User login
Jeff Evans has been editor of Rheumatology News/MDedge Rheumatology and the EULAR Congress News since 2013. He started at Frontline Medical Communications in 2001 and was a reporter for 8 years before serving as editor of Clinical Neurology News and World Neurology, and briefly as editor of GI & Hepatology News. He graduated cum laude from Cornell University (New York) with a BA in biological sciences, concentrating in neurobiology and behavior.
VIDEO: Exercise, manual therapy for OA add incremental benefits to usual care
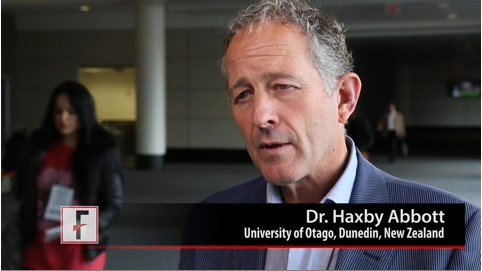
BOSTON – Exercise therapy or manual therapy provide benefits for improving osteoarthritis symptoms and physical function that go over and above what is obtained with usual care alone, according to results from a randomized, controlled trial.
The trial is the first to show the additive effect of manual therapy or exercise therapy on top of usual care. The results of the trial, which had 2 years of follow-up, indicate that in the absence of predictive factors, clinicians should prescribe either one of the interventions based on patient preference in addition to the usual care of NSAIDs and other adjunctive treatments such as massage therapy or specialized footwear, lead investigator Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, said in an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Exercise therapy or manual therapy provide benefits for improving osteoarthritis symptoms and physical function that go over and above what is obtained with usual care alone, according to results from a randomized, controlled trial.
The trial is the first to show the additive effect of manual therapy or exercise therapy on top of usual care. The results of the trial, which had 2 years of follow-up, indicate that in the absence of predictive factors, clinicians should prescribe either one of the interventions based on patient preference in addition to the usual care of NSAIDs and other adjunctive treatments such as massage therapy or specialized footwear, lead investigator Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, said in an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Exercise therapy or manual therapy provide benefits for improving osteoarthritis symptoms and physical function that go over and above what is obtained with usual care alone, according to results from a randomized, controlled trial.
The trial is the first to show the additive effect of manual therapy or exercise therapy on top of usual care. The results of the trial, which had 2 years of follow-up, indicate that in the absence of predictive factors, clinicians should prescribe either one of the interventions based on patient preference in addition to the usual care of NSAIDs and other adjunctive treatments such as massage therapy or specialized footwear, lead investigator Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, said in an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
Evidence builds for importance of CVD, new drug targets at ACR
It’s difficult to highlight the most striking studies or topic areas out of the bounty of research that will be presented at the annual meeting of the American College of Rheumatology, but a few noteworthy studies caught the eye of Dr. Eric L. Matteson, the meeting’s planning subcommittee abstract selection cochair for clinical research.
Some of the studies and topic areas that deserve attention include growing knowledge about the risk of cardiovascular disease in many rheumatic conditions; the conditions in which rheumatoid arthritis (RA) treatment can be cost-effective, and de-escalation of disease-modifying antirheumatic drugs (DMARDs) may be possible; promising clinical results with new drug targets; according to Dr. Matteson, professor of medicine and chair of the department of rheumatology at the Mayo Clinic, Rochester, Minn.
Cardiovascular disease in spondyloarthritis, RA
“One major area in rheumatic diseases is looking at the emerging field of cardiovascular disease. We’ve known that there’s increased risk for heart disease in rheumatoid arthritis patients, not necessarily what to do about it. Now increasingly we’re finding that there’s the same risk in some other inflammatory arthritis diseases,” Dr. Matteson said. A Canadian study to be presented on Tuesday (abstract 2829) is the first population-based cohort study to show that patients with spondyloarthritis are at increased risk for heart disease, although at 40%-50% increased risk of cardiovascular death in comparison to people without spondyloarthritis, it is not at the same magnitude of risk as what is observed for RA, where risk for CV death is doubled in some subgroups, such as women with rheumatoid factor-positive disease.
“I think that’s something that’s new and is significant,” Dr. Matteson said.
Another interesting study to be reported on Sunday provides some initial evidence to suggest that reducing disease activity in RA might reduce the risk of heart failure, which has been shown to be elevated in RA patients. The prospective, cross-sectional study (abstract 945) of patients from a clinic in Germany found progressively lower prevalence of heart failure as 28-joint Disease Activity Score declined, independent of treatment type.
De-escalating DMARDs in RA
Another “hot-button” issue in RA is whether it is possible to reduce therapy, Dr. Matteson noted. On Sunday, German investigators will present a multicenter, randomized controlled trial (abstract 940) showing that while DMARDs can be successfully de-escalated, it’s not clear whether starting the de-escalation process is better done first with a conventional DMARD or a biologic. The presence of anticitrullinated peptide antibodies turned out to be the only predictor of recurrent disease. Another study in the same session (abstract 941) indicated that an attempt to de-escalate biologic treatment was successful in 87% of the selected patients who tried to do so and provided substantial cost savings.
New drug targets in clinical research
One of the unique therapeutic approaches being tried is using autologous dendritic cell immunotherapy to treat RA patients, Dr. Matteson said. “The dendritic cell is an important immune-mediating cell actually not just in rheumatoid arthritis but a lot of other systemic inflammatory conditions including even giant cell arteritis.” A phase I, open-label study (abstract 946) that will be presented on Sunday demonstrated that five vaccinations with high or low doses of the cells over 2- to 4-week intervals in 12 RA patients yielded good to moderate European League Against Rheumatism (EULAR) responses in 7 patients while 12 adverse events occurred in 8 patients.
After not-so-encouraging studies of interleukin-17 as a drug target in RA, its potential in seronegative inflammatory arthritis appears much more promising. The results of a 1-year, phase III trial of secukinumab, a monoclonal antibody to IL-17A, in patients with psoriatic arthritis is “quite hopeful” because there were improvements in clinical parameters of disease and an indication of inhibition of joint erosion (abstract 954). Another phase III study of the drug showed “quite promising effects” in controlling ankylosing spondylitis over the course of 1 year (abstract 819). Both studies will be presented on Sunday.
Noteworthy plenary presentations
“One of the hot areas in lung disease in rheumatic diseases” involves controversy over the value of lung transplantation in patients with systemic sclerosis (SSc) and end-stage lung disease, Dr. Matteson said. A study to be presented in Monday’s plenary session suggests that new methods must be developed to determine which SSc patients can successfully undergo lung transplantation rather than to deny all patients with the condition the chance to undergo the procedure. While the study (abstract 1797) confirmed that patients with SSc have a nearly 50% increased risk of death at 1 year posttransplant when compared with interstitial lung disease patients without SSc, there was no difference in mortality for SSc patients, compared with patients with pulmonary arterial hypertension not caused by SSc.
In Tuesday’s plenary session, investigators will report on the cost-effectiveness of triple therapy, compared with biologics. The results of the study (abstract 2781) suggest that added costs associated with using etanercept prior to a triple-therapy regimen may not be ideal in RA patients for whom methotrexate is not working. Because etanercept has only a small probability of being cost-effective, compared with triple therapy, more health care dollars could be freed up, the authors argue, by adopting the triple regimen prior to etanercept.
Dr. Matteson has received research support from many companies marketing drugs for rheumatic diseases.
It’s difficult to highlight the most striking studies or topic areas out of the bounty of research that will be presented at the annual meeting of the American College of Rheumatology, but a few noteworthy studies caught the eye of Dr. Eric L. Matteson, the meeting’s planning subcommittee abstract selection cochair for clinical research.
Some of the studies and topic areas that deserve attention include growing knowledge about the risk of cardiovascular disease in many rheumatic conditions; the conditions in which rheumatoid arthritis (RA) treatment can be cost-effective, and de-escalation of disease-modifying antirheumatic drugs (DMARDs) may be possible; promising clinical results with new drug targets; according to Dr. Matteson, professor of medicine and chair of the department of rheumatology at the Mayo Clinic, Rochester, Minn.
Cardiovascular disease in spondyloarthritis, RA
“One major area in rheumatic diseases is looking at the emerging field of cardiovascular disease. We’ve known that there’s increased risk for heart disease in rheumatoid arthritis patients, not necessarily what to do about it. Now increasingly we’re finding that there’s the same risk in some other inflammatory arthritis diseases,” Dr. Matteson said. A Canadian study to be presented on Tuesday (abstract 2829) is the first population-based cohort study to show that patients with spondyloarthritis are at increased risk for heart disease, although at 40%-50% increased risk of cardiovascular death in comparison to people without spondyloarthritis, it is not at the same magnitude of risk as what is observed for RA, where risk for CV death is doubled in some subgroups, such as women with rheumatoid factor-positive disease.
“I think that’s something that’s new and is significant,” Dr. Matteson said.
Another interesting study to be reported on Sunday provides some initial evidence to suggest that reducing disease activity in RA might reduce the risk of heart failure, which has been shown to be elevated in RA patients. The prospective, cross-sectional study (abstract 945) of patients from a clinic in Germany found progressively lower prevalence of heart failure as 28-joint Disease Activity Score declined, independent of treatment type.
De-escalating DMARDs in RA
Another “hot-button” issue in RA is whether it is possible to reduce therapy, Dr. Matteson noted. On Sunday, German investigators will present a multicenter, randomized controlled trial (abstract 940) showing that while DMARDs can be successfully de-escalated, it’s not clear whether starting the de-escalation process is better done first with a conventional DMARD or a biologic. The presence of anticitrullinated peptide antibodies turned out to be the only predictor of recurrent disease. Another study in the same session (abstract 941) indicated that an attempt to de-escalate biologic treatment was successful in 87% of the selected patients who tried to do so and provided substantial cost savings.
New drug targets in clinical research
One of the unique therapeutic approaches being tried is using autologous dendritic cell immunotherapy to treat RA patients, Dr. Matteson said. “The dendritic cell is an important immune-mediating cell actually not just in rheumatoid arthritis but a lot of other systemic inflammatory conditions including even giant cell arteritis.” A phase I, open-label study (abstract 946) that will be presented on Sunday demonstrated that five vaccinations with high or low doses of the cells over 2- to 4-week intervals in 12 RA patients yielded good to moderate European League Against Rheumatism (EULAR) responses in 7 patients while 12 adverse events occurred in 8 patients.
After not-so-encouraging studies of interleukin-17 as a drug target in RA, its potential in seronegative inflammatory arthritis appears much more promising. The results of a 1-year, phase III trial of secukinumab, a monoclonal antibody to IL-17A, in patients with psoriatic arthritis is “quite hopeful” because there were improvements in clinical parameters of disease and an indication of inhibition of joint erosion (abstract 954). Another phase III study of the drug showed “quite promising effects” in controlling ankylosing spondylitis over the course of 1 year (abstract 819). Both studies will be presented on Sunday.
Noteworthy plenary presentations
“One of the hot areas in lung disease in rheumatic diseases” involves controversy over the value of lung transplantation in patients with systemic sclerosis (SSc) and end-stage lung disease, Dr. Matteson said. A study to be presented in Monday’s plenary session suggests that new methods must be developed to determine which SSc patients can successfully undergo lung transplantation rather than to deny all patients with the condition the chance to undergo the procedure. While the study (abstract 1797) confirmed that patients with SSc have a nearly 50% increased risk of death at 1 year posttransplant when compared with interstitial lung disease patients without SSc, there was no difference in mortality for SSc patients, compared with patients with pulmonary arterial hypertension not caused by SSc.
In Tuesday’s plenary session, investigators will report on the cost-effectiveness of triple therapy, compared with biologics. The results of the study (abstract 2781) suggest that added costs associated with using etanercept prior to a triple-therapy regimen may not be ideal in RA patients for whom methotrexate is not working. Because etanercept has only a small probability of being cost-effective, compared with triple therapy, more health care dollars could be freed up, the authors argue, by adopting the triple regimen prior to etanercept.
Dr. Matteson has received research support from many companies marketing drugs for rheumatic diseases.
It’s difficult to highlight the most striking studies or topic areas out of the bounty of research that will be presented at the annual meeting of the American College of Rheumatology, but a few noteworthy studies caught the eye of Dr. Eric L. Matteson, the meeting’s planning subcommittee abstract selection cochair for clinical research.
Some of the studies and topic areas that deserve attention include growing knowledge about the risk of cardiovascular disease in many rheumatic conditions; the conditions in which rheumatoid arthritis (RA) treatment can be cost-effective, and de-escalation of disease-modifying antirheumatic drugs (DMARDs) may be possible; promising clinical results with new drug targets; according to Dr. Matteson, professor of medicine and chair of the department of rheumatology at the Mayo Clinic, Rochester, Minn.
Cardiovascular disease in spondyloarthritis, RA
“One major area in rheumatic diseases is looking at the emerging field of cardiovascular disease. We’ve known that there’s increased risk for heart disease in rheumatoid arthritis patients, not necessarily what to do about it. Now increasingly we’re finding that there’s the same risk in some other inflammatory arthritis diseases,” Dr. Matteson said. A Canadian study to be presented on Tuesday (abstract 2829) is the first population-based cohort study to show that patients with spondyloarthritis are at increased risk for heart disease, although at 40%-50% increased risk of cardiovascular death in comparison to people without spondyloarthritis, it is not at the same magnitude of risk as what is observed for RA, where risk for CV death is doubled in some subgroups, such as women with rheumatoid factor-positive disease.
“I think that’s something that’s new and is significant,” Dr. Matteson said.
Another interesting study to be reported on Sunday provides some initial evidence to suggest that reducing disease activity in RA might reduce the risk of heart failure, which has been shown to be elevated in RA patients. The prospective, cross-sectional study (abstract 945) of patients from a clinic in Germany found progressively lower prevalence of heart failure as 28-joint Disease Activity Score declined, independent of treatment type.
De-escalating DMARDs in RA
Another “hot-button” issue in RA is whether it is possible to reduce therapy, Dr. Matteson noted. On Sunday, German investigators will present a multicenter, randomized controlled trial (abstract 940) showing that while DMARDs can be successfully de-escalated, it’s not clear whether starting the de-escalation process is better done first with a conventional DMARD or a biologic. The presence of anticitrullinated peptide antibodies turned out to be the only predictor of recurrent disease. Another study in the same session (abstract 941) indicated that an attempt to de-escalate biologic treatment was successful in 87% of the selected patients who tried to do so and provided substantial cost savings.
New drug targets in clinical research
One of the unique therapeutic approaches being tried is using autologous dendritic cell immunotherapy to treat RA patients, Dr. Matteson said. “The dendritic cell is an important immune-mediating cell actually not just in rheumatoid arthritis but a lot of other systemic inflammatory conditions including even giant cell arteritis.” A phase I, open-label study (abstract 946) that will be presented on Sunday demonstrated that five vaccinations with high or low doses of the cells over 2- to 4-week intervals in 12 RA patients yielded good to moderate European League Against Rheumatism (EULAR) responses in 7 patients while 12 adverse events occurred in 8 patients.
After not-so-encouraging studies of interleukin-17 as a drug target in RA, its potential in seronegative inflammatory arthritis appears much more promising. The results of a 1-year, phase III trial of secukinumab, a monoclonal antibody to IL-17A, in patients with psoriatic arthritis is “quite hopeful” because there were improvements in clinical parameters of disease and an indication of inhibition of joint erosion (abstract 954). Another phase III study of the drug showed “quite promising effects” in controlling ankylosing spondylitis over the course of 1 year (abstract 819). Both studies will be presented on Sunday.
Noteworthy plenary presentations
“One of the hot areas in lung disease in rheumatic diseases” involves controversy over the value of lung transplantation in patients with systemic sclerosis (SSc) and end-stage lung disease, Dr. Matteson said. A study to be presented in Monday’s plenary session suggests that new methods must be developed to determine which SSc patients can successfully undergo lung transplantation rather than to deny all patients with the condition the chance to undergo the procedure. While the study (abstract 1797) confirmed that patients with SSc have a nearly 50% increased risk of death at 1 year posttransplant when compared with interstitial lung disease patients without SSc, there was no difference in mortality for SSc patients, compared with patients with pulmonary arterial hypertension not caused by SSc.
In Tuesday’s plenary session, investigators will report on the cost-effectiveness of triple therapy, compared with biologics. The results of the study (abstract 2781) suggest that added costs associated with using etanercept prior to a triple-therapy regimen may not be ideal in RA patients for whom methotrexate is not working. Because etanercept has only a small probability of being cost-effective, compared with triple therapy, more health care dollars could be freed up, the authors argue, by adopting the triple regimen prior to etanercept.
Dr. Matteson has received research support from many companies marketing drugs for rheumatic diseases.
Disease activity, not lipid levels, appear to affect CV risk with tocilizumab
Rheumatoid arthritis disease activity during treatment with tocilizumab plays a significant role in patients’ risk for major adverse cardiovascular events, rather than increases in lipid levels observed during treatment with the interleukin-6 receptor inhibitor, according to a new analysis of phase III trials and extensions studies of the drug.
The study of 3,986 rheumatoid arthritis (RA) patients treated with tocilizumab for a mean of 3.68 years indicated that reductions in disease activity based on lower 28-joint disease activity score (DAS28) were significantly associated with fewer major adverse cardiovascular events (MACE), defined as definite or probable nonfatal myocardial infarction, nonfatal stroke, or death from a cardiovascular cause.
Conversely, risk for MACE rose with poorer response to treatment, as measured by increases in DAS28 and total swollen and tender joints (Arthritis Rheumatol. 2014 [doi:10.1002/art.38920]).
In addition to DAS28, some traditional risk factors at baseline – older age, history of cardiac disorders, and high ratio of total cholesterol to HDL cholesterol (known as the atherogenic index) – were independent predictors of MACE during treatment, reported Dr. Vijay U. Rao and his colleagues. Dr. Rao was a research fellow with Genentech during the study but is now a cardiologist in private practice in Indianapolis.
The presence of a cardiac disorder increased the risk of MACE, with a hazard ratio of 2.32, and for each 1-unit increase in DAS28, age, and atherogenic index, MACE risk rose by 36%, 7%, and 33%, respectively.
Predictors of future risk of MACE following the trials’ initial 24-week treatment period remained largely the same as baseline predictors for MACE during initial treatment, including measures of higher disease activity.
In contrast, baseline and 24-week levels of systemic markers of inflammation such as erythrocyte sedimentation rate (ESR) and C-reactive protein, as well as changes in ESR and interleukin-6 (IL-6) receptor levels and changes in lipid levels during 24 weeks of tocilizumab treatment, did not predict future risk of MACE.
The IL-6 receptor pathway is thought to play a role in cardiovascular disease, and tocilizumab’s action as a monoclonal antibody against that receptor suggested that its effects might reduce CV risk. However, baseline levels of IL-6 and IL-6 receptor, or levels of IL-6 receptor at 24 weeks, were not associated with MACE.
The investigators found 50 confirmed cases of MACE in pooled data from five randomized, controlled trials and their extension studies that enrolled 3,986 patients with moderate to severe RA who received tocilizumab 4 mg/kg or 8 mg/kg intravenously every 4 weeks in combination with methotrexate or other disease-modifying antirheumatic drugs. The MACE rate was 3.4/1,000 patient-years of exposure, and there were no obvious time trends observed.
Because the trials used in the post hoc analyses were not specifically powered for analyzing MACE risk, the findings should be viewed as “hypothesis generating,” the investigators said.
They also noted that because 31% of patients in the trials discontinued treatment and MACE cases that occurred beyond 6 months after discontinuation were not recorded, there is a chance that those who withdrew were at a different risk for MACE than were those who remained on treatment. They also did not evaluate hypertension and use of statins, antiplatelet medications, or glucocorticoids.
The findings support a previous registry study in which MI risk was halved in responders to antitumor necrosis factor-alpha therapy, compared with nonresponders, according to the authors, as well as in several observational studies in which control of disease activity with nonbiologic DMARDs was associated with lower risk for MI.
The study was funded by F. Hoffmann-La Roche, of which the manufacturer of tocilizumab, Genentech, is a subsidiary. Five of the nine authors were employed by or received funding from Roche or Genentech at the time of the study, two were consultants or received speaking fees from Roche or Genentech, and the remaining two had no disclosures.

|
Dr. Katherine P. Liao |
Dr. Rao and his colleagues’ analysis is “reassuring” in showing a lack of cardiovascular events seen in the pooled data for tocilizumab, but it “cannot provide definitive answers regarding the safety of tocilizumab,” according to Dr. Katherine P. Liao and Dr. Daniel H. Solomon.
An ongoing, randomized, open-label study of CV events in rheumatoid arthritis patients on tocilizumab and etanercept, as well as observational studies comparing tocilizumab and other biologic DMARDs, should provide more important safety information, they noted.
The pooled data analysis highlights additional evidence to support RA disease activity as an important CV risk factor. And it provides additional evidence showing that total cholesterol and LDL cholesterol “may be suboptimal measures to guide CV risk estimation and preventative interventions, since levels appear to fluctuate with therapy in an inverse manner,” Dr. Liao and Dr. Solomon wrote.
|
Dr. Daniel H. Solomon |
Studies that use advanced lipoprotein tests and those that more closely examine the “underlying mechanisms by which inflammation elevates CV risk in RA” have the potential to improve the accuracy of CV risk assessment in RA, they wrote.
Dr. Liao and Dr. Solomon are with the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston. Their comments are taken from an editorial accompanying the study by Dr. Rao and his associates (Arthritis Rheumatol. 2014 [doi:10.1002/art.38925]). Dr. Liao said that she has no disclosures. Dr. Solomon reported receiving research funding through Brigham and Women’s Hospital from Amgen, Lilly, and Pfizer, and has unpaid roles on trials funded by Bristol-Myers Squibb and Pfizer.

|
Dr. Katherine P. Liao |
Dr. Rao and his colleagues’ analysis is “reassuring” in showing a lack of cardiovascular events seen in the pooled data for tocilizumab, but it “cannot provide definitive answers regarding the safety of tocilizumab,” according to Dr. Katherine P. Liao and Dr. Daniel H. Solomon.
An ongoing, randomized, open-label study of CV events in rheumatoid arthritis patients on tocilizumab and etanercept, as well as observational studies comparing tocilizumab and other biologic DMARDs, should provide more important safety information, they noted.
The pooled data analysis highlights additional evidence to support RA disease activity as an important CV risk factor. And it provides additional evidence showing that total cholesterol and LDL cholesterol “may be suboptimal measures to guide CV risk estimation and preventative interventions, since levels appear to fluctuate with therapy in an inverse manner,” Dr. Liao and Dr. Solomon wrote.
|
Dr. Daniel H. Solomon |
Studies that use advanced lipoprotein tests and those that more closely examine the “underlying mechanisms by which inflammation elevates CV risk in RA” have the potential to improve the accuracy of CV risk assessment in RA, they wrote.
Dr. Liao and Dr. Solomon are with the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston. Their comments are taken from an editorial accompanying the study by Dr. Rao and his associates (Arthritis Rheumatol. 2014 [doi:10.1002/art.38925]). Dr. Liao said that she has no disclosures. Dr. Solomon reported receiving research funding through Brigham and Women’s Hospital from Amgen, Lilly, and Pfizer, and has unpaid roles on trials funded by Bristol-Myers Squibb and Pfizer.

|
Dr. Katherine P. Liao |
Dr. Rao and his colleagues’ analysis is “reassuring” in showing a lack of cardiovascular events seen in the pooled data for tocilizumab, but it “cannot provide definitive answers regarding the safety of tocilizumab,” according to Dr. Katherine P. Liao and Dr. Daniel H. Solomon.
An ongoing, randomized, open-label study of CV events in rheumatoid arthritis patients on tocilizumab and etanercept, as well as observational studies comparing tocilizumab and other biologic DMARDs, should provide more important safety information, they noted.
The pooled data analysis highlights additional evidence to support RA disease activity as an important CV risk factor. And it provides additional evidence showing that total cholesterol and LDL cholesterol “may be suboptimal measures to guide CV risk estimation and preventative interventions, since levels appear to fluctuate with therapy in an inverse manner,” Dr. Liao and Dr. Solomon wrote.
|
Dr. Daniel H. Solomon |
Studies that use advanced lipoprotein tests and those that more closely examine the “underlying mechanisms by which inflammation elevates CV risk in RA” have the potential to improve the accuracy of CV risk assessment in RA, they wrote.
Dr. Liao and Dr. Solomon are with the division of rheumatology, immunology, and allergy at Brigham and Women’s Hospital, Boston. Their comments are taken from an editorial accompanying the study by Dr. Rao and his associates (Arthritis Rheumatol. 2014 [doi:10.1002/art.38925]). Dr. Liao said that she has no disclosures. Dr. Solomon reported receiving research funding through Brigham and Women’s Hospital from Amgen, Lilly, and Pfizer, and has unpaid roles on trials funded by Bristol-Myers Squibb and Pfizer.
Rheumatoid arthritis disease activity during treatment with tocilizumab plays a significant role in patients’ risk for major adverse cardiovascular events, rather than increases in lipid levels observed during treatment with the interleukin-6 receptor inhibitor, according to a new analysis of phase III trials and extensions studies of the drug.
The study of 3,986 rheumatoid arthritis (RA) patients treated with tocilizumab for a mean of 3.68 years indicated that reductions in disease activity based on lower 28-joint disease activity score (DAS28) were significantly associated with fewer major adverse cardiovascular events (MACE), defined as definite or probable nonfatal myocardial infarction, nonfatal stroke, or death from a cardiovascular cause.
Conversely, risk for MACE rose with poorer response to treatment, as measured by increases in DAS28 and total swollen and tender joints (Arthritis Rheumatol. 2014 [doi:10.1002/art.38920]).
In addition to DAS28, some traditional risk factors at baseline – older age, history of cardiac disorders, and high ratio of total cholesterol to HDL cholesterol (known as the atherogenic index) – were independent predictors of MACE during treatment, reported Dr. Vijay U. Rao and his colleagues. Dr. Rao was a research fellow with Genentech during the study but is now a cardiologist in private practice in Indianapolis.
The presence of a cardiac disorder increased the risk of MACE, with a hazard ratio of 2.32, and for each 1-unit increase in DAS28, age, and atherogenic index, MACE risk rose by 36%, 7%, and 33%, respectively.
Predictors of future risk of MACE following the trials’ initial 24-week treatment period remained largely the same as baseline predictors for MACE during initial treatment, including measures of higher disease activity.
In contrast, baseline and 24-week levels of systemic markers of inflammation such as erythrocyte sedimentation rate (ESR) and C-reactive protein, as well as changes in ESR and interleukin-6 (IL-6) receptor levels and changes in lipid levels during 24 weeks of tocilizumab treatment, did not predict future risk of MACE.
The IL-6 receptor pathway is thought to play a role in cardiovascular disease, and tocilizumab’s action as a monoclonal antibody against that receptor suggested that its effects might reduce CV risk. However, baseline levels of IL-6 and IL-6 receptor, or levels of IL-6 receptor at 24 weeks, were not associated with MACE.
The investigators found 50 confirmed cases of MACE in pooled data from five randomized, controlled trials and their extension studies that enrolled 3,986 patients with moderate to severe RA who received tocilizumab 4 mg/kg or 8 mg/kg intravenously every 4 weeks in combination with methotrexate or other disease-modifying antirheumatic drugs. The MACE rate was 3.4/1,000 patient-years of exposure, and there were no obvious time trends observed.
Because the trials used in the post hoc analyses were not specifically powered for analyzing MACE risk, the findings should be viewed as “hypothesis generating,” the investigators said.
They also noted that because 31% of patients in the trials discontinued treatment and MACE cases that occurred beyond 6 months after discontinuation were not recorded, there is a chance that those who withdrew were at a different risk for MACE than were those who remained on treatment. They also did not evaluate hypertension and use of statins, antiplatelet medications, or glucocorticoids.
The findings support a previous registry study in which MI risk was halved in responders to antitumor necrosis factor-alpha therapy, compared with nonresponders, according to the authors, as well as in several observational studies in which control of disease activity with nonbiologic DMARDs was associated with lower risk for MI.
The study was funded by F. Hoffmann-La Roche, of which the manufacturer of tocilizumab, Genentech, is a subsidiary. Five of the nine authors were employed by or received funding from Roche or Genentech at the time of the study, two were consultants or received speaking fees from Roche or Genentech, and the remaining two had no disclosures.
Rheumatoid arthritis disease activity during treatment with tocilizumab plays a significant role in patients’ risk for major adverse cardiovascular events, rather than increases in lipid levels observed during treatment with the interleukin-6 receptor inhibitor, according to a new analysis of phase III trials and extensions studies of the drug.
The study of 3,986 rheumatoid arthritis (RA) patients treated with tocilizumab for a mean of 3.68 years indicated that reductions in disease activity based on lower 28-joint disease activity score (DAS28) were significantly associated with fewer major adverse cardiovascular events (MACE), defined as definite or probable nonfatal myocardial infarction, nonfatal stroke, or death from a cardiovascular cause.
Conversely, risk for MACE rose with poorer response to treatment, as measured by increases in DAS28 and total swollen and tender joints (Arthritis Rheumatol. 2014 [doi:10.1002/art.38920]).
In addition to DAS28, some traditional risk factors at baseline – older age, history of cardiac disorders, and high ratio of total cholesterol to HDL cholesterol (known as the atherogenic index) – were independent predictors of MACE during treatment, reported Dr. Vijay U. Rao and his colleagues. Dr. Rao was a research fellow with Genentech during the study but is now a cardiologist in private practice in Indianapolis.
The presence of a cardiac disorder increased the risk of MACE, with a hazard ratio of 2.32, and for each 1-unit increase in DAS28, age, and atherogenic index, MACE risk rose by 36%, 7%, and 33%, respectively.
Predictors of future risk of MACE following the trials’ initial 24-week treatment period remained largely the same as baseline predictors for MACE during initial treatment, including measures of higher disease activity.
In contrast, baseline and 24-week levels of systemic markers of inflammation such as erythrocyte sedimentation rate (ESR) and C-reactive protein, as well as changes in ESR and interleukin-6 (IL-6) receptor levels and changes in lipid levels during 24 weeks of tocilizumab treatment, did not predict future risk of MACE.
The IL-6 receptor pathway is thought to play a role in cardiovascular disease, and tocilizumab’s action as a monoclonal antibody against that receptor suggested that its effects might reduce CV risk. However, baseline levels of IL-6 and IL-6 receptor, or levels of IL-6 receptor at 24 weeks, were not associated with MACE.
The investigators found 50 confirmed cases of MACE in pooled data from five randomized, controlled trials and their extension studies that enrolled 3,986 patients with moderate to severe RA who received tocilizumab 4 mg/kg or 8 mg/kg intravenously every 4 weeks in combination with methotrexate or other disease-modifying antirheumatic drugs. The MACE rate was 3.4/1,000 patient-years of exposure, and there were no obvious time trends observed.
Because the trials used in the post hoc analyses were not specifically powered for analyzing MACE risk, the findings should be viewed as “hypothesis generating,” the investigators said.
They also noted that because 31% of patients in the trials discontinued treatment and MACE cases that occurred beyond 6 months after discontinuation were not recorded, there is a chance that those who withdrew were at a different risk for MACE than were those who remained on treatment. They also did not evaluate hypertension and use of statins, antiplatelet medications, or glucocorticoids.
The findings support a previous registry study in which MI risk was halved in responders to antitumor necrosis factor-alpha therapy, compared with nonresponders, according to the authors, as well as in several observational studies in which control of disease activity with nonbiologic DMARDs was associated with lower risk for MI.
The study was funded by F. Hoffmann-La Roche, of which the manufacturer of tocilizumab, Genentech, is a subsidiary. Five of the nine authors were employed by or received funding from Roche or Genentech at the time of the study, two were consultants or received speaking fees from Roche or Genentech, and the remaining two had no disclosures.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Disease activity, rather than lipid levels, is an independent predictor of cardiovascular event risk during treatment with tocilizumab.
Major finding: The presence of a cardiac disorder increased the risk of MACE, with a hazard ratio of 2.32; for each 1-unit increase in DAS28, age, and atherogenic index, MACE risk rose by 36%, 7%, and 33%, respectively.
Data source: A post hoc analysis of 3,986 patients with rheumatoid arthritis from five tocilizumab randomized, controlled trials and extension studies.
Disclosures: The study was funded by F. Hoffmann-La Roche, of which the manufacturer of tocilizumab, Genentech, is a subsidiary. Five of the nine authors were employed by or received funding from Roche or Genentech at the time of the study, two were consultants or received speaking fees from Roche or Genentech, and the remaining two had no disclosures.
Federal industry foundations partnership for RA, lupus research awards first grants
A total of 11 new research grants have been awarded by the National Institutes of Health as part of the first year of funding for the Accelerating Medicines Partnership in Rheumatoid Arthritis and Lupus.
The $6 million in first-year funding, part of $41.6 million slated for the two autoimmune diseases over a 5-year period as part of the broader Accelerating Medicines Partnership in Rheumatoid Arthritis and Systemic Lupus Erythematosus (AMP RA/SLE) Program was announced Sept. 24.
Over 5 years, the AMP RA/Lupus Network will analyze the interplay among biologic pathways, including at the single cell level, in tissues of patients with RA and lupus. The goal is to integrate data from multiple genome-wide analytic approaches to generate a comprehensive understanding of the mechanisms of tissue damage in RA and lupus.
The AMP RA/SLE Program is funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and National Institute of Allergy and Infectious Diseases (NIAID), and the following members of the AMP: AbbVie, Bristol-Myers Squibb, Merck, Pfizer, Sanofi, Takeda, the Arthritis Foundation, the Lupus Foundation of America, the Lupus Research Institute/Alliance for Lupus Research, and the Rheumatology Research Foundation.
“To date, treatments for RA and lupus have been aimed at decreasing inflammation and pain,” Dr. Stephen I. Katz, director of NIAMS, said in a written statement. “For the first time, we are bringing together multidisciplinary research teams to achieve a broad, systems-level understanding of these diseases, setting the stage for the development of more effective diagnostic and treatment approaches.”
Dr. Anthony S. Fauci, director of NIAID, added: “This program promises to lead to more diagnosis and treatment options for rheumatoid arthritis and lupus. We also anticipate that the flexibility of the program will enable investigators to advance research on related diseases, thus improving our overall understanding of autoimmunity.”
In addition to the AMP RA/Lupus Network’s leadership center, led by Dr. Paul J. Utz of Stanford (Calif.) University and Dr. V. Michael Holers of the University of Colorado, Denver, the 11 grants were awarded to research teams at sites that perform clinical research, technology research, or both. For a list of the research sites and descriptions of the proposed research, click here.
A total of 11 new research grants have been awarded by the National Institutes of Health as part of the first year of funding for the Accelerating Medicines Partnership in Rheumatoid Arthritis and Lupus.
The $6 million in first-year funding, part of $41.6 million slated for the two autoimmune diseases over a 5-year period as part of the broader Accelerating Medicines Partnership in Rheumatoid Arthritis and Systemic Lupus Erythematosus (AMP RA/SLE) Program was announced Sept. 24.
Over 5 years, the AMP RA/Lupus Network will analyze the interplay among biologic pathways, including at the single cell level, in tissues of patients with RA and lupus. The goal is to integrate data from multiple genome-wide analytic approaches to generate a comprehensive understanding of the mechanisms of tissue damage in RA and lupus.
The AMP RA/SLE Program is funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and National Institute of Allergy and Infectious Diseases (NIAID), and the following members of the AMP: AbbVie, Bristol-Myers Squibb, Merck, Pfizer, Sanofi, Takeda, the Arthritis Foundation, the Lupus Foundation of America, the Lupus Research Institute/Alliance for Lupus Research, and the Rheumatology Research Foundation.
“To date, treatments for RA and lupus have been aimed at decreasing inflammation and pain,” Dr. Stephen I. Katz, director of NIAMS, said in a written statement. “For the first time, we are bringing together multidisciplinary research teams to achieve a broad, systems-level understanding of these diseases, setting the stage for the development of more effective diagnostic and treatment approaches.”
Dr. Anthony S. Fauci, director of NIAID, added: “This program promises to lead to more diagnosis and treatment options for rheumatoid arthritis and lupus. We also anticipate that the flexibility of the program will enable investigators to advance research on related diseases, thus improving our overall understanding of autoimmunity.”
In addition to the AMP RA/Lupus Network’s leadership center, led by Dr. Paul J. Utz of Stanford (Calif.) University and Dr. V. Michael Holers of the University of Colorado, Denver, the 11 grants were awarded to research teams at sites that perform clinical research, technology research, or both. For a list of the research sites and descriptions of the proposed research, click here.
A total of 11 new research grants have been awarded by the National Institutes of Health as part of the first year of funding for the Accelerating Medicines Partnership in Rheumatoid Arthritis and Lupus.
The $6 million in first-year funding, part of $41.6 million slated for the two autoimmune diseases over a 5-year period as part of the broader Accelerating Medicines Partnership in Rheumatoid Arthritis and Systemic Lupus Erythematosus (AMP RA/SLE) Program was announced Sept. 24.
Over 5 years, the AMP RA/Lupus Network will analyze the interplay among biologic pathways, including at the single cell level, in tissues of patients with RA and lupus. The goal is to integrate data from multiple genome-wide analytic approaches to generate a comprehensive understanding of the mechanisms of tissue damage in RA and lupus.
The AMP RA/SLE Program is funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and National Institute of Allergy and Infectious Diseases (NIAID), and the following members of the AMP: AbbVie, Bristol-Myers Squibb, Merck, Pfizer, Sanofi, Takeda, the Arthritis Foundation, the Lupus Foundation of America, the Lupus Research Institute/Alliance for Lupus Research, and the Rheumatology Research Foundation.
“To date, treatments for RA and lupus have been aimed at decreasing inflammation and pain,” Dr. Stephen I. Katz, director of NIAMS, said in a written statement. “For the first time, we are bringing together multidisciplinary research teams to achieve a broad, systems-level understanding of these diseases, setting the stage for the development of more effective diagnostic and treatment approaches.”
Dr. Anthony S. Fauci, director of NIAID, added: “This program promises to lead to more diagnosis and treatment options for rheumatoid arthritis and lupus. We also anticipate that the flexibility of the program will enable investigators to advance research on related diseases, thus improving our overall understanding of autoimmunity.”
In addition to the AMP RA/Lupus Network’s leadership center, led by Dr. Paul J. Utz of Stanford (Calif.) University and Dr. V. Michael Holers of the University of Colorado, Denver, the 11 grants were awarded to research teams at sites that perform clinical research, technology research, or both. For a list of the research sites and descriptions of the proposed research, click here.
VIDEO: Novel sphingosine 1-phosphate 1 receptor modulator has promising safety results
BOSTON – Treatment of relapsing-remitting multiple sclerosis patients with the investigational drug RPC1063, a selective, oral sphingosine 1-phosphate 1 receptor modulator, in the phase II RADIANCE trial generated few concerns about potential cardiac events or elevated liver enzymes.
These initial clinical trial results of RPC1063 hint at a potentially better safety profile than the approved sphingosine 1-phosphate receptor modulator fingolimod, which has a high affinity for the sphingosine 1-phosphate 1, 3, 4, and 5 receptor subtypes. Its affinity for the sphingosine 1-phosphate 3 and 4 subtypes are thought to contribute to its potential for cardiac adverse events. RPC1063 could prove to be a safer drug because of its specificity for sphingosine 1-phosphate receptor subtype 1, according to Dr. Jeffrey Cohen, director of the Mellon Center for Multiple Sclerosis at the Cleveland Clinic and primary investigator for the RADIANCE trial. Dr. Cohen spoke with us at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Treatment of relapsing-remitting multiple sclerosis patients with the investigational drug RPC1063, a selective, oral sphingosine 1-phosphate 1 receptor modulator, in the phase II RADIANCE trial generated few concerns about potential cardiac events or elevated liver enzymes.
These initial clinical trial results of RPC1063 hint at a potentially better safety profile than the approved sphingosine 1-phosphate receptor modulator fingolimod, which has a high affinity for the sphingosine 1-phosphate 1, 3, 4, and 5 receptor subtypes. Its affinity for the sphingosine 1-phosphate 3 and 4 subtypes are thought to contribute to its potential for cardiac adverse events. RPC1063 could prove to be a safer drug because of its specificity for sphingosine 1-phosphate receptor subtype 1, according to Dr. Jeffrey Cohen, director of the Mellon Center for Multiple Sclerosis at the Cleveland Clinic and primary investigator for the RADIANCE trial. Dr. Cohen spoke with us at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Treatment of relapsing-remitting multiple sclerosis patients with the investigational drug RPC1063, a selective, oral sphingosine 1-phosphate 1 receptor modulator, in the phase II RADIANCE trial generated few concerns about potential cardiac events or elevated liver enzymes.
These initial clinical trial results of RPC1063 hint at a potentially better safety profile than the approved sphingosine 1-phosphate receptor modulator fingolimod, which has a high affinity for the sphingosine 1-phosphate 1, 3, 4, and 5 receptor subtypes. Its affinity for the sphingosine 1-phosphate 3 and 4 subtypes are thought to contribute to its potential for cardiac adverse events. RPC1063 could prove to be a safer drug because of its specificity for sphingosine 1-phosphate receptor subtype 1, according to Dr. Jeffrey Cohen, director of the Mellon Center for Multiple Sclerosis at the Cleveland Clinic and primary investigator for the RADIANCE trial. Dr. Cohen spoke with us at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At MSBoston 2014
VIDEO: Predicting time to relapse after CIS in largest-ever study of high-risk patients
BOSTON – When trying to predict how quickly high-risk patients with clinically isolated syndrome may convert to clinically definite multiple sclerosis, consider age at onset, disease-modifying drug use, MRI lesion load, and the presence of cerebrospinal fluid oligoclonal bands, according to Dr. Tim Spelman.
Dr. Spelman and his colleagues analyzed the MSBase Incident Study subset of high-risk patients from the MSBase Registry to conduct the largest longitudinal, prospective study of patients followed from onset of clinically isolated syndrome (CIS).
Older age at CIS was protective for conversion to clinically definite MS. The basis for how older age at onset lowers risk “is still somewhat of a mystery because the variable itself doesn’t correlate with other known predictors like oligoclonal bands, MRI, EDSS [Expanded Disease Status Scale],” Dr. Spelman said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. Spinal lesions on MRI also tended to capture about the same amount of risk at baseline as did oligoclonal bands, he noted. Treatment with disease-modifying drugs (DMDs) extended the median time to conversion from 11 months without treatment to 4 years with treatment, regardless of the DMD type or duration.
With all of these predictors assembled, the next phase is to develop a risk calculator, said Dr. Spelman of the Melbourne Brain Centre at the Royal Melbourne Hospital in Parkville, Australia.
[email protected]
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – When trying to predict how quickly high-risk patients with clinically isolated syndrome may convert to clinically definite multiple sclerosis, consider age at onset, disease-modifying drug use, MRI lesion load, and the presence of cerebrospinal fluid oligoclonal bands, according to Dr. Tim Spelman.
Dr. Spelman and his colleagues analyzed the MSBase Incident Study subset of high-risk patients from the MSBase Registry to conduct the largest longitudinal, prospective study of patients followed from onset of clinically isolated syndrome (CIS).
Older age at CIS was protective for conversion to clinically definite MS. The basis for how older age at onset lowers risk “is still somewhat of a mystery because the variable itself doesn’t correlate with other known predictors like oligoclonal bands, MRI, EDSS [Expanded Disease Status Scale],” Dr. Spelman said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. Spinal lesions on MRI also tended to capture about the same amount of risk at baseline as did oligoclonal bands, he noted. Treatment with disease-modifying drugs (DMDs) extended the median time to conversion from 11 months without treatment to 4 years with treatment, regardless of the DMD type or duration.
With all of these predictors assembled, the next phase is to develop a risk calculator, said Dr. Spelman of the Melbourne Brain Centre at the Royal Melbourne Hospital in Parkville, Australia.
[email protected]
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – When trying to predict how quickly high-risk patients with clinically isolated syndrome may convert to clinically definite multiple sclerosis, consider age at onset, disease-modifying drug use, MRI lesion load, and the presence of cerebrospinal fluid oligoclonal bands, according to Dr. Tim Spelman.
Dr. Spelman and his colleagues analyzed the MSBase Incident Study subset of high-risk patients from the MSBase Registry to conduct the largest longitudinal, prospective study of patients followed from onset of clinically isolated syndrome (CIS).
Older age at CIS was protective for conversion to clinically definite MS. The basis for how older age at onset lowers risk “is still somewhat of a mystery because the variable itself doesn’t correlate with other known predictors like oligoclonal bands, MRI, EDSS [Expanded Disease Status Scale],” Dr. Spelman said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. Spinal lesions on MRI also tended to capture about the same amount of risk at baseline as did oligoclonal bands, he noted. Treatment with disease-modifying drugs (DMDs) extended the median time to conversion from 11 months without treatment to 4 years with treatment, regardless of the DMD type or duration.
With all of these predictors assembled, the next phase is to develop a risk calculator, said Dr. Spelman of the Melbourne Brain Centre at the Royal Melbourne Hospital in Parkville, Australia.
[email protected]
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT MSBOSTON 2014
VIDEO: Grants launch large-scale collaboration against progressive MS
BOSTON – The International Progressive MS Alliance has announced the first round of grants to fund groundbreaking research on progressive forms of multiple sclerosis.
A panel of more than 40 experts in multiple sclerosis (MS) reviewed 195 research proposals received from 22 countries. The panel chose to make 22 “challenge” grants to researchers in nine countries. The grants will fund 1- to 2-year pilot studies that represent the first steps in a program that will cumulatively invest nearly $30 million over a 5-year period.
“This is the first time we’ve had a truly global, international initiative,” said Dr. Alan Thompson, chair of the alliance’s scientific steering committee and a neurologist and professor at University College London Faculty on Brain Sciences. “It’s much more about being a catalyst to bring together the best institutions worldwide.”
The announcement was made at a press conference held during the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis, although the press conference was not officially part of the meeting.
Seven of the grants were made to researchers investigating potential new treatments as well as biomarkers and outcome measures that could be used to track disease progression in clinical trials. Another seven funded studies will seek to understand the underlying cause of progressive disease. One grant-winning study aims to discover biomarkers that reflect progression pathophysiology for primary progressive MS.
Three studies will investigate the genetics of progressive subtypes of MS. Two will be used to develop animal models of progressive MS. Two will investigate new rehabilitative methods for patients with progressive disease.
The next step is for the alliance to provide 4 years of funding for a global, collaborative research network of about 10 centers. The next call for research proposals will come at the beginning of November 2014.
In a video interview, we spoke with one of the grant award winners, Francisco Quintana, Ph.D., of Brigham and Women’s Hospital, Boston, about his research proposal and views on the initiative.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The International Progressive MS Alliance has announced the first round of grants to fund groundbreaking research on progressive forms of multiple sclerosis.
A panel of more than 40 experts in multiple sclerosis (MS) reviewed 195 research proposals received from 22 countries. The panel chose to make 22 “challenge” grants to researchers in nine countries. The grants will fund 1- to 2-year pilot studies that represent the first steps in a program that will cumulatively invest nearly $30 million over a 5-year period.
“This is the first time we’ve had a truly global, international initiative,” said Dr. Alan Thompson, chair of the alliance’s scientific steering committee and a neurologist and professor at University College London Faculty on Brain Sciences. “It’s much more about being a catalyst to bring together the best institutions worldwide.”
The announcement was made at a press conference held during the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis, although the press conference was not officially part of the meeting.
Seven of the grants were made to researchers investigating potential new treatments as well as biomarkers and outcome measures that could be used to track disease progression in clinical trials. Another seven funded studies will seek to understand the underlying cause of progressive disease. One grant-winning study aims to discover biomarkers that reflect progression pathophysiology for primary progressive MS.
Three studies will investigate the genetics of progressive subtypes of MS. Two will be used to develop animal models of progressive MS. Two will investigate new rehabilitative methods for patients with progressive disease.
The next step is for the alliance to provide 4 years of funding for a global, collaborative research network of about 10 centers. The next call for research proposals will come at the beginning of November 2014.
In a video interview, we spoke with one of the grant award winners, Francisco Quintana, Ph.D., of Brigham and Women’s Hospital, Boston, about his research proposal and views on the initiative.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The International Progressive MS Alliance has announced the first round of grants to fund groundbreaking research on progressive forms of multiple sclerosis.
A panel of more than 40 experts in multiple sclerosis (MS) reviewed 195 research proposals received from 22 countries. The panel chose to make 22 “challenge” grants to researchers in nine countries. The grants will fund 1- to 2-year pilot studies that represent the first steps in a program that will cumulatively invest nearly $30 million over a 5-year period.
“This is the first time we’ve had a truly global, international initiative,” said Dr. Alan Thompson, chair of the alliance’s scientific steering committee and a neurologist and professor at University College London Faculty on Brain Sciences. “It’s much more about being a catalyst to bring together the best institutions worldwide.”
The announcement was made at a press conference held during the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis, although the press conference was not officially part of the meeting.
Seven of the grants were made to researchers investigating potential new treatments as well as biomarkers and outcome measures that could be used to track disease progression in clinical trials. Another seven funded studies will seek to understand the underlying cause of progressive disease. One grant-winning study aims to discover biomarkers that reflect progression pathophysiology for primary progressive MS.
Three studies will investigate the genetics of progressive subtypes of MS. Two will be used to develop animal models of progressive MS. Two will investigate new rehabilitative methods for patients with progressive disease.
The next step is for the alliance to provide 4 years of funding for a global, collaborative research network of about 10 centers. The next call for research proposals will come at the beginning of November 2014.
In a video interview, we spoke with one of the grant award winners, Francisco Quintana, Ph.D., of Brigham and Women’s Hospital, Boston, about his research proposal and views on the initiative.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Axial MRI better identifies extent of MS lesions in the cervical spinal cord
BOSTON – 3-Tesla axial MR imaging in patients with multiple sclerosis can reveal important information about the extent of lesions in the cervical spinal cord that differentiates milder forms of disease from progressive subtypes, according to new research presented by Dr. Hugh Kearney at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
While most MRI studies of the cervical spinal cord have used sagittal views to determine the number of lesions, axial views can show the extent of lesions and the involvement of gray matter that goes unseen with sagittal views, Dr. Kearney, a researcher at the University College London Institute of Neurology, said in a video interview.
In a study of 120 patients, Dr. Kearney and his colleagues found that this MRI technique, which used a fine resolution of 0.5-by-0.5 mm2, detected extensive focal lesions involving multiple white matter columns significantly more often among patients with progressive subtypes of MS, whereas patients with relapsing remitting disease or clinically isolated syndrome tended to have lesions usually limited to a single spinal cord column. Patients with progressive subtypes also more commonly had involvement of the gray matter and diffuse abnormalities. The presence of lateral column lesions involving gray matter and the number of columns involved was an independent predictor of disability on the Expanded Disability Status Scale.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – 3-Tesla axial MR imaging in patients with multiple sclerosis can reveal important information about the extent of lesions in the cervical spinal cord that differentiates milder forms of disease from progressive subtypes, according to new research presented by Dr. Hugh Kearney at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
While most MRI studies of the cervical spinal cord have used sagittal views to determine the number of lesions, axial views can show the extent of lesions and the involvement of gray matter that goes unseen with sagittal views, Dr. Kearney, a researcher at the University College London Institute of Neurology, said in a video interview.
In a study of 120 patients, Dr. Kearney and his colleagues found that this MRI technique, which used a fine resolution of 0.5-by-0.5 mm2, detected extensive focal lesions involving multiple white matter columns significantly more often among patients with progressive subtypes of MS, whereas patients with relapsing remitting disease or clinically isolated syndrome tended to have lesions usually limited to a single spinal cord column. Patients with progressive subtypes also more commonly had involvement of the gray matter and diffuse abnormalities. The presence of lateral column lesions involving gray matter and the number of columns involved was an independent predictor of disability on the Expanded Disability Status Scale.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – 3-Tesla axial MR imaging in patients with multiple sclerosis can reveal important information about the extent of lesions in the cervical spinal cord that differentiates milder forms of disease from progressive subtypes, according to new research presented by Dr. Hugh Kearney at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
While most MRI studies of the cervical spinal cord have used sagittal views to determine the number of lesions, axial views can show the extent of lesions and the involvement of gray matter that goes unseen with sagittal views, Dr. Kearney, a researcher at the University College London Institute of Neurology, said in a video interview.
In a study of 120 patients, Dr. Kearney and his colleagues found that this MRI technique, which used a fine resolution of 0.5-by-0.5 mm2, detected extensive focal lesions involving multiple white matter columns significantly more often among patients with progressive subtypes of MS, whereas patients with relapsing remitting disease or clinically isolated syndrome tended to have lesions usually limited to a single spinal cord column. Patients with progressive subtypes also more commonly had involvement of the gray matter and diffuse abnormalities. The presence of lateral column lesions involving gray matter and the number of columns involved was an independent predictor of disability on the Expanded Disability Status Scale.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT MSBOSTON 2014
VIDEO: Genetic, environmental, clinical data converge on cause of multiple sclerosis
BOSTON – A model for explaining the pathogenesis of multiple sclerosis is beginning to come together faster than ever before thanks to a wide range of methods that have allowed researchers to find disease-associated gene variants and examine their interaction with environmental factors, according to Dr. David A. Hafler, professor of neurology and immunobiology at Yale University in New Haven, Conn.
Researchers in the International MS Genetics Consortium have used new techniques to analyze the genomes of large cohorts of patients with MS and revealed many single-nucleotide polymorphism variants that affect immune activation that had not been considered before, allowing researchers to identify which immune cells are involved in the disease, Dr. Hafler said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
He and his colleagues also recently have found that areas of the genome that are open to transcription in the T and B cells of patients with MS involve transcription factors that interact with environmental stimuli -- such as smoking, salt intake, lower vitamin D, higher body mass index, and exposure to Epstein-Barr virus -- to lower the threshold of T-cell activation in genetically susceptible individuals, leading to the development of myelin-reactive T cells that secrete pro-inflammatory cytokines such as interleukin-17.
Additional evidence to support the role of immune dysregulation comes from clinical trials in MS that have involved blocking interleukin-17 with the investigational secukinumab and blocking the traffic of T cells to the central nervous system with drugs like fingolimod and natalizumab.
But even with all the knowledge that’s been acquired, Dr. Hafler said there is still much to discover, including how many and which environmental factors play a role; how disease susceptibility variants drive the activation of T cells; and what drives the disease process in secondary progressive MS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A model for explaining the pathogenesis of multiple sclerosis is beginning to come together faster than ever before thanks to a wide range of methods that have allowed researchers to find disease-associated gene variants and examine their interaction with environmental factors, according to Dr. David A. Hafler, professor of neurology and immunobiology at Yale University in New Haven, Conn.
Researchers in the International MS Genetics Consortium have used new techniques to analyze the genomes of large cohorts of patients with MS and revealed many single-nucleotide polymorphism variants that affect immune activation that had not been considered before, allowing researchers to identify which immune cells are involved in the disease, Dr. Hafler said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
He and his colleagues also recently have found that areas of the genome that are open to transcription in the T and B cells of patients with MS involve transcription factors that interact with environmental stimuli -- such as smoking, salt intake, lower vitamin D, higher body mass index, and exposure to Epstein-Barr virus -- to lower the threshold of T-cell activation in genetically susceptible individuals, leading to the development of myelin-reactive T cells that secrete pro-inflammatory cytokines such as interleukin-17.
Additional evidence to support the role of immune dysregulation comes from clinical trials in MS that have involved blocking interleukin-17 with the investigational secukinumab and blocking the traffic of T cells to the central nervous system with drugs like fingolimod and natalizumab.
But even with all the knowledge that’s been acquired, Dr. Hafler said there is still much to discover, including how many and which environmental factors play a role; how disease susceptibility variants drive the activation of T cells; and what drives the disease process in secondary progressive MS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A model for explaining the pathogenesis of multiple sclerosis is beginning to come together faster than ever before thanks to a wide range of methods that have allowed researchers to find disease-associated gene variants and examine their interaction with environmental factors, according to Dr. David A. Hafler, professor of neurology and immunobiology at Yale University in New Haven, Conn.
Researchers in the International MS Genetics Consortium have used new techniques to analyze the genomes of large cohorts of patients with MS and revealed many single-nucleotide polymorphism variants that affect immune activation that had not been considered before, allowing researchers to identify which immune cells are involved in the disease, Dr. Hafler said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis.
He and his colleagues also recently have found that areas of the genome that are open to transcription in the T and B cells of patients with MS involve transcription factors that interact with environmental stimuli -- such as smoking, salt intake, lower vitamin D, higher body mass index, and exposure to Epstein-Barr virus -- to lower the threshold of T-cell activation in genetically susceptible individuals, leading to the development of myelin-reactive T cells that secrete pro-inflammatory cytokines such as interleukin-17.
Additional evidence to support the role of immune dysregulation comes from clinical trials in MS that have involved blocking interleukin-17 with the investigational secukinumab and blocking the traffic of T cells to the central nervous system with drugs like fingolimod and natalizumab.
But even with all the knowledge that’s been acquired, Dr. Hafler said there is still much to discover, including how many and which environmental factors play a role; how disease susceptibility variants drive the activation of T cells; and what drives the disease process in secondary progressive MS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT MSBOSTON 2014
VIDEO: Cognitive impairment may affect pediatric- and adult-onset MS patients similarly
BOSTON – The cognitive outcomes of patients with pediatric-onset or adult-onset relapsing-remitting multiple sclerosis were similar in a small cross-sectional study of patients matched for age, educational level, and physical disability.
The results indicate that despite children’s vulnerability to cognitive deficits during brain maturation, those with pediatric-onset multiple sclerosis (MS) appear to have enough brain plasticity to compensate for the detrimental effects of the disease on cognition, according to Dr. Bahia Hakiki of the University of Florence in Italy.
She and her colleagues found that although 14 patients with pediatric-onset disease had longer mean disease duration than did 30 patients with adult-onset disease (9.8 years vs. 3.7 years) -- as was expected -- they had similar performances on Rao’s Brief Repeatable battery -- commonly used in MS cognitive assessment – and the Stroop test. There also was no difference in the percentage of patients who were classified as cognitively impaired (14% with pediatric onset vs. 30% with adult onset).
Brain MR imaging in a subset of patients found no difference in whole-brain volume, supporting the view that patients with pediatric-onset MS have the ability to compensate for the detrimental effects of MS on cognition, Dr. Hakiki said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. However, she noted that it will be important to study the impact of age at onset on this ability to recover and if it is a risk factor for worse cognitive impairment in adulthood.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The cognitive outcomes of patients with pediatric-onset or adult-onset relapsing-remitting multiple sclerosis were similar in a small cross-sectional study of patients matched for age, educational level, and physical disability.
The results indicate that despite children’s vulnerability to cognitive deficits during brain maturation, those with pediatric-onset multiple sclerosis (MS) appear to have enough brain plasticity to compensate for the detrimental effects of the disease on cognition, according to Dr. Bahia Hakiki of the University of Florence in Italy.
She and her colleagues found that although 14 patients with pediatric-onset disease had longer mean disease duration than did 30 patients with adult-onset disease (9.8 years vs. 3.7 years) -- as was expected -- they had similar performances on Rao’s Brief Repeatable battery -- commonly used in MS cognitive assessment – and the Stroop test. There also was no difference in the percentage of patients who were classified as cognitively impaired (14% with pediatric onset vs. 30% with adult onset).
Brain MR imaging in a subset of patients found no difference in whole-brain volume, supporting the view that patients with pediatric-onset MS have the ability to compensate for the detrimental effects of MS on cognition, Dr. Hakiki said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. However, she noted that it will be important to study the impact of age at onset on this ability to recover and if it is a risk factor for worse cognitive impairment in adulthood.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The cognitive outcomes of patients with pediatric-onset or adult-onset relapsing-remitting multiple sclerosis were similar in a small cross-sectional study of patients matched for age, educational level, and physical disability.
The results indicate that despite children’s vulnerability to cognitive deficits during brain maturation, those with pediatric-onset multiple sclerosis (MS) appear to have enough brain plasticity to compensate for the detrimental effects of the disease on cognition, according to Dr. Bahia Hakiki of the University of Florence in Italy.
She and her colleagues found that although 14 patients with pediatric-onset disease had longer mean disease duration than did 30 patients with adult-onset disease (9.8 years vs. 3.7 years) -- as was expected -- they had similar performances on Rao’s Brief Repeatable battery -- commonly used in MS cognitive assessment – and the Stroop test. There also was no difference in the percentage of patients who were classified as cognitively impaired (14% with pediatric onset vs. 30% with adult onset).
Brain MR imaging in a subset of patients found no difference in whole-brain volume, supporting the view that patients with pediatric-onset MS have the ability to compensate for the detrimental effects of MS on cognition, Dr. Hakiki said in a video interview at the joint meeting of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. However, she noted that it will be important to study the impact of age at onset on this ability to recover and if it is a risk factor for worse cognitive impairment in adulthood.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT MSBOSTON 2014