User login
Jeff Evans has been editor of Rheumatology News/MDedge Rheumatology and the EULAR Congress News since 2013. He started at Frontline Medical Communications in 2001 and was a reporter for 8 years before serving as editor of Clinical Neurology News and World Neurology, and briefly as editor of GI & Hepatology News. He graduated cum laude from Cornell University (New York) with a BA in biological sciences, concentrating in neurobiology and behavior.
VIDEO: Ultrasound of tendons detects early rheumatoid arthritis
ROME – Tenosynovitis on ultrasound might be the next criterion added to the diagnostic criteria for rheumatoid arthritis if it is confirmed as a valid marker for early disease detection, according to Dr. Andrew Filer.
He and his colleagues performed ultrasound assessments of 16 tendon regions in 107 patients in the Birmingham Early Arthritis Cohort Study (BEACON) who had clinically apparent synovitis involving at least one joint with a symptom duration of 3 months or less. They examined patient outcomes at 18 months.
Tenosynovitis in either the extensor carpi ulnaris tendons or the hand flexor tendons independently predicted early RA, and both were still significant independent predictors of early RA in seronegative patients, Dr. Filer of the University of Birmingham (England) said in this video interview at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ROME – Tenosynovitis on ultrasound might be the next criterion added to the diagnostic criteria for rheumatoid arthritis if it is confirmed as a valid marker for early disease detection, according to Dr. Andrew Filer.
He and his colleagues performed ultrasound assessments of 16 tendon regions in 107 patients in the Birmingham Early Arthritis Cohort Study (BEACON) who had clinically apparent synovitis involving at least one joint with a symptom duration of 3 months or less. They examined patient outcomes at 18 months.
Tenosynovitis in either the extensor carpi ulnaris tendons or the hand flexor tendons independently predicted early RA, and both were still significant independent predictors of early RA in seronegative patients, Dr. Filer of the University of Birmingham (England) said in this video interview at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ROME – Tenosynovitis on ultrasound might be the next criterion added to the diagnostic criteria for rheumatoid arthritis if it is confirmed as a valid marker for early disease detection, according to Dr. Andrew Filer.
He and his colleagues performed ultrasound assessments of 16 tendon regions in 107 patients in the Birmingham Early Arthritis Cohort Study (BEACON) who had clinically apparent synovitis involving at least one joint with a symptom duration of 3 months or less. They examined patient outcomes at 18 months.
Tenosynovitis in either the extensor carpi ulnaris tendons or the hand flexor tendons independently predicted early RA, and both were still significant independent predictors of early RA in seronegative patients, Dr. Filer of the University of Birmingham (England) said in this video interview at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EULAR 2015 CONGRESS
VIDEO: Primary care migraine knowledge needs help
WASHINGTON – The development of new educational and training opportunities to increase primary care physicians’ knowledge in diagnosing and managing migraine should extend from medical school student to on-the-job training for attending physicians, according to Dr. Mia Minen, who presented results of a comprehensive survey of primary care physicians’ knowledge about migraine at the annual meeting of the American Academy of Neurology.
Primary care physicians were unsure about when it is best to perform imaging in migraine patients and what kinds of medications are associated with medication overuse headache, said Dr. Minen of the department of neurology at NYU Langone Medical Center. She suggested that a wide range of physicians, including ob.gyns and emergency physicians, could benefit from better knowledge of migraine.
That position was echoed in an interview with Dr. Peter Goadsby of King’s College London and the University of California, San Francisco, who noted that a bigger headache curriculum in medical school and residencies, as well as more on-the-job education, would help greatly.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – The development of new educational and training opportunities to increase primary care physicians’ knowledge in diagnosing and managing migraine should extend from medical school student to on-the-job training for attending physicians, according to Dr. Mia Minen, who presented results of a comprehensive survey of primary care physicians’ knowledge about migraine at the annual meeting of the American Academy of Neurology.
Primary care physicians were unsure about when it is best to perform imaging in migraine patients and what kinds of medications are associated with medication overuse headache, said Dr. Minen of the department of neurology at NYU Langone Medical Center. She suggested that a wide range of physicians, including ob.gyns and emergency physicians, could benefit from better knowledge of migraine.
That position was echoed in an interview with Dr. Peter Goadsby of King’s College London and the University of California, San Francisco, who noted that a bigger headache curriculum in medical school and residencies, as well as more on-the-job education, would help greatly.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – The development of new educational and training opportunities to increase primary care physicians’ knowledge in diagnosing and managing migraine should extend from medical school student to on-the-job training for attending physicians, according to Dr. Mia Minen, who presented results of a comprehensive survey of primary care physicians’ knowledge about migraine at the annual meeting of the American Academy of Neurology.
Primary care physicians were unsure about when it is best to perform imaging in migraine patients and what kinds of medications are associated with medication overuse headache, said Dr. Minen of the department of neurology at NYU Langone Medical Center. She suggested that a wide range of physicians, including ob.gyns and emergency physicians, could benefit from better knowledge of migraine.
That position was echoed in an interview with Dr. Peter Goadsby of King’s College London and the University of California, San Francisco, who noted that a bigger headache curriculum in medical school and residencies, as well as more on-the-job education, would help greatly.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAN 2015 ANNUAL MEETING
Lower Diabetes Risk Seen in Lupus Patients Using Hydroxychloroquine
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
FROM RHEUMATOLOGY
Lower diabetes risk seen in lupus patients using hydroxychloroquine
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
The risk for developing diabetes mellitus among patients with systemic lupus erythematosus declined significantly with increasing use of hydroxychloroquine in a retrospective cohort study of a national health insurance database in Taiwan.
This population-based cohort study is the first to demonstrate that hydroxychloroquine (HCQ) reduces the risk of diabetes in a dose-dependent manner in systemic lupus erythematosus (SLE) patients. In previous research, HCQ use has been shown to improve insulin sensitivity in SLE patients, and in rheumatoid arthritis patients, longer duration of HCQ treatment (> 4 years) has been shown before to have the greatest effect on lowering the incidence of diabetes, according to Dr. Der-Yuan Chen of Taichung (Taiwan) Veterans General Hospital and his associates.
The investigators analyzed the first year of medication use in 8,628 patients with SLE in the National Health Insurance Research Database of Taiwan during 2001-2008, excluding those with less than 3 years of follow-up data and comorbid diagnoses of RA, psoriasis, or diabetes (Rheumatology [Oxford] 2015 Jan. 12 [doi:10.1093/rheumatology/keu451]).
The patients’ mean age was 37 years, and 88% were female. The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion had taken glucocorticoids (92% vs. 73%). Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease.
The effect of HCQ on diabetes risk became apparent in patients with an average daily glucocorticoid dose equivalent to 10 mg prednisolone or greater. That glucocorticoid dose was associated with increased diabetes risk (hazard ratio, 2.29; 95% confidence interval, 1.34-3.93), but a cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take the drug. There was no significant relationship between HCQ use and incident diabetes for those who had a cumulative dose of less than 129 g (HR, 1.13; 95% CI, 0.81-1.59).
Patients who took both an average daily glucocorticoid dose equivalent to at least 10 mg prednisolone and a cumulative dose of less than 129 g HCQ had a higher diabetes risk than did those taking a smaller prednisolone dose, whereas those who took at least 129 g HCQ had a reduced risk of diabetes despite taking high-dose glucocorticoids.
Hazard ratios for diabetes ranged from 0.10 to 0.41 among different groupings of patients who took at least 129 g HCQ, according to age, use of glucocorticoids or disease-modifying antirheumatic drugs, and presence of comorbidities.
The investigators noted that “there are substantial differences in the clinical characteristics of SLE patients with and without HCQ use ... [that] may reflect the discrepancy in lupus disease activity between the two groups.” The patients who had used HCQ were significantly older (49 years vs. 37 years) and a greater proportion of them had taken glucocorticoids (92% vs. 73%).
Those who had taken HCQ had significantly lower rates of hyperlipidemia, hypertension, stroke, and renal disease. HCQ users also took more methotrexate, sulfasalazine, and azathioprine, but less cyclophosphamide, than did those without HCQ use.
While the greater use of cyclophosphamide by HCQ nonusers may indicate more frequent lupus renal involvement and potentially bias them to increased risk of diabetes because of disease activity and chronic inflammation’s effect on insulin resistance, the greater cumulative glucocorticoid dose taken by HCQ users also can predispose to the development of diabetes, the authors said.
The study is limited in its ability to tease out the contributions of clinical characteristics between HCQ users and nonusers, because the patients’ lupus disease severity and laboratory data are unknown, and treatment data were recorded only from the first year. There was also a lack of data on lifestyle, body-mass index, and family history, the investigators said.
The study had no specific funding. The authors declared having no conflicts of interest.
FROM RHEUMATOLOGY
Key clinical point: Cumulative HCQ use of at least 129 g may be associated with lower risk of diabetes in patients with lupus and concomitant glucocorticoid use equivalent to 10 mg/day or more of prednisolone.
Major finding: A cumulative dose of 129 g HCQ or greater (equal to 200 mg/day for 1.8 years) reduced the risk of diabetes (HR, 0.26; 95% CI, 0.18-0.37), compared with those who did not take HCQ.
Data source: A retrospective cohort study of 8,628 patients with SLE in a national health insurance database in Taiwan.
Disclosures: The study had no specific funding. The authors declared having no conflicts of interest.
Intestinal carbidopa-levodopa gets FDA approval
The Food and Drug Administration approved an enteral suspension of carbidopa-levodopa on Jan. 12 under an orphan drug designation for the treatment of motor fluctuations in patients with advanced Parkinson’s disease.
The drug combination, to be marketed as Duopa in the United States, is infused into the jejunum through a surgically placed percutaneous endoscopic gastrostomy tube with a jejunal extension. A portable infusion pump, called the CADD-Legacy 1400, is worn by the patient for up to 16 hours per day, sending 4.63 mg carbidopa and 20 mg levodopa per mL into the jejunum. The maximum recommended daily dose is one cassette, equivalent to 2,000 mg levodopa given over 16 hours, according to the label, which also advises that, prior to initiating Duopa, patients should be converted “from all forms of levodopa to oral immediate-release carbidopa-levodopa tablets (1:4 ratio).”
The rationale for the direct administration of Duopa to the small intestine is the need for a more efficacious way for patients with advanced disease to reduce periods of “off” time in which they experience poor mobility, slowness, and stiffness. Direct administration also bypasses the reduced frequency and predictability of spontaneous gastric emptying seen in patients with advanced disease that can affect “the timing of when orally administered medicines leave the stomach and are absorbed in the small intestine,” according to the manufacturer, AbbVie.
The approval is based on a 12-week, phase III trial of Duopa in 71 patients with advanced Parkinson’s that resulted in 1.9 fewer hours of “off” time and 1.9 more hours of “on” time without dyskinesia per day, compared with patients who were taking immediate-release, oral doses of carbidopa-levodopa.
The carbidopa-levodopa enteral suspension is currently marketed by AbbVie under the name Duodopa in 40 other countries.
The Food and Drug Administration approved an enteral suspension of carbidopa-levodopa on Jan. 12 under an orphan drug designation for the treatment of motor fluctuations in patients with advanced Parkinson’s disease.
The drug combination, to be marketed as Duopa in the United States, is infused into the jejunum through a surgically placed percutaneous endoscopic gastrostomy tube with a jejunal extension. A portable infusion pump, called the CADD-Legacy 1400, is worn by the patient for up to 16 hours per day, sending 4.63 mg carbidopa and 20 mg levodopa per mL into the jejunum. The maximum recommended daily dose is one cassette, equivalent to 2,000 mg levodopa given over 16 hours, according to the label, which also advises that, prior to initiating Duopa, patients should be converted “from all forms of levodopa to oral immediate-release carbidopa-levodopa tablets (1:4 ratio).”
The rationale for the direct administration of Duopa to the small intestine is the need for a more efficacious way for patients with advanced disease to reduce periods of “off” time in which they experience poor mobility, slowness, and stiffness. Direct administration also bypasses the reduced frequency and predictability of spontaneous gastric emptying seen in patients with advanced disease that can affect “the timing of when orally administered medicines leave the stomach and are absorbed in the small intestine,” according to the manufacturer, AbbVie.
The approval is based on a 12-week, phase III trial of Duopa in 71 patients with advanced Parkinson’s that resulted in 1.9 fewer hours of “off” time and 1.9 more hours of “on” time without dyskinesia per day, compared with patients who were taking immediate-release, oral doses of carbidopa-levodopa.
The carbidopa-levodopa enteral suspension is currently marketed by AbbVie under the name Duodopa in 40 other countries.
The Food and Drug Administration approved an enteral suspension of carbidopa-levodopa on Jan. 12 under an orphan drug designation for the treatment of motor fluctuations in patients with advanced Parkinson’s disease.
The drug combination, to be marketed as Duopa in the United States, is infused into the jejunum through a surgically placed percutaneous endoscopic gastrostomy tube with a jejunal extension. A portable infusion pump, called the CADD-Legacy 1400, is worn by the patient for up to 16 hours per day, sending 4.63 mg carbidopa and 20 mg levodopa per mL into the jejunum. The maximum recommended daily dose is one cassette, equivalent to 2,000 mg levodopa given over 16 hours, according to the label, which also advises that, prior to initiating Duopa, patients should be converted “from all forms of levodopa to oral immediate-release carbidopa-levodopa tablets (1:4 ratio).”
The rationale for the direct administration of Duopa to the small intestine is the need for a more efficacious way for patients with advanced disease to reduce periods of “off” time in which they experience poor mobility, slowness, and stiffness. Direct administration also bypasses the reduced frequency and predictability of spontaneous gastric emptying seen in patients with advanced disease that can affect “the timing of when orally administered medicines leave the stomach and are absorbed in the small intestine,” according to the manufacturer, AbbVie.
The approval is based on a 12-week, phase III trial of Duopa in 71 patients with advanced Parkinson’s that resulted in 1.9 fewer hours of “off” time and 1.9 more hours of “on” time without dyskinesia per day, compared with patients who were taking immediate-release, oral doses of carbidopa-levodopa.
The carbidopa-levodopa enteral suspension is currently marketed by AbbVie under the name Duodopa in 40 other countries.
VIDEO: Collaborative clinic aims at heart of CVD prevention in rheumatic diseases
BOSTON – A multidisciplinary clinic of rheumatologists and cardiologists at the Mayo Clinic in Rochester, Minn., is focused on spreading awareness of cardiovascular disease in patients with rheumatic diseases and finding the best ways to prevent it.
The Cardio-Rheumatology Clinic, which was formed in 2013, is one of a growing number of clinics around the world that have started since the first Preventive Cardio-Rheuma Clinic opened at Diakonhjemmet Hospital in Oslo. Two of the founders of the Mayo Clinic’s Cardio-Rheumatology Clinic, Dr. Sharon L. Mulvagh and Dr. Sherine Gabriel, talk about its origins, goals, and vision in a video discussion at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A multidisciplinary clinic of rheumatologists and cardiologists at the Mayo Clinic in Rochester, Minn., is focused on spreading awareness of cardiovascular disease in patients with rheumatic diseases and finding the best ways to prevent it.
The Cardio-Rheumatology Clinic, which was formed in 2013, is one of a growing number of clinics around the world that have started since the first Preventive Cardio-Rheuma Clinic opened at Diakonhjemmet Hospital in Oslo. Two of the founders of the Mayo Clinic’s Cardio-Rheumatology Clinic, Dr. Sharon L. Mulvagh and Dr. Sherine Gabriel, talk about its origins, goals, and vision in a video discussion at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A multidisciplinary clinic of rheumatologists and cardiologists at the Mayo Clinic in Rochester, Minn., is focused on spreading awareness of cardiovascular disease in patients with rheumatic diseases and finding the best ways to prevent it.
The Cardio-Rheumatology Clinic, which was formed in 2013, is one of a growing number of clinics around the world that have started since the first Preventive Cardio-Rheuma Clinic opened at Diakonhjemmet Hospital in Oslo. Two of the founders of the Mayo Clinic’s Cardio-Rheumatology Clinic, Dr. Sharon L. Mulvagh and Dr. Sherine Gabriel, talk about its origins, goals, and vision in a video discussion at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
VIDEO: No Need to Stop Running for Fear of Knee Osteoarthritis
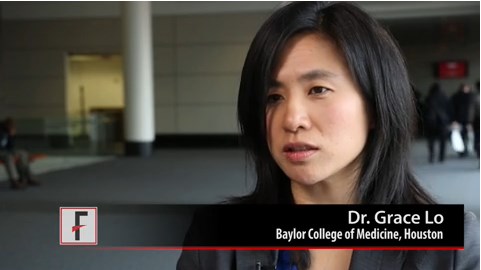
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
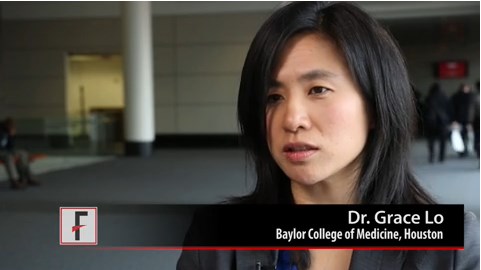
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
VIDEO: No need to stop running for fear of knee osteoarthritis
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– Current running or a history of running did not raise the odds of knee osteoarthritis in the first population-based study of runners.
Until this cross-sectional analysis of participants in the Osteoarthritis Initiative, most studies examining the risk of knee osteoarthritis from running analyzed elite runners and other high-level runners, making them less generalizable to a larger population, according to Dr. Grace Hsiao-Wei Lo of Baylor College of Medicine, Houston.
The findings of no higher odds of symptomatic knee osteoarthritis, compared with nonrunners, were largely consistent across age groupings of runners from 12-18 years of age up to 50 years and older, Dr. Lo said in a video interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
Running history doesn’t contribute to knee OA risk
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: There’s no need to restrict habitual running in people who don’t already have knee OA.
Major finding: Symptomatic radiographic OA occurred in 23% of runners and 30% of nonrunners
Data source: A cross-sectional study of 2,683 community-dwelling participants in the Osteoarthritis Initiative.
Disclosures: Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
OA patients benefit long term from exercise or manual therapy
BOSTON – Improvements in pain, stiffness, and physical function that occur with the addition of exercise therapy or manual therapy to usual care for patients at all stages of osteoarthritis extended out to 2 years in a randomized, controlled trial.
Although evidence already supports the use of exercise therapy or manual therapy for improving the symptoms and physical function of patients with osteoarthritis (OA), the trial is the first to show that either intervention provides benefits over and above that of usual care during the course of 2 years of follow-up.
The investigators, led by Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, randomized 206 patients who met American College of Rheumatology criteria for knee or hip OA to usual care alone, exercise therapy plus usual care, manual therapy plus usual care, or both interventions plus usual care.
Those who received one or both of the interventions underwent 10 treatment sessions, including 7 sessions within the first 9 weeks plus 3 booster sessions (2 at 4 months and 1 at 13 months). Between and after those sessions, participants carried out the interventions on their own.
Mean age of the patients was 66 years. The spectrum of OA ranged from mild to severe, with a mean Western Ontario and McMaster Universities (WOMAC) OA index score of 100.8. The patients had been recruited to the trial from primary care and orthopedic services, the investigators reported at the annual meeting of the American College of Rheumatology.
Exercise therapy consisted of strengthening, range-of-motion, neuromuscular coordination, and aerobics activities; manual therapy consisted of skilled passive movement to joints applied by external force. Physical therapists guided both interventions in one-on-one visits.
The 1-year results, which were published in 2013, showed significant decreases in pain and improvements in physical function in both single-intervention groups, but no significant improvement in the combined therapy group (Osteoarthritis Cartilage 2013;21:525-34).
Among the 186 patients who still remained in the study at 2 years of follow-up, scores on the WOMAC – the trial’s primary outcome – improved by 31.7 points in those who received exercise therapy plus usual care, compared with usual care alone, while patients receiving manual therapy in addition to usual care showed a relative improvement of 30.1 points. While the difference in WOMAC improvement for participants receiving combined exercise therapy and manual therapy in addition to usual care did not meet the a priori threshold for clinical significance (28 points), there was a trend toward benefit, with this group improving 26.2 points more than usual care only.
In all three intervention groups, Dr. Abbott noted that those changes represented greater than 20% declines in WOMAC scores from baseline.
In a planned subanalysis that did not include the approximately 20% of patients in each group who had joint replacement surgery, there was still an improvement in scores from baseline to 2 years, whereas those who received usual care alone were 20% worse, he said.
The effect sizes in the exercise group (0.57), manual therapy group (0.55), and combined therapy group (0.55) were substantially better than were the effect sizes of 0.30-0.35 normally attributed to nonsteroidal anti-inflammatory drugs, Dr. Abbott said. When patients with joint surgery were dropped from the analysis, those effect sizes grew to as high as 0.70 in the manual therapy group.
On the second primary outcome of several physical performance tests (timed up-and-go, 40-meter fast-paced walk, and 30-second sit-to-stand), the participants in the exercise therapy group showed greater mean changes than did patients in the other groups.
The Health Research Council of New Zealand funded the trial. None of the investigators had disclosures.
BOSTON – Improvements in pain, stiffness, and physical function that occur with the addition of exercise therapy or manual therapy to usual care for patients at all stages of osteoarthritis extended out to 2 years in a randomized, controlled trial.
Although evidence already supports the use of exercise therapy or manual therapy for improving the symptoms and physical function of patients with osteoarthritis (OA), the trial is the first to show that either intervention provides benefits over and above that of usual care during the course of 2 years of follow-up.
The investigators, led by Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, randomized 206 patients who met American College of Rheumatology criteria for knee or hip OA to usual care alone, exercise therapy plus usual care, manual therapy plus usual care, or both interventions plus usual care.
Those who received one or both of the interventions underwent 10 treatment sessions, including 7 sessions within the first 9 weeks plus 3 booster sessions (2 at 4 months and 1 at 13 months). Between and after those sessions, participants carried out the interventions on their own.
Mean age of the patients was 66 years. The spectrum of OA ranged from mild to severe, with a mean Western Ontario and McMaster Universities (WOMAC) OA index score of 100.8. The patients had been recruited to the trial from primary care and orthopedic services, the investigators reported at the annual meeting of the American College of Rheumatology.
Exercise therapy consisted of strengthening, range-of-motion, neuromuscular coordination, and aerobics activities; manual therapy consisted of skilled passive movement to joints applied by external force. Physical therapists guided both interventions in one-on-one visits.
The 1-year results, which were published in 2013, showed significant decreases in pain and improvements in physical function in both single-intervention groups, but no significant improvement in the combined therapy group (Osteoarthritis Cartilage 2013;21:525-34).
Among the 186 patients who still remained in the study at 2 years of follow-up, scores on the WOMAC – the trial’s primary outcome – improved by 31.7 points in those who received exercise therapy plus usual care, compared with usual care alone, while patients receiving manual therapy in addition to usual care showed a relative improvement of 30.1 points. While the difference in WOMAC improvement for participants receiving combined exercise therapy and manual therapy in addition to usual care did not meet the a priori threshold for clinical significance (28 points), there was a trend toward benefit, with this group improving 26.2 points more than usual care only.
In all three intervention groups, Dr. Abbott noted that those changes represented greater than 20% declines in WOMAC scores from baseline.
In a planned subanalysis that did not include the approximately 20% of patients in each group who had joint replacement surgery, there was still an improvement in scores from baseline to 2 years, whereas those who received usual care alone were 20% worse, he said.
The effect sizes in the exercise group (0.57), manual therapy group (0.55), and combined therapy group (0.55) were substantially better than were the effect sizes of 0.30-0.35 normally attributed to nonsteroidal anti-inflammatory drugs, Dr. Abbott said. When patients with joint surgery were dropped from the analysis, those effect sizes grew to as high as 0.70 in the manual therapy group.
On the second primary outcome of several physical performance tests (timed up-and-go, 40-meter fast-paced walk, and 30-second sit-to-stand), the participants in the exercise therapy group showed greater mean changes than did patients in the other groups.
The Health Research Council of New Zealand funded the trial. None of the investigators had disclosures.
BOSTON – Improvements in pain, stiffness, and physical function that occur with the addition of exercise therapy or manual therapy to usual care for patients at all stages of osteoarthritis extended out to 2 years in a randomized, controlled trial.
Although evidence already supports the use of exercise therapy or manual therapy for improving the symptoms and physical function of patients with osteoarthritis (OA), the trial is the first to show that either intervention provides benefits over and above that of usual care during the course of 2 years of follow-up.
The investigators, led by Dr. Haxby Abbott of the University of Otago, Dunedin, New Zealand, randomized 206 patients who met American College of Rheumatology criteria for knee or hip OA to usual care alone, exercise therapy plus usual care, manual therapy plus usual care, or both interventions plus usual care.
Those who received one or both of the interventions underwent 10 treatment sessions, including 7 sessions within the first 9 weeks plus 3 booster sessions (2 at 4 months and 1 at 13 months). Between and after those sessions, participants carried out the interventions on their own.
Mean age of the patients was 66 years. The spectrum of OA ranged from mild to severe, with a mean Western Ontario and McMaster Universities (WOMAC) OA index score of 100.8. The patients had been recruited to the trial from primary care and orthopedic services, the investigators reported at the annual meeting of the American College of Rheumatology.
Exercise therapy consisted of strengthening, range-of-motion, neuromuscular coordination, and aerobics activities; manual therapy consisted of skilled passive movement to joints applied by external force. Physical therapists guided both interventions in one-on-one visits.
The 1-year results, which were published in 2013, showed significant decreases in pain and improvements in physical function in both single-intervention groups, but no significant improvement in the combined therapy group (Osteoarthritis Cartilage 2013;21:525-34).
Among the 186 patients who still remained in the study at 2 years of follow-up, scores on the WOMAC – the trial’s primary outcome – improved by 31.7 points in those who received exercise therapy plus usual care, compared with usual care alone, while patients receiving manual therapy in addition to usual care showed a relative improvement of 30.1 points. While the difference in WOMAC improvement for participants receiving combined exercise therapy and manual therapy in addition to usual care did not meet the a priori threshold for clinical significance (28 points), there was a trend toward benefit, with this group improving 26.2 points more than usual care only.
In all three intervention groups, Dr. Abbott noted that those changes represented greater than 20% declines in WOMAC scores from baseline.
In a planned subanalysis that did not include the approximately 20% of patients in each group who had joint replacement surgery, there was still an improvement in scores from baseline to 2 years, whereas those who received usual care alone were 20% worse, he said.
The effect sizes in the exercise group (0.57), manual therapy group (0.55), and combined therapy group (0.55) were substantially better than were the effect sizes of 0.30-0.35 normally attributed to nonsteroidal anti-inflammatory drugs, Dr. Abbott said. When patients with joint surgery were dropped from the analysis, those effect sizes grew to as high as 0.70 in the manual therapy group.
On the second primary outcome of several physical performance tests (timed up-and-go, 40-meter fast-paced walk, and 30-second sit-to-stand), the participants in the exercise therapy group showed greater mean changes than did patients in the other groups.
The Health Research Council of New Zealand funded the trial. None of the investigators had disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Prescribing exercise therapy or manual therapy to patients in various stages of OA can provide long-term benefit in addition to usual care.
Major finding: At 2 years, relative to usual care alone, scores on the WOMAC had improved by 31.7 points in those who received exercise therapy plus usual care, 30.1 points in patients on manual therapy in addition to usual care, and 26.2 points in those who received combined exercise therapy and manual therapy in addition to usual care.
Data source: A trial of 206 patients with OA who were randomized to usual care alone, exercise therapy plus usual care, manual therapy plus usual care, or both interventions plus usual care.
Disclosures: The Health Research Council of New Zealand funded the trial. None of the investigators had disclosures.