User login
Preventing and managing vaginal cuff dehiscence
Vaginal cuff dehiscence, or separation of the vaginal incision, is a rare postoperative complication unique to hysterectomy. Morbidity related to evisceration of abdominal contents can be profound and prompt intervention is required.
A 10-year observational study of 11,000 patients described a 0.24% cumulative incidence after all modes of hysterectomy.1 Though data are varied, the mode of hysterectomy does have an impact on the risk of dehiscence.
Laparoscopic (0.64%-1.35%) and robotic (0.46%-1.5%) hysterectomy have a higher incidence than abdominal (0.15%-0.26%) and vaginal (0.08%-0.25%) approaches.2 The use of monopolar cautery for colpotomy and different closure techniques may account for these differences.
Cuff cellulitis, early sexual intercourse, cigarette smoking, poor nutrition, obesity, menopausal status, and corticosteroid use are all proposed risk factors that promote infection, pressure at the vaginal cuff, and poor wound healing. Although some are modifiable, the rarity of this complication has made establishing causality and promoting prevention challenging.
Prevention
• Preoperatively. Treating bacterial vaginosis, Trichomonas vaginalis, gonorrhea, and chlamydia can decrease the risk of cuff cellulitis and dehiscence.3
• Intraoperatively. Surgeons should ensure adequate vaginal margins (greater than 1 cm) with full-thickness cuff closures while avoiding excessive electrocautery.4 Retrospective data show that transvaginal cuff closure is associated with a decreased risk of dehiscence.5 However, given the lack of randomized data and the difficulty controlling for surgeon experience, gynecologists should use the approach that they are most comfortable with. Though the various laparoscopic cuff closure techniques have limited evidence regarding superiority, some experts propose using two-layer cuff closure and barbed sutures.6-8 Several retrospective studies have found an equivalent or a decreased incidence of cuff dehiscence with barbed sutures, compared with other methods (e.g., 0-Vicryl, Endo Stitch).9,10
• Postoperatively. Women should avoid intercourse and lifting more than 15 pounds for at least 6-8 weeks as the vaginal cuff gains tensile strength. Vaginal estrogen can promote healing in postmenopausal patients.11
Management
Patients with vaginal cuff dehiscence commonly present within the first several weeks to months after surgery with pelvic pain (60%-100%), vaginal bleeding (30%-60%), vaginal discharge (30%), or vaginal pressure/mass (30%).1,7 Posthysterectomy patients with these complaints warrant an urgent evaluation. The diagnosis is made during a pelvic exam.
Broad-spectrum antibiotics are necessary because all vaginal cuff separations or dehiscences expose the peritoneal cavity to vaginal flora. Nonsurgical management is reasonable for small separations – less than 25% of the cuff – if there is no evidence of evisceration.
However, surgically closing all recognized cuff dehiscences is reasonable, given the potential for further separation. A vaginal approach is preferred when possible. Women with vaginal cuff dehiscence, stable vital signs, and no evidence of bowel evisceration can be repaired vaginally without an abdominal survey.
In contrast, women with bowel evisceration have a surgical emergency because of the risk of peritonitis and bowel injury. If the eviscerated bowel is not reducible, it should be irrigated and wrapped in a warm moist towel or gauze in preparation for inspection and reduction in the operating room. If the bowel is reducible, the patient can be placed in Trendelenburg’s position. Her vagina should be packed to reduce the risk of re-evisceration as she moves toward operative cuff repair.
If the physician is concerned about bowel injury, inspection via laparoscopy or laparotomy would be reasonable. However, when bowel injury is not suspected, a vaginal technique for dehiscence repair has been described by Matthews et al.:12
1. Expose the cuff with a weighted speculum and Breisky-Navratil retractors.
2. Sharply debride the cuff edges back to viable tissue.
3. Dissect adherent bowel or omentum to allow for full-thickness closure.
4. Place full-thickness, interrupted delayed absorbable sutures to reapproximate the cuff edges.
Cuff dehiscence is a rare but potentially morbid complication of hysterectomy. Prevention, recognition, and appropriate management can avoid life-threatening sequelae.
References
1. Obstet Gynecol. 2011 Oct;118(4):794-801.
2. JSLS. 2012 Oct-Dec;16(4):530-6.
3. Am J Obstet Gynecol. 1990 Sep;163(3):1016-21; discussion 1021-3.
4. Obstet Gynecol. 2013 Mar;121(3):654-73.
5. Obstet Gynecol. 2012 Sep;120(3):516-23.
6. J Am Assoc Gynecol Laparosc. 2002 Nov;9(4):474-80.
7. Eur J Obstet Gynecol Reprod Biol. 2006 Mar 1;125(1):134-8.
8. Obstet Gynecol. 2009 Aug;114(2 Pt 1):231-5.
9. J Minim Invasive Gynecol. 2011 Mar-Apr;18(2):218-23.
10. Int J Surg. 2015 Jul;19:27-30.
11. Maturitas. 2006 Feb 20;53(3):282-98.
12. Obstet Gynecol. 2014 Oct;124(4):705-8.
Dr. Pierce is a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Vaginal cuff dehiscence, or separation of the vaginal incision, is a rare postoperative complication unique to hysterectomy. Morbidity related to evisceration of abdominal contents can be profound and prompt intervention is required.
A 10-year observational study of 11,000 patients described a 0.24% cumulative incidence after all modes of hysterectomy.1 Though data are varied, the mode of hysterectomy does have an impact on the risk of dehiscence.
Laparoscopic (0.64%-1.35%) and robotic (0.46%-1.5%) hysterectomy have a higher incidence than abdominal (0.15%-0.26%) and vaginal (0.08%-0.25%) approaches.2 The use of monopolar cautery for colpotomy and different closure techniques may account for these differences.
Cuff cellulitis, early sexual intercourse, cigarette smoking, poor nutrition, obesity, menopausal status, and corticosteroid use are all proposed risk factors that promote infection, pressure at the vaginal cuff, and poor wound healing. Although some are modifiable, the rarity of this complication has made establishing causality and promoting prevention challenging.
Prevention
• Preoperatively. Treating bacterial vaginosis, Trichomonas vaginalis, gonorrhea, and chlamydia can decrease the risk of cuff cellulitis and dehiscence.3
• Intraoperatively. Surgeons should ensure adequate vaginal margins (greater than 1 cm) with full-thickness cuff closures while avoiding excessive electrocautery.4 Retrospective data show that transvaginal cuff closure is associated with a decreased risk of dehiscence.5 However, given the lack of randomized data and the difficulty controlling for surgeon experience, gynecologists should use the approach that they are most comfortable with. Though the various laparoscopic cuff closure techniques have limited evidence regarding superiority, some experts propose using two-layer cuff closure and barbed sutures.6-8 Several retrospective studies have found an equivalent or a decreased incidence of cuff dehiscence with barbed sutures, compared with other methods (e.g., 0-Vicryl, Endo Stitch).9,10
• Postoperatively. Women should avoid intercourse and lifting more than 15 pounds for at least 6-8 weeks as the vaginal cuff gains tensile strength. Vaginal estrogen can promote healing in postmenopausal patients.11
Management
Patients with vaginal cuff dehiscence commonly present within the first several weeks to months after surgery with pelvic pain (60%-100%), vaginal bleeding (30%-60%), vaginal discharge (30%), or vaginal pressure/mass (30%).1,7 Posthysterectomy patients with these complaints warrant an urgent evaluation. The diagnosis is made during a pelvic exam.
Broad-spectrum antibiotics are necessary because all vaginal cuff separations or dehiscences expose the peritoneal cavity to vaginal flora. Nonsurgical management is reasonable for small separations – less than 25% of the cuff – if there is no evidence of evisceration.
However, surgically closing all recognized cuff dehiscences is reasonable, given the potential for further separation. A vaginal approach is preferred when possible. Women with vaginal cuff dehiscence, stable vital signs, and no evidence of bowel evisceration can be repaired vaginally without an abdominal survey.
In contrast, women with bowel evisceration have a surgical emergency because of the risk of peritonitis and bowel injury. If the eviscerated bowel is not reducible, it should be irrigated and wrapped in a warm moist towel or gauze in preparation for inspection and reduction in the operating room. If the bowel is reducible, the patient can be placed in Trendelenburg’s position. Her vagina should be packed to reduce the risk of re-evisceration as she moves toward operative cuff repair.
If the physician is concerned about bowel injury, inspection via laparoscopy or laparotomy would be reasonable. However, when bowel injury is not suspected, a vaginal technique for dehiscence repair has been described by Matthews et al.:12
1. Expose the cuff with a weighted speculum and Breisky-Navratil retractors.
2. Sharply debride the cuff edges back to viable tissue.
3. Dissect adherent bowel or omentum to allow for full-thickness closure.
4. Place full-thickness, interrupted delayed absorbable sutures to reapproximate the cuff edges.
Cuff dehiscence is a rare but potentially morbid complication of hysterectomy. Prevention, recognition, and appropriate management can avoid life-threatening sequelae.
References
1. Obstet Gynecol. 2011 Oct;118(4):794-801.
2. JSLS. 2012 Oct-Dec;16(4):530-6.
3. Am J Obstet Gynecol. 1990 Sep;163(3):1016-21; discussion 1021-3.
4. Obstet Gynecol. 2013 Mar;121(3):654-73.
5. Obstet Gynecol. 2012 Sep;120(3):516-23.
6. J Am Assoc Gynecol Laparosc. 2002 Nov;9(4):474-80.
7. Eur J Obstet Gynecol Reprod Biol. 2006 Mar 1;125(1):134-8.
8. Obstet Gynecol. 2009 Aug;114(2 Pt 1):231-5.
9. J Minim Invasive Gynecol. 2011 Mar-Apr;18(2):218-23.
10. Int J Surg. 2015 Jul;19:27-30.
11. Maturitas. 2006 Feb 20;53(3):282-98.
12. Obstet Gynecol. 2014 Oct;124(4):705-8.
Dr. Pierce is a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Vaginal cuff dehiscence, or separation of the vaginal incision, is a rare postoperative complication unique to hysterectomy. Morbidity related to evisceration of abdominal contents can be profound and prompt intervention is required.
A 10-year observational study of 11,000 patients described a 0.24% cumulative incidence after all modes of hysterectomy.1 Though data are varied, the mode of hysterectomy does have an impact on the risk of dehiscence.
Laparoscopic (0.64%-1.35%) and robotic (0.46%-1.5%) hysterectomy have a higher incidence than abdominal (0.15%-0.26%) and vaginal (0.08%-0.25%) approaches.2 The use of monopolar cautery for colpotomy and different closure techniques may account for these differences.
Cuff cellulitis, early sexual intercourse, cigarette smoking, poor nutrition, obesity, menopausal status, and corticosteroid use are all proposed risk factors that promote infection, pressure at the vaginal cuff, and poor wound healing. Although some are modifiable, the rarity of this complication has made establishing causality and promoting prevention challenging.
Prevention
• Preoperatively. Treating bacterial vaginosis, Trichomonas vaginalis, gonorrhea, and chlamydia can decrease the risk of cuff cellulitis and dehiscence.3
• Intraoperatively. Surgeons should ensure adequate vaginal margins (greater than 1 cm) with full-thickness cuff closures while avoiding excessive electrocautery.4 Retrospective data show that transvaginal cuff closure is associated with a decreased risk of dehiscence.5 However, given the lack of randomized data and the difficulty controlling for surgeon experience, gynecologists should use the approach that they are most comfortable with. Though the various laparoscopic cuff closure techniques have limited evidence regarding superiority, some experts propose using two-layer cuff closure and barbed sutures.6-8 Several retrospective studies have found an equivalent or a decreased incidence of cuff dehiscence with barbed sutures, compared with other methods (e.g., 0-Vicryl, Endo Stitch).9,10
• Postoperatively. Women should avoid intercourse and lifting more than 15 pounds for at least 6-8 weeks as the vaginal cuff gains tensile strength. Vaginal estrogen can promote healing in postmenopausal patients.11
Management
Patients with vaginal cuff dehiscence commonly present within the first several weeks to months after surgery with pelvic pain (60%-100%), vaginal bleeding (30%-60%), vaginal discharge (30%), or vaginal pressure/mass (30%).1,7 Posthysterectomy patients with these complaints warrant an urgent evaluation. The diagnosis is made during a pelvic exam.
Broad-spectrum antibiotics are necessary because all vaginal cuff separations or dehiscences expose the peritoneal cavity to vaginal flora. Nonsurgical management is reasonable for small separations – less than 25% of the cuff – if there is no evidence of evisceration.
However, surgically closing all recognized cuff dehiscences is reasonable, given the potential for further separation. A vaginal approach is preferred when possible. Women with vaginal cuff dehiscence, stable vital signs, and no evidence of bowel evisceration can be repaired vaginally without an abdominal survey.
In contrast, women with bowel evisceration have a surgical emergency because of the risk of peritonitis and bowel injury. If the eviscerated bowel is not reducible, it should be irrigated and wrapped in a warm moist towel or gauze in preparation for inspection and reduction in the operating room. If the bowel is reducible, the patient can be placed in Trendelenburg’s position. Her vagina should be packed to reduce the risk of re-evisceration as she moves toward operative cuff repair.
If the physician is concerned about bowel injury, inspection via laparoscopy or laparotomy would be reasonable. However, when bowel injury is not suspected, a vaginal technique for dehiscence repair has been described by Matthews et al.:12
1. Expose the cuff with a weighted speculum and Breisky-Navratil retractors.
2. Sharply debride the cuff edges back to viable tissue.
3. Dissect adherent bowel or omentum to allow for full-thickness closure.
4. Place full-thickness, interrupted delayed absorbable sutures to reapproximate the cuff edges.
Cuff dehiscence is a rare but potentially morbid complication of hysterectomy. Prevention, recognition, and appropriate management can avoid life-threatening sequelae.
References
1. Obstet Gynecol. 2011 Oct;118(4):794-801.
2. JSLS. 2012 Oct-Dec;16(4):530-6.
3. Am J Obstet Gynecol. 1990 Sep;163(3):1016-21; discussion 1021-3.
4. Obstet Gynecol. 2013 Mar;121(3):654-73.
5. Obstet Gynecol. 2012 Sep;120(3):516-23.
6. J Am Assoc Gynecol Laparosc. 2002 Nov;9(4):474-80.
7. Eur J Obstet Gynecol Reprod Biol. 2006 Mar 1;125(1):134-8.
8. Obstet Gynecol. 2009 Aug;114(2 Pt 1):231-5.
9. J Minim Invasive Gynecol. 2011 Mar-Apr;18(2):218-23.
10. Int J Surg. 2015 Jul;19:27-30.
11. Maturitas. 2006 Feb 20;53(3):282-98.
12. Obstet Gynecol. 2014 Oct;124(4):705-8.
Dr. Pierce is a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Vulvar intraepithelial neoplasia: Changing terms and therapy trends
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at [email protected].
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at [email protected].
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at [email protected].
Treating VTE in patients with gynecologic malignancies
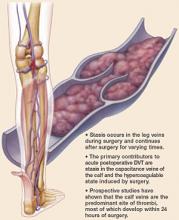
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Risk-reducing salpingectomy during surgery for benign indications
Ovarian cancer is the most deadly gynecologic malignancy in the United States, with 14,270 deaths expected in 2014 (CA Cancer J. Clin. 2014;64:9-29 ). The 5-year overall survival remains less than 50%. Difficulties in treatment arise due to its aggressive nature, coupled with vague symptomatology and no effective screening test. Advanced-stage disease at the time of diagnosis is an unfortunate hallmark.
Traditional teaching about the pathogenesis of ovarian cancers has been that a metaplastic change in the mesothelial ovarian surface leads to their de novo development. Under this paradigm, 70% of serous tumors were ovarian, 17% peritoneal, and 13% tubal in origin. However, a major change occurred when BRCA carriers began having risk-reducing bilateral salpingo-oophorectomies (BSO). Sequential histologic sections of the adnexa found occult malignancy in 30% of fallopian tubes, but similar lesions were not present within the ovary (Am. J. Surg. Pathol. 1020;34:1407-16). Could these cancers in the fallopian tube be the precursor lesion and then seed or spread to the ovarian surface?
Molecular and genetic analysis of these serous tubal intraepithelial carcinoma (STIC) cells found p53 mutations that were identical to those in concurrent “ovarian” tumors. STICs have been identified in 70% of nonhereditary forms of serous ovarian cancer. Under this paradigm of STIC as tubal in origin, only 28% of serous tumors were ovarian and 64% were of tubal origin (Am. J. Surg. Pathol. 2007;31:161-9).
This paradigm shift elicited new hypotheses about the etiology of endometrioid and clear cell types of ovarian cancer. Rather than metaplasia of the surface epithelium, endometrioid and clear cell tumors may result from retrograde menstruation, with the fallopian tube acting as a conduit for cells to gain access to the peritoneal cavity and the ovarian surface. This hypothesis provides a mechanism for the 34% reduction in ovarian cancer with bilateral tubal ligation (Hum. Reprod. Update 2011;17:55-67). Interestingly, in a large collaborative pooled analysis, the risk reduction of tubal ligation was greatest for endometrioid and clear cell subtypes (Int. J. Epidemiol. 2013;42:579-89).
Given the mounting evidence of fallopian tube involvement in the development of ovarian cancers, there are new primary prevention considerations. After 5 or more years of oral contraceptive use, a 50% reduction in the relative risk of ovarian cancer has been reported (Ann. Epidemiol. 2011;21:188-96). Bilateral salpingo-oophorectomy provides a greater than 50% risk reduction even in the highest-risk BRCA-positive population. However, results from the Nurses’ Health Study suggest that while there are fewer cancers in a low-risk population following BSO, it comes with an increase in all-cause mortality, predominately due to negative cardiovascular effects. With these issues in mind, is it time to consider incorporating prophylactic bilateral salpingectomy in benign gynecologic surgery (Obstet. Gynecol. 2013;121:709-16)?
While salpingectomy at the time of hysterectomy for benign conditions or for sterilization is becoming more common, there are concerns about premature loss of ovarian function secondary to compromise of ovarian blood supply. However, amassing data demonstrates preserved ovarian function. A retrospective study comparing total laparoscopic hysterectomy (TLH) to TLH with bilateral salpingectomy found no difference in markers of ovarian function (anti-Müllerian hormone, FSH, antral follicle count, mean ovarian diameters) up to 3 months postoperatively (Gynecol. Oncol. 2013;129:448-51). In a randomized controlled trial, 30 women were 1:1 randomized to TLH vs. TLH with salpingectomy. There was no change in anti-Müllerian hormone levels (at 3 months), operative time, or estimated blood loss (Fertil. Steril. 2013;100:1704-8). While there are concerns about the paucity of long-term follow-up data, these initial studies are encouraging. Additionally, a large retrospective study of 540 BRCA-negative patients found no difference in surgical outcomes with salpingectomy (estimated blood loss, hospital stay), and furthermore, the study found that removal of the tubes significantly reduces the risk of developing subsequent benign adnexal lesions by nearly 50% (J. Cancer Res. Clin. Oncol. 2014;140:859-65).
Though salpingectomy removes tubal re-anastomosis as an option in cases of “tubal ligation regret,” wisely choosing candidates can minimize this risk. Women less than 30 years old are at highest risk for regret, and the decision for salpingectomy in these patients should be made with caution and extensive counseling. Yet recently, emerging thought leaders in family planning have called for removal to be routinely considered (Obstet. Gynecol. 2014;124:596-9).
Surgical technique involves electrosurgery or suture ligation just inferior to the fallopian tube, ligating the fallopian branches of the ovarian and utero-ovarian arteries while avoiding unnecessary involvement of ovarian branches within the mesosalpinx. Since the fimbria are thought to be the site of origin for many serous carcinomas, removing the fimbrial portion of the tube is crucial.
Ovarian cancer remains the most deadly gynecologic malignancy. Efforts to find effective screening methods have not yet delivered. Pathologic data confirms that over half of “ovarian” cancers are actually of tubal origin, and we should consider risk-reducing salpingectomy in the low-risk population. The Society of Gynecologic Oncology in their November 2013 Clinical Practice Statement stated, “For women at average risk of ovarian cancer, risk-reducing salpingectomy should also be discussed and considered with patients at the time of abdominal or pelvic surgery, hysterectomy or in lieu of tubal ligation [once childbearing is complete].”
Dr. Pierce is a third-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. Dr. Pierce and Dr. Clarke-Pearson said that they had no relevant financial disclosures.
Ovarian cancer is the most deadly gynecologic malignancy in the United States, with 14,270 deaths expected in 2014 (CA Cancer J. Clin. 2014;64:9-29 ). The 5-year overall survival remains less than 50%. Difficulties in treatment arise due to its aggressive nature, coupled with vague symptomatology and no effective screening test. Advanced-stage disease at the time of diagnosis is an unfortunate hallmark.
Traditional teaching about the pathogenesis of ovarian cancers has been that a metaplastic change in the mesothelial ovarian surface leads to their de novo development. Under this paradigm, 70% of serous tumors were ovarian, 17% peritoneal, and 13% tubal in origin. However, a major change occurred when BRCA carriers began having risk-reducing bilateral salpingo-oophorectomies (BSO). Sequential histologic sections of the adnexa found occult malignancy in 30% of fallopian tubes, but similar lesions were not present within the ovary (Am. J. Surg. Pathol. 1020;34:1407-16). Could these cancers in the fallopian tube be the precursor lesion and then seed or spread to the ovarian surface?
Molecular and genetic analysis of these serous tubal intraepithelial carcinoma (STIC) cells found p53 mutations that were identical to those in concurrent “ovarian” tumors. STICs have been identified in 70% of nonhereditary forms of serous ovarian cancer. Under this paradigm of STIC as tubal in origin, only 28% of serous tumors were ovarian and 64% were of tubal origin (Am. J. Surg. Pathol. 2007;31:161-9).
This paradigm shift elicited new hypotheses about the etiology of endometrioid and clear cell types of ovarian cancer. Rather than metaplasia of the surface epithelium, endometrioid and clear cell tumors may result from retrograde menstruation, with the fallopian tube acting as a conduit for cells to gain access to the peritoneal cavity and the ovarian surface. This hypothesis provides a mechanism for the 34% reduction in ovarian cancer with bilateral tubal ligation (Hum. Reprod. Update 2011;17:55-67). Interestingly, in a large collaborative pooled analysis, the risk reduction of tubal ligation was greatest for endometrioid and clear cell subtypes (Int. J. Epidemiol. 2013;42:579-89).
Given the mounting evidence of fallopian tube involvement in the development of ovarian cancers, there are new primary prevention considerations. After 5 or more years of oral contraceptive use, a 50% reduction in the relative risk of ovarian cancer has been reported (Ann. Epidemiol. 2011;21:188-96). Bilateral salpingo-oophorectomy provides a greater than 50% risk reduction even in the highest-risk BRCA-positive population. However, results from the Nurses’ Health Study suggest that while there are fewer cancers in a low-risk population following BSO, it comes with an increase in all-cause mortality, predominately due to negative cardiovascular effects. With these issues in mind, is it time to consider incorporating prophylactic bilateral salpingectomy in benign gynecologic surgery (Obstet. Gynecol. 2013;121:709-16)?
While salpingectomy at the time of hysterectomy for benign conditions or for sterilization is becoming more common, there are concerns about premature loss of ovarian function secondary to compromise of ovarian blood supply. However, amassing data demonstrates preserved ovarian function. A retrospective study comparing total laparoscopic hysterectomy (TLH) to TLH with bilateral salpingectomy found no difference in markers of ovarian function (anti-Müllerian hormone, FSH, antral follicle count, mean ovarian diameters) up to 3 months postoperatively (Gynecol. Oncol. 2013;129:448-51). In a randomized controlled trial, 30 women were 1:1 randomized to TLH vs. TLH with salpingectomy. There was no change in anti-Müllerian hormone levels (at 3 months), operative time, or estimated blood loss (Fertil. Steril. 2013;100:1704-8). While there are concerns about the paucity of long-term follow-up data, these initial studies are encouraging. Additionally, a large retrospective study of 540 BRCA-negative patients found no difference in surgical outcomes with salpingectomy (estimated blood loss, hospital stay), and furthermore, the study found that removal of the tubes significantly reduces the risk of developing subsequent benign adnexal lesions by nearly 50% (J. Cancer Res. Clin. Oncol. 2014;140:859-65).
Though salpingectomy removes tubal re-anastomosis as an option in cases of “tubal ligation regret,” wisely choosing candidates can minimize this risk. Women less than 30 years old are at highest risk for regret, and the decision for salpingectomy in these patients should be made with caution and extensive counseling. Yet recently, emerging thought leaders in family planning have called for removal to be routinely considered (Obstet. Gynecol. 2014;124:596-9).
Surgical technique involves electrosurgery or suture ligation just inferior to the fallopian tube, ligating the fallopian branches of the ovarian and utero-ovarian arteries while avoiding unnecessary involvement of ovarian branches within the mesosalpinx. Since the fimbria are thought to be the site of origin for many serous carcinomas, removing the fimbrial portion of the tube is crucial.
Ovarian cancer remains the most deadly gynecologic malignancy. Efforts to find effective screening methods have not yet delivered. Pathologic data confirms that over half of “ovarian” cancers are actually of tubal origin, and we should consider risk-reducing salpingectomy in the low-risk population. The Society of Gynecologic Oncology in their November 2013 Clinical Practice Statement stated, “For women at average risk of ovarian cancer, risk-reducing salpingectomy should also be discussed and considered with patients at the time of abdominal or pelvic surgery, hysterectomy or in lieu of tubal ligation [once childbearing is complete].”
Dr. Pierce is a third-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. Dr. Pierce and Dr. Clarke-Pearson said that they had no relevant financial disclosures.
Ovarian cancer is the most deadly gynecologic malignancy in the United States, with 14,270 deaths expected in 2014 (CA Cancer J. Clin. 2014;64:9-29 ). The 5-year overall survival remains less than 50%. Difficulties in treatment arise due to its aggressive nature, coupled with vague symptomatology and no effective screening test. Advanced-stage disease at the time of diagnosis is an unfortunate hallmark.
Traditional teaching about the pathogenesis of ovarian cancers has been that a metaplastic change in the mesothelial ovarian surface leads to their de novo development. Under this paradigm, 70% of serous tumors were ovarian, 17% peritoneal, and 13% tubal in origin. However, a major change occurred when BRCA carriers began having risk-reducing bilateral salpingo-oophorectomies (BSO). Sequential histologic sections of the adnexa found occult malignancy in 30% of fallopian tubes, but similar lesions were not present within the ovary (Am. J. Surg. Pathol. 1020;34:1407-16). Could these cancers in the fallopian tube be the precursor lesion and then seed or spread to the ovarian surface?
Molecular and genetic analysis of these serous tubal intraepithelial carcinoma (STIC) cells found p53 mutations that were identical to those in concurrent “ovarian” tumors. STICs have been identified in 70% of nonhereditary forms of serous ovarian cancer. Under this paradigm of STIC as tubal in origin, only 28% of serous tumors were ovarian and 64% were of tubal origin (Am. J. Surg. Pathol. 2007;31:161-9).
This paradigm shift elicited new hypotheses about the etiology of endometrioid and clear cell types of ovarian cancer. Rather than metaplasia of the surface epithelium, endometrioid and clear cell tumors may result from retrograde menstruation, with the fallopian tube acting as a conduit for cells to gain access to the peritoneal cavity and the ovarian surface. This hypothesis provides a mechanism for the 34% reduction in ovarian cancer with bilateral tubal ligation (Hum. Reprod. Update 2011;17:55-67). Interestingly, in a large collaborative pooled analysis, the risk reduction of tubal ligation was greatest for endometrioid and clear cell subtypes (Int. J. Epidemiol. 2013;42:579-89).
Given the mounting evidence of fallopian tube involvement in the development of ovarian cancers, there are new primary prevention considerations. After 5 or more years of oral contraceptive use, a 50% reduction in the relative risk of ovarian cancer has been reported (Ann. Epidemiol. 2011;21:188-96). Bilateral salpingo-oophorectomy provides a greater than 50% risk reduction even in the highest-risk BRCA-positive population. However, results from the Nurses’ Health Study suggest that while there are fewer cancers in a low-risk population following BSO, it comes with an increase in all-cause mortality, predominately due to negative cardiovascular effects. With these issues in mind, is it time to consider incorporating prophylactic bilateral salpingectomy in benign gynecologic surgery (Obstet. Gynecol. 2013;121:709-16)?
While salpingectomy at the time of hysterectomy for benign conditions or for sterilization is becoming more common, there are concerns about premature loss of ovarian function secondary to compromise of ovarian blood supply. However, amassing data demonstrates preserved ovarian function. A retrospective study comparing total laparoscopic hysterectomy (TLH) to TLH with bilateral salpingectomy found no difference in markers of ovarian function (anti-Müllerian hormone, FSH, antral follicle count, mean ovarian diameters) up to 3 months postoperatively (Gynecol. Oncol. 2013;129:448-51). In a randomized controlled trial, 30 women were 1:1 randomized to TLH vs. TLH with salpingectomy. There was no change in anti-Müllerian hormone levels (at 3 months), operative time, or estimated blood loss (Fertil. Steril. 2013;100:1704-8). While there are concerns about the paucity of long-term follow-up data, these initial studies are encouraging. Additionally, a large retrospective study of 540 BRCA-negative patients found no difference in surgical outcomes with salpingectomy (estimated blood loss, hospital stay), and furthermore, the study found that removal of the tubes significantly reduces the risk of developing subsequent benign adnexal lesions by nearly 50% (J. Cancer Res. Clin. Oncol. 2014;140:859-65).
Though salpingectomy removes tubal re-anastomosis as an option in cases of “tubal ligation regret,” wisely choosing candidates can minimize this risk. Women less than 30 years old are at highest risk for regret, and the decision for salpingectomy in these patients should be made with caution and extensive counseling. Yet recently, emerging thought leaders in family planning have called for removal to be routinely considered (Obstet. Gynecol. 2014;124:596-9).
Surgical technique involves electrosurgery or suture ligation just inferior to the fallopian tube, ligating the fallopian branches of the ovarian and utero-ovarian arteries while avoiding unnecessary involvement of ovarian branches within the mesosalpinx. Since the fimbria are thought to be the site of origin for many serous carcinomas, removing the fimbrial portion of the tube is crucial.
Ovarian cancer remains the most deadly gynecologic malignancy. Efforts to find effective screening methods have not yet delivered. Pathologic data confirms that over half of “ovarian” cancers are actually of tubal origin, and we should consider risk-reducing salpingectomy in the low-risk population. The Society of Gynecologic Oncology in their November 2013 Clinical Practice Statement stated, “For women at average risk of ovarian cancer, risk-reducing salpingectomy should also be discussed and considered with patients at the time of abdominal or pelvic surgery, hysterectomy or in lieu of tubal ligation [once childbearing is complete].”
Dr. Pierce is a third-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. Dr. Pierce and Dr. Clarke-Pearson said that they had no relevant financial disclosures.
Surgery in an aging population, part 2
Because of the increased risks associated with surgery in an elderly population, a thorough preoperative assessment should include identification of medical problems and important risk factors for increased perioperative morbidity and mortality, a thorough evaluation of the patient’s activities of daily living, and a mini–mental status exam (Primary Care 1989;16:361-76).
The severity of a patient’s illness is a better predictor of perioperative morbidity than age, and therefore age alone should not determine whether gynecologists operate (Clin. Podiatr. Med. Surg. 2003;20:607-26). In elderly patients, we should consider preoperative consultation with the patient’s primary care physician, subspecialists, geriatricians, physical and occupational therapists, and anesthesiologist to evaluate comorbidities and optimize preoperative status. Posthospitalization discharge planning also should start preoperatively if there is a concern that a patient may not be able to be discharged home.
Gynecologists also should consider the indications for surgery and a patient’s life expectancy. Prior to surgery, surgeons should believe that each patient has an expected life span such that they will benefit from the surgery. We should perform the most appropriate and least aggressive surgery and take into consideration the duration of the procedure. Surgeons also should consider functional outcomes, including quality of life, and the goal should be a postoperative return to normal function (Mt. Sinai J. Med. 2012;79:95-106).
Other factors to consider once a gynecologist has decided to operate on an elderly patient include surgical approach, mode of anesthesia, and the need for operative staging. An abdominal surgery is a risk factor for perioperative morbidity. Therefore, a laparoscopic or vaginal approach should be considered in elderly patients. These surgeries may promote more rapid return to functional status, thereby decreasing the risk of postoperative respiratory complications, length of hospital stay, and risk of delirium and postoperative cognitive decline (Curr. Opin. Obstet. Gynecol. 1997;9:300-305).Unfortunately, changes in cardiovascular physiology during abdominal insufflation and desufflation may lead to decreased peripheral perfusion and increased cardiac output. Additionally, a laparoscopic approach can lead to increases in operating time. Therefore, a gynecologist must carefully consider surgical approach.
Another important aspect to consider prior to surgery is whether the procedure can be performed under neuraxial anesthesia. An epidural could be left in place for postoperative pain control and eliminate the need for general anesthesia and postoperative pain control with narcotics. Gynecologic oncologists specifically must consider whether extending the procedure to include surgical staging is necessary and appropriate for each individual patient. A specific example concerns lymph node dissection in endometrial cancer. A recent study has shown that 5-year survival does not differ in women older than 80 years with low-grade endometrial cancer if lymph node dissection is omitted (Gynecol. Oncol. 2012;126:12-15).This may be important in limiting total anesthetic time to under 3 hours in an attempt to decrease perioperative morbidity and mortality.
Specific operating room considerations include patient position, coverage, and orientation. Elderly patients have fragile skin with decreased elasticity and decreased muscle mass. Therefore, they are more sensitive than their younger counterparts to bruising, skin tears, pressure ulcers, and hypothermia. Extra care must be taken during patient positioning to pad joints, avoid tape on fragile skin, and keep her covered with blankets or a warming device. Elderly patients also are at increased risk for venous thromboembolism; therefore sequential compression devices and, potentially, chemoprophylaxis should be used intraoperatively. On emergence from anesthesia, elderly patients should be given their glasses, and operating room staff should speak clearly and loudly to orient the patient to their situation.
Postoperatively, providers and family should continue to orient and reorient elderly patients to person, place, and situation. Good pain control is important, especially with larger abdominal incisions, to decrease respiratory complications and promote early ambulation. NSAIDs or neuraxial anesthesia should be considered to decrease the use of potentially sedating opioids. But avoid NSAIDs in patients with dehydration, congestive heart failure, and preexisting renal disease. It also is important to get patients back to their activities of daily living as soon as possible; therefore inpatient physical and occupational therapy should be considered on the day following surgery. Prior to discharge, care to avoid too many additional medications and attention to potential medication interactions are critical.
Elderly women are at risk for increased postoperative morbidity and mortality; however, with appropriate perioperative planning, these risks can be minimized. Each patient and her situation should be carefully evaluated, and a multidisciplinary team assembled to assist with taking the steps necessary to promote a smooth transition to the outpatient setting and decrease complications.
Dr. Hacker is a rising fourth-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. E-mail them at [email protected].
Because of the increased risks associated with surgery in an elderly population, a thorough preoperative assessment should include identification of medical problems and important risk factors for increased perioperative morbidity and mortality, a thorough evaluation of the patient’s activities of daily living, and a mini–mental status exam (Primary Care 1989;16:361-76).
The severity of a patient’s illness is a better predictor of perioperative morbidity than age, and therefore age alone should not determine whether gynecologists operate (Clin. Podiatr. Med. Surg. 2003;20:607-26). In elderly patients, we should consider preoperative consultation with the patient’s primary care physician, subspecialists, geriatricians, physical and occupational therapists, and anesthesiologist to evaluate comorbidities and optimize preoperative status. Posthospitalization discharge planning also should start preoperatively if there is a concern that a patient may not be able to be discharged home.
Gynecologists also should consider the indications for surgery and a patient’s life expectancy. Prior to surgery, surgeons should believe that each patient has an expected life span such that they will benefit from the surgery. We should perform the most appropriate and least aggressive surgery and take into consideration the duration of the procedure. Surgeons also should consider functional outcomes, including quality of life, and the goal should be a postoperative return to normal function (Mt. Sinai J. Med. 2012;79:95-106).
Other factors to consider once a gynecologist has decided to operate on an elderly patient include surgical approach, mode of anesthesia, and the need for operative staging. An abdominal surgery is a risk factor for perioperative morbidity. Therefore, a laparoscopic or vaginal approach should be considered in elderly patients. These surgeries may promote more rapid return to functional status, thereby decreasing the risk of postoperative respiratory complications, length of hospital stay, and risk of delirium and postoperative cognitive decline (Curr. Opin. Obstet. Gynecol. 1997;9:300-305).Unfortunately, changes in cardiovascular physiology during abdominal insufflation and desufflation may lead to decreased peripheral perfusion and increased cardiac output. Additionally, a laparoscopic approach can lead to increases in operating time. Therefore, a gynecologist must carefully consider surgical approach.
Another important aspect to consider prior to surgery is whether the procedure can be performed under neuraxial anesthesia. An epidural could be left in place for postoperative pain control and eliminate the need for general anesthesia and postoperative pain control with narcotics. Gynecologic oncologists specifically must consider whether extending the procedure to include surgical staging is necessary and appropriate for each individual patient. A specific example concerns lymph node dissection in endometrial cancer. A recent study has shown that 5-year survival does not differ in women older than 80 years with low-grade endometrial cancer if lymph node dissection is omitted (Gynecol. Oncol. 2012;126:12-15).This may be important in limiting total anesthetic time to under 3 hours in an attempt to decrease perioperative morbidity and mortality.
Specific operating room considerations include patient position, coverage, and orientation. Elderly patients have fragile skin with decreased elasticity and decreased muscle mass. Therefore, they are more sensitive than their younger counterparts to bruising, skin tears, pressure ulcers, and hypothermia. Extra care must be taken during patient positioning to pad joints, avoid tape on fragile skin, and keep her covered with blankets or a warming device. Elderly patients also are at increased risk for venous thromboembolism; therefore sequential compression devices and, potentially, chemoprophylaxis should be used intraoperatively. On emergence from anesthesia, elderly patients should be given their glasses, and operating room staff should speak clearly and loudly to orient the patient to their situation.
Postoperatively, providers and family should continue to orient and reorient elderly patients to person, place, and situation. Good pain control is important, especially with larger abdominal incisions, to decrease respiratory complications and promote early ambulation. NSAIDs or neuraxial anesthesia should be considered to decrease the use of potentially sedating opioids. But avoid NSAIDs in patients with dehydration, congestive heart failure, and preexisting renal disease. It also is important to get patients back to their activities of daily living as soon as possible; therefore inpatient physical and occupational therapy should be considered on the day following surgery. Prior to discharge, care to avoid too many additional medications and attention to potential medication interactions are critical.
Elderly women are at risk for increased postoperative morbidity and mortality; however, with appropriate perioperative planning, these risks can be minimized. Each patient and her situation should be carefully evaluated, and a multidisciplinary team assembled to assist with taking the steps necessary to promote a smooth transition to the outpatient setting and decrease complications.
Dr. Hacker is a rising fourth-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. E-mail them at [email protected].
Because of the increased risks associated with surgery in an elderly population, a thorough preoperative assessment should include identification of medical problems and important risk factors for increased perioperative morbidity and mortality, a thorough evaluation of the patient’s activities of daily living, and a mini–mental status exam (Primary Care 1989;16:361-76).
The severity of a patient’s illness is a better predictor of perioperative morbidity than age, and therefore age alone should not determine whether gynecologists operate (Clin. Podiatr. Med. Surg. 2003;20:607-26). In elderly patients, we should consider preoperative consultation with the patient’s primary care physician, subspecialists, geriatricians, physical and occupational therapists, and anesthesiologist to evaluate comorbidities and optimize preoperative status. Posthospitalization discharge planning also should start preoperatively if there is a concern that a patient may not be able to be discharged home.
Gynecologists also should consider the indications for surgery and a patient’s life expectancy. Prior to surgery, surgeons should believe that each patient has an expected life span such that they will benefit from the surgery. We should perform the most appropriate and least aggressive surgery and take into consideration the duration of the procedure. Surgeons also should consider functional outcomes, including quality of life, and the goal should be a postoperative return to normal function (Mt. Sinai J. Med. 2012;79:95-106).
Other factors to consider once a gynecologist has decided to operate on an elderly patient include surgical approach, mode of anesthesia, and the need for operative staging. An abdominal surgery is a risk factor for perioperative morbidity. Therefore, a laparoscopic or vaginal approach should be considered in elderly patients. These surgeries may promote more rapid return to functional status, thereby decreasing the risk of postoperative respiratory complications, length of hospital stay, and risk of delirium and postoperative cognitive decline (Curr. Opin. Obstet. Gynecol. 1997;9:300-305).Unfortunately, changes in cardiovascular physiology during abdominal insufflation and desufflation may lead to decreased peripheral perfusion and increased cardiac output. Additionally, a laparoscopic approach can lead to increases in operating time. Therefore, a gynecologist must carefully consider surgical approach.
Another important aspect to consider prior to surgery is whether the procedure can be performed under neuraxial anesthesia. An epidural could be left in place for postoperative pain control and eliminate the need for general anesthesia and postoperative pain control with narcotics. Gynecologic oncologists specifically must consider whether extending the procedure to include surgical staging is necessary and appropriate for each individual patient. A specific example concerns lymph node dissection in endometrial cancer. A recent study has shown that 5-year survival does not differ in women older than 80 years with low-grade endometrial cancer if lymph node dissection is omitted (Gynecol. Oncol. 2012;126:12-15).This may be important in limiting total anesthetic time to under 3 hours in an attempt to decrease perioperative morbidity and mortality.
Specific operating room considerations include patient position, coverage, and orientation. Elderly patients have fragile skin with decreased elasticity and decreased muscle mass. Therefore, they are more sensitive than their younger counterparts to bruising, skin tears, pressure ulcers, and hypothermia. Extra care must be taken during patient positioning to pad joints, avoid tape on fragile skin, and keep her covered with blankets or a warming device. Elderly patients also are at increased risk for venous thromboembolism; therefore sequential compression devices and, potentially, chemoprophylaxis should be used intraoperatively. On emergence from anesthesia, elderly patients should be given their glasses, and operating room staff should speak clearly and loudly to orient the patient to their situation.
Postoperatively, providers and family should continue to orient and reorient elderly patients to person, place, and situation. Good pain control is important, especially with larger abdominal incisions, to decrease respiratory complications and promote early ambulation. NSAIDs or neuraxial anesthesia should be considered to decrease the use of potentially sedating opioids. But avoid NSAIDs in patients with dehydration, congestive heart failure, and preexisting renal disease. It also is important to get patients back to their activities of daily living as soon as possible; therefore inpatient physical and occupational therapy should be considered on the day following surgery. Prior to discharge, care to avoid too many additional medications and attention to potential medication interactions are critical.
Elderly women are at risk for increased postoperative morbidity and mortality; however, with appropriate perioperative planning, these risks can be minimized. Each patient and her situation should be carefully evaluated, and a multidisciplinary team assembled to assist with taking the steps necessary to promote a smooth transition to the outpatient setting and decrease complications.
Dr. Hacker is a rising fourth-year resident in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at the university. E-mail them at [email protected].
Preventing VTE: Evidence-based perioperative tactics
Pulmonary embolism is a master of disguises. It can appear with classic symptoms such as pleuritic chest pain, hemoptysis, and tachycardia—or it can arrive more insidiously, apparent only as a slight elevation in the respiratory rate.
This matters because 40% of all deaths following gynecologic surgery are directly attributable to pulmonary emboli,1 and pulmonary emboli are the most frequent cause of postoperative death in women with uterine or cervical carcinoma.2
Deep venous thrombosis (DVT) is almost as evasive. We know the signs and symptoms of DVT of the lower extremities—pain, edema, erythema, and a prominent vascular pattern of the superficial veins—but 50% to 80% of patients with these symptoms do not have DVT, and 80% of patients with symptomatic pulmonary embolism have no antecedent signs of thrombosis in the lower extremities.2 Morbidity and expense rise dramatically with DVT, especially when postphlebitic syndrome occurs.
How can we minimize these risks?
A good outcome is most likely when we:
- recognize risk factors,
- provide appropriate perioperative prophylaxis, and
- diagnose and treat venous thromboembolism (VTE) quickly.
This article looks in detail at each of these strategies.
3 factors set the stage for thrombogenesis
- Hypercoagulable state
- Venous stasis
- Vessel endothelial injury
These factors, known as Virchow’s triad, are especially likely at the time of major surgery, or when the patient is advanced in age or has a history of DVT, cancer, lower extremity edema, or venous stasis.
Intraoperative risk factors for postoperative DVT include increased anesthesia time, greater blood loss, and need for transfusion.
Some preventive methods come close to ideal
Being aware of risk factors is vital to provide the appropriate level of prophylaxis (TABLES 1 AND 2).3,4 The first step is identifying high-risk patients and tailoring the regimen to meet their individual needs. The perfect prophylactic method is not yet devised, but would be effective, free of significant side effects, well accepted by the patient and nursing staff, widely applicable to most patient groups, and inexpensive. A number of methods come close.
TABLE 1
Risk factors for thromboembolism
| Major gynecologic surgery |
| Age >40 years |
| Malignancy |
| Previous venous thrombosis (DVT or pulmonary embolism) |
| Obesity |
| Immobility |
| Pregnancy and the postpartum period |
| Oral contraceptives, hormone therapy, or tamoxifen |
| Varicose veins |
| Inherited or acquired thrombophilia (eg, Factor V Leiden) |
| Prolonged surgical procedure |
| Radical vulvectomy, inguinal-femoral lymphadenectomy, or pelvic exenteration |
TABLE 2
Match the preventive strategy to the surgery
| SURGERY | STRATEGY | DURATION OF PROPHYLAXIS* |
|---|---|---|
| Procedures <30 min for benign disease | Prophylaxis not needed | — |
| Laparoscopic gynecologic procedures in women with additional risk factors | Unfractionated heparin, 5,000 bid or | Until hospital discharge |
| LMWH, ≤3,400 U/day or | ||
| External pneumatic compression or | ||
| Graduated compression stockings | ||
| Major surgery for benign disease without additional risk factors | Unfractionated heparin, 5,000 U bid or | Until hospital discharge |
| LMWH, <3,400 U/day or | ||
| External pneumatic compression | ||
| Extensive major surgery in women with cancer or additional risk factors | Unfractionated heparin, 5,000 U tid or | Until hospital discharge |
| LMWH, >3,400 U/day or | ||
| External pneumatic compression | ||
| *For women at particularly high risk (eg, cancer surgery, age >60 years, prior VTE), continue prophylaxis for 2–4 weeks after hospital discharge. | ||
| Modified from Geerts WH, et al20 | ||
Low-dose unfractionated heparin
The most extensively studied prophylactic method is the use of small, subcutaneous doses of heparin. More than 25 controlled trials have shown that, when heparin is given subcutaneously 2 hours before surgery and every 8 to 12 hours afterward, the incidence of DVT diminishes substantially.
The value of low-dose heparin in preventing pulmonary emboli was established by a randomized, controlled, multicenter, international trial, in which fatal postoperative pulmonary emboli declined significantly in general surgery patients given the drug every 8 hours after surgery.5 In gynecologic surgical patients, postoperative DVT also declined significantly.
Increase in minor bleeding complications. Although low-dose heparin is thought to have no measurable effect on coagulation, most large series have noted an increase in minor bleeding complications such as wound hematoma. Up to 10% to 15% of otherwise healthy patients develop transiently prolonged activated partial thromboplastin time (APTT) after 5,000 U of heparin are given subcutaneously.6
Although relatively rare, thrombocytopenia is associated with the use of low-dose heparin. It has been found in 6% of women after gynecologic surgery.6 Therefore, it is reasonable to measure platelets in any patient taking low-dose heparin longer than 4 days to screen for heparin-induced thrombocytopenia.
Fear of major bleeding complications is unsubstantiated. There is ample evidence from placebo-controlled, blinded trials and meta-analysis that the risk of clinically important bleeding does not increase. Moreover, detailed analysis demonstrates that low-dose heparin has a good risk-to-benefit ratio and is cost-effective.
Low-molecular-weight heparins
These drugs are fragments of unfractionated heparin that vary in size from 4,500 to 6,500 daltons. Low-molecular-weight heparin (LMWH) has more anti-Xa and less antithrombin activity than unfractionated heparin and thus has less of an effect on partial thromboplastin time. LMWH may also lead to fewer bleeding complications.7
Once-daily dosing is possible. An increased half-life of 4 hours for LMWH produces greater bioavailability than with low-dose heparin. This allows once-daily dosing.
Pick one: Convenience or cost
Randomized controlled trials have compared LMWH to unfractionated heparin in gynecologic surgical patients. In all studies, DVT occurred in similar, low numbers of women regardless of the heparin used. Bleeding complications also were similar.8
A meta-analysis of general surgery and gynecologic surgery patients from 32 trials likewise found daily LMWH to be as effective as unfractionated heparin in DVT prophylaxis, without any difference in hemorrhagic complications.9
The choice of drugs often boils down to convenience versus cost: Prophylactic LMWH can be given once a day (compared with 2 or 3 times for unfractionated heparin), but is much more expensive.
Mechanical prophylactic methods
External pneumatic compression rivals low-dose heparin. The largest body of literature on mechanical methods to reduce postoperative venous stasis involves intermittent leg compression by pneumatically inflated sleeves placed around the calf or leg during surgery and after. A number of devices and sleeve designs are available, none of which has proven to be superior to the others.
In my experience, calf compression during and after gynecologic surgery lowers the incidence of DVT to a level seen with low-dose heparin. Besides increasing venous flow and pulsatile emptying of the calf veins, pneumatic compression appears to augment endogenous fibrinolysis, which may stimulate lysis of very early thrombi.10
How long is best for external compression? The optimal duration of postoperative external pneumatic compression is unclear. It may be effective when used in the operating room and for the first 24 hours postoperatively in patients with benign conditions who will ambulate on the first day after surgery.11,12
In women undergoing major surgery for gynecologic malignancy, it reduces the incidence of postoperative venous thromboemboli by nearly 3-fold, but only if calf compression is applied intraoperatively and for the first 5 postoperative days.13,14 These women may remain at risk because of stasis and a hypercoagulable state for a longer time than general surgical patients.
External pneumatic leg compression has no serious side effects or risks and is slightly more cost-effective than prophylactic drugs.15 However, to be fully effective, this method must be used consistently, in compliance with the protocol, when the patient is not ambulating.
Stockings can be a help or hazard. Controlled studies of graduated pressure stockings are limited but suggest modest benefit with careful fitting.16 Poorly fitted stockings that roll down the leg may create a tourniquet effect at the knee or mid-thigh. Another disadvantage of the stockings: The limited sizes available do not allow a perfect fit for all patients. This is especially true in obese patients.
The simplicity of elastic stockings and the absence of serious side effects are probably why stockings are often included in routine postoperative care.
Don’t overlook basic precautions. Although they may offer only modest benefit, short preoperative hospital stays and early postoperative ambulation are recommended.
Another basic strategy: elevating the foot of the bed to raise the calf above heart level. This allows gravity to drain the calf veins and should further reduce stasis.
How to detect VTE
DVT has nonspecific signs and symptoms
When DVT occurs in the lower extremities, harbingers such as pain, edema, and erythema are relatively nonspecific; 50% to 80% of patients exhibiting them do not have DVT. Conversely, approximately 80% of patients with symptomatic pulmonary emboli have no signs or symptoms of thrombosis in the lower extremities.
Because of this lack of specificity, additional tests are needed to establish DVT.
Diagnostic studies
A definitive diagnosis of DVT and pulmonary embolism is mandatory because diagnosis based on clinical symptoms and signs alone is frequently wrong. Strategies to reduce the use of ultrasound or spiral CT scanning have been put forward. These studies have evaluated outpatients using algorithms that utilize clinical probability (“clinical decision rule”) and D-dimer levels.
This strategy has been very accurate and avoids the use of ultrasound or spiral CT in low-risk patients. For example, individuals with a low probability score have an incidence of DVT below 5%, so ultrasound is unnecessary. This diagnostic strategy relies on the recognition of elevated D-dimer levels. Unfortunately, D-dimer is increased by a variety of nonthrombotic disorders, including recent surgery, hemorrhage, trauma, pregnancy, and cancer. Therefore, we cannot recommend the use of this strategy for the postoperative gynecologic surgery patient.17,18
Venography no longer the gold standard. Other diagnostic studies may be more useful. Venography has fallen from favor because it is moderately uncomfortable, requires injection of a contrast material that may trigger an allergic reaction or renal injury, and causes phlebitis in approximately 5% of patients.2 Newer, noninvasive diagnostic tests have been developed, fortunately.
Doppler ultrasound. B-mode duplex Doppler imaging is the most common technique to diagnose symptomatic venous thrombosis, especially when it arises in the proximal lower extremity. With duplex Doppler imaging, the femoral vein can be visualized, and clots may be seen directly. Compression of the vein with the tip of the ultrasound probe makes it possible to assess venous collapsibility, which is diminished when a thrombus is present.
Doppler imaging is less accurate when evaluating the calf and pelvic veins.
Magnetic resonance venography (MRV) sensitivity and specificity are comparable to venography. In addition, MRV may detect thrombi in pelvic veins that are not imaged by venography. The primary drawback is the time required to examine the lower extremity and pelvis. Further, MRV rarely identifies calf thrombi (most often not life-threatening, but potentially symptomatic) and is considerably more expensive than ultrasound.
Which prevention strategy works best?
We now consider low-molecular-weight heparin and external pneumatic compression the best choices
Because low-dose unfractionated heparin, low-molecular-weight heparin (LMWH), and external pneumatic compression all reduce the incidence of postoperative venous thromboembolism in high-risk gynecologic surgical patients, the question is: Which strategy is best?
We conducted 2 randomized clinical trials to answer this question.
Trial 1 Low-dose heparin vs pneumatic compression
Women were randomized to receive either low-dose heparin (5,000 U subcutaneously preoperatively and every 8 hours after surgery until hospital discharge) or external pneumatic compression of the calf prior to surgery and until hospital discharge.1
The incidence of DVT was identical in both groups, and no patients developed a pulmonary embolus throughout 30 days of follow-up. However, bleeding complications occurred more often in the group randomized to low-dose heparin. Specifically, nearly 25% had APTT levels in the “therapeutic” range, and significantly more patients required blood transfusions. After this trial, our institution decided to use external pneumatic compression because of its more favorable risk profile.1
Trial 2 LMWH vs pneumatic compression
The question of the best therapy arose again with the advent of LMWH, because of the possibility that these drugs carried a lower risk of bleeding complications. We therefore conducted a second trial to compare LMWH with external pneumatic compression.2
Because higher doses of LMWH had already proven to be more effective in cancer patients, we gave women in the trial 5,000 U dalteparin (Fragmin) preoperatively and 5,000 U daily postoperatively until hospital discharge.
In this trial, external pneumatic compression and LMWH produced similar low frequencies of DVT and no pulmonary emboli throughout 30 days of follow-up. We also found no association between LMWH and bleeding complications or transfusion requirements. Compliance and patient satisfaction were similar for both modalities.2
Bottom line
We now consider LMWH and external pneumatic compression the best choices for prophylaxis in gynecologic surgical patients.
REFERENCES
1. Clarke-Pearson DL, Synan IS, Dodge R, Soper JT, Berchuck A, Coleman RE. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol. 1993;168:1146-1154.
2. Maxwell GL, Synan I, Dodge R, Carroll B, Clarke-Pearson DI. Pneumatic compression versus low molecular weight heparin in gynecologic oncology surgery: a randomized trial. Obstet Gynecol. 2001;98:989-995.
Increasing use of laparoscopic surgery raises an important question: What is the thromboembolic risk of laparoscopy itself? On one hand, many laparoscopic surgeries are prolonged, and intraperitoneal pressure from the pneumoperitoneum reduces venous flow. On the other hand, many patients who have laparoscopy have shorter hospital stays and return sooner to normal activities than those who have open procedures.
Although the risks of venous thromboembolism (VTE) have not been studied as thoroughly as other aspects of laparoscopy, they appear to be low. To date, there are no randomized trials of VTE prophylaxis among women undergoing gynecologic laparoscopy.
The prudent course
Nevertheless, it would seem prudent to consider prophylaxis when women with additional risk factors undergo extensive laparoscopic procedures.
Pulmonary embolism is often stealthy
Many of the typical signs and symptoms of pulmonary embolism are associated with other, more common pulmonary complications following surgery. Classic findings that should alert the physician to the possibility of pulmonary embolism include:
- pleuritic chest pain
- hemoptysis
- shortness of breath
- tachycardia
- tachypnea
Often, however, the signs are subtle and may include only persistent tachycardia or a slight elevation in respiration.
When pulmonary embolism is suspected, a chest x-ray, electrocardiography, and arterial blood gas assessment are warranted. Any abnormality justifies further evaluation by ventilation-perfusion lung scan or a spiral computed tomography scan of the chest. Unfortunately, a high percentage of lung scans are interpreted as “indeterminate.” In such cases, careful clinical evaluation and judgment are needed to determine whether pulmonary arteriography is necessary to document or exclude pulmonary embolism.
Immediate, aggressive therapy is crucial
The treatment of postoperative DVT requires immediate anticoagulant therapy using either unfractionated heparin or LMWH, followed by 6 months of oral anticoagulant therapy with warfarin.
Treatment strategy: Unfractionated heparin
Once VTE is diagnosed, start unfractionated heparin to prevent proximal propagation of the thrombus and allow physiologic thrombolytic pathways to dissolve the clot. After an initial IV bolus of 5,000 U, give the patient a continuous infusion of 30,000 U daily, and adjust the dose to maintain APTT levels at a therapeutic level that is 1.5 to 2.5 times the control value.
Subtherapeutic APTT levels in the first 24 hours mean a risk of recurrent thromboembolism 15 times greater than the risk in patients with appropriate levels. Therefore, aggressive management is warranted to achieve prompt anticoagulation.
Start an oral anticoagulant (warfarin) on the first day of heparin infusion, and monitor the international normalized ratio (INR) daily until a therapeutic level is achieved. The change in the INR after warfarin administration often precedes the anticoagulant effect by about 2 days, during which time low protein C levels are associated with a transient hypercoagulable state. Therefore, it is important to continue the heparin until the INR has been maintained in a therapeutic range for at least 2 days to confirm the proper warfarin dose. Intravenous heparin can be discontinued after 5 days if an adequate INR level has been established.
Alternative strategy: LMWH
A meta-analysis involving more than 1,000 patients from 19 trials suggests that LMWH is more effective, safer, and less costly than unfractionated heparin in preventing recurrent thromboembolism.19 The lower cost derives from the ability to use the drugs in an outpatient setting.
Dosages are unique and weight-adjusted according to each LMWH preparation. Because LMWH has a minimal effect on APTT, serial laboratory monitoring of APTT levels is unnecessary. Nor is monitoring of anti-Xa activity of significant benefit in the dose adjustment of LMWH.
Basic treatment of pulmonary embolism
In most cases, immediate anticoagulant therapy identical to that outlined for DVT is sufficient to prevent repeat thrombosis and embolism and to allow the patient’s endogenous thrombolytic mechanisms to lyse the pulmonary embolus.
Other interventions include:
- Respiratory support, including oxygen, bronchodilators, and intensive care.
- Although massive pulmonary emboli are usually quickly fatal, pulmonary embolectomy has been successful on rare occasions.
- Pulmonary artery catheterization and administration of thrombolytic agents may be important in patients with massive pulmonary embolism.
- Vena cava interruption may be necessary when anticoagulant therapy does not prevent rethrombosis and the formation of emboli from the lower extremities or pelvis. A vena cava umbrella or filter may be inserted percutaneously above the level of the thrombosis and caudad to the renal veins.
Take-home points
- Identify risk factors preoperatively
- VTE prophylaxis is warranted for most gynecologic surgery patients and can reduce the incidence of VTE by at least 60% with appropriate use! Plan prophylaxis in women at moderate, high, and highest risk, and remember that individuals at high and highest risk require more intense prophylaxis to realize a benefit.
- Maintain a high level of suspicion in women with signs and symptoms of DVT or pulmonary embolism in the first postoperative month. It is better to over-evaluate than to miss a potentially fatal complication.
- Treat women with VTE immediately with heparin or LMWH.
1. Jeffcoate TN, Tindall VR. Venous thrombosis and embolism in obstetrics and gynecology. Aust N Z J Obstet Gynecol. 1965;5:119-130.
2. Clarke-Pearson DL, Jelovsek FR, Creasman WT. Thromboembolism complicating surgery for cervical and uterine malignancy: incidence, risk factors, and prophylaxis. Obstet Gynecol. 1983;61:87-94.
3. Clayton JK, Anderson JA, McNicol GP. Preoperative prediction of postoperative deep vein thrombosis. BMJ. 1976;2:910-912.
4. Clarke-Pearson DL, DeLong ER, Synan IS, Coleman RE, Creasman WT. Variables associated with postoperative deep venous thrombosis: a prospective study of 411 gynecology patients and creation of a prognostic model. Obstet Gynecol. 1987;69:146-150.
5. Prevention of fatal postoperative pulmonary embolism by low-dose heparin. An international multicentre trial. Lancet. 1975;2:45-51.
6. Clarke-Pearson DL, DeLong ER, Synan IS, Creasman WT. Complications of low-dose heparin prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 1984;64:689-694.
7. Tapson VF, Hull RD. Management of venous thromboembolic disease. The impact of low-molecular-weight heparin. Clin Chest Med. 1995;16:281-294.
8. Borstad E, Urdal K, Handeland G, Abildgaard U. Comparison of low molecular weight heparin vs. unfractionated heparin in gynecological surgery. II: Reduced dose of low molecular weight heparin. Acta Obstet Gynecol Scand. 1992;71:471-475.
9. Jorgensen LN, Wille-Jorgensen P, Hauch O. Prophylaxis of postoperative thromboembolism with low molecular weight heparins. Br J Surg. 1993;80:689-704.
10. Allenby F, Boardman L, Pflug JJ, Calnan JS. Effects of external pneumatic intermittent compression on fibrinolysis in man. Lancet. 1973;2:1412-1414.
11. Salzman EW, Ploetz J, Bettmann M, Skillman J, Klein L. Intraoperative external pneumatic calf compression to afford long-term prophylaxis against deep vein thrombosis in urological patients. Surgery. 1980;87:239-242.
12. Nicolaides AN, Fernandes e Fernandes J, Pollock AV. Intermittent sequential pneumatic compression of the legs in the prevention of venous stasis and postoperative deep venous thrombosis. Surgery. 1980;87:69-76.
13. Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol. 1984;63:92-98.
14. Clarke-Pearson DL, Creasman WT, Coleman RE, Synan IS, Hinshaw WM. Perioperative external pneumatic calf compression as thromboembolism prophylaxis in gynecologic oncology: report of a randomized controlled trial. Gynecol Oncol. 1984;18:226-232.
15. Maxwell GL, Myers ER, Clarke-Pearson DL. Cost-effectiveness of deep venous thrombosis prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 2000;95:206-214.
16. Scurr JH, Ibrahim SZ, Faber RG, Le Quesne LP. The efficacy of graduated compression stockings in the prevention of deep vein thrombosis. Br J Surg. 1977;64:371-373.
17. Wells PS, Owen C, Doucette S, et al. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
18. Writing Group for the Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical D-dimer testing and computed tomography. JAMA. 2006;295:172-179.
19. Buller HR, Kucher N, Kipfmueller F, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:401S-428S.
20. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(suppl):338S-400S.
The author reports no financial relationships relevant to this article.
Pulmonary embolism is a master of disguises. It can appear with classic symptoms such as pleuritic chest pain, hemoptysis, and tachycardia—or it can arrive more insidiously, apparent only as a slight elevation in the respiratory rate.
This matters because 40% of all deaths following gynecologic surgery are directly attributable to pulmonary emboli,1 and pulmonary emboli are the most frequent cause of postoperative death in women with uterine or cervical carcinoma.2
Deep venous thrombosis (DVT) is almost as evasive. We know the signs and symptoms of DVT of the lower extremities—pain, edema, erythema, and a prominent vascular pattern of the superficial veins—but 50% to 80% of patients with these symptoms do not have DVT, and 80% of patients with symptomatic pulmonary embolism have no antecedent signs of thrombosis in the lower extremities.2 Morbidity and expense rise dramatically with DVT, especially when postphlebitic syndrome occurs.
How can we minimize these risks?
A good outcome is most likely when we:
- recognize risk factors,
- provide appropriate perioperative prophylaxis, and
- diagnose and treat venous thromboembolism (VTE) quickly.
This article looks in detail at each of these strategies.
3 factors set the stage for thrombogenesis
- Hypercoagulable state
- Venous stasis
- Vessel endothelial injury
These factors, known as Virchow’s triad, are especially likely at the time of major surgery, or when the patient is advanced in age or has a history of DVT, cancer, lower extremity edema, or venous stasis.
Intraoperative risk factors for postoperative DVT include increased anesthesia time, greater blood loss, and need for transfusion.
Some preventive methods come close to ideal
Being aware of risk factors is vital to provide the appropriate level of prophylaxis (TABLES 1 AND 2).3,4 The first step is identifying high-risk patients and tailoring the regimen to meet their individual needs. The perfect prophylactic method is not yet devised, but would be effective, free of significant side effects, well accepted by the patient and nursing staff, widely applicable to most patient groups, and inexpensive. A number of methods come close.
TABLE 1
Risk factors for thromboembolism
| Major gynecologic surgery |
| Age >40 years |
| Malignancy |
| Previous venous thrombosis (DVT or pulmonary embolism) |
| Obesity |
| Immobility |
| Pregnancy and the postpartum period |
| Oral contraceptives, hormone therapy, or tamoxifen |
| Varicose veins |
| Inherited or acquired thrombophilia (eg, Factor V Leiden) |
| Prolonged surgical procedure |
| Radical vulvectomy, inguinal-femoral lymphadenectomy, or pelvic exenteration |
TABLE 2
Match the preventive strategy to the surgery
| SURGERY | STRATEGY | DURATION OF PROPHYLAXIS* |
|---|---|---|
| Procedures <30 min for benign disease | Prophylaxis not needed | — |
| Laparoscopic gynecologic procedures in women with additional risk factors | Unfractionated heparin, 5,000 bid or | Until hospital discharge |
| LMWH, ≤3,400 U/day or | ||
| External pneumatic compression or | ||
| Graduated compression stockings | ||
| Major surgery for benign disease without additional risk factors | Unfractionated heparin, 5,000 U bid or | Until hospital discharge |
| LMWH, <3,400 U/day or | ||
| External pneumatic compression | ||
| Extensive major surgery in women with cancer or additional risk factors | Unfractionated heparin, 5,000 U tid or | Until hospital discharge |
| LMWH, >3,400 U/day or | ||
| External pneumatic compression | ||
| *For women at particularly high risk (eg, cancer surgery, age >60 years, prior VTE), continue prophylaxis for 2–4 weeks after hospital discharge. | ||
| Modified from Geerts WH, et al20 | ||
Low-dose unfractionated heparin
The most extensively studied prophylactic method is the use of small, subcutaneous doses of heparin. More than 25 controlled trials have shown that, when heparin is given subcutaneously 2 hours before surgery and every 8 to 12 hours afterward, the incidence of DVT diminishes substantially.
The value of low-dose heparin in preventing pulmonary emboli was established by a randomized, controlled, multicenter, international trial, in which fatal postoperative pulmonary emboli declined significantly in general surgery patients given the drug every 8 hours after surgery.5 In gynecologic surgical patients, postoperative DVT also declined significantly.
Increase in minor bleeding complications. Although low-dose heparin is thought to have no measurable effect on coagulation, most large series have noted an increase in minor bleeding complications such as wound hematoma. Up to 10% to 15% of otherwise healthy patients develop transiently prolonged activated partial thromboplastin time (APTT) after 5,000 U of heparin are given subcutaneously.6
Although relatively rare, thrombocytopenia is associated with the use of low-dose heparin. It has been found in 6% of women after gynecologic surgery.6 Therefore, it is reasonable to measure platelets in any patient taking low-dose heparin longer than 4 days to screen for heparin-induced thrombocytopenia.
Fear of major bleeding complications is unsubstantiated. There is ample evidence from placebo-controlled, blinded trials and meta-analysis that the risk of clinically important bleeding does not increase. Moreover, detailed analysis demonstrates that low-dose heparin has a good risk-to-benefit ratio and is cost-effective.
Low-molecular-weight heparins
These drugs are fragments of unfractionated heparin that vary in size from 4,500 to 6,500 daltons. Low-molecular-weight heparin (LMWH) has more anti-Xa and less antithrombin activity than unfractionated heparin and thus has less of an effect on partial thromboplastin time. LMWH may also lead to fewer bleeding complications.7
Once-daily dosing is possible. An increased half-life of 4 hours for LMWH produces greater bioavailability than with low-dose heparin. This allows once-daily dosing.
Pick one: Convenience or cost
Randomized controlled trials have compared LMWH to unfractionated heparin in gynecologic surgical patients. In all studies, DVT occurred in similar, low numbers of women regardless of the heparin used. Bleeding complications also were similar.8
A meta-analysis of general surgery and gynecologic surgery patients from 32 trials likewise found daily LMWH to be as effective as unfractionated heparin in DVT prophylaxis, without any difference in hemorrhagic complications.9
The choice of drugs often boils down to convenience versus cost: Prophylactic LMWH can be given once a day (compared with 2 or 3 times for unfractionated heparin), but is much more expensive.
Mechanical prophylactic methods
External pneumatic compression rivals low-dose heparin. The largest body of literature on mechanical methods to reduce postoperative venous stasis involves intermittent leg compression by pneumatically inflated sleeves placed around the calf or leg during surgery and after. A number of devices and sleeve designs are available, none of which has proven to be superior to the others.
In my experience, calf compression during and after gynecologic surgery lowers the incidence of DVT to a level seen with low-dose heparin. Besides increasing venous flow and pulsatile emptying of the calf veins, pneumatic compression appears to augment endogenous fibrinolysis, which may stimulate lysis of very early thrombi.10
How long is best for external compression? The optimal duration of postoperative external pneumatic compression is unclear. It may be effective when used in the operating room and for the first 24 hours postoperatively in patients with benign conditions who will ambulate on the first day after surgery.11,12
In women undergoing major surgery for gynecologic malignancy, it reduces the incidence of postoperative venous thromboemboli by nearly 3-fold, but only if calf compression is applied intraoperatively and for the first 5 postoperative days.13,14 These women may remain at risk because of stasis and a hypercoagulable state for a longer time than general surgical patients.
External pneumatic leg compression has no serious side effects or risks and is slightly more cost-effective than prophylactic drugs.15 However, to be fully effective, this method must be used consistently, in compliance with the protocol, when the patient is not ambulating.
Stockings can be a help or hazard. Controlled studies of graduated pressure stockings are limited but suggest modest benefit with careful fitting.16 Poorly fitted stockings that roll down the leg may create a tourniquet effect at the knee or mid-thigh. Another disadvantage of the stockings: The limited sizes available do not allow a perfect fit for all patients. This is especially true in obese patients.
The simplicity of elastic stockings and the absence of serious side effects are probably why stockings are often included in routine postoperative care.
Don’t overlook basic precautions. Although they may offer only modest benefit, short preoperative hospital stays and early postoperative ambulation are recommended.
Another basic strategy: elevating the foot of the bed to raise the calf above heart level. This allows gravity to drain the calf veins and should further reduce stasis.
How to detect VTE
DVT has nonspecific signs and symptoms
When DVT occurs in the lower extremities, harbingers such as pain, edema, and erythema are relatively nonspecific; 50% to 80% of patients exhibiting them do not have DVT. Conversely, approximately 80% of patients with symptomatic pulmonary emboli have no signs or symptoms of thrombosis in the lower extremities.
Because of this lack of specificity, additional tests are needed to establish DVT.
Diagnostic studies
A definitive diagnosis of DVT and pulmonary embolism is mandatory because diagnosis based on clinical symptoms and signs alone is frequently wrong. Strategies to reduce the use of ultrasound or spiral CT scanning have been put forward. These studies have evaluated outpatients using algorithms that utilize clinical probability (“clinical decision rule”) and D-dimer levels.
This strategy has been very accurate and avoids the use of ultrasound or spiral CT in low-risk patients. For example, individuals with a low probability score have an incidence of DVT below 5%, so ultrasound is unnecessary. This diagnostic strategy relies on the recognition of elevated D-dimer levels. Unfortunately, D-dimer is increased by a variety of nonthrombotic disorders, including recent surgery, hemorrhage, trauma, pregnancy, and cancer. Therefore, we cannot recommend the use of this strategy for the postoperative gynecologic surgery patient.17,18
Venography no longer the gold standard. Other diagnostic studies may be more useful. Venography has fallen from favor because it is moderately uncomfortable, requires injection of a contrast material that may trigger an allergic reaction or renal injury, and causes phlebitis in approximately 5% of patients.2 Newer, noninvasive diagnostic tests have been developed, fortunately.
Doppler ultrasound. B-mode duplex Doppler imaging is the most common technique to diagnose symptomatic venous thrombosis, especially when it arises in the proximal lower extremity. With duplex Doppler imaging, the femoral vein can be visualized, and clots may be seen directly. Compression of the vein with the tip of the ultrasound probe makes it possible to assess venous collapsibility, which is diminished when a thrombus is present.
Doppler imaging is less accurate when evaluating the calf and pelvic veins.
Magnetic resonance venography (MRV) sensitivity and specificity are comparable to venography. In addition, MRV may detect thrombi in pelvic veins that are not imaged by venography. The primary drawback is the time required to examine the lower extremity and pelvis. Further, MRV rarely identifies calf thrombi (most often not life-threatening, but potentially symptomatic) and is considerably more expensive than ultrasound.
Which prevention strategy works best?
We now consider low-molecular-weight heparin and external pneumatic compression the best choices
Because low-dose unfractionated heparin, low-molecular-weight heparin (LMWH), and external pneumatic compression all reduce the incidence of postoperative venous thromboembolism in high-risk gynecologic surgical patients, the question is: Which strategy is best?
We conducted 2 randomized clinical trials to answer this question.
Trial 1 Low-dose heparin vs pneumatic compression
Women were randomized to receive either low-dose heparin (5,000 U subcutaneously preoperatively and every 8 hours after surgery until hospital discharge) or external pneumatic compression of the calf prior to surgery and until hospital discharge.1
The incidence of DVT was identical in both groups, and no patients developed a pulmonary embolus throughout 30 days of follow-up. However, bleeding complications occurred more often in the group randomized to low-dose heparin. Specifically, nearly 25% had APTT levels in the “therapeutic” range, and significantly more patients required blood transfusions. After this trial, our institution decided to use external pneumatic compression because of its more favorable risk profile.1
Trial 2 LMWH vs pneumatic compression
The question of the best therapy arose again with the advent of LMWH, because of the possibility that these drugs carried a lower risk of bleeding complications. We therefore conducted a second trial to compare LMWH with external pneumatic compression.2
Because higher doses of LMWH had already proven to be more effective in cancer patients, we gave women in the trial 5,000 U dalteparin (Fragmin) preoperatively and 5,000 U daily postoperatively until hospital discharge.
In this trial, external pneumatic compression and LMWH produced similar low frequencies of DVT and no pulmonary emboli throughout 30 days of follow-up. We also found no association between LMWH and bleeding complications or transfusion requirements. Compliance and patient satisfaction were similar for both modalities.2
Bottom line
We now consider LMWH and external pneumatic compression the best choices for prophylaxis in gynecologic surgical patients.
REFERENCES
1. Clarke-Pearson DL, Synan IS, Dodge R, Soper JT, Berchuck A, Coleman RE. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol. 1993;168:1146-1154.
2. Maxwell GL, Synan I, Dodge R, Carroll B, Clarke-Pearson DI. Pneumatic compression versus low molecular weight heparin in gynecologic oncology surgery: a randomized trial. Obstet Gynecol. 2001;98:989-995.
Increasing use of laparoscopic surgery raises an important question: What is the thromboembolic risk of laparoscopy itself? On one hand, many laparoscopic surgeries are prolonged, and intraperitoneal pressure from the pneumoperitoneum reduces venous flow. On the other hand, many patients who have laparoscopy have shorter hospital stays and return sooner to normal activities than those who have open procedures.
Although the risks of venous thromboembolism (VTE) have not been studied as thoroughly as other aspects of laparoscopy, they appear to be low. To date, there are no randomized trials of VTE prophylaxis among women undergoing gynecologic laparoscopy.
The prudent course
Nevertheless, it would seem prudent to consider prophylaxis when women with additional risk factors undergo extensive laparoscopic procedures.
Pulmonary embolism is often stealthy
Many of the typical signs and symptoms of pulmonary embolism are associated with other, more common pulmonary complications following surgery. Classic findings that should alert the physician to the possibility of pulmonary embolism include:
- pleuritic chest pain
- hemoptysis
- shortness of breath
- tachycardia
- tachypnea
Often, however, the signs are subtle and may include only persistent tachycardia or a slight elevation in respiration.
When pulmonary embolism is suspected, a chest x-ray, electrocardiography, and arterial blood gas assessment are warranted. Any abnormality justifies further evaluation by ventilation-perfusion lung scan or a spiral computed tomography scan of the chest. Unfortunately, a high percentage of lung scans are interpreted as “indeterminate.” In such cases, careful clinical evaluation and judgment are needed to determine whether pulmonary arteriography is necessary to document or exclude pulmonary embolism.
Immediate, aggressive therapy is crucial
The treatment of postoperative DVT requires immediate anticoagulant therapy using either unfractionated heparin or LMWH, followed by 6 months of oral anticoagulant therapy with warfarin.
Treatment strategy: Unfractionated heparin
Once VTE is diagnosed, start unfractionated heparin to prevent proximal propagation of the thrombus and allow physiologic thrombolytic pathways to dissolve the clot. After an initial IV bolus of 5,000 U, give the patient a continuous infusion of 30,000 U daily, and adjust the dose to maintain APTT levels at a therapeutic level that is 1.5 to 2.5 times the control value.
Subtherapeutic APTT levels in the first 24 hours mean a risk of recurrent thromboembolism 15 times greater than the risk in patients with appropriate levels. Therefore, aggressive management is warranted to achieve prompt anticoagulation.
Start an oral anticoagulant (warfarin) on the first day of heparin infusion, and monitor the international normalized ratio (INR) daily until a therapeutic level is achieved. The change in the INR after warfarin administration often precedes the anticoagulant effect by about 2 days, during which time low protein C levels are associated with a transient hypercoagulable state. Therefore, it is important to continue the heparin until the INR has been maintained in a therapeutic range for at least 2 days to confirm the proper warfarin dose. Intravenous heparin can be discontinued after 5 days if an adequate INR level has been established.
Alternative strategy: LMWH
A meta-analysis involving more than 1,000 patients from 19 trials suggests that LMWH is more effective, safer, and less costly than unfractionated heparin in preventing recurrent thromboembolism.19 The lower cost derives from the ability to use the drugs in an outpatient setting.
Dosages are unique and weight-adjusted according to each LMWH preparation. Because LMWH has a minimal effect on APTT, serial laboratory monitoring of APTT levels is unnecessary. Nor is monitoring of anti-Xa activity of significant benefit in the dose adjustment of LMWH.
Basic treatment of pulmonary embolism
In most cases, immediate anticoagulant therapy identical to that outlined for DVT is sufficient to prevent repeat thrombosis and embolism and to allow the patient’s endogenous thrombolytic mechanisms to lyse the pulmonary embolus.
Other interventions include:
- Respiratory support, including oxygen, bronchodilators, and intensive care.
- Although massive pulmonary emboli are usually quickly fatal, pulmonary embolectomy has been successful on rare occasions.
- Pulmonary artery catheterization and administration of thrombolytic agents may be important in patients with massive pulmonary embolism.
- Vena cava interruption may be necessary when anticoagulant therapy does not prevent rethrombosis and the formation of emboli from the lower extremities or pelvis. A vena cava umbrella or filter may be inserted percutaneously above the level of the thrombosis and caudad to the renal veins.
Take-home points
- Identify risk factors preoperatively
- VTE prophylaxis is warranted for most gynecologic surgery patients and can reduce the incidence of VTE by at least 60% with appropriate use! Plan prophylaxis in women at moderate, high, and highest risk, and remember that individuals at high and highest risk require more intense prophylaxis to realize a benefit.
- Maintain a high level of suspicion in women with signs and symptoms of DVT or pulmonary embolism in the first postoperative month. It is better to over-evaluate than to miss a potentially fatal complication.
- Treat women with VTE immediately with heparin or LMWH.
Pulmonary embolism is a master of disguises. It can appear with classic symptoms such as pleuritic chest pain, hemoptysis, and tachycardia—or it can arrive more insidiously, apparent only as a slight elevation in the respiratory rate.
This matters because 40% of all deaths following gynecologic surgery are directly attributable to pulmonary emboli,1 and pulmonary emboli are the most frequent cause of postoperative death in women with uterine or cervical carcinoma.2
Deep venous thrombosis (DVT) is almost as evasive. We know the signs and symptoms of DVT of the lower extremities—pain, edema, erythema, and a prominent vascular pattern of the superficial veins—but 50% to 80% of patients with these symptoms do not have DVT, and 80% of patients with symptomatic pulmonary embolism have no antecedent signs of thrombosis in the lower extremities.2 Morbidity and expense rise dramatically with DVT, especially when postphlebitic syndrome occurs.
How can we minimize these risks?
A good outcome is most likely when we:
- recognize risk factors,
- provide appropriate perioperative prophylaxis, and
- diagnose and treat venous thromboembolism (VTE) quickly.
This article looks in detail at each of these strategies.
3 factors set the stage for thrombogenesis
- Hypercoagulable state
- Venous stasis
- Vessel endothelial injury
These factors, known as Virchow’s triad, are especially likely at the time of major surgery, or when the patient is advanced in age or has a history of DVT, cancer, lower extremity edema, or venous stasis.
Intraoperative risk factors for postoperative DVT include increased anesthesia time, greater blood loss, and need for transfusion.
Some preventive methods come close to ideal
Being aware of risk factors is vital to provide the appropriate level of prophylaxis (TABLES 1 AND 2).3,4 The first step is identifying high-risk patients and tailoring the regimen to meet their individual needs. The perfect prophylactic method is not yet devised, but would be effective, free of significant side effects, well accepted by the patient and nursing staff, widely applicable to most patient groups, and inexpensive. A number of methods come close.
TABLE 1
Risk factors for thromboembolism
| Major gynecologic surgery |
| Age >40 years |
| Malignancy |
| Previous venous thrombosis (DVT or pulmonary embolism) |
| Obesity |
| Immobility |
| Pregnancy and the postpartum period |
| Oral contraceptives, hormone therapy, or tamoxifen |
| Varicose veins |
| Inherited or acquired thrombophilia (eg, Factor V Leiden) |
| Prolonged surgical procedure |
| Radical vulvectomy, inguinal-femoral lymphadenectomy, or pelvic exenteration |
TABLE 2
Match the preventive strategy to the surgery
| SURGERY | STRATEGY | DURATION OF PROPHYLAXIS* |
|---|---|---|
| Procedures <30 min for benign disease | Prophylaxis not needed | — |
| Laparoscopic gynecologic procedures in women with additional risk factors | Unfractionated heparin, 5,000 bid or | Until hospital discharge |
| LMWH, ≤3,400 U/day or | ||
| External pneumatic compression or | ||
| Graduated compression stockings | ||
| Major surgery for benign disease without additional risk factors | Unfractionated heparin, 5,000 U bid or | Until hospital discharge |
| LMWH, <3,400 U/day or | ||
| External pneumatic compression | ||
| Extensive major surgery in women with cancer or additional risk factors | Unfractionated heparin, 5,000 U tid or | Until hospital discharge |
| LMWH, >3,400 U/day or | ||
| External pneumatic compression | ||
| *For women at particularly high risk (eg, cancer surgery, age >60 years, prior VTE), continue prophylaxis for 2–4 weeks after hospital discharge. | ||
| Modified from Geerts WH, et al20 | ||
Low-dose unfractionated heparin
The most extensively studied prophylactic method is the use of small, subcutaneous doses of heparin. More than 25 controlled trials have shown that, when heparin is given subcutaneously 2 hours before surgery and every 8 to 12 hours afterward, the incidence of DVT diminishes substantially.
The value of low-dose heparin in preventing pulmonary emboli was established by a randomized, controlled, multicenter, international trial, in which fatal postoperative pulmonary emboli declined significantly in general surgery patients given the drug every 8 hours after surgery.5 In gynecologic surgical patients, postoperative DVT also declined significantly.
Increase in minor bleeding complications. Although low-dose heparin is thought to have no measurable effect on coagulation, most large series have noted an increase in minor bleeding complications such as wound hematoma. Up to 10% to 15% of otherwise healthy patients develop transiently prolonged activated partial thromboplastin time (APTT) after 5,000 U of heparin are given subcutaneously.6
Although relatively rare, thrombocytopenia is associated with the use of low-dose heparin. It has been found in 6% of women after gynecologic surgery.6 Therefore, it is reasonable to measure platelets in any patient taking low-dose heparin longer than 4 days to screen for heparin-induced thrombocytopenia.
Fear of major bleeding complications is unsubstantiated. There is ample evidence from placebo-controlled, blinded trials and meta-analysis that the risk of clinically important bleeding does not increase. Moreover, detailed analysis demonstrates that low-dose heparin has a good risk-to-benefit ratio and is cost-effective.
Low-molecular-weight heparins
These drugs are fragments of unfractionated heparin that vary in size from 4,500 to 6,500 daltons. Low-molecular-weight heparin (LMWH) has more anti-Xa and less antithrombin activity than unfractionated heparin and thus has less of an effect on partial thromboplastin time. LMWH may also lead to fewer bleeding complications.7
Once-daily dosing is possible. An increased half-life of 4 hours for LMWH produces greater bioavailability than with low-dose heparin. This allows once-daily dosing.
Pick one: Convenience or cost
Randomized controlled trials have compared LMWH to unfractionated heparin in gynecologic surgical patients. In all studies, DVT occurred in similar, low numbers of women regardless of the heparin used. Bleeding complications also were similar.8
A meta-analysis of general surgery and gynecologic surgery patients from 32 trials likewise found daily LMWH to be as effective as unfractionated heparin in DVT prophylaxis, without any difference in hemorrhagic complications.9
The choice of drugs often boils down to convenience versus cost: Prophylactic LMWH can be given once a day (compared with 2 or 3 times for unfractionated heparin), but is much more expensive.
Mechanical prophylactic methods
External pneumatic compression rivals low-dose heparin. The largest body of literature on mechanical methods to reduce postoperative venous stasis involves intermittent leg compression by pneumatically inflated sleeves placed around the calf or leg during surgery and after. A number of devices and sleeve designs are available, none of which has proven to be superior to the others.
In my experience, calf compression during and after gynecologic surgery lowers the incidence of DVT to a level seen with low-dose heparin. Besides increasing venous flow and pulsatile emptying of the calf veins, pneumatic compression appears to augment endogenous fibrinolysis, which may stimulate lysis of very early thrombi.10
How long is best for external compression? The optimal duration of postoperative external pneumatic compression is unclear. It may be effective when used in the operating room and for the first 24 hours postoperatively in patients with benign conditions who will ambulate on the first day after surgery.11,12
In women undergoing major surgery for gynecologic malignancy, it reduces the incidence of postoperative venous thromboemboli by nearly 3-fold, but only if calf compression is applied intraoperatively and for the first 5 postoperative days.13,14 These women may remain at risk because of stasis and a hypercoagulable state for a longer time than general surgical patients.
External pneumatic leg compression has no serious side effects or risks and is slightly more cost-effective than prophylactic drugs.15 However, to be fully effective, this method must be used consistently, in compliance with the protocol, when the patient is not ambulating.
Stockings can be a help or hazard. Controlled studies of graduated pressure stockings are limited but suggest modest benefit with careful fitting.16 Poorly fitted stockings that roll down the leg may create a tourniquet effect at the knee or mid-thigh. Another disadvantage of the stockings: The limited sizes available do not allow a perfect fit for all patients. This is especially true in obese patients.
The simplicity of elastic stockings and the absence of serious side effects are probably why stockings are often included in routine postoperative care.
Don’t overlook basic precautions. Although they may offer only modest benefit, short preoperative hospital stays and early postoperative ambulation are recommended.
Another basic strategy: elevating the foot of the bed to raise the calf above heart level. This allows gravity to drain the calf veins and should further reduce stasis.
How to detect VTE
DVT has nonspecific signs and symptoms
When DVT occurs in the lower extremities, harbingers such as pain, edema, and erythema are relatively nonspecific; 50% to 80% of patients exhibiting them do not have DVT. Conversely, approximately 80% of patients with symptomatic pulmonary emboli have no signs or symptoms of thrombosis in the lower extremities.
Because of this lack of specificity, additional tests are needed to establish DVT.
Diagnostic studies
A definitive diagnosis of DVT and pulmonary embolism is mandatory because diagnosis based on clinical symptoms and signs alone is frequently wrong. Strategies to reduce the use of ultrasound or spiral CT scanning have been put forward. These studies have evaluated outpatients using algorithms that utilize clinical probability (“clinical decision rule”) and D-dimer levels.
This strategy has been very accurate and avoids the use of ultrasound or spiral CT in low-risk patients. For example, individuals with a low probability score have an incidence of DVT below 5%, so ultrasound is unnecessary. This diagnostic strategy relies on the recognition of elevated D-dimer levels. Unfortunately, D-dimer is increased by a variety of nonthrombotic disorders, including recent surgery, hemorrhage, trauma, pregnancy, and cancer. Therefore, we cannot recommend the use of this strategy for the postoperative gynecologic surgery patient.17,18
Venography no longer the gold standard. Other diagnostic studies may be more useful. Venography has fallen from favor because it is moderately uncomfortable, requires injection of a contrast material that may trigger an allergic reaction or renal injury, and causes phlebitis in approximately 5% of patients.2 Newer, noninvasive diagnostic tests have been developed, fortunately.
Doppler ultrasound. B-mode duplex Doppler imaging is the most common technique to diagnose symptomatic venous thrombosis, especially when it arises in the proximal lower extremity. With duplex Doppler imaging, the femoral vein can be visualized, and clots may be seen directly. Compression of the vein with the tip of the ultrasound probe makes it possible to assess venous collapsibility, which is diminished when a thrombus is present.
Doppler imaging is less accurate when evaluating the calf and pelvic veins.
Magnetic resonance venography (MRV) sensitivity and specificity are comparable to venography. In addition, MRV may detect thrombi in pelvic veins that are not imaged by venography. The primary drawback is the time required to examine the lower extremity and pelvis. Further, MRV rarely identifies calf thrombi (most often not life-threatening, but potentially symptomatic) and is considerably more expensive than ultrasound.
Which prevention strategy works best?
We now consider low-molecular-weight heparin and external pneumatic compression the best choices
Because low-dose unfractionated heparin, low-molecular-weight heparin (LMWH), and external pneumatic compression all reduce the incidence of postoperative venous thromboembolism in high-risk gynecologic surgical patients, the question is: Which strategy is best?
We conducted 2 randomized clinical trials to answer this question.
Trial 1 Low-dose heparin vs pneumatic compression
Women were randomized to receive either low-dose heparin (5,000 U subcutaneously preoperatively and every 8 hours after surgery until hospital discharge) or external pneumatic compression of the calf prior to surgery and until hospital discharge.1
The incidence of DVT was identical in both groups, and no patients developed a pulmonary embolus throughout 30 days of follow-up. However, bleeding complications occurred more often in the group randomized to low-dose heparin. Specifically, nearly 25% had APTT levels in the “therapeutic” range, and significantly more patients required blood transfusions. After this trial, our institution decided to use external pneumatic compression because of its more favorable risk profile.1
Trial 2 LMWH vs pneumatic compression
The question of the best therapy arose again with the advent of LMWH, because of the possibility that these drugs carried a lower risk of bleeding complications. We therefore conducted a second trial to compare LMWH with external pneumatic compression.2
Because higher doses of LMWH had already proven to be more effective in cancer patients, we gave women in the trial 5,000 U dalteparin (Fragmin) preoperatively and 5,000 U daily postoperatively until hospital discharge.
In this trial, external pneumatic compression and LMWH produced similar low frequencies of DVT and no pulmonary emboli throughout 30 days of follow-up. We also found no association between LMWH and bleeding complications or transfusion requirements. Compliance and patient satisfaction were similar for both modalities.2
Bottom line
We now consider LMWH and external pneumatic compression the best choices for prophylaxis in gynecologic surgical patients.
REFERENCES
1. Clarke-Pearson DL, Synan IS, Dodge R, Soper JT, Berchuck A, Coleman RE. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol. 1993;168:1146-1154.
2. Maxwell GL, Synan I, Dodge R, Carroll B, Clarke-Pearson DI. Pneumatic compression versus low molecular weight heparin in gynecologic oncology surgery: a randomized trial. Obstet Gynecol. 2001;98:989-995.
Increasing use of laparoscopic surgery raises an important question: What is the thromboembolic risk of laparoscopy itself? On one hand, many laparoscopic surgeries are prolonged, and intraperitoneal pressure from the pneumoperitoneum reduces venous flow. On the other hand, many patients who have laparoscopy have shorter hospital stays and return sooner to normal activities than those who have open procedures.
Although the risks of venous thromboembolism (VTE) have not been studied as thoroughly as other aspects of laparoscopy, they appear to be low. To date, there are no randomized trials of VTE prophylaxis among women undergoing gynecologic laparoscopy.
The prudent course
Nevertheless, it would seem prudent to consider prophylaxis when women with additional risk factors undergo extensive laparoscopic procedures.
Pulmonary embolism is often stealthy
Many of the typical signs and symptoms of pulmonary embolism are associated with other, more common pulmonary complications following surgery. Classic findings that should alert the physician to the possibility of pulmonary embolism include:
- pleuritic chest pain
- hemoptysis
- shortness of breath
- tachycardia
- tachypnea
Often, however, the signs are subtle and may include only persistent tachycardia or a slight elevation in respiration.
When pulmonary embolism is suspected, a chest x-ray, electrocardiography, and arterial blood gas assessment are warranted. Any abnormality justifies further evaluation by ventilation-perfusion lung scan or a spiral computed tomography scan of the chest. Unfortunately, a high percentage of lung scans are interpreted as “indeterminate.” In such cases, careful clinical evaluation and judgment are needed to determine whether pulmonary arteriography is necessary to document or exclude pulmonary embolism.
Immediate, aggressive therapy is crucial
The treatment of postoperative DVT requires immediate anticoagulant therapy using either unfractionated heparin or LMWH, followed by 6 months of oral anticoagulant therapy with warfarin.
Treatment strategy: Unfractionated heparin
Once VTE is diagnosed, start unfractionated heparin to prevent proximal propagation of the thrombus and allow physiologic thrombolytic pathways to dissolve the clot. After an initial IV bolus of 5,000 U, give the patient a continuous infusion of 30,000 U daily, and adjust the dose to maintain APTT levels at a therapeutic level that is 1.5 to 2.5 times the control value.
Subtherapeutic APTT levels in the first 24 hours mean a risk of recurrent thromboembolism 15 times greater than the risk in patients with appropriate levels. Therefore, aggressive management is warranted to achieve prompt anticoagulation.
Start an oral anticoagulant (warfarin) on the first day of heparin infusion, and monitor the international normalized ratio (INR) daily until a therapeutic level is achieved. The change in the INR after warfarin administration often precedes the anticoagulant effect by about 2 days, during which time low protein C levels are associated with a transient hypercoagulable state. Therefore, it is important to continue the heparin until the INR has been maintained in a therapeutic range for at least 2 days to confirm the proper warfarin dose. Intravenous heparin can be discontinued after 5 days if an adequate INR level has been established.
Alternative strategy: LMWH
A meta-analysis involving more than 1,000 patients from 19 trials suggests that LMWH is more effective, safer, and less costly than unfractionated heparin in preventing recurrent thromboembolism.19 The lower cost derives from the ability to use the drugs in an outpatient setting.
Dosages are unique and weight-adjusted according to each LMWH preparation. Because LMWH has a minimal effect on APTT, serial laboratory monitoring of APTT levels is unnecessary. Nor is monitoring of anti-Xa activity of significant benefit in the dose adjustment of LMWH.
Basic treatment of pulmonary embolism
In most cases, immediate anticoagulant therapy identical to that outlined for DVT is sufficient to prevent repeat thrombosis and embolism and to allow the patient’s endogenous thrombolytic mechanisms to lyse the pulmonary embolus.
Other interventions include:
- Respiratory support, including oxygen, bronchodilators, and intensive care.
- Although massive pulmonary emboli are usually quickly fatal, pulmonary embolectomy has been successful on rare occasions.
- Pulmonary artery catheterization and administration of thrombolytic agents may be important in patients with massive pulmonary embolism.
- Vena cava interruption may be necessary when anticoagulant therapy does not prevent rethrombosis and the formation of emboli from the lower extremities or pelvis. A vena cava umbrella or filter may be inserted percutaneously above the level of the thrombosis and caudad to the renal veins.
Take-home points
- Identify risk factors preoperatively
- VTE prophylaxis is warranted for most gynecologic surgery patients and can reduce the incidence of VTE by at least 60% with appropriate use! Plan prophylaxis in women at moderate, high, and highest risk, and remember that individuals at high and highest risk require more intense prophylaxis to realize a benefit.
- Maintain a high level of suspicion in women with signs and symptoms of DVT or pulmonary embolism in the first postoperative month. It is better to over-evaluate than to miss a potentially fatal complication.
- Treat women with VTE immediately with heparin or LMWH.
1. Jeffcoate TN, Tindall VR. Venous thrombosis and embolism in obstetrics and gynecology. Aust N Z J Obstet Gynecol. 1965;5:119-130.
2. Clarke-Pearson DL, Jelovsek FR, Creasman WT. Thromboembolism complicating surgery for cervical and uterine malignancy: incidence, risk factors, and prophylaxis. Obstet Gynecol. 1983;61:87-94.
3. Clayton JK, Anderson JA, McNicol GP. Preoperative prediction of postoperative deep vein thrombosis. BMJ. 1976;2:910-912.
4. Clarke-Pearson DL, DeLong ER, Synan IS, Coleman RE, Creasman WT. Variables associated with postoperative deep venous thrombosis: a prospective study of 411 gynecology patients and creation of a prognostic model. Obstet Gynecol. 1987;69:146-150.
5. Prevention of fatal postoperative pulmonary embolism by low-dose heparin. An international multicentre trial. Lancet. 1975;2:45-51.
6. Clarke-Pearson DL, DeLong ER, Synan IS, Creasman WT. Complications of low-dose heparin prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 1984;64:689-694.
7. Tapson VF, Hull RD. Management of venous thromboembolic disease. The impact of low-molecular-weight heparin. Clin Chest Med. 1995;16:281-294.
8. Borstad E, Urdal K, Handeland G, Abildgaard U. Comparison of low molecular weight heparin vs. unfractionated heparin in gynecological surgery. II: Reduced dose of low molecular weight heparin. Acta Obstet Gynecol Scand. 1992;71:471-475.
9. Jorgensen LN, Wille-Jorgensen P, Hauch O. Prophylaxis of postoperative thromboembolism with low molecular weight heparins. Br J Surg. 1993;80:689-704.
10. Allenby F, Boardman L, Pflug JJ, Calnan JS. Effects of external pneumatic intermittent compression on fibrinolysis in man. Lancet. 1973;2:1412-1414.
11. Salzman EW, Ploetz J, Bettmann M, Skillman J, Klein L. Intraoperative external pneumatic calf compression to afford long-term prophylaxis against deep vein thrombosis in urological patients. Surgery. 1980;87:239-242.
12. Nicolaides AN, Fernandes e Fernandes J, Pollock AV. Intermittent sequential pneumatic compression of the legs in the prevention of venous stasis and postoperative deep venous thrombosis. Surgery. 1980;87:69-76.
13. Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol. 1984;63:92-98.
14. Clarke-Pearson DL, Creasman WT, Coleman RE, Synan IS, Hinshaw WM. Perioperative external pneumatic calf compression as thromboembolism prophylaxis in gynecologic oncology: report of a randomized controlled trial. Gynecol Oncol. 1984;18:226-232.
15. Maxwell GL, Myers ER, Clarke-Pearson DL. Cost-effectiveness of deep venous thrombosis prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 2000;95:206-214.
16. Scurr JH, Ibrahim SZ, Faber RG, Le Quesne LP. The efficacy of graduated compression stockings in the prevention of deep vein thrombosis. Br J Surg. 1977;64:371-373.
17. Wells PS, Owen C, Doucette S, et al. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
18. Writing Group for the Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical D-dimer testing and computed tomography. JAMA. 2006;295:172-179.
19. Buller HR, Kucher N, Kipfmueller F, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:401S-428S.
20. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(suppl):338S-400S.
The author reports no financial relationships relevant to this article.
1. Jeffcoate TN, Tindall VR. Venous thrombosis and embolism in obstetrics and gynecology. Aust N Z J Obstet Gynecol. 1965;5:119-130.
2. Clarke-Pearson DL, Jelovsek FR, Creasman WT. Thromboembolism complicating surgery for cervical and uterine malignancy: incidence, risk factors, and prophylaxis. Obstet Gynecol. 1983;61:87-94.
3. Clayton JK, Anderson JA, McNicol GP. Preoperative prediction of postoperative deep vein thrombosis. BMJ. 1976;2:910-912.
4. Clarke-Pearson DL, DeLong ER, Synan IS, Coleman RE, Creasman WT. Variables associated with postoperative deep venous thrombosis: a prospective study of 411 gynecology patients and creation of a prognostic model. Obstet Gynecol. 1987;69:146-150.
5. Prevention of fatal postoperative pulmonary embolism by low-dose heparin. An international multicentre trial. Lancet. 1975;2:45-51.
6. Clarke-Pearson DL, DeLong ER, Synan IS, Creasman WT. Complications of low-dose heparin prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 1984;64:689-694.
7. Tapson VF, Hull RD. Management of venous thromboembolic disease. The impact of low-molecular-weight heparin. Clin Chest Med. 1995;16:281-294.
8. Borstad E, Urdal K, Handeland G, Abildgaard U. Comparison of low molecular weight heparin vs. unfractionated heparin in gynecological surgery. II: Reduced dose of low molecular weight heparin. Acta Obstet Gynecol Scand. 1992;71:471-475.
9. Jorgensen LN, Wille-Jorgensen P, Hauch O. Prophylaxis of postoperative thromboembolism with low molecular weight heparins. Br J Surg. 1993;80:689-704.
10. Allenby F, Boardman L, Pflug JJ, Calnan JS. Effects of external pneumatic intermittent compression on fibrinolysis in man. Lancet. 1973;2:1412-1414.
11. Salzman EW, Ploetz J, Bettmann M, Skillman J, Klein L. Intraoperative external pneumatic calf compression to afford long-term prophylaxis against deep vein thrombosis in urological patients. Surgery. 1980;87:239-242.
12. Nicolaides AN, Fernandes e Fernandes J, Pollock AV. Intermittent sequential pneumatic compression of the legs in the prevention of venous stasis and postoperative deep venous thrombosis. Surgery. 1980;87:69-76.
13. Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol. 1984;63:92-98.
14. Clarke-Pearson DL, Creasman WT, Coleman RE, Synan IS, Hinshaw WM. Perioperative external pneumatic calf compression as thromboembolism prophylaxis in gynecologic oncology: report of a randomized controlled trial. Gynecol Oncol. 1984;18:226-232.
15. Maxwell GL, Myers ER, Clarke-Pearson DL. Cost-effectiveness of deep venous thrombosis prophylaxis in gynecologic oncology surgery. Obstet Gynecol. 2000;95:206-214.
16. Scurr JH, Ibrahim SZ, Faber RG, Le Quesne LP. The efficacy of graduated compression stockings in the prevention of deep vein thrombosis. Br J Surg. 1977;64:371-373.
17. Wells PS, Owen C, Doucette S, et al. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
18. Writing Group for the Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical D-dimer testing and computed tomography. JAMA. 2006;295:172-179.
19. Buller HR, Kucher N, Kipfmueller F, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:401S-428S.
20. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(suppl):338S-400S.
The author reports no financial relationships relevant to this article.