the overall burden of myeloma rather than chronological age alone,” the investigators wrote.
The information used to calculate a DAFI score is easily obtainable during a clinic visit, according to the authors, who provided an overview of all 25 variables in the journal article.
Further development of a computerized program would further enhance usability in the clinic, allowing for real-time calculation during a patient visit, they said.
Survivorship expert Merry Jennifer Markham, MD, said in the ASCO news release that this frailty index is notable because it accounts for more than just chronological age. “Knowing this information can help oncologists have more informed discussions with patients about their prognosis, which in turn can empower patients and families as they weigh treatment options,” she said.
The research was supported by National Cancer Institute. Dr. Wildes reported honoraria from Carevive Systems and research funding from Janssen Oncology. Another coauthor reported honoraria from Celgene and Janssen, and a consulting or advisory role with Amgen and Takeda.
SOURCE: Mian HS et al. JCO Clin Cancer Inform. 2018 Jul 25. 2018 Jul 25. doi: 10.1200/CCI.18.00043.
FROM JCO CLINICAL CANCER INFORMATICS
Key clinical point: A new index of frailty predicts survival in older patients with multiple myeloma based on accumulation of aging-associated deficits, rather than on chronological age alone.
Major finding: Median overall survival was 26.8 months for patients classified as frail, vs. 43.7 months for nonfrail patients (P = .015).
Study details: Retrospective analysis of 2.7 million records of noncancer patients to create an index subsequently validated in records for 305 patients with newly diagnosed multiple myeloma (aged 66 years and older).
Disclosures: The research was supported by National Cancer Institute. Authors reported disclosures related to Celgene, Janssen, Amgen, Takeda, and Carevive Systems.
Source: Mian HS et al. JCO Clin Cancer Inform. 2018 Jul 25. doi: 10.1200/CCI.18.00043.
ACS NSQIP project collected patient-reported data on surgery outcomes
ORLANDO – A pilot survey to generate had a high response rate and yielded clinically meaningful data, an investigator reported at the American College of Surgeons Quality and Safety Conference.
The 45-question electronic survey, conducted as part of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) had 1,300 respondents with a response rate of 20%, according to Jason B. Liu, MD, an ACS Clinical Scholar-in-Residence and general surgery resident at the University of Chicago.
Results to date have demonstrated that in patients undergoing total knee arthroplasty (TKA), pain had a greater impact on daily activities than for other procedures, Dr. Liu said in a general session presentation the conference.
“Overall, the lesson learned is that in the current health care landscape, with its regulations and privacy issues, it is indeed both feasible and acceptable to electronically measure patient-reported outcomes using the ACS NSQIP platform,” Dr. Liu said at the meeting.
Eighteen hospitals in the United States and Canada participated in the pilot survey, which elicited responses from patients with a median age of 63 years, representing more than 340 types of operations.
The survey incorporates measurements from the PROMIS Pain Interference instrument, which measures how much pain hinders daily activities; PROMIS Global Health, which measures physical and mental health; and aspects of the Consumer Assessment of Healthcare Providers and Systems Surgical Care Survey (S-CAHPS), Dr. Liu said.
The TKA finding is just one example of the data obtained through the pilot, he said. Looking at PROMIS Pain Interference, pain had more impact in TKA patients compared with open GI, breast hernia, and laparoscopic GI procedures. Difference between means ranged from 3.2 to 9.4 for TKA, compared with those procedures.
Conducting the pilot has been an “uphill battle,” according to Dr. Liu, citing critics who wondered if the program would generate meaningful data, whether older patients would respond to an electronic survey, and whether patients would take time to fill out a 45-question survey.
In fact, the average completion time for the survey was just 6.4 minutes, and the median number of items missing was zero, meaning that patients who started the survey tended to finish it, he said.
“We really hope to expand what we’ve learned across all of the [ACS] quality programs so that we can begin to really incorporate the patients’ perspective in improving national surgical quality,” he said.
Dr. Liu had no disclosures to report.
ORLANDO – A pilot survey to generate had a high response rate and yielded clinically meaningful data, an investigator reported at the American College of Surgeons Quality and Safety Conference.
The 45-question electronic survey, conducted as part of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) had 1,300 respondents with a response rate of 20%, according to Jason B. Liu, MD, an ACS Clinical Scholar-in-Residence and general surgery resident at the University of Chicago.
Results to date have demonstrated that in patients undergoing total knee arthroplasty (TKA), pain had a greater impact on daily activities than for other procedures, Dr. Liu said in a general session presentation the conference.
“Overall, the lesson learned is that in the current health care landscape, with its regulations and privacy issues, it is indeed both feasible and acceptable to electronically measure patient-reported outcomes using the ACS NSQIP platform,” Dr. Liu said at the meeting.
Eighteen hospitals in the United States and Canada participated in the pilot survey, which elicited responses from patients with a median age of 63 years, representing more than 340 types of operations.
The survey incorporates measurements from the PROMIS Pain Interference instrument, which measures how much pain hinders daily activities; PROMIS Global Health, which measures physical and mental health; and aspects of the Consumer Assessment of Healthcare Providers and Systems Surgical Care Survey (S-CAHPS), Dr. Liu said.
The TKA finding is just one example of the data obtained through the pilot, he said. Looking at PROMIS Pain Interference, pain had more impact in TKA patients compared with open GI, breast hernia, and laparoscopic GI procedures. Difference between means ranged from 3.2 to 9.4 for TKA, compared with those procedures.
Conducting the pilot has been an “uphill battle,” according to Dr. Liu, citing critics who wondered if the program would generate meaningful data, whether older patients would respond to an electronic survey, and whether patients would take time to fill out a 45-question survey.
In fact, the average completion time for the survey was just 6.4 minutes, and the median number of items missing was zero, meaning that patients who started the survey tended to finish it, he said.
“We really hope to expand what we’ve learned across all of the [ACS] quality programs so that we can begin to really incorporate the patients’ perspective in improving national surgical quality,” he said.
Dr. Liu had no disclosures to report.
ORLANDO – A pilot survey to generate had a high response rate and yielded clinically meaningful data, an investigator reported at the American College of Surgeons Quality and Safety Conference.
The 45-question electronic survey, conducted as part of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) had 1,300 respondents with a response rate of 20%, according to Jason B. Liu, MD, an ACS Clinical Scholar-in-Residence and general surgery resident at the University of Chicago.
Results to date have demonstrated that in patients undergoing total knee arthroplasty (TKA), pain had a greater impact on daily activities than for other procedures, Dr. Liu said in a general session presentation the conference.
“Overall, the lesson learned is that in the current health care landscape, with its regulations and privacy issues, it is indeed both feasible and acceptable to electronically measure patient-reported outcomes using the ACS NSQIP platform,” Dr. Liu said at the meeting.
Eighteen hospitals in the United States and Canada participated in the pilot survey, which elicited responses from patients with a median age of 63 years, representing more than 340 types of operations.
The survey incorporates measurements from the PROMIS Pain Interference instrument, which measures how much pain hinders daily activities; PROMIS Global Health, which measures physical and mental health; and aspects of the Consumer Assessment of Healthcare Providers and Systems Surgical Care Survey (S-CAHPS), Dr. Liu said.
The TKA finding is just one example of the data obtained through the pilot, he said. Looking at PROMIS Pain Interference, pain had more impact in TKA patients compared with open GI, breast hernia, and laparoscopic GI procedures. Difference between means ranged from 3.2 to 9.4 for TKA, compared with those procedures.
Conducting the pilot has been an “uphill battle,” according to Dr. Liu, citing critics who wondered if the program would generate meaningful data, whether older patients would respond to an electronic survey, and whether patients would take time to fill out a 45-question survey.
In fact, the average completion time for the survey was just 6.4 minutes, and the median number of items missing was zero, meaning that patients who started the survey tended to finish it, he said.
“We really hope to expand what we’ve learned across all of the [ACS] quality programs so that we can begin to really incorporate the patients’ perspective in improving national surgical quality,” he said.
Dr. Liu had no disclosures to report.
REPORTING FROM ACSQSC 2018
Key clinical point: Clinically meaningful data on patient-reported outcomes can be obtained using the ACS NSQIP platform.
Major finding: The average completion time for the survey was 6.4 minutes, and the median number of items missing was zero.
Study details: A 45-question electronic survey of 1,300 patients treated at 18 hospitals for 340 different types of surgical procedures.
Disclosures: Dr. Liu had no disclosures to report.
Enhanced recovery initiative improved bariatric length of stay
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
REPORTING FROM ACSQSC 2018
Key clinical point: An evidence-based enhanced recovery protocol reduced length of stay for bariatric surgery patients.
Major finding: Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers.
Study details: Data on 36 bariatric surgery centers and 4,700 patients who underwent procedures in the first 6 months of the data collection period.
Disclosures: Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
Acute care prescriptions can be cut to minimize opioid exposure
ORLANDO – By cutting the number of pills prescribed after a surgical procedure, exposure to opioids can be minimized in a largely opioid-naive patient population at risk of new, persistent use, according to Michael J. Englesbe, MD, FACS, professor of surgery at the University of Michigan, Ann Arbor, who is leading a Michigan initiative to tailor acute care prescribing.
About 90% of surgically patients are opioid-naive, and of those, studies suggest about 6% may become new, persistent opioid users, according to Dr. Englesbe, codirector of the Michigan Opioid Prescribing and Engagement Network (Michigan-OPEN), a state-wide effort to transform acute pain prescribing across all surgical specialties.
“This is a very vulnerable population where their operation can lead to life-changing events way beyond their surgical outcomes,” Dr. Englesbe said in a presentation at the American College of Surgeons Quality and Safety Conference.
“We have to really worry about them,” he added. “It’s hard to identify who they are, and I think minimizing exposure to opioids is the best we have at this point.”
By following evidence-based prescribing guidelines after laparoscopic cholecystectomy, Dr. Englesbe and his colleagues were able to reduce prescription size by 63% with no increase in refills and no change in pain score, according to a research letter recently published in JAMA Surgery.
After adopting the guidelines, median postoperative opioid use dropped from 30 mg to 20 mg (P = .04), they reported.
Laparoscopic cholecystectomy patients could be prescribed as few as 10 5-mg tablets of oxycodone, according to recommendations developed by Michigan-OPEN that are published on opioidprescribing.info. Dr. Englesbe called the website figures “precise prescribing recommendations” that are still relatively generous, meeting or exceeding self-reported use for 75% of patients.
“I think this is an important template for change,” he said. “We’ve found the surgeons in the state very receptive, but more importantly, we’ve been able to partner with other really important stakeholders.” For example, one insurer in the state now aligns some hospital incentive reimbursement based on some of these prescribing methods, he added.
Dr. Englesbe reported no commercial disclosures related to his presentation.
ORLANDO – By cutting the number of pills prescribed after a surgical procedure, exposure to opioids can be minimized in a largely opioid-naive patient population at risk of new, persistent use, according to Michael J. Englesbe, MD, FACS, professor of surgery at the University of Michigan, Ann Arbor, who is leading a Michigan initiative to tailor acute care prescribing.
About 90% of surgically patients are opioid-naive, and of those, studies suggest about 6% may become new, persistent opioid users, according to Dr. Englesbe, codirector of the Michigan Opioid Prescribing and Engagement Network (Michigan-OPEN), a state-wide effort to transform acute pain prescribing across all surgical specialties.
“This is a very vulnerable population where their operation can lead to life-changing events way beyond their surgical outcomes,” Dr. Englesbe said in a presentation at the American College of Surgeons Quality and Safety Conference.
“We have to really worry about them,” he added. “It’s hard to identify who they are, and I think minimizing exposure to opioids is the best we have at this point.”
By following evidence-based prescribing guidelines after laparoscopic cholecystectomy, Dr. Englesbe and his colleagues were able to reduce prescription size by 63% with no increase in refills and no change in pain score, according to a research letter recently published in JAMA Surgery.
After adopting the guidelines, median postoperative opioid use dropped from 30 mg to 20 mg (P = .04), they reported.
Laparoscopic cholecystectomy patients could be prescribed as few as 10 5-mg tablets of oxycodone, according to recommendations developed by Michigan-OPEN that are published on opioidprescribing.info. Dr. Englesbe called the website figures “precise prescribing recommendations” that are still relatively generous, meeting or exceeding self-reported use for 75% of patients.
“I think this is an important template for change,” he said. “We’ve found the surgeons in the state very receptive, but more importantly, we’ve been able to partner with other really important stakeholders.” For example, one insurer in the state now aligns some hospital incentive reimbursement based on some of these prescribing methods, he added.
Dr. Englesbe reported no commercial disclosures related to his presentation.
ORLANDO – By cutting the number of pills prescribed after a surgical procedure, exposure to opioids can be minimized in a largely opioid-naive patient population at risk of new, persistent use, according to Michael J. Englesbe, MD, FACS, professor of surgery at the University of Michigan, Ann Arbor, who is leading a Michigan initiative to tailor acute care prescribing.
About 90% of surgically patients are opioid-naive, and of those, studies suggest about 6% may become new, persistent opioid users, according to Dr. Englesbe, codirector of the Michigan Opioid Prescribing and Engagement Network (Michigan-OPEN), a state-wide effort to transform acute pain prescribing across all surgical specialties.
“This is a very vulnerable population where their operation can lead to life-changing events way beyond their surgical outcomes,” Dr. Englesbe said in a presentation at the American College of Surgeons Quality and Safety Conference.
“We have to really worry about them,” he added. “It’s hard to identify who they are, and I think minimizing exposure to opioids is the best we have at this point.”
By following evidence-based prescribing guidelines after laparoscopic cholecystectomy, Dr. Englesbe and his colleagues were able to reduce prescription size by 63% with no increase in refills and no change in pain score, according to a research letter recently published in JAMA Surgery.
After adopting the guidelines, median postoperative opioid use dropped from 30 mg to 20 mg (P = .04), they reported.
Laparoscopic cholecystectomy patients could be prescribed as few as 10 5-mg tablets of oxycodone, according to recommendations developed by Michigan-OPEN that are published on opioidprescribing.info. Dr. Englesbe called the website figures “precise prescribing recommendations” that are still relatively generous, meeting or exceeding self-reported use for 75% of patients.
“I think this is an important template for change,” he said. “We’ve found the surgeons in the state very receptive, but more importantly, we’ve been able to partner with other really important stakeholders.” For example, one insurer in the state now aligns some hospital incentive reimbursement based on some of these prescribing methods, he added.
Dr. Englesbe reported no commercial disclosures related to his presentation.
EXPERT ANALYSIS FROM ACSQSC 2018
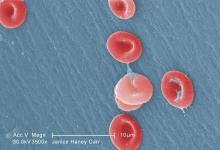
Phase 3 results shed light on L-glutamine use in SCD
Children and adults with sickle cell disease who received L-glutamine alone or with hydroxyurea had a median number of pain episodes that was 25% lower than those who received placebo, according to newly published results from the phase 3 trial that led to the agent’s approval in 2017.
The median number of hospitalizations was 33% lower among individuals receiving L-glutamine than it was among those receiving placebo, in results reported by investigators led by Yutaka Niihara, MD, of the University of California, Los Angeles, and Emmaus Medical.
Blood test results showed persistent elevation of mean corpuscular volume, indicating adherence to hydroxyurea therapy and suggesting that the effect of L-glutamine might be additive, Dr. Niihara and his coauthors wrote in the New England Journal of Medicine.
“L-glutamine thus provides an alternative therapy for those who decline treatment with hydroxyurea or who may have unacceptable side effects from hydroxyurea, as well as an additive therapy to lower the incidence of pain crises for those who may have suboptimal response to hydroxyurea,” they wrote.
The multicenter, randomized, placebo-controlled, double-blind, phase 3 trial by Dr. Niihara and his colleagues included 230 children and adults with sickle cell anemia or sickle-beta0-thalassemia and two or more pain crises in the previous year.
Participants at 31 sites across the United States were randomized to receive L-glutamine powder (n = 152) or placebo (n = 78) orally twice weekly for 48 weeks, followed by a 3-week tapering period. Two-thirds received concomitant hydroxyurea during the trial.
Participants were contacted by telephone weekly during the study to encourage adherence.
A total of 156 individuals completed the study, including 97 of 152 (63.8%) in the L-glutamine arm and 59 of 78 (75.6%) in the placebo arm. The most common reasons for discontinuation were withdrawal of consent, nonadherence, or reasons classified as “other,” according to investigators.
The primary end point was the number of pain crises through week 48 of the trial. A median of 3.0 pain crises occurred in the L-glutamine group, compared with 4.0 in the placebo group (P = .005). Additionally, the median number of hospitalizations was 2.0 for the L-glutamine group versus 3.0 for the placebo group (P = .005).
Nausea, arm or leg pain, and back pain all had an incidence in the L-glutamine group that was 5% higher than in the placebo group, investigators reported.
Based on these results, the Food and Drug administration approved oral L-glutamine powder to reduce the acute complications of sickle cell disease in patients 5 years of age and older in July 2017.
The reasons for study withdrawal were similar in the L-glutamine and placebo groups, despite the higher withdrawal rate in the L-glutamine group, investigators said in a discussion of their results. “Recruitment and retention in a year-long study is difficult in an already burdened population,” they wrote.
The overall noncompletion rate was 32%, similar to the 35% rate seen in a recent multicenter trial of crizanlizumab in patients with sickle cell disease, they added.
Dr. Niihara is the founder and CEO of Emmaus Medical, which sponsored the trial. Other coauthors also reported disclosures related to Emmaus Medical and other companies.
SOURCE: Niihara Y et al. N Engl J Med. 2018 Jul 19;379(3):226-35.
Results of this phase 3 trial were “much awaited” and illustrate the efficacy of L-glutamine in reducing the number of acute vasoocclusive episodes in patients with sickle cell disease.
However, as with any new breakthrough in medicine, there are now compelling questions that need to be answered, Caterina P. Minniti, MD, said in an accompanying editorial.
How to handle cost is one such question. One year of treatment with pharmaceutical-grade L-glutamine carries an estimated cost of $40,515 versus $1,700 for a year of hydroxyurea, but whether the price tag will hinder prescribing of the newer agent has yet to be seen, according to Dr. Minniti.
“This agent certainly has been slow to enter the market because prescribing L-glutamine for patients requires many steps, which may dissuade busy practitioners from actively prescribing it,” she said.
Another question is whether it should be used alongside hydroxyurea, as was done in two-thirds of patients in the present trial. Concomitant use is possible and “most likely advantageous” given that L-glutamine has a different toxicity profile and putatively different mechanism of action from hydroxyurea, Dr. Minniti said.
Who should receive L-glutamine is another important question. Dr. Minniti said that, based on previous trial data, caution may be warranted in giving L-glutamine to patients with significant renal and hepatic dysfunction, but she added that its role could be broad.
“In the absence of specific guidelines, I believe that L-glutamine may be prescribed to persons older than 5 years of age who have any sickle genotype and continue to have episodes of acute disease exacerbations despite appropriate use of hydroxyurea or to those who cannot or do not use hydroxyurea,” she said in the editorial.
Caterina P. Minniti, MD, is with the division of hematology at Montefiore Medical Center at Einstein College of Medicine, New York. These comments are excerpted from her accompanying editorial ( N Engl J Med. 2018;379:292-4 ). Dr. Minniti reported disclosures related to Global Blood Therapeutics and Bayer, along with a patent pending for a topical sodium nitrite formulation.
Results of this phase 3 trial were “much awaited” and illustrate the efficacy of L-glutamine in reducing the number of acute vasoocclusive episodes in patients with sickle cell disease.
However, as with any new breakthrough in medicine, there are now compelling questions that need to be answered, Caterina P. Minniti, MD, said in an accompanying editorial.
How to handle cost is one such question. One year of treatment with pharmaceutical-grade L-glutamine carries an estimated cost of $40,515 versus $1,700 for a year of hydroxyurea, but whether the price tag will hinder prescribing of the newer agent has yet to be seen, according to Dr. Minniti.
“This agent certainly has been slow to enter the market because prescribing L-glutamine for patients requires many steps, which may dissuade busy practitioners from actively prescribing it,” she said.
Another question is whether it should be used alongside hydroxyurea, as was done in two-thirds of patients in the present trial. Concomitant use is possible and “most likely advantageous” given that L-glutamine has a different toxicity profile and putatively different mechanism of action from hydroxyurea, Dr. Minniti said.
Who should receive L-glutamine is another important question. Dr. Minniti said that, based on previous trial data, caution may be warranted in giving L-glutamine to patients with significant renal and hepatic dysfunction, but she added that its role could be broad.
“In the absence of specific guidelines, I believe that L-glutamine may be prescribed to persons older than 5 years of age who have any sickle genotype and continue to have episodes of acute disease exacerbations despite appropriate use of hydroxyurea or to those who cannot or do not use hydroxyurea,” she said in the editorial.
Caterina P. Minniti, MD, is with the division of hematology at Montefiore Medical Center at Einstein College of Medicine, New York. These comments are excerpted from her accompanying editorial ( N Engl J Med. 2018;379:292-4 ). Dr. Minniti reported disclosures related to Global Blood Therapeutics and Bayer, along with a patent pending for a topical sodium nitrite formulation.
Results of this phase 3 trial were “much awaited” and illustrate the efficacy of L-glutamine in reducing the number of acute vasoocclusive episodes in patients with sickle cell disease.
However, as with any new breakthrough in medicine, there are now compelling questions that need to be answered, Caterina P. Minniti, MD, said in an accompanying editorial.
How to handle cost is one such question. One year of treatment with pharmaceutical-grade L-glutamine carries an estimated cost of $40,515 versus $1,700 for a year of hydroxyurea, but whether the price tag will hinder prescribing of the newer agent has yet to be seen, according to Dr. Minniti.
“This agent certainly has been slow to enter the market because prescribing L-glutamine for patients requires many steps, which may dissuade busy practitioners from actively prescribing it,” she said.
Another question is whether it should be used alongside hydroxyurea, as was done in two-thirds of patients in the present trial. Concomitant use is possible and “most likely advantageous” given that L-glutamine has a different toxicity profile and putatively different mechanism of action from hydroxyurea, Dr. Minniti said.
Who should receive L-glutamine is another important question. Dr. Minniti said that, based on previous trial data, caution may be warranted in giving L-glutamine to patients with significant renal and hepatic dysfunction, but she added that its role could be broad.
“In the absence of specific guidelines, I believe that L-glutamine may be prescribed to persons older than 5 years of age who have any sickle genotype and continue to have episodes of acute disease exacerbations despite appropriate use of hydroxyurea or to those who cannot or do not use hydroxyurea,” she said in the editorial.
Caterina P. Minniti, MD, is with the division of hematology at Montefiore Medical Center at Einstein College of Medicine, New York. These comments are excerpted from her accompanying editorial ( N Engl J Med. 2018;379:292-4 ). Dr. Minniti reported disclosures related to Global Blood Therapeutics and Bayer, along with a patent pending for a topical sodium nitrite formulation.
Children and adults with sickle cell disease who received L-glutamine alone or with hydroxyurea had a median number of pain episodes that was 25% lower than those who received placebo, according to newly published results from the phase 3 trial that led to the agent’s approval in 2017.
The median number of hospitalizations was 33% lower among individuals receiving L-glutamine than it was among those receiving placebo, in results reported by investigators led by Yutaka Niihara, MD, of the University of California, Los Angeles, and Emmaus Medical.
Blood test results showed persistent elevation of mean corpuscular volume, indicating adherence to hydroxyurea therapy and suggesting that the effect of L-glutamine might be additive, Dr. Niihara and his coauthors wrote in the New England Journal of Medicine.
“L-glutamine thus provides an alternative therapy for those who decline treatment with hydroxyurea or who may have unacceptable side effects from hydroxyurea, as well as an additive therapy to lower the incidence of pain crises for those who may have suboptimal response to hydroxyurea,” they wrote.
The multicenter, randomized, placebo-controlled, double-blind, phase 3 trial by Dr. Niihara and his colleagues included 230 children and adults with sickle cell anemia or sickle-beta0-thalassemia and two or more pain crises in the previous year.
Participants at 31 sites across the United States were randomized to receive L-glutamine powder (n = 152) or placebo (n = 78) orally twice weekly for 48 weeks, followed by a 3-week tapering period. Two-thirds received concomitant hydroxyurea during the trial.
Participants were contacted by telephone weekly during the study to encourage adherence.
A total of 156 individuals completed the study, including 97 of 152 (63.8%) in the L-glutamine arm and 59 of 78 (75.6%) in the placebo arm. The most common reasons for discontinuation were withdrawal of consent, nonadherence, or reasons classified as “other,” according to investigators.
The primary end point was the number of pain crises through week 48 of the trial. A median of 3.0 pain crises occurred in the L-glutamine group, compared with 4.0 in the placebo group (P = .005). Additionally, the median number of hospitalizations was 2.0 for the L-glutamine group versus 3.0 for the placebo group (P = .005).
Nausea, arm or leg pain, and back pain all had an incidence in the L-glutamine group that was 5% higher than in the placebo group, investigators reported.
Based on these results, the Food and Drug administration approved oral L-glutamine powder to reduce the acute complications of sickle cell disease in patients 5 years of age and older in July 2017.
The reasons for study withdrawal were similar in the L-glutamine and placebo groups, despite the higher withdrawal rate in the L-glutamine group, investigators said in a discussion of their results. “Recruitment and retention in a year-long study is difficult in an already burdened population,” they wrote.
The overall noncompletion rate was 32%, similar to the 35% rate seen in a recent multicenter trial of crizanlizumab in patients with sickle cell disease, they added.
Dr. Niihara is the founder and CEO of Emmaus Medical, which sponsored the trial. Other coauthors also reported disclosures related to Emmaus Medical and other companies.
SOURCE: Niihara Y et al. N Engl J Med. 2018 Jul 19;379(3):226-35.
Children and adults with sickle cell disease who received L-glutamine alone or with hydroxyurea had a median number of pain episodes that was 25% lower than those who received placebo, according to newly published results from the phase 3 trial that led to the agent’s approval in 2017.
The median number of hospitalizations was 33% lower among individuals receiving L-glutamine than it was among those receiving placebo, in results reported by investigators led by Yutaka Niihara, MD, of the University of California, Los Angeles, and Emmaus Medical.
Blood test results showed persistent elevation of mean corpuscular volume, indicating adherence to hydroxyurea therapy and suggesting that the effect of L-glutamine might be additive, Dr. Niihara and his coauthors wrote in the New England Journal of Medicine.
“L-glutamine thus provides an alternative therapy for those who decline treatment with hydroxyurea or who may have unacceptable side effects from hydroxyurea, as well as an additive therapy to lower the incidence of pain crises for those who may have suboptimal response to hydroxyurea,” they wrote.
The multicenter, randomized, placebo-controlled, double-blind, phase 3 trial by Dr. Niihara and his colleagues included 230 children and adults with sickle cell anemia or sickle-beta0-thalassemia and two or more pain crises in the previous year.
Participants at 31 sites across the United States were randomized to receive L-glutamine powder (n = 152) or placebo (n = 78) orally twice weekly for 48 weeks, followed by a 3-week tapering period. Two-thirds received concomitant hydroxyurea during the trial.
Participants were contacted by telephone weekly during the study to encourage adherence.
A total of 156 individuals completed the study, including 97 of 152 (63.8%) in the L-glutamine arm and 59 of 78 (75.6%) in the placebo arm. The most common reasons for discontinuation were withdrawal of consent, nonadherence, or reasons classified as “other,” according to investigators.
The primary end point was the number of pain crises through week 48 of the trial. A median of 3.0 pain crises occurred in the L-glutamine group, compared with 4.0 in the placebo group (P = .005). Additionally, the median number of hospitalizations was 2.0 for the L-glutamine group versus 3.0 for the placebo group (P = .005).
Nausea, arm or leg pain, and back pain all had an incidence in the L-glutamine group that was 5% higher than in the placebo group, investigators reported.
Based on these results, the Food and Drug administration approved oral L-glutamine powder to reduce the acute complications of sickle cell disease in patients 5 years of age and older in July 2017.
The reasons for study withdrawal were similar in the L-glutamine and placebo groups, despite the higher withdrawal rate in the L-glutamine group, investigators said in a discussion of their results. “Recruitment and retention in a year-long study is difficult in an already burdened population,” they wrote.
The overall noncompletion rate was 32%, similar to the 35% rate seen in a recent multicenter trial of crizanlizumab in patients with sickle cell disease, they added.
Dr. Niihara is the founder and CEO of Emmaus Medical, which sponsored the trial. Other coauthors also reported disclosures related to Emmaus Medical and other companies.
SOURCE: Niihara Y et al. N Engl J Med. 2018 Jul 19;379(3):226-35.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: The median number of pain crises was 3.0 in the L-glutamine group, compared with 4.0 in the placebo group (P = .005).
Study details: A multicenter, randomized, placebo-controlled, double-blind, phase 3 trial including 230 chidren and adults with sickle cell anemia or sickle-beta0-thalassemia and two or more pain crises in the previous year.
Disclosures: Dr. Niihara is the founder and CEO of Emmaus Medical, which sponsored the trial. Other coauthors also reported disclosures related to Emmaus Medical and other companies. Source: Niihara Y et al. N Engl J Med. 2018 Jul 19;379(3):226-35.
Medicare’s bundled pay plan didn’t deliver big cost savings
Participation in Medicare’s bundled payments initiative didn’t significantly change payments per episode or care outcomes for the top five medical conditions selected under the program, a new analysis shows.
Payments for the common conditions remained around $24,000 per episode before and during participation in the Bundled Payments for Care Improvement (BPCI) initiative for the 125 participating hospitals evaluated in this study, conducted by Karen E. Joynt Maddox, MD, of Washington University, St. Louis, and her coauthors.
The finding contrasts with a previous study showing that hospitals in BPCI successfully lowered overall Medicare payments for patients who underwent joint replacement.
“Bundling of services to encourage more efficient care has great face validity and enjoys bipartisan support,” Dr. Joynt Maddox and her colleagues wrote. “For such bundling to work for medical conditions, however, more time, new care strategies and partnerships, or additional incentives may be required.”
The Center for Medicare & Medicaid Innovation initiated the voluntary BPCI demonstration project in 2013. The program targets 48 conditions that account for about 70% of Medicare spending. Hospitals that achieve cost targets for a specific condition get to keep a portion of the savings, and they reimburse Medicare for part of the difference when costs are exceeded.
The present study focused on 2013-2015 Medicare claims for the five medical conditions that account for two-thirds of patients enrolled in medical bundles: congestive heart failure, pneumonia, chronic obstructive pulmonary disease, sepsis, and acute myocardial infarction.
Mean baseline payments per episode for those conditions were $24,280 before participation in the BPCI. After hospitals joined, their average payments per episode were $23,993 (P = .41). For a set of matched control hospitals, payments were a mean of $23,901 at baseline and $23,503 in the corresponding follow-up period (P = .08).
That amounted to a $286 payment reduction for BPCI hospitals and a $398 reduction for controls, a difference of $112 (P = .79), the study investigators reported.
Changes in length of stay, readmissions, emergency department use, and clinical complexity of cases from baseline to follow-up periods was not significantly different between BPCI and control hospitals. For example, 90-day mortality increases were seen in both groups, and the degree of increase was not statistically different between the groups.
Those data help fill a gap in research on the BPCI program and BPCI Advanced, a related version of the demonstration project that will have its first cohort of participants starting Oct. 1, 2018.
“Despite the importance of episode-based payment, there has been little research examining its efficacy or determining whether it has unintended consequences, such as hospitals’ selecting patients with relatively less complex conditions to reduce costs and improve outcomes,” Dr. Joynt Maddox and her colleagues cautioned.
It’s unclear why the previous joint replacement study showed a successful reduction in costs under BPCI, while the new study did not. However, patients in the new analysis of the most common bundled conditions were older and had higher rates of poverty and disability.
“As a result of these complexities, patients admitted for medical conditions may have had post-acute care needs that were less amenable to intervention,” Dr. Joynt Maddox said.
The investigators added that hospitals’ lack of effective influence on post–acute-care services may blunt their ability to achieve greater savings under BPCI. Better relationships with skilled nursing facilities, long-term care hospitals, home health agencies, and inpatient rehabilitation facilities could make a difference.
The Commonwealth Fund supported the study. One study author reported personal fees from HHS outside the submitted work, and another reported that he is an associate editor for the New England Journal of Medicine. No other disclosures were reported.
SOURCE: Joynt Maddox KE et al. N Engl J Med. 2018 Jul 19;379(3):260-9.
Participation in Medicare’s bundled payments initiative didn’t significantly change payments per episode or care outcomes for the top five medical conditions selected under the program, a new analysis shows.
Payments for the common conditions remained around $24,000 per episode before and during participation in the Bundled Payments for Care Improvement (BPCI) initiative for the 125 participating hospitals evaluated in this study, conducted by Karen E. Joynt Maddox, MD, of Washington University, St. Louis, and her coauthors.
The finding contrasts with a previous study showing that hospitals in BPCI successfully lowered overall Medicare payments for patients who underwent joint replacement.
“Bundling of services to encourage more efficient care has great face validity and enjoys bipartisan support,” Dr. Joynt Maddox and her colleagues wrote. “For such bundling to work for medical conditions, however, more time, new care strategies and partnerships, or additional incentives may be required.”
The Center for Medicare & Medicaid Innovation initiated the voluntary BPCI demonstration project in 2013. The program targets 48 conditions that account for about 70% of Medicare spending. Hospitals that achieve cost targets for a specific condition get to keep a portion of the savings, and they reimburse Medicare for part of the difference when costs are exceeded.
The present study focused on 2013-2015 Medicare claims for the five medical conditions that account for two-thirds of patients enrolled in medical bundles: congestive heart failure, pneumonia, chronic obstructive pulmonary disease, sepsis, and acute myocardial infarction.
Mean baseline payments per episode for those conditions were $24,280 before participation in the BPCI. After hospitals joined, their average payments per episode were $23,993 (P = .41). For a set of matched control hospitals, payments were a mean of $23,901 at baseline and $23,503 in the corresponding follow-up period (P = .08).
That amounted to a $286 payment reduction for BPCI hospitals and a $398 reduction for controls, a difference of $112 (P = .79), the study investigators reported.
Changes in length of stay, readmissions, emergency department use, and clinical complexity of cases from baseline to follow-up periods was not significantly different between BPCI and control hospitals. For example, 90-day mortality increases were seen in both groups, and the degree of increase was not statistically different between the groups.
Those data help fill a gap in research on the BPCI program and BPCI Advanced, a related version of the demonstration project that will have its first cohort of participants starting Oct. 1, 2018.
“Despite the importance of episode-based payment, there has been little research examining its efficacy or determining whether it has unintended consequences, such as hospitals’ selecting patients with relatively less complex conditions to reduce costs and improve outcomes,” Dr. Joynt Maddox and her colleagues cautioned.
It’s unclear why the previous joint replacement study showed a successful reduction in costs under BPCI, while the new study did not. However, patients in the new analysis of the most common bundled conditions were older and had higher rates of poverty and disability.
“As a result of these complexities, patients admitted for medical conditions may have had post-acute care needs that were less amenable to intervention,” Dr. Joynt Maddox said.
The investigators added that hospitals’ lack of effective influence on post–acute-care services may blunt their ability to achieve greater savings under BPCI. Better relationships with skilled nursing facilities, long-term care hospitals, home health agencies, and inpatient rehabilitation facilities could make a difference.
The Commonwealth Fund supported the study. One study author reported personal fees from HHS outside the submitted work, and another reported that he is an associate editor for the New England Journal of Medicine. No other disclosures were reported.
SOURCE: Joynt Maddox KE et al. N Engl J Med. 2018 Jul 19;379(3):260-9.
Participation in Medicare’s bundled payments initiative didn’t significantly change payments per episode or care outcomes for the top five medical conditions selected under the program, a new analysis shows.
Payments for the common conditions remained around $24,000 per episode before and during participation in the Bundled Payments for Care Improvement (BPCI) initiative for the 125 participating hospitals evaluated in this study, conducted by Karen E. Joynt Maddox, MD, of Washington University, St. Louis, and her coauthors.
The finding contrasts with a previous study showing that hospitals in BPCI successfully lowered overall Medicare payments for patients who underwent joint replacement.
“Bundling of services to encourage more efficient care has great face validity and enjoys bipartisan support,” Dr. Joynt Maddox and her colleagues wrote. “For such bundling to work for medical conditions, however, more time, new care strategies and partnerships, or additional incentives may be required.”
The Center for Medicare & Medicaid Innovation initiated the voluntary BPCI demonstration project in 2013. The program targets 48 conditions that account for about 70% of Medicare spending. Hospitals that achieve cost targets for a specific condition get to keep a portion of the savings, and they reimburse Medicare for part of the difference when costs are exceeded.
The present study focused on 2013-2015 Medicare claims for the five medical conditions that account for two-thirds of patients enrolled in medical bundles: congestive heart failure, pneumonia, chronic obstructive pulmonary disease, sepsis, and acute myocardial infarction.
Mean baseline payments per episode for those conditions were $24,280 before participation in the BPCI. After hospitals joined, their average payments per episode were $23,993 (P = .41). For a set of matched control hospitals, payments were a mean of $23,901 at baseline and $23,503 in the corresponding follow-up period (P = .08).
That amounted to a $286 payment reduction for BPCI hospitals and a $398 reduction for controls, a difference of $112 (P = .79), the study investigators reported.
Changes in length of stay, readmissions, emergency department use, and clinical complexity of cases from baseline to follow-up periods was not significantly different between BPCI and control hospitals. For example, 90-day mortality increases were seen in both groups, and the degree of increase was not statistically different between the groups.
Those data help fill a gap in research on the BPCI program and BPCI Advanced, a related version of the demonstration project that will have its first cohort of participants starting Oct. 1, 2018.
“Despite the importance of episode-based payment, there has been little research examining its efficacy or determining whether it has unintended consequences, such as hospitals’ selecting patients with relatively less complex conditions to reduce costs and improve outcomes,” Dr. Joynt Maddox and her colleagues cautioned.
It’s unclear why the previous joint replacement study showed a successful reduction in costs under BPCI, while the new study did not. However, patients in the new analysis of the most common bundled conditions were older and had higher rates of poverty and disability.
“As a result of these complexities, patients admitted for medical conditions may have had post-acute care needs that were less amenable to intervention,” Dr. Joynt Maddox said.
The investigators added that hospitals’ lack of effective influence on post–acute-care services may blunt their ability to achieve greater savings under BPCI. Better relationships with skilled nursing facilities, long-term care hospitals, home health agencies, and inpatient rehabilitation facilities could make a difference.
The Commonwealth Fund supported the study. One study author reported personal fees from HHS outside the submitted work, and another reported that he is an associate editor for the New England Journal of Medicine. No other disclosures were reported.
SOURCE: Joynt Maddox KE et al. N Engl J Med. 2018 Jul 19;379(3):260-9.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Participation in Medicare’s Bundled Payments for Care Improvement (BPCI) initiative didn’t significantly change payments per episode for the top five medical conditions selected under the program.
Major finding: Baseline payments per episode for those conditions were a mean of $24,280 before participation in the BPCI, and $23,993 after adoption (P = .41).
Study details: A retrospective analysis of Medicare data for 125 hospitals participating in the program and matched control hospitals.
Disclosures: The Commonwealth Fund supported the study. One study author reported personal fees from HHS outside the submitted work, and another reported that he is an associate editor for the New England Journal of Medicine.
Source: Joynt Maddox KE et al. N Engl J Med. 2018 Jul 19;379(3):260-9.
Occult blood in feces linked to more than just colorectal cancer mortality
Occult blood in the feces was associated not only with colorectal cancer mortality, but also mortality from other causes, Scottish investigators have reported based on findings of a large, retrospective study.
A positive guaiac fecal occult blood test (gFOBT) was associated with all-cause mortality excluding colorectal cancer in the study, which included data on individuals screened in Scotland during 2000-2016.
The findings might have important clinical implications beyond colorectal cancer if corroborated by prospective studies in the future, wrote investigator Gillian Libby of the Bowel Screening Research Unit at Ninewells Hospital and Medical School, Dundee, Scotland, and coinvestigators.
“If hemoglobin in feces is a risk factor for all-cause death, it may have the potential as a modifiable biomarker that could be used to assess the efficacy of both lifestyle and drug interventions to reduce the risk of premature mortality,” investigators wrote in a report on the study released in the journal Gut.
The investigators linked gFOBT results for 133,921 screened individuals who ranged in age from 50 to 74 years to mortality data from the National Records of Scotland Database.
As expected, individuals with positive results had a considerably higher risk of death not only from colorectal cancer (hazard ratio, 7.79; 95% confidence interval, 6.13-9.89; P less than .0001) but also for noncolorectal cancer causes combined (HR, 1.58; 95% CI, 1.45-1.73; P less than .0001) after adjustment for age, sex, deprivation, and prescribed medicines.
The higher risk of death held for mortality related to circulatory, respiratory, digestive, endocrine, neuropsychological, and other causes, as reported.
“It is clear from this study that, in the Scottish population, the presence of hemoglobin in the faeces as detected by gFOBT is associated with a number of non-CRC causes of death,” investigators wrote.
These results do corroborate those of one other recent study in Taiwan that showed a relationship between positive gFOBT tests and all-cause mortality.
“In contrast to the Taiwanese study, we were able to examine this association broken down by disease categories and adjusting for confounding factors,” they noted in their discussion of the results.
Funding for the study came from the Chief Scientist Office of the Scottish Government Health Directorates. One study coauthor reported a consultancy with Immunostics, and no other disclosures were reported.
SOURCE: Libby G et al. Gut. 2018. doi: 10.1136/gutjnl-2018-316483.
This study makes the “provocative” suggestion that occult blood in feces may reveal more than was previously thought, Uri Ladabaum, MD, of Stanford (Calif.) University wrote in a commentary.
“If the eye is the window to the soul, is a fecal test the window to general health?” he asked in the commentary appearing in the journal Gut.
The initial surprise that a positive guaiac fecal occult blood test is associated with more than just colorectal cancer (CRC) mortality might be tempered, however, after considering that risk factors for many diseases are integrated, Dr. Ladabaum said. In other words, risk factors for CRC, such as obesity, inactivity, poor diet, or diabetes, may be at least partly responsible for the effects on non-CRC death seen in this study, although authors did try to control for some of those factors in their analyses, he said.
Whether a positive guaiac fecal occult blood test should prompt any additional interventions or alerts to the patient remains a question to be resolved, according to Dr. Ladabaum. “For now, I believe that our enthusiasm for the established CRC screening methods should not be affected, and that the focus after an abnormal fecal occult blood test should be to ensure prompt delivery of a follow-up colonoscopy,” he wrote.
Dr. Ladabaum is with the division of gastroenterology and hepatology and the department of medicine at Stanford (Calif.) University. These comments are from his commentary in Gut (2018. doi: 10.1136/gutjnl-2018-316762). Dr. Ladabaum reported being a consultant for Medtronic and Motus and an advisory board member of Universal Dx.
This study makes the “provocative” suggestion that occult blood in feces may reveal more than was previously thought, Uri Ladabaum, MD, of Stanford (Calif.) University wrote in a commentary.
“If the eye is the window to the soul, is a fecal test the window to general health?” he asked in the commentary appearing in the journal Gut.
The initial surprise that a positive guaiac fecal occult blood test is associated with more than just colorectal cancer (CRC) mortality might be tempered, however, after considering that risk factors for many diseases are integrated, Dr. Ladabaum said. In other words, risk factors for CRC, such as obesity, inactivity, poor diet, or diabetes, may be at least partly responsible for the effects on non-CRC death seen in this study, although authors did try to control for some of those factors in their analyses, he said.
Whether a positive guaiac fecal occult blood test should prompt any additional interventions or alerts to the patient remains a question to be resolved, according to Dr. Ladabaum. “For now, I believe that our enthusiasm for the established CRC screening methods should not be affected, and that the focus after an abnormal fecal occult blood test should be to ensure prompt delivery of a follow-up colonoscopy,” he wrote.
Dr. Ladabaum is with the division of gastroenterology and hepatology and the department of medicine at Stanford (Calif.) University. These comments are from his commentary in Gut (2018. doi: 10.1136/gutjnl-2018-316762). Dr. Ladabaum reported being a consultant for Medtronic and Motus and an advisory board member of Universal Dx.
This study makes the “provocative” suggestion that occult blood in feces may reveal more than was previously thought, Uri Ladabaum, MD, of Stanford (Calif.) University wrote in a commentary.
“If the eye is the window to the soul, is a fecal test the window to general health?” he asked in the commentary appearing in the journal Gut.
The initial surprise that a positive guaiac fecal occult blood test is associated with more than just colorectal cancer (CRC) mortality might be tempered, however, after considering that risk factors for many diseases are integrated, Dr. Ladabaum said. In other words, risk factors for CRC, such as obesity, inactivity, poor diet, or diabetes, may be at least partly responsible for the effects on non-CRC death seen in this study, although authors did try to control for some of those factors in their analyses, he said.
Whether a positive guaiac fecal occult blood test should prompt any additional interventions or alerts to the patient remains a question to be resolved, according to Dr. Ladabaum. “For now, I believe that our enthusiasm for the established CRC screening methods should not be affected, and that the focus after an abnormal fecal occult blood test should be to ensure prompt delivery of a follow-up colonoscopy,” he wrote.
Dr. Ladabaum is with the division of gastroenterology and hepatology and the department of medicine at Stanford (Calif.) University. These comments are from his commentary in Gut (2018. doi: 10.1136/gutjnl-2018-316762). Dr. Ladabaum reported being a consultant for Medtronic and Motus and an advisory board member of Universal Dx.
Occult blood in the feces was associated not only with colorectal cancer mortality, but also mortality from other causes, Scottish investigators have reported based on findings of a large, retrospective study.
A positive guaiac fecal occult blood test (gFOBT) was associated with all-cause mortality excluding colorectal cancer in the study, which included data on individuals screened in Scotland during 2000-2016.
The findings might have important clinical implications beyond colorectal cancer if corroborated by prospective studies in the future, wrote investigator Gillian Libby of the Bowel Screening Research Unit at Ninewells Hospital and Medical School, Dundee, Scotland, and coinvestigators.
“If hemoglobin in feces is a risk factor for all-cause death, it may have the potential as a modifiable biomarker that could be used to assess the efficacy of both lifestyle and drug interventions to reduce the risk of premature mortality,” investigators wrote in a report on the study released in the journal Gut.
The investigators linked gFOBT results for 133,921 screened individuals who ranged in age from 50 to 74 years to mortality data from the National Records of Scotland Database.
As expected, individuals with positive results had a considerably higher risk of death not only from colorectal cancer (hazard ratio, 7.79; 95% confidence interval, 6.13-9.89; P less than .0001) but also for noncolorectal cancer causes combined (HR, 1.58; 95% CI, 1.45-1.73; P less than .0001) after adjustment for age, sex, deprivation, and prescribed medicines.
The higher risk of death held for mortality related to circulatory, respiratory, digestive, endocrine, neuropsychological, and other causes, as reported.
“It is clear from this study that, in the Scottish population, the presence of hemoglobin in the faeces as detected by gFOBT is associated with a number of non-CRC causes of death,” investigators wrote.
These results do corroborate those of one other recent study in Taiwan that showed a relationship between positive gFOBT tests and all-cause mortality.
“In contrast to the Taiwanese study, we were able to examine this association broken down by disease categories and adjusting for confounding factors,” they noted in their discussion of the results.
Funding for the study came from the Chief Scientist Office of the Scottish Government Health Directorates. One study coauthor reported a consultancy with Immunostics, and no other disclosures were reported.
SOURCE: Libby G et al. Gut. 2018. doi: 10.1136/gutjnl-2018-316483.
Occult blood in the feces was associated not only with colorectal cancer mortality, but also mortality from other causes, Scottish investigators have reported based on findings of a large, retrospective study.
A positive guaiac fecal occult blood test (gFOBT) was associated with all-cause mortality excluding colorectal cancer in the study, which included data on individuals screened in Scotland during 2000-2016.
The findings might have important clinical implications beyond colorectal cancer if corroborated by prospective studies in the future, wrote investigator Gillian Libby of the Bowel Screening Research Unit at Ninewells Hospital and Medical School, Dundee, Scotland, and coinvestigators.
“If hemoglobin in feces is a risk factor for all-cause death, it may have the potential as a modifiable biomarker that could be used to assess the efficacy of both lifestyle and drug interventions to reduce the risk of premature mortality,” investigators wrote in a report on the study released in the journal Gut.
The investigators linked gFOBT results for 133,921 screened individuals who ranged in age from 50 to 74 years to mortality data from the National Records of Scotland Database.
As expected, individuals with positive results had a considerably higher risk of death not only from colorectal cancer (hazard ratio, 7.79; 95% confidence interval, 6.13-9.89; P less than .0001) but also for noncolorectal cancer causes combined (HR, 1.58; 95% CI, 1.45-1.73; P less than .0001) after adjustment for age, sex, deprivation, and prescribed medicines.
The higher risk of death held for mortality related to circulatory, respiratory, digestive, endocrine, neuropsychological, and other causes, as reported.
“It is clear from this study that, in the Scottish population, the presence of hemoglobin in the faeces as detected by gFOBT is associated with a number of non-CRC causes of death,” investigators wrote.
These results do corroborate those of one other recent study in Taiwan that showed a relationship between positive gFOBT tests and all-cause mortality.
“In contrast to the Taiwanese study, we were able to examine this association broken down by disease categories and adjusting for confounding factors,” they noted in their discussion of the results.
Funding for the study came from the Chief Scientist Office of the Scottish Government Health Directorates. One study coauthor reported a consultancy with Immunostics, and no other disclosures were reported.
SOURCE: Libby G et al. Gut. 2018. doi: 10.1136/gutjnl-2018-316483.
FROM GUT
Key clinical point: Occult blood in the feces may be associated with not only colorectal cancer mortality, but also mortality from other causes.
Major finding: A positive fecal occult blood test was associated with a higher risk of death from noncolorectal cancer causes (adjusted hazard ratio, 1.58; 95% confidence interval, 1.45-1.73; P less than .0001).
Study details: A retrospective study in Scotland based on 133,921 screened individuals with linked mortality data.
Disclosures: Funding for the study came from the Chief Scientist Office of the Scottish Government Health Directorates. One study coauthor reported a consultancy with Immunostics.
Source: Libby G et al. Gut. 2018. doi: 10.1136/gutjnl-2018-316483.
Probiotics RCTs lack needed safety data, report says
, authors of a systematic review have concluded.
Out of 384 randomized clinical trials, nearly a third gave no information on potential harms associated with probiotics, prebiotics, or products that combine the two, according to authors of the review, which appears in Annals of Internal Medicine.
Only 2% of the trials adequately reported all key safety components, said the authors, led by Aïda Bafeta, PhD, Centre d’Épidémiologie Clinique, Hôpital Hôtel-Dieu, Paris.
“The inadequacy in reporting harms-related results may lead to an inaccurate safety profile and erroneous decision making, with major consequences for patients,” Dr. Bafeta and her colleagues wrote in their review.
While some may assume detailed safety evaluation is unnecessary, caution is especially needed when considering use of probiotics and prebiotics in patients who are vulnerable or critically ill, according to the authors.
“More worrying is that potential risks have been described in case reports and clinical trial results,” they wrote.
Dr. Bafeta and her coauthors cited a 2008 randomized, placebo-controlled trial published in The Lancet showing an increased risk of mortality associated with a particular combination of probiotic strains administered as prophylaxis in patients with predicted severe acute pancreatitis.
A 2011 report by the Agency for Healthcare Research and Quality found that current literature at that time was “not well equipped” to answer with confidence on the safety of probiotics as administered in clinical trials.
In the present report, Dr. Bafeta and her colleagues conducted a systematic review of 384 published randomized trials assessing probiotics, prebiotics, or synbiotics, which are products that combine probiotics and probiotics.
They found that 28% (106 trials) gave no information at all related to harms, while 90% (347) failed to define adverse events, and 97% (372) left out any mention of methods for collecting harms-related information.
Out of 53 studies including hospitalized or critical care patients, 7 reported the number of serious adverse events per study group, they said.
When safety data were included, reporting was often inadequate, according to Dr. Bafeta and her colleagues. Generic statements were used in 37% of the randomized trials, while 5% gave only global statistical comparisons.
Only 2% (nine trials) reported all safety-related parameters recommended by guidelines, such as adverse event definitions, seriousness of adverse events, and number of participant withdrawals due to harms, the reviewers found.
“The safety profile of an intervention should never be presumed,” they wrote. “Rather, it should be rigorously evaluated and reported.”
Probiotics and prebiotics are of increasing interest as treatments that may modify gut microbiota, potentially resulting in health benefits, they said. Probiotics are live microorganisms administered to confer a health benefit in the gut, while prebiotics are ingredients that change the composition or activity of gut microbiota.
No reviews previous to this one have assessed the adequacy of reporting adverse effects in trials of probiotics, prebiotics, and synbiotics, according to Dr. Bafeta and her colleagues, who reported no conflicts of interest associated with their review.
SOURCE: Bafeta A et al. Ann Intern Med. 2018 Jul 17.
, authors of a systematic review have concluded.
Out of 384 randomized clinical trials, nearly a third gave no information on potential harms associated with probiotics, prebiotics, or products that combine the two, according to authors of the review, which appears in Annals of Internal Medicine.
Only 2% of the trials adequately reported all key safety components, said the authors, led by Aïda Bafeta, PhD, Centre d’Épidémiologie Clinique, Hôpital Hôtel-Dieu, Paris.
“The inadequacy in reporting harms-related results may lead to an inaccurate safety profile and erroneous decision making, with major consequences for patients,” Dr. Bafeta and her colleagues wrote in their review.
While some may assume detailed safety evaluation is unnecessary, caution is especially needed when considering use of probiotics and prebiotics in patients who are vulnerable or critically ill, according to the authors.
“More worrying is that potential risks have been described in case reports and clinical trial results,” they wrote.
Dr. Bafeta and her coauthors cited a 2008 randomized, placebo-controlled trial published in The Lancet showing an increased risk of mortality associated with a particular combination of probiotic strains administered as prophylaxis in patients with predicted severe acute pancreatitis.
A 2011 report by the Agency for Healthcare Research and Quality found that current literature at that time was “not well equipped” to answer with confidence on the safety of probiotics as administered in clinical trials.
In the present report, Dr. Bafeta and her colleagues conducted a systematic review of 384 published randomized trials assessing probiotics, prebiotics, or synbiotics, which are products that combine probiotics and probiotics.
They found that 28% (106 trials) gave no information at all related to harms, while 90% (347) failed to define adverse events, and 97% (372) left out any mention of methods for collecting harms-related information.
Out of 53 studies including hospitalized or critical care patients, 7 reported the number of serious adverse events per study group, they said.
When safety data were included, reporting was often inadequate, according to Dr. Bafeta and her colleagues. Generic statements were used in 37% of the randomized trials, while 5% gave only global statistical comparisons.
Only 2% (nine trials) reported all safety-related parameters recommended by guidelines, such as adverse event definitions, seriousness of adverse events, and number of participant withdrawals due to harms, the reviewers found.
“The safety profile of an intervention should never be presumed,” they wrote. “Rather, it should be rigorously evaluated and reported.”
Probiotics and prebiotics are of increasing interest as treatments that may modify gut microbiota, potentially resulting in health benefits, they said. Probiotics are live microorganisms administered to confer a health benefit in the gut, while prebiotics are ingredients that change the composition or activity of gut microbiota.
No reviews previous to this one have assessed the adequacy of reporting adverse effects in trials of probiotics, prebiotics, and synbiotics, according to Dr. Bafeta and her colleagues, who reported no conflicts of interest associated with their review.
SOURCE: Bafeta A et al. Ann Intern Med. 2018 Jul 17.
, authors of a systematic review have concluded.
Out of 384 randomized clinical trials, nearly a third gave no information on potential harms associated with probiotics, prebiotics, or products that combine the two, according to authors of the review, which appears in Annals of Internal Medicine.
Only 2% of the trials adequately reported all key safety components, said the authors, led by Aïda Bafeta, PhD, Centre d’Épidémiologie Clinique, Hôpital Hôtel-Dieu, Paris.
“The inadequacy in reporting harms-related results may lead to an inaccurate safety profile and erroneous decision making, with major consequences for patients,” Dr. Bafeta and her colleagues wrote in their review.
While some may assume detailed safety evaluation is unnecessary, caution is especially needed when considering use of probiotics and prebiotics in patients who are vulnerable or critically ill, according to the authors.
“More worrying is that potential risks have been described in case reports and clinical trial results,” they wrote.
Dr. Bafeta and her coauthors cited a 2008 randomized, placebo-controlled trial published in The Lancet showing an increased risk of mortality associated with a particular combination of probiotic strains administered as prophylaxis in patients with predicted severe acute pancreatitis.
A 2011 report by the Agency for Healthcare Research and Quality found that current literature at that time was “not well equipped” to answer with confidence on the safety of probiotics as administered in clinical trials.
In the present report, Dr. Bafeta and her colleagues conducted a systematic review of 384 published randomized trials assessing probiotics, prebiotics, or synbiotics, which are products that combine probiotics and probiotics.
They found that 28% (106 trials) gave no information at all related to harms, while 90% (347) failed to define adverse events, and 97% (372) left out any mention of methods for collecting harms-related information.
Out of 53 studies including hospitalized or critical care patients, 7 reported the number of serious adverse events per study group, they said.
When safety data were included, reporting was often inadequate, according to Dr. Bafeta and her colleagues. Generic statements were used in 37% of the randomized trials, while 5% gave only global statistical comparisons.
Only 2% (nine trials) reported all safety-related parameters recommended by guidelines, such as adverse event definitions, seriousness of adverse events, and number of participant withdrawals due to harms, the reviewers found.
“The safety profile of an intervention should never be presumed,” they wrote. “Rather, it should be rigorously evaluated and reported.”
Probiotics and prebiotics are of increasing interest as treatments that may modify gut microbiota, potentially resulting in health benefits, they said. Probiotics are live microorganisms administered to confer a health benefit in the gut, while prebiotics are ingredients that change the composition or activity of gut microbiota.
No reviews previous to this one have assessed the adequacy of reporting adverse effects in trials of probiotics, prebiotics, and synbiotics, according to Dr. Bafeta and her colleagues, who reported no conflicts of interest associated with their review.
SOURCE: Bafeta A et al. Ann Intern Med. 2018 Jul 17.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Clinical trials of interventions designed to modify gut microbiota are often lacking adverse event data, making broad conclusions about their safety impossible.
Major finding: Nearly one-third of trials gave no information on potential harms associated with the probiotics, prebiotics, or synbiotics under study, and only 2% reported all key safety components.
Study details: A systematic review of 384 published randomized trials assessing probiotics, prebiotics, or synbiotics,
Disclosures: The study authors reported no conflicts of interest.
Source: Bafeta A et al. Ann Intern Med. 2018 Jul 17.