User login
Sen. Manchin urges withdrawal of Zohydro approval
Sen. Joe Manchin (D-W.Va.) is urging the Department of Health and Human Services to overturn the Food and Drug Administration’s approval of extended-release hydrocodone bitartrate (Zohydro ER), calling the drug "a powerful and dangerous opioid drug product with a high potential for abuse."
In a March 10 letter to HHS Secretary Kathleen Sebelius, Sen. Manchin noted that the FDA approved the drug "despite strong opposition from its own Anesthetic and Analgesic Drug Products Advisory Committee."
The drug is expected to come on the market in March.
"Simply put, the FDA’s approval of Zohydro ER, in its current form, must be stopped before this dangerous drug is sold to the public," Sen. Manchin wrote. Zohydro ER "has up to 10 times as much hydrocodone as Vicodin and Lortab and will come in a formulation that can be easily crushed, snorted, and injected."
In his letter, Manchin raised questions about the drug’s approval. "I am deeply troubled that the reason for Zohydro ER’s approval may be linked to allegations that the FDA gave manufacturers of prescription drugs the opportunity to pay thousands of dollars for the privilege to attend private meetings with FDA officials," he wrote, citing news reports. "Allegations have been raised that a new, scientifically questionable methodology for drug approval was created at these pay-to-play meetings."
The FDA has denied any improprieties regarding those private meetings, which the agency has said were intended to help the FDA better evaluate evidence from clinical trials.
The senator’s letter follows similar efforts of 28 state attorneys general and 8 members of Congress. All voiced concern that the drug could lead to additional overdoses.
Zogenix, which makes the drug, notes the risks of "addiction, abuse, and misuse" in the labeling for hydrocodone bitartrate.
Sen. Joe Manchin (D-W.Va.) is urging the Department of Health and Human Services to overturn the Food and Drug Administration’s approval of extended-release hydrocodone bitartrate (Zohydro ER), calling the drug "a powerful and dangerous opioid drug product with a high potential for abuse."
In a March 10 letter to HHS Secretary Kathleen Sebelius, Sen. Manchin noted that the FDA approved the drug "despite strong opposition from its own Anesthetic and Analgesic Drug Products Advisory Committee."
The drug is expected to come on the market in March.
"Simply put, the FDA’s approval of Zohydro ER, in its current form, must be stopped before this dangerous drug is sold to the public," Sen. Manchin wrote. Zohydro ER "has up to 10 times as much hydrocodone as Vicodin and Lortab and will come in a formulation that can be easily crushed, snorted, and injected."
In his letter, Manchin raised questions about the drug’s approval. "I am deeply troubled that the reason for Zohydro ER’s approval may be linked to allegations that the FDA gave manufacturers of prescription drugs the opportunity to pay thousands of dollars for the privilege to attend private meetings with FDA officials," he wrote, citing news reports. "Allegations have been raised that a new, scientifically questionable methodology for drug approval was created at these pay-to-play meetings."
The FDA has denied any improprieties regarding those private meetings, which the agency has said were intended to help the FDA better evaluate evidence from clinical trials.
The senator’s letter follows similar efforts of 28 state attorneys general and 8 members of Congress. All voiced concern that the drug could lead to additional overdoses.
Zogenix, which makes the drug, notes the risks of "addiction, abuse, and misuse" in the labeling for hydrocodone bitartrate.
Sen. Joe Manchin (D-W.Va.) is urging the Department of Health and Human Services to overturn the Food and Drug Administration’s approval of extended-release hydrocodone bitartrate (Zohydro ER), calling the drug "a powerful and dangerous opioid drug product with a high potential for abuse."
In a March 10 letter to HHS Secretary Kathleen Sebelius, Sen. Manchin noted that the FDA approved the drug "despite strong opposition from its own Anesthetic and Analgesic Drug Products Advisory Committee."
The drug is expected to come on the market in March.
"Simply put, the FDA’s approval of Zohydro ER, in its current form, must be stopped before this dangerous drug is sold to the public," Sen. Manchin wrote. Zohydro ER "has up to 10 times as much hydrocodone as Vicodin and Lortab and will come in a formulation that can be easily crushed, snorted, and injected."
In his letter, Manchin raised questions about the drug’s approval. "I am deeply troubled that the reason for Zohydro ER’s approval may be linked to allegations that the FDA gave manufacturers of prescription drugs the opportunity to pay thousands of dollars for the privilege to attend private meetings with FDA officials," he wrote, citing news reports. "Allegations have been raised that a new, scientifically questionable methodology for drug approval was created at these pay-to-play meetings."
The FDA has denied any improprieties regarding those private meetings, which the agency has said were intended to help the FDA better evaluate evidence from clinical trials.
The senator’s letter follows similar efforts of 28 state attorneys general and 8 members of Congress. All voiced concern that the drug could lead to additional overdoses.
Zogenix, which makes the drug, notes the risks of "addiction, abuse, and misuse" in the labeling for hydrocodone bitartrate.
Panel calls new hepatitis C drug ‘low value’
A panel of California medical experts says two new, once-daily drugs for hepatitis C represent low-value treatment alternatives for the condition because of their high price tags.
The drugs, Gilead Sciences’ sofosbuvir (Sovaldi) and Johnson & Johnson’s simeprevir (Olysio), cost more than $1,000 per pill, pushing the price for the recommended 12-week course of treatment of sofosbuvir to close to $90,000 and treatment with simeprevir to around $66,000, according to the California Technology Assessment Forum (CTAF), an independent group originally convened by the insurance industry to evaluate costs and benefits of treatments.
The Food and Drug Administration approved sofosbuvir and simeprevir late last year. CTAF, which met March 10 to consider the financial and clinical effects of the two new drugs, will issue its final report on the treatments in April.
The group acknowledged in its draft report that therapeutic regimens containing sofosbuvir, approved to treat hepatitis C genotypes 1 through 4, have the potential to "substantially increase" the number of patients achieving sustained virologic response. The drug also offers "the first effective interferon-free option" to patients who can’t take interferon.
"These advantages are considerable," the report said. However, it added, "the clinical advantages of newer treatment regimens would ... come with a substantial potential impact on health care budgets should a large number of patients be treated."
Replacing current care with sofosbuvir-based regimens would increase drug expenditures by $18-$29 billion per year in California alone, the report estimated. Gilead Sciences has maintained that the drug’s up-front costs are justified given that it could decrease the number of patients who ultimately suffer liver failure and need transplants. However, CTAF said it would take 20 years for payers to recoup two-thirds of the drug’s cost.
CTAF was less enthusiastic about simeprevir, which is approved only for treatment of hepatitis C genotype 1. The group said in its report that "use of simeprevir with pegylated interferon and ribavirin appear to provide limited benefit over the previous standard of care," mainly because that regimen decreased anemia and required patients to take fewer pills.
Originally funded and managed by the Blue Shield of California Foundation, in 2013 CTAF became a core program of the nonprofit Institute for Clinical and Economic Review, which includes representatives of payers, clinicians, and drug makers on its board.
Other groups also have complained about the high price of sofosbuvir and simeprevir. For example, in January, the AIDS Healthcare Foundation asked state Medicaid directors to keep sofosbuvir off its formulary because of its cost.
A panel of California medical experts says two new, once-daily drugs for hepatitis C represent low-value treatment alternatives for the condition because of their high price tags.
The drugs, Gilead Sciences’ sofosbuvir (Sovaldi) and Johnson & Johnson’s simeprevir (Olysio), cost more than $1,000 per pill, pushing the price for the recommended 12-week course of treatment of sofosbuvir to close to $90,000 and treatment with simeprevir to around $66,000, according to the California Technology Assessment Forum (CTAF), an independent group originally convened by the insurance industry to evaluate costs and benefits of treatments.
The Food and Drug Administration approved sofosbuvir and simeprevir late last year. CTAF, which met March 10 to consider the financial and clinical effects of the two new drugs, will issue its final report on the treatments in April.
The group acknowledged in its draft report that therapeutic regimens containing sofosbuvir, approved to treat hepatitis C genotypes 1 through 4, have the potential to "substantially increase" the number of patients achieving sustained virologic response. The drug also offers "the first effective interferon-free option" to patients who can’t take interferon.
"These advantages are considerable," the report said. However, it added, "the clinical advantages of newer treatment regimens would ... come with a substantial potential impact on health care budgets should a large number of patients be treated."
Replacing current care with sofosbuvir-based regimens would increase drug expenditures by $18-$29 billion per year in California alone, the report estimated. Gilead Sciences has maintained that the drug’s up-front costs are justified given that it could decrease the number of patients who ultimately suffer liver failure and need transplants. However, CTAF said it would take 20 years for payers to recoup two-thirds of the drug’s cost.
CTAF was less enthusiastic about simeprevir, which is approved only for treatment of hepatitis C genotype 1. The group said in its report that "use of simeprevir with pegylated interferon and ribavirin appear to provide limited benefit over the previous standard of care," mainly because that regimen decreased anemia and required patients to take fewer pills.
Originally funded and managed by the Blue Shield of California Foundation, in 2013 CTAF became a core program of the nonprofit Institute for Clinical and Economic Review, which includes representatives of payers, clinicians, and drug makers on its board.
Other groups also have complained about the high price of sofosbuvir and simeprevir. For example, in January, the AIDS Healthcare Foundation asked state Medicaid directors to keep sofosbuvir off its formulary because of its cost.
A panel of California medical experts says two new, once-daily drugs for hepatitis C represent low-value treatment alternatives for the condition because of their high price tags.
The drugs, Gilead Sciences’ sofosbuvir (Sovaldi) and Johnson & Johnson’s simeprevir (Olysio), cost more than $1,000 per pill, pushing the price for the recommended 12-week course of treatment of sofosbuvir to close to $90,000 and treatment with simeprevir to around $66,000, according to the California Technology Assessment Forum (CTAF), an independent group originally convened by the insurance industry to evaluate costs and benefits of treatments.
The Food and Drug Administration approved sofosbuvir and simeprevir late last year. CTAF, which met March 10 to consider the financial and clinical effects of the two new drugs, will issue its final report on the treatments in April.
The group acknowledged in its draft report that therapeutic regimens containing sofosbuvir, approved to treat hepatitis C genotypes 1 through 4, have the potential to "substantially increase" the number of patients achieving sustained virologic response. The drug also offers "the first effective interferon-free option" to patients who can’t take interferon.
"These advantages are considerable," the report said. However, it added, "the clinical advantages of newer treatment regimens would ... come with a substantial potential impact on health care budgets should a large number of patients be treated."
Replacing current care with sofosbuvir-based regimens would increase drug expenditures by $18-$29 billion per year in California alone, the report estimated. Gilead Sciences has maintained that the drug’s up-front costs are justified given that it could decrease the number of patients who ultimately suffer liver failure and need transplants. However, CTAF said it would take 20 years for payers to recoup two-thirds of the drug’s cost.
CTAF was less enthusiastic about simeprevir, which is approved only for treatment of hepatitis C genotype 1. The group said in its report that "use of simeprevir with pegylated interferon and ribavirin appear to provide limited benefit over the previous standard of care," mainly because that regimen decreased anemia and required patients to take fewer pills.
Originally funded and managed by the Blue Shield of California Foundation, in 2013 CTAF became a core program of the nonprofit Institute for Clinical and Economic Review, which includes representatives of payers, clinicians, and drug makers on its board.
Other groups also have complained about the high price of sofosbuvir and simeprevir. For example, in January, the AIDS Healthcare Foundation asked state Medicaid directors to keep sofosbuvir off its formulary because of its cost.
Title X services still accessed after Mass. health reform law
Publicly funded family planning organizations still played an important role in providing services to both insured and uninsured patients after enactment of the Massachusetts health reform law, according to a study published Jan. 23 in Morbidity and Mortality Weekly Report.
Prior to the 2006 implementation of the state’s health reform, 59% of patients who received services at Title X family planning clinics were uninsured. After enactment, that number decreased somewhat, eventually leveling off at around 36%, Marion Carter of the Centers for Disease Control and Prevention and her colleague wrote.
During 2012, Title X–funded clinics in Massachusetts provided care to 66,227 clients, or about 90% of the volume seen before the 2006 law (MMWR 2014;63:59-62).
"Publicly funded providers continued to be used as providers of choice for many clients with health care coverage and remained as a ‘safety net’ for uninsured persons in need of family planning services," according to the researchers.
The reasons that insured persons would continue to use Title X family planning clinics are unclear, the researchers said, but could include misunderstanding about their insurance coverage or the desire to keep the use of family planning services out of their health insurance records.
"The continued provision of safety-net family planning services is important not just for the individual clients accessing services at these organizations but for broader health equity goals as well," since young adults experience the most unintended pregnancies of any age group in the United States.
The researchers pointed out that other states may see a stronger and continued demand for services than they would have expected given the continued rollout of the Affordable Care Act.
"Public health agencies are encouraged to track such trends to monitor the demand for such services and inform budget planning and resource allocation," they said.
The researchers disclosed no relevant conflicts of interest.
Publicly funded family planning organizations still played an important role in providing services to both insured and uninsured patients after enactment of the Massachusetts health reform law, according to a study published Jan. 23 in Morbidity and Mortality Weekly Report.
Prior to the 2006 implementation of the state’s health reform, 59% of patients who received services at Title X family planning clinics were uninsured. After enactment, that number decreased somewhat, eventually leveling off at around 36%, Marion Carter of the Centers for Disease Control and Prevention and her colleague wrote.
During 2012, Title X–funded clinics in Massachusetts provided care to 66,227 clients, or about 90% of the volume seen before the 2006 law (MMWR 2014;63:59-62).
"Publicly funded providers continued to be used as providers of choice for many clients with health care coverage and remained as a ‘safety net’ for uninsured persons in need of family planning services," according to the researchers.
The reasons that insured persons would continue to use Title X family planning clinics are unclear, the researchers said, but could include misunderstanding about their insurance coverage or the desire to keep the use of family planning services out of their health insurance records.
"The continued provision of safety-net family planning services is important not just for the individual clients accessing services at these organizations but for broader health equity goals as well," since young adults experience the most unintended pregnancies of any age group in the United States.
The researchers pointed out that other states may see a stronger and continued demand for services than they would have expected given the continued rollout of the Affordable Care Act.
"Public health agencies are encouraged to track such trends to monitor the demand for such services and inform budget planning and resource allocation," they said.
The researchers disclosed no relevant conflicts of interest.
Publicly funded family planning organizations still played an important role in providing services to both insured and uninsured patients after enactment of the Massachusetts health reform law, according to a study published Jan. 23 in Morbidity and Mortality Weekly Report.
Prior to the 2006 implementation of the state’s health reform, 59% of patients who received services at Title X family planning clinics were uninsured. After enactment, that number decreased somewhat, eventually leveling off at around 36%, Marion Carter of the Centers for Disease Control and Prevention and her colleague wrote.
During 2012, Title X–funded clinics in Massachusetts provided care to 66,227 clients, or about 90% of the volume seen before the 2006 law (MMWR 2014;63:59-62).
"Publicly funded providers continued to be used as providers of choice for many clients with health care coverage and remained as a ‘safety net’ for uninsured persons in need of family planning services," according to the researchers.
The reasons that insured persons would continue to use Title X family planning clinics are unclear, the researchers said, but could include misunderstanding about their insurance coverage or the desire to keep the use of family planning services out of their health insurance records.
"The continued provision of safety-net family planning services is important not just for the individual clients accessing services at these organizations but for broader health equity goals as well," since young adults experience the most unintended pregnancies of any age group in the United States.
The researchers pointed out that other states may see a stronger and continued demand for services than they would have expected given the continued rollout of the Affordable Care Act.
"Public health agencies are encouraged to track such trends to monitor the demand for such services and inform budget planning and resource allocation," they said.
The researchers disclosed no relevant conflicts of interest.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Major finding: The percentage of uninsured patients accessing care at Title X family planning clinics decreased from 59% before the Massachusetts health reform law to 36% after.
Data source: Title X Family Planning Annual Report data on all funded clinics in Massachusetts, 2005-2012.
Disclosures: The researchers disclosed no relevant conflicts of interest.
ACP urges changes to curb prescription drug abuse
A new national Prescription Drug Monitoring Program is one of several clinical and policy recommendations from the American College of Physicians aimed at reducing patient abuse and street sales of drugs prescribed for pain, sleep disorders, and weight loss.
The proposed national Prescription Drug Monitoring Program potentially could help physicians avoid drug interactions and identify drug-seeking and "doctor shopping" behaviors, according to the policy paper published online in Annals of Internal Medicine (2013 Dec. 10 [doi: 10.7326/M13-2209]).
The paper also calls for the establishment of evidence-based, nonbinding guidelines regarding recommended maximum dosage and duration of therapy for patients taking controlled substance medications. Additional efforts are urged to reduce substance abuse and to increase medical research on addiction and its causes and treatments.
"Prescription drug abuse is found throughout all aspects of our population," the ACP position paper says. "The challenge for physicians and public policymakers is how to deter prescription drug abuse while maintaining patient access to appropriate treatment."
Physicians have an ethical obligation to manage and relieve pain, the position paper said, yet they must do so responsibly and in accordance with scientific evidence. In the paper, ACP said it supports a comprehensive national policy on prescription drug abuse that covers education, monitoring, proper disposal, and enforcement.
According to a 2010 survey from the Substance Abuse and Mental Health Services Administration, 16 million Americans aged 12 years and up had taken a prescription pain reliever, tranquilizer, stimulant, or sedative for nonmedical purposes at least once in the previous year. In addition, another 2010 report found 2.4 million opioid abusers in the United States, 60% of whom obtained the drugs either directly or indirectly through a doctor’s prescription.
The authors did not report any disclosures.
Eleanor M. Summerhill, FCCP: The inappropriate use and abuse of prescription drugs, particularly opioid pain medications, are a growing public health concern in the United States. This American College of Physicians position paper provides recommendations to assist physicians and policymakers in addressing the difficult challenge of appropriately managing pain while deterring prescription drug abuse. One of the most important proposals calls for the establishment of a national Prescription Drug Monitoring Program to more readily identify "doctor shopping" and other signs of abusive behaviors. Other recommendations include the development of evidence-based guidelines regarding maximal dosages and duration of therapy, as well as enhanced educational programs for health care providers and the public at large.
These recommendations are an important first step in providing a framework upon which a more comprehensive public health policy and supporting infrastructure may be built.
Dr. Eleanor M. Summerhill, FCCP, is an associate professor, division of pulmonary and critical care medicine, Warren Alpert Medical School of Brown University, Providence, R.I.
Eleanor M. Summerhill, FCCP: The inappropriate use and abuse of prescription drugs, particularly opioid pain medications, are a growing public health concern in the United States. This American College of Physicians position paper provides recommendations to assist physicians and policymakers in addressing the difficult challenge of appropriately managing pain while deterring prescription drug abuse. One of the most important proposals calls for the establishment of a national Prescription Drug Monitoring Program to more readily identify "doctor shopping" and other signs of abusive behaviors. Other recommendations include the development of evidence-based guidelines regarding maximal dosages and duration of therapy, as well as enhanced educational programs for health care providers and the public at large.
These recommendations are an important first step in providing a framework upon which a more comprehensive public health policy and supporting infrastructure may be built.
Dr. Eleanor M. Summerhill, FCCP, is an associate professor, division of pulmonary and critical care medicine, Warren Alpert Medical School of Brown University, Providence, R.I.
Eleanor M. Summerhill, FCCP: The inappropriate use and abuse of prescription drugs, particularly opioid pain medications, are a growing public health concern in the United States. This American College of Physicians position paper provides recommendations to assist physicians and policymakers in addressing the difficult challenge of appropriately managing pain while deterring prescription drug abuse. One of the most important proposals calls for the establishment of a national Prescription Drug Monitoring Program to more readily identify "doctor shopping" and other signs of abusive behaviors. Other recommendations include the development of evidence-based guidelines regarding maximal dosages and duration of therapy, as well as enhanced educational programs for health care providers and the public at large.
These recommendations are an important first step in providing a framework upon which a more comprehensive public health policy and supporting infrastructure may be built.
Dr. Eleanor M. Summerhill, FCCP, is an associate professor, division of pulmonary and critical care medicine, Warren Alpert Medical School of Brown University, Providence, R.I.
A new national Prescription Drug Monitoring Program is one of several clinical and policy recommendations from the American College of Physicians aimed at reducing patient abuse and street sales of drugs prescribed for pain, sleep disorders, and weight loss.
The proposed national Prescription Drug Monitoring Program potentially could help physicians avoid drug interactions and identify drug-seeking and "doctor shopping" behaviors, according to the policy paper published online in Annals of Internal Medicine (2013 Dec. 10 [doi: 10.7326/M13-2209]).
The paper also calls for the establishment of evidence-based, nonbinding guidelines regarding recommended maximum dosage and duration of therapy for patients taking controlled substance medications. Additional efforts are urged to reduce substance abuse and to increase medical research on addiction and its causes and treatments.
"Prescription drug abuse is found throughout all aspects of our population," the ACP position paper says. "The challenge for physicians and public policymakers is how to deter prescription drug abuse while maintaining patient access to appropriate treatment."
Physicians have an ethical obligation to manage and relieve pain, the position paper said, yet they must do so responsibly and in accordance with scientific evidence. In the paper, ACP said it supports a comprehensive national policy on prescription drug abuse that covers education, monitoring, proper disposal, and enforcement.
According to a 2010 survey from the Substance Abuse and Mental Health Services Administration, 16 million Americans aged 12 years and up had taken a prescription pain reliever, tranquilizer, stimulant, or sedative for nonmedical purposes at least once in the previous year. In addition, another 2010 report found 2.4 million opioid abusers in the United States, 60% of whom obtained the drugs either directly or indirectly through a doctor’s prescription.
The authors did not report any disclosures.
A new national Prescription Drug Monitoring Program is one of several clinical and policy recommendations from the American College of Physicians aimed at reducing patient abuse and street sales of drugs prescribed for pain, sleep disorders, and weight loss.
The proposed national Prescription Drug Monitoring Program potentially could help physicians avoid drug interactions and identify drug-seeking and "doctor shopping" behaviors, according to the policy paper published online in Annals of Internal Medicine (2013 Dec. 10 [doi: 10.7326/M13-2209]).
The paper also calls for the establishment of evidence-based, nonbinding guidelines regarding recommended maximum dosage and duration of therapy for patients taking controlled substance medications. Additional efforts are urged to reduce substance abuse and to increase medical research on addiction and its causes and treatments.
"Prescription drug abuse is found throughout all aspects of our population," the ACP position paper says. "The challenge for physicians and public policymakers is how to deter prescription drug abuse while maintaining patient access to appropriate treatment."
Physicians have an ethical obligation to manage and relieve pain, the position paper said, yet they must do so responsibly and in accordance with scientific evidence. In the paper, ACP said it supports a comprehensive national policy on prescription drug abuse that covers education, monitoring, proper disposal, and enforcement.
According to a 2010 survey from the Substance Abuse and Mental Health Services Administration, 16 million Americans aged 12 years and up had taken a prescription pain reliever, tranquilizer, stimulant, or sedative for nonmedical purposes at least once in the previous year. In addition, another 2010 report found 2.4 million opioid abusers in the United States, 60% of whom obtained the drugs either directly or indirectly through a doctor’s prescription.
The authors did not report any disclosures.
Few neonate label changes result from pediatric studies
Federal policy that encourages the study of drugs in pediatric patients has led to few pharmaceutical label changes that include new information on drug effects in neonates, in a study published Dec. 9 in JAMA Pediatrics.
Dr. Matthew M. Laughon of the department of pediatrics, University of North Carolina at Chapel Hill, and his colleagues looked at drug studies between 1997 and 2010 that included neonates as a result of legislation encouraging this type of research. They then examined the use of all drugs in neonates admitted to 290 neonatal intensive care units between 2005 and 2010 (JAMA Pediatr. 2013 Dec. 9 [doi:10.1001/jamapediatrics.2013.4208]).
Few labeling changes resulted from neonate studies, and even the drugs that did receive labeling changes following studies in neonates were used infrequently, the researchers found.
They identified 28 drugs studied in neonates and 24 related labeling changes. Eleven of those labeling changes established safety and effectiveness of the drugs in neonates.
Meanwhile, in their review of 446,335 hospitalized infants, the researchers identified 399 drugs used and more than 1.5 million drug exposures in the first 28 postnatal days. Close to half of the 28 drugs studied in neonates were not used in any of these patients, and almost another third of the drugs were used in fewer than 60 neonates each.
Since 1997, a combination of federal incentives and requirements has significantly increased pediatric drug research and development and stimulated an increase in pediatric labeling, the study showed. Federal lawmakers permanently reauthorized these incentives in 2012.
Although many label changes have resulted from these policies, "approximately 50% of drug product labeling has insufficient information on the safety, efficacy, or dosing appropriate for use in children," the researchers said.
In addition, "few labeling changes have included infant-specific information," the researchers concluded. "Novel trial designs need to be developed and appropriate study endpoints must be identified and validated. Education of parents and caregivers regarding the need for studies of drugs being given to neonates will also increase trial success. The scientific and clinical research community will need to work together with the [Food and Drug Administration] to conduct essential neonatal studies."
The study used NIH Clinical and Translational Science Award biostatistical services through the division of pediatric quantitative sciences. Dr. Laughon receives support from the U.S. government for work in pediatric and neonatal clinical pharmacology and from the National Institute of Child Health and Human Development. His colleagues disclosed support from the NIH, the Department of Health and Human Services, Thrasher Research Fund, and industry sources.
Dr. Matthew M. Laughon,
Federal policy that encourages the study of drugs in pediatric patients has led to few pharmaceutical label changes that include new information on drug effects in neonates, in a study published Dec. 9 in JAMA Pediatrics.
Dr. Matthew M. Laughon of the department of pediatrics, University of North Carolina at Chapel Hill, and his colleagues looked at drug studies between 1997 and 2010 that included neonates as a result of legislation encouraging this type of research. They then examined the use of all drugs in neonates admitted to 290 neonatal intensive care units between 2005 and 2010 (JAMA Pediatr. 2013 Dec. 9 [doi:10.1001/jamapediatrics.2013.4208]).
Few labeling changes resulted from neonate studies, and even the drugs that did receive labeling changes following studies in neonates were used infrequently, the researchers found.
They identified 28 drugs studied in neonates and 24 related labeling changes. Eleven of those labeling changes established safety and effectiveness of the drugs in neonates.
Meanwhile, in their review of 446,335 hospitalized infants, the researchers identified 399 drugs used and more than 1.5 million drug exposures in the first 28 postnatal days. Close to half of the 28 drugs studied in neonates were not used in any of these patients, and almost another third of the drugs were used in fewer than 60 neonates each.
Since 1997, a combination of federal incentives and requirements has significantly increased pediatric drug research and development and stimulated an increase in pediatric labeling, the study showed. Federal lawmakers permanently reauthorized these incentives in 2012.
Although many label changes have resulted from these policies, "approximately 50% of drug product labeling has insufficient information on the safety, efficacy, or dosing appropriate for use in children," the researchers said.
In addition, "few labeling changes have included infant-specific information," the researchers concluded. "Novel trial designs need to be developed and appropriate study endpoints must be identified and validated. Education of parents and caregivers regarding the need for studies of drugs being given to neonates will also increase trial success. The scientific and clinical research community will need to work together with the [Food and Drug Administration] to conduct essential neonatal studies."
The study used NIH Clinical and Translational Science Award biostatistical services through the division of pediatric quantitative sciences. Dr. Laughon receives support from the U.S. government for work in pediatric and neonatal clinical pharmacology and from the National Institute of Child Health and Human Development. His colleagues disclosed support from the NIH, the Department of Health and Human Services, Thrasher Research Fund, and industry sources.
Federal policy that encourages the study of drugs in pediatric patients has led to few pharmaceutical label changes that include new information on drug effects in neonates, in a study published Dec. 9 in JAMA Pediatrics.
Dr. Matthew M. Laughon of the department of pediatrics, University of North Carolina at Chapel Hill, and his colleagues looked at drug studies between 1997 and 2010 that included neonates as a result of legislation encouraging this type of research. They then examined the use of all drugs in neonates admitted to 290 neonatal intensive care units between 2005 and 2010 (JAMA Pediatr. 2013 Dec. 9 [doi:10.1001/jamapediatrics.2013.4208]).
Few labeling changes resulted from neonate studies, and even the drugs that did receive labeling changes following studies in neonates were used infrequently, the researchers found.
They identified 28 drugs studied in neonates and 24 related labeling changes. Eleven of those labeling changes established safety and effectiveness of the drugs in neonates.
Meanwhile, in their review of 446,335 hospitalized infants, the researchers identified 399 drugs used and more than 1.5 million drug exposures in the first 28 postnatal days. Close to half of the 28 drugs studied in neonates were not used in any of these patients, and almost another third of the drugs were used in fewer than 60 neonates each.
Since 1997, a combination of federal incentives and requirements has significantly increased pediatric drug research and development and stimulated an increase in pediatric labeling, the study showed. Federal lawmakers permanently reauthorized these incentives in 2012.
Although many label changes have resulted from these policies, "approximately 50% of drug product labeling has insufficient information on the safety, efficacy, or dosing appropriate for use in children," the researchers said.
In addition, "few labeling changes have included infant-specific information," the researchers concluded. "Novel trial designs need to be developed and appropriate study endpoints must be identified and validated. Education of parents and caregivers regarding the need for studies of drugs being given to neonates will also increase trial success. The scientific and clinical research community will need to work together with the [Food and Drug Administration] to conduct essential neonatal studies."
The study used NIH Clinical and Translational Science Award biostatistical services through the division of pediatric quantitative sciences. Dr. Laughon receives support from the U.S. government for work in pediatric and neonatal clinical pharmacology and from the National Institute of Child Health and Human Development. His colleagues disclosed support from the NIH, the Department of Health and Human Services, Thrasher Research Fund, and industry sources.
Dr. Matthew M. Laughon,
Dr. Matthew M. Laughon,
FROM JAMA PEDIATRICS
FDA finalizes regulations defining ‘gluten free’ for celiac patients
The Food and Drug Administration has finalized regulations intended to define the term "gluten free" on food packaging in an effort to give celiac disease patients and others following the gluten-free diet confidence that the food they buy is safe for them to consume.
The new regulations, which were nearly a decade in the making, do not require food manufacturers to label products as gluten free. Instead, they lay out the rules to follow if those manufacturers want to voluntarily place "gluten-free" labels on products.
The rules state that manufacturers can label foods "gluten free" if they contain less than 20 parts per million (ppm) of gluten, a protein found in wheat, barley, and rye. According to the FDA, most celiac disease patients can tolerate a small amount of gluten in their food each day.
The regulations prohibit the use of the term "gluten free" on any product that contains wheat, barley, or rye ingredients unless those ingredients have been processed to remove the gluten. Products that are naturally gluten free, such as eggs, fruits, vegetables, and bottled water, also can carry the "gluten free" label.
Physicians who treat celiac disease patients praised the ruling. "Without proper food labeling regulation, celiac patients cannot know what the words ‘gluten free’ mean when they see them on a food label," Dr. Alessio Fasano, medical director of the Center for Celiac Research at MassGeneral Hospital for Children, Boston, said in a statement.
About 3 million people in the United States have celiac disease; many of them are undiagnosed. The regulatory action brings the United States into line with Canada and the European Union, both of which consider "gluten free" to mean less than 20 ppm of gluten.
Manufacturers have1 year to comply with the regulations or risk facing compliance action from the FDA. The agency said that the vast majority of "gluten free"–labeled products on the shelves today – 95% – already comply with the regulations.
The Food and Drug Administration has finalized regulations intended to define the term "gluten free" on food packaging in an effort to give celiac disease patients and others following the gluten-free diet confidence that the food they buy is safe for them to consume.
The new regulations, which were nearly a decade in the making, do not require food manufacturers to label products as gluten free. Instead, they lay out the rules to follow if those manufacturers want to voluntarily place "gluten-free" labels on products.
The rules state that manufacturers can label foods "gluten free" if they contain less than 20 parts per million (ppm) of gluten, a protein found in wheat, barley, and rye. According to the FDA, most celiac disease patients can tolerate a small amount of gluten in their food each day.
The regulations prohibit the use of the term "gluten free" on any product that contains wheat, barley, or rye ingredients unless those ingredients have been processed to remove the gluten. Products that are naturally gluten free, such as eggs, fruits, vegetables, and bottled water, also can carry the "gluten free" label.
Physicians who treat celiac disease patients praised the ruling. "Without proper food labeling regulation, celiac patients cannot know what the words ‘gluten free’ mean when they see them on a food label," Dr. Alessio Fasano, medical director of the Center for Celiac Research at MassGeneral Hospital for Children, Boston, said in a statement.
About 3 million people in the United States have celiac disease; many of them are undiagnosed. The regulatory action brings the United States into line with Canada and the European Union, both of which consider "gluten free" to mean less than 20 ppm of gluten.
Manufacturers have1 year to comply with the regulations or risk facing compliance action from the FDA. The agency said that the vast majority of "gluten free"–labeled products on the shelves today – 95% – already comply with the regulations.
The Food and Drug Administration has finalized regulations intended to define the term "gluten free" on food packaging in an effort to give celiac disease patients and others following the gluten-free diet confidence that the food they buy is safe for them to consume.
The new regulations, which were nearly a decade in the making, do not require food manufacturers to label products as gluten free. Instead, they lay out the rules to follow if those manufacturers want to voluntarily place "gluten-free" labels on products.
The rules state that manufacturers can label foods "gluten free" if they contain less than 20 parts per million (ppm) of gluten, a protein found in wheat, barley, and rye. According to the FDA, most celiac disease patients can tolerate a small amount of gluten in their food each day.
The regulations prohibit the use of the term "gluten free" on any product that contains wheat, barley, or rye ingredients unless those ingredients have been processed to remove the gluten. Products that are naturally gluten free, such as eggs, fruits, vegetables, and bottled water, also can carry the "gluten free" label.
Physicians who treat celiac disease patients praised the ruling. "Without proper food labeling regulation, celiac patients cannot know what the words ‘gluten free’ mean when they see them on a food label," Dr. Alessio Fasano, medical director of the Center for Celiac Research at MassGeneral Hospital for Children, Boston, said in a statement.
About 3 million people in the United States have celiac disease; many of them are undiagnosed. The regulatory action brings the United States into line with Canada and the European Union, both of which consider "gluten free" to mean less than 20 ppm of gluten.
Manufacturers have1 year to comply with the regulations or risk facing compliance action from the FDA. The agency said that the vast majority of "gluten free"–labeled products on the shelves today – 95% – already comply with the regulations.
Betty Ford Center, Hazelden consider possible alliance
The Betty Ford Center and the Hazelden Foundation, two leading substance abuse treatment centers, are exploring the possibility of a formal business alliance, in large part because of the influx of new patients expected as a result of the Affordable Care Act, the two organizations say.
The boards of both institutions have approved "in principle" the concept of a formal alliance between the Betty Ford Center, a licensed addiction treatment hospital in Rancho Mirage, Calif., and Center City, Minn.,–based Hazelden Foundation, which has facilities in five states.
The two make natural partners, according to Mary Pattiz, Ph.D., chairwoman of the Betty Ford Center. "Before Betty Ford Center opened its doors in October 1982, we looked to Hazelden. For more than 30 years, we’ve worked side by side as philosophical partners in providing quality care to alcoholics, addicts, and their families." Both follow treatment protocols based on the Twelve Steps of Alcoholics Anonymous.
The two organizations are working to iron out the details of how an alliance would be structured, said Susan Fox Gillis, chairwoman of Hazelden’s board of trustees. Gillis said in a statement that a top priority in the alliance discussions is making sure Betty Ford’s legacy is honored.
Under the Affordable Care Act, Medicaid and all health insurance policies sold on the insurance exchanges will be required to cover services related to substance abuse disorders. The Substance Abuse and Mental Health Services Administration (SAMHSA) estimates that between 6 million and 10 million currently uninsured individuals have untreated mental illnesses or addictions.
The Betty Ford Center and the Hazelden Foundation, two leading substance abuse treatment centers, are exploring the possibility of a formal business alliance, in large part because of the influx of new patients expected as a result of the Affordable Care Act, the two organizations say.
The boards of both institutions have approved "in principle" the concept of a formal alliance between the Betty Ford Center, a licensed addiction treatment hospital in Rancho Mirage, Calif., and Center City, Minn.,–based Hazelden Foundation, which has facilities in five states.
The two make natural partners, according to Mary Pattiz, Ph.D., chairwoman of the Betty Ford Center. "Before Betty Ford Center opened its doors in October 1982, we looked to Hazelden. For more than 30 years, we’ve worked side by side as philosophical partners in providing quality care to alcoholics, addicts, and their families." Both follow treatment protocols based on the Twelve Steps of Alcoholics Anonymous.
The two organizations are working to iron out the details of how an alliance would be structured, said Susan Fox Gillis, chairwoman of Hazelden’s board of trustees. Gillis said in a statement that a top priority in the alliance discussions is making sure Betty Ford’s legacy is honored.
Under the Affordable Care Act, Medicaid and all health insurance policies sold on the insurance exchanges will be required to cover services related to substance abuse disorders. The Substance Abuse and Mental Health Services Administration (SAMHSA) estimates that between 6 million and 10 million currently uninsured individuals have untreated mental illnesses or addictions.
The Betty Ford Center and the Hazelden Foundation, two leading substance abuse treatment centers, are exploring the possibility of a formal business alliance, in large part because of the influx of new patients expected as a result of the Affordable Care Act, the two organizations say.
The boards of both institutions have approved "in principle" the concept of a formal alliance between the Betty Ford Center, a licensed addiction treatment hospital in Rancho Mirage, Calif., and Center City, Minn.,–based Hazelden Foundation, which has facilities in five states.
The two make natural partners, according to Mary Pattiz, Ph.D., chairwoman of the Betty Ford Center. "Before Betty Ford Center opened its doors in October 1982, we looked to Hazelden. For more than 30 years, we’ve worked side by side as philosophical partners in providing quality care to alcoholics, addicts, and their families." Both follow treatment protocols based on the Twelve Steps of Alcoholics Anonymous.
The two organizations are working to iron out the details of how an alliance would be structured, said Susan Fox Gillis, chairwoman of Hazelden’s board of trustees. Gillis said in a statement that a top priority in the alliance discussions is making sure Betty Ford’s legacy is honored.
Under the Affordable Care Act, Medicaid and all health insurance policies sold on the insurance exchanges will be required to cover services related to substance abuse disorders. The Substance Abuse and Mental Health Services Administration (SAMHSA) estimates that between 6 million and 10 million currently uninsured individuals have untreated mental illnesses or addictions.
Survey: Primary care generates more hospital revenue than specialists
Primary care physicians generated more net hospital revenue on average than did specialists in 2013, marking the first time primary care doctors surpassed specialists in hospital revenue generated, according to a survey of hospital chief financial executives from physician job placement firm Merritt Hawkins.
The increases in revenue generated by family physicians and internists could result from recent trends toward hospital employment of physicians, Merritt Hawkins said in its analysis.
Primary care physicians generated average revenue of $1.57 million each, up about 13% from $1.38 million in 2010, the survey showed. Meanwhile, specialists generated $1.42 million, the lowest average in the 5 years Merritt Hawkins has conducted the survey.
The average annual net revenue generated by individual physicians in all 18 specialties was $1.44 million, a decrease of 9% over average annual net revenue generated by all specialties in 2010 – again, the lowest average number in the survey’s 5-year history.
In primary care, family physicians saw a 22% gain in hospital revenue generated, to an average of $2.1 million per physician, while internists saw 9% gains, to $1.8 million. Pediatricians, meanwhile, had slight losses in hospital revenue generated between 2010 and 2013.
"As primary care physicians become hospital employees, they may be more likely to divert tests, therapies, and other services ‘in-house’ to their hospital employer, rather than to outside resources such as radiology groups or labs, which may have been their pattern when they were in independent practice," the survey authors said.
Gains in revenue generated by family physicians and internists also may result from delivery models’ shifts toward a primary care-driven approach.
Some specialty areas – notably, nephrology – saw significant gains in net hospital revenue between 2010 and 2013. Nephrologists generated an average of $1.17 million each in 2013, a gain of 69% over 2010, the report said. Orthopedic surgeons also generated more revenue for hospitals, as did hematologists/oncologists.
Meanwhile, the survey noted declines in average annual revenue generated by neurology, general surgery, and neurological surgery. Average hospital revenue generated also declined slightly in invasive cardiology, the survey found. Average annual revenue generated by urology, pulmonology, obstetrics/gynecology, and psychiatry was more or less stable in 2013, compared with 2010.
Primary care physicians generated more net hospital revenue on average than did specialists in 2013, marking the first time primary care doctors surpassed specialists in hospital revenue generated, according to a survey of hospital chief financial executives from physician job placement firm Merritt Hawkins.
The increases in revenue generated by family physicians and internists could result from recent trends toward hospital employment of physicians, Merritt Hawkins said in its analysis.
Primary care physicians generated average revenue of $1.57 million each, up about 13% from $1.38 million in 2010, the survey showed. Meanwhile, specialists generated $1.42 million, the lowest average in the 5 years Merritt Hawkins has conducted the survey.
The average annual net revenue generated by individual physicians in all 18 specialties was $1.44 million, a decrease of 9% over average annual net revenue generated by all specialties in 2010 – again, the lowest average number in the survey’s 5-year history.
In primary care, family physicians saw a 22% gain in hospital revenue generated, to an average of $2.1 million per physician, while internists saw 9% gains, to $1.8 million. Pediatricians, meanwhile, had slight losses in hospital revenue generated between 2010 and 2013.
"As primary care physicians become hospital employees, they may be more likely to divert tests, therapies, and other services ‘in-house’ to their hospital employer, rather than to outside resources such as radiology groups or labs, which may have been their pattern when they were in independent practice," the survey authors said.
Gains in revenue generated by family physicians and internists also may result from delivery models’ shifts toward a primary care-driven approach.
Some specialty areas – notably, nephrology – saw significant gains in net hospital revenue between 2010 and 2013. Nephrologists generated an average of $1.17 million each in 2013, a gain of 69% over 2010, the report said. Orthopedic surgeons also generated more revenue for hospitals, as did hematologists/oncologists.
Meanwhile, the survey noted declines in average annual revenue generated by neurology, general surgery, and neurological surgery. Average hospital revenue generated also declined slightly in invasive cardiology, the survey found. Average annual revenue generated by urology, pulmonology, obstetrics/gynecology, and psychiatry was more or less stable in 2013, compared with 2010.
Primary care physicians generated more net hospital revenue on average than did specialists in 2013, marking the first time primary care doctors surpassed specialists in hospital revenue generated, according to a survey of hospital chief financial executives from physician job placement firm Merritt Hawkins.
The increases in revenue generated by family physicians and internists could result from recent trends toward hospital employment of physicians, Merritt Hawkins said in its analysis.
Primary care physicians generated average revenue of $1.57 million each, up about 13% from $1.38 million in 2010, the survey showed. Meanwhile, specialists generated $1.42 million, the lowest average in the 5 years Merritt Hawkins has conducted the survey.
The average annual net revenue generated by individual physicians in all 18 specialties was $1.44 million, a decrease of 9% over average annual net revenue generated by all specialties in 2010 – again, the lowest average number in the survey’s 5-year history.
In primary care, family physicians saw a 22% gain in hospital revenue generated, to an average of $2.1 million per physician, while internists saw 9% gains, to $1.8 million. Pediatricians, meanwhile, had slight losses in hospital revenue generated between 2010 and 2013.
"As primary care physicians become hospital employees, they may be more likely to divert tests, therapies, and other services ‘in-house’ to their hospital employer, rather than to outside resources such as radiology groups or labs, which may have been their pattern when they were in independent practice," the survey authors said.
Gains in revenue generated by family physicians and internists also may result from delivery models’ shifts toward a primary care-driven approach.
Some specialty areas – notably, nephrology – saw significant gains in net hospital revenue between 2010 and 2013. Nephrologists generated an average of $1.17 million each in 2013, a gain of 69% over 2010, the report said. Orthopedic surgeons also generated more revenue for hospitals, as did hematologists/oncologists.
Meanwhile, the survey noted declines in average annual revenue generated by neurology, general surgery, and neurological surgery. Average hospital revenue generated also declined slightly in invasive cardiology, the survey found. Average annual revenue generated by urology, pulmonology, obstetrics/gynecology, and psychiatry was more or less stable in 2013, compared with 2010.
Providers order fewer tests when fees are listed
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
Feds abandon fight for graphic cigarette labels
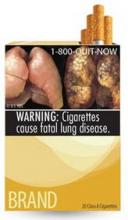
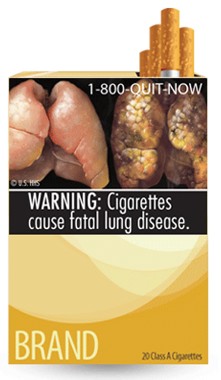
The Food and Drug Administration, facing virulent opposition from the tobacco industry as well as two court decisions that didn’t go its way, has decided to drop its proposals to include graphic, photo-based warning labels on cigarette packs.
Instead, the FDA said it will research new ways to craft warning labels that can reduce tobacco deaths, while still satisfying the courts’ requirements that any regulations not infringe upon tobacco companies’ First Amendment right to free speech. The 2009 Tobacco Control Act requires the FDA to implement new warning labels.
The graphic warning labels, first unveiled in 2011 and intended for placement on all cigarette packages, included disturbing photos such as the corpse of a man who died of tobacco-related causes, disease-riddled lungs, and rotting teeth. Other countries use similar warning labels.
A group of tobacco manufacturers sued the agency to overturn the requirement to use the labels, and two courts – most recently, the U.S. Court of Appeals for the D.C. Circuit – sided with the manufacturers. The Justice Department elected not to appeal the case to the U.S. Supreme Court.
The American Cancer Society Cancer Action Network, the ACS’ advocacy arm, urged the FDA to work quickly to develop new graphic warnings. "The current warning labels have not been changed in 25 years and are widely considered to be ineffective," group president Chris Hansen said in a statement. "Every day that the current warnings remain in place is another day in which ... the health of the nation is compromised."
The Food and Drug Administration, facing virulent opposition from the tobacco industry as well as two court decisions that didn’t go its way, has decided to drop its proposals to include graphic, photo-based warning labels on cigarette packs.
Instead, the FDA said it will research new ways to craft warning labels that can reduce tobacco deaths, while still satisfying the courts’ requirements that any regulations not infringe upon tobacco companies’ First Amendment right to free speech. The 2009 Tobacco Control Act requires the FDA to implement new warning labels.
The graphic warning labels, first unveiled in 2011 and intended for placement on all cigarette packages, included disturbing photos such as the corpse of a man who died of tobacco-related causes, disease-riddled lungs, and rotting teeth. Other countries use similar warning labels.
A group of tobacco manufacturers sued the agency to overturn the requirement to use the labels, and two courts – most recently, the U.S. Court of Appeals for the D.C. Circuit – sided with the manufacturers. The Justice Department elected not to appeal the case to the U.S. Supreme Court.
The American Cancer Society Cancer Action Network, the ACS’ advocacy arm, urged the FDA to work quickly to develop new graphic warnings. "The current warning labels have not been changed in 25 years and are widely considered to be ineffective," group president Chris Hansen said in a statement. "Every day that the current warnings remain in place is another day in which ... the health of the nation is compromised."
The Food and Drug Administration, facing virulent opposition from the tobacco industry as well as two court decisions that didn’t go its way, has decided to drop its proposals to include graphic, photo-based warning labels on cigarette packs.
Instead, the FDA said it will research new ways to craft warning labels that can reduce tobacco deaths, while still satisfying the courts’ requirements that any regulations not infringe upon tobacco companies’ First Amendment right to free speech. The 2009 Tobacco Control Act requires the FDA to implement new warning labels.
The graphic warning labels, first unveiled in 2011 and intended for placement on all cigarette packages, included disturbing photos such as the corpse of a man who died of tobacco-related causes, disease-riddled lungs, and rotting teeth. Other countries use similar warning labels.
A group of tobacco manufacturers sued the agency to overturn the requirement to use the labels, and two courts – most recently, the U.S. Court of Appeals for the D.C. Circuit – sided with the manufacturers. The Justice Department elected not to appeal the case to the U.S. Supreme Court.
The American Cancer Society Cancer Action Network, the ACS’ advocacy arm, urged the FDA to work quickly to develop new graphic warnings. "The current warning labels have not been changed in 25 years and are widely considered to be ineffective," group president Chris Hansen said in a statement. "Every day that the current warnings remain in place is another day in which ... the health of the nation is compromised."