User login
Therese Borden is the editor of CHEST Physician. After 20 years of research, writing, and editing in the field of international development and economics, she began working in the field of medical editing and has held a variety of editorial positions with the company. She holds a PhD in International Economics from American University, Washington, and a BA in history from the University of Washington, Seattle.
Don’t delay palliative care for IPF patients
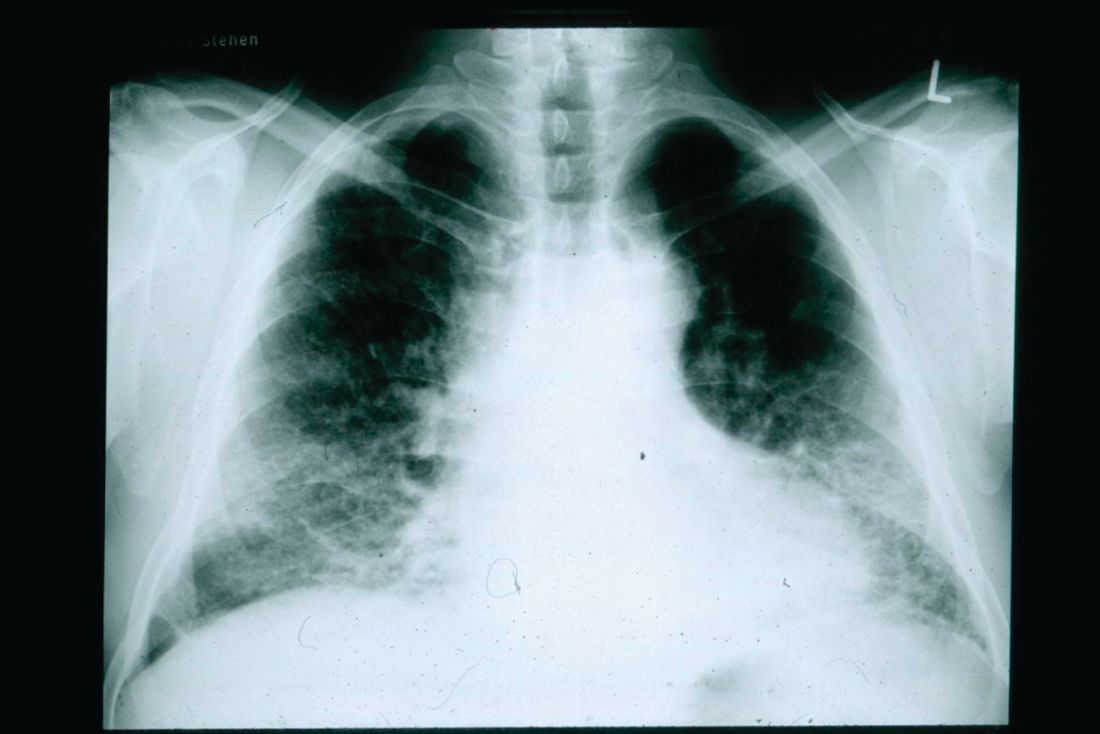
and indicates that early, integrated palliative care should be a priority, according to the finding of a survey study.
“Patients with IPF suffer from exceptionally low [health-related quality of life] together with severe breathlessness and fatigue already two years before death. In addition, physical and emotional well-being further deteriorates near death concurrently with escalating overall symptom burden,” wrote Kaisa Rajala, MD, and her colleagues at Helsinki University Hospital.
They conducted a substudy of patients in the larger FinnishIPF study to assess health-related quality of life (HRQOL) and symptom burden in the period before death. Among 300 patients invited to participate, 247 agreed. Patient disease and sociodemographic data were collected from the FinnishIPF records and the study group completed questionnaires five times at 6 month intervals. The study began in April 2015 and continued until August 2017, by which time 92 (37%) of the patients had died (BMC Pulmonary Medicine 2018;18:172; doi: 0.1186/s12890-018-0738-x).
The investigators used self-reporting tools to look at HRQOL and symptom burden: RAND 36-item Health Survey (RAND-36), the Modified Medical Research and Council Dyspnea Scale (MMRC), the Modified Edmonton Symptom Assessment Scale (ESAS), and the Numeric Rating Scale (NRS).
About 35% of these patients were being treated with antifibrotic medication. Most of the patients had comorbidities, with cardiovascular disease being the most common.
The dimensions of HRQOL studied were physical function, general health, vitality, mental health, social function, and bodily pain. These patients experienced a gradual impairment in HRQOL similar to that of patients with chronic obstructive pulmonary disease, but with a pronounced, rapid deterioration beginning in the last 2 years of life.
The symptom burden also intensified in the last 2 years of life and ramped up significantly in the last 6 months before death. NRS scores are on a scale of 0-10, from no symptoms to worst symptoms. In most clinical situations, NRS scores equal to greater than 4 trigger more comprehensive symptom assessment. The scores for symptoms for these patients during the last 6 months were dyspnea, 7.1 (standard deviation 2.8); tiredness, 6.0 (SD 2.5), cough, 5.0 (SD 3.5), pain with movement, 3.9 (SD 3.1), insomnia, 3.9 (SD 2.9), anxiety, 3.9 (SD 2.9), and depression, 3.6 (SD 3.1).
Investigators noted the steep change in the proportion of patients with MMRC scores greater than or equal to 3 (needing to stop walking after approximately 100 m or a few minutes because of breathlessness) beginning in the last 2 years of life.
The study limitations are its relatively small size, the self-reported data, and the lack of lung function measurements in most patients in the last 6 months of life.
The findings point to the urgent need for early palliative care in IPF patients, the investigators concluded. They noted that the sharp decline in HRQOL is similar to that seen in lung cancer patients, in contrast to the more gradual trend seen in COPD patients.
But there are common benefits of an early palliative program for all of these patients, they stressed. “Early integrated palliative care for patients with lung cancer has shown substantial benefits, such as lower depression scores, higher HRQOL, better communication of end-of-life care preferences, less aggressive care at the end of life, and longer overall survival. Similarly, a randomized trial demonstrated better control of dyspnea and a survival benefit with integrated palliative care in patients with COPD and interstitial lung disease. In addition to cancer patients, early integrated palliative care may reduce end-of-life acute care utilization, and allow patients with IPF to die in their preferred locations. Integrated palliative care in IPF patients seems to lower respiratory-related emergency room visits and hospitalizations and may allow more patients to die at home.”
The study was funded by The Academy of Finland and various Finnish nonprofit organizations funded the study.
SOURCE: Rajala K et al. BMC Pulm Med. 2018;18:172. doi: 0.1186/s12890-018-0738-x.
and indicates that early, integrated palliative care should be a priority, according to the finding of a survey study.
“Patients with IPF suffer from exceptionally low [health-related quality of life] together with severe breathlessness and fatigue already two years before death. In addition, physical and emotional well-being further deteriorates near death concurrently with escalating overall symptom burden,” wrote Kaisa Rajala, MD, and her colleagues at Helsinki University Hospital.
They conducted a substudy of patients in the larger FinnishIPF study to assess health-related quality of life (HRQOL) and symptom burden in the period before death. Among 300 patients invited to participate, 247 agreed. Patient disease and sociodemographic data were collected from the FinnishIPF records and the study group completed questionnaires five times at 6 month intervals. The study began in April 2015 and continued until August 2017, by which time 92 (37%) of the patients had died (BMC Pulmonary Medicine 2018;18:172; doi: 0.1186/s12890-018-0738-x).
The investigators used self-reporting tools to look at HRQOL and symptom burden: RAND 36-item Health Survey (RAND-36), the Modified Medical Research and Council Dyspnea Scale (MMRC), the Modified Edmonton Symptom Assessment Scale (ESAS), and the Numeric Rating Scale (NRS).
About 35% of these patients were being treated with antifibrotic medication. Most of the patients had comorbidities, with cardiovascular disease being the most common.
The dimensions of HRQOL studied were physical function, general health, vitality, mental health, social function, and bodily pain. These patients experienced a gradual impairment in HRQOL similar to that of patients with chronic obstructive pulmonary disease, but with a pronounced, rapid deterioration beginning in the last 2 years of life.
The symptom burden also intensified in the last 2 years of life and ramped up significantly in the last 6 months before death. NRS scores are on a scale of 0-10, from no symptoms to worst symptoms. In most clinical situations, NRS scores equal to greater than 4 trigger more comprehensive symptom assessment. The scores for symptoms for these patients during the last 6 months were dyspnea, 7.1 (standard deviation 2.8); tiredness, 6.0 (SD 2.5), cough, 5.0 (SD 3.5), pain with movement, 3.9 (SD 3.1), insomnia, 3.9 (SD 2.9), anxiety, 3.9 (SD 2.9), and depression, 3.6 (SD 3.1).
Investigators noted the steep change in the proportion of patients with MMRC scores greater than or equal to 3 (needing to stop walking after approximately 100 m or a few minutes because of breathlessness) beginning in the last 2 years of life.
The study limitations are its relatively small size, the self-reported data, and the lack of lung function measurements in most patients in the last 6 months of life.
The findings point to the urgent need for early palliative care in IPF patients, the investigators concluded. They noted that the sharp decline in HRQOL is similar to that seen in lung cancer patients, in contrast to the more gradual trend seen in COPD patients.
But there are common benefits of an early palliative program for all of these patients, they stressed. “Early integrated palliative care for patients with lung cancer has shown substantial benefits, such as lower depression scores, higher HRQOL, better communication of end-of-life care preferences, less aggressive care at the end of life, and longer overall survival. Similarly, a randomized trial demonstrated better control of dyspnea and a survival benefit with integrated palliative care in patients with COPD and interstitial lung disease. In addition to cancer patients, early integrated palliative care may reduce end-of-life acute care utilization, and allow patients with IPF to die in their preferred locations. Integrated palliative care in IPF patients seems to lower respiratory-related emergency room visits and hospitalizations and may allow more patients to die at home.”
The study was funded by The Academy of Finland and various Finnish nonprofit organizations funded the study.
SOURCE: Rajala K et al. BMC Pulm Med. 2018;18:172. doi: 0.1186/s12890-018-0738-x.
and indicates that early, integrated palliative care should be a priority, according to the finding of a survey study.
“Patients with IPF suffer from exceptionally low [health-related quality of life] together with severe breathlessness and fatigue already two years before death. In addition, physical and emotional well-being further deteriorates near death concurrently with escalating overall symptom burden,” wrote Kaisa Rajala, MD, and her colleagues at Helsinki University Hospital.
They conducted a substudy of patients in the larger FinnishIPF study to assess health-related quality of life (HRQOL) and symptom burden in the period before death. Among 300 patients invited to participate, 247 agreed. Patient disease and sociodemographic data were collected from the FinnishIPF records and the study group completed questionnaires five times at 6 month intervals. The study began in April 2015 and continued until August 2017, by which time 92 (37%) of the patients had died (BMC Pulmonary Medicine 2018;18:172; doi: 0.1186/s12890-018-0738-x).
The investigators used self-reporting tools to look at HRQOL and symptom burden: RAND 36-item Health Survey (RAND-36), the Modified Medical Research and Council Dyspnea Scale (MMRC), the Modified Edmonton Symptom Assessment Scale (ESAS), and the Numeric Rating Scale (NRS).
About 35% of these patients were being treated with antifibrotic medication. Most of the patients had comorbidities, with cardiovascular disease being the most common.
The dimensions of HRQOL studied were physical function, general health, vitality, mental health, social function, and bodily pain. These patients experienced a gradual impairment in HRQOL similar to that of patients with chronic obstructive pulmonary disease, but with a pronounced, rapid deterioration beginning in the last 2 years of life.
The symptom burden also intensified in the last 2 years of life and ramped up significantly in the last 6 months before death. NRS scores are on a scale of 0-10, from no symptoms to worst symptoms. In most clinical situations, NRS scores equal to greater than 4 trigger more comprehensive symptom assessment. The scores for symptoms for these patients during the last 6 months were dyspnea, 7.1 (standard deviation 2.8); tiredness, 6.0 (SD 2.5), cough, 5.0 (SD 3.5), pain with movement, 3.9 (SD 3.1), insomnia, 3.9 (SD 2.9), anxiety, 3.9 (SD 2.9), and depression, 3.6 (SD 3.1).
Investigators noted the steep change in the proportion of patients with MMRC scores greater than or equal to 3 (needing to stop walking after approximately 100 m or a few minutes because of breathlessness) beginning in the last 2 years of life.
The study limitations are its relatively small size, the self-reported data, and the lack of lung function measurements in most patients in the last 6 months of life.
The findings point to the urgent need for early palliative care in IPF patients, the investigators concluded. They noted that the sharp decline in HRQOL is similar to that seen in lung cancer patients, in contrast to the more gradual trend seen in COPD patients.
But there are common benefits of an early palliative program for all of these patients, they stressed. “Early integrated palliative care for patients with lung cancer has shown substantial benefits, such as lower depression scores, higher HRQOL, better communication of end-of-life care preferences, less aggressive care at the end of life, and longer overall survival. Similarly, a randomized trial demonstrated better control of dyspnea and a survival benefit with integrated palliative care in patients with COPD and interstitial lung disease. In addition to cancer patients, early integrated palliative care may reduce end-of-life acute care utilization, and allow patients with IPF to die in their preferred locations. Integrated palliative care in IPF patients seems to lower respiratory-related emergency room visits and hospitalizations and may allow more patients to die at home.”
The study was funded by The Academy of Finland and various Finnish nonprofit organizations funded the study.
SOURCE: Rajala K et al. BMC Pulm Med. 2018;18:172. doi: 0.1186/s12890-018-0738-x.
FROM BMC PULMONARY MEDICINE
Pregnancy after ventral hernia repair increased the risk for recurrence
concluded the authors of a systematic review of the literature on hernia and pregnancy.
Erling Omoa, MD, of Bispebjerg Hospital and the University of Copenhagen, and his colleagues surveyed 5,189 articles and chose four cohort studies, four case-control studies, and one case-series study that met their criteria of quality, comparability, and outcomes data. Only randomized, controlled trials, analytical observational studies, and large case series were included. The focus was primary ventral (umbilical and epigastric) and incisional hernia surgery before, during, and after pregnancy.
“The prevalence of clinically relevant primary ventral hernias is very low during pregnancy,” the investigators wrote, but there is a lack on consensus concerning the management of hernia repair in women of childbearing age. “The objective of this systematic review was to examine the risk of recurrence following prepregnancy ventral hernia repair, and secondly, to evaluate the prevalence of ventral hernia during pregnancy and the risk of surgical repair before and after childbirth,” they wrote.
The reviewers evaluated pregnancy following ventral hernia repair as a potential risk factor for hernia recurrence. One study found that subsequent pregnancy was associated with a 1.6-fold increased risk of recurrence. Another found that pregnancy was independently associated with a 73% raised risk of recurrence. The risk of recurrence was no different between mesh and suture repair.
The review found the prevalence of primary ventral and inguinal repair during pregnancy to be low. A single-center cohort study of 20,714 pregnant women of which 17 (0.08%) had umbilical hernias and none of these required repair before delivery. A case series of 126 women who underwent this surgery during pregnancy indicated that this procedure was associated with minimal 30-day morbidity and no deaths. No data was available on fetal morbidity or recurrence in this case series.
Case-control studies reporting on umbilical repair concomitant with elective C-section found that, although adding hernia repair to the procedure increased operative time in some studies, there was no additional complication risk.
Overall, the investigators found several areas in which evidence remains weak, such as the long-term risks for recurrence following pregnancy and long-term outcomes of mesh versus suture repairs. They recommended that patients be counseled on the risk of recurrence linked to subsequent pregnancies and that, if possible, ventral hernia repair should be postponed until after a last planned pregnancy. Watchful waiting until after a delivery was deemed safe in many cases.
The investigators reported no conflicts.
SOURCE: Oma E et al. Am J Surg. 2019 Jan;217:163-8.
concluded the authors of a systematic review of the literature on hernia and pregnancy.
Erling Omoa, MD, of Bispebjerg Hospital and the University of Copenhagen, and his colleagues surveyed 5,189 articles and chose four cohort studies, four case-control studies, and one case-series study that met their criteria of quality, comparability, and outcomes data. Only randomized, controlled trials, analytical observational studies, and large case series were included. The focus was primary ventral (umbilical and epigastric) and incisional hernia surgery before, during, and after pregnancy.
“The prevalence of clinically relevant primary ventral hernias is very low during pregnancy,” the investigators wrote, but there is a lack on consensus concerning the management of hernia repair in women of childbearing age. “The objective of this systematic review was to examine the risk of recurrence following prepregnancy ventral hernia repair, and secondly, to evaluate the prevalence of ventral hernia during pregnancy and the risk of surgical repair before and after childbirth,” they wrote.
The reviewers evaluated pregnancy following ventral hernia repair as a potential risk factor for hernia recurrence. One study found that subsequent pregnancy was associated with a 1.6-fold increased risk of recurrence. Another found that pregnancy was independently associated with a 73% raised risk of recurrence. The risk of recurrence was no different between mesh and suture repair.
The review found the prevalence of primary ventral and inguinal repair during pregnancy to be low. A single-center cohort study of 20,714 pregnant women of which 17 (0.08%) had umbilical hernias and none of these required repair before delivery. A case series of 126 women who underwent this surgery during pregnancy indicated that this procedure was associated with minimal 30-day morbidity and no deaths. No data was available on fetal morbidity or recurrence in this case series.
Case-control studies reporting on umbilical repair concomitant with elective C-section found that, although adding hernia repair to the procedure increased operative time in some studies, there was no additional complication risk.
Overall, the investigators found several areas in which evidence remains weak, such as the long-term risks for recurrence following pregnancy and long-term outcomes of mesh versus suture repairs. They recommended that patients be counseled on the risk of recurrence linked to subsequent pregnancies and that, if possible, ventral hernia repair should be postponed until after a last planned pregnancy. Watchful waiting until after a delivery was deemed safe in many cases.
The investigators reported no conflicts.
SOURCE: Oma E et al. Am J Surg. 2019 Jan;217:163-8.
concluded the authors of a systematic review of the literature on hernia and pregnancy.
Erling Omoa, MD, of Bispebjerg Hospital and the University of Copenhagen, and his colleagues surveyed 5,189 articles and chose four cohort studies, four case-control studies, and one case-series study that met their criteria of quality, comparability, and outcomes data. Only randomized, controlled trials, analytical observational studies, and large case series were included. The focus was primary ventral (umbilical and epigastric) and incisional hernia surgery before, during, and after pregnancy.
“The prevalence of clinically relevant primary ventral hernias is very low during pregnancy,” the investigators wrote, but there is a lack on consensus concerning the management of hernia repair in women of childbearing age. “The objective of this systematic review was to examine the risk of recurrence following prepregnancy ventral hernia repair, and secondly, to evaluate the prevalence of ventral hernia during pregnancy and the risk of surgical repair before and after childbirth,” they wrote.
The reviewers evaluated pregnancy following ventral hernia repair as a potential risk factor for hernia recurrence. One study found that subsequent pregnancy was associated with a 1.6-fold increased risk of recurrence. Another found that pregnancy was independently associated with a 73% raised risk of recurrence. The risk of recurrence was no different between mesh and suture repair.
The review found the prevalence of primary ventral and inguinal repair during pregnancy to be low. A single-center cohort study of 20,714 pregnant women of which 17 (0.08%) had umbilical hernias and none of these required repair before delivery. A case series of 126 women who underwent this surgery during pregnancy indicated that this procedure was associated with minimal 30-day morbidity and no deaths. No data was available on fetal morbidity or recurrence in this case series.
Case-control studies reporting on umbilical repair concomitant with elective C-section found that, although adding hernia repair to the procedure increased operative time in some studies, there was no additional complication risk.
Overall, the investigators found several areas in which evidence remains weak, such as the long-term risks for recurrence following pregnancy and long-term outcomes of mesh versus suture repairs. They recommended that patients be counseled on the risk of recurrence linked to subsequent pregnancies and that, if possible, ventral hernia repair should be postponed until after a last planned pregnancy. Watchful waiting until after a delivery was deemed safe in many cases.
The investigators reported no conflicts.
SOURCE: Oma E et al. Am J Surg. 2019 Jan;217:163-8.
FROM THE AMERICAN JOURNAL OF SURGERY
Clinical trial: Randomized study of lap vs. robotic hernia surgery underway
A multicenter, randomized study comparing
In the trial precis, the researchers wrote, “The robotic platform in surgery is growing exponentially. Despite this, the evidence supporting robotics remains limited. Studies demonstrating benefit, such as improved outcomes or decreased hospital length of stay, are largely cohort studies subject to substantial bias. Among randomized controlled trials, none have demonstrated benefit with robotic surgery.”
Study participants will be randomized to two arms, one for laparoscopic hernia repair and the other for robotic repair. Patients in both arms will be treated with a mid-density polypropylene mesh with a one-sided adhesion barrier.
The primary outcomes studied are length of stay in the hospital and readmissions out to 90 days. Secondary outcomes include the occurrence of surgical-site infection, hematoma, seroma, dehiscence, necrosis, nonhealing wound, hernia recurrence, and several cost and quality-of-life measures.
Patients included must be over age 18 and undergoing elective ventral hernia repair deemed appropriate for minimally invasive repair. Exclusions include those unlikely to survive beyond 2 years based on surgeon judgment or are unlikely to follow up. In addition, patients are excluded if they have advanced COPD or heart failure, a history of open abdomen or extensive lysis of adhesions for bowel obstruction, ascites caused by cirrhosis or malignancy, active infection, or a large hernia larger than 12 cm. Estimated enrollment is 120 patients, and the researchers expect the study to end in 2023.
For more details on the study (NT03490266), go to clinicaltrials.gov.
A multicenter, randomized study comparing
In the trial precis, the researchers wrote, “The robotic platform in surgery is growing exponentially. Despite this, the evidence supporting robotics remains limited. Studies demonstrating benefit, such as improved outcomes or decreased hospital length of stay, are largely cohort studies subject to substantial bias. Among randomized controlled trials, none have demonstrated benefit with robotic surgery.”
Study participants will be randomized to two arms, one for laparoscopic hernia repair and the other for robotic repair. Patients in both arms will be treated with a mid-density polypropylene mesh with a one-sided adhesion barrier.
The primary outcomes studied are length of stay in the hospital and readmissions out to 90 days. Secondary outcomes include the occurrence of surgical-site infection, hematoma, seroma, dehiscence, necrosis, nonhealing wound, hernia recurrence, and several cost and quality-of-life measures.
Patients included must be over age 18 and undergoing elective ventral hernia repair deemed appropriate for minimally invasive repair. Exclusions include those unlikely to survive beyond 2 years based on surgeon judgment or are unlikely to follow up. In addition, patients are excluded if they have advanced COPD or heart failure, a history of open abdomen or extensive lysis of adhesions for bowel obstruction, ascites caused by cirrhosis or malignancy, active infection, or a large hernia larger than 12 cm. Estimated enrollment is 120 patients, and the researchers expect the study to end in 2023.
For more details on the study (NT03490266), go to clinicaltrials.gov.
A multicenter, randomized study comparing
In the trial precis, the researchers wrote, “The robotic platform in surgery is growing exponentially. Despite this, the evidence supporting robotics remains limited. Studies demonstrating benefit, such as improved outcomes or decreased hospital length of stay, are largely cohort studies subject to substantial bias. Among randomized controlled trials, none have demonstrated benefit with robotic surgery.”
Study participants will be randomized to two arms, one for laparoscopic hernia repair and the other for robotic repair. Patients in both arms will be treated with a mid-density polypropylene mesh with a one-sided adhesion barrier.
The primary outcomes studied are length of stay in the hospital and readmissions out to 90 days. Secondary outcomes include the occurrence of surgical-site infection, hematoma, seroma, dehiscence, necrosis, nonhealing wound, hernia recurrence, and several cost and quality-of-life measures.
Patients included must be over age 18 and undergoing elective ventral hernia repair deemed appropriate for minimally invasive repair. Exclusions include those unlikely to survive beyond 2 years based on surgeon judgment or are unlikely to follow up. In addition, patients are excluded if they have advanced COPD or heart failure, a history of open abdomen or extensive lysis of adhesions for bowel obstruction, ascites caused by cirrhosis or malignancy, active infection, or a large hernia larger than 12 cm. Estimated enrollment is 120 patients, and the researchers expect the study to end in 2023.
For more details on the study (NT03490266), go to clinicaltrials.gov.
ALA report: Federal and state actions to limit tobacco use fall short
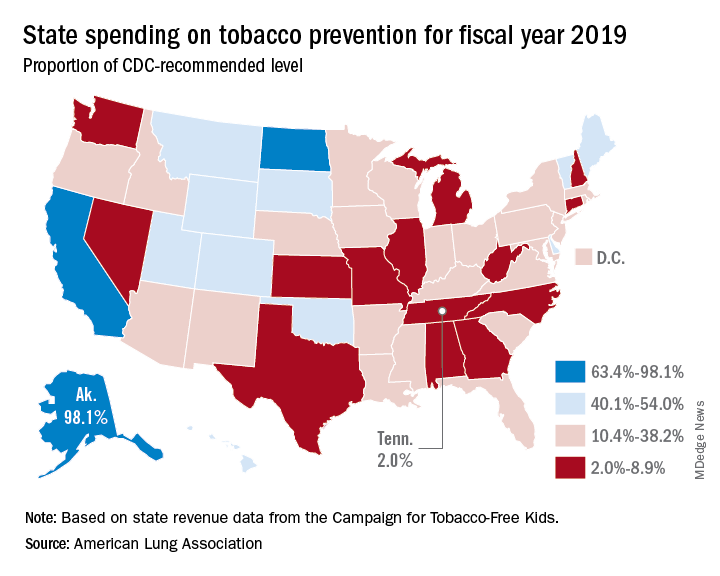
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
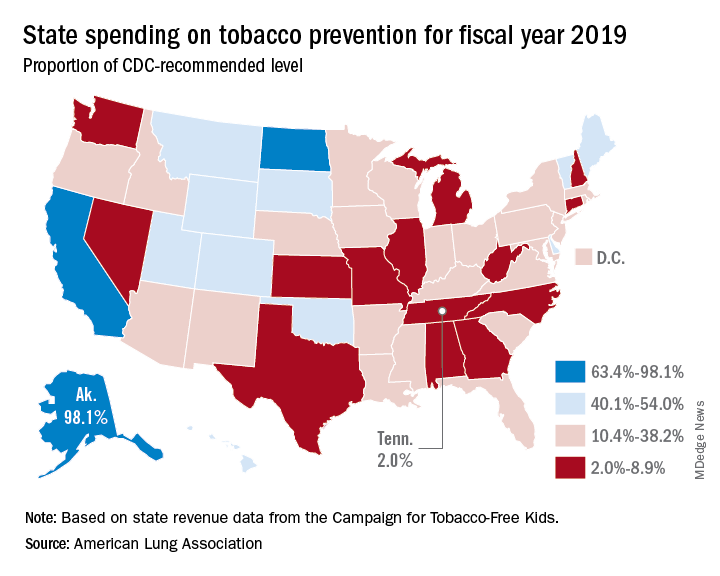
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
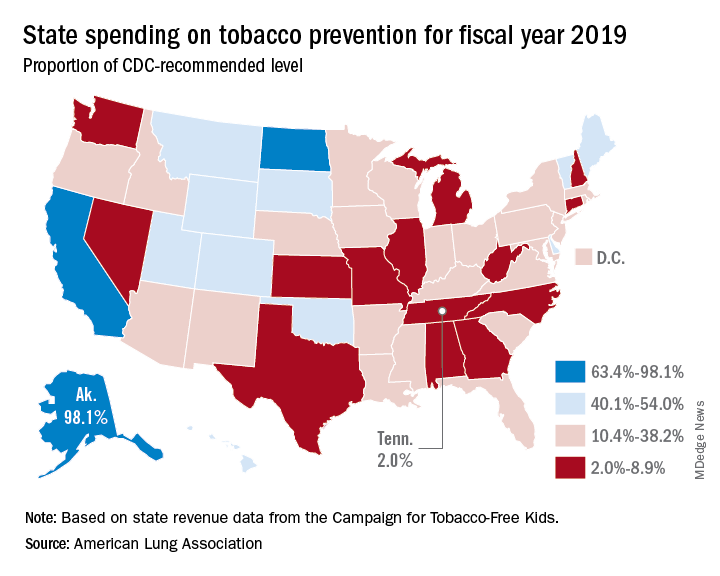
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Clinical trial: AVATaR studies pulmonary complications following robotic surgery
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
Sleep disorders in children with ADHD treated with off-label medications
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
FROM THE JOURNAL OF PEDIATRIC HEALTH CARE
Key clinical point: The most commonly prescribed off-label medications prescribed to children were trazodone (5,190), hydroxyzine (2,539), quetiapine (2,402), and clonazepam (2,145).
Major finding: Most of the prescriptions (63.8%) went to older children aged 12-18 years, and most prescriptions (66.3%) went to males.
Study details: Medicaid claims data for Jan. 1, 2012, to Dec. 31, 2016, yielding 14,567 prescriptions of off-label medications for 2,518 children.
Disclosures: The investigators reported no disclosures.
Source: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Clinical trial: Surgical glue for hernia repair
A observational, prospective trial is underway to study the use of Cyanoacrylate Fixation for Laparoscopic Repair of Inguinal Hernias, a multicenter registry, is currently enrolling patients for laparoscopic inguinal hernia repair using surgical tissue glue for mesh fixation.
The trial expects to enroll 1,000 patients and to be completed by December 2019. The primary outcome is postoperative pain evaluated by patient self-assessment using a visual analog scale. Secondary outcomes include intraoperative and postoperative complications, analgesic intake, postoperative quality of life, recurrences, and longer-term complications.
Included in the participant group are adult patients of both sexes with primary inguinal hernia. Exclusions include patients with recurrent inguinal hernia, patients previously treated with Lichtenstein technique, those allergic to the components of the tissue glue, and those whose life expectancy is under 1 year. The patients will be followed up to 1 year.
For further information about to the study, go to clinicaltrials.gov (NCT01669837).
A observational, prospective trial is underway to study the use of Cyanoacrylate Fixation for Laparoscopic Repair of Inguinal Hernias, a multicenter registry, is currently enrolling patients for laparoscopic inguinal hernia repair using surgical tissue glue for mesh fixation.
The trial expects to enroll 1,000 patients and to be completed by December 2019. The primary outcome is postoperative pain evaluated by patient self-assessment using a visual analog scale. Secondary outcomes include intraoperative and postoperative complications, analgesic intake, postoperative quality of life, recurrences, and longer-term complications.
Included in the participant group are adult patients of both sexes with primary inguinal hernia. Exclusions include patients with recurrent inguinal hernia, patients previously treated with Lichtenstein technique, those allergic to the components of the tissue glue, and those whose life expectancy is under 1 year. The patients will be followed up to 1 year.
For further information about to the study, go to clinicaltrials.gov (NCT01669837).
A observational, prospective trial is underway to study the use of Cyanoacrylate Fixation for Laparoscopic Repair of Inguinal Hernias, a multicenter registry, is currently enrolling patients for laparoscopic inguinal hernia repair using surgical tissue glue for mesh fixation.
The trial expects to enroll 1,000 patients and to be completed by December 2019. The primary outcome is postoperative pain evaluated by patient self-assessment using a visual analog scale. Secondary outcomes include intraoperative and postoperative complications, analgesic intake, postoperative quality of life, recurrences, and longer-term complications.
Included in the participant group are adult patients of both sexes with primary inguinal hernia. Exclusions include patients with recurrent inguinal hernia, patients previously treated with Lichtenstein technique, those allergic to the components of the tissue glue, and those whose life expectancy is under 1 year. The patients will be followed up to 1 year.
For further information about to the study, go to clinicaltrials.gov (NCT01669837).
Recommended reading: Board picks the ‘best of 2018’
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
Robotic vs. conventional laparoscopic surgery for rectal cancer: No winner yet
Robot-assisted rectal surgery is gaining acceptance but, with some exceptions, outcomes are not significantly improved over the conventional laparoscopic approach, a meta-analysis has found.
Conducted by Katie Jones, MD, and her colleagues at Brighton and Sussex (England) University Hospital NHS Trust, the meta-analysis was designed as a follow-up to ROLARR (isrctn.org ID: ISRCTN80500123), a randomized clinical trial in which robot-assisted and. conventional laparoscopic surgery for rectal cancer were studied for risk of conversion to open surgery. That trial findings showed that robot-assisted laparoscopic surgery did not significantly reduce the risk of conversion. For other outcomes (pathology, complications, bladder, and sexual function), the differences between the two approaches were insignificant. But the two surgical approaches did differ on cost: The robot-assisted operation was significantly more expensive than the conventional laparoscopic procedure.
Dr. Jones and her colleagues analyzed data from ROLARR in the context of 27 other qualifying studies and confirmed many of the ROLARR findings. The 27 case control studies comprised 5,547 patients and had comparable outcomes data.
The outcomes of interest were duration of operation, conversion risk, blood loss, length of stay, oncological outcomes, time to first flatus, reoperation rate, postoperative morbidity, and postoperative mortality.
The investigators found that duration of the operation was longer for the robot-assisted procedure, compared with the conventional laparoscopic approach, though this difference was not statistically significant (z = 1.28, P = .20), and blood loss, morbidity, and mortality were similar between the two groups. Oncological outcomes (risk of positive circumferential resection margins, lymph node yield, and length of distal resection margins) were similar for these two surgical approaches.
In contrast to the ROLARR findings, this meta-analysis found that the risk of conversion favored the robot-assisted procedure (z = 5.51, P = .00001). Hospital stay (z = 2.46, P = 01) and time to first flatus outcomes (z = 3.09, P = .002) favored the robot-assisted procedure. Postop morbidity and mortality and reoperation rate were similar in the two groups.
“Based upon the findings of this largest-ever series on the role of robotic surgery in rectal cancer resection, the [robot-assisted procedure] is certainly a feasible technique and oncologically safe surgical intervention but failed to demonstrate any superiority over [the conventional laparoscopic approach] for many surgical outcomes,” the investigators wrote. “Mere advantage of robotic surgery was noted in only three postoperative outcomes, that is early passage of flatus, lower risk of conversion, and shorter hospitalization.”
Dr. Jones and her colleagues declared they had no conflicts of interest.
SOURCE: Jones K et al. World J Gastroentrol. 2018 Nov 15. doi: 10.4251/wjgo.v10.i11.449.
Robot-assisted rectal surgery is gaining acceptance but, with some exceptions, outcomes are not significantly improved over the conventional laparoscopic approach, a meta-analysis has found.
Conducted by Katie Jones, MD, and her colleagues at Brighton and Sussex (England) University Hospital NHS Trust, the meta-analysis was designed as a follow-up to ROLARR (isrctn.org ID: ISRCTN80500123), a randomized clinical trial in which robot-assisted and. conventional laparoscopic surgery for rectal cancer were studied for risk of conversion to open surgery. That trial findings showed that robot-assisted laparoscopic surgery did not significantly reduce the risk of conversion. For other outcomes (pathology, complications, bladder, and sexual function), the differences between the two approaches were insignificant. But the two surgical approaches did differ on cost: The robot-assisted operation was significantly more expensive than the conventional laparoscopic procedure.
Dr. Jones and her colleagues analyzed data from ROLARR in the context of 27 other qualifying studies and confirmed many of the ROLARR findings. The 27 case control studies comprised 5,547 patients and had comparable outcomes data.
The outcomes of interest were duration of operation, conversion risk, blood loss, length of stay, oncological outcomes, time to first flatus, reoperation rate, postoperative morbidity, and postoperative mortality.
The investigators found that duration of the operation was longer for the robot-assisted procedure, compared with the conventional laparoscopic approach, though this difference was not statistically significant (z = 1.28, P = .20), and blood loss, morbidity, and mortality were similar between the two groups. Oncological outcomes (risk of positive circumferential resection margins, lymph node yield, and length of distal resection margins) were similar for these two surgical approaches.
In contrast to the ROLARR findings, this meta-analysis found that the risk of conversion favored the robot-assisted procedure (z = 5.51, P = .00001). Hospital stay (z = 2.46, P = 01) and time to first flatus outcomes (z = 3.09, P = .002) favored the robot-assisted procedure. Postop morbidity and mortality and reoperation rate were similar in the two groups.
“Based upon the findings of this largest-ever series on the role of robotic surgery in rectal cancer resection, the [robot-assisted procedure] is certainly a feasible technique and oncologically safe surgical intervention but failed to demonstrate any superiority over [the conventional laparoscopic approach] for many surgical outcomes,” the investigators wrote. “Mere advantage of robotic surgery was noted in only three postoperative outcomes, that is early passage of flatus, lower risk of conversion, and shorter hospitalization.”
Dr. Jones and her colleagues declared they had no conflicts of interest.
SOURCE: Jones K et al. World J Gastroentrol. 2018 Nov 15. doi: 10.4251/wjgo.v10.i11.449.
Robot-assisted rectal surgery is gaining acceptance but, with some exceptions, outcomes are not significantly improved over the conventional laparoscopic approach, a meta-analysis has found.
Conducted by Katie Jones, MD, and her colleagues at Brighton and Sussex (England) University Hospital NHS Trust, the meta-analysis was designed as a follow-up to ROLARR (isrctn.org ID: ISRCTN80500123), a randomized clinical trial in which robot-assisted and. conventional laparoscopic surgery for rectal cancer were studied for risk of conversion to open surgery. That trial findings showed that robot-assisted laparoscopic surgery did not significantly reduce the risk of conversion. For other outcomes (pathology, complications, bladder, and sexual function), the differences between the two approaches were insignificant. But the two surgical approaches did differ on cost: The robot-assisted operation was significantly more expensive than the conventional laparoscopic procedure.
Dr. Jones and her colleagues analyzed data from ROLARR in the context of 27 other qualifying studies and confirmed many of the ROLARR findings. The 27 case control studies comprised 5,547 patients and had comparable outcomes data.
The outcomes of interest were duration of operation, conversion risk, blood loss, length of stay, oncological outcomes, time to first flatus, reoperation rate, postoperative morbidity, and postoperative mortality.
The investigators found that duration of the operation was longer for the robot-assisted procedure, compared with the conventional laparoscopic approach, though this difference was not statistically significant (z = 1.28, P = .20), and blood loss, morbidity, and mortality were similar between the two groups. Oncological outcomes (risk of positive circumferential resection margins, lymph node yield, and length of distal resection margins) were similar for these two surgical approaches.
In contrast to the ROLARR findings, this meta-analysis found that the risk of conversion favored the robot-assisted procedure (z = 5.51, P = .00001). Hospital stay (z = 2.46, P = 01) and time to first flatus outcomes (z = 3.09, P = .002) favored the robot-assisted procedure. Postop morbidity and mortality and reoperation rate were similar in the two groups.
“Based upon the findings of this largest-ever series on the role of robotic surgery in rectal cancer resection, the [robot-assisted procedure] is certainly a feasible technique and oncologically safe surgical intervention but failed to demonstrate any superiority over [the conventional laparoscopic approach] for many surgical outcomes,” the investigators wrote. “Mere advantage of robotic surgery was noted in only three postoperative outcomes, that is early passage of flatus, lower risk of conversion, and shorter hospitalization.”
Dr. Jones and her colleagues declared they had no conflicts of interest.
SOURCE: Jones K et al. World J Gastroentrol. 2018 Nov 15. doi: 10.4251/wjgo.v10.i11.449.
FROM WORLD JOURNAL OF GASTROINTESTINAL ONCOLOGY
Key clinical point:
Major finding: Duration of the operation was longer for the robot-assisted procedure, compared with the conventional laparoscopic approach (z = 1.28, P = .20), but blood loss, morbidity, and mortality were similar between the two groups.
Study details: Meta-analysis of 27 studies and one RCT of patients who had robot-assisted laparoscopic surgery or conventional laparoscopic surgery for rectal cancer.
Disclosures: The investigators had no disclosures.
Source: Jones K. World J Gastrointest Oncol. 2018 Nov 15. doi: 10.4251/wjgo.v10.i11.449.
Dogs steal the show at CHEST 2018
SAN ANTONIO – Therapy Animals of San Antonio, a non-profit organization that trains and places therapy pets, delighted the attendees of CHEST 2018 with a number of therapy dogs. Christopher L. Carroll, MD, FCCP, and Kathy Jewett, CHEST Director, Membership and Brand Development, spoke about the many benefits pets can bring to patients, including stress reduction and emotional comfort. The therapy dogs also will be visiting the CHEST 2018 meeting on Tuesday and Wednesday, 11:30 a.m. to 1:30 p.m., in the Exhibit Hall.
SAN ANTONIO – Therapy Animals of San Antonio, a non-profit organization that trains and places therapy pets, delighted the attendees of CHEST 2018 with a number of therapy dogs. Christopher L. Carroll, MD, FCCP, and Kathy Jewett, CHEST Director, Membership and Brand Development, spoke about the many benefits pets can bring to patients, including stress reduction and emotional comfort. The therapy dogs also will be visiting the CHEST 2018 meeting on Tuesday and Wednesday, 11:30 a.m. to 1:30 p.m., in the Exhibit Hall.
SAN ANTONIO – Therapy Animals of San Antonio, a non-profit organization that trains and places therapy pets, delighted the attendees of CHEST 2018 with a number of therapy dogs. Christopher L. Carroll, MD, FCCP, and Kathy Jewett, CHEST Director, Membership and Brand Development, spoke about the many benefits pets can bring to patients, including stress reduction and emotional comfort. The therapy dogs also will be visiting the CHEST 2018 meeting on Tuesday and Wednesday, 11:30 a.m. to 1:30 p.m., in the Exhibit Hall.
REPORTING FROM CHEST 2018