User login
Is low-molecular-weight heparin superior to aspirin for VTE prophylaxis?
ILLUSTRATIVE CASE
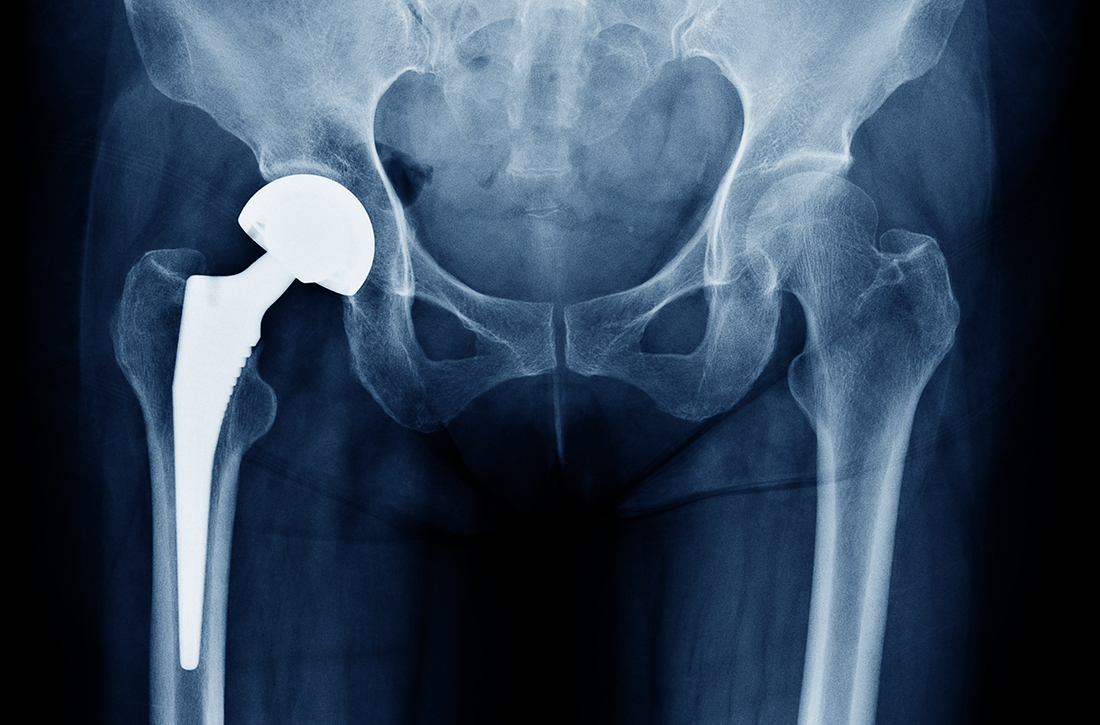
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
ILLUSTRATIVE CASE
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
ILLUSTRATIVE CASE
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
PRACTICE CHANGER
Consider low-molecular-weight heparin (LMWH) rather than aspirin to prevent postoperative venous thromboembolism (VTE) in patients undergoing total hip or knee arthroplasty for osteoarthritis.
STRENGTH OF RECOMMENDATION
B: Based on a single cluster-randomized crossover trial.1
A new standard for treatment of torus fractures of the wrist?
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
PRACTICE CHANGER
For uncomplicated pediatric torus fractures of the distal radius, consider definitive management with soft bandage immobilization until pain resolution, rather than rigid immobilization and clinical follow-up.
STRENGTH OF RECOMMENDATION
B: Based on a single randomized controlled trial with patient-oriented outcomes.1
Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
Can these salt substitutes prevent complications of hypertension?
ILLUSTRATIVE CASE
A 47-year-old man in generally good health presents to a family medicine clinic for a well visit. He does not use tobacco products and had a benign colonoscopy last year. He reports walking for 30 minutes 3 to 4 times per week for exercise, althoug h he has gained 3 lbs over the past 2 years. He has no family history of early coronary artery disease, but his father and older brother have hypertension. His mother has a history of diabetes and hyperlipidemia.
The patient’s physical exam is unremarkable except for an elevated BP reading of 151/82 mm Hg. A review of his chart indicates he has had multiple elevated readings in the past that have ranged from 132/72 mm Hg to 139/89 mm Hg. The patient is interested in antihypertensive treatment but wants to know if modifying his diet and replacing his regular table salt with a salt substitute will lower his high BP. What can you recommend?
Hypertension is a leading cause of CV morbidity and mortality worldwide and is linked to increased dietary sodium intake. An estimated 1.28 billion people worldwide have hypertension; however, more than half of cases are undiagnosed.2 The US Preventive Services Task Force recommends screening for hypertension in adults older than 18 years and confirming elevated measurements conducted in a nonclinical setting before starting medication (grade “A”).3
Cut-points for the diagnosis of hypertension vary. The American Academy of Family Physicians, 4 the Eighth Joint National Committee (JNC 8), 5 the International Society of Hypertension, 6 and the European Society of Cardiology 7 use ≥ 140 mm Hg systolic BP (SBP) or ≥ 90 mm Hg diastolic BP (DBP) to define hypertension. The American College of Cardiology/American Heart Association guidelines use ≥ 130/80 mm Hg. 8
When treating patients with hypertension, primary care physicians often recommend lifestyle modifications such as the
Systematic reviews have shown a measurable improvement in BP with sodium reduction and potassium substitution. 10-12 More importantly, high-quality evidence demonstrates a decreased risk for CV disease, kidney disease, and all-cause mortality with lower dietary sodium intake. 13 Previous studies have shown that potassium-enriched salt substitutes lower BP, but their impact on CV morbidity and mortality is not well defined. Although lowering BP is associated with improved clinical impact, there is a lack of patient-oriented evidence that demonstrates improvement in CV disease and mortality.
The Salt Substitute and Stroke Study (SSaSS), published in 2021, demonstrated the protective effect of salt substitution against stroke, other CV events, and death. 14 Furthermore, this 5-year, cluster-randomized controlled trial of 20,995 participants across 600 villages in China demonstrated reduced CV mortality and BP reduction similar to standard pharmacologic treatment. Prior to SSaSS, 17 randomized controlled trials demonstrated a BP-lowering effect of salt substitutes but did not directly study the impact on clinical outcomes. 13
Continue to: In this 2022 systematic review...
In this 2022 systematic review and meta-analysis, 1 Yin et al evaluated 21 trials, including SSaSS, for the effect of salt substitutes on BP and other clinical outcomes, and the generalizability of the study results to diverse populations. The systematic review included parallel-group, step-wedge, and cluster-randomized controlled trials reporting the effect of salt substitutes on BP or clinical outcomes.
STUDY SUMMARY
Salt substitutes reduced BP across diverse populations
This systematic review and meta-analysis reviewed existing literature for randomized controlled trials investigating the effects of potassium-enriched salt substitutes on clinical outcomes for patients without kidney disease. The most commonly used salt substitute was potassium chloride, at 25% to 65% potassium.
The systematic review identified 21 trials comprising 31,949 study participants from 15 different countries with 1 to 60 months’ duration. Meta-analyses were performed using 19 trials for BP outcomes and 5 trials for vascular outcomes. Eleven trials were rated as having low risk for bias, 8 were deemed to have some concern, and 2 were rated as high risk for bias. Comparisons of data excluding studies with high risk for bias yielded results similar to comparisons of all studies.
The meta-analysis of 19 trials demonstrated reduced SBP (–4.6 mm Hg; 95% CI, –6.1 to –3.1) and DBP (–1.6 mm Hg; 95% CI, –2.4 to –0.8) in participants using potassium-enriched salt substitutes. However, the authors noted substantial heterogeneity among the studies (I 2 > 70%) for both SBP and DBP outcomes. Although there were no subgroup differences for age, sex, hypertension history, or other biomarkers, outcome differences were associated with trial duration, baseline potassium intake, and composition of the salt substitute.
Potassium-enriched salt substitutes were associated with reduced total mortality (risk ratio [RR] = 0.89; 95% CI, 0.85-0.94), CV mortality (RR = 0.87; 95% CI, 0.81-0.94), and CV events (RR = 0.89; 95% CI, 0.85-0.94). In a meta-regression, each 10% reduction in the sodium content of the salt substitute was associated with a 1.5–mm Hg greater reduction in SBP (95% CI, –3.0 to –0.03) and a 1.0–mm Hg greater reduction in DBP (95% CI, –1.8 to –0.1). However, the authors suggest interpreting meta-regression results with caution.
Continue to: Only 2 of the studes...
Only 2 of the studies in the systematic review explicitly reported the adverse effect of hyperkalemia, and there was no statistical difference in events between randomized groups. Eight other studies reported no serious adverse events related to hyperkalemia , and 11 studies did not report on the risk for hyperkalemia.
WHAT’S NEW
High-quality data demonstrate beneficial outcomes
Previous observational and interventional studies demonstrated a BP-lowering effect of salt substitutes, but limited data with poor-quality evidence existed for the impact of salt substitutes on clinical outcomes such as mortality and CV events. This systematic review and meta-analysis suggests that potassium-supplemented salt may reduce BP and secondarily reduce the risk for CV events, CV mortality, and total mortality, without clear harmful effects reported.
CAVEATS
Some patient populations, comorbidities excluded from study
The study did not include patients with kidney disease or those taking potassium-sparing diuretics. Furthermore, the available data do not include primary prevention participants.
Subgroup analyses should be interpreted with caution due to the small number of trials available for individual subgroups. In addition, funnel plot asymmetry for studies reporting DBP suggests at least some effect of publication bias for that outcome.
Although BP reduction due to salt substitutes may be small at an individual level, these levels of reduction may be important at a population level.
CHALLENGES TO IMPLEMENTATION
For appropriate patients, no challenges anticipated
There are no significant challenges to implementing conclusions from this study in the primary care setting. Family physicians should be able to recommend potassium-enriched salt substitutes to patients with hypertension who are not at risk for hyperkalemia, including those with kidney disease, on potassium-sparing diuretics, or with a history of hyperkalemia/hyperkalemic conditions. Salt substitutes, including potassium-enriched salts, are readily available in stores.
1. Yin X, Rodgers A, Perkovic A, et al. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart. 2022;108:1608-1615. doi: 10.1136/heartjnl-2022-321332
2. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957-980. doi: 10.1016/S0140-6736(21)01330-1
3. USPSTF. Hypertension in adults: screening. Final recommendation statement. Published April 27, 2021. Accessed September 18, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening
4. Coles S, Fisher L, Lin KW, et al. Blood pressure targets in adults with hypertension: a clinical practice guideline from the AAFP. Published November 4, 2022. Accessed September 18, 2023. www.aafp.org/dam/AAFP/documents/journals/afp/AAFPHypertensionGuideline.pdf
5. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. doi: 10.1001/jama. 2013.284427
6. Unger T, Borgi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026
7. Mancia G, Kreutz R, Brunstrom M, et al; the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension. 2023 ESH Guidelines for the management of arterial hypertension. Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023; Jun 21. doi: 10.1097/HJH.0000000000003480
8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-e115. 10.1161/HYP.0000000000000065
9. National Center for Health Statistics. National Ambulatory Medical Care Survey: 2014 state and national summary tables. Accessed June 27, 2023. www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf
10. Huang L, Trieu K, Yoshimura S, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. doi: 10.1136/bmj.m315
11. Filippini T, Violi F, D’Amico R, et al. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. 2017;230:127-135. doi: 10.1016/j.ijcard.2016.12.048
12. Brand A, Visser ME, Schoonees A, et al. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev. 2022;8:CD015207. doi: 10.1002/14651858.CD015207
13. He FJ, Tan M, Ma Y, et al. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:632-647. doi: 10.1016/j.jacc.2019.11.055
14. Neal B, Wu Y, Feng X, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med. 2021;385:1067-1077. doi: 10.1056/NEJMoa2105675
ILLUSTRATIVE CASE
A 47-year-old man in generally good health presents to a family medicine clinic for a well visit. He does not use tobacco products and had a benign colonoscopy last year. He reports walking for 30 minutes 3 to 4 times per week for exercise, althoug h he has gained 3 lbs over the past 2 years. He has no family history of early coronary artery disease, but his father and older brother have hypertension. His mother has a history of diabetes and hyperlipidemia.
The patient’s physical exam is unremarkable except for an elevated BP reading of 151/82 mm Hg. A review of his chart indicates he has had multiple elevated readings in the past that have ranged from 132/72 mm Hg to 139/89 mm Hg. The patient is interested in antihypertensive treatment but wants to know if modifying his diet and replacing his regular table salt with a salt substitute will lower his high BP. What can you recommend?
Hypertension is a leading cause of CV morbidity and mortality worldwide and is linked to increased dietary sodium intake. An estimated 1.28 billion people worldwide have hypertension; however, more than half of cases are undiagnosed.2 The US Preventive Services Task Force recommends screening for hypertension in adults older than 18 years and confirming elevated measurements conducted in a nonclinical setting before starting medication (grade “A”).3
Cut-points for the diagnosis of hypertension vary. The American Academy of Family Physicians, 4 the Eighth Joint National Committee (JNC 8), 5 the International Society of Hypertension, 6 and the European Society of Cardiology 7 use ≥ 140 mm Hg systolic BP (SBP) or ≥ 90 mm Hg diastolic BP (DBP) to define hypertension. The American College of Cardiology/American Heart Association guidelines use ≥ 130/80 mm Hg. 8
When treating patients with hypertension, primary care physicians often recommend lifestyle modifications such as the
Systematic reviews have shown a measurable improvement in BP with sodium reduction and potassium substitution. 10-12 More importantly, high-quality evidence demonstrates a decreased risk for CV disease, kidney disease, and all-cause mortality with lower dietary sodium intake. 13 Previous studies have shown that potassium-enriched salt substitutes lower BP, but their impact on CV morbidity and mortality is not well defined. Although lowering BP is associated with improved clinical impact, there is a lack of patient-oriented evidence that demonstrates improvement in CV disease and mortality.
The Salt Substitute and Stroke Study (SSaSS), published in 2021, demonstrated the protective effect of salt substitution against stroke, other CV events, and death. 14 Furthermore, this 5-year, cluster-randomized controlled trial of 20,995 participants across 600 villages in China demonstrated reduced CV mortality and BP reduction similar to standard pharmacologic treatment. Prior to SSaSS, 17 randomized controlled trials demonstrated a BP-lowering effect of salt substitutes but did not directly study the impact on clinical outcomes. 13
Continue to: In this 2022 systematic review...
In this 2022 systematic review and meta-analysis, 1 Yin et al evaluated 21 trials, including SSaSS, for the effect of salt substitutes on BP and other clinical outcomes, and the generalizability of the study results to diverse populations. The systematic review included parallel-group, step-wedge, and cluster-randomized controlled trials reporting the effect of salt substitutes on BP or clinical outcomes.
STUDY SUMMARY
Salt substitutes reduced BP across diverse populations
This systematic review and meta-analysis reviewed existing literature for randomized controlled trials investigating the effects of potassium-enriched salt substitutes on clinical outcomes for patients without kidney disease. The most commonly used salt substitute was potassium chloride, at 25% to 65% potassium.
The systematic review identified 21 trials comprising 31,949 study participants from 15 different countries with 1 to 60 months’ duration. Meta-analyses were performed using 19 trials for BP outcomes and 5 trials for vascular outcomes. Eleven trials were rated as having low risk for bias, 8 were deemed to have some concern, and 2 were rated as high risk for bias. Comparisons of data excluding studies with high risk for bias yielded results similar to comparisons of all studies.
The meta-analysis of 19 trials demonstrated reduced SBP (–4.6 mm Hg; 95% CI, –6.1 to –3.1) and DBP (–1.6 mm Hg; 95% CI, –2.4 to –0.8) in participants using potassium-enriched salt substitutes. However, the authors noted substantial heterogeneity among the studies (I 2 > 70%) for both SBP and DBP outcomes. Although there were no subgroup differences for age, sex, hypertension history, or other biomarkers, outcome differences were associated with trial duration, baseline potassium intake, and composition of the salt substitute.
Potassium-enriched salt substitutes were associated with reduced total mortality (risk ratio [RR] = 0.89; 95% CI, 0.85-0.94), CV mortality (RR = 0.87; 95% CI, 0.81-0.94), and CV events (RR = 0.89; 95% CI, 0.85-0.94). In a meta-regression, each 10% reduction in the sodium content of the salt substitute was associated with a 1.5–mm Hg greater reduction in SBP (95% CI, –3.0 to –0.03) and a 1.0–mm Hg greater reduction in DBP (95% CI, –1.8 to –0.1). However, the authors suggest interpreting meta-regression results with caution.
Continue to: Only 2 of the studes...
Only 2 of the studies in the systematic review explicitly reported the adverse effect of hyperkalemia, and there was no statistical difference in events between randomized groups. Eight other studies reported no serious adverse events related to hyperkalemia , and 11 studies did not report on the risk for hyperkalemia.
WHAT’S NEW
High-quality data demonstrate beneficial outcomes
Previous observational and interventional studies demonstrated a BP-lowering effect of salt substitutes, but limited data with poor-quality evidence existed for the impact of salt substitutes on clinical outcomes such as mortality and CV events. This systematic review and meta-analysis suggests that potassium-supplemented salt may reduce BP and secondarily reduce the risk for CV events, CV mortality, and total mortality, without clear harmful effects reported.
CAVEATS
Some patient populations, comorbidities excluded from study
The study did not include patients with kidney disease or those taking potassium-sparing diuretics. Furthermore, the available data do not include primary prevention participants.
Subgroup analyses should be interpreted with caution due to the small number of trials available for individual subgroups. In addition, funnel plot asymmetry for studies reporting DBP suggests at least some effect of publication bias for that outcome.
Although BP reduction due to salt substitutes may be small at an individual level, these levels of reduction may be important at a population level.
CHALLENGES TO IMPLEMENTATION
For appropriate patients, no challenges anticipated
There are no significant challenges to implementing conclusions from this study in the primary care setting. Family physicians should be able to recommend potassium-enriched salt substitutes to patients with hypertension who are not at risk for hyperkalemia, including those with kidney disease, on potassium-sparing diuretics, or with a history of hyperkalemia/hyperkalemic conditions. Salt substitutes, including potassium-enriched salts, are readily available in stores.
ILLUSTRATIVE CASE
A 47-year-old man in generally good health presents to a family medicine clinic for a well visit. He does not use tobacco products and had a benign colonoscopy last year. He reports walking for 30 minutes 3 to 4 times per week for exercise, althoug h he has gained 3 lbs over the past 2 years. He has no family history of early coronary artery disease, but his father and older brother have hypertension. His mother has a history of diabetes and hyperlipidemia.
The patient’s physical exam is unremarkable except for an elevated BP reading of 151/82 mm Hg. A review of his chart indicates he has had multiple elevated readings in the past that have ranged from 132/72 mm Hg to 139/89 mm Hg. The patient is interested in antihypertensive treatment but wants to know if modifying his diet and replacing his regular table salt with a salt substitute will lower his high BP. What can you recommend?
Hypertension is a leading cause of CV morbidity and mortality worldwide and is linked to increased dietary sodium intake. An estimated 1.28 billion people worldwide have hypertension; however, more than half of cases are undiagnosed.2 The US Preventive Services Task Force recommends screening for hypertension in adults older than 18 years and confirming elevated measurements conducted in a nonclinical setting before starting medication (grade “A”).3
Cut-points for the diagnosis of hypertension vary. The American Academy of Family Physicians, 4 the Eighth Joint National Committee (JNC 8), 5 the International Society of Hypertension, 6 and the European Society of Cardiology 7 use ≥ 140 mm Hg systolic BP (SBP) or ≥ 90 mm Hg diastolic BP (DBP) to define hypertension. The American College of Cardiology/American Heart Association guidelines use ≥ 130/80 mm Hg. 8
When treating patients with hypertension, primary care physicians often recommend lifestyle modifications such as the
Systematic reviews have shown a measurable improvement in BP with sodium reduction and potassium substitution. 10-12 More importantly, high-quality evidence demonstrates a decreased risk for CV disease, kidney disease, and all-cause mortality with lower dietary sodium intake. 13 Previous studies have shown that potassium-enriched salt substitutes lower BP, but their impact on CV morbidity and mortality is not well defined. Although lowering BP is associated with improved clinical impact, there is a lack of patient-oriented evidence that demonstrates improvement in CV disease and mortality.
The Salt Substitute and Stroke Study (SSaSS), published in 2021, demonstrated the protective effect of salt substitution against stroke, other CV events, and death. 14 Furthermore, this 5-year, cluster-randomized controlled trial of 20,995 participants across 600 villages in China demonstrated reduced CV mortality and BP reduction similar to standard pharmacologic treatment. Prior to SSaSS, 17 randomized controlled trials demonstrated a BP-lowering effect of salt substitutes but did not directly study the impact on clinical outcomes. 13
Continue to: In this 2022 systematic review...
In this 2022 systematic review and meta-analysis, 1 Yin et al evaluated 21 trials, including SSaSS, for the effect of salt substitutes on BP and other clinical outcomes, and the generalizability of the study results to diverse populations. The systematic review included parallel-group, step-wedge, and cluster-randomized controlled trials reporting the effect of salt substitutes on BP or clinical outcomes.
STUDY SUMMARY
Salt substitutes reduced BP across diverse populations
This systematic review and meta-analysis reviewed existing literature for randomized controlled trials investigating the effects of potassium-enriched salt substitutes on clinical outcomes for patients without kidney disease. The most commonly used salt substitute was potassium chloride, at 25% to 65% potassium.
The systematic review identified 21 trials comprising 31,949 study participants from 15 different countries with 1 to 60 months’ duration. Meta-analyses were performed using 19 trials for BP outcomes and 5 trials for vascular outcomes. Eleven trials were rated as having low risk for bias, 8 were deemed to have some concern, and 2 were rated as high risk for bias. Comparisons of data excluding studies with high risk for bias yielded results similar to comparisons of all studies.
The meta-analysis of 19 trials demonstrated reduced SBP (–4.6 mm Hg; 95% CI, –6.1 to –3.1) and DBP (–1.6 mm Hg; 95% CI, –2.4 to –0.8) in participants using potassium-enriched salt substitutes. However, the authors noted substantial heterogeneity among the studies (I 2 > 70%) for both SBP and DBP outcomes. Although there were no subgroup differences for age, sex, hypertension history, or other biomarkers, outcome differences were associated with trial duration, baseline potassium intake, and composition of the salt substitute.
Potassium-enriched salt substitutes were associated with reduced total mortality (risk ratio [RR] = 0.89; 95% CI, 0.85-0.94), CV mortality (RR = 0.87; 95% CI, 0.81-0.94), and CV events (RR = 0.89; 95% CI, 0.85-0.94). In a meta-regression, each 10% reduction in the sodium content of the salt substitute was associated with a 1.5–mm Hg greater reduction in SBP (95% CI, –3.0 to –0.03) and a 1.0–mm Hg greater reduction in DBP (95% CI, –1.8 to –0.1). However, the authors suggest interpreting meta-regression results with caution.
Continue to: Only 2 of the studes...
Only 2 of the studies in the systematic review explicitly reported the adverse effect of hyperkalemia, and there was no statistical difference in events between randomized groups. Eight other studies reported no serious adverse events related to hyperkalemia , and 11 studies did not report on the risk for hyperkalemia.
WHAT’S NEW
High-quality data demonstrate beneficial outcomes
Previous observational and interventional studies demonstrated a BP-lowering effect of salt substitutes, but limited data with poor-quality evidence existed for the impact of salt substitutes on clinical outcomes such as mortality and CV events. This systematic review and meta-analysis suggests that potassium-supplemented salt may reduce BP and secondarily reduce the risk for CV events, CV mortality, and total mortality, without clear harmful effects reported.
CAVEATS
Some patient populations, comorbidities excluded from study
The study did not include patients with kidney disease or those taking potassium-sparing diuretics. Furthermore, the available data do not include primary prevention participants.
Subgroup analyses should be interpreted with caution due to the small number of trials available for individual subgroups. In addition, funnel plot asymmetry for studies reporting DBP suggests at least some effect of publication bias for that outcome.
Although BP reduction due to salt substitutes may be small at an individual level, these levels of reduction may be important at a population level.
CHALLENGES TO IMPLEMENTATION
For appropriate patients, no challenges anticipated
There are no significant challenges to implementing conclusions from this study in the primary care setting. Family physicians should be able to recommend potassium-enriched salt substitutes to patients with hypertension who are not at risk for hyperkalemia, including those with kidney disease, on potassium-sparing diuretics, or with a history of hyperkalemia/hyperkalemic conditions. Salt substitutes, including potassium-enriched salts, are readily available in stores.
1. Yin X, Rodgers A, Perkovic A, et al. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart. 2022;108:1608-1615. doi: 10.1136/heartjnl-2022-321332
2. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957-980. doi: 10.1016/S0140-6736(21)01330-1
3. USPSTF. Hypertension in adults: screening. Final recommendation statement. Published April 27, 2021. Accessed September 18, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening
4. Coles S, Fisher L, Lin KW, et al. Blood pressure targets in adults with hypertension: a clinical practice guideline from the AAFP. Published November 4, 2022. Accessed September 18, 2023. www.aafp.org/dam/AAFP/documents/journals/afp/AAFPHypertensionGuideline.pdf
5. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. doi: 10.1001/jama. 2013.284427
6. Unger T, Borgi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026
7. Mancia G, Kreutz R, Brunstrom M, et al; the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension. 2023 ESH Guidelines for the management of arterial hypertension. Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023; Jun 21. doi: 10.1097/HJH.0000000000003480
8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-e115. 10.1161/HYP.0000000000000065
9. National Center for Health Statistics. National Ambulatory Medical Care Survey: 2014 state and national summary tables. Accessed June 27, 2023. www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf
10. Huang L, Trieu K, Yoshimura S, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. doi: 10.1136/bmj.m315
11. Filippini T, Violi F, D’Amico R, et al. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. 2017;230:127-135. doi: 10.1016/j.ijcard.2016.12.048
12. Brand A, Visser ME, Schoonees A, et al. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev. 2022;8:CD015207. doi: 10.1002/14651858.CD015207
13. He FJ, Tan M, Ma Y, et al. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:632-647. doi: 10.1016/j.jacc.2019.11.055
14. Neal B, Wu Y, Feng X, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med. 2021;385:1067-1077. doi: 10.1056/NEJMoa2105675
1. Yin X, Rodgers A, Perkovic A, et al. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart. 2022;108:1608-1615. doi: 10.1136/heartjnl-2022-321332
2. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957-980. doi: 10.1016/S0140-6736(21)01330-1
3. USPSTF. Hypertension in adults: screening. Final recommendation statement. Published April 27, 2021. Accessed September 18, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening
4. Coles S, Fisher L, Lin KW, et al. Blood pressure targets in adults with hypertension: a clinical practice guideline from the AAFP. Published November 4, 2022. Accessed September 18, 2023. www.aafp.org/dam/AAFP/documents/journals/afp/AAFPHypertensionGuideline.pdf
5. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. doi: 10.1001/jama. 2013.284427
6. Unger T, Borgi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026
7. Mancia G, Kreutz R, Brunstrom M, et al; the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension. 2023 ESH Guidelines for the management of arterial hypertension. Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023; Jun 21. doi: 10.1097/HJH.0000000000003480
8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-e115. 10.1161/HYP.0000000000000065
9. National Center for Health Statistics. National Ambulatory Medical Care Survey: 2014 state and national summary tables. Accessed June 27, 2023. www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf
10. Huang L, Trieu K, Yoshimura S, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. doi: 10.1136/bmj.m315
11. Filippini T, Violi F, D’Amico R, et al. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. 2017;230:127-135. doi: 10.1016/j.ijcard.2016.12.048
12. Brand A, Visser ME, Schoonees A, et al. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev. 2022;8:CD015207. doi: 10.1002/14651858.CD015207
13. He FJ, Tan M, Ma Y, et al. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:632-647. doi: 10.1016/j.jacc.2019.11.055
14. Neal B, Wu Y, Feng X, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med. 2021;385:1067-1077. doi: 10.1056/NEJMoa2105675
PRACTICE CHANGER
Consider recommending potassium-enriched salt substitutes for appropriate patients with hypertension to reduce blood pressure (BP) and risk for related cardiovascular (CV) events or mortality.
STRENGTH OF RECOMMENDATION
A: Based on a systematic review and meta-analysis of controlled trials. 1
Yin X, Rodgers A, Perkovic A, et al. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart . 2022;108:1608-1615. doi: 10.1136/heartjnl-2022-321332
Should you treat prediabetes? It’s complicated
ILLUSTRATIVE CASE
A 51-year-old woman with a history of elevated cholesterol and a body mass index (BMI) of 31 presents to your clinic for a scheduled follow-up visit to review recent blood test results. Her A1C was elevated at 5.9%. She wants to know if she should start medication now.
Prediabetes is a high-risk state that confers increased risk for type 2 diabetes (T2D). It is identified by impaired fasting glucose (fasting plasma glucose [FPG], 100-125 mg/dL), impaired glucose tolerance (2-hour oral glucose tolerance test, 140-199 mg/dL), or an elevated A1C (between 5.7% and 6.4%).2
An estimated 96 million Americans—38% of the US adult population—have prediabetes, according to the Centers for Disease Control and Prevention.3 Family physicians frequently encounter this condition when screening for T2D in asymptomatic adults (ages 35 to 70 years) with overweight or obesity, as recommended by the US Preventive Services Task Force (grade “B”).4
To treat, or not? Studies have shown that interventions such as lifestyle modification and use of metformin by patients with prediabetes can decrease their risk for T2D.5,6 In the Diabetes Prevention Program (DPP) study, progression from prediabetes to T2D was reduced to 14% with lifestyle modification and 22% with metformin use, vs 29% with placebo.7
However, there is disagreement about whether to treat prediabetes, particularly with medication. Some argue that metformin is a safe, effective, and cost-saving treatment to prevent T2D and its associated health consequences.8 The current American Diabetes Association (ADA) guidelines suggest that metformin be considered in certain patients with prediabetes and high-risk factors, especially younger age, obesity or hyperglycemia, or a history of gestational diabetes.9 However, only an estimated 1% to 4% of adults with prediabetes are prescribed metformin.10
Others argue that treating a preclinical condition is not a patient-centered approach, especially since not all patients with prediabetes progress to T2D and the risk for development or progression of retinopathy and microalbuminuria is extremely low if A1C levels remain < 7.0%.11 By this standard, pharmacologic treatment should be initiated only if, or when, a patient develops T2D, with a focus on intensive lifestyle intervention for high-risk patients in the interim.11
Given the conflicting viewpoints, ongoing long-term studies on T2D prevention will help guide treatment decisions for patients with prediabetes. The study by Lee et al1 was the first to evaluate the effect of metformin or intensive lifestyle modification on all-cause and cause-specific mortality in patients at high risk for T2D.
Continue to: STUDY SUMMARY
STUDY SUMMARY
No mortality benefit from metformin or lifestyle modification
This secondary analysis evaluated mortality outcomes for patients at risk for T2D who were part of the DPP trial and then were followed long term in the Diabetes Prevention Program Outcomes Study (DPPOS).1 The initial DPP trial included 3234 adult patients at high risk for T2D (defined as having a BMI ≥ 24; an FPG of 95-125 mg/dL; and a 2-hour glucose level of 140-199 mg/dL). Participants were randomized into groups receiving either intensive lifestyle intervention (which focused on achieving ≥ 150 min/wk of exercise and ≥ 7% body weight loss), metformin 850 mg twice daily, or placebo twice daily; the latter 2 groups also received standard exercise and diet recommendations. Mean age was 51 years, mean BMI was 34, and 68% of participants were female.
At the conclusion of the initial 5-year trial, treatment was unmasked and 86% of the patients continued to be followed for long-term outcomes. Patients in the lifestyle group were offered semiannual lifestyle reinforcement, while the metformin group continued to receive the twice-daily 850-mg dose unless a contraindication developed. If FPG levels increased to ≥ 140 mg/dL in the DPP study, or A1C increased to ≥ 7% in the DPPOS, study metformin was discontinued and management of the patient’s diabetes was transferred to their health care provider. By the end of the DPPOS, 53% of patients in the lifestyle group and 55% in the metformin group had progressed to T2D, compared with 60% in the placebo group (P = 0.003).
After a median 21-year follow-up interval, the investigators collected data on cause of death for patients and evaluated hazard ratios (HRs) for overall and cause-specific mortality. In total, 14% of the participants died, with no statistically significant difference in rates between the 3 groups. Cancer (37%) was the leading cause of death in all groups, followed by cardiovascular disease (CVD; 29%).
Compared with the placebo group, patients taking metformin did not have a decreased rate of overall mortality (HR = 0.99; 95% CI, 0.79-1.25), mortality from cancer (HR = 1.04; 95% CI, 0.72-1.52), or mortality due to CVD (HR = 1.08; 95% CI, 0.70-1.66). Similarly, compared with the placebo group, lifestyle intervention did not decrease overall mortality (HR = 1.02; 95% CI, 0.81-1.28), mortality from cancer (HR = 1.07; 95% CI, 0.74-1.55), or mortality due to CVD (HR = 1.18; 95% CI, 0.77-1.81). Results were similar when adjusted for other factors, including out-of-study metformin use, T2D status and duration, BMI change, and other cardiovascular risk factors.
WHAT’S NEW
Long-term data clarifylimits to interventions’ utility
This study looked at long-term follow-up data on mortality outcomes for patients with prediabetes treated with metformin or lifestyle intervention. Although these interventions did support weight loss, reduce the incidence of T2D, and lower cardiovascular risk factors (eg, hypertension, dyslipidemia), the comorbidity benefits did not affect risk for all-cause or cause-specific mortality, which were similar between the treatment and placebo groups.
Continue to: CAVEATS
CAVEATS
Exclusion criteria, residual confounding may limit the findings
Patients with significant cardiovascular or renal disease were excluded, so results may not apply to patients with these comorbidities. Additionally, there was a high amount of “drop-in” use of metformin prescribed by physicians once patients developed T2D, which may not have been controlled for completely. And while the intensive lifestyle intervention group had specific goals, the metformin and placebo groups also were encouraged to follow standard diet and lifestyle recommendations—and during a bridge period, all participants were offered a modified group lifestyle intervention. However, multivariable adjustment did not change the study conclusion.
CHALLENGES TO IMPLEMENTATION
Physicians may be unwilling to change their current prescribing habits
Physicians may not be willing to change their practice of prescribing metformin in prediabetes based on a singular study (with residual confounding) that showed no long-term mortality differences between the study groups. However, there may be long-term morbidity differences of interest to patients that were not specifically evaluated in this study—such as quality-of-life benefits from weight loss that may outweigh the risks (eg, gastrointestinal adverse effects such as diarrhea, nausea, and abdominal pain) of metformin for some patients. Therefore, a discussion of the risks and benefits of treatment for prediabetes should be had with patients at high risk who would prefer a pharmacologic intervention.
1. Lee CG, Heckman-Stoddard B, et al; Diabetes Prevention Program Research Group. Effect of metformin and lifestyle interventions on mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care. 2021;44:2775-2782. doi: 10.2337/dc21-1046
2. American Diabetes Association. Understanding A1C: diagnosis. Accessed July 6, 2023. https://diabetes.org/diabetes/a1c/diagnosis
3. CDC. National diabetes statistics report. Reviewed June 29, 2022. Accessed January 23, 2023. www.cdc.gov/diabetes/data/statistics-report/index.html
4. USPSTF; Davidson KW, Barry MJ, Mangione CM, et al. Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531
5. Hostalek U, Campbell I. Metformin for diabetes prevention: update of the evidence base. Curr Med Res Opin. 2021;37:1705-1717. doi: 10.1080/03007995.2021.1955667
6. Aroda VR, Knowler WC, Crandall JP, et al; Diabetes Prevention Program Research Group. Metformin for diabetes prevention: insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia. 2017;60:1601-1611. doi: 10.1007/s00125-017-4361-9
7. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512
8. Herman WH, Ratner RE. Metformin should be used to treat prediabetes in selected individuals. Diabetes Care. 2020;43:1988-1990. doi: 10.2337/dci20-0030
9. American Diabetes Association. 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(suppl 1):S34-S39. doi: 10.2337/dc21-S003
10. Tseng E, Yeh HC, Maruthur NM. Metformin use in prediabetes among US adults, 2005-2012. Diabetes Care. 2017;40:887-893. doi: 10.2337/dc16-1509
11. Davidson MB. Metformin should not be used to treat prediabetes. Diabetes Care. 2020;43:1983-1987. doi: 10.2337/dc19-2221
ILLUSTRATIVE CASE
A 51-year-old woman with a history of elevated cholesterol and a body mass index (BMI) of 31 presents to your clinic for a scheduled follow-up visit to review recent blood test results. Her A1C was elevated at 5.9%. She wants to know if she should start medication now.
Prediabetes is a high-risk state that confers increased risk for type 2 diabetes (T2D). It is identified by impaired fasting glucose (fasting plasma glucose [FPG], 100-125 mg/dL), impaired glucose tolerance (2-hour oral glucose tolerance test, 140-199 mg/dL), or an elevated A1C (between 5.7% and 6.4%).2
An estimated 96 million Americans—38% of the US adult population—have prediabetes, according to the Centers for Disease Control and Prevention.3 Family physicians frequently encounter this condition when screening for T2D in asymptomatic adults (ages 35 to 70 years) with overweight or obesity, as recommended by the US Preventive Services Task Force (grade “B”).4
To treat, or not? Studies have shown that interventions such as lifestyle modification and use of metformin by patients with prediabetes can decrease their risk for T2D.5,6 In the Diabetes Prevention Program (DPP) study, progression from prediabetes to T2D was reduced to 14% with lifestyle modification and 22% with metformin use, vs 29% with placebo.7
However, there is disagreement about whether to treat prediabetes, particularly with medication. Some argue that metformin is a safe, effective, and cost-saving treatment to prevent T2D and its associated health consequences.8 The current American Diabetes Association (ADA) guidelines suggest that metformin be considered in certain patients with prediabetes and high-risk factors, especially younger age, obesity or hyperglycemia, or a history of gestational diabetes.9 However, only an estimated 1% to 4% of adults with prediabetes are prescribed metformin.10
Others argue that treating a preclinical condition is not a patient-centered approach, especially since not all patients with prediabetes progress to T2D and the risk for development or progression of retinopathy and microalbuminuria is extremely low if A1C levels remain < 7.0%.11 By this standard, pharmacologic treatment should be initiated only if, or when, a patient develops T2D, with a focus on intensive lifestyle intervention for high-risk patients in the interim.11
Given the conflicting viewpoints, ongoing long-term studies on T2D prevention will help guide treatment decisions for patients with prediabetes. The study by Lee et al1 was the first to evaluate the effect of metformin or intensive lifestyle modification on all-cause and cause-specific mortality in patients at high risk for T2D.
Continue to: STUDY SUMMARY
STUDY SUMMARY
No mortality benefit from metformin or lifestyle modification
This secondary analysis evaluated mortality outcomes for patients at risk for T2D who were part of the DPP trial and then were followed long term in the Diabetes Prevention Program Outcomes Study (DPPOS).1 The initial DPP trial included 3234 adult patients at high risk for T2D (defined as having a BMI ≥ 24; an FPG of 95-125 mg/dL; and a 2-hour glucose level of 140-199 mg/dL). Participants were randomized into groups receiving either intensive lifestyle intervention (which focused on achieving ≥ 150 min/wk of exercise and ≥ 7% body weight loss), metformin 850 mg twice daily, or placebo twice daily; the latter 2 groups also received standard exercise and diet recommendations. Mean age was 51 years, mean BMI was 34, and 68% of participants were female.
At the conclusion of the initial 5-year trial, treatment was unmasked and 86% of the patients continued to be followed for long-term outcomes. Patients in the lifestyle group were offered semiannual lifestyle reinforcement, while the metformin group continued to receive the twice-daily 850-mg dose unless a contraindication developed. If FPG levels increased to ≥ 140 mg/dL in the DPP study, or A1C increased to ≥ 7% in the DPPOS, study metformin was discontinued and management of the patient’s diabetes was transferred to their health care provider. By the end of the DPPOS, 53% of patients in the lifestyle group and 55% in the metformin group had progressed to T2D, compared with 60% in the placebo group (P = 0.003).
After a median 21-year follow-up interval, the investigators collected data on cause of death for patients and evaluated hazard ratios (HRs) for overall and cause-specific mortality. In total, 14% of the participants died, with no statistically significant difference in rates between the 3 groups. Cancer (37%) was the leading cause of death in all groups, followed by cardiovascular disease (CVD; 29%).
Compared with the placebo group, patients taking metformin did not have a decreased rate of overall mortality (HR = 0.99; 95% CI, 0.79-1.25), mortality from cancer (HR = 1.04; 95% CI, 0.72-1.52), or mortality due to CVD (HR = 1.08; 95% CI, 0.70-1.66). Similarly, compared with the placebo group, lifestyle intervention did not decrease overall mortality (HR = 1.02; 95% CI, 0.81-1.28), mortality from cancer (HR = 1.07; 95% CI, 0.74-1.55), or mortality due to CVD (HR = 1.18; 95% CI, 0.77-1.81). Results were similar when adjusted for other factors, including out-of-study metformin use, T2D status and duration, BMI change, and other cardiovascular risk factors.
WHAT’S NEW
Long-term data clarifylimits to interventions’ utility
This study looked at long-term follow-up data on mortality outcomes for patients with prediabetes treated with metformin or lifestyle intervention. Although these interventions did support weight loss, reduce the incidence of T2D, and lower cardiovascular risk factors (eg, hypertension, dyslipidemia), the comorbidity benefits did not affect risk for all-cause or cause-specific mortality, which were similar between the treatment and placebo groups.
Continue to: CAVEATS
CAVEATS
Exclusion criteria, residual confounding may limit the findings
Patients with significant cardiovascular or renal disease were excluded, so results may not apply to patients with these comorbidities. Additionally, there was a high amount of “drop-in” use of metformin prescribed by physicians once patients developed T2D, which may not have been controlled for completely. And while the intensive lifestyle intervention group had specific goals, the metformin and placebo groups also were encouraged to follow standard diet and lifestyle recommendations—and during a bridge period, all participants were offered a modified group lifestyle intervention. However, multivariable adjustment did not change the study conclusion.
CHALLENGES TO IMPLEMENTATION
Physicians may be unwilling to change their current prescribing habits
Physicians may not be willing to change their practice of prescribing metformin in prediabetes based on a singular study (with residual confounding) that showed no long-term mortality differences between the study groups. However, there may be long-term morbidity differences of interest to patients that were not specifically evaluated in this study—such as quality-of-life benefits from weight loss that may outweigh the risks (eg, gastrointestinal adverse effects such as diarrhea, nausea, and abdominal pain) of metformin for some patients. Therefore, a discussion of the risks and benefits of treatment for prediabetes should be had with patients at high risk who would prefer a pharmacologic intervention.
ILLUSTRATIVE CASE
A 51-year-old woman with a history of elevated cholesterol and a body mass index (BMI) of 31 presents to your clinic for a scheduled follow-up visit to review recent blood test results. Her A1C was elevated at 5.9%. She wants to know if she should start medication now.
Prediabetes is a high-risk state that confers increased risk for type 2 diabetes (T2D). It is identified by impaired fasting glucose (fasting plasma glucose [FPG], 100-125 mg/dL), impaired glucose tolerance (2-hour oral glucose tolerance test, 140-199 mg/dL), or an elevated A1C (between 5.7% and 6.4%).2
An estimated 96 million Americans—38% of the US adult population—have prediabetes, according to the Centers for Disease Control and Prevention.3 Family physicians frequently encounter this condition when screening for T2D in asymptomatic adults (ages 35 to 70 years) with overweight or obesity, as recommended by the US Preventive Services Task Force (grade “B”).4
To treat, or not? Studies have shown that interventions such as lifestyle modification and use of metformin by patients with prediabetes can decrease their risk for T2D.5,6 In the Diabetes Prevention Program (DPP) study, progression from prediabetes to T2D was reduced to 14% with lifestyle modification and 22% with metformin use, vs 29% with placebo.7
However, there is disagreement about whether to treat prediabetes, particularly with medication. Some argue that metformin is a safe, effective, and cost-saving treatment to prevent T2D and its associated health consequences.8 The current American Diabetes Association (ADA) guidelines suggest that metformin be considered in certain patients with prediabetes and high-risk factors, especially younger age, obesity or hyperglycemia, or a history of gestational diabetes.9 However, only an estimated 1% to 4% of adults with prediabetes are prescribed metformin.10
Others argue that treating a preclinical condition is not a patient-centered approach, especially since not all patients with prediabetes progress to T2D and the risk for development or progression of retinopathy and microalbuminuria is extremely low if A1C levels remain < 7.0%.11 By this standard, pharmacologic treatment should be initiated only if, or when, a patient develops T2D, with a focus on intensive lifestyle intervention for high-risk patients in the interim.11
Given the conflicting viewpoints, ongoing long-term studies on T2D prevention will help guide treatment decisions for patients with prediabetes. The study by Lee et al1 was the first to evaluate the effect of metformin or intensive lifestyle modification on all-cause and cause-specific mortality in patients at high risk for T2D.
Continue to: STUDY SUMMARY
STUDY SUMMARY
No mortality benefit from metformin or lifestyle modification
This secondary analysis evaluated mortality outcomes for patients at risk for T2D who were part of the DPP trial and then were followed long term in the Diabetes Prevention Program Outcomes Study (DPPOS).1 The initial DPP trial included 3234 adult patients at high risk for T2D (defined as having a BMI ≥ 24; an FPG of 95-125 mg/dL; and a 2-hour glucose level of 140-199 mg/dL). Participants were randomized into groups receiving either intensive lifestyle intervention (which focused on achieving ≥ 150 min/wk of exercise and ≥ 7% body weight loss), metformin 850 mg twice daily, or placebo twice daily; the latter 2 groups also received standard exercise and diet recommendations. Mean age was 51 years, mean BMI was 34, and 68% of participants were female.
At the conclusion of the initial 5-year trial, treatment was unmasked and 86% of the patients continued to be followed for long-term outcomes. Patients in the lifestyle group were offered semiannual lifestyle reinforcement, while the metformin group continued to receive the twice-daily 850-mg dose unless a contraindication developed. If FPG levels increased to ≥ 140 mg/dL in the DPP study, or A1C increased to ≥ 7% in the DPPOS, study metformin was discontinued and management of the patient’s diabetes was transferred to their health care provider. By the end of the DPPOS, 53% of patients in the lifestyle group and 55% in the metformin group had progressed to T2D, compared with 60% in the placebo group (P = 0.003).
After a median 21-year follow-up interval, the investigators collected data on cause of death for patients and evaluated hazard ratios (HRs) for overall and cause-specific mortality. In total, 14% of the participants died, with no statistically significant difference in rates between the 3 groups. Cancer (37%) was the leading cause of death in all groups, followed by cardiovascular disease (CVD; 29%).
Compared with the placebo group, patients taking metformin did not have a decreased rate of overall mortality (HR = 0.99; 95% CI, 0.79-1.25), mortality from cancer (HR = 1.04; 95% CI, 0.72-1.52), or mortality due to CVD (HR = 1.08; 95% CI, 0.70-1.66). Similarly, compared with the placebo group, lifestyle intervention did not decrease overall mortality (HR = 1.02; 95% CI, 0.81-1.28), mortality from cancer (HR = 1.07; 95% CI, 0.74-1.55), or mortality due to CVD (HR = 1.18; 95% CI, 0.77-1.81). Results were similar when adjusted for other factors, including out-of-study metformin use, T2D status and duration, BMI change, and other cardiovascular risk factors.
WHAT’S NEW
Long-term data clarifylimits to interventions’ utility
This study looked at long-term follow-up data on mortality outcomes for patients with prediabetes treated with metformin or lifestyle intervention. Although these interventions did support weight loss, reduce the incidence of T2D, and lower cardiovascular risk factors (eg, hypertension, dyslipidemia), the comorbidity benefits did not affect risk for all-cause or cause-specific mortality, which were similar between the treatment and placebo groups.
Continue to: CAVEATS
CAVEATS
Exclusion criteria, residual confounding may limit the findings
Patients with significant cardiovascular or renal disease were excluded, so results may not apply to patients with these comorbidities. Additionally, there was a high amount of “drop-in” use of metformin prescribed by physicians once patients developed T2D, which may not have been controlled for completely. And while the intensive lifestyle intervention group had specific goals, the metformin and placebo groups also were encouraged to follow standard diet and lifestyle recommendations—and during a bridge period, all participants were offered a modified group lifestyle intervention. However, multivariable adjustment did not change the study conclusion.
CHALLENGES TO IMPLEMENTATION
Physicians may be unwilling to change their current prescribing habits
Physicians may not be willing to change their practice of prescribing metformin in prediabetes based on a singular study (with residual confounding) that showed no long-term mortality differences between the study groups. However, there may be long-term morbidity differences of interest to patients that were not specifically evaluated in this study—such as quality-of-life benefits from weight loss that may outweigh the risks (eg, gastrointestinal adverse effects such as diarrhea, nausea, and abdominal pain) of metformin for some patients. Therefore, a discussion of the risks and benefits of treatment for prediabetes should be had with patients at high risk who would prefer a pharmacologic intervention.
1. Lee CG, Heckman-Stoddard B, et al; Diabetes Prevention Program Research Group. Effect of metformin and lifestyle interventions on mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care. 2021;44:2775-2782. doi: 10.2337/dc21-1046
2. American Diabetes Association. Understanding A1C: diagnosis. Accessed July 6, 2023. https://diabetes.org/diabetes/a1c/diagnosis
3. CDC. National diabetes statistics report. Reviewed June 29, 2022. Accessed January 23, 2023. www.cdc.gov/diabetes/data/statistics-report/index.html
4. USPSTF; Davidson KW, Barry MJ, Mangione CM, et al. Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531
5. Hostalek U, Campbell I. Metformin for diabetes prevention: update of the evidence base. Curr Med Res Opin. 2021;37:1705-1717. doi: 10.1080/03007995.2021.1955667
6. Aroda VR, Knowler WC, Crandall JP, et al; Diabetes Prevention Program Research Group. Metformin for diabetes prevention: insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia. 2017;60:1601-1611. doi: 10.1007/s00125-017-4361-9
7. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512
8. Herman WH, Ratner RE. Metformin should be used to treat prediabetes in selected individuals. Diabetes Care. 2020;43:1988-1990. doi: 10.2337/dci20-0030
9. American Diabetes Association. 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(suppl 1):S34-S39. doi: 10.2337/dc21-S003
10. Tseng E, Yeh HC, Maruthur NM. Metformin use in prediabetes among US adults, 2005-2012. Diabetes Care. 2017;40:887-893. doi: 10.2337/dc16-1509
11. Davidson MB. Metformin should not be used to treat prediabetes. Diabetes Care. 2020;43:1983-1987. doi: 10.2337/dc19-2221
1. Lee CG, Heckman-Stoddard B, et al; Diabetes Prevention Program Research Group. Effect of metformin and lifestyle interventions on mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care. 2021;44:2775-2782. doi: 10.2337/dc21-1046
2. American Diabetes Association. Understanding A1C: diagnosis. Accessed July 6, 2023. https://diabetes.org/diabetes/a1c/diagnosis
3. CDC. National diabetes statistics report. Reviewed June 29, 2022. Accessed January 23, 2023. www.cdc.gov/diabetes/data/statistics-report/index.html
4. USPSTF; Davidson KW, Barry MJ, Mangione CM, et al. Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531
5. Hostalek U, Campbell I. Metformin for diabetes prevention: update of the evidence base. Curr Med Res Opin. 2021;37:1705-1717. doi: 10.1080/03007995.2021.1955667
6. Aroda VR, Knowler WC, Crandall JP, et al; Diabetes Prevention Program Research Group. Metformin for diabetes prevention: insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia. 2017;60:1601-1611. doi: 10.1007/s00125-017-4361-9
7. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512
8. Herman WH, Ratner RE. Metformin should be used to treat prediabetes in selected individuals. Diabetes Care. 2020;43:1988-1990. doi: 10.2337/dci20-0030
9. American Diabetes Association. 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(suppl 1):S34-S39. doi: 10.2337/dc21-S003
10. Tseng E, Yeh HC, Maruthur NM. Metformin use in prediabetes among US adults, 2005-2012. Diabetes Care. 2017;40:887-893. doi: 10.2337/dc16-1509
11. Davidson MB. Metformin should not be used to treat prediabetes. Diabetes Care. 2020;43:1983-1987. doi: 10.2337/dc19-2221
PRACTICE CHANGER
STRENGTH OF RECOMMENDATION
B: Based on a long-term follow-up of a randomized controlled trial.1
Lee CG, Heckman-Stoddard B, Dabelea D, et al; Diabetes Prevention Program Research Group. Effect of metformin and lifestyle interventions on mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care. 2021;44:2775-2782. doi: 10.2337/dc21-1046
Is injectable PrEP superior to oral therapy for HIV protection?
ILLUSTRATIVE CASE
A 24-year-old cisgender man with no significant past medical history comes to your office requesting PrEP after starting a new sexual relationship. His partner is a 26-year-old cisgender man with known HIV. The patient reports that balancing graduate school and work has made him very forgetful, and he worries that he won’t remember to take a daily pill. Are there any other PrEP methods you can offer?
The efficacy of PrEP to reduce HIV acquisition has been established across varying populations at high risk for transmission.1 PrEP has been found to reduce the risk for sexual acquisition of HIV by nearly 99%.2
Although the use of PrEP in the United States has increased steadily since 2012, adherence to an oral formulation remains a significant issue. One study of > 13,000 people found that daily oral PrEP was discontinued by 52% of participants, only 60% of whom reinitiated the therapy after discontinuation.2 Although the federal government has required Medicaid and other insurance providers to cover PrEP in an effort to increase access to the medication, this does not necessarily increase adherence to a daily medication in an often otherwise healthy population.
Long-acting injectable forms of PrEP, which have a reduced dosing frequency that may support adherence, have been studied to potentially replace daily oral pills. This latest study compared cabotegravir (CAB-LA), a long-acting IM injection given every 8 weeks, to daily oral PrEP with tenofovir disoproxil fumarate–emtricitabine (TDF-FTC).1
STUDY SUMMARY
Decreased seroconversion without daily pills
This randomized, double-blind, double-dummy, noninferiority trial compared long-acting injectable vs daily oral PrEP formulations for the prevention of HIV across an international population. Patients were randomized to receive either CAB-LA 600 mg IM every 8 weeks or TDF-FTC 300/200 mg orally daily. The double-dummy methodology meant that those patients receiving active CAB-LA also received a daily oral placebo, while those patients receiving active TDF-FTC also received a placebo injection every 8 weeks.
Study participants were cisgender MSM or transgender women who have sex with men; ages 18 years and older; and in good health but considered to be at high risk for HIV infection. To be included, participants had to have a negative HIV serologic test at enrollment, undetectable blood HIV RNA viral load within 14 days of enrollment, and creatinine clearance ≥ 60 mL/min. Exclusion criteria included intravenous (IV) drug use within 90 days of enrollment, coagulopathy, buttock implants or fillers, a seizure disorder, or a QTc interval > 500 ms.1
The intention-to-treat population included 4566 patients: 2282 in the CAB-LA group and 2284 in the TDF-FTC group. Demographic characteristics—including age, race, geographic region, and cohort (MSM vs transgender women)—were not significantly different between groups at baseline. The study lasted 153 weeks, and > 86% of patients were retained at 1 year (median follow-up, 1.4 years; interquartile range, 0.8-1.9).
Continue to: The primary efficacy and safety...
The primary efficacy and safety outcomes of interest were HIV infection and occurrence of a grade ≥ 2 adverse drug reaction, respectively. HIV seroconversion occurred in 13 of 2282 (0.57%) patients in the CAB-LA group and 39 of 2284 (1.7%) patients in the TDF-FTC group (hazard ratio = 0.34; 95% CI, 0.18-0.62). The rate of severe adverse drug reactions was similar between groups. The study was stopped early due to the superiority of CAB-LA.
WHAT’S NEW
Demonstrated superiority of injectable vs oral PrEP
The results of this study could have a monumental impact on the spread of HIV. Since adherence is a known limitation of daily oral PrEP, a long-acting injectable is an intriguing option. The 8-week period between injections offers convenience, allowing primary care physicians (PCPs) to schedule their patients in advance. And because every injection is administered in the office, this option would help PCPs track adherence. Witnessed adherence to the medication, and its demonstrated superiority, could have a significant effect on HIV prevention.
The limited serious adverse effects reported by both groups may ease some PCPs’ hesitation to prescribe CAB-LA.
CAVEATS
More injection-site reactions (but little impact on adherence)
Notably, 81.4% of patients in the CAB-LA group had injection-site reactions vs 31.3% in the TDF-FTC group. However, only 2.4% of patients in the CAB-LA group opted to stop receiving the injections because of these reactions.
Standard PrEP reduces the risk for HIV acquisition from IV drug use by 74%.2 However, because IV drug use was an exclusion criterion in this study, future research will need to assess CAB-LA’s effectiveness in that population.
CHALLENGES TO IMPLEMENTATION
Price and storage requirementsof CAB-LA may create issues
CAB-LA is expensive, costing more than $25,000 per year—significantly outpricing TDF-FTC, which costs approximately $8300 per year.3 Insurance coverage for PrEP, including CAB-LA, varies widely. Given the superiority reflected in this study, more efforts should be made to lower the cost of the medication.
Another hurdle for CAB-LA is that it requires refrigeration for storage. Although likely not an issue in most of the United States, it will make adoption of this method difficult in other parts of the world.
1. Landovitz RJ, Donnell D, Clement ME, et al; HPTN 083 Study Team. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385:595-608. doi: 10.1056/NEJMoa2101016
2. Hojilla JC, Hurley LB, Marcus JL, et al. Characterization of HIV preexposure prophylaxis use behaviors and HIV incidence among US adults in an integrated health care system. JAMA Netw Open. 2021;4:e2122692. doi: 10.1001/jamanetworkopen.2021.22692
3. Neilan AM, Landovitz RJ, Le MH, et al. Cost-effectiveness of long-acting injectable HIV preexposure prophylaxis in the United States: a cost-effectiveness analysis. Ann Intern Med. 2022;175:479-489. doi: 10.7326/M21-1548
ILLUSTRATIVE CASE
A 24-year-old cisgender man with no significant past medical history comes to your office requesting PrEP after starting a new sexual relationship. His partner is a 26-year-old cisgender man with known HIV. The patient reports that balancing graduate school and work has made him very forgetful, and he worries that he won’t remember to take a daily pill. Are there any other PrEP methods you can offer?
The efficacy of PrEP to reduce HIV acquisition has been established across varying populations at high risk for transmission.1 PrEP has been found to reduce the risk for sexual acquisition of HIV by nearly 99%.2
Although the use of PrEP in the United States has increased steadily since 2012, adherence to an oral formulation remains a significant issue. One study of > 13,000 people found that daily oral PrEP was discontinued by 52% of participants, only 60% of whom reinitiated the therapy after discontinuation.2 Although the federal government has required Medicaid and other insurance providers to cover PrEP in an effort to increase access to the medication, this does not necessarily increase adherence to a daily medication in an often otherwise healthy population.
Long-acting injectable forms of PrEP, which have a reduced dosing frequency that may support adherence, have been studied to potentially replace daily oral pills. This latest study compared cabotegravir (CAB-LA), a long-acting IM injection given every 8 weeks, to daily oral PrEP with tenofovir disoproxil fumarate–emtricitabine (TDF-FTC).1
STUDY SUMMARY
Decreased seroconversion without daily pills
This randomized, double-blind, double-dummy, noninferiority trial compared long-acting injectable vs daily oral PrEP formulations for the prevention of HIV across an international population. Patients were randomized to receive either CAB-LA 600 mg IM every 8 weeks or TDF-FTC 300/200 mg orally daily. The double-dummy methodology meant that those patients receiving active CAB-LA also received a daily oral placebo, while those patients receiving active TDF-FTC also received a placebo injection every 8 weeks.
Study participants were cisgender MSM or transgender women who have sex with men; ages 18 years and older; and in good health but considered to be at high risk for HIV infection. To be included, participants had to have a negative HIV serologic test at enrollment, undetectable blood HIV RNA viral load within 14 days of enrollment, and creatinine clearance ≥ 60 mL/min. Exclusion criteria included intravenous (IV) drug use within 90 days of enrollment, coagulopathy, buttock implants or fillers, a seizure disorder, or a QTc interval > 500 ms.1
The intention-to-treat population included 4566 patients: 2282 in the CAB-LA group and 2284 in the TDF-FTC group. Demographic characteristics—including age, race, geographic region, and cohort (MSM vs transgender women)—were not significantly different between groups at baseline. The study lasted 153 weeks, and > 86% of patients were retained at 1 year (median follow-up, 1.4 years; interquartile range, 0.8-1.9).
Continue to: The primary efficacy and safety...
The primary efficacy and safety outcomes of interest were HIV infection and occurrence of a grade ≥ 2 adverse drug reaction, respectively. HIV seroconversion occurred in 13 of 2282 (0.57%) patients in the CAB-LA group and 39 of 2284 (1.7%) patients in the TDF-FTC group (hazard ratio = 0.34; 95% CI, 0.18-0.62). The rate of severe adverse drug reactions was similar between groups. The study was stopped early due to the superiority of CAB-LA.
WHAT’S NEW
Demonstrated superiority of injectable vs oral PrEP
The results of this study could have a monumental impact on the spread of HIV. Since adherence is a known limitation of daily oral PrEP, a long-acting injectable is an intriguing option. The 8-week period between injections offers convenience, allowing primary care physicians (PCPs) to schedule their patients in advance. And because every injection is administered in the office, this option would help PCPs track adherence. Witnessed adherence to the medication, and its demonstrated superiority, could have a significant effect on HIV prevention.
The limited serious adverse effects reported by both groups may ease some PCPs’ hesitation to prescribe CAB-LA.
CAVEATS
More injection-site reactions (but little impact on adherence)
Notably, 81.4% of patients in the CAB-LA group had injection-site reactions vs 31.3% in the TDF-FTC group. However, only 2.4% of patients in the CAB-LA group opted to stop receiving the injections because of these reactions.
Standard PrEP reduces the risk for HIV acquisition from IV drug use by 74%.2 However, because IV drug use was an exclusion criterion in this study, future research will need to assess CAB-LA’s effectiveness in that population.
CHALLENGES TO IMPLEMENTATION
Price and storage requirementsof CAB-LA may create issues
CAB-LA is expensive, costing more than $25,000 per year—significantly outpricing TDF-FTC, which costs approximately $8300 per year.3 Insurance coverage for PrEP, including CAB-LA, varies widely. Given the superiority reflected in this study, more efforts should be made to lower the cost of the medication.
Another hurdle for CAB-LA is that it requires refrigeration for storage. Although likely not an issue in most of the United States, it will make adoption of this method difficult in other parts of the world.
ILLUSTRATIVE CASE
A 24-year-old cisgender man with no significant past medical history comes to your office requesting PrEP after starting a new sexual relationship. His partner is a 26-year-old cisgender man with known HIV. The patient reports that balancing graduate school and work has made him very forgetful, and he worries that he won’t remember to take a daily pill. Are there any other PrEP methods you can offer?
The efficacy of PrEP to reduce HIV acquisition has been established across varying populations at high risk for transmission.1 PrEP has been found to reduce the risk for sexual acquisition of HIV by nearly 99%.2
Although the use of PrEP in the United States has increased steadily since 2012, adherence to an oral formulation remains a significant issue. One study of > 13,000 people found that daily oral PrEP was discontinued by 52% of participants, only 60% of whom reinitiated the therapy after discontinuation.2 Although the federal government has required Medicaid and other insurance providers to cover PrEP in an effort to increase access to the medication, this does not necessarily increase adherence to a daily medication in an often otherwise healthy population.
Long-acting injectable forms of PrEP, which have a reduced dosing frequency that may support adherence, have been studied to potentially replace daily oral pills. This latest study compared cabotegravir (CAB-LA), a long-acting IM injection given every 8 weeks, to daily oral PrEP with tenofovir disoproxil fumarate–emtricitabine (TDF-FTC).1
STUDY SUMMARY
Decreased seroconversion without daily pills
This randomized, double-blind, double-dummy, noninferiority trial compared long-acting injectable vs daily oral PrEP formulations for the prevention of HIV across an international population. Patients were randomized to receive either CAB-LA 600 mg IM every 8 weeks or TDF-FTC 300/200 mg orally daily. The double-dummy methodology meant that those patients receiving active CAB-LA also received a daily oral placebo, while those patients receiving active TDF-FTC also received a placebo injection every 8 weeks.
Study participants were cisgender MSM or transgender women who have sex with men; ages 18 years and older; and in good health but considered to be at high risk for HIV infection. To be included, participants had to have a negative HIV serologic test at enrollment, undetectable blood HIV RNA viral load within 14 days of enrollment, and creatinine clearance ≥ 60 mL/min. Exclusion criteria included intravenous (IV) drug use within 90 days of enrollment, coagulopathy, buttock implants or fillers, a seizure disorder, or a QTc interval > 500 ms.1
The intention-to-treat population included 4566 patients: 2282 in the CAB-LA group and 2284 in the TDF-FTC group. Demographic characteristics—including age, race, geographic region, and cohort (MSM vs transgender women)—were not significantly different between groups at baseline. The study lasted 153 weeks, and > 86% of patients were retained at 1 year (median follow-up, 1.4 years; interquartile range, 0.8-1.9).
Continue to: The primary efficacy and safety...
The primary efficacy and safety outcomes of interest were HIV infection and occurrence of a grade ≥ 2 adverse drug reaction, respectively. HIV seroconversion occurred in 13 of 2282 (0.57%) patients in the CAB-LA group and 39 of 2284 (1.7%) patients in the TDF-FTC group (hazard ratio = 0.34; 95% CI, 0.18-0.62). The rate of severe adverse drug reactions was similar between groups. The study was stopped early due to the superiority of CAB-LA.
WHAT’S NEW
Demonstrated superiority of injectable vs oral PrEP
The results of this study could have a monumental impact on the spread of HIV. Since adherence is a known limitation of daily oral PrEP, a long-acting injectable is an intriguing option. The 8-week period between injections offers convenience, allowing primary care physicians (PCPs) to schedule their patients in advance. And because every injection is administered in the office, this option would help PCPs track adherence. Witnessed adherence to the medication, and its demonstrated superiority, could have a significant effect on HIV prevention.
The limited serious adverse effects reported by both groups may ease some PCPs’ hesitation to prescribe CAB-LA.
CAVEATS
More injection-site reactions (but little impact on adherence)
Notably, 81.4% of patients in the CAB-LA group had injection-site reactions vs 31.3% in the TDF-FTC group. However, only 2.4% of patients in the CAB-LA group opted to stop receiving the injections because of these reactions.
Standard PrEP reduces the risk for HIV acquisition from IV drug use by 74%.2 However, because IV drug use was an exclusion criterion in this study, future research will need to assess CAB-LA’s effectiveness in that population.
CHALLENGES TO IMPLEMENTATION
Price and storage requirementsof CAB-LA may create issues
CAB-LA is expensive, costing more than $25,000 per year—significantly outpricing TDF-FTC, which costs approximately $8300 per year.3 Insurance coverage for PrEP, including CAB-LA, varies widely. Given the superiority reflected in this study, more efforts should be made to lower the cost of the medication.
Another hurdle for CAB-LA is that it requires refrigeration for storage. Although likely not an issue in most of the United States, it will make adoption of this method difficult in other parts of the world.
1. Landovitz RJ, Donnell D, Clement ME, et al; HPTN 083 Study Team. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385:595-608. doi: 10.1056/NEJMoa2101016
2. Hojilla JC, Hurley LB, Marcus JL, et al. Characterization of HIV preexposure prophylaxis use behaviors and HIV incidence among US adults in an integrated health care system. JAMA Netw Open. 2021;4:e2122692. doi: 10.1001/jamanetworkopen.2021.22692
3. Neilan AM, Landovitz RJ, Le MH, et al. Cost-effectiveness of long-acting injectable HIV preexposure prophylaxis in the United States: a cost-effectiveness analysis. Ann Intern Med. 2022;175:479-489. doi: 10.7326/M21-1548
1. Landovitz RJ, Donnell D, Clement ME, et al; HPTN 083 Study Team. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385:595-608. doi: 10.1056/NEJMoa2101016
2. Hojilla JC, Hurley LB, Marcus JL, et al. Characterization of HIV preexposure prophylaxis use behaviors and HIV incidence among US adults in an integrated health care system. JAMA Netw Open. 2021;4:e2122692. doi: 10.1001/jamanetworkopen.2021.22692
3. Neilan AM, Landovitz RJ, Le MH, et al. Cost-effectiveness of long-acting injectable HIV preexposure prophylaxis in the United States: a cost-effectiveness analysis. Ann Intern Med. 2022;175:479-489. doi: 10.7326/M21-1548
PRACTICE CHANGER
Consider intramuscular (IM) injectable cabotegravir every 8 weeks for HIV preexposure prophylaxis (PrEP) in cisgender men who have sex with men (MSM) and in transgender women.
STRENGTH OF RECOMMENDATION
B: Based on a single randomized controlled trial.1
Landovitz RJ, Donnell D, Clement ME, et al; HPTN 083 Study Team. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385:595-608. doi: 10.1056/NEJMoa2101016
Acute Achilles tendon rupture: Skip the surgery?
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
PRACTICE CHANGER
For healthy patients ages 18 to 60 years with acute Achilles tendon rupture, consider nonoperative immobilization, which offered a benefit in function comparable to open-repair or minimally invasive surgery in this randomized controlled trial (RCT).
STRENGTH OF RECOMMENDATION
B: Based on a single RCT.1
Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447