User login
Part 4: Talking to Older Patients About Sex and STIs
Having established that there is a documented increase in sexually transmitted infections (STIs) among older Americans, and furthermore recognizing that a contributing factor to this trend may be communication gaps between patients and their health care providers, I now want to address the “What do we do about it?” aspect of our discussion. As clinicians, we know that the core focus around infectious diseases of any kind is prevention.
There are 3 types of prevention, as noted by Fos and Fine in Introduction to Public Health, all of which fit into our current topic: primary (eliminating risk factors), secondary (early detection), and tertiary (eliminating or moderating disability associated with advanced disease).1 The following recommendations fall into at least one of these categories.
1. All clinicians need to be involved in educating older Americans about the risks for STIs. Providers should routinely ask seniors if they are sexually active and should be prepared to recommend appropriate screening and education resources. Essentially, older adults should be getting the same basic “safe sex” education that younger people receive: learning about STIs, from recognizing the signs to understanding how STIs complicate other chronic medical conditions.2,3
2. Seniors also need education on the importance—and proper use—of condoms. Furthermore, we should go a step further and ensure that free condoms are distributed in places where seniors live and congregate. People older than 60 report the lowest condom use of any population.2,3
3. Information on STI detection and treatment options needs to be well publicized. For example, Medicare provides free STI screenings and low-cost treatments. We need to make sure our older patients are aware of this benefit and encourage them to make use of it.
4. Older Americans should be screened for STIs, regardless of age, per CDC guidelines. Seniors should get annual testing if they have new sexual partners—which means they must be asked the difficult questions.
And that’s the crux of the issue: Family members and clinicians may find it uncomfortable to have this conversation with Grandpa or Grandma. But there should be a dialogue to ensure they are aware of their risk for STIs, as well as how to prevent them.3 A well-known NP colleague reminded me of the importance of emphasizing to our older patients that anything discussed within the encounter is confidential and will not be disclosed without their permission. She starts off her conversations with patients by saying, “A lot of people your age experience …” or “Please don’t be insulted if I ask you about …” or “Is it OK if I ask you a few very personal questions?”
Continue to: It is critical...
It is critical to keep an open mind and accepting attitude when discussing sexuality or intimate issues with older patients. Paying attention to patients’ verbal and nonverbal cues is also essential. Clinicians should never assume older adults are sexually inactive, no longer care about sex, or are necessarily heterosexual. There was an excellent article in the Journal of Family Practice a few years ago on “How to discuss sex with elderly patients” that is worth rereading. In it, the authors suggest using the PLISSIT model to facilitate a conversation with your elderly patient. As explained in the article, the acronym “is a reminder to seek Permission to discuss sexuality, share Limited information about sexual issues that affect the older adult, provide Specific Suggestions to improve sexual health, and offer to provide a referral for Intensive Therapy if needed.”4 The Table offers some examples of how to address each step of PLISSIT.

So, as we wrap up our examination of this issue, I encourage you to open this dialogue with your older patients. In light of the increasing number of older patients with STIs, it is essential for clinicians to obtain an accurate and complete sexual history for patients of any age. That starts with asking the appropriate questions, preferably in a manner that puts the patient at ease to share important details. If you have additional ideas about what we can do to reverse this STI trend, please share them with me at [email protected].
1. Goldstein RL, Goldstein K, Dwelle TL. Introduction to Public Health. 2nd ed. New York, NY: Springer Publishing Co; 2015.
2. Cohen JK. STDs on the rise among senior. Becker's Hospital Review. May 18, 2018. www.beckershospitalreview.com/population-health/stds-on-the-rise-among-seniors.html. Accessed May 22, 2019.
3. Humphrey D. Seniors at high risk for sexually transmitted diseases [STDs]. HomeHelpers. March 31, 2018. https://www.homehelpershomecare.com/clearwater/blog/2018/13/seniors-at-high-risk-for-sexually-transmitted-diseases-stds. Accessed Mary 22, 2019.
4. Omole F, Fresh EM, Sow C, et al. How to discuss sex with elderly patients. J Fam Pract. 2014;63(4):E1-E4.
Having established that there is a documented increase in sexually transmitted infections (STIs) among older Americans, and furthermore recognizing that a contributing factor to this trend may be communication gaps between patients and their health care providers, I now want to address the “What do we do about it?” aspect of our discussion. As clinicians, we know that the core focus around infectious diseases of any kind is prevention.
There are 3 types of prevention, as noted by Fos and Fine in Introduction to Public Health, all of which fit into our current topic: primary (eliminating risk factors), secondary (early detection), and tertiary (eliminating or moderating disability associated with advanced disease).1 The following recommendations fall into at least one of these categories.
1. All clinicians need to be involved in educating older Americans about the risks for STIs. Providers should routinely ask seniors if they are sexually active and should be prepared to recommend appropriate screening and education resources. Essentially, older adults should be getting the same basic “safe sex” education that younger people receive: learning about STIs, from recognizing the signs to understanding how STIs complicate other chronic medical conditions.2,3
2. Seniors also need education on the importance—and proper use—of condoms. Furthermore, we should go a step further and ensure that free condoms are distributed in places where seniors live and congregate. People older than 60 report the lowest condom use of any population.2,3
3. Information on STI detection and treatment options needs to be well publicized. For example, Medicare provides free STI screenings and low-cost treatments. We need to make sure our older patients are aware of this benefit and encourage them to make use of it.
4. Older Americans should be screened for STIs, regardless of age, per CDC guidelines. Seniors should get annual testing if they have new sexual partners—which means they must be asked the difficult questions.
And that’s the crux of the issue: Family members and clinicians may find it uncomfortable to have this conversation with Grandpa or Grandma. But there should be a dialogue to ensure they are aware of their risk for STIs, as well as how to prevent them.3 A well-known NP colleague reminded me of the importance of emphasizing to our older patients that anything discussed within the encounter is confidential and will not be disclosed without their permission. She starts off her conversations with patients by saying, “A lot of people your age experience …” or “Please don’t be insulted if I ask you about …” or “Is it OK if I ask you a few very personal questions?”
Continue to: It is critical...
It is critical to keep an open mind and accepting attitude when discussing sexuality or intimate issues with older patients. Paying attention to patients’ verbal and nonverbal cues is also essential. Clinicians should never assume older adults are sexually inactive, no longer care about sex, or are necessarily heterosexual. There was an excellent article in the Journal of Family Practice a few years ago on “How to discuss sex with elderly patients” that is worth rereading. In it, the authors suggest using the PLISSIT model to facilitate a conversation with your elderly patient. As explained in the article, the acronym “is a reminder to seek Permission to discuss sexuality, share Limited information about sexual issues that affect the older adult, provide Specific Suggestions to improve sexual health, and offer to provide a referral for Intensive Therapy if needed.”4 The Table offers some examples of how to address each step of PLISSIT.

So, as we wrap up our examination of this issue, I encourage you to open this dialogue with your older patients. In light of the increasing number of older patients with STIs, it is essential for clinicians to obtain an accurate and complete sexual history for patients of any age. That starts with asking the appropriate questions, preferably in a manner that puts the patient at ease to share important details. If you have additional ideas about what we can do to reverse this STI trend, please share them with me at [email protected].
Having established that there is a documented increase in sexually transmitted infections (STIs) among older Americans, and furthermore recognizing that a contributing factor to this trend may be communication gaps between patients and their health care providers, I now want to address the “What do we do about it?” aspect of our discussion. As clinicians, we know that the core focus around infectious diseases of any kind is prevention.
There are 3 types of prevention, as noted by Fos and Fine in Introduction to Public Health, all of which fit into our current topic: primary (eliminating risk factors), secondary (early detection), and tertiary (eliminating or moderating disability associated with advanced disease).1 The following recommendations fall into at least one of these categories.
1. All clinicians need to be involved in educating older Americans about the risks for STIs. Providers should routinely ask seniors if they are sexually active and should be prepared to recommend appropriate screening and education resources. Essentially, older adults should be getting the same basic “safe sex” education that younger people receive: learning about STIs, from recognizing the signs to understanding how STIs complicate other chronic medical conditions.2,3
2. Seniors also need education on the importance—and proper use—of condoms. Furthermore, we should go a step further and ensure that free condoms are distributed in places where seniors live and congregate. People older than 60 report the lowest condom use of any population.2,3
3. Information on STI detection and treatment options needs to be well publicized. For example, Medicare provides free STI screenings and low-cost treatments. We need to make sure our older patients are aware of this benefit and encourage them to make use of it.
4. Older Americans should be screened for STIs, regardless of age, per CDC guidelines. Seniors should get annual testing if they have new sexual partners—which means they must be asked the difficult questions.
And that’s the crux of the issue: Family members and clinicians may find it uncomfortable to have this conversation with Grandpa or Grandma. But there should be a dialogue to ensure they are aware of their risk for STIs, as well as how to prevent them.3 A well-known NP colleague reminded me of the importance of emphasizing to our older patients that anything discussed within the encounter is confidential and will not be disclosed without their permission. She starts off her conversations with patients by saying, “A lot of people your age experience …” or “Please don’t be insulted if I ask you about …” or “Is it OK if I ask you a few very personal questions?”
Continue to: It is critical...
It is critical to keep an open mind and accepting attitude when discussing sexuality or intimate issues with older patients. Paying attention to patients’ verbal and nonverbal cues is also essential. Clinicians should never assume older adults are sexually inactive, no longer care about sex, or are necessarily heterosexual. There was an excellent article in the Journal of Family Practice a few years ago on “How to discuss sex with elderly patients” that is worth rereading. In it, the authors suggest using the PLISSIT model to facilitate a conversation with your elderly patient. As explained in the article, the acronym “is a reminder to seek Permission to discuss sexuality, share Limited information about sexual issues that affect the older adult, provide Specific Suggestions to improve sexual health, and offer to provide a referral for Intensive Therapy if needed.”4 The Table offers some examples of how to address each step of PLISSIT.

So, as we wrap up our examination of this issue, I encourage you to open this dialogue with your older patients. In light of the increasing number of older patients with STIs, it is essential for clinicians to obtain an accurate and complete sexual history for patients of any age. That starts with asking the appropriate questions, preferably in a manner that puts the patient at ease to share important details. If you have additional ideas about what we can do to reverse this STI trend, please share them with me at [email protected].
1. Goldstein RL, Goldstein K, Dwelle TL. Introduction to Public Health. 2nd ed. New York, NY: Springer Publishing Co; 2015.
2. Cohen JK. STDs on the rise among senior. Becker's Hospital Review. May 18, 2018. www.beckershospitalreview.com/population-health/stds-on-the-rise-among-seniors.html. Accessed May 22, 2019.
3. Humphrey D. Seniors at high risk for sexually transmitted diseases [STDs]. HomeHelpers. March 31, 2018. https://www.homehelpershomecare.com/clearwater/blog/2018/13/seniors-at-high-risk-for-sexually-transmitted-diseases-stds. Accessed Mary 22, 2019.
4. Omole F, Fresh EM, Sow C, et al. How to discuss sex with elderly patients. J Fam Pract. 2014;63(4):E1-E4.
1. Goldstein RL, Goldstein K, Dwelle TL. Introduction to Public Health. 2nd ed. New York, NY: Springer Publishing Co; 2015.
2. Cohen JK. STDs on the rise among senior. Becker's Hospital Review. May 18, 2018. www.beckershospitalreview.com/population-health/stds-on-the-rise-among-seniors.html. Accessed May 22, 2019.
3. Humphrey D. Seniors at high risk for sexually transmitted diseases [STDs]. HomeHelpers. March 31, 2018. https://www.homehelpershomecare.com/clearwater/blog/2018/13/seniors-at-high-risk-for-sexually-transmitted-diseases-stds. Accessed Mary 22, 2019.
4. Omole F, Fresh EM, Sow C, et al. How to discuss sex with elderly patients. J Fam Pract. 2014;63(4):E1-E4.
Part 3: Talkin’ ’bout My Generation
Members of the baby boom generation (yes, my generation)—the nomenclature given to the 76 million people born between 1946 and 1964—are now in our 50s, 60s, and 70s. Many of us are enjoying our retirement while others are still working. Regardless of our circumstances, we all share one challenge: aging as comfortably as we can. It’s a fact of our lives that as we age, we battle risk factors for a variety of conditions, ranging from diabetes, heart disease, and Alzheimer disease to … sexually transmitted infections (STIs).
Ever since I saw the statistics about increasing rates of STIs among older Americans, I’ve been mulling possible explanations for this trend. In conversation with my CR colleagues, the question arose as to whether the fact that the current population of senior citizens is comprised largely of Baby Boomers has had an impact. It’s certainly worth considering!
We (the Baby Boomers) are more savvy, assertive, health-conscious, and engaged in our health care than the generations that preceded us.1,2 When I look around at my friends and colleagues, I see a group of people who want to live more active lives and remain socially engaged—even as we manage our chronic conditions! As self-determining patients, we are likely to question established principles of medical care, demanding greater attention to our own definitions of health-related quality of life, including a satisfactory sex life.3
In fact, some of this increase in STIs among older Americans could be explained by the availability of treatments that address the sexual dysfunction that comes with aging. Previous generations of older adults have faced menopause and erectile dysfunction—but Baby Boomers are living and aging at a time when the symptoms can be more effectively managed. For older women, there are bioidentical hormones to replace those lost during menopause, which is often cited as the primary offender affecting their sexual lives (despite research suggesting that social and psychologic factors—emotional well-being, a strong emotional association with one’s partner, and positive body image—may be more foretelling of sexual activity later in life than the hormonal changes related to menopause).4
As for erectile dysfunction, yes, some men still feel awkward about bringing it up with their clinician; it can feel enfeebling for men to acknowledge, even though the physiologic changes are explained by the biology of aging (as we alluded to last week). Continuing sales of Viagra and Cialis suggest that boomer men are overcoming the stigmas of revealing their erectile dysfunction, however.
And maybe that is a contributing factor to this trend in STIs: We are being equipped for sexual performance, but perhaps we haven’t been adequately educated on what the consequences of our sexual encounters are. A lot of today’s seniors were already married when sex education gained prominence and perhaps missed the “safe sex” talks.
When I discussed this with a colleague of mine—a retired employee of the State Department—he noted that this topic was talked about even among US Embassy staff! At the risk of making a sweeping generalization and stating the obvious, he observed that “sexual mores have changed over time. Even many generations ago, they thought previous generations had been restrictive about sexual behavior!” Nevertheless, we agreed that the generation now emerging as “older Americans” grew up during the ’60s Free Love movement—and that philosophy seems to have carried into some individuals’ current sexual behavior. My colleague also noted that “as we get older, we lose partners—and sexual monogamy is lost with the loss of a partner.”
Continue to: The Baby Boomers...
The Baby Boomers are by far the most sexually liberal generation of older adults that this country has ever seen. Providing health care to this population requires addressing all health care needs, including sexual health and prevention. Next week, we’ll examine ways clinicians can comfortably broach these topics with older patients.
In the meantime, I’d love to hear your thoughts: Is this the Second Spring of the Summer of Love generation? Whether you’re a Boomer or a Millennial or anyone in between, feel free to write to me at [email protected].
1. Kickbusch I, Payne L. Twenty-first century health promotion: the public health revolution meets the wellness revolution. Health Promot Int. 2003;18(4):275-278.
2. Wilson LB, Simson SP (eds). Civic Engagement and the Baby Boomer Generation: Research, Policy, and Practice Perspectives. New York, NY: Haworth Press; 2006.
3. Kane RL, Kane RA. What older people want from long-term care, and how they can get it. Health Aff. 2001;20(6):114-127.
4. Bancroft J, Loftus J, Long JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32(3):193-208.
Members of the baby boom generation (yes, my generation)—the nomenclature given to the 76 million people born between 1946 and 1964—are now in our 50s, 60s, and 70s. Many of us are enjoying our retirement while others are still working. Regardless of our circumstances, we all share one challenge: aging as comfortably as we can. It’s a fact of our lives that as we age, we battle risk factors for a variety of conditions, ranging from diabetes, heart disease, and Alzheimer disease to … sexually transmitted infections (STIs).
Ever since I saw the statistics about increasing rates of STIs among older Americans, I’ve been mulling possible explanations for this trend. In conversation with my CR colleagues, the question arose as to whether the fact that the current population of senior citizens is comprised largely of Baby Boomers has had an impact. It’s certainly worth considering!
We (the Baby Boomers) are more savvy, assertive, health-conscious, and engaged in our health care than the generations that preceded us.1,2 When I look around at my friends and colleagues, I see a group of people who want to live more active lives and remain socially engaged—even as we manage our chronic conditions! As self-determining patients, we are likely to question established principles of medical care, demanding greater attention to our own definitions of health-related quality of life, including a satisfactory sex life.3
In fact, some of this increase in STIs among older Americans could be explained by the availability of treatments that address the sexual dysfunction that comes with aging. Previous generations of older adults have faced menopause and erectile dysfunction—but Baby Boomers are living and aging at a time when the symptoms can be more effectively managed. For older women, there are bioidentical hormones to replace those lost during menopause, which is often cited as the primary offender affecting their sexual lives (despite research suggesting that social and psychologic factors—emotional well-being, a strong emotional association with one’s partner, and positive body image—may be more foretelling of sexual activity later in life than the hormonal changes related to menopause).4
As for erectile dysfunction, yes, some men still feel awkward about bringing it up with their clinician; it can feel enfeebling for men to acknowledge, even though the physiologic changes are explained by the biology of aging (as we alluded to last week). Continuing sales of Viagra and Cialis suggest that boomer men are overcoming the stigmas of revealing their erectile dysfunction, however.
And maybe that is a contributing factor to this trend in STIs: We are being equipped for sexual performance, but perhaps we haven’t been adequately educated on what the consequences of our sexual encounters are. A lot of today’s seniors were already married when sex education gained prominence and perhaps missed the “safe sex” talks.
When I discussed this with a colleague of mine—a retired employee of the State Department—he noted that this topic was talked about even among US Embassy staff! At the risk of making a sweeping generalization and stating the obvious, he observed that “sexual mores have changed over time. Even many generations ago, they thought previous generations had been restrictive about sexual behavior!” Nevertheless, we agreed that the generation now emerging as “older Americans” grew up during the ’60s Free Love movement—and that philosophy seems to have carried into some individuals’ current sexual behavior. My colleague also noted that “as we get older, we lose partners—and sexual monogamy is lost with the loss of a partner.”
Continue to: The Baby Boomers...
The Baby Boomers are by far the most sexually liberal generation of older adults that this country has ever seen. Providing health care to this population requires addressing all health care needs, including sexual health and prevention. Next week, we’ll examine ways clinicians can comfortably broach these topics with older patients.
In the meantime, I’d love to hear your thoughts: Is this the Second Spring of the Summer of Love generation? Whether you’re a Boomer or a Millennial or anyone in between, feel free to write to me at [email protected].
Members of the baby boom generation (yes, my generation)—the nomenclature given to the 76 million people born between 1946 and 1964—are now in our 50s, 60s, and 70s. Many of us are enjoying our retirement while others are still working. Regardless of our circumstances, we all share one challenge: aging as comfortably as we can. It’s a fact of our lives that as we age, we battle risk factors for a variety of conditions, ranging from diabetes, heart disease, and Alzheimer disease to … sexually transmitted infections (STIs).
Ever since I saw the statistics about increasing rates of STIs among older Americans, I’ve been mulling possible explanations for this trend. In conversation with my CR colleagues, the question arose as to whether the fact that the current population of senior citizens is comprised largely of Baby Boomers has had an impact. It’s certainly worth considering!
We (the Baby Boomers) are more savvy, assertive, health-conscious, and engaged in our health care than the generations that preceded us.1,2 When I look around at my friends and colleagues, I see a group of people who want to live more active lives and remain socially engaged—even as we manage our chronic conditions! As self-determining patients, we are likely to question established principles of medical care, demanding greater attention to our own definitions of health-related quality of life, including a satisfactory sex life.3
In fact, some of this increase in STIs among older Americans could be explained by the availability of treatments that address the sexual dysfunction that comes with aging. Previous generations of older adults have faced menopause and erectile dysfunction—but Baby Boomers are living and aging at a time when the symptoms can be more effectively managed. For older women, there are bioidentical hormones to replace those lost during menopause, which is often cited as the primary offender affecting their sexual lives (despite research suggesting that social and psychologic factors—emotional well-being, a strong emotional association with one’s partner, and positive body image—may be more foretelling of sexual activity later in life than the hormonal changes related to menopause).4
As for erectile dysfunction, yes, some men still feel awkward about bringing it up with their clinician; it can feel enfeebling for men to acknowledge, even though the physiologic changes are explained by the biology of aging (as we alluded to last week). Continuing sales of Viagra and Cialis suggest that boomer men are overcoming the stigmas of revealing their erectile dysfunction, however.
And maybe that is a contributing factor to this trend in STIs: We are being equipped for sexual performance, but perhaps we haven’t been adequately educated on what the consequences of our sexual encounters are. A lot of today’s seniors were already married when sex education gained prominence and perhaps missed the “safe sex” talks.
When I discussed this with a colleague of mine—a retired employee of the State Department—he noted that this topic was talked about even among US Embassy staff! At the risk of making a sweeping generalization and stating the obvious, he observed that “sexual mores have changed over time. Even many generations ago, they thought previous generations had been restrictive about sexual behavior!” Nevertheless, we agreed that the generation now emerging as “older Americans” grew up during the ’60s Free Love movement—and that philosophy seems to have carried into some individuals’ current sexual behavior. My colleague also noted that “as we get older, we lose partners—and sexual monogamy is lost with the loss of a partner.”
Continue to: The Baby Boomers...
The Baby Boomers are by far the most sexually liberal generation of older adults that this country has ever seen. Providing health care to this population requires addressing all health care needs, including sexual health and prevention. Next week, we’ll examine ways clinicians can comfortably broach these topics with older patients.
In the meantime, I’d love to hear your thoughts: Is this the Second Spring of the Summer of Love generation? Whether you’re a Boomer or a Millennial or anyone in between, feel free to write to me at [email protected].
1. Kickbusch I, Payne L. Twenty-first century health promotion: the public health revolution meets the wellness revolution. Health Promot Int. 2003;18(4):275-278.
2. Wilson LB, Simson SP (eds). Civic Engagement and the Baby Boomer Generation: Research, Policy, and Practice Perspectives. New York, NY: Haworth Press; 2006.
3. Kane RL, Kane RA. What older people want from long-term care, and how they can get it. Health Aff. 2001;20(6):114-127.
4. Bancroft J, Loftus J, Long JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32(3):193-208.
1. Kickbusch I, Payne L. Twenty-first century health promotion: the public health revolution meets the wellness revolution. Health Promot Int. 2003;18(4):275-278.
2. Wilson LB, Simson SP (eds). Civic Engagement and the Baby Boomer Generation: Research, Policy, and Practice Perspectives. New York, NY: Haworth Press; 2006.
3. Kane RL, Kane RA. What older people want from long-term care, and how they can get it. Health Aff. 2001;20(6):114-127.
4. Bancroft J, Loftus J, Long JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32(3):193-208.
Part 2: Why the Increase?
As established last week, there has been a startling increase in sexually transmitted infections (STIs) among older adults in the United States. The burning question on everyone’s mind (certainly mine!) is: Why? Engaging in some “educated speculation” yields many factors possibly driving this trend. For example:
1. Provider Reluctance. Older Americans may not get regular screenings for STIs because their health care providers are often reluctant to raise the issue. That may be fueled by lack of awareness on the clinician’s part: More than 60% of individuals older than 60 have sex at least once a month, yet this population is rarely considered to be “at risk” for STIs.1
2. Patient Embarrassment/awkwardness. For many older Americans, admitting that they are having sex makes them feel awkward or embarrassed. Reluctance to share intimate details means they may not seek evaluation and treatment for symptoms that seem related to their sexual health or activity.
3. Effects of Aging. There are 2 sides to this coin: actual physiologic changes that occur with age and assumptions that all changes are just part of aging. As people get older, their immune systems tend to deteriorate, making them more vulnerable to contracting any disease—including STIs. After menopause, women's vaginal tissues thin and natural lubrication declines, increasing their risk for microtears that can leave them susceptible to infectious organisms. And let’s be honest: Some STI symptoms, such as fatigue, weakness, and changes in memory, are nonspecific and may be mistaken by clinicians for the regular progression of age.2
4. Social Changes. The world has changed since most older adults last dove into the dating pool. We now have online dating services, some of which cater to a mature audience; as a result, people may be less familiar with their partner’s sexual history. Compounding that, many older adults just aren’t accustomed to thinking of themselves or a partner as being at high risk for STIs—and if you don’t even think about it, you definitely won’t ask. Widowed or divorced adults may date more than one person at a time, raising their risk for infection after a long period of monogamy. Seniors also may not be accustomed to using a condom or do not use one because they think the risk for STIs is minimal or nonexistent. Seniors may not consider oral or anal sex as a way of contracting or transmitting STIs.3
5. Medical Advances. Compared with previous generations, today’s seniors have an easier time having sex at an older age, thanks to the availability of medications such as sildenafil (Viagra) and tadalafil (Cialis) for men with erectile dysfunction. There has also been an increase in postmenopausal women requesting and receiving bioidentical hormone replacement. With increased libido and ability to perform come more sexual encounters among the older population—and as a result, more opportunities for STIs to spread. Are there other reasons for the increase in STIs in this population? Next week we’ll consider the unique societal influences of the Baby Boom generation. In the meantime, please share your insights with me at [email protected].
1. Boskey E. STDs in the elderly community. Verywell Health. February 14, 2018. www.verywellhealth.com/stds-the-elderly-3133189. Accessed May 8, 2019.
2. East A. (2017). Seniors and STDs: common sexually transmitted diseases. CaringPeople. June 23, 2017. https://caringpeopleinc.com/blog/seniors-common-sexually-transmitted-diseases. Accessed May 8, 2019.
3. Harvard Medical School. Sexually transmitted disease? At my age? Harvard Health Letter. February 2018. www.health.harvard.edu/diseases-and-conditions/sexually-transmitted-disease-at-my-age. Accessed May 8, 2019.
As established last week, there has been a startling increase in sexually transmitted infections (STIs) among older adults in the United States. The burning question on everyone’s mind (certainly mine!) is: Why? Engaging in some “educated speculation” yields many factors possibly driving this trend. For example:
1. Provider Reluctance. Older Americans may not get regular screenings for STIs because their health care providers are often reluctant to raise the issue. That may be fueled by lack of awareness on the clinician’s part: More than 60% of individuals older than 60 have sex at least once a month, yet this population is rarely considered to be “at risk” for STIs.1
2. Patient Embarrassment/awkwardness. For many older Americans, admitting that they are having sex makes them feel awkward or embarrassed. Reluctance to share intimate details means they may not seek evaluation and treatment for symptoms that seem related to their sexual health or activity.
3. Effects of Aging. There are 2 sides to this coin: actual physiologic changes that occur with age and assumptions that all changes are just part of aging. As people get older, their immune systems tend to deteriorate, making them more vulnerable to contracting any disease—including STIs. After menopause, women's vaginal tissues thin and natural lubrication declines, increasing their risk for microtears that can leave them susceptible to infectious organisms. And let’s be honest: Some STI symptoms, such as fatigue, weakness, and changes in memory, are nonspecific and may be mistaken by clinicians for the regular progression of age.2
4. Social Changes. The world has changed since most older adults last dove into the dating pool. We now have online dating services, some of which cater to a mature audience; as a result, people may be less familiar with their partner’s sexual history. Compounding that, many older adults just aren’t accustomed to thinking of themselves or a partner as being at high risk for STIs—and if you don’t even think about it, you definitely won’t ask. Widowed or divorced adults may date more than one person at a time, raising their risk for infection after a long period of monogamy. Seniors also may not be accustomed to using a condom or do not use one because they think the risk for STIs is minimal or nonexistent. Seniors may not consider oral or anal sex as a way of contracting or transmitting STIs.3
5. Medical Advances. Compared with previous generations, today’s seniors have an easier time having sex at an older age, thanks to the availability of medications such as sildenafil (Viagra) and tadalafil (Cialis) for men with erectile dysfunction. There has also been an increase in postmenopausal women requesting and receiving bioidentical hormone replacement. With increased libido and ability to perform come more sexual encounters among the older population—and as a result, more opportunities for STIs to spread. Are there other reasons for the increase in STIs in this population? Next week we’ll consider the unique societal influences of the Baby Boom generation. In the meantime, please share your insights with me at [email protected].
As established last week, there has been a startling increase in sexually transmitted infections (STIs) among older adults in the United States. The burning question on everyone’s mind (certainly mine!) is: Why? Engaging in some “educated speculation” yields many factors possibly driving this trend. For example:
1. Provider Reluctance. Older Americans may not get regular screenings for STIs because their health care providers are often reluctant to raise the issue. That may be fueled by lack of awareness on the clinician’s part: More than 60% of individuals older than 60 have sex at least once a month, yet this population is rarely considered to be “at risk” for STIs.1
2. Patient Embarrassment/awkwardness. For many older Americans, admitting that they are having sex makes them feel awkward or embarrassed. Reluctance to share intimate details means they may not seek evaluation and treatment for symptoms that seem related to their sexual health or activity.
3. Effects of Aging. There are 2 sides to this coin: actual physiologic changes that occur with age and assumptions that all changes are just part of aging. As people get older, their immune systems tend to deteriorate, making them more vulnerable to contracting any disease—including STIs. After menopause, women's vaginal tissues thin and natural lubrication declines, increasing their risk for microtears that can leave them susceptible to infectious organisms. And let’s be honest: Some STI symptoms, such as fatigue, weakness, and changes in memory, are nonspecific and may be mistaken by clinicians for the regular progression of age.2
4. Social Changes. The world has changed since most older adults last dove into the dating pool. We now have online dating services, some of which cater to a mature audience; as a result, people may be less familiar with their partner’s sexual history. Compounding that, many older adults just aren’t accustomed to thinking of themselves or a partner as being at high risk for STIs—and if you don’t even think about it, you definitely won’t ask. Widowed or divorced adults may date more than one person at a time, raising their risk for infection after a long period of monogamy. Seniors also may not be accustomed to using a condom or do not use one because they think the risk for STIs is minimal or nonexistent. Seniors may not consider oral or anal sex as a way of contracting or transmitting STIs.3
5. Medical Advances. Compared with previous generations, today’s seniors have an easier time having sex at an older age, thanks to the availability of medications such as sildenafil (Viagra) and tadalafil (Cialis) for men with erectile dysfunction. There has also been an increase in postmenopausal women requesting and receiving bioidentical hormone replacement. With increased libido and ability to perform come more sexual encounters among the older population—and as a result, more opportunities for STIs to spread. Are there other reasons for the increase in STIs in this population? Next week we’ll consider the unique societal influences of the Baby Boom generation. In the meantime, please share your insights with me at [email protected].
1. Boskey E. STDs in the elderly community. Verywell Health. February 14, 2018. www.verywellhealth.com/stds-the-elderly-3133189. Accessed May 8, 2019.
2. East A. (2017). Seniors and STDs: common sexually transmitted diseases. CaringPeople. June 23, 2017. https://caringpeopleinc.com/blog/seniors-common-sexually-transmitted-diseases. Accessed May 8, 2019.
3. Harvard Medical School. Sexually transmitted disease? At my age? Harvard Health Letter. February 2018. www.health.harvard.edu/diseases-and-conditions/sexually-transmitted-disease-at-my-age. Accessed May 8, 2019.
1. Boskey E. STDs in the elderly community. Verywell Health. February 14, 2018. www.verywellhealth.com/stds-the-elderly-3133189. Accessed May 8, 2019.
2. East A. (2017). Seniors and STDs: common sexually transmitted diseases. CaringPeople. June 23, 2017. https://caringpeopleinc.com/blog/seniors-common-sexually-transmitted-diseases. Accessed May 8, 2019.
3. Harvard Medical School. Sexually transmitted disease? At my age? Harvard Health Letter. February 2018. www.health.harvard.edu/diseases-and-conditions/sexually-transmitted-disease-at-my-age. Accessed May 8, 2019.
Part 1: A Disturbing Trend
While reviewing some epidemiology data for a lecture recently, I couldn’t believe my eyes: The numbers indicated an increase in sexually transmitted infections (STIs) among older Americans. Filled with doubt about the accuracy, I decided to research further. My first stop was a PA colleague who works with a mobile urgent care company that specializes in retirement communities—and she confirmed that she has witnessed this “trend”!
The fundamental public health concern for older Americans is, of course, long-term illness, disability, and dependency on others. However, experts on aging agree that since the last century, disability rates among those older than 65 have declined, as have the number of seniors living in nursing homes. Suffice it to say, the good news is that Americans are living longer—the bad news, they are doing so with an increased risk for cardiovascular disease and malignant neoplasms. The other downside is that seniors have increased risk for infectious diseases.1
Healthy People 2020 continues to recognize HIV and other STIs as problems in the United States and to promote efforts to reduce them. Unfortunately, prevention strategies for older adults in primary care settings are often not aimed at these diseases. More broadly, sexual behaviors tend to be discussed less with this population.2
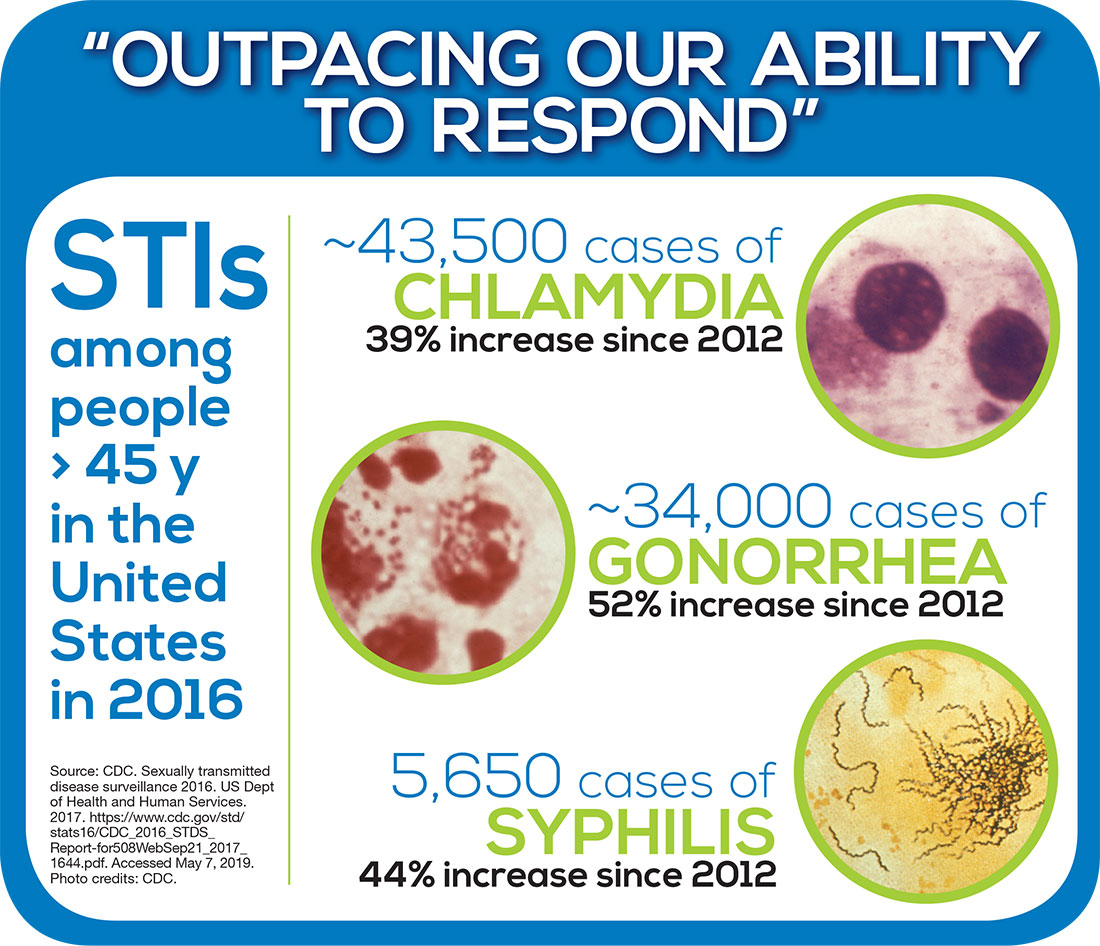
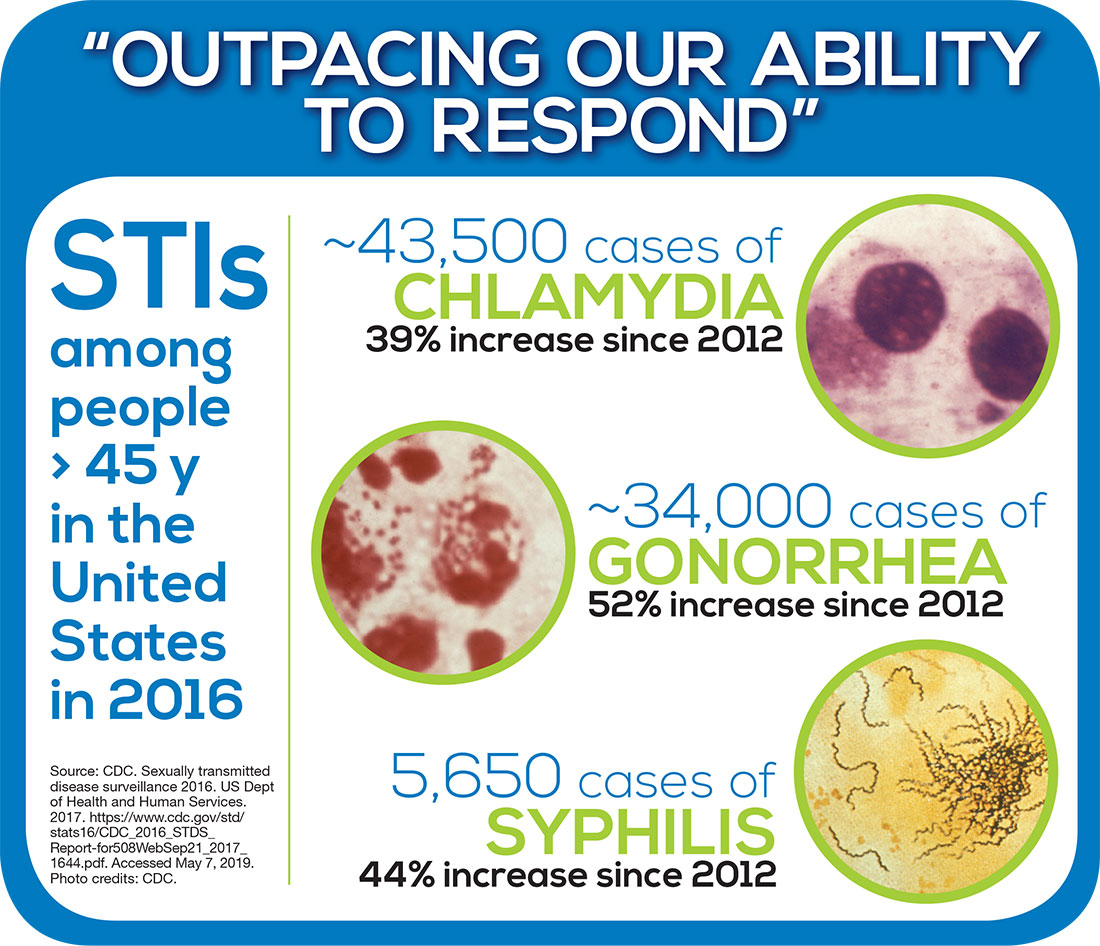
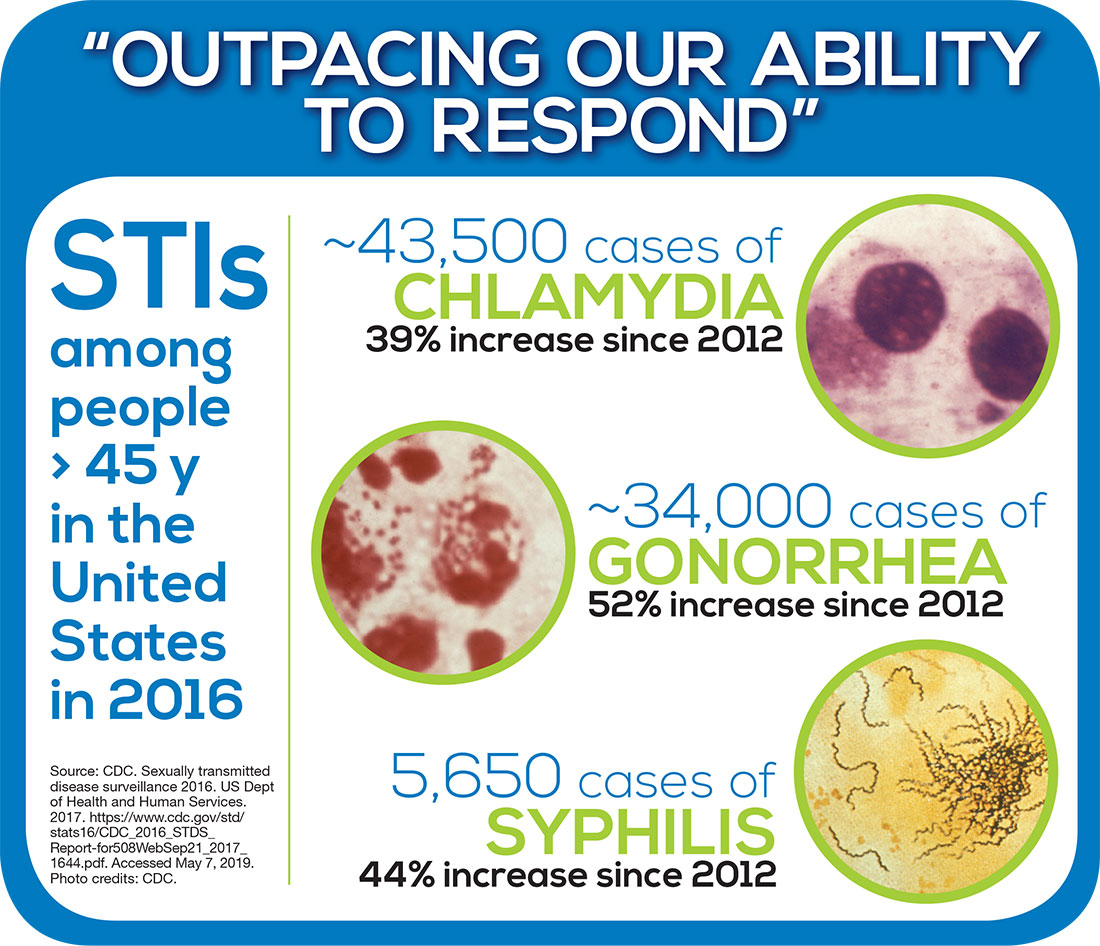
The disturbing climb in STIs among older Americans is part of a more momentous national trend that the CDC says must be tackled. Overall rates of STIs in 2016 were the highest ever recorded in a single year.3 And although STI rates are highest among people ages 15 to 24, the upsurge among older Americans is larger than it is for the rest of the US population. According to the CDC, in 2016, there were 82,938 cases of gonorrhea, syphilis, and chlamydia reported among Americans ages 45 and older—about a 20% percent increase from 2015 and continuing a trend of annual increases since at least 2012.3 The infographic shows the rates for individual STIs.
The CDC notes that STIs put people “at risk for severe, lifelong health outcomes like chronic pain, severe reproductive health complications, and HIV" particularly if left untreated.4 Jonathan Mermin, MD, Director of the CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention has described STIs as “a persistent enemy, growing in number and outpacing our ability to respond.”5
Over the next 3 weeks, we will explore this public health issue—starting next week with the big question: Why is this trend occurring? In the meantime, feel free to share your thoughts with me at [email protected]. See you next Thursday!
1. Schneider M. Introduction to Public Health. 5th ed. Burlington, MA: Jones and Bartlett Learning; 2017.
2. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020: Sexually transmitted diseases. www.healthypeople.gov/2020/topics-objectives/topic/sexually-transmitted-diseases. Accessed May 6, 2019.
3. CDC. 2016 Sexually Transmitted Diseases Surveillance. www.cdc.gov/std/stats16/default.htm. Accessed May 6, 2019.
4. CDC. Fact sheet: reported STDs in the United States, 2017. www.cdc.gov/nchhstp/newsroom/docs/factsheets/std-trends-508.pdf. Accessed May 6, 2019.
5. CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. STDs at record high, indicating urgent need for prevention [press release]. September 26, 2017. www.cdc.gov/nchhstp/newsroom/2017/std-surveillance-report-2016-press-release.html. Accessed May 6, 2019.
While reviewing some epidemiology data for a lecture recently, I couldn’t believe my eyes: The numbers indicated an increase in sexually transmitted infections (STIs) among older Americans. Filled with doubt about the accuracy, I decided to research further. My first stop was a PA colleague who works with a mobile urgent care company that specializes in retirement communities—and she confirmed that she has witnessed this “trend”!
The fundamental public health concern for older Americans is, of course, long-term illness, disability, and dependency on others. However, experts on aging agree that since the last century, disability rates among those older than 65 have declined, as have the number of seniors living in nursing homes. Suffice it to say, the good news is that Americans are living longer—the bad news, they are doing so with an increased risk for cardiovascular disease and malignant neoplasms. The other downside is that seniors have increased risk for infectious diseases.1
Healthy People 2020 continues to recognize HIV and other STIs as problems in the United States and to promote efforts to reduce them. Unfortunately, prevention strategies for older adults in primary care settings are often not aimed at these diseases. More broadly, sexual behaviors tend to be discussed less with this population.2
The disturbing climb in STIs among older Americans is part of a more momentous national trend that the CDC says must be tackled. Overall rates of STIs in 2016 were the highest ever recorded in a single year.3 And although STI rates are highest among people ages 15 to 24, the upsurge among older Americans is larger than it is for the rest of the US population. According to the CDC, in 2016, there were 82,938 cases of gonorrhea, syphilis, and chlamydia reported among Americans ages 45 and older—about a 20% percent increase from 2015 and continuing a trend of annual increases since at least 2012.3 The infographic shows the rates for individual STIs.
The CDC notes that STIs put people “at risk for severe, lifelong health outcomes like chronic pain, severe reproductive health complications, and HIV" particularly if left untreated.4 Jonathan Mermin, MD, Director of the CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention has described STIs as “a persistent enemy, growing in number and outpacing our ability to respond.”5
Over the next 3 weeks, we will explore this public health issue—starting next week with the big question: Why is this trend occurring? In the meantime, feel free to share your thoughts with me at [email protected]. See you next Thursday!
While reviewing some epidemiology data for a lecture recently, I couldn’t believe my eyes: The numbers indicated an increase in sexually transmitted infections (STIs) among older Americans. Filled with doubt about the accuracy, I decided to research further. My first stop was a PA colleague who works with a mobile urgent care company that specializes in retirement communities—and she confirmed that she has witnessed this “trend”!
The fundamental public health concern for older Americans is, of course, long-term illness, disability, and dependency on others. However, experts on aging agree that since the last century, disability rates among those older than 65 have declined, as have the number of seniors living in nursing homes. Suffice it to say, the good news is that Americans are living longer—the bad news, they are doing so with an increased risk for cardiovascular disease and malignant neoplasms. The other downside is that seniors have increased risk for infectious diseases.1
Healthy People 2020 continues to recognize HIV and other STIs as problems in the United States and to promote efforts to reduce them. Unfortunately, prevention strategies for older adults in primary care settings are often not aimed at these diseases. More broadly, sexual behaviors tend to be discussed less with this population.2
The disturbing climb in STIs among older Americans is part of a more momentous national trend that the CDC says must be tackled. Overall rates of STIs in 2016 were the highest ever recorded in a single year.3 And although STI rates are highest among people ages 15 to 24, the upsurge among older Americans is larger than it is for the rest of the US population. According to the CDC, in 2016, there were 82,938 cases of gonorrhea, syphilis, and chlamydia reported among Americans ages 45 and older—about a 20% percent increase from 2015 and continuing a trend of annual increases since at least 2012.3 The infographic shows the rates for individual STIs.
The CDC notes that STIs put people “at risk for severe, lifelong health outcomes like chronic pain, severe reproductive health complications, and HIV" particularly if left untreated.4 Jonathan Mermin, MD, Director of the CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention has described STIs as “a persistent enemy, growing in number and outpacing our ability to respond.”5
Over the next 3 weeks, we will explore this public health issue—starting next week with the big question: Why is this trend occurring? In the meantime, feel free to share your thoughts with me at [email protected]. See you next Thursday!
1. Schneider M. Introduction to Public Health. 5th ed. Burlington, MA: Jones and Bartlett Learning; 2017.
2. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020: Sexually transmitted diseases. www.healthypeople.gov/2020/topics-objectives/topic/sexually-transmitted-diseases. Accessed May 6, 2019.
3. CDC. 2016 Sexually Transmitted Diseases Surveillance. www.cdc.gov/std/stats16/default.htm. Accessed May 6, 2019.
4. CDC. Fact sheet: reported STDs in the United States, 2017. www.cdc.gov/nchhstp/newsroom/docs/factsheets/std-trends-508.pdf. Accessed May 6, 2019.
5. CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. STDs at record high, indicating urgent need for prevention [press release]. September 26, 2017. www.cdc.gov/nchhstp/newsroom/2017/std-surveillance-report-2016-press-release.html. Accessed May 6, 2019.
1. Schneider M. Introduction to Public Health. 5th ed. Burlington, MA: Jones and Bartlett Learning; 2017.
2. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020: Sexually transmitted diseases. www.healthypeople.gov/2020/topics-objectives/topic/sexually-transmitted-diseases. Accessed May 6, 2019.
3. CDC. 2016 Sexually Transmitted Diseases Surveillance. www.cdc.gov/std/stats16/default.htm. Accessed May 6, 2019.
4. CDC. Fact sheet: reported STDs in the United States, 2017. www.cdc.gov/nchhstp/newsroom/docs/factsheets/std-trends-508.pdf. Accessed May 6, 2019.
5. CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. STDs at record high, indicating urgent need for prevention [press release]. September 26, 2017. www.cdc.gov/nchhstp/newsroom/2017/std-surveillance-report-2016-press-release.html. Accessed May 6, 2019.
Working With Parents to Vaccinate Children
Global outbreaks of infectious diseases—such as smallpox, pertussis, dysentery, and scarlet fever—seem like fodder for the history books. It was centuries ago that epidemics wiped out large swathes of the world population. Many people living and raising children today have never witnessed the devastating effects of measles, mumps, polio, and influenza—diseases that have been substantially reduced or even eradicated.1 Why? Because since the early 1900s, we have had scientifically developed and widely distributed vaccines at our disposal.
In context, it is incredible to realize that we are still in the beginning stages of vaccine research and development. From that perspective, it is perhaps not as surprising that some parents are hesitant to vaccinate their children—after all, do we really know everything we can and should know about inoculation? Parental resistance to or refusal of vaccination is further fueled by tainted research (Andrew Wakefield was forced to retract his findings that “validated” a link between thimerosal in vaccines and autism) and misinformation propagated on the Internet.2
But what has long been a source of frustration to those who support routine vaccination has, in recent years, started to become a public health issue. Measles outbreaks are no longer historical artifacts—they are real, as evidenced by the current rise in cases centered in Clark County, Washington. Through the first full week of February 2019, there were 101 confirmed cases of measles in the US, half of which occurred in Washington State—leading the governor to declare a public health emergency.3
This has, of course, reinvigorated the ongoing discussion about parental refusal to vaccinate. Enough has been said on this topic, by both public officials and private individuals, in a variety of venues over the years. So I’d like to focus instead on the role that individual health care providers can play in this situation.
Over the years, many of my colleagues have shared stories about parents who have refused to vaccinate their children. We know many things: These parents often fear complications from vaccination more than complications of disease. Many have religious or philosophical reasons for their reluctance or refusal to vaccinate their children. Some have concerns about vaccine safety or effectiveness. We know these things … but we don’t always know how to speak with parents about these issues.
It is somewhat ironic that the core motivation for hesitant parents and well-meaning clinicians is the same: care and protection of the child. The difficulty lies in the disparate view of what that entails. As NPs and PAs, though, our duty is to seek health benefits for and minimize harm to the patients in our care. Part of our role, when those patients are children, is to provide parents with the necessary risk-benefit information to help them make informed decisions. When the subject is vaccination, we must listen carefully and be respectful of parents’ concerns; we must recognize that their decision-making criteria may differ from ours.
So how can we bridge the gap with parents who “don’t see it the way we do”? We start by being honest with them about what is and isn’t known as far as the risks and benefits of vaccination in general or a vaccine in particular. This means acknowledging that although vaccines are very safe, they are not risk-free or 100% effective. But this also gives us the opportunity to provide them with validated data and to emphasize that the risks of any vaccine should not be considered in a silo but rather in comparison with the risks of the disease in question or of the lack of immunization.
Continue to: Helpfully, Leask and colleagues...
Helpfully, Leask and colleagues have classified parental positions on vaccination, which also provided the groundwork to offer strategies for communicating with each group.4 They identified five classes:
Unquestioning acceptors (30% to 40% of parents), who vaccinate their children and typically have no specific questions about the need for or safety of vaccines. Since this group tends to have a good relationship with their health care team but less detailed knowledge about vaccination, clinicians should continue to build rapport while providing scientific information about the vaccine being recommended or administered.4
Cautious acceptors (25% to 35%), who vaccinate their children despite having minor concerns. They tend to recognize the risk for adverse effects and hope their child will not be affected. In addition to building rapport, clinicians should provide verbal and numeric descriptions of relevant vaccine data and explain common adverse effects and disease risks.4
Hesitant vaccinators (20% to 30%), who are on the fence about the benefits and safety of vaccination. Their focus is more on the negative aspects, and they may not feel particularly trusting of their health care provider. Therefore, gaining trust is vital—parents in this group are eager to discuss their concerns with their clinician and have their questions answered satisfactorily. Motivational interviewing using a guiding style may be a helpful tool.4
Late or selective vaccinators (2% to 27%), who have significant doubts about the safety and necessity of vaccines, resulting in their choice to delay vaccination or select only some of the recommended vaccines for their child. These parents may require additional time—possibly a second appointment—in which to fully discuss their concerns. Be sure to provide up-to-date information on the risks and benefits of a vaccine, and use decision aids as appropriate.4
Continue to: Refusers...
Refusers (<2%), who have concerns about the number of vaccines children receive and conflicting feelings about whom to trust and how best to get answers to their questions. This group tends to demonstrate high knowledge levels about vaccination but may be the most argumentative when presented with information. Emphasize the importance of protecting the child from an infectious disease and reinforce the effectiveness of the vaccine. Use statistics rather than anecdotes. But above all, spend the time needed to provide refusers with a thorough understanding of the risks of not immunizing their child.4
Although it is not a universal sentiment, many parents confer trust on their health care providers. We can use this trust in a respectful, noncoercive, and non-condescending manner by providing research-supported facts about vaccines. Clinicians who listen with a compassionate ear will be in the best position to lead the hesitant, late or selective, or refusing parents to confidently make an informed decision that immunization is the best way to protect their children from vaccine-preventable diseases.4
Rather than yet again focusing on the negative, I’d like to ask: Have you had a success story of helping parents to choose vaccination for their children? How did you overcome their concerns? Share your experience with me at [email protected].
1. CDC. Achievements in public health, 1900-1999 impact of vaccines universally recommended for children—United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48(12):243-248.
2. Wakefield AJ, Murch SH, Anthony A, et al. RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351(9103):637-641.
3. Franki R. United States now over 100 measles cases for the year. MDEdge Family Practice. February 11, 2019.
4. Leask J, Kinnersley P, Jackson C, et al. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12:154.
Global outbreaks of infectious diseases—such as smallpox, pertussis, dysentery, and scarlet fever—seem like fodder for the history books. It was centuries ago that epidemics wiped out large swathes of the world population. Many people living and raising children today have never witnessed the devastating effects of measles, mumps, polio, and influenza—diseases that have been substantially reduced or even eradicated.1 Why? Because since the early 1900s, we have had scientifically developed and widely distributed vaccines at our disposal.
In context, it is incredible to realize that we are still in the beginning stages of vaccine research and development. From that perspective, it is perhaps not as surprising that some parents are hesitant to vaccinate their children—after all, do we really know everything we can and should know about inoculation? Parental resistance to or refusal of vaccination is further fueled by tainted research (Andrew Wakefield was forced to retract his findings that “validated” a link between thimerosal in vaccines and autism) and misinformation propagated on the Internet.2
But what has long been a source of frustration to those who support routine vaccination has, in recent years, started to become a public health issue. Measles outbreaks are no longer historical artifacts—they are real, as evidenced by the current rise in cases centered in Clark County, Washington. Through the first full week of February 2019, there were 101 confirmed cases of measles in the US, half of which occurred in Washington State—leading the governor to declare a public health emergency.3
This has, of course, reinvigorated the ongoing discussion about parental refusal to vaccinate. Enough has been said on this topic, by both public officials and private individuals, in a variety of venues over the years. So I’d like to focus instead on the role that individual health care providers can play in this situation.
Over the years, many of my colleagues have shared stories about parents who have refused to vaccinate their children. We know many things: These parents often fear complications from vaccination more than complications of disease. Many have religious or philosophical reasons for their reluctance or refusal to vaccinate their children. Some have concerns about vaccine safety or effectiveness. We know these things … but we don’t always know how to speak with parents about these issues.
It is somewhat ironic that the core motivation for hesitant parents and well-meaning clinicians is the same: care and protection of the child. The difficulty lies in the disparate view of what that entails. As NPs and PAs, though, our duty is to seek health benefits for and minimize harm to the patients in our care. Part of our role, when those patients are children, is to provide parents with the necessary risk-benefit information to help them make informed decisions. When the subject is vaccination, we must listen carefully and be respectful of parents’ concerns; we must recognize that their decision-making criteria may differ from ours.
So how can we bridge the gap with parents who “don’t see it the way we do”? We start by being honest with them about what is and isn’t known as far as the risks and benefits of vaccination in general or a vaccine in particular. This means acknowledging that although vaccines are very safe, they are not risk-free or 100% effective. But this also gives us the opportunity to provide them with validated data and to emphasize that the risks of any vaccine should not be considered in a silo but rather in comparison with the risks of the disease in question or of the lack of immunization.
Continue to: Helpfully, Leask and colleagues...
Helpfully, Leask and colleagues have classified parental positions on vaccination, which also provided the groundwork to offer strategies for communicating with each group.4 They identified five classes:
Unquestioning acceptors (30% to 40% of parents), who vaccinate their children and typically have no specific questions about the need for or safety of vaccines. Since this group tends to have a good relationship with their health care team but less detailed knowledge about vaccination, clinicians should continue to build rapport while providing scientific information about the vaccine being recommended or administered.4
Cautious acceptors (25% to 35%), who vaccinate their children despite having minor concerns. They tend to recognize the risk for adverse effects and hope their child will not be affected. In addition to building rapport, clinicians should provide verbal and numeric descriptions of relevant vaccine data and explain common adverse effects and disease risks.4
Hesitant vaccinators (20% to 30%), who are on the fence about the benefits and safety of vaccination. Their focus is more on the negative aspects, and they may not feel particularly trusting of their health care provider. Therefore, gaining trust is vital—parents in this group are eager to discuss their concerns with their clinician and have their questions answered satisfactorily. Motivational interviewing using a guiding style may be a helpful tool.4
Late or selective vaccinators (2% to 27%), who have significant doubts about the safety and necessity of vaccines, resulting in their choice to delay vaccination or select only some of the recommended vaccines for their child. These parents may require additional time—possibly a second appointment—in which to fully discuss their concerns. Be sure to provide up-to-date information on the risks and benefits of a vaccine, and use decision aids as appropriate.4
Continue to: Refusers...
Refusers (<2%), who have concerns about the number of vaccines children receive and conflicting feelings about whom to trust and how best to get answers to their questions. This group tends to demonstrate high knowledge levels about vaccination but may be the most argumentative when presented with information. Emphasize the importance of protecting the child from an infectious disease and reinforce the effectiveness of the vaccine. Use statistics rather than anecdotes. But above all, spend the time needed to provide refusers with a thorough understanding of the risks of not immunizing their child.4
Although it is not a universal sentiment, many parents confer trust on their health care providers. We can use this trust in a respectful, noncoercive, and non-condescending manner by providing research-supported facts about vaccines. Clinicians who listen with a compassionate ear will be in the best position to lead the hesitant, late or selective, or refusing parents to confidently make an informed decision that immunization is the best way to protect their children from vaccine-preventable diseases.4
Rather than yet again focusing on the negative, I’d like to ask: Have you had a success story of helping parents to choose vaccination for their children? How did you overcome their concerns? Share your experience with me at [email protected].
Global outbreaks of infectious diseases—such as smallpox, pertussis, dysentery, and scarlet fever—seem like fodder for the history books. It was centuries ago that epidemics wiped out large swathes of the world population. Many people living and raising children today have never witnessed the devastating effects of measles, mumps, polio, and influenza—diseases that have been substantially reduced or even eradicated.1 Why? Because since the early 1900s, we have had scientifically developed and widely distributed vaccines at our disposal.
In context, it is incredible to realize that we are still in the beginning stages of vaccine research and development. From that perspective, it is perhaps not as surprising that some parents are hesitant to vaccinate their children—after all, do we really know everything we can and should know about inoculation? Parental resistance to or refusal of vaccination is further fueled by tainted research (Andrew Wakefield was forced to retract his findings that “validated” a link between thimerosal in vaccines and autism) and misinformation propagated on the Internet.2
But what has long been a source of frustration to those who support routine vaccination has, in recent years, started to become a public health issue. Measles outbreaks are no longer historical artifacts—they are real, as evidenced by the current rise in cases centered in Clark County, Washington. Through the first full week of February 2019, there were 101 confirmed cases of measles in the US, half of which occurred in Washington State—leading the governor to declare a public health emergency.3
This has, of course, reinvigorated the ongoing discussion about parental refusal to vaccinate. Enough has been said on this topic, by both public officials and private individuals, in a variety of venues over the years. So I’d like to focus instead on the role that individual health care providers can play in this situation.
Over the years, many of my colleagues have shared stories about parents who have refused to vaccinate their children. We know many things: These parents often fear complications from vaccination more than complications of disease. Many have religious or philosophical reasons for their reluctance or refusal to vaccinate their children. Some have concerns about vaccine safety or effectiveness. We know these things … but we don’t always know how to speak with parents about these issues.
It is somewhat ironic that the core motivation for hesitant parents and well-meaning clinicians is the same: care and protection of the child. The difficulty lies in the disparate view of what that entails. As NPs and PAs, though, our duty is to seek health benefits for and minimize harm to the patients in our care. Part of our role, when those patients are children, is to provide parents with the necessary risk-benefit information to help them make informed decisions. When the subject is vaccination, we must listen carefully and be respectful of parents’ concerns; we must recognize that their decision-making criteria may differ from ours.
So how can we bridge the gap with parents who “don’t see it the way we do”? We start by being honest with them about what is and isn’t known as far as the risks and benefits of vaccination in general or a vaccine in particular. This means acknowledging that although vaccines are very safe, they are not risk-free or 100% effective. But this also gives us the opportunity to provide them with validated data and to emphasize that the risks of any vaccine should not be considered in a silo but rather in comparison with the risks of the disease in question or of the lack of immunization.
Continue to: Helpfully, Leask and colleagues...
Helpfully, Leask and colleagues have classified parental positions on vaccination, which also provided the groundwork to offer strategies for communicating with each group.4 They identified five classes:
Unquestioning acceptors (30% to 40% of parents), who vaccinate their children and typically have no specific questions about the need for or safety of vaccines. Since this group tends to have a good relationship with their health care team but less detailed knowledge about vaccination, clinicians should continue to build rapport while providing scientific information about the vaccine being recommended or administered.4
Cautious acceptors (25% to 35%), who vaccinate their children despite having minor concerns. They tend to recognize the risk for adverse effects and hope their child will not be affected. In addition to building rapport, clinicians should provide verbal and numeric descriptions of relevant vaccine data and explain common adverse effects and disease risks.4
Hesitant vaccinators (20% to 30%), who are on the fence about the benefits and safety of vaccination. Their focus is more on the negative aspects, and they may not feel particularly trusting of their health care provider. Therefore, gaining trust is vital—parents in this group are eager to discuss their concerns with their clinician and have their questions answered satisfactorily. Motivational interviewing using a guiding style may be a helpful tool.4
Late or selective vaccinators (2% to 27%), who have significant doubts about the safety and necessity of vaccines, resulting in their choice to delay vaccination or select only some of the recommended vaccines for their child. These parents may require additional time—possibly a second appointment—in which to fully discuss their concerns. Be sure to provide up-to-date information on the risks and benefits of a vaccine, and use decision aids as appropriate.4
Continue to: Refusers...
Refusers (<2%), who have concerns about the number of vaccines children receive and conflicting feelings about whom to trust and how best to get answers to their questions. This group tends to demonstrate high knowledge levels about vaccination but may be the most argumentative when presented with information. Emphasize the importance of protecting the child from an infectious disease and reinforce the effectiveness of the vaccine. Use statistics rather than anecdotes. But above all, spend the time needed to provide refusers with a thorough understanding of the risks of not immunizing their child.4
Although it is not a universal sentiment, many parents confer trust on their health care providers. We can use this trust in a respectful, noncoercive, and non-condescending manner by providing research-supported facts about vaccines. Clinicians who listen with a compassionate ear will be in the best position to lead the hesitant, late or selective, or refusing parents to confidently make an informed decision that immunization is the best way to protect their children from vaccine-preventable diseases.4
Rather than yet again focusing on the negative, I’d like to ask: Have you had a success story of helping parents to choose vaccination for their children? How did you overcome their concerns? Share your experience with me at [email protected].
1. CDC. Achievements in public health, 1900-1999 impact of vaccines universally recommended for children—United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48(12):243-248.
2. Wakefield AJ, Murch SH, Anthony A, et al. RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351(9103):637-641.
3. Franki R. United States now over 100 measles cases for the year. MDEdge Family Practice. February 11, 2019.
4. Leask J, Kinnersley P, Jackson C, et al. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12:154.
1. CDC. Achievements in public health, 1900-1999 impact of vaccines universally recommended for children—United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48(12):243-248.
2. Wakefield AJ, Murch SH, Anthony A, et al. RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351(9103):637-641.
3. Franki R. United States now over 100 measles cases for the year. MDEdge Family Practice. February 11, 2019.
4. Leask J, Kinnersley P, Jackson C, et al. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12:154.
OTP: Pipe Dream, Smoke Screen, or the Right Thing?
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
Do You Trust Your Employer?
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
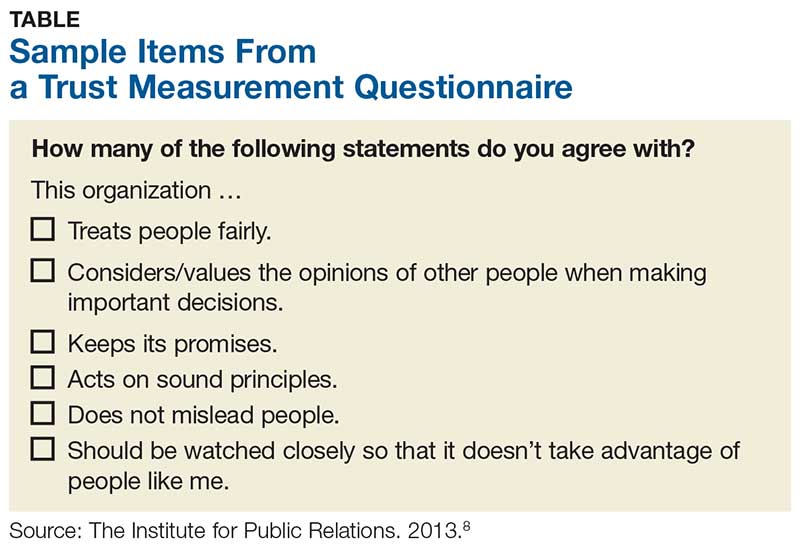
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
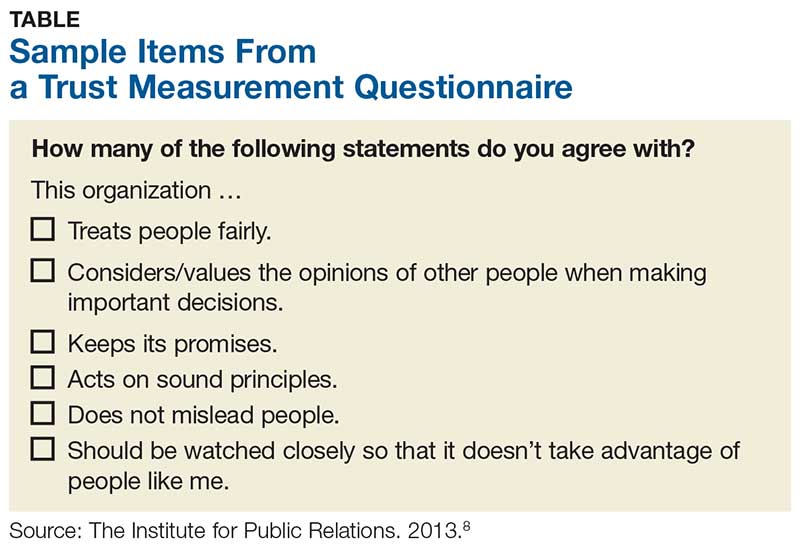
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
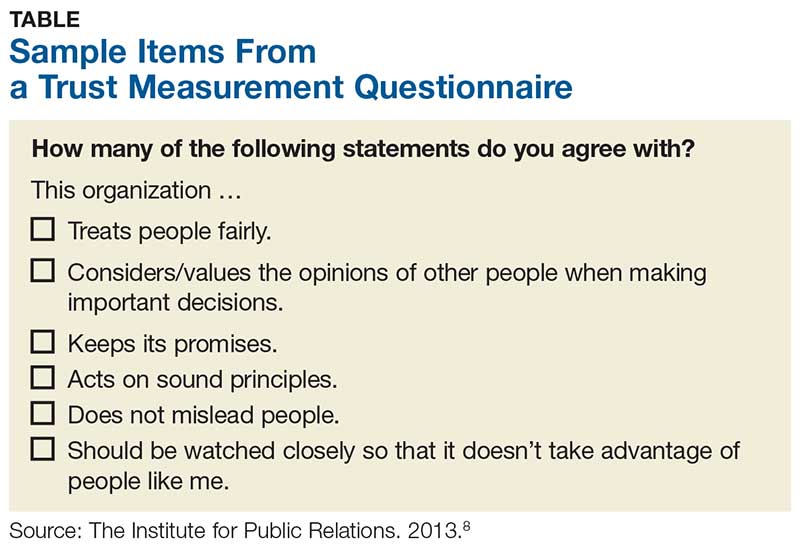
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
Silent No More: Harassment in the Workplace
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
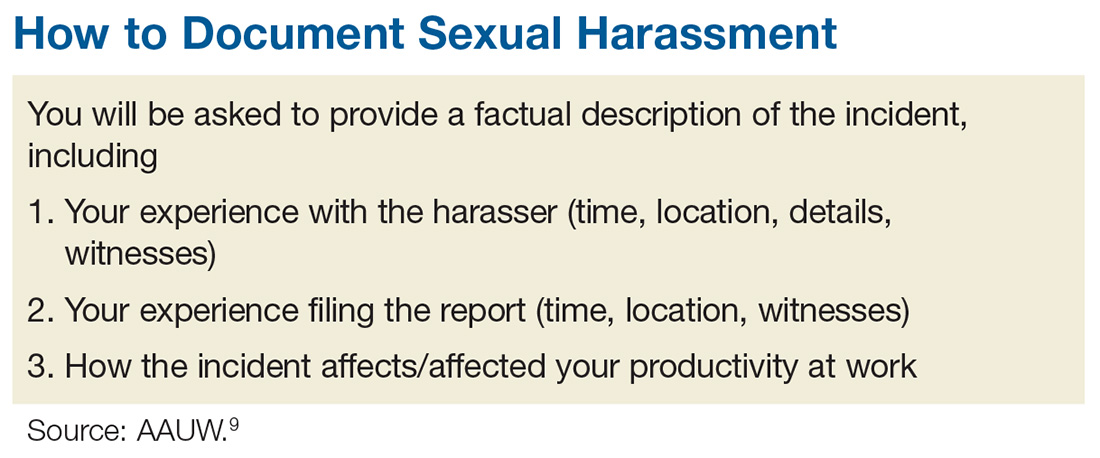
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
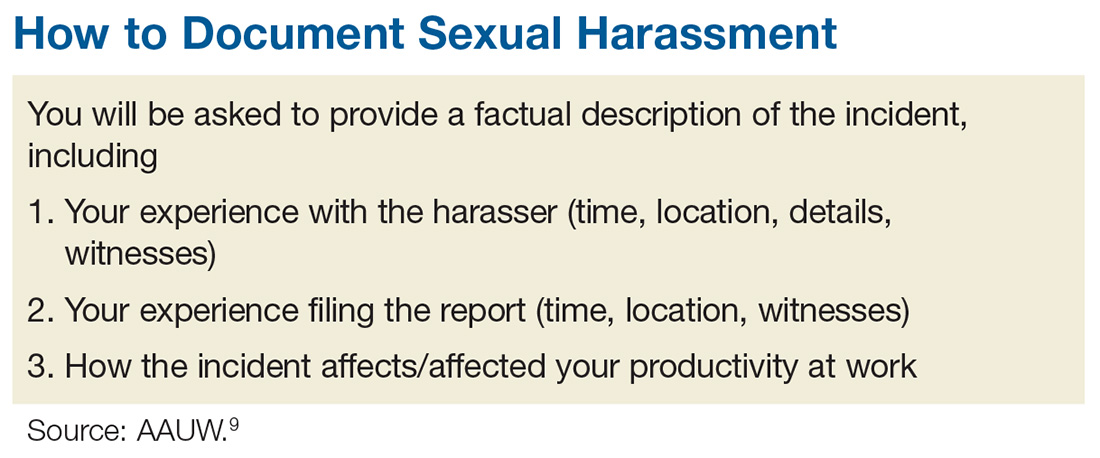
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
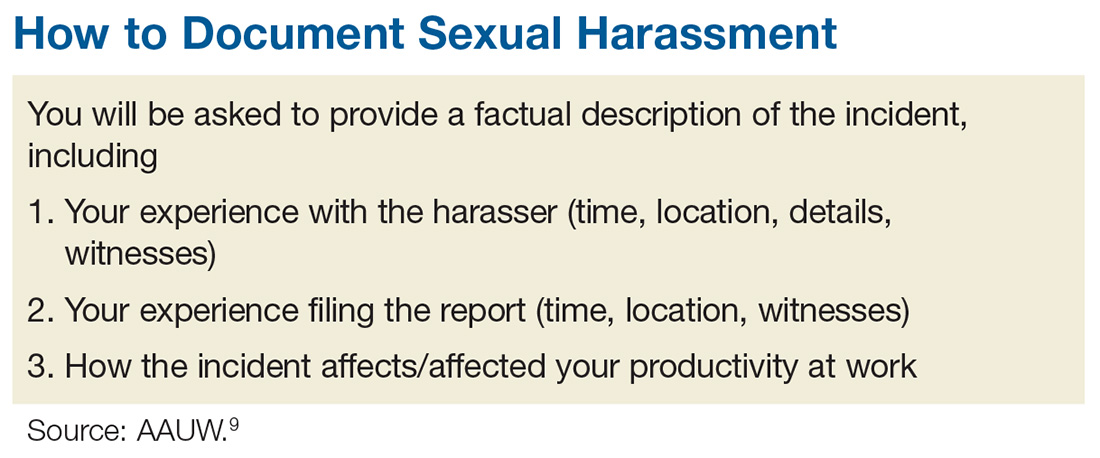
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
If You Were Surgeon General ...
This past August, President Trump, with the advice and consent of the United States Senate, nominated Indiana Health Commissioner Jerome M. Adams, MD, MPH, as the nation’s 20th Surgeon General (SG). As the country’s “doctor,” the SG has access to the best available scientific information to advise Americans of ways to improve their health and decrease risk for illness and injury. Overseen by the Office of the Assistant Secretary for Health, the Office of the Surgeon General has no budget or line authority. As a political appointee, the SG ranks three levels below a presidential cabinet member and reports to an assistant health secretary.1
The SG nominally oversees the US Public Health Service Commissioned Corps, an exclusive group of more than 6,700 public health professionals working throughout the federal government with the mission to protect, promote, and advance the health of our nation.2 In 2010, under the Affordable Care Act, the SG was designated as Chair of the National Prevention Council, which coordinates and leads 20 executive departments encouraging prevention, wellness, and health promotion activities.
Past SGs, during their time in office, have quietly gone about their duties, although some have used their platform to raise awareness of specific public health concerns. C. Everett Koop (a Reagan appointee) is among the most-remembered SGs, thanks in part to his use of the media to promote his causes, specifically smoking cessation and AIDS prevention. Newly appointed Dr. Adams, an anesthesiologist by training, is known for his focus on the opioid epidemic, tobacco use, and infant mortality.
As we’ve seen over the years, the limitations of the SG’s role equate to a mixed bag of “results.” For every C. Everett Koop (whether you agree with his views or not, he was prolific!), there are several SGs who came and went from office without making a blip on the public’s radar. Since health care remains at the forefront of our national conversation, the burning question is: If you were a consultant to the SG, which health issues would you prioritize?
I posed this question to 30 of my PA and NP colleagues. While certainly not an official survey—rather, a straw poll—I was nonetheless surprised by the overlap in responses. Here are some of the highlights.
Substance abuse/opioid crisis. Globally, one in every eight deaths result from the use of tobacco, alcohol, and other drugs. According to Humphreys et al, the implications of addiction are clear: It will do massive and increasing damage to humanity if not addressed emergently and at the source.3 But to do so, we must understand the root cause. Neuroscientific research has shown that repeated addictive drug use can rewire the brain’s motivational and reward circuits and influence decision-making.3
This is evidenced by the startling fact that every day, an average of 91 Americans die of opioid overdose.3 In March, the Director-General of the World Health Organization called for more scientifically informed public policies regarding addiction.4 The President’s Commission on Combating Drug Addiction and the Opioid Crisis released a preliminary report in August recommending next steps, which included the declaration of a federal state of emergency.5
Mental health. As you may recall from my December 2016 editorial, mental health is a forgotten facet of primary care—and one that is imperative to address.6 Only 43% of family physicians in this country provide mental health care; furthermore, half of Americans with mental health conditions go without essential care, and those with intellectual and developmental disabilities are significantly underserved.6 Perhaps increased efforts to attend to mental health in primary care will subsequently reduce addiction and substance abuse rates, resulting in a physically and mentally healthier America.
Oral health. Dr. Koop was known for his quote, “You can’t be healthy without good oral health.” Unfortunately, the major challenge expressed in Oral Health in America: A Report of the Surgeon General—“not all Americans have achieved the same level of oral health and well-being”—is as relevant today as it was when the report was released in 2000.7 We must therefore accelerate efforts toward achieving this goal. We must also address the need for a more diverse and well-distributed oral health workforce.
The CDC Division of Oral Health has made oral health an integral component of public health programs, with a goal of eliminating disparities and improving oral health for all. Continued investment in research, such as that undertaken by the National Institute of Dental and Craniofacial Research Centers for Research to Reduce Disparities in Oral Health, is critical.8 Lastly, we must continue to expand initiatives to prevent tobacco use and promote better dietary choices.
Obesity. Literature on the health consequences of obesity in both adults and children has increased exponentially in recent decades, due to the condition’s alarming prevalence in the US and other industrialized countries. The CDC reports significant racial and ethnic disparities in obesity, specifically among Hispanics/Latinos compared to non-Hispanic whites. Because obesity significantly contributes to acute and chronic diseases and has a direct relationship to morbidity and mortality, public health officials should target health prevention messages and interventions to those populations with the greatest need.9
Kidney disease. An estimated 31 million people in the US have chronic kidney disease (CKD), and it is the eighth leading cause of death in this country. Shockingly, 9 out of 10 people who have stage 3 CKD are not even aware they have it.10 The cost of CKD in the US is extortionate; research in this area is horrifically underfunded compared to that for other chronic diseases. The entire NIH budget for CKD is $31 billion, while the expense to the patient population is $32 billion—and every five minutes, someone’s kidneys fail.11
The seemingly obvious question is, what can we do to prevent CKD? As far back as 1948, SG Thomas Parran Jr. advocated for preventive and curative services.12 Alas, I recently came across an excellent poem by Joseph Malins (circa 1855) that speaks volumes about prevention versus cure (see box).
Environmental threats/emerging viruses. Particular attention should be paid to newly identified infectious agents, both locally and internationally, to prevent public health problems—for example, the Zika virus epidemic. In 1896, William Osler said, “Humanity has but three great enemies: infection, famine, and war; of these, by far the greatest, by far the most terrible is infection.”13 We know the factors that contribute to the emergence of new infections: the evolution of pathogenic infectious agents (microbial adaptation and change), development of drug resistance, and vector resistance to pesticides. Other important factors include climate and changing ecosystems, economic development and land use (eg, urbanization, deforestation), and technology and industry (eg, food processing and handling).14
Access to health care. Last but certainly not least, every respondent emphasized that we need to prioritize access to health care and eliminate socioeconomic disparities. But when we recognize that these disparities exist across all populations, we see that this is not an easy task. Lack of health insurance, lack of financial resources, irregular sources of care, legal obstacles, structural barriers, lack of health care providers, language barriers, socioeconomic disparity, and age are all contributing factors that are also obstacles.15 But in order for any of the previously discussed changes in health care to be influential, they must be accessible.
And so I open the floor to you, colleagues: What do you think should be done to improve access to health care? What are your pressing public health issues? Share your thoughts with me at [email protected].
1. Scutti S. Dr. Jerome Adams confirmed as Surgeon General. www.cnn.com/2017/08/04/health/jerome-adams-surgeon-general-confirmation/index.html. Accessed September 1, 2017.
2. U.S. Department of Health and Human Services. About the Office of the Surgeon General. www.surgeongeneral.gov/about/index.html. Accessed September 1, 2017.
3. Humphreys K, Malenka RC, Knutson B, MacCoun RJ. Brains, environments, and policy responses to addiction. Science. 2017;356(6344):1237-1238.
4. Chan M. Opening remarks at the 60th session of the Commission on Narcotic Drugs. www.who.int/dg/speeches/2017/commission-narcotic-drugs/en/. Accessed September 1, 2017.
5. Burns J. Opioid Task Force recommends state of emergency and (sort of) bold treatment agenda. www.forbes.com/sites/janetwburns/2017/08/02/opioid-task-force-recommends-state-of-emergency-and-sort-of-bold-treatment-agenda/#378810163956. Accessed September 1, 2017.
6. Danielsen RD. Mental health: a forgotten facet of primary care. Clinician Reviews. 2016;26(12):7,46.
7. NIH National Institute of Dental and Craniofacial Research. Oral health in America: report of the Surgeon General (executive summary). Rockville, MD: National Institute of Dental and Craniofacial Research; 2000. Page 287.
8. Satcher D, Nottingham JH. Revisiting oral health in America: a report of the Surgeon General. AJPH. 2017;107(suppl 1):S32-S33.
9. Hu F. Obesity Epidemiology. 2008; New York: Oxford University Press. 5-7.
10. American Kidney Fund. 2015 kidney disease statistics. www.kidneyfund.org/assets/pdf/kidney-disease-statistics.pdf. Accessed September 7, 2017.
11. Tyler. Statistics on chronic kidney disease (CKD) that may shock you. www.dietitiansathome.com/post/statistics-on-chronic-kidney-disease-ckd.
12. Sledge D. Linking public health and individual medicine: the health policy approach of Surgeon General Thomas Parran. Am J Public Health. 2017;107(4):509-516.
13. Osler W. The study of the fevers of the south. JAMA. 1896;XXVI(21):999-1004.
14. Fauci AS, Touchette NA, Folkers GK. Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases. Emerging Infectious Diseases. 2005;11(4):519-525.
15. Mandal A. Disparities in access to health care. www.news-medical.net/health/Disparities-in-Access-to-Health-Care.aspx. Accessed September 1, 2017.
This past August, President Trump, with the advice and consent of the United States Senate, nominated Indiana Health Commissioner Jerome M. Adams, MD, MPH, as the nation’s 20th Surgeon General (SG). As the country’s “doctor,” the SG has access to the best available scientific information to advise Americans of ways to improve their health and decrease risk for illness and injury. Overseen by the Office of the Assistant Secretary for Health, the Office of the Surgeon General has no budget or line authority. As a political appointee, the SG ranks three levels below a presidential cabinet member and reports to an assistant health secretary.1
The SG nominally oversees the US Public Health Service Commissioned Corps, an exclusive group of more than 6,700 public health professionals working throughout the federal government with the mission to protect, promote, and advance the health of our nation.2 In 2010, under the Affordable Care Act, the SG was designated as Chair of the National Prevention Council, which coordinates and leads 20 executive departments encouraging prevention, wellness, and health promotion activities.
Past SGs, during their time in office, have quietly gone about their duties, although some have used their platform to raise awareness of specific public health concerns. C. Everett Koop (a Reagan appointee) is among the most-remembered SGs, thanks in part to his use of the media to promote his causes, specifically smoking cessation and AIDS prevention. Newly appointed Dr. Adams, an anesthesiologist by training, is known for his focus on the opioid epidemic, tobacco use, and infant mortality.
As we’ve seen over the years, the limitations of the SG’s role equate to a mixed bag of “results.” For every C. Everett Koop (whether you agree with his views or not, he was prolific!), there are several SGs who came and went from office without making a blip on the public’s radar. Since health care remains at the forefront of our national conversation, the burning question is: If you were a consultant to the SG, which health issues would you prioritize?
I posed this question to 30 of my PA and NP colleagues. While certainly not an official survey—rather, a straw poll—I was nonetheless surprised by the overlap in responses. Here are some of the highlights.
Substance abuse/opioid crisis. Globally, one in every eight deaths result from the use of tobacco, alcohol, and other drugs. According to Humphreys et al, the implications of addiction are clear: It will do massive and increasing damage to humanity if not addressed emergently and at the source.3 But to do so, we must understand the root cause. Neuroscientific research has shown that repeated addictive drug use can rewire the brain’s motivational and reward circuits and influence decision-making.3
This is evidenced by the startling fact that every day, an average of 91 Americans die of opioid overdose.3 In March, the Director-General of the World Health Organization called for more scientifically informed public policies regarding addiction.4 The President’s Commission on Combating Drug Addiction and the Opioid Crisis released a preliminary report in August recommending next steps, which included the declaration of a federal state of emergency.5
Mental health. As you may recall from my December 2016 editorial, mental health is a forgotten facet of primary care—and one that is imperative to address.6 Only 43% of family physicians in this country provide mental health care; furthermore, half of Americans with mental health conditions go without essential care, and those with intellectual and developmental disabilities are significantly underserved.6 Perhaps increased efforts to attend to mental health in primary care will subsequently reduce addiction and substance abuse rates, resulting in a physically and mentally healthier America.
Oral health. Dr. Koop was known for his quote, “You can’t be healthy without good oral health.” Unfortunately, the major challenge expressed in Oral Health in America: A Report of the Surgeon General—“not all Americans have achieved the same level of oral health and well-being”—is as relevant today as it was when the report was released in 2000.7 We must therefore accelerate efforts toward achieving this goal. We must also address the need for a more diverse and well-distributed oral health workforce.
The CDC Division of Oral Health has made oral health an integral component of public health programs, with a goal of eliminating disparities and improving oral health for all. Continued investment in research, such as that undertaken by the National Institute of Dental and Craniofacial Research Centers for Research to Reduce Disparities in Oral Health, is critical.8 Lastly, we must continue to expand initiatives to prevent tobacco use and promote better dietary choices.
Obesity. Literature on the health consequences of obesity in both adults and children has increased exponentially in recent decades, due to the condition’s alarming prevalence in the US and other industrialized countries. The CDC reports significant racial and ethnic disparities in obesity, specifically among Hispanics/Latinos compared to non-Hispanic whites. Because obesity significantly contributes to acute and chronic diseases and has a direct relationship to morbidity and mortality, public health officials should target health prevention messages and interventions to those populations with the greatest need.9
Kidney disease. An estimated 31 million people in the US have chronic kidney disease (CKD), and it is the eighth leading cause of death in this country. Shockingly, 9 out of 10 people who have stage 3 CKD are not even aware they have it.10 The cost of CKD in the US is extortionate; research in this area is horrifically underfunded compared to that for other chronic diseases. The entire NIH budget for CKD is $31 billion, while the expense to the patient population is $32 billion—and every five minutes, someone’s kidneys fail.11
The seemingly obvious question is, what can we do to prevent CKD? As far back as 1948, SG Thomas Parran Jr. advocated for preventive and curative services.12 Alas, I recently came across an excellent poem by Joseph Malins (circa 1855) that speaks volumes about prevention versus cure (see box).
Environmental threats/emerging viruses. Particular attention should be paid to newly identified infectious agents, both locally and internationally, to prevent public health problems—for example, the Zika virus epidemic. In 1896, William Osler said, “Humanity has but three great enemies: infection, famine, and war; of these, by far the greatest, by far the most terrible is infection.”13 We know the factors that contribute to the emergence of new infections: the evolution of pathogenic infectious agents (microbial adaptation and change), development of drug resistance, and vector resistance to pesticides. Other important factors include climate and changing ecosystems, economic development and land use (eg, urbanization, deforestation), and technology and industry (eg, food processing and handling).14
Access to health care. Last but certainly not least, every respondent emphasized that we need to prioritize access to health care and eliminate socioeconomic disparities. But when we recognize that these disparities exist across all populations, we see that this is not an easy task. Lack of health insurance, lack of financial resources, irregular sources of care, legal obstacles, structural barriers, lack of health care providers, language barriers, socioeconomic disparity, and age are all contributing factors that are also obstacles.15 But in order for any of the previously discussed changes in health care to be influential, they must be accessible.
And so I open the floor to you, colleagues: What do you think should be done to improve access to health care? What are your pressing public health issues? Share your thoughts with me at [email protected].
This past August, President Trump, with the advice and consent of the United States Senate, nominated Indiana Health Commissioner Jerome M. Adams, MD, MPH, as the nation’s 20th Surgeon General (SG). As the country’s “doctor,” the SG has access to the best available scientific information to advise Americans of ways to improve their health and decrease risk for illness and injury. Overseen by the Office of the Assistant Secretary for Health, the Office of the Surgeon General has no budget or line authority. As a political appointee, the SG ranks three levels below a presidential cabinet member and reports to an assistant health secretary.1
The SG nominally oversees the US Public Health Service Commissioned Corps, an exclusive group of more than 6,700 public health professionals working throughout the federal government with the mission to protect, promote, and advance the health of our nation.2 In 2010, under the Affordable Care Act, the SG was designated as Chair of the National Prevention Council, which coordinates and leads 20 executive departments encouraging prevention, wellness, and health promotion activities.
Past SGs, during their time in office, have quietly gone about their duties, although some have used their platform to raise awareness of specific public health concerns. C. Everett Koop (a Reagan appointee) is among the most-remembered SGs, thanks in part to his use of the media to promote his causes, specifically smoking cessation and AIDS prevention. Newly appointed Dr. Adams, an anesthesiologist by training, is known for his focus on the opioid epidemic, tobacco use, and infant mortality.
As we’ve seen over the years, the limitations of the SG’s role equate to a mixed bag of “results.” For every C. Everett Koop (whether you agree with his views or not, he was prolific!), there are several SGs who came and went from office without making a blip on the public’s radar. Since health care remains at the forefront of our national conversation, the burning question is: If you were a consultant to the SG, which health issues would you prioritize?
I posed this question to 30 of my PA and NP colleagues. While certainly not an official survey—rather, a straw poll—I was nonetheless surprised by the overlap in responses. Here are some of the highlights.
Substance abuse/opioid crisis. Globally, one in every eight deaths result from the use of tobacco, alcohol, and other drugs. According to Humphreys et al, the implications of addiction are clear: It will do massive and increasing damage to humanity if not addressed emergently and at the source.3 But to do so, we must understand the root cause. Neuroscientific research has shown that repeated addictive drug use can rewire the brain’s motivational and reward circuits and influence decision-making.3
This is evidenced by the startling fact that every day, an average of 91 Americans die of opioid overdose.3 In March, the Director-General of the World Health Organization called for more scientifically informed public policies regarding addiction.4 The President’s Commission on Combating Drug Addiction and the Opioid Crisis released a preliminary report in August recommending next steps, which included the declaration of a federal state of emergency.5
Mental health. As you may recall from my December 2016 editorial, mental health is a forgotten facet of primary care—and one that is imperative to address.6 Only 43% of family physicians in this country provide mental health care; furthermore, half of Americans with mental health conditions go without essential care, and those with intellectual and developmental disabilities are significantly underserved.6 Perhaps increased efforts to attend to mental health in primary care will subsequently reduce addiction and substance abuse rates, resulting in a physically and mentally healthier America.
Oral health. Dr. Koop was known for his quote, “You can’t be healthy without good oral health.” Unfortunately, the major challenge expressed in Oral Health in America: A Report of the Surgeon General—“not all Americans have achieved the same level of oral health and well-being”—is as relevant today as it was when the report was released in 2000.7 We must therefore accelerate efforts toward achieving this goal. We must also address the need for a more diverse and well-distributed oral health workforce.
The CDC Division of Oral Health has made oral health an integral component of public health programs, with a goal of eliminating disparities and improving oral health for all. Continued investment in research, such as that undertaken by the National Institute of Dental and Craniofacial Research Centers for Research to Reduce Disparities in Oral Health, is critical.8 Lastly, we must continue to expand initiatives to prevent tobacco use and promote better dietary choices.
Obesity. Literature on the health consequences of obesity in both adults and children has increased exponentially in recent decades, due to the condition’s alarming prevalence in the US and other industrialized countries. The CDC reports significant racial and ethnic disparities in obesity, specifically among Hispanics/Latinos compared to non-Hispanic whites. Because obesity significantly contributes to acute and chronic diseases and has a direct relationship to morbidity and mortality, public health officials should target health prevention messages and interventions to those populations with the greatest need.9
Kidney disease. An estimated 31 million people in the US have chronic kidney disease (CKD), and it is the eighth leading cause of death in this country. Shockingly, 9 out of 10 people who have stage 3 CKD are not even aware they have it.10 The cost of CKD in the US is extortionate; research in this area is horrifically underfunded compared to that for other chronic diseases. The entire NIH budget for CKD is $31 billion, while the expense to the patient population is $32 billion—and every five minutes, someone’s kidneys fail.11
The seemingly obvious question is, what can we do to prevent CKD? As far back as 1948, SG Thomas Parran Jr. advocated for preventive and curative services.12 Alas, I recently came across an excellent poem by Joseph Malins (circa 1855) that speaks volumes about prevention versus cure (see box).
Environmental threats/emerging viruses. Particular attention should be paid to newly identified infectious agents, both locally and internationally, to prevent public health problems—for example, the Zika virus epidemic. In 1896, William Osler said, “Humanity has but three great enemies: infection, famine, and war; of these, by far the greatest, by far the most terrible is infection.”13 We know the factors that contribute to the emergence of new infections: the evolution of pathogenic infectious agents (microbial adaptation and change), development of drug resistance, and vector resistance to pesticides. Other important factors include climate and changing ecosystems, economic development and land use (eg, urbanization, deforestation), and technology and industry (eg, food processing and handling).14
Access to health care. Last but certainly not least, every respondent emphasized that we need to prioritize access to health care and eliminate socioeconomic disparities. But when we recognize that these disparities exist across all populations, we see that this is not an easy task. Lack of health insurance, lack of financial resources, irregular sources of care, legal obstacles, structural barriers, lack of health care providers, language barriers, socioeconomic disparity, and age are all contributing factors that are also obstacles.15 But in order for any of the previously discussed changes in health care to be influential, they must be accessible.
And so I open the floor to you, colleagues: What do you think should be done to improve access to health care? What are your pressing public health issues? Share your thoughts with me at [email protected].
1. Scutti S. Dr. Jerome Adams confirmed as Surgeon General. www.cnn.com/2017/08/04/health/jerome-adams-surgeon-general-confirmation/index.html. Accessed September 1, 2017.
2. U.S. Department of Health and Human Services. About the Office of the Surgeon General. www.surgeongeneral.gov/about/index.html. Accessed September 1, 2017.
3. Humphreys K, Malenka RC, Knutson B, MacCoun RJ. Brains, environments, and policy responses to addiction. Science. 2017;356(6344):1237-1238.
4. Chan M. Opening remarks at the 60th session of the Commission on Narcotic Drugs. www.who.int/dg/speeches/2017/commission-narcotic-drugs/en/. Accessed September 1, 2017.
5. Burns J. Opioid Task Force recommends state of emergency and (sort of) bold treatment agenda. www.forbes.com/sites/janetwburns/2017/08/02/opioid-task-force-recommends-state-of-emergency-and-sort-of-bold-treatment-agenda/#378810163956. Accessed September 1, 2017.
6. Danielsen RD. Mental health: a forgotten facet of primary care. Clinician Reviews. 2016;26(12):7,46.
7. NIH National Institute of Dental and Craniofacial Research. Oral health in America: report of the Surgeon General (executive summary). Rockville, MD: National Institute of Dental and Craniofacial Research; 2000. Page 287.
8. Satcher D, Nottingham JH. Revisiting oral health in America: a report of the Surgeon General. AJPH. 2017;107(suppl 1):S32-S33.
9. Hu F. Obesity Epidemiology. 2008; New York: Oxford University Press. 5-7.
10. American Kidney Fund. 2015 kidney disease statistics. www.kidneyfund.org/assets/pdf/kidney-disease-statistics.pdf. Accessed September 7, 2017.
11. Tyler. Statistics on chronic kidney disease (CKD) that may shock you. www.dietitiansathome.com/post/statistics-on-chronic-kidney-disease-ckd.
12. Sledge D. Linking public health and individual medicine: the health policy approach of Surgeon General Thomas Parran. Am J Public Health. 2017;107(4):509-516.
13. Osler W. The study of the fevers of the south. JAMA. 1896;XXVI(21):999-1004.
14. Fauci AS, Touchette NA, Folkers GK. Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases. Emerging Infectious Diseases. 2005;11(4):519-525.
15. Mandal A. Disparities in access to health care. www.news-medical.net/health/Disparities-in-Access-to-Health-Care.aspx. Accessed September 1, 2017.
1. Scutti S. Dr. Jerome Adams confirmed as Surgeon General. www.cnn.com/2017/08/04/health/jerome-adams-surgeon-general-confirmation/index.html. Accessed September 1, 2017.
2. U.S. Department of Health and Human Services. About the Office of the Surgeon General. www.surgeongeneral.gov/about/index.html. Accessed September 1, 2017.
3. Humphreys K, Malenka RC, Knutson B, MacCoun RJ. Brains, environments, and policy responses to addiction. Science. 2017;356(6344):1237-1238.
4. Chan M. Opening remarks at the 60th session of the Commission on Narcotic Drugs. www.who.int/dg/speeches/2017/commission-narcotic-drugs/en/. Accessed September 1, 2017.
5. Burns J. Opioid Task Force recommends state of emergency and (sort of) bold treatment agenda. www.forbes.com/sites/janetwburns/2017/08/02/opioid-task-force-recommends-state-of-emergency-and-sort-of-bold-treatment-agenda/#378810163956. Accessed September 1, 2017.
6. Danielsen RD. Mental health: a forgotten facet of primary care. Clinician Reviews. 2016;26(12):7,46.
7. NIH National Institute of Dental and Craniofacial Research. Oral health in America: report of the Surgeon General (executive summary). Rockville, MD: National Institute of Dental and Craniofacial Research; 2000. Page 287.
8. Satcher D, Nottingham JH. Revisiting oral health in America: a report of the Surgeon General. AJPH. 2017;107(suppl 1):S32-S33.
9. Hu F. Obesity Epidemiology. 2008; New York: Oxford University Press. 5-7.
10. American Kidney Fund. 2015 kidney disease statistics. www.kidneyfund.org/assets/pdf/kidney-disease-statistics.pdf. Accessed September 7, 2017.
11. Tyler. Statistics on chronic kidney disease (CKD) that may shock you. www.dietitiansathome.com/post/statistics-on-chronic-kidney-disease-ckd.
12. Sledge D. Linking public health and individual medicine: the health policy approach of Surgeon General Thomas Parran. Am J Public Health. 2017;107(4):509-516.
13. Osler W. The study of the fevers of the south. JAMA. 1896;XXVI(21):999-1004.
14. Fauci AS, Touchette NA, Folkers GK. Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases. Emerging Infectious Diseases. 2005;11(4):519-525.
15. Mandal A. Disparities in access to health care. www.news-medical.net/health/Disparities-in-Access-to-Health-Care.aspx. Accessed September 1, 2017.
