User login
Welcome to three new Editorial Advisory Board members!
We are pleased to welcome Dr. Joseph B. Domachowske, Dr. Howard Smart, and Dr. Francis E. Rushton Jr. to the Pediatric News Editorial Advisory Board.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University in Syracuse. He serves on the New York State American Academy of Pediatrics Chapter 1 executive committee, volunteers as his district’s immunization champion, and is an appointed member of the New York State Immunization Advisory Council. He also enjoys his work as an AAP PREP-ID editorial board member. His overlapping clinical and research interests include immunization advocacy and studies related to the treatment and prevention of viral respiratory tract infections, particularly respiratory syncytial virus. He has published more than 120 papers and book chapters in these areas. Dr. Domachowske has had the privilege of presenting on his global vaccine advocacy efforts with funding through AAP’s Shot@Life program.
Dr. Rushton Jr. is a clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics (QTIP) network. He has practiced pediatrics in Beaufort, S.C., for 32 years and is the author of “Family Support in Community Pediatrics, Confronting the Challenge. “Dr. Rushton’s academic interests include quality improvement, community pediatrics, early brain development, home visitation, and group well child care.
Dr. Smart practices general pediatrics and adolescent medicine as a member of the Sharp Rees-Stealy Medical Group in San Diego. He is a voluntary assistant clinical professor of pediatrics at the University of California, San Diego, and is currently chief of pediatrics at Sharp Mary Birch Hospital for Women & Newborns. Dr. Smart’s interests include medical informatics, health care IT, and specifically clinical decision support and the use of data to drive clinical quality improvement.
We are pleased to welcome Dr. Joseph B. Domachowske, Dr. Howard Smart, and Dr. Francis E. Rushton Jr. to the Pediatric News Editorial Advisory Board.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University in Syracuse. He serves on the New York State American Academy of Pediatrics Chapter 1 executive committee, volunteers as his district’s immunization champion, and is an appointed member of the New York State Immunization Advisory Council. He also enjoys his work as an AAP PREP-ID editorial board member. His overlapping clinical and research interests include immunization advocacy and studies related to the treatment and prevention of viral respiratory tract infections, particularly respiratory syncytial virus. He has published more than 120 papers and book chapters in these areas. Dr. Domachowske has had the privilege of presenting on his global vaccine advocacy efforts with funding through AAP’s Shot@Life program.
Dr. Rushton Jr. is a clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics (QTIP) network. He has practiced pediatrics in Beaufort, S.C., for 32 years and is the author of “Family Support in Community Pediatrics, Confronting the Challenge. “Dr. Rushton’s academic interests include quality improvement, community pediatrics, early brain development, home visitation, and group well child care.
Dr. Smart practices general pediatrics and adolescent medicine as a member of the Sharp Rees-Stealy Medical Group in San Diego. He is a voluntary assistant clinical professor of pediatrics at the University of California, San Diego, and is currently chief of pediatrics at Sharp Mary Birch Hospital for Women & Newborns. Dr. Smart’s interests include medical informatics, health care IT, and specifically clinical decision support and the use of data to drive clinical quality improvement.
We are pleased to welcome Dr. Joseph B. Domachowske, Dr. Howard Smart, and Dr. Francis E. Rushton Jr. to the Pediatric News Editorial Advisory Board.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University in Syracuse. He serves on the New York State American Academy of Pediatrics Chapter 1 executive committee, volunteers as his district’s immunization champion, and is an appointed member of the New York State Immunization Advisory Council. He also enjoys his work as an AAP PREP-ID editorial board member. His overlapping clinical and research interests include immunization advocacy and studies related to the treatment and prevention of viral respiratory tract infections, particularly respiratory syncytial virus. He has published more than 120 papers and book chapters in these areas. Dr. Domachowske has had the privilege of presenting on his global vaccine advocacy efforts with funding through AAP’s Shot@Life program.
Dr. Rushton Jr. is a clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics (QTIP) network. He has practiced pediatrics in Beaufort, S.C., for 32 years and is the author of “Family Support in Community Pediatrics, Confronting the Challenge. “Dr. Rushton’s academic interests include quality improvement, community pediatrics, early brain development, home visitation, and group well child care.
Dr. Smart practices general pediatrics and adolescent medicine as a member of the Sharp Rees-Stealy Medical Group in San Diego. He is a voluntary assistant clinical professor of pediatrics at the University of California, San Diego, and is currently chief of pediatrics at Sharp Mary Birch Hospital for Women & Newborns. Dr. Smart’s interests include medical informatics, health care IT, and specifically clinical decision support and the use of data to drive clinical quality improvement.
Survey: ObGyns’ salaries rose slightly in 2013
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
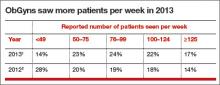
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
FDA Advisory Committee recommends HPV test as primary screening tool for cervical cancer
The US Food and Drug Administration (FDA) Microbiology Devices Panel of the Medical Devices Advisory Committee has unanimously recommended that the cobas HPV (human papillomavirus) test be used as a first-line primary screening tool in women aged 25 years and older to assess their risk of cervical cancer based on the presence of clinically relevant high-risk HPV DNA. The committee’s recommendation indicates that the benefits outweigh the risks of the test, and that the cobas HPV test is safe and effective for the proposed indication for use.1
If approved by the FDA, the cobas HPV test would become the “first and only HPV test indicated as the first-line primary screen of cervical cancer in the United States.”2 Although the FDA is not required to follow the Advisory Committee’s recommendation, it takes the advice into consideration.
Data behind the recommendation
The Advisory Committee’s recommendation is supported by data from the ATHENA study, which included more than 47,000 women – the largest US-based registration study for cervical cancer screening. Data show that when the cobas HPV test was used as the primary test and Pap cytology as a secondary test, significantly more cervical disease was detected compared with Pap screening alone.2
“Through technological and scientific advancement, we now have a better screening tool for cervical cancer. Women around the world deserve the best tool to know their risk and reduce their chances of developing cervical cancer,” said Roland Diggelmann, COO for the Division of Roche Diagnostics, the company who developed and manufactures the test. “We look forward to working with the FDA and medical community to support the growing understanding and awareness of the role that HPV plays in cervical disease, and the importance of the cobas HPV test, which provides the necessary medical benefit to become the first-line test in a cervical cancer screening strategy.”2
How could current practice change as a result of final FDA approval?
The cobas HPV test is currently FDA-approved for co-testing with the Pap smear in women older than age 30 for cervical cancer screening, and for screening patients aged 21 and older with abnormal cervical cytology results.
Mark H. Einstein, MD, MS, chair of the cervical cancer education efforts of the Foundation for Women’s Cancer and professor of obstetrics and gynecology at Albert Einstein Cancer Center and Montefiore Medical Center in Bronx, New York, says final approval of this testing as a primary screening tool represents significant changes to clinical practice. However, “similar to what happened when co-testing [with the cobas HPV test] was approved, it took time for scientific stakeholding groups to update clinical guidelines, then years before clinicians adopted it into routine practice.”
“Unlike a new prescription, clinical algorithms tend to be 'hard-wired' into clinicians heads, and adopting significant change is a process,” Einstein says. “It’s likely that a new cervical cancer screening testing clinical algorithm would be adopted by some clinicians early and by many clinicians over time.” He added that the Society of Gynecologic Oncologists and the American Society for Colposcopy and Cervical Pathology have an interim clinical guidance document currently drafted, and those guidelines will be released soon after any decisions by the FDA.
When that time comes (assuming final FDA approval is received), Einstein says, “some clinical settings will be able to start with the more sensitive HPV test. For some patients, this will be followed by genotyping or cytology. This has been shown to be an effective strategy for honing in on the most at-risk women in a screening population.”
- FDA Executive Summary: March 12, 2014. 2014 Meeting Materials of the Microbiology Devices Panel. FDA Web site. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/MicrobiologyDevicesPanel/UCM388564.pdf. Accessed March 14, 2014.
- FDA Advisory Committee unanimously recommends Roche's HPV Test as primary screening tool for detection of women at high risk for cervical cancer [media release]. http://www.roche.com/media/media_releases/med-cor-2014-03-13.htm. Published March 13, 2014. Accessed March 14, 2014.
The US Food and Drug Administration (FDA) Microbiology Devices Panel of the Medical Devices Advisory Committee has unanimously recommended that the cobas HPV (human papillomavirus) test be used as a first-line primary screening tool in women aged 25 years and older to assess their risk of cervical cancer based on the presence of clinically relevant high-risk HPV DNA. The committee’s recommendation indicates that the benefits outweigh the risks of the test, and that the cobas HPV test is safe and effective for the proposed indication for use.1
If approved by the FDA, the cobas HPV test would become the “first and only HPV test indicated as the first-line primary screen of cervical cancer in the United States.”2 Although the FDA is not required to follow the Advisory Committee’s recommendation, it takes the advice into consideration.
Data behind the recommendation
The Advisory Committee’s recommendation is supported by data from the ATHENA study, which included more than 47,000 women – the largest US-based registration study for cervical cancer screening. Data show that when the cobas HPV test was used as the primary test and Pap cytology as a secondary test, significantly more cervical disease was detected compared with Pap screening alone.2
“Through technological and scientific advancement, we now have a better screening tool for cervical cancer. Women around the world deserve the best tool to know their risk and reduce their chances of developing cervical cancer,” said Roland Diggelmann, COO for the Division of Roche Diagnostics, the company who developed and manufactures the test. “We look forward to working with the FDA and medical community to support the growing understanding and awareness of the role that HPV plays in cervical disease, and the importance of the cobas HPV test, which provides the necessary medical benefit to become the first-line test in a cervical cancer screening strategy.”2
How could current practice change as a result of final FDA approval?
The cobas HPV test is currently FDA-approved for co-testing with the Pap smear in women older than age 30 for cervical cancer screening, and for screening patients aged 21 and older with abnormal cervical cytology results.
Mark H. Einstein, MD, MS, chair of the cervical cancer education efforts of the Foundation for Women’s Cancer and professor of obstetrics and gynecology at Albert Einstein Cancer Center and Montefiore Medical Center in Bronx, New York, says final approval of this testing as a primary screening tool represents significant changes to clinical practice. However, “similar to what happened when co-testing [with the cobas HPV test] was approved, it took time for scientific stakeholding groups to update clinical guidelines, then years before clinicians adopted it into routine practice.”
“Unlike a new prescription, clinical algorithms tend to be 'hard-wired' into clinicians heads, and adopting significant change is a process,” Einstein says. “It’s likely that a new cervical cancer screening testing clinical algorithm would be adopted by some clinicians early and by many clinicians over time.” He added that the Society of Gynecologic Oncologists and the American Society for Colposcopy and Cervical Pathology have an interim clinical guidance document currently drafted, and those guidelines will be released soon after any decisions by the FDA.
When that time comes (assuming final FDA approval is received), Einstein says, “some clinical settings will be able to start with the more sensitive HPV test. For some patients, this will be followed by genotyping or cytology. This has been shown to be an effective strategy for honing in on the most at-risk women in a screening population.”
The US Food and Drug Administration (FDA) Microbiology Devices Panel of the Medical Devices Advisory Committee has unanimously recommended that the cobas HPV (human papillomavirus) test be used as a first-line primary screening tool in women aged 25 years and older to assess their risk of cervical cancer based on the presence of clinically relevant high-risk HPV DNA. The committee’s recommendation indicates that the benefits outweigh the risks of the test, and that the cobas HPV test is safe and effective for the proposed indication for use.1
If approved by the FDA, the cobas HPV test would become the “first and only HPV test indicated as the first-line primary screen of cervical cancer in the United States.”2 Although the FDA is not required to follow the Advisory Committee’s recommendation, it takes the advice into consideration.
Data behind the recommendation
The Advisory Committee’s recommendation is supported by data from the ATHENA study, which included more than 47,000 women – the largest US-based registration study for cervical cancer screening. Data show that when the cobas HPV test was used as the primary test and Pap cytology as a secondary test, significantly more cervical disease was detected compared with Pap screening alone.2
“Through technological and scientific advancement, we now have a better screening tool for cervical cancer. Women around the world deserve the best tool to know their risk and reduce their chances of developing cervical cancer,” said Roland Diggelmann, COO for the Division of Roche Diagnostics, the company who developed and manufactures the test. “We look forward to working with the FDA and medical community to support the growing understanding and awareness of the role that HPV plays in cervical disease, and the importance of the cobas HPV test, which provides the necessary medical benefit to become the first-line test in a cervical cancer screening strategy.”2
How could current practice change as a result of final FDA approval?
The cobas HPV test is currently FDA-approved for co-testing with the Pap smear in women older than age 30 for cervical cancer screening, and for screening patients aged 21 and older with abnormal cervical cytology results.
Mark H. Einstein, MD, MS, chair of the cervical cancer education efforts of the Foundation for Women’s Cancer and professor of obstetrics and gynecology at Albert Einstein Cancer Center and Montefiore Medical Center in Bronx, New York, says final approval of this testing as a primary screening tool represents significant changes to clinical practice. However, “similar to what happened when co-testing [with the cobas HPV test] was approved, it took time for scientific stakeholding groups to update clinical guidelines, then years before clinicians adopted it into routine practice.”
“Unlike a new prescription, clinical algorithms tend to be 'hard-wired' into clinicians heads, and adopting significant change is a process,” Einstein says. “It’s likely that a new cervical cancer screening testing clinical algorithm would be adopted by some clinicians early and by many clinicians over time.” He added that the Society of Gynecologic Oncologists and the American Society for Colposcopy and Cervical Pathology have an interim clinical guidance document currently drafted, and those guidelines will be released soon after any decisions by the FDA.
When that time comes (assuming final FDA approval is received), Einstein says, “some clinical settings will be able to start with the more sensitive HPV test. For some patients, this will be followed by genotyping or cytology. This has been shown to be an effective strategy for honing in on the most at-risk women in a screening population.”
- FDA Executive Summary: March 12, 2014. 2014 Meeting Materials of the Microbiology Devices Panel. FDA Web site. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/MicrobiologyDevicesPanel/UCM388564.pdf. Accessed March 14, 2014.
- FDA Advisory Committee unanimously recommends Roche's HPV Test as primary screening tool for detection of women at high risk for cervical cancer [media release]. http://www.roche.com/media/media_releases/med-cor-2014-03-13.htm. Published March 13, 2014. Accessed March 14, 2014.
- FDA Executive Summary: March 12, 2014. 2014 Meeting Materials of the Microbiology Devices Panel. FDA Web site. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/MicrobiologyDevicesPanel/UCM388564.pdf. Accessed March 14, 2014.
- FDA Advisory Committee unanimously recommends Roche's HPV Test as primary screening tool for detection of women at high risk for cervical cancer [media release]. http://www.roche.com/media/media_releases/med-cor-2014-03-13.htm. Published March 13, 2014. Accessed March 14, 2014.
Hysterectomy routes and surgical outcomes in obese patients analyzed
In obese women, laparoscopic hysterectomy provided the shortest operating time with minimal blood loss when compared with vaginal hysterectomy, according to a poster presented at the 42nd AAGL Global Congress in Washington, DC, in November 2013.1
Teresa Tam, MD, Gerald Harkins, MD, and researchers at Penn State Milton S. Hershey Medical Center in Hershey, Pennsylvania, reported on a retrospective cohort study conducted to compare the routes of hysterectomy and surgical outcomes in obese patients.
Of the 1,286 patients who underwent hysterectomy between December 1, 2009, and December 1, 2012, at Hershey Medical Center, 596 met the obese body mass index (BMI) inclusion criteria (BMI >30 kg/m2). Mean (SD) BMI was 36.5 (5.8) kg/m2 and the mean (SD) patient age was 45 (10) years. Mean (SD) gravidity was 2.44 (1.85) and mean (SD) parity was 1.97 (1.41).
Reasons for surgery were restricted to benign indications, including leiomyoma (31%); abnormal uterine bleeding (29%); and endometriosis (17%).
The following approaches to hysterectomy were included:
- abdominal hysterectomy [total abdominal and supracervical] (AH; n = 7)
- vaginal hysterectomy (VH; n = 84)
- laparoscopic-assisted vaginal hysterectomy (LAVH; n = 16)
- total laparoscopic hysterectomy [conventional and robotic] (TLH; n = 295)
- laparoscopic supracervical hysterectomy [conventional and robotic] (LSH; n = 194).
Comparisons to AH were not considered in the results (n = 7). Less than 1% of the hysterectomies were abdominal cases, with majority (5 out of 7 AHs) performed being combined cases, in conjunction with colorectal service for colon or rectal malignancies. Data on preoperative indications, estimated blood loss, operating time, length of stay, and postoperative complications were compared.
The largest differences in median (SD) operating time were between TLH and LAVH (80 min vs 137.5 min, respectively; P <.001) and LSH and LAVH (90 min vs 137.5 min, respectively; P <.001).
The only statistically significant difference with regard to patients’ median (SD) length of stay was between TLH and VH (1.07 days vs 1.12 days, respectively; P = .005), but the researchers did not consider a difference of 0.05 days (1.2 hours) to be clinically relevant.
The odds of estimated blood loss of 200 mL or greater were significantly higher with VH than with TLH (35.0% vs 3.4%, respectively; odds ratio [OR] = 15.3; 95% confidence interval [CI], 7.0–33.4; P <.001). The odds of estimated blood loss also were significantly higher with VH than with LSH (35.0% vs. 8.4%; OR = 5.9; 95% CI, 3.0–11.7; P <.001).
No association was found between high BMI and surgical complications, the authors reported. However, due to the study’s retrospective nature, Tam and Harkins note that surgeon selection bias on the route of hysterectomy could be based on concerns with operative access and outcomes in obese patients. The authors concur that more studies need to be performed comparing robotic with conventional laparoscopic routes of hysterectomy in the obese.
“In this study, laparoscopic hysterectomy offered the shortest operating time with minimal blood loss compared to the vaginal route in the obese patient population,” the authors concluded.
They noted, however, that, “Although performing hysterectomy in obese patients can be challenging, this study reaffirms that a minimally invasive approach to hysterectomy is both safe and effective. Providing either a vaginal or laparoscopic modality to hysterectomy is often requested by patients, and is supported by the American Congress of Obstetricians and Gynecologists (ACOG) and the AAGL.”
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
Reference
Tam T, Gupta M, Alligood-Percoco N, de los Reyes S, Davies M, Harkins G. Comparison of routes of hysterectomy and their surgical outcomes in obese patients. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
In obese women, laparoscopic hysterectomy provided the shortest operating time with minimal blood loss when compared with vaginal hysterectomy, according to a poster presented at the 42nd AAGL Global Congress in Washington, DC, in November 2013.1
Teresa Tam, MD, Gerald Harkins, MD, and researchers at Penn State Milton S. Hershey Medical Center in Hershey, Pennsylvania, reported on a retrospective cohort study conducted to compare the routes of hysterectomy and surgical outcomes in obese patients.
Of the 1,286 patients who underwent hysterectomy between December 1, 2009, and December 1, 2012, at Hershey Medical Center, 596 met the obese body mass index (BMI) inclusion criteria (BMI >30 kg/m2). Mean (SD) BMI was 36.5 (5.8) kg/m2 and the mean (SD) patient age was 45 (10) years. Mean (SD) gravidity was 2.44 (1.85) and mean (SD) parity was 1.97 (1.41).
Reasons for surgery were restricted to benign indications, including leiomyoma (31%); abnormal uterine bleeding (29%); and endometriosis (17%).
The following approaches to hysterectomy were included:
- abdominal hysterectomy [total abdominal and supracervical] (AH; n = 7)
- vaginal hysterectomy (VH; n = 84)
- laparoscopic-assisted vaginal hysterectomy (LAVH; n = 16)
- total laparoscopic hysterectomy [conventional and robotic] (TLH; n = 295)
- laparoscopic supracervical hysterectomy [conventional and robotic] (LSH; n = 194).
Comparisons to AH were not considered in the results (n = 7). Less than 1% of the hysterectomies were abdominal cases, with majority (5 out of 7 AHs) performed being combined cases, in conjunction with colorectal service for colon or rectal malignancies. Data on preoperative indications, estimated blood loss, operating time, length of stay, and postoperative complications were compared.
The largest differences in median (SD) operating time were between TLH and LAVH (80 min vs 137.5 min, respectively; P <.001) and LSH and LAVH (90 min vs 137.5 min, respectively; P <.001).
The only statistically significant difference with regard to patients’ median (SD) length of stay was between TLH and VH (1.07 days vs 1.12 days, respectively; P = .005), but the researchers did not consider a difference of 0.05 days (1.2 hours) to be clinically relevant.
The odds of estimated blood loss of 200 mL or greater were significantly higher with VH than with TLH (35.0% vs 3.4%, respectively; odds ratio [OR] = 15.3; 95% confidence interval [CI], 7.0–33.4; P <.001). The odds of estimated blood loss also were significantly higher with VH than with LSH (35.0% vs. 8.4%; OR = 5.9; 95% CI, 3.0–11.7; P <.001).
No association was found between high BMI and surgical complications, the authors reported. However, due to the study’s retrospective nature, Tam and Harkins note that surgeon selection bias on the route of hysterectomy could be based on concerns with operative access and outcomes in obese patients. The authors concur that more studies need to be performed comparing robotic with conventional laparoscopic routes of hysterectomy in the obese.
“In this study, laparoscopic hysterectomy offered the shortest operating time with minimal blood loss compared to the vaginal route in the obese patient population,” the authors concluded.
They noted, however, that, “Although performing hysterectomy in obese patients can be challenging, this study reaffirms that a minimally invasive approach to hysterectomy is both safe and effective. Providing either a vaginal or laparoscopic modality to hysterectomy is often requested by patients, and is supported by the American Congress of Obstetricians and Gynecologists (ACOG) and the AAGL.”
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
In obese women, laparoscopic hysterectomy provided the shortest operating time with minimal blood loss when compared with vaginal hysterectomy, according to a poster presented at the 42nd AAGL Global Congress in Washington, DC, in November 2013.1
Teresa Tam, MD, Gerald Harkins, MD, and researchers at Penn State Milton S. Hershey Medical Center in Hershey, Pennsylvania, reported on a retrospective cohort study conducted to compare the routes of hysterectomy and surgical outcomes in obese patients.
Of the 1,286 patients who underwent hysterectomy between December 1, 2009, and December 1, 2012, at Hershey Medical Center, 596 met the obese body mass index (BMI) inclusion criteria (BMI >30 kg/m2). Mean (SD) BMI was 36.5 (5.8) kg/m2 and the mean (SD) patient age was 45 (10) years. Mean (SD) gravidity was 2.44 (1.85) and mean (SD) parity was 1.97 (1.41).
Reasons for surgery were restricted to benign indications, including leiomyoma (31%); abnormal uterine bleeding (29%); and endometriosis (17%).
The following approaches to hysterectomy were included:
- abdominal hysterectomy [total abdominal and supracervical] (AH; n = 7)
- vaginal hysterectomy (VH; n = 84)
- laparoscopic-assisted vaginal hysterectomy (LAVH; n = 16)
- total laparoscopic hysterectomy [conventional and robotic] (TLH; n = 295)
- laparoscopic supracervical hysterectomy [conventional and robotic] (LSH; n = 194).
Comparisons to AH were not considered in the results (n = 7). Less than 1% of the hysterectomies were abdominal cases, with majority (5 out of 7 AHs) performed being combined cases, in conjunction with colorectal service for colon or rectal malignancies. Data on preoperative indications, estimated blood loss, operating time, length of stay, and postoperative complications were compared.
The largest differences in median (SD) operating time were between TLH and LAVH (80 min vs 137.5 min, respectively; P <.001) and LSH and LAVH (90 min vs 137.5 min, respectively; P <.001).
The only statistically significant difference with regard to patients’ median (SD) length of stay was between TLH and VH (1.07 days vs 1.12 days, respectively; P = .005), but the researchers did not consider a difference of 0.05 days (1.2 hours) to be clinically relevant.
The odds of estimated blood loss of 200 mL or greater were significantly higher with VH than with TLH (35.0% vs 3.4%, respectively; odds ratio [OR] = 15.3; 95% confidence interval [CI], 7.0–33.4; P <.001). The odds of estimated blood loss also were significantly higher with VH than with LSH (35.0% vs. 8.4%; OR = 5.9; 95% CI, 3.0–11.7; P <.001).
No association was found between high BMI and surgical complications, the authors reported. However, due to the study’s retrospective nature, Tam and Harkins note that surgeon selection bias on the route of hysterectomy could be based on concerns with operative access and outcomes in obese patients. The authors concur that more studies need to be performed comparing robotic with conventional laparoscopic routes of hysterectomy in the obese.
“In this study, laparoscopic hysterectomy offered the shortest operating time with minimal blood loss compared to the vaginal route in the obese patient population,” the authors concluded.
They noted, however, that, “Although performing hysterectomy in obese patients can be challenging, this study reaffirms that a minimally invasive approach to hysterectomy is both safe and effective. Providing either a vaginal or laparoscopic modality to hysterectomy is often requested by patients, and is supported by the American Congress of Obstetricians and Gynecologists (ACOG) and the AAGL.”
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
Reference
Tam T, Gupta M, Alligood-Percoco N, de los Reyes S, Davies M, Harkins G. Comparison of routes of hysterectomy and their surgical outcomes in obese patients. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
Reference
Tam T, Gupta M, Alligood-Percoco N, de los Reyes S, Davies M, Harkins G. Comparison of routes of hysterectomy and their surgical outcomes in obese patients. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
Gyns can treat men for STDs again, ABOG says
When the American Board of Obstetrics and Gynecology (ABOG) announced in September that, with a few exceptions, gynecologists could lose their board certification if they treated men, gynecologists were forced to stop treating male patients. This decision has now been altered, and gynecologists are now allowed to treat male patients for sexually transmitted diseases (STDs) and to screen men for anal cancer.1
Experts in anal cancer and patient advocacy groups lobbied ABOG to revise their position based on gynecologists’ long-standing tradition of treating men and women for STDs. Anal cancer is usually caused by human papillomavirus. Although rare, the incidence of anal cancer is increasing, especially among those infected with human immunodeficiency virus.1
ABOG’s new statement reads2:
To remain certified by ABOG the care of male patients is prohibited except in the
following circumstances:
- active government service
- evaluation of fertility
- genetic counseling and testing of a couple
- evaluation and management of sexually transmitted infections
- administration of immunizations
- management of transgender conditions
- emergency, pandemic, humanitarian or disaster response care
- family planning services, not to include vasectomy
- newborn circumcision
- completion of ACGME-accredited training and certification in other specialties.
Mark H. Einstein, MD, professor in the Department of Obstetrics and Gynecology and Women’s Health at Montefiore Medical Center in Bronx, New York, and author of “Update on Cervical Disease” (OBG Management, May 2013), was forced to discontinue seeing male patients. He commented, “Cool heads have prevailed. This is the best decision for our patients.”1
We want to hear from you. Tell us what you think!
- Grady D. Gynecologists may treat men, board says in switch. The New York Times. http://www.nytimes.com/2013/11/27/health/gynecologists-may-treat-men-board-says-in-switch.html?emc=eta1. Published November 26, 2013. Accessed December 5, 2013.
- American Board of Obstetrics & Gynecology. Definition of an ABOG-certified Obstetrician-Gynecologist. ABO+G Web site. http://www.abog.org/definition.asp. Revised 11/26/13. Accessed December 5, 2013.
When the American Board of Obstetrics and Gynecology (ABOG) announced in September that, with a few exceptions, gynecologists could lose their board certification if they treated men, gynecologists were forced to stop treating male patients. This decision has now been altered, and gynecologists are now allowed to treat male patients for sexually transmitted diseases (STDs) and to screen men for anal cancer.1
Experts in anal cancer and patient advocacy groups lobbied ABOG to revise their position based on gynecologists’ long-standing tradition of treating men and women for STDs. Anal cancer is usually caused by human papillomavirus. Although rare, the incidence of anal cancer is increasing, especially among those infected with human immunodeficiency virus.1
ABOG’s new statement reads2:
To remain certified by ABOG the care of male patients is prohibited except in the
following circumstances:
- active government service
- evaluation of fertility
- genetic counseling and testing of a couple
- evaluation and management of sexually transmitted infections
- administration of immunizations
- management of transgender conditions
- emergency, pandemic, humanitarian or disaster response care
- family planning services, not to include vasectomy
- newborn circumcision
- completion of ACGME-accredited training and certification in other specialties.
Mark H. Einstein, MD, professor in the Department of Obstetrics and Gynecology and Women’s Health at Montefiore Medical Center in Bronx, New York, and author of “Update on Cervical Disease” (OBG Management, May 2013), was forced to discontinue seeing male patients. He commented, “Cool heads have prevailed. This is the best decision for our patients.”1
We want to hear from you. Tell us what you think!
When the American Board of Obstetrics and Gynecology (ABOG) announced in September that, with a few exceptions, gynecologists could lose their board certification if they treated men, gynecologists were forced to stop treating male patients. This decision has now been altered, and gynecologists are now allowed to treat male patients for sexually transmitted diseases (STDs) and to screen men for anal cancer.1
Experts in anal cancer and patient advocacy groups lobbied ABOG to revise their position based on gynecologists’ long-standing tradition of treating men and women for STDs. Anal cancer is usually caused by human papillomavirus. Although rare, the incidence of anal cancer is increasing, especially among those infected with human immunodeficiency virus.1
ABOG’s new statement reads2:
To remain certified by ABOG the care of male patients is prohibited except in the
following circumstances:
- active government service
- evaluation of fertility
- genetic counseling and testing of a couple
- evaluation and management of sexually transmitted infections
- administration of immunizations
- management of transgender conditions
- emergency, pandemic, humanitarian or disaster response care
- family planning services, not to include vasectomy
- newborn circumcision
- completion of ACGME-accredited training and certification in other specialties.
Mark H. Einstein, MD, professor in the Department of Obstetrics and Gynecology and Women’s Health at Montefiore Medical Center in Bronx, New York, and author of “Update on Cervical Disease” (OBG Management, May 2013), was forced to discontinue seeing male patients. He commented, “Cool heads have prevailed. This is the best decision for our patients.”1
We want to hear from you. Tell us what you think!
- Grady D. Gynecologists may treat men, board says in switch. The New York Times. http://www.nytimes.com/2013/11/27/health/gynecologists-may-treat-men-board-says-in-switch.html?emc=eta1. Published November 26, 2013. Accessed December 5, 2013.
- American Board of Obstetrics & Gynecology. Definition of an ABOG-certified Obstetrician-Gynecologist. ABO+G Web site. http://www.abog.org/definition.asp. Revised 11/26/13. Accessed December 5, 2013.
- Grady D. Gynecologists may treat men, board says in switch. The New York Times. http://www.nytimes.com/2013/11/27/health/gynecologists-may-treat-men-board-says-in-switch.html?emc=eta1. Published November 26, 2013. Accessed December 5, 2013.
- American Board of Obstetrics & Gynecology. Definition of an ABOG-certified Obstetrician-Gynecologist. ABO+G Web site. http://www.abog.org/definition.asp. Revised 11/26/13. Accessed December 5, 2013.
Helping Patients Navigate the Web
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
CDC urges flu vaccination for all, especially pregnant women
In an appeal for increased vaccination against influenza, the Centers for Disease Control and Prevention (CDC) announced that, although vaccination coverage has increased for some groups of the population, the nation needs to do better. Recommendations from the Advisory Committee on Immunization Practices reported seasonal influenza vaccination data in the CDC’s Morbidity and Mortality Weekly Report (MMWR) on September 20, 2013.1
More children aged 6 months through 17 years received the influenza vaccine during the 2012–2013 season (56.6%), up 5.1% from the 2011–2012 season. Smaller increases were reported for adults aged 18 years and older at 41.5%, up 2.7% from 2011–2012. Overall, 45% of the entire US population aged 6 months and older was vaccinated in 2012–2013. However, this falls short of public health goals.2
Howard K. Koh, MD, Assistant Secretary for Health at the US Department of Health and Human Services, pointed out that, although the increases in number of those who received the influenza vaccine last year is significant, there is more work to do. “Despite substantial progress, we can do even more to make our country healthier through prevention. Flu vaccination should represent a simple investment we make year in and year out to maximize the gift of health.”2
What vaccines will be available for the 2013-2014 season?
The 2013-2014 influenza vaccine is detailed in MMWR1:
Risk of complications from influenza
Mothers. Vaccination to prevent influenza is particularly important for those who are at increased risk for severe complications from influenza. Pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant because of changes in the immune system, heart, and lungs during pregnancy.1
Increased severity of influenza among pregnant women was reported during pandemics in 1918–1919, 1957–1958, and 2009–2010. Severe infections were also observed among postpartum (within 2 weeks after delivery) women during the 2009–2010 pandemic.1
One study by Cox et al indicated an increase in delivery complications, including fetal distress, preterm labor, and cesarean delivery, for pregnant women with respiratory hospitalizations during the flu season.1
Vaccination coverage has increased in pregnant women in the last few years, but, unlike other groups where rates continue to increase, coverage in pregnant women appears to have stalled at around 50%.2
Pregnant women who were treated with antivirals more than 4 days after symptoms arose were more likely to be admitted to an ICU (57% vs 9%; 95% confidence interval [CI] 3.5–10.6] than those treated within 2 days on symptom onset.1
Infants. Pregnant women have protective levels of anti-influenza antibodies after vaccination that are passively transferred to their children. In a randomized controlled trial of vaccinated pregnant women who later breastfed their children, infants of vaccinated women had a 63% reduction in laboratory-confirmed influenza during the first 6 months of life. In addition, authors Zaman et al reported a 29% reduction in respiratory illness with fever among the infants and a 36% reduction in respiratory illness with fever among their mothers during the first 6 months after birth.1
Another study by Eick et al found that infants aged less than 6 months who were born to women who were given influenza vaccination during pregnancy had significantly reduced risk for influenza virus infection (relative risk [RR]: 0.59; 95% CI = 0.37–0.93) and hospitalization for influenza-like illness (ILI) (RR: 0.61; 95% CI = 0.45–0.84).1
Infants born to women with laboratory-confirmed flu during pregnancy did not have higher rates of low birthweight, congenital abnormalities, or lower Apgar scores compared with infants born to uninfected women.1
ACOG recommendations for pregnant and postpartum women
Because of the increased risk for serious illness and complications from influenza, the American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are pregnant or who might be pregnant in the upcoming influenza season receive the IIV vaccine. This vaccination can be administered at any time during pregnancy, before and during the influenza season.3
LAIV is not recommended for pregnant women. Postpartum women can receive either LAIV or IIV. Pregnant and postpartum women do not need to avoid contact with persons recently vaccinated with LAIV.1
Recommendations for nonpregnant women
The CDC continues to recommend annual influenza vaccination for all persons ages 6 months or older. Among healthy younger adults, seasonal influenza is typically less acute and results less often in hospitalization, as compared with children aged <5 years, adults aged ≥65 years, pregnant women, or persons with chronic medical conditions. The flu is a significant reason for outpatient medical visits and worker absenteeism among healthy adults aged 19 through 49 years.1
For specific guidelines, visit the CDC’s “Influenza Vaccination: A Summary for Clinicians” at http://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm.
What can you, as a physician, do?
Health-care professionals are critical to the vaccination program and need to lead by example. “If you are around people at high risk for flu complications, you need to get vaccinated,” said Anne Schuchat, MD, Assistant Surgeon General, US Publish Health Service, and Director of the National Center for Immunization and Respiratory Diseases at the CDC.2
The CDC reported that 72% of health-care personal received a vaccination in 2012–2013. Physicians had the highest coverage at 92.3%.2
“Patients also look to you,” said Dr. Schuchat. “Data show that a personal recommendation makes a big difference to patients.”2
For example, pregnant women whose physicians recommend flu vaccination are five times more likely to get vaccinated. Dr. Schuchat also reminded healthcare professionals that they should begin vaccinating patients as soon as vaccine is available in their area.
- Grahskopf LA, Shay DK, Shimabukuro TT, et al; Advisory Committee on Immunization Practices. Prevention and control of seasonal influenza with Vaccines. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2013;62(RR07):1–43. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w. Accessed September 26, 2013.
- Flu vaccination coverage on the rise; health officials urge continued vigilance [press release] (Susan Heins, e-mail communication, September 26, 2013).
- Committee of Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion No. 468: Influenza vaccination during pregnancy. Obstet Gynecol. 2010;116(4):1006–1007.
In an appeal for increased vaccination against influenza, the Centers for Disease Control and Prevention (CDC) announced that, although vaccination coverage has increased for some groups of the population, the nation needs to do better. Recommendations from the Advisory Committee on Immunization Practices reported seasonal influenza vaccination data in the CDC’s Morbidity and Mortality Weekly Report (MMWR) on September 20, 2013.1
More children aged 6 months through 17 years received the influenza vaccine during the 2012–2013 season (56.6%), up 5.1% from the 2011–2012 season. Smaller increases were reported for adults aged 18 years and older at 41.5%, up 2.7% from 2011–2012. Overall, 45% of the entire US population aged 6 months and older was vaccinated in 2012–2013. However, this falls short of public health goals.2
Howard K. Koh, MD, Assistant Secretary for Health at the US Department of Health and Human Services, pointed out that, although the increases in number of those who received the influenza vaccine last year is significant, there is more work to do. “Despite substantial progress, we can do even more to make our country healthier through prevention. Flu vaccination should represent a simple investment we make year in and year out to maximize the gift of health.”2
What vaccines will be available for the 2013-2014 season?
The 2013-2014 influenza vaccine is detailed in MMWR1:
Risk of complications from influenza
Mothers. Vaccination to prevent influenza is particularly important for those who are at increased risk for severe complications from influenza. Pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant because of changes in the immune system, heart, and lungs during pregnancy.1
Increased severity of influenza among pregnant women was reported during pandemics in 1918–1919, 1957–1958, and 2009–2010. Severe infections were also observed among postpartum (within 2 weeks after delivery) women during the 2009–2010 pandemic.1
One study by Cox et al indicated an increase in delivery complications, including fetal distress, preterm labor, and cesarean delivery, for pregnant women with respiratory hospitalizations during the flu season.1
Vaccination coverage has increased in pregnant women in the last few years, but, unlike other groups where rates continue to increase, coverage in pregnant women appears to have stalled at around 50%.2
Pregnant women who were treated with antivirals more than 4 days after symptoms arose were more likely to be admitted to an ICU (57% vs 9%; 95% confidence interval [CI] 3.5–10.6] than those treated within 2 days on symptom onset.1
Infants. Pregnant women have protective levels of anti-influenza antibodies after vaccination that are passively transferred to their children. In a randomized controlled trial of vaccinated pregnant women who later breastfed their children, infants of vaccinated women had a 63% reduction in laboratory-confirmed influenza during the first 6 months of life. In addition, authors Zaman et al reported a 29% reduction in respiratory illness with fever among the infants and a 36% reduction in respiratory illness with fever among their mothers during the first 6 months after birth.1
Another study by Eick et al found that infants aged less than 6 months who were born to women who were given influenza vaccination during pregnancy had significantly reduced risk for influenza virus infection (relative risk [RR]: 0.59; 95% CI = 0.37–0.93) and hospitalization for influenza-like illness (ILI) (RR: 0.61; 95% CI = 0.45–0.84).1
Infants born to women with laboratory-confirmed flu during pregnancy did not have higher rates of low birthweight, congenital abnormalities, or lower Apgar scores compared with infants born to uninfected women.1
ACOG recommendations for pregnant and postpartum women
Because of the increased risk for serious illness and complications from influenza, the American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are pregnant or who might be pregnant in the upcoming influenza season receive the IIV vaccine. This vaccination can be administered at any time during pregnancy, before and during the influenza season.3
LAIV is not recommended for pregnant women. Postpartum women can receive either LAIV or IIV. Pregnant and postpartum women do not need to avoid contact with persons recently vaccinated with LAIV.1
Recommendations for nonpregnant women
The CDC continues to recommend annual influenza vaccination for all persons ages 6 months or older. Among healthy younger adults, seasonal influenza is typically less acute and results less often in hospitalization, as compared with children aged <5 years, adults aged ≥65 years, pregnant women, or persons with chronic medical conditions. The flu is a significant reason for outpatient medical visits and worker absenteeism among healthy adults aged 19 through 49 years.1
For specific guidelines, visit the CDC’s “Influenza Vaccination: A Summary for Clinicians” at http://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm.
What can you, as a physician, do?
Health-care professionals are critical to the vaccination program and need to lead by example. “If you are around people at high risk for flu complications, you need to get vaccinated,” said Anne Schuchat, MD, Assistant Surgeon General, US Publish Health Service, and Director of the National Center for Immunization and Respiratory Diseases at the CDC.2
The CDC reported that 72% of health-care personal received a vaccination in 2012–2013. Physicians had the highest coverage at 92.3%.2
“Patients also look to you,” said Dr. Schuchat. “Data show that a personal recommendation makes a big difference to patients.”2
For example, pregnant women whose physicians recommend flu vaccination are five times more likely to get vaccinated. Dr. Schuchat also reminded healthcare professionals that they should begin vaccinating patients as soon as vaccine is available in their area.
In an appeal for increased vaccination against influenza, the Centers for Disease Control and Prevention (CDC) announced that, although vaccination coverage has increased for some groups of the population, the nation needs to do better. Recommendations from the Advisory Committee on Immunization Practices reported seasonal influenza vaccination data in the CDC’s Morbidity and Mortality Weekly Report (MMWR) on September 20, 2013.1
More children aged 6 months through 17 years received the influenza vaccine during the 2012–2013 season (56.6%), up 5.1% from the 2011–2012 season. Smaller increases were reported for adults aged 18 years and older at 41.5%, up 2.7% from 2011–2012. Overall, 45% of the entire US population aged 6 months and older was vaccinated in 2012–2013. However, this falls short of public health goals.2
Howard K. Koh, MD, Assistant Secretary for Health at the US Department of Health and Human Services, pointed out that, although the increases in number of those who received the influenza vaccine last year is significant, there is more work to do. “Despite substantial progress, we can do even more to make our country healthier through prevention. Flu vaccination should represent a simple investment we make year in and year out to maximize the gift of health.”2
What vaccines will be available for the 2013-2014 season?
The 2013-2014 influenza vaccine is detailed in MMWR1:
Risk of complications from influenza
Mothers. Vaccination to prevent influenza is particularly important for those who are at increased risk for severe complications from influenza. Pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant because of changes in the immune system, heart, and lungs during pregnancy.1
Increased severity of influenza among pregnant women was reported during pandemics in 1918–1919, 1957–1958, and 2009–2010. Severe infections were also observed among postpartum (within 2 weeks after delivery) women during the 2009–2010 pandemic.1
One study by Cox et al indicated an increase in delivery complications, including fetal distress, preterm labor, and cesarean delivery, for pregnant women with respiratory hospitalizations during the flu season.1
Vaccination coverage has increased in pregnant women in the last few years, but, unlike other groups where rates continue to increase, coverage in pregnant women appears to have stalled at around 50%.2
Pregnant women who were treated with antivirals more than 4 days after symptoms arose were more likely to be admitted to an ICU (57% vs 9%; 95% confidence interval [CI] 3.5–10.6] than those treated within 2 days on symptom onset.1
Infants. Pregnant women have protective levels of anti-influenza antibodies after vaccination that are passively transferred to their children. In a randomized controlled trial of vaccinated pregnant women who later breastfed their children, infants of vaccinated women had a 63% reduction in laboratory-confirmed influenza during the first 6 months of life. In addition, authors Zaman et al reported a 29% reduction in respiratory illness with fever among the infants and a 36% reduction in respiratory illness with fever among their mothers during the first 6 months after birth.1
Another study by Eick et al found that infants aged less than 6 months who were born to women who were given influenza vaccination during pregnancy had significantly reduced risk for influenza virus infection (relative risk [RR]: 0.59; 95% CI = 0.37–0.93) and hospitalization for influenza-like illness (ILI) (RR: 0.61; 95% CI = 0.45–0.84).1
Infants born to women with laboratory-confirmed flu during pregnancy did not have higher rates of low birthweight, congenital abnormalities, or lower Apgar scores compared with infants born to uninfected women.1
ACOG recommendations for pregnant and postpartum women
Because of the increased risk for serious illness and complications from influenza, the American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are pregnant or who might be pregnant in the upcoming influenza season receive the IIV vaccine. This vaccination can be administered at any time during pregnancy, before and during the influenza season.3
LAIV is not recommended for pregnant women. Postpartum women can receive either LAIV or IIV. Pregnant and postpartum women do not need to avoid contact with persons recently vaccinated with LAIV.1
Recommendations for nonpregnant women
The CDC continues to recommend annual influenza vaccination for all persons ages 6 months or older. Among healthy younger adults, seasonal influenza is typically less acute and results less often in hospitalization, as compared with children aged <5 years, adults aged ≥65 years, pregnant women, or persons with chronic medical conditions. The flu is a significant reason for outpatient medical visits and worker absenteeism among healthy adults aged 19 through 49 years.1
For specific guidelines, visit the CDC’s “Influenza Vaccination: A Summary for Clinicians” at http://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm.
What can you, as a physician, do?
Health-care professionals are critical to the vaccination program and need to lead by example. “If you are around people at high risk for flu complications, you need to get vaccinated,” said Anne Schuchat, MD, Assistant Surgeon General, US Publish Health Service, and Director of the National Center for Immunization and Respiratory Diseases at the CDC.2
The CDC reported that 72% of health-care personal received a vaccination in 2012–2013. Physicians had the highest coverage at 92.3%.2
“Patients also look to you,” said Dr. Schuchat. “Data show that a personal recommendation makes a big difference to patients.”2
For example, pregnant women whose physicians recommend flu vaccination are five times more likely to get vaccinated. Dr. Schuchat also reminded healthcare professionals that they should begin vaccinating patients as soon as vaccine is available in their area.
- Grahskopf LA, Shay DK, Shimabukuro TT, et al; Advisory Committee on Immunization Practices. Prevention and control of seasonal influenza with Vaccines. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2013;62(RR07):1–43. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w. Accessed September 26, 2013.
- Flu vaccination coverage on the rise; health officials urge continued vigilance [press release] (Susan Heins, e-mail communication, September 26, 2013).
- Committee of Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion No. 468: Influenza vaccination during pregnancy. Obstet Gynecol. 2010;116(4):1006–1007.
- Grahskopf LA, Shay DK, Shimabukuro TT, et al; Advisory Committee on Immunization Practices. Prevention and control of seasonal influenza with Vaccines. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2013;62(RR07):1–43. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w. Accessed September 26, 2013.
- Flu vaccination coverage on the rise; health officials urge continued vigilance [press release] (Susan Heins, e-mail communication, September 26, 2013).
- Committee of Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion No. 468: Influenza vaccination during pregnancy. Obstet Gynecol. 2010;116(4):1006–1007.
Mean income for ObGyns increased in 2012
ObGyns’ mean income was $242,000 in 2012, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported similar incomes in 2011 and 2012. In 2012, 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earned less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (9% of orthopedic respondents were female). Response rates also matter: of those who responded to the full Medscape poll, 31% were female; of ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
- single-specialty (office-based) group practices: $264,000
- multispecialty (office-based) group practices: $252,000
- hospitals: $216,000
- academic: $212,000
- solo practices (office-based): $208,000
- outpatient clinics: $206,000.
When ranked by work situation, partners beat all other settings at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
Money issues
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization. In 2012, that jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with potentially reduced Medicare payments in 2012 than in 2011. The new report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review annual payments from insurers and drop those who pay the least or create the most trouble. In 2012, 26% of ObGyns reported that they already follow this practice or are planning to take that advice. However, 29% will keep all insurers; they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes; 19% of all physicians said yes.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
- In 2011, 41% of ObGyns regularly discussed the cost of services with their patients; 48% occasionally discussed cost if the patient brought it up (89% total).
- In 2012, 35% of ObGyns regularly discussed cost with their patients; 41% occasionally discussed cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
How you spend your time
How many hours do you work? The number of hours in a workweek remained about the same. In 2012, 11% of ObGyns worked 41 to 45 hours; 13% worked 46 to 50 hours; 4% worked 51 to 55 hours; 9% worked 56 to 60 hours; and 20% reported working less than 30 hours.1
Time spent with patients? In 2012, most ObGyns spent less than 16 minutes with a patient: 30% reported spending 13 to 16 minutes; another 30% spent less than 13 minutes; and 17% saw patients for 21 minutes or longer.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1,094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
ObGyns’ mean income was $242,000 in 2012, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported similar incomes in 2011 and 2012. In 2012, 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earned less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (9% of orthopedic respondents were female). Response rates also matter: of those who responded to the full Medscape poll, 31% were female; of ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
- single-specialty (office-based) group practices: $264,000
- multispecialty (office-based) group practices: $252,000
- hospitals: $216,000
- academic: $212,000
- solo practices (office-based): $208,000
- outpatient clinics: $206,000.
When ranked by work situation, partners beat all other settings at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
Money issues
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization. In 2012, that jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with potentially reduced Medicare payments in 2012 than in 2011. The new report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review annual payments from insurers and drop those who pay the least or create the most trouble. In 2012, 26% of ObGyns reported that they already follow this practice or are planning to take that advice. However, 29% will keep all insurers; they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes; 19% of all physicians said yes.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
- In 2011, 41% of ObGyns regularly discussed the cost of services with their patients; 48% occasionally discussed cost if the patient brought it up (89% total).
- In 2012, 35% of ObGyns regularly discussed cost with their patients; 41% occasionally discussed cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
How you spend your time
How many hours do you work? The number of hours in a workweek remained about the same. In 2012, 11% of ObGyns worked 41 to 45 hours; 13% worked 46 to 50 hours; 4% worked 51 to 55 hours; 9% worked 56 to 60 hours; and 20% reported working less than 30 hours.1
Time spent with patients? In 2012, most ObGyns spent less than 16 minutes with a patient: 30% reported spending 13 to 16 minutes; another 30% spent less than 13 minutes; and 17% saw patients for 21 minutes or longer.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1,094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
ObGyns’ mean income was $242,000 in 2012, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported similar incomes in 2011 and 2012. In 2012, 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earned less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (9% of orthopedic respondents were female). Response rates also matter: of those who responded to the full Medscape poll, 31% were female; of ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
- single-specialty (office-based) group practices: $264,000
- multispecialty (office-based) group practices: $252,000
- hospitals: $216,000
- academic: $212,000
- solo practices (office-based): $208,000
- outpatient clinics: $206,000.
When ranked by work situation, partners beat all other settings at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
Money issues
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization. In 2012, that jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with potentially reduced Medicare payments in 2012 than in 2011. The new report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review annual payments from insurers and drop those who pay the least or create the most trouble. In 2012, 26% of ObGyns reported that they already follow this practice or are planning to take that advice. However, 29% will keep all insurers; they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes; 19% of all physicians said yes.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
- In 2011, 41% of ObGyns regularly discussed the cost of services with their patients; 48% occasionally discussed cost if the patient brought it up (89% total).
- In 2012, 35% of ObGyns regularly discussed cost with their patients; 41% occasionally discussed cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
How you spend your time
How many hours do you work? The number of hours in a workweek remained about the same. In 2012, 11% of ObGyns worked 41 to 45 hours; 13% worked 46 to 50 hours; 4% worked 51 to 55 hours; 9% worked 56 to 60 hours; and 20% reported working less than 30 hours.1
Time spent with patients? In 2012, most ObGyns spent less than 16 minutes with a patient: 30% reported spending 13 to 16 minutes; another 30% spent less than 13 minutes; and 17% saw patients for 21 minutes or longer.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1,094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
The most rewarding part of the job
Discussing cost with patients
How ObGyns spend their time
Long-term increase seen in abdominal sacrocolpopexy failure rates
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
Predicting the Future of Genetics
Thirteen years ago, scientists cracked the human genetic code, opening a world of new possibilities in medical care. At the time, it was (rightfully) trumpeted as a remarkable achievement, a sort of final frontier conquered. Soon, everyone would be able to have their own DNA sequenced, diseases would be identified early enough to prevent them, and medications could be tailored to the needs of the patient and his/her particular manifestation of a condition.
Flash-forward to the present day, and the clinical landscape doesn’t look quite as different as expected. Yes, there have been strides in the identification of genetic components to illnesses. Yes, in many cases, the results of genetic testing may lead patients to make choices that alter their outcomes. But there are still a lot of unknowns, as well as gray areas, when it comes to genetics.
For human beings in general—and Americans in particular—“soon” is never really soon enough. But it might actually be a good thing that genetics is still in the process of revolutionizing the way medicine is practiced. Because the truth is, we may not be fully equipped to handle the reality.
Not Ready for Prime Time
According to GeneTests.org, the National Center for Biotechnology Information's online database, genetic testing is available for 2,978 diseases (the majority are clinical tests, while 233 are for research purposes only). Figure 1 maps the exponential growth in available genetic tests since 1993 (seven years before the Human Genome Project was completed).
Continually, new information becomes available about genes associated with particular illnesses. The difficulty lies in putting it into an appropriate context.
"Many NPs and PAs—and probably primary care docs—don't really have a good understanding of genetics," says Ruth McCaffrey, ND, DNP, ARNP,BC, FNP, GNP, Professor, College of Nursing, Florida Atlantic University. "And therefore, they don't want to bring it up with patients, because they don't know how to help people."
A key aspect—before even delving into the specifics of what genetic testing can offer a particular patient—is managing expectations, both patients' and providers'. Genetics holds a wealth of promise for the future, but that future is not necessarily now. Pharmacogenetics, for example, has not advanced as researchers had hoped; while there are instances in which a medication may be selected based on the patient's genetic make-up (think of Alzheimer's disease), the field has not come to fruition yet.
So having genetic knowledge may not translate to useful action. And that leaves a lot of room for frustration and anxiety.
What Can You Tell Me?
While genetic tests can be used for diagnosis—someone demonstrating features of Down syndrome, for example, might be tested to confirm the presence of an extra copy of chromosome 21—most are performed for predictive purposes. And that has opened up a realm of uncertainty, because many patients—and even some clinicians—do not understand the concept of absolute risk.
The problem has been compounded by the influx of direct-to-consumer (DTC) genetic testing kits. Visit certain Web sites—even the ubiquitous Amazon.com—and you can purchase a kit that provides everything you need to swab the inside of your cheek and send the sample away to a laboratory for analysis. The resultant report will indicate your likelihood of developing certain diseases. (Note: The FDA, among other federal agencies, has questioned the accuracy of some of these kits and whether their marketing claims promise more than they can deliver.) But patients often can't put that information into a proper perspective.
"When I had my DTC genetic testing," Rackover says (he decided he couldn't teach students about it if he didn't experience it for himself), "I received 42 pages of information. And I had to learn to deal with absolute risk. It's basically a communications game of helping people deal with information they don't want to know."
Genetic testing that is ordered, or recommended, by a clinician will have a context to it. The patient will presumably have undergone counseling with a genetics specialist, and/or the primary care provider may have explained to the patient why the testing is beneficial and what information can be gleaned. But when people submit their own samples, they often aren't prepared for the answers they receive.
Even when patients bring their results to a primary care provider, that clinician might not be able to offer much enlightenment if he or she is not comfortable with and knowledgeable about genetics. Even to someone with medical or nursing training, the information can be dense and confusing. In fact, today's situation reminds Rackover of the 1970s, when CT scans and MRIs were making their debut.
"I remember this famous neurosurgeon in Philadelphia telling me, 'This machine is coming from England that is going to revolutionize medicine,'" he recalls. "That was the CT scan. Then when that and the MRI first came out, radiologists didn't know what they were looking at. There was too much information. And what we're getting from all the genetic testing is: The high-level stuff is very good information, but we don't know what it relates to yet."
Dealing With Risk
The usefulness of genetic testing varies by specialty and circumstance. It has perhaps gained the most traction (though not without sociopolitical controversy) in the field of obstetrics. Knowing what genes might be passed to a fetus or what conditions the child is likely to have provides prospective parents with options—whether that means terminating the pregnancy or preparing to raise a child with special needs.
"Certainly if a couple is thinking about becoming pregnant, genetic testing is warranted," McCaffrey says. Screening for Down syndrome is routine in the United States, but she notes, "[The test] is very inaccurate. So we get them all worried and then do amniocentesis. It would be better to do a pre-pregnancy genetic screen than to wait until their fourth month of pregnancy and do the alpha-fetoprotein test."
Another area in which genetic screening is prominent, though plagued by controversy, is breast cancer. Preventive measures are available, but some question whether the current options are too extreme or whether women might regret, say, undergoing prophylactic mastectomy if new treatments become available before their risk would ever reach the highest category.
"That's one end of the spectrum," McCaffrey says. "But if you know you have BRCA2, you might be more vigilant in testing for ovarian cancer. That's the biggest thing we can do, overall—if you have a patient who has the gene for a certain disease, you're going to be much more vigilant at monitoring them."
Again, genetic information has to be put in context. Having a particular gene does occasionally guarantee you will develop a disease (eg, Huntington's disease). But in most cases, it's more of a tip-off that something might happen sometime in the future. Rackover, for example, was told he had an increased risk for Crohn's disease, but since he was already 61 at the time of testing and has never had any symptoms, it wasn't something that especially concerned him. Someone less informed about the concept of risk, however, might have panicked and started demanding treatment for a condition he doesn't have and may never develop.
And then there are cases such as Huntington's disease, for which nothing can be done. A patient who discovers he or she has one of the associated genes might make different life decisions, but there is no prevention plan that can be put into action. This also raises the conundrum of sharing the news with relatives—who may or may not want to know, who may or may not want to consider their own risk. We tend to think of genes as a personal matter, but they're not. We share them with others.
All in the Family (History)
That, according to Rackover, is the heart of the matter—the essential piece that many clinicians overlook. Genetic tests are tools that can assist patients and providers in formulating health care plans. But amidst the buzz that surrounds any advancement in clinical practice, clinicians are losing sight of the fundamentals. The first step doesn't have to be ordering a genetic test. The first step is asking the right questions and listening to the answers.
Family history provides the first clues to a genetic puzzle; it is what can help a provider determine whether genetic testing is warranted. There are instances in which you don't need a genetic test to decide the appropriate course of action; you just need common sense.
Don't believe it? Here's food for thought: Rackover conducts physical exams for the military. One day, he saw a young Korean woman. On her preliminary screening survey, she mentioned having seen a health care provider in the previous year and receiving a prescription for oral contraceptives. There is nothing unusual about that. Except ...
"When I looked at the family history, I saw her mother had a stroke. So I asked, 'How old was your mother?' figuring she was, well, old," Rackover says. "Well, she was 38! And then she told me that both her aunts had a pulmonary embolism."
Thirteen years ago, scientists cracked the human genetic code, opening a world of new possibilities in medical care. At the time, it was (rightfully) trumpeted as a remarkable achievement, a sort of final frontier conquered. Soon, everyone would be able to have their own DNA sequenced, diseases would be identified early enough to prevent them, and medications could be tailored to the needs of the patient and his/her particular manifestation of a condition.
Flash-forward to the present day, and the clinical landscape doesn’t look quite as different as expected. Yes, there have been strides in the identification of genetic components to illnesses. Yes, in many cases, the results of genetic testing may lead patients to make choices that alter their outcomes. But there are still a lot of unknowns, as well as gray areas, when it comes to genetics.
For human beings in general—and Americans in particular—“soon” is never really soon enough. But it might actually be a good thing that genetics is still in the process of revolutionizing the way medicine is practiced. Because the truth is, we may not be fully equipped to handle the reality.
Not Ready for Prime Time
According to GeneTests.org, the National Center for Biotechnology Information's online database, genetic testing is available for 2,978 diseases (the majority are clinical tests, while 233 are for research purposes only). Figure 1 maps the exponential growth in available genetic tests since 1993 (seven years before the Human Genome Project was completed).
Continually, new information becomes available about genes associated with particular illnesses. The difficulty lies in putting it into an appropriate context.
"Many NPs and PAs—and probably primary care docs—don't really have a good understanding of genetics," says Ruth McCaffrey, ND, DNP, ARNP,BC, FNP, GNP, Professor, College of Nursing, Florida Atlantic University. "And therefore, they don't want to bring it up with patients, because they don't know how to help people."
A key aspect—before even delving into the specifics of what genetic testing can offer a particular patient—is managing expectations, both patients' and providers'. Genetics holds a wealth of promise for the future, but that future is not necessarily now. Pharmacogenetics, for example, has not advanced as researchers had hoped; while there are instances in which a medication may be selected based on the patient's genetic make-up (think of Alzheimer's disease), the field has not come to fruition yet.
So having genetic knowledge may not translate to useful action. And that leaves a lot of room for frustration and anxiety.
What Can You Tell Me?
While genetic tests can be used for diagnosis—someone demonstrating features of Down syndrome, for example, might be tested to confirm the presence of an extra copy of chromosome 21—most are performed for predictive purposes. And that has opened up a realm of uncertainty, because many patients—and even some clinicians—do not understand the concept of absolute risk.
The problem has been compounded by the influx of direct-to-consumer (DTC) genetic testing kits. Visit certain Web sites—even the ubiquitous Amazon.com—and you can purchase a kit that provides everything you need to swab the inside of your cheek and send the sample away to a laboratory for analysis. The resultant report will indicate your likelihood of developing certain diseases. (Note: The FDA, among other federal agencies, has questioned the accuracy of some of these kits and whether their marketing claims promise more than they can deliver.) But patients often can't put that information into a proper perspective.
"When I had my DTC genetic testing," Rackover says (he decided he couldn't teach students about it if he didn't experience it for himself), "I received 42 pages of information. And I had to learn to deal with absolute risk. It's basically a communications game of helping people deal with information they don't want to know."
Genetic testing that is ordered, or recommended, by a clinician will have a context to it. The patient will presumably have undergone counseling with a genetics specialist, and/or the primary care provider may have explained to the patient why the testing is beneficial and what information can be gleaned. But when people submit their own samples, they often aren't prepared for the answers they receive.
Even when patients bring their results to a primary care provider, that clinician might not be able to offer much enlightenment if he or she is not comfortable with and knowledgeable about genetics. Even to someone with medical or nursing training, the information can be dense and confusing. In fact, today's situation reminds Rackover of the 1970s, when CT scans and MRIs were making their debut.
"I remember this famous neurosurgeon in Philadelphia telling me, 'This machine is coming from England that is going to revolutionize medicine,'" he recalls. "That was the CT scan. Then when that and the MRI first came out, radiologists didn't know what they were looking at. There was too much information. And what we're getting from all the genetic testing is: The high-level stuff is very good information, but we don't know what it relates to yet."
Dealing With Risk
The usefulness of genetic testing varies by specialty and circumstance. It has perhaps gained the most traction (though not without sociopolitical controversy) in the field of obstetrics. Knowing what genes might be passed to a fetus or what conditions the child is likely to have provides prospective parents with options—whether that means terminating the pregnancy or preparing to raise a child with special needs.
"Certainly if a couple is thinking about becoming pregnant, genetic testing is warranted," McCaffrey says. Screening for Down syndrome is routine in the United States, but she notes, "[The test] is very inaccurate. So we get them all worried and then do amniocentesis. It would be better to do a pre-pregnancy genetic screen than to wait until their fourth month of pregnancy and do the alpha-fetoprotein test."
Another area in which genetic screening is prominent, though plagued by controversy, is breast cancer. Preventive measures are available, but some question whether the current options are too extreme or whether women might regret, say, undergoing prophylactic mastectomy if new treatments become available before their risk would ever reach the highest category.
"That's one end of the spectrum," McCaffrey says. "But if you know you have BRCA2, you might be more vigilant in testing for ovarian cancer. That's the biggest thing we can do, overall—if you have a patient who has the gene for a certain disease, you're going to be much more vigilant at monitoring them."
Again, genetic information has to be put in context. Having a particular gene does occasionally guarantee you will develop a disease (eg, Huntington's disease). But in most cases, it's more of a tip-off that something might happen sometime in the future. Rackover, for example, was told he had an increased risk for Crohn's disease, but since he was already 61 at the time of testing and has never had any symptoms, it wasn't something that especially concerned him. Someone less informed about the concept of risk, however, might have panicked and started demanding treatment for a condition he doesn't have and may never develop.
And then there are cases such as Huntington's disease, for which nothing can be done. A patient who discovers he or she has one of the associated genes might make different life decisions, but there is no prevention plan that can be put into action. This also raises the conundrum of sharing the news with relatives—who may or may not want to know, who may or may not want to consider their own risk. We tend to think of genes as a personal matter, but they're not. We share them with others.
All in the Family (History)
That, according to Rackover, is the heart of the matter—the essential piece that many clinicians overlook. Genetic tests are tools that can assist patients and providers in formulating health care plans. But amidst the buzz that surrounds any advancement in clinical practice, clinicians are losing sight of the fundamentals. The first step doesn't have to be ordering a genetic test. The first step is asking the right questions and listening to the answers.
Family history provides the first clues to a genetic puzzle; it is what can help a provider determine whether genetic testing is warranted. There are instances in which you don't need a genetic test to decide the appropriate course of action; you just need common sense.
Don't believe it? Here's food for thought: Rackover conducts physical exams for the military. One day, he saw a young Korean woman. On her preliminary screening survey, she mentioned having seen a health care provider in the previous year and receiving a prescription for oral contraceptives. There is nothing unusual about that. Except ...
"When I looked at the family history, I saw her mother had a stroke. So I asked, 'How old was your mother?' figuring she was, well, old," Rackover says. "Well, she was 38! And then she told me that both her aunts had a pulmonary embolism."
Thirteen years ago, scientists cracked the human genetic code, opening a world of new possibilities in medical care. At the time, it was (rightfully) trumpeted as a remarkable achievement, a sort of final frontier conquered. Soon, everyone would be able to have their own DNA sequenced, diseases would be identified early enough to prevent them, and medications could be tailored to the needs of the patient and his/her particular manifestation of a condition.
Flash-forward to the present day, and the clinical landscape doesn’t look quite as different as expected. Yes, there have been strides in the identification of genetic components to illnesses. Yes, in many cases, the results of genetic testing may lead patients to make choices that alter their outcomes. But there are still a lot of unknowns, as well as gray areas, when it comes to genetics.
For human beings in general—and Americans in particular—“soon” is never really soon enough. But it might actually be a good thing that genetics is still in the process of revolutionizing the way medicine is practiced. Because the truth is, we may not be fully equipped to handle the reality.
Not Ready for Prime Time
According to GeneTests.org, the National Center for Biotechnology Information's online database, genetic testing is available for 2,978 diseases (the majority are clinical tests, while 233 are for research purposes only). Figure 1 maps the exponential growth in available genetic tests since 1993 (seven years before the Human Genome Project was completed).
Continually, new information becomes available about genes associated with particular illnesses. The difficulty lies in putting it into an appropriate context.
"Many NPs and PAs—and probably primary care docs—don't really have a good understanding of genetics," says Ruth McCaffrey, ND, DNP, ARNP,BC, FNP, GNP, Professor, College of Nursing, Florida Atlantic University. "And therefore, they don't want to bring it up with patients, because they don't know how to help people."
A key aspect—before even delving into the specifics of what genetic testing can offer a particular patient—is managing expectations, both patients' and providers'. Genetics holds a wealth of promise for the future, but that future is not necessarily now. Pharmacogenetics, for example, has not advanced as researchers had hoped; while there are instances in which a medication may be selected based on the patient's genetic make-up (think of Alzheimer's disease), the field has not come to fruition yet.
So having genetic knowledge may not translate to useful action. And that leaves a lot of room for frustration and anxiety.
What Can You Tell Me?
While genetic tests can be used for diagnosis—someone demonstrating features of Down syndrome, for example, might be tested to confirm the presence of an extra copy of chromosome 21—most are performed for predictive purposes. And that has opened up a realm of uncertainty, because many patients—and even some clinicians—do not understand the concept of absolute risk.
The problem has been compounded by the influx of direct-to-consumer (DTC) genetic testing kits. Visit certain Web sites—even the ubiquitous Amazon.com—and you can purchase a kit that provides everything you need to swab the inside of your cheek and send the sample away to a laboratory for analysis. The resultant report will indicate your likelihood of developing certain diseases. (Note: The FDA, among other federal agencies, has questioned the accuracy of some of these kits and whether their marketing claims promise more than they can deliver.) But patients often can't put that information into a proper perspective.
"When I had my DTC genetic testing," Rackover says (he decided he couldn't teach students about it if he didn't experience it for himself), "I received 42 pages of information. And I had to learn to deal with absolute risk. It's basically a communications game of helping people deal with information they don't want to know."
Genetic testing that is ordered, or recommended, by a clinician will have a context to it. The patient will presumably have undergone counseling with a genetics specialist, and/or the primary care provider may have explained to the patient why the testing is beneficial and what information can be gleaned. But when people submit their own samples, they often aren't prepared for the answers they receive.
Even when patients bring their results to a primary care provider, that clinician might not be able to offer much enlightenment if he or she is not comfortable with and knowledgeable about genetics. Even to someone with medical or nursing training, the information can be dense and confusing. In fact, today's situation reminds Rackover of the 1970s, when CT scans and MRIs were making their debut.
"I remember this famous neurosurgeon in Philadelphia telling me, 'This machine is coming from England that is going to revolutionize medicine,'" he recalls. "That was the CT scan. Then when that and the MRI first came out, radiologists didn't know what they were looking at. There was too much information. And what we're getting from all the genetic testing is: The high-level stuff is very good information, but we don't know what it relates to yet."
Dealing With Risk
The usefulness of genetic testing varies by specialty and circumstance. It has perhaps gained the most traction (though not without sociopolitical controversy) in the field of obstetrics. Knowing what genes might be passed to a fetus or what conditions the child is likely to have provides prospective parents with options—whether that means terminating the pregnancy or preparing to raise a child with special needs.
"Certainly if a couple is thinking about becoming pregnant, genetic testing is warranted," McCaffrey says. Screening for Down syndrome is routine in the United States, but she notes, "[The test] is very inaccurate. So we get them all worried and then do amniocentesis. It would be better to do a pre-pregnancy genetic screen than to wait until their fourth month of pregnancy and do the alpha-fetoprotein test."
Another area in which genetic screening is prominent, though plagued by controversy, is breast cancer. Preventive measures are available, but some question whether the current options are too extreme or whether women might regret, say, undergoing prophylactic mastectomy if new treatments become available before their risk would ever reach the highest category.
"That's one end of the spectrum," McCaffrey says. "But if you know you have BRCA2, you might be more vigilant in testing for ovarian cancer. That's the biggest thing we can do, overall—if you have a patient who has the gene for a certain disease, you're going to be much more vigilant at monitoring them."
Again, genetic information has to be put in context. Having a particular gene does occasionally guarantee you will develop a disease (eg, Huntington's disease). But in most cases, it's more of a tip-off that something might happen sometime in the future. Rackover, for example, was told he had an increased risk for Crohn's disease, but since he was already 61 at the time of testing and has never had any symptoms, it wasn't something that especially concerned him. Someone less informed about the concept of risk, however, might have panicked and started demanding treatment for a condition he doesn't have and may never develop.
And then there are cases such as Huntington's disease, for which nothing can be done. A patient who discovers he or she has one of the associated genes might make different life decisions, but there is no prevention plan that can be put into action. This also raises the conundrum of sharing the news with relatives—who may or may not want to know, who may or may not want to consider their own risk. We tend to think of genes as a personal matter, but they're not. We share them with others.
All in the Family (History)
That, according to Rackover, is the heart of the matter—the essential piece that many clinicians overlook. Genetic tests are tools that can assist patients and providers in formulating health care plans. But amidst the buzz that surrounds any advancement in clinical practice, clinicians are losing sight of the fundamentals. The first step doesn't have to be ordering a genetic test. The first step is asking the right questions and listening to the answers.
Family history provides the first clues to a genetic puzzle; it is what can help a provider determine whether genetic testing is warranted. There are instances in which you don't need a genetic test to decide the appropriate course of action; you just need common sense.
Don't believe it? Here's food for thought: Rackover conducts physical exams for the military. One day, he saw a young Korean woman. On her preliminary screening survey, she mentioned having seen a health care provider in the previous year and receiving a prescription for oral contraceptives. There is nothing unusual about that. Except ...
"When I looked at the family history, I saw her mother had a stroke. So I asked, 'How old was your mother?' figuring she was, well, old," Rackover says. "Well, she was 38! And then she told me that both her aunts had a pulmonary embolism."