User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
FDA: REMS no longer necessary for epoetin, darbepoetin
The Food and Drug Administration no longer requires certification of doctors and hospitals to prescribe epoetin alfa (Procrit, Epogen) or darbepoetin alfa (Aranesp) for chemotherapy anemia.
A Risk Evaluation and Mitigation Strategy (REMS) program was put in place in 2011 to make sure that the benefits of erythropoiesis-stimulating agents (ESAs) outweighed the risks when prescribed. Under the program, providers were required to become certified in the ESA REMS and to demonstrate that each patient had received counseling on the benefits and risks of the therapies prior to use.
Amgen’s prescriber surveys demonstrated “acceptable knowledge” of the need to counsel patients about the risks. Utilization data indicated “appropriate prescribing” as an alternative to transfusion.
In addition, in an evaluation of the impact of multiple regulatory actions, the FDA determined that full implementation of the ESA REMS in 2011 had minimal impact on trends in ESA utilization metrics, the FDA wrote.
The FDA concluded that regulatory actions and label changes – and the cut in payments for nonrenal indications from the Center for Medicare & Medicaid Services – were enough to reduce overuse in chemotherapy.
However, while the REMS is no longer necessary, the FDA says serious risks of shortened overall survival and/or increased risk of tumor progression or recurrence associated with these drugs remain and health care providers should continue to discuss the risks and benefits of using ESAs with each patient before initiating use.
The Food and Drug Administration no longer requires certification of doctors and hospitals to prescribe epoetin alfa (Procrit, Epogen) or darbepoetin alfa (Aranesp) for chemotherapy anemia.
A Risk Evaluation and Mitigation Strategy (REMS) program was put in place in 2011 to make sure that the benefits of erythropoiesis-stimulating agents (ESAs) outweighed the risks when prescribed. Under the program, providers were required to become certified in the ESA REMS and to demonstrate that each patient had received counseling on the benefits and risks of the therapies prior to use.
Amgen’s prescriber surveys demonstrated “acceptable knowledge” of the need to counsel patients about the risks. Utilization data indicated “appropriate prescribing” as an alternative to transfusion.
In addition, in an evaluation of the impact of multiple regulatory actions, the FDA determined that full implementation of the ESA REMS in 2011 had minimal impact on trends in ESA utilization metrics, the FDA wrote.
The FDA concluded that regulatory actions and label changes – and the cut in payments for nonrenal indications from the Center for Medicare & Medicaid Services – were enough to reduce overuse in chemotherapy.
However, while the REMS is no longer necessary, the FDA says serious risks of shortened overall survival and/or increased risk of tumor progression or recurrence associated with these drugs remain and health care providers should continue to discuss the risks and benefits of using ESAs with each patient before initiating use.
The Food and Drug Administration no longer requires certification of doctors and hospitals to prescribe epoetin alfa (Procrit, Epogen) or darbepoetin alfa (Aranesp) for chemotherapy anemia.
A Risk Evaluation and Mitigation Strategy (REMS) program was put in place in 2011 to make sure that the benefits of erythropoiesis-stimulating agents (ESAs) outweighed the risks when prescribed. Under the program, providers were required to become certified in the ESA REMS and to demonstrate that each patient had received counseling on the benefits and risks of the therapies prior to use.
Amgen’s prescriber surveys demonstrated “acceptable knowledge” of the need to counsel patients about the risks. Utilization data indicated “appropriate prescribing” as an alternative to transfusion.
In addition, in an evaluation of the impact of multiple regulatory actions, the FDA determined that full implementation of the ESA REMS in 2011 had minimal impact on trends in ESA utilization metrics, the FDA wrote.
The FDA concluded that regulatory actions and label changes – and the cut in payments for nonrenal indications from the Center for Medicare & Medicaid Services – were enough to reduce overuse in chemotherapy.
However, while the REMS is no longer necessary, the FDA says serious risks of shortened overall survival and/or increased risk of tumor progression or recurrence associated with these drugs remain and health care providers should continue to discuss the risks and benefits of using ESAs with each patient before initiating use.
Avoid hysterectomy in POP repairs
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
Bundled maternal HIV, well-baby visits boost ART adherence
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
AT CROI
Key clinical point:
Major finding: At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the control arm. Women in the integrated group breastfed for about 9 months, versus 3 months in the split-care group.
Data source: A randomized trial of 472 new moms with HIV and their babies in Cape Town, South Africa.
Disclosures: Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
Lightweight mesh reduces erosion risk after sacrocolpopexy
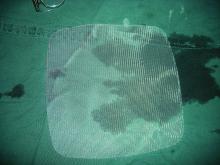
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The odds ratio for ultralightweight polypropylene (Restorelle Y) exposure, versus heavier polypropylene mesh, was not statistically significant (OR, 2.18; 95% CI, 0.33-14.57).
Data source: A single-center study matching 133 erosion cases to 261 controls.
Disclosures: There was no industry funding of the study, and the investigators reported no financial disclosures.
Predicting extraction of an intact uterus in robotic-assisted laparoscopic hysterectomy
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The sensitivity of the scoring system was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Data source: Single-center review of 367 robotic total laparoscopic hysterectomies during 2012-2015.
Disclosures: There was no external funding for the work, and the investigators reported having no relevant financial disclosures.
Confirmatory blood typing unnecessary for closed prolapse repairs
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: Given the 0.4% risk of transfusion reactions in unscreened women, the risk of serious transfusion reactions was 1 in 50,000 women with closed apical prolapse repairs.
Data source: A review of more than 600 cases of apical prolapse surgery at a single center.
Disclosures: There was no industry funding, and the investigators reported having no relevant financial disclosures.
Birth defects found in 10% of confirmed U.S. Zika pregnancies
FROM MMWR
About 1 in 10 pregnant women with confirmed Zika infection in the United States had a fetus or baby with Zika-related birth defects in 2016, officials at the Centers for Disease Control and Prevention reported.
Among 972 completed pregnancies with laboratory evidence of possible recent Zika virus infection – 895 liveborn infants and 77 pregnancy losses – there were 51 fetuses/infants with Zika-related birth defects (5%). Among 250 pregnancies with laboratory-confirmed Zika infection, there were 24 cases of birth defects (10%). Among the 60 pregnancies in which Zika infection was confirmed and onset occurred during the first trimester, there were nine cases of birth defects (15%).
“We are seeing about 30-40 new Zika cases in pregnant women each week in the United States. With the current tally of more than 1,600 pregnant women with evidence of Zika” reported in at least 44 states, mostly from travel to endemic areas, “this devastating outbreak is far from over,” CDC Acting Director Anne Schuchat, MD, said during an April 4 press conference.
But current birth defect estimates may not reflect the full impact of Zika virus in pregnancy, since some Zika-related developmental problems may not become apparent until months after birth. “We recommend babies receive close developmental monitoring and follow-up,” she said.
Despite CDC recommendations, one in three infants with possible congenital Zika infection had no report of Zika testing at birth, and only 1 in 4 had brain imaging (Morb Mortal Wkly Rep. 2017 Apr 4. doi: 10.15585/mmwr.mm6613e1).
“Because the full clinical spectrum of congenital Zika virus infection is not yet known, all infants born to women with laboratory evidence of possible recent Zika virus infection during pregnancy should receive postnatal neuroimaging and Zika virus testing in addition to a comprehensive newborn physical exam and hearing screen,” the CDC officials wrote.
Birth defects – most commonly microcephaly or brain abnormalities – were reported in similar proportions of fetuses/infants whose mothers did and did not report Zika symptoms.
Dr. Schuchat noted that Zika virus can cause vision problems, hearing problems, and seizures. Some infants have little or no control over their arms or legs, and cannot reach out to touch things because of their constricted joints. There can be problems reaching developmental milestones, such as sitting up, as well as problems with feeding, swallowing, and breathing. Some babies cry inconsolably. Others may be born with a normal head size but experience slow head growth later on and develop microcephaly.
The study confirms the need for pregnant women to continue taking steps to prevent Zika virus exposure through mosquito bites and sexual transmission.
“We encourage [health care providers] to ask about possible Zika exposure when caring for both pregnant women and their babies, and to follow CDC guidance for evaluation and care of infants with possible Zika infection,” said Peggy Honein, PhD, senior investigator on the review, in a statement.
The mothers of the 51 fetuses or infants with birth defects were exposed to Zika during trips to 16 countries, including Barbados, Belize, Brazil, Cape Verde, Colombia, Dominican Republic, El Salvador, Guatemala, Guyana, Haiti, Honduras, Jamaica, Mexico, Puerto Rico, Republic of Marshall Islands, and Venezuela.
FROM MMWR
About 1 in 10 pregnant women with confirmed Zika infection in the United States had a fetus or baby with Zika-related birth defects in 2016, officials at the Centers for Disease Control and Prevention reported.
Among 972 completed pregnancies with laboratory evidence of possible recent Zika virus infection – 895 liveborn infants and 77 pregnancy losses – there were 51 fetuses/infants with Zika-related birth defects (5%). Among 250 pregnancies with laboratory-confirmed Zika infection, there were 24 cases of birth defects (10%). Among the 60 pregnancies in which Zika infection was confirmed and onset occurred during the first trimester, there were nine cases of birth defects (15%).
“We are seeing about 30-40 new Zika cases in pregnant women each week in the United States. With the current tally of more than 1,600 pregnant women with evidence of Zika” reported in at least 44 states, mostly from travel to endemic areas, “this devastating outbreak is far from over,” CDC Acting Director Anne Schuchat, MD, said during an April 4 press conference.
But current birth defect estimates may not reflect the full impact of Zika virus in pregnancy, since some Zika-related developmental problems may not become apparent until months after birth. “We recommend babies receive close developmental monitoring and follow-up,” she said.
Despite CDC recommendations, one in three infants with possible congenital Zika infection had no report of Zika testing at birth, and only 1 in 4 had brain imaging (Morb Mortal Wkly Rep. 2017 Apr 4. doi: 10.15585/mmwr.mm6613e1).
“Because the full clinical spectrum of congenital Zika virus infection is not yet known, all infants born to women with laboratory evidence of possible recent Zika virus infection during pregnancy should receive postnatal neuroimaging and Zika virus testing in addition to a comprehensive newborn physical exam and hearing screen,” the CDC officials wrote.
Birth defects – most commonly microcephaly or brain abnormalities – were reported in similar proportions of fetuses/infants whose mothers did and did not report Zika symptoms.
Dr. Schuchat noted that Zika virus can cause vision problems, hearing problems, and seizures. Some infants have little or no control over their arms or legs, and cannot reach out to touch things because of their constricted joints. There can be problems reaching developmental milestones, such as sitting up, as well as problems with feeding, swallowing, and breathing. Some babies cry inconsolably. Others may be born with a normal head size but experience slow head growth later on and develop microcephaly.
The study confirms the need for pregnant women to continue taking steps to prevent Zika virus exposure through mosquito bites and sexual transmission.
“We encourage [health care providers] to ask about possible Zika exposure when caring for both pregnant women and their babies, and to follow CDC guidance for evaluation and care of infants with possible Zika infection,” said Peggy Honein, PhD, senior investigator on the review, in a statement.
The mothers of the 51 fetuses or infants with birth defects were exposed to Zika during trips to 16 countries, including Barbados, Belize, Brazil, Cape Verde, Colombia, Dominican Republic, El Salvador, Guatemala, Guyana, Haiti, Honduras, Jamaica, Mexico, Puerto Rico, Republic of Marshall Islands, and Venezuela.
FROM MMWR
About 1 in 10 pregnant women with confirmed Zika infection in the United States had a fetus or baby with Zika-related birth defects in 2016, officials at the Centers for Disease Control and Prevention reported.
Among 972 completed pregnancies with laboratory evidence of possible recent Zika virus infection – 895 liveborn infants and 77 pregnancy losses – there were 51 fetuses/infants with Zika-related birth defects (5%). Among 250 pregnancies with laboratory-confirmed Zika infection, there were 24 cases of birth defects (10%). Among the 60 pregnancies in which Zika infection was confirmed and onset occurred during the first trimester, there were nine cases of birth defects (15%).
“We are seeing about 30-40 new Zika cases in pregnant women each week in the United States. With the current tally of more than 1,600 pregnant women with evidence of Zika” reported in at least 44 states, mostly from travel to endemic areas, “this devastating outbreak is far from over,” CDC Acting Director Anne Schuchat, MD, said during an April 4 press conference.
But current birth defect estimates may not reflect the full impact of Zika virus in pregnancy, since some Zika-related developmental problems may not become apparent until months after birth. “We recommend babies receive close developmental monitoring and follow-up,” she said.
Despite CDC recommendations, one in three infants with possible congenital Zika infection had no report of Zika testing at birth, and only 1 in 4 had brain imaging (Morb Mortal Wkly Rep. 2017 Apr 4. doi: 10.15585/mmwr.mm6613e1).
“Because the full clinical spectrum of congenital Zika virus infection is not yet known, all infants born to women with laboratory evidence of possible recent Zika virus infection during pregnancy should receive postnatal neuroimaging and Zika virus testing in addition to a comprehensive newborn physical exam and hearing screen,” the CDC officials wrote.
Birth defects – most commonly microcephaly or brain abnormalities – were reported in similar proportions of fetuses/infants whose mothers did and did not report Zika symptoms.
Dr. Schuchat noted that Zika virus can cause vision problems, hearing problems, and seizures. Some infants have little or no control over their arms or legs, and cannot reach out to touch things because of their constricted joints. There can be problems reaching developmental milestones, such as sitting up, as well as problems with feeding, swallowing, and breathing. Some babies cry inconsolably. Others may be born with a normal head size but experience slow head growth later on and develop microcephaly.
The study confirms the need for pregnant women to continue taking steps to prevent Zika virus exposure through mosquito bites and sexual transmission.
“We encourage [health care providers] to ask about possible Zika exposure when caring for both pregnant women and their babies, and to follow CDC guidance for evaluation and care of infants with possible Zika infection,” said Peggy Honein, PhD, senior investigator on the review, in a statement.
The mothers of the 51 fetuses or infants with birth defects were exposed to Zika during trips to 16 countries, including Barbados, Belize, Brazil, Cape Verde, Colombia, Dominican Republic, El Salvador, Guatemala, Guyana, Haiti, Honduras, Jamaica, Mexico, Puerto Rico, Republic of Marshall Islands, and Venezuela.
Long-term durability low for nonmesh vaginal prolapse repair
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: The overall 5-year success rate was 39% in women randomized to bilateral uterosacral ligament suspension and 30% in women randomized to unilateral sacrospinous ligament fixation.
Data source: The first randomized trial to compare the two commonly used techniques was conducted among 218 women at nine U.S. centers in the Pelvic Floor Disorders Network.
Disclosures: The Pelvic Floor Disorders Network is funded by the National Institutes of Health. The lead investigator reported having no relevant financial disclosures.
Statins may protect against HIV rebound
SEATTLE – Statins appeared to reduce the risk of viral rebound in HIV patients on antiretroviral therapy, suggesting modest antiviral activity, according to a review of 19,324 HIV-positive veterans who started combination ART from 1995-2011.
It’s been shown before that statins are active against HIV in vitro; the new study is likely the first to show an effect in actual patients, and it was only found in those who used statins consistently, perhaps because of the drugs’ short half-life. “In addition to their cardiovascular benefits, statins could increase the durability of successful antiretroviral therapy. Whether this effect is direct or mediated by [statins’] anti-inflammatory properties merits further evaluation,” concluded investigators led by Henning Drechsler, MD, an infectious disease specialist at the Dallas Veterans Affairs Medical Center.
After adjusting for a range of confounders, including demographics, substance use, and ART adherence assessed by pharmacy fill records, the team found that statins use within 7 days of testing was associated with almost a 20% drop in the risk of decreased risk of VF (adjusted HR 0.81, 95% 0.75-0.88), with a similar benefit for use within 3 months. There was no protective effect for blood pressure drugs, and a slight increase for patients on cardioprotective aspirin.
About a third of the patients – almost all men, around 48 years old – had at least tried statins, generally after their viral loads were suppressed and most often pravastatin or simvastatin. Statins’ protection against VF was present over the whole study period and among all types of ART and levels, but became less pronounced after 2005 in patients with optimal ART adherence, and in those taking newer options. The median observation time was 5.9 years.
“I am very confident that this is not a data fluke,” Dr. Drechsler said at the 2017 Conference on Retroviruses and Opportunistic Infections. He noted that there may even be role for statin use in HIV patients without dyslipidemia, but with the current study, “it’s hard to say. You really do need a prospect study.”
He plans to keep looking into the issue. Meanwhile, a large trial of statin use in HIV is underway.
Dr. Drechsler said he had no disclosures.
SEATTLE – Statins appeared to reduce the risk of viral rebound in HIV patients on antiretroviral therapy, suggesting modest antiviral activity, according to a review of 19,324 HIV-positive veterans who started combination ART from 1995-2011.
It’s been shown before that statins are active against HIV in vitro; the new study is likely the first to show an effect in actual patients, and it was only found in those who used statins consistently, perhaps because of the drugs’ short half-life. “In addition to their cardiovascular benefits, statins could increase the durability of successful antiretroviral therapy. Whether this effect is direct or mediated by [statins’] anti-inflammatory properties merits further evaluation,” concluded investigators led by Henning Drechsler, MD, an infectious disease specialist at the Dallas Veterans Affairs Medical Center.
After adjusting for a range of confounders, including demographics, substance use, and ART adherence assessed by pharmacy fill records, the team found that statins use within 7 days of testing was associated with almost a 20% drop in the risk of decreased risk of VF (adjusted HR 0.81, 95% 0.75-0.88), with a similar benefit for use within 3 months. There was no protective effect for blood pressure drugs, and a slight increase for patients on cardioprotective aspirin.
About a third of the patients – almost all men, around 48 years old – had at least tried statins, generally after their viral loads were suppressed and most often pravastatin or simvastatin. Statins’ protection against VF was present over the whole study period and among all types of ART and levels, but became less pronounced after 2005 in patients with optimal ART adherence, and in those taking newer options. The median observation time was 5.9 years.
“I am very confident that this is not a data fluke,” Dr. Drechsler said at the 2017 Conference on Retroviruses and Opportunistic Infections. He noted that there may even be role for statin use in HIV patients without dyslipidemia, but with the current study, “it’s hard to say. You really do need a prospect study.”
He plans to keep looking into the issue. Meanwhile, a large trial of statin use in HIV is underway.
Dr. Drechsler said he had no disclosures.
SEATTLE – Statins appeared to reduce the risk of viral rebound in HIV patients on antiretroviral therapy, suggesting modest antiviral activity, according to a review of 19,324 HIV-positive veterans who started combination ART from 1995-2011.
It’s been shown before that statins are active against HIV in vitro; the new study is likely the first to show an effect in actual patients, and it was only found in those who used statins consistently, perhaps because of the drugs’ short half-life. “In addition to their cardiovascular benefits, statins could increase the durability of successful antiretroviral therapy. Whether this effect is direct or mediated by [statins’] anti-inflammatory properties merits further evaluation,” concluded investigators led by Henning Drechsler, MD, an infectious disease specialist at the Dallas Veterans Affairs Medical Center.
After adjusting for a range of confounders, including demographics, substance use, and ART adherence assessed by pharmacy fill records, the team found that statins use within 7 days of testing was associated with almost a 20% drop in the risk of decreased risk of VF (adjusted HR 0.81, 95% 0.75-0.88), with a similar benefit for use within 3 months. There was no protective effect for blood pressure drugs, and a slight increase for patients on cardioprotective aspirin.
About a third of the patients – almost all men, around 48 years old – had at least tried statins, generally after their viral loads were suppressed and most often pravastatin or simvastatin. Statins’ protection against VF was present over the whole study period and among all types of ART and levels, but became less pronounced after 2005 in patients with optimal ART adherence, and in those taking newer options. The median observation time was 5.9 years.
“I am very confident that this is not a data fluke,” Dr. Drechsler said at the 2017 Conference on Retroviruses and Opportunistic Infections. He noted that there may even be role for statin use in HIV patients without dyslipidemia, but with the current study, “it’s hard to say. You really do need a prospect study.”
He plans to keep looking into the issue. Meanwhile, a large trial of statin use in HIV is underway.
Dr. Drechsler said he had no disclosures.
AT CROI 2017
Don’t shy away from vaginal salpingectomy
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Three-quarters of women undergoing vaginal hysterectomy for benign reasons had successful concomitant bilateral vaginal salpingectomy.
Data source: A single-center, observational study among 70 women undergoing vaginal hysterectomy for benign reasons.
Disclosures: There was no external funding and the investigators reported no relevant financial disclosures.