User login
Optimal gestational age for cell-free DNA sampling in obese women
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
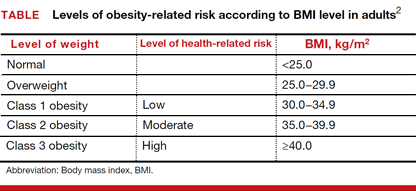
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
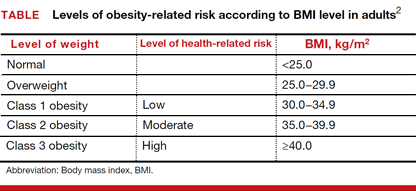
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
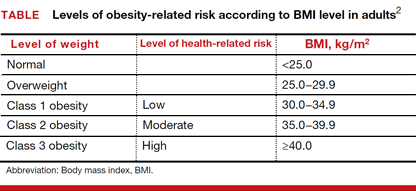
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
ObGyn salaries jumped in the last year
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
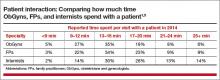
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
In this Article
- ACOG takes aim at burnout
- Considering salary and leadership disparities
- ObGyns’ greatest practice concerns
Trading Kidneys: Innovative Program Could Save Thousands of Lives
While editing this month’s Renal Consult, I noted the mention of “paired kidney exchange” with particular interest. In 2005, I heard about a relatively new concept: matching two or more incompatible kidney donor-recipient pairs to create compatible matches. After conducting some research and interviewing experts, I wrote an article on paired kidney exchange for our sister publication, Clinician News. In the subsequent decade, the concept of paired exchange has expanded to the point that as many as 70 people have participated in a 35-kidney exchange. —AMH
Last year, almost 27,000 Americans received an organ transplant—a new national record, according to the US Department of Health and Human Services. Donations from living persons reached nearly 7,000, an increase of 2.3% from 2003. But despite these positive numbers, nearly 88,000 people are on the waiting list for an organ, and about 6,200 died last year before one became available.
But in some areas of the country, an innovative program is gaining momentum: paired kidney exchange, which puts together two or more incompatible donor-recipient pairs to create compatible matches. And while it will not close the gap between patients in need and those who receive, experts believe it could help thousands of people each year.
The real struggle is finding more willing donors. But Francis Delmonico, MD, Medical Director, New England Organ Bank, Newton, Massachusetts, says paired exchange is “an adjunct. When it can be of help, it’s helped a number of people already. And as with any of this, it’s a lot of work but it’s a tactic that we ought to try and apply anytime we can.”
“There are about 10,000 people who could be put into a program like this,” says Michael A. Rees, MD, PhD, Associate Professor, Department of Urology, Medical College of Ohio, Toledo. “Once you put them into the program, we would hope that 2,000 to 3,000 per year could be matched up and we could do that many extra kidney transplants a year. And that would certainly help to close the gap.”
Continue for how it works >>
HOW IT WORKS
Paired kidney exchange got its start in the US at Johns Hopkins Comprehensive Transplant Center, Baltimore, in 2001. The concept is simple: Recipient A needs a kidney and has a family member or friend, Donor A, who is willing to give. However, testing reveals that Donor A and Recipient A are incompatible. Meanwhile, Recipient B and Donor B find themselves with the same problem. But, it turns out, Donor B could give to Recipient A and Donor A could give to Recipient B. The patients and their donors are approached with the idea of an exchange, and if they agree, two people receive needed organs.
Twenty-two patients have received kidneys through the Johns Hopkins program, according to Robert A. Montgomery, MD, PhD, Director, Incompatible Kidney Transplant Programs (InKTP). Surgeons at Johns Hopkins have also expanded the exchange to three donor-recipient pairs; “triple swap” operations were performed at the hospital in 2003 and 2004.
“Everyone, when they come for an incompatible transplant, is offered the option of a paired exchange, because … if there’s any way to get a compatible kidney, that’s what you try for first,” says Janet Hiller, RN, MSN, Clinical Nurse Specialist, InKTP. “We’ve only had probably two out of a hundred [patients] who have thought, ‘No, I’d rather just get the kidney from my spouse or loved one.’”
“Patients are surprisingly open to this option, and almost all of them … request it when they are initially seen by me,” Montgomery told Clinician News via e-mail. “Some [recipients] have expressed apprehension about not knowing the donor and not being sure they have taken good care of their kidney. The donors have rarely expressed any concerns; they just want their loved one to receive a kidney…. It has universally been a positive experience.”
Ohio’s Rees first heard about paired exchange at a conference in 2001. He returned to his institution and consulted with the living donor coordinator to see if any pairs could be formed from people who had been willing to donate but unable due to blood type or other incompatibility problems. After identifying two pairs (out of 10 possibilities) for whom an exchange might work, Rees brought the patients and donors in for testing. But alas, the match wasn’t quite right.
“It became clear to me that if I really wanted to make this work, I needed a lot more than 10 pairs [to start with],” Rees says. “The numbers—if you try to match up people—go up logarithmically the more pairs that you have. So the chances you have of creating pairs go up exponentially.”
With this realization in mind, Rees set out to find someone willing to write a computer program that could identify potential matches from a larger bank of people pooled from several facilities. After some false starts—no computer programmer would work on the project for academic glory, the only reward Rees could offer—he convinced his father, Alan, to help. The senior Rees’ prototype was the basis for the current system, which links 10 transplant centers in Ohio.
Working with a larger pool of colleagues required numerous teleconference calls to iron out details for the statewide program. Among the questions were, “Are we going to make the donor travel, or are we going to cut the kidney out at home and ship the kidney in a box of ice to the place where it’s going to be transplanted?” he recalls. “And we decided that the donor has to travel.”
The first kidney exchange in the state of Ohio was performed in early November 2004. The third was scheduled for mid-April.
Creating one system to be shared by medical institutions that would normally be competitors took some work. “Trying to get us all to play in the same sandbox was very difficult,” Rees acknowledges. “But we did that; we stuck it out. And we all agreed to come up with something that we all think is a great idea and should help our patients.”
Delmonico, who is also a Professor of Surgery at Harvard Medical School and Visiting Surgeon in the Transplant Unit at Massachusetts General Hospital, Boston, has also seen the gratifying cooperation between medical professionals. “Institutions are competitive in terms of medical care—that’s no mystery,” he says. “But in this instance, the physicians have been simply magnificent in trying to help patients. Innovative programs can be developed and sustained through the kind of collaboration that is going on here.”
The New England paired exchange program, dating back to 2002, is a collaboration involving a dozen hospitals. It started with a paper-and-pen effort (blood type–incompatible patients would be brought to the attention of Delmonico, who would then contact each transplant center, seeking others) but now has its own computer system.
New England also has another variation on the exchange program that is unique to the region, according to Delmonico. “Let’s say I wanted to give to you but I can’t. I’ll give to somebody on the list, and as a result of that donation, you would get a priority for the next available deceased donor kidney in New England,” he explains. “We’ve done that about 20 times now.”
Continue for going national >>
GOING NATIONAL
So where does paired exchange go from here? Johns Hopkins’ Montgomery organized a consensus meeting in March to discuss the possibility of creating a national network; Hiller, Rees, and Delmonico attended.
“I think our goal should be to one day have a national program,” Rees says. “But shipping somebody from Toledo down to Cincinnati is a lot easier to sell to a patient than shipping somebody from Toledo to Los Angeles. And the logistics of trying to do that when you have a whole different set of insurance companies … would be a lot more complicated. So, I think the way to begin is to do it on a more regional basis and prove that the concept works, that people can be satisfied with it, and then begin to expand it.”
Delmonico also thinks a national program is essential. “We need to enlarge the possibility of paired donation and exchange,” he says. “It will not happen successfully in a regional system. There aren’t enough patients that can be identified.” Questions to be answered before such a program could exist, Delmonico notes, include where the system will be based and who will administer it.
“There was a lot of agreement—though not total consensus—on the fact that UNOS, the United Network for Organ Sharing, would be the most likely place to ‘house’ and to manage the data,” Hiller reports. “They have all those systems in place already [and] are capable of managing this large database.”
Delmonico, as Vice President of UNOS, points out, “We have no authority to do that yet. Whether or not the country wants us to do that also remains to be determined.” But the UNOS Board of Directors is open to the idea; last year, they endorsed the concept of establishing a national paired exchange program with the understanding that details would have to be worked out over time, according to a UNOS spokesperson.
Another obstacle to widespread paired donation may be perceptions of it in the eyes of the government and critics: Could it be construed as a violation of the 1984 National Organ Transplant Act, which says that an organ should not be transplanted for a “value consideration”? Legal experts have assured Delmonico that paired exchanges can be interpreted as a gift.
“The government is also, properly, not wanting to see this as a slope toward buying and selling organs,” Delmonico says. “And I am adamantly opposed to that. In the instances that we’ve done paired exchange here, that’s not in the mix. That’s not our motivation, nor has it been the motivation of these donors. We wouldn’t do it if we felt that was the case.”
Montgomery says it will take several years to get a national system set up. But the bottom line for transplant surgeons is that a national paired kidney exchange program would do a world of good, two people at a time. “This is clearly what is best for our patients,” Montgomery says.
“The bigger we can get, if we can spread it nationally, the more people it will help,” Rees says. “And so we have to think of a way to do this so that we’re all satisfied that it’s moving forward in a way that will make everyone happy.”
Reprinted from Clinician News. 2005;9(5):cover, 3, 15.
While editing this month’s Renal Consult, I noted the mention of “paired kidney exchange” with particular interest. In 2005, I heard about a relatively new concept: matching two or more incompatible kidney donor-recipient pairs to create compatible matches. After conducting some research and interviewing experts, I wrote an article on paired kidney exchange for our sister publication, Clinician News. In the subsequent decade, the concept of paired exchange has expanded to the point that as many as 70 people have participated in a 35-kidney exchange. —AMH
Last year, almost 27,000 Americans received an organ transplant—a new national record, according to the US Department of Health and Human Services. Donations from living persons reached nearly 7,000, an increase of 2.3% from 2003. But despite these positive numbers, nearly 88,000 people are on the waiting list for an organ, and about 6,200 died last year before one became available.
But in some areas of the country, an innovative program is gaining momentum: paired kidney exchange, which puts together two or more incompatible donor-recipient pairs to create compatible matches. And while it will not close the gap between patients in need and those who receive, experts believe it could help thousands of people each year.
The real struggle is finding more willing donors. But Francis Delmonico, MD, Medical Director, New England Organ Bank, Newton, Massachusetts, says paired exchange is “an adjunct. When it can be of help, it’s helped a number of people already. And as with any of this, it’s a lot of work but it’s a tactic that we ought to try and apply anytime we can.”
“There are about 10,000 people who could be put into a program like this,” says Michael A. Rees, MD, PhD, Associate Professor, Department of Urology, Medical College of Ohio, Toledo. “Once you put them into the program, we would hope that 2,000 to 3,000 per year could be matched up and we could do that many extra kidney transplants a year. And that would certainly help to close the gap.”
Continue for how it works >>
HOW IT WORKS
Paired kidney exchange got its start in the US at Johns Hopkins Comprehensive Transplant Center, Baltimore, in 2001. The concept is simple: Recipient A needs a kidney and has a family member or friend, Donor A, who is willing to give. However, testing reveals that Donor A and Recipient A are incompatible. Meanwhile, Recipient B and Donor B find themselves with the same problem. But, it turns out, Donor B could give to Recipient A and Donor A could give to Recipient B. The patients and their donors are approached with the idea of an exchange, and if they agree, two people receive needed organs.
Twenty-two patients have received kidneys through the Johns Hopkins program, according to Robert A. Montgomery, MD, PhD, Director, Incompatible Kidney Transplant Programs (InKTP). Surgeons at Johns Hopkins have also expanded the exchange to three donor-recipient pairs; “triple swap” operations were performed at the hospital in 2003 and 2004.
“Everyone, when they come for an incompatible transplant, is offered the option of a paired exchange, because … if there’s any way to get a compatible kidney, that’s what you try for first,” says Janet Hiller, RN, MSN, Clinical Nurse Specialist, InKTP. “We’ve only had probably two out of a hundred [patients] who have thought, ‘No, I’d rather just get the kidney from my spouse or loved one.’”
“Patients are surprisingly open to this option, and almost all of them … request it when they are initially seen by me,” Montgomery told Clinician News via e-mail. “Some [recipients] have expressed apprehension about not knowing the donor and not being sure they have taken good care of their kidney. The donors have rarely expressed any concerns; they just want their loved one to receive a kidney…. It has universally been a positive experience.”
Ohio’s Rees first heard about paired exchange at a conference in 2001. He returned to his institution and consulted with the living donor coordinator to see if any pairs could be formed from people who had been willing to donate but unable due to blood type or other incompatibility problems. After identifying two pairs (out of 10 possibilities) for whom an exchange might work, Rees brought the patients and donors in for testing. But alas, the match wasn’t quite right.
“It became clear to me that if I really wanted to make this work, I needed a lot more than 10 pairs [to start with],” Rees says. “The numbers—if you try to match up people—go up logarithmically the more pairs that you have. So the chances you have of creating pairs go up exponentially.”
With this realization in mind, Rees set out to find someone willing to write a computer program that could identify potential matches from a larger bank of people pooled from several facilities. After some false starts—no computer programmer would work on the project for academic glory, the only reward Rees could offer—he convinced his father, Alan, to help. The senior Rees’ prototype was the basis for the current system, which links 10 transplant centers in Ohio.
Working with a larger pool of colleagues required numerous teleconference calls to iron out details for the statewide program. Among the questions were, “Are we going to make the donor travel, or are we going to cut the kidney out at home and ship the kidney in a box of ice to the place where it’s going to be transplanted?” he recalls. “And we decided that the donor has to travel.”
The first kidney exchange in the state of Ohio was performed in early November 2004. The third was scheduled for mid-April.
Creating one system to be shared by medical institutions that would normally be competitors took some work. “Trying to get us all to play in the same sandbox was very difficult,” Rees acknowledges. “But we did that; we stuck it out. And we all agreed to come up with something that we all think is a great idea and should help our patients.”
Delmonico, who is also a Professor of Surgery at Harvard Medical School and Visiting Surgeon in the Transplant Unit at Massachusetts General Hospital, Boston, has also seen the gratifying cooperation between medical professionals. “Institutions are competitive in terms of medical care—that’s no mystery,” he says. “But in this instance, the physicians have been simply magnificent in trying to help patients. Innovative programs can be developed and sustained through the kind of collaboration that is going on here.”
The New England paired exchange program, dating back to 2002, is a collaboration involving a dozen hospitals. It started with a paper-and-pen effort (blood type–incompatible patients would be brought to the attention of Delmonico, who would then contact each transplant center, seeking others) but now has its own computer system.
New England also has another variation on the exchange program that is unique to the region, according to Delmonico. “Let’s say I wanted to give to you but I can’t. I’ll give to somebody on the list, and as a result of that donation, you would get a priority for the next available deceased donor kidney in New England,” he explains. “We’ve done that about 20 times now.”
Continue for going national >>
GOING NATIONAL
So where does paired exchange go from here? Johns Hopkins’ Montgomery organized a consensus meeting in March to discuss the possibility of creating a national network; Hiller, Rees, and Delmonico attended.
“I think our goal should be to one day have a national program,” Rees says. “But shipping somebody from Toledo down to Cincinnati is a lot easier to sell to a patient than shipping somebody from Toledo to Los Angeles. And the logistics of trying to do that when you have a whole different set of insurance companies … would be a lot more complicated. So, I think the way to begin is to do it on a more regional basis and prove that the concept works, that people can be satisfied with it, and then begin to expand it.”
Delmonico also thinks a national program is essential. “We need to enlarge the possibility of paired donation and exchange,” he says. “It will not happen successfully in a regional system. There aren’t enough patients that can be identified.” Questions to be answered before such a program could exist, Delmonico notes, include where the system will be based and who will administer it.
“There was a lot of agreement—though not total consensus—on the fact that UNOS, the United Network for Organ Sharing, would be the most likely place to ‘house’ and to manage the data,” Hiller reports. “They have all those systems in place already [and] are capable of managing this large database.”
Delmonico, as Vice President of UNOS, points out, “We have no authority to do that yet. Whether or not the country wants us to do that also remains to be determined.” But the UNOS Board of Directors is open to the idea; last year, they endorsed the concept of establishing a national paired exchange program with the understanding that details would have to be worked out over time, according to a UNOS spokesperson.
Another obstacle to widespread paired donation may be perceptions of it in the eyes of the government and critics: Could it be construed as a violation of the 1984 National Organ Transplant Act, which says that an organ should not be transplanted for a “value consideration”? Legal experts have assured Delmonico that paired exchanges can be interpreted as a gift.
“The government is also, properly, not wanting to see this as a slope toward buying and selling organs,” Delmonico says. “And I am adamantly opposed to that. In the instances that we’ve done paired exchange here, that’s not in the mix. That’s not our motivation, nor has it been the motivation of these donors. We wouldn’t do it if we felt that was the case.”
Montgomery says it will take several years to get a national system set up. But the bottom line for transplant surgeons is that a national paired kidney exchange program would do a world of good, two people at a time. “This is clearly what is best for our patients,” Montgomery says.
“The bigger we can get, if we can spread it nationally, the more people it will help,” Rees says. “And so we have to think of a way to do this so that we’re all satisfied that it’s moving forward in a way that will make everyone happy.”
Reprinted from Clinician News. 2005;9(5):cover, 3, 15.
While editing this month’s Renal Consult, I noted the mention of “paired kidney exchange” with particular interest. In 2005, I heard about a relatively new concept: matching two or more incompatible kidney donor-recipient pairs to create compatible matches. After conducting some research and interviewing experts, I wrote an article on paired kidney exchange for our sister publication, Clinician News. In the subsequent decade, the concept of paired exchange has expanded to the point that as many as 70 people have participated in a 35-kidney exchange. —AMH
Last year, almost 27,000 Americans received an organ transplant—a new national record, according to the US Department of Health and Human Services. Donations from living persons reached nearly 7,000, an increase of 2.3% from 2003. But despite these positive numbers, nearly 88,000 people are on the waiting list for an organ, and about 6,200 died last year before one became available.
But in some areas of the country, an innovative program is gaining momentum: paired kidney exchange, which puts together two or more incompatible donor-recipient pairs to create compatible matches. And while it will not close the gap between patients in need and those who receive, experts believe it could help thousands of people each year.
The real struggle is finding more willing donors. But Francis Delmonico, MD, Medical Director, New England Organ Bank, Newton, Massachusetts, says paired exchange is “an adjunct. When it can be of help, it’s helped a number of people already. And as with any of this, it’s a lot of work but it’s a tactic that we ought to try and apply anytime we can.”
“There are about 10,000 people who could be put into a program like this,” says Michael A. Rees, MD, PhD, Associate Professor, Department of Urology, Medical College of Ohio, Toledo. “Once you put them into the program, we would hope that 2,000 to 3,000 per year could be matched up and we could do that many extra kidney transplants a year. And that would certainly help to close the gap.”
Continue for how it works >>
HOW IT WORKS
Paired kidney exchange got its start in the US at Johns Hopkins Comprehensive Transplant Center, Baltimore, in 2001. The concept is simple: Recipient A needs a kidney and has a family member or friend, Donor A, who is willing to give. However, testing reveals that Donor A and Recipient A are incompatible. Meanwhile, Recipient B and Donor B find themselves with the same problem. But, it turns out, Donor B could give to Recipient A and Donor A could give to Recipient B. The patients and their donors are approached with the idea of an exchange, and if they agree, two people receive needed organs.
Twenty-two patients have received kidneys through the Johns Hopkins program, according to Robert A. Montgomery, MD, PhD, Director, Incompatible Kidney Transplant Programs (InKTP). Surgeons at Johns Hopkins have also expanded the exchange to three donor-recipient pairs; “triple swap” operations were performed at the hospital in 2003 and 2004.
“Everyone, when they come for an incompatible transplant, is offered the option of a paired exchange, because … if there’s any way to get a compatible kidney, that’s what you try for first,” says Janet Hiller, RN, MSN, Clinical Nurse Specialist, InKTP. “We’ve only had probably two out of a hundred [patients] who have thought, ‘No, I’d rather just get the kidney from my spouse or loved one.’”
“Patients are surprisingly open to this option, and almost all of them … request it when they are initially seen by me,” Montgomery told Clinician News via e-mail. “Some [recipients] have expressed apprehension about not knowing the donor and not being sure they have taken good care of their kidney. The donors have rarely expressed any concerns; they just want their loved one to receive a kidney…. It has universally been a positive experience.”
Ohio’s Rees first heard about paired exchange at a conference in 2001. He returned to his institution and consulted with the living donor coordinator to see if any pairs could be formed from people who had been willing to donate but unable due to blood type or other incompatibility problems. After identifying two pairs (out of 10 possibilities) for whom an exchange might work, Rees brought the patients and donors in for testing. But alas, the match wasn’t quite right.
“It became clear to me that if I really wanted to make this work, I needed a lot more than 10 pairs [to start with],” Rees says. “The numbers—if you try to match up people—go up logarithmically the more pairs that you have. So the chances you have of creating pairs go up exponentially.”
With this realization in mind, Rees set out to find someone willing to write a computer program that could identify potential matches from a larger bank of people pooled from several facilities. After some false starts—no computer programmer would work on the project for academic glory, the only reward Rees could offer—he convinced his father, Alan, to help. The senior Rees’ prototype was the basis for the current system, which links 10 transplant centers in Ohio.
Working with a larger pool of colleagues required numerous teleconference calls to iron out details for the statewide program. Among the questions were, “Are we going to make the donor travel, or are we going to cut the kidney out at home and ship the kidney in a box of ice to the place where it’s going to be transplanted?” he recalls. “And we decided that the donor has to travel.”
The first kidney exchange in the state of Ohio was performed in early November 2004. The third was scheduled for mid-April.
Creating one system to be shared by medical institutions that would normally be competitors took some work. “Trying to get us all to play in the same sandbox was very difficult,” Rees acknowledges. “But we did that; we stuck it out. And we all agreed to come up with something that we all think is a great idea and should help our patients.”
Delmonico, who is also a Professor of Surgery at Harvard Medical School and Visiting Surgeon in the Transplant Unit at Massachusetts General Hospital, Boston, has also seen the gratifying cooperation between medical professionals. “Institutions are competitive in terms of medical care—that’s no mystery,” he says. “But in this instance, the physicians have been simply magnificent in trying to help patients. Innovative programs can be developed and sustained through the kind of collaboration that is going on here.”
The New England paired exchange program, dating back to 2002, is a collaboration involving a dozen hospitals. It started with a paper-and-pen effort (blood type–incompatible patients would be brought to the attention of Delmonico, who would then contact each transplant center, seeking others) but now has its own computer system.
New England also has another variation on the exchange program that is unique to the region, according to Delmonico. “Let’s say I wanted to give to you but I can’t. I’ll give to somebody on the list, and as a result of that donation, you would get a priority for the next available deceased donor kidney in New England,” he explains. “We’ve done that about 20 times now.”
Continue for going national >>
GOING NATIONAL
So where does paired exchange go from here? Johns Hopkins’ Montgomery organized a consensus meeting in March to discuss the possibility of creating a national network; Hiller, Rees, and Delmonico attended.
“I think our goal should be to one day have a national program,” Rees says. “But shipping somebody from Toledo down to Cincinnati is a lot easier to sell to a patient than shipping somebody from Toledo to Los Angeles. And the logistics of trying to do that when you have a whole different set of insurance companies … would be a lot more complicated. So, I think the way to begin is to do it on a more regional basis and prove that the concept works, that people can be satisfied with it, and then begin to expand it.”
Delmonico also thinks a national program is essential. “We need to enlarge the possibility of paired donation and exchange,” he says. “It will not happen successfully in a regional system. There aren’t enough patients that can be identified.” Questions to be answered before such a program could exist, Delmonico notes, include where the system will be based and who will administer it.
“There was a lot of agreement—though not total consensus—on the fact that UNOS, the United Network for Organ Sharing, would be the most likely place to ‘house’ and to manage the data,” Hiller reports. “They have all those systems in place already [and] are capable of managing this large database.”
Delmonico, as Vice President of UNOS, points out, “We have no authority to do that yet. Whether or not the country wants us to do that also remains to be determined.” But the UNOS Board of Directors is open to the idea; last year, they endorsed the concept of establishing a national paired exchange program with the understanding that details would have to be worked out over time, according to a UNOS spokesperson.
Another obstacle to widespread paired donation may be perceptions of it in the eyes of the government and critics: Could it be construed as a violation of the 1984 National Organ Transplant Act, which says that an organ should not be transplanted for a “value consideration”? Legal experts have assured Delmonico that paired exchanges can be interpreted as a gift.
“The government is also, properly, not wanting to see this as a slope toward buying and selling organs,” Delmonico says. “And I am adamantly opposed to that. In the instances that we’ve done paired exchange here, that’s not in the mix. That’s not our motivation, nor has it been the motivation of these donors. We wouldn’t do it if we felt that was the case.”
Montgomery says it will take several years to get a national system set up. But the bottom line for transplant surgeons is that a national paired kidney exchange program would do a world of good, two people at a time. “This is clearly what is best for our patients,” Montgomery says.
“The bigger we can get, if we can spread it nationally, the more people it will help,” Rees says. “And so we have to think of a way to do this so that we’re all satisfied that it’s moving forward in a way that will make everyone happy.”
Reprinted from Clinician News. 2005;9(5):cover, 3, 15.
HIV: Still Epidemic After 30 Years
December 1st is World AIDS Day. This article, from June 2012, was inspired by a conversation I had with a friend who was pursuing her Masters in Public Health. For a group project in epidemiology, she had tested a survey mechanism among college undergrads—a disturbing number of whom responded that they did not understand what “HIV” meant. We began ruminating on how “young people” (not substantially younger than ourselves) could be so clueless about a disease that had had such a devastating impact within recent memory. My question: Would this lack of awareness eventually result in a resurgence of a disease that, in truth, has never really gone away? —AMH
In the 30 years since the first cases of HIV were diagnosed in the United States, almost 620,000 people have died of AIDS in this country. In a very short period in the early 1980s, HIV morphed from completely unknown to epidemic in its scope; at one point, an estimated 130,000 new infections occurred each year in the US.
Today, that number has decreased substantially, to about 50,000 new infections per year. (Data from 2000 indicated the annual rate of new infections was 56,300, while CDC surveillance data from 46 reporting states in 2010 put the number at around 47,000.) In addition, the development and use of highly effective antiretroviral therapy has meant that people with HIV can live longer, healthier lives—provided, of course, that they have access to and comply with treatment.
Despite these improvements, however, is it acceptable that 1.2 million people in the US are living with HIV (20% of whom don’t even know it)? “No, that number is certainly not satisfactory,” says Folusho E. Ogunfiditimi, MPH, PA-C, Director of Advanced Practice Providers at Henry Ford Health System in Detroit and a member of the American Academy of Physician Assistants Clinical and Health Affairs Commission. “We cannot take our foot off the pedal regarding education, prevention, looking at outcomes, and also looking at the impact of disparities and trying to eliminate those disparities.”
Continue for what HIV is >>
OMG, WHAT'S HIV?
It is possible that American success at reducing (though hardly eliminating) the spread of HIV has actually undermined awareness. It sometimes seems to be a national characteristic that if we don’t see people dying in droves before our very eyes, we don’t think there’s a problem. A Kaiser Family Foundation survey conducted in 2009 revealed that just 6% of Americans considered HIV/AIDS to be “the most urgent health problem facing the nation,” down from a high of 44% in 1995.
In the 1980s and early 1990s, HIV and AIDS were hot topics in the news; it was impossible not to hear tales of horror or fear on a daily basis. While the reduction in misinformation dissemination is probably a positive, the Kaiser survey indicated that only 45% of Americans reported hearing, seeing, or reading “a lot” or “some” about the domestic problem of HIV/AIDS in the previous year. This might not be deeply concerning—there are, after all, plenty of other issues to discuss—until you realize that 62% of Americans consider the media to be their prime source of information about HIV/AIDS (compared with just 13% who say their health care provider is).
While awareness is an issue across demographic groups, the most potentially concerning is younger adults. This is a generation who most likely cannot tell you who Ryan White was and whose members were not alive during (or were far too young to remember) the major crisis of the HIV/AIDS epidemic.
“Sexually, they’ve grown up in an era where we have really good treatments,” says Susan LeLacheur, DrPH, PA-C, Associate Professor of Physician Assistant Studies at the George Washington University in Washington, DC, and a national lecturer on infectious disease and HIV infection. “When they meet people with HIV, those people are healthy.”
“Because we have, for lack of a better term, taken our foot off the pedal regarding HIV/AIDS awareness,” says Ogunfiditimi, “we run the risk of having people coming out of high school and into college not being as aware as we might have been in that age-group in the ’80s and early ’90s.”
In the Kaiser survey, 45% of respondents ages 18 to 29 indicated they had never been tested for HIV. Of those, 70% gave as a reason “you don’t think you’re at risk” and 33%, “your doctor never recommended it.”
In 2008, the CDC estimated that 25% of new HIV infections occur among adolescents and young adults (ie, those ages 13 to 29). This is part of the reason Ogunfiditimi says a renewed focus on education is essential; he also thinks PAs and NPs are well suited to provide that information, given their reputation as patient educators and their frequent work at the community level.
“We need to take this message back to those [age-]groups, back to those communities and schools,” he says, “and conduct health education seminars and HIV/AIDS awareness programs in the schools so that we can start to educate our younger ones.”
Continue for targeted or universal screening? >>
TARGETED OR UNIVERSAL SCREENING?
Under the direction of President Obama, who has said the US “is at a crossroads” in terms of HIV/AIDS, facing “a domestic epidemic that demands a renewed commitment, increased public attention, and leadership,” the White House Office of National AIDS Policy (ONAP) has set ambitious goals for HIV prevention. Outlined in the National HIV/AIDS Strategy for the United States, those goals—with a deadline of 2015—include:
• Decrease the annual new HIV infection rate by 25%.
• Decrease the HIV transmission rate (currently 5 persons infected per year per 100 people living with HIV) by 30%.
• Increase the number of people living with HIV who know of their infection from 79% to 90%.
• Increase the number of people with newly diagnosed HIV who have regular health care within three months from 65% to 85%.
The strategy (available at www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf) was commissioned and developed in response to concern that without bold action, “we face a new era of rising infections, greater challenges in serving people living with HIV, and higher health care costs,” as stated in the executive summary of the report.
It may not help the cause that health care providers receive seemingly mixed messages about how to approach HIV screening. Since 2006, the CDC has recommended routine screening for HIV, stating that “HIV screening is recommended for patients in all health-care settings after the patient is notified that testing will be performed unless the patient declines (opt-out screening).” The CDC expressly recommended that separate written consent and prevention counseling should not be required, in part as an acknowledgement that busy practicing clinicians who have to screen for a multitude of conditions and often provide acute care during an office visit are under time constraints.
“That doesn’t mean you don’t do any counseling at all,” says Julie G. Stewart, DNP, MPH, MSN, FNP, Assistant Professor and Coordinator of the FNP Program at Sacred Heart University and an HIV NP at Southwest Community Health Center in Bridgeport, Connecticut, “but having discussions with your patients about their life and their health and their risk factors in every facet should include HIV testing.”
At the same time, both the CDC and ONAP emphasize that certain populations are at higher risk for HIV infection and therefore need to be targeted. These include:
• Gay, bisexual, and other men who have sex with men: 2% of the US population but 61% of new infections (2009 data)
• Black men and women: 14% of the population but 44% of new HIV infections
• Hispanic and Latino persons: 16% of the population but 20% of new HIV infections
• Injection-drug users: 9% of new HIV infections
The CDC also reports that heterosexual persons account for 27% of new HIV infections.
In a tough economic climate, when the US investment in response to the domestic HIV epidemic has risen to more than $19 billion per year, it makes sense to strategize how to most effectively utilize available resources to reduce disease burden. But do we run the risk of missing cases because we make too many assumptions about who is or is not likely to have this infection?
“The information that has been pushed out there has really tried to focus on these high-risk groups—and yes, we understand that those groups need to be identified,” says Ogunfiditimi. “But when you’re trying to increase the amount of testing, then the message needs to be more general so that practitioners who have natural biases won’t implement those biases into their decision as to whether to test someone.”
“What worries me is that the recommendation has been to test everyone at least once, and then again as indicated,” says LeLacheur. “‘As indicated’ means you have to ask. In parts of the country where HIV is not as prevalent as it is in DC, I can understand how it falls off the radar. But there are still a few [cases]—maybe not one in 20, maybe more like one or two in a clinician’s lifetime—and there is just no telling from the outside.”
“Perception of risk is huge,” adds Stewart. Her state was one of the first to mandate prenatal HIV testing, and she recalls instances in which a woman tested positive and the clinician was shocked because, Stewart says, “the perception was that ‘She is not at any risk at all,’ based on where she lives and her background. But the clinician didn’t really know.”
LeLacheur also points out that assumptions work both ways: “Oh, he’s a nice boy” and “Oh, he’s not a nice boy.” In one of her classes, a gay male student shared his experience seeking a diagnosis for what turned out to be Crohn’s disease. “The minute he told his clinician he was gay, all of a sudden he had AIDS and the clinician wouldn’t look anywhere else,” LeLacheur reports. “And that just wasn’t an issue; this was a kid who had been raised in an era of safer sex and had been very careful.”
Advocates say that implementing universal screening, per the CDC’s recommendation, would not only capture more cases but would also reduce the stigma associated with targeted screening.
Continue for truths and consequences >>
TRUTHS AND CONSEQUENCES
So perceptions and assumptions play important roles in how the US addresses HIV testing—both the perceptions of some patients that they are not at risk or that having HIV isn’t a big deal anymore, and the assumptions by health care providers that they don’t need to screen all patients for HIV. That faulty logic can have dire consequences, even if HIV is no longer an automatic death sentence.
“I think there’s a lot of passive testing, a lot of disease-induced or behavior-induced testing,” Ogunfiditimi says. “A patient comes in with complaints of what sounds like a sexually transmitted infection and that may spur a provider to initiate the discussion around HIV and subsequently do testing to back that up. But I don’t get the sense that HIV testing is promoted significantly.”
“They get sick” is how Stewart says many people learn their HIV status. “That is still frequently the way people become aware of their illness—they are sick in the hospital with an opportunistic infection…. If we can identify people who are HIV-infected earlier, we can capture them at higher CD4 counts, and then they have an improved life expectancy. We can start treatment, and that also impacts transmission.”
Echoing Stewart’s comments, LeLacheur also notes that the major pneumonia or other infection that leads to hospitalization and diagnosis of HIV can cause permanent damage. “I have a couple of patients who appear to be poststroke because of a viral infection in their brains that people get very late in HIV,” she says. “Now, their viral loads are undetectable and their CD4s are very high. Their immune systems are in good shape, and in every other way they’re healthy. But they can’t walk.”
For those misguided patients who think HIV isn’t such a big deal these days, LeLacheur has some hard facts clinicians can share. “You don’t realize until after you have HIV and someone explains it to you that the minute you get it, it essentially knocks out the entire immune system in your intestinal tract—which is more than half of your immune system—and that’s never coming back,” she says. “That infection in the gut is never going away; the medicines don’t touch it. So your digestion will never be right. There are things we can’t fix about HIV.”
And heaven help the patient who tries to rationalize that “you just take one pill a day.” First of all, that one pill ties up your liver, as LeLacheur points out, and second of all, HIV medications cost about $16,000 a year. Not many people can afford that on their own, and some states have 700-person-long waiting lists for assistance programs.
The consensus among clinicians who treat HIV-infected patients is that, yes, the US is much better off than it was at the height of the crisis. But there is still enough disease, still enough devastation, to warrant continued vigilance. And that starts with talking to all patients about HIV.
Ask the questions, they advise, do the test, and be prepared to refer patients to a specialist who can help them manage their illness. But don’t drop the ball on those patients even when they have specialty care; study up on drug interactions and know what you are prescribing to patients taking antiretroviral therapy.
“As PAs and NPs, we absolutely have to be the ones carrying that banner up front,” Ogunfiditimi says. “We’re the ones who have that opportunity to spend time with those patients and make sure we walk them through the urgency and the importance of being aware that this disease is still very rampant in our communities. I don’t want to say that we have taken it for granted, but we have definitely not paid as much attention as we used to in the ’80s and the ’90s, and we need to get back to that.”
“We can never forget,” Stewart concludes. “We spend a lot of time learning about and testing for breast cancer, prostate cancer, diabetes, and hypertension, all in an effort to take care of our patients the best we can. Screening for HIV should be in that same category.”
Reprinted from Clinician Reviews. 2012;22(6):cover, 11-14, 33-35.
December 1st is World AIDS Day. This article, from June 2012, was inspired by a conversation I had with a friend who was pursuing her Masters in Public Health. For a group project in epidemiology, she had tested a survey mechanism among college undergrads—a disturbing number of whom responded that they did not understand what “HIV” meant. We began ruminating on how “young people” (not substantially younger than ourselves) could be so clueless about a disease that had had such a devastating impact within recent memory. My question: Would this lack of awareness eventually result in a resurgence of a disease that, in truth, has never really gone away? —AMH
In the 30 years since the first cases of HIV were diagnosed in the United States, almost 620,000 people have died of AIDS in this country. In a very short period in the early 1980s, HIV morphed from completely unknown to epidemic in its scope; at one point, an estimated 130,000 new infections occurred each year in the US.
Today, that number has decreased substantially, to about 50,000 new infections per year. (Data from 2000 indicated the annual rate of new infections was 56,300, while CDC surveillance data from 46 reporting states in 2010 put the number at around 47,000.) In addition, the development and use of highly effective antiretroviral therapy has meant that people with HIV can live longer, healthier lives—provided, of course, that they have access to and comply with treatment.
Despite these improvements, however, is it acceptable that 1.2 million people in the US are living with HIV (20% of whom don’t even know it)? “No, that number is certainly not satisfactory,” says Folusho E. Ogunfiditimi, MPH, PA-C, Director of Advanced Practice Providers at Henry Ford Health System in Detroit and a member of the American Academy of Physician Assistants Clinical and Health Affairs Commission. “We cannot take our foot off the pedal regarding education, prevention, looking at outcomes, and also looking at the impact of disparities and trying to eliminate those disparities.”
Continue for what HIV is >>
OMG, WHAT'S HIV?
It is possible that American success at reducing (though hardly eliminating) the spread of HIV has actually undermined awareness. It sometimes seems to be a national characteristic that if we don’t see people dying in droves before our very eyes, we don’t think there’s a problem. A Kaiser Family Foundation survey conducted in 2009 revealed that just 6% of Americans considered HIV/AIDS to be “the most urgent health problem facing the nation,” down from a high of 44% in 1995.
In the 1980s and early 1990s, HIV and AIDS were hot topics in the news; it was impossible not to hear tales of horror or fear on a daily basis. While the reduction in misinformation dissemination is probably a positive, the Kaiser survey indicated that only 45% of Americans reported hearing, seeing, or reading “a lot” or “some” about the domestic problem of HIV/AIDS in the previous year. This might not be deeply concerning—there are, after all, plenty of other issues to discuss—until you realize that 62% of Americans consider the media to be their prime source of information about HIV/AIDS (compared with just 13% who say their health care provider is).
While awareness is an issue across demographic groups, the most potentially concerning is younger adults. This is a generation who most likely cannot tell you who Ryan White was and whose members were not alive during (or were far too young to remember) the major crisis of the HIV/AIDS epidemic.
“Sexually, they’ve grown up in an era where we have really good treatments,” says Susan LeLacheur, DrPH, PA-C, Associate Professor of Physician Assistant Studies at the George Washington University in Washington, DC, and a national lecturer on infectious disease and HIV infection. “When they meet people with HIV, those people are healthy.”
“Because we have, for lack of a better term, taken our foot off the pedal regarding HIV/AIDS awareness,” says Ogunfiditimi, “we run the risk of having people coming out of high school and into college not being as aware as we might have been in that age-group in the ’80s and early ’90s.”
In the Kaiser survey, 45% of respondents ages 18 to 29 indicated they had never been tested for HIV. Of those, 70% gave as a reason “you don’t think you’re at risk” and 33%, “your doctor never recommended it.”
In 2008, the CDC estimated that 25% of new HIV infections occur among adolescents and young adults (ie, those ages 13 to 29). This is part of the reason Ogunfiditimi says a renewed focus on education is essential; he also thinks PAs and NPs are well suited to provide that information, given their reputation as patient educators and their frequent work at the community level.
“We need to take this message back to those [age-]groups, back to those communities and schools,” he says, “and conduct health education seminars and HIV/AIDS awareness programs in the schools so that we can start to educate our younger ones.”
Continue for targeted or universal screening? >>
TARGETED OR UNIVERSAL SCREENING?
Under the direction of President Obama, who has said the US “is at a crossroads” in terms of HIV/AIDS, facing “a domestic epidemic that demands a renewed commitment, increased public attention, and leadership,” the White House Office of National AIDS Policy (ONAP) has set ambitious goals for HIV prevention. Outlined in the National HIV/AIDS Strategy for the United States, those goals—with a deadline of 2015—include:
• Decrease the annual new HIV infection rate by 25%.
• Decrease the HIV transmission rate (currently 5 persons infected per year per 100 people living with HIV) by 30%.
• Increase the number of people living with HIV who know of their infection from 79% to 90%.
• Increase the number of people with newly diagnosed HIV who have regular health care within three months from 65% to 85%.
The strategy (available at www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf) was commissioned and developed in response to concern that without bold action, “we face a new era of rising infections, greater challenges in serving people living with HIV, and higher health care costs,” as stated in the executive summary of the report.
It may not help the cause that health care providers receive seemingly mixed messages about how to approach HIV screening. Since 2006, the CDC has recommended routine screening for HIV, stating that “HIV screening is recommended for patients in all health-care settings after the patient is notified that testing will be performed unless the patient declines (opt-out screening).” The CDC expressly recommended that separate written consent and prevention counseling should not be required, in part as an acknowledgement that busy practicing clinicians who have to screen for a multitude of conditions and often provide acute care during an office visit are under time constraints.
“That doesn’t mean you don’t do any counseling at all,” says Julie G. Stewart, DNP, MPH, MSN, FNP, Assistant Professor and Coordinator of the FNP Program at Sacred Heart University and an HIV NP at Southwest Community Health Center in Bridgeport, Connecticut, “but having discussions with your patients about their life and their health and their risk factors in every facet should include HIV testing.”
At the same time, both the CDC and ONAP emphasize that certain populations are at higher risk for HIV infection and therefore need to be targeted. These include:
• Gay, bisexual, and other men who have sex with men: 2% of the US population but 61% of new infections (2009 data)
• Black men and women: 14% of the population but 44% of new HIV infections
• Hispanic and Latino persons: 16% of the population but 20% of new HIV infections
• Injection-drug users: 9% of new HIV infections
The CDC also reports that heterosexual persons account for 27% of new HIV infections.
In a tough economic climate, when the US investment in response to the domestic HIV epidemic has risen to more than $19 billion per year, it makes sense to strategize how to most effectively utilize available resources to reduce disease burden. But do we run the risk of missing cases because we make too many assumptions about who is or is not likely to have this infection?
“The information that has been pushed out there has really tried to focus on these high-risk groups—and yes, we understand that those groups need to be identified,” says Ogunfiditimi. “But when you’re trying to increase the amount of testing, then the message needs to be more general so that practitioners who have natural biases won’t implement those biases into their decision as to whether to test someone.”
“What worries me is that the recommendation has been to test everyone at least once, and then again as indicated,” says LeLacheur. “‘As indicated’ means you have to ask. In parts of the country where HIV is not as prevalent as it is in DC, I can understand how it falls off the radar. But there are still a few [cases]—maybe not one in 20, maybe more like one or two in a clinician’s lifetime—and there is just no telling from the outside.”
“Perception of risk is huge,” adds Stewart. Her state was one of the first to mandate prenatal HIV testing, and she recalls instances in which a woman tested positive and the clinician was shocked because, Stewart says, “the perception was that ‘She is not at any risk at all,’ based on where she lives and her background. But the clinician didn’t really know.”
LeLacheur also points out that assumptions work both ways: “Oh, he’s a nice boy” and “Oh, he’s not a nice boy.” In one of her classes, a gay male student shared his experience seeking a diagnosis for what turned out to be Crohn’s disease. “The minute he told his clinician he was gay, all of a sudden he had AIDS and the clinician wouldn’t look anywhere else,” LeLacheur reports. “And that just wasn’t an issue; this was a kid who had been raised in an era of safer sex and had been very careful.”
Advocates say that implementing universal screening, per the CDC’s recommendation, would not only capture more cases but would also reduce the stigma associated with targeted screening.
Continue for truths and consequences >>
TRUTHS AND CONSEQUENCES
So perceptions and assumptions play important roles in how the US addresses HIV testing—both the perceptions of some patients that they are not at risk or that having HIV isn’t a big deal anymore, and the assumptions by health care providers that they don’t need to screen all patients for HIV. That faulty logic can have dire consequences, even if HIV is no longer an automatic death sentence.
“I think there’s a lot of passive testing, a lot of disease-induced or behavior-induced testing,” Ogunfiditimi says. “A patient comes in with complaints of what sounds like a sexually transmitted infection and that may spur a provider to initiate the discussion around HIV and subsequently do testing to back that up. But I don’t get the sense that HIV testing is promoted significantly.”
“They get sick” is how Stewart says many people learn their HIV status. “That is still frequently the way people become aware of their illness—they are sick in the hospital with an opportunistic infection…. If we can identify people who are HIV-infected earlier, we can capture them at higher CD4 counts, and then they have an improved life expectancy. We can start treatment, and that also impacts transmission.”
Echoing Stewart’s comments, LeLacheur also notes that the major pneumonia or other infection that leads to hospitalization and diagnosis of HIV can cause permanent damage. “I have a couple of patients who appear to be poststroke because of a viral infection in their brains that people get very late in HIV,” she says. “Now, their viral loads are undetectable and their CD4s are very high. Their immune systems are in good shape, and in every other way they’re healthy. But they can’t walk.”
For those misguided patients who think HIV isn’t such a big deal these days, LeLacheur has some hard facts clinicians can share. “You don’t realize until after you have HIV and someone explains it to you that the minute you get it, it essentially knocks out the entire immune system in your intestinal tract—which is more than half of your immune system—and that’s never coming back,” she says. “That infection in the gut is never going away; the medicines don’t touch it. So your digestion will never be right. There are things we can’t fix about HIV.”
And heaven help the patient who tries to rationalize that “you just take one pill a day.” First of all, that one pill ties up your liver, as LeLacheur points out, and second of all, HIV medications cost about $16,000 a year. Not many people can afford that on their own, and some states have 700-person-long waiting lists for assistance programs.
The consensus among clinicians who treat HIV-infected patients is that, yes, the US is much better off than it was at the height of the crisis. But there is still enough disease, still enough devastation, to warrant continued vigilance. And that starts with talking to all patients about HIV.
Ask the questions, they advise, do the test, and be prepared to refer patients to a specialist who can help them manage their illness. But don’t drop the ball on those patients even when they have specialty care; study up on drug interactions and know what you are prescribing to patients taking antiretroviral therapy.
“As PAs and NPs, we absolutely have to be the ones carrying that banner up front,” Ogunfiditimi says. “We’re the ones who have that opportunity to spend time with those patients and make sure we walk them through the urgency and the importance of being aware that this disease is still very rampant in our communities. I don’t want to say that we have taken it for granted, but we have definitely not paid as much attention as we used to in the ’80s and the ’90s, and we need to get back to that.”
“We can never forget,” Stewart concludes. “We spend a lot of time learning about and testing for breast cancer, prostate cancer, diabetes, and hypertension, all in an effort to take care of our patients the best we can. Screening for HIV should be in that same category.”
Reprinted from Clinician Reviews. 2012;22(6):cover, 11-14, 33-35.
December 1st is World AIDS Day. This article, from June 2012, was inspired by a conversation I had with a friend who was pursuing her Masters in Public Health. For a group project in epidemiology, she had tested a survey mechanism among college undergrads—a disturbing number of whom responded that they did not understand what “HIV” meant. We began ruminating on how “young people” (not substantially younger than ourselves) could be so clueless about a disease that had had such a devastating impact within recent memory. My question: Would this lack of awareness eventually result in a resurgence of a disease that, in truth, has never really gone away? —AMH
In the 30 years since the first cases of HIV were diagnosed in the United States, almost 620,000 people have died of AIDS in this country. In a very short period in the early 1980s, HIV morphed from completely unknown to epidemic in its scope; at one point, an estimated 130,000 new infections occurred each year in the US.
Today, that number has decreased substantially, to about 50,000 new infections per year. (Data from 2000 indicated the annual rate of new infections was 56,300, while CDC surveillance data from 46 reporting states in 2010 put the number at around 47,000.) In addition, the development and use of highly effective antiretroviral therapy has meant that people with HIV can live longer, healthier lives—provided, of course, that they have access to and comply with treatment.
Despite these improvements, however, is it acceptable that 1.2 million people in the US are living with HIV (20% of whom don’t even know it)? “No, that number is certainly not satisfactory,” says Folusho E. Ogunfiditimi, MPH, PA-C, Director of Advanced Practice Providers at Henry Ford Health System in Detroit and a member of the American Academy of Physician Assistants Clinical and Health Affairs Commission. “We cannot take our foot off the pedal regarding education, prevention, looking at outcomes, and also looking at the impact of disparities and trying to eliminate those disparities.”
Continue for what HIV is >>
OMG, WHAT'S HIV?
It is possible that American success at reducing (though hardly eliminating) the spread of HIV has actually undermined awareness. It sometimes seems to be a national characteristic that if we don’t see people dying in droves before our very eyes, we don’t think there’s a problem. A Kaiser Family Foundation survey conducted in 2009 revealed that just 6% of Americans considered HIV/AIDS to be “the most urgent health problem facing the nation,” down from a high of 44% in 1995.
In the 1980s and early 1990s, HIV and AIDS were hot topics in the news; it was impossible not to hear tales of horror or fear on a daily basis. While the reduction in misinformation dissemination is probably a positive, the Kaiser survey indicated that only 45% of Americans reported hearing, seeing, or reading “a lot” or “some” about the domestic problem of HIV/AIDS in the previous year. This might not be deeply concerning—there are, after all, plenty of other issues to discuss—until you realize that 62% of Americans consider the media to be their prime source of information about HIV/AIDS (compared with just 13% who say their health care provider is).
While awareness is an issue across demographic groups, the most potentially concerning is younger adults. This is a generation who most likely cannot tell you who Ryan White was and whose members were not alive during (or were far too young to remember) the major crisis of the HIV/AIDS epidemic.
“Sexually, they’ve grown up in an era where we have really good treatments,” says Susan LeLacheur, DrPH, PA-C, Associate Professor of Physician Assistant Studies at the George Washington University in Washington, DC, and a national lecturer on infectious disease and HIV infection. “When they meet people with HIV, those people are healthy.”
“Because we have, for lack of a better term, taken our foot off the pedal regarding HIV/AIDS awareness,” says Ogunfiditimi, “we run the risk of having people coming out of high school and into college not being as aware as we might have been in that age-group in the ’80s and early ’90s.”
In the Kaiser survey, 45% of respondents ages 18 to 29 indicated they had never been tested for HIV. Of those, 70% gave as a reason “you don’t think you’re at risk” and 33%, “your doctor never recommended it.”
In 2008, the CDC estimated that 25% of new HIV infections occur among adolescents and young adults (ie, those ages 13 to 29). This is part of the reason Ogunfiditimi says a renewed focus on education is essential; he also thinks PAs and NPs are well suited to provide that information, given their reputation as patient educators and their frequent work at the community level.
“We need to take this message back to those [age-]groups, back to those communities and schools,” he says, “and conduct health education seminars and HIV/AIDS awareness programs in the schools so that we can start to educate our younger ones.”
Continue for targeted or universal screening? >>
TARGETED OR UNIVERSAL SCREENING?
Under the direction of President Obama, who has said the US “is at a crossroads” in terms of HIV/AIDS, facing “a domestic epidemic that demands a renewed commitment, increased public attention, and leadership,” the White House Office of National AIDS Policy (ONAP) has set ambitious goals for HIV prevention. Outlined in the National HIV/AIDS Strategy for the United States, those goals—with a deadline of 2015—include:
• Decrease the annual new HIV infection rate by 25%.
• Decrease the HIV transmission rate (currently 5 persons infected per year per 100 people living with HIV) by 30%.
• Increase the number of people living with HIV who know of their infection from 79% to 90%.
• Increase the number of people with newly diagnosed HIV who have regular health care within three months from 65% to 85%.
The strategy (available at www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf) was commissioned and developed in response to concern that without bold action, “we face a new era of rising infections, greater challenges in serving people living with HIV, and higher health care costs,” as stated in the executive summary of the report.
It may not help the cause that health care providers receive seemingly mixed messages about how to approach HIV screening. Since 2006, the CDC has recommended routine screening for HIV, stating that “HIV screening is recommended for patients in all health-care settings after the patient is notified that testing will be performed unless the patient declines (opt-out screening).” The CDC expressly recommended that separate written consent and prevention counseling should not be required, in part as an acknowledgement that busy practicing clinicians who have to screen for a multitude of conditions and often provide acute care during an office visit are under time constraints.
“That doesn’t mean you don’t do any counseling at all,” says Julie G. Stewart, DNP, MPH, MSN, FNP, Assistant Professor and Coordinator of the FNP Program at Sacred Heart University and an HIV NP at Southwest Community Health Center in Bridgeport, Connecticut, “but having discussions with your patients about their life and their health and their risk factors in every facet should include HIV testing.”
At the same time, both the CDC and ONAP emphasize that certain populations are at higher risk for HIV infection and therefore need to be targeted. These include:
• Gay, bisexual, and other men who have sex with men: 2% of the US population but 61% of new infections (2009 data)
• Black men and women: 14% of the population but 44% of new HIV infections
• Hispanic and Latino persons: 16% of the population but 20% of new HIV infections
• Injection-drug users: 9% of new HIV infections
The CDC also reports that heterosexual persons account for 27% of new HIV infections.
In a tough economic climate, when the US investment in response to the domestic HIV epidemic has risen to more than $19 billion per year, it makes sense to strategize how to most effectively utilize available resources to reduce disease burden. But do we run the risk of missing cases because we make too many assumptions about who is or is not likely to have this infection?
“The information that has been pushed out there has really tried to focus on these high-risk groups—and yes, we understand that those groups need to be identified,” says Ogunfiditimi. “But when you’re trying to increase the amount of testing, then the message needs to be more general so that practitioners who have natural biases won’t implement those biases into their decision as to whether to test someone.”
“What worries me is that the recommendation has been to test everyone at least once, and then again as indicated,” says LeLacheur. “‘As indicated’ means you have to ask. In parts of the country where HIV is not as prevalent as it is in DC, I can understand how it falls off the radar. But there are still a few [cases]—maybe not one in 20, maybe more like one or two in a clinician’s lifetime—and there is just no telling from the outside.”
“Perception of risk is huge,” adds Stewart. Her state was one of the first to mandate prenatal HIV testing, and she recalls instances in which a woman tested positive and the clinician was shocked because, Stewart says, “the perception was that ‘She is not at any risk at all,’ based on where she lives and her background. But the clinician didn’t really know.”
LeLacheur also points out that assumptions work both ways: “Oh, he’s a nice boy” and “Oh, he’s not a nice boy.” In one of her classes, a gay male student shared his experience seeking a diagnosis for what turned out to be Crohn’s disease. “The minute he told his clinician he was gay, all of a sudden he had AIDS and the clinician wouldn’t look anywhere else,” LeLacheur reports. “And that just wasn’t an issue; this was a kid who had been raised in an era of safer sex and had been very careful.”
Advocates say that implementing universal screening, per the CDC’s recommendation, would not only capture more cases but would also reduce the stigma associated with targeted screening.
Continue for truths and consequences >>
TRUTHS AND CONSEQUENCES
So perceptions and assumptions play important roles in how the US addresses HIV testing—both the perceptions of some patients that they are not at risk or that having HIV isn’t a big deal anymore, and the assumptions by health care providers that they don’t need to screen all patients for HIV. That faulty logic can have dire consequences, even if HIV is no longer an automatic death sentence.
“I think there’s a lot of passive testing, a lot of disease-induced or behavior-induced testing,” Ogunfiditimi says. “A patient comes in with complaints of what sounds like a sexually transmitted infection and that may spur a provider to initiate the discussion around HIV and subsequently do testing to back that up. But I don’t get the sense that HIV testing is promoted significantly.”
“They get sick” is how Stewart says many people learn their HIV status. “That is still frequently the way people become aware of their illness—they are sick in the hospital with an opportunistic infection…. If we can identify people who are HIV-infected earlier, we can capture them at higher CD4 counts, and then they have an improved life expectancy. We can start treatment, and that also impacts transmission.”
Echoing Stewart’s comments, LeLacheur also notes that the major pneumonia or other infection that leads to hospitalization and diagnosis of HIV can cause permanent damage. “I have a couple of patients who appear to be poststroke because of a viral infection in their brains that people get very late in HIV,” she says. “Now, their viral loads are undetectable and their CD4s are very high. Their immune systems are in good shape, and in every other way they’re healthy. But they can’t walk.”
For those misguided patients who think HIV isn’t such a big deal these days, LeLacheur has some hard facts clinicians can share. “You don’t realize until after you have HIV and someone explains it to you that the minute you get it, it essentially knocks out the entire immune system in your intestinal tract—which is more than half of your immune system—and that’s never coming back,” she says. “That infection in the gut is never going away; the medicines don’t touch it. So your digestion will never be right. There are things we can’t fix about HIV.”
And heaven help the patient who tries to rationalize that “you just take one pill a day.” First of all, that one pill ties up your liver, as LeLacheur points out, and second of all, HIV medications cost about $16,000 a year. Not many people can afford that on their own, and some states have 700-person-long waiting lists for assistance programs.
The consensus among clinicians who treat HIV-infected patients is that, yes, the US is much better off than it was at the height of the crisis. But there is still enough disease, still enough devastation, to warrant continued vigilance. And that starts with talking to all patients about HIV.
Ask the questions, they advise, do the test, and be prepared to refer patients to a specialist who can help them manage their illness. But don’t drop the ball on those patients even when they have specialty care; study up on drug interactions and know what you are prescribing to patients taking antiretroviral therapy.
“As PAs and NPs, we absolutely have to be the ones carrying that banner up front,” Ogunfiditimi says. “We’re the ones who have that opportunity to spend time with those patients and make sure we walk them through the urgency and the importance of being aware that this disease is still very rampant in our communities. I don’t want to say that we have taken it for granted, but we have definitely not paid as much attention as we used to in the ’80s and the ’90s, and we need to get back to that.”
“We can never forget,” Stewart concludes. “We spend a lot of time learning about and testing for breast cancer, prostate cancer, diabetes, and hypertension, all in an effort to take care of our patients the best we can. Screening for HIV should be in that same category.”
Reprinted from Clinician Reviews. 2012;22(6):cover, 11-14, 33-35.
Voices for Change: AANP Celebrates 25 Years
When I started editing Marie-Eileen Onieal’s editorial for this issue, her reference to the grassroots origins of the American Academy of Nurse Practitioners (now “Association”) reminded me of this article, which appeared in June 2010 to mark the organization’s 25th anniversary. Although five years have passed, I vividly recall the passion, enthusiasm, and wisdom of the founders, whose message about taking action to create positive change still resonates. They were inspiring to speak to, and never have I enjoyed working on an article more. —AMH
Picture it: Kansas City, 1984. At a meeting sponsored by the American Nurses Association (ANA), conversation among the NP attendees from across the United States focuses on the widely perceived need for “common representation” of their distinct interests. Who among the existing nursing organizations has the time, money, and/or inclination to serve as the voice of all NPs, providing a conduit for communication and leadership in legislative efforts to remove barriers to practice?
As it will turn out, the answer is no one—at least, not in the way these NPs envision. So they decide to do something about that … and since the result of their collaborative vision is the American Academy of Nurse Practitioners (AANP), you have a pretty good idea how it worked out.
AANP is celebrating its 25th anniversary this year—a milestone its founders probably never doubted would be reached, although others initially questioned the viability of such an organization.
“The feeling was that if it was needed, it would grow, and if it wasn’t needed, it wouldn’t grow,” recalls Jan Towers, PhD, NP-C, CRNP, FAANP, a founding member and past president who continues to serve AANP as Director of Health Policy. “And indeed it grew—so I think we know what our answer was!”
A SEPARATE BUT EQUAL NEED
Of course, creating a new professional organization was not as simple as a group of individuals putting their heads together. And yet, in a certain sense, it was that easy.
Shortly after those initial discussions in Kansas City, there was another conference in Washington, DC. During a panel discussion with executives from the insurance and advertising industries, it became evident that the biggest issue for NPs was “no one knew who we were,” says Clinician Reviews NP Editor-in-Chief Marie-Eileen Onieal, PhD, CPNP, FAANP, also a founder and past president of AANP. Clearly, that situation needed to be remedied—but how?
At that time, many NPs were members of ANA (and, it should be noted, many still are). However, since ANA represents all of nursing, the bulk of its resources could not be devoted to NPs. The organization had created a Council of Primary Care NPs in 1974, but the “renegade” NPs of 1984 felt that structure didn’t provide the latitude they wanted in their representation.
“We needed a way to really work together and have our undivided attention focused on NP issues,” Towers says. Onieal adds, “We weren’t abandoning our ‘nursing-ness,’ but clearly we had separate and distinctly different issues at hand than did the general populace of the nursing profession.”
The fact that NPs from across the country—remember, this is pre-Internet—shared this viewpoint added strength to the argument. If dozens of people who didn’t really know one another could see the same need, it must be real—and therefore, it had to be addressed.
“The [NP] role had been around since 1965, but nursing faculty were just beginning to define what NP education ought to look like,” says Carole Kain, DNS, ARNP, PNP-BC, a founding member and the first president of AANP. (She was Carole Kerwin then.) “A lot of things were changing in the profession, and we all wanted to be part of defining what that change meant. It was everybody coming together with a skill set that set us on this course.”
The time was certainly ripe. In her files, Kain still has a copy of a document discussing a referendum the American Medical Association passed in 1984, in which “they said they were actually going to try to inhibit the practice of NPs, PAs, nurse-midwives, and pharmacists, as to prescribing and taking care of patients.”
In addition to that restrictive attitude—a cause to rally around for NPs nationwide—the NP profession had reached a tipping point in terms of growth. “Enough of us had been prepared, but we were still small enough to be spread out [across the country],” Towers says. “We needed some way to connect.”
By the time they left Washington, DC, a steering committee had been formed to explore the need for an organization representing the nation’s approximately 24,000 NPs. They were expected to report back to the ANA one year later, at a meeting in Chicago. And so, the hard work began.
SO, YOU WANT TO START AN ORGANIZATION?
For a group of virtual strangers who had never started an organization before, they went about their business in a methodical and logical way. Different task forces were created, including one to look into how to do articles of incorporation and other “legalese” pieces, and another to develop a list of reasons why a separate organization was needed.
Onieal recalls a good deal of traveling that she and some other NPs did “to every NP meeting, every NP gathering, across the US for a year. We had a petition, and I’d say, ‘All I want to know is whether you think we should start an NP organization.’” The list grew over the course of the year.
In the meantime, contact was made with the handful of existing NP organizations, to see if any of them could meet the needs of the profession at large: the National Association of Pediatric NPs (1973), the National Association of NPs in Reproductive Health (which became the National Association of NPs in Women’s Health; 1980), and the National Conference of Gerontological NPs (1981). But obviously, since these groups had been tasked by their members with representing the interests of NPs in specific fields, their responses boiled down to “We can’t help you—but we wish you well.”
By the time the Chicago meeting rolled around in May 1985, about the only thing left to do was announce the new organization’s formation. Bylaws had already been drafted, and Onieal’s (now former) address in Lowell, Massachusetts, had been chosen as the original headquarters of the organization. (Trivia: AANP was originally incorporated in Lowell, before relocating to Austin, Texas.)
During a panel session in Chicago, Kain and Onieal told the assembled crowd, “This is what we need: We need to be heard as independent providers. We need to have some say in how our practice is regulated. We need … an organization that will allow us to learn from each other across the country,” as Kain recalls.
The official press release announcing AANP’s creation reads: “The overall purpose of the AANP is to promote high standards of health care as delivered by nurse practitioners and to act as a forum to enhance the identity and continuity of nurse practitioners. It is nationwide in scope and welcomes all nurse practitioners, regardless of specialty. The first year’s focus will be on networking and communications.”
AANP’s first elected officers were Kain (President), Towers (President-Elect), Onieal (Treasurer), Madeline D. Wiley, MSN, ARNP (Recording Secretary), and Robert T. Smithing, MSN, ARNP (Communications Secretary). Annual membership dues were $60.
25 YEARS OF PROGRESS
The leaders and members of the newly formed AANP wasted little time in setting out to accomplish their organizational goals. As Onieal says, “When we started, we had a five-year plan and a 10-year plan. And in five years, we got through all of that.”
With the initial focus on networking and communications, 10 geographical regions were established, based on the National Health Service Corps regions, and regional directors were found. So were individual reps from every state, each of whom then “started talking to people within their state,” Kain says.
For Towers, the focus was on legislative and regulatory issues, just as it is today. “One of the first things we started doing was finding ways to influence policy, both in Washington and in our states,” she says. “Early on, we started working on reimbursement.”
An early victory was getting NPs reimbursement through the Federal Employees Health Benefits Program (1986-1987). On the Medicare front, AANP had a significant impact in securing reimbursement for NPs working in rural areas and in long-term care facilities (1989-1990). Additional milestones include mandated Medicare payment for family and pediatric NPs regardless of supervision status (the early ’90s) and direct Medicare reimbursement for NPs regardless of setting (1997).
Seeing all that has been accomplished in 25 years is still a little amazing, even to the people who set the wheels in motion. “We’re funding research, and we have a foundation that gives scholarships,” Kain says. “Those are things we talked about as ‘someday’ dreams, but now they’re actualizations.”
She’s greeted every day by signs of how much has changed since 1985. “I can remember the initial discussions about having a certification program, talking to the psychometricians about how we’d start up the exam and which criteria we’d use,” she reflects. “And now, the NPs that I’m teaching are using that certification exam to get their licensure!”
As much as Onieal appreciates all the services that AANP has grown to offer its members, she also recognizes the core value of the organization. “One of our primary purposes was to let people know what NPs are all about—to clarify that we’re not LPNs, we’re not students, we’re not people who couldn’t go to medical school and decided to do this instead; this was our chosen profession,” she says. “I think we’ve been successful in doing that.”
THE ULTIMATE COLLABORATION
The founders of AANP never doubted that forming the organization was the right thing to do, which probably confirms that they were the best people to do the job. Instead of expending energy on doubts or infighting, they figured out what needed to be done and moved forward.
Kain still has a “vivid mental picture” of the early days in Kansas City and Washington, DC, when there was no organization and therefore no budget, so meetings were held in someone’s hotel room. “There would be people sitting on the bed, on the floor, standing up; we’re all crammed into the room,” she remembers with a laugh. “And people are talking, and we’re polite to one another, we’re respectful of one another. We’re passionate. We’re talking about the difficulties and why we need this. And if you could put that into a bottle, you could start a new organization right now!”
That spirit of collaboration is still a viable part of the organization, one that Onieal is proud of. “If anybody ever had an interest in doing something or being something within the organization, the doors were open,” she says. “Early on, a couple of students said, ‘But we have needs, too,’ so we said, ‘Fine, we’ll start a student special interest group. No problem.’” The point, after all, had always been to learn from one another.
If there is one lesson the AANP founders hope to pass along to future generations, it’s that great change can be brought about by a small group of (seemingly) ordinary people with extraordinary determination. They don’t want statues erected in their honor, but they do want others to be inspired to take an active role in the continuous evolution of the NP profession—especially since, as Towers observes, “There is still work to be done.”
“We need to get all the state practice acts on a level playing field,” she notes, “which we’re well on the way to doing now with our consensus document and the model rules and regulations. We need to have recognition within all the payment systems, and remove barriers within existing laws that prevent NPs from practicing to their fullest capability.”
The significant changes that have been brought about in the past 25 years can be difficult to fathom for those who did not witness them. In 2010, the NP profession is well established. (The same is true for PAs.) Students deciding their future choose these professions in part because of all they will be able to do and accomplish within their roles.
What they don’t always recognize is that it took hard work and continued vigilance on the part of those who have preceded them to achieve the privileges that today’s clinicians—and perhaps tomorrow’s—run the risk of taking for granted.
“We’re not done, and I don’t want anyone to think they can rest on the laurels of what has gone before or think that without their involvement it will continue,” says Kain. “It won’t. We need them. We need new blood, new thoughts, new ideas, to face the new challenges.”
When she reflects on how a group of near-strangers got together and made a mark on the history of their profession, she concludes, simply, “Others can do the same thing. They just have to want to, and see the need.”
Reprinted from Clinician Reviews. 2010;20(6):cover, 5-8.
When I started editing Marie-Eileen Onieal’s editorial for this issue, her reference to the grassroots origins of the American Academy of Nurse Practitioners (now “Association”) reminded me of this article, which appeared in June 2010 to mark the organization’s 25th anniversary. Although five years have passed, I vividly recall the passion, enthusiasm, and wisdom of the founders, whose message about taking action to create positive change still resonates. They were inspiring to speak to, and never have I enjoyed working on an article more. —AMH
Picture it: Kansas City, 1984. At a meeting sponsored by the American Nurses Association (ANA), conversation among the NP attendees from across the United States focuses on the widely perceived need for “common representation” of their distinct interests. Who among the existing nursing organizations has the time, money, and/or inclination to serve as the voice of all NPs, providing a conduit for communication and leadership in legislative efforts to remove barriers to practice?
As it will turn out, the answer is no one—at least, not in the way these NPs envision. So they decide to do something about that … and since the result of their collaborative vision is the American Academy of Nurse Practitioners (AANP), you have a pretty good idea how it worked out.
AANP is celebrating its 25th anniversary this year—a milestone its founders probably never doubted would be reached, although others initially questioned the viability of such an organization.
“The feeling was that if it was needed, it would grow, and if it wasn’t needed, it wouldn’t grow,” recalls Jan Towers, PhD, NP-C, CRNP, FAANP, a founding member and past president who continues to serve AANP as Director of Health Policy. “And indeed it grew—so I think we know what our answer was!”
A SEPARATE BUT EQUAL NEED
Of course, creating a new professional organization was not as simple as a group of individuals putting their heads together. And yet, in a certain sense, it was that easy.
Shortly after those initial discussions in Kansas City, there was another conference in Washington, DC. During a panel discussion with executives from the insurance and advertising industries, it became evident that the biggest issue for NPs was “no one knew who we were,” says Clinician Reviews NP Editor-in-Chief Marie-Eileen Onieal, PhD, CPNP, FAANP, also a founder and past president of AANP. Clearly, that situation needed to be remedied—but how?
At that time, many NPs were members of ANA (and, it should be noted, many still are). However, since ANA represents all of nursing, the bulk of its resources could not be devoted to NPs. The organization had created a Council of Primary Care NPs in 1974, but the “renegade” NPs of 1984 felt that structure didn’t provide the latitude they wanted in their representation.
“We needed a way to really work together and have our undivided attention focused on NP issues,” Towers says. Onieal adds, “We weren’t abandoning our ‘nursing-ness,’ but clearly we had separate and distinctly different issues at hand than did the general populace of the nursing profession.”
The fact that NPs from across the country—remember, this is pre-Internet—shared this viewpoint added strength to the argument. If dozens of people who didn’t really know one another could see the same need, it must be real—and therefore, it had to be addressed.
“The [NP] role had been around since 1965, but nursing faculty were just beginning to define what NP education ought to look like,” says Carole Kain, DNS, ARNP, PNP-BC, a founding member and the first president of AANP. (She was Carole Kerwin then.) “A lot of things were changing in the profession, and we all wanted to be part of defining what that change meant. It was everybody coming together with a skill set that set us on this course.”
The time was certainly ripe. In her files, Kain still has a copy of a document discussing a referendum the American Medical Association passed in 1984, in which “they said they were actually going to try to inhibit the practice of NPs, PAs, nurse-midwives, and pharmacists, as to prescribing and taking care of patients.”
In addition to that restrictive attitude—a cause to rally around for NPs nationwide—the NP profession had reached a tipping point in terms of growth. “Enough of us had been prepared, but we were still small enough to be spread out [across the country],” Towers says. “We needed some way to connect.”
By the time they left Washington, DC, a steering committee had been formed to explore the need for an organization representing the nation’s approximately 24,000 NPs. They were expected to report back to the ANA one year later, at a meeting in Chicago. And so, the hard work began.
SO, YOU WANT TO START AN ORGANIZATION?
For a group of virtual strangers who had never started an organization before, they went about their business in a methodical and logical way. Different task forces were created, including one to look into how to do articles of incorporation and other “legalese” pieces, and another to develop a list of reasons why a separate organization was needed.
Onieal recalls a good deal of traveling that she and some other NPs did “to every NP meeting, every NP gathering, across the US for a year. We had a petition, and I’d say, ‘All I want to know is whether you think we should start an NP organization.’” The list grew over the course of the year.
In the meantime, contact was made with the handful of existing NP organizations, to see if any of them could meet the needs of the profession at large: the National Association of Pediatric NPs (1973), the National Association of NPs in Reproductive Health (which became the National Association of NPs in Women’s Health; 1980), and the National Conference of Gerontological NPs (1981). But obviously, since these groups had been tasked by their members with representing the interests of NPs in specific fields, their responses boiled down to “We can’t help you—but we wish you well.”
By the time the Chicago meeting rolled around in May 1985, about the only thing left to do was announce the new organization’s formation. Bylaws had already been drafted, and Onieal’s (now former) address in Lowell, Massachusetts, had been chosen as the original headquarters of the organization. (Trivia: AANP was originally incorporated in Lowell, before relocating to Austin, Texas.)
During a panel session in Chicago, Kain and Onieal told the assembled crowd, “This is what we need: We need to be heard as independent providers. We need to have some say in how our practice is regulated. We need … an organization that will allow us to learn from each other across the country,” as Kain recalls.
The official press release announcing AANP’s creation reads: “The overall purpose of the AANP is to promote high standards of health care as delivered by nurse practitioners and to act as a forum to enhance the identity and continuity of nurse practitioners. It is nationwide in scope and welcomes all nurse practitioners, regardless of specialty. The first year’s focus will be on networking and communications.”
AANP’s first elected officers were Kain (President), Towers (President-Elect), Onieal (Treasurer), Madeline D. Wiley, MSN, ARNP (Recording Secretary), and Robert T. Smithing, MSN, ARNP (Communications Secretary). Annual membership dues were $60.
25 YEARS OF PROGRESS
The leaders and members of the newly formed AANP wasted little time in setting out to accomplish their organizational goals. As Onieal says, “When we started, we had a five-year plan and a 10-year plan. And in five years, we got through all of that.”
With the initial focus on networking and communications, 10 geographical regions were established, based on the National Health Service Corps regions, and regional directors were found. So were individual reps from every state, each of whom then “started talking to people within their state,” Kain says.
For Towers, the focus was on legislative and regulatory issues, just as it is today. “One of the first things we started doing was finding ways to influence policy, both in Washington and in our states,” she says. “Early on, we started working on reimbursement.”
An early victory was getting NPs reimbursement through the Federal Employees Health Benefits Program (1986-1987). On the Medicare front, AANP had a significant impact in securing reimbursement for NPs working in rural areas and in long-term care facilities (1989-1990). Additional milestones include mandated Medicare payment for family and pediatric NPs regardless of supervision status (the early ’90s) and direct Medicare reimbursement for NPs regardless of setting (1997).
Seeing all that has been accomplished in 25 years is still a little amazing, even to the people who set the wheels in motion. “We’re funding research, and we have a foundation that gives scholarships,” Kain says. “Those are things we talked about as ‘someday’ dreams, but now they’re actualizations.”
She’s greeted every day by signs of how much has changed since 1985. “I can remember the initial discussions about having a certification program, talking to the psychometricians about how we’d start up the exam and which criteria we’d use,” she reflects. “And now, the NPs that I’m teaching are using that certification exam to get their licensure!”
As much as Onieal appreciates all the services that AANP has grown to offer its members, she also recognizes the core value of the organization. “One of our primary purposes was to let people know what NPs are all about—to clarify that we’re not LPNs, we’re not students, we’re not people who couldn’t go to medical school and decided to do this instead; this was our chosen profession,” she says. “I think we’ve been successful in doing that.”
THE ULTIMATE COLLABORATION
The founders of AANP never doubted that forming the organization was the right thing to do, which probably confirms that they were the best people to do the job. Instead of expending energy on doubts or infighting, they figured out what needed to be done and moved forward.
Kain still has a “vivid mental picture” of the early days in Kansas City and Washington, DC, when there was no organization and therefore no budget, so meetings were held in someone’s hotel room. “There would be people sitting on the bed, on the floor, standing up; we’re all crammed into the room,” she remembers with a laugh. “And people are talking, and we’re polite to one another, we’re respectful of one another. We’re passionate. We’re talking about the difficulties and why we need this. And if you could put that into a bottle, you could start a new organization right now!”
That spirit of collaboration is still a viable part of the organization, one that Onieal is proud of. “If anybody ever had an interest in doing something or being something within the organization, the doors were open,” she says. “Early on, a couple of students said, ‘But we have needs, too,’ so we said, ‘Fine, we’ll start a student special interest group. No problem.’” The point, after all, had always been to learn from one another.
If there is one lesson the AANP founders hope to pass along to future generations, it’s that great change can be brought about by a small group of (seemingly) ordinary people with extraordinary determination. They don’t want statues erected in their honor, but they do want others to be inspired to take an active role in the continuous evolution of the NP profession—especially since, as Towers observes, “There is still work to be done.”
“We need to get all the state practice acts on a level playing field,” she notes, “which we’re well on the way to doing now with our consensus document and the model rules and regulations. We need to have recognition within all the payment systems, and remove barriers within existing laws that prevent NPs from practicing to their fullest capability.”
The significant changes that have been brought about in the past 25 years can be difficult to fathom for those who did not witness them. In 2010, the NP profession is well established. (The same is true for PAs.) Students deciding their future choose these professions in part because of all they will be able to do and accomplish within their roles.
What they don’t always recognize is that it took hard work and continued vigilance on the part of those who have preceded them to achieve the privileges that today’s clinicians—and perhaps tomorrow’s—run the risk of taking for granted.
“We’re not done, and I don’t want anyone to think they can rest on the laurels of what has gone before or think that without their involvement it will continue,” says Kain. “It won’t. We need them. We need new blood, new thoughts, new ideas, to face the new challenges.”
When she reflects on how a group of near-strangers got together and made a mark on the history of their profession, she concludes, simply, “Others can do the same thing. They just have to want to, and see the need.”
Reprinted from Clinician Reviews. 2010;20(6):cover, 5-8.
When I started editing Marie-Eileen Onieal’s editorial for this issue, her reference to the grassroots origins of the American Academy of Nurse Practitioners (now “Association”) reminded me of this article, which appeared in June 2010 to mark the organization’s 25th anniversary. Although five years have passed, I vividly recall the passion, enthusiasm, and wisdom of the founders, whose message about taking action to create positive change still resonates. They were inspiring to speak to, and never have I enjoyed working on an article more. —AMH
Picture it: Kansas City, 1984. At a meeting sponsored by the American Nurses Association (ANA), conversation among the NP attendees from across the United States focuses on the widely perceived need for “common representation” of their distinct interests. Who among the existing nursing organizations has the time, money, and/or inclination to serve as the voice of all NPs, providing a conduit for communication and leadership in legislative efforts to remove barriers to practice?
As it will turn out, the answer is no one—at least, not in the way these NPs envision. So they decide to do something about that … and since the result of their collaborative vision is the American Academy of Nurse Practitioners (AANP), you have a pretty good idea how it worked out.
AANP is celebrating its 25th anniversary this year—a milestone its founders probably never doubted would be reached, although others initially questioned the viability of such an organization.
“The feeling was that if it was needed, it would grow, and if it wasn’t needed, it wouldn’t grow,” recalls Jan Towers, PhD, NP-C, CRNP, FAANP, a founding member and past president who continues to serve AANP as Director of Health Policy. “And indeed it grew—so I think we know what our answer was!”
A SEPARATE BUT EQUAL NEED
Of course, creating a new professional organization was not as simple as a group of individuals putting their heads together. And yet, in a certain sense, it was that easy.
Shortly after those initial discussions in Kansas City, there was another conference in Washington, DC. During a panel discussion with executives from the insurance and advertising industries, it became evident that the biggest issue for NPs was “no one knew who we were,” says Clinician Reviews NP Editor-in-Chief Marie-Eileen Onieal, PhD, CPNP, FAANP, also a founder and past president of AANP. Clearly, that situation needed to be remedied—but how?
At that time, many NPs were members of ANA (and, it should be noted, many still are). However, since ANA represents all of nursing, the bulk of its resources could not be devoted to NPs. The organization had created a Council of Primary Care NPs in 1974, but the “renegade” NPs of 1984 felt that structure didn’t provide the latitude they wanted in their representation.
“We needed a way to really work together and have our undivided attention focused on NP issues,” Towers says. Onieal adds, “We weren’t abandoning our ‘nursing-ness,’ but clearly we had separate and distinctly different issues at hand than did the general populace of the nursing profession.”
The fact that NPs from across the country—remember, this is pre-Internet—shared this viewpoint added strength to the argument. If dozens of people who didn’t really know one another could see the same need, it must be real—and therefore, it had to be addressed.
“The [NP] role had been around since 1965, but nursing faculty were just beginning to define what NP education ought to look like,” says Carole Kain, DNS, ARNP, PNP-BC, a founding member and the first president of AANP. (She was Carole Kerwin then.) “A lot of things were changing in the profession, and we all wanted to be part of defining what that change meant. It was everybody coming together with a skill set that set us on this course.”
The time was certainly ripe. In her files, Kain still has a copy of a document discussing a referendum the American Medical Association passed in 1984, in which “they said they were actually going to try to inhibit the practice of NPs, PAs, nurse-midwives, and pharmacists, as to prescribing and taking care of patients.”
In addition to that restrictive attitude—a cause to rally around for NPs nationwide—the NP profession had reached a tipping point in terms of growth. “Enough of us had been prepared, but we were still small enough to be spread out [across the country],” Towers says. “We needed some way to connect.”
By the time they left Washington, DC, a steering committee had been formed to explore the need for an organization representing the nation’s approximately 24,000 NPs. They were expected to report back to the ANA one year later, at a meeting in Chicago. And so, the hard work began.
SO, YOU WANT TO START AN ORGANIZATION?
For a group of virtual strangers who had never started an organization before, they went about their business in a methodical and logical way. Different task forces were created, including one to look into how to do articles of incorporation and other “legalese” pieces, and another to develop a list of reasons why a separate organization was needed.
Onieal recalls a good deal of traveling that she and some other NPs did “to every NP meeting, every NP gathering, across the US for a year. We had a petition, and I’d say, ‘All I want to know is whether you think we should start an NP organization.’” The list grew over the course of the year.
In the meantime, contact was made with the handful of existing NP organizations, to see if any of them could meet the needs of the profession at large: the National Association of Pediatric NPs (1973), the National Association of NPs in Reproductive Health (which became the National Association of NPs in Women’s Health; 1980), and the National Conference of Gerontological NPs (1981). But obviously, since these groups had been tasked by their members with representing the interests of NPs in specific fields, their responses boiled down to “We can’t help you—but we wish you well.”
By the time the Chicago meeting rolled around in May 1985, about the only thing left to do was announce the new organization’s formation. Bylaws had already been drafted, and Onieal’s (now former) address in Lowell, Massachusetts, had been chosen as the original headquarters of the organization. (Trivia: AANP was originally incorporated in Lowell, before relocating to Austin, Texas.)
During a panel session in Chicago, Kain and Onieal told the assembled crowd, “This is what we need: We need to be heard as independent providers. We need to have some say in how our practice is regulated. We need … an organization that will allow us to learn from each other across the country,” as Kain recalls.
The official press release announcing AANP’s creation reads: “The overall purpose of the AANP is to promote high standards of health care as delivered by nurse practitioners and to act as a forum to enhance the identity and continuity of nurse practitioners. It is nationwide in scope and welcomes all nurse practitioners, regardless of specialty. The first year’s focus will be on networking and communications.”
AANP’s first elected officers were Kain (President), Towers (President-Elect), Onieal (Treasurer), Madeline D. Wiley, MSN, ARNP (Recording Secretary), and Robert T. Smithing, MSN, ARNP (Communications Secretary). Annual membership dues were $60.
25 YEARS OF PROGRESS
The leaders and members of the newly formed AANP wasted little time in setting out to accomplish their organizational goals. As Onieal says, “When we started, we had a five-year plan and a 10-year plan. And in five years, we got through all of that.”
With the initial focus on networking and communications, 10 geographical regions were established, based on the National Health Service Corps regions, and regional directors were found. So were individual reps from every state, each of whom then “started talking to people within their state,” Kain says.
For Towers, the focus was on legislative and regulatory issues, just as it is today. “One of the first things we started doing was finding ways to influence policy, both in Washington and in our states,” she says. “Early on, we started working on reimbursement.”
An early victory was getting NPs reimbursement through the Federal Employees Health Benefits Program (1986-1987). On the Medicare front, AANP had a significant impact in securing reimbursement for NPs working in rural areas and in long-term care facilities (1989-1990). Additional milestones include mandated Medicare payment for family and pediatric NPs regardless of supervision status (the early ’90s) and direct Medicare reimbursement for NPs regardless of setting (1997).
Seeing all that has been accomplished in 25 years is still a little amazing, even to the people who set the wheels in motion. “We’re funding research, and we have a foundation that gives scholarships,” Kain says. “Those are things we talked about as ‘someday’ dreams, but now they’re actualizations.”
She’s greeted every day by signs of how much has changed since 1985. “I can remember the initial discussions about having a certification program, talking to the psychometricians about how we’d start up the exam and which criteria we’d use,” she reflects. “And now, the NPs that I’m teaching are using that certification exam to get their licensure!”
As much as Onieal appreciates all the services that AANP has grown to offer its members, she also recognizes the core value of the organization. “One of our primary purposes was to let people know what NPs are all about—to clarify that we’re not LPNs, we’re not students, we’re not people who couldn’t go to medical school and decided to do this instead; this was our chosen profession,” she says. “I think we’ve been successful in doing that.”
THE ULTIMATE COLLABORATION
The founders of AANP never doubted that forming the organization was the right thing to do, which probably confirms that they were the best people to do the job. Instead of expending energy on doubts or infighting, they figured out what needed to be done and moved forward.
Kain still has a “vivid mental picture” of the early days in Kansas City and Washington, DC, when there was no organization and therefore no budget, so meetings were held in someone’s hotel room. “There would be people sitting on the bed, on the floor, standing up; we’re all crammed into the room,” she remembers with a laugh. “And people are talking, and we’re polite to one another, we’re respectful of one another. We’re passionate. We’re talking about the difficulties and why we need this. And if you could put that into a bottle, you could start a new organization right now!”
That spirit of collaboration is still a viable part of the organization, one that Onieal is proud of. “If anybody ever had an interest in doing something or being something within the organization, the doors were open,” she says. “Early on, a couple of students said, ‘But we have needs, too,’ so we said, ‘Fine, we’ll start a student special interest group. No problem.’” The point, after all, had always been to learn from one another.
If there is one lesson the AANP founders hope to pass along to future generations, it’s that great change can be brought about by a small group of (seemingly) ordinary people with extraordinary determination. They don’t want statues erected in their honor, but they do want others to be inspired to take an active role in the continuous evolution of the NP profession—especially since, as Towers observes, “There is still work to be done.”
“We need to get all the state practice acts on a level playing field,” she notes, “which we’re well on the way to doing now with our consensus document and the model rules and regulations. We need to have recognition within all the payment systems, and remove barriers within existing laws that prevent NPs from practicing to their fullest capability.”
The significant changes that have been brought about in the past 25 years can be difficult to fathom for those who did not witness them. In 2010, the NP profession is well established. (The same is true for PAs.) Students deciding their future choose these professions in part because of all they will be able to do and accomplish within their roles.
What they don’t always recognize is that it took hard work and continued vigilance on the part of those who have preceded them to achieve the privileges that today’s clinicians—and perhaps tomorrow’s—run the risk of taking for granted.
“We’re not done, and I don’t want anyone to think they can rest on the laurels of what has gone before or think that without their involvement it will continue,” says Kain. “It won’t. We need them. We need new blood, new thoughts, new ideas, to face the new challenges.”
When she reflects on how a group of near-strangers got together and made a mark on the history of their profession, she concludes, simply, “Others can do the same thing. They just have to want to, and see the need.”
Reprinted from Clinician Reviews. 2010;20(6):cover, 5-8.
ObGyn salaries continue gradual improvement
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
In this article
- Which practice settings pay better?
- Would you select a career in ObGyn again?
- Comparing time spent with patients
Is the use of a containment bag at minimally invasive hysterectomy or myomectomy effective at reducing tissue spillage?
Tissue extraction during laparoscopic or robot-assisted laparoscopic gynecologic surgery raises safety concerns for dissemination of tissue during the open, or uncontained, electromechanical morcellation process. Researchers from Brigham & Women’s Hospital in Boston, Massachusetts, investigated whether contained tissue extraction using power morcellators entirely within a bag is safe and practical for preventing tissue spillage. Goggins and colleagues presented their findings in a poster at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco, California.
A total of 76 women at 4 institutions underwent laparoscopic or robotic multiport surgery (42 hysterectomy; 34 myomectomy). The average (SD) age and body mass index of the women were 43.16 (8.53) years and 26.47 kg/m2 (5.93), respectively. After surgical dissection, each specimen was placed into a containment bag that also included blue dye. The bag was insufflated intracorporeally and electromechanical morcellation and extraction of tissue were performed. The bag was evaluated visually for dye leakage or tears before and after the procedure.
Results
In one case, there was a tear in the bag before morcellation; no bag tears occurred during the morcellation process. Spillage of dye or tissue was noted in 7 cases, although containment bags were intact in each instance. One patient experienced intraoperative blood loss (3600 mL), and that procedure was converted to open radical hysterectomy. The most common pathologic finding was benign leiomyoma.
Conclusion
Goggins and colleagues concluded, “Contained tissue extraction using electromechanical morcellation and intracorporeally insufflated bags may provide a safe alternative to uncontained morcellation by decreasing the spread of tissue in the peritoneal cavity while allowing for the traditional benefits of laparoscopy.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Goggins ER, Greenberg JA, Cohen SL, Morris SN, Brown DN, Einarsson JI. Efficacy of contained tissue extraction for minimizing tissue dissemination during laparoscopic hysterectomy and myomectomy. Obstet Gynecol. 2015;125(5)(suppl):29S.
Tissue extraction during laparoscopic or robot-assisted laparoscopic gynecologic surgery raises safety concerns for dissemination of tissue during the open, or uncontained, electromechanical morcellation process. Researchers from Brigham & Women’s Hospital in Boston, Massachusetts, investigated whether contained tissue extraction using power morcellators entirely within a bag is safe and practical for preventing tissue spillage. Goggins and colleagues presented their findings in a poster at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco, California.
A total of 76 women at 4 institutions underwent laparoscopic or robotic multiport surgery (42 hysterectomy; 34 myomectomy). The average (SD) age and body mass index of the women were 43.16 (8.53) years and 26.47 kg/m2 (5.93), respectively. After surgical dissection, each specimen was placed into a containment bag that also included blue dye. The bag was insufflated intracorporeally and electromechanical morcellation and extraction of tissue were performed. The bag was evaluated visually for dye leakage or tears before and after the procedure.
Results
In one case, there was a tear in the bag before morcellation; no bag tears occurred during the morcellation process. Spillage of dye or tissue was noted in 7 cases, although containment bags were intact in each instance. One patient experienced intraoperative blood loss (3600 mL), and that procedure was converted to open radical hysterectomy. The most common pathologic finding was benign leiomyoma.
Conclusion
Goggins and colleagues concluded, “Contained tissue extraction using electromechanical morcellation and intracorporeally insufflated bags may provide a safe alternative to uncontained morcellation by decreasing the spread of tissue in the peritoneal cavity while allowing for the traditional benefits of laparoscopy.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Tissue extraction during laparoscopic or robot-assisted laparoscopic gynecologic surgery raises safety concerns for dissemination of tissue during the open, or uncontained, electromechanical morcellation process. Researchers from Brigham & Women’s Hospital in Boston, Massachusetts, investigated whether contained tissue extraction using power morcellators entirely within a bag is safe and practical for preventing tissue spillage. Goggins and colleagues presented their findings in a poster at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco, California.
A total of 76 women at 4 institutions underwent laparoscopic or robotic multiport surgery (42 hysterectomy; 34 myomectomy). The average (SD) age and body mass index of the women were 43.16 (8.53) years and 26.47 kg/m2 (5.93), respectively. After surgical dissection, each specimen was placed into a containment bag that also included blue dye. The bag was insufflated intracorporeally and electromechanical morcellation and extraction of tissue were performed. The bag was evaluated visually for dye leakage or tears before and after the procedure.
Results
In one case, there was a tear in the bag before morcellation; no bag tears occurred during the morcellation process. Spillage of dye or tissue was noted in 7 cases, although containment bags were intact in each instance. One patient experienced intraoperative blood loss (3600 mL), and that procedure was converted to open radical hysterectomy. The most common pathologic finding was benign leiomyoma.
Conclusion
Goggins and colleagues concluded, “Contained tissue extraction using electromechanical morcellation and intracorporeally insufflated bags may provide a safe alternative to uncontained morcellation by decreasing the spread of tissue in the peritoneal cavity while allowing for the traditional benefits of laparoscopy.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Goggins ER, Greenberg JA, Cohen SL, Morris SN, Brown DN, Einarsson JI. Efficacy of contained tissue extraction for minimizing tissue dissemination during laparoscopic hysterectomy and myomectomy. Obstet Gynecol. 2015;125(5)(suppl):29S.
Reference
- Goggins ER, Greenberg JA, Cohen SL, Morris SN, Brown DN, Einarsson JI. Efficacy of contained tissue extraction for minimizing tissue dissemination during laparoscopic hysterectomy and myomectomy. Obstet Gynecol. 2015;125(5)(suppl):29S.
Healing the Broken Places
May is Mental Health Month; in recognition of this—and our 25th anniversary—we decided to reprint this 2008 feature article on the state of mental health care in the United States. It’s the story I am personally most proud of telling, but rereading it today leads me to wonder: How much progress have we actually made? Please share your thoughts and experiences with me at [email protected]. —AMH
Broken. Grossly underfunded. In crisis. That’s how psychiatric and behavioral health specialists describe the current state of mental health care in the United States. The problems that plague the health care system in general—workforce shortages, barriers to access, and inadequate reimbursement—are only exacerbated in mental health.
“Mental illness isn’t glamorous,” says Don St. John, MA, PA-C, who practices in adult outpatient psychiatry at the University of Iowa Behavioral Health in Iowa City. Taking an example from the academic medical center setting, he adds, “It’s nice to have the cardiac surgery wing dedicated to or named after your family—but nobody wants a mental health wing named after them.”
Stigma is perhaps the greatest challenge with this patient population. “Until this country really embraces the notion that mental health is inherent in every aspect of a person’s general health,” says Gail W. Stuart, PhD, APRN, FAAN, Professor and Dean of the College of Nursing at Medical University of South Carolina, Charleston, “I think the stigma issue is going to continue to make it difficult to overcome these problems.”
FROM HOSPITALS TO JAILS
The current state of mental health care in the US is perhaps a direct result of the deinstitutionalization that occurred in the 1980s. By that time, most mental health hospitals were overcrowded and, in the worst cases, patients were subject to neglect and even abuse. (Recall, if you can, Geraldo Rivera skulking through the dark at Willowbrook State School in Staten Island, NY; his 1972 exposé brought the issue to the forefront.)
Following the public outcry over the treatment of these patients who—mentally ill or not—were people, there was a movement to reduce the number of long-term hospitalizations for mental illness. Along the way, the number of hospital beds available for mentally ill patients also declined, as freestanding hospitals and private facilities closed. What have these patients been left with?
“The thought was that people would be maintained in the community—there would be community support services, halfway houses, boarding homes, community-based programs,” says Catherine R. Judd, MS, PA-C, President of the Association of Psychiatric PAs, who works in the Department of Psychiatry at the University of Texas Southwestern Medical Center, Dallas. “The idea is good, but unfortunately, most of those programs have really not materialized to the extent or with the capacity to take care of the people who are out there.”
Without these services—and with an overtaxed health care system in general—many patients with mental illness find themselves adrift. And, eventually, incarcerated. An estimate from the US Department of Justice indicates that 24% of state and 21% of local prisoners have a recent history of mental illness. The largest psychiatric hospital in the country is the Los Angeles County Jail.
The problem is so widespread and so serious that both Judd and Jeanne Clement, EdD, APRN, BC, FAAN, President of the American Psychiatric Nurses Association (APNA), describe it in identical terms: “The jails and prisons have become the de facto mental health system.”
“More and more mentally ill people are in the streets, not receiving services, not taking medication as prescribed, with less-than-optimal case management in the community,” says Judd, who also works with the chronic mentally ill at the Dallas County Jail. “So, they are picked up on substance abuse–related charges or criminal trespassing or burglary. Consequently, they’re brought to jail.”
In Dallas, a divert court has been established, with the aim of getting chronic, persistent mentally ill patients “back to clinics and back on medication as quickly as possible without incarcerating them,” Judd notes. For such a program to succeed, of course, you need clinics—and providers—to divert these patients to.
Next: Problems of access >>
PROBLEMS OF ACCESS
Talk with clinicians who work in psychiatry, mental health, or behavioral health settings, and you’ll hear a familiar litany of problems. For one thing, there is the shortage of providers. “Here in Iowa, we’ve got areas where we have one psychiatrist covering five counties,” St. John says. “It’s almost impossible to get in with someone, and then when you do, it’s a five- or 10-minute appointment, because they’re just so busy.”
The number of clinicians choosing psychiatry—particularly psychiatric nursing—has declined significantly, perhaps due to insufficient funding for educational programs. “The highest number we had going into psychiatric nursing was when the National Institute of Mental Health, which was then separate from the NIH, had training grants,” explains Clement, who is the Director of the Graduate Specialty Program in Psychiatric–Mental Health Nursing at Ohio State University, Columbus. “And many of us who had those training grants are getting way past retirement age!”
The allure of other specialties also keeps people from mental health fields. “There are a lot of jobs and openings for PAs in psychiatry,” St. John says, “but there are a lot of jobs in orthopedics or surgery, too—and that’s what tends to draw them.”
The shortage of mental health care providers and subsequent lack of access to services means a larger role for primary care providers. High-profile expert panels have highlighted the need for integration of mental health into primary care settings—which St. John says is already largely the case.
“Most mental illness is treated in primary care, not in mental health settings,” he points out. “Mental health settings should really be reserved for the more challenging patients, the more difficult diagnoses and problems, and co-occurring illnesses.”
“Most primary care clinicians have some education in relationship to diagnosing and treating mild to moderate mental health issues, and then they refer on when needed,” Clement says. “The problem is, referring on is more and more difficult if there aren’t any people to refer to, or if waiting lists are as long as they currently are.”
Time is just as much of a problem in primary care as it is in specialty care, and when it comes to psychiatric and behavioral disorders, you can’t just order a lab test or an x-ray. “In psychiatry, you have to talk with the person and try to figure out what’s going on in their head and how that’s affecting their function,” St. John says. “It takes more time, and in primary care, that’s the problem they have. They’ve got appointments that may only have 10 minutes uled, and that’s not adequate to obtain a decent psychiatric history.”
The importance of both primary care providers and mental health specialists cannot be downplayed, because mental illnesses are among the most disabling and deadly. “If you look at disabling conditions, depression is right up there at the top,” St. John says. “Actually, it’s predicted that in the next three or four years, worldwide, depression will be the number one disabling illness.”
Anorexia is associated with a 15% death rate, and the completed suicide rate for persons with severe depression is also 15%. “If you were to look at one issue alone that we’re missing the boat on, it’s suicide,” Stuart says. “There are more suicides globally than there are deaths from war and violence combined—and the incidence of suicide is rising. So if, for example, a primary care provider sees someone who’s depressed, they have to go the next step and also ask about potential suicidal thought.”
Clement says it is equally important to integrate primary care services into mental health settings, since many patients with mental illnesses “are not going to show up in a private office in a primary care setting. And people with mental illness die 25 years earlier than the general population, from treatable medical illnesses.”
This is why, for example, the APNA is partnering with the Smoking Cessation Leadership Center. “Persons with mental illness are purchasing approximately half of the cigarettes that are being bought in the US,” Clement says. “And many of the treatable medical illnesses that people are dying from are related to smoking. It’s a whole person you’re working with, not just a brain or a body.”
REIMBURSEMENT ISSUE
Reimbursement is one of the major deterrents to the pursuit of a career in mental health care. “The whole reimbursement issue makes it difficult to attract people to work in mental health, particularly in community-based clinics, state hospitals, prisons, and jails,” which Judd says results in a lack of services for the seriously mentally ill and decreased access for people of low income.
The biggest problem is parity—or rather, the lack of it. What services are covered and at what rate tends to vary by state, and mental health is often not covered at the same rate as physical health. “There are a number of states that now have parity in mental health,” Clement observes. “If insurance is offered for physical health and [includes] mental health coverage, it has to be at exactly the same level as physical health, in terms of copays and lifetime limits.” But even so, there is not always parity in parity.
Furthermore, many people who need mental health services fall under the Medicaid program, which is state-based and just as variable. “Definitions of ‘medical necessity’ differ, and providers don’t get paid unless they can document according to medical necessity,” Clement says. “Even though what people—particularly those in the Medicaid and public mental health systems—need, along with their treatment, is a community-based program that helps people find jobs and housing. But that’s not ‘medical necessity.’”
Another problem is the sheer expense of some of the medications for mental disorders. “A lot of the drugs that we use to treat serious mental illnesses are horrendously expensive,” St. John notes. “They’ll almost bankrupt some states.…We just don’t have those budgets.”
Achieving parity and improving reimbursement is a slow process. Clement has been involved at the federal level with a parity bill, but as she notes, “that has not been resolved in terms of the differences between the House and the Senate.” Since so many of the programs are administered at a state level anyway, some suggest that might be a good place to begin working on reform.
In October 2007, the Annapolis Coalition, of which Stuart is President of the Board of Directors, released an action plan for reforming the mental health system—particularly for addressing workforce needs. The report (available at www.annapoliscoalition.org) includes the most specific recommendations possible in an overarching “framework” document, and Stuart says the coalition is currently working with some states—including North Carolina, Connecticut, New Mexico, and California—to identify and prioritize their needs and determine how best to tailor the plan to them.
“We’re really approaching it not at a federal level but seeing that the true change would come about at a state level,” Stuart says. “The need is derived differently by each state. If I can use the analogy, it’s a little bit like having a general way of approaching hypertension, but then you tailor it to the individual.”
Whether at the state or federal level, St. John thinks major changes to reimbursement for mental health care will require a cultural shift. “We reimburse for activity, we reimburse for procedures; we don’t reimburse for time spent or for decision making or thinking,” he points out. When a clinician is being reimbursed 50% (compared to 90% for other medical care), or $12 to $15 per visit for providing medication management, “You have to see large volumes of people in order to get reimbursed enough to pay for yourself and your staff.”
In the current economic climate, finding the money is going to take some shuffling. “It would be unrealistic to say that there are new dollars out there, because clearly there are not,” Stuart says. “So I think the issue is to reallocate the current resources that are out there and evaluate, Are we getting the best return on our investment of these dollars?”
The irony is that the people with the greatest needs for treatment, monitoring, and support services are the ones who face the biggest barriers to accessing care. “Services are more readily available to people who have jobs, have insurance—which would tell you in and of itself they’re probably higher functioning to start with,” Judd says. “I mean, if you’re having stress holding down a job, you’re probably higher functioning at your baseline than the homeless person who is living in the streets and under bridges and doesn’t go to shelters because they’re too paranoid to be around other people.”
Continue for taking the shame out of mental illness >>
TAKING THE SHAME OUT OF MENTAL ILLNESS
No discussion of mental health care can be complete without addressing the stigma associated with mental illness. Americans may have responded with outrage when they saw the deplorable conditions at mental hospitals, but many are still leery of being associated with a mental illness, whether in themselves or in a family member. And the cases that garner the most media attention are not necessarily the ones that reduce stigma.
What Americans see on the nightly news is the schizophrenic man who stops taking his medication and then stabs another man to death while he’s waiting for a train. Or the mother with chronic depression who can’t get out of bed until someone notices her kids look dirty and underfed, and Social Services steps in to remove them from the home. Do we, as a society, recognize the double tragedy of those situations? Or do we shake our heads in disgust, slap on a “crazy guy” or “bad mom” label, and change the channel?
Public service campaigns are trying to reduce the stigma associated with mental illness, to point out that it can affect anyone. The faces of the mentally ill are diverse: There’s the grandfather with Alzheimer’s disease who mistakes his granddaughter for his daughter. The 2-year-old autistic girl who has difficulty connecting with family and friends. The soldiers returning from the war zones in Iraq and Afghanistan, struggling with posttraumatic stress disorder (PTSD).
“The message that is being sent that needs to be broadcast more and heard with a different ear is that there is no health without mental health,” Clement says. St. John adds that it will take “a lot of time and education” to get that message out to the public, to let people know that it’s OK—in fact, it’s better—to acknowledge mental illness and seek help for it.
Stuart thinks the troops’ return from overseas, which is generating more stories about traumatic brain injury, PTSD, depression, and suicide, may start to turn the tide. “Perhaps because these are our veterans and our heroes, they’ve served the country, it’s opening up a public discussion in a way that’s different from seeing the aberrant, violent patient who does something very disruptive,” she says. “So, in a sense—and this sounds odd—we’re normalizing mental health problems, saying that all kinds of people from all walks of life can develop mental health problems, just as they can develop physical health problems.”
The key will be ensuring that the pendulum doesn’t swing too far the other way and cause the “stigma reduction” movement to generate its own problems. “On the one hand, we’re trying to destigmatize mental illness, but on the other hand, it [sometimes] seems like we’re calling any aberrant behavior or problems in life, stress or problems of adjustment, a mental illness,” Judd observes.
There are certain niches in which mental illness seems almost “trendy,” and industry advertising may encourage that. “Pharmaceutical companies are putting advertisements out there that would imply, ‘Gee, you’re getting divorced because you had conflict in your marriage—maybe you have bipolar disorder’ or ‘Your child isn’t doing well in school, so surely he has ADHD and needs to be on medication,’” Judd says. “There’s this promoting of drugs for anything and everything. And so that’s kind of the other extreme, where any problems in life in functioning must be because of a mental illness, and therefore you need a drug.”
RESTORED TO LIFE
With such a grim picture of mental health care in the US, it hardly seems surprising that clinicians don’t flock to the specialty. Yet, Clement, Judd, St. John, and Stuart did. Why?
For Judd, “the science of it is extremely interesting.” She thinks that as psychiatry becomes more biological and clinicians delve more deeply into what is affecting a patient’s function (Is it trauma, prenatal influences, infection, genetics?) and how that impacts treatment choices, more practitioners might choose mental health care. But the biggest reward, she says, is seeing people “return to a higher level of functioning.”
“I have never, ever sat down with a client that I have not felt privileged to be allowed into their lives,” says Clement, who has been a nurse for 49 years and a psychiatric nurse for 47 of them. “People allow clinicians into their lives in a very different way than they do anybody else.”
That can be especially true in mental health, when clinicians must interact on a very intimate level with their patients. It can be challenging, frustrating, even devastating (such as when a patient takes his or her own life). But it can also be infinitely rewarding. That is why St. John moved from family practice and emergency settings to psychiatry, where he has spent the past 15 years.
“When you see people who kind of get back into life and start working more toward their life goals, and you start seeing them get back into their family and their work and their social function, perking up and engaging in the world,” he says, his voice conveying a deep sense of fulfillment, “there’s just nothing more rewarding than that.”
Reprinted from Clinician Reviews. 2008;18(10):cover, 6-8.
May is Mental Health Month; in recognition of this—and our 25th anniversary—we decided to reprint this 2008 feature article on the state of mental health care in the United States. It’s the story I am personally most proud of telling, but rereading it today leads me to wonder: How much progress have we actually made? Please share your thoughts and experiences with me at [email protected]. —AMH
Broken. Grossly underfunded. In crisis. That’s how psychiatric and behavioral health specialists describe the current state of mental health care in the United States. The problems that plague the health care system in general—workforce shortages, barriers to access, and inadequate reimbursement—are only exacerbated in mental health.
“Mental illness isn’t glamorous,” says Don St. John, MA, PA-C, who practices in adult outpatient psychiatry at the University of Iowa Behavioral Health in Iowa City. Taking an example from the academic medical center setting, he adds, “It’s nice to have the cardiac surgery wing dedicated to or named after your family—but nobody wants a mental health wing named after them.”
Stigma is perhaps the greatest challenge with this patient population. “Until this country really embraces the notion that mental health is inherent in every aspect of a person’s general health,” says Gail W. Stuart, PhD, APRN, FAAN, Professor and Dean of the College of Nursing at Medical University of South Carolina, Charleston, “I think the stigma issue is going to continue to make it difficult to overcome these problems.”
FROM HOSPITALS TO JAILS
The current state of mental health care in the US is perhaps a direct result of the deinstitutionalization that occurred in the 1980s. By that time, most mental health hospitals were overcrowded and, in the worst cases, patients were subject to neglect and even abuse. (Recall, if you can, Geraldo Rivera skulking through the dark at Willowbrook State School in Staten Island, NY; his 1972 exposé brought the issue to the forefront.)
Following the public outcry over the treatment of these patients who—mentally ill or not—were people, there was a movement to reduce the number of long-term hospitalizations for mental illness. Along the way, the number of hospital beds available for mentally ill patients also declined, as freestanding hospitals and private facilities closed. What have these patients been left with?
“The thought was that people would be maintained in the community—there would be community support services, halfway houses, boarding homes, community-based programs,” says Catherine R. Judd, MS, PA-C, President of the Association of Psychiatric PAs, who works in the Department of Psychiatry at the University of Texas Southwestern Medical Center, Dallas. “The idea is good, but unfortunately, most of those programs have really not materialized to the extent or with the capacity to take care of the people who are out there.”
Without these services—and with an overtaxed health care system in general—many patients with mental illness find themselves adrift. And, eventually, incarcerated. An estimate from the US Department of Justice indicates that 24% of state and 21% of local prisoners have a recent history of mental illness. The largest psychiatric hospital in the country is the Los Angeles County Jail.
The problem is so widespread and so serious that both Judd and Jeanne Clement, EdD, APRN, BC, FAAN, President of the American Psychiatric Nurses Association (APNA), describe it in identical terms: “The jails and prisons have become the de facto mental health system.”
“More and more mentally ill people are in the streets, not receiving services, not taking medication as prescribed, with less-than-optimal case management in the community,” says Judd, who also works with the chronic mentally ill at the Dallas County Jail. “So, they are picked up on substance abuse–related charges or criminal trespassing or burglary. Consequently, they’re brought to jail.”
In Dallas, a divert court has been established, with the aim of getting chronic, persistent mentally ill patients “back to clinics and back on medication as quickly as possible without incarcerating them,” Judd notes. For such a program to succeed, of course, you need clinics—and providers—to divert these patients to.
Next: Problems of access >>
PROBLEMS OF ACCESS
Talk with clinicians who work in psychiatry, mental health, or behavioral health settings, and you’ll hear a familiar litany of problems. For one thing, there is the shortage of providers. “Here in Iowa, we’ve got areas where we have one psychiatrist covering five counties,” St. John says. “It’s almost impossible to get in with someone, and then when you do, it’s a five- or 10-minute appointment, because they’re just so busy.”
The number of clinicians choosing psychiatry—particularly psychiatric nursing—has declined significantly, perhaps due to insufficient funding for educational programs. “The highest number we had going into psychiatric nursing was when the National Institute of Mental Health, which was then separate from the NIH, had training grants,” explains Clement, who is the Director of the Graduate Specialty Program in Psychiatric–Mental Health Nursing at Ohio State University, Columbus. “And many of us who had those training grants are getting way past retirement age!”
The allure of other specialties also keeps people from mental health fields. “There are a lot of jobs and openings for PAs in psychiatry,” St. John says, “but there are a lot of jobs in orthopedics or surgery, too—and that’s what tends to draw them.”
The shortage of mental health care providers and subsequent lack of access to services means a larger role for primary care providers. High-profile expert panels have highlighted the need for integration of mental health into primary care settings—which St. John says is already largely the case.
“Most mental illness is treated in primary care, not in mental health settings,” he points out. “Mental health settings should really be reserved for the more challenging patients, the more difficult diagnoses and problems, and co-occurring illnesses.”
“Most primary care clinicians have some education in relationship to diagnosing and treating mild to moderate mental health issues, and then they refer on when needed,” Clement says. “The problem is, referring on is more and more difficult if there aren’t any people to refer to, or if waiting lists are as long as they currently are.”
Time is just as much of a problem in primary care as it is in specialty care, and when it comes to psychiatric and behavioral disorders, you can’t just order a lab test or an x-ray. “In psychiatry, you have to talk with the person and try to figure out what’s going on in their head and how that’s affecting their function,” St. John says. “It takes more time, and in primary care, that’s the problem they have. They’ve got appointments that may only have 10 minutes uled, and that’s not adequate to obtain a decent psychiatric history.”
The importance of both primary care providers and mental health specialists cannot be downplayed, because mental illnesses are among the most disabling and deadly. “If you look at disabling conditions, depression is right up there at the top,” St. John says. “Actually, it’s predicted that in the next three or four years, worldwide, depression will be the number one disabling illness.”
Anorexia is associated with a 15% death rate, and the completed suicide rate for persons with severe depression is also 15%. “If you were to look at one issue alone that we’re missing the boat on, it’s suicide,” Stuart says. “There are more suicides globally than there are deaths from war and violence combined—and the incidence of suicide is rising. So if, for example, a primary care provider sees someone who’s depressed, they have to go the next step and also ask about potential suicidal thought.”
Clement says it is equally important to integrate primary care services into mental health settings, since many patients with mental illnesses “are not going to show up in a private office in a primary care setting. And people with mental illness die 25 years earlier than the general population, from treatable medical illnesses.”
This is why, for example, the APNA is partnering with the Smoking Cessation Leadership Center. “Persons with mental illness are purchasing approximately half of the cigarettes that are being bought in the US,” Clement says. “And many of the treatable medical illnesses that people are dying from are related to smoking. It’s a whole person you’re working with, not just a brain or a body.”
REIMBURSEMENT ISSUE
Reimbursement is one of the major deterrents to the pursuit of a career in mental health care. “The whole reimbursement issue makes it difficult to attract people to work in mental health, particularly in community-based clinics, state hospitals, prisons, and jails,” which Judd says results in a lack of services for the seriously mentally ill and decreased access for people of low income.
The biggest problem is parity—or rather, the lack of it. What services are covered and at what rate tends to vary by state, and mental health is often not covered at the same rate as physical health. “There are a number of states that now have parity in mental health,” Clement observes. “If insurance is offered for physical health and [includes] mental health coverage, it has to be at exactly the same level as physical health, in terms of copays and lifetime limits.” But even so, there is not always parity in parity.
Furthermore, many people who need mental health services fall under the Medicaid program, which is state-based and just as variable. “Definitions of ‘medical necessity’ differ, and providers don’t get paid unless they can document according to medical necessity,” Clement says. “Even though what people—particularly those in the Medicaid and public mental health systems—need, along with their treatment, is a community-based program that helps people find jobs and housing. But that’s not ‘medical necessity.’”
Another problem is the sheer expense of some of the medications for mental disorders. “A lot of the drugs that we use to treat serious mental illnesses are horrendously expensive,” St. John notes. “They’ll almost bankrupt some states.…We just don’t have those budgets.”
Achieving parity and improving reimbursement is a slow process. Clement has been involved at the federal level with a parity bill, but as she notes, “that has not been resolved in terms of the differences between the House and the Senate.” Since so many of the programs are administered at a state level anyway, some suggest that might be a good place to begin working on reform.
In October 2007, the Annapolis Coalition, of which Stuart is President of the Board of Directors, released an action plan for reforming the mental health system—particularly for addressing workforce needs. The report (available at www.annapoliscoalition.org) includes the most specific recommendations possible in an overarching “framework” document, and Stuart says the coalition is currently working with some states—including North Carolina, Connecticut, New Mexico, and California—to identify and prioritize their needs and determine how best to tailor the plan to them.
“We’re really approaching it not at a federal level but seeing that the true change would come about at a state level,” Stuart says. “The need is derived differently by each state. If I can use the analogy, it’s a little bit like having a general way of approaching hypertension, but then you tailor it to the individual.”
Whether at the state or federal level, St. John thinks major changes to reimbursement for mental health care will require a cultural shift. “We reimburse for activity, we reimburse for procedures; we don’t reimburse for time spent or for decision making or thinking,” he points out. When a clinician is being reimbursed 50% (compared to 90% for other medical care), or $12 to $15 per visit for providing medication management, “You have to see large volumes of people in order to get reimbursed enough to pay for yourself and your staff.”
In the current economic climate, finding the money is going to take some shuffling. “It would be unrealistic to say that there are new dollars out there, because clearly there are not,” Stuart says. “So I think the issue is to reallocate the current resources that are out there and evaluate, Are we getting the best return on our investment of these dollars?”
The irony is that the people with the greatest needs for treatment, monitoring, and support services are the ones who face the biggest barriers to accessing care. “Services are more readily available to people who have jobs, have insurance—which would tell you in and of itself they’re probably higher functioning to start with,” Judd says. “I mean, if you’re having stress holding down a job, you’re probably higher functioning at your baseline than the homeless person who is living in the streets and under bridges and doesn’t go to shelters because they’re too paranoid to be around other people.”
Continue for taking the shame out of mental illness >>
TAKING THE SHAME OUT OF MENTAL ILLNESS
No discussion of mental health care can be complete without addressing the stigma associated with mental illness. Americans may have responded with outrage when they saw the deplorable conditions at mental hospitals, but many are still leery of being associated with a mental illness, whether in themselves or in a family member. And the cases that garner the most media attention are not necessarily the ones that reduce stigma.
What Americans see on the nightly news is the schizophrenic man who stops taking his medication and then stabs another man to death while he’s waiting for a train. Or the mother with chronic depression who can’t get out of bed until someone notices her kids look dirty and underfed, and Social Services steps in to remove them from the home. Do we, as a society, recognize the double tragedy of those situations? Or do we shake our heads in disgust, slap on a “crazy guy” or “bad mom” label, and change the channel?
Public service campaigns are trying to reduce the stigma associated with mental illness, to point out that it can affect anyone. The faces of the mentally ill are diverse: There’s the grandfather with Alzheimer’s disease who mistakes his granddaughter for his daughter. The 2-year-old autistic girl who has difficulty connecting with family and friends. The soldiers returning from the war zones in Iraq and Afghanistan, struggling with posttraumatic stress disorder (PTSD).
“The message that is being sent that needs to be broadcast more and heard with a different ear is that there is no health without mental health,” Clement says. St. John adds that it will take “a lot of time and education” to get that message out to the public, to let people know that it’s OK—in fact, it’s better—to acknowledge mental illness and seek help for it.
Stuart thinks the troops’ return from overseas, which is generating more stories about traumatic brain injury, PTSD, depression, and suicide, may start to turn the tide. “Perhaps because these are our veterans and our heroes, they’ve served the country, it’s opening up a public discussion in a way that’s different from seeing the aberrant, violent patient who does something very disruptive,” she says. “So, in a sense—and this sounds odd—we’re normalizing mental health problems, saying that all kinds of people from all walks of life can develop mental health problems, just as they can develop physical health problems.”
The key will be ensuring that the pendulum doesn’t swing too far the other way and cause the “stigma reduction” movement to generate its own problems. “On the one hand, we’re trying to destigmatize mental illness, but on the other hand, it [sometimes] seems like we’re calling any aberrant behavior or problems in life, stress or problems of adjustment, a mental illness,” Judd observes.
There are certain niches in which mental illness seems almost “trendy,” and industry advertising may encourage that. “Pharmaceutical companies are putting advertisements out there that would imply, ‘Gee, you’re getting divorced because you had conflict in your marriage—maybe you have bipolar disorder’ or ‘Your child isn’t doing well in school, so surely he has ADHD and needs to be on medication,’” Judd says. “There’s this promoting of drugs for anything and everything. And so that’s kind of the other extreme, where any problems in life in functioning must be because of a mental illness, and therefore you need a drug.”
RESTORED TO LIFE
With such a grim picture of mental health care in the US, it hardly seems surprising that clinicians don’t flock to the specialty. Yet, Clement, Judd, St. John, and Stuart did. Why?
For Judd, “the science of it is extremely interesting.” She thinks that as psychiatry becomes more biological and clinicians delve more deeply into what is affecting a patient’s function (Is it trauma, prenatal influences, infection, genetics?) and how that impacts treatment choices, more practitioners might choose mental health care. But the biggest reward, she says, is seeing people “return to a higher level of functioning.”
“I have never, ever sat down with a client that I have not felt privileged to be allowed into their lives,” says Clement, who has been a nurse for 49 years and a psychiatric nurse for 47 of them. “People allow clinicians into their lives in a very different way than they do anybody else.”
That can be especially true in mental health, when clinicians must interact on a very intimate level with their patients. It can be challenging, frustrating, even devastating (such as when a patient takes his or her own life). But it can also be infinitely rewarding. That is why St. John moved from family practice and emergency settings to psychiatry, where he has spent the past 15 years.
“When you see people who kind of get back into life and start working more toward their life goals, and you start seeing them get back into their family and their work and their social function, perking up and engaging in the world,” he says, his voice conveying a deep sense of fulfillment, “there’s just nothing more rewarding than that.”
Reprinted from Clinician Reviews. 2008;18(10):cover, 6-8.
May is Mental Health Month; in recognition of this—and our 25th anniversary—we decided to reprint this 2008 feature article on the state of mental health care in the United States. It’s the story I am personally most proud of telling, but rereading it today leads me to wonder: How much progress have we actually made? Please share your thoughts and experiences with me at [email protected]. —AMH
Broken. Grossly underfunded. In crisis. That’s how psychiatric and behavioral health specialists describe the current state of mental health care in the United States. The problems that plague the health care system in general—workforce shortages, barriers to access, and inadequate reimbursement—are only exacerbated in mental health.
“Mental illness isn’t glamorous,” says Don St. John, MA, PA-C, who practices in adult outpatient psychiatry at the University of Iowa Behavioral Health in Iowa City. Taking an example from the academic medical center setting, he adds, “It’s nice to have the cardiac surgery wing dedicated to or named after your family—but nobody wants a mental health wing named after them.”
Stigma is perhaps the greatest challenge with this patient population. “Until this country really embraces the notion that mental health is inherent in every aspect of a person’s general health,” says Gail W. Stuart, PhD, APRN, FAAN, Professor and Dean of the College of Nursing at Medical University of South Carolina, Charleston, “I think the stigma issue is going to continue to make it difficult to overcome these problems.”
FROM HOSPITALS TO JAILS
The current state of mental health care in the US is perhaps a direct result of the deinstitutionalization that occurred in the 1980s. By that time, most mental health hospitals were overcrowded and, in the worst cases, patients were subject to neglect and even abuse. (Recall, if you can, Geraldo Rivera skulking through the dark at Willowbrook State School in Staten Island, NY; his 1972 exposé brought the issue to the forefront.)
Following the public outcry over the treatment of these patients who—mentally ill or not—were people, there was a movement to reduce the number of long-term hospitalizations for mental illness. Along the way, the number of hospital beds available for mentally ill patients also declined, as freestanding hospitals and private facilities closed. What have these patients been left with?
“The thought was that people would be maintained in the community—there would be community support services, halfway houses, boarding homes, community-based programs,” says Catherine R. Judd, MS, PA-C, President of the Association of Psychiatric PAs, who works in the Department of Psychiatry at the University of Texas Southwestern Medical Center, Dallas. “The idea is good, but unfortunately, most of those programs have really not materialized to the extent or with the capacity to take care of the people who are out there.”
Without these services—and with an overtaxed health care system in general—many patients with mental illness find themselves adrift. And, eventually, incarcerated. An estimate from the US Department of Justice indicates that 24% of state and 21% of local prisoners have a recent history of mental illness. The largest psychiatric hospital in the country is the Los Angeles County Jail.
The problem is so widespread and so serious that both Judd and Jeanne Clement, EdD, APRN, BC, FAAN, President of the American Psychiatric Nurses Association (APNA), describe it in identical terms: “The jails and prisons have become the de facto mental health system.”
“More and more mentally ill people are in the streets, not receiving services, not taking medication as prescribed, with less-than-optimal case management in the community,” says Judd, who also works with the chronic mentally ill at the Dallas County Jail. “So, they are picked up on substance abuse–related charges or criminal trespassing or burglary. Consequently, they’re brought to jail.”
In Dallas, a divert court has been established, with the aim of getting chronic, persistent mentally ill patients “back to clinics and back on medication as quickly as possible without incarcerating them,” Judd notes. For such a program to succeed, of course, you need clinics—and providers—to divert these patients to.
Next: Problems of access >>
PROBLEMS OF ACCESS
Talk with clinicians who work in psychiatry, mental health, or behavioral health settings, and you’ll hear a familiar litany of problems. For one thing, there is the shortage of providers. “Here in Iowa, we’ve got areas where we have one psychiatrist covering five counties,” St. John says. “It’s almost impossible to get in with someone, and then when you do, it’s a five- or 10-minute appointment, because they’re just so busy.”
The number of clinicians choosing psychiatry—particularly psychiatric nursing—has declined significantly, perhaps due to insufficient funding for educational programs. “The highest number we had going into psychiatric nursing was when the National Institute of Mental Health, which was then separate from the NIH, had training grants,” explains Clement, who is the Director of the Graduate Specialty Program in Psychiatric–Mental Health Nursing at Ohio State University, Columbus. “And many of us who had those training grants are getting way past retirement age!”
The allure of other specialties also keeps people from mental health fields. “There are a lot of jobs and openings for PAs in psychiatry,” St. John says, “but there are a lot of jobs in orthopedics or surgery, too—and that’s what tends to draw them.”
The shortage of mental health care providers and subsequent lack of access to services means a larger role for primary care providers. High-profile expert panels have highlighted the need for integration of mental health into primary care settings—which St. John says is already largely the case.
“Most mental illness is treated in primary care, not in mental health settings,” he points out. “Mental health settings should really be reserved for the more challenging patients, the more difficult diagnoses and problems, and co-occurring illnesses.”
“Most primary care clinicians have some education in relationship to diagnosing and treating mild to moderate mental health issues, and then they refer on when needed,” Clement says. “The problem is, referring on is more and more difficult if there aren’t any people to refer to, or if waiting lists are as long as they currently are.”
Time is just as much of a problem in primary care as it is in specialty care, and when it comes to psychiatric and behavioral disorders, you can’t just order a lab test or an x-ray. “In psychiatry, you have to talk with the person and try to figure out what’s going on in their head and how that’s affecting their function,” St. John says. “It takes more time, and in primary care, that’s the problem they have. They’ve got appointments that may only have 10 minutes uled, and that’s not adequate to obtain a decent psychiatric history.”
The importance of both primary care providers and mental health specialists cannot be downplayed, because mental illnesses are among the most disabling and deadly. “If you look at disabling conditions, depression is right up there at the top,” St. John says. “Actually, it’s predicted that in the next three or four years, worldwide, depression will be the number one disabling illness.”
Anorexia is associated with a 15% death rate, and the completed suicide rate for persons with severe depression is also 15%. “If you were to look at one issue alone that we’re missing the boat on, it’s suicide,” Stuart says. “There are more suicides globally than there are deaths from war and violence combined—and the incidence of suicide is rising. So if, for example, a primary care provider sees someone who’s depressed, they have to go the next step and also ask about potential suicidal thought.”
Clement says it is equally important to integrate primary care services into mental health settings, since many patients with mental illnesses “are not going to show up in a private office in a primary care setting. And people with mental illness die 25 years earlier than the general population, from treatable medical illnesses.”
This is why, for example, the APNA is partnering with the Smoking Cessation Leadership Center. “Persons with mental illness are purchasing approximately half of the cigarettes that are being bought in the US,” Clement says. “And many of the treatable medical illnesses that people are dying from are related to smoking. It’s a whole person you’re working with, not just a brain or a body.”
REIMBURSEMENT ISSUE
Reimbursement is one of the major deterrents to the pursuit of a career in mental health care. “The whole reimbursement issue makes it difficult to attract people to work in mental health, particularly in community-based clinics, state hospitals, prisons, and jails,” which Judd says results in a lack of services for the seriously mentally ill and decreased access for people of low income.
The biggest problem is parity—or rather, the lack of it. What services are covered and at what rate tends to vary by state, and mental health is often not covered at the same rate as physical health. “There are a number of states that now have parity in mental health,” Clement observes. “If insurance is offered for physical health and [includes] mental health coverage, it has to be at exactly the same level as physical health, in terms of copays and lifetime limits.” But even so, there is not always parity in parity.
Furthermore, many people who need mental health services fall under the Medicaid program, which is state-based and just as variable. “Definitions of ‘medical necessity’ differ, and providers don’t get paid unless they can document according to medical necessity,” Clement says. “Even though what people—particularly those in the Medicaid and public mental health systems—need, along with their treatment, is a community-based program that helps people find jobs and housing. But that’s not ‘medical necessity.’”
Another problem is the sheer expense of some of the medications for mental disorders. “A lot of the drugs that we use to treat serious mental illnesses are horrendously expensive,” St. John notes. “They’ll almost bankrupt some states.…We just don’t have those budgets.”
Achieving parity and improving reimbursement is a slow process. Clement has been involved at the federal level with a parity bill, but as she notes, “that has not been resolved in terms of the differences between the House and the Senate.” Since so many of the programs are administered at a state level anyway, some suggest that might be a good place to begin working on reform.
In October 2007, the Annapolis Coalition, of which Stuart is President of the Board of Directors, released an action plan for reforming the mental health system—particularly for addressing workforce needs. The report (available at www.annapoliscoalition.org) includes the most specific recommendations possible in an overarching “framework” document, and Stuart says the coalition is currently working with some states—including North Carolina, Connecticut, New Mexico, and California—to identify and prioritize their needs and determine how best to tailor the plan to them.
“We’re really approaching it not at a federal level but seeing that the true change would come about at a state level,” Stuart says. “The need is derived differently by each state. If I can use the analogy, it’s a little bit like having a general way of approaching hypertension, but then you tailor it to the individual.”
Whether at the state or federal level, St. John thinks major changes to reimbursement for mental health care will require a cultural shift. “We reimburse for activity, we reimburse for procedures; we don’t reimburse for time spent or for decision making or thinking,” he points out. When a clinician is being reimbursed 50% (compared to 90% for other medical care), or $12 to $15 per visit for providing medication management, “You have to see large volumes of people in order to get reimbursed enough to pay for yourself and your staff.”
In the current economic climate, finding the money is going to take some shuffling. “It would be unrealistic to say that there are new dollars out there, because clearly there are not,” Stuart says. “So I think the issue is to reallocate the current resources that are out there and evaluate, Are we getting the best return on our investment of these dollars?”
The irony is that the people with the greatest needs for treatment, monitoring, and support services are the ones who face the biggest barriers to accessing care. “Services are more readily available to people who have jobs, have insurance—which would tell you in and of itself they’re probably higher functioning to start with,” Judd says. “I mean, if you’re having stress holding down a job, you’re probably higher functioning at your baseline than the homeless person who is living in the streets and under bridges and doesn’t go to shelters because they’re too paranoid to be around other people.”
Continue for taking the shame out of mental illness >>
TAKING THE SHAME OUT OF MENTAL ILLNESS
No discussion of mental health care can be complete without addressing the stigma associated with mental illness. Americans may have responded with outrage when they saw the deplorable conditions at mental hospitals, but many are still leery of being associated with a mental illness, whether in themselves or in a family member. And the cases that garner the most media attention are not necessarily the ones that reduce stigma.
What Americans see on the nightly news is the schizophrenic man who stops taking his medication and then stabs another man to death while he’s waiting for a train. Or the mother with chronic depression who can’t get out of bed until someone notices her kids look dirty and underfed, and Social Services steps in to remove them from the home. Do we, as a society, recognize the double tragedy of those situations? Or do we shake our heads in disgust, slap on a “crazy guy” or “bad mom” label, and change the channel?
Public service campaigns are trying to reduce the stigma associated with mental illness, to point out that it can affect anyone. The faces of the mentally ill are diverse: There’s the grandfather with Alzheimer’s disease who mistakes his granddaughter for his daughter. The 2-year-old autistic girl who has difficulty connecting with family and friends. The soldiers returning from the war zones in Iraq and Afghanistan, struggling with posttraumatic stress disorder (PTSD).
“The message that is being sent that needs to be broadcast more and heard with a different ear is that there is no health without mental health,” Clement says. St. John adds that it will take “a lot of time and education” to get that message out to the public, to let people know that it’s OK—in fact, it’s better—to acknowledge mental illness and seek help for it.
Stuart thinks the troops’ return from overseas, which is generating more stories about traumatic brain injury, PTSD, depression, and suicide, may start to turn the tide. “Perhaps because these are our veterans and our heroes, they’ve served the country, it’s opening up a public discussion in a way that’s different from seeing the aberrant, violent patient who does something very disruptive,” she says. “So, in a sense—and this sounds odd—we’re normalizing mental health problems, saying that all kinds of people from all walks of life can develop mental health problems, just as they can develop physical health problems.”
The key will be ensuring that the pendulum doesn’t swing too far the other way and cause the “stigma reduction” movement to generate its own problems. “On the one hand, we’re trying to destigmatize mental illness, but on the other hand, it [sometimes] seems like we’re calling any aberrant behavior or problems in life, stress or problems of adjustment, a mental illness,” Judd observes.
There are certain niches in which mental illness seems almost “trendy,” and industry advertising may encourage that. “Pharmaceutical companies are putting advertisements out there that would imply, ‘Gee, you’re getting divorced because you had conflict in your marriage—maybe you have bipolar disorder’ or ‘Your child isn’t doing well in school, so surely he has ADHD and needs to be on medication,’” Judd says. “There’s this promoting of drugs for anything and everything. And so that’s kind of the other extreme, where any problems in life in functioning must be because of a mental illness, and therefore you need a drug.”
RESTORED TO LIFE
With such a grim picture of mental health care in the US, it hardly seems surprising that clinicians don’t flock to the specialty. Yet, Clement, Judd, St. John, and Stuart did. Why?
For Judd, “the science of it is extremely interesting.” She thinks that as psychiatry becomes more biological and clinicians delve more deeply into what is affecting a patient’s function (Is it trauma, prenatal influences, infection, genetics?) and how that impacts treatment choices, more practitioners might choose mental health care. But the biggest reward, she says, is seeing people “return to a higher level of functioning.”
“I have never, ever sat down with a client that I have not felt privileged to be allowed into their lives,” says Clement, who has been a nurse for 49 years and a psychiatric nurse for 47 of them. “People allow clinicians into their lives in a very different way than they do anybody else.”
That can be especially true in mental health, when clinicians must interact on a very intimate level with their patients. It can be challenging, frustrating, even devastating (such as when a patient takes his or her own life). But it can also be infinitely rewarding. That is why St. John moved from family practice and emergency settings to psychiatry, where he has spent the past 15 years.
“When you see people who kind of get back into life and start working more toward their life goals, and you start seeing them get back into their family and their work and their social function, perking up and engaging in the world,” he says, his voice conveying a deep sense of fulfillment, “there’s just nothing more rewarding than that.”
Reprinted from Clinician Reviews. 2008;18(10):cover, 6-8.
ObGyns, and US women, are embracing LARCs
Use of long-acting reversible contraception (LARC) has increased nearly 5-fold in the last decade, reported the Centers for Disease Control and Prevention (CDC) in a National Center for Health Statistics (NCHS) Data Brief on the trends in LARC use among US women aged 15 to 44.1
Data from the National Survey of Family Growth indicate that LARCs, which include intrauterine devices (IUDs) and subdermal hormonal implants, are gaining popularity because of their high efficacy in preventing unintended pregnancies. LARCs have demonstrated greater efficacy in preventing unintended pregnancy among all women compared with other contraceptive methods, including the oral contraceptive pill and the transdermal patch.
Age-related trends
For women aged 15 to 44, LARC use doubled between 2002 (1.5%) and the period 2006–2010 (3.8%) and then nearly doubled again for 2011–2013 (7.2%). IUD use increased 83% from the 2006–2010 period (3.5%) to the 2011–2013 period (6.4%). Implant use tripled from 2002 (0.3%) to the 2011–2013 period (0.8%).
LARC use was higher among women aged 25 to 34 than among women aged 15 to 24. The difference in LARC use was not statistically significant between women aged 25 to 34 and women aged 35 to 44.
- LARC use increased nearly 4-fold for women aged 15 to 24 between 2002 (0.6%) and 2006–2010 (2.3%), and doubled again for 2011–2013 (5.0%).
- LARC use almost doubled among women aged 25 to 34 from 2006–2010 to 2011–2013 (5.3% to 11.1%).
- LARC use tripled between 2002 (1.1%) and 2006–2010 (3.8%) for women aged 35 to 44, and increased to 5.3% in 2011–2013.
Patterns of use by race
Although LARC use tripled for non-Hispanic white women and increased 4-fold for non-Hispanic black women between 2002 and 2006–2010, use among Hispanic women declined 10% during this period. LARC use increased by 129% among Hispanic women and by 128% among non-Hispanic white women from 2006–2010 to 2011–2013. Use of LARCs in non-Hispanic black women increased by 30% during this same period.
Parous vs nulliparous women
Women who have had at least one birth use LARC at a higher rate than women who have had no previous births. During the period 2011–2013, rate of use was 3 times greater among parous (11.0%) women compared with nulliparous (2.8%) women.
- Among parous women, LARC use increased from 2.4% in 2002 to 6.3% in 2006–2010, and to 10.6% in 2011–2013.
- In nulliparous women, LARC use increased 10-fold between 2006–2010 and 2011–2013.
For additional information, visit the NCHS Data Brief at http://www.cdc.gov/nchs/data/databriefs/db188.htm
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS data brief, no 188. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/databriefs/db188.htm. Updated February 24, 2015. Accessed March 25, 2015.
Use of long-acting reversible contraception (LARC) has increased nearly 5-fold in the last decade, reported the Centers for Disease Control and Prevention (CDC) in a National Center for Health Statistics (NCHS) Data Brief on the trends in LARC use among US women aged 15 to 44.1
Data from the National Survey of Family Growth indicate that LARCs, which include intrauterine devices (IUDs) and subdermal hormonal implants, are gaining popularity because of their high efficacy in preventing unintended pregnancies. LARCs have demonstrated greater efficacy in preventing unintended pregnancy among all women compared with other contraceptive methods, including the oral contraceptive pill and the transdermal patch.
Age-related trends
For women aged 15 to 44, LARC use doubled between 2002 (1.5%) and the period 2006–2010 (3.8%) and then nearly doubled again for 2011–2013 (7.2%). IUD use increased 83% from the 2006–2010 period (3.5%) to the 2011–2013 period (6.4%). Implant use tripled from 2002 (0.3%) to the 2011–2013 period (0.8%).
LARC use was higher among women aged 25 to 34 than among women aged 15 to 24. The difference in LARC use was not statistically significant between women aged 25 to 34 and women aged 35 to 44.
- LARC use increased nearly 4-fold for women aged 15 to 24 between 2002 (0.6%) and 2006–2010 (2.3%), and doubled again for 2011–2013 (5.0%).
- LARC use almost doubled among women aged 25 to 34 from 2006–2010 to 2011–2013 (5.3% to 11.1%).
- LARC use tripled between 2002 (1.1%) and 2006–2010 (3.8%) for women aged 35 to 44, and increased to 5.3% in 2011–2013.
Patterns of use by race
Although LARC use tripled for non-Hispanic white women and increased 4-fold for non-Hispanic black women between 2002 and 2006–2010, use among Hispanic women declined 10% during this period. LARC use increased by 129% among Hispanic women and by 128% among non-Hispanic white women from 2006–2010 to 2011–2013. Use of LARCs in non-Hispanic black women increased by 30% during this same period.
Parous vs nulliparous women
Women who have had at least one birth use LARC at a higher rate than women who have had no previous births. During the period 2011–2013, rate of use was 3 times greater among parous (11.0%) women compared with nulliparous (2.8%) women.
- Among parous women, LARC use increased from 2.4% in 2002 to 6.3% in 2006–2010, and to 10.6% in 2011–2013.
- In nulliparous women, LARC use increased 10-fold between 2006–2010 and 2011–2013.
For additional information, visit the NCHS Data Brief at http://www.cdc.gov/nchs/data/databriefs/db188.htm
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Use of long-acting reversible contraception (LARC) has increased nearly 5-fold in the last decade, reported the Centers for Disease Control and Prevention (CDC) in a National Center for Health Statistics (NCHS) Data Brief on the trends in LARC use among US women aged 15 to 44.1
Data from the National Survey of Family Growth indicate that LARCs, which include intrauterine devices (IUDs) and subdermal hormonal implants, are gaining popularity because of their high efficacy in preventing unintended pregnancies. LARCs have demonstrated greater efficacy in preventing unintended pregnancy among all women compared with other contraceptive methods, including the oral contraceptive pill and the transdermal patch.
Age-related trends
For women aged 15 to 44, LARC use doubled between 2002 (1.5%) and the period 2006–2010 (3.8%) and then nearly doubled again for 2011–2013 (7.2%). IUD use increased 83% from the 2006–2010 period (3.5%) to the 2011–2013 period (6.4%). Implant use tripled from 2002 (0.3%) to the 2011–2013 period (0.8%).
LARC use was higher among women aged 25 to 34 than among women aged 15 to 24. The difference in LARC use was not statistically significant between women aged 25 to 34 and women aged 35 to 44.
- LARC use increased nearly 4-fold for women aged 15 to 24 between 2002 (0.6%) and 2006–2010 (2.3%), and doubled again for 2011–2013 (5.0%).
- LARC use almost doubled among women aged 25 to 34 from 2006–2010 to 2011–2013 (5.3% to 11.1%).
- LARC use tripled between 2002 (1.1%) and 2006–2010 (3.8%) for women aged 35 to 44, and increased to 5.3% in 2011–2013.
Patterns of use by race
Although LARC use tripled for non-Hispanic white women and increased 4-fold for non-Hispanic black women between 2002 and 2006–2010, use among Hispanic women declined 10% during this period. LARC use increased by 129% among Hispanic women and by 128% among non-Hispanic white women from 2006–2010 to 2011–2013. Use of LARCs in non-Hispanic black women increased by 30% during this same period.
Parous vs nulliparous women
Women who have had at least one birth use LARC at a higher rate than women who have had no previous births. During the period 2011–2013, rate of use was 3 times greater among parous (11.0%) women compared with nulliparous (2.8%) women.
- Among parous women, LARC use increased from 2.4% in 2002 to 6.3% in 2006–2010, and to 10.6% in 2011–2013.
- In nulliparous women, LARC use increased 10-fold between 2006–2010 and 2011–2013.
For additional information, visit the NCHS Data Brief at http://www.cdc.gov/nchs/data/databriefs/db188.htm
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS data brief, no 188. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/databriefs/db188.htm. Updated February 24, 2015. Accessed March 25, 2015.
Reference
- Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS data brief, no 188. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/databriefs/db188.htm. Updated February 24, 2015. Accessed March 25, 2015.
Use of NIPT reduces invasive testing at one medical center
Following the introduction of noninvasive prenatal testing (NIPT) at the Maine Medical Center in Portland, the number of invasive prenatal diagnostic procedures decreased.
In a retrospective study, Joseph R. Wax, MD, and colleagues gathered statistics on the rates of genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection among women who were at increased risk for aneuploidy. These rates were compared before and after the availability of NIPT.
The study included 1,046 women who underwent NIPT between June 1, 2012, and February 1, 2013, as well as 1,464 women who would have been eligible for NIPT if it had been available between December 1, 2010, and November 30, 2011. All women were aged 35 years or older and had ultrasound findings suggestive of increased risk of aneuploidy, a positive aneuploidy screen, prior trisomic fetus, or parental balanced translocation with increased risk for trisomy 13 or 21. One laboratory performed NIPT after patients received genetic counseling. The two groups were compared by maternal demographics, aneuploidy risk factors, rates of genetic counseling, invasive diagnostic procedures, and trisomy 21 detection.1
Results of the study
A total of 33 fetuses with trisomy 21 were identified by positive aneuploidy screening. After the introduction of NIPT, genetic counseling for aneuploidy risk increased (adjusted odds ratio [aOR], 1.77; P <.0001). However, the overall use of invasive diagnostic testing (aOR, 0.42; P <.0001), including amniocentesis (aOR, 0.37, P <.0001), decreased, although the prenatal diagnosis of trisomy 21 remained similar (88% vs 100%; P = .86).1
Dr. Wax and colleagues concluded that, “NIPT in clinical practice uses more genetic counseling resources but requires significantly fewer invasive procedures to maintain the detection rates of trisomy 21.”1
Reference
1. Wax JR, Cartin A, Chard R, Lucas FL, Pinette MG. Noninvasive prenatal testing: Impact on genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection. J Clinic Ultrasound. 2015;43(1):1–6.
Following the introduction of noninvasive prenatal testing (NIPT) at the Maine Medical Center in Portland, the number of invasive prenatal diagnostic procedures decreased.
In a retrospective study, Joseph R. Wax, MD, and colleagues gathered statistics on the rates of genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection among women who were at increased risk for aneuploidy. These rates were compared before and after the availability of NIPT.
The study included 1,046 women who underwent NIPT between June 1, 2012, and February 1, 2013, as well as 1,464 women who would have been eligible for NIPT if it had been available between December 1, 2010, and November 30, 2011. All women were aged 35 years or older and had ultrasound findings suggestive of increased risk of aneuploidy, a positive aneuploidy screen, prior trisomic fetus, or parental balanced translocation with increased risk for trisomy 13 or 21. One laboratory performed NIPT after patients received genetic counseling. The two groups were compared by maternal demographics, aneuploidy risk factors, rates of genetic counseling, invasive diagnostic procedures, and trisomy 21 detection.1
Results of the study
A total of 33 fetuses with trisomy 21 were identified by positive aneuploidy screening. After the introduction of NIPT, genetic counseling for aneuploidy risk increased (adjusted odds ratio [aOR], 1.77; P <.0001). However, the overall use of invasive diagnostic testing (aOR, 0.42; P <.0001), including amniocentesis (aOR, 0.37, P <.0001), decreased, although the prenatal diagnosis of trisomy 21 remained similar (88% vs 100%; P = .86).1
Dr. Wax and colleagues concluded that, “NIPT in clinical practice uses more genetic counseling resources but requires significantly fewer invasive procedures to maintain the detection rates of trisomy 21.”1
Following the introduction of noninvasive prenatal testing (NIPT) at the Maine Medical Center in Portland, the number of invasive prenatal diagnostic procedures decreased.
In a retrospective study, Joseph R. Wax, MD, and colleagues gathered statistics on the rates of genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection among women who were at increased risk for aneuploidy. These rates were compared before and after the availability of NIPT.
The study included 1,046 women who underwent NIPT between June 1, 2012, and February 1, 2013, as well as 1,464 women who would have been eligible for NIPT if it had been available between December 1, 2010, and November 30, 2011. All women were aged 35 years or older and had ultrasound findings suggestive of increased risk of aneuploidy, a positive aneuploidy screen, prior trisomic fetus, or parental balanced translocation with increased risk for trisomy 13 or 21. One laboratory performed NIPT after patients received genetic counseling. The two groups were compared by maternal demographics, aneuploidy risk factors, rates of genetic counseling, invasive diagnostic procedures, and trisomy 21 detection.1
Results of the study
A total of 33 fetuses with trisomy 21 were identified by positive aneuploidy screening. After the introduction of NIPT, genetic counseling for aneuploidy risk increased (adjusted odds ratio [aOR], 1.77; P <.0001). However, the overall use of invasive diagnostic testing (aOR, 0.42; P <.0001), including amniocentesis (aOR, 0.37, P <.0001), decreased, although the prenatal diagnosis of trisomy 21 remained similar (88% vs 100%; P = .86).1
Dr. Wax and colleagues concluded that, “NIPT in clinical practice uses more genetic counseling resources but requires significantly fewer invasive procedures to maintain the detection rates of trisomy 21.”1
Reference
1. Wax JR, Cartin A, Chard R, Lucas FL, Pinette MG. Noninvasive prenatal testing: Impact on genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection. J Clinic Ultrasound. 2015;43(1):1–6.
Reference
1. Wax JR, Cartin A, Chard R, Lucas FL, Pinette MG. Noninvasive prenatal testing: Impact on genetic counseling, invasive prenatal diagnosis, and trisomy 21 detection. J Clinic Ultrasound. 2015;43(1):1–6.