User login
HPV: Changing the Statistics
In the world of research, an “n of 1” is considered an insufficient sample size to make an inference about a population. While distinguishing significance in research is vital in the scientific world, this statistical view often feels invalid when the “n of 1” is you or someone you know. And when the statistic is a diagnosis of cancer, that “1” feels even more noteworthy.
We know that cancer is a devastating disease that results in an increasing number of diagnoses each day. Case in point, the American Cancer Society estimates that more than 4,700 new cancers will be diagnosed each day in 2018.1 Most of us know that breast, colon, lung, and prostate cancer are the main contributors to those staggering numbers. But did you know that the incidence of oropharyngeal cancers (OPCs) is increasing? I didn’t.
It is estimated that 51,540 new cancer cases in 2018 will be of the oral cavity and pharynx and will cause approximately 10,000 deaths in the United States (US).1 Included in this estimate is the increasing incidence of human papillomavirus–associated oropharyngeal cancers (HPV-OPCs). The “n of 1” that started this discussion? That was a colleague of mine, who received just such a diagnosis. And the causative factor was surprising to me.
Now, please don’t misunderstand me—I know that HPV, a group of more than 150 related viruses, is the most common sexually transmitted infection (STI) in the US.2 I also know that HPV is implicated in genital warts and in cervical and anal cancers. The virus, which is transmitted through intimate skin-to-skin contact, is acquired by many during their adolescent and young adult years.2 Currently, 84 million Americans have HPV, and 14 million new cases are diagnosed each year.3
The most serious of those health problems, HPV-related cancers (which include cervical, vulvovaginal, anal, and oropharyngeal), are on the rise in the US.4 The prevalence of HPV in oropharyngeal tumors increased from 16.3% during the 1980s to 72.7% during the 2000s.5 Moreover, HPV has been implicated in 12% to 63% of all oropharyngeal cancers.6 Fifteen years ago, researchers concluded that HPV type 16 was the cause of 90% of cases of HPV-positive squamous cell carcinomas of the head and neck.7,8 At any given time, 7% of the population between ages 14 and 69 are infected by the virus within the oral mucosa.9
For my colleague—and many of us—the ship of prevention has sailed. But what disconcerts me most about this rise in HPV-related cancers is that, as of 2006, we have a vaccine that protects against infection with the two most prevalent cancer-causing HPV types. And yet, our vaccination rates continue to fall short of the Office of Disease Prevention and Health Promotion’s goal of having 80% of females ages 13 to 15 fully vaccinated against HPV.10
Continue to: Research has shown that parents of young adolescents...
Research has shown that parents of young adolescents are often upset by the recommendation that their children receive the HPV vaccine.11 Common beliefs are that the vaccine will give adolescents permission to become sexually active—or, conversely, that the adolescent isn’t sexually active, so the vaccine isn’t necessary. The reality of the situation: Adolescents don’t consider oral sex as having sexual relations, and oral sex is often the first sexual encounter for young people. Adolescents also regard oral sex as less risky than vaginal sex.12 So, many have unknowingly put themselves at risk while thinking they are actually being “safe.”
There are ways to reduce cancer risk, but few interventions are more effective than HPV vaccination.13 Given the incidence of HPV-OPC, it’s time to debunk the misbeliefs about sexual activity and move on to a concerted effort to promote HPV vaccination. Recent advertising about the HPV vaccine has emphasized the consequence of cancer in its messages. I applaud this new direction—it could be key to reversing the persistently low rate of HPV vaccination and changing that “n of 1” to zero. Share your trials and triumphs in promoting HPV vaccination with me at [email protected].
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. CDC. Human papillomavirus (HPV). www.cdc.gov/hpv/parents/whatishpv.html. Accessed August 8, 2018.
3. Patel EU, Grabowski MK, Eisenberg AL, et al. Increases in human papillomavirus vaccination among adolescent and young adult males in the United States, 2011-2016. J Infect Dis. 2018;218(1):109-113.
4. Dilley S, Scarinci I, Kimberlin D, Straughn JM. Preventing human papillomavirus-related cancers: we are all in this together. Am J Obstet Gynecol. 2017;216(6):576.e1-576.e5.
5. Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29(32):4294-4301.
6. Chandrani P, Kulkarni V, Iyer P, et al. NGS-based approach to determine the presence of HPV and their sites of integration in human cancer genome. Br J Cancer. 2015;112 (12):1958-1965.
7. Herrero R, Castellsague X, Pawlita M, et al; IARC Multicenter Oral Cancer Study Group. Human papillomavirus and oral cancer: the International Agency for Research on Cancer multicenter study. J Natl Cancer Inst. 2003;95(23):1772-1783.
8. Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709-720.
9. Golusin´ski W, Leemans CR, Dietz D, eds. HPV Infection in Head and Neck Cancer. Cham, Switzerland: Springer International Publishing; 2017.
10. Office of Disease Prevention and Health Promotion. Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for females by age 13 to 15 years. www.healthypeople.gov/node/4657/data_details. Accessed August 8, 2018.
11. National Cancer Institute; National Institutes of Health. President’s cancer panel annual report 2012–2013. Accelerating HPV vaccine uptake: urgency for action to prevent cancer. https://deainfo.nci.nih.gov/advisory/pcp/annualReports/HPV/index.htm. Accessed August 8, 2018.
12. Halpern-Felsher BL, Cornell JL, Kropp RY, Tschann JM. Oral versus vaginal sex among adolescents: perceptions, attitudes, and behavior. Pediatrics. 2005;115(4):845-851.
13. National Foundation for Infectious Diseases. Call to action: HPV vaccination as a public health priority. www.nfid.org/publications/cta/hpv-call-to-action.pdf. Accessed August 8, 2018.
In the world of research, an “n of 1” is considered an insufficient sample size to make an inference about a population. While distinguishing significance in research is vital in the scientific world, this statistical view often feels invalid when the “n of 1” is you or someone you know. And when the statistic is a diagnosis of cancer, that “1” feels even more noteworthy.
We know that cancer is a devastating disease that results in an increasing number of diagnoses each day. Case in point, the American Cancer Society estimates that more than 4,700 new cancers will be diagnosed each day in 2018.1 Most of us know that breast, colon, lung, and prostate cancer are the main contributors to those staggering numbers. But did you know that the incidence of oropharyngeal cancers (OPCs) is increasing? I didn’t.
It is estimated that 51,540 new cancer cases in 2018 will be of the oral cavity and pharynx and will cause approximately 10,000 deaths in the United States (US).1 Included in this estimate is the increasing incidence of human papillomavirus–associated oropharyngeal cancers (HPV-OPCs). The “n of 1” that started this discussion? That was a colleague of mine, who received just such a diagnosis. And the causative factor was surprising to me.
Now, please don’t misunderstand me—I know that HPV, a group of more than 150 related viruses, is the most common sexually transmitted infection (STI) in the US.2 I also know that HPV is implicated in genital warts and in cervical and anal cancers. The virus, which is transmitted through intimate skin-to-skin contact, is acquired by many during their adolescent and young adult years.2 Currently, 84 million Americans have HPV, and 14 million new cases are diagnosed each year.3
The most serious of those health problems, HPV-related cancers (which include cervical, vulvovaginal, anal, and oropharyngeal), are on the rise in the US.4 The prevalence of HPV in oropharyngeal tumors increased from 16.3% during the 1980s to 72.7% during the 2000s.5 Moreover, HPV has been implicated in 12% to 63% of all oropharyngeal cancers.6 Fifteen years ago, researchers concluded that HPV type 16 was the cause of 90% of cases of HPV-positive squamous cell carcinomas of the head and neck.7,8 At any given time, 7% of the population between ages 14 and 69 are infected by the virus within the oral mucosa.9
For my colleague—and many of us—the ship of prevention has sailed. But what disconcerts me most about this rise in HPV-related cancers is that, as of 2006, we have a vaccine that protects against infection with the two most prevalent cancer-causing HPV types. And yet, our vaccination rates continue to fall short of the Office of Disease Prevention and Health Promotion’s goal of having 80% of females ages 13 to 15 fully vaccinated against HPV.10
Continue to: Research has shown that parents of young adolescents...
Research has shown that parents of young adolescents are often upset by the recommendation that their children receive the HPV vaccine.11 Common beliefs are that the vaccine will give adolescents permission to become sexually active—or, conversely, that the adolescent isn’t sexually active, so the vaccine isn’t necessary. The reality of the situation: Adolescents don’t consider oral sex as having sexual relations, and oral sex is often the first sexual encounter for young people. Adolescents also regard oral sex as less risky than vaginal sex.12 So, many have unknowingly put themselves at risk while thinking they are actually being “safe.”
There are ways to reduce cancer risk, but few interventions are more effective than HPV vaccination.13 Given the incidence of HPV-OPC, it’s time to debunk the misbeliefs about sexual activity and move on to a concerted effort to promote HPV vaccination. Recent advertising about the HPV vaccine has emphasized the consequence of cancer in its messages. I applaud this new direction—it could be key to reversing the persistently low rate of HPV vaccination and changing that “n of 1” to zero. Share your trials and triumphs in promoting HPV vaccination with me at [email protected].
In the world of research, an “n of 1” is considered an insufficient sample size to make an inference about a population. While distinguishing significance in research is vital in the scientific world, this statistical view often feels invalid when the “n of 1” is you or someone you know. And when the statistic is a diagnosis of cancer, that “1” feels even more noteworthy.
We know that cancer is a devastating disease that results in an increasing number of diagnoses each day. Case in point, the American Cancer Society estimates that more than 4,700 new cancers will be diagnosed each day in 2018.1 Most of us know that breast, colon, lung, and prostate cancer are the main contributors to those staggering numbers. But did you know that the incidence of oropharyngeal cancers (OPCs) is increasing? I didn’t.
It is estimated that 51,540 new cancer cases in 2018 will be of the oral cavity and pharynx and will cause approximately 10,000 deaths in the United States (US).1 Included in this estimate is the increasing incidence of human papillomavirus–associated oropharyngeal cancers (HPV-OPCs). The “n of 1” that started this discussion? That was a colleague of mine, who received just such a diagnosis. And the causative factor was surprising to me.
Now, please don’t misunderstand me—I know that HPV, a group of more than 150 related viruses, is the most common sexually transmitted infection (STI) in the US.2 I also know that HPV is implicated in genital warts and in cervical and anal cancers. The virus, which is transmitted through intimate skin-to-skin contact, is acquired by many during their adolescent and young adult years.2 Currently, 84 million Americans have HPV, and 14 million new cases are diagnosed each year.3
The most serious of those health problems, HPV-related cancers (which include cervical, vulvovaginal, anal, and oropharyngeal), are on the rise in the US.4 The prevalence of HPV in oropharyngeal tumors increased from 16.3% during the 1980s to 72.7% during the 2000s.5 Moreover, HPV has been implicated in 12% to 63% of all oropharyngeal cancers.6 Fifteen years ago, researchers concluded that HPV type 16 was the cause of 90% of cases of HPV-positive squamous cell carcinomas of the head and neck.7,8 At any given time, 7% of the population between ages 14 and 69 are infected by the virus within the oral mucosa.9
For my colleague—and many of us—the ship of prevention has sailed. But what disconcerts me most about this rise in HPV-related cancers is that, as of 2006, we have a vaccine that protects against infection with the two most prevalent cancer-causing HPV types. And yet, our vaccination rates continue to fall short of the Office of Disease Prevention and Health Promotion’s goal of having 80% of females ages 13 to 15 fully vaccinated against HPV.10
Continue to: Research has shown that parents of young adolescents...
Research has shown that parents of young adolescents are often upset by the recommendation that their children receive the HPV vaccine.11 Common beliefs are that the vaccine will give adolescents permission to become sexually active—or, conversely, that the adolescent isn’t sexually active, so the vaccine isn’t necessary. The reality of the situation: Adolescents don’t consider oral sex as having sexual relations, and oral sex is often the first sexual encounter for young people. Adolescents also regard oral sex as less risky than vaginal sex.12 So, many have unknowingly put themselves at risk while thinking they are actually being “safe.”
There are ways to reduce cancer risk, but few interventions are more effective than HPV vaccination.13 Given the incidence of HPV-OPC, it’s time to debunk the misbeliefs about sexual activity and move on to a concerted effort to promote HPV vaccination. Recent advertising about the HPV vaccine has emphasized the consequence of cancer in its messages. I applaud this new direction—it could be key to reversing the persistently low rate of HPV vaccination and changing that “n of 1” to zero. Share your trials and triumphs in promoting HPV vaccination with me at [email protected].
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. CDC. Human papillomavirus (HPV). www.cdc.gov/hpv/parents/whatishpv.html. Accessed August 8, 2018.
3. Patel EU, Grabowski MK, Eisenberg AL, et al. Increases in human papillomavirus vaccination among adolescent and young adult males in the United States, 2011-2016. J Infect Dis. 2018;218(1):109-113.
4. Dilley S, Scarinci I, Kimberlin D, Straughn JM. Preventing human papillomavirus-related cancers: we are all in this together. Am J Obstet Gynecol. 2017;216(6):576.e1-576.e5.
5. Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29(32):4294-4301.
6. Chandrani P, Kulkarni V, Iyer P, et al. NGS-based approach to determine the presence of HPV and their sites of integration in human cancer genome. Br J Cancer. 2015;112 (12):1958-1965.
7. Herrero R, Castellsague X, Pawlita M, et al; IARC Multicenter Oral Cancer Study Group. Human papillomavirus and oral cancer: the International Agency for Research on Cancer multicenter study. J Natl Cancer Inst. 2003;95(23):1772-1783.
8. Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709-720.
9. Golusin´ski W, Leemans CR, Dietz D, eds. HPV Infection in Head and Neck Cancer. Cham, Switzerland: Springer International Publishing; 2017.
10. Office of Disease Prevention and Health Promotion. Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for females by age 13 to 15 years. www.healthypeople.gov/node/4657/data_details. Accessed August 8, 2018.
11. National Cancer Institute; National Institutes of Health. President’s cancer panel annual report 2012–2013. Accelerating HPV vaccine uptake: urgency for action to prevent cancer. https://deainfo.nci.nih.gov/advisory/pcp/annualReports/HPV/index.htm. Accessed August 8, 2018.
12. Halpern-Felsher BL, Cornell JL, Kropp RY, Tschann JM. Oral versus vaginal sex among adolescents: perceptions, attitudes, and behavior. Pediatrics. 2005;115(4):845-851.
13. National Foundation for Infectious Diseases. Call to action: HPV vaccination as a public health priority. www.nfid.org/publications/cta/hpv-call-to-action.pdf. Accessed August 8, 2018.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. CDC. Human papillomavirus (HPV). www.cdc.gov/hpv/parents/whatishpv.html. Accessed August 8, 2018.
3. Patel EU, Grabowski MK, Eisenberg AL, et al. Increases in human papillomavirus vaccination among adolescent and young adult males in the United States, 2011-2016. J Infect Dis. 2018;218(1):109-113.
4. Dilley S, Scarinci I, Kimberlin D, Straughn JM. Preventing human papillomavirus-related cancers: we are all in this together. Am J Obstet Gynecol. 2017;216(6):576.e1-576.e5.
5. Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29(32):4294-4301.
6. Chandrani P, Kulkarni V, Iyer P, et al. NGS-based approach to determine the presence of HPV and their sites of integration in human cancer genome. Br J Cancer. 2015;112 (12):1958-1965.
7. Herrero R, Castellsague X, Pawlita M, et al; IARC Multicenter Oral Cancer Study Group. Human papillomavirus and oral cancer: the International Agency for Research on Cancer multicenter study. J Natl Cancer Inst. 2003;95(23):1772-1783.
8. Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709-720.
9. Golusin´ski W, Leemans CR, Dietz D, eds. HPV Infection in Head and Neck Cancer. Cham, Switzerland: Springer International Publishing; 2017.
10. Office of Disease Prevention and Health Promotion. Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for females by age 13 to 15 years. www.healthypeople.gov/node/4657/data_details. Accessed August 8, 2018.
11. National Cancer Institute; National Institutes of Health. President’s cancer panel annual report 2012–2013. Accelerating HPV vaccine uptake: urgency for action to prevent cancer. https://deainfo.nci.nih.gov/advisory/pcp/annualReports/HPV/index.htm. Accessed August 8, 2018.
12. Halpern-Felsher BL, Cornell JL, Kropp RY, Tschann JM. Oral versus vaginal sex among adolescents: perceptions, attitudes, and behavior. Pediatrics. 2005;115(4):845-851.
13. National Foundation for Infectious Diseases. Call to action: HPV vaccination as a public health priority. www.nfid.org/publications/cta/hpv-call-to-action.pdf. Accessed August 8, 2018.
Brand Who? Brand You!
During the early days of the American Academy of Nurse Practitioners (incorporated in 1985), I spotted a full-page ad by the Campaign Consultants of America addressed to professional fundraisers. What caught my eye was a photograph of a mother with the tagline, “There’s only one person who understands you better than we do, and she still doesn’t understand what you do for a living.” I pulled the page from the magazine and made a note to consider using it to promote the NP profession. What we needed at the time, despite being an established profession, was to public
Historically, branding has been a task undertaken by a company’s marketing department or an advertising agency to identify elements that differentiate their product from the competition’s. Designing a logo, creating a jingle (Oscar-Mayer, anyone?), or recording a sound bite are the means to emphasize the difference. It paints the mental picture people have of a company, a product, or a provider. These cues remind the consumer about the product. So, how does this apply to the NP (and PA) profession?
The importance of establishing a “brand”—of distinguishing ourselves as competent clinicians with a specific skillset to offer the primary care community—cannot be overstated. Personal branding is a key component of fostering patient loyalty, building your reputation, and increasing referrals to your practice. Understanding the needs and desires of patients, their families, and the community is crucial. Our personal brand emphasizes our assets and expertise. While it can be difficult to look at yourself objectively (especially your assets), it is necessary in today’s competitive world of health care.
NPs constitute the fastest-growing segment of the primary care workforce in the US. More than 50 years of transforming health care as we know it has made us indispensable as health care providers. The literature has long supported the position that NPs provide care that is effective, patient-centered, and evidenced-based. Who we are, what we do, and how well we do it has been documented in myriad reports, surveys, and publications. Yet in many ways, we continue to struggle with an in-between identity. Despite our increasing responsibility in the clinical realm, some are still confused as to who we are.
We are known as nurses first, yet much of the health care we now provide was traditionally in the “physician-only” domain. And because of that history, our ability to function to the fullest extent of our education has been hobbled. These practice restrictions are counterproductive at a time when our nation is facing serious public health challenges.
Over the years, barriers to practice have slowly been whittled away, but full appreciation and recognition of our professional excellence and our contribution to improve the nation’s health is lacking. The fact that much of the research on health status and health ranking fails to include NPs and PAs is testimony that we remain somewhat invisible. And that, my friends, is exactly why it is time to revisit that aforementioned advertisement—not because our mothers don’t know what we do, but because, to some degree, we have eased off the belief that there are still obstacles to full access to NPs as primary care providers. And that is the origin of the need to establish your own brand.
Creating and maintaining your personal brand necessitates that you be multi-functional. You must be a role model, a mentor, and a voice that is respected and reliable. Your brand should advertise what you are known for and what motivates people to seek you, specifically, for their health care needs. Be relentlessly focused on what you do that adds value. As NPs, we have a unique blend of nursing and medicine that allows us to provide the patient-centered care that is central to meeting the existing and future primary care needs of our nation. From our roots in nursing, we offer patients high-quality care and a provider to partner with them in developing their plan of care.
Continue to: A foundational component of building your brand is...
A foundational component of building your brand is positioning yourself as a credible expert and leader. We each have a unique collection of experiences in preventive and primary care. Share that experience by getting involved in your community: participate in health fairs, interact with local news media, or volunteer to serve on your local health board. Emphasize the quality, flexibility, and continuity of care that you can provide. Share any survey findings that demonstrate your ability to anticipate, meet, and even exceed patients’ needs. Demonstrate your ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs.
As the nation continues to face a shortage of primary care providers and services—a gap that NPs and PAs are equipped to fill—it’s time for us to promote ourselves and advertise all that we can do. This isn’t just for our own sakes, but for our patients’ as well. Give some serious thought (and even more serious effort) to imagining and developing yourself as a brand. Define your brand’s attributes and the qualities or characteristics that make you distinctive from your competitors (or even your colleagues). You are the CEO of brand YOU!
If you have examples of how you promote your personal brand, please share them with me at [email protected].
During the early days of the American Academy of Nurse Practitioners (incorporated in 1985), I spotted a full-page ad by the Campaign Consultants of America addressed to professional fundraisers. What caught my eye was a photograph of a mother with the tagline, “There’s only one person who understands you better than we do, and she still doesn’t understand what you do for a living.” I pulled the page from the magazine and made a note to consider using it to promote the NP profession. What we needed at the time, despite being an established profession, was to public
Historically, branding has been a task undertaken by a company’s marketing department or an advertising agency to identify elements that differentiate their product from the competition’s. Designing a logo, creating a jingle (Oscar-Mayer, anyone?), or recording a sound bite are the means to emphasize the difference. It paints the mental picture people have of a company, a product, or a provider. These cues remind the consumer about the product. So, how does this apply to the NP (and PA) profession?
The importance of establishing a “brand”—of distinguishing ourselves as competent clinicians with a specific skillset to offer the primary care community—cannot be overstated. Personal branding is a key component of fostering patient loyalty, building your reputation, and increasing referrals to your practice. Understanding the needs and desires of patients, their families, and the community is crucial. Our personal brand emphasizes our assets and expertise. While it can be difficult to look at yourself objectively (especially your assets), it is necessary in today’s competitive world of health care.
NPs constitute the fastest-growing segment of the primary care workforce in the US. More than 50 years of transforming health care as we know it has made us indispensable as health care providers. The literature has long supported the position that NPs provide care that is effective, patient-centered, and evidenced-based. Who we are, what we do, and how well we do it has been documented in myriad reports, surveys, and publications. Yet in many ways, we continue to struggle with an in-between identity. Despite our increasing responsibility in the clinical realm, some are still confused as to who we are.
We are known as nurses first, yet much of the health care we now provide was traditionally in the “physician-only” domain. And because of that history, our ability to function to the fullest extent of our education has been hobbled. These practice restrictions are counterproductive at a time when our nation is facing serious public health challenges.
Over the years, barriers to practice have slowly been whittled away, but full appreciation and recognition of our professional excellence and our contribution to improve the nation’s health is lacking. The fact that much of the research on health status and health ranking fails to include NPs and PAs is testimony that we remain somewhat invisible. And that, my friends, is exactly why it is time to revisit that aforementioned advertisement—not because our mothers don’t know what we do, but because, to some degree, we have eased off the belief that there are still obstacles to full access to NPs as primary care providers. And that is the origin of the need to establish your own brand.
Creating and maintaining your personal brand necessitates that you be multi-functional. You must be a role model, a mentor, and a voice that is respected and reliable. Your brand should advertise what you are known for and what motivates people to seek you, specifically, for their health care needs. Be relentlessly focused on what you do that adds value. As NPs, we have a unique blend of nursing and medicine that allows us to provide the patient-centered care that is central to meeting the existing and future primary care needs of our nation. From our roots in nursing, we offer patients high-quality care and a provider to partner with them in developing their plan of care.
Continue to: A foundational component of building your brand is...
A foundational component of building your brand is positioning yourself as a credible expert and leader. We each have a unique collection of experiences in preventive and primary care. Share that experience by getting involved in your community: participate in health fairs, interact with local news media, or volunteer to serve on your local health board. Emphasize the quality, flexibility, and continuity of care that you can provide. Share any survey findings that demonstrate your ability to anticipate, meet, and even exceed patients’ needs. Demonstrate your ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs.
As the nation continues to face a shortage of primary care providers and services—a gap that NPs and PAs are equipped to fill—it’s time for us to promote ourselves and advertise all that we can do. This isn’t just for our own sakes, but for our patients’ as well. Give some serious thought (and even more serious effort) to imagining and developing yourself as a brand. Define your brand’s attributes and the qualities or characteristics that make you distinctive from your competitors (or even your colleagues). You are the CEO of brand YOU!
If you have examples of how you promote your personal brand, please share them with me at [email protected].
During the early days of the American Academy of Nurse Practitioners (incorporated in 1985), I spotted a full-page ad by the Campaign Consultants of America addressed to professional fundraisers. What caught my eye was a photograph of a mother with the tagline, “There’s only one person who understands you better than we do, and she still doesn’t understand what you do for a living.” I pulled the page from the magazine and made a note to consider using it to promote the NP profession. What we needed at the time, despite being an established profession, was to public
Historically, branding has been a task undertaken by a company’s marketing department or an advertising agency to identify elements that differentiate their product from the competition’s. Designing a logo, creating a jingle (Oscar-Mayer, anyone?), or recording a sound bite are the means to emphasize the difference. It paints the mental picture people have of a company, a product, or a provider. These cues remind the consumer about the product. So, how does this apply to the NP (and PA) profession?
The importance of establishing a “brand”—of distinguishing ourselves as competent clinicians with a specific skillset to offer the primary care community—cannot be overstated. Personal branding is a key component of fostering patient loyalty, building your reputation, and increasing referrals to your practice. Understanding the needs and desires of patients, their families, and the community is crucial. Our personal brand emphasizes our assets and expertise. While it can be difficult to look at yourself objectively (especially your assets), it is necessary in today’s competitive world of health care.
NPs constitute the fastest-growing segment of the primary care workforce in the US. More than 50 years of transforming health care as we know it has made us indispensable as health care providers. The literature has long supported the position that NPs provide care that is effective, patient-centered, and evidenced-based. Who we are, what we do, and how well we do it has been documented in myriad reports, surveys, and publications. Yet in many ways, we continue to struggle with an in-between identity. Despite our increasing responsibility in the clinical realm, some are still confused as to who we are.
We are known as nurses first, yet much of the health care we now provide was traditionally in the “physician-only” domain. And because of that history, our ability to function to the fullest extent of our education has been hobbled. These practice restrictions are counterproductive at a time when our nation is facing serious public health challenges.
Over the years, barriers to practice have slowly been whittled away, but full appreciation and recognition of our professional excellence and our contribution to improve the nation’s health is lacking. The fact that much of the research on health status and health ranking fails to include NPs and PAs is testimony that we remain somewhat invisible. And that, my friends, is exactly why it is time to revisit that aforementioned advertisement—not because our mothers don’t know what we do, but because, to some degree, we have eased off the belief that there are still obstacles to full access to NPs as primary care providers. And that is the origin of the need to establish your own brand.
Creating and maintaining your personal brand necessitates that you be multi-functional. You must be a role model, a mentor, and a voice that is respected and reliable. Your brand should advertise what you are known for and what motivates people to seek you, specifically, for their health care needs. Be relentlessly focused on what you do that adds value. As NPs, we have a unique blend of nursing and medicine that allows us to provide the patient-centered care that is central to meeting the existing and future primary care needs of our nation. From our roots in nursing, we offer patients high-quality care and a provider to partner with them in developing their plan of care.
Continue to: A foundational component of building your brand is...
A foundational component of building your brand is positioning yourself as a credible expert and leader. We each have a unique collection of experiences in preventive and primary care. Share that experience by getting involved in your community: participate in health fairs, interact with local news media, or volunteer to serve on your local health board. Emphasize the quality, flexibility, and continuity of care that you can provide. Share any survey findings that demonstrate your ability to anticipate, meet, and even exceed patients’ needs. Demonstrate your ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs.
As the nation continues to face a shortage of primary care providers and services—a gap that NPs and PAs are equipped to fill—it’s time for us to promote ourselves and advertise all that we can do. This isn’t just for our own sakes, but for our patients’ as well. Give some serious thought (and even more serious effort) to imagining and developing yourself as a brand. Define your brand’s attributes and the qualities or characteristics that make you distinctive from your competitors (or even your colleagues). You are the CEO of brand YOU!
If you have examples of how you promote your personal brand, please share them with me at [email protected].
Up in Arms About Gun Violence
Gun violence in America is a cancer—a metastasis that must be eradicated. As a nation, we continually mourn an ever-rising toll of victims and question why this senseless, tragic loss of life is repeated year after year. What is the reason for the increasing frequency of mass shootings? How is it that we are unable to stem the spread of this plague of gun-related deaths? When will we put an end to the massacres?
All good questions. And they have once again become the hue and cry of many people in the wake of the shooting at Marjory Stoneman Douglas High School in Parkland, Florida. This particular tragedy marked the 30th mass shooting in 2018—in other words, the latest in a line of tragedies that “should have” been preventable.1
Whatever your political stance on the issue of guns, surely we can all agree that it is a problem that more than 549,000 acts of gun violence occur each year.2 In 2015 (the most recent year for which a National Vital Statistics Report is available), there were 36,252 firearm-related deaths in the US—a rate of 11.1 deaths per 100,000 population. From 2012 to 2014, nearly 1,300 children died each year from a firearm-related injury.3 These statistics support the need to change our thinking about guns and gun violence.
Thus far, the discussion about gun control has tended to focus on passing and enforcing laws. We know that the US, compared to other countries, has fairly lenient restrictions for who can buy a gun and what kinds of guns can be purchased.4 In fact, many Americans can buy a gun in less than an hour, while in some countries, the process takes months.4 Furthermore, across the nation, there is no systematic fashion of gun regulation or ownership.
The challenge of how to balance gun safety and gun rights is an ongoing, yet one-focus, approach. The debate needs to be broadened; it’s time we stop talking about just the gun. We need to address the problem of firearm injuries in the context of a public health issue.5
A common assumption is that mental illness or high stress levels trigger gun violence. According to data from the Sandy Hook Promise organization, most criminal gun violence is committed by individuals who lack mental wellness (ie, coping skills, anger management, and other social/emotional skills).6 But other statistics contradict that notion. For example, a 2011 report in The Atlantic did not support mental illness as a causative factor in gun violence.7 And evidence presented by the Consortium for Risk-Based Firearm Policy indicates that the majority of people with mental illness do not engage in violence against others.8 The Consortium noted, however, that a small group of individuals with serious mental illness does have a propensity toward violence. It is this—the risk for dangerous behavior, rather than mental illness alone—that must be the focus for preventing gun violence.
Dangerous behaviors are those that carry a high risk for harm or injury to oneself or others.9 Emotional problems, social conflicts, access to weapons, and altered states of mind (via alcohol and drugs) all contribute to violent and homicidal behavior in adolescents.10 A worrisome fact: A nationwide study of mass shootings from 2009 to 2016 revealed that in at least 42% of these incidents there was documentation that the attacker exhibited dangerous warning signs before the shooting.11 So, in many cases of violent behavior, the perpetrator threatens others or his own life before actually carrying out his plan.12 But surely we must be able to do more than sit and watch for warning signs.
Continue to: Might tighter gun control laws...
Might tighter gun control laws help to mitigate this crisis? Perhaps; but we must also consider the importance of mental health care reform. In order to prevent gun violence, we need to understand (and address) the cause. We therefore need funding for mental health services to assist those who are at risk for harming themselves and others.
Instead of solely viewing gun control as a yes-or-no issue, we need to examine the intersection between mental health and violence. While our mental health care system is not equipped to help everyone, we need to acknowledge that gun-related deaths are preventable—and we need to make the choice to invest in that prevention.
Thus far, the ongoing debate about gun safety has largely centered around the Second Amendment, which has a two-fold obligation: the right of US citizens to be protected from violence and the right of the people to bear arms. Proponents on both sides of this polarizing issue have rallied to support their position; this often takes the form of shouting and counter-shouting (and sometimes threats)—and we make no progress on the core issue, which is that too many people in this country die because of gun violence.
We stand at the crossroads of realizing that something must be done. Share your reasoned suggestions (no rants, please!) for how we, as a nation, can combat gun violence and gun-related deaths with me at [email protected].
1. Robinson M, Gould S. There have been 30 mass shootings in the US so far in 2018 – here’s the full list. February 15, 2018. www.businessinsider.com/how-many-mass-shootings-in-america-this-year-2018-2. Accessed April 13, 2018.
2. CDC; Murphy SL, Xu J, Kochanek K, et al. National Vital Statistics Reports. Deaths: final data for 2015. www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_06.pdf. Accessed April 13, 2018.
3. Fowler KA, Dahlberg LL, Haileyesus T, et al. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1): e20163486.
4. Carlsen A, Chinoy S. How to buy a gun in 15 countries. The New York Times. March 2, 2018.
5. Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-273.
6. Gun violence in America fact sheet: average 2003-2013. https://d3n8a8pro7vhmx.cloudfront.net/promise/pages/17/attachments/original/1445441287/Gun_Facts.pdf?1445441287. Accessed April 13, 2018.
7. Florida R. The geography of gun deaths. January 13, 2011. The Atlantic. Accessed April 13, 2018.
8. Consortium for Risk-Based Firearm Policy. Guns, public health, and mental illness: an evidence-based approach for state policy. December 2, 2013. https://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-center-for-gun-policy-and-research/publications/GPHMI-State.pdf. Accessed April 9, 2018.
9. Conner MG. The risk of violent and homicidal behavior in children. May 21, 2014. http://oregoncounseling.org/ArticlesPapers/Documents/childviolence.htm. Accessed April 13, 2018.
10. U.S. National Library of Medicine. Dangerous behavior. www.definitions.net/definition/dangerous behavior.11. Everytown for Gun Safety. Mass shootings in the United States: 2009-2016. March 2017. https://everytownresearch.org/wp-content/uploads/2017/04/Analysis_of_Mass_Shooting_062117.pdf. Accessed April 13, 2018.
12. Minnesota Advocates for Human Rights. Assessing lethal and extremely dangerous behavior. www.hotpeachpages.net/lang/EnglishTraining/LethalityModule_2.pdf. Accessed April 13, 2018.
Gun violence in America is a cancer—a metastasis that must be eradicated. As a nation, we continually mourn an ever-rising toll of victims and question why this senseless, tragic loss of life is repeated year after year. What is the reason for the increasing frequency of mass shootings? How is it that we are unable to stem the spread of this plague of gun-related deaths? When will we put an end to the massacres?
All good questions. And they have once again become the hue and cry of many people in the wake of the shooting at Marjory Stoneman Douglas High School in Parkland, Florida. This particular tragedy marked the 30th mass shooting in 2018—in other words, the latest in a line of tragedies that “should have” been preventable.1
Whatever your political stance on the issue of guns, surely we can all agree that it is a problem that more than 549,000 acts of gun violence occur each year.2 In 2015 (the most recent year for which a National Vital Statistics Report is available), there were 36,252 firearm-related deaths in the US—a rate of 11.1 deaths per 100,000 population. From 2012 to 2014, nearly 1,300 children died each year from a firearm-related injury.3 These statistics support the need to change our thinking about guns and gun violence.
Thus far, the discussion about gun control has tended to focus on passing and enforcing laws. We know that the US, compared to other countries, has fairly lenient restrictions for who can buy a gun and what kinds of guns can be purchased.4 In fact, many Americans can buy a gun in less than an hour, while in some countries, the process takes months.4 Furthermore, across the nation, there is no systematic fashion of gun regulation or ownership.
The challenge of how to balance gun safety and gun rights is an ongoing, yet one-focus, approach. The debate needs to be broadened; it’s time we stop talking about just the gun. We need to address the problem of firearm injuries in the context of a public health issue.5
A common assumption is that mental illness or high stress levels trigger gun violence. According to data from the Sandy Hook Promise organization, most criminal gun violence is committed by individuals who lack mental wellness (ie, coping skills, anger management, and other social/emotional skills).6 But other statistics contradict that notion. For example, a 2011 report in The Atlantic did not support mental illness as a causative factor in gun violence.7 And evidence presented by the Consortium for Risk-Based Firearm Policy indicates that the majority of people with mental illness do not engage in violence against others.8 The Consortium noted, however, that a small group of individuals with serious mental illness does have a propensity toward violence. It is this—the risk for dangerous behavior, rather than mental illness alone—that must be the focus for preventing gun violence.
Dangerous behaviors are those that carry a high risk for harm or injury to oneself or others.9 Emotional problems, social conflicts, access to weapons, and altered states of mind (via alcohol and drugs) all contribute to violent and homicidal behavior in adolescents.10 A worrisome fact: A nationwide study of mass shootings from 2009 to 2016 revealed that in at least 42% of these incidents there was documentation that the attacker exhibited dangerous warning signs before the shooting.11 So, in many cases of violent behavior, the perpetrator threatens others or his own life before actually carrying out his plan.12 But surely we must be able to do more than sit and watch for warning signs.
Continue to: Might tighter gun control laws...
Might tighter gun control laws help to mitigate this crisis? Perhaps; but we must also consider the importance of mental health care reform. In order to prevent gun violence, we need to understand (and address) the cause. We therefore need funding for mental health services to assist those who are at risk for harming themselves and others.
Instead of solely viewing gun control as a yes-or-no issue, we need to examine the intersection between mental health and violence. While our mental health care system is not equipped to help everyone, we need to acknowledge that gun-related deaths are preventable—and we need to make the choice to invest in that prevention.
Thus far, the ongoing debate about gun safety has largely centered around the Second Amendment, which has a two-fold obligation: the right of US citizens to be protected from violence and the right of the people to bear arms. Proponents on both sides of this polarizing issue have rallied to support their position; this often takes the form of shouting and counter-shouting (and sometimes threats)—and we make no progress on the core issue, which is that too many people in this country die because of gun violence.
We stand at the crossroads of realizing that something must be done. Share your reasoned suggestions (no rants, please!) for how we, as a nation, can combat gun violence and gun-related deaths with me at [email protected].
Gun violence in America is a cancer—a metastasis that must be eradicated. As a nation, we continually mourn an ever-rising toll of victims and question why this senseless, tragic loss of life is repeated year after year. What is the reason for the increasing frequency of mass shootings? How is it that we are unable to stem the spread of this plague of gun-related deaths? When will we put an end to the massacres?
All good questions. And they have once again become the hue and cry of many people in the wake of the shooting at Marjory Stoneman Douglas High School in Parkland, Florida. This particular tragedy marked the 30th mass shooting in 2018—in other words, the latest in a line of tragedies that “should have” been preventable.1
Whatever your political stance on the issue of guns, surely we can all agree that it is a problem that more than 549,000 acts of gun violence occur each year.2 In 2015 (the most recent year for which a National Vital Statistics Report is available), there were 36,252 firearm-related deaths in the US—a rate of 11.1 deaths per 100,000 population. From 2012 to 2014, nearly 1,300 children died each year from a firearm-related injury.3 These statistics support the need to change our thinking about guns and gun violence.
Thus far, the discussion about gun control has tended to focus on passing and enforcing laws. We know that the US, compared to other countries, has fairly lenient restrictions for who can buy a gun and what kinds of guns can be purchased.4 In fact, many Americans can buy a gun in less than an hour, while in some countries, the process takes months.4 Furthermore, across the nation, there is no systematic fashion of gun regulation or ownership.
The challenge of how to balance gun safety and gun rights is an ongoing, yet one-focus, approach. The debate needs to be broadened; it’s time we stop talking about just the gun. We need to address the problem of firearm injuries in the context of a public health issue.5
A common assumption is that mental illness or high stress levels trigger gun violence. According to data from the Sandy Hook Promise organization, most criminal gun violence is committed by individuals who lack mental wellness (ie, coping skills, anger management, and other social/emotional skills).6 But other statistics contradict that notion. For example, a 2011 report in The Atlantic did not support mental illness as a causative factor in gun violence.7 And evidence presented by the Consortium for Risk-Based Firearm Policy indicates that the majority of people with mental illness do not engage in violence against others.8 The Consortium noted, however, that a small group of individuals with serious mental illness does have a propensity toward violence. It is this—the risk for dangerous behavior, rather than mental illness alone—that must be the focus for preventing gun violence.
Dangerous behaviors are those that carry a high risk for harm or injury to oneself or others.9 Emotional problems, social conflicts, access to weapons, and altered states of mind (via alcohol and drugs) all contribute to violent and homicidal behavior in adolescents.10 A worrisome fact: A nationwide study of mass shootings from 2009 to 2016 revealed that in at least 42% of these incidents there was documentation that the attacker exhibited dangerous warning signs before the shooting.11 So, in many cases of violent behavior, the perpetrator threatens others or his own life before actually carrying out his plan.12 But surely we must be able to do more than sit and watch for warning signs.
Continue to: Might tighter gun control laws...
Might tighter gun control laws help to mitigate this crisis? Perhaps; but we must also consider the importance of mental health care reform. In order to prevent gun violence, we need to understand (and address) the cause. We therefore need funding for mental health services to assist those who are at risk for harming themselves and others.
Instead of solely viewing gun control as a yes-or-no issue, we need to examine the intersection between mental health and violence. While our mental health care system is not equipped to help everyone, we need to acknowledge that gun-related deaths are preventable—and we need to make the choice to invest in that prevention.
Thus far, the ongoing debate about gun safety has largely centered around the Second Amendment, which has a two-fold obligation: the right of US citizens to be protected from violence and the right of the people to bear arms. Proponents on both sides of this polarizing issue have rallied to support their position; this often takes the form of shouting and counter-shouting (and sometimes threats)—and we make no progress on the core issue, which is that too many people in this country die because of gun violence.
We stand at the crossroads of realizing that something must be done. Share your reasoned suggestions (no rants, please!) for how we, as a nation, can combat gun violence and gun-related deaths with me at [email protected].
1. Robinson M, Gould S. There have been 30 mass shootings in the US so far in 2018 – here’s the full list. February 15, 2018. www.businessinsider.com/how-many-mass-shootings-in-america-this-year-2018-2. Accessed April 13, 2018.
2. CDC; Murphy SL, Xu J, Kochanek K, et al. National Vital Statistics Reports. Deaths: final data for 2015. www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_06.pdf. Accessed April 13, 2018.
3. Fowler KA, Dahlberg LL, Haileyesus T, et al. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1): e20163486.
4. Carlsen A, Chinoy S. How to buy a gun in 15 countries. The New York Times. March 2, 2018.
5. Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-273.
6. Gun violence in America fact sheet: average 2003-2013. https://d3n8a8pro7vhmx.cloudfront.net/promise/pages/17/attachments/original/1445441287/Gun_Facts.pdf?1445441287. Accessed April 13, 2018.
7. Florida R. The geography of gun deaths. January 13, 2011. The Atlantic. Accessed April 13, 2018.
8. Consortium for Risk-Based Firearm Policy. Guns, public health, and mental illness: an evidence-based approach for state policy. December 2, 2013. https://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-center-for-gun-policy-and-research/publications/GPHMI-State.pdf. Accessed April 9, 2018.
9. Conner MG. The risk of violent and homicidal behavior in children. May 21, 2014. http://oregoncounseling.org/ArticlesPapers/Documents/childviolence.htm. Accessed April 13, 2018.
10. U.S. National Library of Medicine. Dangerous behavior. www.definitions.net/definition/dangerous behavior.11. Everytown for Gun Safety. Mass shootings in the United States: 2009-2016. March 2017. https://everytownresearch.org/wp-content/uploads/2017/04/Analysis_of_Mass_Shooting_062117.pdf. Accessed April 13, 2018.
12. Minnesota Advocates for Human Rights. Assessing lethal and extremely dangerous behavior. www.hotpeachpages.net/lang/EnglishTraining/LethalityModule_2.pdf. Accessed April 13, 2018.
1. Robinson M, Gould S. There have been 30 mass shootings in the US so far in 2018 – here’s the full list. February 15, 2018. www.businessinsider.com/how-many-mass-shootings-in-america-this-year-2018-2. Accessed April 13, 2018.
2. CDC; Murphy SL, Xu J, Kochanek K, et al. National Vital Statistics Reports. Deaths: final data for 2015. www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_06.pdf. Accessed April 13, 2018.
3. Fowler KA, Dahlberg LL, Haileyesus T, et al. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1): e20163486.
4. Carlsen A, Chinoy S. How to buy a gun in 15 countries. The New York Times. March 2, 2018.
5. Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-273.
6. Gun violence in America fact sheet: average 2003-2013. https://d3n8a8pro7vhmx.cloudfront.net/promise/pages/17/attachments/original/1445441287/Gun_Facts.pdf?1445441287. Accessed April 13, 2018.
7. Florida R. The geography of gun deaths. January 13, 2011. The Atlantic. Accessed April 13, 2018.
8. Consortium for Risk-Based Firearm Policy. Guns, public health, and mental illness: an evidence-based approach for state policy. December 2, 2013. https://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-center-for-gun-policy-and-research/publications/GPHMI-State.pdf. Accessed April 9, 2018.
9. Conner MG. The risk of violent and homicidal behavior in children. May 21, 2014. http://oregoncounseling.org/ArticlesPapers/Documents/childviolence.htm. Accessed April 13, 2018.
10. U.S. National Library of Medicine. Dangerous behavior. www.definitions.net/definition/dangerous behavior.11. Everytown for Gun Safety. Mass shootings in the United States: 2009-2016. March 2017. https://everytownresearch.org/wp-content/uploads/2017/04/Analysis_of_Mass_Shooting_062117.pdf. Accessed April 13, 2018.
12. Minnesota Advocates for Human Rights. Assessing lethal and extremely dangerous behavior. www.hotpeachpages.net/lang/EnglishTraining/LethalityModule_2.pdf. Accessed April 13, 2018.
Taking the Bite Out of Nutrition
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
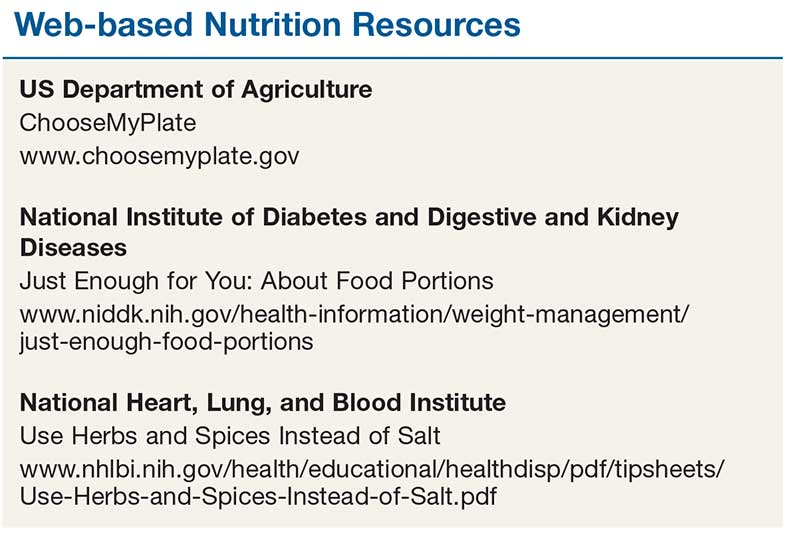
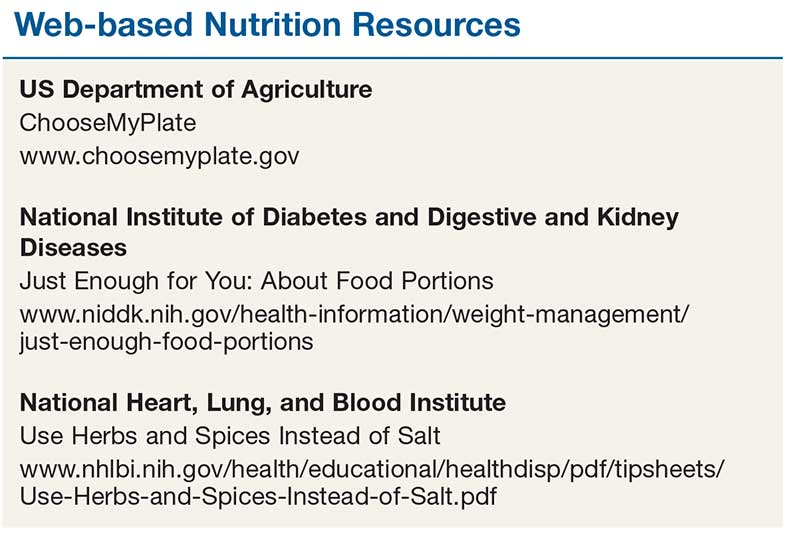
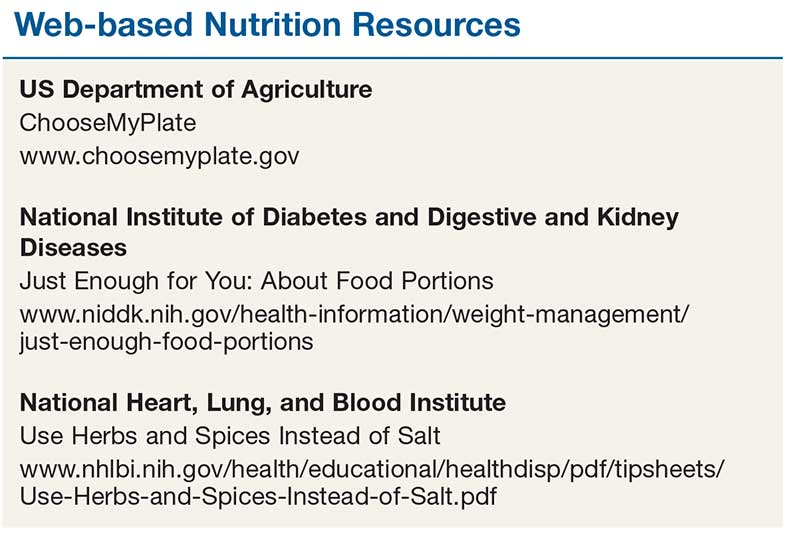
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
As March arrives, we rejoice in the promise of spring sunlight and start planning ahead for summer and its associated clothing, which tends to be a bit more … revealing, shall we say. If we’re really motivated, we might dust off our (quickly forgotten) New Year’s weight-loss resolutions, adjusting our carb:veggie ratio to get beach-ready. Furthermore, March historically signified the start of farming season—making it a natural fit for National Nutrition Month.
In 1973, the Academy of Nutrition and Dietetics (AND) initiated a week-long campaign to educate the public about hea
This guidance is needed more now than ever before. About 75% of Americans follow a diet that is low in fruits, vegetables, dairy, and oils (compared to the recommended values)—and most exceed the recommended allotment for added sugars, sodium, and saturated fats.2 It’s no surprise, then, that two-thirds of US adults are either overweight or obese.2
It is imperative that we, as health care providers, provide our patients and their families with practical, evidence-based information about healthy food choices. But are we sufficiently educated to provide that guidance?
I admit, my confidence in my nutritional knowledge falls short of the mark. I vaguely recall nutrition being discussed in one of my basic nursing courses; diets designed for specific disease entities were introduced as I progressed in my education. But a specific nutrition course is not a requirement in the Commission on Collegiate Nursing Education’s Essentials of Baccalaureate Education for Professional Nursing Practice—even though nutrition is directly linked to wellness and health promotion is an essential component of nursing practice.3 (This inconsistency in nutrition education holds true for our PA colleagues, as well.)
How, then, do we educate ourselves so that we can impart the necessary guidance to our patients? The plethora of articles—some more scholarly than others—on what we should and should not eat can be very confusing.
Generally, though, the soundest advice encourages a healthy lifestyle, with emphasis on consistent, enjoyable eating practices and regular physical activity. Of particular note: The word “diet” is not included in most guides. Rather, we are advised to make small changes to the way we think about eating.
Substituting fruit for added sugar, whole grains for refined grains, and oils for solid fats are just a few simple ways to transition to a healthier eating regimen.2 Another adaptation is to plan out meals and snacks prior to food shopping; this not only prevents us from making poor choices and purchasing items based on impulse or hunger, but also decreases food waste. These comparatively small adjustments can make a real difference over time.
To help achieve the goal of a healthy lifestyle, AND offers the following suggestions:
- Include a variety of healthful foods from all food groups on a regular basis.
- Consider which food items you have on hand before buying more at the store.
- Buy only an amount that can be eaten within a few days (or stored in the freezer) and plan ways to use leftovers later in the week.
- Be mindful of portion sizes.
- Find activities you enjoy to keep you physically active throughout the week.4
We also have a resource at our fingertips that we often overlook: registered dietitian nutritionists (RDNs). These professionals are educated specifically to provide counseling on food choices and can help clear the murky waters surrounding nutrition. An RDN can partner with a consumer to develop a safe, effective, sustainable eating plan that takes into consideration health status, lifestyle, and personal taste preferences.
In addition to RDN colleagues, there are trustworthy, easy-to-navigate websites that provide resources on nutrition and healthy eating. They also have tools we can provide to our patients and their families (see box). For example, ChooseMyPlate (www.choosemyplate.gov) is an interactive site based on the Dietary Guidelines for Americans that provides information on how much of each food group should be eaten each day. It also includes resources for planning well-balanced, healthy meals and a series of fact sheets with tips that can be useful for patients. The National Institutes of Health also offers practical guidance on differentiating a portion from a serving, controlling portion size (both at home and when eating out), and finding alternatives to salt when you want or need to season food.
Reviewing even just one or two of these resources can improve your knowledge about healthy eating habits. Since a balanced and tasty meal plan is a recipe for success, let’s make better nutrition our mantra. We can help our patients, and perhaps learn something ourselves!
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.
1. Academy of Nutrition and Dietetics. National Nutrition Month®. www.eatright.org/resource/food/resources/national-nutrition-month/national-nutrition-month. Accessed February 13, 2018.
2. US Department of Agriculture. Dietary Guidelines for Americans, 2015-2020. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines. Accessed February 13, 2018.
3. American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. Accessed February 13, 2018.
4. Academy of Nutrition and Dietetics. National Nutrition Month® celebration toolkit. www.eatright.org/resource/food/resources/national-nutrition-month/toolkit. Accessed February 13, 2018.
Stressed for Success
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
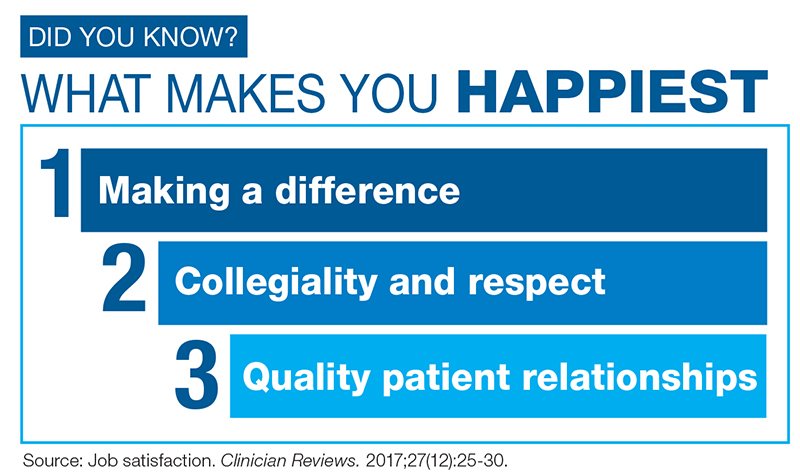
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
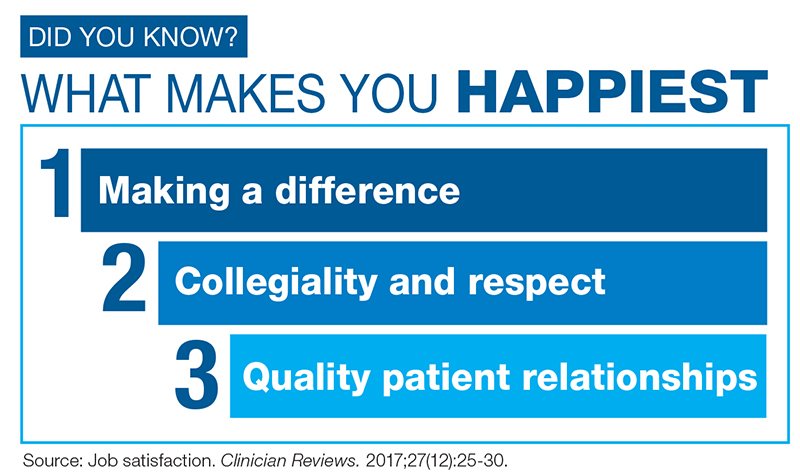
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
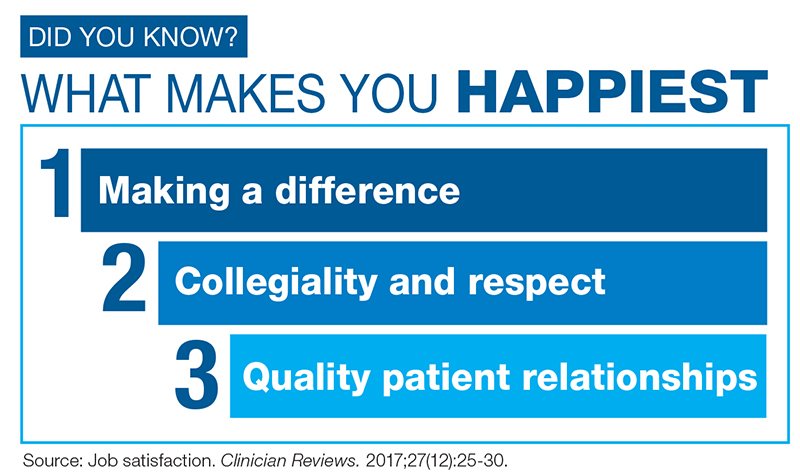
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
The Tempest Within
On the heels of Hurricane Harvey, which devastated the city of Houston and other communities in Texas and Louisiana, Hurricane Irma ravaged several islands in the Caribbean—and then headed for the states. In the days before she made landfall in the US, the media offered seemingly minute-to-minute updates on her progress. Each new forecast seemed to contradict the previous, demonstrating the unpredictability of natural disasters. But as the hurricane crept closer, one thing was evident: Florida was going to take a hard hit.
Keeping up with the fluctuating weather report was like watching a tennis match: East Coast … nope, not the East Coast … probably the middle of the state. We breathed periodic sighs of relief but remained leery. Then, several of the spaghetti plots (may I never hear that term again!) showed Irma veering west—right over our heads. Hysteria set in. One meteorologist sounded absolutely frantic as she warned people to GET READY!!!!
Now, to be clear: My purpose in writing is not to disparage media coverage or governmental response, nor to minimize anyone else’s struggles. Rather, I want to share how the hurricane affected my neighbors, friends, family, and myself—and continues to do so, weeks afterward.
Once Irma’s course was set, we swept into action. Our emergency plan included hurricane-proofing our home—protective awnings placed over the windows; outside decorations put away; grill stored properly; palm trees trimmed—and laying in sufficient supplies (gallon jugs of water, needed medications, bread and peanut butter). We gathered important documents, filled the car with gas, and made sure to have cash on hand. This flurry of activity got the adrenaline pumping, but there was something satisfying about checking off each item on our list. Before you knew it, we were set.
Then Governor Scott took the proactive step of declaring a state of emergency, before Irma was even in striking distance. This was beneficial for all Floridians, since it positioned us to receive federal assistance if needed and allowed local officials to act quickly, without the burden of bureaucracy or red tape.
However, as this news spread, our phones began to ring, buzz, and ping. Friends around the country wanted to know, “Are you okay?” and to offer us a place to stay if we needed to get out. These well-intentioned messages were appreciated—but each expression of concern reminded us that we were facing something big. We were fine, though. Prepared. And the storm could still bypass us or at least hit in a weakened state.
As Irma moved closer, the nervous energy in our little community began to rise. Some neighbors headed north several days before the predicted arrival, spending hours in traffic. We were glad we’d decided to shelter in place instead! Our decision was met with worried looks and wringing hands, which perplexed us. After all, we live about two miles from the Gulf of Mexico and 40-plus feet above sea level. My parents had moved to the area in 1978, and Dad always told us it was where people evacuated to, not from. No problem!
Except … then the mandatory evacuation notice was given. Uh oh! Time to revisit our “shelter in place” plan. What were the options again?
Plan A: Call a friend who lives three towns away in a non-evacuation zone. But her daughter gets evacuated every storm, so she, her husband, and their three dogs had already claimed the guest room.
Plan B: Call another friend in the next town over. She was happy to accommodate us! We planned to arrive the night before the predicted hit and wait out the storm there. The plan was foolproof ... until she also got a mandatory evacuation notice.
Plan C: Find a hotel in a safe area. No luck—all booked.
Admittedly, with each snag in our plans, our stress and anxiety increased. We began to question our initial decision to stay put. Had we missed our opportunity to get out of town?
Then, thankfully, the phone rang. Our friend’s daughter had miraculously secured us hotel rooms about 30 miles from our home.
The strangest thing about riding out a hurricane is that you have days of anticipation and action—you prepare—and then you just have to wait. In the confines of our “bunker,” we had naught to do but track the storm. For three days, local television stations aired only the weather; there was no respite from the red tracking markers. The endless barrage of information added to our already heightened stress levels. We wondered what we would face once we returned home. The thought of major damage sickened us.
Three days after Irma visited, we were cleared to head home. We were admittedly nervous to see what she had left behind—but incredibly, we found our house exactly as we had left it. We hugged each other, in tears. The surrounding damage ranged from minor to major, but thankfully, no one was injured. Neighbors who had fled town asked us to send pictures of their homes so they could see for themselves. The consensus: What was broken can be fixed; we are all thankful to have survived. In a way, I expected that to be the end of the story. But I was wrong.
In my February 2010 editorial, I addressed the aftermath of the earthquake that had struck Haiti the month before.1 Seven years later, 2.5 million Haitians are still in need of humanitarian aid, and 55,000 people are in camps and makeshift camps.2 You might be thinking, “An earthquake in Haiti is much different from a hurricane in the United States.” That may be true, but some victims of Hurricane Sandy are still trying to repair damage to their homes, five years later.3 So while Hurricanes Irma and Harvey—let alone Hurricane Sandy—are already off the front pages, the despair, emotional impact, and disbelief associated with the disasters endure. As one woman described, “You’re in complete shock. You’re trying to figure out, ‘Is this happening to me? Am I in some sort of dream I can’t wake up from?’”3
We are not people who are easily discouraged or quick to worry about things we can’t control. But this experience was very different: The sensory overload was unnerving, and the anxiety and stress linger. As a result, I have an entirely new perspective on the effect of disaster on mental health. The worst we suffered was four days without power, yet as I write this weeks later, I find myself in tears, reliving the fear and anxiety we felt during Irma’s wrath. We were ready for a hurricane, but not for the emotional turmoil that has followed.
Have you experienced a disaster, natural or otherwise, that left you shaken? Share your experience, and any advice you may have, with me at [email protected].
1. Onieal ME. When helping hands are tied. Clinician Reviews. 2010;20(2):C2, 18-20.
2. Cook J. 7 years after Haiti’s earthquake, millions still need aid. www.huffingtonpost.com/entry/haiti-earthquake-anniversary_us_5875108de4b02b5f858b3f9c. Accessed October 6, 2017.
3. Sandoval E, Marcius CR, Durkin E, Dillon N. Hurricane Sandy victims’ homes still uninhabitable nearly five years later. www.nydailynews.com/new-york/hurricane-sandy-victims-living-limbo-years-article-1.3463866. Accessed October 6, 2017.
On the heels of Hurricane Harvey, which devastated the city of Houston and other communities in Texas and Louisiana, Hurricane Irma ravaged several islands in the Caribbean—and then headed for the states. In the days before she made landfall in the US, the media offered seemingly minute-to-minute updates on her progress. Each new forecast seemed to contradict the previous, demonstrating the unpredictability of natural disasters. But as the hurricane crept closer, one thing was evident: Florida was going to take a hard hit.
Keeping up with the fluctuating weather report was like watching a tennis match: East Coast … nope, not the East Coast … probably the middle of the state. We breathed periodic sighs of relief but remained leery. Then, several of the spaghetti plots (may I never hear that term again!) showed Irma veering west—right over our heads. Hysteria set in. One meteorologist sounded absolutely frantic as she warned people to GET READY!!!!
Now, to be clear: My purpose in writing is not to disparage media coverage or governmental response, nor to minimize anyone else’s struggles. Rather, I want to share how the hurricane affected my neighbors, friends, family, and myself—and continues to do so, weeks afterward.
Once Irma’s course was set, we swept into action. Our emergency plan included hurricane-proofing our home—protective awnings placed over the windows; outside decorations put away; grill stored properly; palm trees trimmed—and laying in sufficient supplies (gallon jugs of water, needed medications, bread and peanut butter). We gathered important documents, filled the car with gas, and made sure to have cash on hand. This flurry of activity got the adrenaline pumping, but there was something satisfying about checking off each item on our list. Before you knew it, we were set.
Then Governor Scott took the proactive step of declaring a state of emergency, before Irma was even in striking distance. This was beneficial for all Floridians, since it positioned us to receive federal assistance if needed and allowed local officials to act quickly, without the burden of bureaucracy or red tape.
However, as this news spread, our phones began to ring, buzz, and ping. Friends around the country wanted to know, “Are you okay?” and to offer us a place to stay if we needed to get out. These well-intentioned messages were appreciated—but each expression of concern reminded us that we were facing something big. We were fine, though. Prepared. And the storm could still bypass us or at least hit in a weakened state.
As Irma moved closer, the nervous energy in our little community began to rise. Some neighbors headed north several days before the predicted arrival, spending hours in traffic. We were glad we’d decided to shelter in place instead! Our decision was met with worried looks and wringing hands, which perplexed us. After all, we live about two miles from the Gulf of Mexico and 40-plus feet above sea level. My parents had moved to the area in 1978, and Dad always told us it was where people evacuated to, not from. No problem!
Except … then the mandatory evacuation notice was given. Uh oh! Time to revisit our “shelter in place” plan. What were the options again?
Plan A: Call a friend who lives three towns away in a non-evacuation zone. But her daughter gets evacuated every storm, so she, her husband, and their three dogs had already claimed the guest room.
Plan B: Call another friend in the next town over. She was happy to accommodate us! We planned to arrive the night before the predicted hit and wait out the storm there. The plan was foolproof ... until she also got a mandatory evacuation notice.
Plan C: Find a hotel in a safe area. No luck—all booked.
Admittedly, with each snag in our plans, our stress and anxiety increased. We began to question our initial decision to stay put. Had we missed our opportunity to get out of town?
Then, thankfully, the phone rang. Our friend’s daughter had miraculously secured us hotel rooms about 30 miles from our home.
The strangest thing about riding out a hurricane is that you have days of anticipation and action—you prepare—and then you just have to wait. In the confines of our “bunker,” we had naught to do but track the storm. For three days, local television stations aired only the weather; there was no respite from the red tracking markers. The endless barrage of information added to our already heightened stress levels. We wondered what we would face once we returned home. The thought of major damage sickened us.
Three days after Irma visited, we were cleared to head home. We were admittedly nervous to see what she had left behind—but incredibly, we found our house exactly as we had left it. We hugged each other, in tears. The surrounding damage ranged from minor to major, but thankfully, no one was injured. Neighbors who had fled town asked us to send pictures of their homes so they could see for themselves. The consensus: What was broken can be fixed; we are all thankful to have survived. In a way, I expected that to be the end of the story. But I was wrong.
In my February 2010 editorial, I addressed the aftermath of the earthquake that had struck Haiti the month before.1 Seven years later, 2.5 million Haitians are still in need of humanitarian aid, and 55,000 people are in camps and makeshift camps.2 You might be thinking, “An earthquake in Haiti is much different from a hurricane in the United States.” That may be true, but some victims of Hurricane Sandy are still trying to repair damage to their homes, five years later.3 So while Hurricanes Irma and Harvey—let alone Hurricane Sandy—are already off the front pages, the despair, emotional impact, and disbelief associated with the disasters endure. As one woman described, “You’re in complete shock. You’re trying to figure out, ‘Is this happening to me? Am I in some sort of dream I can’t wake up from?’”3
We are not people who are easily discouraged or quick to worry about things we can’t control. But this experience was very different: The sensory overload was unnerving, and the anxiety and stress linger. As a result, I have an entirely new perspective on the effect of disaster on mental health. The worst we suffered was four days without power, yet as I write this weeks later, I find myself in tears, reliving the fear and anxiety we felt during Irma’s wrath. We were ready for a hurricane, but not for the emotional turmoil that has followed.
Have you experienced a disaster, natural or otherwise, that left you shaken? Share your experience, and any advice you may have, with me at [email protected].
On the heels of Hurricane Harvey, which devastated the city of Houston and other communities in Texas and Louisiana, Hurricane Irma ravaged several islands in the Caribbean—and then headed for the states. In the days before she made landfall in the US, the media offered seemingly minute-to-minute updates on her progress. Each new forecast seemed to contradict the previous, demonstrating the unpredictability of natural disasters. But as the hurricane crept closer, one thing was evident: Florida was going to take a hard hit.
Keeping up with the fluctuating weather report was like watching a tennis match: East Coast … nope, not the East Coast … probably the middle of the state. We breathed periodic sighs of relief but remained leery. Then, several of the spaghetti plots (may I never hear that term again!) showed Irma veering west—right over our heads. Hysteria set in. One meteorologist sounded absolutely frantic as she warned people to GET READY!!!!
Now, to be clear: My purpose in writing is not to disparage media coverage or governmental response, nor to minimize anyone else’s struggles. Rather, I want to share how the hurricane affected my neighbors, friends, family, and myself—and continues to do so, weeks afterward.
Once Irma’s course was set, we swept into action. Our emergency plan included hurricane-proofing our home—protective awnings placed over the windows; outside decorations put away; grill stored properly; palm trees trimmed—and laying in sufficient supplies (gallon jugs of water, needed medications, bread and peanut butter). We gathered important documents, filled the car with gas, and made sure to have cash on hand. This flurry of activity got the adrenaline pumping, but there was something satisfying about checking off each item on our list. Before you knew it, we were set.
Then Governor Scott took the proactive step of declaring a state of emergency, before Irma was even in striking distance. This was beneficial for all Floridians, since it positioned us to receive federal assistance if needed and allowed local officials to act quickly, without the burden of bureaucracy or red tape.
However, as this news spread, our phones began to ring, buzz, and ping. Friends around the country wanted to know, “Are you okay?” and to offer us a place to stay if we needed to get out. These well-intentioned messages were appreciated—but each expression of concern reminded us that we were facing something big. We were fine, though. Prepared. And the storm could still bypass us or at least hit in a weakened state.
As Irma moved closer, the nervous energy in our little community began to rise. Some neighbors headed north several days before the predicted arrival, spending hours in traffic. We were glad we’d decided to shelter in place instead! Our decision was met with worried looks and wringing hands, which perplexed us. After all, we live about two miles from the Gulf of Mexico and 40-plus feet above sea level. My parents had moved to the area in 1978, and Dad always told us it was where people evacuated to, not from. No problem!
Except … then the mandatory evacuation notice was given. Uh oh! Time to revisit our “shelter in place” plan. What were the options again?
Plan A: Call a friend who lives three towns away in a non-evacuation zone. But her daughter gets evacuated every storm, so she, her husband, and their three dogs had already claimed the guest room.
Plan B: Call another friend in the next town over. She was happy to accommodate us! We planned to arrive the night before the predicted hit and wait out the storm there. The plan was foolproof ... until she also got a mandatory evacuation notice.
Plan C: Find a hotel in a safe area. No luck—all booked.
Admittedly, with each snag in our plans, our stress and anxiety increased. We began to question our initial decision to stay put. Had we missed our opportunity to get out of town?
Then, thankfully, the phone rang. Our friend’s daughter had miraculously secured us hotel rooms about 30 miles from our home.
The strangest thing about riding out a hurricane is that you have days of anticipation and action—you prepare—and then you just have to wait. In the confines of our “bunker,” we had naught to do but track the storm. For three days, local television stations aired only the weather; there was no respite from the red tracking markers. The endless barrage of information added to our already heightened stress levels. We wondered what we would face once we returned home. The thought of major damage sickened us.
Three days after Irma visited, we were cleared to head home. We were admittedly nervous to see what she had left behind—but incredibly, we found our house exactly as we had left it. We hugged each other, in tears. The surrounding damage ranged from minor to major, but thankfully, no one was injured. Neighbors who had fled town asked us to send pictures of their homes so they could see for themselves. The consensus: What was broken can be fixed; we are all thankful to have survived. In a way, I expected that to be the end of the story. But I was wrong.
In my February 2010 editorial, I addressed the aftermath of the earthquake that had struck Haiti the month before.1 Seven years later, 2.5 million Haitians are still in need of humanitarian aid, and 55,000 people are in camps and makeshift camps.2 You might be thinking, “An earthquake in Haiti is much different from a hurricane in the United States.” That may be true, but some victims of Hurricane Sandy are still trying to repair damage to their homes, five years later.3 So while Hurricanes Irma and Harvey—let alone Hurricane Sandy—are already off the front pages, the despair, emotional impact, and disbelief associated with the disasters endure. As one woman described, “You’re in complete shock. You’re trying to figure out, ‘Is this happening to me? Am I in some sort of dream I can’t wake up from?’”3
We are not people who are easily discouraged or quick to worry about things we can’t control. But this experience was very different: The sensory overload was unnerving, and the anxiety and stress linger. As a result, I have an entirely new perspective on the effect of disaster on mental health. The worst we suffered was four days without power, yet as I write this weeks later, I find myself in tears, reliving the fear and anxiety we felt during Irma’s wrath. We were ready for a hurricane, but not for the emotional turmoil that has followed.
Have you experienced a disaster, natural or otherwise, that left you shaken? Share your experience, and any advice you may have, with me at [email protected].
1. Onieal ME. When helping hands are tied. Clinician Reviews. 2010;20(2):C2, 18-20.
2. Cook J. 7 years after Haiti’s earthquake, millions still need aid. www.huffingtonpost.com/entry/haiti-earthquake-anniversary_us_5875108de4b02b5f858b3f9c. Accessed October 6, 2017.
3. Sandoval E, Marcius CR, Durkin E, Dillon N. Hurricane Sandy victims’ homes still uninhabitable nearly five years later. www.nydailynews.com/new-york/hurricane-sandy-victims-living-limbo-years-article-1.3463866. Accessed October 6, 2017.
1. Onieal ME. When helping hands are tied. Clinician Reviews. 2010;20(2):C2, 18-20.
2. Cook J. 7 years after Haiti’s earthquake, millions still need aid. www.huffingtonpost.com/entry/haiti-earthquake-anniversary_us_5875108de4b02b5f858b3f9c. Accessed October 6, 2017.
3. Sandoval E, Marcius CR, Durkin E, Dillon N. Hurricane Sandy victims’ homes still uninhabitable nearly five years later. www.nydailynews.com/new-york/hurricane-sandy-victims-living-limbo-years-article-1.3463866. Accessed October 6, 2017.
Are Aspartame’s Benefits Sugarcoated?
Since my high school days, I have used some form of artificial sweetener in lieu of sugar. Long believing that sugar avoidance was the key to weight maintenance, I didn’t give much thought to the published ill effects of sugar substitutes—after all, I wasn’t a mouse, and I wasn’t consuming mass doses. Did the artificial sweeteners assist in controlling my weight? Quite honestly, I doubt it—but I was so used to being “sugar free” that I was habituated to using these products.
Several years ago at a luncheon, I was reaching for a packet of artificial sweetener to pour into my iced tea when an NP friend stopped me. She and her husband (a pharmacist) had sworn off these products after noting that he was having issues with his cognition and experiencing increased irritability. With no obvious cause for these symptoms, they investigated his diet. He had, over the previous year, increased his use of aspartame. They found research supporting an association between aspartame and changes in behavior and cognition. When he stopped using the product, they both noticed a return to his former jovial, intellectual self. I acknowledged their research conclusion as an “n = 1” but gave it no further credence.
More recently, friends who had adopted an “all-natural” diet chastised me for drinking sugar-free seltzer. I had switched years ago from diet sodas to this beverage as my primary source of hydration. What could be wrong? It had zero calories, no sodium, and no sugar. Ah, but it contained aspartame! Since switching to a food plan without aspartame, my friends had observed that they were feeling better and more alert. Hmm, sounded familiar … maybe there was something to these claims after all. I did a little research of my own, and was I surprised!
On the exterior, aspartame is a highly studied food additive with decades of research demonstrating its safety for human consumption.1 But what exactly happens when this sweetener is ingested? First, aspartame breaks down into amino acids and methanol (ie, wood alcohol). The methanol continues to break down into formaldehyde and formic acid, a substance commonly found in bee and ant venom (see Figure). And if that weren’t enough, a potential brain tumor agent (aspartylphenylalanine diketopiperazine) is also a residual byproduct.2,3 As you might expect, these components and byproducts come with varying adverse effects and potential health risks.
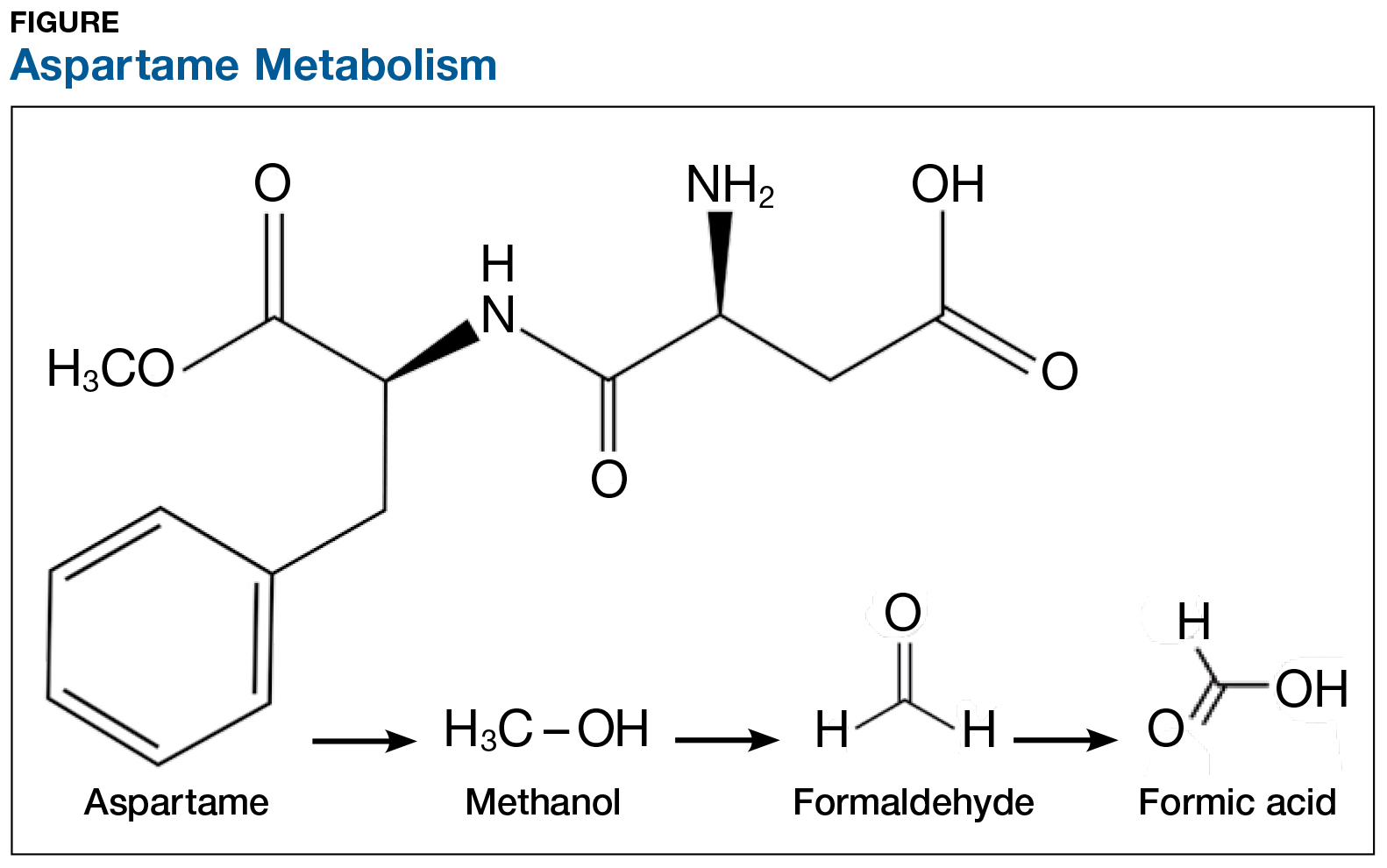
The majority of artificially sweetened beverages (ASBs) contain aspartame. As early as 1984—a mere six months after aspartame was approved for use in soft drinks—the FDA, with the assistance of the CDC, undertook an investigation of consumer complaints related to its use. The research team interviewed 517 complainants; 346 (67%) reported neurologic/behavioral symptoms, including headache, dizziness, and mood alteration.4 Despite that statistic, however, the researchers reported no evidence for the existence of serious, widespread, adverse health consequences resulting from aspartame consumption.4
Reading these reports reminded me of my friends’ comments and strongly suggested to me that soft drinks containing aspartame may be hard on the brain. Further to this point, a recent study found that ASB consumption is associated with an increased risk for stroke and dementia.5
Additional studies—including evaluations of possible associations between aspartame and headaches, seizures, behavior, cognition, and mood, as well as allergic-type reactions and use by potentially sensitive subpopulations—have been conducted. The verdict? Scientists maintain that aspartame is safe and that there are no unresolved questions regarding its safety when used as intended.6 Some researchers question the validity of the link between ASB consumption and negative health consequences, suggesting that individuals in worse health consume diet beverages in an effort to slow health deterioration or to lose weight.7 Yet, the debate about the effects of aspartame on our organs continues.
The number of epidemiologic studies that document strong associations between frequent ASB consumption and illness suggests that substituting or promoting artificial sweeteners as “healthy alternatives” to sugar may not be advisable.8 In fact, the most recent studies indicate that artificial sweeteners—the very compounds marketed to assist with weight control—can lead to weight gain, as they trick our brains into craving high-calorie foods. Moreover, ASB consumption is associated with a 21% increased risk for type 2 diabetes.9 Azad and colleagues found that evidence does not clearly support the use of nonnutritive sweeteners for weight management; they recommend using caution with these products until the long-term risks and benefits are fully understood.7
Is satisfying your sweet tooth with sugar alternatives worth the potential risk? Most of the studies conducted to support or refute aspartame-related health concerns prove correlation, not causality. A purist might point out that many of the studies have limitations that can lead to faulty conclusions. Be that as it may, it still gives one pause.
Small doses of aspartame each day might not be a tipping point toward the documented health complaints, but the consistent concerns about its effects were enough for me to make the switch to plain water, and sugar for my coffee. I do believe that Mary Poppins was correct—a spoonful of sugar does help—and I, for one, am following her lead.
What do you think? Are these concerns unfounded, or are we sweetening our road to poor health? Share your thoughts with me at [email protected].
1. Novella S. Aspartame: truth vs. fiction. https://sciencebasedmedicine.org/aspartame-truth-vs-fiction/. Accessed August 1, 2017.
2. Barua J, Bal A. Emerging facts about aspartame. www.manningsscience.com/uploads/8/6/8/1/8681125/article-on-aspartame.pdf. Accessed August 1, 2017.
3. Supersweet blog. Learning about sweeteners. https://supersweetblog.wordpress.com/aspartame/. Accessed August 1, 2017.
4. CDC. Evaluation of consumer complaints related to aspartame use. MMWR Morb Mortal Wkly Rep. 1984;33(43):605-607.
5. Pase MP, Himali JJ, Beiser AS, et al. Sugar- and artificially sweetened beverages and the risks of incident stroke and dementia: a prospective cohort study. Stroke. 2017;48(5): 1139-1146.
6. Butchko HH, Stargel WW, Comer CP, et al. Aspartame: review of safety. Regul Toxicol Pharmacol. 2002;35(2):S1- S93.
7. Azad MB, Abou-Setta AM, Chauhan BF, et al. Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ. 2017;189(28): E929-E939.
8. Wersching H, Gardener H, Sacco L. Sugar-sweetened and artificially sweetened beverages in relation to stroke and dementia. Stroke. 2017;48(5):1129-1131.
9. Huang M, Quddus A, Stinson L, et al. Artificially sweetened beverages, sugar-sweetened beverages, plain water, and incident diabetes mellitus in postmenopausal women: the prospective Women’s Health Initiative observational study. Am J Clin Nutr. 2017;106:614-622.
Since my high school days, I have used some form of artificial sweetener in lieu of sugar. Long believing that sugar avoidance was the key to weight maintenance, I didn’t give much thought to the published ill effects of sugar substitutes—after all, I wasn’t a mouse, and I wasn’t consuming mass doses. Did the artificial sweeteners assist in controlling my weight? Quite honestly, I doubt it—but I was so used to being “sugar free” that I was habituated to using these products.
Several years ago at a luncheon, I was reaching for a packet of artificial sweetener to pour into my iced tea when an NP friend stopped me. She and her husband (a pharmacist) had sworn off these products after noting that he was having issues with his cognition and experiencing increased irritability. With no obvious cause for these symptoms, they investigated his diet. He had, over the previous year, increased his use of aspartame. They found research supporting an association between aspartame and changes in behavior and cognition. When he stopped using the product, they both noticed a return to his former jovial, intellectual self. I acknowledged their research conclusion as an “n = 1” but gave it no further credence.
More recently, friends who had adopted an “all-natural” diet chastised me for drinking sugar-free seltzer. I had switched years ago from diet sodas to this beverage as my primary source of hydration. What could be wrong? It had zero calories, no sodium, and no sugar. Ah, but it contained aspartame! Since switching to a food plan without aspartame, my friends had observed that they were feeling better and more alert. Hmm, sounded familiar … maybe there was something to these claims after all. I did a little research of my own, and was I surprised!
On the exterior, aspartame is a highly studied food additive with decades of research demonstrating its safety for human consumption.1 But what exactly happens when this sweetener is ingested? First, aspartame breaks down into amino acids and methanol (ie, wood alcohol). The methanol continues to break down into formaldehyde and formic acid, a substance commonly found in bee and ant venom (see Figure). And if that weren’t enough, a potential brain tumor agent (aspartylphenylalanine diketopiperazine) is also a residual byproduct.2,3 As you might expect, these components and byproducts come with varying adverse effects and potential health risks.
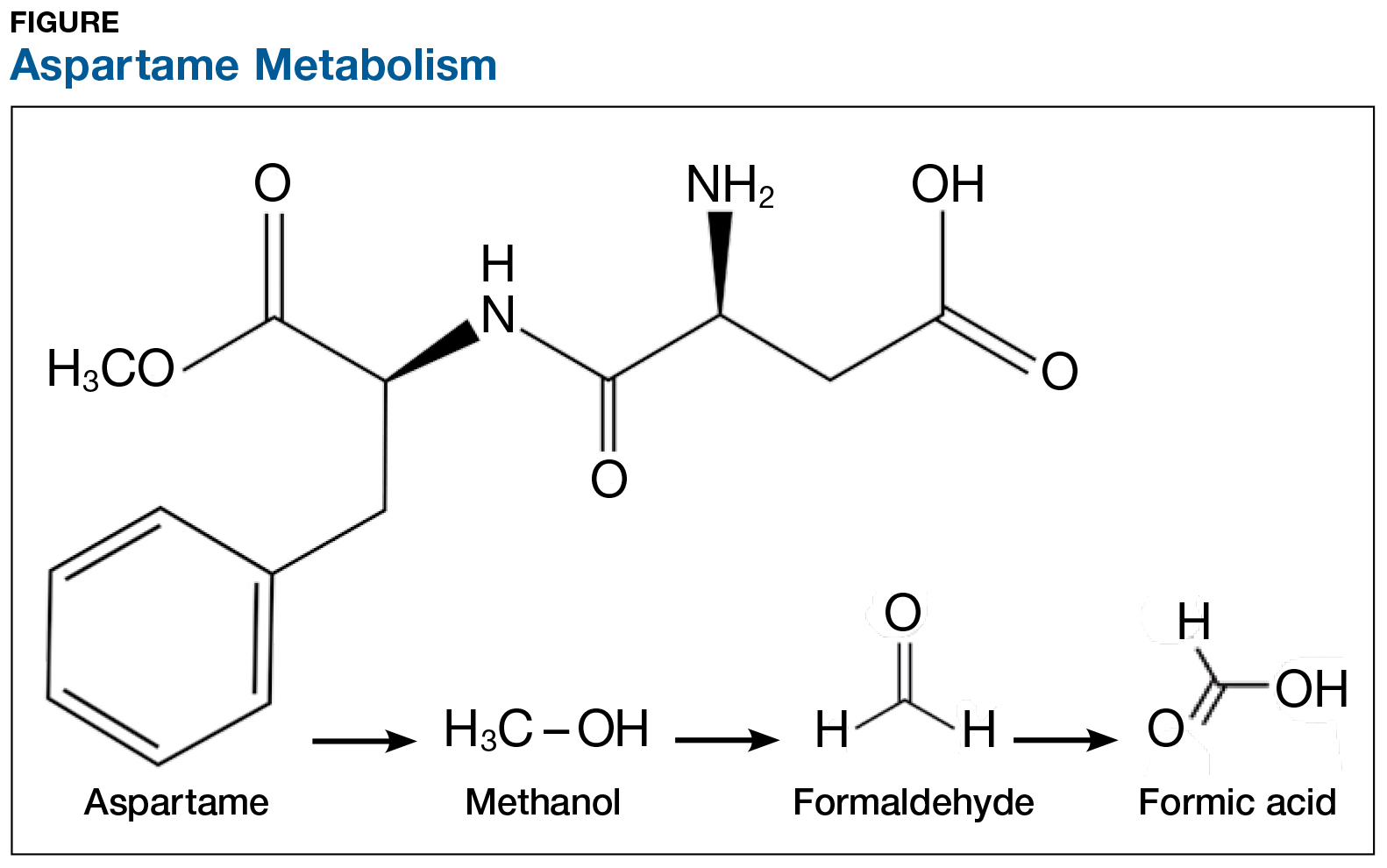
The majority of artificially sweetened beverages (ASBs) contain aspartame. As early as 1984—a mere six months after aspartame was approved for use in soft drinks—the FDA, with the assistance of the CDC, undertook an investigation of consumer complaints related to its use. The research team interviewed 517 complainants; 346 (67%) reported neurologic/behavioral symptoms, including headache, dizziness, and mood alteration.4 Despite that statistic, however, the researchers reported no evidence for the existence of serious, widespread, adverse health consequences resulting from aspartame consumption.4
Reading these reports reminded me of my friends’ comments and strongly suggested to me that soft drinks containing aspartame may be hard on the brain. Further to this point, a recent study found that ASB consumption is associated with an increased risk for stroke and dementia.5
Additional studies—including evaluations of possible associations between aspartame and headaches, seizures, behavior, cognition, and mood, as well as allergic-type reactions and use by potentially sensitive subpopulations—have been conducted. The verdict? Scientists maintain that aspartame is safe and that there are no unresolved questions regarding its safety when used as intended.6 Some researchers question the validity of the link between ASB consumption and negative health consequences, suggesting that individuals in worse health consume diet beverages in an effort to slow health deterioration or to lose weight.7 Yet, the debate about the effects of aspartame on our organs continues.
The number of epidemiologic studies that document strong associations between frequent ASB consumption and illness suggests that substituting or promoting artificial sweeteners as “healthy alternatives” to sugar may not be advisable.8 In fact, the most recent studies indicate that artificial sweeteners—the very compounds marketed to assist with weight control—can lead to weight gain, as they trick our brains into craving high-calorie foods. Moreover, ASB consumption is associated with a 21% increased risk for type 2 diabetes.9 Azad and colleagues found that evidence does not clearly support the use of nonnutritive sweeteners for weight management; they recommend using caution with these products until the long-term risks and benefits are fully understood.7
Is satisfying your sweet tooth with sugar alternatives worth the potential risk? Most of the studies conducted to support or refute aspartame-related health concerns prove correlation, not causality. A purist might point out that many of the studies have limitations that can lead to faulty conclusions. Be that as it may, it still gives one pause.
Small doses of aspartame each day might not be a tipping point toward the documented health complaints, but the consistent concerns about its effects were enough for me to make the switch to plain water, and sugar for my coffee. I do believe that Mary Poppins was correct—a spoonful of sugar does help—and I, for one, am following her lead.
What do you think? Are these concerns unfounded, or are we sweetening our road to poor health? Share your thoughts with me at [email protected].
Since my high school days, I have used some form of artificial sweetener in lieu of sugar. Long believing that sugar avoidance was the key to weight maintenance, I didn’t give much thought to the published ill effects of sugar substitutes—after all, I wasn’t a mouse, and I wasn’t consuming mass doses. Did the artificial sweeteners assist in controlling my weight? Quite honestly, I doubt it—but I was so used to being “sugar free” that I was habituated to using these products.
Several years ago at a luncheon, I was reaching for a packet of artificial sweetener to pour into my iced tea when an NP friend stopped me. She and her husband (a pharmacist) had sworn off these products after noting that he was having issues with his cognition and experiencing increased irritability. With no obvious cause for these symptoms, they investigated his diet. He had, over the previous year, increased his use of aspartame. They found research supporting an association between aspartame and changes in behavior and cognition. When he stopped using the product, they both noticed a return to his former jovial, intellectual self. I acknowledged their research conclusion as an “n = 1” but gave it no further credence.
More recently, friends who had adopted an “all-natural” diet chastised me for drinking sugar-free seltzer. I had switched years ago from diet sodas to this beverage as my primary source of hydration. What could be wrong? It had zero calories, no sodium, and no sugar. Ah, but it contained aspartame! Since switching to a food plan without aspartame, my friends had observed that they were feeling better and more alert. Hmm, sounded familiar … maybe there was something to these claims after all. I did a little research of my own, and was I surprised!
On the exterior, aspartame is a highly studied food additive with decades of research demonstrating its safety for human consumption.1 But what exactly happens when this sweetener is ingested? First, aspartame breaks down into amino acids and methanol (ie, wood alcohol). The methanol continues to break down into formaldehyde and formic acid, a substance commonly found in bee and ant venom (see Figure). And if that weren’t enough, a potential brain tumor agent (aspartylphenylalanine diketopiperazine) is also a residual byproduct.2,3 As you might expect, these components and byproducts come with varying adverse effects and potential health risks.
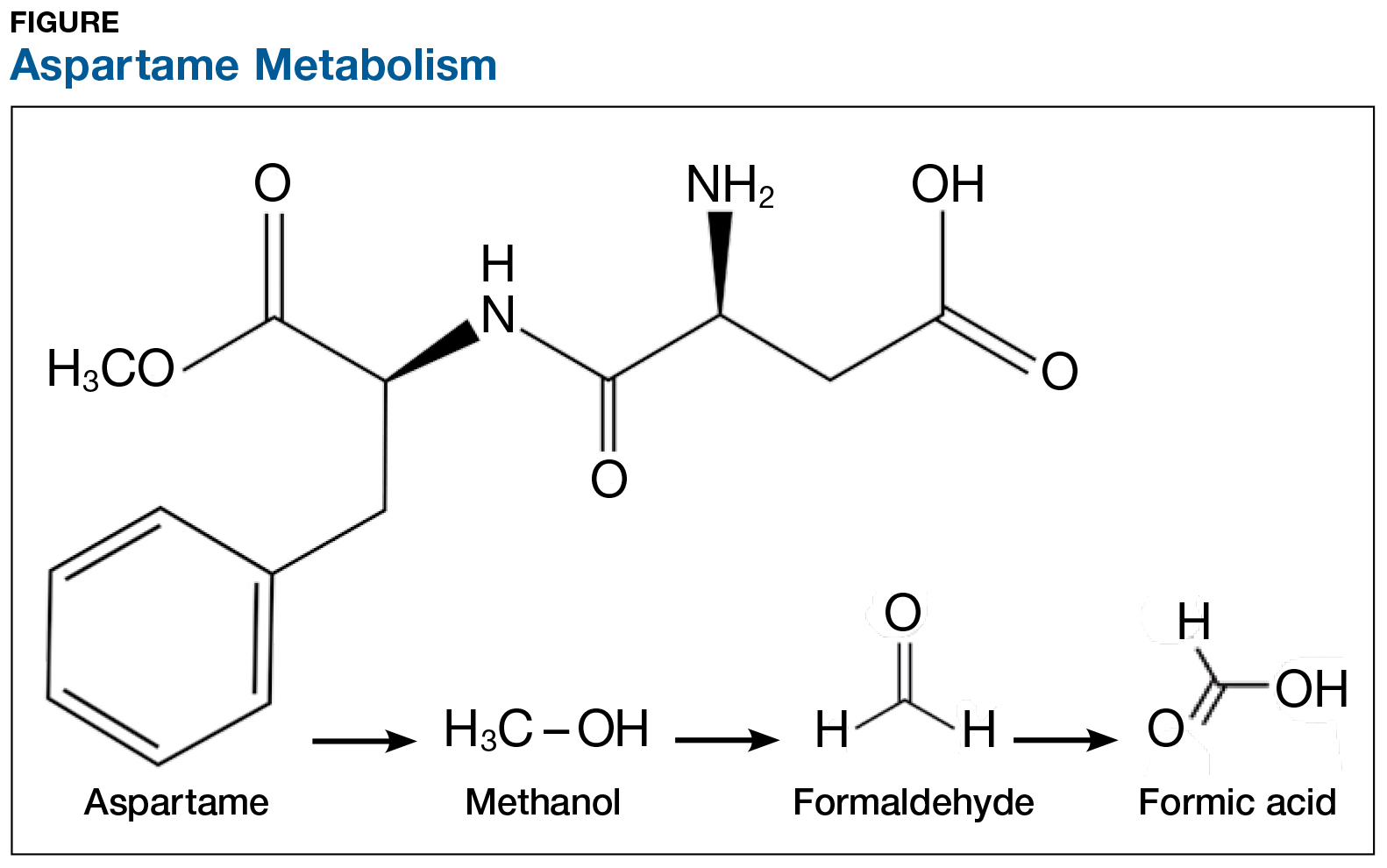
The majority of artificially sweetened beverages (ASBs) contain aspartame. As early as 1984—a mere six months after aspartame was approved for use in soft drinks—the FDA, with the assistance of the CDC, undertook an investigation of consumer complaints related to its use. The research team interviewed 517 complainants; 346 (67%) reported neurologic/behavioral symptoms, including headache, dizziness, and mood alteration.4 Despite that statistic, however, the researchers reported no evidence for the existence of serious, widespread, adverse health consequences resulting from aspartame consumption.4
Reading these reports reminded me of my friends’ comments and strongly suggested to me that soft drinks containing aspartame may be hard on the brain. Further to this point, a recent study found that ASB consumption is associated with an increased risk for stroke and dementia.5
Additional studies—including evaluations of possible associations between aspartame and headaches, seizures, behavior, cognition, and mood, as well as allergic-type reactions and use by potentially sensitive subpopulations—have been conducted. The verdict? Scientists maintain that aspartame is safe and that there are no unresolved questions regarding its safety when used as intended.6 Some researchers question the validity of the link between ASB consumption and negative health consequences, suggesting that individuals in worse health consume diet beverages in an effort to slow health deterioration or to lose weight.7 Yet, the debate about the effects of aspartame on our organs continues.
The number of epidemiologic studies that document strong associations between frequent ASB consumption and illness suggests that substituting or promoting artificial sweeteners as “healthy alternatives” to sugar may not be advisable.8 In fact, the most recent studies indicate that artificial sweeteners—the very compounds marketed to assist with weight control—can lead to weight gain, as they trick our brains into craving high-calorie foods. Moreover, ASB consumption is associated with a 21% increased risk for type 2 diabetes.9 Azad and colleagues found that evidence does not clearly support the use of nonnutritive sweeteners for weight management; they recommend using caution with these products until the long-term risks and benefits are fully understood.7
Is satisfying your sweet tooth with sugar alternatives worth the potential risk? Most of the studies conducted to support or refute aspartame-related health concerns prove correlation, not causality. A purist might point out that many of the studies have limitations that can lead to faulty conclusions. Be that as it may, it still gives one pause.
Small doses of aspartame each day might not be a tipping point toward the documented health complaints, but the consistent concerns about its effects were enough for me to make the switch to plain water, and sugar for my coffee. I do believe that Mary Poppins was correct—a spoonful of sugar does help—and I, for one, am following her lead.
What do you think? Are these concerns unfounded, or are we sweetening our road to poor health? Share your thoughts with me at [email protected].
1. Novella S. Aspartame: truth vs. fiction. https://sciencebasedmedicine.org/aspartame-truth-vs-fiction/. Accessed August 1, 2017.
2. Barua J, Bal A. Emerging facts about aspartame. www.manningsscience.com/uploads/8/6/8/1/8681125/article-on-aspartame.pdf. Accessed August 1, 2017.
3. Supersweet blog. Learning about sweeteners. https://supersweetblog.wordpress.com/aspartame/. Accessed August 1, 2017.
4. CDC. Evaluation of consumer complaints related to aspartame use. MMWR Morb Mortal Wkly Rep. 1984;33(43):605-607.
5. Pase MP, Himali JJ, Beiser AS, et al. Sugar- and artificially sweetened beverages and the risks of incident stroke and dementia: a prospective cohort study. Stroke. 2017;48(5): 1139-1146.
6. Butchko HH, Stargel WW, Comer CP, et al. Aspartame: review of safety. Regul Toxicol Pharmacol. 2002;35(2):S1- S93.
7. Azad MB, Abou-Setta AM, Chauhan BF, et al. Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ. 2017;189(28): E929-E939.
8. Wersching H, Gardener H, Sacco L. Sugar-sweetened and artificially sweetened beverages in relation to stroke and dementia. Stroke. 2017;48(5):1129-1131.
9. Huang M, Quddus A, Stinson L, et al. Artificially sweetened beverages, sugar-sweetened beverages, plain water, and incident diabetes mellitus in postmenopausal women: the prospective Women’s Health Initiative observational study. Am J Clin Nutr. 2017;106:614-622.
1. Novella S. Aspartame: truth vs. fiction. https://sciencebasedmedicine.org/aspartame-truth-vs-fiction/. Accessed August 1, 2017.
2. Barua J, Bal A. Emerging facts about aspartame. www.manningsscience.com/uploads/8/6/8/1/8681125/article-on-aspartame.pdf. Accessed August 1, 2017.
3. Supersweet blog. Learning about sweeteners. https://supersweetblog.wordpress.com/aspartame/. Accessed August 1, 2017.
4. CDC. Evaluation of consumer complaints related to aspartame use. MMWR Morb Mortal Wkly Rep. 1984;33(43):605-607.
5. Pase MP, Himali JJ, Beiser AS, et al. Sugar- and artificially sweetened beverages and the risks of incident stroke and dementia: a prospective cohort study. Stroke. 2017;48(5): 1139-1146.
6. Butchko HH, Stargel WW, Comer CP, et al. Aspartame: review of safety. Regul Toxicol Pharmacol. 2002;35(2):S1- S93.
7. Azad MB, Abou-Setta AM, Chauhan BF, et al. Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ. 2017;189(28): E929-E939.
8. Wersching H, Gardener H, Sacco L. Sugar-sweetened and artificially sweetened beverages in relation to stroke and dementia. Stroke. 2017;48(5):1129-1131.
9. Huang M, Quddus A, Stinson L, et al. Artificially sweetened beverages, sugar-sweetened beverages, plain water, and incident diabetes mellitus in postmenopausal women: the prospective Women’s Health Initiative observational study. Am J Clin Nutr. 2017;106:614-622.
More Than “Teen Angst”: What to Watch For
The incidence of high-risk behavior among teenagers has attracted increased media attention lately. It feels like a new report surfaces every day detailing the death of one or more teens as a result of alcohol, illicit drug use, or speeding. These risky behaviors grab our attention; they are overt and somewhat public. But behaviors that correlate with anxiety and depression, which can in turn lead to suicide or suicidal ideation, are more subtle—and that is what concerns me.
The data on suicide is staggering. On a daily basis, almost 3,000 people worldwide complete suicide, and approximately 20 times as many survive a suicide attempt.1 Annually, deaths resulting from suicide exceed deaths from homicide and war combined.2 In 2013, there were 41,149 suicides in the US—that translates to a rate of 113 suicides each day, or one every 13 minutes.3 Suicide has surpassed homicide to become the second leading cause of death among 10- to 29-year-olds; in 2012, suicide claimed the lives of more than 5,000 people within this age bracket.4,5 In the 2013 Youth Risk Behavior Survey (YRBS), 17.7% of high school students reported seriously considering suicide during the prior 12 months, and nearly 9% of those students had attempted suicide during that same period.6 I wonder how many of those students exhibited telling behaviors that went unnoticed.
What are these subtle signs that are so easily overlooked? Behaviors most might consider “within the norm” of today’s youth—hours playing video games, sending hundreds of texts every day, lack of exercise, and lack of sleep. Research has demonstrated that moderate-to-vigorous physical activity reduces the incidence of depression in adolescents.7 A 2014 study of European teens published in World Psychiatry found that the adolescents most at risk for symptoms of depression and anxiety are those who are fixated on media, don’t get enough sleep, and have a sedentary lifestyle.8 Hmm... sounds like many US teenagers today. While that doesn’t mean that every teen who lacks sleep, plays video games, or isn’t active is at risk, we do need to pay closer attention to them, because this combination exacerbates risk.
There’s another unhealthy habit that contributes to the risk for teen suicidality: smoking and use of electronic vapor products (EVPs). The 2015 YRBS, which surveyed more than 15,000 high school students, noted that 3.2% smoked cigarettes only, 15.8% used EVPs only, and 7.5% were dual users. Analysis of that data identified associations between health-risk behaviors and both cigarette smoking and EVP use.9 Teens who smoked or used EVPs were more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers. Moreover, compared with nonusers, cigarette-only, EVP-only, and dual smokers were significantly more likely to attempt suicide; cigarette-only smokers were more likely than EVP-only users to attempt suicide.9
Smoking, inactivity, sleep deprivation, and social isolation (because texting or face-timing with your friends is not being social) are a recipe for depression and anxiety in an adolescent. Sleep deprivation alone has been linked to depression and may be associated with a decreased ability to control, inhibit, or change emotional responses.10 Far too often, teens view suicide as the only relief from these feelings.
Awareness of this problem has grown in the past 30 years. The YRBS was developed in 1990 to monitor priority health risk behaviors that contribute to the leading causes of death, disability, and social problems among youth in the US—one of which is suicide.11 In 2001, the Department of Health and Human Services introduced the National Strategy for Suicide Prevention, the first national program of its kind, and released an evidence-based practice guide for school-based suicide prevention plans.12 The 2002 Institute of Medicine report Reducing Suicide: A National Imperative recognized the need for early recognition and prevention of suicidality.13 And yet, we still have the staggering statistics I cited earlier.
Because of their proximity to children and adolescents, schools are frequently viewed as an integral setting for youth suicide prevention efforts. It is encouraging that suicide prevention programs exist in more than 77% of US public schools—but disheartening that it is not 100%.
And what about the rest of us? What can we, as health care providers, do to stem this tide of teen suicide? The importance of early prevention strategies to reduce onset of suicidal thoughts and help identify persons who are at risk for or are currently contemplating suicide cannot be overemphasized. We need more health care practitioners who are trained to assess suicide plans and to intervene with young persons. This involves education in recognizing risk factors and making appropriate referrals, expanding access to social services, reducing stigma and other barriers to seeking help, and providing awareness that suicide prevention is paramount.
It is incumbent on us as health care providers to screen for and ask our teenaged patients about those subtle behaviors. As adults, it is our responsibility to support and watch over our youth. In the words of former Surgeon General David Satcher, “We must act now. We cannot change the past, but together we can shape a different future.”14
1. World Health Organization. World Suicide Prevention Day. www.who.int/mediacentre/news/statements/2007/s16/en/. Accessed February 2, 2017
2. World Health Organization. Suicide huge but preventable public health problem, says WHO. www.who.int/mediacentre/news/releases/2004/pr61/en. Accessed February 2, 2017.
3. CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). www.cdc.gov/injury/wisqars/index.html. Accessed February 2, 2017.
4. World Health Organization. Suicide. www.who.int/mediacentre/factsheets/fs398/en. Accessed February 2, 2017.
5. CDC. Suicide trends among persons aged 10-24 years—United States, 1994-2012. www.cdc.gov/mmwr/pdf/wk/mm6408.pdf. Accessed February 2, 2017.
6. CDC. Trends in the prevalence of suicide-related behavior. National Youth Risk Behavior Survey: 1991-2013. www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/us_suicide_trend_yrbs.pdf. Accessed February 2, 2017.
7. Zahl T, Steinsbekk S, Wichstrøm L. Physical activity, sedentary behavior, and symptoms of major depression in middle childhood. Pediatrics. 2017;139(2):e20161711.
8. Carli V, Hoven CW, Wasserman C, et al. A newly identified group of adolescents at “invisible” risk for psychopathology and suicidal behavior: findings from the SEYLE study. World Psychiatry. 2014;13(1):78-86.
9. Demissie Z, Everett Jones S, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921.
10. National Sleep Foundation. Adolescent sleep needs and patterns. https://sleepfoundation.org/sites/default/files/sleep_and_teens_report1.pdf. Accessed February 2, 2017.
11. CDC. Youth Risk Behavior Surveillance System (YRBSS) overview. www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Accessed February 2, 2017.
12. Cooper GD, Clements PT, Holt K. A review and application of suicide prevention programs in high school settings. Issues Ment Health Nurs. 2011;32(11):696-702.
13. Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: National Academics Press; 2002.
14. US Public Health Service. The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: 1999.
The incidence of high-risk behavior among teenagers has attracted increased media attention lately. It feels like a new report surfaces every day detailing the death of one or more teens as a result of alcohol, illicit drug use, or speeding. These risky behaviors grab our attention; they are overt and somewhat public. But behaviors that correlate with anxiety and depression, which can in turn lead to suicide or suicidal ideation, are more subtle—and that is what concerns me.
The data on suicide is staggering. On a daily basis, almost 3,000 people worldwide complete suicide, and approximately 20 times as many survive a suicide attempt.1 Annually, deaths resulting from suicide exceed deaths from homicide and war combined.2 In 2013, there were 41,149 suicides in the US—that translates to a rate of 113 suicides each day, or one every 13 minutes.3 Suicide has surpassed homicide to become the second leading cause of death among 10- to 29-year-olds; in 2012, suicide claimed the lives of more than 5,000 people within this age bracket.4,5 In the 2013 Youth Risk Behavior Survey (YRBS), 17.7% of high school students reported seriously considering suicide during the prior 12 months, and nearly 9% of those students had attempted suicide during that same period.6 I wonder how many of those students exhibited telling behaviors that went unnoticed.
What are these subtle signs that are so easily overlooked? Behaviors most might consider “within the norm” of today’s youth—hours playing video games, sending hundreds of texts every day, lack of exercise, and lack of sleep. Research has demonstrated that moderate-to-vigorous physical activity reduces the incidence of depression in adolescents.7 A 2014 study of European teens published in World Psychiatry found that the adolescents most at risk for symptoms of depression and anxiety are those who are fixated on media, don’t get enough sleep, and have a sedentary lifestyle.8 Hmm... sounds like many US teenagers today. While that doesn’t mean that every teen who lacks sleep, plays video games, or isn’t active is at risk, we do need to pay closer attention to them, because this combination exacerbates risk.
There’s another unhealthy habit that contributes to the risk for teen suicidality: smoking and use of electronic vapor products (EVPs). The 2015 YRBS, which surveyed more than 15,000 high school students, noted that 3.2% smoked cigarettes only, 15.8% used EVPs only, and 7.5% were dual users. Analysis of that data identified associations between health-risk behaviors and both cigarette smoking and EVP use.9 Teens who smoked or used EVPs were more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers. Moreover, compared with nonusers, cigarette-only, EVP-only, and dual smokers were significantly more likely to attempt suicide; cigarette-only smokers were more likely than EVP-only users to attempt suicide.9
Smoking, inactivity, sleep deprivation, and social isolation (because texting or face-timing with your friends is not being social) are a recipe for depression and anxiety in an adolescent. Sleep deprivation alone has been linked to depression and may be associated with a decreased ability to control, inhibit, or change emotional responses.10 Far too often, teens view suicide as the only relief from these feelings.
Awareness of this problem has grown in the past 30 years. The YRBS was developed in 1990 to monitor priority health risk behaviors that contribute to the leading causes of death, disability, and social problems among youth in the US—one of which is suicide.11 In 2001, the Department of Health and Human Services introduced the National Strategy for Suicide Prevention, the first national program of its kind, and released an evidence-based practice guide for school-based suicide prevention plans.12 The 2002 Institute of Medicine report Reducing Suicide: A National Imperative recognized the need for early recognition and prevention of suicidality.13 And yet, we still have the staggering statistics I cited earlier.
Because of their proximity to children and adolescents, schools are frequently viewed as an integral setting for youth suicide prevention efforts. It is encouraging that suicide prevention programs exist in more than 77% of US public schools—but disheartening that it is not 100%.
And what about the rest of us? What can we, as health care providers, do to stem this tide of teen suicide? The importance of early prevention strategies to reduce onset of suicidal thoughts and help identify persons who are at risk for or are currently contemplating suicide cannot be overemphasized. We need more health care practitioners who are trained to assess suicide plans and to intervene with young persons. This involves education in recognizing risk factors and making appropriate referrals, expanding access to social services, reducing stigma and other barriers to seeking help, and providing awareness that suicide prevention is paramount.
It is incumbent on us as health care providers to screen for and ask our teenaged patients about those subtle behaviors. As adults, it is our responsibility to support and watch over our youth. In the words of former Surgeon General David Satcher, “We must act now. We cannot change the past, but together we can shape a different future.”14
The incidence of high-risk behavior among teenagers has attracted increased media attention lately. It feels like a new report surfaces every day detailing the death of one or more teens as a result of alcohol, illicit drug use, or speeding. These risky behaviors grab our attention; they are overt and somewhat public. But behaviors that correlate with anxiety and depression, which can in turn lead to suicide or suicidal ideation, are more subtle—and that is what concerns me.
The data on suicide is staggering. On a daily basis, almost 3,000 people worldwide complete suicide, and approximately 20 times as many survive a suicide attempt.1 Annually, deaths resulting from suicide exceed deaths from homicide and war combined.2 In 2013, there were 41,149 suicides in the US—that translates to a rate of 113 suicides each day, or one every 13 minutes.3 Suicide has surpassed homicide to become the second leading cause of death among 10- to 29-year-olds; in 2012, suicide claimed the lives of more than 5,000 people within this age bracket.4,5 In the 2013 Youth Risk Behavior Survey (YRBS), 17.7% of high school students reported seriously considering suicide during the prior 12 months, and nearly 9% of those students had attempted suicide during that same period.6 I wonder how many of those students exhibited telling behaviors that went unnoticed.
What are these subtle signs that are so easily overlooked? Behaviors most might consider “within the norm” of today’s youth—hours playing video games, sending hundreds of texts every day, lack of exercise, and lack of sleep. Research has demonstrated that moderate-to-vigorous physical activity reduces the incidence of depression in adolescents.7 A 2014 study of European teens published in World Psychiatry found that the adolescents most at risk for symptoms of depression and anxiety are those who are fixated on media, don’t get enough sleep, and have a sedentary lifestyle.8 Hmm... sounds like many US teenagers today. While that doesn’t mean that every teen who lacks sleep, plays video games, or isn’t active is at risk, we do need to pay closer attention to them, because this combination exacerbates risk.
There’s another unhealthy habit that contributes to the risk for teen suicidality: smoking and use of electronic vapor products (EVPs). The 2015 YRBS, which surveyed more than 15,000 high school students, noted that 3.2% smoked cigarettes only, 15.8% used EVPs only, and 7.5% were dual users. Analysis of that data identified associations between health-risk behaviors and both cigarette smoking and EVP use.9 Teens who smoked or used EVPs were more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers. Moreover, compared with nonusers, cigarette-only, EVP-only, and dual smokers were significantly more likely to attempt suicide; cigarette-only smokers were more likely than EVP-only users to attempt suicide.9
Smoking, inactivity, sleep deprivation, and social isolation (because texting or face-timing with your friends is not being social) are a recipe for depression and anxiety in an adolescent. Sleep deprivation alone has been linked to depression and may be associated with a decreased ability to control, inhibit, or change emotional responses.10 Far too often, teens view suicide as the only relief from these feelings.
Awareness of this problem has grown in the past 30 years. The YRBS was developed in 1990 to monitor priority health risk behaviors that contribute to the leading causes of death, disability, and social problems among youth in the US—one of which is suicide.11 In 2001, the Department of Health and Human Services introduced the National Strategy for Suicide Prevention, the first national program of its kind, and released an evidence-based practice guide for school-based suicide prevention plans.12 The 2002 Institute of Medicine report Reducing Suicide: A National Imperative recognized the need for early recognition and prevention of suicidality.13 And yet, we still have the staggering statistics I cited earlier.
Because of their proximity to children and adolescents, schools are frequently viewed as an integral setting for youth suicide prevention efforts. It is encouraging that suicide prevention programs exist in more than 77% of US public schools—but disheartening that it is not 100%.
And what about the rest of us? What can we, as health care providers, do to stem this tide of teen suicide? The importance of early prevention strategies to reduce onset of suicidal thoughts and help identify persons who are at risk for or are currently contemplating suicide cannot be overemphasized. We need more health care practitioners who are trained to assess suicide plans and to intervene with young persons. This involves education in recognizing risk factors and making appropriate referrals, expanding access to social services, reducing stigma and other barriers to seeking help, and providing awareness that suicide prevention is paramount.
It is incumbent on us as health care providers to screen for and ask our teenaged patients about those subtle behaviors. As adults, it is our responsibility to support and watch over our youth. In the words of former Surgeon General David Satcher, “We must act now. We cannot change the past, but together we can shape a different future.”14
1. World Health Organization. World Suicide Prevention Day. www.who.int/mediacentre/news/statements/2007/s16/en/. Accessed February 2, 2017
2. World Health Organization. Suicide huge but preventable public health problem, says WHO. www.who.int/mediacentre/news/releases/2004/pr61/en. Accessed February 2, 2017.
3. CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). www.cdc.gov/injury/wisqars/index.html. Accessed February 2, 2017.
4. World Health Organization. Suicide. www.who.int/mediacentre/factsheets/fs398/en. Accessed February 2, 2017.
5. CDC. Suicide trends among persons aged 10-24 years—United States, 1994-2012. www.cdc.gov/mmwr/pdf/wk/mm6408.pdf. Accessed February 2, 2017.
6. CDC. Trends in the prevalence of suicide-related behavior. National Youth Risk Behavior Survey: 1991-2013. www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/us_suicide_trend_yrbs.pdf. Accessed February 2, 2017.
7. Zahl T, Steinsbekk S, Wichstrøm L. Physical activity, sedentary behavior, and symptoms of major depression in middle childhood. Pediatrics. 2017;139(2):e20161711.
8. Carli V, Hoven CW, Wasserman C, et al. A newly identified group of adolescents at “invisible” risk for psychopathology and suicidal behavior: findings from the SEYLE study. World Psychiatry. 2014;13(1):78-86.
9. Demissie Z, Everett Jones S, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921.
10. National Sleep Foundation. Adolescent sleep needs and patterns. https://sleepfoundation.org/sites/default/files/sleep_and_teens_report1.pdf. Accessed February 2, 2017.
11. CDC. Youth Risk Behavior Surveillance System (YRBSS) overview. www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Accessed February 2, 2017.
12. Cooper GD, Clements PT, Holt K. A review and application of suicide prevention programs in high school settings. Issues Ment Health Nurs. 2011;32(11):696-702.
13. Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: National Academics Press; 2002.
14. US Public Health Service. The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: 1999.
1. World Health Organization. World Suicide Prevention Day. www.who.int/mediacentre/news/statements/2007/s16/en/. Accessed February 2, 2017
2. World Health Organization. Suicide huge but preventable public health problem, says WHO. www.who.int/mediacentre/news/releases/2004/pr61/en. Accessed February 2, 2017.
3. CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). www.cdc.gov/injury/wisqars/index.html. Accessed February 2, 2017.
4. World Health Organization. Suicide. www.who.int/mediacentre/factsheets/fs398/en. Accessed February 2, 2017.
5. CDC. Suicide trends among persons aged 10-24 years—United States, 1994-2012. www.cdc.gov/mmwr/pdf/wk/mm6408.pdf. Accessed February 2, 2017.
6. CDC. Trends in the prevalence of suicide-related behavior. National Youth Risk Behavior Survey: 1991-2013. www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/us_suicide_trend_yrbs.pdf. Accessed February 2, 2017.
7. Zahl T, Steinsbekk S, Wichstrøm L. Physical activity, sedentary behavior, and symptoms of major depression in middle childhood. Pediatrics. 2017;139(2):e20161711.
8. Carli V, Hoven CW, Wasserman C, et al. A newly identified group of adolescents at “invisible” risk for psychopathology and suicidal behavior: findings from the SEYLE study. World Psychiatry. 2014;13(1):78-86.
9. Demissie Z, Everett Jones S, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921.
10. National Sleep Foundation. Adolescent sleep needs and patterns. https://sleepfoundation.org/sites/default/files/sleep_and_teens_report1.pdf. Accessed February 2, 2017.
11. CDC. Youth Risk Behavior Surveillance System (YRBSS) overview. www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Accessed February 2, 2017.
12. Cooper GD, Clements PT, Holt K. A review and application of suicide prevention programs in high school settings. Issues Ment Health Nurs. 2011;32(11):696-702.
13. Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: National Academics Press; 2002.
14. US Public Health Service. The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: 1999.
Patient Satisfaction: Within Arm’s Reach, or Bending Over Backward?
In our December 2016 issue, we reported the results of our first annual survey on nonmonetary compensation (ie, the “perks”) and overall employment satisfaction (Clinician Reviews. 2016;26[12]:23-26). But the feedback I found most interesting came from the narrative responses—particularly those referencing patient satisfaction and the stress it creates for NPs and PAs.
Safety, quality, and affordability ha
Judging by the verbatim responses to our survey, NPs and PAs are concerned that quality measures don’t reflect the demands of our practice or focus on what matters to our patients.
One participant analogized, “Medicine is now like McDonalds or Burger King—patients want it their way, regardless of whether it’s in their best interest. I was fee-for-service for more than 10 years. As reimbursements have decreased significantly over time, I’m now employed by a hospital. I have become a waitress, considering my patients’ wishes—not for the benefit of their health, but to meet their more trivial ‘needs.’ These requirements can be as absurd as a specific brand of sweetener! If patients’ preferred sugar substitutes aren’t offered at my hospital, their ‘satisfaction’ may drop and I won’t get reimbursed as much. It’s a miserable experience.”
Perhaps the disparate views of what matters—Is it the softness of the pillows, or is it measurable improvement in the patient’s condition?—is the origin of the stress expressed by clinicians. This dissonance, in my opinion, exists among all involved—providers, patients, and payers. Today, patients see themselves as buyers of health services, and health care corporations have begun to function as a service industry. It may also explain why the concept of patient satisfaction has seemingly morphed into customer service, frustrating many of our colleagues.
Because it can affect clinical outcomes, patient retention, and medical malpractice claims, patient satisfaction is commonly used as a proxy for the success of doctors and hospitals.1 We know there is a correlation between higher patient satisfaction rates and improved outcomes—and conversely, research has demonstrated that unmet expectations significantly decrease satisfaction.2
However, there has been no explicit definition of patient satisfaction, nor systematic consideration of its determinants and consequences.3 As a result, measurement of “satisfaction” and its use as an indicator of quality of care remains controversial among health care providers. It can be a difficult concept to embrace.
Even setting aside the question of “amenities” and focusing on actual clinical care, satisfaction has different meanings for different people. For some, it is a positive, immediate improvement in the patient’s condition (recall my comments on pain management in my previous editorial).4 While that might be an unrealistic expectation, it is a factor in whether the patient and/or family express satisfaction with the care provided.
These high (if not unreasonable) expectations are fueled by the availability of information via the Internet. Patient attitudes and perceptions prior to receiving care also play a role. Instead of correlating with high-quality, appropriate, affordable care, a patient’s satisfaction might instead be based on the fulfillment of his or her predetermined ideas as to what treatment is needed!
The impetus for this change in perspective was the development of the patient-centered care model, which has patient satisfaction at its core.5 The model is intended to make patients partners in their health care; instead of depending solely on provider tools or standards, patients and providers discuss the options and preferences and develop a plan of care together. We all know that the relationship between patients and their providers greatly affects both treatment outcomes and patient satisfaction. But implementing a patient-centered care model means understanding and accepting from the start that patients will be asked to rate or judge their health care. It is therefore essential that there is agreement as to the standards that constitute “quality care” and congruence between these beliefs and the satisfaction ratings. You need to know what your patient expects to determine your likelihood of delivering it.
The patient-provider relationship has been a focus of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Hospital Survey, which, since 2006, has measured patients’ perceptions of their hospital experiences.6 The CAHPS Clinician and Group Survey, initiated in 2011, is a standardized tool to measure patients’ perceptions of care in an office setting.7 Data from both surveys are used to improve performance and productivity in these settings. But while the information about quality of care has enabled consumers to make more informed decisions, the data are in many ways limited and subjective.
What cannot be measured by either survey alone is the health of patients, employees, and the community. This limitation is reflected in the feedback to our survey, which suggests a preponderance of NP and PA dissatisfaction with the current methods of evaluating the health care system. How much strain is incurred when evaluative measures fail to demonstrate that high-quality, safe, affordable care is being provided? That is difficult to ascertain, but it does give one pause. We know that providers who experience professional satisfaction have higher overall patient satisfaction scores.8 If we’re frustrated, are we able to provide the highest quality care? If not, our scores will suffer. If our scores drop … around we go again.
Currently, most data collection methods focus on physicians, making NPs and PAs “invisible” providers. That certainly won’t help our satisfaction! Only when the data gleaned from these measurement tools include all ambulatory settings, and all providers are recognized as valued contributors to patient health and satisfaction, will we have the information we need to improve satisfaction levels. That will benefit not only our patients, but also ourselves.
Please share your thoughts on patient satisfaction and “customer service” by emailing [email protected].
1. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010; 3(3):151-155.
2. Jackson JL,Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609-620.
3. Linder-Pelz SU. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16(5):577-582.
4. Onieal ME. The paradox of pain management. Clinician Reviews. 2016;26(11):12,16.
5. Rickert J. Measuring patient satisfaction: a bridge between patient and physician perceptions of care. http://healthaffairs.org/blog/2014/05/09/measuring-patient-satisfaction-a-bridge-between-patient-and-physician-perceptions-of-care. Accessed December 1, 2016.
6. Centers for Medicare & Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems CAHPS® Hospital Survey. www.hcahpsonline.org/home.aspx. Accessed December 1, 2016.
7. Agency for Healthcare Research and Quality. Consumer Assessment of Healthcare Providers and Systems Clinician and Group Survey. www.ahrq.gov/cahps/surveys-guidance/cg/index.html. Accessed December 1, 2016.
8. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
In our December 2016 issue, we reported the results of our first annual survey on nonmonetary compensation (ie, the “perks”) and overall employment satisfaction (Clinician Reviews. 2016;26[12]:23-26). But the feedback I found most interesting came from the narrative responses—particularly those referencing patient satisfaction and the stress it creates for NPs and PAs.
Safety, quality, and affordability ha
Judging by the verbatim responses to our survey, NPs and PAs are concerned that quality measures don’t reflect the demands of our practice or focus on what matters to our patients.
One participant analogized, “Medicine is now like McDonalds or Burger King—patients want it their way, regardless of whether it’s in their best interest. I was fee-for-service for more than 10 years. As reimbursements have decreased significantly over time, I’m now employed by a hospital. I have become a waitress, considering my patients’ wishes—not for the benefit of their health, but to meet their more trivial ‘needs.’ These requirements can be as absurd as a specific brand of sweetener! If patients’ preferred sugar substitutes aren’t offered at my hospital, their ‘satisfaction’ may drop and I won’t get reimbursed as much. It’s a miserable experience.”
Perhaps the disparate views of what matters—Is it the softness of the pillows, or is it measurable improvement in the patient’s condition?—is the origin of the stress expressed by clinicians. This dissonance, in my opinion, exists among all involved—providers, patients, and payers. Today, patients see themselves as buyers of health services, and health care corporations have begun to function as a service industry. It may also explain why the concept of patient satisfaction has seemingly morphed into customer service, frustrating many of our colleagues.
Because it can affect clinical outcomes, patient retention, and medical malpractice claims, patient satisfaction is commonly used as a proxy for the success of doctors and hospitals.1 We know there is a correlation between higher patient satisfaction rates and improved outcomes—and conversely, research has demonstrated that unmet expectations significantly decrease satisfaction.2
However, there has been no explicit definition of patient satisfaction, nor systematic consideration of its determinants and consequences.3 As a result, measurement of “satisfaction” and its use as an indicator of quality of care remains controversial among health care providers. It can be a difficult concept to embrace.
Even setting aside the question of “amenities” and focusing on actual clinical care, satisfaction has different meanings for different people. For some, it is a positive, immediate improvement in the patient’s condition (recall my comments on pain management in my previous editorial).4 While that might be an unrealistic expectation, it is a factor in whether the patient and/or family express satisfaction with the care provided.
These high (if not unreasonable) expectations are fueled by the availability of information via the Internet. Patient attitudes and perceptions prior to receiving care also play a role. Instead of correlating with high-quality, appropriate, affordable care, a patient’s satisfaction might instead be based on the fulfillment of his or her predetermined ideas as to what treatment is needed!
The impetus for this change in perspective was the development of the patient-centered care model, which has patient satisfaction at its core.5 The model is intended to make patients partners in their health care; instead of depending solely on provider tools or standards, patients and providers discuss the options and preferences and develop a plan of care together. We all know that the relationship between patients and their providers greatly affects both treatment outcomes and patient satisfaction. But implementing a patient-centered care model means understanding and accepting from the start that patients will be asked to rate or judge their health care. It is therefore essential that there is agreement as to the standards that constitute “quality care” and congruence between these beliefs and the satisfaction ratings. You need to know what your patient expects to determine your likelihood of delivering it.
The patient-provider relationship has been a focus of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Hospital Survey, which, since 2006, has measured patients’ perceptions of their hospital experiences.6 The CAHPS Clinician and Group Survey, initiated in 2011, is a standardized tool to measure patients’ perceptions of care in an office setting.7 Data from both surveys are used to improve performance and productivity in these settings. But while the information about quality of care has enabled consumers to make more informed decisions, the data are in many ways limited and subjective.
What cannot be measured by either survey alone is the health of patients, employees, and the community. This limitation is reflected in the feedback to our survey, which suggests a preponderance of NP and PA dissatisfaction with the current methods of evaluating the health care system. How much strain is incurred when evaluative measures fail to demonstrate that high-quality, safe, affordable care is being provided? That is difficult to ascertain, but it does give one pause. We know that providers who experience professional satisfaction have higher overall patient satisfaction scores.8 If we’re frustrated, are we able to provide the highest quality care? If not, our scores will suffer. If our scores drop … around we go again.
Currently, most data collection methods focus on physicians, making NPs and PAs “invisible” providers. That certainly won’t help our satisfaction! Only when the data gleaned from these measurement tools include all ambulatory settings, and all providers are recognized as valued contributors to patient health and satisfaction, will we have the information we need to improve satisfaction levels. That will benefit not only our patients, but also ourselves.
Please share your thoughts on patient satisfaction and “customer service” by emailing [email protected].
In our December 2016 issue, we reported the results of our first annual survey on nonmonetary compensation (ie, the “perks”) and overall employment satisfaction (Clinician Reviews. 2016;26[12]:23-26). But the feedback I found most interesting came from the narrative responses—particularly those referencing patient satisfaction and the stress it creates for NPs and PAs.
Safety, quality, and affordability ha
Judging by the verbatim responses to our survey, NPs and PAs are concerned that quality measures don’t reflect the demands of our practice or focus on what matters to our patients.
One participant analogized, “Medicine is now like McDonalds or Burger King—patients want it their way, regardless of whether it’s in their best interest. I was fee-for-service for more than 10 years. As reimbursements have decreased significantly over time, I’m now employed by a hospital. I have become a waitress, considering my patients’ wishes—not for the benefit of their health, but to meet their more trivial ‘needs.’ These requirements can be as absurd as a specific brand of sweetener! If patients’ preferred sugar substitutes aren’t offered at my hospital, their ‘satisfaction’ may drop and I won’t get reimbursed as much. It’s a miserable experience.”
Perhaps the disparate views of what matters—Is it the softness of the pillows, or is it measurable improvement in the patient’s condition?—is the origin of the stress expressed by clinicians. This dissonance, in my opinion, exists among all involved—providers, patients, and payers. Today, patients see themselves as buyers of health services, and health care corporations have begun to function as a service industry. It may also explain why the concept of patient satisfaction has seemingly morphed into customer service, frustrating many of our colleagues.
Because it can affect clinical outcomes, patient retention, and medical malpractice claims, patient satisfaction is commonly used as a proxy for the success of doctors and hospitals.1 We know there is a correlation between higher patient satisfaction rates and improved outcomes—and conversely, research has demonstrated that unmet expectations significantly decrease satisfaction.2
However, there has been no explicit definition of patient satisfaction, nor systematic consideration of its determinants and consequences.3 As a result, measurement of “satisfaction” and its use as an indicator of quality of care remains controversial among health care providers. It can be a difficult concept to embrace.
Even setting aside the question of “amenities” and focusing on actual clinical care, satisfaction has different meanings for different people. For some, it is a positive, immediate improvement in the patient’s condition (recall my comments on pain management in my previous editorial).4 While that might be an unrealistic expectation, it is a factor in whether the patient and/or family express satisfaction with the care provided.
These high (if not unreasonable) expectations are fueled by the availability of information via the Internet. Patient attitudes and perceptions prior to receiving care also play a role. Instead of correlating with high-quality, appropriate, affordable care, a patient’s satisfaction might instead be based on the fulfillment of his or her predetermined ideas as to what treatment is needed!
The impetus for this change in perspective was the development of the patient-centered care model, which has patient satisfaction at its core.5 The model is intended to make patients partners in their health care; instead of depending solely on provider tools or standards, patients and providers discuss the options and preferences and develop a plan of care together. We all know that the relationship between patients and their providers greatly affects both treatment outcomes and patient satisfaction. But implementing a patient-centered care model means understanding and accepting from the start that patients will be asked to rate or judge their health care. It is therefore essential that there is agreement as to the standards that constitute “quality care” and congruence between these beliefs and the satisfaction ratings. You need to know what your patient expects to determine your likelihood of delivering it.
The patient-provider relationship has been a focus of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Hospital Survey, which, since 2006, has measured patients’ perceptions of their hospital experiences.6 The CAHPS Clinician and Group Survey, initiated in 2011, is a standardized tool to measure patients’ perceptions of care in an office setting.7 Data from both surveys are used to improve performance and productivity in these settings. But while the information about quality of care has enabled consumers to make more informed decisions, the data are in many ways limited and subjective.
What cannot be measured by either survey alone is the health of patients, employees, and the community. This limitation is reflected in the feedback to our survey, which suggests a preponderance of NP and PA dissatisfaction with the current methods of evaluating the health care system. How much strain is incurred when evaluative measures fail to demonstrate that high-quality, safe, affordable care is being provided? That is difficult to ascertain, but it does give one pause. We know that providers who experience professional satisfaction have higher overall patient satisfaction scores.8 If we’re frustrated, are we able to provide the highest quality care? If not, our scores will suffer. If our scores drop … around we go again.
Currently, most data collection methods focus on physicians, making NPs and PAs “invisible” providers. That certainly won’t help our satisfaction! Only when the data gleaned from these measurement tools include all ambulatory settings, and all providers are recognized as valued contributors to patient health and satisfaction, will we have the information we need to improve satisfaction levels. That will benefit not only our patients, but also ourselves.
Please share your thoughts on patient satisfaction and “customer service” by emailing [email protected].
1. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010; 3(3):151-155.
2. Jackson JL,Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609-620.
3. Linder-Pelz SU. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16(5):577-582.
4. Onieal ME. The paradox of pain management. Clinician Reviews. 2016;26(11):12,16.
5. Rickert J. Measuring patient satisfaction: a bridge between patient and physician perceptions of care. http://healthaffairs.org/blog/2014/05/09/measuring-patient-satisfaction-a-bridge-between-patient-and-physician-perceptions-of-care. Accessed December 1, 2016.
6. Centers for Medicare & Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems CAHPS® Hospital Survey. www.hcahpsonline.org/home.aspx. Accessed December 1, 2016.
7. Agency for Healthcare Research and Quality. Consumer Assessment of Healthcare Providers and Systems Clinician and Group Survey. www.ahrq.gov/cahps/surveys-guidance/cg/index.html. Accessed December 1, 2016.
8. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
1. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010; 3(3):151-155.
2. Jackson JL,Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609-620.
3. Linder-Pelz SU. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16(5):577-582.
4. Onieal ME. The paradox of pain management. Clinician Reviews. 2016;26(11):12,16.
5. Rickert J. Measuring patient satisfaction: a bridge between patient and physician perceptions of care. http://healthaffairs.org/blog/2014/05/09/measuring-patient-satisfaction-a-bridge-between-patient-and-physician-perceptions-of-care. Accessed December 1, 2016.
6. Centers for Medicare & Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems CAHPS® Hospital Survey. www.hcahpsonline.org/home.aspx. Accessed December 1, 2016.
7. Agency for Healthcare Research and Quality. Consumer Assessment of Healthcare Providers and Systems Clinician and Group Survey. www.ahrq.gov/cahps/surveys-guidance/cg/index.html. Accessed December 1, 2016.
8. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122-128.
The Paradox of Pain Management
Pain was introduced as the “fifth vital sign” in the 1990s, ranking it as important a measure as blood pressure, heart and respiratory rate, and temperature.1 The American Pain Society promoted this notion to increase awareness of pain treatment among health care professionals. Emphasizing its importance, the Veterans Health Administration in 1999 launched the “Pain as the 5th Vital Sign” initiative, which mandated a pain intensity rating at all clinical encounters.2
Interestingly, the Joint Commission standards never stated that pain needed to be treated as a vital sign. But many organizations started to require documentation of routine pain screening for all patients. Health care providers were instructed to inquire about pain and to treat it as an essential element of health history.
These changes were quite controversial. The additional measure, while important, competed with other priority screening needs, including diabetes, cancer, and hypertension. There was—and continues to be—quite the debate on whether pain actually can be measured and what impact that information has on the quality of care.
I do not intend to enter that debate here. Instead, I want to discuss what continues to be a conundrum for me: the paradox of pain management.
For many patients, especially those in acute or emergency care settings, the presenting complaint is pain. I would submit that for many the expectation is for pain to be immediately and permanently relieved. But is this a realistic goal?
I recall a lecture on pain management I attended years ago; at that time, the approach involved early identification and prompt, aggressive treatment. When asked “How much medication and for how long?” the lecturer used diabetes as a treatment model, stating, “You would increase insulin until the blood glucose was controlled—don’t be afraid to increase pain medication until the pain is controlled.” In the early days of pain management, that was the accepted norm. The possibility that a “zero” on the pain scale was unattainable for some patients was not considered.
Yet seemingly overnight, once pain was decreed a vital sign, health care providers were mandated to measure it and faced with the responsibility to treat it. This resulted in a vague 0-1
Faced with growing concern for undertreated pain in the US, however, many of us strove to achieve a balance of sufficient yet appropriate treatment. We struggled to determine how to relieve the pain our patients experienced without creating other problems, such as undesirable side effects, misuse, or addiction. That predicament, paired with the ever-increasing direct-to-consumer advertisements about pain relief and the insistence by (some, not all) patients that nonnarcotic pain medication is ineffective, bred the crisis of opioid overuse and addiction we now face.
But just as I chose not to debate the impact of pain measurement on quality of care, I also choose not to debate the existence of the opioid crisis. What I want to emphasize is that all policy changes have consequences. I reach out to you, my colleagues, for innovative ideas to strike the delicate balance of appropriate use of narcotics. How do we address the needs of patients whose pain is more than just an inconvenience and for whom daily use of a narcotic allows them to function—while also avoiding the pitfalls that we are now regularly warned about?
I have no doubt that each of us knows at least one person—a patient, a family member, a neighbor—for whom pain is a daily occurrence. But we must put that in perspective; not all pain is a barrier to physical and emotional functioning. Data suggest that a “33% to 50% decrease in pain intensity is meaningful from a patient’s perspective and represents a reasonable standard of intervention efficacy.”3 For those who deal with chronic pain, even a slight improvement is progress.
So, while the American Medical Association and the American Pain Society bicker about whether pain is the “fifth vital sign,” we must find a better means to resolve the discord in our society.4 Banning all opioid use is not the answer, but neither is considering narcotics the default treatment for pain.
We must remind our patients, our policymakers, and ourselves that identifying and assessing pain is not equated with writing an opioid or narcotic prescription. Nor will removing those medications from our formulary mitigate the crisis. We need to communicate a clear, consistent message that pain is real, that some pain is a fact of life, and that we will help our patients.
However, it is incumbent upon us to adopt a systematic yet personalized plan of care that is effective, cost conscious, culturally and developmentally appropriate, and safe—and that plan may or may not include prescribing narcotics. We have much work ahead of us in order to minimize the potential for misuse of these medications without impeding patients’ access to necessary health care.
Please share your thoughts on this conundrum by writing to [email protected].
1. Veterans Health Administration. Pain as the 5th vital sign toolkit. www.va.gov/PAINMAN AGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Accessed October 5, 2016.
2. Mularski RA, White-Chu F, Overbay D, et al. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med . 2006;21(6):607-612.
3. Gordon DB, Dahl JL, Miaskowski C, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management. Arch Intern Med . 2005; 165(14):1574-1580.
4. Anson P. AMA drops pain as a vital sign . Pain News Network. June 16, 2016. www.painnewsnetwork.org/stories/2016/6/16/ama-drops-pain-as-vital-sign. Accessed October 5, 2016.
Pain was introduced as the “fifth vital sign” in the 1990s, ranking it as important a measure as blood pressure, heart and respiratory rate, and temperature.1 The American Pain Society promoted this notion to increase awareness of pain treatment among health care professionals. Emphasizing its importance, the Veterans Health Administration in 1999 launched the “Pain as the 5th Vital Sign” initiative, which mandated a pain intensity rating at all clinical encounters.2
Interestingly, the Joint Commission standards never stated that pain needed to be treated as a vital sign. But many organizations started to require documentation of routine pain screening for all patients. Health care providers were instructed to inquire about pain and to treat it as an essential element of health history.
These changes were quite controversial. The additional measure, while important, competed with other priority screening needs, including diabetes, cancer, and hypertension. There was—and continues to be—quite the debate on whether pain actually can be measured and what impact that information has on the quality of care.
I do not intend to enter that debate here. Instead, I want to discuss what continues to be a conundrum for me: the paradox of pain management.
For many patients, especially those in acute or emergency care settings, the presenting complaint is pain. I would submit that for many the expectation is for pain to be immediately and permanently relieved. But is this a realistic goal?
I recall a lecture on pain management I attended years ago; at that time, the approach involved early identification and prompt, aggressive treatment. When asked “How much medication and for how long?” the lecturer used diabetes as a treatment model, stating, “You would increase insulin until the blood glucose was controlled—don’t be afraid to increase pain medication until the pain is controlled.” In the early days of pain management, that was the accepted norm. The possibility that a “zero” on the pain scale was unattainable for some patients was not considered.
Yet seemingly overnight, once pain was decreed a vital sign, health care providers were mandated to measure it and faced with the responsibility to treat it. This resulted in a vague 0-1
Faced with growing concern for undertreated pain in the US, however, many of us strove to achieve a balance of sufficient yet appropriate treatment. We struggled to determine how to relieve the pain our patients experienced without creating other problems, such as undesirable side effects, misuse, or addiction. That predicament, paired with the ever-increasing direct-to-consumer advertisements about pain relief and the insistence by (some, not all) patients that nonnarcotic pain medication is ineffective, bred the crisis of opioid overuse and addiction we now face.
But just as I chose not to debate the impact of pain measurement on quality of care, I also choose not to debate the existence of the opioid crisis. What I want to emphasize is that all policy changes have consequences. I reach out to you, my colleagues, for innovative ideas to strike the delicate balance of appropriate use of narcotics. How do we address the needs of patients whose pain is more than just an inconvenience and for whom daily use of a narcotic allows them to function—while also avoiding the pitfalls that we are now regularly warned about?
I have no doubt that each of us knows at least one person—a patient, a family member, a neighbor—for whom pain is a daily occurrence. But we must put that in perspective; not all pain is a barrier to physical and emotional functioning. Data suggest that a “33% to 50% decrease in pain intensity is meaningful from a patient’s perspective and represents a reasonable standard of intervention efficacy.”3 For those who deal with chronic pain, even a slight improvement is progress.
So, while the American Medical Association and the American Pain Society bicker about whether pain is the “fifth vital sign,” we must find a better means to resolve the discord in our society.4 Banning all opioid use is not the answer, but neither is considering narcotics the default treatment for pain.
We must remind our patients, our policymakers, and ourselves that identifying and assessing pain is not equated with writing an opioid or narcotic prescription. Nor will removing those medications from our formulary mitigate the crisis. We need to communicate a clear, consistent message that pain is real, that some pain is a fact of life, and that we will help our patients.
However, it is incumbent upon us to adopt a systematic yet personalized plan of care that is effective, cost conscious, culturally and developmentally appropriate, and safe—and that plan may or may not include prescribing narcotics. We have much work ahead of us in order to minimize the potential for misuse of these medications without impeding patients’ access to necessary health care.
Please share your thoughts on this conundrum by writing to [email protected].
Pain was introduced as the “fifth vital sign” in the 1990s, ranking it as important a measure as blood pressure, heart and respiratory rate, and temperature.1 The American Pain Society promoted this notion to increase awareness of pain treatment among health care professionals. Emphasizing its importance, the Veterans Health Administration in 1999 launched the “Pain as the 5th Vital Sign” initiative, which mandated a pain intensity rating at all clinical encounters.2
Interestingly, the Joint Commission standards never stated that pain needed to be treated as a vital sign. But many organizations started to require documentation of routine pain screening for all patients. Health care providers were instructed to inquire about pain and to treat it as an essential element of health history.
These changes were quite controversial. The additional measure, while important, competed with other priority screening needs, including diabetes, cancer, and hypertension. There was—and continues to be—quite the debate on whether pain actually can be measured and what impact that information has on the quality of care.
I do not intend to enter that debate here. Instead, I want to discuss what continues to be a conundrum for me: the paradox of pain management.
For many patients, especially those in acute or emergency care settings, the presenting complaint is pain. I would submit that for many the expectation is for pain to be immediately and permanently relieved. But is this a realistic goal?
I recall a lecture on pain management I attended years ago; at that time, the approach involved early identification and prompt, aggressive treatment. When asked “How much medication and for how long?” the lecturer used diabetes as a treatment model, stating, “You would increase insulin until the blood glucose was controlled—don’t be afraid to increase pain medication until the pain is controlled.” In the early days of pain management, that was the accepted norm. The possibility that a “zero” on the pain scale was unattainable for some patients was not considered.
Yet seemingly overnight, once pain was decreed a vital sign, health care providers were mandated to measure it and faced with the responsibility to treat it. This resulted in a vague 0-1
Faced with growing concern for undertreated pain in the US, however, many of us strove to achieve a balance of sufficient yet appropriate treatment. We struggled to determine how to relieve the pain our patients experienced without creating other problems, such as undesirable side effects, misuse, or addiction. That predicament, paired with the ever-increasing direct-to-consumer advertisements about pain relief and the insistence by (some, not all) patients that nonnarcotic pain medication is ineffective, bred the crisis of opioid overuse and addiction we now face.
But just as I chose not to debate the impact of pain measurement on quality of care, I also choose not to debate the existence of the opioid crisis. What I want to emphasize is that all policy changes have consequences. I reach out to you, my colleagues, for innovative ideas to strike the delicate balance of appropriate use of narcotics. How do we address the needs of patients whose pain is more than just an inconvenience and for whom daily use of a narcotic allows them to function—while also avoiding the pitfalls that we are now regularly warned about?
I have no doubt that each of us knows at least one person—a patient, a family member, a neighbor—for whom pain is a daily occurrence. But we must put that in perspective; not all pain is a barrier to physical and emotional functioning. Data suggest that a “33% to 50% decrease in pain intensity is meaningful from a patient’s perspective and represents a reasonable standard of intervention efficacy.”3 For those who deal with chronic pain, even a slight improvement is progress.
So, while the American Medical Association and the American Pain Society bicker about whether pain is the “fifth vital sign,” we must find a better means to resolve the discord in our society.4 Banning all opioid use is not the answer, but neither is considering narcotics the default treatment for pain.
We must remind our patients, our policymakers, and ourselves that identifying and assessing pain is not equated with writing an opioid or narcotic prescription. Nor will removing those medications from our formulary mitigate the crisis. We need to communicate a clear, consistent message that pain is real, that some pain is a fact of life, and that we will help our patients.
However, it is incumbent upon us to adopt a systematic yet personalized plan of care that is effective, cost conscious, culturally and developmentally appropriate, and safe—and that plan may or may not include prescribing narcotics. We have much work ahead of us in order to minimize the potential for misuse of these medications without impeding patients’ access to necessary health care.
Please share your thoughts on this conundrum by writing to [email protected].
1. Veterans Health Administration. Pain as the 5th vital sign toolkit. www.va.gov/PAINMAN AGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Accessed October 5, 2016.
2. Mularski RA, White-Chu F, Overbay D, et al. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med . 2006;21(6):607-612.
3. Gordon DB, Dahl JL, Miaskowski C, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management. Arch Intern Med . 2005; 165(14):1574-1580.
4. Anson P. AMA drops pain as a vital sign . Pain News Network. June 16, 2016. www.painnewsnetwork.org/stories/2016/6/16/ama-drops-pain-as-vital-sign. Accessed October 5, 2016.
1. Veterans Health Administration. Pain as the 5th vital sign toolkit. www.va.gov/PAINMAN AGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Accessed October 5, 2016.
2. Mularski RA, White-Chu F, Overbay D, et al. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med . 2006;21(6):607-612.
3. Gordon DB, Dahl JL, Miaskowski C, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management. Arch Intern Med . 2005; 165(14):1574-1580.
4. Anson P. AMA drops pain as a vital sign . Pain News Network. June 16, 2016. www.painnewsnetwork.org/stories/2016/6/16/ama-drops-pain-as-vital-sign. Accessed October 5, 2016.
