User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Minimal Dissection Reduces Herniation After Pediatric Fundoplication
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
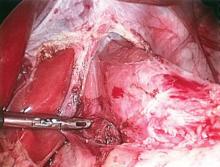
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
Minimal Dissection Reduces Herniation After Pediatric Fundoplication
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
HUNTINGTON BEACH, CALIF. – Fewer herniations and gastroesophageal reflux complications were seen in children undergoing minimal-dissection laparoscopic fundoplication than in those undergoing a more conventional procedure in a randomized trial of 177 patients.
In recent years, surgeons have debated whether it’s best during pediatric fundoplication to free the esophagus from the phrenoesophageal membrane or leave it embedded in that anatomical anchor.
The conventional approach allows the surgeon to pull a bit of the esophagus into the abdomen so that it can be wrapped with the gastric fundus, as is done in adults. The second approach leaves the esophagus and its attachments in place; the top of the stomach is simply wrapped around the gastroesophageal junction.
Not only does minimal-dissection laparoscopic fundoplication control reflux at least as well as the conventional approach does, it also greatly reduces the likelihood that the fundal wrap and stomach will herniate into the chest cavity, said Dr. Shawn St. Peter at the annual Academic Surgical Congress.
The trial randomized 87 children to laparoscopic fundoplication with circumferential division of the phrenoesophageal attachments; 90 children were randomized to laparoscopic fundoplication with minimal esophageal mobilization and no violation of the phrenoesophageal membrane.
The groups had no statistically significant differences in preoperative reflux symptoms, weight, neurologic impairment, or other parameters. The mean age in both groups was about 2 years; slightly more than half were male.
Dr. St. Peter, a pediatric surgeon at the Children’s Mercy Hospital in Kansas City, Mo., and five other surgeons each performed roughly equal numbers of both procedures.
At 1-year follow-up, the herniation rate by contrast study was 30% in children who had their phrenoesophageal membrane taken down, and 7.8% when it was left alone (P = .002).
Similarly, 18.4% of children in the take-down group needed at least one surgery to reduce a herniation; the redo rate in the minimal-dissection group was 3.3% (P = .006).
The minimal-dissection group also had fewer postop gastroesophageal reflux complications – weight loss, pneumonia, and acute life-threatening events – although the trend was not statistically significant (J. Pediatr. Surg. 2011;46:163-8).
"The results are very, very clear, and show that going forward we should be doing the minimal-dissection approach. This study should significantly change practice," said Dr. R. Lawrence Moss, surgeon-in-chief at Nationwide Children’s Hospital in Columbus, Ohio.
"This is one of the most significant studies in [pediatric] surgery for a long time, and it sets a standard that technique questions can be answered in a scientific manner. It really raises the bar for all of us," said Dr. Moss, who did not participate in the trial but was familiar with its results.
The most satisfying outcome of the trial was the reduction in hernias, Dr. St. Peter said in an interview following his presentation.
Adults aren’t typically at risk for fundal wrap herniation; the adult diaphragm is strong enough to hold the wrap in place. In children, however, simple inhalation – because of negative chest pressure – can sometimes pop the wrap and stomach into the chest, where they get stuck on top of the diaphragm.
"Anybody who does fundos [in children] has at least one patient who has had that problem. It’s a nightmare," Dr. St. Peter said. Postoperative retching, vomiting, and gagging may occur, and attempts to reduce the hernia sometimes fail. If multiple attempts fail, the stomach may no longer empty properly, leaving children with chronic gastric pain and other long-term complications.
During minimal-dissection laparoscopic fundoplication, Dr. St. Peter takes down the gastrohepatic ligament up toward diaphragm, without touching the phrenoesophageal membrane. He then bluntly creates an opening into the abdomen directly behind the esophagus, preserving all the anterolateral attachments.
Without membrane dissection, the operation goes a bit faster. But surgeons must be careful: "Even gentle manipulation can be enough to free up the diaphragm from the esophagus in a baby," he said.
Dr. St. Peter and his colleagues are investigating whether esophagocrural sutures – which were placed in all trial subjects – are needed when the phrenoesophageal membrane is left intact.
Those sutures are important when it’s taken down, but "if you never open the door, putting four sutures in the seam of the door seems silly," Dr. St. Peter said.
Thus far, they have enrolled 35 patients in a randomized trial aiming for a total enrollment of 120 patients. Half will get the sutures; the other half will not. But all the children will leave the OR with their esophageal attachments intact.
"The second we closed the study, that was the last time we took down a membrane," Dr. St. Peter said.
He and Dr. Moss said they have no conflicts of interest. The trial received no outside funding.
Major Finding: The risk of postop fundal wrap herniation is greatly reduced when the esophagus is not freed from the phrenoesophageal membrane during pediatric fundoplication.
Data Source: Prospective, randomized trial involving 177 children.
Disclosures: Dr. St. Peter said he has no conflicts of interest; the study received no outside funding.
Study Casts Doubt on Need for High-Dose Perioperative Steroids
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
FROM THE ANNUAL ACADEMIC SURGICAL CONGRESS
Study Casts Doubt on Need for High-Dose Perioperative Steroids
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
HUNTINGTON BEACH, CALIF. – For the past several decades, surgical patients have been given supraphysiologic perioperative steroid doses to prevent cardiovascular collapse, but results of a recent pilot study suggest it’s time to rethink the high-dose dogma.
There were two case reports in the 1950s of cardiovascular collapse and death in patients who were abruptly taken off steroids just before surgery (JAMA 1952;149:1542-3; Ann. Intern. Med. 1953;39:116-26).
"We don’t know what exactly happened to those patients, [but] if you look at a lot of the surgical textbooks, they’ll recommend high-dose steroids," sometimes in the range of 100-mg IV hydrocortisone every 8 hours, explained Dr. Karen Zaghiyan, a surgery resident at Cedars-Sinai Medical Center in Los Angeles, in an interview.
The problem is that steroids pose risks such as wound infection and delayed healing, plus hypertension, hyperglycemia, and psychosis, among others.
Until now, there’s been "no good evidence to support [the move] one way or the other," Dr. Zaghiyan said.
She and her colleagues at Cedars-Sinai eschewed high-dose perioperative steroids in 26 inflammatory bowel disease (IBD) patients who underwent 32 colorectal procedures, including 10 ileocolic resections and 9 ileal pouch anal anastomoses. Dr. Zaghiyan presented the results of their study at the annual Academic Surgical Congress.
The patients’ median age was 40 years, and 19 were men.
In all, 22 operations were done on patients who had been off steroids 1-12 months (median, 6 months); those patients got no perioperative steroids. Ten operations were done on patients taking 5-40 mg of prednisone daily (median, 23 mg); those patients remained on the IV hydrocortisone equivalent of their customary dose, followed by a postoperative taper.
There was no cardiovascular collapse in the perioperative period, and there was no need for vasopressors or steroid rescue. Although there were hemodynamic problems, they did not appear to be related to adrenal insufficiency.
Three patients became hypotensive because of operative or postoperative bleeding; their systolic blood pressure dropped below 90 mmHg, but they responded to transfusions. Another case of hypotension responded to fluid bolus; a fifth resolved on its own and may have been the result of a faulty blood pressure reading.
Heart rates temporarily topped 120 beats per minute in five patients and fell below 60 bpm in eight; the tachy- and bradycardia were not associated with hypotension, and resolved without intervention.
Temperatures climbed above 100.4° F in nine patients, but fevers resolved with simple cooling measures or acetaminophen. There was no hypothermia.
If any of those problems were caused by adrenal insufficiency, resolving them would have required steroids, Dr. Zaghiyan said.
"Steroid-treated IBD patients undergoing major colorectal surgery appear to have no clinically significant hemodynamic instability when treated with low-dose perioperative steroids. Management of these patients with perioperative low-dose steroids appears to be safe," Dr. Zaghiyan concluded.
The findings did not surprise Dr. Stefan Holubar, a colorectal surgeon at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., who has been trying low-dose steroids in his own IBD surgical cases.
"I thought [this study] was really fantastic. It adds some evidence" to a practice that is gaining acceptance among colorectal surgeons after "being adopted from the transplant literature. It hasn’t really been studied in colorectal surgery," Dr. Holubar said.
"I think we overtreat patients with steroids," but although it may be okay to give low-dose steroids, it may be inappropriate to give nothing, he said, adding that more research is needed.
Dr. Zaghiyan and her colleagues have begun to enroll 120 IBD patients into a prospective trial that will randomize patients to low- or high-dose perioperative steroids. In addition to hemodynamic instability, they will investigate more subtle signs of adrenal insufficiency, including nausea, vomiting, and lethargy.
They plan to publish their interim results later this year.
Dr. Zaghiyan and Dr. Holubar said they have no conflicts of interest.
FROM THE ANNUAL ACADEMIC SURGICAL CONGRESS
Major Finding: IBD patients did not develop hemodynamic instability related to adrenal insufficiency when they underwent colorectal surgery without high-dose perioperative steroids.
Data Source: Retrospective study of 26 steroid-dependent or recently dependent patients.
Disclosures: Dr. Zaghiyan said she has no conflicts of interest.
Cadaver Artery Grafts May Help Save Limbs
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
FROM THE ANNUAL ACADEMIC SURGICAL CONGRESS
Cadaver Artery Grafts May Help Save Limbs
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
HUNTINGTON BEACH, CALIF. – Cryopreserved arterial homografts show promise for reperfusion in patients with severe vascular disease whose only other option may be a below- or above-the-knee amputation, results of a retrospective case series suggested.
Dr. Joseph Naoum and his colleagues in the division of vascular surgery at Methodist Hospital in Houston successfully used cryopreserved arterial homografts–arteries harvested from cadavers and frozen–to reperfuse feet in 13 such patients.
After 18 months, the cumulative patency rate was 58.6%, Dr. Naoum said at the annual Academic Surgical Congress.
"If we had not used arterial homografts, [these patients] would have certainly required below-the-knee or above-the-knee amputations," Dr. Naoum said in an interview.
The findings add weight to the small body of literature showing that homografts can help in such cases.
The patients’ average age was 71 years, and five were men. Comorbidities included peripheral vascular disease (12 patients), diabetes (7), foot infections or gangrene (10), foot ischemia but no wound (2), and an infected Gore-Tex graft (1).
Dr. Naoum said he chose arterial homografts instead of vein homografts to cut down potential graft complications; arteries have more uniform diameters and no valves.
Four patients got femoral below-the-knee popliteal grafts; four had femoral- to anterior-tibial-artery grafts; and three had femoral- to posterior-tibial-artery grafts. Two patients received femoral- to peroneal-artery grafts.
Only patients who could tolerate the surgery, which is a longer and more complicated procedure than leg amputation, and who were currently ambulatory underwent the procedure.
"There is no point using these homografts to preserve limbs if patients are not walking," Dr Naoum noted.
The grafts cost about $3,000 and range in length from about 25 to 35 cm, depending on the donor.
"We like to ask for the longest piece possible," to avoid splicing. "However, we get what is available based on the diameter requested and blood-type match," Dr. Naoum said.
Once thawed per supplier directions, the homografts handle like any other graft tissue. Suturing is standard.
Dr. Naoum said he and some of his colleagues like to tunnel the grafts under subcutaneous fat instead of anatomically, to minimize compression. They also prefer to arterialize the graft before making the distal anastomoses to elongate the graft for better sizing and to work out any kinks, he said.
Patients were told to stop smoking after their operations (five of them smoked), and they were put on aspirin, Plavix (clopidogrel), and a statin, if they were not on one already. There’s no evidence that antirejection drugs are needed, Dr. Naoum said.
Two patients later needed toe amputations, and four required transmetatarsal amputations.
The 18-month patency rate was less than the perhaps 75% patency rate that would be expected had they been grafted with their own veins. Even so, the restored blood flow "was enough to allow the wounds to heal," Dr. Naoum said.
He said he plans to continue studying the use of arterial homografts to better define factors associated with good outcomes.
"What is needed is a greater experience to identify patients who will benefit most from such procedures, and those in whom an amputation may obviate a bypass that will not last," he said.
Dr. Naoum is also curious about why the grafts fail; two patients needed angioplasty to keep their grafts open, and thrombectomy was performed in one.
Cryopreservation makes cells thicker, perhaps causing intimal tears and scarring. Poor runoff is also a problem. If distal vessels can’t handle the new blood flow, pressure builds up in the graft, leading to clots and other problems, he said.
Dr. Naoum said that he was a consultant for CryoLife Inc., a major supplier of arterial homografts, in 2009, but is no longer involved with the company. He said he received no discounts on the grafts used in the case series.
FROM THE ANNUAL ACADEMIC SURGICAL CONGRESS
Major Finding: Ischemic feet reperfused with arterial homografts led to an 18-month cumulative patency rate of 58.6% in 13 patients.
Data Source: Retrospective case series.
Disclosures: Dr. Naoum said he had no relevant financial disclosures.
Despite Small Steps, EHR Interoperability Remains Elusive
SEATTLE – True electronic health record interoperability, with seamless information transfer between systems made by different companies, is still years off, agreed panelists discussing health information technology at the Swedish Medical Center Symposium "Innovation in the Age of Reform."
They also agreed that when interoperability comes, it will quickly identify emerging public health problems, address outcomes disparities, and lead to new drugs and other treatments because connected systems will, in effect, function as a massive clinical database.
"We would be a failure as an industry if we weren’t [eventually] able to find problems with chloromycetin and thalidomide [for example] much earlier" using the new technology, said Judith Faulkner, founder and CEO of the electronic health records (EHR) company Epic Systems. "I would hope we can focus on things such as autism and figure out the causes."
The lack of EHR standardization stands in the way of such potential, panelists said. The tens of thousands of data elements in Epic’s database are different from the elements in the Cerner database, which are different from those in the AllScripts database, said Peter Neupert, corporate vice president of Microsoft’s health solutions group.
One of the reasons, he said, is that vendors have little economic incentive to share information and standardize their approaches.
If an interoperability solution is not found, however, "China’s going to figure it out and export it here, or India is going to export it here," said Mr. Neupert. Those countries are developing health information technology to sell at lower prices than U.S. developers’ prices, he said.
Microsoft’s HealthVault allows consumers to store health information online for quick access wherever they’re treated, among other functions. Amalga, another Microsoft product, allows organizations to aggregate and mine clinical data.
Epic is developing Care Everywhere, a system to transfer medical records – with patients’ consent – across different EHR systems. It’s also working on a Connect the Docs system to facilitate communication and expertise-sharing between physicians, Ms. Faulkner said.
The federal government is working on interoperability fixes, too, said panelists. The current incentives for physicians and hospitals to install EHR systems include the goal that they eventually will be interoperable.
Among other measures, the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act funds the formation of regional health information repositories that can be queried by providers. The Office of the National Coordinator for Health Information Technology created by the act is developing a secure, e-mail–like system over which providers can exchange patients’ medical information.
HITECH , however, "is a start, not a finish," said Rep. Jay Inslee (D-Wash.), also a panelist. He agreed that the challenge remains in "making sure systems can work together."
Mr. Neupert expressed confidence. "Computing is going to get 1,000 times faster in the next 10 years. With cheap storage and 1,000 times the processing power, we can translate stuff in Epic’s data store [and] Cerner’s data store and every other data store into a meaningful operational data asset. It’s going to be really fabulous for individuals."
SEATTLE – True electronic health record interoperability, with seamless information transfer between systems made by different companies, is still years off, agreed panelists discussing health information technology at the Swedish Medical Center Symposium "Innovation in the Age of Reform."
They also agreed that when interoperability comes, it will quickly identify emerging public health problems, address outcomes disparities, and lead to new drugs and other treatments because connected systems will, in effect, function as a massive clinical database.
"We would be a failure as an industry if we weren’t [eventually] able to find problems with chloromycetin and thalidomide [for example] much earlier" using the new technology, said Judith Faulkner, founder and CEO of the electronic health records (EHR) company Epic Systems. "I would hope we can focus on things such as autism and figure out the causes."
The lack of EHR standardization stands in the way of such potential, panelists said. The tens of thousands of data elements in Epic’s database are different from the elements in the Cerner database, which are different from those in the AllScripts database, said Peter Neupert, corporate vice president of Microsoft’s health solutions group.
One of the reasons, he said, is that vendors have little economic incentive to share information and standardize their approaches.
If an interoperability solution is not found, however, "China’s going to figure it out and export it here, or India is going to export it here," said Mr. Neupert. Those countries are developing health information technology to sell at lower prices than U.S. developers’ prices, he said.
Microsoft’s HealthVault allows consumers to store health information online for quick access wherever they’re treated, among other functions. Amalga, another Microsoft product, allows organizations to aggregate and mine clinical data.
Epic is developing Care Everywhere, a system to transfer medical records – with patients’ consent – across different EHR systems. It’s also working on a Connect the Docs system to facilitate communication and expertise-sharing between physicians, Ms. Faulkner said.
The federal government is working on interoperability fixes, too, said panelists. The current incentives for physicians and hospitals to install EHR systems include the goal that they eventually will be interoperable.
Among other measures, the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act funds the formation of regional health information repositories that can be queried by providers. The Office of the National Coordinator for Health Information Technology created by the act is developing a secure, e-mail–like system over which providers can exchange patients’ medical information.
HITECH , however, "is a start, not a finish," said Rep. Jay Inslee (D-Wash.), also a panelist. He agreed that the challenge remains in "making sure systems can work together."
Mr. Neupert expressed confidence. "Computing is going to get 1,000 times faster in the next 10 years. With cheap storage and 1,000 times the processing power, we can translate stuff in Epic’s data store [and] Cerner’s data store and every other data store into a meaningful operational data asset. It’s going to be really fabulous for individuals."
SEATTLE – True electronic health record interoperability, with seamless information transfer between systems made by different companies, is still years off, agreed panelists discussing health information technology at the Swedish Medical Center Symposium "Innovation in the Age of Reform."
They also agreed that when interoperability comes, it will quickly identify emerging public health problems, address outcomes disparities, and lead to new drugs and other treatments because connected systems will, in effect, function as a massive clinical database.
"We would be a failure as an industry if we weren’t [eventually] able to find problems with chloromycetin and thalidomide [for example] much earlier" using the new technology, said Judith Faulkner, founder and CEO of the electronic health records (EHR) company Epic Systems. "I would hope we can focus on things such as autism and figure out the causes."
The lack of EHR standardization stands in the way of such potential, panelists said. The tens of thousands of data elements in Epic’s database are different from the elements in the Cerner database, which are different from those in the AllScripts database, said Peter Neupert, corporate vice president of Microsoft’s health solutions group.
One of the reasons, he said, is that vendors have little economic incentive to share information and standardize their approaches.
If an interoperability solution is not found, however, "China’s going to figure it out and export it here, or India is going to export it here," said Mr. Neupert. Those countries are developing health information technology to sell at lower prices than U.S. developers’ prices, he said.
Microsoft’s HealthVault allows consumers to store health information online for quick access wherever they’re treated, among other functions. Amalga, another Microsoft product, allows organizations to aggregate and mine clinical data.
Epic is developing Care Everywhere, a system to transfer medical records – with patients’ consent – across different EHR systems. It’s also working on a Connect the Docs system to facilitate communication and expertise-sharing between physicians, Ms. Faulkner said.
The federal government is working on interoperability fixes, too, said panelists. The current incentives for physicians and hospitals to install EHR systems include the goal that they eventually will be interoperable.
Among other measures, the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act funds the formation of regional health information repositories that can be queried by providers. The Office of the National Coordinator for Health Information Technology created by the act is developing a secure, e-mail–like system over which providers can exchange patients’ medical information.
HITECH , however, "is a start, not a finish," said Rep. Jay Inslee (D-Wash.), also a panelist. He agreed that the challenge remains in "making sure systems can work together."
Mr. Neupert expressed confidence. "Computing is going to get 1,000 times faster in the next 10 years. With cheap storage and 1,000 times the processing power, we can translate stuff in Epic’s data store [and] Cerner’s data store and every other data store into a meaningful operational data asset. It’s going to be really fabulous for individuals."
FROM THE SWEDISH MEDICAL CENTER SYMPOSIUM "INNOVATION IN THE AGE OF REFORM"
Reminders to Patients Help Reduce Nonurgent ED Visits
SAN ANTONIO – When the Family Medical Center of Johnstown, Pa., encouraged patients to use its services for nonemergency care – instead of the nearby Memorial Medical Center emergency department – the number of center patients using the ED declined.
The results of the intervention were presented in a poster by Dr. Jeanne Spencer and Dr. Rashmin Adesara at a conference on practice improvement sponsored by the Society of Teachers of Family Medicine. The conference was also sponsored by the American Academy of Family Physicians.
The reminders came in the form of posters mounted in the Family Medical Center (FMC), a residency program with about 1,000 patient visits per month, plus follow-up letters to FMC patients who had used the ED for routine care during FMC operating hours.
Like most EDs, "[Memorial Medical Center] is overcrowded, and at times the wait times are longer than we want. We all recognized some of the people going to the [ED] would have been better served coming to our office. We were trying to encourage them to come to the FMC," said the center’s director, Dr. Spencer, in an interview.
Some FMC patients were visiting the ED two to three times per month, either out of habit, because they were not aware that the center had same-day appointments, or because they assumed they would get better care in the ED, according to Dr. Adesara, who was a third-year FMC resident when he tackled the problem with Dr. Spencer’s help.
Money probably wasn’t the issue. Medicaid patients – the focus of the intervention – had no copay in the ED, but only a $2-$3 copay at the FMC, Dr. Adesara said, also in an interview.
The posters – a large one in the waiting room, smaller versions in the exam rooms – were hung in July 2009.
"We are here for you" was the message stated prominently on the posters.
The posters asked patients to call FMC for nonemergencies before going to the ED, and displayed the FMC’s telephone number. Patients were also reminded they’d be treated more quickly at the center, and by doctors who knew their medical histories.
Those who went to the ED anyway for nonurgent care got Dr. Spencer’s letter, after they were identified by Dr. Adesara’s record reviews.
"As your primary care physician, we came to know that you recently visited the emergency room. We hope that you are feeling better now," the form letter began.
It reemphasized the poster message, and mentioned the same-day appointments.
"Next time you have a problem like back pain, ear ache, nausea, diarrhea, sinus infection, [or] sore throat, call us before going to the emergency room. In most cases, we will be able to schedule you an appointment that meets your needs," the letter concluded.
Dr. Adesara sent 316 letters from July to the end of September; only two people complained, insisting their ED visits had been emergencies.
To assess the impact of the interventions, he compared the percentage of Memorial Medical Center ED visits by FMC patients from April to June 2009 – the period before the posters went up and the letters went out – to their percentage from October to December 2009, the postintervention period.
FMC patients accounted for about 7% of 17,865 total emergency room visits from April to June. The percentage began to decline during the intervention period, and then stabilized at about 6% of 17,363 ED visits from October to December.
Meanwhile, the percentage of patients from an internal medicine clinic in FMC’s building – which served as a control in the study – increased slightly from about 1.3% to 1.4% of ED visits over the same period.
"Our intervention appears to have resulted in a decrease in total ED utilization by our patients," Dr. Spencer and Dr. Adesara concluded in a poster displaying the study results.
"Putting up the posters is very quick and inexpensive. We bought our large poster for $25," she said. They are still up in the FMC.
Likewise, "if you see somebody going to the [ED] all the time, it might be pretty easy to have a staff person send them a quick letter to encourage them to come to the office rather than the [ED]," she said.
The study had no external funding and the investigators reported no conflicts of interest.
SAN ANTONIO – When the Family Medical Center of Johnstown, Pa., encouraged patients to use its services for nonemergency care – instead of the nearby Memorial Medical Center emergency department – the number of center patients using the ED declined.
The results of the intervention were presented in a poster by Dr. Jeanne Spencer and Dr. Rashmin Adesara at a conference on practice improvement sponsored by the Society of Teachers of Family Medicine. The conference was also sponsored by the American Academy of Family Physicians.
The reminders came in the form of posters mounted in the Family Medical Center (FMC), a residency program with about 1,000 patient visits per month, plus follow-up letters to FMC patients who had used the ED for routine care during FMC operating hours.
Like most EDs, "[Memorial Medical Center] is overcrowded, and at times the wait times are longer than we want. We all recognized some of the people going to the [ED] would have been better served coming to our office. We were trying to encourage them to come to the FMC," said the center’s director, Dr. Spencer, in an interview.
Some FMC patients were visiting the ED two to three times per month, either out of habit, because they were not aware that the center had same-day appointments, or because they assumed they would get better care in the ED, according to Dr. Adesara, who was a third-year FMC resident when he tackled the problem with Dr. Spencer’s help.
Money probably wasn’t the issue. Medicaid patients – the focus of the intervention – had no copay in the ED, but only a $2-$3 copay at the FMC, Dr. Adesara said, also in an interview.
The posters – a large one in the waiting room, smaller versions in the exam rooms – were hung in July 2009.
"We are here for you" was the message stated prominently on the posters.
The posters asked patients to call FMC for nonemergencies before going to the ED, and displayed the FMC’s telephone number. Patients were also reminded they’d be treated more quickly at the center, and by doctors who knew their medical histories.
Those who went to the ED anyway for nonurgent care got Dr. Spencer’s letter, after they were identified by Dr. Adesara’s record reviews.
"As your primary care physician, we came to know that you recently visited the emergency room. We hope that you are feeling better now," the form letter began.
It reemphasized the poster message, and mentioned the same-day appointments.
"Next time you have a problem like back pain, ear ache, nausea, diarrhea, sinus infection, [or] sore throat, call us before going to the emergency room. In most cases, we will be able to schedule you an appointment that meets your needs," the letter concluded.
Dr. Adesara sent 316 letters from July to the end of September; only two people complained, insisting their ED visits had been emergencies.
To assess the impact of the interventions, he compared the percentage of Memorial Medical Center ED visits by FMC patients from April to June 2009 – the period before the posters went up and the letters went out – to their percentage from October to December 2009, the postintervention period.
FMC patients accounted for about 7% of 17,865 total emergency room visits from April to June. The percentage began to decline during the intervention period, and then stabilized at about 6% of 17,363 ED visits from October to December.
Meanwhile, the percentage of patients from an internal medicine clinic in FMC’s building – which served as a control in the study – increased slightly from about 1.3% to 1.4% of ED visits over the same period.
"Our intervention appears to have resulted in a decrease in total ED utilization by our patients," Dr. Spencer and Dr. Adesara concluded in a poster displaying the study results.
"Putting up the posters is very quick and inexpensive. We bought our large poster for $25," she said. They are still up in the FMC.
Likewise, "if you see somebody going to the [ED] all the time, it might be pretty easy to have a staff person send them a quick letter to encourage them to come to the office rather than the [ED]," she said.
The study had no external funding and the investigators reported no conflicts of interest.
SAN ANTONIO – When the Family Medical Center of Johnstown, Pa., encouraged patients to use its services for nonemergency care – instead of the nearby Memorial Medical Center emergency department – the number of center patients using the ED declined.
The results of the intervention were presented in a poster by Dr. Jeanne Spencer and Dr. Rashmin Adesara at a conference on practice improvement sponsored by the Society of Teachers of Family Medicine. The conference was also sponsored by the American Academy of Family Physicians.
The reminders came in the form of posters mounted in the Family Medical Center (FMC), a residency program with about 1,000 patient visits per month, plus follow-up letters to FMC patients who had used the ED for routine care during FMC operating hours.
Like most EDs, "[Memorial Medical Center] is overcrowded, and at times the wait times are longer than we want. We all recognized some of the people going to the [ED] would have been better served coming to our office. We were trying to encourage them to come to the FMC," said the center’s director, Dr. Spencer, in an interview.
Some FMC patients were visiting the ED two to three times per month, either out of habit, because they were not aware that the center had same-day appointments, or because they assumed they would get better care in the ED, according to Dr. Adesara, who was a third-year FMC resident when he tackled the problem with Dr. Spencer’s help.
Money probably wasn’t the issue. Medicaid patients – the focus of the intervention – had no copay in the ED, but only a $2-$3 copay at the FMC, Dr. Adesara said, also in an interview.
The posters – a large one in the waiting room, smaller versions in the exam rooms – were hung in July 2009.
"We are here for you" was the message stated prominently on the posters.
The posters asked patients to call FMC for nonemergencies before going to the ED, and displayed the FMC’s telephone number. Patients were also reminded they’d be treated more quickly at the center, and by doctors who knew their medical histories.
Those who went to the ED anyway for nonurgent care got Dr. Spencer’s letter, after they were identified by Dr. Adesara’s record reviews.
"As your primary care physician, we came to know that you recently visited the emergency room. We hope that you are feeling better now," the form letter began.
It reemphasized the poster message, and mentioned the same-day appointments.
"Next time you have a problem like back pain, ear ache, nausea, diarrhea, sinus infection, [or] sore throat, call us before going to the emergency room. In most cases, we will be able to schedule you an appointment that meets your needs," the letter concluded.
Dr. Adesara sent 316 letters from July to the end of September; only two people complained, insisting their ED visits had been emergencies.
To assess the impact of the interventions, he compared the percentage of Memorial Medical Center ED visits by FMC patients from April to June 2009 – the period before the posters went up and the letters went out – to their percentage from October to December 2009, the postintervention period.
FMC patients accounted for about 7% of 17,865 total emergency room visits from April to June. The percentage began to decline during the intervention period, and then stabilized at about 6% of 17,363 ED visits from October to December.
Meanwhile, the percentage of patients from an internal medicine clinic in FMC’s building – which served as a control in the study – increased slightly from about 1.3% to 1.4% of ED visits over the same period.
"Our intervention appears to have resulted in a decrease in total ED utilization by our patients," Dr. Spencer and Dr. Adesara concluded in a poster displaying the study results.
"Putting up the posters is very quick and inexpensive. We bought our large poster for $25," she said. They are still up in the FMC.
Likewise, "if you see somebody going to the [ED] all the time, it might be pretty easy to have a staff person send them a quick letter to encourage them to come to the office rather than the [ED]," she said.
The study had no external funding and the investigators reported no conflicts of interest.
FROM THE SOCIETY OF TEACHERS OF FAMILY MEDICINE CONFERENCE ON PRACTICE IMPROVEMENT
Major Finding: After an intervention encouraging patients of a family medicine center to use its services for routine care instead of a local emergency department, the percentage of ED patients from the center dropped from 7% to 6%.
Data Source: A 9-month, prospective study.
Disclosures: The study had no external funding and investigators reported no conflicts of interest.
Therapy Better Than Drugs for Eating Disorders
LOS ANGELES – There is very little evidence – and in some cases none at all – to support common pharmacologic treatments for anorexia and bulimia nervosa, according to Michael Strober, Ph.D.
Eating disorders "are the black hole of pharmacotherapy in psychiatry. There’s not much at this point in time we have to offer," Dr. Strober, director of the eating disorders program at the UCLA Neuropsychiatric Institute and Hospital, reported at a psychopharmacology update sponsored by the American Academy of Child and Adolescent Psychiatry.
For anorexia nervosa, evidence is stronger for family-based therapy in which families are taught to help a child eat and maintain weight.
Cognitive-behavioral therapy (CBT) is more effective than drugs for bulimia nervosa and remains its treatment of choice, said Dr. Strober, who estimated he’s treated more than 8,000 eating disorder patients during a career dating back to 1975.
Although selective serotonin reuptake inhibitors (SSRIs) are widely used to treat anorexia, "there is absolutely not a speck of evidence that these drugs, in the acutely malnourished state, are effective," or that they help maintain weight gain, said Dr. Strober, who also serves as director of the adolescent mood disorders program at the institute.
There is slight evidence for the atypical antipsychotic, olanzapine (Zyprexa).
In a trial funded by the drug’s maker, Eli Lilly, 16 anorexia patients were randomized to outpatient day treatment plus olanzapine, and 18 to day treatment plus placebo.
The mean body mass index was low-normal in both groups at the end of 13 weeks (19.66 kg/m2 in the placebo group vs. 20.30 in the olanzapine group). However, placebo patients started with a lower mean BMI of 15.93, compared with 16.39 among olanzapine patients.
Also, at week 13, 55.6% of placebo patients but 87.5% of olanzapine patients achieved the target BMI of 18.5 (Am. J. Psychiatry 2008;165:1281-8).
The differences were "not very dramatic," but were statistically significant, Dr. Strober said.
"We have no idea what the mechanism is. We don’t know if it’s mediated by improved psychological state or weight gain associated with olanzapine," he said.
Given the lack of data, Dr. Strober said that he and his colleagues typically refeed anorexia inpatients for a few weeks, and only then add atypical antipsychotics if they aren’t managing well.
"I generally think [they] have more of an effect than the SSRIs, although we have patients receiving SSRIs who report less anxiety and psychological discomfort with weight gain," Dr. Strober said.
In general, however, "I have never seen a robust clinical effect of these agents," he said.
For bulimia, antidepressants have been shown to help.
"Regardless of the antidepressant used, in the majority of published studies – we really don’t know how many unpublished studies have been buried – active drug separates from placebo," Dr. Strober said.
"What this means is that about 60%-65% of people randomized to active treatment report a response (defined as a 50% or greater reduction in the frequency of binge eating)," compared with placebo responses of about 35%-40%, he said.
"We get remission rates – which means no bingeing or purging the last 2 weeks of the trial – of about 10% on active drug, maybe 0%-3% on placebo," he said.
However, about 50% of responders "have a recurrence of their symptoms" within 5 months, "so these are not very effective drugs for the majority of patients," Dr. Strober said.
CBT does better: "After 12-16 weeks, we get response rates (defined in the same way) that are roughly 65%-70%. You get about 35%-38% that are fully remitted, and that response tends to be more durable," he said.
Evidence also supports family-based therapy (FBT) for anorexia nervosa.
In a recent study, 121 subjects aged 12-18 years with mild to moderate illness – the trial excluded patients below 75% of their ideal body weight – were randomized to either individual therapy or FBT.
At the end of treatment and at 12 months’ follow-up, body weights were normal in about half of FBT patients but only in about a quarter of individual therapy patients (Arch. Gen. Psychiatry 2010;67:1025-32).
"There’s a signal here, I think – a powerful signal," Dr. Strober said. "This is a meaningful difference."
Family-based therapy "is an important treatment. We don’t really know what the ingredient is; we just know that this has been helpful for a number of families, but you really have to be very skilled in working with these people," he said.
Dr. Strober said he has no disclosures.
LOS ANGELES – There is very little evidence – and in some cases none at all – to support common pharmacologic treatments for anorexia and bulimia nervosa, according to Michael Strober, Ph.D.
Eating disorders "are the black hole of pharmacotherapy in psychiatry. There’s not much at this point in time we have to offer," Dr. Strober, director of the eating disorders program at the UCLA Neuropsychiatric Institute and Hospital, reported at a psychopharmacology update sponsored by the American Academy of Child and Adolescent Psychiatry.
For anorexia nervosa, evidence is stronger for family-based therapy in which families are taught to help a child eat and maintain weight.
Cognitive-behavioral therapy (CBT) is more effective than drugs for bulimia nervosa and remains its treatment of choice, said Dr. Strober, who estimated he’s treated more than 8,000 eating disorder patients during a career dating back to 1975.
Although selective serotonin reuptake inhibitors (SSRIs) are widely used to treat anorexia, "there is absolutely not a speck of evidence that these drugs, in the acutely malnourished state, are effective," or that they help maintain weight gain, said Dr. Strober, who also serves as director of the adolescent mood disorders program at the institute.
There is slight evidence for the atypical antipsychotic, olanzapine (Zyprexa).
In a trial funded by the drug’s maker, Eli Lilly, 16 anorexia patients were randomized to outpatient day treatment plus olanzapine, and 18 to day treatment plus placebo.
The mean body mass index was low-normal in both groups at the end of 13 weeks (19.66 kg/m2 in the placebo group vs. 20.30 in the olanzapine group). However, placebo patients started with a lower mean BMI of 15.93, compared with 16.39 among olanzapine patients.
Also, at week 13, 55.6% of placebo patients but 87.5% of olanzapine patients achieved the target BMI of 18.5 (Am. J. Psychiatry 2008;165:1281-8).
The differences were "not very dramatic," but were statistically significant, Dr. Strober said.
"We have no idea what the mechanism is. We don’t know if it’s mediated by improved psychological state or weight gain associated with olanzapine," he said.
Given the lack of data, Dr. Strober said that he and his colleagues typically refeed anorexia inpatients for a few weeks, and only then add atypical antipsychotics if they aren’t managing well.
"I generally think [they] have more of an effect than the SSRIs, although we have patients receiving SSRIs who report less anxiety and psychological discomfort with weight gain," Dr. Strober said.
In general, however, "I have never seen a robust clinical effect of these agents," he said.
For bulimia, antidepressants have been shown to help.
"Regardless of the antidepressant used, in the majority of published studies – we really don’t know how many unpublished studies have been buried – active drug separates from placebo," Dr. Strober said.
"What this means is that about 60%-65% of people randomized to active treatment report a response (defined as a 50% or greater reduction in the frequency of binge eating)," compared with placebo responses of about 35%-40%, he said.
"We get remission rates – which means no bingeing or purging the last 2 weeks of the trial – of about 10% on active drug, maybe 0%-3% on placebo," he said.
However, about 50% of responders "have a recurrence of their symptoms" within 5 months, "so these are not very effective drugs for the majority of patients," Dr. Strober said.
CBT does better: "After 12-16 weeks, we get response rates (defined in the same way) that are roughly 65%-70%. You get about 35%-38% that are fully remitted, and that response tends to be more durable," he said.
Evidence also supports family-based therapy (FBT) for anorexia nervosa.
In a recent study, 121 subjects aged 12-18 years with mild to moderate illness – the trial excluded patients below 75% of their ideal body weight – were randomized to either individual therapy or FBT.
At the end of treatment and at 12 months’ follow-up, body weights were normal in about half of FBT patients but only in about a quarter of individual therapy patients (Arch. Gen. Psychiatry 2010;67:1025-32).
"There’s a signal here, I think – a powerful signal," Dr. Strober said. "This is a meaningful difference."
Family-based therapy "is an important treatment. We don’t really know what the ingredient is; we just know that this has been helpful for a number of families, but you really have to be very skilled in working with these people," he said.
Dr. Strober said he has no disclosures.
LOS ANGELES – There is very little evidence – and in some cases none at all – to support common pharmacologic treatments for anorexia and bulimia nervosa, according to Michael Strober, Ph.D.
Eating disorders "are the black hole of pharmacotherapy in psychiatry. There’s not much at this point in time we have to offer," Dr. Strober, director of the eating disorders program at the UCLA Neuropsychiatric Institute and Hospital, reported at a psychopharmacology update sponsored by the American Academy of Child and Adolescent Psychiatry.
For anorexia nervosa, evidence is stronger for family-based therapy in which families are taught to help a child eat and maintain weight.
Cognitive-behavioral therapy (CBT) is more effective than drugs for bulimia nervosa and remains its treatment of choice, said Dr. Strober, who estimated he’s treated more than 8,000 eating disorder patients during a career dating back to 1975.
Although selective serotonin reuptake inhibitors (SSRIs) are widely used to treat anorexia, "there is absolutely not a speck of evidence that these drugs, in the acutely malnourished state, are effective," or that they help maintain weight gain, said Dr. Strober, who also serves as director of the adolescent mood disorders program at the institute.
There is slight evidence for the atypical antipsychotic, olanzapine (Zyprexa).
In a trial funded by the drug’s maker, Eli Lilly, 16 anorexia patients were randomized to outpatient day treatment plus olanzapine, and 18 to day treatment plus placebo.
The mean body mass index was low-normal in both groups at the end of 13 weeks (19.66 kg/m2 in the placebo group vs. 20.30 in the olanzapine group). However, placebo patients started with a lower mean BMI of 15.93, compared with 16.39 among olanzapine patients.
Also, at week 13, 55.6% of placebo patients but 87.5% of olanzapine patients achieved the target BMI of 18.5 (Am. J. Psychiatry 2008;165:1281-8).
The differences were "not very dramatic," but were statistically significant, Dr. Strober said.
"We have no idea what the mechanism is. We don’t know if it’s mediated by improved psychological state or weight gain associated with olanzapine," he said.
Given the lack of data, Dr. Strober said that he and his colleagues typically refeed anorexia inpatients for a few weeks, and only then add atypical antipsychotics if they aren’t managing well.
"I generally think [they] have more of an effect than the SSRIs, although we have patients receiving SSRIs who report less anxiety and psychological discomfort with weight gain," Dr. Strober said.
In general, however, "I have never seen a robust clinical effect of these agents," he said.
For bulimia, antidepressants have been shown to help.
"Regardless of the antidepressant used, in the majority of published studies – we really don’t know how many unpublished studies have been buried – active drug separates from placebo," Dr. Strober said.
"What this means is that about 60%-65% of people randomized to active treatment report a response (defined as a 50% or greater reduction in the frequency of binge eating)," compared with placebo responses of about 35%-40%, he said.
"We get remission rates – which means no bingeing or purging the last 2 weeks of the trial – of about 10% on active drug, maybe 0%-3% on placebo," he said.
However, about 50% of responders "have a recurrence of their symptoms" within 5 months, "so these are not very effective drugs for the majority of patients," Dr. Strober said.
CBT does better: "After 12-16 weeks, we get response rates (defined in the same way) that are roughly 65%-70%. You get about 35%-38% that are fully remitted, and that response tends to be more durable," he said.
Evidence also supports family-based therapy (FBT) for anorexia nervosa.
In a recent study, 121 subjects aged 12-18 years with mild to moderate illness – the trial excluded patients below 75% of their ideal body weight – were randomized to either individual therapy or FBT.
At the end of treatment and at 12 months’ follow-up, body weights were normal in about half of FBT patients but only in about a quarter of individual therapy patients (Arch. Gen. Psychiatry 2010;67:1025-32).
"There’s a signal here, I think – a powerful signal," Dr. Strober said. "This is a meaningful difference."
Family-based therapy "is an important treatment. We don’t really know what the ingredient is; we just know that this has been helpful for a number of families, but you really have to be very skilled in working with these people," he said.
Dr. Strober said he has no disclosures.
FROM THE AMERICAN ACADEMY OF CHILD AND ADOLESCENT PSYCHIATRY
Keep Open Mind About Alternative Autism Treatments
LOS ANGELES – When conventional approaches fail to help autistic children, parents who suggest alternative treatments should not be ignored, according to Dr. Robert L. Hendren.
Instead, it’s better to talk to them about their ideas and keep an open mind, said Dr. Hendren, director of child and adolescent psychiatry at the University of California, San Francisco. "I try to weigh the evidence [with families], but if they’re doing something I think is dangerous, or they’re avoiding other kinds of treatments, I tend to tell them," he said.
When there’s no harm to an alternative treatment, after a few months, Dr. Hendren said he will help parents assess whether it is working and ask them to reconsider his treatment ideas.
The reasoned approach means parents feel comfortable telling him the alternatives they’re trying and letting alternative practitioners know that Dr. Hendren is involved in the case, he said. Also, with evidence emerging that mitochondrial dysfunction, chronic inflammation, maternal toxin exposure, oxidative stress, and other problems might play a role in autism, some treatments now considered alternative eventually might prove useful, he said at the update, sponsored by the American Academy of Child and Adolescent Psychiatry.
Dr. Hendren analyzed the evidence – or lack thereof – for many of the currently hot complementary and alternative approaches.
Casein and gluten-free diets are among them. There’s no harm, so long as families work with nutritionists to ensure that children get enough calcium and protein, he said. There’s no harm in trying glutathione, vitamin D, and omega-3 fatty acids, either; Dr. Hendren, in fact, prescribes the latter two for his own patients. Evidence is lacking, however, for amino acids, thyroid supplements, and antifungals. "I don’t think the jury is in on methyl B12 [injections] yet," he said.
Chelation is hot for autism, too, but "I don’t think there’s any reason to try it," he said. "I don’t tell parents that they ought to do it, but I say at least find somebody who knows what they’re doing," he said.
Therapy and Medications
What’s known to help autistic children, among other things, are speech and occupational therapy, cognitive-behavioral treatments, social skills training, and reducing stress by, for instance, removing children from upsetting situations.
Medications can help, too.
For children with comorbid attention-deficit/hyperactivity disorder, stimulants "can make a big difference in their inattention," Dr. Hendren said.
He said he favors immediate-release formulations, titrated up slowly from low doses, and warns parents that stimulants might temporarily unhinge their child.
If that happens, atomoxetine is an option, though stimulants seem to work better for inattention, Dr. Hendren said.
Short-acting tranquilizers like lorazepam help anxiety, especially in tense situations like a visit to the doctor’s office.
As with stimulants, Dr. Hendren said he starts low – 0.5 mg, for example – and slowly titrates up to effect, perhaps going as high as 1 or 2 mg.
"A number of kids do quite well on alpha-adrenergic agonists" as well, he said.
The drugs "seem to help dampen them down, and can be especially useful in some of the younger kids [who] are just very hyperactive and having a lot of difficulty with their impulsivity," he said.
Clonidine is a bit more sedating than guanfacine (Tenex), which can be a benefit.
And some kids do well on Intuniv, the long-acting guanfacine formulation, but "parents don’t like paying that extra price" for the newer medication, Dr. Hendren said.
Topiramate also helps calm anxious children, but Dr. Hendren said he avoids exceeding 75 mg, because the drug can make children squirrelly.
Melatonin helps with sleep problems, "but at times we need to titrate up to as high as 6 or even 8 or 9 mg," he said.
Selective serotonin reuptake inhibitors (SSRIs) might help curb impulsive and compulsive behavior, though a recent study raises doubts about their use in autism (Arch. Gen. Psychiatry 2009;66:583-90). SSRI activation remains a concern, as well.
Among Dr. Hendren’s colleagues, the preference is for escitalopram or sertraline, because these drugs seem less activating. Again, titration is slow from a low dose. He said he prefers "escitalopram because I find I can usually get within range with 20 mg; occasionally I’ll go to 30 mg." Sertraline requires higher dosages. Also, "I like the side effect profile better," he said.
Atypicals and Other Options
Risperidone and aripiprazole, the only drugs approved for autism symptoms, both help irritability, behavior problems, and children who become easily unglued, Dr. Hendren said.
But atypical antipsychotics are associated with significant side effects, including weight gain, sedation, and salivation.
"I’ve had three kids in my practice [who] developed clear symptoms of tardive dyskinesia on risperidone that went away when the medication was taken away," he said. "Some parents are willing to take the risk, but it’s a risk I have them write about."
He’s also had younger girls or boys develop breast buds on risperidone and lactate. In those cases, he usually switches to aripiprazole, though sometimes, children don’t do as well.
Lowering the risperidone dose is another option. "I have some children [whom] I’ve kept just below lactating on risperidone," he said.
When all else fails, there’s some evidence to support propranolol and low-dose naltrexone cream for aggression; divalproex might help affect instability.
Amantadine, d-cycloserine, memantine, cholinesterase inhibitors, and nicotinic agonists all have studies suggesting a small effect size, he said.
Dr. Hendren disclosed that he is an adviser to BioMarin Pharmaceutical Inc., and receives research funding from that company plus Curemark LLC, Forest Laboratories Inc., and Autism Speaks.
LOS ANGELES – When conventional approaches fail to help autistic children, parents who suggest alternative treatments should not be ignored, according to Dr. Robert L. Hendren.
Instead, it’s better to talk to them about their ideas and keep an open mind, said Dr. Hendren, director of child and adolescent psychiatry at the University of California, San Francisco. "I try to weigh the evidence [with families], but if they’re doing something I think is dangerous, or they’re avoiding other kinds of treatments, I tend to tell them," he said.
When there’s no harm to an alternative treatment, after a few months, Dr. Hendren said he will help parents assess whether it is working and ask them to reconsider his treatment ideas.
The reasoned approach means parents feel comfortable telling him the alternatives they’re trying and letting alternative practitioners know that Dr. Hendren is involved in the case, he said. Also, with evidence emerging that mitochondrial dysfunction, chronic inflammation, maternal toxin exposure, oxidative stress, and other problems might play a role in autism, some treatments now considered alternative eventually might prove useful, he said at the update, sponsored by the American Academy of Child and Adolescent Psychiatry.
Dr. Hendren analyzed the evidence – or lack thereof – for many of the currently hot complementary and alternative approaches.
Casein and gluten-free diets are among them. There’s no harm, so long as families work with nutritionists to ensure that children get enough calcium and protein, he said. There’s no harm in trying glutathione, vitamin D, and omega-3 fatty acids, either; Dr. Hendren, in fact, prescribes the latter two for his own patients. Evidence is lacking, however, for amino acids, thyroid supplements, and antifungals. "I don’t think the jury is in on methyl B12 [injections] yet," he said.
Chelation is hot for autism, too, but "I don’t think there’s any reason to try it," he said. "I don’t tell parents that they ought to do it, but I say at least find somebody who knows what they’re doing," he said.
Therapy and Medications
What’s known to help autistic children, among other things, are speech and occupational therapy, cognitive-behavioral treatments, social skills training, and reducing stress by, for instance, removing children from upsetting situations.
Medications can help, too.
For children with comorbid attention-deficit/hyperactivity disorder, stimulants "can make a big difference in their inattention," Dr. Hendren said.
He said he favors immediate-release formulations, titrated up slowly from low doses, and warns parents that stimulants might temporarily unhinge their child.
If that happens, atomoxetine is an option, though stimulants seem to work better for inattention, Dr. Hendren said.
Short-acting tranquilizers like lorazepam help anxiety, especially in tense situations like a visit to the doctor’s office.
As with stimulants, Dr. Hendren said he starts low – 0.5 mg, for example – and slowly titrates up to effect, perhaps going as high as 1 or 2 mg.
"A number of kids do quite well on alpha-adrenergic agonists" as well, he said.
The drugs "seem to help dampen them down, and can be especially useful in some of the younger kids [who] are just very hyperactive and having a lot of difficulty with their impulsivity," he said.
Clonidine is a bit more sedating than guanfacine (Tenex), which can be a benefit.
And some kids do well on Intuniv, the long-acting guanfacine formulation, but "parents don’t like paying that extra price" for the newer medication, Dr. Hendren said.
Topiramate also helps calm anxious children, but Dr. Hendren said he avoids exceeding 75 mg, because the drug can make children squirrelly.
Melatonin helps with sleep problems, "but at times we need to titrate up to as high as 6 or even 8 or 9 mg," he said.
Selective serotonin reuptake inhibitors (SSRIs) might help curb impulsive and compulsive behavior, though a recent study raises doubts about their use in autism (Arch. Gen. Psychiatry 2009;66:583-90). SSRI activation remains a concern, as well.
Among Dr. Hendren’s colleagues, the preference is for escitalopram or sertraline, because these drugs seem less activating. Again, titration is slow from a low dose. He said he prefers "escitalopram because I find I can usually get within range with 20 mg; occasionally I’ll go to 30 mg." Sertraline requires higher dosages. Also, "I like the side effect profile better," he said.
Atypicals and Other Options
Risperidone and aripiprazole, the only drugs approved for autism symptoms, both help irritability, behavior problems, and children who become easily unglued, Dr. Hendren said.
But atypical antipsychotics are associated with significant side effects, including weight gain, sedation, and salivation.
"I’ve had three kids in my practice [who] developed clear symptoms of tardive dyskinesia on risperidone that went away when the medication was taken away," he said. "Some parents are willing to take the risk, but it’s a risk I have them write about."
He’s also had younger girls or boys develop breast buds on risperidone and lactate. In those cases, he usually switches to aripiprazole, though sometimes, children don’t do as well.
Lowering the risperidone dose is another option. "I have some children [whom] I’ve kept just below lactating on risperidone," he said.
When all else fails, there’s some evidence to support propranolol and low-dose naltrexone cream for aggression; divalproex might help affect instability.
Amantadine, d-cycloserine, memantine, cholinesterase inhibitors, and nicotinic agonists all have studies suggesting a small effect size, he said.
Dr. Hendren disclosed that he is an adviser to BioMarin Pharmaceutical Inc., and receives research funding from that company plus Curemark LLC, Forest Laboratories Inc., and Autism Speaks.
LOS ANGELES – When conventional approaches fail to help autistic children, parents who suggest alternative treatments should not be ignored, according to Dr. Robert L. Hendren.
Instead, it’s better to talk to them about their ideas and keep an open mind, said Dr. Hendren, director of child and adolescent psychiatry at the University of California, San Francisco. "I try to weigh the evidence [with families], but if they’re doing something I think is dangerous, or they’re avoiding other kinds of treatments, I tend to tell them," he said.
When there’s no harm to an alternative treatment, after a few months, Dr. Hendren said he will help parents assess whether it is working and ask them to reconsider his treatment ideas.
The reasoned approach means parents feel comfortable telling him the alternatives they’re trying and letting alternative practitioners know that Dr. Hendren is involved in the case, he said. Also, with evidence emerging that mitochondrial dysfunction, chronic inflammation, maternal toxin exposure, oxidative stress, and other problems might play a role in autism, some treatments now considered alternative eventually might prove useful, he said at the update, sponsored by the American Academy of Child and Adolescent Psychiatry.
Dr. Hendren analyzed the evidence – or lack thereof – for many of the currently hot complementary and alternative approaches.
Casein and gluten-free diets are among them. There’s no harm, so long as families work with nutritionists to ensure that children get enough calcium and protein, he said. There’s no harm in trying glutathione, vitamin D, and omega-3 fatty acids, either; Dr. Hendren, in fact, prescribes the latter two for his own patients. Evidence is lacking, however, for amino acids, thyroid supplements, and antifungals. "I don’t think the jury is in on methyl B12 [injections] yet," he said.
Chelation is hot for autism, too, but "I don’t think there’s any reason to try it," he said. "I don’t tell parents that they ought to do it, but I say at least find somebody who knows what they’re doing," he said.
Therapy and Medications
What’s known to help autistic children, among other things, are speech and occupational therapy, cognitive-behavioral treatments, social skills training, and reducing stress by, for instance, removing children from upsetting situations.
Medications can help, too.
For children with comorbid attention-deficit/hyperactivity disorder, stimulants "can make a big difference in their inattention," Dr. Hendren said.
He said he favors immediate-release formulations, titrated up slowly from low doses, and warns parents that stimulants might temporarily unhinge their child.
If that happens, atomoxetine is an option, though stimulants seem to work better for inattention, Dr. Hendren said.
Short-acting tranquilizers like lorazepam help anxiety, especially in tense situations like a visit to the doctor’s office.
As with stimulants, Dr. Hendren said he starts low – 0.5 mg, for example – and slowly titrates up to effect, perhaps going as high as 1 or 2 mg.
"A number of kids do quite well on alpha-adrenergic agonists" as well, he said.
The drugs "seem to help dampen them down, and can be especially useful in some of the younger kids [who] are just very hyperactive and having a lot of difficulty with their impulsivity," he said.
Clonidine is a bit more sedating than guanfacine (Tenex), which can be a benefit.
And some kids do well on Intuniv, the long-acting guanfacine formulation, but "parents don’t like paying that extra price" for the newer medication, Dr. Hendren said.
Topiramate also helps calm anxious children, but Dr. Hendren said he avoids exceeding 75 mg, because the drug can make children squirrelly.
Melatonin helps with sleep problems, "but at times we need to titrate up to as high as 6 or even 8 or 9 mg," he said.
Selective serotonin reuptake inhibitors (SSRIs) might help curb impulsive and compulsive behavior, though a recent study raises doubts about their use in autism (Arch. Gen. Psychiatry 2009;66:583-90). SSRI activation remains a concern, as well.
Among Dr. Hendren’s colleagues, the preference is for escitalopram or sertraline, because these drugs seem less activating. Again, titration is slow from a low dose. He said he prefers "escitalopram because I find I can usually get within range with 20 mg; occasionally I’ll go to 30 mg." Sertraline requires higher dosages. Also, "I like the side effect profile better," he said.
Atypicals and Other Options
Risperidone and aripiprazole, the only drugs approved for autism symptoms, both help irritability, behavior problems, and children who become easily unglued, Dr. Hendren said.
But atypical antipsychotics are associated with significant side effects, including weight gain, sedation, and salivation.
"I’ve had three kids in my practice [who] developed clear symptoms of tardive dyskinesia on risperidone that went away when the medication was taken away," he said. "Some parents are willing to take the risk, but it’s a risk I have them write about."
He’s also had younger girls or boys develop breast buds on risperidone and lactate. In those cases, he usually switches to aripiprazole, though sometimes, children don’t do as well.
Lowering the risperidone dose is another option. "I have some children [whom] I’ve kept just below lactating on risperidone," he said.
When all else fails, there’s some evidence to support propranolol and low-dose naltrexone cream for aggression; divalproex might help affect instability.
Amantadine, d-cycloserine, memantine, cholinesterase inhibitors, and nicotinic agonists all have studies suggesting a small effect size, he said.
Dr. Hendren disclosed that he is an adviser to BioMarin Pharmaceutical Inc., and receives research funding from that company plus Curemark LLC, Forest Laboratories Inc., and Autism Speaks.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY UPDATE