User login
On-demand pill protocol protects against HIV
Offer patients at high risk for human immunodeficiency virus (HIV), particularly men who have sex with men, preexposure prophylaxis (PrEP) with a combination pill of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) on an on-demand basis to decrease HIV-1 infection rates.
Strength of recommendation
B: Based on one good quality randomized control trial.1
Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
ILLUSTRATIVE CASE
Your patient is a 31-year-old man who has sex with men. He is sexually active with several different partners. He asks you if there is anything he can do to decrease his risk of becoming infected with human immunodeficiency virus (HIV). Besides recommending condom use, what should you offer him?
In most high-income countries, including the United States, HIV-1 infection continues to occur in high-risk groups, especially among men who have sex with men (MSM).2 Without a vaccine, condom use has served as the primary method of preventing infection.
In 2014, the Centers for Disease Control and Prevention (CDC) began recommending daily use of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) in high-risk individuals, as a form of preexposure prophylaxis (PrEP).3-5 This recommendation is based primarily on the Preexposure Prophylaxis Initiative (iPrEx) trial, which showed a relative reduction of 44% (number needed to treat [NNT]=46 over 1.2 years) in the incidence of new HIV-1 infection among men and transgender women who have sex with men when TDF-FTC was used on a daily basis.6 However, the effectiveness of this strategy in the real world has not been as high as hoped, presumably because of the difficulty in getting patients to take the medication on a daily basis.7,8
While it would likely improve adherence rates, the use of prophylaxis in an on-demand manner is not currently recommended.5 That is because, until now, there have been no studies demonstrating the effectiveness of PrEP used episodically and taken only around the time of potential exposure.
STUDY SUMMARY
Fewer pills improves adherence, reduces HIV infection rates
The Intervention Preventive de l’Exposition aux Risques avec et pour les Gays (IPERGAY) study was a double-blind, multicenter study conducted in France and Canada that assessed the efficacy and safety of prophylaxis with TDF-FTC used in an on-demand fashion by MSM.1 The study hypothesis was that adherence would be higher if chemoprophylaxis was taken only around the time of intercourse, rather than daily, and that this would further reduce the risk of HIV infection.
The study randomized 414 participants who were considered to be at high risk for acquiring HIV-1 infection. The investigators defined high risk as having a history of unprotected anal sex with at least 2 partners in the previous 6 months. Other inclusion criteria included age ≥18 years, and male or transgender female sex. Exclusion criteria included current HIV infection, hepatitis B or C infection, creatinine clearance <60 mL/min, alanine aminotransferase level >2.5 times the upper limit of normal, and significant glycosuria or proteinuria.
The pill and visit schedule. After excluding those who withdrew consent, were lost to follow-up, or who acquired HIV-1 infection, the study participants (199 in the TDF-FTC group and 201 in the placebo group) were randomized to take TDF-FTC or placebo before and after sexual activity. The dose of TDF-FTC was fixed at 300 mg of TDF and 200 mg of FTC per pill. The participants were instructed to take a loading dose of 2 pills of TDF-FTC or placebo with food 2 to 24 hours prior to intercourse, followed by a third pill 24 hours after taking the first 2 pills, and a fourth pill 24 hours after the third pill. If there were multiple consecutive days with episodes of sexual intercourse, participants were to take one pill on each of the days of intercourse, and then the 2 post-exposure pills. If sexual activity resumed within a week of the prior episode, participants were instructed to take only one pill when resuming the preexposure prophylaxis; otherwise, they were to begin again with 2 pills 2 to 24 hours prior to intercourse and repeat the protocol.
Study coordinators followed participants 4 and 8 weeks after enrollment, and then every 8 weeks subsequently. The investigators tested the participants for HIV-1 and HIV-2 at each visit and assessed adherence by pill count and drug levels in plasma, as well as with an at-home, computer-assisted interview completed by each participant prior to each visit.
Participants received counseling from a peer community member and were offered preventative services and testing for other sexually transmitted infections. They were given free condoms and gel at each visit, as well as enough pills (TDF-FTC or placebo) to cover daily use until their next visit.
Forty-three percent took the pills correctly. The participants were followed for a median of 9.3 months. Overall, 72% of the participants took the study drugs (TDF-FTC or placebo), although 29% took a suboptimal dose. There was no change in the sexual behavior of the participants during the study. The study was unblinded after 20 months and is continuing as an open-label study because of the discontinuation of another preexposure prophylaxis study in the United Kingdom, which showed an NNT of 13 to prevent one new HIV infection per year.3
An independent data and safety monitoring board recommended the unblinding because the placebo group was considered to be at significantly increased risk of contracting HIV without PrEP. The open-label part of the study, iPrex-OLE, completed enrollment and data gathering in November 2013, and the data analysis and results are presently pending.9
Eighty-six percent relative reduction in HIV. The primary end-point was the diagnosis of HIV-1 infection, and the results were based on an intention-to-treat analysis. HIV-1 infection was diagnosed in 19 study participants, with 3 of those new cases occurring between the time of randomization and enrollment. Fourteen of the cases were in the placebo group (6.6 infections per 100 person-years) and 2 of the new cases were in the TDF-FTC group (incidence 0.91 per 100 person-years). This translated to a relative reduction in the incidence of new HIV-1 seroconversion in the TDF-FTC group of 86% (95% confidence interval, 40%-98%; P=.002; NNT=17 over 9.3 months).
The 2 study participants in the TDF-FTC group diagnosed with new HIV-1 were found to be non-adherent to the prescribed prophylaxis, as they returned 58 and 60 of the 60 pills administered to them, and no study drugs were found in their plasma samples.
Adverse events included gastrointestinal symptoms of nausea, vomiting, diarrhea, and abdominal pain and were seen at a greater rate (14% vs 5%, P=.002; number needed to harm=11) in the treatment group than in the placebo group. There were also mild increases in serum creatinine level (seen in 18% of the TDF-FTC group), but only 2 participants had a transient decrease in creatinine clearance to <60 mL/min. None of the participants discontinued medications due to renal issues.
WHAT’S NEW
Risk reduction with on-demand use is nearly double that of daily use
This is the first study to look at on-demand preexposure prophylaxis with TDF-FTC to decrease the incidence of HIV-1 infection in high-risk MSM. The risk reduction in this study (86%) was much better than the 44% seen in the prior study that used daily PrEP in this population.6 We suspect the higher benefit of on-demand PrEP is likely due to increased compliance with medication use.
CAVEATS
Is fewer pills enough to maintain adherence over time?
The median length of follow-up in the study was 9.3 months. One concern is that adherence may wane over time, decreasing the efficacy of the prophylaxis. Continued efforts to improve compliance with this type of PrEP may be needed to ensure efficacy. Since the study was shortened and reported early, we will need to wait for the results of the open-label study to fully assess the risks of adverse events.
CHALLENGES TO IMPLEMENTATION
Efficacy and convenience come at a cost
The main challenge to implementation could be the cost of TDF-FTC, the retail price of which is about $50 per dose.10 Insurance coverage for the medication varies.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
2. Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS. 2013;27:2665-2678.
3. McCormack S, Dunn DT, Desai M, et al. Preexposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53-60.
4. Youle M, Wainberg MA. Could chemoprophylaxis be used as an HIV prevention strategy while we wait for an effective vaccine? AIDS. 2003;17:937-938.
5. US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States – 2014. A clinical practice guideline. Available at: https://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf. Accessed June 4, 2016.
6. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599.
7. Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372:509-518.
8. Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411-422.
9. IPrEx open-label extension. Available at: http://www.iprexnews.com. Accessed July 13, 2016.
10. GoodRx. Truvada. Available at: https://www.goodrx.com/truvada. Accessed June 4, 2016.
Offer patients at high risk for human immunodeficiency virus (HIV), particularly men who have sex with men, preexposure prophylaxis (PrEP) with a combination pill of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) on an on-demand basis to decrease HIV-1 infection rates.
Strength of recommendation
B: Based on one good quality randomized control trial.1
Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
ILLUSTRATIVE CASE
Your patient is a 31-year-old man who has sex with men. He is sexually active with several different partners. He asks you if there is anything he can do to decrease his risk of becoming infected with human immunodeficiency virus (HIV). Besides recommending condom use, what should you offer him?
In most high-income countries, including the United States, HIV-1 infection continues to occur in high-risk groups, especially among men who have sex with men (MSM).2 Without a vaccine, condom use has served as the primary method of preventing infection.
In 2014, the Centers for Disease Control and Prevention (CDC) began recommending daily use of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) in high-risk individuals, as a form of preexposure prophylaxis (PrEP).3-5 This recommendation is based primarily on the Preexposure Prophylaxis Initiative (iPrEx) trial, which showed a relative reduction of 44% (number needed to treat [NNT]=46 over 1.2 years) in the incidence of new HIV-1 infection among men and transgender women who have sex with men when TDF-FTC was used on a daily basis.6 However, the effectiveness of this strategy in the real world has not been as high as hoped, presumably because of the difficulty in getting patients to take the medication on a daily basis.7,8
While it would likely improve adherence rates, the use of prophylaxis in an on-demand manner is not currently recommended.5 That is because, until now, there have been no studies demonstrating the effectiveness of PrEP used episodically and taken only around the time of potential exposure.
STUDY SUMMARY
Fewer pills improves adherence, reduces HIV infection rates
The Intervention Preventive de l’Exposition aux Risques avec et pour les Gays (IPERGAY) study was a double-blind, multicenter study conducted in France and Canada that assessed the efficacy and safety of prophylaxis with TDF-FTC used in an on-demand fashion by MSM.1 The study hypothesis was that adherence would be higher if chemoprophylaxis was taken only around the time of intercourse, rather than daily, and that this would further reduce the risk of HIV infection.
The study randomized 414 participants who were considered to be at high risk for acquiring HIV-1 infection. The investigators defined high risk as having a history of unprotected anal sex with at least 2 partners in the previous 6 months. Other inclusion criteria included age ≥18 years, and male or transgender female sex. Exclusion criteria included current HIV infection, hepatitis B or C infection, creatinine clearance <60 mL/min, alanine aminotransferase level >2.5 times the upper limit of normal, and significant glycosuria or proteinuria.
The pill and visit schedule. After excluding those who withdrew consent, were lost to follow-up, or who acquired HIV-1 infection, the study participants (199 in the TDF-FTC group and 201 in the placebo group) were randomized to take TDF-FTC or placebo before and after sexual activity. The dose of TDF-FTC was fixed at 300 mg of TDF and 200 mg of FTC per pill. The participants were instructed to take a loading dose of 2 pills of TDF-FTC or placebo with food 2 to 24 hours prior to intercourse, followed by a third pill 24 hours after taking the first 2 pills, and a fourth pill 24 hours after the third pill. If there were multiple consecutive days with episodes of sexual intercourse, participants were to take one pill on each of the days of intercourse, and then the 2 post-exposure pills. If sexual activity resumed within a week of the prior episode, participants were instructed to take only one pill when resuming the preexposure prophylaxis; otherwise, they were to begin again with 2 pills 2 to 24 hours prior to intercourse and repeat the protocol.
Study coordinators followed participants 4 and 8 weeks after enrollment, and then every 8 weeks subsequently. The investigators tested the participants for HIV-1 and HIV-2 at each visit and assessed adherence by pill count and drug levels in plasma, as well as with an at-home, computer-assisted interview completed by each participant prior to each visit.
Participants received counseling from a peer community member and were offered preventative services and testing for other sexually transmitted infections. They were given free condoms and gel at each visit, as well as enough pills (TDF-FTC or placebo) to cover daily use until their next visit.
Forty-three percent took the pills correctly. The participants were followed for a median of 9.3 months. Overall, 72% of the participants took the study drugs (TDF-FTC or placebo), although 29% took a suboptimal dose. There was no change in the sexual behavior of the participants during the study. The study was unblinded after 20 months and is continuing as an open-label study because of the discontinuation of another preexposure prophylaxis study in the United Kingdom, which showed an NNT of 13 to prevent one new HIV infection per year.3
An independent data and safety monitoring board recommended the unblinding because the placebo group was considered to be at significantly increased risk of contracting HIV without PrEP. The open-label part of the study, iPrex-OLE, completed enrollment and data gathering in November 2013, and the data analysis and results are presently pending.9
Eighty-six percent relative reduction in HIV. The primary end-point was the diagnosis of HIV-1 infection, and the results were based on an intention-to-treat analysis. HIV-1 infection was diagnosed in 19 study participants, with 3 of those new cases occurring between the time of randomization and enrollment. Fourteen of the cases were in the placebo group (6.6 infections per 100 person-years) and 2 of the new cases were in the TDF-FTC group (incidence 0.91 per 100 person-years). This translated to a relative reduction in the incidence of new HIV-1 seroconversion in the TDF-FTC group of 86% (95% confidence interval, 40%-98%; P=.002; NNT=17 over 9.3 months).
The 2 study participants in the TDF-FTC group diagnosed with new HIV-1 were found to be non-adherent to the prescribed prophylaxis, as they returned 58 and 60 of the 60 pills administered to them, and no study drugs were found in their plasma samples.
Adverse events included gastrointestinal symptoms of nausea, vomiting, diarrhea, and abdominal pain and were seen at a greater rate (14% vs 5%, P=.002; number needed to harm=11) in the treatment group than in the placebo group. There were also mild increases in serum creatinine level (seen in 18% of the TDF-FTC group), but only 2 participants had a transient decrease in creatinine clearance to <60 mL/min. None of the participants discontinued medications due to renal issues.
WHAT’S NEW
Risk reduction with on-demand use is nearly double that of daily use
This is the first study to look at on-demand preexposure prophylaxis with TDF-FTC to decrease the incidence of HIV-1 infection in high-risk MSM. The risk reduction in this study (86%) was much better than the 44% seen in the prior study that used daily PrEP in this population.6 We suspect the higher benefit of on-demand PrEP is likely due to increased compliance with medication use.
CAVEATS
Is fewer pills enough to maintain adherence over time?
The median length of follow-up in the study was 9.3 months. One concern is that adherence may wane over time, decreasing the efficacy of the prophylaxis. Continued efforts to improve compliance with this type of PrEP may be needed to ensure efficacy. Since the study was shortened and reported early, we will need to wait for the results of the open-label study to fully assess the risks of adverse events.
CHALLENGES TO IMPLEMENTATION
Efficacy and convenience come at a cost
The main challenge to implementation could be the cost of TDF-FTC, the retail price of which is about $50 per dose.10 Insurance coverage for the medication varies.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Offer patients at high risk for human immunodeficiency virus (HIV), particularly men who have sex with men, preexposure prophylaxis (PrEP) with a combination pill of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) on an on-demand basis to decrease HIV-1 infection rates.
Strength of recommendation
B: Based on one good quality randomized control trial.1
Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
ILLUSTRATIVE CASE
Your patient is a 31-year-old man who has sex with men. He is sexually active with several different partners. He asks you if there is anything he can do to decrease his risk of becoming infected with human immunodeficiency virus (HIV). Besides recommending condom use, what should you offer him?
In most high-income countries, including the United States, HIV-1 infection continues to occur in high-risk groups, especially among men who have sex with men (MSM).2 Without a vaccine, condom use has served as the primary method of preventing infection.
In 2014, the Centers for Disease Control and Prevention (CDC) began recommending daily use of tenofovir disoproxil fumarate and emtricitabine (TDF-FTC) in high-risk individuals, as a form of preexposure prophylaxis (PrEP).3-5 This recommendation is based primarily on the Preexposure Prophylaxis Initiative (iPrEx) trial, which showed a relative reduction of 44% (number needed to treat [NNT]=46 over 1.2 years) in the incidence of new HIV-1 infection among men and transgender women who have sex with men when TDF-FTC was used on a daily basis.6 However, the effectiveness of this strategy in the real world has not been as high as hoped, presumably because of the difficulty in getting patients to take the medication on a daily basis.7,8
While it would likely improve adherence rates, the use of prophylaxis in an on-demand manner is not currently recommended.5 That is because, until now, there have been no studies demonstrating the effectiveness of PrEP used episodically and taken only around the time of potential exposure.
STUDY SUMMARY
Fewer pills improves adherence, reduces HIV infection rates
The Intervention Preventive de l’Exposition aux Risques avec et pour les Gays (IPERGAY) study was a double-blind, multicenter study conducted in France and Canada that assessed the efficacy and safety of prophylaxis with TDF-FTC used in an on-demand fashion by MSM.1 The study hypothesis was that adherence would be higher if chemoprophylaxis was taken only around the time of intercourse, rather than daily, and that this would further reduce the risk of HIV infection.
The study randomized 414 participants who were considered to be at high risk for acquiring HIV-1 infection. The investigators defined high risk as having a history of unprotected anal sex with at least 2 partners in the previous 6 months. Other inclusion criteria included age ≥18 years, and male or transgender female sex. Exclusion criteria included current HIV infection, hepatitis B or C infection, creatinine clearance <60 mL/min, alanine aminotransferase level >2.5 times the upper limit of normal, and significant glycosuria or proteinuria.
The pill and visit schedule. After excluding those who withdrew consent, were lost to follow-up, or who acquired HIV-1 infection, the study participants (199 in the TDF-FTC group and 201 in the placebo group) were randomized to take TDF-FTC or placebo before and after sexual activity. The dose of TDF-FTC was fixed at 300 mg of TDF and 200 mg of FTC per pill. The participants were instructed to take a loading dose of 2 pills of TDF-FTC or placebo with food 2 to 24 hours prior to intercourse, followed by a third pill 24 hours after taking the first 2 pills, and a fourth pill 24 hours after the third pill. If there were multiple consecutive days with episodes of sexual intercourse, participants were to take one pill on each of the days of intercourse, and then the 2 post-exposure pills. If sexual activity resumed within a week of the prior episode, participants were instructed to take only one pill when resuming the preexposure prophylaxis; otherwise, they were to begin again with 2 pills 2 to 24 hours prior to intercourse and repeat the protocol.
Study coordinators followed participants 4 and 8 weeks after enrollment, and then every 8 weeks subsequently. The investigators tested the participants for HIV-1 and HIV-2 at each visit and assessed adherence by pill count and drug levels in plasma, as well as with an at-home, computer-assisted interview completed by each participant prior to each visit.
Participants received counseling from a peer community member and were offered preventative services and testing for other sexually transmitted infections. They were given free condoms and gel at each visit, as well as enough pills (TDF-FTC or placebo) to cover daily use until their next visit.
Forty-three percent took the pills correctly. The participants were followed for a median of 9.3 months. Overall, 72% of the participants took the study drugs (TDF-FTC or placebo), although 29% took a suboptimal dose. There was no change in the sexual behavior of the participants during the study. The study was unblinded after 20 months and is continuing as an open-label study because of the discontinuation of another preexposure prophylaxis study in the United Kingdom, which showed an NNT of 13 to prevent one new HIV infection per year.3
An independent data and safety monitoring board recommended the unblinding because the placebo group was considered to be at significantly increased risk of contracting HIV without PrEP. The open-label part of the study, iPrex-OLE, completed enrollment and data gathering in November 2013, and the data analysis and results are presently pending.9
Eighty-six percent relative reduction in HIV. The primary end-point was the diagnosis of HIV-1 infection, and the results were based on an intention-to-treat analysis. HIV-1 infection was diagnosed in 19 study participants, with 3 of those new cases occurring between the time of randomization and enrollment. Fourteen of the cases were in the placebo group (6.6 infections per 100 person-years) and 2 of the new cases were in the TDF-FTC group (incidence 0.91 per 100 person-years). This translated to a relative reduction in the incidence of new HIV-1 seroconversion in the TDF-FTC group of 86% (95% confidence interval, 40%-98%; P=.002; NNT=17 over 9.3 months).
The 2 study participants in the TDF-FTC group diagnosed with new HIV-1 were found to be non-adherent to the prescribed prophylaxis, as they returned 58 and 60 of the 60 pills administered to them, and no study drugs were found in their plasma samples.
Adverse events included gastrointestinal symptoms of nausea, vomiting, diarrhea, and abdominal pain and were seen at a greater rate (14% vs 5%, P=.002; number needed to harm=11) in the treatment group than in the placebo group. There were also mild increases in serum creatinine level (seen in 18% of the TDF-FTC group), but only 2 participants had a transient decrease in creatinine clearance to <60 mL/min. None of the participants discontinued medications due to renal issues.
WHAT’S NEW
Risk reduction with on-demand use is nearly double that of daily use
This is the first study to look at on-demand preexposure prophylaxis with TDF-FTC to decrease the incidence of HIV-1 infection in high-risk MSM. The risk reduction in this study (86%) was much better than the 44% seen in the prior study that used daily PrEP in this population.6 We suspect the higher benefit of on-demand PrEP is likely due to increased compliance with medication use.
CAVEATS
Is fewer pills enough to maintain adherence over time?
The median length of follow-up in the study was 9.3 months. One concern is that adherence may wane over time, decreasing the efficacy of the prophylaxis. Continued efforts to improve compliance with this type of PrEP may be needed to ensure efficacy. Since the study was shortened and reported early, we will need to wait for the results of the open-label study to fully assess the risks of adverse events.
CHALLENGES TO IMPLEMENTATION
Efficacy and convenience come at a cost
The main challenge to implementation could be the cost of TDF-FTC, the retail price of which is about $50 per dose.10 Insurance coverage for the medication varies.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
2. Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS. 2013;27:2665-2678.
3. McCormack S, Dunn DT, Desai M, et al. Preexposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53-60.
4. Youle M, Wainberg MA. Could chemoprophylaxis be used as an HIV prevention strategy while we wait for an effective vaccine? AIDS. 2003;17:937-938.
5. US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States – 2014. A clinical practice guideline. Available at: https://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf. Accessed June 4, 2016.
6. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599.
7. Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372:509-518.
8. Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411-422.
9. IPrEx open-label extension. Available at: http://www.iprexnews.com. Accessed July 13, 2016.
10. GoodRx. Truvada. Available at: https://www.goodrx.com/truvada. Accessed June 4, 2016.
1. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246.
2. Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS. 2013;27:2665-2678.
3. McCormack S, Dunn DT, Desai M, et al. Preexposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53-60.
4. Youle M, Wainberg MA. Could chemoprophylaxis be used as an HIV prevention strategy while we wait for an effective vaccine? AIDS. 2003;17:937-938.
5. US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States – 2014. A clinical practice guideline. Available at: https://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf. Accessed June 4, 2016.
6. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599.
7. Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372:509-518.
8. Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411-422.
9. IPrEx open-label extension. Available at: http://www.iprexnews.com. Accessed July 13, 2016.
10. GoodRx. Truvada. Available at: https://www.goodrx.com/truvada. Accessed June 4, 2016.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Kidney Stones? It’s Time to Rethink Those Meds
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
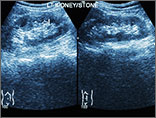
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
Kidney stones? It’s time to rethink those meds
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Skip This Step When Checking Lipid Levels
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
Skip this step when checking lipid levels
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), high-density lipoprotein cholesterol (HDL), and low-density lipoprotein cholesterol (LDL) levels are equally predictive of cardiovascular mortality and all-cause mortality.1
Strength of recommendation
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.
Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
Illustrative case
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million US adults have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 years and older, for all men ages 20 to 35 years who are at increased risk for coronary heart disease, and for all women ages 20 years and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these tests can be performed on fasting or nonfasting samples, but if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels >400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The Centers for Disease Control and Prevention (CDC) estimates that over 20% of US adults (more than 48 million people) have not had a screening lipid panel in the previous 5 years.12 One barrier to screening is that both physicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
STUDY SUMMARY: There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES-III survey to compare the prognostic value of fasting vs nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES-III is a nationally representative cross-sectional survey that was performed from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 years and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible due to missing HDL, TC, or triglyceride levels were excluded. Those with triglycerides ≥400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥8 hours or <8 hours) and followed for a mean of 14 (± .22) years. To control for possible cofounders, researchers used propensity score matching to identify 4299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator curve (ROC) using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment of potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (<100 mg/dL, 100-130 mg/dL, and >130 mg/dL).
As expected, compared to individuals in the first LDL tertile (<100 mg/dL), those with a higher LDL had an increased risk of all-cause mortality (hazard ratio [HR]=1.61; 95% confidence interval [CI], 1.25-2.08 [second tertile] and HR=2.10; 95% CI, 1.70-2.61 [third tertile]). The prognostic value of fasting vs nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 [95% CI, 0.56-0.61] vs 0.58 [95% CI, 0.56-0.60]; P=.73).
The risk of cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting vs nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 [95% CI, 0.62-0.66] vs 0.63 [95% CI, 0.60-0.65]; P=.49). In addition, fasting vs nonfasting C-statistics were similar for both diabetic and non-diabetic patients.
WHAT’S NEW: Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL values for predicting mortality; it demonstrated that they are essentially the same.
CAVEATS: Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels >400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides >400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION: Dropping the requirement to fast goes against established practice
It may be difficult for physicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
* The C-statistic is the probability that predicting the outcome is better than chance and is used to compare the goodness of fit of logistic regression models. Values for this measure range from 0.5 to 1.0. A value of 0.5 indicates that the model is no better than chance at making a prediction of membership in a group and a value of 1.0 indicates that the model perfectly identifies those within a group and those not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. Centers for Disease Control and Prevention (CDC). Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Final recommendation statement: Lipid disorders in adults (cholesterol, dyslipidemia): Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed January 20, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult - 2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; Centers for Disease Control and Prevention (CDC). Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed October 13, 2014.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), high-density lipoprotein cholesterol (HDL), and low-density lipoprotein cholesterol (LDL) levels are equally predictive of cardiovascular mortality and all-cause mortality.1
Strength of recommendation
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.
Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
Illustrative case
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million US adults have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 years and older, for all men ages 20 to 35 years who are at increased risk for coronary heart disease, and for all women ages 20 years and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these tests can be performed on fasting or nonfasting samples, but if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels >400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The Centers for Disease Control and Prevention (CDC) estimates that over 20% of US adults (more than 48 million people) have not had a screening lipid panel in the previous 5 years.12 One barrier to screening is that both physicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
STUDY SUMMARY: There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES-III survey to compare the prognostic value of fasting vs nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES-III is a nationally representative cross-sectional survey that was performed from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 years and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible due to missing HDL, TC, or triglyceride levels were excluded. Those with triglycerides ≥400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥8 hours or <8 hours) and followed for a mean of 14 (± .22) years. To control for possible cofounders, researchers used propensity score matching to identify 4299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator curve (ROC) using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment of potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (<100 mg/dL, 100-130 mg/dL, and >130 mg/dL).
As expected, compared to individuals in the first LDL tertile (<100 mg/dL), those with a higher LDL had an increased risk of all-cause mortality (hazard ratio [HR]=1.61; 95% confidence interval [CI], 1.25-2.08 [second tertile] and HR=2.10; 95% CI, 1.70-2.61 [third tertile]). The prognostic value of fasting vs nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 [95% CI, 0.56-0.61] vs 0.58 [95% CI, 0.56-0.60]; P=.73).
The risk of cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting vs nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 [95% CI, 0.62-0.66] vs 0.63 [95% CI, 0.60-0.65]; P=.49). In addition, fasting vs nonfasting C-statistics were similar for both diabetic and non-diabetic patients.
WHAT’S NEW: Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL values for predicting mortality; it demonstrated that they are essentially the same.
CAVEATS: Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels >400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides >400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION: Dropping the requirement to fast goes against established practice
It may be difficult for physicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
* The C-statistic is the probability that predicting the outcome is better than chance and is used to compare the goodness of fit of logistic regression models. Values for this measure range from 0.5 to 1.0. A value of 0.5 indicates that the model is no better than chance at making a prediction of membership in a group and a value of 1.0 indicates that the model perfectly identifies those within a group and those not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), high-density lipoprotein cholesterol (HDL), and low-density lipoprotein cholesterol (LDL) levels are equally predictive of cardiovascular mortality and all-cause mortality.1
Strength of recommendation
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.
Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
Illustrative case
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million US adults have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 years and older, for all men ages 20 to 35 years who are at increased risk for coronary heart disease, and for all women ages 20 years and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these tests can be performed on fasting or nonfasting samples, but if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels >400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The Centers for Disease Control and Prevention (CDC) estimates that over 20% of US adults (more than 48 million people) have not had a screening lipid panel in the previous 5 years.12 One barrier to screening is that both physicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
STUDY SUMMARY: There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES-III survey to compare the prognostic value of fasting vs nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES-III is a nationally representative cross-sectional survey that was performed from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 years and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible due to missing HDL, TC, or triglyceride levels were excluded. Those with triglycerides ≥400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥8 hours or <8 hours) and followed for a mean of 14 (± .22) years. To control for possible cofounders, researchers used propensity score matching to identify 4299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator curve (ROC) using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment of potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (<100 mg/dL, 100-130 mg/dL, and >130 mg/dL).
As expected, compared to individuals in the first LDL tertile (<100 mg/dL), those with a higher LDL had an increased risk of all-cause mortality (hazard ratio [HR]=1.61; 95% confidence interval [CI], 1.25-2.08 [second tertile] and HR=2.10; 95% CI, 1.70-2.61 [third tertile]). The prognostic value of fasting vs nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 [95% CI, 0.56-0.61] vs 0.58 [95% CI, 0.56-0.60]; P=.73).
The risk of cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting vs nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 [95% CI, 0.62-0.66] vs 0.63 [95% CI, 0.60-0.65]; P=.49). In addition, fasting vs nonfasting C-statistics were similar for both diabetic and non-diabetic patients.
WHAT’S NEW: Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL values for predicting mortality; it demonstrated that they are essentially the same.
CAVEATS: Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels >400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides >400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION: Dropping the requirement to fast goes against established practice
It may be difficult for physicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
* The C-statistic is the probability that predicting the outcome is better than chance and is used to compare the goodness of fit of logistic regression models. Values for this measure range from 0.5 to 1.0. A value of 0.5 indicates that the model is no better than chance at making a prediction of membership in a group and a value of 1.0 indicates that the model perfectly identifies those within a group and those not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. Centers for Disease Control and Prevention (CDC). Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Final recommendation statement: Lipid disorders in adults (cholesterol, dyslipidemia): Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed January 20, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult - 2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; Centers for Disease Control and Prevention (CDC). Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed October 13, 2014.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. Centers for Disease Control and Prevention (CDC). Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Final recommendation statement: Lipid disorders in adults (cholesterol, dyslipidemia): Screening. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed January 20, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult - 2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; Centers for Disease Control and Prevention (CDC). Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed October 13, 2014.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
Copyright © 2015 Family Physicians Inquiries Network. All rights reserved.
An Antiemetic for Irritable Bowel Syndrome?
PRACTICE CHANGER
Consider prescribing ondansetron (up to 24 mg/d) for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
STRENGTH OF RECOMMENDATION
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).1
ILLUSTRATIVE CASE
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation.
She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits: constipation (IBS-C), diarrhea (IBS-D), or alternating periods of both—mixed (IBS-M).2 The diagnosis is based on Rome III criteria, which include recurrent abdominal pain or discomfort on at least three days per month in the past three months associated with two or more of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments—including fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors—are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5-HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns about ischemic colitis and severe constipation.12 It was reintroduced in 2002 but can be prescribed only by clinicians who enroll in a prescribing program provided by the manufacturer, and there are restrictions on its use.
Ondansetron—another 5-HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted an RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
Study summary >>
STUDY SUMMARY
Ondansetron improves stool consistency, severity of IBS symptoms
In a five-week, double-blind crossover RCT, Garsed et al1 compared ondansetron with placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria included pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or enrollment in another trial.
Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last two weeks of the study. There was a two- to three-week washout between treatment periods.
The primary endpoint was average stool consistency in the last two weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (type 1) to watery (type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was –0.9, indicating slightly more formed stool with use of ondansetron. Scores for IBS severity—mild (a score of 75 to 175 out of 500), moderate (175 to 300), or severe (> 300)—were reduced by more points with ondansetron than with placebo (83 ± 9.8 vs 37 ± 9.7, respectively). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation and lower urgency scores. Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group.
Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as seven days but returned after ondansetron use stopped (typically within two weeks). Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW
Another option for IBS-D
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS
Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation.
This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk for adverse effects.15
CHALLENGES TO IMPLEMENTATION
Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who have diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation or those with mixed symptoms.
REFERENCES
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(10):600-602.
PRACTICE CHANGER
Consider prescribing ondansetron (up to 24 mg/d) for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
STRENGTH OF RECOMMENDATION
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).1
ILLUSTRATIVE CASE
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation.
She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits: constipation (IBS-C), diarrhea (IBS-D), or alternating periods of both—mixed (IBS-M).2 The diagnosis is based on Rome III criteria, which include recurrent abdominal pain or discomfort on at least three days per month in the past three months associated with two or more of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments—including fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors—are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5-HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns about ischemic colitis and severe constipation.12 It was reintroduced in 2002 but can be prescribed only by clinicians who enroll in a prescribing program provided by the manufacturer, and there are restrictions on its use.
Ondansetron—another 5-HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted an RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
Study summary >>
STUDY SUMMARY
Ondansetron improves stool consistency, severity of IBS symptoms
In a five-week, double-blind crossover RCT, Garsed et al1 compared ondansetron with placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria included pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or enrollment in another trial.
Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last two weeks of the study. There was a two- to three-week washout between treatment periods.
The primary endpoint was average stool consistency in the last two weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (type 1) to watery (type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was –0.9, indicating slightly more formed stool with use of ondansetron. Scores for IBS severity—mild (a score of 75 to 175 out of 500), moderate (175 to 300), or severe (> 300)—were reduced by more points with ondansetron than with placebo (83 ± 9.8 vs 37 ± 9.7, respectively). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation and lower urgency scores. Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group.
Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as seven days but returned after ondansetron use stopped (typically within two weeks). Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW
Another option for IBS-D
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS
Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation.
This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk for adverse effects.15
CHALLENGES TO IMPLEMENTATION
Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who have diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation or those with mixed symptoms.
REFERENCES
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(10):600-602.
PRACTICE CHANGER
Consider prescribing ondansetron (up to 24 mg/d) for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
STRENGTH OF RECOMMENDATION
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).1
ILLUSTRATIVE CASE
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation.
She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits: constipation (IBS-C), diarrhea (IBS-D), or alternating periods of both—mixed (IBS-M).2 The diagnosis is based on Rome III criteria, which include recurrent abdominal pain or discomfort on at least three days per month in the past three months associated with two or more of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments—including fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors—are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5-HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns about ischemic colitis and severe constipation.12 It was reintroduced in 2002 but can be prescribed only by clinicians who enroll in a prescribing program provided by the manufacturer, and there are restrictions on its use.
Ondansetron—another 5-HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted an RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
Study summary >>
STUDY SUMMARY
Ondansetron improves stool consistency, severity of IBS symptoms
In a five-week, double-blind crossover RCT, Garsed et al1 compared ondansetron with placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria included pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or enrollment in another trial.
Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last two weeks of the study. There was a two- to three-week washout between treatment periods.
The primary endpoint was average stool consistency in the last two weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (type 1) to watery (type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was –0.9, indicating slightly more formed stool with use of ondansetron. Scores for IBS severity—mild (a score of 75 to 175 out of 500), moderate (175 to 300), or severe (> 300)—were reduced by more points with ondansetron than with placebo (83 ± 9.8 vs 37 ± 9.7, respectively). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation and lower urgency scores. Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group.
Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as seven days but returned after ondansetron use stopped (typically within two weeks). Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW
Another option for IBS-D
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS
Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation.
This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk for adverse effects.15
CHALLENGES TO IMPLEMENTATION
Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who have diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation or those with mixed symptoms.
REFERENCES
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(10):600-602.
An antiemetic for irritable bowel syndrome?
Consider prescribing ondansetron up to 24 mg/d for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
Strength of recommendation
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).
Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
Illustrative case
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation. She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn’s disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits (constipation [IBS-C], diarrhea [IBS-D], or alternating periods of both—mixed [IBS-M]).2 It is diagnosed based on Rome III criteria—recurrent abdominal pain or discomfort at least 3 days/month in the last 3 months associated with ≥2 of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments, which include fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors, are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns of ischemic colitis and severe constipation.12 It was reintroduced in 2002, but can be prescribed only by physicians who enroll in a prescribing program provided by the manufacturer, and the drug has restrictions on its use.
Ondansetron—a different 5HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted a RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
STUDY SUMMARY: Ondansetron improves stool consistency, severity of IBS symptoms
In a 5-week, double-blind crossover RCT, Garsed et al1 compared ondansetron vs placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria were pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or being in another trial. Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last 2 weeks of the study. There was a 2- to 3-week washout between treatment periods.
The primary endpoint was average stool consistency in the last 2 weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (Type 1) to watery (Type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was -0.9 (95% confidence interval [CI], -1.1 to -0.6; P<.001), indicating slightly more formed stool with use of ondansetron. The IBS Severity Scoring System score (maximum score 500 points, with mild, moderate, and severe cases indicated by scores of 75-175, 175-300, and >300, respectively) was reduced by more points with ondansetron than placebo (83 ± 9.8 vs 37 ± 9.7; P=.001). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation (P=.002) and lower urgency scores (P<.001). Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group (95% CI, 6-14 hours; P<.001). Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as 7 days but returned after stopping ondansetron, typically within 2 weeks. Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW: Another option for IBS patients with diarrhea
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS: Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation. This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk of adverse effects.15
CHALLENGES TO IMPLEMENTATION: Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who suffer from diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation, or those with mixed symptoms.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
Consider prescribing ondansetron up to 24 mg/d for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
Strength of recommendation
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).
Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
Illustrative case
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation. She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn’s disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits (constipation [IBS-C], diarrhea [IBS-D], or alternating periods of both—mixed [IBS-M]).2 It is diagnosed based on Rome III criteria—recurrent abdominal pain or discomfort at least 3 days/month in the last 3 months associated with ≥2 of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments, which include fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors, are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns of ischemic colitis and severe constipation.12 It was reintroduced in 2002, but can be prescribed only by physicians who enroll in a prescribing program provided by the manufacturer, and the drug has restrictions on its use.
Ondansetron—a different 5HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted a RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
STUDY SUMMARY: Ondansetron improves stool consistency, severity of IBS symptoms
In a 5-week, double-blind crossover RCT, Garsed et al1 compared ondansetron vs placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria were pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or being in another trial. Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last 2 weeks of the study. There was a 2- to 3-week washout between treatment periods.
The primary endpoint was average stool consistency in the last 2 weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (Type 1) to watery (Type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was -0.9 (95% confidence interval [CI], -1.1 to -0.6; P<.001), indicating slightly more formed stool with use of ondansetron. The IBS Severity Scoring System score (maximum score 500 points, with mild, moderate, and severe cases indicated by scores of 75-175, 175-300, and >300, respectively) was reduced by more points with ondansetron than placebo (83 ± 9.8 vs 37 ± 9.7; P=.001). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation (P=.002) and lower urgency scores (P<.001). Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group (95% CI, 6-14 hours; P<.001). Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as 7 days but returned after stopping ondansetron, typically within 2 weeks. Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW: Another option for IBS patients with diarrhea
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS: Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation. This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk of adverse effects.15
CHALLENGES TO IMPLEMENTATION: Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who suffer from diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation, or those with mixed symptoms.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Consider prescribing ondansetron up to 24 mg/d for patients who have irritable bowel syndrome with diarrhea (IBS-D).1
Strength of recommendation
B: Based on a well-done double-blind, placebo-controlled randomized controlled trial (RCT).
Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
Illustrative case
A 23-year-old woman who was diagnosed with irritable bowel syndrome (IBS) comes to your clinic with complaints of increased frequency of defecation with watery stools and generalized, cramping abdominal pain. She also notes increased passage of mucus and a sensation of incomplete evacuation. She says the only thing that relieves her pain is defecation. She has tried loperamide, acetaminophen, and ibuprofen without relief. She does not have Crohn’s disease or ulcerative colitis. What else can you offer her that is safe and effective?
IBS is a chronic, episodic functional gastrointestinal disorder characterized by abdominal pain or discomfort and altered bowel habits (constipation [IBS-C], diarrhea [IBS-D], or alternating periods of both—mixed [IBS-M]).2 It is diagnosed based on Rome III criteria—recurrent abdominal pain or discomfort at least 3 days/month in the last 3 months associated with ≥2 of the following: improvement with defecation, onset associated with a change in frequency of stool, and onset associated with a change in form (appearance) of stool.3 IBS often is unrecognized or untreated, and as few as 25% of patients with IBS seek care.4
IBS-D affects approximately 5% of the general population in North America.5,6 IBS-D is associated with a considerably decreased quality of life and is a common cause of work absenteeism.7,8 Because many conditions can cause diarrhea, patients typically undergo numerous tests before receiving an accurate diagnosis, which creates a financial burden.9
For many patients, current IBS treatments, which include fiber supplements, laxatives, antidiarrheal medications, antispasmodics, and antidepressants such as tricyclics and selective serotonin reuptake inhibitors, are unsatisfactory.10 Alosetron, a 5-hydroxytryptamine 3 (5HT3) receptor antagonist, has been used to treat IBS-D,11 but this medication was voluntarily withdrawn from the US market in 2000 due to concerns of ischemic colitis and severe constipation.12 It was reintroduced in 2002, but can be prescribed only by physicians who enroll in a prescribing program provided by the manufacturer, and the drug has restrictions on its use.
Ondansetron—a different 5HT3 receptor antagonist used to treat nausea and vomiting caused by chemotherapy—may be another option for treating IBS-D. Garsed et al1 recently conducted a RCT to evaluate the efficacy of ondansetron for patients with IBS-D.
STUDY SUMMARY: Ondansetron improves stool consistency, severity of IBS symptoms
In a 5-week, double-blind crossover RCT, Garsed et al1 compared ondansetron vs placebo for symptom relief in 120 patients who met Rome III criteria for IBS-D. All patients were ages 18 to 75 and had no evidence of inflammatory bowel disease. Exclusion criteria were pregnancy or breastfeeding, unwillingness to stop antidiarrheal medication, prior abdominal surgery other than appendectomy or cholecystectomy, or being in another trial. Patients were started on ondansetron 4 mg/d with dose titration up to 24 mg/d based on response; no dose adjustments were allowed during the last 2 weeks of the study. There was a 2- to 3-week washout between treatment periods.
The primary endpoint was average stool consistency in the last 2 weeks of treatment, as measured by the Bristol Stool Form (BSF) scale.13 The BSF is a visual scale that depicts stool as hard (Type 1) to watery (Type 7); types 3 and 4 describe normal stools. The study also looked at urgency and frequency of defecation, bowel transit time, and pain scores.
Treatment with ondansetron resulted in a small but statistically significant improvement in stool consistency. The mean difference in BSF score between ondansetron and placebo was -0.9 (95% confidence interval [CI], -1.1 to -0.6; P<.001), indicating slightly more formed stool with use of ondansetron. The IBS Severity Scoring System score (maximum score 500 points, with mild, moderate, and severe cases indicated by scores of 75-175, 175-300, and >300, respectively) was reduced by more points with ondansetron than placebo (83 ± 9.8 vs 37 ± 9.7; P=.001). Although this mean difference of 46 points fell just short of the 50-point threshold that is considered clinically significant, many patients exceeded this threshold.
Compared to those who received placebo, patients who took ondansetron also had less frequent defecation (P=.002) and lower urgency scores (P<.001). Gut transit time was lengthened in the ondansetron group by 10 hours more than in the placebo group (95% CI, 6-14 hours; P<.001). Pain scores did not change significantly for patients taking ondansetron, although they experienced significantly fewer days of urgency and bloating. Symptoms typically improved in as little as 7 days but returned after stopping ondansetron, typically within 2 weeks. Sixty-five percent of patients reported adequate relief with ondansetron, compared to 14% with placebo.
Patients whose diarrhea was more severe at baseline didn’t respond as well to ondansetron as did those whose diarrhea was less severe. The only frequent adverse effect was constipation, which occurred in 9% of patients receiving ondansetron and 2% of those on placebo.
WHAT’S NEW: Another option for IBS patients with diarrhea
A prior, smaller study of ondansetron that used a lower dosage (12 mg/d) suggested benefit in IBS-D.14 In that study, ondansetron decreased diarrhea and functional dyspepsia. The study by Garsed et al1 is the first large RCT to show significantly improved stool consistency, less frequent defecation, and less urgency and bloating from using ondansetron to treat IBS-D.
CAVEATS: Ondansetron doesn’t appear to reduce pain
In Garsed et al,1 patients who received ondansetron did not experience relief from pain, which is one of the main complaints of IBS. However, this study did find slight improvement in formed stools, symptom relief that approached—but did not quite reach—clinical significance, fewer days with urgency and bloating, and less frequent defecation. This study did not evaluate the long-term effects of ondansetron use. However, ondansetron has been used for other indications for more than 25 years and has been reported to have a low risk of adverse effects.15
CHALLENGES TO IMPLEMENTATION: Remember ondansetron is not for IBS patients with constipation
Proper use of this drug among patients with IBS is key. The primary benefits of ondansetron are limited to IBS patients who suffer from diarrhea, and not constipation. Ondansetron should not be prescribed to IBS patients who experience constipation, or those with mixed symptoms.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
1. Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63:1617-1625.
2. Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77-81.
3. Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237-241.
4. Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Qual Life Res. 2000;9:161-176.
5. Saito YA, Locke GR, Talley NJ, et al. A comparison of the Rome and Manning criteria for case identification in epidemiological investigations of irritable bowel syndrome. Am J Gastroenterol. 2000;95:2816-2824.
6. Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82.
7. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896-904.
8. Schuster MM. Diagnostic evaluation of the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:269-278.
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511.
10. Talley NJ. Pharmacologic therapy for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:750-758.
11. Andresen V, Montori VM, Keller J, et al. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545-555.
12. Chang L, Chey WD, Harris L, et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am J Gastroenterol. 2006;101:1069-1079.
13. Heaton KW, O’Donnell LJ. An office guide to whole-gut transit time. Patients’ recollection of their stool form. J Clin Gastroenterol. 1994;19:28-30.
14. Maxton DG, Morris J, Whorwell PJ. Selective 5‐hydroxytryptamine antagonism: a role in irritable bowel syndrome and functional dyspepsia? Aliment Pharmacol Ther. 1996;10:595-599.
15. Gill SK, Einarson A. The safety of drugs for the treatment of nausea and vomiting of pregnancy. Expert Opin Drug Saf. 2007;6:685-694.
Copyright © 2014 Family Physicians Inquiries Network. All rights reserved.
Skip the Compression Stockings Following DVT
PRACTICE CHANGER
Do not recommend elastic compression stockings to decrease the incidence of postthrombotic syndrome after deep vein thrombosis.1
STRENGTH OF RECOMMENDATION
B: Based on a large randomized controlled trial1
ILLUSTRATIVE CASE
A 56-year-old man presents to your clinic three days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin (5 mg/d) with enoxaparin bridging (120 mg/d). He has read about postthrombotic syndrome (PTS) online and is very concerned about this possible adverse effect. He asks about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by decreasing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior research suggested that use of ECS can reduce PTS incidence by half, but the studies were small, single-center, and not placebo-controlled.6,7
On the next page: Study summary >>
STUDY SUMMARY
RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active versus placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (five to 10 days of heparin and three to six months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of less than six months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30 to 40 mm Hg graduated) ECS or identical-looking placebo ECS (< 5 mm Hg compression at the ankle) for two years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from waking until bedtime.
Follow-up occurred at one, six, 12, 18, and 24 months. The primary outcome was cumulative incidence of PTS diagnosed at six months or later using the Ginsberg criteria of ipsilateral pain and swelling of at least one month’s duration.8 Secondary outcomes included severity of PTS, leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively through use of a validated scale (the Villalta scale) for PTS severity and two questionnaires to assess QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including BMI, VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age of participants in the study group was 55.4 years and in the placebo group, 54.8 years. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both groups used the stockings; at 24 months, that was reduced to a little less than 70%. The percentage of people who used the stockings for at least three days per week was similar in both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group and 12.7% in the placebo group (hazard ratio, 1.13). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on outcomes. There was a marginal benefit for ECS for women versus men, but this does not likely reflect a true difference because the confidence intervals surrounding the hazard ratios for men and women overlapped and crossed the null value.
On the next page: What's new & challenges to implementation >>
WHAT’S NEW
New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements that recommend for or against the use of ECS after DVT.
CAVEATS
High nonadherence rates might have affected results
In both groups, adherence to the assigned intervention diminished throughout the study (from 95% at one month to slightly less than 70% at two years). Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the two-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported previously. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION
There are no barriers to ending this practice
We can identify no challenges to implementation of this recommendation.
On the next page: References >>
REFERENCES
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996; 125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141: 308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:
500-509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:
759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006; 59:1049-1056.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(7):388-390.
PRACTICE CHANGER
Do not recommend elastic compression stockings to decrease the incidence of postthrombotic syndrome after deep vein thrombosis.1
STRENGTH OF RECOMMENDATION
B: Based on a large randomized controlled trial1
ILLUSTRATIVE CASE
A 56-year-old man presents to your clinic three days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin (5 mg/d) with enoxaparin bridging (120 mg/d). He has read about postthrombotic syndrome (PTS) online and is very concerned about this possible adverse effect. He asks about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by decreasing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior research suggested that use of ECS can reduce PTS incidence by half, but the studies were small, single-center, and not placebo-controlled.6,7
On the next page: Study summary >>
STUDY SUMMARY
RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active versus placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (five to 10 days of heparin and three to six months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of less than six months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30 to 40 mm Hg graduated) ECS or identical-looking placebo ECS (< 5 mm Hg compression at the ankle) for two years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from waking until bedtime.
Follow-up occurred at one, six, 12, 18, and 24 months. The primary outcome was cumulative incidence of PTS diagnosed at six months or later using the Ginsberg criteria of ipsilateral pain and swelling of at least one month’s duration.8 Secondary outcomes included severity of PTS, leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively through use of a validated scale (the Villalta scale) for PTS severity and two questionnaires to assess QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including BMI, VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age of participants in the study group was 55.4 years and in the placebo group, 54.8 years. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both groups used the stockings; at 24 months, that was reduced to a little less than 70%. The percentage of people who used the stockings for at least three days per week was similar in both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group and 12.7% in the placebo group (hazard ratio, 1.13). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on outcomes. There was a marginal benefit for ECS for women versus men, but this does not likely reflect a true difference because the confidence intervals surrounding the hazard ratios for men and women overlapped and crossed the null value.
On the next page: What's new & challenges to implementation >>
WHAT’S NEW
New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements that recommend for or against the use of ECS after DVT.
CAVEATS
High nonadherence rates might have affected results
In both groups, adherence to the assigned intervention diminished throughout the study (from 95% at one month to slightly less than 70% at two years). Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the two-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported previously. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION
There are no barriers to ending this practice
We can identify no challenges to implementation of this recommendation.
On the next page: References >>
REFERENCES
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996; 125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141: 308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:
500-509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:
759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006; 59:1049-1056.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(7):388-390.
PRACTICE CHANGER
Do not recommend elastic compression stockings to decrease the incidence of postthrombotic syndrome after deep vein thrombosis.1
STRENGTH OF RECOMMENDATION
B: Based on a large randomized controlled trial1
ILLUSTRATIVE CASE
A 56-year-old man presents to your clinic three days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin (5 mg/d) with enoxaparin bridging (120 mg/d). He has read about postthrombotic syndrome (PTS) online and is very concerned about this possible adverse effect. He asks about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by decreasing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior research suggested that use of ECS can reduce PTS incidence by half, but the studies were small, single-center, and not placebo-controlled.6,7
On the next page: Study summary >>
STUDY SUMMARY
RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active versus placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (five to 10 days of heparin and three to six months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of less than six months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30 to 40 mm Hg graduated) ECS or identical-looking placebo ECS (< 5 mm Hg compression at the ankle) for two years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from waking until bedtime.
Follow-up occurred at one, six, 12, 18, and 24 months. The primary outcome was cumulative incidence of PTS diagnosed at six months or later using the Ginsberg criteria of ipsilateral pain and swelling of at least one month’s duration.8 Secondary outcomes included severity of PTS, leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively through use of a validated scale (the Villalta scale) for PTS severity and two questionnaires to assess QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including BMI, VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age of participants in the study group was 55.4 years and in the placebo group, 54.8 years. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both groups used the stockings; at 24 months, that was reduced to a little less than 70%. The percentage of people who used the stockings for at least three days per week was similar in both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group and 12.7% in the placebo group (hazard ratio, 1.13). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on outcomes. There was a marginal benefit for ECS for women versus men, but this does not likely reflect a true difference because the confidence intervals surrounding the hazard ratios for men and women overlapped and crossed the null value.
On the next page: What's new & challenges to implementation >>
WHAT’S NEW
New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements that recommend for or against the use of ECS after DVT.
CAVEATS
High nonadherence rates might have affected results
In both groups, adherence to the assigned intervention diminished throughout the study (from 95% at one month to slightly less than 70% at two years). Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the two-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported previously. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION
There are no barriers to ending this practice
We can identify no challenges to implementation of this recommendation.
On the next page: References >>
REFERENCES
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996; 125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141: 308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:
500-509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:
759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006; 59:1049-1056.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(7):388-390.
Skip the compression stockings following DVT
Do not recommend elastic compression stockings (ECS) to decrease the incidence of post-thrombotic syndrome (PTS) after deep vein thrombosis (DVT).1
Strength of recommendation
B: Based on a large, randomized controlled trial
Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
Illustrative case
A 56-year-old man comes to your clinic 3 days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin, 5 mg/d, with enoxaparin bridging, 120 mg/d. He has read about post-thrombotic syndrome (PTS) online and is very concerned about this possible side effect. He is asking about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by reducing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior studies suggested that using ECS can cut the incidence of PTS in half.6,7 However, these were small, single-center studies, and they were not placebo-controlled.6,7
STUDY SUMMARY: RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active vs placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (5-10 days of heparin and 3-6 months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of <6 months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30-40 mm Hg graduated) ECS or identical-looking placebo ECS with <5 mm Hg compression at the ankle for 2 years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from when they woke until they went to bed.
Participants were followed at one, 6, 12, 18, and 24 months. The primary outcome was the cumulative incidence of PTS diagnosed at 6 months or later using Ginsberg’s criteria of ipsilateral pain and swelling of at least 1 month’s duration.8 Secondary outcomes included severity of PTS, presence of leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively using a validated scale (the Villalta scale) for PTS severity and the 36-item Short Form Health Survey (SF-36) and the Venous Insufficiency Epidemiological and Economic Study Quality of Life (VEINES-QOL) questionnaire to measure QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including body mass index (BMI), VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age was 55.4 years in the study group (standard deviation [SD] ± 15.3 years) and 54.8 years (SD ± 15.8 years) in the place- bo group. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both the active and placebo groups used the stockings; at 24 months, a little less than 70% of the participants in both groups continued to use the stockings. The percentage of people who used the stockings for at least 3 days a week was similar across both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group vs 12.7% in the placebo group, with a hazard ratio of 1.13 (95% confidence interval [CI], .73-1.76; P=.58). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on the outcomes. There was a marginal benefit for ECS for women (P=.047) over men, but this does not likely reflect a true difference because the CIs surrounding the hazard ratios for men and women overlapped and crossed the null value.
WHAT'S NEW: New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements for or against the use of ECS after DVT.
CAVEATS: High nonadherence rates might have affected the results
In both groups, adherence to the assigned intervention diminished throughout the study. Overall, approximately 95% of patients reported wearing their stockings at one month; this dropped to just under 70% by 2 years. Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the 2-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported in previous studies. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION: There are no barriers to ending this practice
We see no challenges to implementation of this recommendation.
Acknowledgement
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141:308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:500- 509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006;59:1049-1056.
Do not recommend elastic compression stockings (ECS) to decrease the incidence of post-thrombotic syndrome (PTS) after deep vein thrombosis (DVT).1
Strength of recommendation
B: Based on a large, randomized controlled trial
Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
Illustrative case
A 56-year-old man comes to your clinic 3 days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin, 5 mg/d, with enoxaparin bridging, 120 mg/d. He has read about post-thrombotic syndrome (PTS) online and is very concerned about this possible side effect. He is asking about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by reducing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior studies suggested that using ECS can cut the incidence of PTS in half.6,7 However, these were small, single-center studies, and they were not placebo-controlled.6,7
STUDY SUMMARY: RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active vs placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (5-10 days of heparin and 3-6 months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of <6 months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30-40 mm Hg graduated) ECS or identical-looking placebo ECS with <5 mm Hg compression at the ankle for 2 years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from when they woke until they went to bed.
Participants were followed at one, 6, 12, 18, and 24 months. The primary outcome was the cumulative incidence of PTS diagnosed at 6 months or later using Ginsberg’s criteria of ipsilateral pain and swelling of at least 1 month’s duration.8 Secondary outcomes included severity of PTS, presence of leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively using a validated scale (the Villalta scale) for PTS severity and the 36-item Short Form Health Survey (SF-36) and the Venous Insufficiency Epidemiological and Economic Study Quality of Life (VEINES-QOL) questionnaire to measure QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including body mass index (BMI), VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age was 55.4 years in the study group (standard deviation [SD] ± 15.3 years) and 54.8 years (SD ± 15.8 years) in the place- bo group. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both the active and placebo groups used the stockings; at 24 months, a little less than 70% of the participants in both groups continued to use the stockings. The percentage of people who used the stockings for at least 3 days a week was similar across both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group vs 12.7% in the placebo group, with a hazard ratio of 1.13 (95% confidence interval [CI], .73-1.76; P=.58). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on the outcomes. There was a marginal benefit for ECS for women (P=.047) over men, but this does not likely reflect a true difference because the CIs surrounding the hazard ratios for men and women overlapped and crossed the null value.
WHAT'S NEW: New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements for or against the use of ECS after DVT.
CAVEATS: High nonadherence rates might have affected the results
In both groups, adherence to the assigned intervention diminished throughout the study. Overall, approximately 95% of patients reported wearing their stockings at one month; this dropped to just under 70% by 2 years. Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the 2-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported in previous studies. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION: There are no barriers to ending this practice
We see no challenges to implementation of this recommendation.
Acknowledgement
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Do not recommend elastic compression stockings (ECS) to decrease the incidence of post-thrombotic syndrome (PTS) after deep vein thrombosis (DVT).1
Strength of recommendation
B: Based on a large, randomized controlled trial
Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
Illustrative case
A 56-year-old man comes to your clinic 3 days after receiving a diagnosis of lower extremity deep vein thrombosis (DVT). He was prescribed warfarin, 5 mg/d, with enoxaparin bridging, 120 mg/d. He has read about post-thrombotic syndrome (PTS) online and is very concerned about this possible side effect. He is asking about using elastic compression stockings (ECS). What should you tell him?
PTS can be a frustrating, debilitating condition. Its clinical features range from minor limb swelling to severe edema and pain, irreversible skin changes, and leg ulcerations.2 It occurs in 25% to 50% of patients after DVT.3 Because current PTS treatments are not very effective, prevention is essential.4,5
Patients are frequently encouraged to wear ECS after DVT to reduce the incidence of PTS by reducing venous hypertension and reflux. These stockings are expensive and uncomfortable. Prior studies suggested that using ECS can cut the incidence of PTS in half.6,7 However, these were small, single-center studies, and they were not placebo-controlled.6,7
STUDY SUMMARY: RCT sets aside a common practice
Kahn et al1 conducted a randomized, placebo-controlled trial of active vs placebo ECS in patients from 24 centers in the United States and Canada who’d had an ultrasound-confirmed proximal DVT (in the popliteal or more proximal deep leg vein) within the previous 14 days. Most patients received standard anticoagulation therapy to treat their DVT (5-10 days of heparin and 3-6 months of warfarin). Patients were excluded if they had received thrombolytics, had arterial claudication, had a life expectancy of <6 months, were unable to put on ECS due to physical disabilities or allergy, or were unable to participate in follow-up visits.
Patients were randomly assigned to wear active (30-40 mm Hg graduated) ECS or identical-looking placebo ECS with <5 mm Hg compression at the ankle for 2 years. Providers, study personnel and statisticians, and patients were all blinded to treatment allocation. Patients were asked to wear the stocking on the affected leg each day from when they woke until they went to bed.
Participants were followed at one, 6, 12, 18, and 24 months. The primary outcome was the cumulative incidence of PTS diagnosed at 6 months or later using Ginsberg’s criteria of ipsilateral pain and swelling of at least 1 month’s duration.8 Secondary outcomes included severity of PTS, presence of leg ulcers, recurrence of venous thromboembolism (VTE), death, adverse events, venous valvular reflux, and quality of life (QOL). Outcomes were measured objectively using a validated scale (the Villalta scale) for PTS severity and the 36-item Short Form Health Survey (SF-36) and the Venous Insufficiency Epidemiological and Economic Study Quality of Life (VEINES-QOL) questionnaire to measure QOL.9-11
There were 409 patients in the ECS group and 394 in the placebo group. Baseline characteristics, including body mass index (BMI), VTE risk factors, and anticoagulation treatment regimens, were similar between groups. The average age was 55.4 years in the study group (standard deviation [SD] ± 15.3 years) and 54.8 years (SD ± 15.8 years) in the place- bo group. Men comprised 62.4% of the active group and 57.9% of the placebo group. Approximately 90% of the participants in both groups were white.
At one month, approximately 95% of participants in both the active and placebo groups used the stockings; at 24 months, a little less than 70% of the participants in both groups continued to use the stockings. The percentage of people who used the stockings for at least 3 days a week was similar across both groups.
The cumulative incidence of PTS during follow-up was 14.2% in the active group vs 12.7% in the placebo group, with a hazard ratio of 1.13 (95% confidence interval [CI], .73-1.76; P=.58). There were no differences in any of the secondary outcomes. Prespecified subgroup analyses found that age, BMI, and severity of DVT had no effect on the outcomes. There was a marginal benefit for ECS for women (P=.047) over men, but this does not likely reflect a true difference because the CIs surrounding the hazard ratios for men and women overlapped and crossed the null value.
WHAT'S NEW: New evidence contradicts previous studies
Two prior studies showed that using 30 to 40 mm Hg ECS decreased the incidence of PTS after proximal DVT.6,7 However, these were smaller, open-label, single-center studies. This study by Kahn et al1 was the first placebo-controlled, randomized, multicenter study that used validated instruments to measure PTS and QOL. It found no benefit in using ECS, thus contradicting the results of the prior studies.
There are currently no guidelines or consensus statements for or against the use of ECS after DVT.
CAVEATS: High nonadherence rates might have affected the results
In both groups, adherence to the assigned intervention diminished throughout the study. Overall, approximately 95% of patients reported wearing their stockings at one month; this dropped to just under 70% by 2 years. Theoretically, this could have affected efficacy outcomes. However, the decrease was similar in both groups and represents what is observed in clinical practice. A prespecified per protocol analysis of patients who wore their ECS more regularly found no benefit.
It is possible that a “placebo effect” could explain the lack of difference between groups. However, the placebo stockings provided virtually no compression, and the 2-year cumulative incidence of PTS in both the treatment and placebo groups was similar to that seen in control groups in prior studies.6,7
Finally, the incidence of PTS in this study was much lower than the 25% to 50% incidence reported in previous studies. Kahn et al1 suggested that this was because they used more stringent and standardized criteria for PTS than was used in previous research.
CHALLENGES TO IMPLEMENTATION: There are no barriers to ending this practice
We see no challenges to implementation of this recommendation.
Acknowledgement
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141:308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:500- 509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006;59:1049-1056.
1. Kahn SR, Shapiro S, Wells PS, et al; SOX trial investigators. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet. 2014;383:880-888.
2. Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698-707.
3. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
4. Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest. 2012;141:308-320.
5. Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:500- 509.
6. Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
7. Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
8. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
9. Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994;24:158a.
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-263.
11. Kahn SR, Lamping DL, Ducruet T, et al; VETO Study Investigators. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006;59:1049-1056.
Copyright © 2014 Family Physicians Inquiries Network. All rights reserved.
Should You Consider Antibiotics for Exacerbations of Mild COPD?
PRACTICE CHANGER
Consider antibiotics for patients with exacerbations of mild to moderate chronic obstructive pulmonary disease (COPD).1
STRENGTH OF RECOMMENDATION
B: Based on a single well-done multicenter randomized controlled trial (RCT) with quality evidence.1
ILLUSTRATIVE CASE
A 45-year-old man with a history of mild COPD seeks treatment for worsening dyspnea and increased (nonpurulent) sputum production. He denies fever or chills. On exam, he has coarse breath sounds and scattered wheezes. Should you add antibiotics to his treatment?
COPD exacerbations—a worsening of symptoms beyond day-to-day variations that leads to a medication change—are part of the disease course and can accelerate lung function decline, decrease quality of life, and, when severe, increase mortality.2 Infections cause an estimated 50% to 70% of COPD exacerbations.2-4
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend using antibiotics to treat exacerbations in patients with moderate or severe COPD who
• Have increased dyspnea, sputum volume, and sputum purulence;
• Have two of these symptoms if increased sputum purulence is one of them; or
• Require mechanical ventilation.2
According to the GOLD guidelines, the choice of antibiotic should be based on local antibiograms; common options include amoxicillin, amoxicillin/clavulanate, azithromycin, and doxycycline.2 Although the GOLD guidelines cover use of antibiotics for COPD exacerbations, this recommendation is based on analyses of studies that focused on patients with moderate or severe COPD.2 There has been little research on using antibiotics for exacerbations of mild COPD.
STUDY SUMMARY
Using antibiotics often resolves symptoms
Llor et al1 conducted a multicenter, double-blind, placebo-controlled RCT to examine the effectiveness of antibiotic treatment for COPD exacerbations. Participants (ages 40 and older) had mild to moderate COPD, defined as 10 or more pack-years of smoking, an FEV1 greater than 50%, and an FEV1/FVC ratio lower than 0.7. An exacerbation was defined as at least one of the following: increased dyspnea, increased sputum volume, or sputum purulence.
Patients were randomly assigned to receive amoxicillin/clavulanate 500/125 mg or placebo three times a day for eight days. Primary endpoints were clinical cure (resolution of symptoms) and clinical success (resolution or improvement of symptoms) at days 9 to 11, as determined by physician assessment. Secondary measures included cure and clinical success at day 20 and time until next exacerbation. Patients were monitored for one year after the exacerbation.
There were 162 patients in the antibiotic group and 156 in the placebo group; the two groups were demographically similar. In each group, four patients withdrew consent and were removed from analysis. By the 9-to-11-day follow-up visit, 74.1% of patients in the antibiotic group had clinical cure, compared with 59.9% in the placebo group (number needed to treat [NNT] = 7). Clinical success also was significantly greater with antibiotics compared with placebo (90.5% vs 80.9%).
The clinical cure rate at day 20 also was significantly greater in patients on antibiotics compared with placebo (81.6% vs 67.8%; NNT = 7). During the one-year follow-up, 58% of patients in the antibiotic group and 73.2% of those in the placebo group experienced additional exacerbations. Time to next exacerbation was significantly longer in patients taking antibiotics (233 days vs 160 days).
Can CRP level help determine who should receive antibiotics?
Previous studies have identified biomarkers, including C-reactive protein (CRP), that indicate COPD exacerbation but have not linked them to clinical course.5-7 In this study, researchers measured CRP in patients receiving placebo to determine if this biomarker could predict clinical outcomes.
The researchers found that the clinical success rate among patients with a CRP lower than 40 mg/L was 87.6%, while only 34.5% of patients with a CRP greater than 40 mg/L experienced clinical success (sensitivity and specificity for clinical success at this cutoff were 0.655 and 0.876, respectively). This suggests that antibiotics might be appropriate for patients with an exacerbation of mild or moderate COPD who have a CRP greater than 40 mg/L.
There were 35 adverse events: 23 in the antibiotics group and 12 in the placebo group. Two patients in the antibiotics group discontinued treatment as a result. Most adverse events involved mild gastrointestinal problems.
Continued on next page >>
WHAT’S NEW?
Evidence supports antibiotics for mild to moderate COPD
Few placebo-controlled trials have addressed antibiotic use for exacerbations in patients with mild to moderate COPD.2,8,9 This study demonstrated that, compared with placebo, symptom resolution and clinical success is greater with amoxicillin/clavulanate and that antibiotic treatment also may increase time until next exacerbation.
The study also looked at the relationship of CRP and exacerbations in the placebo group. Higher spontaneous clinical cure rates were noted when the CRP was lower than 40 mg/L.
CAVEATS
Effects of concomitant medications are unclear
In both the placebo and antibiotic groups, patients were taking other medications (including short- and long-acting β-agonists, anticholinergics, theophyllines, and oral or inhaled corticosteroids). Roughly the same number of patients in each group took additional medications, but researchers did not conduct a subgroup analysis to see if patients treated with these medications responded differently from those who received antibiotics alone.
GOLD guidelines already suggest antibiotics for exacerbations in patients with moderate COPD.2 In this study, 89% of patients met criteria for moderate COPD and 11% for mild COPD. Though the percentage of patients who had mild COPD was small, we believe the results of this study warrant consideration of antibiotic use in patients with mild disease. Local antibiograms may show increased resistance to amoxicillin/clavulanate; this study did not address the use of other antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotic overuse may be a concern
Concerns about antibiotic resistance may make clinicians reluctant to prescribe the drugs for those with mild to moderate COPD.
REFERENCES
1. Llor C, Moragas A, Hernández S, et al. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(8):716-723.
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. January 2014. www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Accessed April 15, 2014.
3. Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847-852.
4. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925-931.
5. Vollenweider DJ, Jarrett H, Steurer-Stey CA, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;12:CD010257.
6. Bartlett, JG, Sethi S. Management of infection in acute exacerbations of chronic obstructive pulmonary disease. In: Basow DS, ed. UpToDate. www.uptodate.com. Last updated March 27, 2012. Accessed January 2, 2013.
7. Lacoma A, Prat C, Andreo F, et al. Value of procalcitonin, C-reactive protein, and neopterin in exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:157-169.
8. Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med. 2009;15(2):120-125.
9. Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353-2361.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(4):E11-E13.
PRACTICE CHANGER
Consider antibiotics for patients with exacerbations of mild to moderate chronic obstructive pulmonary disease (COPD).1
STRENGTH OF RECOMMENDATION
B: Based on a single well-done multicenter randomized controlled trial (RCT) with quality evidence.1
ILLUSTRATIVE CASE
A 45-year-old man with a history of mild COPD seeks treatment for worsening dyspnea and increased (nonpurulent) sputum production. He denies fever or chills. On exam, he has coarse breath sounds and scattered wheezes. Should you add antibiotics to his treatment?
COPD exacerbations—a worsening of symptoms beyond day-to-day variations that leads to a medication change—are part of the disease course and can accelerate lung function decline, decrease quality of life, and, when severe, increase mortality.2 Infections cause an estimated 50% to 70% of COPD exacerbations.2-4
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend using antibiotics to treat exacerbations in patients with moderate or severe COPD who
• Have increased dyspnea, sputum volume, and sputum purulence;
• Have two of these symptoms if increased sputum purulence is one of them; or
• Require mechanical ventilation.2
According to the GOLD guidelines, the choice of antibiotic should be based on local antibiograms; common options include amoxicillin, amoxicillin/clavulanate, azithromycin, and doxycycline.2 Although the GOLD guidelines cover use of antibiotics for COPD exacerbations, this recommendation is based on analyses of studies that focused on patients with moderate or severe COPD.2 There has been little research on using antibiotics for exacerbations of mild COPD.
STUDY SUMMARY
Using antibiotics often resolves symptoms
Llor et al1 conducted a multicenter, double-blind, placebo-controlled RCT to examine the effectiveness of antibiotic treatment for COPD exacerbations. Participants (ages 40 and older) had mild to moderate COPD, defined as 10 or more pack-years of smoking, an FEV1 greater than 50%, and an FEV1/FVC ratio lower than 0.7. An exacerbation was defined as at least one of the following: increased dyspnea, increased sputum volume, or sputum purulence.
Patients were randomly assigned to receive amoxicillin/clavulanate 500/125 mg or placebo three times a day for eight days. Primary endpoints were clinical cure (resolution of symptoms) and clinical success (resolution or improvement of symptoms) at days 9 to 11, as determined by physician assessment. Secondary measures included cure and clinical success at day 20 and time until next exacerbation. Patients were monitored for one year after the exacerbation.
There were 162 patients in the antibiotic group and 156 in the placebo group; the two groups were demographically similar. In each group, four patients withdrew consent and were removed from analysis. By the 9-to-11-day follow-up visit, 74.1% of patients in the antibiotic group had clinical cure, compared with 59.9% in the placebo group (number needed to treat [NNT] = 7). Clinical success also was significantly greater with antibiotics compared with placebo (90.5% vs 80.9%).
The clinical cure rate at day 20 also was significantly greater in patients on antibiotics compared with placebo (81.6% vs 67.8%; NNT = 7). During the one-year follow-up, 58% of patients in the antibiotic group and 73.2% of those in the placebo group experienced additional exacerbations. Time to next exacerbation was significantly longer in patients taking antibiotics (233 days vs 160 days).
Can CRP level help determine who should receive antibiotics?
Previous studies have identified biomarkers, including C-reactive protein (CRP), that indicate COPD exacerbation but have not linked them to clinical course.5-7 In this study, researchers measured CRP in patients receiving placebo to determine if this biomarker could predict clinical outcomes.
The researchers found that the clinical success rate among patients with a CRP lower than 40 mg/L was 87.6%, while only 34.5% of patients with a CRP greater than 40 mg/L experienced clinical success (sensitivity and specificity for clinical success at this cutoff were 0.655 and 0.876, respectively). This suggests that antibiotics might be appropriate for patients with an exacerbation of mild or moderate COPD who have a CRP greater than 40 mg/L.
There were 35 adverse events: 23 in the antibiotics group and 12 in the placebo group. Two patients in the antibiotics group discontinued treatment as a result. Most adverse events involved mild gastrointestinal problems.
Continued on next page >>
WHAT’S NEW?
Evidence supports antibiotics for mild to moderate COPD
Few placebo-controlled trials have addressed antibiotic use for exacerbations in patients with mild to moderate COPD.2,8,9 This study demonstrated that, compared with placebo, symptom resolution and clinical success is greater with amoxicillin/clavulanate and that antibiotic treatment also may increase time until next exacerbation.
The study also looked at the relationship of CRP and exacerbations in the placebo group. Higher spontaneous clinical cure rates were noted when the CRP was lower than 40 mg/L.
CAVEATS
Effects of concomitant medications are unclear
In both the placebo and antibiotic groups, patients were taking other medications (including short- and long-acting β-agonists, anticholinergics, theophyllines, and oral or inhaled corticosteroids). Roughly the same number of patients in each group took additional medications, but researchers did not conduct a subgroup analysis to see if patients treated with these medications responded differently from those who received antibiotics alone.
GOLD guidelines already suggest antibiotics for exacerbations in patients with moderate COPD.2 In this study, 89% of patients met criteria for moderate COPD and 11% for mild COPD. Though the percentage of patients who had mild COPD was small, we believe the results of this study warrant consideration of antibiotic use in patients with mild disease. Local antibiograms may show increased resistance to amoxicillin/clavulanate; this study did not address the use of other antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotic overuse may be a concern
Concerns about antibiotic resistance may make clinicians reluctant to prescribe the drugs for those with mild to moderate COPD.
REFERENCES
1. Llor C, Moragas A, Hernández S, et al. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(8):716-723.
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. January 2014. www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Accessed April 15, 2014.
3. Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847-852.
4. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925-931.
5. Vollenweider DJ, Jarrett H, Steurer-Stey CA, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;12:CD010257.
6. Bartlett, JG, Sethi S. Management of infection in acute exacerbations of chronic obstructive pulmonary disease. In: Basow DS, ed. UpToDate. www.uptodate.com. Last updated March 27, 2012. Accessed January 2, 2013.
7. Lacoma A, Prat C, Andreo F, et al. Value of procalcitonin, C-reactive protein, and neopterin in exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:157-169.
8. Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med. 2009;15(2):120-125.
9. Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353-2361.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(4):E11-E13.
PRACTICE CHANGER
Consider antibiotics for patients with exacerbations of mild to moderate chronic obstructive pulmonary disease (COPD).1
STRENGTH OF RECOMMENDATION
B: Based on a single well-done multicenter randomized controlled trial (RCT) with quality evidence.1
ILLUSTRATIVE CASE
A 45-year-old man with a history of mild COPD seeks treatment for worsening dyspnea and increased (nonpurulent) sputum production. He denies fever or chills. On exam, he has coarse breath sounds and scattered wheezes. Should you add antibiotics to his treatment?
COPD exacerbations—a worsening of symptoms beyond day-to-day variations that leads to a medication change—are part of the disease course and can accelerate lung function decline, decrease quality of life, and, when severe, increase mortality.2 Infections cause an estimated 50% to 70% of COPD exacerbations.2-4
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend using antibiotics to treat exacerbations in patients with moderate or severe COPD who
• Have increased dyspnea, sputum volume, and sputum purulence;
• Have two of these symptoms if increased sputum purulence is one of them; or
• Require mechanical ventilation.2
According to the GOLD guidelines, the choice of antibiotic should be based on local antibiograms; common options include amoxicillin, amoxicillin/clavulanate, azithromycin, and doxycycline.2 Although the GOLD guidelines cover use of antibiotics for COPD exacerbations, this recommendation is based on analyses of studies that focused on patients with moderate or severe COPD.2 There has been little research on using antibiotics for exacerbations of mild COPD.
STUDY SUMMARY
Using antibiotics often resolves symptoms
Llor et al1 conducted a multicenter, double-blind, placebo-controlled RCT to examine the effectiveness of antibiotic treatment for COPD exacerbations. Participants (ages 40 and older) had mild to moderate COPD, defined as 10 or more pack-years of smoking, an FEV1 greater than 50%, and an FEV1/FVC ratio lower than 0.7. An exacerbation was defined as at least one of the following: increased dyspnea, increased sputum volume, or sputum purulence.
Patients were randomly assigned to receive amoxicillin/clavulanate 500/125 mg or placebo three times a day for eight days. Primary endpoints were clinical cure (resolution of symptoms) and clinical success (resolution or improvement of symptoms) at days 9 to 11, as determined by physician assessment. Secondary measures included cure and clinical success at day 20 and time until next exacerbation. Patients were monitored for one year after the exacerbation.
There were 162 patients in the antibiotic group and 156 in the placebo group; the two groups were demographically similar. In each group, four patients withdrew consent and were removed from analysis. By the 9-to-11-day follow-up visit, 74.1% of patients in the antibiotic group had clinical cure, compared with 59.9% in the placebo group (number needed to treat [NNT] = 7). Clinical success also was significantly greater with antibiotics compared with placebo (90.5% vs 80.9%).
The clinical cure rate at day 20 also was significantly greater in patients on antibiotics compared with placebo (81.6% vs 67.8%; NNT = 7). During the one-year follow-up, 58% of patients in the antibiotic group and 73.2% of those in the placebo group experienced additional exacerbations. Time to next exacerbation was significantly longer in patients taking antibiotics (233 days vs 160 days).
Can CRP level help determine who should receive antibiotics?
Previous studies have identified biomarkers, including C-reactive protein (CRP), that indicate COPD exacerbation but have not linked them to clinical course.5-7 In this study, researchers measured CRP in patients receiving placebo to determine if this biomarker could predict clinical outcomes.
The researchers found that the clinical success rate among patients with a CRP lower than 40 mg/L was 87.6%, while only 34.5% of patients with a CRP greater than 40 mg/L experienced clinical success (sensitivity and specificity for clinical success at this cutoff were 0.655 and 0.876, respectively). This suggests that antibiotics might be appropriate for patients with an exacerbation of mild or moderate COPD who have a CRP greater than 40 mg/L.
There were 35 adverse events: 23 in the antibiotics group and 12 in the placebo group. Two patients in the antibiotics group discontinued treatment as a result. Most adverse events involved mild gastrointestinal problems.
Continued on next page >>
WHAT’S NEW?
Evidence supports antibiotics for mild to moderate COPD
Few placebo-controlled trials have addressed antibiotic use for exacerbations in patients with mild to moderate COPD.2,8,9 This study demonstrated that, compared with placebo, symptom resolution and clinical success is greater with amoxicillin/clavulanate and that antibiotic treatment also may increase time until next exacerbation.
The study also looked at the relationship of CRP and exacerbations in the placebo group. Higher spontaneous clinical cure rates were noted when the CRP was lower than 40 mg/L.
CAVEATS
Effects of concomitant medications are unclear
In both the placebo and antibiotic groups, patients were taking other medications (including short- and long-acting β-agonists, anticholinergics, theophyllines, and oral or inhaled corticosteroids). Roughly the same number of patients in each group took additional medications, but researchers did not conduct a subgroup analysis to see if patients treated with these medications responded differently from those who received antibiotics alone.
GOLD guidelines already suggest antibiotics for exacerbations in patients with moderate COPD.2 In this study, 89% of patients met criteria for moderate COPD and 11% for mild COPD. Though the percentage of patients who had mild COPD was small, we believe the results of this study warrant consideration of antibiotic use in patients with mild disease. Local antibiograms may show increased resistance to amoxicillin/clavulanate; this study did not address the use of other antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotic overuse may be a concern
Concerns about antibiotic resistance may make clinicians reluctant to prescribe the drugs for those with mild to moderate COPD.
REFERENCES
1. Llor C, Moragas A, Hernández S, et al. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(8):716-723.
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. January 2014. www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Accessed April 15, 2014.
3. Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847-852.
4. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925-931.
5. Vollenweider DJ, Jarrett H, Steurer-Stey CA, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;12:CD010257.
6. Bartlett, JG, Sethi S. Management of infection in acute exacerbations of chronic obstructive pulmonary disease. In: Basow DS, ed. UpToDate. www.uptodate.com. Last updated March 27, 2012. Accessed January 2, 2013.
7. Lacoma A, Prat C, Andreo F, et al. Value of procalcitonin, C-reactive protein, and neopterin in exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:157-169.
8. Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med. 2009;15(2):120-125.
9. Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353-2361.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2014. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2014;63(4):E11-E13.