User login
Catherine Cooper Nellist is editor of Pediatric News and Ob. Gyn. News. She has more than 30 years of experience reporting, writing, and editing stories about clinical medicine and the U.S. health care industry. Prior to taking the helm of these award-winning publications, Catherine covered major medical research meetings throughout the United States and Canada, and had been editor of Clinical Psychiatry News, and Dermatology News. She joined the company in 1984 after graduating magna cum laude from Dickinson College, Carlisle, Pa., with a BA in English.
Clinical pattern may help distinguish pediatric NMN from subungal melanoma
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Psoriasis patients often have history of childhood trauma
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
RSV immunoprophylaxis in premature infants doesn’t prevent later asthma
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
FROM THE LANCET
Interventions urged to stop rising NAS, stem Medicaid costs
The incidence of neonatal abstinence syndrome (NAS) and the corresponding costs to Medicaid are unlikely to decline unless interventions focus on stopping opioid use by low-income mothers, said Tyler N.A. Winkelman, MD, of Hennepin County Medical Center, Minneapolis, and his associates.
Dr. Winkelman and his associates conducted a serial cross-sectional analysis that used 9,115,457 birth discharge records from the 2004-2014 National Inpatient Sample (NIS), which were representative of 43.6 million weighted births. Overall, 3,991,336 infants were covered by Medicaid, which were representative of 19.1 million weighted births. There were 35,629 (0.89%) infants with a diagnosis of NAS, which were representative of 173,384 weighted births. Medicaid was the primary payer for 74% (95% confidence interval, 68.9%-77.9%) of NAS-related births in 2004 and 82% (95% CI, 80.5%-83.5%) of NAS-related births in 2014.
Infants with NAS who were enrolled in Medicaid were significantly more likely to be male, live in a rural county, and have comorbidities reflective of the syndrome than were infants without NAS who were enrolled in Medicaid, the researchers wrote in Pediatrics.
from 1.5 per 1,000 hospital births (95% CI, 1.2-1.9) to 8 per 1,000 hospital births (95% CI, 7.2-8.7), as the opioid epidemic worsened in the country.
Infants with NAS who were covered by Medicaid had a greater chance of being transferred to another hospital for care (9% vs. 7%; P = .02) and stay in the hospital longer (17 days vs. 15 days; P less than .001), compared with infants with NAS who were covered by private insurance.
NAS is costly. In the 2011-2014 era, mean hospital costs for a NAS infant covered by Medicaid were more than fivefold higher than for an infant without NAS ($19,340/birth vs. $3,700/birth; P less than .001). After adjustment for inflation, mean hospital costs for infants with NAS who were covered by Medicaid increased 26% between 2004-2006 and 2011-2014 ($15,350 vs. $19,340; P less than .001), the researchers reported. Annual hospital costs, which were adjusted for inflation to 2014 U.S. dollars, for all infants with NAS who were covered by Medicaid rose from $65.4 million in 2004 to $462 million in 2014.
“With the disproportionate impact of NAS on the Medicaid population, we suggest that NAS incidence rates are unlikely to improve without interventions targeted at low-income mothers and infants,” Dr. Winkelman and his associates concluded.
Nonpharmacologic interventions are available to help NAS infants. “Systematic implementation of policies that support rooming-in, breastfeeding, swaddling, on-demand feeding schedules, and minimization of sleep disruption may reduce symptoms of NAS and reduce the duration of, or even eliminate the need for, pharmacologic treatment of NAS,” the researchers said. “Pharmacologic treatment with buprenorphine, for example, has been shown to reduce hospital length of stay by 35%.”
Another intervention is medication-assisted treatment during pregnancy, which studies have shown “improves outcomes and reduces costs associated with NAS, compared with attempted abstinence,” Dr. Winkelman and his associates said. It does not necessarily reduce NAS incidence, but “it may prevent prolonged hospital stays due to preterm birth, reduce NICU [neonatal intensive care unit] admissions, decrease the severity of NAS symptoms, and improve birth outcomes for some infants.”
The researchers also endorsed screening, referral, and treatment for substance abuse and mental health disorders among reproductive age women, including adolescents, because these are risk factors for opioid abuse.
One author was supported by an award from the National Institute on Drug Abuse. None of the other authors had relevant financial disclosures.
SOURCE: Winkelman TNA et al. Pediatrics. 2018;141(4):e20173520.
The incidence of neonatal abstinence syndrome (NAS) and the corresponding costs to Medicaid are unlikely to decline unless interventions focus on stopping opioid use by low-income mothers, said Tyler N.A. Winkelman, MD, of Hennepin County Medical Center, Minneapolis, and his associates.
Dr. Winkelman and his associates conducted a serial cross-sectional analysis that used 9,115,457 birth discharge records from the 2004-2014 National Inpatient Sample (NIS), which were representative of 43.6 million weighted births. Overall, 3,991,336 infants were covered by Medicaid, which were representative of 19.1 million weighted births. There were 35,629 (0.89%) infants with a diagnosis of NAS, which were representative of 173,384 weighted births. Medicaid was the primary payer for 74% (95% confidence interval, 68.9%-77.9%) of NAS-related births in 2004 and 82% (95% CI, 80.5%-83.5%) of NAS-related births in 2014.
Infants with NAS who were enrolled in Medicaid were significantly more likely to be male, live in a rural county, and have comorbidities reflective of the syndrome than were infants without NAS who were enrolled in Medicaid, the researchers wrote in Pediatrics.
from 1.5 per 1,000 hospital births (95% CI, 1.2-1.9) to 8 per 1,000 hospital births (95% CI, 7.2-8.7), as the opioid epidemic worsened in the country.
Infants with NAS who were covered by Medicaid had a greater chance of being transferred to another hospital for care (9% vs. 7%; P = .02) and stay in the hospital longer (17 days vs. 15 days; P less than .001), compared with infants with NAS who were covered by private insurance.
NAS is costly. In the 2011-2014 era, mean hospital costs for a NAS infant covered by Medicaid were more than fivefold higher than for an infant without NAS ($19,340/birth vs. $3,700/birth; P less than .001). After adjustment for inflation, mean hospital costs for infants with NAS who were covered by Medicaid increased 26% between 2004-2006 and 2011-2014 ($15,350 vs. $19,340; P less than .001), the researchers reported. Annual hospital costs, which were adjusted for inflation to 2014 U.S. dollars, for all infants with NAS who were covered by Medicaid rose from $65.4 million in 2004 to $462 million in 2014.
“With the disproportionate impact of NAS on the Medicaid population, we suggest that NAS incidence rates are unlikely to improve without interventions targeted at low-income mothers and infants,” Dr. Winkelman and his associates concluded.
Nonpharmacologic interventions are available to help NAS infants. “Systematic implementation of policies that support rooming-in, breastfeeding, swaddling, on-demand feeding schedules, and minimization of sleep disruption may reduce symptoms of NAS and reduce the duration of, or even eliminate the need for, pharmacologic treatment of NAS,” the researchers said. “Pharmacologic treatment with buprenorphine, for example, has been shown to reduce hospital length of stay by 35%.”
Another intervention is medication-assisted treatment during pregnancy, which studies have shown “improves outcomes and reduces costs associated with NAS, compared with attempted abstinence,” Dr. Winkelman and his associates said. It does not necessarily reduce NAS incidence, but “it may prevent prolonged hospital stays due to preterm birth, reduce NICU [neonatal intensive care unit] admissions, decrease the severity of NAS symptoms, and improve birth outcomes for some infants.”
The researchers also endorsed screening, referral, and treatment for substance abuse and mental health disorders among reproductive age women, including adolescents, because these are risk factors for opioid abuse.
One author was supported by an award from the National Institute on Drug Abuse. None of the other authors had relevant financial disclosures.
SOURCE: Winkelman TNA et al. Pediatrics. 2018;141(4):e20173520.
The incidence of neonatal abstinence syndrome (NAS) and the corresponding costs to Medicaid are unlikely to decline unless interventions focus on stopping opioid use by low-income mothers, said Tyler N.A. Winkelman, MD, of Hennepin County Medical Center, Minneapolis, and his associates.
Dr. Winkelman and his associates conducted a serial cross-sectional analysis that used 9,115,457 birth discharge records from the 2004-2014 National Inpatient Sample (NIS), which were representative of 43.6 million weighted births. Overall, 3,991,336 infants were covered by Medicaid, which were representative of 19.1 million weighted births. There were 35,629 (0.89%) infants with a diagnosis of NAS, which were representative of 173,384 weighted births. Medicaid was the primary payer for 74% (95% confidence interval, 68.9%-77.9%) of NAS-related births in 2004 and 82% (95% CI, 80.5%-83.5%) of NAS-related births in 2014.
Infants with NAS who were enrolled in Medicaid were significantly more likely to be male, live in a rural county, and have comorbidities reflective of the syndrome than were infants without NAS who were enrolled in Medicaid, the researchers wrote in Pediatrics.
from 1.5 per 1,000 hospital births (95% CI, 1.2-1.9) to 8 per 1,000 hospital births (95% CI, 7.2-8.7), as the opioid epidemic worsened in the country.
Infants with NAS who were covered by Medicaid had a greater chance of being transferred to another hospital for care (9% vs. 7%; P = .02) and stay in the hospital longer (17 days vs. 15 days; P less than .001), compared with infants with NAS who were covered by private insurance.
NAS is costly. In the 2011-2014 era, mean hospital costs for a NAS infant covered by Medicaid were more than fivefold higher than for an infant without NAS ($19,340/birth vs. $3,700/birth; P less than .001). After adjustment for inflation, mean hospital costs for infants with NAS who were covered by Medicaid increased 26% between 2004-2006 and 2011-2014 ($15,350 vs. $19,340; P less than .001), the researchers reported. Annual hospital costs, which were adjusted for inflation to 2014 U.S. dollars, for all infants with NAS who were covered by Medicaid rose from $65.4 million in 2004 to $462 million in 2014.
“With the disproportionate impact of NAS on the Medicaid population, we suggest that NAS incidence rates are unlikely to improve without interventions targeted at low-income mothers and infants,” Dr. Winkelman and his associates concluded.
Nonpharmacologic interventions are available to help NAS infants. “Systematic implementation of policies that support rooming-in, breastfeeding, swaddling, on-demand feeding schedules, and minimization of sleep disruption may reduce symptoms of NAS and reduce the duration of, or even eliminate the need for, pharmacologic treatment of NAS,” the researchers said. “Pharmacologic treatment with buprenorphine, for example, has been shown to reduce hospital length of stay by 35%.”
Another intervention is medication-assisted treatment during pregnancy, which studies have shown “improves outcomes and reduces costs associated with NAS, compared with attempted abstinence,” Dr. Winkelman and his associates said. It does not necessarily reduce NAS incidence, but “it may prevent prolonged hospital stays due to preterm birth, reduce NICU [neonatal intensive care unit] admissions, decrease the severity of NAS symptoms, and improve birth outcomes for some infants.”
The researchers also endorsed screening, referral, and treatment for substance abuse and mental health disorders among reproductive age women, including adolescents, because these are risk factors for opioid abuse.
One author was supported by an award from the National Institute on Drug Abuse. None of the other authors had relevant financial disclosures.
SOURCE: Winkelman TNA et al. Pediatrics. 2018;141(4):e20173520.
FROM PEDIATRICS
Key clinical point:
Major finding: In 2011-2014, mean hospital costs for NAS infants covered by Medicaid were more than fivefold higher than for infants without NAS ($19,340/birth vs. $3,700/birth).
Study details: A serial cross-sectional analysis that usd data from the 2004-2014 National Inpatient Sample (NIS) of 9,115,457 birth discharge records.
Disclosures: Stephen W. Patrick, MD, was supported by an award from the National Institute on Drug Abuse. None of the other authors had relevant financial disclosures.
Source: Winkelman TNA et al. Pediatrics. 2018;141(4):e20173520.
Tanning addiction associated with multiple behavioral comorbidities
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Follow-up care for pediatric concussions not heeded in Ontario
reported Liraz Fridman, PhD, of York University, Toronto, and associates.
In a 10-year, retrospective, population-based study, 126,654 children aged 5-18 years presented with concussions to emergency departments and physician offices in Ontario between April 1, 2003, and March 31, 2014. In 2003, 7,126 children were evaluated for a concussion, compared with 21,681 children by 2013.
Limitations to this study include that children treated by athletic therapists or chiropractors would have been missed, and that these data may not generalize across Canada or the United States, they said.
“In Ontario, the rate of follow-up care for concussions nearly tripled in both emergency departments and physician’s offices. Despite this significant improvement over time, more than two-thirds of all child and youth concussion patients still do not receive the minimum standard of care, according to accepted guidelines,” the researchers wrote, adding that the study’s findings suggest that better instructions for health care providers on management of concussion are needed.
SOURCE: Fridman L et al. J Pediatr. 2018;192:184-8
reported Liraz Fridman, PhD, of York University, Toronto, and associates.
In a 10-year, retrospective, population-based study, 126,654 children aged 5-18 years presented with concussions to emergency departments and physician offices in Ontario between April 1, 2003, and March 31, 2014. In 2003, 7,126 children were evaluated for a concussion, compared with 21,681 children by 2013.
Limitations to this study include that children treated by athletic therapists or chiropractors would have been missed, and that these data may not generalize across Canada or the United States, they said.
“In Ontario, the rate of follow-up care for concussions nearly tripled in both emergency departments and physician’s offices. Despite this significant improvement over time, more than two-thirds of all child and youth concussion patients still do not receive the minimum standard of care, according to accepted guidelines,” the researchers wrote, adding that the study’s findings suggest that better instructions for health care providers on management of concussion are needed.
SOURCE: Fridman L et al. J Pediatr. 2018;192:184-8
reported Liraz Fridman, PhD, of York University, Toronto, and associates.
In a 10-year, retrospective, population-based study, 126,654 children aged 5-18 years presented with concussions to emergency departments and physician offices in Ontario between April 1, 2003, and March 31, 2014. In 2003, 7,126 children were evaluated for a concussion, compared with 21,681 children by 2013.
Limitations to this study include that children treated by athletic therapists or chiropractors would have been missed, and that these data may not generalize across Canada or the United States, they said.
“In Ontario, the rate of follow-up care for concussions nearly tripled in both emergency departments and physician’s offices. Despite this significant improvement over time, more than two-thirds of all child and youth concussion patients still do not receive the minimum standard of care, according to accepted guidelines,” the researchers wrote, adding that the study’s findings suggest that better instructions for health care providers on management of concussion are needed.
SOURCE: Fridman L et al. J Pediatr. 2018;192:184-8
FROM THE JOURNAL OF PEDIATRICS
Vaccine priming determines teen susceptibility to pertussis
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
FROM VACCINE
Mercury vapor from skin cream caused neurotoxicity in toddler
researchers at the University of Arizona, Tucson, found in the case of a toddler who presented with puzzling symptoms.
“Although mercury toxicity is rare and has variable symptoms, it is valuable for clinicians to consider this diagnosis in cases of unexplained hypertension and neurologic findings,” Michael R. Ori, MD, and his associates wrote in the Journal of Pediatrics.
U.S. federal law has prohibited mercury in cosmetics beyond trace amounts (1 mg/kg) since 1973 because of toxicity concerns, but mercury-containing skin creams remain a public health problem in the United States.
A 17-month-old previously healthy girl was seen by her pediatrician because of a 3-week history of fussiness, constipation, decreased appetite, and temperature to 37.7° C. A chest radiograph was normal, as was a urinalysis. Two days later, the child was taken to the emergency department with symptoms of rhinorrhea, congestion, fussiness, and a fever of 38.3° C. She was sent home with a presumptive diagnosis of a viral syndrome. Her symptoms had not resolved 1 week later, and she returned to the pediatrician, having developed a limp with tenderness in the right knee. A radiograph of the knee was unremarkable, repeat urinalysis showed no evidence of a urinary tract infection, and an abdominal x-ray showed a large stool burden. She had a 0.5-kg weight loss and new hypertension, and was afebrile.
The child was admitted to the hospital the next day for an endocrine work-up, but no noticeable abnormalities were found. She became increasingly fussy with a poor appetite and continued weight loss, persistent hypertension, and an inability to walk. Heavy metal screening on day 18 revealed an elevated whole blood mercury level of 26 mcg/L (normal is less than 10 mcg/L), with a random spot urine mercury level of 243 mcg/g creatinine (normal is less than 35 mcg/g creatinine). Repeated chelation with succimer was provided. On day 61, she had significant delay in receptive language and fine motor skills on a Bayley scale. On the most recent evaluation on day 222, she was shy and had stereotypical hand-flapping behavior when stressed, the investigators reported.
Multiple conversations with the patient’s mother eventually identified the source of mercury as a skin-lightening facial cream she had been using for 4 months, which she stored in the refrigerator. The cream was produced and purchased in a beauty salon in Mexico. Several containers of the cream were sent to an Arizona state laboratory; they were found to have mercury levels between 27,000 and 34,000 mg/kg. The mother and the grandmother had no symptoms or findings on physical exam, but had markedly elevated first-void urine mercury levels of 197 mcg/g creatinine for the mother and 222 mcg/g creatinine for the grandmother, the researchers reported.
Testing of the home the family rented found ambient air mercury vapor levels ranged from 1,900 to 2,800 ng/m3 for most areas. Federal agencies recommend remediation for levels greater than 1,000 ng/m3; remediation was performed in the home, with some household items disposed of in a hazardous waste landfill.
This toddler’s exposure to mercury was from contact with contaminated people, objects, and vapor, although the mercury-containing cream was not directly put on her skin. Of these sources of contact, vapor may have contributed the most. There likely was incidental dermal contact through contaminated bed linens, and she also likely had incidental oral contact from contaminated objects that she put in her mouth, Dr. Ori and his associates reported.
Over time, central nervous system penetration occurs with neurologic dysfunction; “this was the dominant feature of this patient’s presentation, with debilitating leg pain, anorexia, constipation, neurasthenia, and hypertension. Acrodynia, meaning extremity pain, is an idiosyncratic reaction to mercury exposure seen in childhood. Symptoms include irritability,weakness, paresthesias, a pink papular rash, and desquamation of the palms and soles. Our patient did not have the characteristic dermal findings but did have other symptoms consistent with acrodynia,” they noted.
The authors declared no conflicts of interest.
SOURCE: Ori MR et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2017.12.0.23.
researchers at the University of Arizona, Tucson, found in the case of a toddler who presented with puzzling symptoms.
“Although mercury toxicity is rare and has variable symptoms, it is valuable for clinicians to consider this diagnosis in cases of unexplained hypertension and neurologic findings,” Michael R. Ori, MD, and his associates wrote in the Journal of Pediatrics.
U.S. federal law has prohibited mercury in cosmetics beyond trace amounts (1 mg/kg) since 1973 because of toxicity concerns, but mercury-containing skin creams remain a public health problem in the United States.
A 17-month-old previously healthy girl was seen by her pediatrician because of a 3-week history of fussiness, constipation, decreased appetite, and temperature to 37.7° C. A chest radiograph was normal, as was a urinalysis. Two days later, the child was taken to the emergency department with symptoms of rhinorrhea, congestion, fussiness, and a fever of 38.3° C. She was sent home with a presumptive diagnosis of a viral syndrome. Her symptoms had not resolved 1 week later, and she returned to the pediatrician, having developed a limp with tenderness in the right knee. A radiograph of the knee was unremarkable, repeat urinalysis showed no evidence of a urinary tract infection, and an abdominal x-ray showed a large stool burden. She had a 0.5-kg weight loss and new hypertension, and was afebrile.
The child was admitted to the hospital the next day for an endocrine work-up, but no noticeable abnormalities were found. She became increasingly fussy with a poor appetite and continued weight loss, persistent hypertension, and an inability to walk. Heavy metal screening on day 18 revealed an elevated whole blood mercury level of 26 mcg/L (normal is less than 10 mcg/L), with a random spot urine mercury level of 243 mcg/g creatinine (normal is less than 35 mcg/g creatinine). Repeated chelation with succimer was provided. On day 61, she had significant delay in receptive language and fine motor skills on a Bayley scale. On the most recent evaluation on day 222, she was shy and had stereotypical hand-flapping behavior when stressed, the investigators reported.
Multiple conversations with the patient’s mother eventually identified the source of mercury as a skin-lightening facial cream she had been using for 4 months, which she stored in the refrigerator. The cream was produced and purchased in a beauty salon in Mexico. Several containers of the cream were sent to an Arizona state laboratory; they were found to have mercury levels between 27,000 and 34,000 mg/kg. The mother and the grandmother had no symptoms or findings on physical exam, but had markedly elevated first-void urine mercury levels of 197 mcg/g creatinine for the mother and 222 mcg/g creatinine for the grandmother, the researchers reported.
Testing of the home the family rented found ambient air mercury vapor levels ranged from 1,900 to 2,800 ng/m3 for most areas. Federal agencies recommend remediation for levels greater than 1,000 ng/m3; remediation was performed in the home, with some household items disposed of in a hazardous waste landfill.
This toddler’s exposure to mercury was from contact with contaminated people, objects, and vapor, although the mercury-containing cream was not directly put on her skin. Of these sources of contact, vapor may have contributed the most. There likely was incidental dermal contact through contaminated bed linens, and she also likely had incidental oral contact from contaminated objects that she put in her mouth, Dr. Ori and his associates reported.
Over time, central nervous system penetration occurs with neurologic dysfunction; “this was the dominant feature of this patient’s presentation, with debilitating leg pain, anorexia, constipation, neurasthenia, and hypertension. Acrodynia, meaning extremity pain, is an idiosyncratic reaction to mercury exposure seen in childhood. Symptoms include irritability,weakness, paresthesias, a pink papular rash, and desquamation of the palms and soles. Our patient did not have the characteristic dermal findings but did have other symptoms consistent with acrodynia,” they noted.
The authors declared no conflicts of interest.
SOURCE: Ori MR et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2017.12.0.23.
researchers at the University of Arizona, Tucson, found in the case of a toddler who presented with puzzling symptoms.
“Although mercury toxicity is rare and has variable symptoms, it is valuable for clinicians to consider this diagnosis in cases of unexplained hypertension and neurologic findings,” Michael R. Ori, MD, and his associates wrote in the Journal of Pediatrics.
U.S. federal law has prohibited mercury in cosmetics beyond trace amounts (1 mg/kg) since 1973 because of toxicity concerns, but mercury-containing skin creams remain a public health problem in the United States.
A 17-month-old previously healthy girl was seen by her pediatrician because of a 3-week history of fussiness, constipation, decreased appetite, and temperature to 37.7° C. A chest radiograph was normal, as was a urinalysis. Two days later, the child was taken to the emergency department with symptoms of rhinorrhea, congestion, fussiness, and a fever of 38.3° C. She was sent home with a presumptive diagnosis of a viral syndrome. Her symptoms had not resolved 1 week later, and she returned to the pediatrician, having developed a limp with tenderness in the right knee. A radiograph of the knee was unremarkable, repeat urinalysis showed no evidence of a urinary tract infection, and an abdominal x-ray showed a large stool burden. She had a 0.5-kg weight loss and new hypertension, and was afebrile.
The child was admitted to the hospital the next day for an endocrine work-up, but no noticeable abnormalities were found. She became increasingly fussy with a poor appetite and continued weight loss, persistent hypertension, and an inability to walk. Heavy metal screening on day 18 revealed an elevated whole blood mercury level of 26 mcg/L (normal is less than 10 mcg/L), with a random spot urine mercury level of 243 mcg/g creatinine (normal is less than 35 mcg/g creatinine). Repeated chelation with succimer was provided. On day 61, she had significant delay in receptive language and fine motor skills on a Bayley scale. On the most recent evaluation on day 222, she was shy and had stereotypical hand-flapping behavior when stressed, the investigators reported.
Multiple conversations with the patient’s mother eventually identified the source of mercury as a skin-lightening facial cream she had been using for 4 months, which she stored in the refrigerator. The cream was produced and purchased in a beauty salon in Mexico. Several containers of the cream were sent to an Arizona state laboratory; they were found to have mercury levels between 27,000 and 34,000 mg/kg. The mother and the grandmother had no symptoms or findings on physical exam, but had markedly elevated first-void urine mercury levels of 197 mcg/g creatinine for the mother and 222 mcg/g creatinine for the grandmother, the researchers reported.
Testing of the home the family rented found ambient air mercury vapor levels ranged from 1,900 to 2,800 ng/m3 for most areas. Federal agencies recommend remediation for levels greater than 1,000 ng/m3; remediation was performed in the home, with some household items disposed of in a hazardous waste landfill.
This toddler’s exposure to mercury was from contact with contaminated people, objects, and vapor, although the mercury-containing cream was not directly put on her skin. Of these sources of contact, vapor may have contributed the most. There likely was incidental dermal contact through contaminated bed linens, and she also likely had incidental oral contact from contaminated objects that she put in her mouth, Dr. Ori and his associates reported.
Over time, central nervous system penetration occurs with neurologic dysfunction; “this was the dominant feature of this patient’s presentation, with debilitating leg pain, anorexia, constipation, neurasthenia, and hypertension. Acrodynia, meaning extremity pain, is an idiosyncratic reaction to mercury exposure seen in childhood. Symptoms include irritability,weakness, paresthesias, a pink papular rash, and desquamation of the palms and soles. Our patient did not have the characteristic dermal findings but did have other symptoms consistent with acrodynia,” they noted.
The authors declared no conflicts of interest.
SOURCE: Ori MR et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2017.12.0.23.
FROM THE JOURNAL OF PEDIATRICS
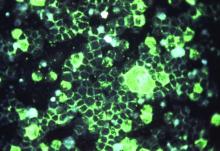
Dermoscopy will help diagnose pediatric melanomas
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point:
Major finding: On dermoscopy, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03).
Data source: Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across 9 countries.
Disclosures: The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was cofinanced by numerous other grants.
Source: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88.
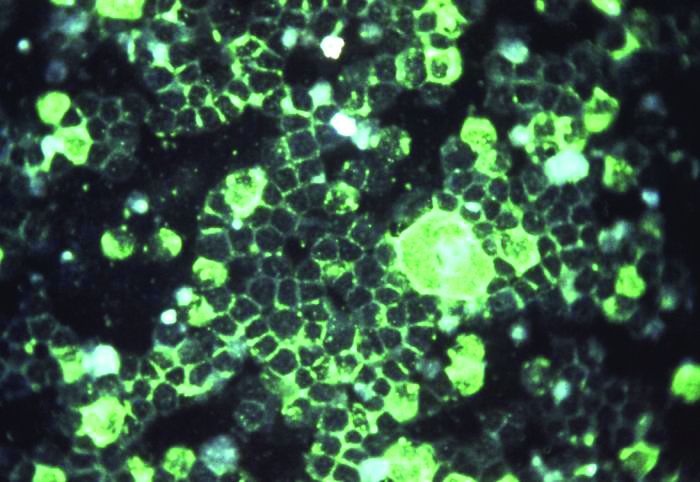
Satisfaction is high for cantharidin in molluscum contagiosum
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY