User login
VIDEO: Creative cuts make more aesthetic surgical dressings
ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

AT FSDDS 14
VIDEO: Best practices in treating low testosterone in men
LAS VEGAS – Analysis of data from a company that provides therapy for low testosterone showed that the treatment was not associated with a higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The findings clash with what two recent studies – one published in JAMA and the other in PLoS One – found, which showed that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Dr. Aaron Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, puts the studies in perspective in this interview, and shares how patients should be treated based on current data and available knowledge.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Analysis of data from a company that provides therapy for low testosterone showed that the treatment was not associated with a higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The findings clash with what two recent studies – one published in JAMA and the other in PLoS One – found, which showed that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Dr. Aaron Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, puts the studies in perspective in this interview, and shares how patients should be treated based on current data and available knowledge.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Analysis of data from a company that provides therapy for low testosterone showed that the treatment was not associated with a higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The findings clash with what two recent studies – one published in JAMA and the other in PLoS One – found, which showed that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Dr. Aaron Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, puts the studies in perspective in this interview, and shares how patients should be treated based on current data and available knowledge.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM AACE 2014
Testosterone therapy may not be associated with CV risk
LAS VEGAS – Analysis of data from a low testosterone therapy company showed that the treatment was not associated with higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The authors of the unpublished study analyzed 20,000 patient records, and when they compared the data with two community data sets, they found that the study’s patient group had seven and nine times lower risk of developing MI and strokes, respectively. Researchers said they found no evidence of worsening of preexisting MI or strokes in the study group.
The findings clash with what two recent studies found – one published in JAMA and the other in PLoS One – which was that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Meanwhile, this is not the first time that an observational study has shown a cardioprotective role for testosterone therapy in men.
“I don’t think this study adds much to the studies that have already been done,” said Dr. Bradley D. Anawalt, chief of medicine at the University of Washington Medical Center, Seattle, and chairman of Hormone Health Network at the Endocrine Society.
Dr. Aaron I. Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, said that he wasn’t sure what could be concluded from the study. “It’s not prospective, it’s not blinded, there’s no control group, and it’s an observational study all over again.”
The one thing all experts, including the study authors, agree on is that there’s a need for a prospective randomized, controlled trial to prove or disprove a cause and effect relationship between testosterone therapy and risk of cardiovascular disease in men.
Dr. Robert Tan led the Low T Center study and presented the results on May 16 at the annual meeting of the American Association of Clinical Endocrinologists. He said he was an independent contractor for the company.
He conducted a cross-sectional analysis of the data from the electronic health records of 40 Low T Centers across the United States, selecting patients who had MI and stroke before and after testosterone therapy, between 2009 and 2014. The Low T Centers, which solely treat men with low testosterone, require regular 2-week monitoring of patients for safety and efficacy of the therapy.
There were four nonfatal MIs and two probable fatal MIs. The rate of new MI was 30/100,000 patients. Forty-six patients had MI before therapy and none had adverse outcomes after testosterone therapy, he reported.
Two patients had strokes, and the rate of new stroke was 10/100,000 patients. Twelve patients had a stroke before therapy, and there were no adverse outcomes after therapy, according to the findings.
For comparison, Dr. Tan used the closest available data sets, from Kaiser Permanente for MI (208/100,000) and Northern Manhattan Registry for stroke (93/100,000). The rate ratios showed that the patients in the study group were seven times less likely to have a myocardial infarction, and nine times less likely to have a stroke.
So why the difference?
“Maybe it’s not so much the drug, but maybe it’s the way the medication is given,” and is monitored, speculated Dr. Tan, also of the University of Texas, Houston. In addition, patients treated at Low T Centers were younger than 65 years, and excluded the older and sicker Medicare population.
Dr. Anawalt raised concerns about the fact that the analysis was done on a patient population treated at a company that has built a business model around treating men with low testosterone. He also said that the comparison groups — Kaiser Permanente and Northern Manhattan Registry — weren’t quite comparable.
He said that physicians should continue to carefully monitor their patients to avoid excessive dosage or erythrocytosis; know that in men with clearly established hypogonadism, it is safe to assume that benefits of testosterone therapy outweigh the risks; and be cautious when prescribing testosterone in men with borderline low testosterone, particularly in older men.
The findings highlight the fact that there are still many questions left to be answered, and this is just a glimpse into how much there is left to be learned about the effect of testosterone therapy on men’s cardiovascular health, Dr. Tan said.
Dr. Tan was an independent contractor for Low T Center. Dr. Anawalt and Dr. Vinik had no disclosures.
LAS VEGAS – Analysis of data from a low testosterone therapy company showed that the treatment was not associated with higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The authors of the unpublished study analyzed 20,000 patient records, and when they compared the data with two community data sets, they found that the study’s patient group had seven and nine times lower risk of developing MI and strokes, respectively. Researchers said they found no evidence of worsening of preexisting MI or strokes in the study group.
The findings clash with what two recent studies found – one published in JAMA and the other in PLoS One – which was that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Meanwhile, this is not the first time that an observational study has shown a cardioprotective role for testosterone therapy in men.
“I don’t think this study adds much to the studies that have already been done,” said Dr. Bradley D. Anawalt, chief of medicine at the University of Washington Medical Center, Seattle, and chairman of Hormone Health Network at the Endocrine Society.
Dr. Aaron I. Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, said that he wasn’t sure what could be concluded from the study. “It’s not prospective, it’s not blinded, there’s no control group, and it’s an observational study all over again.”
The one thing all experts, including the study authors, agree on is that there’s a need for a prospective randomized, controlled trial to prove or disprove a cause and effect relationship between testosterone therapy and risk of cardiovascular disease in men.
Dr. Robert Tan led the Low T Center study and presented the results on May 16 at the annual meeting of the American Association of Clinical Endocrinologists. He said he was an independent contractor for the company.
He conducted a cross-sectional analysis of the data from the electronic health records of 40 Low T Centers across the United States, selecting patients who had MI and stroke before and after testosterone therapy, between 2009 and 2014. The Low T Centers, which solely treat men with low testosterone, require regular 2-week monitoring of patients for safety and efficacy of the therapy.
There were four nonfatal MIs and two probable fatal MIs. The rate of new MI was 30/100,000 patients. Forty-six patients had MI before therapy and none had adverse outcomes after testosterone therapy, he reported.
Two patients had strokes, and the rate of new stroke was 10/100,000 patients. Twelve patients had a stroke before therapy, and there were no adverse outcomes after therapy, according to the findings.
For comparison, Dr. Tan used the closest available data sets, from Kaiser Permanente for MI (208/100,000) and Northern Manhattan Registry for stroke (93/100,000). The rate ratios showed that the patients in the study group were seven times less likely to have a myocardial infarction, and nine times less likely to have a stroke.
So why the difference?
“Maybe it’s not so much the drug, but maybe it’s the way the medication is given,” and is monitored, speculated Dr. Tan, also of the University of Texas, Houston. In addition, patients treated at Low T Centers were younger than 65 years, and excluded the older and sicker Medicare population.
Dr. Anawalt raised concerns about the fact that the analysis was done on a patient population treated at a company that has built a business model around treating men with low testosterone. He also said that the comparison groups — Kaiser Permanente and Northern Manhattan Registry — weren’t quite comparable.
He said that physicians should continue to carefully monitor their patients to avoid excessive dosage or erythrocytosis; know that in men with clearly established hypogonadism, it is safe to assume that benefits of testosterone therapy outweigh the risks; and be cautious when prescribing testosterone in men with borderline low testosterone, particularly in older men.
The findings highlight the fact that there are still many questions left to be answered, and this is just a glimpse into how much there is left to be learned about the effect of testosterone therapy on men’s cardiovascular health, Dr. Tan said.
Dr. Tan was an independent contractor for Low T Center. Dr. Anawalt and Dr. Vinik had no disclosures.
LAS VEGAS – Analysis of data from a low testosterone therapy company showed that the treatment was not associated with higher risk of myocardial infarction and stroke in men, and it may have played a protective role.
The authors of the unpublished study analyzed 20,000 patient records, and when they compared the data with two community data sets, they found that the study’s patient group had seven and nine times lower risk of developing MI and strokes, respectively. Researchers said they found no evidence of worsening of preexisting MI or strokes in the study group.
The findings clash with what two recent studies found – one published in JAMA and the other in PLoS One – which was that testosterone therapy increased the risk of MI and stroke in men, prompting the Food and Drug Administration to reassess the safety of the approved treatments.
Meanwhile, this is not the first time that an observational study has shown a cardioprotective role for testosterone therapy in men.
“I don’t think this study adds much to the studies that have already been done,” said Dr. Bradley D. Anawalt, chief of medicine at the University of Washington Medical Center, Seattle, and chairman of Hormone Health Network at the Endocrine Society.
Dr. Aaron I. Vinik, Murray Waitzer Endowed Chair for Diabetes Research at Eastern Virginia Medical School, Norfolk, said that he wasn’t sure what could be concluded from the study. “It’s not prospective, it’s not blinded, there’s no control group, and it’s an observational study all over again.”
The one thing all experts, including the study authors, agree on is that there’s a need for a prospective randomized, controlled trial to prove or disprove a cause and effect relationship between testosterone therapy and risk of cardiovascular disease in men.
Dr. Robert Tan led the Low T Center study and presented the results on May 16 at the annual meeting of the American Association of Clinical Endocrinologists. He said he was an independent contractor for the company.
He conducted a cross-sectional analysis of the data from the electronic health records of 40 Low T Centers across the United States, selecting patients who had MI and stroke before and after testosterone therapy, between 2009 and 2014. The Low T Centers, which solely treat men with low testosterone, require regular 2-week monitoring of patients for safety and efficacy of the therapy.
There were four nonfatal MIs and two probable fatal MIs. The rate of new MI was 30/100,000 patients. Forty-six patients had MI before therapy and none had adverse outcomes after testosterone therapy, he reported.
Two patients had strokes, and the rate of new stroke was 10/100,000 patients. Twelve patients had a stroke before therapy, and there were no adverse outcomes after therapy, according to the findings.
For comparison, Dr. Tan used the closest available data sets, from Kaiser Permanente for MI (208/100,000) and Northern Manhattan Registry for stroke (93/100,000). The rate ratios showed that the patients in the study group were seven times less likely to have a myocardial infarction, and nine times less likely to have a stroke.
So why the difference?
“Maybe it’s not so much the drug, but maybe it’s the way the medication is given,” and is monitored, speculated Dr. Tan, also of the University of Texas, Houston. In addition, patients treated at Low T Centers were younger than 65 years, and excluded the older and sicker Medicare population.
Dr. Anawalt raised concerns about the fact that the analysis was done on a patient population treated at a company that has built a business model around treating men with low testosterone. He also said that the comparison groups — Kaiser Permanente and Northern Manhattan Registry — weren’t quite comparable.
He said that physicians should continue to carefully monitor their patients to avoid excessive dosage or erythrocytosis; know that in men with clearly established hypogonadism, it is safe to assume that benefits of testosterone therapy outweigh the risks; and be cautious when prescribing testosterone in men with borderline low testosterone, particularly in older men.
The findings highlight the fact that there are still many questions left to be answered, and this is just a glimpse into how much there is left to be learned about the effect of testosterone therapy on men’s cardiovascular health, Dr. Tan said.
Dr. Tan was an independent contractor for Low T Center. Dr. Anawalt and Dr. Vinik had no disclosures.
AACE/ACE Introduce New Obesity Diagnosis Framework
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.

Twitter: @naseemmiller
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.

Twitter: @naseemmiller
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.

Twitter: @naseemmiller
VIDEO: AACE/ACE introduce new obesity diagnosis framework
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.
Twitter: @naseemmiller
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.
Twitter: @naseemmiller
LAS VEGAS —Your patient’s body mass index indicates obesity. Now, what’s the course of action?
The American Association of Clinical Endocrinologists and the American College of Endocrinology are aiming to address this gap in diagnosis and treatment of obesity through a new framework.
The four-step approach starts with BMI measurement, then clinical assessment, complication staging, and finally treatment.
In a video interview, Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee, explained why the new framework is important and how physicians can apply it to their practice at the AACE annual meeting.
The document, or advanced framework, is in its last stages of completion.
Twitter: @naseemmiller
VIDEO: U.S. Hispanics show varying diabetes rates by country of origin
LAS VEGAS – When it comes to treating Hispanic patients, one size doesn’t fit all, according to results from the ongoing Hispanic Community Health Study/Study of Latinos.
In a video interview, Dr. Larissa Avilés-Santa, a medical officer at the National Heart, Lung, and Blood Institute in Bethesda, Md., talks about the study’s findings and provides advice to physicians at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – When it comes to treating Hispanic patients, one size doesn’t fit all, according to results from the ongoing Hispanic Community Health Study/Study of Latinos.
In a video interview, Dr. Larissa Avilés-Santa, a medical officer at the National Heart, Lung, and Blood Institute in Bethesda, Md., talks about the study’s findings and provides advice to physicians at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – When it comes to treating Hispanic patients, one size doesn’t fit all, according to results from the ongoing Hispanic Community Health Study/Study of Latinos.
In a video interview, Dr. Larissa Avilés-Santa, a medical officer at the National Heart, Lung, and Blood Institute in Bethesda, Md., talks about the study’s findings and provides advice to physicians at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT AACE 14
VIDEO: HbA1c focus of diabetes education program
LAS VEGAS – In its fourth year, the Blood Sugar Basics program, which is the American College of Endocrinology and Merck’s diabetes education program, is turning its attention to hemoglobin A1c, because many patients with diabetes fail to achieve an HbA1c of 6.5% or less, the program’s leaders said.
This year’s campaign was unveiled at the annual meeting of the American Association of Clinical Endocrinologists.
With the goal of increasing the number of patients who achieve their HbA1c goal, the program has established three missions for patients: Talk to your physician; set goals and commit to a plan; and revisit and reassess.
The program’s website (bloodsugarbasics.com), which has had a facelift, provides forms and easy-to-follow guidelines for patients. The association is also distributing printed information about the program to AACE members, and this year, it is reaching out to primary care physicians, because there simply aren’t enough endocrinologists, said Dr. Etie Moghissi, who has helped develop the program since its inception in 2010.
Blood Sugar Basics is among a handful of credible diabetes education programs online, including the National Diabetes Education Program.
In a video interview, Dr. Moghissi of the department of medicine at the University of California, Los Angeles, explains the program’s goals, and why physicians should consider it as an educational source for their patients.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – In its fourth year, the Blood Sugar Basics program, which is the American College of Endocrinology and Merck’s diabetes education program, is turning its attention to hemoglobin A1c, because many patients with diabetes fail to achieve an HbA1c of 6.5% or less, the program’s leaders said.
This year’s campaign was unveiled at the annual meeting of the American Association of Clinical Endocrinologists.
With the goal of increasing the number of patients who achieve their HbA1c goal, the program has established three missions for patients: Talk to your physician; set goals and commit to a plan; and revisit and reassess.
The program’s website (bloodsugarbasics.com), which has had a facelift, provides forms and easy-to-follow guidelines for patients. The association is also distributing printed information about the program to AACE members, and this year, it is reaching out to primary care physicians, because there simply aren’t enough endocrinologists, said Dr. Etie Moghissi, who has helped develop the program since its inception in 2010.
Blood Sugar Basics is among a handful of credible diabetes education programs online, including the National Diabetes Education Program.
In a video interview, Dr. Moghissi of the department of medicine at the University of California, Los Angeles, explains the program’s goals, and why physicians should consider it as an educational source for their patients.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – In its fourth year, the Blood Sugar Basics program, which is the American College of Endocrinology and Merck’s diabetes education program, is turning its attention to hemoglobin A1c, because many patients with diabetes fail to achieve an HbA1c of 6.5% or less, the program’s leaders said.
This year’s campaign was unveiled at the annual meeting of the American Association of Clinical Endocrinologists.
With the goal of increasing the number of patients who achieve their HbA1c goal, the program has established three missions for patients: Talk to your physician; set goals and commit to a plan; and revisit and reassess.
The program’s website (bloodsugarbasics.com), which has had a facelift, provides forms and easy-to-follow guidelines for patients. The association is also distributing printed information about the program to AACE members, and this year, it is reaching out to primary care physicians, because there simply aren’t enough endocrinologists, said Dr. Etie Moghissi, who has helped develop the program since its inception in 2010.
Blood Sugar Basics is among a handful of credible diabetes education programs online, including the National Diabetes Education Program.
In a video interview, Dr. Moghissi of the department of medicine at the University of California, Los Angeles, explains the program’s goals, and why physicians should consider it as an educational source for their patients.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT AACE 2014
VIDEO: Spruce up your suturing; try these techniques
ORLANDO – Inspired by sewing lessons during her childhood, Dr. Cyndi Yag-Howard has developed several suturing techniques that help promote better wound healing and yield more aesthetically pleasing results.
She has published several of her techniques, including the SICM (subcutaneous inverted cross mattress) stitch (Dermatol. Surg. 2011;37:1503-5) and the Zipper stitch (Dermatol. Surg. 2013;39:1400-2), and she has a few more in the works. In a video interview after her presentation at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Yag-Howard, who is in private practice in Naples, Fla., shared the how-to’s of several of her suturing techniques.
On Twitter @naseemmiller
ORLANDO – Inspired by sewing lessons during her childhood, Dr. Cyndi Yag-Howard has developed several suturing techniques that help promote better wound healing and yield more aesthetically pleasing results.
She has published several of her techniques, including the SICM (subcutaneous inverted cross mattress) stitch (Dermatol. Surg. 2011;37:1503-5) and the Zipper stitch (Dermatol. Surg. 2013;39:1400-2), and she has a few more in the works. In a video interview after her presentation at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Yag-Howard, who is in private practice in Naples, Fla., shared the how-to’s of several of her suturing techniques.
On Twitter @naseemmiller
ORLANDO – Inspired by sewing lessons during her childhood, Dr. Cyndi Yag-Howard has developed several suturing techniques that help promote better wound healing and yield more aesthetically pleasing results.
She has published several of her techniques, including the SICM (subcutaneous inverted cross mattress) stitch (Dermatol. Surg. 2011;37:1503-5) and the Zipper stitch (Dermatol. Surg. 2013;39:1400-2), and she has a few more in the works. In a video interview after her presentation at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Yag-Howard, who is in private practice in Naples, Fla., shared the how-to’s of several of her suturing techniques.
On Twitter @naseemmiller
AT FSDDS 2014
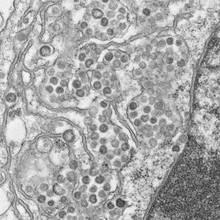
MERS – What Clinicians Need to Know
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
According to the latest update, the patient is a male US citizen in his 60s who lives and works in Riyadh, Saudi Arabia. He traveled from Riyadh to Chicago on April 24, via London’s Heathrow airport, and then to Indiana by bus.
Officials at Community Hospital in Munster, where he’s being treated, said on May 5 that the patient is doing well, is off oxygen, and walking around.
Since the first confirmed MERS case in Saudi Arabia, 263 cases have been confirmed in 12 countries, and there have been 92 deaths, according to a recent CDC briefing.
But how big a worry is MERS for US clinicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged clinicians to check the CDC website for the latest updates and practice protocols. Clinicians can also visit the World Health Organization’s website for the latest global updates.

On Twitter @naseemmiller
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
According to the latest update, the patient is a male US citizen in his 60s who lives and works in Riyadh, Saudi Arabia. He traveled from Riyadh to Chicago on April 24, via London’s Heathrow airport, and then to Indiana by bus.
Officials at Community Hospital in Munster, where he’s being treated, said on May 5 that the patient is doing well, is off oxygen, and walking around.
Since the first confirmed MERS case in Saudi Arabia, 263 cases have been confirmed in 12 countries, and there have been 92 deaths, according to a recent CDC briefing.
But how big a worry is MERS for US clinicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged clinicians to check the CDC website for the latest updates and practice protocols. Clinicians can also visit the World Health Organization’s website for the latest global updates.

On Twitter @naseemmiller
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
According to the latest update, the patient is a male US citizen in his 60s who lives and works in Riyadh, Saudi Arabia. He traveled from Riyadh to Chicago on April 24, via London’s Heathrow airport, and then to Indiana by bus.
Officials at Community Hospital in Munster, where he’s being treated, said on May 5 that the patient is doing well, is off oxygen, and walking around.
Since the first confirmed MERS case in Saudi Arabia, 263 cases have been confirmed in 12 countries, and there have been 92 deaths, according to a recent CDC briefing.
But how big a worry is MERS for US clinicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged clinicians to check the CDC website for the latest updates and practice protocols. Clinicians can also visit the World Health Organization’s website for the latest global updates.

On Twitter @naseemmiller
VIDEO: Pediatrician’s guide to talking about guns
VANCOUVER, B.C. – The evidence is strong. Having guns at home increases the risk of accidental injury, suicide, and homicide among youth. Nearly 20,600 youths between the ages of 1 and 24 years sustain firearm injuries each year, and 6,570 of them die.
Firearm injuries cause twice as many deaths as cancer, five times as many as heart disease, and 20 times as many as infections in this age group, according to presenters who spoke during a symposium about firearm injury prevention at the annual meeting of the Pediatric Academic Societies.
"We must continue to raise awareness about the public health and social consequences of firearm injury in children," symposium cochair Dr. Barbara J. Stoll, chair of the pediatrics department at Emory University in Atlanta, noted in a written statement. "We hope to focus the discussion on up-to-date evidence, rather than politics or personal opinion, and to identify gaps in knowledge and build the case for expanded research. Firearm injury has not gone away. We must address the tragedy of these preventable injuries and deaths," Dr. Stoll said.
But because the issue is highly politicized, pediatricians might hesitate to bring it up in conversation during routine office visits.
Dr. Robert Sege, director of the division of family and child advocacy at Boston Medical Center, shared his advice during this video interview on how to approach the topic without creating tension or push-back.
Dr. Sege had no relevant conflicts of interest.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER, B.C. – The evidence is strong. Having guns at home increases the risk of accidental injury, suicide, and homicide among youth. Nearly 20,600 youths between the ages of 1 and 24 years sustain firearm injuries each year, and 6,570 of them die.
Firearm injuries cause twice as many deaths as cancer, five times as many as heart disease, and 20 times as many as infections in this age group, according to presenters who spoke during a symposium about firearm injury prevention at the annual meeting of the Pediatric Academic Societies.
"We must continue to raise awareness about the public health and social consequences of firearm injury in children," symposium cochair Dr. Barbara J. Stoll, chair of the pediatrics department at Emory University in Atlanta, noted in a written statement. "We hope to focus the discussion on up-to-date evidence, rather than politics or personal opinion, and to identify gaps in knowledge and build the case for expanded research. Firearm injury has not gone away. We must address the tragedy of these preventable injuries and deaths," Dr. Stoll said.
But because the issue is highly politicized, pediatricians might hesitate to bring it up in conversation during routine office visits.
Dr. Robert Sege, director of the division of family and child advocacy at Boston Medical Center, shared his advice during this video interview on how to approach the topic without creating tension or push-back.
Dr. Sege had no relevant conflicts of interest.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER, B.C. – The evidence is strong. Having guns at home increases the risk of accidental injury, suicide, and homicide among youth. Nearly 20,600 youths between the ages of 1 and 24 years sustain firearm injuries each year, and 6,570 of them die.
Firearm injuries cause twice as many deaths as cancer, five times as many as heart disease, and 20 times as many as infections in this age group, according to presenters who spoke during a symposium about firearm injury prevention at the annual meeting of the Pediatric Academic Societies.
"We must continue to raise awareness about the public health and social consequences of firearm injury in children," symposium cochair Dr. Barbara J. Stoll, chair of the pediatrics department at Emory University in Atlanta, noted in a written statement. "We hope to focus the discussion on up-to-date evidence, rather than politics or personal opinion, and to identify gaps in knowledge and build the case for expanded research. Firearm injury has not gone away. We must address the tragedy of these preventable injuries and deaths," Dr. Stoll said.
But because the issue is highly politicized, pediatricians might hesitate to bring it up in conversation during routine office visits.
Dr. Robert Sege, director of the division of family and child advocacy at Boston Medical Center, shared his advice during this video interview on how to approach the topic without creating tension or push-back.
Dr. Sege had no relevant conflicts of interest.
On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE PAS ANNUAL MEETING