User login
Translucent particles found in Hemlibra
But toxicology and safety assessments conducted by the company found that the benefit-risk profile of the product remains unchanged.
Hemlibra is a bispecific factor IXa– and factor X–directed antibody that has been approved in the United States and other countries for routine prophylaxis in adult and pediatric patients with hemophilia A, with or without factor VIII inhibitors. It is administered as a subcutaneous injection.
The particles were first identified in March 2019 during a routine examination of drug product batches by Genentech. At the time, the company informed the U.S. Food and Drug Administration; the European Medicines Agency; Swissmedic; Health Canada; and the Ministry for Health, Labour, and Welfare in Japan. An initial company assessment found that the particles consisted of protein (Hemlibra drug substance) and silicone oil (polydimethylsiloxane), an organic polymer included in all parenteral medicines, according to Genentech.
Since the health authorities all agreed with the company’s initial conclusion that the product’s safety remained unchanged, no further action was taken.
The presence of the particles became more widely known in early October 2019, when Genentech notified the National Hemophilia Foundation, the NHF’s Medical and Scientific Advisory Council (MASAC), and the Hemophilia Federation of America. Genentech officials reached out to these groups after finishing a root cause investigation and issuing a final report to health authorities concluding that there was no change in the benefit-risk profile, according to a company spokesman.
MASAC issued its own statement recommending no change in prescribing or interruption in the use of Hemlibra. This is an “interim recommendation pending our assessment of the full review by Roche/Genentech of their manufacturing and quality control,” MASAC said. The council noted that it had been informed by representatives from Roche/Genentech that there have been no reports of adverse events linked to the particulate matter. Additionally, the problem had been present since the initial clinical trials of the product, but was only recently identified.
But at least one patient advocate is raising concerns about the timing of this notification. Jesse Clark, president and CEO of HemoAware, wants to know why patients were not informed of the particle issue for more than 6 months.
“The bleeding disorder community was never notified by either Genentech or any other agency,” Mr. Clark said in an interview. “The lack of transparency and communication is extremely concerning.”
A spokesman for Genentech said the company had not alerted patients earlier because there was no indication of an impact on the safety of the product. “We take inquiries from the community very seriously and are providing context and additional details in response to requests from patient organizations,” he said in an interview.
The company does not expect this issue to impact any patients in the United States and the availability of Hemlibra will not be affected, he added.
But toxicology and safety assessments conducted by the company found that the benefit-risk profile of the product remains unchanged.
Hemlibra is a bispecific factor IXa– and factor X–directed antibody that has been approved in the United States and other countries for routine prophylaxis in adult and pediatric patients with hemophilia A, with or without factor VIII inhibitors. It is administered as a subcutaneous injection.
The particles were first identified in March 2019 during a routine examination of drug product batches by Genentech. At the time, the company informed the U.S. Food and Drug Administration; the European Medicines Agency; Swissmedic; Health Canada; and the Ministry for Health, Labour, and Welfare in Japan. An initial company assessment found that the particles consisted of protein (Hemlibra drug substance) and silicone oil (polydimethylsiloxane), an organic polymer included in all parenteral medicines, according to Genentech.
Since the health authorities all agreed with the company’s initial conclusion that the product’s safety remained unchanged, no further action was taken.
The presence of the particles became more widely known in early October 2019, when Genentech notified the National Hemophilia Foundation, the NHF’s Medical and Scientific Advisory Council (MASAC), and the Hemophilia Federation of America. Genentech officials reached out to these groups after finishing a root cause investigation and issuing a final report to health authorities concluding that there was no change in the benefit-risk profile, according to a company spokesman.
MASAC issued its own statement recommending no change in prescribing or interruption in the use of Hemlibra. This is an “interim recommendation pending our assessment of the full review by Roche/Genentech of their manufacturing and quality control,” MASAC said. The council noted that it had been informed by representatives from Roche/Genentech that there have been no reports of adverse events linked to the particulate matter. Additionally, the problem had been present since the initial clinical trials of the product, but was only recently identified.
But at least one patient advocate is raising concerns about the timing of this notification. Jesse Clark, president and CEO of HemoAware, wants to know why patients were not informed of the particle issue for more than 6 months.
“The bleeding disorder community was never notified by either Genentech or any other agency,” Mr. Clark said in an interview. “The lack of transparency and communication is extremely concerning.”
A spokesman for Genentech said the company had not alerted patients earlier because there was no indication of an impact on the safety of the product. “We take inquiries from the community very seriously and are providing context and additional details in response to requests from patient organizations,” he said in an interview.
The company does not expect this issue to impact any patients in the United States and the availability of Hemlibra will not be affected, he added.
But toxicology and safety assessments conducted by the company found that the benefit-risk profile of the product remains unchanged.
Hemlibra is a bispecific factor IXa– and factor X–directed antibody that has been approved in the United States and other countries for routine prophylaxis in adult and pediatric patients with hemophilia A, with or without factor VIII inhibitors. It is administered as a subcutaneous injection.
The particles were first identified in March 2019 during a routine examination of drug product batches by Genentech. At the time, the company informed the U.S. Food and Drug Administration; the European Medicines Agency; Swissmedic; Health Canada; and the Ministry for Health, Labour, and Welfare in Japan. An initial company assessment found that the particles consisted of protein (Hemlibra drug substance) and silicone oil (polydimethylsiloxane), an organic polymer included in all parenteral medicines, according to Genentech.
Since the health authorities all agreed with the company’s initial conclusion that the product’s safety remained unchanged, no further action was taken.
The presence of the particles became more widely known in early October 2019, when Genentech notified the National Hemophilia Foundation, the NHF’s Medical and Scientific Advisory Council (MASAC), and the Hemophilia Federation of America. Genentech officials reached out to these groups after finishing a root cause investigation and issuing a final report to health authorities concluding that there was no change in the benefit-risk profile, according to a company spokesman.
MASAC issued its own statement recommending no change in prescribing or interruption in the use of Hemlibra. This is an “interim recommendation pending our assessment of the full review by Roche/Genentech of their manufacturing and quality control,” MASAC said. The council noted that it had been informed by representatives from Roche/Genentech that there have been no reports of adverse events linked to the particulate matter. Additionally, the problem had been present since the initial clinical trials of the product, but was only recently identified.
But at least one patient advocate is raising concerns about the timing of this notification. Jesse Clark, president and CEO of HemoAware, wants to know why patients were not informed of the particle issue for more than 6 months.
“The bleeding disorder community was never notified by either Genentech or any other agency,” Mr. Clark said in an interview. “The lack of transparency and communication is extremely concerning.”
A spokesman for Genentech said the company had not alerted patients earlier because there was no indication of an impact on the safety of the product. “We take inquiries from the community very seriously and are providing context and additional details in response to requests from patient organizations,” he said in an interview.
The company does not expect this issue to impact any patients in the United States and the availability of Hemlibra will not be affected, he added.
Progressive myeloma after induction? Go straight to transplant
Patients with multiple myeloma who don’t respond to induction therapy may be better off advancing straight to autologous stem cell therapy, rather than undergoing salvage therapy before transplant, according to findings of an analysis that included both real-world and clinical trial patients.
Joanna Blocka, MD, of the University Hospital of Heidelberg (Germany) and colleagues found similar progression-free and overall survival rates for patients who had progressive disease and underwent autologous stem cell therapy (ASCT), compared with patients who underwent salvage therapy and improved to at least stable disease before proceeding to transplant. The findings were published in Leukemia & Lymphoma.
The real-world analysis included 1,599 patients with multiple myeloma who had undergone ASCT between 1991 and 2016. More than half of the patients (58%) were not enrolled in clinical trials. The remainder were split between the German-Speaking Myeloma Multicenter Group (GMMG)-HD3 and GMMG-HD4 trials, which compared various induction regimens.
Just 23 patients in the analysis received salvage therapy because of progressive disease and deepened their response before ASCT. Of these patients, 12 received novel agents in induction therapy and 11 received older medications.
Looking across all 1,599 patients, 5.3% achieved complete remission before first ASCT. Most patients (71.8%) achieved partial remission, 9.7% had a minimal response, and 5.7% had stable disease. A group of 120 patients (7.5%) progressed between the last course of induction and ASCT.
The researchers compared the progression-free and overall survival rates of patients with progressive disease versus those who had stable disease or better before their first transplant. Both univariable and multivariable analysis showed no statistically significant differences in either survival outcome between the two groups.
In the multivariable analysis, there was a hazard ratio of 1.23 (95% confidence interval, 0.98-1.56) for progression-free survival for patients with progressive disease versus those who responded to induction therapy. Similarly, the HR for overall survival between the two groups was 1.24 (95% CI, 0.93-1.65).
The researchers also analyzed the groups based on whether they received novel or older agents during induction.
Patients with progressive disease who received novel agents had significantly worse progression-free survival (22.2 months), compared with patients who responded to treatment with novel agents (22.2 months vs. 29.1 months; P = .03). The same trend was seen with overall survival in these groups (54.4 months vs. 97.5 months; P less than .001).
Rates of survival were similar for patients with progressive disease and responders who had received older medications at induction.
“This might be explained by a prognostically disadvantageous disease biology in patients nonresponsive to novel agents,” the researchers wrote.
The researchers also compared survival outcomes for the 120 patients who underwent ASCT with progressive disease versus the 23 patients who received salvage therapy and improved their response to at least stable disease before transplant. Univariable analysis showed that salvage patients actually did worse than those with progressive disease who proceeded straight to transplant – 12.1 months versus 22.9 months of progression-free survival (P = .04) and 33.1 versus 69.5 months of overall survival (P = .08). But on multivariable analysis, there was no significant difference between the two groups for progression-free survival (HR, 0.71; 95% CI, 0.28-1.80; P = .5) or overall survival (HR, 0.77; 95% CI, 0.30-1.95; P = .6). The use of novel agents did not appear to affect the survival outcomes in these patients.
The worse outcomes seen among salvage patients observed in univariable analysis “might be due to a cumulative toxic effect of salvage therapy,” the researchers suggested. “An alternative explanation could be that the patients who were offered salvage therapy might have had more aggressive disease than those who did not undergo salvage therapy.”
Dr. Blocka reported having no relevant financial disclosures. Other coauthors reported relationships with Janssen, Amgen, Bristol-Myers Squibb, Celgene, and others.
SOURCE: Blocka J et al. Leuk Lymphoma. 2019 Aug 19. doi: 10.1080/10428194.2019.1646905.
Patients with multiple myeloma who don’t respond to induction therapy may be better off advancing straight to autologous stem cell therapy, rather than undergoing salvage therapy before transplant, according to findings of an analysis that included both real-world and clinical trial patients.
Joanna Blocka, MD, of the University Hospital of Heidelberg (Germany) and colleagues found similar progression-free and overall survival rates for patients who had progressive disease and underwent autologous stem cell therapy (ASCT), compared with patients who underwent salvage therapy and improved to at least stable disease before proceeding to transplant. The findings were published in Leukemia & Lymphoma.
The real-world analysis included 1,599 patients with multiple myeloma who had undergone ASCT between 1991 and 2016. More than half of the patients (58%) were not enrolled in clinical trials. The remainder were split between the German-Speaking Myeloma Multicenter Group (GMMG)-HD3 and GMMG-HD4 trials, which compared various induction regimens.
Just 23 patients in the analysis received salvage therapy because of progressive disease and deepened their response before ASCT. Of these patients, 12 received novel agents in induction therapy and 11 received older medications.
Looking across all 1,599 patients, 5.3% achieved complete remission before first ASCT. Most patients (71.8%) achieved partial remission, 9.7% had a minimal response, and 5.7% had stable disease. A group of 120 patients (7.5%) progressed between the last course of induction and ASCT.
The researchers compared the progression-free and overall survival rates of patients with progressive disease versus those who had stable disease or better before their first transplant. Both univariable and multivariable analysis showed no statistically significant differences in either survival outcome between the two groups.
In the multivariable analysis, there was a hazard ratio of 1.23 (95% confidence interval, 0.98-1.56) for progression-free survival for patients with progressive disease versus those who responded to induction therapy. Similarly, the HR for overall survival between the two groups was 1.24 (95% CI, 0.93-1.65).
The researchers also analyzed the groups based on whether they received novel or older agents during induction.
Patients with progressive disease who received novel agents had significantly worse progression-free survival (22.2 months), compared with patients who responded to treatment with novel agents (22.2 months vs. 29.1 months; P = .03). The same trend was seen with overall survival in these groups (54.4 months vs. 97.5 months; P less than .001).
Rates of survival were similar for patients with progressive disease and responders who had received older medications at induction.
“This might be explained by a prognostically disadvantageous disease biology in patients nonresponsive to novel agents,” the researchers wrote.
The researchers also compared survival outcomes for the 120 patients who underwent ASCT with progressive disease versus the 23 patients who received salvage therapy and improved their response to at least stable disease before transplant. Univariable analysis showed that salvage patients actually did worse than those with progressive disease who proceeded straight to transplant – 12.1 months versus 22.9 months of progression-free survival (P = .04) and 33.1 versus 69.5 months of overall survival (P = .08). But on multivariable analysis, there was no significant difference between the two groups for progression-free survival (HR, 0.71; 95% CI, 0.28-1.80; P = .5) or overall survival (HR, 0.77; 95% CI, 0.30-1.95; P = .6). The use of novel agents did not appear to affect the survival outcomes in these patients.
The worse outcomes seen among salvage patients observed in univariable analysis “might be due to a cumulative toxic effect of salvage therapy,” the researchers suggested. “An alternative explanation could be that the patients who were offered salvage therapy might have had more aggressive disease than those who did not undergo salvage therapy.”
Dr. Blocka reported having no relevant financial disclosures. Other coauthors reported relationships with Janssen, Amgen, Bristol-Myers Squibb, Celgene, and others.
SOURCE: Blocka J et al. Leuk Lymphoma. 2019 Aug 19. doi: 10.1080/10428194.2019.1646905.
Patients with multiple myeloma who don’t respond to induction therapy may be better off advancing straight to autologous stem cell therapy, rather than undergoing salvage therapy before transplant, according to findings of an analysis that included both real-world and clinical trial patients.
Joanna Blocka, MD, of the University Hospital of Heidelberg (Germany) and colleagues found similar progression-free and overall survival rates for patients who had progressive disease and underwent autologous stem cell therapy (ASCT), compared with patients who underwent salvage therapy and improved to at least stable disease before proceeding to transplant. The findings were published in Leukemia & Lymphoma.
The real-world analysis included 1,599 patients with multiple myeloma who had undergone ASCT between 1991 and 2016. More than half of the patients (58%) were not enrolled in clinical trials. The remainder were split between the German-Speaking Myeloma Multicenter Group (GMMG)-HD3 and GMMG-HD4 trials, which compared various induction regimens.
Just 23 patients in the analysis received salvage therapy because of progressive disease and deepened their response before ASCT. Of these patients, 12 received novel agents in induction therapy and 11 received older medications.
Looking across all 1,599 patients, 5.3% achieved complete remission before first ASCT. Most patients (71.8%) achieved partial remission, 9.7% had a minimal response, and 5.7% had stable disease. A group of 120 patients (7.5%) progressed between the last course of induction and ASCT.
The researchers compared the progression-free and overall survival rates of patients with progressive disease versus those who had stable disease or better before their first transplant. Both univariable and multivariable analysis showed no statistically significant differences in either survival outcome between the two groups.
In the multivariable analysis, there was a hazard ratio of 1.23 (95% confidence interval, 0.98-1.56) for progression-free survival for patients with progressive disease versus those who responded to induction therapy. Similarly, the HR for overall survival between the two groups was 1.24 (95% CI, 0.93-1.65).
The researchers also analyzed the groups based on whether they received novel or older agents during induction.
Patients with progressive disease who received novel agents had significantly worse progression-free survival (22.2 months), compared with patients who responded to treatment with novel agents (22.2 months vs. 29.1 months; P = .03). The same trend was seen with overall survival in these groups (54.4 months vs. 97.5 months; P less than .001).
Rates of survival were similar for patients with progressive disease and responders who had received older medications at induction.
“This might be explained by a prognostically disadvantageous disease biology in patients nonresponsive to novel agents,” the researchers wrote.
The researchers also compared survival outcomes for the 120 patients who underwent ASCT with progressive disease versus the 23 patients who received salvage therapy and improved their response to at least stable disease before transplant. Univariable analysis showed that salvage patients actually did worse than those with progressive disease who proceeded straight to transplant – 12.1 months versus 22.9 months of progression-free survival (P = .04) and 33.1 versus 69.5 months of overall survival (P = .08). But on multivariable analysis, there was no significant difference between the two groups for progression-free survival (HR, 0.71; 95% CI, 0.28-1.80; P = .5) or overall survival (HR, 0.77; 95% CI, 0.30-1.95; P = .6). The use of novel agents did not appear to affect the survival outcomes in these patients.
The worse outcomes seen among salvage patients observed in univariable analysis “might be due to a cumulative toxic effect of salvage therapy,” the researchers suggested. “An alternative explanation could be that the patients who were offered salvage therapy might have had more aggressive disease than those who did not undergo salvage therapy.”
Dr. Blocka reported having no relevant financial disclosures. Other coauthors reported relationships with Janssen, Amgen, Bristol-Myers Squibb, Celgene, and others.
SOURCE: Blocka J et al. Leuk Lymphoma. 2019 Aug 19. doi: 10.1080/10428194.2019.1646905.
FROM LEUKEMIA & LYMPHOMA
Key clinical point:
Major finding: There was no difference between patients with progressive disease who went straight to ASCT and patients who received salvage therapy, both in terms of progression-free survival (hazard ratio, 0.71; 95% confidence interval, 0.28-1.80; P = .5) and overall survival (HR, 0.77; 95% CI, 0.30-1.95; P = .6).
Study details: An analysis of 1,599 patients with multiple myeloma who underwent ASCT. A subanalysis compared 120 patients with progressive disease before ASCT with 23 patients who received salvage treatment before ASCT.
Disclosures: Dr. Blocka reported having no relevant financial disclosures. Other coauthors reported relationships with Janssen, Amgen, Bristol-Myers Squibb, Celgene, and others.
Source: Blocka J et al. Leuk Lymphoma. 2019 Aug 19. doi: 10.1080/10428194.2019.1646905.
Calquence earns breakthrough designation for CLL monotherapy
The Bruton tyrosine kinase inhibitor is already approved for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy, and multiple trials are underway to evaluate the drug’s use in a variety of B-cell malignancies, according to the drug’s sponsor, AstraZeneca.
The current designation was based on preliminary results from two phase 3 trials – ELEVATE-TN and ASCEND. In the three-arm ELEVATE-TN trial, researchers evaluated acalabrutinib alone or in combination with obinutuzumab versus chlorambucil plus obinutuzumab in previously untreated patients with CLL. In the two-arm ASCEND trial, previously treated patients with CLL were randomized to receive acalabrutinib monotherapy or the physician’s choice of either rituximab plus idelalisib or rituximab plus bendamustine.
Interim analyses of the two trials showed that acalabrutinib alone, or in combination, significantly improved progression-free survival without raising safety concerns.
Breakthrough therapy designation allows for an expedited review by the FDA for treatments aimed at treating serious conditions where there is preliminary clinical evidence showing a substantial improvement over an available therapy or a clinically significant endpoint.
The Bruton tyrosine kinase inhibitor is already approved for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy, and multiple trials are underway to evaluate the drug’s use in a variety of B-cell malignancies, according to the drug’s sponsor, AstraZeneca.
The current designation was based on preliminary results from two phase 3 trials – ELEVATE-TN and ASCEND. In the three-arm ELEVATE-TN trial, researchers evaluated acalabrutinib alone or in combination with obinutuzumab versus chlorambucil plus obinutuzumab in previously untreated patients with CLL. In the two-arm ASCEND trial, previously treated patients with CLL were randomized to receive acalabrutinib monotherapy or the physician’s choice of either rituximab plus idelalisib or rituximab plus bendamustine.
Interim analyses of the two trials showed that acalabrutinib alone, or in combination, significantly improved progression-free survival without raising safety concerns.
Breakthrough therapy designation allows for an expedited review by the FDA for treatments aimed at treating serious conditions where there is preliminary clinical evidence showing a substantial improvement over an available therapy or a clinically significant endpoint.
The Bruton tyrosine kinase inhibitor is already approved for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy, and multiple trials are underway to evaluate the drug’s use in a variety of B-cell malignancies, according to the drug’s sponsor, AstraZeneca.
The current designation was based on preliminary results from two phase 3 trials – ELEVATE-TN and ASCEND. In the three-arm ELEVATE-TN trial, researchers evaluated acalabrutinib alone or in combination with obinutuzumab versus chlorambucil plus obinutuzumab in previously untreated patients with CLL. In the two-arm ASCEND trial, previously treated patients with CLL were randomized to receive acalabrutinib monotherapy or the physician’s choice of either rituximab plus idelalisib or rituximab plus bendamustine.
Interim analyses of the two trials showed that acalabrutinib alone, or in combination, significantly improved progression-free survival without raising safety concerns.
Breakthrough therapy designation allows for an expedited review by the FDA for treatments aimed at treating serious conditions where there is preliminary clinical evidence showing a substantial improvement over an available therapy or a clinically significant endpoint.
Low-dose radiation therapy looks effective in hard-to-treat MCL
Low-dose radiation therapy – with or without concurrent chemotherapy – appears promising as a treatment for patients with relapsed or refractory mantle cell lymphoma (MCL) or at least a bridge to subsequent therapy, according to findings published in Blood Advances.
Matthew S. Ning, MD, of the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and colleagues, said this is the first study to evaluate low-dose radiation therapy (LDRT) with chemotherapy as a treatment modality outside of palliative care for relapsed, multiple refractory MCL patients.
“Our findings indicate that LDRT imparts excellent [local control], minimal toxicity, and favorable outcomes in this setting,” the researchers said.
The study included 19 patients with a total of 98 sites of relapsed, refractory MCL who were treated from 2014 to 2018. The median follow-up was 51.3 months from initial diagnosis and 15.4 months from initial treatment with low-dose radiation therapy, given at a dose of 4 Gy.
These were hard-to-treat patients who had received multiple prior therapies since diagnosis, including carfilzomib, ibrutinib, bortezomib, anthracycline, and rituximab. In total, 8 of the patients had previously undergone autologous stem cell transplant and 11 were refractory to ibrutinib by the time of initial radiation therapy.
Median age of the patients was 69 years; 15 patients had classical histology and 4 had blastoid variant. Among the 98 tumor sites treated, the median tumor size was 2.8 cm.
In all, 14 patients received initial LDRT that was concurrent with chemotherapy. The remaining 5 patients had stopped chemotherapy prior to starting LDRT.
LDRT was given in 1-2 daily fractions via 3-dimensional conformal radiation therapy or electron beam.
Of the 98 tumor sites treated, complete response was achieved for 79 sites (81%) and the median time to complete response was 2.7 months after the start of LDRT. The researchers removed one patient who was an outlier with 27 tumor sites treated, and that dropped the complete response rate down to 76%. The overall response rate, which include an additional five sites with partial response, was 86%.
The researchers found links between complete response and soft tissue site versus non–soft tissue site (hazard ratio, 1.80; 1.12-2.90, P = .02). However, there were no associations between response and chemo-refractory status, ibrutinib-refractory status, prior chemotherapy courts, receipt of concurrent chemotherapy, tumor size, number of fractions, lesions treated per course, or blastoid variant.
The overall survival at 1 year after LDRT initiation was 90% and the 1-year progression-free survival was 55%. All five patients who died were refractory to ibrutinib.
The researchers reported finding no radiation therapy–related toxicities, even when patients received concurrent chemotherapy.
The use of LDRT has the potential to bridge refractory patients to subsequent therapies or to provide treatment breaks as patients recover from toxicities, the researchers said. However, they called for additional studies to confirm that this approach improves progression-free survival over chemotherapy alone.
The study was supported in part by a grant from the National Cancer Institute. The researchers reported having no competing financial interests.
SOURCE: Ning MS et al. Blood Adv. 2019. Jul 9;3(13):2035-9.
Low-dose radiation therapy – with or without concurrent chemotherapy – appears promising as a treatment for patients with relapsed or refractory mantle cell lymphoma (MCL) or at least a bridge to subsequent therapy, according to findings published in Blood Advances.
Matthew S. Ning, MD, of the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and colleagues, said this is the first study to evaluate low-dose radiation therapy (LDRT) with chemotherapy as a treatment modality outside of palliative care for relapsed, multiple refractory MCL patients.
“Our findings indicate that LDRT imparts excellent [local control], minimal toxicity, and favorable outcomes in this setting,” the researchers said.
The study included 19 patients with a total of 98 sites of relapsed, refractory MCL who were treated from 2014 to 2018. The median follow-up was 51.3 months from initial diagnosis and 15.4 months from initial treatment with low-dose radiation therapy, given at a dose of 4 Gy.
These were hard-to-treat patients who had received multiple prior therapies since diagnosis, including carfilzomib, ibrutinib, bortezomib, anthracycline, and rituximab. In total, 8 of the patients had previously undergone autologous stem cell transplant and 11 were refractory to ibrutinib by the time of initial radiation therapy.
Median age of the patients was 69 years; 15 patients had classical histology and 4 had blastoid variant. Among the 98 tumor sites treated, the median tumor size was 2.8 cm.
In all, 14 patients received initial LDRT that was concurrent with chemotherapy. The remaining 5 patients had stopped chemotherapy prior to starting LDRT.
LDRT was given in 1-2 daily fractions via 3-dimensional conformal radiation therapy or electron beam.
Of the 98 tumor sites treated, complete response was achieved for 79 sites (81%) and the median time to complete response was 2.7 months after the start of LDRT. The researchers removed one patient who was an outlier with 27 tumor sites treated, and that dropped the complete response rate down to 76%. The overall response rate, which include an additional five sites with partial response, was 86%.
The researchers found links between complete response and soft tissue site versus non–soft tissue site (hazard ratio, 1.80; 1.12-2.90, P = .02). However, there were no associations between response and chemo-refractory status, ibrutinib-refractory status, prior chemotherapy courts, receipt of concurrent chemotherapy, tumor size, number of fractions, lesions treated per course, or blastoid variant.
The overall survival at 1 year after LDRT initiation was 90% and the 1-year progression-free survival was 55%. All five patients who died were refractory to ibrutinib.
The researchers reported finding no radiation therapy–related toxicities, even when patients received concurrent chemotherapy.
The use of LDRT has the potential to bridge refractory patients to subsequent therapies or to provide treatment breaks as patients recover from toxicities, the researchers said. However, they called for additional studies to confirm that this approach improves progression-free survival over chemotherapy alone.
The study was supported in part by a grant from the National Cancer Institute. The researchers reported having no competing financial interests.
SOURCE: Ning MS et al. Blood Adv. 2019. Jul 9;3(13):2035-9.
Low-dose radiation therapy – with or without concurrent chemotherapy – appears promising as a treatment for patients with relapsed or refractory mantle cell lymphoma (MCL) or at least a bridge to subsequent therapy, according to findings published in Blood Advances.
Matthew S. Ning, MD, of the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and colleagues, said this is the first study to evaluate low-dose radiation therapy (LDRT) with chemotherapy as a treatment modality outside of palliative care for relapsed, multiple refractory MCL patients.
“Our findings indicate that LDRT imparts excellent [local control], minimal toxicity, and favorable outcomes in this setting,” the researchers said.
The study included 19 patients with a total of 98 sites of relapsed, refractory MCL who were treated from 2014 to 2018. The median follow-up was 51.3 months from initial diagnosis and 15.4 months from initial treatment with low-dose radiation therapy, given at a dose of 4 Gy.
These were hard-to-treat patients who had received multiple prior therapies since diagnosis, including carfilzomib, ibrutinib, bortezomib, anthracycline, and rituximab. In total, 8 of the patients had previously undergone autologous stem cell transplant and 11 were refractory to ibrutinib by the time of initial radiation therapy.
Median age of the patients was 69 years; 15 patients had classical histology and 4 had blastoid variant. Among the 98 tumor sites treated, the median tumor size was 2.8 cm.
In all, 14 patients received initial LDRT that was concurrent with chemotherapy. The remaining 5 patients had stopped chemotherapy prior to starting LDRT.
LDRT was given in 1-2 daily fractions via 3-dimensional conformal radiation therapy or electron beam.
Of the 98 tumor sites treated, complete response was achieved for 79 sites (81%) and the median time to complete response was 2.7 months after the start of LDRT. The researchers removed one patient who was an outlier with 27 tumor sites treated, and that dropped the complete response rate down to 76%. The overall response rate, which include an additional five sites with partial response, was 86%.
The researchers found links between complete response and soft tissue site versus non–soft tissue site (hazard ratio, 1.80; 1.12-2.90, P = .02). However, there were no associations between response and chemo-refractory status, ibrutinib-refractory status, prior chemotherapy courts, receipt of concurrent chemotherapy, tumor size, number of fractions, lesions treated per course, or blastoid variant.
The overall survival at 1 year after LDRT initiation was 90% and the 1-year progression-free survival was 55%. All five patients who died were refractory to ibrutinib.
The researchers reported finding no radiation therapy–related toxicities, even when patients received concurrent chemotherapy.
The use of LDRT has the potential to bridge refractory patients to subsequent therapies or to provide treatment breaks as patients recover from toxicities, the researchers said. However, they called for additional studies to confirm that this approach improves progression-free survival over chemotherapy alone.
The study was supported in part by a grant from the National Cancer Institute. The researchers reported having no competing financial interests.
SOURCE: Ning MS et al. Blood Adv. 2019. Jul 9;3(13):2035-9.
FROM BLOOD ADVANCES
Key clinical point:
Major finding: The overall survival was 90% at 1 year following the initiation of low-dose radiation therapy (4 Gy).
Study details: A study of 19 patients with relapsed, refractory mantle cell lymphoma who received low-dose radiation at doses of 4 Gy at 98 sites of disease.
Disclosures: The study was supported in part by a grant from the National Cancer Institute. The researchers reported having no competing financial interests.
Source: Ning MS et al. Blood Adv. 2019. Jul 9;3(13):2035-9.
ABIM rolls out shorter, tailored MOC exams in oncology
Oncologists who specialize in treating hematologic malignancies or breast cancer will have more options for fulfilling their maintenance of certification exam requirements beginning next year.
The American Board of Internal Medicine (ABIM), in partnership with the American Society of Clinical Oncology (ASCO), will begin offering a more frequent, more specialized, and lower-stakes exam as an alternative to the current 10-year examination.
The new pathway was announced by ABIM and ASCO in May 2018 after 2 years of gathering feedback from physicians about the need for an exam that tests them in their area of practice – rather than all areas of oncology.
Now the groups are rolling out the first three assessments created under this model – general oncology, hematologic malignancies, and breast cancer. This will be followed in 2022 by exams in gastrointestinal malignancies and lung cancer/thoracic malignancies. Additional new exams will roll out in even-numbered years based on the level of physician interest.
Registration will begin on Dec. 1, 2019, for the 2020 exam, which will be offered in March and September.
Here’s how it works: Oncologists who choose the new ABIM/ASCO Medical Oncology Learning & Assessment pathway will forgo the 10-year exam in favor of shorter exams every 2 years. The new exam – which is about one-third the size of the traditional exam – is given online and can be taken at home, at the office, or at a test center.
The 2-year exam is pass/fail and physicians are allowed one retake. If they fail twice, they must take the 10-year exam.
The cost over 10 years will be the same, regardless of whether one takes the traditional exam or follows the newer path, according to ABIM.
ABIM and ASCO also have designed education around the exam. After registration, test-takers will be supplied with study materials and after the test they’ll receive additional, tailored education on questions that they got wrong.
Giving physicians feedback on how they can improve is a major change, said Richard G. Battaglia, MD, chief medical officer for ABIM. He said that one of the main messages they heard from physicians was that the exam needed to have educational value.
The other message they heard over and over, Dr. Battaglia said, is that practice tends to focus over time and that physicians want to be assessed on what they see every day.
For that reason, the big shift is in the tailored nature of the exam. All of the 2-year exams offered will contain a core module with questions that every oncologist should know, related to symptom management, disease assessment, and principles of genetics and genomics. That core module will make up 25% of the test.
The remaining 75% of the exam will be disease focused, with questions on diagnosis, testing, treatment, prognosis, and common case examples, said Jamie Von Roenn, MD, vice president of education, science, and professional development at ASCO.
While test takers will have access to resources, such as UpToDate, during the exam, Dr. Von Roenn said don’t expect to be tested on obscure knowledge or asked about rare conditions. “All of the questions are clinical vignettes,” she said. “These are common questions that oncologists face in practice.”
The 2-year general oncology exam will follow the same overall blueprint as the traditional maintenance of certification exam, but will be “very clinically based,” Dr. Von Roenn said. “We’re not asking for things that you can look up,” she said. The exam will instead be focused on how to apply knowledge to common clinical examples.
For that reason, Dr. Von Roenn and Dr. Battaglia said physicians won’t need to spend time and money on intensive exam preparation.
“I actually suspect that people who are busy clinicians wouldn’t need to study, period,” Dr. Von Roenn said.
Richard Larson, MD, reviewed some of the materials for the hematologic malignancies exam and said the test is focused on practical scenarios.
“It’s certainly reasonable to take the test without taking a lot of time to prepare for it,” if physicians are attending annual meetings and grand rounds, and staying current on the medical literature, said Dr. Larson, professor of medicine in the department of hematology-oncology at the University of Chicago, “We’re not aiming at the zebras.”
Thomas LeBlanc, MD, who was not involved with the development of the exam, called this a welcome and overdue change.
“As someone who sees and treats only patients with blood cancers, it doesn’t make sense for me to be tested on largely solid tumor knowledge, with very little of the exam content being in the area of my practice,” said Dr. LeBlanc, associate professor of medicine at Duke University, Durham, N.C. “That’s what the old examination process is like. If I haven’t kept up on how to treat colon cancer, how does that reflect anything meaningful about my abilities as a leukemia specialist?”
Dr. Battaglia encouraged any oncologist with an assessment due date coming up in the next 2 years to consider the new format. For physicians whose oncology certification has lapsed, they can regain certification by successfully passing two of the general oncology exams.
Another reason to consider trying out the new test in 2020 is that physicians can take it with “no consequence.” While normally physicians have an assessment requirement every 10 years, physicians due to pass an exam in 2020 will not be penalized if they take this shorter test option next year and are unsuccessful. They instead will get a chance to try again in 2022.
Regardless of what specialty area clinicians choose for the 2-year exam, their certificate will be in medical oncology. Opting for the 2-year exam won’t affect other certificates. Clinicians can continue to take the 10-year exam for other areas in which they are certified, Dr. Battaglia said.
Dr. Battaglia said that ABIM is looking for ways to decrease the burden on physicians who are dual boarded, and is having conversations with the specialty boards of medical oncology and hematology about how to do that, but those are early-stage discussions. “It’s on our radar screen,” he said.
The American Society of Hematology has suggested to ABIM that “longitudinal, formative assessments” are a more appropriate way to engage physicians in maintaining certification. ASH submitted comments to the American Board of Medical Specialties, which oversees ABIM, earlier this year on the best ways to overhaul maintenance of certification. While the society continues to advocate for this change, ASH officials are also working with ABIM to implement changes to the current hematology recertification assessment requirement.
“The society is looking forward to working with ABIM to ensure future hematology maintenance of certification exams are more focused on the needs of each practitioner as reflected in the mix of patients and diseases cared for in that practice,” said Alan Lichtin, MD, a hematologist at the Cleveland Clinic who serves as chair of ASH’s maintenance of certification working group. “ASH is currently exploring opportunities to work with ABIM to identify common practice profiles, with the intent to introduce an updated Knowledge Check In for hematology in 2021.”
Oncologists who specialize in treating hematologic malignancies or breast cancer will have more options for fulfilling their maintenance of certification exam requirements beginning next year.
The American Board of Internal Medicine (ABIM), in partnership with the American Society of Clinical Oncology (ASCO), will begin offering a more frequent, more specialized, and lower-stakes exam as an alternative to the current 10-year examination.
The new pathway was announced by ABIM and ASCO in May 2018 after 2 years of gathering feedback from physicians about the need for an exam that tests them in their area of practice – rather than all areas of oncology.
Now the groups are rolling out the first three assessments created under this model – general oncology, hematologic malignancies, and breast cancer. This will be followed in 2022 by exams in gastrointestinal malignancies and lung cancer/thoracic malignancies. Additional new exams will roll out in even-numbered years based on the level of physician interest.
Registration will begin on Dec. 1, 2019, for the 2020 exam, which will be offered in March and September.
Here’s how it works: Oncologists who choose the new ABIM/ASCO Medical Oncology Learning & Assessment pathway will forgo the 10-year exam in favor of shorter exams every 2 years. The new exam – which is about one-third the size of the traditional exam – is given online and can be taken at home, at the office, or at a test center.
The 2-year exam is pass/fail and physicians are allowed one retake. If they fail twice, they must take the 10-year exam.
The cost over 10 years will be the same, regardless of whether one takes the traditional exam or follows the newer path, according to ABIM.
ABIM and ASCO also have designed education around the exam. After registration, test-takers will be supplied with study materials and after the test they’ll receive additional, tailored education on questions that they got wrong.
Giving physicians feedback on how they can improve is a major change, said Richard G. Battaglia, MD, chief medical officer for ABIM. He said that one of the main messages they heard from physicians was that the exam needed to have educational value.
The other message they heard over and over, Dr. Battaglia said, is that practice tends to focus over time and that physicians want to be assessed on what they see every day.
For that reason, the big shift is in the tailored nature of the exam. All of the 2-year exams offered will contain a core module with questions that every oncologist should know, related to symptom management, disease assessment, and principles of genetics and genomics. That core module will make up 25% of the test.
The remaining 75% of the exam will be disease focused, with questions on diagnosis, testing, treatment, prognosis, and common case examples, said Jamie Von Roenn, MD, vice president of education, science, and professional development at ASCO.
While test takers will have access to resources, such as UpToDate, during the exam, Dr. Von Roenn said don’t expect to be tested on obscure knowledge or asked about rare conditions. “All of the questions are clinical vignettes,” she said. “These are common questions that oncologists face in practice.”
The 2-year general oncology exam will follow the same overall blueprint as the traditional maintenance of certification exam, but will be “very clinically based,” Dr. Von Roenn said. “We’re not asking for things that you can look up,” she said. The exam will instead be focused on how to apply knowledge to common clinical examples.
For that reason, Dr. Von Roenn and Dr. Battaglia said physicians won’t need to spend time and money on intensive exam preparation.
“I actually suspect that people who are busy clinicians wouldn’t need to study, period,” Dr. Von Roenn said.
Richard Larson, MD, reviewed some of the materials for the hematologic malignancies exam and said the test is focused on practical scenarios.
“It’s certainly reasonable to take the test without taking a lot of time to prepare for it,” if physicians are attending annual meetings and grand rounds, and staying current on the medical literature, said Dr. Larson, professor of medicine in the department of hematology-oncology at the University of Chicago, “We’re not aiming at the zebras.”
Thomas LeBlanc, MD, who was not involved with the development of the exam, called this a welcome and overdue change.
“As someone who sees and treats only patients with blood cancers, it doesn’t make sense for me to be tested on largely solid tumor knowledge, with very little of the exam content being in the area of my practice,” said Dr. LeBlanc, associate professor of medicine at Duke University, Durham, N.C. “That’s what the old examination process is like. If I haven’t kept up on how to treat colon cancer, how does that reflect anything meaningful about my abilities as a leukemia specialist?”
Dr. Battaglia encouraged any oncologist with an assessment due date coming up in the next 2 years to consider the new format. For physicians whose oncology certification has lapsed, they can regain certification by successfully passing two of the general oncology exams.
Another reason to consider trying out the new test in 2020 is that physicians can take it with “no consequence.” While normally physicians have an assessment requirement every 10 years, physicians due to pass an exam in 2020 will not be penalized if they take this shorter test option next year and are unsuccessful. They instead will get a chance to try again in 2022.
Regardless of what specialty area clinicians choose for the 2-year exam, their certificate will be in medical oncology. Opting for the 2-year exam won’t affect other certificates. Clinicians can continue to take the 10-year exam for other areas in which they are certified, Dr. Battaglia said.
Dr. Battaglia said that ABIM is looking for ways to decrease the burden on physicians who are dual boarded, and is having conversations with the specialty boards of medical oncology and hematology about how to do that, but those are early-stage discussions. “It’s on our radar screen,” he said.
The American Society of Hematology has suggested to ABIM that “longitudinal, formative assessments” are a more appropriate way to engage physicians in maintaining certification. ASH submitted comments to the American Board of Medical Specialties, which oversees ABIM, earlier this year on the best ways to overhaul maintenance of certification. While the society continues to advocate for this change, ASH officials are also working with ABIM to implement changes to the current hematology recertification assessment requirement.
“The society is looking forward to working with ABIM to ensure future hematology maintenance of certification exams are more focused on the needs of each practitioner as reflected in the mix of patients and diseases cared for in that practice,” said Alan Lichtin, MD, a hematologist at the Cleveland Clinic who serves as chair of ASH’s maintenance of certification working group. “ASH is currently exploring opportunities to work with ABIM to identify common practice profiles, with the intent to introduce an updated Knowledge Check In for hematology in 2021.”
Oncologists who specialize in treating hematologic malignancies or breast cancer will have more options for fulfilling their maintenance of certification exam requirements beginning next year.
The American Board of Internal Medicine (ABIM), in partnership with the American Society of Clinical Oncology (ASCO), will begin offering a more frequent, more specialized, and lower-stakes exam as an alternative to the current 10-year examination.
The new pathway was announced by ABIM and ASCO in May 2018 after 2 years of gathering feedback from physicians about the need for an exam that tests them in their area of practice – rather than all areas of oncology.
Now the groups are rolling out the first three assessments created under this model – general oncology, hematologic malignancies, and breast cancer. This will be followed in 2022 by exams in gastrointestinal malignancies and lung cancer/thoracic malignancies. Additional new exams will roll out in even-numbered years based on the level of physician interest.
Registration will begin on Dec. 1, 2019, for the 2020 exam, which will be offered in March and September.
Here’s how it works: Oncologists who choose the new ABIM/ASCO Medical Oncology Learning & Assessment pathway will forgo the 10-year exam in favor of shorter exams every 2 years. The new exam – which is about one-third the size of the traditional exam – is given online and can be taken at home, at the office, or at a test center.
The 2-year exam is pass/fail and physicians are allowed one retake. If they fail twice, they must take the 10-year exam.
The cost over 10 years will be the same, regardless of whether one takes the traditional exam or follows the newer path, according to ABIM.
ABIM and ASCO also have designed education around the exam. After registration, test-takers will be supplied with study materials and after the test they’ll receive additional, tailored education on questions that they got wrong.
Giving physicians feedback on how they can improve is a major change, said Richard G. Battaglia, MD, chief medical officer for ABIM. He said that one of the main messages they heard from physicians was that the exam needed to have educational value.
The other message they heard over and over, Dr. Battaglia said, is that practice tends to focus over time and that physicians want to be assessed on what they see every day.
For that reason, the big shift is in the tailored nature of the exam. All of the 2-year exams offered will contain a core module with questions that every oncologist should know, related to symptom management, disease assessment, and principles of genetics and genomics. That core module will make up 25% of the test.
The remaining 75% of the exam will be disease focused, with questions on diagnosis, testing, treatment, prognosis, and common case examples, said Jamie Von Roenn, MD, vice president of education, science, and professional development at ASCO.
While test takers will have access to resources, such as UpToDate, during the exam, Dr. Von Roenn said don’t expect to be tested on obscure knowledge or asked about rare conditions. “All of the questions are clinical vignettes,” she said. “These are common questions that oncologists face in practice.”
The 2-year general oncology exam will follow the same overall blueprint as the traditional maintenance of certification exam, but will be “very clinically based,” Dr. Von Roenn said. “We’re not asking for things that you can look up,” she said. The exam will instead be focused on how to apply knowledge to common clinical examples.
For that reason, Dr. Von Roenn and Dr. Battaglia said physicians won’t need to spend time and money on intensive exam preparation.
“I actually suspect that people who are busy clinicians wouldn’t need to study, period,” Dr. Von Roenn said.
Richard Larson, MD, reviewed some of the materials for the hematologic malignancies exam and said the test is focused on practical scenarios.
“It’s certainly reasonable to take the test without taking a lot of time to prepare for it,” if physicians are attending annual meetings and grand rounds, and staying current on the medical literature, said Dr. Larson, professor of medicine in the department of hematology-oncology at the University of Chicago, “We’re not aiming at the zebras.”
Thomas LeBlanc, MD, who was not involved with the development of the exam, called this a welcome and overdue change.
“As someone who sees and treats only patients with blood cancers, it doesn’t make sense for me to be tested on largely solid tumor knowledge, with very little of the exam content being in the area of my practice,” said Dr. LeBlanc, associate professor of medicine at Duke University, Durham, N.C. “That’s what the old examination process is like. If I haven’t kept up on how to treat colon cancer, how does that reflect anything meaningful about my abilities as a leukemia specialist?”
Dr. Battaglia encouraged any oncologist with an assessment due date coming up in the next 2 years to consider the new format. For physicians whose oncology certification has lapsed, they can regain certification by successfully passing two of the general oncology exams.
Another reason to consider trying out the new test in 2020 is that physicians can take it with “no consequence.” While normally physicians have an assessment requirement every 10 years, physicians due to pass an exam in 2020 will not be penalized if they take this shorter test option next year and are unsuccessful. They instead will get a chance to try again in 2022.
Regardless of what specialty area clinicians choose for the 2-year exam, their certificate will be in medical oncology. Opting for the 2-year exam won’t affect other certificates. Clinicians can continue to take the 10-year exam for other areas in which they are certified, Dr. Battaglia said.
Dr. Battaglia said that ABIM is looking for ways to decrease the burden on physicians who are dual boarded, and is having conversations with the specialty boards of medical oncology and hematology about how to do that, but those are early-stage discussions. “It’s on our radar screen,” he said.
The American Society of Hematology has suggested to ABIM that “longitudinal, formative assessments” are a more appropriate way to engage physicians in maintaining certification. ASH submitted comments to the American Board of Medical Specialties, which oversees ABIM, earlier this year on the best ways to overhaul maintenance of certification. While the society continues to advocate for this change, ASH officials are also working with ABIM to implement changes to the current hematology recertification assessment requirement.
“The society is looking forward to working with ABIM to ensure future hematology maintenance of certification exams are more focused on the needs of each practitioner as reflected in the mix of patients and diseases cared for in that practice,” said Alan Lichtin, MD, a hematologist at the Cleveland Clinic who serves as chair of ASH’s maintenance of certification working group. “ASH is currently exploring opportunities to work with ABIM to identify common practice profiles, with the intent to introduce an updated Knowledge Check In for hematology in 2021.”
Cleveland Clinic targets time to treat in cancer
CHICAGO – In 2014, the average time from diagnosis to treatment initiation for new cancer patients at the Cleveland Clinic was 29-41 days, depending on whether the patient was diagnosed internally or externally. That figure was not acceptable, said Brian J. Bolwell, MD, chairman of the Cleveland Clinic’s Taussig Cancer Institute.
Since then, the time-to-treat metric has improved dramatically, dropping 33%. Today, time to treat for new cancer patients is 25-31 days, depending on the site of diagnosis.
To get there, leaders at the cancer center examined the causes of delay within each of their disease programs. The analysis revealed that less than 20% of the time it was patient preferences that slowed down the initiation of treatment, but that more than 80% of the time the delay was on the part of their institution.
Dr. Bolwell said this led them to start tracking every newly diagnosed patient who came through the cancer center to ensure they didn’t fall through the cracks, and that they were treated as rapidly as possible.
But figuring out how to get patients to treatment quicker depended on the type of cancer they had, since each type of cancer had different challenges and different points of entry to the health care system.
“So for breast cancer, it turns out a lot of the challenges might be coordination of surgery because sometimes a general surgeon has to work with a reconstructive-plastic surgeon and coordinating the surgical schedules might drastically lengthen time to treat,” he said during an interview at the annual meeting of the American Society of Clinical Oncology.
They helped address that problem by scheduling breast cancer patients for surgery by the next available operating room slot, rather than doing the scheduling by surgeon.
There are additional barriers to achieving a rapid time to treat standard, including prior authorization, Dr. Bolwell said. But they are continuing to chip away at the metric, working within each cancer type to lower the obstacles to treatment. “I don’t think we’ll ever be satisfied with where we are,” Dr. Bolwell said.
Dr. Bolwell reported having no relevant financial disclosures.
CHICAGO – In 2014, the average time from diagnosis to treatment initiation for new cancer patients at the Cleveland Clinic was 29-41 days, depending on whether the patient was diagnosed internally or externally. That figure was not acceptable, said Brian J. Bolwell, MD, chairman of the Cleveland Clinic’s Taussig Cancer Institute.
Since then, the time-to-treat metric has improved dramatically, dropping 33%. Today, time to treat for new cancer patients is 25-31 days, depending on the site of diagnosis.
To get there, leaders at the cancer center examined the causes of delay within each of their disease programs. The analysis revealed that less than 20% of the time it was patient preferences that slowed down the initiation of treatment, but that more than 80% of the time the delay was on the part of their institution.
Dr. Bolwell said this led them to start tracking every newly diagnosed patient who came through the cancer center to ensure they didn’t fall through the cracks, and that they were treated as rapidly as possible.
But figuring out how to get patients to treatment quicker depended on the type of cancer they had, since each type of cancer had different challenges and different points of entry to the health care system.
“So for breast cancer, it turns out a lot of the challenges might be coordination of surgery because sometimes a general surgeon has to work with a reconstructive-plastic surgeon and coordinating the surgical schedules might drastically lengthen time to treat,” he said during an interview at the annual meeting of the American Society of Clinical Oncology.
They helped address that problem by scheduling breast cancer patients for surgery by the next available operating room slot, rather than doing the scheduling by surgeon.
There are additional barriers to achieving a rapid time to treat standard, including prior authorization, Dr. Bolwell said. But they are continuing to chip away at the metric, working within each cancer type to lower the obstacles to treatment. “I don’t think we’ll ever be satisfied with where we are,” Dr. Bolwell said.
Dr. Bolwell reported having no relevant financial disclosures.
CHICAGO – In 2014, the average time from diagnosis to treatment initiation for new cancer patients at the Cleveland Clinic was 29-41 days, depending on whether the patient was diagnosed internally or externally. That figure was not acceptable, said Brian J. Bolwell, MD, chairman of the Cleveland Clinic’s Taussig Cancer Institute.
Since then, the time-to-treat metric has improved dramatically, dropping 33%. Today, time to treat for new cancer patients is 25-31 days, depending on the site of diagnosis.
To get there, leaders at the cancer center examined the causes of delay within each of their disease programs. The analysis revealed that less than 20% of the time it was patient preferences that slowed down the initiation of treatment, but that more than 80% of the time the delay was on the part of their institution.
Dr. Bolwell said this led them to start tracking every newly diagnosed patient who came through the cancer center to ensure they didn’t fall through the cracks, and that they were treated as rapidly as possible.
But figuring out how to get patients to treatment quicker depended on the type of cancer they had, since each type of cancer had different challenges and different points of entry to the health care system.
“So for breast cancer, it turns out a lot of the challenges might be coordination of surgery because sometimes a general surgeon has to work with a reconstructive-plastic surgeon and coordinating the surgical schedules might drastically lengthen time to treat,” he said during an interview at the annual meeting of the American Society of Clinical Oncology.
They helped address that problem by scheduling breast cancer patients for surgery by the next available operating room slot, rather than doing the scheduling by surgeon.
There are additional barriers to achieving a rapid time to treat standard, including prior authorization, Dr. Bolwell said. But they are continuing to chip away at the metric, working within each cancer type to lower the obstacles to treatment. “I don’t think we’ll ever be satisfied with where we are,” Dr. Bolwell said.
Dr. Bolwell reported having no relevant financial disclosures.
FROM ASCO 2019
Low intensity bridging may be best path to CAR T in adult ALL
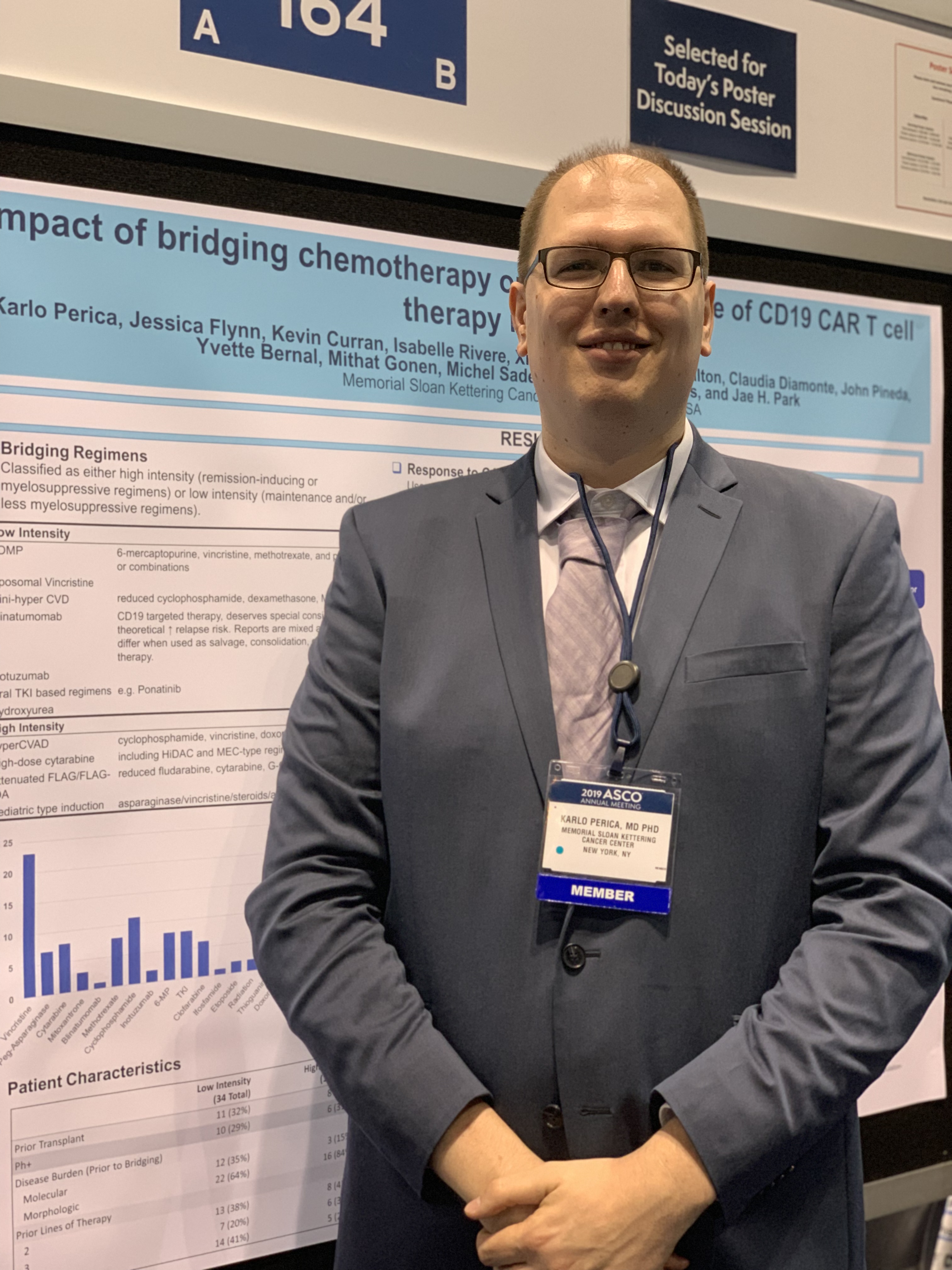
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
FROM ASCO 2019
FDA approves PI3K inhibitor alpelisib for breast cancer
The Food and Drug Administration has approved the first PI3K inhibitor for the treatment of breast cancer.
The drug, alpelisib (Piqray), was approved for use in combination with fulvestrant for men and postmenopausal women who have hormone receptor (HR)–positive, human epidermal growth factor receptor 2 (HER2)–negative, PIK3CA-mutated, advanced or metastatic breast cancer after progression on, or after, an endocrine-based regimen. The approval was announced by the FDA in a statement.
The agency also approved a diagnostic test – the therascreen PIK3CA RGQ PCR Kit – for detecting the PIK3CA mutation. The approval is based on results from the SOLAR-1 trial. In 572 HR-positive, HER2-negative patients with advanced or metastatic breast cancer who progressed after, or during, treatment with an aromatase inhibitor, the addition of alpelisib to fulvestrant significantly improved progression-free survival in patients with PIK3CA mutated tumors.
Median progression-free survival was 5.7 months on fulvestrant plus placebo, versus 11 months with fulvestrant plus alpelisib (hazard ratio for progression or death, 0.65; 95% confidence interval, 0.50-0.85; P less than .001). The results of the trial were recently published in the New England Journal of Medicine (2019 May 16;380[20]:1929-40).
In the FDA statement, Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, noted that alpelisib is the “first PI3K inhibitor to demonstrate a clinically meaningful benefit in treating patients with this type of breast cancer.”
The drug’s application was approved under the Real-Time Oncology Review pilot program, which allows the FDA to begin analyzing efficacy and safety databases before a new drug application is even submitted.
The FDA noted that patients should not start treatment on alpelisib if they have a history of severe skin reactions, such as Stevens-Johnson syndrome, erythema multiforme, or toxic epidermal necrolysis.
The Food and Drug Administration has approved the first PI3K inhibitor for the treatment of breast cancer.
The drug, alpelisib (Piqray), was approved for use in combination with fulvestrant for men and postmenopausal women who have hormone receptor (HR)–positive, human epidermal growth factor receptor 2 (HER2)–negative, PIK3CA-mutated, advanced or metastatic breast cancer after progression on, or after, an endocrine-based regimen. The approval was announced by the FDA in a statement.
The agency also approved a diagnostic test – the therascreen PIK3CA RGQ PCR Kit – for detecting the PIK3CA mutation. The approval is based on results from the SOLAR-1 trial. In 572 HR-positive, HER2-negative patients with advanced or metastatic breast cancer who progressed after, or during, treatment with an aromatase inhibitor, the addition of alpelisib to fulvestrant significantly improved progression-free survival in patients with PIK3CA mutated tumors.
Median progression-free survival was 5.7 months on fulvestrant plus placebo, versus 11 months with fulvestrant plus alpelisib (hazard ratio for progression or death, 0.65; 95% confidence interval, 0.50-0.85; P less than .001). The results of the trial were recently published in the New England Journal of Medicine (2019 May 16;380[20]:1929-40).
In the FDA statement, Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, noted that alpelisib is the “first PI3K inhibitor to demonstrate a clinically meaningful benefit in treating patients with this type of breast cancer.”
The drug’s application was approved under the Real-Time Oncology Review pilot program, which allows the FDA to begin analyzing efficacy and safety databases before a new drug application is even submitted.
The FDA noted that patients should not start treatment on alpelisib if they have a history of severe skin reactions, such as Stevens-Johnson syndrome, erythema multiforme, or toxic epidermal necrolysis.
The Food and Drug Administration has approved the first PI3K inhibitor for the treatment of breast cancer.
The drug, alpelisib (Piqray), was approved for use in combination with fulvestrant for men and postmenopausal women who have hormone receptor (HR)–positive, human epidermal growth factor receptor 2 (HER2)–negative, PIK3CA-mutated, advanced or metastatic breast cancer after progression on, or after, an endocrine-based regimen. The approval was announced by the FDA in a statement.
The agency also approved a diagnostic test – the therascreen PIK3CA RGQ PCR Kit – for detecting the PIK3CA mutation. The approval is based on results from the SOLAR-1 trial. In 572 HR-positive, HER2-negative patients with advanced or metastatic breast cancer who progressed after, or during, treatment with an aromatase inhibitor, the addition of alpelisib to fulvestrant significantly improved progression-free survival in patients with PIK3CA mutated tumors.
Median progression-free survival was 5.7 months on fulvestrant plus placebo, versus 11 months with fulvestrant plus alpelisib (hazard ratio for progression or death, 0.65; 95% confidence interval, 0.50-0.85; P less than .001). The results of the trial were recently published in the New England Journal of Medicine (2019 May 16;380[20]:1929-40).
In the FDA statement, Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, noted that alpelisib is the “first PI3K inhibitor to demonstrate a clinically meaningful benefit in treating patients with this type of breast cancer.”
The drug’s application was approved under the Real-Time Oncology Review pilot program, which allows the FDA to begin analyzing efficacy and safety databases before a new drug application is even submitted.
The FDA noted that patients should not start treatment on alpelisib if they have a history of severe skin reactions, such as Stevens-Johnson syndrome, erythema multiforme, or toxic epidermal necrolysis.
Trial follow-up spotlights survival gains in follicular lymphoma
Results from a 13-year follow-up of a trial comparing two types of rituximab-based chemotherapy as upfront treatment for patients with follicular lymphoma show an “extraordinary improvement” in overall survival, compared with the prerituximab era.
In a finding that the researchers termed “somewhat unexpected,” complete remission was the strongest factor in long-term survival.
Between March 2000 and May 2005, researchers enrolled 136 high-risk follicular lymphoma patients in the GITMO-IIL trial to evaluate the superiority of high-dose chemotherapy with rituximab and autograft (R-HDS) versus conventional chemotherapy with rituximab (R-CHOP) as frontline therapy. At a median follow-up of 4 years, there was no survival advantage for R-HDS.
In the current analysis – that had a 13-year median follow-up – median survival had not yet been reached. As of February 2017, two-thirds of all patients were alive at their last follow-up. Overall survival was 68.5% in the R-CHOP arm and 64.5% in the R-HDS arm, Riccardo Bruna, MD, of the European Institute of Oncology in Milano, Italy, and his colleagues, reported in Haematologica.
The main causes of death for the 46 patients who had died as of long-term follow-up were disease progression and secondary malignancies. Other causes included cardiovascular events, infections, graft failure following autograft, anaphylactic shock, and late sudden death.
Complete remission was seen in 98 patients (73.1%) overall – 59.1% in the R-CHOP arm and 86.7% in the R-HDS arm. Achieving durable complete remission was associated with prolonged survival, the researchers reported. Of the 79 patients in complete remission at 2 years after the start of treatment, 65 (82.3%) were alive at 13 years, compared with 21 (58.3%) of 36 patients who had an early relapse (P = .003).
“[Complete remission] achievement was the most important factor for prolonged survival,” the researchers wrote. “The importance of disease response is further emphasized by the first-time observation that [molecular remission] achievement is associated with survival duration and a high proportion of patients had prolonged survival in the absence of disease recurrence.”
The researchers reported that this is longest ever follow-up reported for first-line treatment of follicular lymphoma with rituximab-based chemotherapy.
This work was supported in part by the Ministero Italiano Università e Ricerca and by Banca del Piemonte. The initial clinical trial was supported by Compagnia di San Paolo, Regione Piemonte, and Roche, which provided rituximab for the study.
SOURCE: Bruna R et al. Haematologica. 2019 Apr 11. doi: 10.3324/haematol.2018.209932.
Results from a 13-year follow-up of a trial comparing two types of rituximab-based chemotherapy as upfront treatment for patients with follicular lymphoma show an “extraordinary improvement” in overall survival, compared with the prerituximab era.
In a finding that the researchers termed “somewhat unexpected,” complete remission was the strongest factor in long-term survival.
Between March 2000 and May 2005, researchers enrolled 136 high-risk follicular lymphoma patients in the GITMO-IIL trial to evaluate the superiority of high-dose chemotherapy with rituximab and autograft (R-HDS) versus conventional chemotherapy with rituximab (R-CHOP) as frontline therapy. At a median follow-up of 4 years, there was no survival advantage for R-HDS.
In the current analysis – that had a 13-year median follow-up – median survival had not yet been reached. As of February 2017, two-thirds of all patients were alive at their last follow-up. Overall survival was 68.5% in the R-CHOP arm and 64.5% in the R-HDS arm, Riccardo Bruna, MD, of the European Institute of Oncology in Milano, Italy, and his colleagues, reported in Haematologica.
The main causes of death for the 46 patients who had died as of long-term follow-up were disease progression and secondary malignancies. Other causes included cardiovascular events, infections, graft failure following autograft, anaphylactic shock, and late sudden death.
Complete remission was seen in 98 patients (73.1%) overall – 59.1% in the R-CHOP arm and 86.7% in the R-HDS arm. Achieving durable complete remission was associated with prolonged survival, the researchers reported. Of the 79 patients in complete remission at 2 years after the start of treatment, 65 (82.3%) were alive at 13 years, compared with 21 (58.3%) of 36 patients who had an early relapse (P = .003).
“[Complete remission] achievement was the most important factor for prolonged survival,” the researchers wrote. “The importance of disease response is further emphasized by the first-time observation that [molecular remission] achievement is associated with survival duration and a high proportion of patients had prolonged survival in the absence of disease recurrence.”
The researchers reported that this is longest ever follow-up reported for first-line treatment of follicular lymphoma with rituximab-based chemotherapy.
This work was supported in part by the Ministero Italiano Università e Ricerca and by Banca del Piemonte. The initial clinical trial was supported by Compagnia di San Paolo, Regione Piemonte, and Roche, which provided rituximab for the study.
SOURCE: Bruna R et al. Haematologica. 2019 Apr 11. doi: 10.3324/haematol.2018.209932.
Results from a 13-year follow-up of a trial comparing two types of rituximab-based chemotherapy as upfront treatment for patients with follicular lymphoma show an “extraordinary improvement” in overall survival, compared with the prerituximab era.
In a finding that the researchers termed “somewhat unexpected,” complete remission was the strongest factor in long-term survival.
Between March 2000 and May 2005, researchers enrolled 136 high-risk follicular lymphoma patients in the GITMO-IIL trial to evaluate the superiority of high-dose chemotherapy with rituximab and autograft (R-HDS) versus conventional chemotherapy with rituximab (R-CHOP) as frontline therapy. At a median follow-up of 4 years, there was no survival advantage for R-HDS.
In the current analysis – that had a 13-year median follow-up – median survival had not yet been reached. As of February 2017, two-thirds of all patients were alive at their last follow-up. Overall survival was 68.5% in the R-CHOP arm and 64.5% in the R-HDS arm, Riccardo Bruna, MD, of the European Institute of Oncology in Milano, Italy, and his colleagues, reported in Haematologica.
The main causes of death for the 46 patients who had died as of long-term follow-up were disease progression and secondary malignancies. Other causes included cardiovascular events, infections, graft failure following autograft, anaphylactic shock, and late sudden death.
Complete remission was seen in 98 patients (73.1%) overall – 59.1% in the R-CHOP arm and 86.7% in the R-HDS arm. Achieving durable complete remission was associated with prolonged survival, the researchers reported. Of the 79 patients in complete remission at 2 years after the start of treatment, 65 (82.3%) were alive at 13 years, compared with 21 (58.3%) of 36 patients who had an early relapse (P = .003).
“[Complete remission] achievement was the most important factor for prolonged survival,” the researchers wrote. “The importance of disease response is further emphasized by the first-time observation that [molecular remission] achievement is associated with survival duration and a high proportion of patients had prolonged survival in the absence of disease recurrence.”
The researchers reported that this is longest ever follow-up reported for first-line treatment of follicular lymphoma with rituximab-based chemotherapy.
This work was supported in part by the Ministero Italiano Università e Ricerca and by Banca del Piemonte. The initial clinical trial was supported by Compagnia di San Paolo, Regione Piemonte, and Roche, which provided rituximab for the study.
SOURCE: Bruna R et al. Haematologica. 2019 Apr 11. doi: 10.3324/haematol.2018.209932.
FROM HAEMATOLOGICA
FDA approves venetoclax/obinutuzumab combo for CLL
The Food and Drug Administration has approved the combination of venetoclax (Venclexta) plus obinutuzumab (Gazyva) for patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma.
The approval provides a chemotherapy-free, fixed duration treatment. The FDA based the approval on the results of the phase 3 CLL14 trial, which will be presented at the 2019 annual meeting of the American Society of Clinical Oncology.
Researchers randomized 432 patients to either a 12-month duration of venetoclax with a 6-month duration of obinutuzumab or to a 6-month duration of obinutuzumab plus chlorambucil and another 6-month duration of chlorambucil.
The newly approved combination reduced the risk of disease progression or death (progression-free survival as assessed by an independent review committee) by 67%, compared with obinutuzumab/chlorambucil (hazard ratio, 0.33; P less than .0001).
Venetoclax/obinutuzumab also had a higher rate of minimal residual disease negativity in bone marrow and peripheral blood, compared to the other combination, according to Genentech.
The most common adverse reactions of any grade reported for venetoclax/obinutuzumab were neutropenia, diarrhea, fatigue, nausea, anemia, and upper respiratory tract infection.
The Food and Drug Administration has approved the combination of venetoclax (Venclexta) plus obinutuzumab (Gazyva) for patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma.
The approval provides a chemotherapy-free, fixed duration treatment. The FDA based the approval on the results of the phase 3 CLL14 trial, which will be presented at the 2019 annual meeting of the American Society of Clinical Oncology.
Researchers randomized 432 patients to either a 12-month duration of venetoclax with a 6-month duration of obinutuzumab or to a 6-month duration of obinutuzumab plus chlorambucil and another 6-month duration of chlorambucil.
The newly approved combination reduced the risk of disease progression or death (progression-free survival as assessed by an independent review committee) by 67%, compared with obinutuzumab/chlorambucil (hazard ratio, 0.33; P less than .0001).
Venetoclax/obinutuzumab also had a higher rate of minimal residual disease negativity in bone marrow and peripheral blood, compared to the other combination, according to Genentech.
The most common adverse reactions of any grade reported for venetoclax/obinutuzumab were neutropenia, diarrhea, fatigue, nausea, anemia, and upper respiratory tract infection.
The Food and Drug Administration has approved the combination of venetoclax (Venclexta) plus obinutuzumab (Gazyva) for patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma.
The approval provides a chemotherapy-free, fixed duration treatment. The FDA based the approval on the results of the phase 3 CLL14 trial, which will be presented at the 2019 annual meeting of the American Society of Clinical Oncology.
Researchers randomized 432 patients to either a 12-month duration of venetoclax with a 6-month duration of obinutuzumab or to a 6-month duration of obinutuzumab plus chlorambucil and another 6-month duration of chlorambucil.
The newly approved combination reduced the risk of disease progression or death (progression-free survival as assessed by an independent review committee) by 67%, compared with obinutuzumab/chlorambucil (hazard ratio, 0.33; P less than .0001).
Venetoclax/obinutuzumab also had a higher rate of minimal residual disease negativity in bone marrow and peripheral blood, compared to the other combination, according to Genentech.
The most common adverse reactions of any grade reported for venetoclax/obinutuzumab were neutropenia, diarrhea, fatigue, nausea, anemia, and upper respiratory tract infection.