User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Androgen receptor screening not ready for triple-negative breast cancer
LAS VEGAS – Despite the early promise of antiandrogen therapy, it’s not time yet to routinely screen women with triple-negative breast cancer for androgen receptors, according to Tiffany A. Traina, MD, the head of research into the disease at Memorial Sloan Kettering Cancer Center, New York.
There’s no standardized test for androgen receptors in breast cancer, so people “are doing different kinds of testing.” In the literature, “the range of AR positivity is anywhere from 12% to 79%, which reflects how we are all over the map in methodology; you might just as well throw a dart at the board. I would encourage screening in the context of the ongoing trials,” Dr. Traina said.
More than a decade ago, Memorial Sloan Kettering found a subset of TNBC that had ARs, which was peculiar because the tumors weren’t otherwise responsive to hormones. Androgen exposure increased growth, but the AR antagonist flutamide (Eulexin)blocked it. “It was thought provoking. There are a lot of drugs in the prostate cancer world” such as flutamide that shut down androgens, she said (Oncogene. 2006 Jun 29;25[28]:3994-4008).
Several have been tried, and investigations are ongoing. The work matters because TNBC is a particularly bad diagnosis. Blocking androgens seems to give some women a few more months of life.
Dr. Traina was the senior author in an early proof-of-concept study for AR blockade that involved 26 women with metastatic TNBC who had been through up to eight prior chemotherapy regimens. The women received 150 mg daily of the prostate cancer AR antagonist bicalutamide (Casodex). Disease remained stable in five (19%) for more than 6 months. Median progression-free survival was 12 weeks, which was “not that far off from what you get with [standard] chemotherapies. This was encouraging, and it led to multiple other trials looking at targeted therapies,” she said (Clin Cancer Res. 2013 Oct 1; 19[19]: 5505-12).
Dr. Traina led a phase II investigation of the prostate cancer AR antagonist enzalutamide (Xtandi) in 118 women with advanced AR-positive TNBC. Her team created an androgen-driven gene signature as a potential biomarker of response. Median progression-free survival was 32 weeks in the 56 women (47%) who were positive for the gene signature, but 9 weeks in those who were not. There were two complete responses and five partial responses with enzalutamide. Currently, “we are looking at using enzalutamide for patients with AR-positive TNBC in the early stage after failure of standard therapies,” she said.
French investigators recently reported a 6-month clinical benefit – including one complete response – in 7 (21%) of 34 women with locally advanced or metastatic TNBC who were treated with 1,000 mg daily of abiraterone acetate (Zytiga), an androgen biosynthesis inhibitor approved for prostate cancer (Ann Oncol. 2016 May;27[5]:812-8).
“We still have a ways to go” before AR treatment reaches the clinic for routine breast cancer treatment, “but there’s reason for hope,” Dr. Traina said.
Dr. Traina reported funding, honoraria, and steering committing payments from a number of companies working on or marketing TNBC AR drugs, including Pfizer, Astellas, Innocrin, AstraZeneca, Eisai, and Merck.
LAS VEGAS – Despite the early promise of antiandrogen therapy, it’s not time yet to routinely screen women with triple-negative breast cancer for androgen receptors, according to Tiffany A. Traina, MD, the head of research into the disease at Memorial Sloan Kettering Cancer Center, New York.
There’s no standardized test for androgen receptors in breast cancer, so people “are doing different kinds of testing.” In the literature, “the range of AR positivity is anywhere from 12% to 79%, which reflects how we are all over the map in methodology; you might just as well throw a dart at the board. I would encourage screening in the context of the ongoing trials,” Dr. Traina said.
More than a decade ago, Memorial Sloan Kettering found a subset of TNBC that had ARs, which was peculiar because the tumors weren’t otherwise responsive to hormones. Androgen exposure increased growth, but the AR antagonist flutamide (Eulexin)blocked it. “It was thought provoking. There are a lot of drugs in the prostate cancer world” such as flutamide that shut down androgens, she said (Oncogene. 2006 Jun 29;25[28]:3994-4008).
Several have been tried, and investigations are ongoing. The work matters because TNBC is a particularly bad diagnosis. Blocking androgens seems to give some women a few more months of life.
Dr. Traina was the senior author in an early proof-of-concept study for AR blockade that involved 26 women with metastatic TNBC who had been through up to eight prior chemotherapy regimens. The women received 150 mg daily of the prostate cancer AR antagonist bicalutamide (Casodex). Disease remained stable in five (19%) for more than 6 months. Median progression-free survival was 12 weeks, which was “not that far off from what you get with [standard] chemotherapies. This was encouraging, and it led to multiple other trials looking at targeted therapies,” she said (Clin Cancer Res. 2013 Oct 1; 19[19]: 5505-12).
Dr. Traina led a phase II investigation of the prostate cancer AR antagonist enzalutamide (Xtandi) in 118 women with advanced AR-positive TNBC. Her team created an androgen-driven gene signature as a potential biomarker of response. Median progression-free survival was 32 weeks in the 56 women (47%) who were positive for the gene signature, but 9 weeks in those who were not. There were two complete responses and five partial responses with enzalutamide. Currently, “we are looking at using enzalutamide for patients with AR-positive TNBC in the early stage after failure of standard therapies,” she said.
French investigators recently reported a 6-month clinical benefit – including one complete response – in 7 (21%) of 34 women with locally advanced or metastatic TNBC who were treated with 1,000 mg daily of abiraterone acetate (Zytiga), an androgen biosynthesis inhibitor approved for prostate cancer (Ann Oncol. 2016 May;27[5]:812-8).
“We still have a ways to go” before AR treatment reaches the clinic for routine breast cancer treatment, “but there’s reason for hope,” Dr. Traina said.
Dr. Traina reported funding, honoraria, and steering committing payments from a number of companies working on or marketing TNBC AR drugs, including Pfizer, Astellas, Innocrin, AstraZeneca, Eisai, and Merck.
LAS VEGAS – Despite the early promise of antiandrogen therapy, it’s not time yet to routinely screen women with triple-negative breast cancer for androgen receptors, according to Tiffany A. Traina, MD, the head of research into the disease at Memorial Sloan Kettering Cancer Center, New York.
There’s no standardized test for androgen receptors in breast cancer, so people “are doing different kinds of testing.” In the literature, “the range of AR positivity is anywhere from 12% to 79%, which reflects how we are all over the map in methodology; you might just as well throw a dart at the board. I would encourage screening in the context of the ongoing trials,” Dr. Traina said.
More than a decade ago, Memorial Sloan Kettering found a subset of TNBC that had ARs, which was peculiar because the tumors weren’t otherwise responsive to hormones. Androgen exposure increased growth, but the AR antagonist flutamide (Eulexin)blocked it. “It was thought provoking. There are a lot of drugs in the prostate cancer world” such as flutamide that shut down androgens, she said (Oncogene. 2006 Jun 29;25[28]:3994-4008).
Several have been tried, and investigations are ongoing. The work matters because TNBC is a particularly bad diagnosis. Blocking androgens seems to give some women a few more months of life.
Dr. Traina was the senior author in an early proof-of-concept study for AR blockade that involved 26 women with metastatic TNBC who had been through up to eight prior chemotherapy regimens. The women received 150 mg daily of the prostate cancer AR antagonist bicalutamide (Casodex). Disease remained stable in five (19%) for more than 6 months. Median progression-free survival was 12 weeks, which was “not that far off from what you get with [standard] chemotherapies. This was encouraging, and it led to multiple other trials looking at targeted therapies,” she said (Clin Cancer Res. 2013 Oct 1; 19[19]: 5505-12).
Dr. Traina led a phase II investigation of the prostate cancer AR antagonist enzalutamide (Xtandi) in 118 women with advanced AR-positive TNBC. Her team created an androgen-driven gene signature as a potential biomarker of response. Median progression-free survival was 32 weeks in the 56 women (47%) who were positive for the gene signature, but 9 weeks in those who were not. There were two complete responses and five partial responses with enzalutamide. Currently, “we are looking at using enzalutamide for patients with AR-positive TNBC in the early stage after failure of standard therapies,” she said.
French investigators recently reported a 6-month clinical benefit – including one complete response – in 7 (21%) of 34 women with locally advanced or metastatic TNBC who were treated with 1,000 mg daily of abiraterone acetate (Zytiga), an androgen biosynthesis inhibitor approved for prostate cancer (Ann Oncol. 2016 May;27[5]:812-8).
“We still have a ways to go” before AR treatment reaches the clinic for routine breast cancer treatment, “but there’s reason for hope,” Dr. Traina said.
Dr. Traina reported funding, honoraria, and steering committing payments from a number of companies working on or marketing TNBC AR drugs, including Pfizer, Astellas, Innocrin, AstraZeneca, Eisai, and Merck.
EXPERT ANALYSIS FROM ASBS 2017
Radiation bests mastectomy for occult breast cancer
LAS VEGAS – Overall survival was better when women with occult breast cancer had axillary lymph node dissection and radiation, instead of mastectomy, in a database review of 934 cases by the University of Maryland Medical Center, Baltimore, the largest review to date of how best to handle the problem.
Five- and 10-year overall survival was 90.8% and 84.8%, respectively, among the 342 women treated with axillary lymph node dissection (ALND) plus adjuvant radiation, versus 80.0% and 69.8% among the 592 who had ALND and mastectomies, plus or minus radiation, according to an analysis of the National Cancer Database from 2004-2013. The results were presented at the annual meeting of the American Society of Breast Surgeons.
ALND plus radiation was independently associated with overall survival on multivariate analysis (HR 0.51, 95% CI 0.32-0.81, P = .004), and was associated with fewer comorbidities, use of chemotherapy, number of positive nodes, and number of nodes examined, compared with mastectomy.
Women treated with ALND plus radiation “had significantly better overall survival than those treated with mastectomy, even after adjusting for other covariates. We believe the study supports overall use of this treatment approach in patients with occult breast cancer,” said lead investigator, Lindsay Hessler, MD, of University of Maryland, Baltimore.
Occult breast cancer – axillary lymph node metastases without clinical or radiologic evidence of a primary breast tumor – is rare and accounted for less than 0.1% of the 2.03 million breast cancer cases in the database. It’s been unclear how best to treat it; most of the previous investigations were small single-center series and case reports.
The only other significant review was smaller, with 750 women in the Surveillance, Epidemiology, and End Results database treated from 1983 to 2006, the “vast majority” before routine use of breast MRI. It showed that “definitive locoregional treatment with either mastectomy or [radiation therapy] improves [overall survival] in patients with occult breast cancer and axillary metastasis who undergo ALND,” but it didn’t suggest which option is best. The National Comprehensive Cancer Network recommends either approach (Cancer. 2010 Sep 1;116[17]:4000-6).
The new University of Maryland findings “confirm that women do not need to have a mastectomy if you can’t find the cancer in their breast. Women do better if you radiate the breast instead of removing it. A lot of academic centers are doing this now, but some people don’t know about it. This needs to be implemented in a more widespread fashion,” said Shelley Hwang, MD, a surgical oncologist at Duke University, Durham, N.C., who moderated Dr. Hessler’s presentation.
Indeed, patients were most likely to be treated with radiation and ALND at an academic center (OR 2.03, 95% CI 1.5-2.74, P less than .001), the only factor on multivariate analysis related to treatment choice.
The review excluded women with only internal mammary lymph node involvement, those with lumpectomies, and women who had less than four nodes recovered on ALND. Mastectomy and radiation patients were similar in nodal stage, race, income, insurance, estrogen receptor status, comorbidities, and year of diagnosis. On pathology, a tumor was found in about a third of the patients who had mastectomies. MRI use and recurrence rates were unavailable in the National Cancer Database.
The findings are subject to all the limits of database reviews, including the possible confounder that women treated at university hospitals might also have had more optimal systemic therapy, as an audience member noted.
The investigators said they had no financial disclosures.
LAS VEGAS – Overall survival was better when women with occult breast cancer had axillary lymph node dissection and radiation, instead of mastectomy, in a database review of 934 cases by the University of Maryland Medical Center, Baltimore, the largest review to date of how best to handle the problem.
Five- and 10-year overall survival was 90.8% and 84.8%, respectively, among the 342 women treated with axillary lymph node dissection (ALND) plus adjuvant radiation, versus 80.0% and 69.8% among the 592 who had ALND and mastectomies, plus or minus radiation, according to an analysis of the National Cancer Database from 2004-2013. The results were presented at the annual meeting of the American Society of Breast Surgeons.
ALND plus radiation was independently associated with overall survival on multivariate analysis (HR 0.51, 95% CI 0.32-0.81, P = .004), and was associated with fewer comorbidities, use of chemotherapy, number of positive nodes, and number of nodes examined, compared with mastectomy.
Women treated with ALND plus radiation “had significantly better overall survival than those treated with mastectomy, even after adjusting for other covariates. We believe the study supports overall use of this treatment approach in patients with occult breast cancer,” said lead investigator, Lindsay Hessler, MD, of University of Maryland, Baltimore.
Occult breast cancer – axillary lymph node metastases without clinical or radiologic evidence of a primary breast tumor – is rare and accounted for less than 0.1% of the 2.03 million breast cancer cases in the database. It’s been unclear how best to treat it; most of the previous investigations were small single-center series and case reports.
The only other significant review was smaller, with 750 women in the Surveillance, Epidemiology, and End Results database treated from 1983 to 2006, the “vast majority” before routine use of breast MRI. It showed that “definitive locoregional treatment with either mastectomy or [radiation therapy] improves [overall survival] in patients with occult breast cancer and axillary metastasis who undergo ALND,” but it didn’t suggest which option is best. The National Comprehensive Cancer Network recommends either approach (Cancer. 2010 Sep 1;116[17]:4000-6).
The new University of Maryland findings “confirm that women do not need to have a mastectomy if you can’t find the cancer in their breast. Women do better if you radiate the breast instead of removing it. A lot of academic centers are doing this now, but some people don’t know about it. This needs to be implemented in a more widespread fashion,” said Shelley Hwang, MD, a surgical oncologist at Duke University, Durham, N.C., who moderated Dr. Hessler’s presentation.
Indeed, patients were most likely to be treated with radiation and ALND at an academic center (OR 2.03, 95% CI 1.5-2.74, P less than .001), the only factor on multivariate analysis related to treatment choice.
The review excluded women with only internal mammary lymph node involvement, those with lumpectomies, and women who had less than four nodes recovered on ALND. Mastectomy and radiation patients were similar in nodal stage, race, income, insurance, estrogen receptor status, comorbidities, and year of diagnosis. On pathology, a tumor was found in about a third of the patients who had mastectomies. MRI use and recurrence rates were unavailable in the National Cancer Database.
The findings are subject to all the limits of database reviews, including the possible confounder that women treated at university hospitals might also have had more optimal systemic therapy, as an audience member noted.
The investigators said they had no financial disclosures.
LAS VEGAS – Overall survival was better when women with occult breast cancer had axillary lymph node dissection and radiation, instead of mastectomy, in a database review of 934 cases by the University of Maryland Medical Center, Baltimore, the largest review to date of how best to handle the problem.
Five- and 10-year overall survival was 90.8% and 84.8%, respectively, among the 342 women treated with axillary lymph node dissection (ALND) plus adjuvant radiation, versus 80.0% and 69.8% among the 592 who had ALND and mastectomies, plus or minus radiation, according to an analysis of the National Cancer Database from 2004-2013. The results were presented at the annual meeting of the American Society of Breast Surgeons.
ALND plus radiation was independently associated with overall survival on multivariate analysis (HR 0.51, 95% CI 0.32-0.81, P = .004), and was associated with fewer comorbidities, use of chemotherapy, number of positive nodes, and number of nodes examined, compared with mastectomy.
Women treated with ALND plus radiation “had significantly better overall survival than those treated with mastectomy, even after adjusting for other covariates. We believe the study supports overall use of this treatment approach in patients with occult breast cancer,” said lead investigator, Lindsay Hessler, MD, of University of Maryland, Baltimore.
Occult breast cancer – axillary lymph node metastases without clinical or radiologic evidence of a primary breast tumor – is rare and accounted for less than 0.1% of the 2.03 million breast cancer cases in the database. It’s been unclear how best to treat it; most of the previous investigations were small single-center series and case reports.
The only other significant review was smaller, with 750 women in the Surveillance, Epidemiology, and End Results database treated from 1983 to 2006, the “vast majority” before routine use of breast MRI. It showed that “definitive locoregional treatment with either mastectomy or [radiation therapy] improves [overall survival] in patients with occult breast cancer and axillary metastasis who undergo ALND,” but it didn’t suggest which option is best. The National Comprehensive Cancer Network recommends either approach (Cancer. 2010 Sep 1;116[17]:4000-6).
The new University of Maryland findings “confirm that women do not need to have a mastectomy if you can’t find the cancer in their breast. Women do better if you radiate the breast instead of removing it. A lot of academic centers are doing this now, but some people don’t know about it. This needs to be implemented in a more widespread fashion,” said Shelley Hwang, MD, a surgical oncologist at Duke University, Durham, N.C., who moderated Dr. Hessler’s presentation.
Indeed, patients were most likely to be treated with radiation and ALND at an academic center (OR 2.03, 95% CI 1.5-2.74, P less than .001), the only factor on multivariate analysis related to treatment choice.
The review excluded women with only internal mammary lymph node involvement, those with lumpectomies, and women who had less than four nodes recovered on ALND. Mastectomy and radiation patients were similar in nodal stage, race, income, insurance, estrogen receptor status, comorbidities, and year of diagnosis. On pathology, a tumor was found in about a third of the patients who had mastectomies. MRI use and recurrence rates were unavailable in the National Cancer Database.
The findings are subject to all the limits of database reviews, including the possible confounder that women treated at university hospitals might also have had more optimal systemic therapy, as an audience member noted.
The investigators said they had no financial disclosures.
AT ASBS 2017
Key clinical point:
Major finding: Five- and 10-year overall survival was 90.8% and 84.8%, respectively, among the 342 women treated with axillary lymph node dissection (ALND) plus adjuvant radiation, versus 80.0% and 69.8% among the 592 who had ALND and mastectomies, plus or minus radiation.
Data source: Review of 934 cases in the National Cancer Database.
Disclosures: The investigators said they had no financial disclosures.
Mastectomy unnecessary for some breast cancer recurrences
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
EXPERT ANALYSIS FROM ASBS 2017
VIDEO: Dr. Lisa Newman on triple negative breast cancer in African American women
LAS VEGAS – The heavy burden of triple negative and other aggressive breast cancers among African American women cannot be simplified to socioeconomic factors alone.
International investigations by Lisa Newman, MD, director of the Breast Oncology Program at the Henry Ford Health System, Detroit, and other researchers are making it clear that genetic factors play a significant role.
She explained the latest findings and what they mean for screening, genetic referral, and treatment in an interview at the American Society of Breast Surgeons annual meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – The heavy burden of triple negative and other aggressive breast cancers among African American women cannot be simplified to socioeconomic factors alone.
International investigations by Lisa Newman, MD, director of the Breast Oncology Program at the Henry Ford Health System, Detroit, and other researchers are making it clear that genetic factors play a significant role.
She explained the latest findings and what they mean for screening, genetic referral, and treatment in an interview at the American Society of Breast Surgeons annual meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – The heavy burden of triple negative and other aggressive breast cancers among African American women cannot be simplified to socioeconomic factors alone.
International investigations by Lisa Newman, MD, director of the Breast Oncology Program at the Henry Ford Health System, Detroit, and other researchers are making it clear that genetic factors play a significant role.
She explained the latest findings and what they mean for screening, genetic referral, and treatment in an interview at the American Society of Breast Surgeons annual meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASBS 2017
VIDEO: How to pick surgical margins with mixed breast lesions
LAS VEGAS – According to recent guidelines, no ink on tumor is the right surgical margin for early stage invasive breast cancer and 2 mm is the right lumpectomy margin for ductal carcinoma in situ (DCIS) treated with whole breast radiation. But, what do you do when invasive carcinoma is associated with DCIS?
It’s a common question for breast surgeons. Monica Morrow, MD, chief of breast surgery at Memorial Sloan-Kettering Cancer Center in New York City, explained how to handle the situation in a video interview at the annual meeting of the American Society of Breast Surgeons.
She was the senior author on the 2014 invasive breast cancer guidelines and the lead author on the 2016 DCIS guidelines, both of which were consensus statements on surgical margins from the Society of Surgical Oncology and other groups (Ann Surg Oncol. 2014 Mar;21[3]:704-16; Ann Surg Oncol. 2016 Nov;23[12]:3801-10).
Dr. Morrow explained the thinking behind the guidelines and how to apply them to mixed lesions and other clinical scenarios, as well as their limitations and what remains to be determined. A key point is that a margin less than 2 mm is not by itself an indication for mastectomy in DCIS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – According to recent guidelines, no ink on tumor is the right surgical margin for early stage invasive breast cancer and 2 mm is the right lumpectomy margin for ductal carcinoma in situ (DCIS) treated with whole breast radiation. But, what do you do when invasive carcinoma is associated with DCIS?
It’s a common question for breast surgeons. Monica Morrow, MD, chief of breast surgery at Memorial Sloan-Kettering Cancer Center in New York City, explained how to handle the situation in a video interview at the annual meeting of the American Society of Breast Surgeons.
She was the senior author on the 2014 invasive breast cancer guidelines and the lead author on the 2016 DCIS guidelines, both of which were consensus statements on surgical margins from the Society of Surgical Oncology and other groups (Ann Surg Oncol. 2014 Mar;21[3]:704-16; Ann Surg Oncol. 2016 Nov;23[12]:3801-10).
Dr. Morrow explained the thinking behind the guidelines and how to apply them to mixed lesions and other clinical scenarios, as well as their limitations and what remains to be determined. A key point is that a margin less than 2 mm is not by itself an indication for mastectomy in DCIS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – According to recent guidelines, no ink on tumor is the right surgical margin for early stage invasive breast cancer and 2 mm is the right lumpectomy margin for ductal carcinoma in situ (DCIS) treated with whole breast radiation. But, what do you do when invasive carcinoma is associated with DCIS?
It’s a common question for breast surgeons. Monica Morrow, MD, chief of breast surgery at Memorial Sloan-Kettering Cancer Center in New York City, explained how to handle the situation in a video interview at the annual meeting of the American Society of Breast Surgeons.
She was the senior author on the 2014 invasive breast cancer guidelines and the lead author on the 2016 DCIS guidelines, both of which were consensus statements on surgical margins from the Society of Surgical Oncology and other groups (Ann Surg Oncol. 2014 Mar;21[3]:704-16; Ann Surg Oncol. 2016 Nov;23[12]:3801-10).
Dr. Morrow explained the thinking behind the guidelines and how to apply them to mixed lesions and other clinical scenarios, as well as their limitations and what remains to be determined. A key point is that a margin less than 2 mm is not by itself an indication for mastectomy in DCIS.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
From ASBS 2017
Don’t rely on MRI findings after DCIS needle biopsy
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
At ASBS 2017
Key clinical point:
Major finding: Of 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology.
Data source: Single-center review of 54 DCIS cases.
Disclosures: There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
How to reduce the open hysterectomy rate
SAN ANTONIO – About a decade ago, the Northern California Permanente Medical Group realized it had a problem: There were too many open hysterectomies being performed.
“We had a large number of low-volume surgeons doing a lot of open hysterectomies,” said Andrew Walter, MD, a gynecologic surgeon at the Permanente Medical Group (TPMG) campus in Roseville, Calif., part of Kaiser Permanente. Across 15 hospitals in the system, “our open rate was 64% in 2007.”
To address the problem, “our leadership basically set targets; we then provided surgical education and training in minimally invasive hysterectomy,” Dr. Walter said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Kaiser Permanente is a capitated system, but even so, its experience in reducing open hysterectomy rates may be useful for other systems dealing with the same problem.
At first, Dr. Walter and his colleagues didn’t know how much of an improvement could be made. “In 2008, we said, ‘Okay, 60% seems doable’” as a minimally invasive target rate, Dr. Walter said. TPMG hit that target, and “the chiefs looked at the numbers and said we can do a little bit better.” With some more effort, the rate of minimally invasive hysterectomies hit 80%, and then 90%, about where it stands today, with a corresponding drop in open rates.
“It will be interesting to see if someone says, ‘Let’s try 95%,’ ” Dr. Walter said.
However, the process hasn’t been easy, and it hasn’t been entirely evidence based, he said. “We are working with hundreds of gynecologists, and very few of them have had advanced training. But ultimately, it worked.”
Surgeons trained with TPMG peers experienced in minimally invasive hysterectomy, and both surgeons were kept on full salary during the learning process. It took about 5-15 cases before learner surgeons were considered proficient. “Funded proctoring is the most important aspect of the program,” he said.
TPMG also reduced the number of physicians doing hysterectomies from 416 to 228 in 2015. “This was the hard part, deciding who is a surgeon and who is not,” Dr. Walter said. “I would like to tell you that these were Kumbaya moments, but there was consternation, and there remains consternation about the process.” A number of ob.gyns. voluntarily gave up their surgical privileges, saying, ‘Thank God I don’t have to operate anymore,’ ” he said.
For low-volume surgeons – those who performed 10 or fewer hysterectomies a year – who wanted stay in the operating room, “we either had to push them into this training or encourage them to give up their surgical practices.” The more than 3,600 hysterectomies performed annually at TPMG facilities are now mostly done by surgeons doing at least 11 of these procedures a year, and often more than 20.
TPMG also paid for training courses at outside institutions, and department chiefs were held accountable for performance.
“Obviously, there are unique processes within Kaiser Permanente that facilitated this, but some of them are not unique. Physician support by enhanced training – that’s something that can be done. The barriers are reimbursement, and deciding who is a surgeon,” he said.
The next target is vaginal hysterectomy. Rates have been stable lately at about 30%, but “we have found that many patients, when reviewed, are vaginal hysterectomy candidates. We’ve set a target of 40%.” The procedure needs to be incentivized, Dr. Walter said, but it’s unclear how to do that at this point.
Dr. Walter reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – About a decade ago, the Northern California Permanente Medical Group realized it had a problem: There were too many open hysterectomies being performed.
“We had a large number of low-volume surgeons doing a lot of open hysterectomies,” said Andrew Walter, MD, a gynecologic surgeon at the Permanente Medical Group (TPMG) campus in Roseville, Calif., part of Kaiser Permanente. Across 15 hospitals in the system, “our open rate was 64% in 2007.”
To address the problem, “our leadership basically set targets; we then provided surgical education and training in minimally invasive hysterectomy,” Dr. Walter said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Kaiser Permanente is a capitated system, but even so, its experience in reducing open hysterectomy rates may be useful for other systems dealing with the same problem.
At first, Dr. Walter and his colleagues didn’t know how much of an improvement could be made. “In 2008, we said, ‘Okay, 60% seems doable’” as a minimally invasive target rate, Dr. Walter said. TPMG hit that target, and “the chiefs looked at the numbers and said we can do a little bit better.” With some more effort, the rate of minimally invasive hysterectomies hit 80%, and then 90%, about where it stands today, with a corresponding drop in open rates.
“It will be interesting to see if someone says, ‘Let’s try 95%,’ ” Dr. Walter said.
However, the process hasn’t been easy, and it hasn’t been entirely evidence based, he said. “We are working with hundreds of gynecologists, and very few of them have had advanced training. But ultimately, it worked.”
Surgeons trained with TPMG peers experienced in minimally invasive hysterectomy, and both surgeons were kept on full salary during the learning process. It took about 5-15 cases before learner surgeons were considered proficient. “Funded proctoring is the most important aspect of the program,” he said.
TPMG also reduced the number of physicians doing hysterectomies from 416 to 228 in 2015. “This was the hard part, deciding who is a surgeon and who is not,” Dr. Walter said. “I would like to tell you that these were Kumbaya moments, but there was consternation, and there remains consternation about the process.” A number of ob.gyns. voluntarily gave up their surgical privileges, saying, ‘Thank God I don’t have to operate anymore,’ ” he said.
For low-volume surgeons – those who performed 10 or fewer hysterectomies a year – who wanted stay in the operating room, “we either had to push them into this training or encourage them to give up their surgical practices.” The more than 3,600 hysterectomies performed annually at TPMG facilities are now mostly done by surgeons doing at least 11 of these procedures a year, and often more than 20.
TPMG also paid for training courses at outside institutions, and department chiefs were held accountable for performance.
“Obviously, there are unique processes within Kaiser Permanente that facilitated this, but some of them are not unique. Physician support by enhanced training – that’s something that can be done. The barriers are reimbursement, and deciding who is a surgeon,” he said.
The next target is vaginal hysterectomy. Rates have been stable lately at about 30%, but “we have found that many patients, when reviewed, are vaginal hysterectomy candidates. We’ve set a target of 40%.” The procedure needs to be incentivized, Dr. Walter said, but it’s unclear how to do that at this point.
Dr. Walter reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – About a decade ago, the Northern California Permanente Medical Group realized it had a problem: There were too many open hysterectomies being performed.
“We had a large number of low-volume surgeons doing a lot of open hysterectomies,” said Andrew Walter, MD, a gynecologic surgeon at the Permanente Medical Group (TPMG) campus in Roseville, Calif., part of Kaiser Permanente. Across 15 hospitals in the system, “our open rate was 64% in 2007.”
To address the problem, “our leadership basically set targets; we then provided surgical education and training in minimally invasive hysterectomy,” Dr. Walter said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Kaiser Permanente is a capitated system, but even so, its experience in reducing open hysterectomy rates may be useful for other systems dealing with the same problem.
At first, Dr. Walter and his colleagues didn’t know how much of an improvement could be made. “In 2008, we said, ‘Okay, 60% seems doable’” as a minimally invasive target rate, Dr. Walter said. TPMG hit that target, and “the chiefs looked at the numbers and said we can do a little bit better.” With some more effort, the rate of minimally invasive hysterectomies hit 80%, and then 90%, about where it stands today, with a corresponding drop in open rates.
“It will be interesting to see if someone says, ‘Let’s try 95%,’ ” Dr. Walter said.
However, the process hasn’t been easy, and it hasn’t been entirely evidence based, he said. “We are working with hundreds of gynecologists, and very few of them have had advanced training. But ultimately, it worked.”
Surgeons trained with TPMG peers experienced in minimally invasive hysterectomy, and both surgeons were kept on full salary during the learning process. It took about 5-15 cases before learner surgeons were considered proficient. “Funded proctoring is the most important aspect of the program,” he said.
TPMG also reduced the number of physicians doing hysterectomies from 416 to 228 in 2015. “This was the hard part, deciding who is a surgeon and who is not,” Dr. Walter said. “I would like to tell you that these were Kumbaya moments, but there was consternation, and there remains consternation about the process.” A number of ob.gyns. voluntarily gave up their surgical privileges, saying, ‘Thank God I don’t have to operate anymore,’ ” he said.
For low-volume surgeons – those who performed 10 or fewer hysterectomies a year – who wanted stay in the operating room, “we either had to push them into this training or encourage them to give up their surgical practices.” The more than 3,600 hysterectomies performed annually at TPMG facilities are now mostly done by surgeons doing at least 11 of these procedures a year, and often more than 20.
TPMG also paid for training courses at outside institutions, and department chiefs were held accountable for performance.
“Obviously, there are unique processes within Kaiser Permanente that facilitated this, but some of them are not unique. Physician support by enhanced training – that’s something that can be done. The barriers are reimbursement, and deciding who is a surgeon,” he said.
The next target is vaginal hysterectomy. Rates have been stable lately at about 30%, but “we have found that many patients, when reviewed, are vaginal hysterectomy candidates. We’ve set a target of 40%.” The procedure needs to be incentivized, Dr. Walter said, but it’s unclear how to do that at this point.
Dr. Walter reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
EXPERT ANALYSIS FROM SGS 2017
EHR price alert doesn’t reduce lab orders
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
Key clinical point:
Major finding: There were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
Data source: Analysis involving 98,529 patients and 142,921 admissions of the effect of Medicare reimbursement information on lab test ordering
Disclosures: This study was funded by the University of Pennsylvania Health System. The senior investigator Mitesh Patel, MD, an assistant professor of medicine at the University of Pennsylvania, Philadelphia, is a principal at Catalyst Health, a technology and behavioral change consulting firm. The authors had no other disclosures.
HIV demographics shifting in U.S.
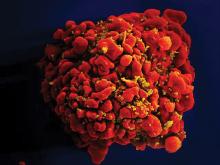
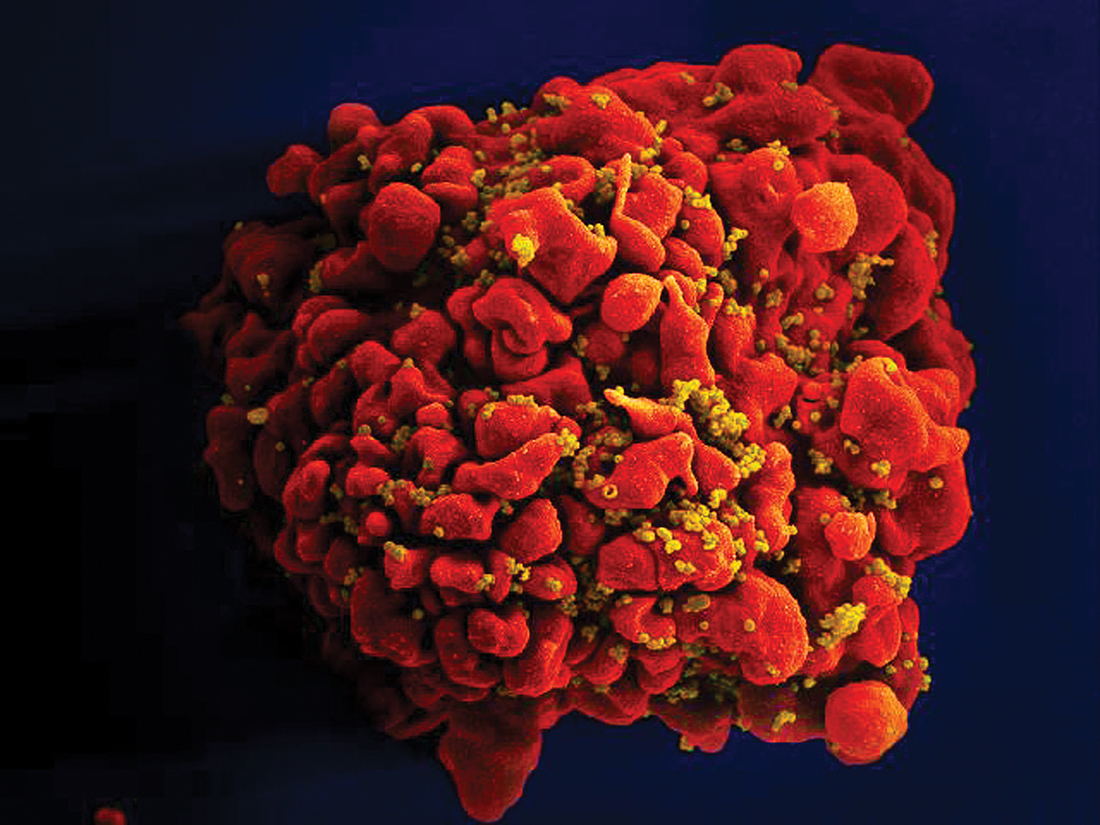
The number of people living with diagnosed HIV in the United States will increase to 1,232,054 by 2045, up from 917,294 in 2013, according to projections based on the National HIV Surveillance System and U.S. census data.
The number of people with HIV over age 55 will more than double from 232,113 to 470,221, though the annual growth rate will slow from 1.8% to 0.8%. By 2025, older people will comprise about 38% of the entire HIV population, said investigators led by epidemiologist Julia Hood, of the University of Washington Department of Epidemiology, Seattle.
The number of Hispanic and black people living with HIV is projected to grow consistently, shifting the demographics of people living with HIV from 32% to 23% white; 42% to 38% black; and 20% to 32% Hispanic by 2045 (AIDS Care. 2017 Apr 10:1-8).
The growing number of black patients “reflects disparities in HIV incidence; while among Hispanics/ Latinos, the growing number … is largely driven by immigration. These results underscore the importance of expanding coverage of HIV care, treatment, and prevention programs to ethnic/racial minorities, ensuring such programs are culturally and linguistically appropriate,” they said.
Overall, “these changing population dynamics should be considered in current decisions about resource allocation, human resource needs, HIV-prevention programs, and design of research studies.” However, “major technological advancements in HIV prevention (e.g., vaccines) and cure could occur in future decades, potentially nullifying the applicability of our projections,” the investigators said.
The authors had no conflicts of interest.
The number of people living with diagnosed HIV in the United States will increase to 1,232,054 by 2045, up from 917,294 in 2013, according to projections based on the National HIV Surveillance System and U.S. census data.
The number of people with HIV over age 55 will more than double from 232,113 to 470,221, though the annual growth rate will slow from 1.8% to 0.8%. By 2025, older people will comprise about 38% of the entire HIV population, said investigators led by epidemiologist Julia Hood, of the University of Washington Department of Epidemiology, Seattle.
The number of Hispanic and black people living with HIV is projected to grow consistently, shifting the demographics of people living with HIV from 32% to 23% white; 42% to 38% black; and 20% to 32% Hispanic by 2045 (AIDS Care. 2017 Apr 10:1-8).
The growing number of black patients “reflects disparities in HIV incidence; while among Hispanics/ Latinos, the growing number … is largely driven by immigration. These results underscore the importance of expanding coverage of HIV care, treatment, and prevention programs to ethnic/racial minorities, ensuring such programs are culturally and linguistically appropriate,” they said.
Overall, “these changing population dynamics should be considered in current decisions about resource allocation, human resource needs, HIV-prevention programs, and design of research studies.” However, “major technological advancements in HIV prevention (e.g., vaccines) and cure could occur in future decades, potentially nullifying the applicability of our projections,” the investigators said.
The authors had no conflicts of interest.
The number of people living with diagnosed HIV in the United States will increase to 1,232,054 by 2045, up from 917,294 in 2013, according to projections based on the National HIV Surveillance System and U.S. census data.
The number of people with HIV over age 55 will more than double from 232,113 to 470,221, though the annual growth rate will slow from 1.8% to 0.8%. By 2025, older people will comprise about 38% of the entire HIV population, said investigators led by epidemiologist Julia Hood, of the University of Washington Department of Epidemiology, Seattle.
The number of Hispanic and black people living with HIV is projected to grow consistently, shifting the demographics of people living with HIV from 32% to 23% white; 42% to 38% black; and 20% to 32% Hispanic by 2045 (AIDS Care. 2017 Apr 10:1-8).
The growing number of black patients “reflects disparities in HIV incidence; while among Hispanics/ Latinos, the growing number … is largely driven by immigration. These results underscore the importance of expanding coverage of HIV care, treatment, and prevention programs to ethnic/racial minorities, ensuring such programs are culturally and linguistically appropriate,” they said.
Overall, “these changing population dynamics should be considered in current decisions about resource allocation, human resource needs, HIV-prevention programs, and design of research studies.” However, “major technological advancements in HIV prevention (e.g., vaccines) and cure could occur in future decades, potentially nullifying the applicability of our projections,” the investigators said.
The authors had no conflicts of interest.
Liposomal bupivacaine cut need for opioids after gyn surgery
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Pain scores, assessed by diary, were lower in the liposomal bupivacaine group 4 hours after discharge on a 100-mm visual analogue scale (3.5 mm versus 13 mm, P = .014).
Data source: Randomized trial with 109 women at Good Samaritan Hospital, Cincinnati.
Disclosures: The investigators reported having no relevant financial disclosures.