User login
What is the best approach to benign paroxysmal positional vertigo in the elderly?
A CANALITH REPOSITIONING MANEUVER (CRM), such as the Epley or Semont maneuver, should be the first-line treatment for benign paroxysmal positional vertigo (BPPV) in the elderly (strength of recommendation [SOR]: A, several good-quality randomized controlled trials [RCTs]).
Following the Epley maneuver with self-treatment at home using a modified Epley procedure improves outcomes (SOR: B, a single good-quality RCT). Postural restrictions aren’t necessary after CRM treatment (SOR: A, several good-quality RCTs).
Medications don’t work as well as a CRM, but studies comparing treatments are limited (SOR: B, a single good-quality RCT).
Evidence summary
No epidemiologic data on BPPV in the United States are available, but experts describe increasing incidence with advancing age. A recent German study found a lifetime prevalence of 2.4%, with a cumulative incidence approaching 10% by age 80.1 Treatments include repositioning maneuvers (regimens of positioning the patient’s head and body) and medication. Evidence about treating BPPV in elderly patients specifically is limited.2-4
These 2 maneuvers work best
Both Epley’s CRM and Semont’s liberatory maneuver have been shown to treat BPPV effectively. (For descriptions of the maneuvers and video links, see “How the Epley and Semont maneuvers work”.)
An RCT with 124 participants (mean age 58.3 years) demonstrated that either Epley’s or Semont’s maneuver decreased the frequency of vertigo more than a sham maneuver (P=.021 and P=.010, respectively).5 Both maneuvers were more effective than the Brandt-Daroff home exercises (P=.033).5
Another high-quality, double-blind RCT with 67 participants (median age 59 years) reported an improvement in vertigo and nystagmus at 24 hours among 80% of patients treated with Epley’s CRM, compared with 10% of those who received a sham maneuver (P<.001; number needed to treat [NNT]=1; 95% confidence interval [CI], 1-2).6
An RCT that enrolled 80 participants (median age 64 years) found complete resolution of BPPV symptoms and a negative Dix-Hallpike test 1 week after treatment in 88% of patients who received Epley’s CRM plus self-treatment (a modified Epley’s maneuver) compared with 69% who received Epley’s CRM alone (P=.048; NNT=5; 95% CI, 3-124).7
THE EPLEY MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the right, then lies down quickly on the table on a pillow positioned under her shoulders. After maintaining this position for 30 seconds, the patient turns her head 90° to the left without raising it from the table and waits 30 more seconds. The patient then turns her head and body as a unit 90° to the left and waits another 30 seconds before sitting up on the left side of the table.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but would begin with her head positioned to the left side, eventually rotating her body to the right side, and end by sitting up on the right side of the exam table.
The following link leads to a video showing the modified Epley’s CRM for treating right-ear, posterior canal BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video2.mpg
THE SEMONT MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the left, then drops rapidly to the right side so that her head contacts the table just behind the right ear. After waiting in this position for 30 seconds, the patient moves quickly and smoothly toward the left side (without stopping in the upright position) so that the left side of her forehead rests on the exam table. She holds this position for 30 seconds, then sits upright again.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but begin with her head positioned to the right side.
The following link leads to a video demonstrating Semont’s liberatory maneuver for treating right-ear BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video1.mpg
Posture restrictions are unnecessary
An RCT involving 50 participants (mean age 60.9 years) demonstrated that postprocedure postural restrictions were unnecessary and didn’t improve BPPV remission rates among patients receiving CRM (P=.97). No differences were noted by age or sex.8 Two prospective nonrandomized studies found that the recurrence rate of BPPV symptoms was 15% to 18% at 12 months and 37% to 50% at 40 to 60 months.9,10
Drug studies are scarce, but CRM appears to work better
Studies of drug treatment among patients with BPPV are extremely limited because BPPV as a cause of vertigo is often an exclusion criterion among medication trials. A small (N=20; age range 32-67 years) double-blinded RCT found no difference in dizziness symptom scores for participants with BPPV who took diazepam (5 mg, 3 times daily), lorazepam (1 mg, 3 times daily), or placebo (1 capsule, 3 times daily) over a period of 4 weeks.11
An RCT of 156 patients (mean age 74 years) with BPPV compared a calcium channel blocker (flunarizine, which isn’t available in the United States) with Semont’s liberatory maneuver or no therapy (observation only). Semont’s maneuver was more effective at the 6-month follow-up than either the calcium channel blocker or no therapy; the rates of asymptomatic patients with a negative Dix-Hallpike test at follow-up were 94%, 58%, and 34%, respectively (P<.001).3
Although meclizine is often used in clinical practice, only 1 double-blind RCT from 1972 (N=31, age range 21-77 years) reported improvement in symptoms and physical findings for meclizine compared with placebo in patients with BPPV.12
Recommendations
In a review article, Furman and Cass describe the diagnostic maneuver (Dix-Hallpike) and treatment maneuver (Epley) for BPPV.13 They recommend using either Epley’s or Semont’s maneuver for initial treatment.
The authors noted that vestibular suppressant medications may decrease the intensity of symptoms but don’t reduce the frequency of recurrent vertigo attacks. Moreover, medications produce unwanted side effects (somnolence, lethargy, worsened balance) and may prove counterproductive by delaying the central nervous system’s adaptation to a peripheral vestibular abnormality.
1. von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710-715.
2. Lea P, Kushnir M, Shpirer Y, et al. Approach to benign paroxysmal positional vertigo in old age. Isr Med Assoc J. 2005;7:447-450.
3. Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004;114:827-831.
4. Angeli SI, Hawley R, Gomez O. Systematic approach to benign paroxysmal positional vertigo in the elderly. Otolaryngol Head Neck Surg. 2003;128:719-725.
5. Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005;26:1034-1040.
6. von Brevern M, Seelig T, Radtke A, et al. Short-term efficacy of Epley’s manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980-982.
7. Tanimoto H, Doi K, Katata K, et al. Self-treatment for benign paroxysmal positional vertigo of the posterior semicircular canal. Neurology. 2005;65:1299-1300.
8. Simoceli L, Bittar RS, Greters ME. Posture restrictions do not interfere in the results of canalith repositioning maneuver. Rev Bras Otorrinolaringol. 2005;71:55-59.
9. Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000;122:647-652.
10. Sakaida M, Takeuchi K, Ishinaga H, et al. Long-term outcome of benign paroxysmal positional vertigo. Neurology. 2003;60:1532-1534.
11. McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980;9:472-477.
12. Cohen B, DeJong JM. Meclizine and placebo in treating vertigo of vestibular origin. Relative efficacy in a double-blind study. Arch Neurol. 1972;27:129-135.
13. Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341:1590-1596.
A CANALITH REPOSITIONING MANEUVER (CRM), such as the Epley or Semont maneuver, should be the first-line treatment for benign paroxysmal positional vertigo (BPPV) in the elderly (strength of recommendation [SOR]: A, several good-quality randomized controlled trials [RCTs]).
Following the Epley maneuver with self-treatment at home using a modified Epley procedure improves outcomes (SOR: B, a single good-quality RCT). Postural restrictions aren’t necessary after CRM treatment (SOR: A, several good-quality RCTs).
Medications don’t work as well as a CRM, but studies comparing treatments are limited (SOR: B, a single good-quality RCT).
Evidence summary
No epidemiologic data on BPPV in the United States are available, but experts describe increasing incidence with advancing age. A recent German study found a lifetime prevalence of 2.4%, with a cumulative incidence approaching 10% by age 80.1 Treatments include repositioning maneuvers (regimens of positioning the patient’s head and body) and medication. Evidence about treating BPPV in elderly patients specifically is limited.2-4
These 2 maneuvers work best
Both Epley’s CRM and Semont’s liberatory maneuver have been shown to treat BPPV effectively. (For descriptions of the maneuvers and video links, see “How the Epley and Semont maneuvers work”.)
An RCT with 124 participants (mean age 58.3 years) demonstrated that either Epley’s or Semont’s maneuver decreased the frequency of vertigo more than a sham maneuver (P=.021 and P=.010, respectively).5 Both maneuvers were more effective than the Brandt-Daroff home exercises (P=.033).5
Another high-quality, double-blind RCT with 67 participants (median age 59 years) reported an improvement in vertigo and nystagmus at 24 hours among 80% of patients treated with Epley’s CRM, compared with 10% of those who received a sham maneuver (P<.001; number needed to treat [NNT]=1; 95% confidence interval [CI], 1-2).6
An RCT that enrolled 80 participants (median age 64 years) found complete resolution of BPPV symptoms and a negative Dix-Hallpike test 1 week after treatment in 88% of patients who received Epley’s CRM plus self-treatment (a modified Epley’s maneuver) compared with 69% who received Epley’s CRM alone (P=.048; NNT=5; 95% CI, 3-124).7
THE EPLEY MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the right, then lies down quickly on the table on a pillow positioned under her shoulders. After maintaining this position for 30 seconds, the patient turns her head 90° to the left without raising it from the table and waits 30 more seconds. The patient then turns her head and body as a unit 90° to the left and waits another 30 seconds before sitting up on the left side of the table.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but would begin with her head positioned to the left side, eventually rotating her body to the right side, and end by sitting up on the right side of the exam table.
The following link leads to a video showing the modified Epley’s CRM for treating right-ear, posterior canal BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video2.mpg
THE SEMONT MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the left, then drops rapidly to the right side so that her head contacts the table just behind the right ear. After waiting in this position for 30 seconds, the patient moves quickly and smoothly toward the left side (without stopping in the upright position) so that the left side of her forehead rests on the exam table. She holds this position for 30 seconds, then sits upright again.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but begin with her head positioned to the right side.
The following link leads to a video demonstrating Semont’s liberatory maneuver for treating right-ear BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video1.mpg
Posture restrictions are unnecessary
An RCT involving 50 participants (mean age 60.9 years) demonstrated that postprocedure postural restrictions were unnecessary and didn’t improve BPPV remission rates among patients receiving CRM (P=.97). No differences were noted by age or sex.8 Two prospective nonrandomized studies found that the recurrence rate of BPPV symptoms was 15% to 18% at 12 months and 37% to 50% at 40 to 60 months.9,10
Drug studies are scarce, but CRM appears to work better
Studies of drug treatment among patients with BPPV are extremely limited because BPPV as a cause of vertigo is often an exclusion criterion among medication trials. A small (N=20; age range 32-67 years) double-blinded RCT found no difference in dizziness symptom scores for participants with BPPV who took diazepam (5 mg, 3 times daily), lorazepam (1 mg, 3 times daily), or placebo (1 capsule, 3 times daily) over a period of 4 weeks.11
An RCT of 156 patients (mean age 74 years) with BPPV compared a calcium channel blocker (flunarizine, which isn’t available in the United States) with Semont’s liberatory maneuver or no therapy (observation only). Semont’s maneuver was more effective at the 6-month follow-up than either the calcium channel blocker or no therapy; the rates of asymptomatic patients with a negative Dix-Hallpike test at follow-up were 94%, 58%, and 34%, respectively (P<.001).3
Although meclizine is often used in clinical practice, only 1 double-blind RCT from 1972 (N=31, age range 21-77 years) reported improvement in symptoms and physical findings for meclizine compared with placebo in patients with BPPV.12
Recommendations
In a review article, Furman and Cass describe the diagnostic maneuver (Dix-Hallpike) and treatment maneuver (Epley) for BPPV.13 They recommend using either Epley’s or Semont’s maneuver for initial treatment.
The authors noted that vestibular suppressant medications may decrease the intensity of symptoms but don’t reduce the frequency of recurrent vertigo attacks. Moreover, medications produce unwanted side effects (somnolence, lethargy, worsened balance) and may prove counterproductive by delaying the central nervous system’s adaptation to a peripheral vestibular abnormality.
A CANALITH REPOSITIONING MANEUVER (CRM), such as the Epley or Semont maneuver, should be the first-line treatment for benign paroxysmal positional vertigo (BPPV) in the elderly (strength of recommendation [SOR]: A, several good-quality randomized controlled trials [RCTs]).
Following the Epley maneuver with self-treatment at home using a modified Epley procedure improves outcomes (SOR: B, a single good-quality RCT). Postural restrictions aren’t necessary after CRM treatment (SOR: A, several good-quality RCTs).
Medications don’t work as well as a CRM, but studies comparing treatments are limited (SOR: B, a single good-quality RCT).
Evidence summary
No epidemiologic data on BPPV in the United States are available, but experts describe increasing incidence with advancing age. A recent German study found a lifetime prevalence of 2.4%, with a cumulative incidence approaching 10% by age 80.1 Treatments include repositioning maneuvers (regimens of positioning the patient’s head and body) and medication. Evidence about treating BPPV in elderly patients specifically is limited.2-4
These 2 maneuvers work best
Both Epley’s CRM and Semont’s liberatory maneuver have been shown to treat BPPV effectively. (For descriptions of the maneuvers and video links, see “How the Epley and Semont maneuvers work”.)
An RCT with 124 participants (mean age 58.3 years) demonstrated that either Epley’s or Semont’s maneuver decreased the frequency of vertigo more than a sham maneuver (P=.021 and P=.010, respectively).5 Both maneuvers were more effective than the Brandt-Daroff home exercises (P=.033).5
Another high-quality, double-blind RCT with 67 participants (median age 59 years) reported an improvement in vertigo and nystagmus at 24 hours among 80% of patients treated with Epley’s CRM, compared with 10% of those who received a sham maneuver (P<.001; number needed to treat [NNT]=1; 95% confidence interval [CI], 1-2).6
An RCT that enrolled 80 participants (median age 64 years) found complete resolution of BPPV symptoms and a negative Dix-Hallpike test 1 week after treatment in 88% of patients who received Epley’s CRM plus self-treatment (a modified Epley’s maneuver) compared with 69% who received Epley’s CRM alone (P=.048; NNT=5; 95% CI, 3-124).7
THE EPLEY MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the right, then lies down quickly on the table on a pillow positioned under her shoulders. After maintaining this position for 30 seconds, the patient turns her head 90° to the left without raising it from the table and waits 30 more seconds. The patient then turns her head and body as a unit 90° to the left and waits another 30 seconds before sitting up on the left side of the table.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but would begin with her head positioned to the left side, eventually rotating her body to the right side, and end by sitting up on the right side of the exam table.
The following link leads to a video showing the modified Epley’s CRM for treating right-ear, posterior canal BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video2.mpg
THE SEMONT MANEUVER
A patient with right-ear BPPV sits on the exam table with her head turned 45° to the left, then drops rapidly to the right side so that her head contacts the table just behind the right ear. After waiting in this position for 30 seconds, the patient moves quickly and smoothly toward the left side (without stopping in the upright position) so that the left side of her forehead rests on the exam table. She holds this position for 30 seconds, then sits upright again.
A patient with left-ear BPPV would perform the maneuver in a similar fashion, but begin with her head positioned to the right side.
The following link leads to a video demonstrating Semont’s liberatory maneuver for treating right-ear BPPV: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video1.mpg
Posture restrictions are unnecessary
An RCT involving 50 participants (mean age 60.9 years) demonstrated that postprocedure postural restrictions were unnecessary and didn’t improve BPPV remission rates among patients receiving CRM (P=.97). No differences were noted by age or sex.8 Two prospective nonrandomized studies found that the recurrence rate of BPPV symptoms was 15% to 18% at 12 months and 37% to 50% at 40 to 60 months.9,10
Drug studies are scarce, but CRM appears to work better
Studies of drug treatment among patients with BPPV are extremely limited because BPPV as a cause of vertigo is often an exclusion criterion among medication trials. A small (N=20; age range 32-67 years) double-blinded RCT found no difference in dizziness symptom scores for participants with BPPV who took diazepam (5 mg, 3 times daily), lorazepam (1 mg, 3 times daily), or placebo (1 capsule, 3 times daily) over a period of 4 weeks.11
An RCT of 156 patients (mean age 74 years) with BPPV compared a calcium channel blocker (flunarizine, which isn’t available in the United States) with Semont’s liberatory maneuver or no therapy (observation only). Semont’s maneuver was more effective at the 6-month follow-up than either the calcium channel blocker or no therapy; the rates of asymptomatic patients with a negative Dix-Hallpike test at follow-up were 94%, 58%, and 34%, respectively (P<.001).3
Although meclizine is often used in clinical practice, only 1 double-blind RCT from 1972 (N=31, age range 21-77 years) reported improvement in symptoms and physical findings for meclizine compared with placebo in patients with BPPV.12
Recommendations
In a review article, Furman and Cass describe the diagnostic maneuver (Dix-Hallpike) and treatment maneuver (Epley) for BPPV.13 They recommend using either Epley’s or Semont’s maneuver for initial treatment.
The authors noted that vestibular suppressant medications may decrease the intensity of symptoms but don’t reduce the frequency of recurrent vertigo attacks. Moreover, medications produce unwanted side effects (somnolence, lethargy, worsened balance) and may prove counterproductive by delaying the central nervous system’s adaptation to a peripheral vestibular abnormality.
1. von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710-715.
2. Lea P, Kushnir M, Shpirer Y, et al. Approach to benign paroxysmal positional vertigo in old age. Isr Med Assoc J. 2005;7:447-450.
3. Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004;114:827-831.
4. Angeli SI, Hawley R, Gomez O. Systematic approach to benign paroxysmal positional vertigo in the elderly. Otolaryngol Head Neck Surg. 2003;128:719-725.
5. Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005;26:1034-1040.
6. von Brevern M, Seelig T, Radtke A, et al. Short-term efficacy of Epley’s manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980-982.
7. Tanimoto H, Doi K, Katata K, et al. Self-treatment for benign paroxysmal positional vertigo of the posterior semicircular canal. Neurology. 2005;65:1299-1300.
8. Simoceli L, Bittar RS, Greters ME. Posture restrictions do not interfere in the results of canalith repositioning maneuver. Rev Bras Otorrinolaringol. 2005;71:55-59.
9. Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000;122:647-652.
10. Sakaida M, Takeuchi K, Ishinaga H, et al. Long-term outcome of benign paroxysmal positional vertigo. Neurology. 2003;60:1532-1534.
11. McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980;9:472-477.
12. Cohen B, DeJong JM. Meclizine and placebo in treating vertigo of vestibular origin. Relative efficacy in a double-blind study. Arch Neurol. 1972;27:129-135.
13. Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341:1590-1596.
1. von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710-715.
2. Lea P, Kushnir M, Shpirer Y, et al. Approach to benign paroxysmal positional vertigo in old age. Isr Med Assoc J. 2005;7:447-450.
3. Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004;114:827-831.
4. Angeli SI, Hawley R, Gomez O. Systematic approach to benign paroxysmal positional vertigo in the elderly. Otolaryngol Head Neck Surg. 2003;128:719-725.
5. Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005;26:1034-1040.
6. von Brevern M, Seelig T, Radtke A, et al. Short-term efficacy of Epley’s manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980-982.
7. Tanimoto H, Doi K, Katata K, et al. Self-treatment for benign paroxysmal positional vertigo of the posterior semicircular canal. Neurology. 2005;65:1299-1300.
8. Simoceli L, Bittar RS, Greters ME. Posture restrictions do not interfere in the results of canalith repositioning maneuver. Rev Bras Otorrinolaringol. 2005;71:55-59.
9. Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000;122:647-652.
10. Sakaida M, Takeuchi K, Ishinaga H, et al. Long-term outcome of benign paroxysmal positional vertigo. Neurology. 2003;60:1532-1534.
11. McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980;9:472-477.
12. Cohen B, DeJong JM. Meclizine and placebo in treating vertigo of vestibular origin. Relative efficacy in a double-blind study. Arch Neurol. 1972;27:129-135.
13. Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341:1590-1596.
Evidence-based answers from the Family Physicians Inquiries Network
What is the best way to evaluate an acute traumatic knee injury?
Use the Ottawa Knee Rules. When there is a possibility of fracture, they can guide the use of radiography in adults who present with isolated knee pain. However, information on use of these rules in the pediatric population is limited (strength of recommendation [SOR]: A, based on systematic review of high-quality studies and a validated clinical decision rule). Specific physical examination maneuvers (such as the Lachman and McMurray tests) may be helpful when assessing for meniscal or ligamentous injury (SOR: C, based on studies of intermediate outcomes).
Sonographic examination of a traumatized knee can accurately detect internal knee derangement (SOR: C, based on studies of intermediate outcomes). Magnetic resonance imaging (MRI) of the knee is the noninvasive standard for diagnosing internal knee derangement, and it is useful for both adult and pediatric patients (SOR: C, based on studies of intermediate outcomes).
Ottawa rules for ankles—yes, but they’re good for knees, too
Daniel Spogen, MD
University of Nevada, Reno
The evidence presented here suggests a number of practical and useful approaches for the evaluation of acute knee injury—something that’s especially helpful for family physicians and those who, like me, have worked a lot of sporting events.
The Ottawa rules, which can be used to rule out fracture without an x-ray, are fairly well known for ankle injuries, but are not as well known for knees. A Lachman test, Drawer sign, and McMurray test are useful in diagnosing the presence of internal ligamentous injuries without MRI, and an ultrasound can help to detect knee effusion when it is not clinically obvious.
A good physical examination and an ultrasound can effectively rule out serious knee injury with high specificity. When serious injury is suspected, x-ray and MRI are very useful for fracture and ligamentous injury, respectively.
Evidence summary
These criteria help determine who needs an x-ray
The Ottawa Knee Rules recommend knee x-rays for any patient meeting one of these criteria:1
- ≥55 years of age
- Tenderness over the head of the fibula or isolated to the patella without other bony tenderness
- Unable to flex the knee to 90°, or unable to bear weight (for at least 4 steps) both immediately and in the emergency department.
Ottawa rules for knee x-ray
A knee x-ray is required only for knee injury patients with any of these findings:
- 55 years of age or older
- isolated tenderness of the patella (no bone tenderness of the knee other than the patella)
- tenderness at the head of the fibula
- inability to flex the knee to 90°
- inability to weight bear both immediately and in the ED (4 steps, unable to transfer weight twice onto each lower limb regardless of limping). (www.gp-training.net/rheum/ottawa.htm)
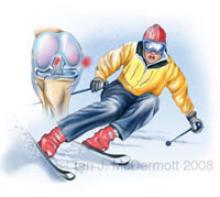
A downhill skier is catching the inside edge of the front of a ski in the snow, forcing external rotation of the tibia relative to the femur. The detail of the knee joint shows injury to the medial collateral ligament and anterior cruciate ligament.
In a systematic review,2 the Ottawa rules had a pooled negative likelihood ratio (LR–) of 0.05 (95% confidence interval [CI], 0.02–0.23). A prospective study of the Ottawa rules among children with acute knee injury demonstrated a positive likelihood ratio (LR+) of 1.81 (95% CI, 1.47–2.21) and an LR– of 0.16 (95% CI, 0.02–1.04).3 However, limited information is available in the pediatric population.
Ultrasound and MRI both perform well
Physical examination (including the Lachman test, Drawer sign, and McMurray test) by an orthopedist or sports medicine–trained physician was 74% to 88% sensitive and 72% to 95% specific for suspected meniscal or ligamentous injuries; MRI added marginal value in referral decisions regarding these conditions.4
In a small nonrandomized study of adult knee trauma, sonographic diagnosis of an effusion (by an expert) had an LR+ for diagnosing an internal derangement of the knee of 2.0 (95% CI, 0.67–5.96) and an LR– of 0.33 (95% CI, 0.12–0.96), as compared with the gold standard of MRI.5
In a nonrandomized prospective study of adults receiving MRI of the knee prior to arthroscopy, MRI identified meniscal and ligamentous lesions of the knee satisfactorily (Table 1).6 In a retrospective study of adolescents (11 to 17 years of age) having knee MRIs and undergoing knee surgery, MRI compared favorably with the operative (gold standard) diagnosis (Table 2).7
TABLE 1
MRI can accurately identify meniscal and ligamentous knee lesions in adults
| INJURY | LR+ | LR– |
|---|---|---|
| Medial meniscus | 13.7 | 0.02 |
| Lateral meniscus | 14.3 | 0.08 |
| Anterior cruciate ligament | 21.5 | 0.01 |
| Posterior cruciate ligament | 100 | 0.01 |
| Intra-articular cartilage lesion | 14.9 | 0.25 |
| *Adapted from Vaz et al,2005.6 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio. | ||
TABLE 2
MRI compares well with operative Dx in identifying knee lesions in adolescents
| INJURY | LR+ (95% CI) | LR– (95% CI) |
|---|---|---|
| Medial meniscus | 7.18 (3.34–15.46) | 0.10 (0.01–0.63) |
| Lateral meniscus | 20.53 (5.27–80.07) | 0.07 (0.01–0.46) |
| Anterior cruciate ligament | 100 | 0 |
| *Adapted from Major et al, 2003.7 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio; CI, confidence interval. | ||
Recommendations from others
University of Michigan Health System8 guidelines indicate the following:
- Most knee pain is caused by patellofemoral syndrome and osteoarthritis.
- MRI of the knee has not been proven to be superior to the clinical exam by an experienced examiner in the evaluation of acute knee injuries.
- MRI may be useful to assess bone pathology underlying chronic knee pain.
- Differentiating between knee pain without constitutional symptoms, knee pain with constitutional symptoms, and traumatic knee pain is helpful in determining a diagnosis.
- Patients with knee pain and swelling who have non-bloody aspirates may also have serious knee pathology.
1. Stiell IG, Greenberg GH, Wells GA, et al. Derivation of a decision rule for the use of radiography in acute knee injuries. Ann Emerg Med 1995;26:405-413.
2. Bachmann LM, Haberzeth S, Steurer J, ter Riet G. The accuracy of the Ottawa Knee Rule to rule out knee fractures: a systematic review. Ann Intern Med 2004;140:121-124.
3. Khine H, Dorfman DH, Avner JR. Applicability of Ottawa Knee Rule for knee injury in children. Pediatr Emerg Care 2001;17:401-404.
4. Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003;139:575-588.
5. Wang C-Y, Wang H-K, Hsu C-Y, Shieh J-Y, Wang TG, Jiang C-C. Role of sonographic examination in traumatic knee internal derangement. Arch Physical Med Rehab 2007;88:984-987.
6. Vaz CE, Camargo OP, Santana PJ, Valezi AC. Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics 2005;60:445-450.
7. Major NM, Beard LN, Jr, Helms CA. Accuracy of MR imaging of the knee in adolescents. AJR Am J Roentgenol 2003;180:17-19.
8. University of Michigan Health system Knee pain or swelling: acute or chronic. Ann Arbor: University of Michigan Health System; 2005. Available at: cme.med.umich.edu/pdf/guideline/knee.pdf. Accessed January 7, 2008.
Use the Ottawa Knee Rules. When there is a possibility of fracture, they can guide the use of radiography in adults who present with isolated knee pain. However, information on use of these rules in the pediatric population is limited (strength of recommendation [SOR]: A, based on systematic review of high-quality studies and a validated clinical decision rule). Specific physical examination maneuvers (such as the Lachman and McMurray tests) may be helpful when assessing for meniscal or ligamentous injury (SOR: C, based on studies of intermediate outcomes).
Sonographic examination of a traumatized knee can accurately detect internal knee derangement (SOR: C, based on studies of intermediate outcomes). Magnetic resonance imaging (MRI) of the knee is the noninvasive standard for diagnosing internal knee derangement, and it is useful for both adult and pediatric patients (SOR: C, based on studies of intermediate outcomes).
Ottawa rules for ankles—yes, but they’re good for knees, too
Daniel Spogen, MD
University of Nevada, Reno
The evidence presented here suggests a number of practical and useful approaches for the evaluation of acute knee injury—something that’s especially helpful for family physicians and those who, like me, have worked a lot of sporting events.
The Ottawa rules, which can be used to rule out fracture without an x-ray, are fairly well known for ankle injuries, but are not as well known for knees. A Lachman test, Drawer sign, and McMurray test are useful in diagnosing the presence of internal ligamentous injuries without MRI, and an ultrasound can help to detect knee effusion when it is not clinically obvious.
A good physical examination and an ultrasound can effectively rule out serious knee injury with high specificity. When serious injury is suspected, x-ray and MRI are very useful for fracture and ligamentous injury, respectively.
Evidence summary
These criteria help determine who needs an x-ray
The Ottawa Knee Rules recommend knee x-rays for any patient meeting one of these criteria:1
- ≥55 years of age
- Tenderness over the head of the fibula or isolated to the patella without other bony tenderness
- Unable to flex the knee to 90°, or unable to bear weight (for at least 4 steps) both immediately and in the emergency department.
Ottawa rules for knee x-ray
A knee x-ray is required only for knee injury patients with any of these findings:
- 55 years of age or older
- isolated tenderness of the patella (no bone tenderness of the knee other than the patella)
- tenderness at the head of the fibula
- inability to flex the knee to 90°
- inability to weight bear both immediately and in the ED (4 steps, unable to transfer weight twice onto each lower limb regardless of limping). (www.gp-training.net/rheum/ottawa.htm)
A downhill skier is catching the inside edge of the front of a ski in the snow, forcing external rotation of the tibia relative to the femur. The detail of the knee joint shows injury to the medial collateral ligament and anterior cruciate ligament.
In a systematic review,2 the Ottawa rules had a pooled negative likelihood ratio (LR–) of 0.05 (95% confidence interval [CI], 0.02–0.23). A prospective study of the Ottawa rules among children with acute knee injury demonstrated a positive likelihood ratio (LR+) of 1.81 (95% CI, 1.47–2.21) and an LR– of 0.16 (95% CI, 0.02–1.04).3 However, limited information is available in the pediatric population.
Ultrasound and MRI both perform well
Physical examination (including the Lachman test, Drawer sign, and McMurray test) by an orthopedist or sports medicine–trained physician was 74% to 88% sensitive and 72% to 95% specific for suspected meniscal or ligamentous injuries; MRI added marginal value in referral decisions regarding these conditions.4
In a small nonrandomized study of adult knee trauma, sonographic diagnosis of an effusion (by an expert) had an LR+ for diagnosing an internal derangement of the knee of 2.0 (95% CI, 0.67–5.96) and an LR– of 0.33 (95% CI, 0.12–0.96), as compared with the gold standard of MRI.5
In a nonrandomized prospective study of adults receiving MRI of the knee prior to arthroscopy, MRI identified meniscal and ligamentous lesions of the knee satisfactorily (Table 1).6 In a retrospective study of adolescents (11 to 17 years of age) having knee MRIs and undergoing knee surgery, MRI compared favorably with the operative (gold standard) diagnosis (Table 2).7
TABLE 1
MRI can accurately identify meniscal and ligamentous knee lesions in adults
| INJURY | LR+ | LR– |
|---|---|---|
| Medial meniscus | 13.7 | 0.02 |
| Lateral meniscus | 14.3 | 0.08 |
| Anterior cruciate ligament | 21.5 | 0.01 |
| Posterior cruciate ligament | 100 | 0.01 |
| Intra-articular cartilage lesion | 14.9 | 0.25 |
| *Adapted from Vaz et al,2005.6 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio. | ||
TABLE 2
MRI compares well with operative Dx in identifying knee lesions in adolescents
| INJURY | LR+ (95% CI) | LR– (95% CI) |
|---|---|---|
| Medial meniscus | 7.18 (3.34–15.46) | 0.10 (0.01–0.63) |
| Lateral meniscus | 20.53 (5.27–80.07) | 0.07 (0.01–0.46) |
| Anterior cruciate ligament | 100 | 0 |
| *Adapted from Major et al, 2003.7 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio; CI, confidence interval. | ||
Recommendations from others
University of Michigan Health System8 guidelines indicate the following:
- Most knee pain is caused by patellofemoral syndrome and osteoarthritis.
- MRI of the knee has not been proven to be superior to the clinical exam by an experienced examiner in the evaluation of acute knee injuries.
- MRI may be useful to assess bone pathology underlying chronic knee pain.
- Differentiating between knee pain without constitutional symptoms, knee pain with constitutional symptoms, and traumatic knee pain is helpful in determining a diagnosis.
- Patients with knee pain and swelling who have non-bloody aspirates may also have serious knee pathology.
Use the Ottawa Knee Rules. When there is a possibility of fracture, they can guide the use of radiography in adults who present with isolated knee pain. However, information on use of these rules in the pediatric population is limited (strength of recommendation [SOR]: A, based on systematic review of high-quality studies and a validated clinical decision rule). Specific physical examination maneuvers (such as the Lachman and McMurray tests) may be helpful when assessing for meniscal or ligamentous injury (SOR: C, based on studies of intermediate outcomes).
Sonographic examination of a traumatized knee can accurately detect internal knee derangement (SOR: C, based on studies of intermediate outcomes). Magnetic resonance imaging (MRI) of the knee is the noninvasive standard for diagnosing internal knee derangement, and it is useful for both adult and pediatric patients (SOR: C, based on studies of intermediate outcomes).
Ottawa rules for ankles—yes, but they’re good for knees, too
Daniel Spogen, MD
University of Nevada, Reno
The evidence presented here suggests a number of practical and useful approaches for the evaluation of acute knee injury—something that’s especially helpful for family physicians and those who, like me, have worked a lot of sporting events.
The Ottawa rules, which can be used to rule out fracture without an x-ray, are fairly well known for ankle injuries, but are not as well known for knees. A Lachman test, Drawer sign, and McMurray test are useful in diagnosing the presence of internal ligamentous injuries without MRI, and an ultrasound can help to detect knee effusion when it is not clinically obvious.
A good physical examination and an ultrasound can effectively rule out serious knee injury with high specificity. When serious injury is suspected, x-ray and MRI are very useful for fracture and ligamentous injury, respectively.
Evidence summary
These criteria help determine who needs an x-ray
The Ottawa Knee Rules recommend knee x-rays for any patient meeting one of these criteria:1
- ≥55 years of age
- Tenderness over the head of the fibula or isolated to the patella without other bony tenderness
- Unable to flex the knee to 90°, or unable to bear weight (for at least 4 steps) both immediately and in the emergency department.
Ottawa rules for knee x-ray
A knee x-ray is required only for knee injury patients with any of these findings:
- 55 years of age or older
- isolated tenderness of the patella (no bone tenderness of the knee other than the patella)
- tenderness at the head of the fibula
- inability to flex the knee to 90°
- inability to weight bear both immediately and in the ED (4 steps, unable to transfer weight twice onto each lower limb regardless of limping). (www.gp-training.net/rheum/ottawa.htm)
A downhill skier is catching the inside edge of the front of a ski in the snow, forcing external rotation of the tibia relative to the femur. The detail of the knee joint shows injury to the medial collateral ligament and anterior cruciate ligament.
In a systematic review,2 the Ottawa rules had a pooled negative likelihood ratio (LR–) of 0.05 (95% confidence interval [CI], 0.02–0.23). A prospective study of the Ottawa rules among children with acute knee injury demonstrated a positive likelihood ratio (LR+) of 1.81 (95% CI, 1.47–2.21) and an LR– of 0.16 (95% CI, 0.02–1.04).3 However, limited information is available in the pediatric population.
Ultrasound and MRI both perform well
Physical examination (including the Lachman test, Drawer sign, and McMurray test) by an orthopedist or sports medicine–trained physician was 74% to 88% sensitive and 72% to 95% specific for suspected meniscal or ligamentous injuries; MRI added marginal value in referral decisions regarding these conditions.4
In a small nonrandomized study of adult knee trauma, sonographic diagnosis of an effusion (by an expert) had an LR+ for diagnosing an internal derangement of the knee of 2.0 (95% CI, 0.67–5.96) and an LR– of 0.33 (95% CI, 0.12–0.96), as compared with the gold standard of MRI.5
In a nonrandomized prospective study of adults receiving MRI of the knee prior to arthroscopy, MRI identified meniscal and ligamentous lesions of the knee satisfactorily (Table 1).6 In a retrospective study of adolescents (11 to 17 years of age) having knee MRIs and undergoing knee surgery, MRI compared favorably with the operative (gold standard) diagnosis (Table 2).7
TABLE 1
MRI can accurately identify meniscal and ligamentous knee lesions in adults
| INJURY | LR+ | LR– |
|---|---|---|
| Medial meniscus | 13.7 | 0.02 |
| Lateral meniscus | 14.3 | 0.08 |
| Anterior cruciate ligament | 21.5 | 0.01 |
| Posterior cruciate ligament | 100 | 0.01 |
| Intra-articular cartilage lesion | 14.9 | 0.25 |
| *Adapted from Vaz et al,2005.6 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio. | ||
TABLE 2
MRI compares well with operative Dx in identifying knee lesions in adolescents
| INJURY | LR+ (95% CI) | LR– (95% CI) |
|---|---|---|
| Medial meniscus | 7.18 (3.34–15.46) | 0.10 (0.01–0.63) |
| Lateral meniscus | 20.53 (5.27–80.07) | 0.07 (0.01–0.46) |
| Anterior cruciate ligament | 100 | 0 |
| *Adapted from Major et al, 2003.7 | ||
| MRI, magnetic resonance imaging; LR, likelihood ratio; CI, confidence interval. | ||
Recommendations from others
University of Michigan Health System8 guidelines indicate the following:
- Most knee pain is caused by patellofemoral syndrome and osteoarthritis.
- MRI of the knee has not been proven to be superior to the clinical exam by an experienced examiner in the evaluation of acute knee injuries.
- MRI may be useful to assess bone pathology underlying chronic knee pain.
- Differentiating between knee pain without constitutional symptoms, knee pain with constitutional symptoms, and traumatic knee pain is helpful in determining a diagnosis.
- Patients with knee pain and swelling who have non-bloody aspirates may also have serious knee pathology.
1. Stiell IG, Greenberg GH, Wells GA, et al. Derivation of a decision rule for the use of radiography in acute knee injuries. Ann Emerg Med 1995;26:405-413.
2. Bachmann LM, Haberzeth S, Steurer J, ter Riet G. The accuracy of the Ottawa Knee Rule to rule out knee fractures: a systematic review. Ann Intern Med 2004;140:121-124.
3. Khine H, Dorfman DH, Avner JR. Applicability of Ottawa Knee Rule for knee injury in children. Pediatr Emerg Care 2001;17:401-404.
4. Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003;139:575-588.
5. Wang C-Y, Wang H-K, Hsu C-Y, Shieh J-Y, Wang TG, Jiang C-C. Role of sonographic examination in traumatic knee internal derangement. Arch Physical Med Rehab 2007;88:984-987.
6. Vaz CE, Camargo OP, Santana PJ, Valezi AC. Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics 2005;60:445-450.
7. Major NM, Beard LN, Jr, Helms CA. Accuracy of MR imaging of the knee in adolescents. AJR Am J Roentgenol 2003;180:17-19.
8. University of Michigan Health system Knee pain or swelling: acute or chronic. Ann Arbor: University of Michigan Health System; 2005. Available at: cme.med.umich.edu/pdf/guideline/knee.pdf. Accessed January 7, 2008.
1. Stiell IG, Greenberg GH, Wells GA, et al. Derivation of a decision rule for the use of radiography in acute knee injuries. Ann Emerg Med 1995;26:405-413.
2. Bachmann LM, Haberzeth S, Steurer J, ter Riet G. The accuracy of the Ottawa Knee Rule to rule out knee fractures: a systematic review. Ann Intern Med 2004;140:121-124.
3. Khine H, Dorfman DH, Avner JR. Applicability of Ottawa Knee Rule for knee injury in children. Pediatr Emerg Care 2001;17:401-404.
4. Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003;139:575-588.
5. Wang C-Y, Wang H-K, Hsu C-Y, Shieh J-Y, Wang TG, Jiang C-C. Role of sonographic examination in traumatic knee internal derangement. Arch Physical Med Rehab 2007;88:984-987.
6. Vaz CE, Camargo OP, Santana PJ, Valezi AC. Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics 2005;60:445-450.
7. Major NM, Beard LN, Jr, Helms CA. Accuracy of MR imaging of the knee in adolescents. AJR Am J Roentgenol 2003;180:17-19.
8. University of Michigan Health system Knee pain or swelling: acute or chronic. Ann Arbor: University of Michigan Health System; 2005. Available at: cme.med.umich.edu/pdf/guideline/knee.pdf. Accessed January 7, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
What are effective medical treatments for adults with acute migraine?
Medications collectively referred to as “triptans” (eg, sumatriptan, naratriptan, etc) have been shown to be effective for acute migraine (strength of recommendation [SOR]: A). Nonsteroidal anti-inflammatory drugs (NSAIDs)—including aspirin, ibuprofen, naproxen sodium, diclofenac potassium, ketoprofen, tolfenamic acid, and ketorolac—are also effective (SOR: A). The combination of acetaminophen/aspirin/caffeine is effective (SOR: B). Parenteral dihydroergotamine (DHE), when administered with an antiemetic, is as effective as, or more effective than meperidine, valproate, or ketorolac (SOR: B). Prochlorperazine is more effective than metoclopramide in headache pain reduction (SOR: A). Isometheptene mucate/dichloralphenazone/acetaminophen is as effective as low-dose oral sumatriptan (SOR: B).
Inadequate response to medication? Increase dose or change route
Robert Sheeler, MD
Mayo Clinic, Rochester, Minn
For mild to moderate migraine headache attacks, NSAIDs or products containing acetaminophen and/or aspirin with caffeine or isometheptene mucate/dichloralphenazone/acetaminophen, when used intermittently, are frequently effective. More severe attacks generally respond better to migraine-specific medications such as triptans and ergot derivatives—the latter may be less likely to cause secondary rebound (analgesic overuse) headaches. Inadequate response to migraine-specific medication should prompt the prescriber to increase dose or change route to insure absorption (ie, nasal, rectal, or injectable).
Emerging evidence suggests combining a triptan plus an NSAID may produce higher response rates and more durable responses. Narcotics should generally be avoided. Valproate, ketorolac, IV magnesium, prochlorperazine, and metoclopramide are all somewhat effective for acute migraine, the latter 2 agents having the advantage of helping nausea but with the disadvantage of causing extrapyramidal reactions. A short course of oral steroids may break persistent attacks. Patients with frequent and intense headache patterns should be offered prophylactic therapy and not just abortive treatments.
Evidence summary
The prevalence of migraine headache is 6% among men and 15% to 17% among women.1 However, no standardized approach exists for the treatment of acute migraine headache. Systematic reviews of randomized controlled trials (RCTs) summarized that oral sumatriptan (Imitrex), eletriptan (Relpax), and rizatriptan (Maxalt) reduced migraine headache pain and increased the pain-free response rate for adults when compared with placebo.2-4 The number needed to treat (NNT) ranged from 3.9 to 9.9 for a given triptan’s lower dose to 2.6 to 5.1 for the higher dose.2-4 RCTs reported superior efficacy of oral almotriptan (Axert), frovatriptan (Frova), and zolmitriptan (Zomig), as well as intranasal sumatriptan and zolmitriptan when compared with placebo.
The following NSAIDs reduced headache severity more than placebo 2 hours after treatment: aspirin (1000 mg; NNT=2.4), ibuprofen (1200 mg; NNT=1.8), naproxen (750 mg; NNT=2.0), tolfenamic acid (not available in the US; NNT=1.2), and the combination product of acetaminophen/aspirin/caffeine (Excedrin Migraine, et al) (NNT=1.7).5 Acetaminophen 1000 mg orally has been reported to be superior to placebo for treating pain, functional disability, and photo/phonophobia among patients who did not require bedrest with their headaches and did not vomit more than 20% of the time. However, it was not superior to placebo when given intravenously for more severe acute migraine. No placebo-controlled trials exist for the use of ketorolac (Toradol); there are only comparison studies against other active migraine medications. Ketoprofen (Orudis) has placebo-controlled RCT data supporting its efficacy.
A meta-analysis6 of RCTs of parenteral metoclopramide (Reglan) revealed significant pain reduction (odds ratio [OR]=2.84; 95% confidence interval [CI], 1.05–7.68). When compared with other antiemetics (chlorpromazine [Thorazine] and prochlorperazine [Compazine]), metoclopramide was either less effective (OR=0.39; 95% CI, 0.18–0.87) or no different (OR=0.64; 95% CI, 0.23–1.76) than other therapies for reducing migraine pain. No difference was noted between parenteral metoclopramide and subcutaneous sumatriptan (OR=2.27; 95% CI, 0.64–8.11); however, metoclopramide was more effective than ibuprofen in pain reduction scores (standard deviation data missing in this study).
A systematic review7 revealed that dihydroergotamine (DHE) alone was less effective than subcutaneous sumatriptan in migraine pain reduction (OR=0.44; 95% CI, 0.25–0.77) or headache resolution (OR=0.05; 95% CI, 0.01–0.42). No differences were seen between DHE alone and chlorpromazine or lidocaine. Three studies revealed DHE plus metoclopramide was more effective than or equal to other agents for headache pain reduction at 2 hours: one vs ketorolac IM (OR=7; 95% CI, 0.86–56.89), one vs meperidine (Demerol) plus hydroxyzine (Vistaril, Atarax) IM (OR=47.67; 95% CI, 4.32–526.17), and one vs valproate IV (OR=0.67; 95% CI, 0.19–2.33).7 Specifically, treatment with DHE plus metoclopramide was superior to ketorolac for pain reduction (P=.03), but patients did not differ in disability scores (P=.06). DHE plus metoclopramide achieved greater reductions in pain scale scores than meperidine plus hydroxyzine (P<.001). No significant difference in pain reduction was noted between DHE plus metoclopramide and valproate (P=.36).
A multicenter, double-blind, randomized parallel group study8 showed no difference between the combination product isometheptene mucate, dichloralphenazone with acetaminophen (Midrin, Duradrin, etc) (used as recommended in the package insert with a maximum of up to 5 tablets within 24 hours) vs oral sumatriptan (initial dose of 25 mg with a repeat 25 mg dose in 2 hours). No placebo arm was used in this study.
Recommendations from others
The Institute for Clinical Systems Improvement recommends the use of vasoactive drugs over narcotics and barbiturates for treatment of moderately severe migraine headaches.9 The American Academy of Neurology recommends migraine-specific medications (triptans, DHE) for moderate to severe migraines or those mild to moderate migraines that responded poorly to NSAIDs or other over-the-counter preparations.10
1. Stewart WF, Shechter A, Rasmussen BK. Migraine prevalence: a review of population-based studies. Neurology 1994;44:S17-S23.
2. McCrory DC, Gray RN. Oral sumatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3)::CD002915.-
3. Oldman AD, Smith LA, McQuay HJ, Moore RA. Rizatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003221.-
4. Smith LA, Oldman AD, McQuay HJ, Moore RA. Eletriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003224.-
5. Snow V, Weiss K, Wall EM, Mottur-Pilson C. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med 2002;137:840-849.
6. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral metoclopramide for acute migraine: meta-analysis of randomised controlled trials. BMJ 2004;329:1369-1373.
7. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral dihydroergotamine for acute migraine headache: a systematic review of the literature. Ann Emerg Med 2005;45:393-401.
8. Freitag FG, Cady R, DiSerio F, et al. Comparative study of a combination of isometheptene mucate, dichloralphenazone with acetaminophen and sumatriptan succinate in the treatment of migraine. Headache 2001;41:391-398.
9. ICSI Health Care Guideline: Diagnosis and Treatment of Headache Bloomington, Minn: Institute for Clinical Systems Improvement (ICSI); 2004. Available at www.icsi.org/knowledge/detail.asp?catID=29&itemID=183. Accessed on May 17, 2006.
10. Silberstein SD. Practice Parameter: Evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:754-762.
Medications collectively referred to as “triptans” (eg, sumatriptan, naratriptan, etc) have been shown to be effective for acute migraine (strength of recommendation [SOR]: A). Nonsteroidal anti-inflammatory drugs (NSAIDs)—including aspirin, ibuprofen, naproxen sodium, diclofenac potassium, ketoprofen, tolfenamic acid, and ketorolac—are also effective (SOR: A). The combination of acetaminophen/aspirin/caffeine is effective (SOR: B). Parenteral dihydroergotamine (DHE), when administered with an antiemetic, is as effective as, or more effective than meperidine, valproate, or ketorolac (SOR: B). Prochlorperazine is more effective than metoclopramide in headache pain reduction (SOR: A). Isometheptene mucate/dichloralphenazone/acetaminophen is as effective as low-dose oral sumatriptan (SOR: B).
Inadequate response to medication? Increase dose or change route
Robert Sheeler, MD
Mayo Clinic, Rochester, Minn
For mild to moderate migraine headache attacks, NSAIDs or products containing acetaminophen and/or aspirin with caffeine or isometheptene mucate/dichloralphenazone/acetaminophen, when used intermittently, are frequently effective. More severe attacks generally respond better to migraine-specific medications such as triptans and ergot derivatives—the latter may be less likely to cause secondary rebound (analgesic overuse) headaches. Inadequate response to migraine-specific medication should prompt the prescriber to increase dose or change route to insure absorption (ie, nasal, rectal, or injectable).
Emerging evidence suggests combining a triptan plus an NSAID may produce higher response rates and more durable responses. Narcotics should generally be avoided. Valproate, ketorolac, IV magnesium, prochlorperazine, and metoclopramide are all somewhat effective for acute migraine, the latter 2 agents having the advantage of helping nausea but with the disadvantage of causing extrapyramidal reactions. A short course of oral steroids may break persistent attacks. Patients with frequent and intense headache patterns should be offered prophylactic therapy and not just abortive treatments.
Evidence summary
The prevalence of migraine headache is 6% among men and 15% to 17% among women.1 However, no standardized approach exists for the treatment of acute migraine headache. Systematic reviews of randomized controlled trials (RCTs) summarized that oral sumatriptan (Imitrex), eletriptan (Relpax), and rizatriptan (Maxalt) reduced migraine headache pain and increased the pain-free response rate for adults when compared with placebo.2-4 The number needed to treat (NNT) ranged from 3.9 to 9.9 for a given triptan’s lower dose to 2.6 to 5.1 for the higher dose.2-4 RCTs reported superior efficacy of oral almotriptan (Axert), frovatriptan (Frova), and zolmitriptan (Zomig), as well as intranasal sumatriptan and zolmitriptan when compared with placebo.
The following NSAIDs reduced headache severity more than placebo 2 hours after treatment: aspirin (1000 mg; NNT=2.4), ibuprofen (1200 mg; NNT=1.8), naproxen (750 mg; NNT=2.0), tolfenamic acid (not available in the US; NNT=1.2), and the combination product of acetaminophen/aspirin/caffeine (Excedrin Migraine, et al) (NNT=1.7).5 Acetaminophen 1000 mg orally has been reported to be superior to placebo for treating pain, functional disability, and photo/phonophobia among patients who did not require bedrest with their headaches and did not vomit more than 20% of the time. However, it was not superior to placebo when given intravenously for more severe acute migraine. No placebo-controlled trials exist for the use of ketorolac (Toradol); there are only comparison studies against other active migraine medications. Ketoprofen (Orudis) has placebo-controlled RCT data supporting its efficacy.
A meta-analysis6 of RCTs of parenteral metoclopramide (Reglan) revealed significant pain reduction (odds ratio [OR]=2.84; 95% confidence interval [CI], 1.05–7.68). When compared with other antiemetics (chlorpromazine [Thorazine] and prochlorperazine [Compazine]), metoclopramide was either less effective (OR=0.39; 95% CI, 0.18–0.87) or no different (OR=0.64; 95% CI, 0.23–1.76) than other therapies for reducing migraine pain. No difference was noted between parenteral metoclopramide and subcutaneous sumatriptan (OR=2.27; 95% CI, 0.64–8.11); however, metoclopramide was more effective than ibuprofen in pain reduction scores (standard deviation data missing in this study).
A systematic review7 revealed that dihydroergotamine (DHE) alone was less effective than subcutaneous sumatriptan in migraine pain reduction (OR=0.44; 95% CI, 0.25–0.77) or headache resolution (OR=0.05; 95% CI, 0.01–0.42). No differences were seen between DHE alone and chlorpromazine or lidocaine. Three studies revealed DHE plus metoclopramide was more effective than or equal to other agents for headache pain reduction at 2 hours: one vs ketorolac IM (OR=7; 95% CI, 0.86–56.89), one vs meperidine (Demerol) plus hydroxyzine (Vistaril, Atarax) IM (OR=47.67; 95% CI, 4.32–526.17), and one vs valproate IV (OR=0.67; 95% CI, 0.19–2.33).7 Specifically, treatment with DHE plus metoclopramide was superior to ketorolac for pain reduction (P=.03), but patients did not differ in disability scores (P=.06). DHE plus metoclopramide achieved greater reductions in pain scale scores than meperidine plus hydroxyzine (P<.001). No significant difference in pain reduction was noted between DHE plus metoclopramide and valproate (P=.36).
A multicenter, double-blind, randomized parallel group study8 showed no difference between the combination product isometheptene mucate, dichloralphenazone with acetaminophen (Midrin, Duradrin, etc) (used as recommended in the package insert with a maximum of up to 5 tablets within 24 hours) vs oral sumatriptan (initial dose of 25 mg with a repeat 25 mg dose in 2 hours). No placebo arm was used in this study.
Recommendations from others
The Institute for Clinical Systems Improvement recommends the use of vasoactive drugs over narcotics and barbiturates for treatment of moderately severe migraine headaches.9 The American Academy of Neurology recommends migraine-specific medications (triptans, DHE) for moderate to severe migraines or those mild to moderate migraines that responded poorly to NSAIDs or other over-the-counter preparations.10
Medications collectively referred to as “triptans” (eg, sumatriptan, naratriptan, etc) have been shown to be effective for acute migraine (strength of recommendation [SOR]: A). Nonsteroidal anti-inflammatory drugs (NSAIDs)—including aspirin, ibuprofen, naproxen sodium, diclofenac potassium, ketoprofen, tolfenamic acid, and ketorolac—are also effective (SOR: A). The combination of acetaminophen/aspirin/caffeine is effective (SOR: B). Parenteral dihydroergotamine (DHE), when administered with an antiemetic, is as effective as, or more effective than meperidine, valproate, or ketorolac (SOR: B). Prochlorperazine is more effective than metoclopramide in headache pain reduction (SOR: A). Isometheptene mucate/dichloralphenazone/acetaminophen is as effective as low-dose oral sumatriptan (SOR: B).
Inadequate response to medication? Increase dose or change route
Robert Sheeler, MD
Mayo Clinic, Rochester, Minn
For mild to moderate migraine headache attacks, NSAIDs or products containing acetaminophen and/or aspirin with caffeine or isometheptene mucate/dichloralphenazone/acetaminophen, when used intermittently, are frequently effective. More severe attacks generally respond better to migraine-specific medications such as triptans and ergot derivatives—the latter may be less likely to cause secondary rebound (analgesic overuse) headaches. Inadequate response to migraine-specific medication should prompt the prescriber to increase dose or change route to insure absorption (ie, nasal, rectal, or injectable).
Emerging evidence suggests combining a triptan plus an NSAID may produce higher response rates and more durable responses. Narcotics should generally be avoided. Valproate, ketorolac, IV magnesium, prochlorperazine, and metoclopramide are all somewhat effective for acute migraine, the latter 2 agents having the advantage of helping nausea but with the disadvantage of causing extrapyramidal reactions. A short course of oral steroids may break persistent attacks. Patients with frequent and intense headache patterns should be offered prophylactic therapy and not just abortive treatments.
Evidence summary
The prevalence of migraine headache is 6% among men and 15% to 17% among women.1 However, no standardized approach exists for the treatment of acute migraine headache. Systematic reviews of randomized controlled trials (RCTs) summarized that oral sumatriptan (Imitrex), eletriptan (Relpax), and rizatriptan (Maxalt) reduced migraine headache pain and increased the pain-free response rate for adults when compared with placebo.2-4 The number needed to treat (NNT) ranged from 3.9 to 9.9 for a given triptan’s lower dose to 2.6 to 5.1 for the higher dose.2-4 RCTs reported superior efficacy of oral almotriptan (Axert), frovatriptan (Frova), and zolmitriptan (Zomig), as well as intranasal sumatriptan and zolmitriptan when compared with placebo.
The following NSAIDs reduced headache severity more than placebo 2 hours after treatment: aspirin (1000 mg; NNT=2.4), ibuprofen (1200 mg; NNT=1.8), naproxen (750 mg; NNT=2.0), tolfenamic acid (not available in the US; NNT=1.2), and the combination product of acetaminophen/aspirin/caffeine (Excedrin Migraine, et al) (NNT=1.7).5 Acetaminophen 1000 mg orally has been reported to be superior to placebo for treating pain, functional disability, and photo/phonophobia among patients who did not require bedrest with their headaches and did not vomit more than 20% of the time. However, it was not superior to placebo when given intravenously for more severe acute migraine. No placebo-controlled trials exist for the use of ketorolac (Toradol); there are only comparison studies against other active migraine medications. Ketoprofen (Orudis) has placebo-controlled RCT data supporting its efficacy.
A meta-analysis6 of RCTs of parenteral metoclopramide (Reglan) revealed significant pain reduction (odds ratio [OR]=2.84; 95% confidence interval [CI], 1.05–7.68). When compared with other antiemetics (chlorpromazine [Thorazine] and prochlorperazine [Compazine]), metoclopramide was either less effective (OR=0.39; 95% CI, 0.18–0.87) or no different (OR=0.64; 95% CI, 0.23–1.76) than other therapies for reducing migraine pain. No difference was noted between parenteral metoclopramide and subcutaneous sumatriptan (OR=2.27; 95% CI, 0.64–8.11); however, metoclopramide was more effective than ibuprofen in pain reduction scores (standard deviation data missing in this study).
A systematic review7 revealed that dihydroergotamine (DHE) alone was less effective than subcutaneous sumatriptan in migraine pain reduction (OR=0.44; 95% CI, 0.25–0.77) or headache resolution (OR=0.05; 95% CI, 0.01–0.42). No differences were seen between DHE alone and chlorpromazine or lidocaine. Three studies revealed DHE plus metoclopramide was more effective than or equal to other agents for headache pain reduction at 2 hours: one vs ketorolac IM (OR=7; 95% CI, 0.86–56.89), one vs meperidine (Demerol) plus hydroxyzine (Vistaril, Atarax) IM (OR=47.67; 95% CI, 4.32–526.17), and one vs valproate IV (OR=0.67; 95% CI, 0.19–2.33).7 Specifically, treatment with DHE plus metoclopramide was superior to ketorolac for pain reduction (P=.03), but patients did not differ in disability scores (P=.06). DHE plus metoclopramide achieved greater reductions in pain scale scores than meperidine plus hydroxyzine (P<.001). No significant difference in pain reduction was noted between DHE plus metoclopramide and valproate (P=.36).
A multicenter, double-blind, randomized parallel group study8 showed no difference between the combination product isometheptene mucate, dichloralphenazone with acetaminophen (Midrin, Duradrin, etc) (used as recommended in the package insert with a maximum of up to 5 tablets within 24 hours) vs oral sumatriptan (initial dose of 25 mg with a repeat 25 mg dose in 2 hours). No placebo arm was used in this study.
Recommendations from others
The Institute for Clinical Systems Improvement recommends the use of vasoactive drugs over narcotics and barbiturates for treatment of moderately severe migraine headaches.9 The American Academy of Neurology recommends migraine-specific medications (triptans, DHE) for moderate to severe migraines or those mild to moderate migraines that responded poorly to NSAIDs or other over-the-counter preparations.10
1. Stewart WF, Shechter A, Rasmussen BK. Migraine prevalence: a review of population-based studies. Neurology 1994;44:S17-S23.
2. McCrory DC, Gray RN. Oral sumatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3)::CD002915.-
3. Oldman AD, Smith LA, McQuay HJ, Moore RA. Rizatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003221.-
4. Smith LA, Oldman AD, McQuay HJ, Moore RA. Eletriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003224.-
5. Snow V, Weiss K, Wall EM, Mottur-Pilson C. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med 2002;137:840-849.
6. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral metoclopramide for acute migraine: meta-analysis of randomised controlled trials. BMJ 2004;329:1369-1373.
7. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral dihydroergotamine for acute migraine headache: a systematic review of the literature. Ann Emerg Med 2005;45:393-401.
8. Freitag FG, Cady R, DiSerio F, et al. Comparative study of a combination of isometheptene mucate, dichloralphenazone with acetaminophen and sumatriptan succinate in the treatment of migraine. Headache 2001;41:391-398.
9. ICSI Health Care Guideline: Diagnosis and Treatment of Headache Bloomington, Minn: Institute for Clinical Systems Improvement (ICSI); 2004. Available at www.icsi.org/knowledge/detail.asp?catID=29&itemID=183. Accessed on May 17, 2006.
10. Silberstein SD. Practice Parameter: Evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:754-762.
1. Stewart WF, Shechter A, Rasmussen BK. Migraine prevalence: a review of population-based studies. Neurology 1994;44:S17-S23.
2. McCrory DC, Gray RN. Oral sumatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3)::CD002915.-
3. Oldman AD, Smith LA, McQuay HJ, Moore RA. Rizatriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003221.-
4. Smith LA, Oldman AD, McQuay HJ, Moore RA. Eletriptan for acute migraine. Cochrane Database Syst Rev 2005;(3):CD003224.-
5. Snow V, Weiss K, Wall EM, Mottur-Pilson C. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med 2002;137:840-849.
6. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral metoclopramide for acute migraine: meta-analysis of randomised controlled trials. BMJ 2004;329:1369-1373.
7. Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral dihydroergotamine for acute migraine headache: a systematic review of the literature. Ann Emerg Med 2005;45:393-401.
8. Freitag FG, Cady R, DiSerio F, et al. Comparative study of a combination of isometheptene mucate, dichloralphenazone with acetaminophen and sumatriptan succinate in the treatment of migraine. Headache 2001;41:391-398.
9. ICSI Health Care Guideline: Diagnosis and Treatment of Headache Bloomington, Minn: Institute for Clinical Systems Improvement (ICSI); 2004. Available at www.icsi.org/knowledge/detail.asp?catID=29&itemID=183. Accessed on May 17, 2006.
10. Silberstein SD. Practice Parameter: Evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:754-762.
Evidence-based answers from the Family Physicians Inquiries Network