User login
Timing Is Everything: CAR T for Follicular Lymphoma
“CAR T-cells offer patients with relapsed or refractory follicular lymphoma the most durable responses and improved chance of survival beyond all other available therapies. This holds true for a broad range of high-risk disease features in patients with relapsed or refractory FL. Furthermore, it accomplishes this with a single infusion, and a discrete toxicity that is predictable, reversible and manageable,” said Caron Jacobson, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Presenting at the Great Debates & Updates Hematologic Malignancies conference, held April 5-6 in New York City, Dr. Jacobson argued that more patients with R/R FL should be treated with CAR T.
She cited follow-up results from the ZUMA-5 study indicating that patients with R/R FL treated with the CAR T axicabtagene ciloleucel (YESCARTA; Kite Pharma) have a median progression free survival (PFS) of 57.3 months and a complete response rate (CR) of 80%. Furthermore, the lymphoma-specific four-year PFS appears to be reaching a plateau, suggesting that some patients treated with the agent may be cured.
The most significant drawback of treatment with axicabtagene ciloleucel is cytokine release syndrome (CRS) and neurotoxicity, which occurred at grade three and higher in 6% and 15%, of ZUMA-5 participants, respectively.
Two newer studies of anti-CD-19 CAR T-cell therapy in R/R FL, tisagenlecleucel in ELARA and lisocabtagene maraleucel in TRANSCEND FL, suggest that other CAR T-cell treatments can be as effective as axicabtagene ciloleucel, but with fewer side effects.
At a median follow up of 29 months, CR among patients in the ELARA study was 68.1%, and the overall response rate (ORR) was 86.2%. Fewer than half of patients had any CRS, and none had grade three or higher. Only 10% of patients had serious neurologic events, with only 1% of these events rated as grade three or higher.
At a median of 18.1 months, patients in the TRANSCEND FL study had a CR of 94% and an ORR of 97%. Over 58% of patients had CRS but it was grade three or higher only 1% of the time (one patient); 15% of patients had neurologic toxicity, but it was grade three or higher only 2% of the time (three patients).
Dr. Jacobson’s opponent in the debate, Peter Martin, MD, of NewYork–Presbyterian Hospital, Weill Cornell Medicine in New York City, acknowledged the strong performance of CAR T in R/R FL patients but argued that they should be used only in a small subset of patients.
“About 20% of patients will experience an early recurrence or progression of diseases within 24 months (PoD-24) which is associated with worse outcomes. About half of those patients experienced transformation, so they have diffuse large B-cell lymphoma, and they’re getting CAR T-cells. In the end, only 10% of patients with follicular lymphoma are relapsed or refractory and should consider getting Car T-cell therapy,” said Dr. Martin, who focused the rest of his presentation on the best options for treating patients with indolent R/R FL who did not have PoD-24.
He said these patients may be able to avoid the side effects of CAR T and perform well when treated with lenalidomide rituximab (R2) or bispecific antibodies. Data from the MAGNIFY trial of patients with R/R FL indicate that patients treated with R2 who did not experience relapse less than 24 months after starting treatment and were not heavily refractory to rituximab achieved a median PFS of over 4 years, with grade 3 or higher adverse events occurring in 5% of patients or less.
Treatment with bispecific antibodies, although inferior in performance to CAR T-cell therapy, may offer durable responses in some R/R CL patients without the risk of side effects associated with CAR T.
Mosunetuzumab, a bispecific antibody that is currently approved for follicular lymphoma, is designed with step-up dosing to reduce cytokine release syndrome and “achieved a complete response rate of 60% and a median PFS that looks like it’s probably about two years,” said Dr. Martin, noting that some patients continue to do well after the 3-year mark and speculated that “there will be some really long-term responders.”
In addition to the possibly durable nature of bispecific antibodies, they induce cytokine release syndrome at a much lower rate than CAR T, and most side effects are manageable in an outpatient setting, “usually just with Tylenol occasionally with a dose of steroids,” said Dr. Martin.
He contrasted this response with CAR T-cell therapy, which requires referral and travel to a specialized center for at least 1 month around the time of therapy.
Despite the differences of opinion between the presenters about whether CAR T should be used more or less in R/R FL, essentially the two specialists were making recommendations for different patient groups.
Dr. Jacobson observed that “Dr. Martin is looking at the 80% of people who do really well with follicular lymphoma." Those are the people who don’t require a third line of therapy. They are the people who don’t have PoD-24. I’m looking at the 20% of people who either do require a third line of therapy or who do have PoD-24, and we’re not treating nearly enough of those patients with follicular lymphoma.
“We’re actually arguing about treatment strategies for different populations of patients. And I think ultimately, we agree more than we disagree in the end,” she concluded.
The notion that CAR T, chemotherapy, and bispecific antibodies all have a place in treating R/R FL patients is supported by Charalambos (Babis) Andreadis, MD, hematologist at the University of California San Francisco’s Helen Diller Family Comprehensive Care Center. “If I had a patient with follicular who relapsed 24 months or later after primary therapy and had active disease that needed treatment, most providers would do a lenalidomide-based or chemo-based regimen. Down the line either bispecific or CAR T would be appropriate in third line,” said Dr. Andreadis.
However, he noted,“for someone who is an early progressor, I would similarly not be able to use either [chemotherapy or bispecific antibodies] in second line [therapy] but would definitely think that early CART would be a good option to consider given the longevity of the observed responses so far.”
Dr. Martin disclosed ties with AbbVie, AstraZeneca, BeiGene, Daiichi Sankyo, Epizyme, Genentech, Janssen, Merck, and PeproMene. Dr. Jacobson reported relationships with AbbVie, Abintus Bio, ADC Therapeutics, Appia Bio, AstraZeneca, BMS/Celgene, Caribou Bio, Daiichi Sankyo, ImmPACT Bio, Ipsen, Janssen, Kite/Gilead, MorphoSys, Novartis, Sana, Synthekine, Kite/Gilead, and Pfizer. Dr. Andreadis had no disclosures.
“CAR T-cells offer patients with relapsed or refractory follicular lymphoma the most durable responses and improved chance of survival beyond all other available therapies. This holds true for a broad range of high-risk disease features in patients with relapsed or refractory FL. Furthermore, it accomplishes this with a single infusion, and a discrete toxicity that is predictable, reversible and manageable,” said Caron Jacobson, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Presenting at the Great Debates & Updates Hematologic Malignancies conference, held April 5-6 in New York City, Dr. Jacobson argued that more patients with R/R FL should be treated with CAR T.
She cited follow-up results from the ZUMA-5 study indicating that patients with R/R FL treated with the CAR T axicabtagene ciloleucel (YESCARTA; Kite Pharma) have a median progression free survival (PFS) of 57.3 months and a complete response rate (CR) of 80%. Furthermore, the lymphoma-specific four-year PFS appears to be reaching a plateau, suggesting that some patients treated with the agent may be cured.
The most significant drawback of treatment with axicabtagene ciloleucel is cytokine release syndrome (CRS) and neurotoxicity, which occurred at grade three and higher in 6% and 15%, of ZUMA-5 participants, respectively.
Two newer studies of anti-CD-19 CAR T-cell therapy in R/R FL, tisagenlecleucel in ELARA and lisocabtagene maraleucel in TRANSCEND FL, suggest that other CAR T-cell treatments can be as effective as axicabtagene ciloleucel, but with fewer side effects.
At a median follow up of 29 months, CR among patients in the ELARA study was 68.1%, and the overall response rate (ORR) was 86.2%. Fewer than half of patients had any CRS, and none had grade three or higher. Only 10% of patients had serious neurologic events, with only 1% of these events rated as grade three or higher.
At a median of 18.1 months, patients in the TRANSCEND FL study had a CR of 94% and an ORR of 97%. Over 58% of patients had CRS but it was grade three or higher only 1% of the time (one patient); 15% of patients had neurologic toxicity, but it was grade three or higher only 2% of the time (three patients).
Dr. Jacobson’s opponent in the debate, Peter Martin, MD, of NewYork–Presbyterian Hospital, Weill Cornell Medicine in New York City, acknowledged the strong performance of CAR T in R/R FL patients but argued that they should be used only in a small subset of patients.
“About 20% of patients will experience an early recurrence or progression of diseases within 24 months (PoD-24) which is associated with worse outcomes. About half of those patients experienced transformation, so they have diffuse large B-cell lymphoma, and they’re getting CAR T-cells. In the end, only 10% of patients with follicular lymphoma are relapsed or refractory and should consider getting Car T-cell therapy,” said Dr. Martin, who focused the rest of his presentation on the best options for treating patients with indolent R/R FL who did not have PoD-24.
He said these patients may be able to avoid the side effects of CAR T and perform well when treated with lenalidomide rituximab (R2) or bispecific antibodies. Data from the MAGNIFY trial of patients with R/R FL indicate that patients treated with R2 who did not experience relapse less than 24 months after starting treatment and were not heavily refractory to rituximab achieved a median PFS of over 4 years, with grade 3 or higher adverse events occurring in 5% of patients or less.
Treatment with bispecific antibodies, although inferior in performance to CAR T-cell therapy, may offer durable responses in some R/R CL patients without the risk of side effects associated with CAR T.
Mosunetuzumab, a bispecific antibody that is currently approved for follicular lymphoma, is designed with step-up dosing to reduce cytokine release syndrome and “achieved a complete response rate of 60% and a median PFS that looks like it’s probably about two years,” said Dr. Martin, noting that some patients continue to do well after the 3-year mark and speculated that “there will be some really long-term responders.”
In addition to the possibly durable nature of bispecific antibodies, they induce cytokine release syndrome at a much lower rate than CAR T, and most side effects are manageable in an outpatient setting, “usually just with Tylenol occasionally with a dose of steroids,” said Dr. Martin.
He contrasted this response with CAR T-cell therapy, which requires referral and travel to a specialized center for at least 1 month around the time of therapy.
Despite the differences of opinion between the presenters about whether CAR T should be used more or less in R/R FL, essentially the two specialists were making recommendations for different patient groups.
Dr. Jacobson observed that “Dr. Martin is looking at the 80% of people who do really well with follicular lymphoma." Those are the people who don’t require a third line of therapy. They are the people who don’t have PoD-24. I’m looking at the 20% of people who either do require a third line of therapy or who do have PoD-24, and we’re not treating nearly enough of those patients with follicular lymphoma.
“We’re actually arguing about treatment strategies for different populations of patients. And I think ultimately, we agree more than we disagree in the end,” she concluded.
The notion that CAR T, chemotherapy, and bispecific antibodies all have a place in treating R/R FL patients is supported by Charalambos (Babis) Andreadis, MD, hematologist at the University of California San Francisco’s Helen Diller Family Comprehensive Care Center. “If I had a patient with follicular who relapsed 24 months or later after primary therapy and had active disease that needed treatment, most providers would do a lenalidomide-based or chemo-based regimen. Down the line either bispecific or CAR T would be appropriate in third line,” said Dr. Andreadis.
However, he noted,“for someone who is an early progressor, I would similarly not be able to use either [chemotherapy or bispecific antibodies] in second line [therapy] but would definitely think that early CART would be a good option to consider given the longevity of the observed responses so far.”
Dr. Martin disclosed ties with AbbVie, AstraZeneca, BeiGene, Daiichi Sankyo, Epizyme, Genentech, Janssen, Merck, and PeproMene. Dr. Jacobson reported relationships with AbbVie, Abintus Bio, ADC Therapeutics, Appia Bio, AstraZeneca, BMS/Celgene, Caribou Bio, Daiichi Sankyo, ImmPACT Bio, Ipsen, Janssen, Kite/Gilead, MorphoSys, Novartis, Sana, Synthekine, Kite/Gilead, and Pfizer. Dr. Andreadis had no disclosures.
“CAR T-cells offer patients with relapsed or refractory follicular lymphoma the most durable responses and improved chance of survival beyond all other available therapies. This holds true for a broad range of high-risk disease features in patients with relapsed or refractory FL. Furthermore, it accomplishes this with a single infusion, and a discrete toxicity that is predictable, reversible and manageable,” said Caron Jacobson, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Presenting at the Great Debates & Updates Hematologic Malignancies conference, held April 5-6 in New York City, Dr. Jacobson argued that more patients with R/R FL should be treated with CAR T.
She cited follow-up results from the ZUMA-5 study indicating that patients with R/R FL treated with the CAR T axicabtagene ciloleucel (YESCARTA; Kite Pharma) have a median progression free survival (PFS) of 57.3 months and a complete response rate (CR) of 80%. Furthermore, the lymphoma-specific four-year PFS appears to be reaching a plateau, suggesting that some patients treated with the agent may be cured.
The most significant drawback of treatment with axicabtagene ciloleucel is cytokine release syndrome (CRS) and neurotoxicity, which occurred at grade three and higher in 6% and 15%, of ZUMA-5 participants, respectively.
Two newer studies of anti-CD-19 CAR T-cell therapy in R/R FL, tisagenlecleucel in ELARA and lisocabtagene maraleucel in TRANSCEND FL, suggest that other CAR T-cell treatments can be as effective as axicabtagene ciloleucel, but with fewer side effects.
At a median follow up of 29 months, CR among patients in the ELARA study was 68.1%, and the overall response rate (ORR) was 86.2%. Fewer than half of patients had any CRS, and none had grade three or higher. Only 10% of patients had serious neurologic events, with only 1% of these events rated as grade three or higher.
At a median of 18.1 months, patients in the TRANSCEND FL study had a CR of 94% and an ORR of 97%. Over 58% of patients had CRS but it was grade three or higher only 1% of the time (one patient); 15% of patients had neurologic toxicity, but it was grade three or higher only 2% of the time (three patients).
Dr. Jacobson’s opponent in the debate, Peter Martin, MD, of NewYork–Presbyterian Hospital, Weill Cornell Medicine in New York City, acknowledged the strong performance of CAR T in R/R FL patients but argued that they should be used only in a small subset of patients.
“About 20% of patients will experience an early recurrence or progression of diseases within 24 months (PoD-24) which is associated with worse outcomes. About half of those patients experienced transformation, so they have diffuse large B-cell lymphoma, and they’re getting CAR T-cells. In the end, only 10% of patients with follicular lymphoma are relapsed or refractory and should consider getting Car T-cell therapy,” said Dr. Martin, who focused the rest of his presentation on the best options for treating patients with indolent R/R FL who did not have PoD-24.
He said these patients may be able to avoid the side effects of CAR T and perform well when treated with lenalidomide rituximab (R2) or bispecific antibodies. Data from the MAGNIFY trial of patients with R/R FL indicate that patients treated with R2 who did not experience relapse less than 24 months after starting treatment and were not heavily refractory to rituximab achieved a median PFS of over 4 years, with grade 3 or higher adverse events occurring in 5% of patients or less.
Treatment with bispecific antibodies, although inferior in performance to CAR T-cell therapy, may offer durable responses in some R/R CL patients without the risk of side effects associated with CAR T.
Mosunetuzumab, a bispecific antibody that is currently approved for follicular lymphoma, is designed with step-up dosing to reduce cytokine release syndrome and “achieved a complete response rate of 60% and a median PFS that looks like it’s probably about two years,” said Dr. Martin, noting that some patients continue to do well after the 3-year mark and speculated that “there will be some really long-term responders.”
In addition to the possibly durable nature of bispecific antibodies, they induce cytokine release syndrome at a much lower rate than CAR T, and most side effects are manageable in an outpatient setting, “usually just with Tylenol occasionally with a dose of steroids,” said Dr. Martin.
He contrasted this response with CAR T-cell therapy, which requires referral and travel to a specialized center for at least 1 month around the time of therapy.
Despite the differences of opinion between the presenters about whether CAR T should be used more or less in R/R FL, essentially the two specialists were making recommendations for different patient groups.
Dr. Jacobson observed that “Dr. Martin is looking at the 80% of people who do really well with follicular lymphoma." Those are the people who don’t require a third line of therapy. They are the people who don’t have PoD-24. I’m looking at the 20% of people who either do require a third line of therapy or who do have PoD-24, and we’re not treating nearly enough of those patients with follicular lymphoma.
“We’re actually arguing about treatment strategies for different populations of patients. And I think ultimately, we agree more than we disagree in the end,” she concluded.
The notion that CAR T, chemotherapy, and bispecific antibodies all have a place in treating R/R FL patients is supported by Charalambos (Babis) Andreadis, MD, hematologist at the University of California San Francisco’s Helen Diller Family Comprehensive Care Center. “If I had a patient with follicular who relapsed 24 months or later after primary therapy and had active disease that needed treatment, most providers would do a lenalidomide-based or chemo-based regimen. Down the line either bispecific or CAR T would be appropriate in third line,” said Dr. Andreadis.
However, he noted,“for someone who is an early progressor, I would similarly not be able to use either [chemotherapy or bispecific antibodies] in second line [therapy] but would definitely think that early CART would be a good option to consider given the longevity of the observed responses so far.”
Dr. Martin disclosed ties with AbbVie, AstraZeneca, BeiGene, Daiichi Sankyo, Epizyme, Genentech, Janssen, Merck, and PeproMene. Dr. Jacobson reported relationships with AbbVie, Abintus Bio, ADC Therapeutics, Appia Bio, AstraZeneca, BMS/Celgene, Caribou Bio, Daiichi Sankyo, ImmPACT Bio, Ipsen, Janssen, Kite/Gilead, MorphoSys, Novartis, Sana, Synthekine, Kite/Gilead, and Pfizer. Dr. Andreadis had no disclosures.
ALL: Which Life-Saving Tx Is Best?
The comparative benefits and limitations of these two treatments for r/r ALL were a topic for discussion at the Great Debates & Updates Hematological Malignancies conference, held April 5-6 in New York City.
“Every single patient with ALL should benefit from bispecific antibodies before getting CAR-T cells, and I want to make the case that everybody should get CAR T as well. But they should get blinatumomab before they get CAR T,” said Elias Jabbour, MD, of the MD Anderson Cancer Center at The University of Texas in Houston, whose presentation focused on the merits of bispecific antibodies.
His argument was based on data indicating that patients have better chances of long-term remission with the use of bispecific antibodies when they are administered in an earlier round of salvage treatment — and the fact that patients who are not cured with these drugs can still achieve a lower disease burden and perform better on CAR T-cell therapy than those who don’t receive the drugs.
“When blinatumomab is used as a consolidation during the first salvage treatment and spaces out transplantation, 3-year overall survival increases in the relapse setting, deepening responses and reducing the rate of VOD (veno-occlusive disease). The safety and efficacy of CAR T depends on a disease burden. If you have a minimal residual disease (MRD), you have a safer outcome and a better outcome in the long run,” Dr. Jabbour explained.
This point of view is supported by data from the treatment of patients r/r ALL with low intensity chemotherapy + inotuzumab ozogamicin (Besponsa; Pfizer) +/- blinatumomab (Blincyto; Amgen), knows as Mini-HCVD + Ino +/-Blina. Trial members achieved a median overall survival (OS) rate of 17 months, a 3-year survival rate of 42%, and an overall MRD negativity rate of 85%.
Dr. Jabbour noted that blinatumomab has its limitations. Generally, this treatment is administered intravenously every few weeks and can be cumbersome for patients who must travel to an infusion center. However, data from a phase 1b trial of single agent subcutaneous blinatumomab for advanced ALL has demonstrated that this formulation can be effective and can lead to MRD negativity, possibly paving the way for easier administration of the drug.
Aditi Shastri, MD, a leukemia specialist at New York’s Montefiore Medical Center who attended the debate, agreed that the data presented did support Dr. Jabbour’s contention that subcutaneous blinatumomab could make treatment available to even more people with r/r ALL. “It’s easier to administer than the blina pump and could act as a bridge to curative therapies like AlloHSCT,” she said.
Jae Park, MD, a leukemia and cellular therapy specialist at Memorial Sloan Kettering Cancer Center in New York City, argued that CAR T is the most potent therapy for r/r ALL. Dr. Park agreed that inotuzumab and blinatumomab have yielded tremendous progress in the treatment of patients with r/r ALL, but he noted that bispecific antibodies lack some of the advantages of CAR T.
Dr. Park said that the biggest difference between the two therapies is that CAR T requires but a single infusion of a living drug. Patients do need to stay close to treatment centers to receive treatment for toxicities, but after about 28 days, they can go home and be monitored from a distance. Furthermore, patients may start by receiving 1 million T-cells, but those cells exponentially expand 100,000- to 1,000,000-fold, meaning that the T-cells to treat cancer have the potential to persist for months and sometimes years.
Furthermore, results from ZUMA-3 Trial of the CD19-targeting CAR T-Cell therapy brexucabtagene autoleucel (Tecartus; Kite Pharma) suggest that CAR T outperforms Mini-HCVD + Ino +/-Blina in patients with r/r ALL. Participants in the trial showed an overall response rate around 80%, a 71% complete response rate, and a median OS of 25.4 months. Patients who achieved a complete response had an even better median OS of 47 months. Although this was not a head-to-head trial with Mini-HCVD + Ino +/-Blina, if the plateau of long-term survivors continues, “this drug could be set apart from treatment with monoclonal antibodies,” Dr. Park said.
However, brexucabtagene autoleucel is not a cure or even an option for all patients. Some patients are too frail to get the drug, and they risk experiencing cytokine release syndrome (CRS). Data from the FELIX study suggest that the CAR T-cell treatment Obe-cel could offer a safety profile that reduces the risk of serious side effects while remaining effective at treating r/r ALL. Obe-cel showed efficacy very similar to that of brexucabtagene autoleucel, with a 70%-80% response rate, and only 2% of patients experienced CRS.
Dr. Park noted that the next frontier in CAR T-cell therapy is figuring out which patients will respond well to CAR T and which are going to need more treatment after CAR T. However, he noted that evidence suggests patients with low MRD are likely to do best on CAR T and that bispecific antibodies can help patients get to what might be the best chance at a cure for r/r ALL, namely CAR-T.
The moderator of the debate, Jessica Altman, MD, professor of medicine, hematology oncology division, Feinberg School of Medicine at Northwestern University in Chicago, noted: “My take home is that antibody therapy and CAR-T will be sequenced and used together.” She noted that blinatumomab is moving into the front line of therapy, as in the E1910 trials, and how this treatment allows for study and use of CAR T earlier in the care of patients “when there may be less toxicity and higher response.”
Jabbour concluded on a similar note, adding that the “cure for this disease will happen in our lifetime. We will shorten therapy by doing immunotherapy upfront followed by CAR T consolidation and no more transplantation. I don’t think antibodies immunotherapies or CAR T need be competitive, they can be used in a complimentary fashion.”
Jabbour reported no financial disclosures. Park disclosed ties with Allogene, Artiva Biotherapeutics, Amgen, Affyimmune, BeBiopharma, Beigene, Bright Pharmaceuticals, Autolus, Caribou Biosciences, Galapagos, Kite, Medpace, Minerva Biotechnologies, Pfizer, Servier, Sobi, and Takeda. Neither Altman nor Shastri reported any disclosures.
The comparative benefits and limitations of these two treatments for r/r ALL were a topic for discussion at the Great Debates & Updates Hematological Malignancies conference, held April 5-6 in New York City.
“Every single patient with ALL should benefit from bispecific antibodies before getting CAR-T cells, and I want to make the case that everybody should get CAR T as well. But they should get blinatumomab before they get CAR T,” said Elias Jabbour, MD, of the MD Anderson Cancer Center at The University of Texas in Houston, whose presentation focused on the merits of bispecific antibodies.
His argument was based on data indicating that patients have better chances of long-term remission with the use of bispecific antibodies when they are administered in an earlier round of salvage treatment — and the fact that patients who are not cured with these drugs can still achieve a lower disease burden and perform better on CAR T-cell therapy than those who don’t receive the drugs.
“When blinatumomab is used as a consolidation during the first salvage treatment and spaces out transplantation, 3-year overall survival increases in the relapse setting, deepening responses and reducing the rate of VOD (veno-occlusive disease). The safety and efficacy of CAR T depends on a disease burden. If you have a minimal residual disease (MRD), you have a safer outcome and a better outcome in the long run,” Dr. Jabbour explained.
This point of view is supported by data from the treatment of patients r/r ALL with low intensity chemotherapy + inotuzumab ozogamicin (Besponsa; Pfizer) +/- blinatumomab (Blincyto; Amgen), knows as Mini-HCVD + Ino +/-Blina. Trial members achieved a median overall survival (OS) rate of 17 months, a 3-year survival rate of 42%, and an overall MRD negativity rate of 85%.
Dr. Jabbour noted that blinatumomab has its limitations. Generally, this treatment is administered intravenously every few weeks and can be cumbersome for patients who must travel to an infusion center. However, data from a phase 1b trial of single agent subcutaneous blinatumomab for advanced ALL has demonstrated that this formulation can be effective and can lead to MRD negativity, possibly paving the way for easier administration of the drug.
Aditi Shastri, MD, a leukemia specialist at New York’s Montefiore Medical Center who attended the debate, agreed that the data presented did support Dr. Jabbour’s contention that subcutaneous blinatumomab could make treatment available to even more people with r/r ALL. “It’s easier to administer than the blina pump and could act as a bridge to curative therapies like AlloHSCT,” she said.
Jae Park, MD, a leukemia and cellular therapy specialist at Memorial Sloan Kettering Cancer Center in New York City, argued that CAR T is the most potent therapy for r/r ALL. Dr. Park agreed that inotuzumab and blinatumomab have yielded tremendous progress in the treatment of patients with r/r ALL, but he noted that bispecific antibodies lack some of the advantages of CAR T.
Dr. Park said that the biggest difference between the two therapies is that CAR T requires but a single infusion of a living drug. Patients do need to stay close to treatment centers to receive treatment for toxicities, but after about 28 days, they can go home and be monitored from a distance. Furthermore, patients may start by receiving 1 million T-cells, but those cells exponentially expand 100,000- to 1,000,000-fold, meaning that the T-cells to treat cancer have the potential to persist for months and sometimes years.
Furthermore, results from ZUMA-3 Trial of the CD19-targeting CAR T-Cell therapy brexucabtagene autoleucel (Tecartus; Kite Pharma) suggest that CAR T outperforms Mini-HCVD + Ino +/-Blina in patients with r/r ALL. Participants in the trial showed an overall response rate around 80%, a 71% complete response rate, and a median OS of 25.4 months. Patients who achieved a complete response had an even better median OS of 47 months. Although this was not a head-to-head trial with Mini-HCVD + Ino +/-Blina, if the plateau of long-term survivors continues, “this drug could be set apart from treatment with monoclonal antibodies,” Dr. Park said.
However, brexucabtagene autoleucel is not a cure or even an option for all patients. Some patients are too frail to get the drug, and they risk experiencing cytokine release syndrome (CRS). Data from the FELIX study suggest that the CAR T-cell treatment Obe-cel could offer a safety profile that reduces the risk of serious side effects while remaining effective at treating r/r ALL. Obe-cel showed efficacy very similar to that of brexucabtagene autoleucel, with a 70%-80% response rate, and only 2% of patients experienced CRS.
Dr. Park noted that the next frontier in CAR T-cell therapy is figuring out which patients will respond well to CAR T and which are going to need more treatment after CAR T. However, he noted that evidence suggests patients with low MRD are likely to do best on CAR T and that bispecific antibodies can help patients get to what might be the best chance at a cure for r/r ALL, namely CAR-T.
The moderator of the debate, Jessica Altman, MD, professor of medicine, hematology oncology division, Feinberg School of Medicine at Northwestern University in Chicago, noted: “My take home is that antibody therapy and CAR-T will be sequenced and used together.” She noted that blinatumomab is moving into the front line of therapy, as in the E1910 trials, and how this treatment allows for study and use of CAR T earlier in the care of patients “when there may be less toxicity and higher response.”
Jabbour concluded on a similar note, adding that the “cure for this disease will happen in our lifetime. We will shorten therapy by doing immunotherapy upfront followed by CAR T consolidation and no more transplantation. I don’t think antibodies immunotherapies or CAR T need be competitive, they can be used in a complimentary fashion.”
Jabbour reported no financial disclosures. Park disclosed ties with Allogene, Artiva Biotherapeutics, Amgen, Affyimmune, BeBiopharma, Beigene, Bright Pharmaceuticals, Autolus, Caribou Biosciences, Galapagos, Kite, Medpace, Minerva Biotechnologies, Pfizer, Servier, Sobi, and Takeda. Neither Altman nor Shastri reported any disclosures.
The comparative benefits and limitations of these two treatments for r/r ALL were a topic for discussion at the Great Debates & Updates Hematological Malignancies conference, held April 5-6 in New York City.
“Every single patient with ALL should benefit from bispecific antibodies before getting CAR-T cells, and I want to make the case that everybody should get CAR T as well. But they should get blinatumomab before they get CAR T,” said Elias Jabbour, MD, of the MD Anderson Cancer Center at The University of Texas in Houston, whose presentation focused on the merits of bispecific antibodies.
His argument was based on data indicating that patients have better chances of long-term remission with the use of bispecific antibodies when they are administered in an earlier round of salvage treatment — and the fact that patients who are not cured with these drugs can still achieve a lower disease burden and perform better on CAR T-cell therapy than those who don’t receive the drugs.
“When blinatumomab is used as a consolidation during the first salvage treatment and spaces out transplantation, 3-year overall survival increases in the relapse setting, deepening responses and reducing the rate of VOD (veno-occlusive disease). The safety and efficacy of CAR T depends on a disease burden. If you have a minimal residual disease (MRD), you have a safer outcome and a better outcome in the long run,” Dr. Jabbour explained.
This point of view is supported by data from the treatment of patients r/r ALL with low intensity chemotherapy + inotuzumab ozogamicin (Besponsa; Pfizer) +/- blinatumomab (Blincyto; Amgen), knows as Mini-HCVD + Ino +/-Blina. Trial members achieved a median overall survival (OS) rate of 17 months, a 3-year survival rate of 42%, and an overall MRD negativity rate of 85%.
Dr. Jabbour noted that blinatumomab has its limitations. Generally, this treatment is administered intravenously every few weeks and can be cumbersome for patients who must travel to an infusion center. However, data from a phase 1b trial of single agent subcutaneous blinatumomab for advanced ALL has demonstrated that this formulation can be effective and can lead to MRD negativity, possibly paving the way for easier administration of the drug.
Aditi Shastri, MD, a leukemia specialist at New York’s Montefiore Medical Center who attended the debate, agreed that the data presented did support Dr. Jabbour’s contention that subcutaneous blinatumomab could make treatment available to even more people with r/r ALL. “It’s easier to administer than the blina pump and could act as a bridge to curative therapies like AlloHSCT,” she said.
Jae Park, MD, a leukemia and cellular therapy specialist at Memorial Sloan Kettering Cancer Center in New York City, argued that CAR T is the most potent therapy for r/r ALL. Dr. Park agreed that inotuzumab and blinatumomab have yielded tremendous progress in the treatment of patients with r/r ALL, but he noted that bispecific antibodies lack some of the advantages of CAR T.
Dr. Park said that the biggest difference between the two therapies is that CAR T requires but a single infusion of a living drug. Patients do need to stay close to treatment centers to receive treatment for toxicities, but after about 28 days, they can go home and be monitored from a distance. Furthermore, patients may start by receiving 1 million T-cells, but those cells exponentially expand 100,000- to 1,000,000-fold, meaning that the T-cells to treat cancer have the potential to persist for months and sometimes years.
Furthermore, results from ZUMA-3 Trial of the CD19-targeting CAR T-Cell therapy brexucabtagene autoleucel (Tecartus; Kite Pharma) suggest that CAR T outperforms Mini-HCVD + Ino +/-Blina in patients with r/r ALL. Participants in the trial showed an overall response rate around 80%, a 71% complete response rate, and a median OS of 25.4 months. Patients who achieved a complete response had an even better median OS of 47 months. Although this was not a head-to-head trial with Mini-HCVD + Ino +/-Blina, if the plateau of long-term survivors continues, “this drug could be set apart from treatment with monoclonal antibodies,” Dr. Park said.
However, brexucabtagene autoleucel is not a cure or even an option for all patients. Some patients are too frail to get the drug, and they risk experiencing cytokine release syndrome (CRS). Data from the FELIX study suggest that the CAR T-cell treatment Obe-cel could offer a safety profile that reduces the risk of serious side effects while remaining effective at treating r/r ALL. Obe-cel showed efficacy very similar to that of brexucabtagene autoleucel, with a 70%-80% response rate, and only 2% of patients experienced CRS.
Dr. Park noted that the next frontier in CAR T-cell therapy is figuring out which patients will respond well to CAR T and which are going to need more treatment after CAR T. However, he noted that evidence suggests patients with low MRD are likely to do best on CAR T and that bispecific antibodies can help patients get to what might be the best chance at a cure for r/r ALL, namely CAR-T.
The moderator of the debate, Jessica Altman, MD, professor of medicine, hematology oncology division, Feinberg School of Medicine at Northwestern University in Chicago, noted: “My take home is that antibody therapy and CAR-T will be sequenced and used together.” She noted that blinatumomab is moving into the front line of therapy, as in the E1910 trials, and how this treatment allows for study and use of CAR T earlier in the care of patients “when there may be less toxicity and higher response.”
Jabbour concluded on a similar note, adding that the “cure for this disease will happen in our lifetime. We will shorten therapy by doing immunotherapy upfront followed by CAR T consolidation and no more transplantation. I don’t think antibodies immunotherapies or CAR T need be competitive, they can be used in a complimentary fashion.”
Jabbour reported no financial disclosures. Park disclosed ties with Allogene, Artiva Biotherapeutics, Amgen, Affyimmune, BeBiopharma, Beigene, Bright Pharmaceuticals, Autolus, Caribou Biosciences, Galapagos, Kite, Medpace, Minerva Biotechnologies, Pfizer, Servier, Sobi, and Takeda. Neither Altman nor Shastri reported any disclosures.
FROM GREAT DEBATES & UPDATES HEMATOLOGIC MALIGNANCIES
Magic Wand Initiative Empowers Dermatologists to Innovate
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
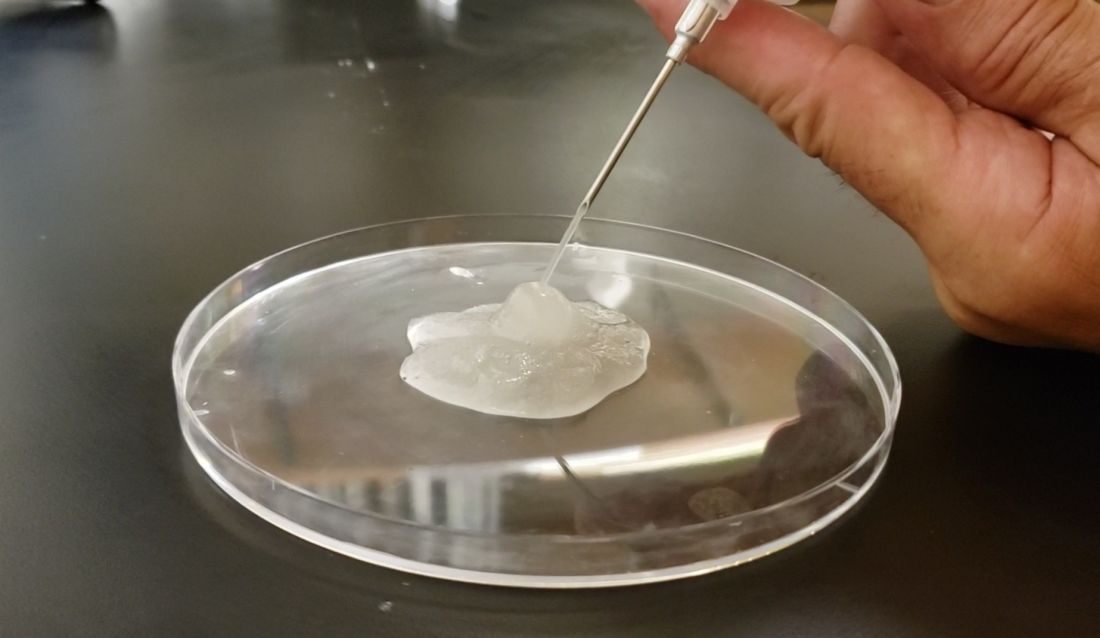
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
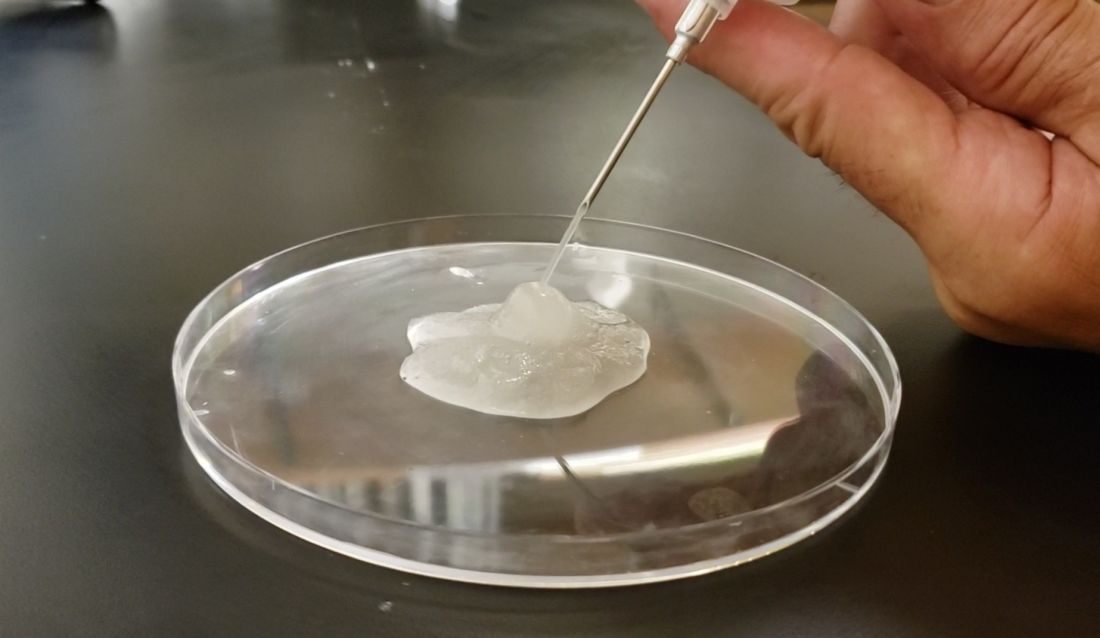
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
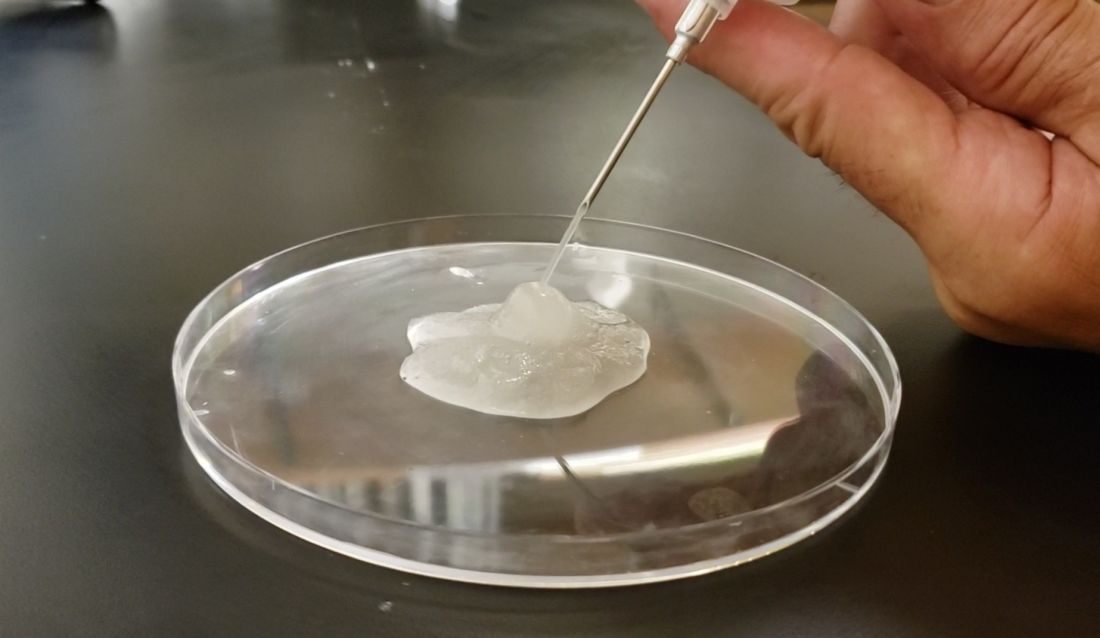
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
What’s new in acne treatment?
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
DLBCL treatment options: CAR T outperforms ASCT
NEW YORK – according to evidence presented at the 2023 Lymphoma, Leukemia, and Myeloma Congress.
DLBCL is characterized by the National Institutes of Health as an aggressive malignancy and the most common lymphoma. Research presented at the conference indicated that 60%70% of patients were cured with six to eight cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP).
“In the past, if a relapsed of refractory DLBCL patient couldn’t get a transplant, they were likely headed for palliative care. CAR T-cell therapy is no longer experimental. Not only can we offer it to patients who are ineligible for transplant (and manage the side effects), the treatment has proven to offer better overall survival and cure rates, even in patients who eligible for ASCT,” said presenter Jason Westin, MD, director of the lymphoma clinical research program at the University of Texas MD Anderson Cancer Center, Houston.
The ZUMA-7 phase 3trial among patients with early r/r DLBCL demonstrated the superiority of CAR T-cell therapy with the agent, axicabtagene ciloleucel (YESCARTA, Kita Pharma) versus standard of care (chemoimmunotherapy followed by high-dose chemotherapy and ASCT). Those in the axicabtagene ciloleucel (axi-cel) group had a median progression free survival (PFS) of 14.7 months and an estimated 4-year overall survival (OS) rate of 54.6% compared to 3.7 months and 46% in the control group.
Patients treated with axi-cel experienced a higher rate of adverse events (AE) grade 3 of higher, compared with the ACST group (91% vs. 83%) Furthermore, patients who received axi-cel had cytokine release syndrome (6%) and neurologic events in (21%) grade 3 or higher, compared with 0% and less than 1% in the ASCT group.
At the conference, Dr. Westin’s copanelist Jennifer Amengual, MD, of Columbia University Irving Medical Center, New York, interpreted the data on adverse events (AEs) from ZUMA-7 to mean that if a patient is especially susceptible to CAR T side effects, then ASCT could be preferred. She also outlined a second strategy that shows promise when a patient has either failed CAR T and ASCT or whose frailty demands an approach that avoids AEs.
Dr. Amengual cited a study in which patients with r/r DLBCL were treated with the bispecific antibody glofitamab (Columvi/Roche), which induced a complete response in 39% of patients at a median follow-up of 12.6 months and a 12-month PFS rate of 37%. Those treated with the agent experienced cytokine release syndrome and neurologic events grade 3 or higher, at a rate of 4% and 3% respectively.
“Efforts to make off-the-shelf CAR T therapy are ongoing. With some fine-tuning the PFS and OS with bispecific antibodies will likely approach or exceed both CAR T and ACST. The fact that they could come right off the shelf, rather than having to be tailor made for each patient, gives them a huge advantage in terms of cost and availability, while maintaining what appears to be an excellent safety profile” said Morton Colman, MD, professor of medicine at Weill Cornell Medicine, New York, and chair of the 2023 Lymphoma, Leukemia, and Myeloma Congress.
Dr. Amengual disclosed ties with Astra Zeneca and Incyte. Dr. Westin reported ties with Abbie, ADC therapeutics, AstraZeneca, Bristol-Myers Squibb, Genentech, GenMad, Hanssen, Kite/Gilead, Morphosys/Incyte, Novartis, Nurix, Regeneron, and SeaGen. Dr. Coleman had no disclosures.
NEW YORK – according to evidence presented at the 2023 Lymphoma, Leukemia, and Myeloma Congress.
DLBCL is characterized by the National Institutes of Health as an aggressive malignancy and the most common lymphoma. Research presented at the conference indicated that 60%70% of patients were cured with six to eight cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP).
“In the past, if a relapsed of refractory DLBCL patient couldn’t get a transplant, they were likely headed for palliative care. CAR T-cell therapy is no longer experimental. Not only can we offer it to patients who are ineligible for transplant (and manage the side effects), the treatment has proven to offer better overall survival and cure rates, even in patients who eligible for ASCT,” said presenter Jason Westin, MD, director of the lymphoma clinical research program at the University of Texas MD Anderson Cancer Center, Houston.
The ZUMA-7 phase 3trial among patients with early r/r DLBCL demonstrated the superiority of CAR T-cell therapy with the agent, axicabtagene ciloleucel (YESCARTA, Kita Pharma) versus standard of care (chemoimmunotherapy followed by high-dose chemotherapy and ASCT). Those in the axicabtagene ciloleucel (axi-cel) group had a median progression free survival (PFS) of 14.7 months and an estimated 4-year overall survival (OS) rate of 54.6% compared to 3.7 months and 46% in the control group.
Patients treated with axi-cel experienced a higher rate of adverse events (AE) grade 3 of higher, compared with the ACST group (91% vs. 83%) Furthermore, patients who received axi-cel had cytokine release syndrome (6%) and neurologic events in (21%) grade 3 or higher, compared with 0% and less than 1% in the ASCT group.
At the conference, Dr. Westin’s copanelist Jennifer Amengual, MD, of Columbia University Irving Medical Center, New York, interpreted the data on adverse events (AEs) from ZUMA-7 to mean that if a patient is especially susceptible to CAR T side effects, then ASCT could be preferred. She also outlined a second strategy that shows promise when a patient has either failed CAR T and ASCT or whose frailty demands an approach that avoids AEs.
Dr. Amengual cited a study in which patients with r/r DLBCL were treated with the bispecific antibody glofitamab (Columvi/Roche), which induced a complete response in 39% of patients at a median follow-up of 12.6 months and a 12-month PFS rate of 37%. Those treated with the agent experienced cytokine release syndrome and neurologic events grade 3 or higher, at a rate of 4% and 3% respectively.
“Efforts to make off-the-shelf CAR T therapy are ongoing. With some fine-tuning the PFS and OS with bispecific antibodies will likely approach or exceed both CAR T and ACST. The fact that they could come right off the shelf, rather than having to be tailor made for each patient, gives them a huge advantage in terms of cost and availability, while maintaining what appears to be an excellent safety profile” said Morton Colman, MD, professor of medicine at Weill Cornell Medicine, New York, and chair of the 2023 Lymphoma, Leukemia, and Myeloma Congress.
Dr. Amengual disclosed ties with Astra Zeneca and Incyte. Dr. Westin reported ties with Abbie, ADC therapeutics, AstraZeneca, Bristol-Myers Squibb, Genentech, GenMad, Hanssen, Kite/Gilead, Morphosys/Incyte, Novartis, Nurix, Regeneron, and SeaGen. Dr. Coleman had no disclosures.
NEW YORK – according to evidence presented at the 2023 Lymphoma, Leukemia, and Myeloma Congress.
DLBCL is characterized by the National Institutes of Health as an aggressive malignancy and the most common lymphoma. Research presented at the conference indicated that 60%70% of patients were cured with six to eight cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP).
“In the past, if a relapsed of refractory DLBCL patient couldn’t get a transplant, they were likely headed for palliative care. CAR T-cell therapy is no longer experimental. Not only can we offer it to patients who are ineligible for transplant (and manage the side effects), the treatment has proven to offer better overall survival and cure rates, even in patients who eligible for ASCT,” said presenter Jason Westin, MD, director of the lymphoma clinical research program at the University of Texas MD Anderson Cancer Center, Houston.
The ZUMA-7 phase 3trial among patients with early r/r DLBCL demonstrated the superiority of CAR T-cell therapy with the agent, axicabtagene ciloleucel (YESCARTA, Kita Pharma) versus standard of care (chemoimmunotherapy followed by high-dose chemotherapy and ASCT). Those in the axicabtagene ciloleucel (axi-cel) group had a median progression free survival (PFS) of 14.7 months and an estimated 4-year overall survival (OS) rate of 54.6% compared to 3.7 months and 46% in the control group.
Patients treated with axi-cel experienced a higher rate of adverse events (AE) grade 3 of higher, compared with the ACST group (91% vs. 83%) Furthermore, patients who received axi-cel had cytokine release syndrome (6%) and neurologic events in (21%) grade 3 or higher, compared with 0% and less than 1% in the ASCT group.
At the conference, Dr. Westin’s copanelist Jennifer Amengual, MD, of Columbia University Irving Medical Center, New York, interpreted the data on adverse events (AEs) from ZUMA-7 to mean that if a patient is especially susceptible to CAR T side effects, then ASCT could be preferred. She also outlined a second strategy that shows promise when a patient has either failed CAR T and ASCT or whose frailty demands an approach that avoids AEs.
Dr. Amengual cited a study in which patients with r/r DLBCL were treated with the bispecific antibody glofitamab (Columvi/Roche), which induced a complete response in 39% of patients at a median follow-up of 12.6 months and a 12-month PFS rate of 37%. Those treated with the agent experienced cytokine release syndrome and neurologic events grade 3 or higher, at a rate of 4% and 3% respectively.
“Efforts to make off-the-shelf CAR T therapy are ongoing. With some fine-tuning the PFS and OS with bispecific antibodies will likely approach or exceed both CAR T and ACST. The fact that they could come right off the shelf, rather than having to be tailor made for each patient, gives them a huge advantage in terms of cost and availability, while maintaining what appears to be an excellent safety profile” said Morton Colman, MD, professor of medicine at Weill Cornell Medicine, New York, and chair of the 2023 Lymphoma, Leukemia, and Myeloma Congress.
Dr. Amengual disclosed ties with Astra Zeneca and Incyte. Dr. Westin reported ties with Abbie, ADC therapeutics, AstraZeneca, Bristol-Myers Squibb, Genentech, GenMad, Hanssen, Kite/Gilead, Morphosys/Incyte, Novartis, Nurix, Regeneron, and SeaGen. Dr. Coleman had no disclosures.
AT LLM CONGRESS 2023
Rare lymphomas: Desperately seeking new txs
“Over the past 5 years, researchers have gotten a clearer picture of the different subtypes of peripheral T-cell lymphomas, and with this knowledge we are trying to identify potential targets of new treatments. Despite some progress, the need for these new treatments is still acute, due to the disease’s many subtypes and the difficulty of enrolling sufficient numbers of patients in clinical trials,” said Julie M. Vose, MD, MBA, of the University of Nebraska Medical Center, Omaha, speaking at the Lymphoma, Leukemia and Myeloma Congress 2023, in New York. Before her presentation at this year’s conference, Dr. Vose was awarded the SASS-ARENA Foundation’s John Ultmann Award for Major Contributions to Lymphoma Research.
Dr. Vose noted that only one subtype of PTCL, ALK+ ALCL, responds well to frontline treatment with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone). Patients with the ALK+ ALCL signature treated with CHOP have a 5-year overall survival (OS) rate of 70%-90%, but this group only makes up about 6% of PTCL cases in North America, she added.
One of the most promising breakthroughs in treatment has been the addition of the anti-CD30 antibody-drug conjugate brentuximab vedotin (BV) to chemotherapy with CHP (cyclophosphamide, doxorubicin, prednisone), Dr. Vose said. Results from the ECHELON-2 trial indicate that CD30+ PTCL patients have improved performance with R-CHP, compared with CHOP; 5-year progression free survival (PFS) rates were 51.4% with R+CHP versus 43.0% with CHOP, and 5-year overall survival rates were 70.1% versus 61.0%, respectively.
“ALCL is one of the most prevalent PTCL subtypes and accounts for about 24% of all PTCL; the current standard-of-care for induction treatment in these patients is BV-CHP,” said Jia Ruan, MD, PhD, of Weill Cornell Medicine in New York. Dr. Ruan explained the limitation of adding BV-CHP, saying “We don’t have as effective biological targeted therapies in other subtypes of T-cell lymphoma, such as PTCL NOS [not-other specified] or angioimmunoblastic T-cell lymphoma.”
There is evidence that autologous stem cell transplant (ACST) can increase PFS and OS in newly diagnosed patients with angioimmunoblastic T-cell lymphoma (AITL), but not in patients with other types of newly diagnosed PTCL. The estimated 2-year OS and PFS for patients with AITL who received ASCT + chemotherapy were 93.3% and 68.8 respectively versus 52.9% and 41.2 in the non-ASCT group. This news is promising, yet Dr. Vose presented statistics indicating that AITL PTCL has been estimated to account for less than 19% of PTCL cases.
Despite the improvements in PFS and OS in a few subtypes for frontline PTCL, 60% of patients with non-ALCL PTCL will relapse, and relapsed/ refractory (R/R) PTCL patients have a median PFS of 9.6 months. Several studies have shown some promise for improving outcomes in R/R PTCL patients, such as the phase-II PRIMO study of duvelisib (a dual PI3K-delta,gamma inhibitor), in which there was an overall response rate of 50% and a complete response rate of 32%. Despite these modest gains, the prognosis for most PTCL patients remains poor. Dr. Vose concluded her presentation by reiterating the need for new agents and for further research. She emphasized that studies will need to be collaborative and international to enroll sufficient patients.
Dr Ruan drew a similar conclusion, noting “We need to increase clinical, translational and basic research on a collaborative scale, so that we can advance bench-to-bedside discovery and bring new treatment to patients quickly.”
Dr. Vose disclosed research funding from Epizyme, GenMab, Kite, Novartis, and Lilly. Dr. Ruan disclosed clinical research trial support from BMS and Daiichi Sankyo.
“Over the past 5 years, researchers have gotten a clearer picture of the different subtypes of peripheral T-cell lymphomas, and with this knowledge we are trying to identify potential targets of new treatments. Despite some progress, the need for these new treatments is still acute, due to the disease’s many subtypes and the difficulty of enrolling sufficient numbers of patients in clinical trials,” said Julie M. Vose, MD, MBA, of the University of Nebraska Medical Center, Omaha, speaking at the Lymphoma, Leukemia and Myeloma Congress 2023, in New York. Before her presentation at this year’s conference, Dr. Vose was awarded the SASS-ARENA Foundation’s John Ultmann Award for Major Contributions to Lymphoma Research.
Dr. Vose noted that only one subtype of PTCL, ALK+ ALCL, responds well to frontline treatment with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone). Patients with the ALK+ ALCL signature treated with CHOP have a 5-year overall survival (OS) rate of 70%-90%, but this group only makes up about 6% of PTCL cases in North America, she added.
One of the most promising breakthroughs in treatment has been the addition of the anti-CD30 antibody-drug conjugate brentuximab vedotin (BV) to chemotherapy with CHP (cyclophosphamide, doxorubicin, prednisone), Dr. Vose said. Results from the ECHELON-2 trial indicate that CD30+ PTCL patients have improved performance with R-CHP, compared with CHOP; 5-year progression free survival (PFS) rates were 51.4% with R+CHP versus 43.0% with CHOP, and 5-year overall survival rates were 70.1% versus 61.0%, respectively.
“ALCL is one of the most prevalent PTCL subtypes and accounts for about 24% of all PTCL; the current standard-of-care for induction treatment in these patients is BV-CHP,” said Jia Ruan, MD, PhD, of Weill Cornell Medicine in New York. Dr. Ruan explained the limitation of adding BV-CHP, saying “We don’t have as effective biological targeted therapies in other subtypes of T-cell lymphoma, such as PTCL NOS [not-other specified] or angioimmunoblastic T-cell lymphoma.”
There is evidence that autologous stem cell transplant (ACST) can increase PFS and OS in newly diagnosed patients with angioimmunoblastic T-cell lymphoma (AITL), but not in patients with other types of newly diagnosed PTCL. The estimated 2-year OS and PFS for patients with AITL who received ASCT + chemotherapy were 93.3% and 68.8 respectively versus 52.9% and 41.2 in the non-ASCT group. This news is promising, yet Dr. Vose presented statistics indicating that AITL PTCL has been estimated to account for less than 19% of PTCL cases.
Despite the improvements in PFS and OS in a few subtypes for frontline PTCL, 60% of patients with non-ALCL PTCL will relapse, and relapsed/ refractory (R/R) PTCL patients have a median PFS of 9.6 months. Several studies have shown some promise for improving outcomes in R/R PTCL patients, such as the phase-II PRIMO study of duvelisib (a dual PI3K-delta,gamma inhibitor), in which there was an overall response rate of 50% and a complete response rate of 32%. Despite these modest gains, the prognosis for most PTCL patients remains poor. Dr. Vose concluded her presentation by reiterating the need for new agents and for further research. She emphasized that studies will need to be collaborative and international to enroll sufficient patients.
Dr Ruan drew a similar conclusion, noting “We need to increase clinical, translational and basic research on a collaborative scale, so that we can advance bench-to-bedside discovery and bring new treatment to patients quickly.”
Dr. Vose disclosed research funding from Epizyme, GenMab, Kite, Novartis, and Lilly. Dr. Ruan disclosed clinical research trial support from BMS and Daiichi Sankyo.
“Over the past 5 years, researchers have gotten a clearer picture of the different subtypes of peripheral T-cell lymphomas, and with this knowledge we are trying to identify potential targets of new treatments. Despite some progress, the need for these new treatments is still acute, due to the disease’s many subtypes and the difficulty of enrolling sufficient numbers of patients in clinical trials,” said Julie M. Vose, MD, MBA, of the University of Nebraska Medical Center, Omaha, speaking at the Lymphoma, Leukemia and Myeloma Congress 2023, in New York. Before her presentation at this year’s conference, Dr. Vose was awarded the SASS-ARENA Foundation’s John Ultmann Award for Major Contributions to Lymphoma Research.
Dr. Vose noted that only one subtype of PTCL, ALK+ ALCL, responds well to frontline treatment with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone). Patients with the ALK+ ALCL signature treated with CHOP have a 5-year overall survival (OS) rate of 70%-90%, but this group only makes up about 6% of PTCL cases in North America, she added.
One of the most promising breakthroughs in treatment has been the addition of the anti-CD30 antibody-drug conjugate brentuximab vedotin (BV) to chemotherapy with CHP (cyclophosphamide, doxorubicin, prednisone), Dr. Vose said. Results from the ECHELON-2 trial indicate that CD30+ PTCL patients have improved performance with R-CHP, compared with CHOP; 5-year progression free survival (PFS) rates were 51.4% with R+CHP versus 43.0% with CHOP, and 5-year overall survival rates were 70.1% versus 61.0%, respectively.
“ALCL is one of the most prevalent PTCL subtypes and accounts for about 24% of all PTCL; the current standard-of-care for induction treatment in these patients is BV-CHP,” said Jia Ruan, MD, PhD, of Weill Cornell Medicine in New York. Dr. Ruan explained the limitation of adding BV-CHP, saying “We don’t have as effective biological targeted therapies in other subtypes of T-cell lymphoma, such as PTCL NOS [not-other specified] or angioimmunoblastic T-cell lymphoma.”
There is evidence that autologous stem cell transplant (ACST) can increase PFS and OS in newly diagnosed patients with angioimmunoblastic T-cell lymphoma (AITL), but not in patients with other types of newly diagnosed PTCL. The estimated 2-year OS and PFS for patients with AITL who received ASCT + chemotherapy were 93.3% and 68.8 respectively versus 52.9% and 41.2 in the non-ASCT group. This news is promising, yet Dr. Vose presented statistics indicating that AITL PTCL has been estimated to account for less than 19% of PTCL cases.
Despite the improvements in PFS and OS in a few subtypes for frontline PTCL, 60% of patients with non-ALCL PTCL will relapse, and relapsed/ refractory (R/R) PTCL patients have a median PFS of 9.6 months. Several studies have shown some promise for improving outcomes in R/R PTCL patients, such as the phase-II PRIMO study of duvelisib (a dual PI3K-delta,gamma inhibitor), in which there was an overall response rate of 50% and a complete response rate of 32%. Despite these modest gains, the prognosis for most PTCL patients remains poor. Dr. Vose concluded her presentation by reiterating the need for new agents and for further research. She emphasized that studies will need to be collaborative and international to enroll sufficient patients.
Dr Ruan drew a similar conclusion, noting “We need to increase clinical, translational and basic research on a collaborative scale, so that we can advance bench-to-bedside discovery and bring new treatment to patients quickly.”
Dr. Vose disclosed research funding from Epizyme, GenMab, Kite, Novartis, and Lilly. Dr. Ruan disclosed clinical research trial support from BMS and Daiichi Sankyo.
AT LLM CONGRESS 2023
Frontline myeloma treatments: ASCT vs. CAR T
“In an otherwise healthy treatment-naive patient with multiple myeloma, to ensure the best chances of overall survival, I would always recommend standard of care consolidation therapy of chemotherapy + ASCT,” said Sergio Giralt, MD, of New York’s Memorial Sloan Kettering Cancer Center, debating the merits of ASCT versus CAR T as consolidation therapy at the Lymphoma, Leukemia & Myeloma (LLM) Congress 2023 in New York.
Final results from the phase II GRIFFIN trial highlight the benchmarks that CAR T-cell therapy would need to reach to achieve equivalence with ASCT. At a 4-year follow-up, newly diagnosed MM patients who received daratumumab, lenalidomide, bortezomib, and dexamethasone (D-RVd) followed by ASCT + D-RVd consolidation, and daratumumab maintenance, had a progression-free survival (PFS) rate of 87.3%, 92.7% overall survival (OS) rate, and 50% achieved minimal residual disease negativity.
Dr. Adriana Rossi, MD, assistant professor of medicine, Icahn School of Medicine at Mount Sinai, New York, cited a convergence of evidence suggesting that CAR T could achieve impressive results as a consolidation therapy in fit patients with MM, including: CARTITUDE 1 and CARTITUDE 4, which studied CAR T in RR MM patients. However, due to the fact that no head-to-head study of CAR T vs. ASCT as consolidation therapy in otherwise healthy MM patients exists, “There is not enough long-term data to support the equivalence CAR T with ASCT,” Dr. Giralt concluded.
Dr. Rossi further advocated for considering CAR T as a consolidation treatment because of the risks of secondary malignancies associated with ACST maintenance regimens.
Dr. Giralt rebutted this argument by citing data about averse events (AE) in studies of CAR-T therapies in RR MM patients like KarMMa-2, in which grade 3-4 neutropenia, anemia, and thrombocytopenia occurred in 94.6%, 45.9%, and 37.8% of patients respectively. Furthermore, 2 of 37 patients in KarMMA died (1 pneumonia, 1 pseudomonal sepsis), while rates of death from AEs related to ASCT occur in less than 1% of patients, according to Dr. Giralt.
Beyond a dearth of evidence thus far about the long term PFS, OS, and safety profile superiority of CAR-T therapies, compared with ASCT in treatment-naive MM patients, Dr. Giralt also noted the facts that CAR T-cell therapies are expensive and require manufacturing infrastructure also demonstrate that they cannot be easily adopted everywhere, even as a third-line therapy.
“In many places like Morocco, where I practice, we do not have access to CAR-T therapies,” said Sadia Zafad, MD, of the Clinique Al Madina Hematology and Oncology Center in Casablanca, Morocco. Dr. Zafad attended the debate.
A lack of access to CAR T is also a problem in the United States, where wait times for the therapy can stretch up to 6 months, getting insurance approval is challenging, and many patients simply don’t live near a center where CAR T-cell therapy is available. Citing all these factors, Dr. Giralt concluded: “Even if CAR T can be shown to have the same results as transplant, it is much more resource-intensive than transplant, and insurers are going to start saying there’s no necessary benefit. We have yet to use value as a primary end point, but as cancer care gets more and more expensive, that’s going to come up more, for CAR T and other novel therapies.”
Dr. Giralt reported relationships with Actinuum, Amgen, BMS, Celgene, Crisper, J&J, Jazz, Kite, Miltenyi, Novartis, Sanofi, and Takeda. Dr. Rossi disclosed ties with Adaptive, BMS, Celgene, JNJ, Sanofi & Genzyme. Dr. Zafad reported no disclosures.
“In an otherwise healthy treatment-naive patient with multiple myeloma, to ensure the best chances of overall survival, I would always recommend standard of care consolidation therapy of chemotherapy + ASCT,” said Sergio Giralt, MD, of New York’s Memorial Sloan Kettering Cancer Center, debating the merits of ASCT versus CAR T as consolidation therapy at the Lymphoma, Leukemia & Myeloma (LLM) Congress 2023 in New York.
Final results from the phase II GRIFFIN trial highlight the benchmarks that CAR T-cell therapy would need to reach to achieve equivalence with ASCT. At a 4-year follow-up, newly diagnosed MM patients who received daratumumab, lenalidomide, bortezomib, and dexamethasone (D-RVd) followed by ASCT + D-RVd consolidation, and daratumumab maintenance, had a progression-free survival (PFS) rate of 87.3%, 92.7% overall survival (OS) rate, and 50% achieved minimal residual disease negativity.
Dr. Adriana Rossi, MD, assistant professor of medicine, Icahn School of Medicine at Mount Sinai, New York, cited a convergence of evidence suggesting that CAR T could achieve impressive results as a consolidation therapy in fit patients with MM, including: CARTITUDE 1 and CARTITUDE 4, which studied CAR T in RR MM patients. However, due to the fact that no head-to-head study of CAR T vs. ASCT as consolidation therapy in otherwise healthy MM patients exists, “There is not enough long-term data to support the equivalence CAR T with ASCT,” Dr. Giralt concluded.
Dr. Rossi further advocated for considering CAR T as a consolidation treatment because of the risks of secondary malignancies associated with ACST maintenance regimens.
Dr. Giralt rebutted this argument by citing data about averse events (AE) in studies of CAR-T therapies in RR MM patients like KarMMa-2, in which grade 3-4 neutropenia, anemia, and thrombocytopenia occurred in 94.6%, 45.9%, and 37.8% of patients respectively. Furthermore, 2 of 37 patients in KarMMA died (1 pneumonia, 1 pseudomonal sepsis), while rates of death from AEs related to ASCT occur in less than 1% of patients, according to Dr. Giralt.
Beyond a dearth of evidence thus far about the long term PFS, OS, and safety profile superiority of CAR-T therapies, compared with ASCT in treatment-naive MM patients, Dr. Giralt also noted the facts that CAR T-cell therapies are expensive and require manufacturing infrastructure also demonstrate that they cannot be easily adopted everywhere, even as a third-line therapy.
“In many places like Morocco, where I practice, we do not have access to CAR-T therapies,” said Sadia Zafad, MD, of the Clinique Al Madina Hematology and Oncology Center in Casablanca, Morocco. Dr. Zafad attended the debate.
A lack of access to CAR T is also a problem in the United States, where wait times for the therapy can stretch up to 6 months, getting insurance approval is challenging, and many patients simply don’t live near a center where CAR T-cell therapy is available. Citing all these factors, Dr. Giralt concluded: “Even if CAR T can be shown to have the same results as transplant, it is much more resource-intensive than transplant, and insurers are going to start saying there’s no necessary benefit. We have yet to use value as a primary end point, but as cancer care gets more and more expensive, that’s going to come up more, for CAR T and other novel therapies.”
Dr. Giralt reported relationships with Actinuum, Amgen, BMS, Celgene, Crisper, J&J, Jazz, Kite, Miltenyi, Novartis, Sanofi, and Takeda. Dr. Rossi disclosed ties with Adaptive, BMS, Celgene, JNJ, Sanofi & Genzyme. Dr. Zafad reported no disclosures.
“In an otherwise healthy treatment-naive patient with multiple myeloma, to ensure the best chances of overall survival, I would always recommend standard of care consolidation therapy of chemotherapy + ASCT,” said Sergio Giralt, MD, of New York’s Memorial Sloan Kettering Cancer Center, debating the merits of ASCT versus CAR T as consolidation therapy at the Lymphoma, Leukemia & Myeloma (LLM) Congress 2023 in New York.
Final results from the phase II GRIFFIN trial highlight the benchmarks that CAR T-cell therapy would need to reach to achieve equivalence with ASCT. At a 4-year follow-up, newly diagnosed MM patients who received daratumumab, lenalidomide, bortezomib, and dexamethasone (D-RVd) followed by ASCT + D-RVd consolidation, and daratumumab maintenance, had a progression-free survival (PFS) rate of 87.3%, 92.7% overall survival (OS) rate, and 50% achieved minimal residual disease negativity.
Dr. Adriana Rossi, MD, assistant professor of medicine, Icahn School of Medicine at Mount Sinai, New York, cited a convergence of evidence suggesting that CAR T could achieve impressive results as a consolidation therapy in fit patients with MM, including: CARTITUDE 1 and CARTITUDE 4, which studied CAR T in RR MM patients. However, due to the fact that no head-to-head study of CAR T vs. ASCT as consolidation therapy in otherwise healthy MM patients exists, “There is not enough long-term data to support the equivalence CAR T with ASCT,” Dr. Giralt concluded.
Dr. Rossi further advocated for considering CAR T as a consolidation treatment because of the risks of secondary malignancies associated with ACST maintenance regimens.
Dr. Giralt rebutted this argument by citing data about averse events (AE) in studies of CAR-T therapies in RR MM patients like KarMMa-2, in which grade 3-4 neutropenia, anemia, and thrombocytopenia occurred in 94.6%, 45.9%, and 37.8% of patients respectively. Furthermore, 2 of 37 patients in KarMMA died (1 pneumonia, 1 pseudomonal sepsis), while rates of death from AEs related to ASCT occur in less than 1% of patients, according to Dr. Giralt.
Beyond a dearth of evidence thus far about the long term PFS, OS, and safety profile superiority of CAR-T therapies, compared with ASCT in treatment-naive MM patients, Dr. Giralt also noted the facts that CAR T-cell therapies are expensive and require manufacturing infrastructure also demonstrate that they cannot be easily adopted everywhere, even as a third-line therapy.
“In many places like Morocco, where I practice, we do not have access to CAR-T therapies,” said Sadia Zafad, MD, of the Clinique Al Madina Hematology and Oncology Center in Casablanca, Morocco. Dr. Zafad attended the debate.
A lack of access to CAR T is also a problem in the United States, where wait times for the therapy can stretch up to 6 months, getting insurance approval is challenging, and many patients simply don’t live near a center where CAR T-cell therapy is available. Citing all these factors, Dr. Giralt concluded: “Even if CAR T can be shown to have the same results as transplant, it is much more resource-intensive than transplant, and insurers are going to start saying there’s no necessary benefit. We have yet to use value as a primary end point, but as cancer care gets more and more expensive, that’s going to come up more, for CAR T and other novel therapies.”
Dr. Giralt reported relationships with Actinuum, Amgen, BMS, Celgene, Crisper, J&J, Jazz, Kite, Miltenyi, Novartis, Sanofi, and Takeda. Dr. Rossi disclosed ties with Adaptive, BMS, Celgene, JNJ, Sanofi & Genzyme. Dr. Zafad reported no disclosures.
AT LLM CONGRESS 2023
Nationwide hematologists shortage: What’s being done?
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.
CLL combo treatment: Phase-3 study inconclusive
The difference in PFS between the IVO arm, 85%, versus 87% in the IO arm was statistically insignificant.
“Due to the early read-out and the futility boundaries being crossed, long-term follow-up will be critical to understand if there are any long-term benefits to IVO,” said study principal investigator Jennifer A. Woyach MD, professor in the division of hematology at The Ohio State University Comprehensive Care Center (OSUCCC – The James) in Columbus.
The 14-month follow-up data includes results from 465 CLL patients aged 65+ (median age 74 years, 67.5% male) who were treatment naive. The IO and IVO arms had 232 and 233 participants respectively, patients across both arms had Eastern Cooperative Oncology Group scores of 0-1 (97%), occurrence of Del (17p) was 13%, and a Rai stage status of III/IV was 55%, slightly more patients in the IO arm had unmutated IGHV 55% vs. 47% in the IVO arm. Researchers noted that, as expected, patients in the IVO group had a greater occurrence of hematologic adverse events graded at 3 or above, 61% VS 48% in the IO arm, P =.006.
The trial was spurred by the fact that many CLL patients on IO therapy must remain on treatment indefinitely, and an earlier phase II trial suggested that IVO therapy could lead to deep remission and therapy discontinuation.
Looking at the complete response (CR) rates and undetectable minimal residual disease (uMRD) rates across both arms suggested that there may be some hope that IVO could help CLL patients achieve deep remissions and discontinue therapy. Patients in the IVO arm had a CR of 68.5% and uMRD of 86.8% while only 31.3% of those in the IO arm had a CR and 33.3% achieved uMRD status.
“Despite the impressive CR and uMRD results, this study demonstrates that IVO is not superior to IO in terms of progression-free survival. However, because many patients in the IVO arm have discontinued treatment while those in the IO arm remain on ibrutinib, we think that it will be very important to continue to follow these patients long term, to see if there are advantages to this time limited therapy, especially in terms of toxicity, that we cannot appreciate with this follow-up,” said Dr. Woyach.
The Alliance for Clinical Trials in Oncology cooperative group, including OSUCCC James, is currently working to design the next frontline CLL study for older patients that builds on this work.
Dr. Woyach disclosed ties with Abbvie, AstraZeneca, Beigene, Genentech, Janssen, Loxo/Lilly, Merck, Newave, Pharmacyclics, and Schrodinger.
The difference in PFS between the IVO arm, 85%, versus 87% in the IO arm was statistically insignificant.
“Due to the early read-out and the futility boundaries being crossed, long-term follow-up will be critical to understand if there are any long-term benefits to IVO,” said study principal investigator Jennifer A. Woyach MD, professor in the division of hematology at The Ohio State University Comprehensive Care Center (OSUCCC – The James) in Columbus.
The 14-month follow-up data includes results from 465 CLL patients aged 65+ (median age 74 years, 67.5% male) who were treatment naive. The IO and IVO arms had 232 and 233 participants respectively, patients across both arms had Eastern Cooperative Oncology Group scores of 0-1 (97%), occurrence of Del (17p) was 13%, and a Rai stage status of III/IV was 55%, slightly more patients in the IO arm had unmutated IGHV 55% vs. 47% in the IVO arm. Researchers noted that, as expected, patients in the IVO group had a greater occurrence of hematologic adverse events graded at 3 or above, 61% VS 48% in the IO arm, P =.006.
The trial was spurred by the fact that many CLL patients on IO therapy must remain on treatment indefinitely, and an earlier phase II trial suggested that IVO therapy could lead to deep remission and therapy discontinuation.
Looking at the complete response (CR) rates and undetectable minimal residual disease (uMRD) rates across both arms suggested that there may be some hope that IVO could help CLL patients achieve deep remissions and discontinue therapy. Patients in the IVO arm had a CR of 68.5% and uMRD of 86.8% while only 31.3% of those in the IO arm had a CR and 33.3% achieved uMRD status.
“Despite the impressive CR and uMRD results, this study demonstrates that IVO is not superior to IO in terms of progression-free survival. However, because many patients in the IVO arm have discontinued treatment while those in the IO arm remain on ibrutinib, we think that it will be very important to continue to follow these patients long term, to see if there are advantages to this time limited therapy, especially in terms of toxicity, that we cannot appreciate with this follow-up,” said Dr. Woyach.
The Alliance for Clinical Trials in Oncology cooperative group, including OSUCCC James, is currently working to design the next frontline CLL study for older patients that builds on this work.
Dr. Woyach disclosed ties with Abbvie, AstraZeneca, Beigene, Genentech, Janssen, Loxo/Lilly, Merck, Newave, Pharmacyclics, and Schrodinger.
The difference in PFS between the IVO arm, 85%, versus 87% in the IO arm was statistically insignificant.
“Due to the early read-out and the futility boundaries being crossed, long-term follow-up will be critical to understand if there are any long-term benefits to IVO,” said study principal investigator Jennifer A. Woyach MD, professor in the division of hematology at The Ohio State University Comprehensive Care Center (OSUCCC – The James) in Columbus.
The 14-month follow-up data includes results from 465 CLL patients aged 65+ (median age 74 years, 67.5% male) who were treatment naive. The IO and IVO arms had 232 and 233 participants respectively, patients across both arms had Eastern Cooperative Oncology Group scores of 0-1 (97%), occurrence of Del (17p) was 13%, and a Rai stage status of III/IV was 55%, slightly more patients in the IO arm had unmutated IGHV 55% vs. 47% in the IVO arm. Researchers noted that, as expected, patients in the IVO group had a greater occurrence of hematologic adverse events graded at 3 or above, 61% VS 48% in the IO arm, P =.006.
The trial was spurred by the fact that many CLL patients on IO therapy must remain on treatment indefinitely, and an earlier phase II trial suggested that IVO therapy could lead to deep remission and therapy discontinuation.
Looking at the complete response (CR) rates and undetectable minimal residual disease (uMRD) rates across both arms suggested that there may be some hope that IVO could help CLL patients achieve deep remissions and discontinue therapy. Patients in the IVO arm had a CR of 68.5% and uMRD of 86.8% while only 31.3% of those in the IO arm had a CR and 33.3% achieved uMRD status.
“Despite the impressive CR and uMRD results, this study demonstrates that IVO is not superior to IO in terms of progression-free survival. However, because many patients in the IVO arm have discontinued treatment while those in the IO arm remain on ibrutinib, we think that it will be very important to continue to follow these patients long term, to see if there are advantages to this time limited therapy, especially in terms of toxicity, that we cannot appreciate with this follow-up,” said Dr. Woyach.
The Alliance for Clinical Trials in Oncology cooperative group, including OSUCCC James, is currently working to design the next frontline CLL study for older patients that builds on this work.
Dr. Woyach disclosed ties with Abbvie, AstraZeneca, Beigene, Genentech, Janssen, Loxo/Lilly, Merck, Newave, Pharmacyclics, and Schrodinger.
New CLL meds: Improved survival rates, 1990-2018
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS & PREVENTION