User login
Produce and promises
Most of us are in medicine because we find joy and fulfillment in treating patients. That’s why we signed up for the long educational slog, and why many of us continue to practice medicine long after all the bills have been paid. That is why we all find obstructions between us and our patients so maddening.
I guess Medicare was a great boon for seniors, who found health insurance increasingly more difficult to afford, and for doctors, who now got paid in something other than produce and promises by indigent, elderly patients. The American Medical Association opposed the adoption of Medicare, fearing that it would interfere with the physician-patient relationship. This may sound quaint now, especially at a time when there are calls for Medicare for all. While it is hard to argue against Medicare improving access to health care, the AMA was right about the government’s intrusion into the physician-patient relationship, which has become progressively more intrusive. Medicare has undergone major revisions at least five times; none of these revisions has simplified care. Think about the steadily increasing documentation requirements, audits, inflation-ravaged fee schedules, and MIPS [Merit-Based Incentive Payment System], and MACRA [Medicare Access and CHIP Reauthorization Act of 2015], although the current proposed Medicare rule, with a two-level fee schedule and reduced documentation, claims to eliminate 50 hours of charting per year.
The next big blow was ERISA (the Employee Retirement Income Security Act of 1974), which really did not seem relevant to medical practice at the time. However, embedded in this law was indemnification of insurers from patient lawsuits. Well, OK, insurers don’t practice medicine, right? Fast-forward to today, when critical medical decisions, including which test can be ordered and which drug can be administered, are driven by insurers – who can delay or refuse care and who cannot be legally blamed for the death or harm of the patient. That’s right, step therapy and prior authorizations would not be possible without ERISA.
Of course, absolutely the most onerous intrusion on the physician-patient relationship is the American Recovery and Reinvestment Act of 2014, which mandated electronic health records. I believe this is the major cause of current physician burnout, which has created the worst and most intrusive barrier between physicians and patients to date. Talk about good intentions gone awry!
In addition, now private equity has entered into medicine, in part in response to these issues and intrusions. But has this improved the patient-physician relationship, or just made things worse?
A big selling point of these private equity–backed groups is the central handling of administrative issues, such as billing, coding, compliance, human resources, prior authorizations, as well as other back-office functions. Some groups even claim to improve patient care and value, by instituting quality metrics for care (I would love to see these published). These services all must be paid for, and the logical argument is that pooling these services will result in efficiency and cost less overall.
Maybe so, but private equity creates yet another barrier between the patient and the physician while it eliminate others. These businesses are driven by profit; they are private equity after all. They are a more insidious threat to the physician-patient relationship and the future of medicine than are clumsy laws, since private equity commoditizes patients and their care. .
Any barrier between the patient and the physician is bad, and two or three barriers make things logarithmically worse. No wonder physicians have become cynical and disillusioned. It makes you pause and wonder, how much do we currently pay in time and overhead to navigate these barriers? Maybe we should call it all even. Maybe we would come out ahead if we counted in produce, promises, and unobstructed patient care.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Most of us are in medicine because we find joy and fulfillment in treating patients. That’s why we signed up for the long educational slog, and why many of us continue to practice medicine long after all the bills have been paid. That is why we all find obstructions between us and our patients so maddening.
I guess Medicare was a great boon for seniors, who found health insurance increasingly more difficult to afford, and for doctors, who now got paid in something other than produce and promises by indigent, elderly patients. The American Medical Association opposed the adoption of Medicare, fearing that it would interfere with the physician-patient relationship. This may sound quaint now, especially at a time when there are calls for Medicare for all. While it is hard to argue against Medicare improving access to health care, the AMA was right about the government’s intrusion into the physician-patient relationship, which has become progressively more intrusive. Medicare has undergone major revisions at least five times; none of these revisions has simplified care. Think about the steadily increasing documentation requirements, audits, inflation-ravaged fee schedules, and MIPS [Merit-Based Incentive Payment System], and MACRA [Medicare Access and CHIP Reauthorization Act of 2015], although the current proposed Medicare rule, with a two-level fee schedule and reduced documentation, claims to eliminate 50 hours of charting per year.
The next big blow was ERISA (the Employee Retirement Income Security Act of 1974), which really did not seem relevant to medical practice at the time. However, embedded in this law was indemnification of insurers from patient lawsuits. Well, OK, insurers don’t practice medicine, right? Fast-forward to today, when critical medical decisions, including which test can be ordered and which drug can be administered, are driven by insurers – who can delay or refuse care and who cannot be legally blamed for the death or harm of the patient. That’s right, step therapy and prior authorizations would not be possible without ERISA.
Of course, absolutely the most onerous intrusion on the physician-patient relationship is the American Recovery and Reinvestment Act of 2014, which mandated electronic health records. I believe this is the major cause of current physician burnout, which has created the worst and most intrusive barrier between physicians and patients to date. Talk about good intentions gone awry!
In addition, now private equity has entered into medicine, in part in response to these issues and intrusions. But has this improved the patient-physician relationship, or just made things worse?
A big selling point of these private equity–backed groups is the central handling of administrative issues, such as billing, coding, compliance, human resources, prior authorizations, as well as other back-office functions. Some groups even claim to improve patient care and value, by instituting quality metrics for care (I would love to see these published). These services all must be paid for, and the logical argument is that pooling these services will result in efficiency and cost less overall.
Maybe so, but private equity creates yet another barrier between the patient and the physician while it eliminate others. These businesses are driven by profit; they are private equity after all. They are a more insidious threat to the physician-patient relationship and the future of medicine than are clumsy laws, since private equity commoditizes patients and their care. .
Any barrier between the patient and the physician is bad, and two or three barriers make things logarithmically worse. No wonder physicians have become cynical and disillusioned. It makes you pause and wonder, how much do we currently pay in time and overhead to navigate these barriers? Maybe we should call it all even. Maybe we would come out ahead if we counted in produce, promises, and unobstructed patient care.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Most of us are in medicine because we find joy and fulfillment in treating patients. That’s why we signed up for the long educational slog, and why many of us continue to practice medicine long after all the bills have been paid. That is why we all find obstructions between us and our patients so maddening.
I guess Medicare was a great boon for seniors, who found health insurance increasingly more difficult to afford, and for doctors, who now got paid in something other than produce and promises by indigent, elderly patients. The American Medical Association opposed the adoption of Medicare, fearing that it would interfere with the physician-patient relationship. This may sound quaint now, especially at a time when there are calls for Medicare for all. While it is hard to argue against Medicare improving access to health care, the AMA was right about the government’s intrusion into the physician-patient relationship, which has become progressively more intrusive. Medicare has undergone major revisions at least five times; none of these revisions has simplified care. Think about the steadily increasing documentation requirements, audits, inflation-ravaged fee schedules, and MIPS [Merit-Based Incentive Payment System], and MACRA [Medicare Access and CHIP Reauthorization Act of 2015], although the current proposed Medicare rule, with a two-level fee schedule and reduced documentation, claims to eliminate 50 hours of charting per year.
The next big blow was ERISA (the Employee Retirement Income Security Act of 1974), which really did not seem relevant to medical practice at the time. However, embedded in this law was indemnification of insurers from patient lawsuits. Well, OK, insurers don’t practice medicine, right? Fast-forward to today, when critical medical decisions, including which test can be ordered and which drug can be administered, are driven by insurers – who can delay or refuse care and who cannot be legally blamed for the death or harm of the patient. That’s right, step therapy and prior authorizations would not be possible without ERISA.
Of course, absolutely the most onerous intrusion on the physician-patient relationship is the American Recovery and Reinvestment Act of 2014, which mandated electronic health records. I believe this is the major cause of current physician burnout, which has created the worst and most intrusive barrier between physicians and patients to date. Talk about good intentions gone awry!
In addition, now private equity has entered into medicine, in part in response to these issues and intrusions. But has this improved the patient-physician relationship, or just made things worse?
A big selling point of these private equity–backed groups is the central handling of administrative issues, such as billing, coding, compliance, human resources, prior authorizations, as well as other back-office functions. Some groups even claim to improve patient care and value, by instituting quality metrics for care (I would love to see these published). These services all must be paid for, and the logical argument is that pooling these services will result in efficiency and cost less overall.
Maybe so, but private equity creates yet another barrier between the patient and the physician while it eliminate others. These businesses are driven by profit; they are private equity after all. They are a more insidious threat to the physician-patient relationship and the future of medicine than are clumsy laws, since private equity commoditizes patients and their care. .
Any barrier between the patient and the physician is bad, and two or three barriers make things logarithmically worse. No wonder physicians have become cynical and disillusioned. It makes you pause and wonder, how much do we currently pay in time and overhead to navigate these barriers? Maybe we should call it all even. Maybe we would come out ahead if we counted in produce, promises, and unobstructed patient care.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The 2019 Medicare proposed rule might just make your head explode
When sitting through interminable meetings, endless reports, and unfocused discussions, I often feel a building pressure in my head that, if it continues, will surely result in my brain exploding. I used to carry in my pocket an elastic compression bandage, intending to wrap it around my head as a signal to the offending speakers, but never had the heart to use it. Still, that bandage in my pocket was the backup resource that gave me solace, gave me patience.
Yet, my emergency bandage was nowhere to be found while I was reading the 2019 Medicare proposed rule, which unexpectedly triggered the threat of a brain explosion.
I was prepared for the usual proposed rule of about 1,500 pages of dense, bureaucratic “Engfish,” proposing a cut here, a tuck there, an occasional evisceration, and several correctable errors. This time, though, the proposed rule is wide open, disruptive, uninformed, and disappointing to almost all medical practitioners.
For dermatology, it starts out promisingly, by collapsing the evaluation and management (E/M) codes into two levels, instead of five. That should benefit us slightly, because our coding usually falls at about level three. Also, it would simplify record keeping by only requiring level two documentation and not making docs repeatedly reenter data. Well, OK so far.
Keep reading, though, and then the hammer falls: a proposed 50% reduction in reimbursement for any procedure performed on the same day as the E/M code. What?! Implementation of this change would result in an estimated 20% reduction in reimbursement for dermatologists who, as a courtesy to their patients, do procedures on the same day as an evaluation visit. And this proposed change would likely hurt ophthalmologists, otolaryngologists, and even primary care physicians who do same-day procedures.
There are new extended-care codes that only primary care docs could use, and some other extended care codes for specialists (dermatology is not mentioned) that pay about $5 extra. There is a bone thrown to telemedicine, since telemedicine coverage is supported, including “store and forward,” but not if the patient is seen in person within a week, “or at the soonest available appointment.” Very strange.
The current reimbursement system is a carefully honed, carefully balanced, work of reasonable rational thought by the current procedural terminology committee, the American Medical Association’s RVS Update Committee (RUC) and the Centers for Medicare & Medicaid Services. CMS officials sit at the table at all these meetings, frequently comment, and the agency has the power of final approval. No one loves the final product, particularly the participants, but there are procedures and rules, an appeals process, and the process allows for a rough form of justice administered by your medical peers. Who better to decide what is fair to pay anyone out of a fixed reimbursement pool?
Unfortunately, there seems to be no institutional memory in this year’s final rule. For example, since it came out, various branches of organized medicine have held urgent meetings at which it was pointed out that a 50% reduction in procedures on the same day as an evaluation and management code is inappropriate, since the overlapping work and practice expense already had been removed for such codes by the relative value update committee. This observation reportedly came as a surprise to the CMS attendees – a most disturbing admission.
There was also discouraging news about the global period survey. Dermatology reported only 3% of the global visits possible.
It turns out that CMS did not look for additional 99024 visits beyond the 10- or 90-day global period in the surveyed states and did not look at practices of fewer than 10 dermatologists, even if they did report. Think about it, how many dermatology groups do you know of 10 or more dermatologists in Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, and Rhode Island? How often do you delay suture removal beyond 10 days? How many times do you see a patient back for a triamcinolone injection or reassurance at no charge more than 10 days after procedures? Talk about a flawed process destined to fail!
The loss of global periods will hurt much, much more than the 50% cut in procedures on the same day as an E/M code. The premalignant and benign destruction codes could be cut by 75% – and good luck in charging for suture removal after surgery. We are talking about another 20% reimbursement cut if implemented.
The American Academy of Dermatology and other dermatology societies are actively involved in responding to the CMS regarding the shortcomings of the proposed rule. Be prepared to be called upon to submit your comments to CMS soon. I am hopeful that much of these misguided proposals can be corrected, but it will take a concerted effort of numerous individual dermatologists, including you.
Finally, I advise you to read the final rule for yourself. And, unlike me, do not forget to keep your emergency wrap handy!
Comments will be taken at www.regulations.gov through Sept. 10, 2018.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected] .
When sitting through interminable meetings, endless reports, and unfocused discussions, I often feel a building pressure in my head that, if it continues, will surely result in my brain exploding. I used to carry in my pocket an elastic compression bandage, intending to wrap it around my head as a signal to the offending speakers, but never had the heart to use it. Still, that bandage in my pocket was the backup resource that gave me solace, gave me patience.
Yet, my emergency bandage was nowhere to be found while I was reading the 2019 Medicare proposed rule, which unexpectedly triggered the threat of a brain explosion.
I was prepared for the usual proposed rule of about 1,500 pages of dense, bureaucratic “Engfish,” proposing a cut here, a tuck there, an occasional evisceration, and several correctable errors. This time, though, the proposed rule is wide open, disruptive, uninformed, and disappointing to almost all medical practitioners.
For dermatology, it starts out promisingly, by collapsing the evaluation and management (E/M) codes into two levels, instead of five. That should benefit us slightly, because our coding usually falls at about level three. Also, it would simplify record keeping by only requiring level two documentation and not making docs repeatedly reenter data. Well, OK so far.
Keep reading, though, and then the hammer falls: a proposed 50% reduction in reimbursement for any procedure performed on the same day as the E/M code. What?! Implementation of this change would result in an estimated 20% reduction in reimbursement for dermatologists who, as a courtesy to their patients, do procedures on the same day as an evaluation visit. And this proposed change would likely hurt ophthalmologists, otolaryngologists, and even primary care physicians who do same-day procedures.
There are new extended-care codes that only primary care docs could use, and some other extended care codes for specialists (dermatology is not mentioned) that pay about $5 extra. There is a bone thrown to telemedicine, since telemedicine coverage is supported, including “store and forward,” but not if the patient is seen in person within a week, “or at the soonest available appointment.” Very strange.
The current reimbursement system is a carefully honed, carefully balanced, work of reasonable rational thought by the current procedural terminology committee, the American Medical Association’s RVS Update Committee (RUC) and the Centers for Medicare & Medicaid Services. CMS officials sit at the table at all these meetings, frequently comment, and the agency has the power of final approval. No one loves the final product, particularly the participants, but there are procedures and rules, an appeals process, and the process allows for a rough form of justice administered by your medical peers. Who better to decide what is fair to pay anyone out of a fixed reimbursement pool?
Unfortunately, there seems to be no institutional memory in this year’s final rule. For example, since it came out, various branches of organized medicine have held urgent meetings at which it was pointed out that a 50% reduction in procedures on the same day as an evaluation and management code is inappropriate, since the overlapping work and practice expense already had been removed for such codes by the relative value update committee. This observation reportedly came as a surprise to the CMS attendees – a most disturbing admission.
There was also discouraging news about the global period survey. Dermatology reported only 3% of the global visits possible.
It turns out that CMS did not look for additional 99024 visits beyond the 10- or 90-day global period in the surveyed states and did not look at practices of fewer than 10 dermatologists, even if they did report. Think about it, how many dermatology groups do you know of 10 or more dermatologists in Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, and Rhode Island? How often do you delay suture removal beyond 10 days? How many times do you see a patient back for a triamcinolone injection or reassurance at no charge more than 10 days after procedures? Talk about a flawed process destined to fail!
The loss of global periods will hurt much, much more than the 50% cut in procedures on the same day as an E/M code. The premalignant and benign destruction codes could be cut by 75% – and good luck in charging for suture removal after surgery. We are talking about another 20% reimbursement cut if implemented.
The American Academy of Dermatology and other dermatology societies are actively involved in responding to the CMS regarding the shortcomings of the proposed rule. Be prepared to be called upon to submit your comments to CMS soon. I am hopeful that much of these misguided proposals can be corrected, but it will take a concerted effort of numerous individual dermatologists, including you.
Finally, I advise you to read the final rule for yourself. And, unlike me, do not forget to keep your emergency wrap handy!
Comments will be taken at www.regulations.gov through Sept. 10, 2018.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected] .
When sitting through interminable meetings, endless reports, and unfocused discussions, I often feel a building pressure in my head that, if it continues, will surely result in my brain exploding. I used to carry in my pocket an elastic compression bandage, intending to wrap it around my head as a signal to the offending speakers, but never had the heart to use it. Still, that bandage in my pocket was the backup resource that gave me solace, gave me patience.
Yet, my emergency bandage was nowhere to be found while I was reading the 2019 Medicare proposed rule, which unexpectedly triggered the threat of a brain explosion.
I was prepared for the usual proposed rule of about 1,500 pages of dense, bureaucratic “Engfish,” proposing a cut here, a tuck there, an occasional evisceration, and several correctable errors. This time, though, the proposed rule is wide open, disruptive, uninformed, and disappointing to almost all medical practitioners.
For dermatology, it starts out promisingly, by collapsing the evaluation and management (E/M) codes into two levels, instead of five. That should benefit us slightly, because our coding usually falls at about level three. Also, it would simplify record keeping by only requiring level two documentation and not making docs repeatedly reenter data. Well, OK so far.
Keep reading, though, and then the hammer falls: a proposed 50% reduction in reimbursement for any procedure performed on the same day as the E/M code. What?! Implementation of this change would result in an estimated 20% reduction in reimbursement for dermatologists who, as a courtesy to their patients, do procedures on the same day as an evaluation visit. And this proposed change would likely hurt ophthalmologists, otolaryngologists, and even primary care physicians who do same-day procedures.
There are new extended-care codes that only primary care docs could use, and some other extended care codes for specialists (dermatology is not mentioned) that pay about $5 extra. There is a bone thrown to telemedicine, since telemedicine coverage is supported, including “store and forward,” but not if the patient is seen in person within a week, “or at the soonest available appointment.” Very strange.
The current reimbursement system is a carefully honed, carefully balanced, work of reasonable rational thought by the current procedural terminology committee, the American Medical Association’s RVS Update Committee (RUC) and the Centers for Medicare & Medicaid Services. CMS officials sit at the table at all these meetings, frequently comment, and the agency has the power of final approval. No one loves the final product, particularly the participants, but there are procedures and rules, an appeals process, and the process allows for a rough form of justice administered by your medical peers. Who better to decide what is fair to pay anyone out of a fixed reimbursement pool?
Unfortunately, there seems to be no institutional memory in this year’s final rule. For example, since it came out, various branches of organized medicine have held urgent meetings at which it was pointed out that a 50% reduction in procedures on the same day as an evaluation and management code is inappropriate, since the overlapping work and practice expense already had been removed for such codes by the relative value update committee. This observation reportedly came as a surprise to the CMS attendees – a most disturbing admission.
There was also discouraging news about the global period survey. Dermatology reported only 3% of the global visits possible.
It turns out that CMS did not look for additional 99024 visits beyond the 10- or 90-day global period in the surveyed states and did not look at practices of fewer than 10 dermatologists, even if they did report. Think about it, how many dermatology groups do you know of 10 or more dermatologists in Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, and Rhode Island? How often do you delay suture removal beyond 10 days? How many times do you see a patient back for a triamcinolone injection or reassurance at no charge more than 10 days after procedures? Talk about a flawed process destined to fail!
The loss of global periods will hurt much, much more than the 50% cut in procedures on the same day as an E/M code. The premalignant and benign destruction codes could be cut by 75% – and good luck in charging for suture removal after surgery. We are talking about another 20% reimbursement cut if implemented.
The American Academy of Dermatology and other dermatology societies are actively involved in responding to the CMS regarding the shortcomings of the proposed rule. Be prepared to be called upon to submit your comments to CMS soon. I am hopeful that much of these misguided proposals can be corrected, but it will take a concerted effort of numerous individual dermatologists, including you.
Finally, I advise you to read the final rule for yourself. And, unlike me, do not forget to keep your emergency wrap handy!
Comments will be taken at www.regulations.gov through Sept. 10, 2018.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected] .
Unlikely mentors
Mentorship is a hot topic. Mentors are generally perceived as knowledgeable, kind, generous souls who will guide mentees through tough challenges and be your pal. I suggest to you that while such encounters are marvelous, and to be sought out, some of the most important lessons are taught by members of the opposite cast.
The presiding secretary of the Ohio state medical board was a brigadier general, still active reserve, tall with a bristling countenance. I was president of the Ohio Dermatological Association and was accompanied by Mark Bechtel, MD, who was our chair of state legislation. We had been invited to , and that there had not been any deaths related to local anesthesia administered by dermatologists in Ohio (or anywhere else). We expected to tell the medical board there was nothing to worry about, and we could all go home. This was 17 years ago.
It quickly became apparent that there had been an extensive prior dialogue between the medical board and representatives of the American College of Surgeons and the American Society of Anesthesiologists. They sat at the head table with the secretary of the medical board.
“In our experience, there are really some dangerous procedures going on in the office setting under local anesthesia, and this area desperately needs regulation,” the anesthesiologist’s representative said. The surgeon’s representative chimed in: “From what I’ve heard, office surgery is a ticking time bomb and needs regulation, and as soon as possible.” This prattle went on and on, with the medical board secretary sympathetically nodding his head. I raised my hand and was ignored – and ignored. It became apparent that this was a show trial, and our opinion was not really wanted, just our attendance noted in the minutes. Finally, I stood up and protested, and pointed out that all of this “testimony” was conjecture and personal opinion, and that there was no factual basis for their claims. The president stiffened, stood up, and started barking orders.He told me to “sit down and not speak unless I was called on.” I sat down and shut up. And I was never called on. Mark Bechtel put a calming hand on my arm. Goodness, I had not been treated like that since junior high.
I soon realized that dermatologists were not at all important to the medical board, and that the medical board had no idea about our safety and efficiency and really did not care.
Following the meeting, I was told by Larry Lanier (the American Academy of Dermatology state legislative liaison at the time) that Ohio was to be the test state to restrict local anesthesia and tumescent anesthesia nationwide. He explained that some widely reported liposuction-related deaths in Florida had given the medical board the “justification” to act. He went on to explain that yes, there were no data either way, but we had better hire a lobbyist and hope for the best.
I was stunned by what I now call (in this case, rough) “mentorship” by the medical board secretary. I understood I could meekly go along – or get angry. I chose the latter, and it has greatly changed my career.
Now, this was not a hot, red, foam-at-the-mouth mad, but a slow burn, the kind that sustains, not consumes.
I went home and did a literature review and was disheartened to find absolutely nothing in the literature on the safety record of dermatologists in the office setting or on the safety of office surgery in general under local anesthesia. We had nothing to back us up.
I looked up the liposuction deaths in Florida and discovered the procedures were all done under general anesthesia or deep sedation by surgeons of one type or another. I also discovered that Florida had enacted mandatory reporting, and the reports could be had for copying costs. I ordered all available, 9 months of data.
We dermatologists passed a special assessment and hired a lobbyist who told us we were too late to have any impact on the impending restrictions. We took a resolution opposing the medical board rules – which would have eliminated using any sedation in the office, even haloperidol and tumescent anesthesia – to the state medical society and got it passed despite the medical board secretary (who was a former president of the society) testifying against us. The Florida data showed no deaths or injuries from using local anesthesia in the office by anyone, and I succeeded in getting a letter addressing that data published expeditiously in the Journal of the American Medical Association (JAMA 2001;285[20]:2582).
The president of the American Society for Dermatologic Surgery at that time, Stephen Mandy, MD, came to town and testified against the proposed restrictions along with about 60 physicians, including dermatologists, plastic surgeons, and other physicians who perform office-based surgery who we had rallied to join us from across the state. So many colleagues joined us, in fact, that some of us had to sit on the floor during the proceedings.
The proposed restrictions evaporated. I and many others have since devoted our research efforts to solidifying dermatology’s safety and quality record. Dr. Bechtel, professor of dermatology at Ohio State University, Columbus, is now secretary of the state medical board. At the last annual state meeting, I thanked the brigadier general, the former secretary of the medical board, for his unlikely mentorship. He smiled and we got our picture taken together.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Mentorship is a hot topic. Mentors are generally perceived as knowledgeable, kind, generous souls who will guide mentees through tough challenges and be your pal. I suggest to you that while such encounters are marvelous, and to be sought out, some of the most important lessons are taught by members of the opposite cast.
The presiding secretary of the Ohio state medical board was a brigadier general, still active reserve, tall with a bristling countenance. I was president of the Ohio Dermatological Association and was accompanied by Mark Bechtel, MD, who was our chair of state legislation. We had been invited to , and that there had not been any deaths related to local anesthesia administered by dermatologists in Ohio (or anywhere else). We expected to tell the medical board there was nothing to worry about, and we could all go home. This was 17 years ago.
It quickly became apparent that there had been an extensive prior dialogue between the medical board and representatives of the American College of Surgeons and the American Society of Anesthesiologists. They sat at the head table with the secretary of the medical board.
“In our experience, there are really some dangerous procedures going on in the office setting under local anesthesia, and this area desperately needs regulation,” the anesthesiologist’s representative said. The surgeon’s representative chimed in: “From what I’ve heard, office surgery is a ticking time bomb and needs regulation, and as soon as possible.” This prattle went on and on, with the medical board secretary sympathetically nodding his head. I raised my hand and was ignored – and ignored. It became apparent that this was a show trial, and our opinion was not really wanted, just our attendance noted in the minutes. Finally, I stood up and protested, and pointed out that all of this “testimony” was conjecture and personal opinion, and that there was no factual basis for their claims. The president stiffened, stood up, and started barking orders.He told me to “sit down and not speak unless I was called on.” I sat down and shut up. And I was never called on. Mark Bechtel put a calming hand on my arm. Goodness, I had not been treated like that since junior high.
I soon realized that dermatologists were not at all important to the medical board, and that the medical board had no idea about our safety and efficiency and really did not care.
Following the meeting, I was told by Larry Lanier (the American Academy of Dermatology state legislative liaison at the time) that Ohio was to be the test state to restrict local anesthesia and tumescent anesthesia nationwide. He explained that some widely reported liposuction-related deaths in Florida had given the medical board the “justification” to act. He went on to explain that yes, there were no data either way, but we had better hire a lobbyist and hope for the best.
I was stunned by what I now call (in this case, rough) “mentorship” by the medical board secretary. I understood I could meekly go along – or get angry. I chose the latter, and it has greatly changed my career.
Now, this was not a hot, red, foam-at-the-mouth mad, but a slow burn, the kind that sustains, not consumes.
I went home and did a literature review and was disheartened to find absolutely nothing in the literature on the safety record of dermatologists in the office setting or on the safety of office surgery in general under local anesthesia. We had nothing to back us up.
I looked up the liposuction deaths in Florida and discovered the procedures were all done under general anesthesia or deep sedation by surgeons of one type or another. I also discovered that Florida had enacted mandatory reporting, and the reports could be had for copying costs. I ordered all available, 9 months of data.
We dermatologists passed a special assessment and hired a lobbyist who told us we were too late to have any impact on the impending restrictions. We took a resolution opposing the medical board rules – which would have eliminated using any sedation in the office, even haloperidol and tumescent anesthesia – to the state medical society and got it passed despite the medical board secretary (who was a former president of the society) testifying against us. The Florida data showed no deaths or injuries from using local anesthesia in the office by anyone, and I succeeded in getting a letter addressing that data published expeditiously in the Journal of the American Medical Association (JAMA 2001;285[20]:2582).
The president of the American Society for Dermatologic Surgery at that time, Stephen Mandy, MD, came to town and testified against the proposed restrictions along with about 60 physicians, including dermatologists, plastic surgeons, and other physicians who perform office-based surgery who we had rallied to join us from across the state. So many colleagues joined us, in fact, that some of us had to sit on the floor during the proceedings.
The proposed restrictions evaporated. I and many others have since devoted our research efforts to solidifying dermatology’s safety and quality record. Dr. Bechtel, professor of dermatology at Ohio State University, Columbus, is now secretary of the state medical board. At the last annual state meeting, I thanked the brigadier general, the former secretary of the medical board, for his unlikely mentorship. He smiled and we got our picture taken together.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Mentorship is a hot topic. Mentors are generally perceived as knowledgeable, kind, generous souls who will guide mentees through tough challenges and be your pal. I suggest to you that while such encounters are marvelous, and to be sought out, some of the most important lessons are taught by members of the opposite cast.
The presiding secretary of the Ohio state medical board was a brigadier general, still active reserve, tall with a bristling countenance. I was president of the Ohio Dermatological Association and was accompanied by Mark Bechtel, MD, who was our chair of state legislation. We had been invited to , and that there had not been any deaths related to local anesthesia administered by dermatologists in Ohio (or anywhere else). We expected to tell the medical board there was nothing to worry about, and we could all go home. This was 17 years ago.
It quickly became apparent that there had been an extensive prior dialogue between the medical board and representatives of the American College of Surgeons and the American Society of Anesthesiologists. They sat at the head table with the secretary of the medical board.
“In our experience, there are really some dangerous procedures going on in the office setting under local anesthesia, and this area desperately needs regulation,” the anesthesiologist’s representative said. The surgeon’s representative chimed in: “From what I’ve heard, office surgery is a ticking time bomb and needs regulation, and as soon as possible.” This prattle went on and on, with the medical board secretary sympathetically nodding his head. I raised my hand and was ignored – and ignored. It became apparent that this was a show trial, and our opinion was not really wanted, just our attendance noted in the minutes. Finally, I stood up and protested, and pointed out that all of this “testimony” was conjecture and personal opinion, and that there was no factual basis for their claims. The president stiffened, stood up, and started barking orders.He told me to “sit down and not speak unless I was called on.” I sat down and shut up. And I was never called on. Mark Bechtel put a calming hand on my arm. Goodness, I had not been treated like that since junior high.
I soon realized that dermatologists were not at all important to the medical board, and that the medical board had no idea about our safety and efficiency and really did not care.
Following the meeting, I was told by Larry Lanier (the American Academy of Dermatology state legislative liaison at the time) that Ohio was to be the test state to restrict local anesthesia and tumescent anesthesia nationwide. He explained that some widely reported liposuction-related deaths in Florida had given the medical board the “justification” to act. He went on to explain that yes, there were no data either way, but we had better hire a lobbyist and hope for the best.
I was stunned by what I now call (in this case, rough) “mentorship” by the medical board secretary. I understood I could meekly go along – or get angry. I chose the latter, and it has greatly changed my career.
Now, this was not a hot, red, foam-at-the-mouth mad, but a slow burn, the kind that sustains, not consumes.
I went home and did a literature review and was disheartened to find absolutely nothing in the literature on the safety record of dermatologists in the office setting or on the safety of office surgery in general under local anesthesia. We had nothing to back us up.
I looked up the liposuction deaths in Florida and discovered the procedures were all done under general anesthesia or deep sedation by surgeons of one type or another. I also discovered that Florida had enacted mandatory reporting, and the reports could be had for copying costs. I ordered all available, 9 months of data.
We dermatologists passed a special assessment and hired a lobbyist who told us we were too late to have any impact on the impending restrictions. We took a resolution opposing the medical board rules – which would have eliminated using any sedation in the office, even haloperidol and tumescent anesthesia – to the state medical society and got it passed despite the medical board secretary (who was a former president of the society) testifying against us. The Florida data showed no deaths or injuries from using local anesthesia in the office by anyone, and I succeeded in getting a letter addressing that data published expeditiously in the Journal of the American Medical Association (JAMA 2001;285[20]:2582).
The president of the American Society for Dermatologic Surgery at that time, Stephen Mandy, MD, came to town and testified against the proposed restrictions along with about 60 physicians, including dermatologists, plastic surgeons, and other physicians who perform office-based surgery who we had rallied to join us from across the state. So many colleagues joined us, in fact, that some of us had to sit on the floor during the proceedings.
The proposed restrictions evaporated. I and many others have since devoted our research efforts to solidifying dermatology’s safety and quality record. Dr. Bechtel, professor of dermatology at Ohio State University, Columbus, is now secretary of the state medical board. At the last annual state meeting, I thanked the brigadier general, the former secretary of the medical board, for his unlikely mentorship. He smiled and we got our picture taken together.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Why contribute to your political action committee?
I got a phone call recently from a friend north of me. “Gosh, did you hear about the State of Ohio Board of Pharmacy ransacking a dermatologist’s office?” he asked. Yes, I had heard about it, and explained that the office compounding rule in Ohio, the reason behind this surprise search and practice, was the subject of an active struggle going on at the state and federal level (see “Beware the state pharmacy board,” Dermatology News, June 3, 2016). I also told him that the pharmacy board swooped into that location because the office had registered for a license to mix drugs (defined by the board as altering a prescription drug by mixing, diluting, or combining), and agreed to unannounced inspections – and that while the dermatologist was not fined, there was a list of compliance issues to be met, including recording the lot number of all samples, keeping separate paper records of each time he mixed medications, and the promise of a return visit soon.
I went on to explain that representatives – past presidents and board members – of the Ohio Dermatological Association (accompanied by Lisa Albany, director of state policy at the American Academy of Dermatology’s Washington office) had met with the state pharmacy board and explained how ridiculous these regulations were. It was a frustrating meeting.
This was obviously unacceptable, and we went on to meet with state legislators, then federal legislators, and even the Food and Drug Administration. The Ohio Dermatological Association, the American Society for Dermatologic Surgery, the American College of Mohs Surgery, and the AAD all went to Washington, DC, and to the FDA last fall. The Ohio State Medical Association and the American Medical Association lined up in opposition to the rules. The state pharmacy board withdrew its rules and reopened the comment period. We are still waiting to hear back and have encouraged the pharmacy board to wait for FDA and USP (United States Pharmacopeia) guidance.
So, what has this got to do with SkinPAC, our dermatology political action committee?
When our groups went to Washington to talk to our representatives and senators, we had access to all the movers and shakers who could act on this issue because of the AAD Association’s contacts though SkinPAC.
The point I want to make is that . There are many issues directly affecting dermatology, not only compounding, but loss of global periods (see “Time for dermatologists in nine states to start submitting CPT Code 99024,” Dermatology News, July 18, 2017), MACRA reform, MACRA relief, and legislative relief for medication pricing.
So, I told my northern friend who called to attend the AAD’s legislative conference in Washington (July 15-17), regularly contribute to SkinPAC, and get five of his colleagues to sign up too. This is a solid investment of your time and money. Not participating will make it more likely that you will soon need a pharmacy license (in addition to your medical license), may have to start charging patients to remove their sutures, be forced into larger groups to demonstrate quality, and continue to have to explain why a once-cheap generic drug now costs thousands of dollars. Seems like a good investment to me.
Dr. Coldiron is vice chair of the dermatology political action committee (SkinPAC). He is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I got a phone call recently from a friend north of me. “Gosh, did you hear about the State of Ohio Board of Pharmacy ransacking a dermatologist’s office?” he asked. Yes, I had heard about it, and explained that the office compounding rule in Ohio, the reason behind this surprise search and practice, was the subject of an active struggle going on at the state and federal level (see “Beware the state pharmacy board,” Dermatology News, June 3, 2016). I also told him that the pharmacy board swooped into that location because the office had registered for a license to mix drugs (defined by the board as altering a prescription drug by mixing, diluting, or combining), and agreed to unannounced inspections – and that while the dermatologist was not fined, there was a list of compliance issues to be met, including recording the lot number of all samples, keeping separate paper records of each time he mixed medications, and the promise of a return visit soon.
I went on to explain that representatives – past presidents and board members – of the Ohio Dermatological Association (accompanied by Lisa Albany, director of state policy at the American Academy of Dermatology’s Washington office) had met with the state pharmacy board and explained how ridiculous these regulations were. It was a frustrating meeting.
This was obviously unacceptable, and we went on to meet with state legislators, then federal legislators, and even the Food and Drug Administration. The Ohio Dermatological Association, the American Society for Dermatologic Surgery, the American College of Mohs Surgery, and the AAD all went to Washington, DC, and to the FDA last fall. The Ohio State Medical Association and the American Medical Association lined up in opposition to the rules. The state pharmacy board withdrew its rules and reopened the comment period. We are still waiting to hear back and have encouraged the pharmacy board to wait for FDA and USP (United States Pharmacopeia) guidance.
So, what has this got to do with SkinPAC, our dermatology political action committee?
When our groups went to Washington to talk to our representatives and senators, we had access to all the movers and shakers who could act on this issue because of the AAD Association’s contacts though SkinPAC.
The point I want to make is that . There are many issues directly affecting dermatology, not only compounding, but loss of global periods (see “Time for dermatologists in nine states to start submitting CPT Code 99024,” Dermatology News, July 18, 2017), MACRA reform, MACRA relief, and legislative relief for medication pricing.
So, I told my northern friend who called to attend the AAD’s legislative conference in Washington (July 15-17), regularly contribute to SkinPAC, and get five of his colleagues to sign up too. This is a solid investment of your time and money. Not participating will make it more likely that you will soon need a pharmacy license (in addition to your medical license), may have to start charging patients to remove their sutures, be forced into larger groups to demonstrate quality, and continue to have to explain why a once-cheap generic drug now costs thousands of dollars. Seems like a good investment to me.
Dr. Coldiron is vice chair of the dermatology political action committee (SkinPAC). He is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I got a phone call recently from a friend north of me. “Gosh, did you hear about the State of Ohio Board of Pharmacy ransacking a dermatologist’s office?” he asked. Yes, I had heard about it, and explained that the office compounding rule in Ohio, the reason behind this surprise search and practice, was the subject of an active struggle going on at the state and federal level (see “Beware the state pharmacy board,” Dermatology News, June 3, 2016). I also told him that the pharmacy board swooped into that location because the office had registered for a license to mix drugs (defined by the board as altering a prescription drug by mixing, diluting, or combining), and agreed to unannounced inspections – and that while the dermatologist was not fined, there was a list of compliance issues to be met, including recording the lot number of all samples, keeping separate paper records of each time he mixed medications, and the promise of a return visit soon.
I went on to explain that representatives – past presidents and board members – of the Ohio Dermatological Association (accompanied by Lisa Albany, director of state policy at the American Academy of Dermatology’s Washington office) had met with the state pharmacy board and explained how ridiculous these regulations were. It was a frustrating meeting.
This was obviously unacceptable, and we went on to meet with state legislators, then federal legislators, and even the Food and Drug Administration. The Ohio Dermatological Association, the American Society for Dermatologic Surgery, the American College of Mohs Surgery, and the AAD all went to Washington, DC, and to the FDA last fall. The Ohio State Medical Association and the American Medical Association lined up in opposition to the rules. The state pharmacy board withdrew its rules and reopened the comment period. We are still waiting to hear back and have encouraged the pharmacy board to wait for FDA and USP (United States Pharmacopeia) guidance.
So, what has this got to do with SkinPAC, our dermatology political action committee?
When our groups went to Washington to talk to our representatives and senators, we had access to all the movers and shakers who could act on this issue because of the AAD Association’s contacts though SkinPAC.
The point I want to make is that . There are many issues directly affecting dermatology, not only compounding, but loss of global periods (see “Time for dermatologists in nine states to start submitting CPT Code 99024,” Dermatology News, July 18, 2017), MACRA reform, MACRA relief, and legislative relief for medication pricing.
So, I told my northern friend who called to attend the AAD’s legislative conference in Washington (July 15-17), regularly contribute to SkinPAC, and get five of his colleagues to sign up too. This is a solid investment of your time and money. Not participating will make it more likely that you will soon need a pharmacy license (in addition to your medical license), may have to start charging patients to remove their sutures, be forced into larger groups to demonstrate quality, and continue to have to explain why a once-cheap generic drug now costs thousands of dollars. Seems like a good investment to me.
Dr. Coldiron is vice chair of the dermatology political action committee (SkinPAC). He is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Melanoma in situ: It’s hard to know what you don’t know
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.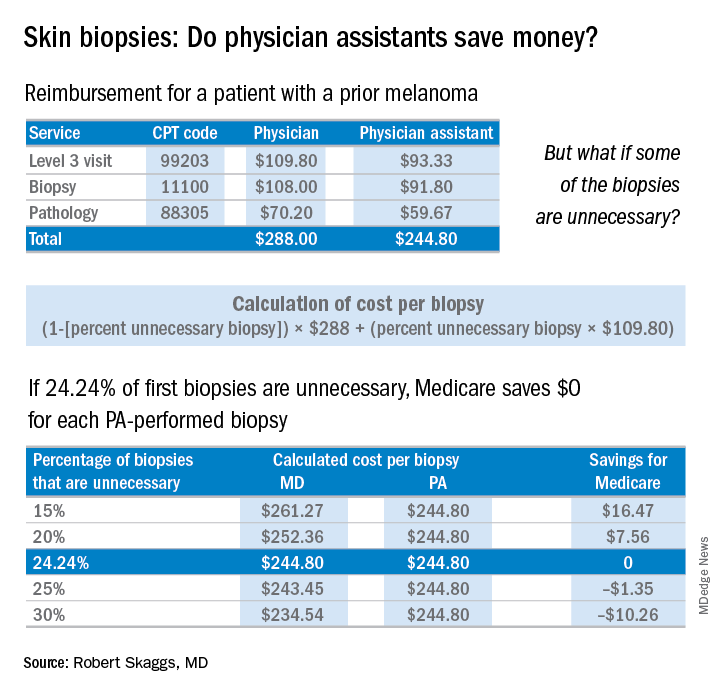
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.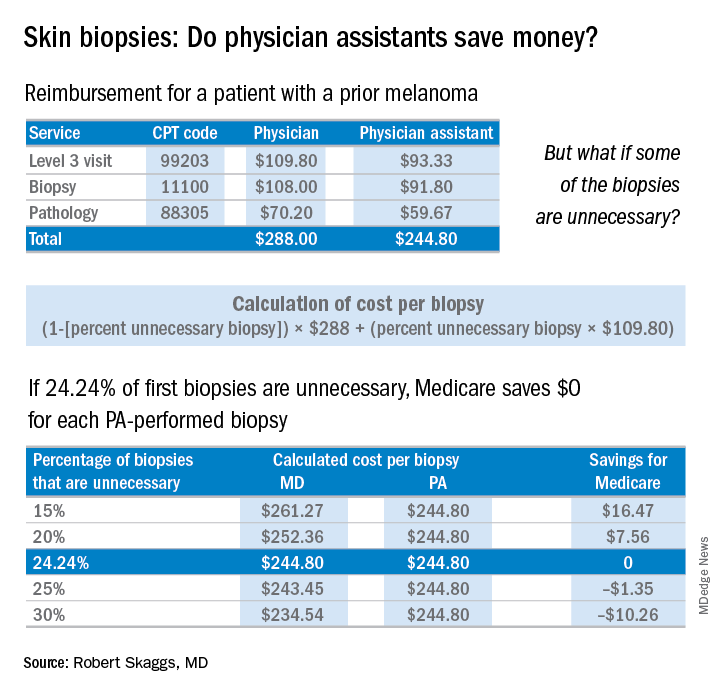
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.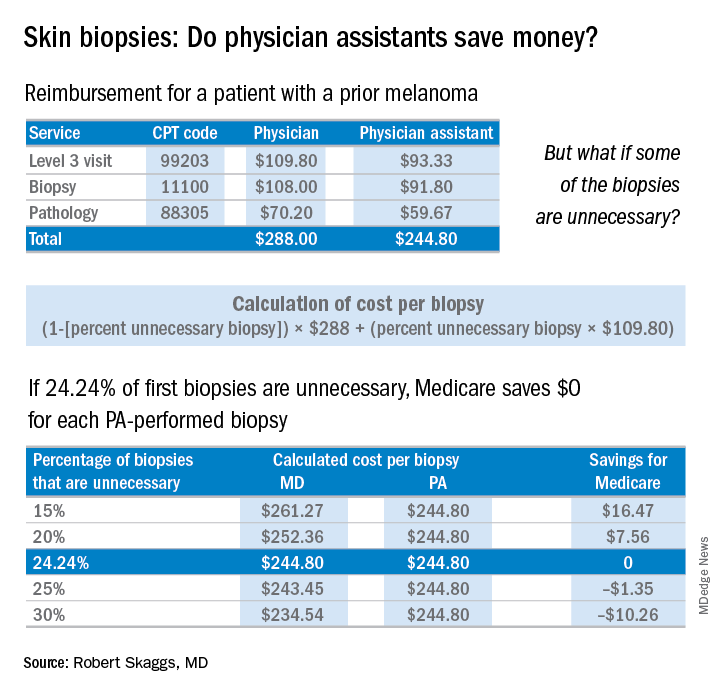
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Tanning is the new tobacco
I was driving to work the other day, perched up in my pickup truck (somehow you knew that) and noticed a fancy race car in front of me with a vanity tag. It read HRTATTK 4. Well, I thought after four heart attacks maybe I would splurge on a special car too (more likely a newer truck). Then I noticed smoke coming out of the driver’s window, and I could see this guy in his side view mirror, presumably Mr. “Heart Attack 4,” puffing away on a cigarette. Wow.
Then I got to work and saw my secretary, who works with her oxygen on, out back puffing a cigarette. Wow.
It turns out that cigarette smoke contains substances that act as a monoamine oxidase (MAO) A inhibitor, prolonging the dopamine high in the brain (Proc Natl Acad Sci U S A. 1996 Nov 26;93[24]:14065-9). Makes sense and may explain the above smoking behavior. I truly believe cigarettes are as or more addictive than any other dopamine enhancing drug.
More than 50 years ago, a national campaign against smoking was launched after the 1964 Surgeon General’s report concluded that smoking was a major health hazard. (Looking back, one of the few losses of not having to pull journal articles from the stacks in the library, is that medical students and residents can’t shake their heads in wonder at the cigarette ads in old medical journals.) The impact of the national antismoking campaign has been dramatic, but smoking remains the leading preventable cause of death in the United States and globally, according to the Centers for Disease Control and Prevention.
in 2006, from 1992 (Arch Dermatol. 2010;146[3]:283-7), dermatologists had good footing on which to start a major prevention campaign. The American Cancer Society got on board, and in 2014, acting surgeon general Boris Lushniak, MD, issued a call to action to prevent skin cancer along with Howard Koh, MD, the assistant secretary of health, in “The Surgeon General’s Call to Action to Prevent Skin Cancer” in 2014, and the campaign was on.
Well, I am delighted to pass on a report from Leonard Lichtenfeld, MD, deputy chief medical officer for the American Cancer Society, who recently described in his March 2018 blog what may the first signs of the effectiveness of efforts to promote protection from ultraviolet ray exposure (JAMA Dermatol. 2018;154[3]:361-2). He writes: “In young white women ages 15 to 24, the incidence of melanoma has declined an average of 5.5% per year from January 2005 through December 2014. Not 5.5% over those ten years but 5.5 % PER YEAR. That’s remarkable, to say the least.”
As for the reasons behind these trends, he says, “no one can say for certain,” but he refers to national data indicating that indoor tanning has decreased in the past few years, especially among adolescents and young adults.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was driving to work the other day, perched up in my pickup truck (somehow you knew that) and noticed a fancy race car in front of me with a vanity tag. It read HRTATTK 4. Well, I thought after four heart attacks maybe I would splurge on a special car too (more likely a newer truck). Then I noticed smoke coming out of the driver’s window, and I could see this guy in his side view mirror, presumably Mr. “Heart Attack 4,” puffing away on a cigarette. Wow.
Then I got to work and saw my secretary, who works with her oxygen on, out back puffing a cigarette. Wow.
It turns out that cigarette smoke contains substances that act as a monoamine oxidase (MAO) A inhibitor, prolonging the dopamine high in the brain (Proc Natl Acad Sci U S A. 1996 Nov 26;93[24]:14065-9). Makes sense and may explain the above smoking behavior. I truly believe cigarettes are as or more addictive than any other dopamine enhancing drug.
More than 50 years ago, a national campaign against smoking was launched after the 1964 Surgeon General’s report concluded that smoking was a major health hazard. (Looking back, one of the few losses of not having to pull journal articles from the stacks in the library, is that medical students and residents can’t shake their heads in wonder at the cigarette ads in old medical journals.) The impact of the national antismoking campaign has been dramatic, but smoking remains the leading preventable cause of death in the United States and globally, according to the Centers for Disease Control and Prevention.
in 2006, from 1992 (Arch Dermatol. 2010;146[3]:283-7), dermatologists had good footing on which to start a major prevention campaign. The American Cancer Society got on board, and in 2014, acting surgeon general Boris Lushniak, MD, issued a call to action to prevent skin cancer along with Howard Koh, MD, the assistant secretary of health, in “The Surgeon General’s Call to Action to Prevent Skin Cancer” in 2014, and the campaign was on.
Well, I am delighted to pass on a report from Leonard Lichtenfeld, MD, deputy chief medical officer for the American Cancer Society, who recently described in his March 2018 blog what may the first signs of the effectiveness of efforts to promote protection from ultraviolet ray exposure (JAMA Dermatol. 2018;154[3]:361-2). He writes: “In young white women ages 15 to 24, the incidence of melanoma has declined an average of 5.5% per year from January 2005 through December 2014. Not 5.5% over those ten years but 5.5 % PER YEAR. That’s remarkable, to say the least.”
As for the reasons behind these trends, he says, “no one can say for certain,” but he refers to national data indicating that indoor tanning has decreased in the past few years, especially among adolescents and young adults.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was driving to work the other day, perched up in my pickup truck (somehow you knew that) and noticed a fancy race car in front of me with a vanity tag. It read HRTATTK 4. Well, I thought after four heart attacks maybe I would splurge on a special car too (more likely a newer truck). Then I noticed smoke coming out of the driver’s window, and I could see this guy in his side view mirror, presumably Mr. “Heart Attack 4,” puffing away on a cigarette. Wow.
Then I got to work and saw my secretary, who works with her oxygen on, out back puffing a cigarette. Wow.
It turns out that cigarette smoke contains substances that act as a monoamine oxidase (MAO) A inhibitor, prolonging the dopamine high in the brain (Proc Natl Acad Sci U S A. 1996 Nov 26;93[24]:14065-9). Makes sense and may explain the above smoking behavior. I truly believe cigarettes are as or more addictive than any other dopamine enhancing drug.
More than 50 years ago, a national campaign against smoking was launched after the 1964 Surgeon General’s report concluded that smoking was a major health hazard. (Looking back, one of the few losses of not having to pull journal articles from the stacks in the library, is that medical students and residents can’t shake their heads in wonder at the cigarette ads in old medical journals.) The impact of the national antismoking campaign has been dramatic, but smoking remains the leading preventable cause of death in the United States and globally, according to the Centers for Disease Control and Prevention.
in 2006, from 1992 (Arch Dermatol. 2010;146[3]:283-7), dermatologists had good footing on which to start a major prevention campaign. The American Cancer Society got on board, and in 2014, acting surgeon general Boris Lushniak, MD, issued a call to action to prevent skin cancer along with Howard Koh, MD, the assistant secretary of health, in “The Surgeon General’s Call to Action to Prevent Skin Cancer” in 2014, and the campaign was on.
Well, I am delighted to pass on a report from Leonard Lichtenfeld, MD, deputy chief medical officer for the American Cancer Society, who recently described in his March 2018 blog what may the first signs of the effectiveness of efforts to promote protection from ultraviolet ray exposure (JAMA Dermatol. 2018;154[3]:361-2). He writes: “In young white women ages 15 to 24, the incidence of melanoma has declined an average of 5.5% per year from January 2005 through December 2014. Not 5.5% over those ten years but 5.5 % PER YEAR. That’s remarkable, to say the least.”
As for the reasons behind these trends, he says, “no one can say for certain,” but he refers to national data indicating that indoor tanning has decreased in the past few years, especially among adolescents and young adults.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The Rest of the Story: Anthem rescinds modifier 25 reductions
When I was a kid, there used to be a radio show by Paul Harvey called “The Rest of the Story.” I loved this show because there was always a big back story behind the happy ending. And that’s how I feel now, it is indeed a happy day, and glad we should be, because the modifier 25 reductions have been rescinded by Anthem. But there is much more to the story, so here is the back story.
The OIG report kicked several things into motion. Insurers started auditing physicians for using modifier 25. The American Academy of Dermatology (AAD) rapidly educated membership on documentation requirements for billing modifier 25. That is, in many cases, separate evaluation and management services should be billed on the same day as a minor procedure, but the chart wasn’t showing the needed details. In an audit, if it is not in the chart, it wasn’t done.
The American Medical Association’s RVS Update Committee (RUC) took note of the OIG report and started to reduce overlapping time and payments on codes being reviewed, which were performed more than 50% of the time on the same day as an evaluation and management code.
The situation was stable for a number of years. Insurers would audit and reclaim some funds and physicians would try and document more. Then, one of the few good things about an electronic medical record became apparent. The documentation became overwhelming. You want to audit me? Here, you can have a BIG “chaw” of records in a PDF. No hassle for staff, just click a few buttons, and no lost records, which mean an automatic loss for doctors. No more settlements by doctors because it just wasn’t worth the time.
In 2012, Harvard Pilgrim HealthCare in Boston started routinely reducing the evaluation and management payment by 50% when filed with modifier 25. No audit, no review, just whack! The Massachusetts Academy of Dermatology vigorously opposed this, as did the AAD. In 2014, Tufts Health Plan followed suit, followed by Blue Cross & Blue Shield of Rhode Island in 2016. Then, in 2017, Anthem started rolling this policy out across the United States. Dermatologists felt like we were howling alone in the wilderness.
The AAD has a committee that deserves special mention here. The Patient Access and Payer Relations (PAPR) Committee, chaired by Howard Rogers, MD, was established to develop relationships with insurers so problems like this could be corrected expeditiously. Dr. Howard and the committee worked tirelessly on the modifier 25 problem. They pointed out that the RUC already had taken value out of the minor procedure codes to account for any overlap. State dermatology, state medical, and specialty societies all were alerted and protested. The PAPR committee had numerous calls with insurers, and Dr. Howard traveled all over the country to meet with Anthem representatives.
Perhaps what Anthem didn’t realize was that, in 2015, two new CPT codes for advanced care planning by primary care physicians (think written advanced directives) were approved for payment by Medicare in 2016, in addition to the regular visit, with a modifier 25 – as well they should have been. That 50% reduction would affect primary care as well.
The howling took on a new timbre.
Last year, the AAD-AMA delegation, led by Cyndi Yag-Howard, MD, took the lead on getting the AMA to adopt a tough stance on modifier 25 reductions. The AMA backed our position, and AMA trustee and chair elect of the AMA Board of Trustees, dermatologist Jack Resneck Jr., MD – with the help of dermatology RUC team lead Scott Collins, MD – outlined in succinct detail, proof that reductions by insurers were inappropriate. The AMA president and chair of the board of trustees took special interest in this issue, and Dr. Resneck personally assured the dermatology delegation that this was at the top of their priority list.
This, my colleagues, is why it is so important for you to join and support your academy, your state dermatology, state medical, and national medical societies. A lifetime of membership fees has just been credited to you.
Anthem then took the 50% reduction down to 25%. Not good enough, so PAPR agreed to call in the cavalry. A consultant who knows all the large employers who buy insurance from Anthem was contacted. Phone calls were made, the tipping point was reached, and Anthem finally rescinded its policy, announcing in late February that the company had decided not to proceed with the policy.
And that, my friends, is the rest of the story.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
When I was a kid, there used to be a radio show by Paul Harvey called “The Rest of the Story.” I loved this show because there was always a big back story behind the happy ending. And that’s how I feel now, it is indeed a happy day, and glad we should be, because the modifier 25 reductions have been rescinded by Anthem. But there is much more to the story, so here is the back story.
The OIG report kicked several things into motion. Insurers started auditing physicians for using modifier 25. The American Academy of Dermatology (AAD) rapidly educated membership on documentation requirements for billing modifier 25. That is, in many cases, separate evaluation and management services should be billed on the same day as a minor procedure, but the chart wasn’t showing the needed details. In an audit, if it is not in the chart, it wasn’t done.
The American Medical Association’s RVS Update Committee (RUC) took note of the OIG report and started to reduce overlapping time and payments on codes being reviewed, which were performed more than 50% of the time on the same day as an evaluation and management code.
The situation was stable for a number of years. Insurers would audit and reclaim some funds and physicians would try and document more. Then, one of the few good things about an electronic medical record became apparent. The documentation became overwhelming. You want to audit me? Here, you can have a BIG “chaw” of records in a PDF. No hassle for staff, just click a few buttons, and no lost records, which mean an automatic loss for doctors. No more settlements by doctors because it just wasn’t worth the time.
In 2012, Harvard Pilgrim HealthCare in Boston started routinely reducing the evaluation and management payment by 50% when filed with modifier 25. No audit, no review, just whack! The Massachusetts Academy of Dermatology vigorously opposed this, as did the AAD. In 2014, Tufts Health Plan followed suit, followed by Blue Cross & Blue Shield of Rhode Island in 2016. Then, in 2017, Anthem started rolling this policy out across the United States. Dermatologists felt like we were howling alone in the wilderness.
The AAD has a committee that deserves special mention here. The Patient Access and Payer Relations (PAPR) Committee, chaired by Howard Rogers, MD, was established to develop relationships with insurers so problems like this could be corrected expeditiously. Dr. Howard and the committee worked tirelessly on the modifier 25 problem. They pointed out that the RUC already had taken value out of the minor procedure codes to account for any overlap. State dermatology, state medical, and specialty societies all were alerted and protested. The PAPR committee had numerous calls with insurers, and Dr. Howard traveled all over the country to meet with Anthem representatives.
Perhaps what Anthem didn’t realize was that, in 2015, two new CPT codes for advanced care planning by primary care physicians (think written advanced directives) were approved for payment by Medicare in 2016, in addition to the regular visit, with a modifier 25 – as well they should have been. That 50% reduction would affect primary care as well.
The howling took on a new timbre.
Last year, the AAD-AMA delegation, led by Cyndi Yag-Howard, MD, took the lead on getting the AMA to adopt a tough stance on modifier 25 reductions. The AMA backed our position, and AMA trustee and chair elect of the AMA Board of Trustees, dermatologist Jack Resneck Jr., MD – with the help of dermatology RUC team lead Scott Collins, MD – outlined in succinct detail, proof that reductions by insurers were inappropriate. The AMA president and chair of the board of trustees took special interest in this issue, and Dr. Resneck personally assured the dermatology delegation that this was at the top of their priority list.
This, my colleagues, is why it is so important for you to join and support your academy, your state dermatology, state medical, and national medical societies. A lifetime of membership fees has just been credited to you.
Anthem then took the 50% reduction down to 25%. Not good enough, so PAPR agreed to call in the cavalry. A consultant who knows all the large employers who buy insurance from Anthem was contacted. Phone calls were made, the tipping point was reached, and Anthem finally rescinded its policy, announcing in late February that the company had decided not to proceed with the policy.
And that, my friends, is the rest of the story.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
When I was a kid, there used to be a radio show by Paul Harvey called “The Rest of the Story.” I loved this show because there was always a big back story behind the happy ending. And that’s how I feel now, it is indeed a happy day, and glad we should be, because the modifier 25 reductions have been rescinded by Anthem. But there is much more to the story, so here is the back story.
The OIG report kicked several things into motion. Insurers started auditing physicians for using modifier 25. The American Academy of Dermatology (AAD) rapidly educated membership on documentation requirements for billing modifier 25. That is, in many cases, separate evaluation and management services should be billed on the same day as a minor procedure, but the chart wasn’t showing the needed details. In an audit, if it is not in the chart, it wasn’t done.
The American Medical Association’s RVS Update Committee (RUC) took note of the OIG report and started to reduce overlapping time and payments on codes being reviewed, which were performed more than 50% of the time on the same day as an evaluation and management code.
The situation was stable for a number of years. Insurers would audit and reclaim some funds and physicians would try and document more. Then, one of the few good things about an electronic medical record became apparent. The documentation became overwhelming. You want to audit me? Here, you can have a BIG “chaw” of records in a PDF. No hassle for staff, just click a few buttons, and no lost records, which mean an automatic loss for doctors. No more settlements by doctors because it just wasn’t worth the time.
In 2012, Harvard Pilgrim HealthCare in Boston started routinely reducing the evaluation and management payment by 50% when filed with modifier 25. No audit, no review, just whack! The Massachusetts Academy of Dermatology vigorously opposed this, as did the AAD. In 2014, Tufts Health Plan followed suit, followed by Blue Cross & Blue Shield of Rhode Island in 2016. Then, in 2017, Anthem started rolling this policy out across the United States. Dermatologists felt like we were howling alone in the wilderness.
The AAD has a committee that deserves special mention here. The Patient Access and Payer Relations (PAPR) Committee, chaired by Howard Rogers, MD, was established to develop relationships with insurers so problems like this could be corrected expeditiously. Dr. Howard and the committee worked tirelessly on the modifier 25 problem. They pointed out that the RUC already had taken value out of the minor procedure codes to account for any overlap. State dermatology, state medical, and specialty societies all were alerted and protested. The PAPR committee had numerous calls with insurers, and Dr. Howard traveled all over the country to meet with Anthem representatives.
Perhaps what Anthem didn’t realize was that, in 2015, two new CPT codes for advanced care planning by primary care physicians (think written advanced directives) were approved for payment by Medicare in 2016, in addition to the regular visit, with a modifier 25 – as well they should have been. That 50% reduction would affect primary care as well.
The howling took on a new timbre.
Last year, the AAD-AMA delegation, led by Cyndi Yag-Howard, MD, took the lead on getting the AMA to adopt a tough stance on modifier 25 reductions. The AMA backed our position, and AMA trustee and chair elect of the AMA Board of Trustees, dermatologist Jack Resneck Jr., MD – with the help of dermatology RUC team lead Scott Collins, MD – outlined in succinct detail, proof that reductions by insurers were inappropriate. The AMA president and chair of the board of trustees took special interest in this issue, and Dr. Resneck personally assured the dermatology delegation that this was at the top of their priority list.
This, my colleagues, is why it is so important for you to join and support your academy, your state dermatology, state medical, and national medical societies. A lifetime of membership fees has just been credited to you.
Anthem then took the 50% reduction down to 25%. Not good enough, so PAPR agreed to call in the cavalry. A consultant who knows all the large employers who buy insurance from Anthem was contacted. Phone calls were made, the tipping point was reached, and Anthem finally rescinded its policy, announcing in late February that the company had decided not to proceed with the policy.
And that, my friends, is the rest of the story.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
It takes a missile to focus your mind
I was one of about 600 dermatologists sitting in a lecture hall during a meeting in Maui when our muted smartphones suddenly started howling in unison. A text message popped up stating, “BALLISTIC MISSILE THREAT INBOUND TO HAWAII. SEEK IMMEDIATE SHELTER. THIS IS NOT A DRILL.” We all assumed a nuclear weapon from North Korea was headed our way.
The lecture was interrupted. The confused and concerned attendees milled around. The immediate response was largely “this can’t be real.” Meanwhile, the text alarm went off again transmitting the same message. The hotel intercom repeated the message and warned us to get inside the ballroom.
Among the attendees was David Cohen, trained in disaster preparedness. He ran up to his room, filled his bathtub, and put his mattress against the glass window. Richard Winkelman went down to the beach where he could at least witness what was about to annihilate him. Dirk Elston speculated the missile’s target was Kauai, where nuclear weapons are siloed. My wife was confident that the missiles would be intercepted, similar to the way they are under the Israeli missile defense system, and shot down before they hit any target.
And so, we mostly waited. The 30 minutes of largely silent confusion gave me a unique opportunity for self-reflection. I realized that many of my issues are petty and that I am insignificant in the scheme of things. I have never felt so helpless in my life. My mind entered a sort of fugue state, and I looked back on my life and realized it had been a darn good ride. I thought about my teenage children. I realized I had many, many things to be grateful for. I felt a huge burden lift off my shoulders and felt like I was floating about an inch above the floor. As I stared into nothingness, I internally reprioritized objectives. I was ready to die.
Then, just as suddenly and unpredictably as it arrived, the alert was called off. The imminent attack was no more than the mistaken push of a button.
But the event remains a defining moment for me. All the small battles that make up a life and career will continue, but I can no longer take them as seriously, and I will now take more time to reflect. I think I will get closer to God. I will try to be a better man, a better father, and a better citizen. It changed me, I think for the better.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was one of about 600 dermatologists sitting in a lecture hall during a meeting in Maui when our muted smartphones suddenly started howling in unison. A text message popped up stating, “BALLISTIC MISSILE THREAT INBOUND TO HAWAII. SEEK IMMEDIATE SHELTER. THIS IS NOT A DRILL.” We all assumed a nuclear weapon from North Korea was headed our way.
The lecture was interrupted. The confused and concerned attendees milled around. The immediate response was largely “this can’t be real.” Meanwhile, the text alarm went off again transmitting the same message. The hotel intercom repeated the message and warned us to get inside the ballroom.
Among the attendees was David Cohen, trained in disaster preparedness. He ran up to his room, filled his bathtub, and put his mattress against the glass window. Richard Winkelman went down to the beach where he could at least witness what was about to annihilate him. Dirk Elston speculated the missile’s target was Kauai, where nuclear weapons are siloed. My wife was confident that the missiles would be intercepted, similar to the way they are under the Israeli missile defense system, and shot down before they hit any target.
And so, we mostly waited. The 30 minutes of largely silent confusion gave me a unique opportunity for self-reflection. I realized that many of my issues are petty and that I am insignificant in the scheme of things. I have never felt so helpless in my life. My mind entered a sort of fugue state, and I looked back on my life and realized it had been a darn good ride. I thought about my teenage children. I realized I had many, many things to be grateful for. I felt a huge burden lift off my shoulders and felt like I was floating about an inch above the floor. As I stared into nothingness, I internally reprioritized objectives. I was ready to die.
Then, just as suddenly and unpredictably as it arrived, the alert was called off. The imminent attack was no more than the mistaken push of a button.
But the event remains a defining moment for me. All the small battles that make up a life and career will continue, but I can no longer take them as seriously, and I will now take more time to reflect. I think I will get closer to God. I will try to be a better man, a better father, and a better citizen. It changed me, I think for the better.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was one of about 600 dermatologists sitting in a lecture hall during a meeting in Maui when our muted smartphones suddenly started howling in unison. A text message popped up stating, “BALLISTIC MISSILE THREAT INBOUND TO HAWAII. SEEK IMMEDIATE SHELTER. THIS IS NOT A DRILL.” We all assumed a nuclear weapon from North Korea was headed our way.
The lecture was interrupted. The confused and concerned attendees milled around. The immediate response was largely “this can’t be real.” Meanwhile, the text alarm went off again transmitting the same message. The hotel intercom repeated the message and warned us to get inside the ballroom.
Among the attendees was David Cohen, trained in disaster preparedness. He ran up to his room, filled his bathtub, and put his mattress against the glass window. Richard Winkelman went down to the beach where he could at least witness what was about to annihilate him. Dirk Elston speculated the missile’s target was Kauai, where nuclear weapons are siloed. My wife was confident that the missiles would be intercepted, similar to the way they are under the Israeli missile defense system, and shot down before they hit any target.
And so, we mostly waited. The 30 minutes of largely silent confusion gave me a unique opportunity for self-reflection. I realized that many of my issues are petty and that I am insignificant in the scheme of things. I have never felt so helpless in my life. My mind entered a sort of fugue state, and I looked back on my life and realized it had been a darn good ride. I thought about my teenage children. I realized I had many, many things to be grateful for. I felt a huge burden lift off my shoulders and felt like I was floating about an inch above the floor. As I stared into nothingness, I internally reprioritized objectives. I was ready to die.
Then, just as suddenly and unpredictably as it arrived, the alert was called off. The imminent attack was no more than the mistaken push of a button.
But the event remains a defining moment for me. All the small battles that make up a life and career will continue, but I can no longer take them as seriously, and I will now take more time to reflect. I think I will get closer to God. I will try to be a better man, a better father, and a better citizen. It changed me, I think for the better.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Sentinel node biopsy: Who needs it?
More than 17 years ago, I published an article that was largely ignored, predicating that patient benefit from the sentinel node biopsy procedure was unlikely.
I asserted that the lymph nodes are not a reliable filter for melanoma cells, lymphatic drainage is capricious, and many individuals (especially younger ones) have benign neval rests in their lymph nodes that cannot be distinguished from melanoma deposits, since they are both positive for the S100 protein (Int J Dermatol. 2000 Nov;39[11]:807-11). In addition, multiple uncontrolled studies had shown that locating sentinel nodes, followed by a complete lymph node dissection, had no survival benefit. At the time, I argued that sentinel node biopsy should be performed only if the patient was going to be enrolled in a clinical study.
Many surgical oncologists have built their careers around the flawed premise that removing the draining nodes would cure melanoma. It doesn’t. It is past time to admit it and move on.
So, if completion node dissection does not save lives, why do a sentinel node biopsy? I recently asked a dermatologist friend, who is a committed acolyte of the sentinel node biopsy school, why he continues to recommend sentinel node biopsy if there is no benefit from complete node dissection. His quick response was that patients want to know if they are at higher risk of metastatic disease so that they can be followed closely with high-resolution ultrasound at a major cancer center and can be eligible for clinical trials. His reply gave me pause, so I asked why completion node dissection was still being recommended. I was told that some patients with positive sentinel nodes lived far away, and if they would not make regular follow-up visits for high-resolution ultrasound, the surgical oncologists do completion node dissection to ensure “local nodal control.” Yipes! You’re going to rip my groin out because I like quiet county living?
I doubt that patients would be enthusiastic if told beforehand that sentinel node biopsies costs $14,000-$18,000, and has a 9% complication rate, and one-third of those patients who have complications end up with permanent lymphedema. I wondered if the patients were told they could have a genetic test done on their already excised melanoma tissue that would tell them if they were in a high-risk group without having an additional invasive surgical procedure. I wondered if they were told that 10%-30% of people with negative sentinel nodes go on to develop metastatic disease. I also wondered if they had been told they would have to walk around with their melanoma, which could spread at any time, for several additional weeks, while waiting for the results of their sentinel node biopsy, instead of having the melanoma immediately removed by their dermatologist. I also wondered if they had been told that high-resolution ultrasound has not definitively been shown to be superior to clinical palpation of the lymph nodes.
I looked into the possibility of clinical trials for patients with positive sentinel nodes, as well. Based on my search of clinical trials.gov in January, there are 33 trials in the United States studying patients with stage 3 (positive sentinel node) or greater disease. If I had a positive sentinel node, I would look for a study in which I had a chance of getting nivolumab, which recently has been shown to be superior to ipilimumab in the phase 3 Checkmate 238 trial published in 2017 (N Engl J Med 2017 Nov 9; 377:1824-35).
But I am getting ahead of myself.
As a thinking man, if I had a thick melanoma (that was less than 2 mm), I would opt for a genetic test of my already excised melanoma tissue. If the results of that genetic test (which has near identical sensitivity and specificity for developing metastatic disease as a sentinel node) put me in the low-risk group, I would pass on the sentinel node biopsy. This would eliminate a lot of unnecessary surgery. If I fell into the high-risk group, I would consider a sentinel node biopsy so I could get into a study, or determine if I needed to find a way to get my insurance to pay, or if I could personally afford nivolumab. Even if I opted not to take the drug, because of the potential risk of high-grade side effects, the high-risk genetic profile tells me I would still need more frequent follow-up.
These are exciting times. I am looking forward to clinical trials that allow a patient with a high-risk genetic profile to go directly into a trial. We are moving into the realm of individualized genomic medicine in which metastatic melanoma truly becomes a curable disease.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Coldiron has no financial or other conflicts of interest with Castle Biosciences, the manufacturer of the DecisionDx-Melanoma genetic expression profile test. Email him at [email protected].
More than 17 years ago, I published an article that was largely ignored, predicating that patient benefit from the sentinel node biopsy procedure was unlikely.
I asserted that the lymph nodes are not a reliable filter for melanoma cells, lymphatic drainage is capricious, and many individuals (especially younger ones) have benign neval rests in their lymph nodes that cannot be distinguished from melanoma deposits, since they are both positive for the S100 protein (Int J Dermatol. 2000 Nov;39[11]:807-11). In addition, multiple uncontrolled studies had shown that locating sentinel nodes, followed by a complete lymph node dissection, had no survival benefit. At the time, I argued that sentinel node biopsy should be performed only if the patient was going to be enrolled in a clinical study.
Many surgical oncologists have built their careers around the flawed premise that removing the draining nodes would cure melanoma. It doesn’t. It is past time to admit it and move on.
So, if completion node dissection does not save lives, why do a sentinel node biopsy? I recently asked a dermatologist friend, who is a committed acolyte of the sentinel node biopsy school, why he continues to recommend sentinel node biopsy if there is no benefit from complete node dissection. His quick response was that patients want to know if they are at higher risk of metastatic disease so that they can be followed closely with high-resolution ultrasound at a major cancer center and can be eligible for clinical trials. His reply gave me pause, so I asked why completion node dissection was still being recommended. I was told that some patients with positive sentinel nodes lived far away, and if they would not make regular follow-up visits for high-resolution ultrasound, the surgical oncologists do completion node dissection to ensure “local nodal control.” Yipes! You’re going to rip my groin out because I like quiet county living?
I doubt that patients would be enthusiastic if told beforehand that sentinel node biopsies costs $14,000-$18,000, and has a 9% complication rate, and one-third of those patients who have complications end up with permanent lymphedema. I wondered if the patients were told they could have a genetic test done on their already excised melanoma tissue that would tell them if they were in a high-risk group without having an additional invasive surgical procedure. I wondered if they were told that 10%-30% of people with negative sentinel nodes go on to develop metastatic disease. I also wondered if they had been told they would have to walk around with their melanoma, which could spread at any time, for several additional weeks, while waiting for the results of their sentinel node biopsy, instead of having the melanoma immediately removed by their dermatologist. I also wondered if they had been told that high-resolution ultrasound has not definitively been shown to be superior to clinical palpation of the lymph nodes.
I looked into the possibility of clinical trials for patients with positive sentinel nodes, as well. Based on my search of clinical trials.gov in January, there are 33 trials in the United States studying patients with stage 3 (positive sentinel node) or greater disease. If I had a positive sentinel node, I would look for a study in which I had a chance of getting nivolumab, which recently has been shown to be superior to ipilimumab in the phase 3 Checkmate 238 trial published in 2017 (N Engl J Med 2017 Nov 9; 377:1824-35).
But I am getting ahead of myself.
As a thinking man, if I had a thick melanoma (that was less than 2 mm), I would opt for a genetic test of my already excised melanoma tissue. If the results of that genetic test (which has near identical sensitivity and specificity for developing metastatic disease as a sentinel node) put me in the low-risk group, I would pass on the sentinel node biopsy. This would eliminate a lot of unnecessary surgery. If I fell into the high-risk group, I would consider a sentinel node biopsy so I could get into a study, or determine if I needed to find a way to get my insurance to pay, or if I could personally afford nivolumab. Even if I opted not to take the drug, because of the potential risk of high-grade side effects, the high-risk genetic profile tells me I would still need more frequent follow-up.
These are exciting times. I am looking forward to clinical trials that allow a patient with a high-risk genetic profile to go directly into a trial. We are moving into the realm of individualized genomic medicine in which metastatic melanoma truly becomes a curable disease.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Coldiron has no financial or other conflicts of interest with Castle Biosciences, the manufacturer of the DecisionDx-Melanoma genetic expression profile test. Email him at [email protected].
More than 17 years ago, I published an article that was largely ignored, predicating that patient benefit from the sentinel node biopsy procedure was unlikely.
I asserted that the lymph nodes are not a reliable filter for melanoma cells, lymphatic drainage is capricious, and many individuals (especially younger ones) have benign neval rests in their lymph nodes that cannot be distinguished from melanoma deposits, since they are both positive for the S100 protein (Int J Dermatol. 2000 Nov;39[11]:807-11). In addition, multiple uncontrolled studies had shown that locating sentinel nodes, followed by a complete lymph node dissection, had no survival benefit. At the time, I argued that sentinel node biopsy should be performed only if the patient was going to be enrolled in a clinical study.
Many surgical oncologists have built their careers around the flawed premise that removing the draining nodes would cure melanoma. It doesn’t. It is past time to admit it and move on.
So, if completion node dissection does not save lives, why do a sentinel node biopsy? I recently asked a dermatologist friend, who is a committed acolyte of the sentinel node biopsy school, why he continues to recommend sentinel node biopsy if there is no benefit from complete node dissection. His quick response was that patients want to know if they are at higher risk of metastatic disease so that they can be followed closely with high-resolution ultrasound at a major cancer center and can be eligible for clinical trials. His reply gave me pause, so I asked why completion node dissection was still being recommended. I was told that some patients with positive sentinel nodes lived far away, and if they would not make regular follow-up visits for high-resolution ultrasound, the surgical oncologists do completion node dissection to ensure “local nodal control.” Yipes! You’re going to rip my groin out because I like quiet county living?
I doubt that patients would be enthusiastic if told beforehand that sentinel node biopsies costs $14,000-$18,000, and has a 9% complication rate, and one-third of those patients who have complications end up with permanent lymphedema. I wondered if the patients were told they could have a genetic test done on their already excised melanoma tissue that would tell them if they were in a high-risk group without having an additional invasive surgical procedure. I wondered if they were told that 10%-30% of people with negative sentinel nodes go on to develop metastatic disease. I also wondered if they had been told they would have to walk around with their melanoma, which could spread at any time, for several additional weeks, while waiting for the results of their sentinel node biopsy, instead of having the melanoma immediately removed by their dermatologist. I also wondered if they had been told that high-resolution ultrasound has not definitively been shown to be superior to clinical palpation of the lymph nodes.
I looked into the possibility of clinical trials for patients with positive sentinel nodes, as well. Based on my search of clinical trials.gov in January, there are 33 trials in the United States studying patients with stage 3 (positive sentinel node) or greater disease. If I had a positive sentinel node, I would look for a study in which I had a chance of getting nivolumab, which recently has been shown to be superior to ipilimumab in the phase 3 Checkmate 238 trial published in 2017 (N Engl J Med 2017 Nov 9; 377:1824-35).
But I am getting ahead of myself.
As a thinking man, if I had a thick melanoma (that was less than 2 mm), I would opt for a genetic test of my already excised melanoma tissue. If the results of that genetic test (which has near identical sensitivity and specificity for developing metastatic disease as a sentinel node) put me in the low-risk group, I would pass on the sentinel node biopsy. This would eliminate a lot of unnecessary surgery. If I fell into the high-risk group, I would consider a sentinel node biopsy so I could get into a study, or determine if I needed to find a way to get my insurance to pay, or if I could personally afford nivolumab. Even if I opted not to take the drug, because of the potential risk of high-grade side effects, the high-risk genetic profile tells me I would still need more frequent follow-up.
These are exciting times. I am looking forward to clinical trials that allow a patient with a high-risk genetic profile to go directly into a trial. We are moving into the realm of individualized genomic medicine in which metastatic melanoma truly becomes a curable disease.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Coldiron has no financial or other conflicts of interest with Castle Biosciences, the manufacturer of the DecisionDx-Melanoma genetic expression profile test. Email him at [email protected].
‘We have met the enemy and he is us’
In a recent article, the New York Times publicly exposed behavior that can only be described as appalling: Some dermatologists have been using unsupervised physician assistants (PAs) and nurse practitioners (NPs) to perform dermatology services on patients, including frail nursing home patients, many with dementia or other similar cognitive impairments, to increase their profits.
The dermatologic organizations responding to the article included the American Academy of Dermatology, which, in a letter to the editor, stated that a board-certified dermatologist should “provide direct supervision of any nonphysician (PA/ARNP) for optimum dermatologic care,” a statement that was affirmed by the American College of Mohs Surgery. The American Society for Dermatologic Surgery and the Women’s Dermatologic Society sent similar, even more strongly worded letters.
Well, talk is cheap, and it is time for societies to step up and enforce their bylaws or amend them in order to remove members who practice in such an unethical fashion.
Also in November, an important paper by Adewole S. Adamson, MD, and his colleagues was published in JAMA Dermatology concerning the geographic distribution of physician extenders who billed Medicare independently for common dermatologic procedures in 2014 (doi: 10.1001/jamadermatol.2017.5039). The study found that they are geographically distributed in the same areas – suburbs and cities – where dermatologists already are located. In fact, 92% of those who were independently billing were employed by a dermatologist. The majority (71%) were in counties with high dermatologist density, while only 3% were in counties without dermatologists.
The argument that paraprofessionals provide care for the neglected in underserved areas of the country is unfounded. Physician extenders practice mostly in the same areas in which physicians practice, predominantly in the suburbs. This has been previously demonstrated by the American Medical Association and other surveys (N Engl J Med. 2013;368:1935-41).
In addition, as noted in the past, there are midlevel professionals who bill independently (that is, without direct supervision) for destruction of premalignant lesions, biopsies of skin lesions, excisions of skin cancer, surgical repairs, and flaps/grafts (JAMA Dermatol. 2014 Nov;150[11]:1153-9). But – based on a new finding in the Adamson study, and perhaps the most concerning – this list now includes the interpretation of pathology.
It must be noted that NPs and PAs are trained in primary care, even if up to a master’s degree or PhD level. This does not qualify them to practice specialty medicine independently. Neither does working for, or shadowing, a dermatologist, even if it is a near equivalent to completing a dermatology residency after medical school. PAs and NPs are qualified to practice primary care (PAs with a physician, NPs sometimes without) but not specialty medicine. They can work in a specialty medicine setting if they are directly supervised by a specialty physician.
In summary, “we have met the enemy and he is us,” to quote the comic strip character Pogo. As pointed out in the New York Times article, a few dermatologists are enabling and financially benefiting from paraprofessionals who practice dermatology, without any formal training.
The malpractice risk is huge. The insurance industry will surely realize that this costs them more, not less, because of additional biopsies, pathology interpretations, and missed diagnoses. Now the lay press has caught on to this abuse, and the exposure will not stop here. They will flip over every dermatologist using midlevel professionals in this fashion, starting with the biggest and working their way down
Fair warning has been given to those who use this practice model for their personal gain by the New York Times exposure and the hard lines drawn by the dermatology specialty societies. This technique of boosting profits is unsustainable. Dermatologists must supervise midlevel professionals or face public embarrassment, ethics probes from professional societies, audits, and possibly worse.
Our specialty should take this opportunity to distance itself from these profiteers. The patients hopefully will learn that they are being shortchanged, and demand to see a “real” dermatologist instead of a dermatology “provider.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
In a recent article, the New York Times publicly exposed behavior that can only be described as appalling: Some dermatologists have been using unsupervised physician assistants (PAs) and nurse practitioners (NPs) to perform dermatology services on patients, including frail nursing home patients, many with dementia or other similar cognitive impairments, to increase their profits.
The dermatologic organizations responding to the article included the American Academy of Dermatology, which, in a letter to the editor, stated that a board-certified dermatologist should “provide direct supervision of any nonphysician (PA/ARNP) for optimum dermatologic care,” a statement that was affirmed by the American College of Mohs Surgery. The American Society for Dermatologic Surgery and the Women’s Dermatologic Society sent similar, even more strongly worded letters.
Well, talk is cheap, and it is time for societies to step up and enforce their bylaws or amend them in order to remove members who practice in such an unethical fashion.
Also in November, an important paper by Adewole S. Adamson, MD, and his colleagues was published in JAMA Dermatology concerning the geographic distribution of physician extenders who billed Medicare independently for common dermatologic procedures in 2014 (doi: 10.1001/jamadermatol.2017.5039). The study found that they are geographically distributed in the same areas – suburbs and cities – where dermatologists already are located. In fact, 92% of those who were independently billing were employed by a dermatologist. The majority (71%) were in counties with high dermatologist density, while only 3% were in counties without dermatologists.
The argument that paraprofessionals provide care for the neglected in underserved areas of the country is unfounded. Physician extenders practice mostly in the same areas in which physicians practice, predominantly in the suburbs. This has been previously demonstrated by the American Medical Association and other surveys (N Engl J Med. 2013;368:1935-41).
In addition, as noted in the past, there are midlevel professionals who bill independently (that is, without direct supervision) for destruction of premalignant lesions, biopsies of skin lesions, excisions of skin cancer, surgical repairs, and flaps/grafts (JAMA Dermatol. 2014 Nov;150[11]:1153-9). But – based on a new finding in the Adamson study, and perhaps the most concerning – this list now includes the interpretation of pathology.
It must be noted that NPs and PAs are trained in primary care, even if up to a master’s degree or PhD level. This does not qualify them to practice specialty medicine independently. Neither does working for, or shadowing, a dermatologist, even if it is a near equivalent to completing a dermatology residency after medical school. PAs and NPs are qualified to practice primary care (PAs with a physician, NPs sometimes without) but not specialty medicine. They can work in a specialty medicine setting if they are directly supervised by a specialty physician.
In summary, “we have met the enemy and he is us,” to quote the comic strip character Pogo. As pointed out in the New York Times article, a few dermatologists are enabling and financially benefiting from paraprofessionals who practice dermatology, without any formal training.
The malpractice risk is huge. The insurance industry will surely realize that this costs them more, not less, because of additional biopsies, pathology interpretations, and missed diagnoses. Now the lay press has caught on to this abuse, and the exposure will not stop here. They will flip over every dermatologist using midlevel professionals in this fashion, starting with the biggest and working their way down
Fair warning has been given to those who use this practice model for their personal gain by the New York Times exposure and the hard lines drawn by the dermatology specialty societies. This technique of boosting profits is unsustainable. Dermatologists must supervise midlevel professionals or face public embarrassment, ethics probes from professional societies, audits, and possibly worse.
Our specialty should take this opportunity to distance itself from these profiteers. The patients hopefully will learn that they are being shortchanged, and demand to see a “real” dermatologist instead of a dermatology “provider.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
In a recent article, the New York Times publicly exposed behavior that can only be described as appalling: Some dermatologists have been using unsupervised physician assistants (PAs) and nurse practitioners (NPs) to perform dermatology services on patients, including frail nursing home patients, many with dementia or other similar cognitive impairments, to increase their profits.
The dermatologic organizations responding to the article included the American Academy of Dermatology, which, in a letter to the editor, stated that a board-certified dermatologist should “provide direct supervision of any nonphysician (PA/ARNP) for optimum dermatologic care,” a statement that was affirmed by the American College of Mohs Surgery. The American Society for Dermatologic Surgery and the Women’s Dermatologic Society sent similar, even more strongly worded letters.
Well, talk is cheap, and it is time for societies to step up and enforce their bylaws or amend them in order to remove members who practice in such an unethical fashion.
Also in November, an important paper by Adewole S. Adamson, MD, and his colleagues was published in JAMA Dermatology concerning the geographic distribution of physician extenders who billed Medicare independently for common dermatologic procedures in 2014 (doi: 10.1001/jamadermatol.2017.5039). The study found that they are geographically distributed in the same areas – suburbs and cities – where dermatologists already are located. In fact, 92% of those who were independently billing were employed by a dermatologist. The majority (71%) were in counties with high dermatologist density, while only 3% were in counties without dermatologists.
The argument that paraprofessionals provide care for the neglected in underserved areas of the country is unfounded. Physician extenders practice mostly in the same areas in which physicians practice, predominantly in the suburbs. This has been previously demonstrated by the American Medical Association and other surveys (N Engl J Med. 2013;368:1935-41).
In addition, as noted in the past, there are midlevel professionals who bill independently (that is, without direct supervision) for destruction of premalignant lesions, biopsies of skin lesions, excisions of skin cancer, surgical repairs, and flaps/grafts (JAMA Dermatol. 2014 Nov;150[11]:1153-9). But – based on a new finding in the Adamson study, and perhaps the most concerning – this list now includes the interpretation of pathology.
It must be noted that NPs and PAs are trained in primary care, even if up to a master’s degree or PhD level. This does not qualify them to practice specialty medicine independently. Neither does working for, or shadowing, a dermatologist, even if it is a near equivalent to completing a dermatology residency after medical school. PAs and NPs are qualified to practice primary care (PAs with a physician, NPs sometimes without) but not specialty medicine. They can work in a specialty medicine setting if they are directly supervised by a specialty physician.
In summary, “we have met the enemy and he is us,” to quote the comic strip character Pogo. As pointed out in the New York Times article, a few dermatologists are enabling and financially benefiting from paraprofessionals who practice dermatology, without any formal training.
The malpractice risk is huge. The insurance industry will surely realize that this costs them more, not less, because of additional biopsies, pathology interpretations, and missed diagnoses. Now the lay press has caught on to this abuse, and the exposure will not stop here. They will flip over every dermatologist using midlevel professionals in this fashion, starting with the biggest and working their way down
Fair warning has been given to those who use this practice model for their personal gain by the New York Times exposure and the hard lines drawn by the dermatology specialty societies. This technique of boosting profits is unsustainable. Dermatologists must supervise midlevel professionals or face public embarrassment, ethics probes from professional societies, audits, and possibly worse.
Our specialty should take this opportunity to distance itself from these profiteers. The patients hopefully will learn that they are being shortchanged, and demand to see a “real” dermatologist instead of a dermatology “provider.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].







