User login
VIDEO: What’s known so far about plasma exchange in MS, neuromyelitis optica
DALLAS – Plasma exchange, or PLEX, is a type of therapeutic apheresis that has been shown to be effective for acute attacks of demyelinating disease, but it’s not to be used for treatment of chronic or progressive multiple sclerosis.
Dr. Brian G. Weinshenker, professor of neurology at the Mayo Clinic College of Medicine in Rochester, Minn., summarized the current evidence and indications for plasma exchange in individuals with multiple sclerosis or neuromyelitis optica and shared a few practice tips at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
For the latest guidelines, visit the American Academy of Neurology and the American Society for Apheresis.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – Plasma exchange, or PLEX, is a type of therapeutic apheresis that has been shown to be effective for acute attacks of demyelinating disease, but it’s not to be used for treatment of chronic or progressive multiple sclerosis.
Dr. Brian G. Weinshenker, professor of neurology at the Mayo Clinic College of Medicine in Rochester, Minn., summarized the current evidence and indications for plasma exchange in individuals with multiple sclerosis or neuromyelitis optica and shared a few practice tips at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
For the latest guidelines, visit the American Academy of Neurology and the American Society for Apheresis.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – Plasma exchange, or PLEX, is a type of therapeutic apheresis that has been shown to be effective for acute attacks of demyelinating disease, but it’s not to be used for treatment of chronic or progressive multiple sclerosis.
Dr. Brian G. Weinshenker, professor of neurology at the Mayo Clinic College of Medicine in Rochester, Minn., summarized the current evidence and indications for plasma exchange in individuals with multiple sclerosis or neuromyelitis optica and shared a few practice tips at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
For the latest guidelines, visit the American Academy of Neurology and the American Society for Apheresis.
[email protected] On Twitter @naseemsmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE CMSC/ACTRIMS ANNUAL MEETING
Tips for Vaccinating Multiple Sclerosis Patients
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT THE CMSC/ACTRIMS ANNUAL MEETING
VIDEO: Tips for vaccinating multiple sclerosis patients
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DALLAS – Vaccinations are beneficial for individuals with multiple sclerosis because they help avoid infections, which in turn lower the risk of relapse.
But while inactive vaccines are considered safe for MS patients, the use of live vaccines such as Varivax, Zostavax, or yellow fever vaccine is more nuanced, especially as more disease-modifying therapies (DMT) become available. There are limited data available about the effect of live vaccines on patients who are on DMTs, and the final decision comes down to the risk-benefit ratio, said, Dr. Patricia K. Coyle, professor of neurology and director of the MS Comprehensive Care Center at Stony Brook (N.Y.) University Medical Center.
In a video interview at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Dr. Coyle summarizes what’s known so far about vaccines and MS, and provides tips to clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT THE CMSC/ACTRIMS ANNUAL MEETING
Exercise is generally safe for MS patients
DALLAS – Exercise is generally safe for individuals with multiple sclerosis, according to a systematic review of randomized, controlled trials, supporting the promotion of exercise in this patient group.
The analysis showed that persons with MS who exercised had 27% lower risk of relapse, compared with patients who didn’t exercise. However, those who exercised had a 67% higher risk of adverse events, but the rate was no higher than adverse events (AEs) in healthy populations.
"Patients with MS should not be deterred from exercise participation for concern of experiencing a relapse or adverse events, and such patients would further be expected to experience the many benefits of exercise training documented in the literature," wrote Mr. Matthew E. Platta and his colleagues in a study that was published in the Journal of the Neurological Sciences (2014 May 19 [doi:10.1016/j.jns.2014.05.016]).
Although reviews have shown the benefits of exercise for individuals with MS, none have looked at the risks of relapse and other AEs, Mr. Platta said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
Mr. Platta, a graduate student in the department of kinesiology and community health at the University of Illinois at Urbana-Champaign, and his colleagues analyzed 26 trials, including 1,295 participants. The trials were published up to November 2013 and examined the effect of exercise on MS relapses and adverse events. All trials included a nontreatment control arm.
The exercises included yoga, resistance training, aerobics, aquatics, and combined aerobics and resistance training.
Results showed that there were 26 relapses in the control groups, compared with 29 in the exercise group, corresponding with 6.3% and 4.6% of participants in the control and exercise groups, respectively.
The exercise group also had a 27% lower relative risk of relapse.
As for AEs, there were 5 in the control group, compared with 13 in the exercise group (or 1.2% and 2.0% in each group, respectively).
But the exercise group had a 67% higher relative risk of AEs, compared with the control group. However, the rate was not higher than the rates of AEs associated with exercise training in healthy populations, the researchers said.
The most common AEs in the control group were illness, ankle sprain, knee pain, and fall. The exercise group had additional AEs, including stroke, low back pain, trigeminal neuralgia, traffic accident, upper respiratory tract infection, rheumatoid arthritis flare up, and hernia. The most common types of AEs were musculoskeletal injuries (46%) and illnesses (23%).
"MS patients and clinicians can expect a low occurrence of AEs with exercise training, and, when AEs do occur, such events are commonly musculoskeletal in nature," Mr. Platta and his colleagues wrote.
There was no difference in the dropout rate between the two groups. The authors noted that "Future research might consider the inclusion of behavioral strategies for reducing dropout in RCTs of exercise training in MS."
They said that some of the analysis limitations include lack of complete reporting on the exercise training protocols, and potential for attention bias in the exercise group, compared with the control group.
Also, there was considerable variation in the type and prescription of exercises, they said. The sessions were between 1 and 5 days per week for 20-90 minutes per day. The duration of the programs was 4-24 weeks. Mr. Platta said there were too few trials to analyze the effect of different types of exercise separately.
The authors added that it is also important to record frequency and severity of temporary symptomatic changes in response to acute exercise bouts.
"Take-home message is that, taking into account that there are a lot of benefits to exercise, our findings show that the amount of relapses and adverse events are not too high to prevent physicians from recommending exercise [to individuals with MS]."
Mr. Platta and his coauthors had no disclosures.
On Twitter @naseemsmiller
DALLAS – Exercise is generally safe for individuals with multiple sclerosis, according to a systematic review of randomized, controlled trials, supporting the promotion of exercise in this patient group.
The analysis showed that persons with MS who exercised had 27% lower risk of relapse, compared with patients who didn’t exercise. However, those who exercised had a 67% higher risk of adverse events, but the rate was no higher than adverse events (AEs) in healthy populations.
"Patients with MS should not be deterred from exercise participation for concern of experiencing a relapse or adverse events, and such patients would further be expected to experience the many benefits of exercise training documented in the literature," wrote Mr. Matthew E. Platta and his colleagues in a study that was published in the Journal of the Neurological Sciences (2014 May 19 [doi:10.1016/j.jns.2014.05.016]).
Although reviews have shown the benefits of exercise for individuals with MS, none have looked at the risks of relapse and other AEs, Mr. Platta said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
Mr. Platta, a graduate student in the department of kinesiology and community health at the University of Illinois at Urbana-Champaign, and his colleagues analyzed 26 trials, including 1,295 participants. The trials were published up to November 2013 and examined the effect of exercise on MS relapses and adverse events. All trials included a nontreatment control arm.
The exercises included yoga, resistance training, aerobics, aquatics, and combined aerobics and resistance training.
Results showed that there were 26 relapses in the control groups, compared with 29 in the exercise group, corresponding with 6.3% and 4.6% of participants in the control and exercise groups, respectively.
The exercise group also had a 27% lower relative risk of relapse.
As for AEs, there were 5 in the control group, compared with 13 in the exercise group (or 1.2% and 2.0% in each group, respectively).
But the exercise group had a 67% higher relative risk of AEs, compared with the control group. However, the rate was not higher than the rates of AEs associated with exercise training in healthy populations, the researchers said.
The most common AEs in the control group were illness, ankle sprain, knee pain, and fall. The exercise group had additional AEs, including stroke, low back pain, trigeminal neuralgia, traffic accident, upper respiratory tract infection, rheumatoid arthritis flare up, and hernia. The most common types of AEs were musculoskeletal injuries (46%) and illnesses (23%).
"MS patients and clinicians can expect a low occurrence of AEs with exercise training, and, when AEs do occur, such events are commonly musculoskeletal in nature," Mr. Platta and his colleagues wrote.
There was no difference in the dropout rate between the two groups. The authors noted that "Future research might consider the inclusion of behavioral strategies for reducing dropout in RCTs of exercise training in MS."
They said that some of the analysis limitations include lack of complete reporting on the exercise training protocols, and potential for attention bias in the exercise group, compared with the control group.
Also, there was considerable variation in the type and prescription of exercises, they said. The sessions were between 1 and 5 days per week for 20-90 minutes per day. The duration of the programs was 4-24 weeks. Mr. Platta said there were too few trials to analyze the effect of different types of exercise separately.
The authors added that it is also important to record frequency and severity of temporary symptomatic changes in response to acute exercise bouts.
"Take-home message is that, taking into account that there are a lot of benefits to exercise, our findings show that the amount of relapses and adverse events are not too high to prevent physicians from recommending exercise [to individuals with MS]."
Mr. Platta and his coauthors had no disclosures.
On Twitter @naseemsmiller
DALLAS – Exercise is generally safe for individuals with multiple sclerosis, according to a systematic review of randomized, controlled trials, supporting the promotion of exercise in this patient group.
The analysis showed that persons with MS who exercised had 27% lower risk of relapse, compared with patients who didn’t exercise. However, those who exercised had a 67% higher risk of adverse events, but the rate was no higher than adverse events (AEs) in healthy populations.
"Patients with MS should not be deterred from exercise participation for concern of experiencing a relapse or adverse events, and such patients would further be expected to experience the many benefits of exercise training documented in the literature," wrote Mr. Matthew E. Platta and his colleagues in a study that was published in the Journal of the Neurological Sciences (2014 May 19 [doi:10.1016/j.jns.2014.05.016]).
Although reviews have shown the benefits of exercise for individuals with MS, none have looked at the risks of relapse and other AEs, Mr. Platta said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
Mr. Platta, a graduate student in the department of kinesiology and community health at the University of Illinois at Urbana-Champaign, and his colleagues analyzed 26 trials, including 1,295 participants. The trials were published up to November 2013 and examined the effect of exercise on MS relapses and adverse events. All trials included a nontreatment control arm.
The exercises included yoga, resistance training, aerobics, aquatics, and combined aerobics and resistance training.
Results showed that there were 26 relapses in the control groups, compared with 29 in the exercise group, corresponding with 6.3% and 4.6% of participants in the control and exercise groups, respectively.
The exercise group also had a 27% lower relative risk of relapse.
As for AEs, there were 5 in the control group, compared with 13 in the exercise group (or 1.2% and 2.0% in each group, respectively).
But the exercise group had a 67% higher relative risk of AEs, compared with the control group. However, the rate was not higher than the rates of AEs associated with exercise training in healthy populations, the researchers said.
The most common AEs in the control group were illness, ankle sprain, knee pain, and fall. The exercise group had additional AEs, including stroke, low back pain, trigeminal neuralgia, traffic accident, upper respiratory tract infection, rheumatoid arthritis flare up, and hernia. The most common types of AEs were musculoskeletal injuries (46%) and illnesses (23%).
"MS patients and clinicians can expect a low occurrence of AEs with exercise training, and, when AEs do occur, such events are commonly musculoskeletal in nature," Mr. Platta and his colleagues wrote.
There was no difference in the dropout rate between the two groups. The authors noted that "Future research might consider the inclusion of behavioral strategies for reducing dropout in RCTs of exercise training in MS."
They said that some of the analysis limitations include lack of complete reporting on the exercise training protocols, and potential for attention bias in the exercise group, compared with the control group.
Also, there was considerable variation in the type and prescription of exercises, they said. The sessions were between 1 and 5 days per week for 20-90 minutes per day. The duration of the programs was 4-24 weeks. Mr. Platta said there were too few trials to analyze the effect of different types of exercise separately.
The authors added that it is also important to record frequency and severity of temporary symptomatic changes in response to acute exercise bouts.
"Take-home message is that, taking into account that there are a lot of benefits to exercise, our findings show that the amount of relapses and adverse events are not too high to prevent physicians from recommending exercise [to individuals with MS]."
Mr. Platta and his coauthors had no disclosures.
On Twitter @naseemsmiller
AT THE CMSC/ACTRIMS ANNUAL MEETING
Key clinical point: The frequency of relapses and adverse events are not too high to prevent physicians from recommending exercise to individuals with MS.
Major finding: Persons with MS who exercised had 27% lower risk of relapse, compared with patients who didn’t exercise, and 67% higher risk of adverse events, but the rate was no higher than adverse events in healthy populations.
Data source: Analysis of 26 randomized trials, including 1,295 participants with MS.
Disclosures: Mr. Platta and his coauthors had no disclosures.
VIDEO: New MS database could change practice
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE CMSC/ACTRIMS ANNUAL MEETING
New obesity algorithm covers complications in addition to BMI
LAS VEGAS– A newly introduced statement proposes to change how obesity is diagnosed and treated.
The American Association of Clinical Endocrinologists and the American College of Endocrinology are suggesting algorithms to determine stages for the disease, each of which comes with a set of therapy recommendations.
"Right now it’s obesity, or overweight/obesity, or Class 1, 2, 3 obesity – it’s all [body mass index]. BMI doesn’t convey actionability. It doesn’t convey a medical meaning," said Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee at the annual meeting of the American Association of Clinical Endocrinologists.
AACE/ACE leaders hope that their new diagnostic algorithm will fill that gap.
"We’re using weight loss therapy to treat the complications of obesity in a medical model," Dr. Garvey said.
According to the framework, which is not finalized yet, the diagnostic categories of obesity will be:
• Overweight: BMI of 25-29.9 kg/m2, with no obesity-related complications.
• Obesity Stage 0: BMI of at least 30, with no obesity-related complications.
• Obesity Stage 1: BMI of at least 25 and one or more complications that are mild to moderate in severity.
• Obesity stage 2: BMI of greater than or equal to 25 and one or more severe complications.
Also, a four-step diagnosis and treatment approach is recommended for all patients:
1. BMI screening and adjusting for ethnic differences.
2. Clinical evaluation for the presence of obesity-related complications, by using a checklist.
3. Staging for the severity of complications using complication-specific criteria.
4. Selection of prevention and/or intervention strategies targeting specific complications guided by the AACE/ACE obesity management algorithm.
AACE/ACE leaders pointed out that today there are better tools to treat obesity than ever before, including improvements in lifestyle intervention, new medications, and improvements in bariatric surgery, yet there’s limited access and penetrance of these tools in the clinic. They said they hoped the new algorithm would help incorporate available therapies into treating obese patients.
The algorithm emerged from the AACE/ACE 2014 Consensus Conference on Obesity, which included medical professionals, industry representatives, advocacy groups, and regulators. One of the findings that everyone agreed on was that the diagnostic definition of obesity needed to improve.
The current definition of obesity "didn’t give all the stakeholders a reason to buy into a concerted plan." Employers would say, "I bring somebody down from a BMI of 38 to 34. But what does that mean? "How is it benefiting me? How is it benefiting my company? Why would I want to invest in that? But if they’re treating Stage 2, that’s telling them that that person is overweight, has excessive body fat, and it’s impacting their health and they have complications that can be remedied by weight loss and use of more aggressive therapies. All of that is embedded in that simple term," Dr. Garvey said.
The AACE/ACE is not the first to issue a diagnosis or treatment guideline for obesity, which was declared a disease by the American Medical Association in 2013.
There are a lot of commonalities to the guidelines," said Dr. Garvey, professor and chair at the department of Nutrition Sciences at the University of Alabama at Birmingham. They’re all addressing obesity and therapy and attempt to improve patients’ health. "I think we’re more focused on using weight loss as a therapy to treat obesity-related complications," Dr. Garvey said.
AACE/ACE is holding another consensus conference later this year as a step toward finalizing the framework.
Dr. Garvey is a consultant for Daiichi Sankyo, Liposcience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, Astra Zeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @naseemmiller
LAS VEGAS– A newly introduced statement proposes to change how obesity is diagnosed and treated.
The American Association of Clinical Endocrinologists and the American College of Endocrinology are suggesting algorithms to determine stages for the disease, each of which comes with a set of therapy recommendations.
"Right now it’s obesity, or overweight/obesity, or Class 1, 2, 3 obesity – it’s all [body mass index]. BMI doesn’t convey actionability. It doesn’t convey a medical meaning," said Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee at the annual meeting of the American Association of Clinical Endocrinologists.
AACE/ACE leaders hope that their new diagnostic algorithm will fill that gap.
"We’re using weight loss therapy to treat the complications of obesity in a medical model," Dr. Garvey said.
According to the framework, which is not finalized yet, the diagnostic categories of obesity will be:
• Overweight: BMI of 25-29.9 kg/m2, with no obesity-related complications.
• Obesity Stage 0: BMI of at least 30, with no obesity-related complications.
• Obesity Stage 1: BMI of at least 25 and one or more complications that are mild to moderate in severity.
• Obesity stage 2: BMI of greater than or equal to 25 and one or more severe complications.
Also, a four-step diagnosis and treatment approach is recommended for all patients:
1. BMI screening and adjusting for ethnic differences.
2. Clinical evaluation for the presence of obesity-related complications, by using a checklist.
3. Staging for the severity of complications using complication-specific criteria.
4. Selection of prevention and/or intervention strategies targeting specific complications guided by the AACE/ACE obesity management algorithm.
AACE/ACE leaders pointed out that today there are better tools to treat obesity than ever before, including improvements in lifestyle intervention, new medications, and improvements in bariatric surgery, yet there’s limited access and penetrance of these tools in the clinic. They said they hoped the new algorithm would help incorporate available therapies into treating obese patients.
The algorithm emerged from the AACE/ACE 2014 Consensus Conference on Obesity, which included medical professionals, industry representatives, advocacy groups, and regulators. One of the findings that everyone agreed on was that the diagnostic definition of obesity needed to improve.
The current definition of obesity "didn’t give all the stakeholders a reason to buy into a concerted plan." Employers would say, "I bring somebody down from a BMI of 38 to 34. But what does that mean? "How is it benefiting me? How is it benefiting my company? Why would I want to invest in that? But if they’re treating Stage 2, that’s telling them that that person is overweight, has excessive body fat, and it’s impacting their health and they have complications that can be remedied by weight loss and use of more aggressive therapies. All of that is embedded in that simple term," Dr. Garvey said.
The AACE/ACE is not the first to issue a diagnosis or treatment guideline for obesity, which was declared a disease by the American Medical Association in 2013.
There are a lot of commonalities to the guidelines," said Dr. Garvey, professor and chair at the department of Nutrition Sciences at the University of Alabama at Birmingham. They’re all addressing obesity and therapy and attempt to improve patients’ health. "I think we’re more focused on using weight loss as a therapy to treat obesity-related complications," Dr. Garvey said.
AACE/ACE is holding another consensus conference later this year as a step toward finalizing the framework.
Dr. Garvey is a consultant for Daiichi Sankyo, Liposcience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, Astra Zeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @naseemmiller
LAS VEGAS– A newly introduced statement proposes to change how obesity is diagnosed and treated.
The American Association of Clinical Endocrinologists and the American College of Endocrinology are suggesting algorithms to determine stages for the disease, each of which comes with a set of therapy recommendations.
"Right now it’s obesity, or overweight/obesity, or Class 1, 2, 3 obesity – it’s all [body mass index]. BMI doesn’t convey actionability. It doesn’t convey a medical meaning," said Dr. W. Timothy Garvey, chair of the AACE Obesity Scientific Committee at the annual meeting of the American Association of Clinical Endocrinologists.
AACE/ACE leaders hope that their new diagnostic algorithm will fill that gap.
"We’re using weight loss therapy to treat the complications of obesity in a medical model," Dr. Garvey said.
According to the framework, which is not finalized yet, the diagnostic categories of obesity will be:
• Overweight: BMI of 25-29.9 kg/m2, with no obesity-related complications.
• Obesity Stage 0: BMI of at least 30, with no obesity-related complications.
• Obesity Stage 1: BMI of at least 25 and one or more complications that are mild to moderate in severity.
• Obesity stage 2: BMI of greater than or equal to 25 and one or more severe complications.
Also, a four-step diagnosis and treatment approach is recommended for all patients:
1. BMI screening and adjusting for ethnic differences.
2. Clinical evaluation for the presence of obesity-related complications, by using a checklist.
3. Staging for the severity of complications using complication-specific criteria.
4. Selection of prevention and/or intervention strategies targeting specific complications guided by the AACE/ACE obesity management algorithm.
AACE/ACE leaders pointed out that today there are better tools to treat obesity than ever before, including improvements in lifestyle intervention, new medications, and improvements in bariatric surgery, yet there’s limited access and penetrance of these tools in the clinic. They said they hoped the new algorithm would help incorporate available therapies into treating obese patients.
The algorithm emerged from the AACE/ACE 2014 Consensus Conference on Obesity, which included medical professionals, industry representatives, advocacy groups, and regulators. One of the findings that everyone agreed on was that the diagnostic definition of obesity needed to improve.
The current definition of obesity "didn’t give all the stakeholders a reason to buy into a concerted plan." Employers would say, "I bring somebody down from a BMI of 38 to 34. But what does that mean? "How is it benefiting me? How is it benefiting my company? Why would I want to invest in that? But if they’re treating Stage 2, that’s telling them that that person is overweight, has excessive body fat, and it’s impacting their health and they have complications that can be remedied by weight loss and use of more aggressive therapies. All of that is embedded in that simple term," Dr. Garvey said.
The AACE/ACE is not the first to issue a diagnosis or treatment guideline for obesity, which was declared a disease by the American Medical Association in 2013.
There are a lot of commonalities to the guidelines," said Dr. Garvey, professor and chair at the department of Nutrition Sciences at the University of Alabama at Birmingham. They’re all addressing obesity and therapy and attempt to improve patients’ health. "I think we’re more focused on using weight loss as a therapy to treat obesity-related complications," Dr. Garvey said.
AACE/ACE is holding another consensus conference later this year as a step toward finalizing the framework.
Dr. Garvey is a consultant for Daiichi Sankyo, Liposcience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, Astra Zeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @naseemmiller
AT AACE 2014
VIDEO: Endocrinology initiatives can improve transgender care
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
AT AACE 14
VIDEO: Hypogonadism, hypercortisolemia may mean anorexia in men
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM AACE 14
VIDEO: Coffee break at AACE – What I’ve learned
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT AACE 14
EXCLUSIVE VIDEO: MERS – What physicians need to know
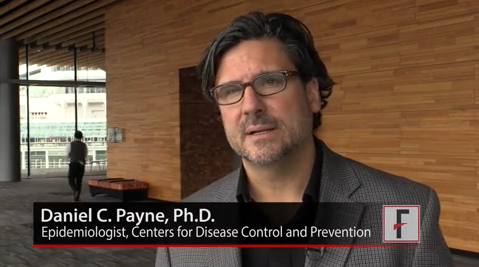
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
How big a worry is MERS for U.S. physicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged physicians to check the CDC website for the latest updates and practice protocols. Physicians can also visit the World Health Organization’s website for the latest global updates.
On Twitter @naseemmiller
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
How big a worry is MERS for U.S. physicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged physicians to check the CDC website for the latest updates and practice protocols. Physicians can also visit the World Health Organization’s website for the latest global updates.
On Twitter @naseemmiller
VANCOUVER, B.C. – Dr. Daniel C. Payne has been investigating the Middle East Respiratory Syndrome coronavirus since the first case was reported in the Arabian Peninsula nearly 2 years ago.
An epidemiologist with the Centers for Disease Control and Prevention, Dr. Payne has traveled to the sites of outbreak and has worked with foreign officials to study and track down the virus.
Meanwhile, in the United States, CDC officials have been preparing for the potential arrival of the virus for the past year, Dr. Payne said. So when the first case was confirmed on May 2 in Munster, Ind., all the pieces were in place and health officials were ready.
How big a worry is MERS for U.S. physicians, what critical questions should they ask their patients, and what precautions should they take? Dr. Payne addressed some of these major concerns in a video interview during the annual meeting of the Pediatric Academic Societies and shared the silver lining to the virus’s arrival in the United States.
He also encouraged physicians to check the CDC website for the latest updates and practice protocols. Physicians can also visit the World Health Organization’s website for the latest global updates.
On Twitter @naseemmiller
AT THE PAS ANNUAL MEETING