User login
Anti–PD1 Immune Checkpoint Inhibitor–Induced Bullous Pemphigoid in Metastatic Melanoma and Non–Small Cell Lung Cancer
Immune checkpoint inhibitors are used for a variety of advanced malignancies, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma. Anti–programmed cell death 1 (PD1) targeted therapies, such as pembrolizumab and nivolumab, are improving patient survival. This class of immunotherapy is revolutionary but is associated with autoimmune adverse effects. A rare but increasingly reported adverse effect of anti-PD1 therapy is bullous pemphigoid (BP), an autoimmune blistering disease directed against
High clinical suspicion, early diagnosis, and proper management of immunotherapy-related BP are imperative for keeping patients on life-prolonging treatment. We present 3 cases of BP secondary to anti-PD1 immunotherapy in patients with melanoma or non–small cell lung cancer to highlight the diagnosis and treatment of BP as well as emphasize the importance of the dermatologist in the care of patients with immunotherapy-related skin disease.
Case Reports
Patient 1
A 72-year-old woman with metastatic BRAF-mutated melanoma from an unknown primary site presented with intensely pruritic papules on the back, chest, and extremities of 4 months’ duration. She described her symptoms as insidious in onset and refractory to clobetasol ointment, oral diphenhydramine, and over-the-counter anti-itch creams. The patient had been treated with oral dabrafenib 150 mg twice daily and trametinib 2 mg/d but was switched to pembrolizumab when the disease progressed. After 8 months, she had a complete radiologic response to pembrolizumab 2 mg/kg every 3 weeks, which was discontinued in favor of observation 3 months prior to presentation to dermatology.
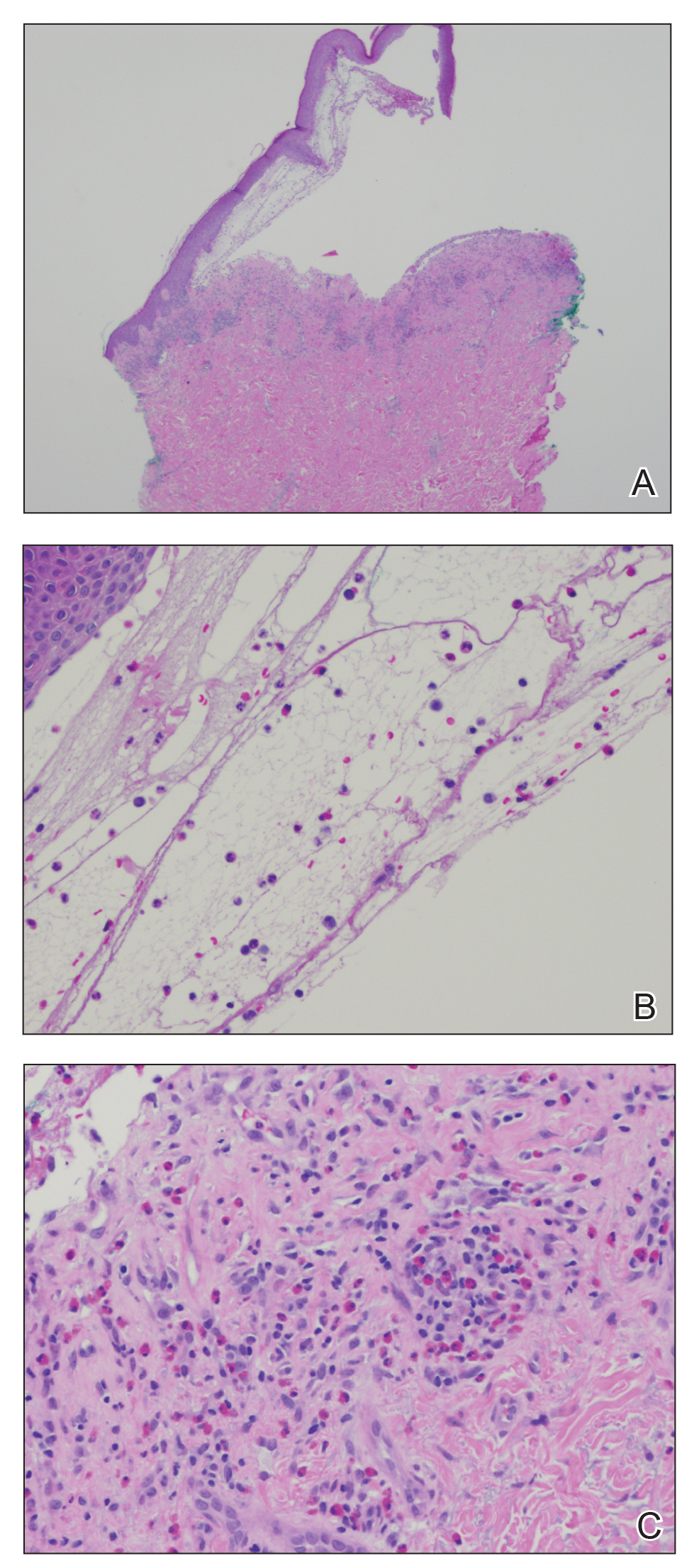
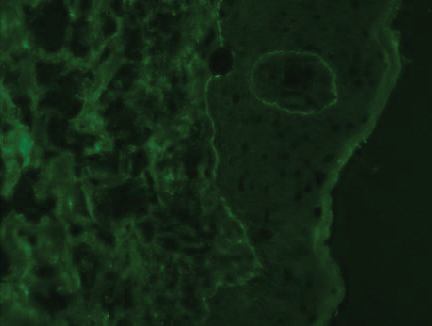
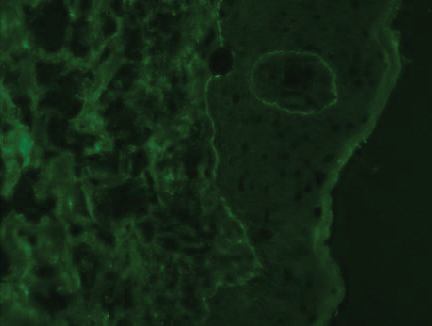
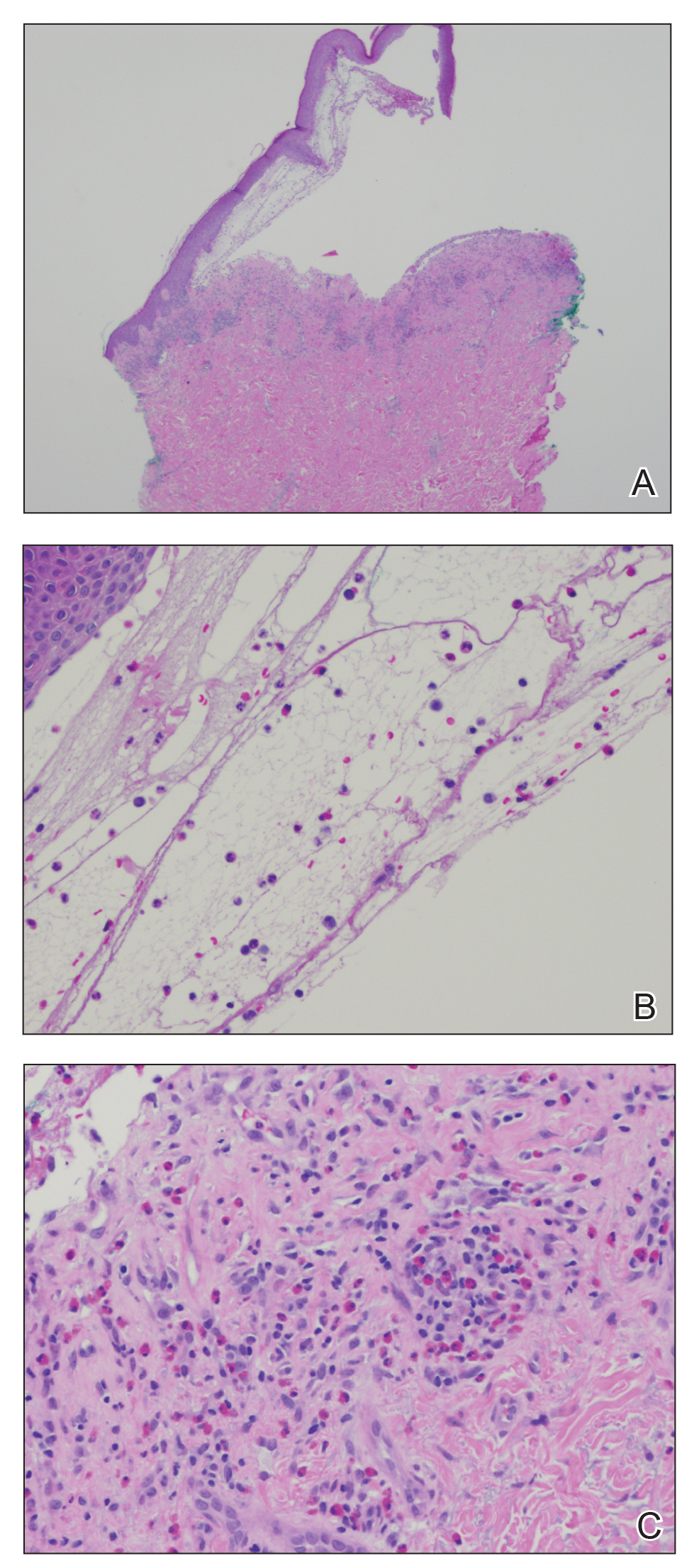
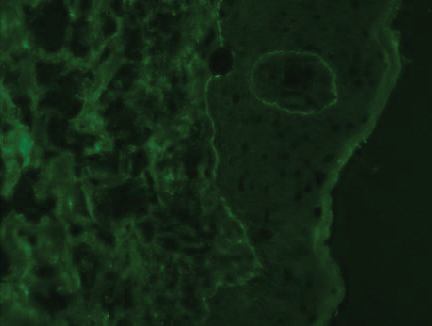
At the current presentation, physical examination revealed innumerable erythematous, excoriated, 2- to 4-mm, red papules diffusely scattered on the upper back, chest, abdomen, and thighs, with one 8×4-mm vesicle on the right side of the upper back (Figure 1). Discrete areas of depigmented macules, consistent with vitiligo, coalesced into patches on the legs, thighs, arms, and back. The patient was started on a 3-week oral prednisone taper for symptom relief. A hematoxylin and eosin (H&E)–stained punch biopsy of the back revealed a subepidermal split with eosinophils and a dense eosinophilic infiltrate in the dermis (Figure 2). Direct immunofluorescence (DIF) studies from a specimen adjacent to the biopsy collected for H&E staining showed linear deposition of IgA, IgG, and C3 along the dermoepidermal junction (Figure 3). Histologic findings were consistent with BP.

The patient was started on doxycycline 100 mg twice daily and clobetasol ointment 0.05% once daily to supplement the prednisone taper. At 3-week follow-up, she reported pruritus and a few erythematous macules but no new bullae. At 12 weeks, some papules persisted; however, the patient was averse to using systemic agents and decided that symptoms were adequately controlled with clobetasol ointment and oral doxycycline.
Because the patient currently remains in clinical and radiologic remission, anti-PD1 immune checkpoint inhibitors have not been restarted but remain an option for the future if disease recurs
Patient 2
An 82-year-old man with a history of stage IIC desmoplastic melanoma presented to dermatology with an intensely pruritic eruption on the legs, arms, waist, upper torso, and scalp of 3 weeks’ duration. Clobetasol ointment had provided minimal relief.
Six months prior to presenting to dermatology, the patient underwent immunotherapy with 4 cycles of ipilimumab 200 mg intravenous (IV) and nivolumab 240 mg IV every 2 weeks, receiving ipilimumab during the first cycle only because of a lack of availability at the pharmacy. He then received nivolumab 240 mg IV every 2 weeks as maintenance therapy. After the second dose of nivolumab maintenance therapy, however, he developed generalized bullae and pruritus. Dermatology was consulted during an oncology appointment, and his oncologist decided to hold nivolumab.
Physical examination revealed generalized tense and eroded bullae covering more than 50% of the body surface area and affecting the scalp, arms, legs, torso, and buttocks. Two punch biopsies were obtained. Hematoxylin and eosin staining revealed a subepidermal split with predominantly eosinophils and scattered neutrophils. Direct immunofluorescence studies showed linear deposition of IgG, IgA, and C3 along the dermoepidermal junction, consistent with BP.
The patient’s BP was difficult to control, requiring several hospital admissions for wound care, high-dose systemic steroids, and initiation of mycophenolate mofetil. After 4 months of waxing and waning symptoms, the BP was controlled with mycophenolate mofetil 1500 mg/d; clobetasol ointment 0.05%; and diphenhydramine for pruritus. Due to the prolonged recovery and severity of BP, the patient’s oncologist deemed that he was not a candidate for future immunotherapy.
Patient 3
A 68-year-old man with PD1-negative, metastatic, well-differentiated squamous cell carcinoma of the lung presented to dermatology with a pruritic rash of 3 weeks’ duration. He had been receiving nivolumab for 2 years after disease progressed on prior chemotherapies and experienced several grade 1 or grade 2 nivolumab-induced autoimmune reactions including thyroiditis, dermatitis, and nephritis, for which he was taking prednisone 5 mg/d for suppression.
Physical examination revealed psoriasiform pink plaques on the arms, chest, and legs. The differential diagnosis at the time favored psoriasiform dermatitis over lichenoid dermatitis. A punch biopsy revealed psoriasiform dermatitis. The patient was prescribed fluocinonide ointment 0.05% daily. His plaques improved with topical steroids.
The patient returned approximately 1 month later with a report of a new blistering rash on the legs. Physical examination revealed interval improvement of the psoriasiform plaques on the scalp, torso, and extremities, but tense bullae were seen on the thighs, with surrounding superficial erosions at sites of recent bullae. Punch biopsies of the skin for H&E staining and DIF showed BP.
Prednisone was increased to 50 mg/d for a 3-week taper. Doxycycline 100 mg twice daily was started. The patient’s skin disease continued to be difficult to control with therapy; nivolumab was held by his oncologist.
Comment
Immunotherapy with immune checkpoint blockade represents a successful application of immune recognition to treat metastatic cancers, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma.
Anti-PD1 targeted therapies improve survival in solid and hematologic malignancies, with a response rate as high as 40% in melanoma.2 Although these medications can prolong survival, many are associated with loss of self-tolerance and severe autoimmunelike events that can limit therapy.3 An exception is PD1-induced vitiligo, which patient 1 developed and has been associated with a better response to therapy.4
Anti-PD1–induced BP is a newly reported adverse effect. In its early stages, BP can be difficult to differentiate from eczematous or urticarial dermatitis.5-8 Discontinuation of immunotherapy has been reported in more than 70% of patients who develop BP.1 There are reports of successful treatment of BP with a course of a PD1 inhibitor,9 but 2 of our patients had severe BP that led to discontinuation of immunotherapy.
Consider Prescreening
Given that development of BP often leads to cessation of therapy, identifying patients at risk prior to starting an immune checkpoint inhibitor might have clinical utility. Biopsy with DIF is the gold standard for diagnosis, but serologic testing can be a useful adjunct because enzyme-linked immunosorbent assay for BP antigen 1 and BP antigen 2 has a reported sensitivity and specificity of 87% and 98%, respectively.10 Serologic testing prior to starting therapy with an immune checkpoint inhibitor can provide a baseline for patients. A rise in titer, in conjunction with onset of a rash, might aid in earlier diagnosis, particularly because urticarial BP can be difficult to diagnose clinically.
Further study on the utility vs cost-benefit of these screening modalities is warranted. Their predictive utility might be limited, however, and positive serologic test results might have unanticipated consequences, such as hesitation in treating patients, thus leading to a delay in therapy or access to these medications.
Conclusion
The expanding use of immune checkpoint inhibitors is increasing survival in patients with metastatic melanoma and other malignancies. Adverse effects are part of the continuum of immune system stimulation, with overstimulation resulting in dermatitis; thyroiditis; pneumonitis; and less commonly hypophysitis, vitiligo, and colitis.
Rarely, immune checkpoint inhibition induces BP. Development of BP leads to discontinuation of therapy in more than half of reported cases due to lack of adequate treatment for this skin disease and its impact on quality of life. Therefore, quick diagnosis of BP in patients on immunotherapy and successful management techniques can prevent discontinuation of these lifesaving cancer therapies. For that reason, dermatologists play an important role in the management of patients on immune checkpoint inhibitors for cancer.
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669.
- Márquez-Rodas, I, Cerezuela P, Soria A, et al. Immune checkpoint inhibitors: therapeutic advances in melanoma. Ann Transl Med. 2015;3:267.
- Friedman CF, Proverbs-Singh TA, Postow MA. Treatment of the immune-related adverse effects of immune checkpoint inhibitors a review. JAMA Oncol. 2016;2:1346-1353.
- Hua C, Boussemart L, Mateus C, et al. Association of vitiligo with tumor response in patients with metastatic melanoma treated with pembrolizumab. JAMA Dermatol. 2016;152:45-51.
- Hwang SJE, Carlos G, Chou S, et al. Bullous pemphigoid, an autoantibody-mediated disease, is a novel immune-related adverse event in patients treated with anti-programmed cell death 1 antibodies. Melanoma Res. 2016;26:413-416.
- Damsky W, Kole L, Tomayko MM. Development of bullous pemphigoid during nivolumab therapy. JAAD Case Rep. 2016;2:442-444.
- Garje R, Chau JJ, Chung J, et al. Acute flare of bullous pemphigus with pembrolizumab used for treatment of metastatic urothelial cancer. J Immunother. 2018;41:42-44.
- Ito M, Hoashi T, Endo Y, et al. Atypical pemphigus developed in a patient with urothelial carcinoma treated with nivolumab. J Dermatol. 2019;46:e90-e92.
- Chen W-S, Tetzlaff MT, Diwan H, et al. Suprabasal acantholytic dermatologic toxicities associated checkpoint inhibitor therapy: a spectrum of immune reactions from paraneoplastic pemphigus-like to Grover-like lesions. J Cutan Pathol. 2018;45:764-773.
- Muglia C, Bronsnick T, Kirkorian AY, et al. Questioning the specificity and sensitivity of ELISA for bullous pemphigoid diagnosis. Cutis. 2017;99:E27-E30.
Immune checkpoint inhibitors are used for a variety of advanced malignancies, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma. Anti–programmed cell death 1 (PD1) targeted therapies, such as pembrolizumab and nivolumab, are improving patient survival. This class of immunotherapy is revolutionary but is associated with autoimmune adverse effects. A rare but increasingly reported adverse effect of anti-PD1 therapy is bullous pemphigoid (BP), an autoimmune blistering disease directed against
High clinical suspicion, early diagnosis, and proper management of immunotherapy-related BP are imperative for keeping patients on life-prolonging treatment. We present 3 cases of BP secondary to anti-PD1 immunotherapy in patients with melanoma or non–small cell lung cancer to highlight the diagnosis and treatment of BP as well as emphasize the importance of the dermatologist in the care of patients with immunotherapy-related skin disease.
Case Reports
Patient 1
A 72-year-old woman with metastatic BRAF-mutated melanoma from an unknown primary site presented with intensely pruritic papules on the back, chest, and extremities of 4 months’ duration. She described her symptoms as insidious in onset and refractory to clobetasol ointment, oral diphenhydramine, and over-the-counter anti-itch creams. The patient had been treated with oral dabrafenib 150 mg twice daily and trametinib 2 mg/d but was switched to pembrolizumab when the disease progressed. After 8 months, she had a complete radiologic response to pembrolizumab 2 mg/kg every 3 weeks, which was discontinued in favor of observation 3 months prior to presentation to dermatology.
At the current presentation, physical examination revealed innumerable erythematous, excoriated, 2- to 4-mm, red papules diffusely scattered on the upper back, chest, abdomen, and thighs, with one 8×4-mm vesicle on the right side of the upper back (Figure 1). Discrete areas of depigmented macules, consistent with vitiligo, coalesced into patches on the legs, thighs, arms, and back. The patient was started on a 3-week oral prednisone taper for symptom relief. A hematoxylin and eosin (H&E)–stained punch biopsy of the back revealed a subepidermal split with eosinophils and a dense eosinophilic infiltrate in the dermis (Figure 2). Direct immunofluorescence (DIF) studies from a specimen adjacent to the biopsy collected for H&E staining showed linear deposition of IgA, IgG, and C3 along the dermoepidermal junction (Figure 3). Histologic findings were consistent with BP.

The patient was started on doxycycline 100 mg twice daily and clobetasol ointment 0.05% once daily to supplement the prednisone taper. At 3-week follow-up, she reported pruritus and a few erythematous macules but no new bullae. At 12 weeks, some papules persisted; however, the patient was averse to using systemic agents and decided that symptoms were adequately controlled with clobetasol ointment and oral doxycycline.
Because the patient currently remains in clinical and radiologic remission, anti-PD1 immune checkpoint inhibitors have not been restarted but remain an option for the future if disease recurs
Patient 2
An 82-year-old man with a history of stage IIC desmoplastic melanoma presented to dermatology with an intensely pruritic eruption on the legs, arms, waist, upper torso, and scalp of 3 weeks’ duration. Clobetasol ointment had provided minimal relief.
Six months prior to presenting to dermatology, the patient underwent immunotherapy with 4 cycles of ipilimumab 200 mg intravenous (IV) and nivolumab 240 mg IV every 2 weeks, receiving ipilimumab during the first cycle only because of a lack of availability at the pharmacy. He then received nivolumab 240 mg IV every 2 weeks as maintenance therapy. After the second dose of nivolumab maintenance therapy, however, he developed generalized bullae and pruritus. Dermatology was consulted during an oncology appointment, and his oncologist decided to hold nivolumab.
Physical examination revealed generalized tense and eroded bullae covering more than 50% of the body surface area and affecting the scalp, arms, legs, torso, and buttocks. Two punch biopsies were obtained. Hematoxylin and eosin staining revealed a subepidermal split with predominantly eosinophils and scattered neutrophils. Direct immunofluorescence studies showed linear deposition of IgG, IgA, and C3 along the dermoepidermal junction, consistent with BP.
The patient’s BP was difficult to control, requiring several hospital admissions for wound care, high-dose systemic steroids, and initiation of mycophenolate mofetil. After 4 months of waxing and waning symptoms, the BP was controlled with mycophenolate mofetil 1500 mg/d; clobetasol ointment 0.05%; and diphenhydramine for pruritus. Due to the prolonged recovery and severity of BP, the patient’s oncologist deemed that he was not a candidate for future immunotherapy.
Patient 3
A 68-year-old man with PD1-negative, metastatic, well-differentiated squamous cell carcinoma of the lung presented to dermatology with a pruritic rash of 3 weeks’ duration. He had been receiving nivolumab for 2 years after disease progressed on prior chemotherapies and experienced several grade 1 or grade 2 nivolumab-induced autoimmune reactions including thyroiditis, dermatitis, and nephritis, for which he was taking prednisone 5 mg/d for suppression.
Physical examination revealed psoriasiform pink plaques on the arms, chest, and legs. The differential diagnosis at the time favored psoriasiform dermatitis over lichenoid dermatitis. A punch biopsy revealed psoriasiform dermatitis. The patient was prescribed fluocinonide ointment 0.05% daily. His plaques improved with topical steroids.
The patient returned approximately 1 month later with a report of a new blistering rash on the legs. Physical examination revealed interval improvement of the psoriasiform plaques on the scalp, torso, and extremities, but tense bullae were seen on the thighs, with surrounding superficial erosions at sites of recent bullae. Punch biopsies of the skin for H&E staining and DIF showed BP.
Prednisone was increased to 50 mg/d for a 3-week taper. Doxycycline 100 mg twice daily was started. The patient’s skin disease continued to be difficult to control with therapy; nivolumab was held by his oncologist.
Comment
Immunotherapy with immune checkpoint blockade represents a successful application of immune recognition to treat metastatic cancers, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma.
Anti-PD1 targeted therapies improve survival in solid and hematologic malignancies, with a response rate as high as 40% in melanoma.2 Although these medications can prolong survival, many are associated with loss of self-tolerance and severe autoimmunelike events that can limit therapy.3 An exception is PD1-induced vitiligo, which patient 1 developed and has been associated with a better response to therapy.4
Anti-PD1–induced BP is a newly reported adverse effect. In its early stages, BP can be difficult to differentiate from eczematous or urticarial dermatitis.5-8 Discontinuation of immunotherapy has been reported in more than 70% of patients who develop BP.1 There are reports of successful treatment of BP with a course of a PD1 inhibitor,9 but 2 of our patients had severe BP that led to discontinuation of immunotherapy.
Consider Prescreening
Given that development of BP often leads to cessation of therapy, identifying patients at risk prior to starting an immune checkpoint inhibitor might have clinical utility. Biopsy with DIF is the gold standard for diagnosis, but serologic testing can be a useful adjunct because enzyme-linked immunosorbent assay for BP antigen 1 and BP antigen 2 has a reported sensitivity and specificity of 87% and 98%, respectively.10 Serologic testing prior to starting therapy with an immune checkpoint inhibitor can provide a baseline for patients. A rise in titer, in conjunction with onset of a rash, might aid in earlier diagnosis, particularly because urticarial BP can be difficult to diagnose clinically.
Further study on the utility vs cost-benefit of these screening modalities is warranted. Their predictive utility might be limited, however, and positive serologic test results might have unanticipated consequences, such as hesitation in treating patients, thus leading to a delay in therapy or access to these medications.
Conclusion
The expanding use of immune checkpoint inhibitors is increasing survival in patients with metastatic melanoma and other malignancies. Adverse effects are part of the continuum of immune system stimulation, with overstimulation resulting in dermatitis; thyroiditis; pneumonitis; and less commonly hypophysitis, vitiligo, and colitis.
Rarely, immune checkpoint inhibition induces BP. Development of BP leads to discontinuation of therapy in more than half of reported cases due to lack of adequate treatment for this skin disease and its impact on quality of life. Therefore, quick diagnosis of BP in patients on immunotherapy and successful management techniques can prevent discontinuation of these lifesaving cancer therapies. For that reason, dermatologists play an important role in the management of patients on immune checkpoint inhibitors for cancer.
Immune checkpoint inhibitors are used for a variety of advanced malignancies, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma. Anti–programmed cell death 1 (PD1) targeted therapies, such as pembrolizumab and nivolumab, are improving patient survival. This class of immunotherapy is revolutionary but is associated with autoimmune adverse effects. A rare but increasingly reported adverse effect of anti-PD1 therapy is bullous pemphigoid (BP), an autoimmune blistering disease directed against
High clinical suspicion, early diagnosis, and proper management of immunotherapy-related BP are imperative for keeping patients on life-prolonging treatment. We present 3 cases of BP secondary to anti-PD1 immunotherapy in patients with melanoma or non–small cell lung cancer to highlight the diagnosis and treatment of BP as well as emphasize the importance of the dermatologist in the care of patients with immunotherapy-related skin disease.
Case Reports
Patient 1
A 72-year-old woman with metastatic BRAF-mutated melanoma from an unknown primary site presented with intensely pruritic papules on the back, chest, and extremities of 4 months’ duration. She described her symptoms as insidious in onset and refractory to clobetasol ointment, oral diphenhydramine, and over-the-counter anti-itch creams. The patient had been treated with oral dabrafenib 150 mg twice daily and trametinib 2 mg/d but was switched to pembrolizumab when the disease progressed. After 8 months, she had a complete radiologic response to pembrolizumab 2 mg/kg every 3 weeks, which was discontinued in favor of observation 3 months prior to presentation to dermatology.
At the current presentation, physical examination revealed innumerable erythematous, excoriated, 2- to 4-mm, red papules diffusely scattered on the upper back, chest, abdomen, and thighs, with one 8×4-mm vesicle on the right side of the upper back (Figure 1). Discrete areas of depigmented macules, consistent with vitiligo, coalesced into patches on the legs, thighs, arms, and back. The patient was started on a 3-week oral prednisone taper for symptom relief. A hematoxylin and eosin (H&E)–stained punch biopsy of the back revealed a subepidermal split with eosinophils and a dense eosinophilic infiltrate in the dermis (Figure 2). Direct immunofluorescence (DIF) studies from a specimen adjacent to the biopsy collected for H&E staining showed linear deposition of IgA, IgG, and C3 along the dermoepidermal junction (Figure 3). Histologic findings were consistent with BP.

The patient was started on doxycycline 100 mg twice daily and clobetasol ointment 0.05% once daily to supplement the prednisone taper. At 3-week follow-up, she reported pruritus and a few erythematous macules but no new bullae. At 12 weeks, some papules persisted; however, the patient was averse to using systemic agents and decided that symptoms were adequately controlled with clobetasol ointment and oral doxycycline.
Because the patient currently remains in clinical and radiologic remission, anti-PD1 immune checkpoint inhibitors have not been restarted but remain an option for the future if disease recurs
Patient 2
An 82-year-old man with a history of stage IIC desmoplastic melanoma presented to dermatology with an intensely pruritic eruption on the legs, arms, waist, upper torso, and scalp of 3 weeks’ duration. Clobetasol ointment had provided minimal relief.
Six months prior to presenting to dermatology, the patient underwent immunotherapy with 4 cycles of ipilimumab 200 mg intravenous (IV) and nivolumab 240 mg IV every 2 weeks, receiving ipilimumab during the first cycle only because of a lack of availability at the pharmacy. He then received nivolumab 240 mg IV every 2 weeks as maintenance therapy. After the second dose of nivolumab maintenance therapy, however, he developed generalized bullae and pruritus. Dermatology was consulted during an oncology appointment, and his oncologist decided to hold nivolumab.
Physical examination revealed generalized tense and eroded bullae covering more than 50% of the body surface area and affecting the scalp, arms, legs, torso, and buttocks. Two punch biopsies were obtained. Hematoxylin and eosin staining revealed a subepidermal split with predominantly eosinophils and scattered neutrophils. Direct immunofluorescence studies showed linear deposition of IgG, IgA, and C3 along the dermoepidermal junction, consistent with BP.
The patient’s BP was difficult to control, requiring several hospital admissions for wound care, high-dose systemic steroids, and initiation of mycophenolate mofetil. After 4 months of waxing and waning symptoms, the BP was controlled with mycophenolate mofetil 1500 mg/d; clobetasol ointment 0.05%; and diphenhydramine for pruritus. Due to the prolonged recovery and severity of BP, the patient’s oncologist deemed that he was not a candidate for future immunotherapy.
Patient 3
A 68-year-old man with PD1-negative, metastatic, well-differentiated squamous cell carcinoma of the lung presented to dermatology with a pruritic rash of 3 weeks’ duration. He had been receiving nivolumab for 2 years after disease progressed on prior chemotherapies and experienced several grade 1 or grade 2 nivolumab-induced autoimmune reactions including thyroiditis, dermatitis, and nephritis, for which he was taking prednisone 5 mg/d for suppression.
Physical examination revealed psoriasiform pink plaques on the arms, chest, and legs. The differential diagnosis at the time favored psoriasiform dermatitis over lichenoid dermatitis. A punch biopsy revealed psoriasiform dermatitis. The patient was prescribed fluocinonide ointment 0.05% daily. His plaques improved with topical steroids.
The patient returned approximately 1 month later with a report of a new blistering rash on the legs. Physical examination revealed interval improvement of the psoriasiform plaques on the scalp, torso, and extremities, but tense bullae were seen on the thighs, with surrounding superficial erosions at sites of recent bullae. Punch biopsies of the skin for H&E staining and DIF showed BP.
Prednisone was increased to 50 mg/d for a 3-week taper. Doxycycline 100 mg twice daily was started. The patient’s skin disease continued to be difficult to control with therapy; nivolumab was held by his oncologist.
Comment
Immunotherapy with immune checkpoint blockade represents a successful application of immune recognition to treat metastatic cancers, including melanoma, non–small cell lung cancer, urothelial cancer, and renal cell carcinoma.
Anti-PD1 targeted therapies improve survival in solid and hematologic malignancies, with a response rate as high as 40% in melanoma.2 Although these medications can prolong survival, many are associated with loss of self-tolerance and severe autoimmunelike events that can limit therapy.3 An exception is PD1-induced vitiligo, which patient 1 developed and has been associated with a better response to therapy.4
Anti-PD1–induced BP is a newly reported adverse effect. In its early stages, BP can be difficult to differentiate from eczematous or urticarial dermatitis.5-8 Discontinuation of immunotherapy has been reported in more than 70% of patients who develop BP.1 There are reports of successful treatment of BP with a course of a PD1 inhibitor,9 but 2 of our patients had severe BP that led to discontinuation of immunotherapy.
Consider Prescreening
Given that development of BP often leads to cessation of therapy, identifying patients at risk prior to starting an immune checkpoint inhibitor might have clinical utility. Biopsy with DIF is the gold standard for diagnosis, but serologic testing can be a useful adjunct because enzyme-linked immunosorbent assay for BP antigen 1 and BP antigen 2 has a reported sensitivity and specificity of 87% and 98%, respectively.10 Serologic testing prior to starting therapy with an immune checkpoint inhibitor can provide a baseline for patients. A rise in titer, in conjunction with onset of a rash, might aid in earlier diagnosis, particularly because urticarial BP can be difficult to diagnose clinically.
Further study on the utility vs cost-benefit of these screening modalities is warranted. Their predictive utility might be limited, however, and positive serologic test results might have unanticipated consequences, such as hesitation in treating patients, thus leading to a delay in therapy or access to these medications.
Conclusion
The expanding use of immune checkpoint inhibitors is increasing survival in patients with metastatic melanoma and other malignancies. Adverse effects are part of the continuum of immune system stimulation, with overstimulation resulting in dermatitis; thyroiditis; pneumonitis; and less commonly hypophysitis, vitiligo, and colitis.
Rarely, immune checkpoint inhibition induces BP. Development of BP leads to discontinuation of therapy in more than half of reported cases due to lack of adequate treatment for this skin disease and its impact on quality of life. Therefore, quick diagnosis of BP in patients on immunotherapy and successful management techniques can prevent discontinuation of these lifesaving cancer therapies. For that reason, dermatologists play an important role in the management of patients on immune checkpoint inhibitors for cancer.
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669.
- Márquez-Rodas, I, Cerezuela P, Soria A, et al. Immune checkpoint inhibitors: therapeutic advances in melanoma. Ann Transl Med. 2015;3:267.
- Friedman CF, Proverbs-Singh TA, Postow MA. Treatment of the immune-related adverse effects of immune checkpoint inhibitors a review. JAMA Oncol. 2016;2:1346-1353.
- Hua C, Boussemart L, Mateus C, et al. Association of vitiligo with tumor response in patients with metastatic melanoma treated with pembrolizumab. JAMA Dermatol. 2016;152:45-51.
- Hwang SJE, Carlos G, Chou S, et al. Bullous pemphigoid, an autoantibody-mediated disease, is a novel immune-related adverse event in patients treated with anti-programmed cell death 1 antibodies. Melanoma Res. 2016;26:413-416.
- Damsky W, Kole L, Tomayko MM. Development of bullous pemphigoid during nivolumab therapy. JAAD Case Rep. 2016;2:442-444.
- Garje R, Chau JJ, Chung J, et al. Acute flare of bullous pemphigus with pembrolizumab used for treatment of metastatic urothelial cancer. J Immunother. 2018;41:42-44.
- Ito M, Hoashi T, Endo Y, et al. Atypical pemphigus developed in a patient with urothelial carcinoma treated with nivolumab. J Dermatol. 2019;46:e90-e92.
- Chen W-S, Tetzlaff MT, Diwan H, et al. Suprabasal acantholytic dermatologic toxicities associated checkpoint inhibitor therapy: a spectrum of immune reactions from paraneoplastic pemphigus-like to Grover-like lesions. J Cutan Pathol. 2018;45:764-773.
- Muglia C, Bronsnick T, Kirkorian AY, et al. Questioning the specificity and sensitivity of ELISA for bullous pemphigoid diagnosis. Cutis. 2017;99:E27-E30.
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669.
- Márquez-Rodas, I, Cerezuela P, Soria A, et al. Immune checkpoint inhibitors: therapeutic advances in melanoma. Ann Transl Med. 2015;3:267.
- Friedman CF, Proverbs-Singh TA, Postow MA. Treatment of the immune-related adverse effects of immune checkpoint inhibitors a review. JAMA Oncol. 2016;2:1346-1353.
- Hua C, Boussemart L, Mateus C, et al. Association of vitiligo with tumor response in patients with metastatic melanoma treated with pembrolizumab. JAMA Dermatol. 2016;152:45-51.
- Hwang SJE, Carlos G, Chou S, et al. Bullous pemphigoid, an autoantibody-mediated disease, is a novel immune-related adverse event in patients treated with anti-programmed cell death 1 antibodies. Melanoma Res. 2016;26:413-416.
- Damsky W, Kole L, Tomayko MM. Development of bullous pemphigoid during nivolumab therapy. JAAD Case Rep. 2016;2:442-444.
- Garje R, Chau JJ, Chung J, et al. Acute flare of bullous pemphigus with pembrolizumab used for treatment of metastatic urothelial cancer. J Immunother. 2018;41:42-44.
- Ito M, Hoashi T, Endo Y, et al. Atypical pemphigus developed in a patient with urothelial carcinoma treated with nivolumab. J Dermatol. 2019;46:e90-e92.
- Chen W-S, Tetzlaff MT, Diwan H, et al. Suprabasal acantholytic dermatologic toxicities associated checkpoint inhibitor therapy: a spectrum of immune reactions from paraneoplastic pemphigus-like to Grover-like lesions. J Cutan Pathol. 2018;45:764-773.
- Muglia C, Bronsnick T, Kirkorian AY, et al. Questioning the specificity and sensitivity of ELISA for bullous pemphigoid diagnosis. Cutis. 2017;99:E27-E30.
Practice Points
- Anti–programmed cell death 1 (PD1) targeted therapies improve survival in solid and hematologic malignancies but are associated with autoimmune side effects, with bullous pemphigoid (BP) being the newest reported.
- Bullous pemphigoid can develop months into immunotherapy treatment.
- Bullous pemphigoid should be on the differential diagnosis in a patient who is on an anti-PD1 immune checkpoint inhibitor and develops 1 or more of the following: pruritus, dermatitis, and vesicles.
- Early diagnosis of BP is essential for keeping patients on immunotherapy because its severity often results in temporary or permanent discontinuation of treatment.
Linear Depressions and Progressive Tightening of the Extremities
The Diagnosis: Eosinophilic Fasciitis (Shulman Syndrome)
In 1984, Shulman1 reported 2 cases of diffuse fasciitis with hypergammaglobulinemia and eosinophilia, which was later termed eosinophilic fasciitis (EF) by Rodnan et al.2 Eosinophilic fasciitis also is commonly known as diffuse fasciitis with eosinophilia3 or Shulman syndrome.3,4 It is an inflammatory condition of unknown etiology and pathogenesis, though an underlying autoimmune process has been proposed.3,5 The disorder is characterized by inflammation and subsequent fibrosis of deep fascia2 with variable involvement of the underlying muscle. It often is referred to as a sclerodermalike condition2,5-8 and is considered to be one of a group of fibrosing connective tissue disorders that may be confused with systemic sclerosis.3,4,6,9 Although the cause of EF is unknown, more than 50% of cases are associated with vigorous exercise or trauma.3 Other reported triggers and associations include Borrelia burgdorferi infection,5,6,10 arthropod bites,5,10 lymphoproliferative and hematologic disorders,5,6,10 inflammatory arthritis,6 morphea,3 thyroid dysfunction,5,6,10 statins,5,10 and phenytoin.5,10
There have been more than 250 cases of EF reported in the literature.3 Some authors report more frequent occurrence in males,3,4 while others report equal occurrence of disease in both males and females.5,10 Eosinophilic fasciitis has the highest incidence during the second to sixth decades of life,3,10 though childhood cases have been reported.3,11 White individuals appear to be affected most often, but sporadic cases in other ethnic groups also have been reported.3
The clinical presentation of EF frequently is characterized by the rapid onset of erythema, pain, and nonpitting edema of the involved areas.5,7,10,11 Fatigue and itching also are reported symptoms.12 A cobblestone texture of the skin may be noted, commonly referred to as the peau d’orange effect.6,10 Woody induration subsequently develops, which may lead to contracture or limited range of motion.5,7,11-13 The distal extremities, particularly the forearms and calves, are the most common areas affected by EF.3 There usually is symmetric involvement; however, unilateral cases of EF also have been reported.3,6,10 Linear indentations may form along the vasculature of the involved areas when the extremities are lifted or extended. These indentations serve to demarcate the underlying muscle groups, forming the groove sign or venous furrowing.3,5,14 The epidermis is not characteristically involved in EF and wrinkling of the skin can be elicited by pinching,3 which may be helpful in clinically distinguishing EF from scleroderma. Sparing of the digits is another characteristic feature of adult-onset EF.3,10 However, involvement of the digits resulting in painless contracture has been reported in multiple childhood cases and may represent a phenotype specific to children.11 Involvement of the trunk is less frequently observed but may serve as a poor prognostic indicator; indeed, patients demonstrating young age of onset, morphealike skin sclerosis, and trunk involvement are more likely to develop refractory disease.15
Eosinophilic fasciitis is characterized by various laboratory abnormalities. Peripheral eosinophilia, hypergammaglobulinemia, elevated sedimentation rate,3,6,9,10,13,15 and elevated C-reactive protein3,6 are commonly reported; however, antinuclear antibody, rheumatoid factor, or antibodies associated with systemic sclerosis are not frequently found.3,6 There are no laboratory abnormalities required to render a diagnosis of EF, and absence of peripheral eosinophilia has been noted in up to 20% of cases.3,4 An elevation of creatine kinase or aldolase levels may be present if muscle is involved.3,6 In general, abnormal laboratory findings have not been found to correlate with disease activity13,15 and do not appear to have prognostic significance.15
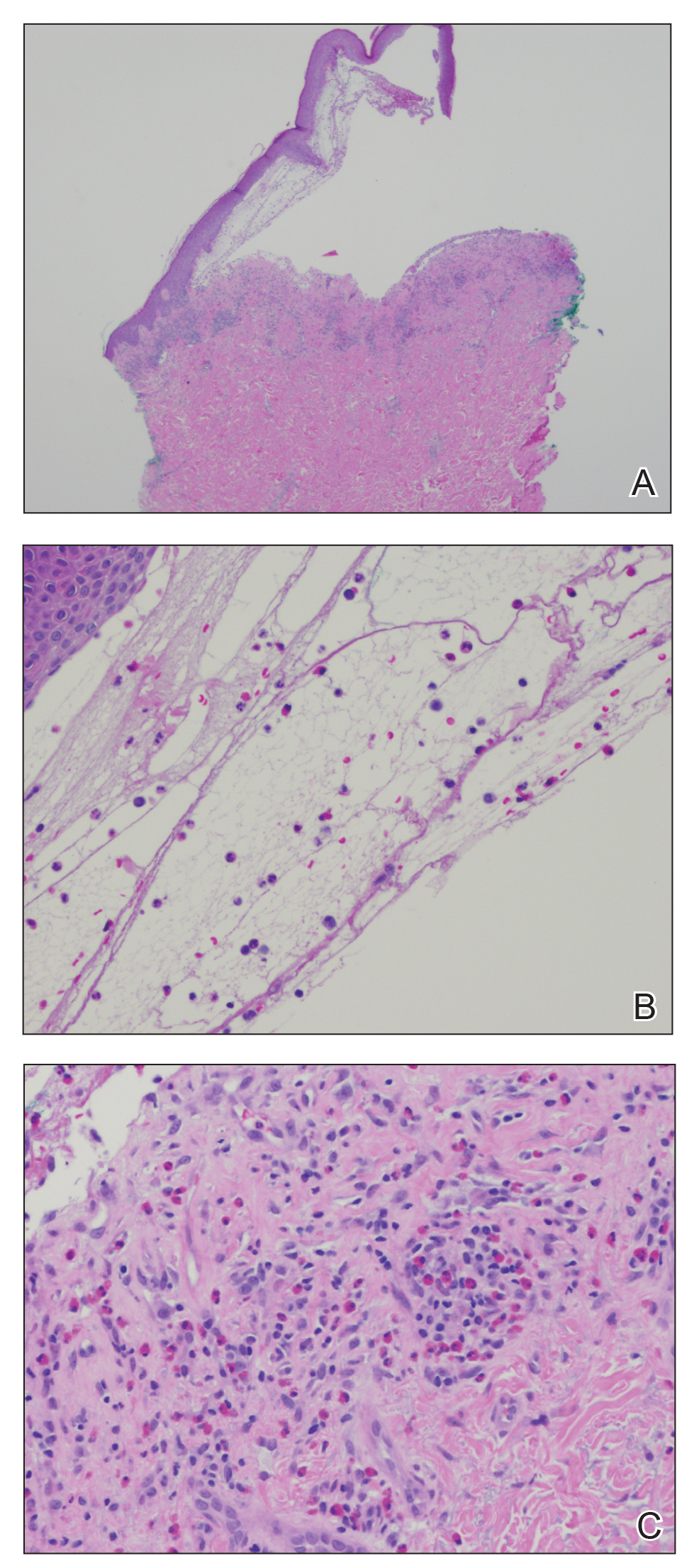
Biopsy of involved tissue characteristically reveals fascial thickening and fibrosis.10,13,15 A lymphoplasmacytic infiltrate normally is found in the subcutaneous tissues and fascia and may extend to involve the deeper dermis15 but usually spares the epidermis.3 It is important to note that increased numbers of eosinophils are not always found in the affected fascia, especially in the later stages of the disease and after steroid treatment.3,15 Muscle involvement is variable. When muscle is involved, histologic features range from mild inflammation with no evidence of necrosis3 to substantial fibrinoid necrosis.13
Magnetic resonance imaging has become a valuable tool in the diagnosis and treatment of EF. Magnetic resonance imaging findings in EF patients typically reveal fascial thickening on T1-weighted images, enhancement after the use of contrast, and hyperintensity on T2-weighted images.7 Magnetic resonance imaging has proven useful in supporting clinical diagnosis, monitoring disease activity, identifying optimal biopsy location, and determining response to treatment.3,7,8,11,13 Magnetic resonance imaging also has been proven to be particularly useful with atypical clinical presentations.8 Although deep tissue biopsy remains the gold standard for diagnosis,13 magnetic resonance imaging may provide equal or superior diagnostic information.
In general, the prognosis is very good, and the majority of patients will achieve complete remission and cure.3 Up to one-third of patients with EF may experience spontaneous remission without any treatment intervention.10 The condition generally is highly responsive to oral corticosteroids,6,10,15 and it has been reported that up to 70% of patients will respond to corticosteroid treatment.3 Most patients respond to a daily dose of prednisone (0.5–1.5 mg/kg), which is continued until clinical response is observed and then followed by a slow steroid taper over a period of several months.3 Patients with persistent fibrosis often require adjunctive therapy in addition to corticosteroids. A variety of adjunctive therapies have been reported to be effective, including hydroxychloroquine sulfate,5,10,13,15,16 azathioprine,15,16 ibuprofen,10,15 D-penicillamine,5,15 cyclophosphomide,15 methotrexate,6,13,15 cyclosporine,13,15 psoralen plus UVA,5,6,15 extracorporeal photochemotherapy,5,6,10,16 colchicine,5 cimetidine,5,6,10,16 infliximab,5,6 griseofulvin,16 ketotifen,16 sulfasalazine,13 and dapsone.16 Physical therapy has been reported to be useful in preventing permanent joint contractures.3,5,10,13,16 If treatment fails, the possibility of underlying malignancy must be considered3; however, long courses of treatment are not uncommon. Some patients may need 12 to 18 months of treatment for full response, and even refractory cases are likely to eventually achieve full remission.3
1. Shulman LE. Diffuse fasciitis with hypergammaglobulinemia and eosinophilia: a new syndrome? J Rheumatol. 1984;11:569-570.
2. Rodnan GP, DiBartolomeo AG, Medsger TA. Eosinophilic fasciitis: report of six cases of a newly recognized scleroderma-like syndrome. Arthritis Rheum. 1975;18:525.
3. Boin F, Hummers LK. Scleroderma-like fibrosing disorders. Rheum Dis Clin North Am. 2008;34:199-220, ix.
4. Carneiro S, Brotas A, Lamy F, et al. Eosinophilic fasciitis (Shulman syndrome). Cutis. 2005;75:228-232.
5. Horacek E, Sator PG, Gschnait F. “Venous furrowing”: a clue to the diagnosis of eosinophilic fasciitis. a case of eosinophilic fasciitis ultimately treated with oral PUVA therapy. Dermatology. 2007;215:89-90.
6. Daniel RS, Brown AN. Case report of unilateral eosinophilic fasciitis in a Vietnamese woman. Amer J Med Sci. 2009;337:153-154.
7. Moulton SJ, Kransdorf MJ, Ginsburg WW, et al. Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenol. 2005;184:975-978.
8. Sugimoto T, Nitta N, Kashiwagi A. Usefulness of magnetic resonance imaging in eosinophilic fasciitis [published online ahead of print January 9, 2007]. Rhuematol Int. 2007;27:791-792.
9. Mori Y, Kahari VM, Varga J. Scleroderma-like cutaneous syndromes. Curr Rheumatol Rep. 2002;4:113-122.
10. Antic M, Lautenschlager S, Itin PH. Eosinophilic fasciitis 30 years after—what do we really know? report of 11 patients and review of the literature. Dermatology. 2006;213:93-101.
11. Ortega-Loayza AG, Merritt BG, Groben PA, et al. Eosinophilic fasciitis in a female child. J Am Acad Dermatol. 2008;58(suppl 5):S72-S74.
12. Kroft EB, de Jong EM, Evers AW. Physical burden of symptoms in patients with localized scleroderma and eosinophilic fasciitis. Arch Dermatol. 2008;144:1394-1395.
13. Bischoff L, Derk CT. Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of literature. Int J Dermatol. 2008;47:29-35.
14. Al Hammadi A, Turchin T. Groove sign and eosinophilic fasciitis. J Cutan Med Surg. 2008;12:49.
15. Endo Y, Tamura A, Matsushima Y, et al. Eosinophilic fasciitis: report of two cases and a systemic review of the literature dealing with clinical variables that predict outcome. Clin Rheumatol. 2007;26:1445-1451.
16. Smith LC, Cox NH. Dapsone treatment for eosinophilic fasciitis. Arch Dermatol. 2008;144:845-847.
The Diagnosis: Eosinophilic Fasciitis (Shulman Syndrome)
In 1984, Shulman1 reported 2 cases of diffuse fasciitis with hypergammaglobulinemia and eosinophilia, which was later termed eosinophilic fasciitis (EF) by Rodnan et al.2 Eosinophilic fasciitis also is commonly known as diffuse fasciitis with eosinophilia3 or Shulman syndrome.3,4 It is an inflammatory condition of unknown etiology and pathogenesis, though an underlying autoimmune process has been proposed.3,5 The disorder is characterized by inflammation and subsequent fibrosis of deep fascia2 with variable involvement of the underlying muscle. It often is referred to as a sclerodermalike condition2,5-8 and is considered to be one of a group of fibrosing connective tissue disorders that may be confused with systemic sclerosis.3,4,6,9 Although the cause of EF is unknown, more than 50% of cases are associated with vigorous exercise or trauma.3 Other reported triggers and associations include Borrelia burgdorferi infection,5,6,10 arthropod bites,5,10 lymphoproliferative and hematologic disorders,5,6,10 inflammatory arthritis,6 morphea,3 thyroid dysfunction,5,6,10 statins,5,10 and phenytoin.5,10
There have been more than 250 cases of EF reported in the literature.3 Some authors report more frequent occurrence in males,3,4 while others report equal occurrence of disease in both males and females.5,10 Eosinophilic fasciitis has the highest incidence during the second to sixth decades of life,3,10 though childhood cases have been reported.3,11 White individuals appear to be affected most often, but sporadic cases in other ethnic groups also have been reported.3
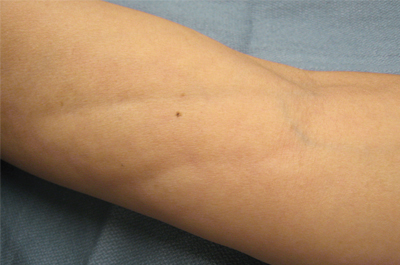
The clinical presentation of EF frequently is characterized by the rapid onset of erythema, pain, and nonpitting edema of the involved areas.5,7,10,11 Fatigue and itching also are reported symptoms.12 A cobblestone texture of the skin may be noted, commonly referred to as the peau d’orange effect.6,10 Woody induration subsequently develops, which may lead to contracture or limited range of motion.5,7,11-13 The distal extremities, particularly the forearms and calves, are the most common areas affected by EF.3 There usually is symmetric involvement; however, unilateral cases of EF also have been reported.3,6,10 Linear indentations may form along the vasculature of the involved areas when the extremities are lifted or extended. These indentations serve to demarcate the underlying muscle groups, forming the groove sign or venous furrowing.3,5,14 The epidermis is not characteristically involved in EF and wrinkling of the skin can be elicited by pinching,3 which may be helpful in clinically distinguishing EF from scleroderma. Sparing of the digits is another characteristic feature of adult-onset EF.3,10 However, involvement of the digits resulting in painless contracture has been reported in multiple childhood cases and may represent a phenotype specific to children.11 Involvement of the trunk is less frequently observed but may serve as a poor prognostic indicator; indeed, patients demonstrating young age of onset, morphealike skin sclerosis, and trunk involvement are more likely to develop refractory disease.15
Eosinophilic fasciitis is characterized by various laboratory abnormalities. Peripheral eosinophilia, hypergammaglobulinemia, elevated sedimentation rate,3,6,9,10,13,15 and elevated C-reactive protein3,6 are commonly reported; however, antinuclear antibody, rheumatoid factor, or antibodies associated with systemic sclerosis are not frequently found.3,6 There are no laboratory abnormalities required to render a diagnosis of EF, and absence of peripheral eosinophilia has been noted in up to 20% of cases.3,4 An elevation of creatine kinase or aldolase levels may be present if muscle is involved.3,6 In general, abnormal laboratory findings have not been found to correlate with disease activity13,15 and do not appear to have prognostic significance.15
Biopsy of involved tissue characteristically reveals fascial thickening and fibrosis.10,13,15 A lymphoplasmacytic infiltrate normally is found in the subcutaneous tissues and fascia and may extend to involve the deeper dermis15 but usually spares the epidermis.3 It is important to note that increased numbers of eosinophils are not always found in the affected fascia, especially in the later stages of the disease and after steroid treatment.3,15 Muscle involvement is variable. When muscle is involved, histologic features range from mild inflammation with no evidence of necrosis3 to substantial fibrinoid necrosis.13
Magnetic resonance imaging has become a valuable tool in the diagnosis and treatment of EF. Magnetic resonance imaging findings in EF patients typically reveal fascial thickening on T1-weighted images, enhancement after the use of contrast, and hyperintensity on T2-weighted images.7 Magnetic resonance imaging has proven useful in supporting clinical diagnosis, monitoring disease activity, identifying optimal biopsy location, and determining response to treatment.3,7,8,11,13 Magnetic resonance imaging also has been proven to be particularly useful with atypical clinical presentations.8 Although deep tissue biopsy remains the gold standard for diagnosis,13 magnetic resonance imaging may provide equal or superior diagnostic information.
In general, the prognosis is very good, and the majority of patients will achieve complete remission and cure.3 Up to one-third of patients with EF may experience spontaneous remission without any treatment intervention.10 The condition generally is highly responsive to oral corticosteroids,6,10,15 and it has been reported that up to 70% of patients will respond to corticosteroid treatment.3 Most patients respond to a daily dose of prednisone (0.5–1.5 mg/kg), which is continued until clinical response is observed and then followed by a slow steroid taper over a period of several months.3 Patients with persistent fibrosis often require adjunctive therapy in addition to corticosteroids. A variety of adjunctive therapies have been reported to be effective, including hydroxychloroquine sulfate,5,10,13,15,16 azathioprine,15,16 ibuprofen,10,15 D-penicillamine,5,15 cyclophosphomide,15 methotrexate,6,13,15 cyclosporine,13,15 psoralen plus UVA,5,6,15 extracorporeal photochemotherapy,5,6,10,16 colchicine,5 cimetidine,5,6,10,16 infliximab,5,6 griseofulvin,16 ketotifen,16 sulfasalazine,13 and dapsone.16 Physical therapy has been reported to be useful in preventing permanent joint contractures.3,5,10,13,16 If treatment fails, the possibility of underlying malignancy must be considered3; however, long courses of treatment are not uncommon. Some patients may need 12 to 18 months of treatment for full response, and even refractory cases are likely to eventually achieve full remission.3
The Diagnosis: Eosinophilic Fasciitis (Shulman Syndrome)
In 1984, Shulman1 reported 2 cases of diffuse fasciitis with hypergammaglobulinemia and eosinophilia, which was later termed eosinophilic fasciitis (EF) by Rodnan et al.2 Eosinophilic fasciitis also is commonly known as diffuse fasciitis with eosinophilia3 or Shulman syndrome.3,4 It is an inflammatory condition of unknown etiology and pathogenesis, though an underlying autoimmune process has been proposed.3,5 The disorder is characterized by inflammation and subsequent fibrosis of deep fascia2 with variable involvement of the underlying muscle. It often is referred to as a sclerodermalike condition2,5-8 and is considered to be one of a group of fibrosing connective tissue disorders that may be confused with systemic sclerosis.3,4,6,9 Although the cause of EF is unknown, more than 50% of cases are associated with vigorous exercise or trauma.3 Other reported triggers and associations include Borrelia burgdorferi infection,5,6,10 arthropod bites,5,10 lymphoproliferative and hematologic disorders,5,6,10 inflammatory arthritis,6 morphea,3 thyroid dysfunction,5,6,10 statins,5,10 and phenytoin.5,10
There have been more than 250 cases of EF reported in the literature.3 Some authors report more frequent occurrence in males,3,4 while others report equal occurrence of disease in both males and females.5,10 Eosinophilic fasciitis has the highest incidence during the second to sixth decades of life,3,10 though childhood cases have been reported.3,11 White individuals appear to be affected most often, but sporadic cases in other ethnic groups also have been reported.3
The clinical presentation of EF frequently is characterized by the rapid onset of erythema, pain, and nonpitting edema of the involved areas.5,7,10,11 Fatigue and itching also are reported symptoms.12 A cobblestone texture of the skin may be noted, commonly referred to as the peau d’orange effect.6,10 Woody induration subsequently develops, which may lead to contracture or limited range of motion.5,7,11-13 The distal extremities, particularly the forearms and calves, are the most common areas affected by EF.3 There usually is symmetric involvement; however, unilateral cases of EF also have been reported.3,6,10 Linear indentations may form along the vasculature of the involved areas when the extremities are lifted or extended. These indentations serve to demarcate the underlying muscle groups, forming the groove sign or venous furrowing.3,5,14 The epidermis is not characteristically involved in EF and wrinkling of the skin can be elicited by pinching,3 which may be helpful in clinically distinguishing EF from scleroderma. Sparing of the digits is another characteristic feature of adult-onset EF.3,10 However, involvement of the digits resulting in painless contracture has been reported in multiple childhood cases and may represent a phenotype specific to children.11 Involvement of the trunk is less frequently observed but may serve as a poor prognostic indicator; indeed, patients demonstrating young age of onset, morphealike skin sclerosis, and trunk involvement are more likely to develop refractory disease.15
Eosinophilic fasciitis is characterized by various laboratory abnormalities. Peripheral eosinophilia, hypergammaglobulinemia, elevated sedimentation rate,3,6,9,10,13,15 and elevated C-reactive protein3,6 are commonly reported; however, antinuclear antibody, rheumatoid factor, or antibodies associated with systemic sclerosis are not frequently found.3,6 There are no laboratory abnormalities required to render a diagnosis of EF, and absence of peripheral eosinophilia has been noted in up to 20% of cases.3,4 An elevation of creatine kinase or aldolase levels may be present if muscle is involved.3,6 In general, abnormal laboratory findings have not been found to correlate with disease activity13,15 and do not appear to have prognostic significance.15
Biopsy of involved tissue characteristically reveals fascial thickening and fibrosis.10,13,15 A lymphoplasmacytic infiltrate normally is found in the subcutaneous tissues and fascia and may extend to involve the deeper dermis15 but usually spares the epidermis.3 It is important to note that increased numbers of eosinophils are not always found in the affected fascia, especially in the later stages of the disease and after steroid treatment.3,15 Muscle involvement is variable. When muscle is involved, histologic features range from mild inflammation with no evidence of necrosis3 to substantial fibrinoid necrosis.13
Magnetic resonance imaging has become a valuable tool in the diagnosis and treatment of EF. Magnetic resonance imaging findings in EF patients typically reveal fascial thickening on T1-weighted images, enhancement after the use of contrast, and hyperintensity on T2-weighted images.7 Magnetic resonance imaging has proven useful in supporting clinical diagnosis, monitoring disease activity, identifying optimal biopsy location, and determining response to treatment.3,7,8,11,13 Magnetic resonance imaging also has been proven to be particularly useful with atypical clinical presentations.8 Although deep tissue biopsy remains the gold standard for diagnosis,13 magnetic resonance imaging may provide equal or superior diagnostic information.
In general, the prognosis is very good, and the majority of patients will achieve complete remission and cure.3 Up to one-third of patients with EF may experience spontaneous remission without any treatment intervention.10 The condition generally is highly responsive to oral corticosteroids,6,10,15 and it has been reported that up to 70% of patients will respond to corticosteroid treatment.3 Most patients respond to a daily dose of prednisone (0.5–1.5 mg/kg), which is continued until clinical response is observed and then followed by a slow steroid taper over a period of several months.3 Patients with persistent fibrosis often require adjunctive therapy in addition to corticosteroids. A variety of adjunctive therapies have been reported to be effective, including hydroxychloroquine sulfate,5,10,13,15,16 azathioprine,15,16 ibuprofen,10,15 D-penicillamine,5,15 cyclophosphomide,15 methotrexate,6,13,15 cyclosporine,13,15 psoralen plus UVA,5,6,15 extracorporeal photochemotherapy,5,6,10,16 colchicine,5 cimetidine,5,6,10,16 infliximab,5,6 griseofulvin,16 ketotifen,16 sulfasalazine,13 and dapsone.16 Physical therapy has been reported to be useful in preventing permanent joint contractures.3,5,10,13,16 If treatment fails, the possibility of underlying malignancy must be considered3; however, long courses of treatment are not uncommon. Some patients may need 12 to 18 months of treatment for full response, and even refractory cases are likely to eventually achieve full remission.3
1. Shulman LE. Diffuse fasciitis with hypergammaglobulinemia and eosinophilia: a new syndrome? J Rheumatol. 1984;11:569-570.
2. Rodnan GP, DiBartolomeo AG, Medsger TA. Eosinophilic fasciitis: report of six cases of a newly recognized scleroderma-like syndrome. Arthritis Rheum. 1975;18:525.
3. Boin F, Hummers LK. Scleroderma-like fibrosing disorders. Rheum Dis Clin North Am. 2008;34:199-220, ix.
4. Carneiro S, Brotas A, Lamy F, et al. Eosinophilic fasciitis (Shulman syndrome). Cutis. 2005;75:228-232.
5. Horacek E, Sator PG, Gschnait F. “Venous furrowing”: a clue to the diagnosis of eosinophilic fasciitis. a case of eosinophilic fasciitis ultimately treated with oral PUVA therapy. Dermatology. 2007;215:89-90.
6. Daniel RS, Brown AN. Case report of unilateral eosinophilic fasciitis in a Vietnamese woman. Amer J Med Sci. 2009;337:153-154.
7. Moulton SJ, Kransdorf MJ, Ginsburg WW, et al. Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenol. 2005;184:975-978.
8. Sugimoto T, Nitta N, Kashiwagi A. Usefulness of magnetic resonance imaging in eosinophilic fasciitis [published online ahead of print January 9, 2007]. Rhuematol Int. 2007;27:791-792.
9. Mori Y, Kahari VM, Varga J. Scleroderma-like cutaneous syndromes. Curr Rheumatol Rep. 2002;4:113-122.
10. Antic M, Lautenschlager S, Itin PH. Eosinophilic fasciitis 30 years after—what do we really know? report of 11 patients and review of the literature. Dermatology. 2006;213:93-101.
11. Ortega-Loayza AG, Merritt BG, Groben PA, et al. Eosinophilic fasciitis in a female child. J Am Acad Dermatol. 2008;58(suppl 5):S72-S74.
12. Kroft EB, de Jong EM, Evers AW. Physical burden of symptoms in patients with localized scleroderma and eosinophilic fasciitis. Arch Dermatol. 2008;144:1394-1395.
13. Bischoff L, Derk CT. Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of literature. Int J Dermatol. 2008;47:29-35.
14. Al Hammadi A, Turchin T. Groove sign and eosinophilic fasciitis. J Cutan Med Surg. 2008;12:49.
15. Endo Y, Tamura A, Matsushima Y, et al. Eosinophilic fasciitis: report of two cases and a systemic review of the literature dealing with clinical variables that predict outcome. Clin Rheumatol. 2007;26:1445-1451.
16. Smith LC, Cox NH. Dapsone treatment for eosinophilic fasciitis. Arch Dermatol. 2008;144:845-847.
1. Shulman LE. Diffuse fasciitis with hypergammaglobulinemia and eosinophilia: a new syndrome? J Rheumatol. 1984;11:569-570.
2. Rodnan GP, DiBartolomeo AG, Medsger TA. Eosinophilic fasciitis: report of six cases of a newly recognized scleroderma-like syndrome. Arthritis Rheum. 1975;18:525.
3. Boin F, Hummers LK. Scleroderma-like fibrosing disorders. Rheum Dis Clin North Am. 2008;34:199-220, ix.
4. Carneiro S, Brotas A, Lamy F, et al. Eosinophilic fasciitis (Shulman syndrome). Cutis. 2005;75:228-232.
5. Horacek E, Sator PG, Gschnait F. “Venous furrowing”: a clue to the diagnosis of eosinophilic fasciitis. a case of eosinophilic fasciitis ultimately treated with oral PUVA therapy. Dermatology. 2007;215:89-90.
6. Daniel RS, Brown AN. Case report of unilateral eosinophilic fasciitis in a Vietnamese woman. Amer J Med Sci. 2009;337:153-154.
7. Moulton SJ, Kransdorf MJ, Ginsburg WW, et al. Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenol. 2005;184:975-978.
8. Sugimoto T, Nitta N, Kashiwagi A. Usefulness of magnetic resonance imaging in eosinophilic fasciitis [published online ahead of print January 9, 2007]. Rhuematol Int. 2007;27:791-792.
9. Mori Y, Kahari VM, Varga J. Scleroderma-like cutaneous syndromes. Curr Rheumatol Rep. 2002;4:113-122.
10. Antic M, Lautenschlager S, Itin PH. Eosinophilic fasciitis 30 years after—what do we really know? report of 11 patients and review of the literature. Dermatology. 2006;213:93-101.
11. Ortega-Loayza AG, Merritt BG, Groben PA, et al. Eosinophilic fasciitis in a female child. J Am Acad Dermatol. 2008;58(suppl 5):S72-S74.
12. Kroft EB, de Jong EM, Evers AW. Physical burden of symptoms in patients with localized scleroderma and eosinophilic fasciitis. Arch Dermatol. 2008;144:1394-1395.
13. Bischoff L, Derk CT. Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of literature. Int J Dermatol. 2008;47:29-35.
14. Al Hammadi A, Turchin T. Groove sign and eosinophilic fasciitis. J Cutan Med Surg. 2008;12:49.
15. Endo Y, Tamura A, Matsushima Y, et al. Eosinophilic fasciitis: report of two cases and a systemic review of the literature dealing with clinical variables that predict outcome. Clin Rheumatol. 2007;26:1445-1451.
16. Smith LC, Cox NH. Dapsone treatment for eosinophilic fasciitis. Arch Dermatol. 2008;144:845-847.
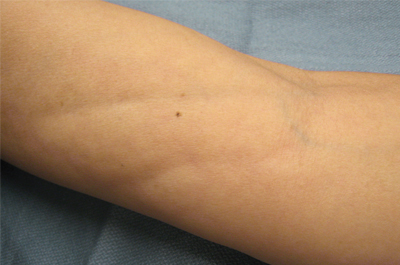
A 50-year-old woman presented with progressive tightening of her extremities of 2 months’ duration with eventual involvement of her trunk. On physical examination, the distal aspect of the patient’s bilateral upper and lower extremities were indurated, tender to palpation, and had a limited range of motion. On extension, linear depressions were noted on the ventral aspects of her forearms.