User login
Therese Borden is the editor of CHEST Physician. After 20 years of research, writing, and editing in the field of international development and economics, she began working in the field of medical editing and has held a variety of editorial positions with the company. She holds a PhD in International Economics from American University, Washington, and a BA in history from the University of Washington, Seattle.
Vaping-associated lung injury cases nears 1,300
according to a statement released by the Centers for Disease Control and Prevention.
These cases have been reported to the CDC from 49 states, the District of Columbia, and the U.S. Virgin Islands. The increase in lung injury cases from Oct. 1 (reported to be 1,080) represents both new patients and recent reporting of patients previously identified to the CDC.
Twenty-six deaths have been confirmed in 21 states and more deaths are currently being reviewed.
The causes of the injuries are still under investigation. The CDC stated, “The latest findings from the investigation into lung injuries associated with e-cigarette use, or vaping, suggest products containing THC play a role in the outbreak. All patients have a reported history of e-cigarette product use, or vaping, and no consistent evidence of an infectious cause has been discovered. Therefore, the suspected cause is a chemical exposure.” The specific chemical causing the lung injuries associated with vaping remains unknown at this time.
The CDC has created information hubs and resources for the public, for health care providers, and for state and local health department officials. The CDC has also provided additional resources to address the outbreak of vaping-associated lung injuries.
according to a statement released by the Centers for Disease Control and Prevention.
These cases have been reported to the CDC from 49 states, the District of Columbia, and the U.S. Virgin Islands. The increase in lung injury cases from Oct. 1 (reported to be 1,080) represents both new patients and recent reporting of patients previously identified to the CDC.
Twenty-six deaths have been confirmed in 21 states and more deaths are currently being reviewed.
The causes of the injuries are still under investigation. The CDC stated, “The latest findings from the investigation into lung injuries associated with e-cigarette use, or vaping, suggest products containing THC play a role in the outbreak. All patients have a reported history of e-cigarette product use, or vaping, and no consistent evidence of an infectious cause has been discovered. Therefore, the suspected cause is a chemical exposure.” The specific chemical causing the lung injuries associated with vaping remains unknown at this time.
The CDC has created information hubs and resources for the public, for health care providers, and for state and local health department officials. The CDC has also provided additional resources to address the outbreak of vaping-associated lung injuries.
according to a statement released by the Centers for Disease Control and Prevention.
These cases have been reported to the CDC from 49 states, the District of Columbia, and the U.S. Virgin Islands. The increase in lung injury cases from Oct. 1 (reported to be 1,080) represents both new patients and recent reporting of patients previously identified to the CDC.
Twenty-six deaths have been confirmed in 21 states and more deaths are currently being reviewed.
The causes of the injuries are still under investigation. The CDC stated, “The latest findings from the investigation into lung injuries associated with e-cigarette use, or vaping, suggest products containing THC play a role in the outbreak. All patients have a reported history of e-cigarette product use, or vaping, and no consistent evidence of an infectious cause has been discovered. Therefore, the suspected cause is a chemical exposure.” The specific chemical causing the lung injuries associated with vaping remains unknown at this time.
The CDC has created information hubs and resources for the public, for health care providers, and for state and local health department officials. The CDC has also provided additional resources to address the outbreak of vaping-associated lung injuries.
REPORTING FROM CDC
Environmental Scan: Drivers of change in education, content delivery, and career advancement
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
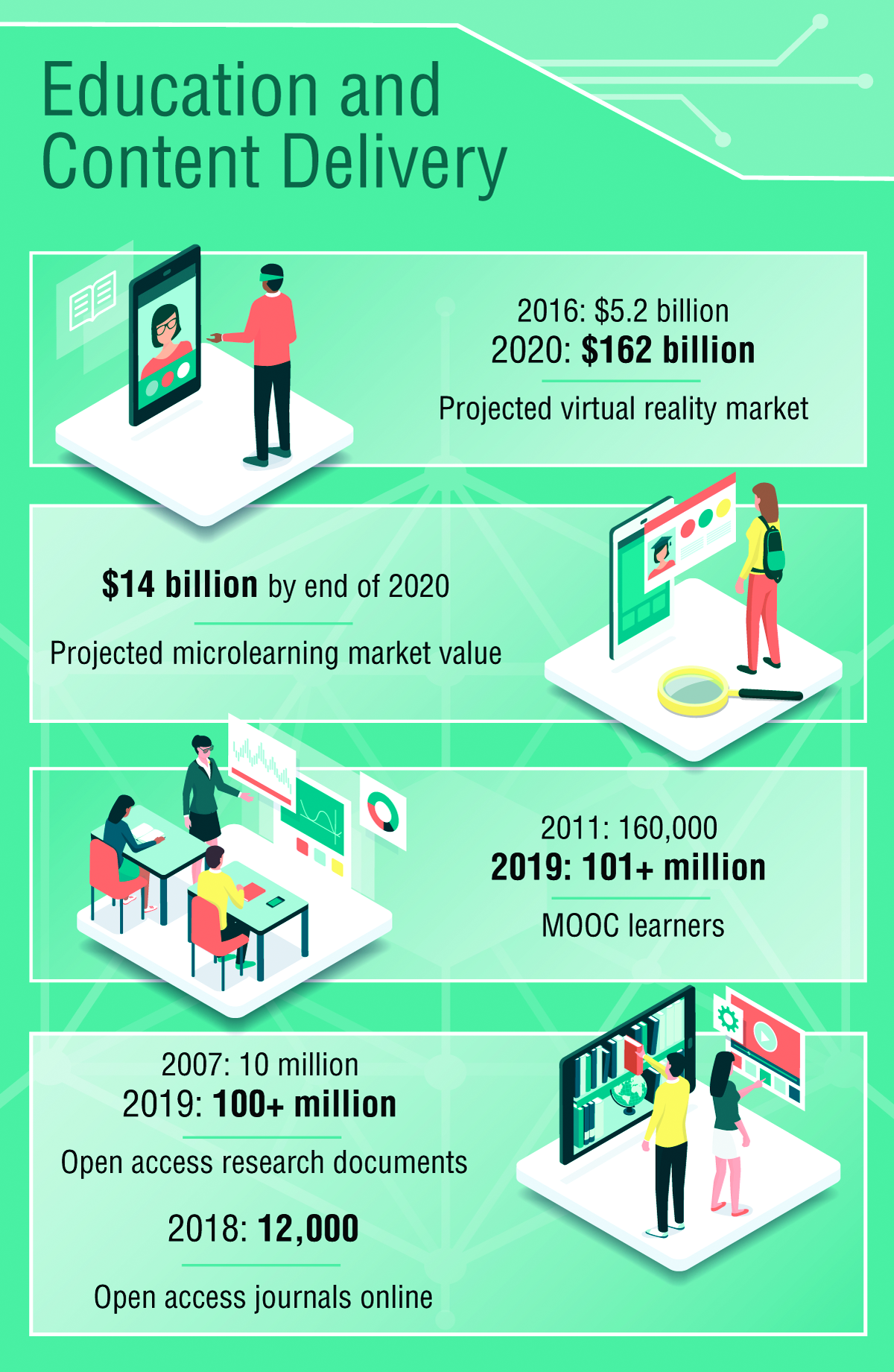
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Serum testosterone and estradiol levels associated with current asthma in women
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Environmental scan: Drivers of change in technology
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
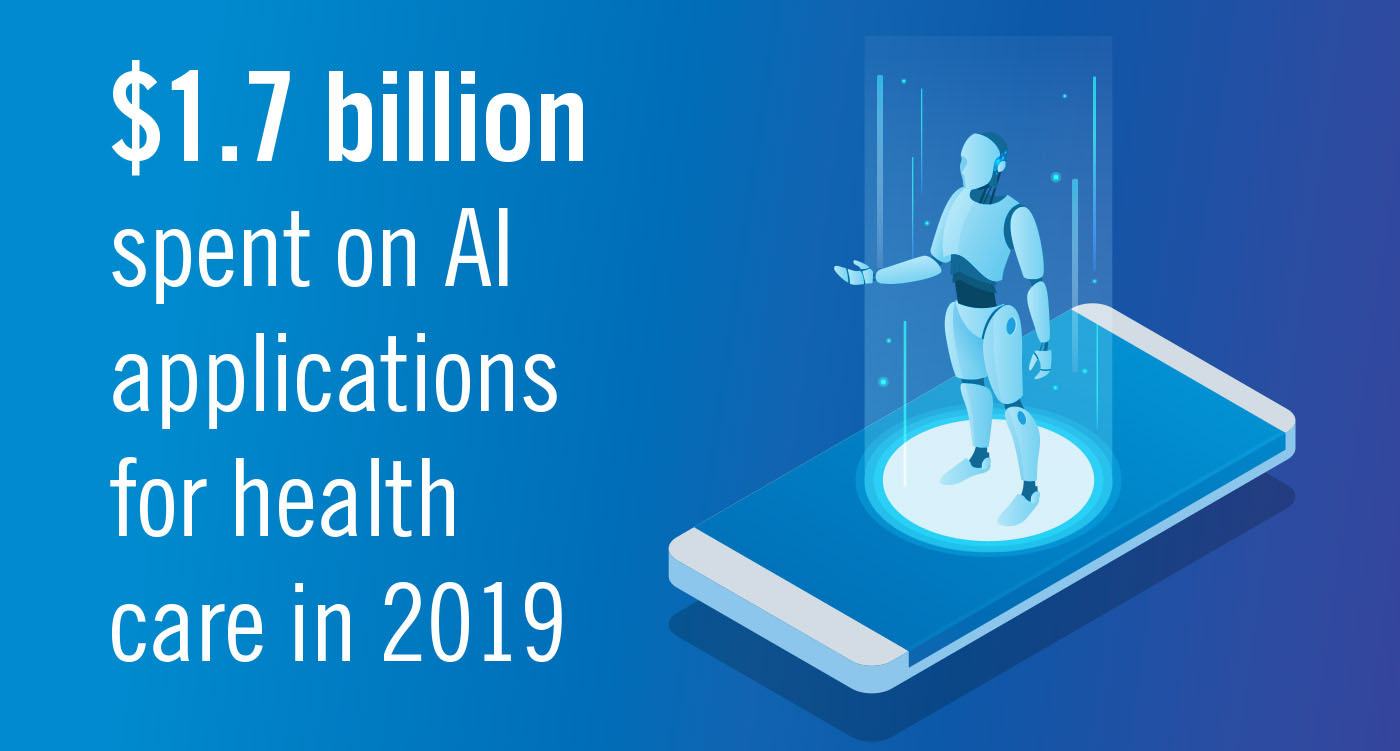
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Environmental Scan: Economy and workforce
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
Sleep disorder treatment tied to lower suicide attempt risk in veterans
in a large case-control matched study of patients in the Veterans Health Administration database.
However, treatment for sleep disorders was correlated to a reduced risk for suicide attempts.
Todd M. Bishop, PhD, of the Center of Excellence for Suicide Prevention, Canandaigua (N.Y.) VA Medical Center, and the department of psychiatry, University of Rochester (N.Y.) Medical Center, and his colleagues wrote that suicide is the 10th most frequent cause of death in the United States, and “nowhere is the suicide rate more alarming than among military veterans, who after adjusting for age and gender, have an approximately 1.5 times greater risk for suicide as compared to the civilian population.”
Previous research has explored the link between sleep disturbances and suicide attempts. But less has been done to look at specific sleep problems, and little research has examined the role of sleep medicine interventions and suicide attempt risk.
The investigators conducted a study to establish the association between suicide attempts and specific sleep disorders, and to examine the correlation between sleep medicine treatment and suicide attempts. Their sample consisted of 60,102 veterans who had received care within the VHA between Oct. 1, 2012, and Sept. 20, 2014. Half of the sample had a documented suicide attempt in the medical record (n = 30,051) and half did not (n = 30,051). The overall sample was predominately male (87.1%) with a mean age of 48.6 years. More than half the sample identified as white (67.4%).
Suicide attempts, sleep disturbance, and medical and mental health comorbidities were identified via ICD codes and prescription records. The predominant sleep disorders studied were insomnia, sleep-related breathing disorder (SRBD), and nightmares. The first suicide attempt in the study period was determined to be the index date for the case-control matching.
Overall, sleep disturbances were much more prevalent among cases than controls (insomnia, 46.2% vs. 12.6%), sleep-related breathing disorder (8.6% vs. 4.8%), and nightmares (7.1% vs. 1.6%). A logistic regression analysis was undertaken to examine the relationship between specific sleep disorders and suicide attempts. Insomnia, nightmares, and SRBD were each associated with increased odds of a suicide attempt with the following odds ratios: insomnia (odds ratio, 5.62; 95% confidence interval, 5.39-5.86), nightmares (OR, 2.49; 95% CI, 2.23-2.77), and sleep-related breathing disorder (OR, 1.37; 95% CI, 1.27-1.48).
A second model included known drivers of suicide attempts (PTSD, depression, anxiety disorders, schizophrenia, bipolar disorder, substance use disorder, medical comorbidity, and obesity). But after controlling for these factors, neither nightmares (OR, 0.96; 95% CI, 0.85-1.09) nor sleep-related breathing disorders (OR, 0.87, 95% CI, 0.79-0.94) remained positively associated with suicide attempt, but the association of insomnia with suicide attempt was maintained (OR, 1.51; 95% CI, 1.43-1.59).
The question of the impact of sleep medicine interventions on suicide attempts was studied with a third regression model adding the number of sleep medicine clinic visits in the 180 days prior to the suicide attempt index date as an independent variable. The variables in this model were limited to insomnia, SRBD, and nightmares. The investigators found that “for each sleep medicine clinic visit within the 6 months prior to index date the likelihood of suicide attempt is 11% less (OR, 0.89; 95% CI, 0.82-0.97).”
The limitations of the study include the lack of information on sleep treatment modalities or medications provided during the clinic visits, and the overlapping of sleep disturbance with other mental health conditions, such as alcohol dependence and PTSD. In addition, “some insomnia medications are labeled for risk of suicidal ideation and behavior, so there is some chance that the medications rather than insomnia itself were associated with the increased suicidal behavior,” the investigators wrote.
In addition to an analysis of specific types of sleep disorders associated with suicide attempts, the study showed that treatment of sleep disorders may have an important role in suicide prevention. The investigators concluded: “Identifying populations at risk for suicide prior to a first attempt is an important, but difficult task of suicide prevention. Prevention efforts can be aimed at modifiable risk factors that arise early on a patient’s trajectory toward a suicide attempt.”
The study was supported by the VISN 2 Center of Excellence for Suicide Prevention, Canandaigua VAMC. The authors had no disclosures.
SOURCE: Bishop TM et al. Sleep Med. 2019 Jul 25. doi: 10.1016/j.sleep.2019.07.016.
in a large case-control matched study of patients in the Veterans Health Administration database.
However, treatment for sleep disorders was correlated to a reduced risk for suicide attempts.
Todd M. Bishop, PhD, of the Center of Excellence for Suicide Prevention, Canandaigua (N.Y.) VA Medical Center, and the department of psychiatry, University of Rochester (N.Y.) Medical Center, and his colleagues wrote that suicide is the 10th most frequent cause of death in the United States, and “nowhere is the suicide rate more alarming than among military veterans, who after adjusting for age and gender, have an approximately 1.5 times greater risk for suicide as compared to the civilian population.”
Previous research has explored the link between sleep disturbances and suicide attempts. But less has been done to look at specific sleep problems, and little research has examined the role of sleep medicine interventions and suicide attempt risk.
The investigators conducted a study to establish the association between suicide attempts and specific sleep disorders, and to examine the correlation between sleep medicine treatment and suicide attempts. Their sample consisted of 60,102 veterans who had received care within the VHA between Oct. 1, 2012, and Sept. 20, 2014. Half of the sample had a documented suicide attempt in the medical record (n = 30,051) and half did not (n = 30,051). The overall sample was predominately male (87.1%) with a mean age of 48.6 years. More than half the sample identified as white (67.4%).
Suicide attempts, sleep disturbance, and medical and mental health comorbidities were identified via ICD codes and prescription records. The predominant sleep disorders studied were insomnia, sleep-related breathing disorder (SRBD), and nightmares. The first suicide attempt in the study period was determined to be the index date for the case-control matching.
Overall, sleep disturbances were much more prevalent among cases than controls (insomnia, 46.2% vs. 12.6%), sleep-related breathing disorder (8.6% vs. 4.8%), and nightmares (7.1% vs. 1.6%). A logistic regression analysis was undertaken to examine the relationship between specific sleep disorders and suicide attempts. Insomnia, nightmares, and SRBD were each associated with increased odds of a suicide attempt with the following odds ratios: insomnia (odds ratio, 5.62; 95% confidence interval, 5.39-5.86), nightmares (OR, 2.49; 95% CI, 2.23-2.77), and sleep-related breathing disorder (OR, 1.37; 95% CI, 1.27-1.48).
A second model included known drivers of suicide attempts (PTSD, depression, anxiety disorders, schizophrenia, bipolar disorder, substance use disorder, medical comorbidity, and obesity). But after controlling for these factors, neither nightmares (OR, 0.96; 95% CI, 0.85-1.09) nor sleep-related breathing disorders (OR, 0.87, 95% CI, 0.79-0.94) remained positively associated with suicide attempt, but the association of insomnia with suicide attempt was maintained (OR, 1.51; 95% CI, 1.43-1.59).
The question of the impact of sleep medicine interventions on suicide attempts was studied with a third regression model adding the number of sleep medicine clinic visits in the 180 days prior to the suicide attempt index date as an independent variable. The variables in this model were limited to insomnia, SRBD, and nightmares. The investigators found that “for each sleep medicine clinic visit within the 6 months prior to index date the likelihood of suicide attempt is 11% less (OR, 0.89; 95% CI, 0.82-0.97).”
The limitations of the study include the lack of information on sleep treatment modalities or medications provided during the clinic visits, and the overlapping of sleep disturbance with other mental health conditions, such as alcohol dependence and PTSD. In addition, “some insomnia medications are labeled for risk of suicidal ideation and behavior, so there is some chance that the medications rather than insomnia itself were associated with the increased suicidal behavior,” the investigators wrote.
In addition to an analysis of specific types of sleep disorders associated with suicide attempts, the study showed that treatment of sleep disorders may have an important role in suicide prevention. The investigators concluded: “Identifying populations at risk for suicide prior to a first attempt is an important, but difficult task of suicide prevention. Prevention efforts can be aimed at modifiable risk factors that arise early on a patient’s trajectory toward a suicide attempt.”
The study was supported by the VISN 2 Center of Excellence for Suicide Prevention, Canandaigua VAMC. The authors had no disclosures.
SOURCE: Bishop TM et al. Sleep Med. 2019 Jul 25. doi: 10.1016/j.sleep.2019.07.016.
in a large case-control matched study of patients in the Veterans Health Administration database.
However, treatment for sleep disorders was correlated to a reduced risk for suicide attempts.
Todd M. Bishop, PhD, of the Center of Excellence for Suicide Prevention, Canandaigua (N.Y.) VA Medical Center, and the department of psychiatry, University of Rochester (N.Y.) Medical Center, and his colleagues wrote that suicide is the 10th most frequent cause of death in the United States, and “nowhere is the suicide rate more alarming than among military veterans, who after adjusting for age and gender, have an approximately 1.5 times greater risk for suicide as compared to the civilian population.”
Previous research has explored the link between sleep disturbances and suicide attempts. But less has been done to look at specific sleep problems, and little research has examined the role of sleep medicine interventions and suicide attempt risk.
The investigators conducted a study to establish the association between suicide attempts and specific sleep disorders, and to examine the correlation between sleep medicine treatment and suicide attempts. Their sample consisted of 60,102 veterans who had received care within the VHA between Oct. 1, 2012, and Sept. 20, 2014. Half of the sample had a documented suicide attempt in the medical record (n = 30,051) and half did not (n = 30,051). The overall sample was predominately male (87.1%) with a mean age of 48.6 years. More than half the sample identified as white (67.4%).
Suicide attempts, sleep disturbance, and medical and mental health comorbidities were identified via ICD codes and prescription records. The predominant sleep disorders studied were insomnia, sleep-related breathing disorder (SRBD), and nightmares. The first suicide attempt in the study period was determined to be the index date for the case-control matching.
Overall, sleep disturbances were much more prevalent among cases than controls (insomnia, 46.2% vs. 12.6%), sleep-related breathing disorder (8.6% vs. 4.8%), and nightmares (7.1% vs. 1.6%). A logistic regression analysis was undertaken to examine the relationship between specific sleep disorders and suicide attempts. Insomnia, nightmares, and SRBD were each associated with increased odds of a suicide attempt with the following odds ratios: insomnia (odds ratio, 5.62; 95% confidence interval, 5.39-5.86), nightmares (OR, 2.49; 95% CI, 2.23-2.77), and sleep-related breathing disorder (OR, 1.37; 95% CI, 1.27-1.48).
A second model included known drivers of suicide attempts (PTSD, depression, anxiety disorders, schizophrenia, bipolar disorder, substance use disorder, medical comorbidity, and obesity). But after controlling for these factors, neither nightmares (OR, 0.96; 95% CI, 0.85-1.09) nor sleep-related breathing disorders (OR, 0.87, 95% CI, 0.79-0.94) remained positively associated with suicide attempt, but the association of insomnia with suicide attempt was maintained (OR, 1.51; 95% CI, 1.43-1.59).
The question of the impact of sleep medicine interventions on suicide attempts was studied with a third regression model adding the number of sleep medicine clinic visits in the 180 days prior to the suicide attempt index date as an independent variable. The variables in this model were limited to insomnia, SRBD, and nightmares. The investigators found that “for each sleep medicine clinic visit within the 6 months prior to index date the likelihood of suicide attempt is 11% less (OR, 0.89; 95% CI, 0.82-0.97).”
The limitations of the study include the lack of information on sleep treatment modalities or medications provided during the clinic visits, and the overlapping of sleep disturbance with other mental health conditions, such as alcohol dependence and PTSD. In addition, “some insomnia medications are labeled for risk of suicidal ideation and behavior, so there is some chance that the medications rather than insomnia itself were associated with the increased suicidal behavior,” the investigators wrote.
In addition to an analysis of specific types of sleep disorders associated with suicide attempts, the study showed that treatment of sleep disorders may have an important role in suicide prevention. The investigators concluded: “Identifying populations at risk for suicide prior to a first attempt is an important, but difficult task of suicide prevention. Prevention efforts can be aimed at modifiable risk factors that arise early on a patient’s trajectory toward a suicide attempt.”
The study was supported by the VISN 2 Center of Excellence for Suicide Prevention, Canandaigua VAMC. The authors had no disclosures.
SOURCE: Bishop TM et al. Sleep Med. 2019 Jul 25. doi: 10.1016/j.sleep.2019.07.016.
REPORTING FROM SLEEP MEDICINE
Vaping device marketers take aim at youth through social media
with targeted messages and images, a study of e-cigarette promotion has found.
In 2018, the JUUL company declared a commitment to support efforts to raise the age of legal purchase of tobacco to age 21 years in all U.S. states. In addition, JUUL deleted its official Facebook and Instagram accounts in November 2018, but the promotion of these products has continued through affiliated marketing campaigns from other online vendors.
Vaping among teens has shot up in popularity in recent years. The prevalence of vaping among young people aged 16-19 years has been estimated at 16% in 2018, up from 11% in 2017 (BMJ. 2019 Jun 19. doi: 10.1136/bmj.12219. A study published in JAMA Pediatrics (2019;173[7]:690-92) found that an estimated 81% of users following a popular Twitter account (@JUULvapor) were aged 13-20 years, with 45% in the 13-17 year age range.
Elizabeth C. Hair, PhD, senior vice president of the Truth Initiative Schroeder Institute, and a team of investigators conducted a study of the “proliferation of JUUL-related content across four themes over a 3-month period: overt promotional content, nicotine and addiction-related content, lifestyle content, and content related to youth culture.” The study appeared online in Tobacco Control (2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824).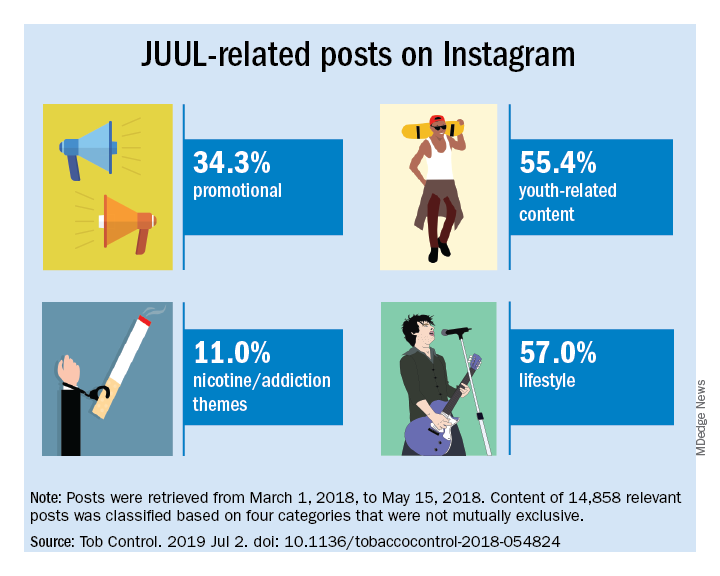
The investigators did a content analysis of social media posts on Instagram related to JUUL and JUUL-like products from March 1 to May 15, 2018. Hash-tag keyword queries of JUUL-related posts on Instagram were collected from the Instagram application programming interface through NUVI, a licensed syndicator of the Instagram firehose. The researchers used 50 hashtags to capture and enumerate individual posts. Examples of the hashtags used are #juul, #juuling, #juulvapor, #juulpod, #switchtojuul, and #juulgang. All posts were included from the official JUUL account and JUUL-related accounts with the highest number of followers at the time of data collection (e.g., @juulcentral, @juulnation, @juul_university, @juul.girls).
The search identified 14,838 posts by 5,201 unique users that featured content relating to product promotion, nicotine and addiction messages, youth culture, and lifestyle themes. Posts were rated promotional incluced branded content, URLs linking to commercial websites, and hashtags indicating affiliations with commercial sites.
Nicotine/addiction posts contained “references to nicotine, including compatible pod-related brand names and nicotine content, as well as any references to addiction or nicotine dependence (e.g., daily use, being an addict, junkie, “nichead,” fiend, maniac), or effects of nicotine use (e.g., “buzz”).
Youth-themed posts included stylistic features such as jargon or slang, acronyms common among youth (e.g., di4j, doit4juul), youth-oriented cartoons, JUUL wrap imagery, youth entertainment, and music. Posts with references to school, the classroom, and other places frequented by youth and youth social networks, family, and peers were included in the youth-themed category.
Lifestyle content referenced "social norms and acceptability-related messages contained any mentions of online or offline communitiesand peer groups (eg, collegelife, juulgirls, juulgang, vapeusa, collegedaily, vapelyfe hashtags) as well as JUUL use during social activities, events, social acceptance of JUULing and any mentions of JUULing as a characteristic of cultural or social identity."
Content analysis of the posts found that 34.3% were promotional, 11% referenced nicotine and addiction themes, and 55.4% featured youth-oriented cultural themes, and 57% featured lifestyle themes. There was overlap among the categories, for example, the 71.9% of the promotional posts had lifestyle messages included and 86.3% of the nicotine/addiction posts contained lifestyle elements. The promotional posts also contained some hashtags referencing cannabis (#420, #710).
An additional feature of the promotional posts is the incentivizing messages. “More than more than a third of JUUL-related posts containing overt promotional content that highlights ways to obtain products at reduced cost, such as giveaways and incentivized friend-tagging. This finding is consistent with previous research which found that Twitter users employed person-tagging (e.g., @username) when purchasing JUUL, suggesting friend-tagging plays an important role in motivating product use,” the researchers wrote.
The study was limited by the short time frame, the analysis of Instagram postings only, and the limitation of only 50 hashtags. These limitations may result in underreporting of the amount of JUUL-related social media messaging that targets youth. In addition, the investigators did not analyze the origin of accounts or the identity of the individuals creating the content.
“The results of this study demonstrate the reach of organic posts that contain JUUL-related content, and posts by third-party vendors of vaping products, who continue to push explicitly youth-targeted advertisements for JUUL and similar e-cigarette products under JUUL-related hashtags,” Dr. Hair wrote. “Our research and studies done by others in the field are one way to build the evidence base to advocate for stricter social media marketing restrictions on tobacco products that are applicable to all players in the field.”
She added that the Food and Drug Administration should use its power to restrict e-cigarette manufacturers from using social media to market to young people. “We also think that social media platforms should do more to adopt and enforce strong and well-enforced policies against the promotion of any tobacco products to young adults,” she concluded.
The study was sponsored by the Truth Initiative. The Truth Initiative was created as a part of the Master Settlement Agreement (MSA) that was negotiated between the tobacco industry and 46 states and the District of Columbia in 1998. The MSA created the American Legacy Foundation (now known as the Truth Initiative), a nonprofit research and educational organization that focuses its efforts on preventing teen smoking and encouraging smokers to quit.
SOURCE: Czaplicki L et al. Tob Control. 2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824.
This article was updated 7/17/2019.
with targeted messages and images, a study of e-cigarette promotion has found.
In 2018, the JUUL company declared a commitment to support efforts to raise the age of legal purchase of tobacco to age 21 years in all U.S. states. In addition, JUUL deleted its official Facebook and Instagram accounts in November 2018, but the promotion of these products has continued through affiliated marketing campaigns from other online vendors.
Vaping among teens has shot up in popularity in recent years. The prevalence of vaping among young people aged 16-19 years has been estimated at 16% in 2018, up from 11% in 2017 (BMJ. 2019 Jun 19. doi: 10.1136/bmj.12219. A study published in JAMA Pediatrics (2019;173[7]:690-92) found that an estimated 81% of users following a popular Twitter account (@JUULvapor) were aged 13-20 years, with 45% in the 13-17 year age range.
Elizabeth C. Hair, PhD, senior vice president of the Truth Initiative Schroeder Institute, and a team of investigators conducted a study of the “proliferation of JUUL-related content across four themes over a 3-month period: overt promotional content, nicotine and addiction-related content, lifestyle content, and content related to youth culture.” The study appeared online in Tobacco Control (2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824).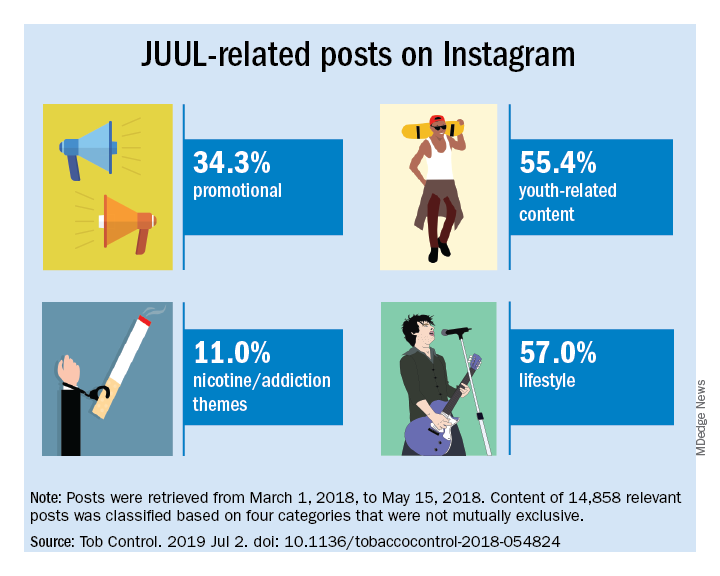
The investigators did a content analysis of social media posts on Instagram related to JUUL and JUUL-like products from March 1 to May 15, 2018. Hash-tag keyword queries of JUUL-related posts on Instagram were collected from the Instagram application programming interface through NUVI, a licensed syndicator of the Instagram firehose. The researchers used 50 hashtags to capture and enumerate individual posts. Examples of the hashtags used are #juul, #juuling, #juulvapor, #juulpod, #switchtojuul, and #juulgang. All posts were included from the official JUUL account and JUUL-related accounts with the highest number of followers at the time of data collection (e.g., @juulcentral, @juulnation, @juul_university, @juul.girls).
The search identified 14,838 posts by 5,201 unique users that featured content relating to product promotion, nicotine and addiction messages, youth culture, and lifestyle themes. Posts were rated promotional incluced branded content, URLs linking to commercial websites, and hashtags indicating affiliations with commercial sites.
Nicotine/addiction posts contained “references to nicotine, including compatible pod-related brand names and nicotine content, as well as any references to addiction or nicotine dependence (e.g., daily use, being an addict, junkie, “nichead,” fiend, maniac), or effects of nicotine use (e.g., “buzz”).
Youth-themed posts included stylistic features such as jargon or slang, acronyms common among youth (e.g., di4j, doit4juul), youth-oriented cartoons, JUUL wrap imagery, youth entertainment, and music. Posts with references to school, the classroom, and other places frequented by youth and youth social networks, family, and peers were included in the youth-themed category.
Lifestyle content referenced "social norms and acceptability-related messages contained any mentions of online or offline communitiesand peer groups (eg, collegelife, juulgirls, juulgang, vapeusa, collegedaily, vapelyfe hashtags) as well as JUUL use during social activities, events, social acceptance of JUULing and any mentions of JUULing as a characteristic of cultural or social identity."
Content analysis of the posts found that 34.3% were promotional, 11% referenced nicotine and addiction themes, and 55.4% featured youth-oriented cultural themes, and 57% featured lifestyle themes. There was overlap among the categories, for example, the 71.9% of the promotional posts had lifestyle messages included and 86.3% of the nicotine/addiction posts contained lifestyle elements. The promotional posts also contained some hashtags referencing cannabis (#420, #710).
An additional feature of the promotional posts is the incentivizing messages. “More than more than a third of JUUL-related posts containing overt promotional content that highlights ways to obtain products at reduced cost, such as giveaways and incentivized friend-tagging. This finding is consistent with previous research which found that Twitter users employed person-tagging (e.g., @username) when purchasing JUUL, suggesting friend-tagging plays an important role in motivating product use,” the researchers wrote.
The study was limited by the short time frame, the analysis of Instagram postings only, and the limitation of only 50 hashtags. These limitations may result in underreporting of the amount of JUUL-related social media messaging that targets youth. In addition, the investigators did not analyze the origin of accounts or the identity of the individuals creating the content.
“The results of this study demonstrate the reach of organic posts that contain JUUL-related content, and posts by third-party vendors of vaping products, who continue to push explicitly youth-targeted advertisements for JUUL and similar e-cigarette products under JUUL-related hashtags,” Dr. Hair wrote. “Our research and studies done by others in the field are one way to build the evidence base to advocate for stricter social media marketing restrictions on tobacco products that are applicable to all players in the field.”
She added that the Food and Drug Administration should use its power to restrict e-cigarette manufacturers from using social media to market to young people. “We also think that social media platforms should do more to adopt and enforce strong and well-enforced policies against the promotion of any tobacco products to young adults,” she concluded.
The study was sponsored by the Truth Initiative. The Truth Initiative was created as a part of the Master Settlement Agreement (MSA) that was negotiated between the tobacco industry and 46 states and the District of Columbia in 1998. The MSA created the American Legacy Foundation (now known as the Truth Initiative), a nonprofit research and educational organization that focuses its efforts on preventing teen smoking and encouraging smokers to quit.
SOURCE: Czaplicki L et al. Tob Control. 2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824.
This article was updated 7/17/2019.
with targeted messages and images, a study of e-cigarette promotion has found.
In 2018, the JUUL company declared a commitment to support efforts to raise the age of legal purchase of tobacco to age 21 years in all U.S. states. In addition, JUUL deleted its official Facebook and Instagram accounts in November 2018, but the promotion of these products has continued through affiliated marketing campaigns from other online vendors.
Vaping among teens has shot up in popularity in recent years. The prevalence of vaping among young people aged 16-19 years has been estimated at 16% in 2018, up from 11% in 2017 (BMJ. 2019 Jun 19. doi: 10.1136/bmj.12219. A study published in JAMA Pediatrics (2019;173[7]:690-92) found that an estimated 81% of users following a popular Twitter account (@JUULvapor) were aged 13-20 years, with 45% in the 13-17 year age range.
Elizabeth C. Hair, PhD, senior vice president of the Truth Initiative Schroeder Institute, and a team of investigators conducted a study of the “proliferation of JUUL-related content across four themes over a 3-month period: overt promotional content, nicotine and addiction-related content, lifestyle content, and content related to youth culture.” The study appeared online in Tobacco Control (2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824).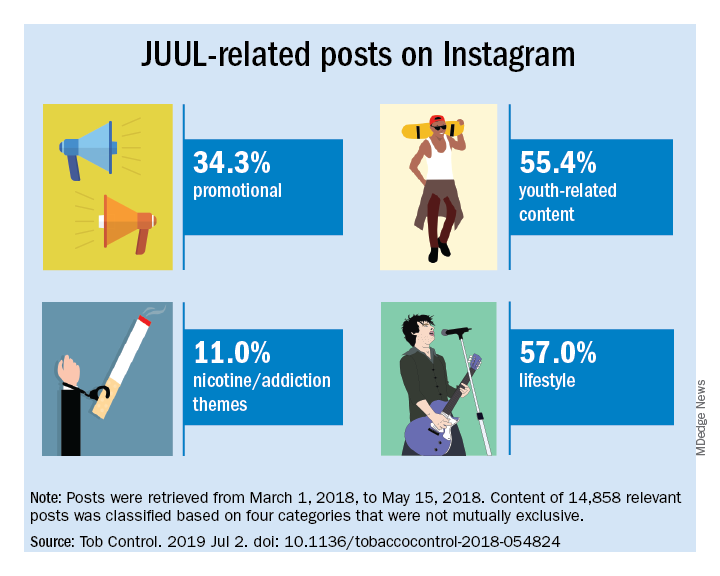
The investigators did a content analysis of social media posts on Instagram related to JUUL and JUUL-like products from March 1 to May 15, 2018. Hash-tag keyword queries of JUUL-related posts on Instagram were collected from the Instagram application programming interface through NUVI, a licensed syndicator of the Instagram firehose. The researchers used 50 hashtags to capture and enumerate individual posts. Examples of the hashtags used are #juul, #juuling, #juulvapor, #juulpod, #switchtojuul, and #juulgang. All posts were included from the official JUUL account and JUUL-related accounts with the highest number of followers at the time of data collection (e.g., @juulcentral, @juulnation, @juul_university, @juul.girls).
The search identified 14,838 posts by 5,201 unique users that featured content relating to product promotion, nicotine and addiction messages, youth culture, and lifestyle themes. Posts were rated promotional incluced branded content, URLs linking to commercial websites, and hashtags indicating affiliations with commercial sites.
Nicotine/addiction posts contained “references to nicotine, including compatible pod-related brand names and nicotine content, as well as any references to addiction or nicotine dependence (e.g., daily use, being an addict, junkie, “nichead,” fiend, maniac), or effects of nicotine use (e.g., “buzz”).
Youth-themed posts included stylistic features such as jargon or slang, acronyms common among youth (e.g., di4j, doit4juul), youth-oriented cartoons, JUUL wrap imagery, youth entertainment, and music. Posts with references to school, the classroom, and other places frequented by youth and youth social networks, family, and peers were included in the youth-themed category.
Lifestyle content referenced "social norms and acceptability-related messages contained any mentions of online or offline communitiesand peer groups (eg, collegelife, juulgirls, juulgang, vapeusa, collegedaily, vapelyfe hashtags) as well as JUUL use during social activities, events, social acceptance of JUULing and any mentions of JUULing as a characteristic of cultural or social identity."
Content analysis of the posts found that 34.3% were promotional, 11% referenced nicotine and addiction themes, and 55.4% featured youth-oriented cultural themes, and 57% featured lifestyle themes. There was overlap among the categories, for example, the 71.9% of the promotional posts had lifestyle messages included and 86.3% of the nicotine/addiction posts contained lifestyle elements. The promotional posts also contained some hashtags referencing cannabis (#420, #710).
An additional feature of the promotional posts is the incentivizing messages. “More than more than a third of JUUL-related posts containing overt promotional content that highlights ways to obtain products at reduced cost, such as giveaways and incentivized friend-tagging. This finding is consistent with previous research which found that Twitter users employed person-tagging (e.g., @username) when purchasing JUUL, suggesting friend-tagging plays an important role in motivating product use,” the researchers wrote.
The study was limited by the short time frame, the analysis of Instagram postings only, and the limitation of only 50 hashtags. These limitations may result in underreporting of the amount of JUUL-related social media messaging that targets youth. In addition, the investigators did not analyze the origin of accounts or the identity of the individuals creating the content.
“The results of this study demonstrate the reach of organic posts that contain JUUL-related content, and posts by third-party vendors of vaping products, who continue to push explicitly youth-targeted advertisements for JUUL and similar e-cigarette products under JUUL-related hashtags,” Dr. Hair wrote. “Our research and studies done by others in the field are one way to build the evidence base to advocate for stricter social media marketing restrictions on tobacco products that are applicable to all players in the field.”
She added that the Food and Drug Administration should use its power to restrict e-cigarette manufacturers from using social media to market to young people. “We also think that social media platforms should do more to adopt and enforce strong and well-enforced policies against the promotion of any tobacco products to young adults,” she concluded.
The study was sponsored by the Truth Initiative. The Truth Initiative was created as a part of the Master Settlement Agreement (MSA) that was negotiated between the tobacco industry and 46 states and the District of Columbia in 1998. The MSA created the American Legacy Foundation (now known as the Truth Initiative), a nonprofit research and educational organization that focuses its efforts on preventing teen smoking and encouraging smokers to quit.
SOURCE: Czaplicki L et al. Tob Control. 2019 Jul 2; doi: 10.1136/tobaccocontrol-2018-054824.
This article was updated 7/17/2019.
FROM TOBACCO CONTROL
Environmental Scan: Drivers of change in health care
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: the CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Chest physicians are witnessing a revolution within the environment in which they practice. Information technology, changing consumer behavior, and the social imperative to contain costs are coming together to transform health care.
Innovation in the prevention, diagnosis, and treatment of health-related issues is being fueled by the emergence of accessible and affordable technology-based solutions and changes in patient approaches to health care. Consumers and employers are increasingly motivated to look for cost-effective options for health in care delivery and for economical access to innovations.1 Organizations will need to respond with a strategy that aligns with the changing environment and position physicians to lead these trends in the direction of improved patient care.2
Enabling technologies like electronic health records, blockchain, and artificial intelligence will increase connectivity among all the stakeholders in the health-care system. The exponential increase in connectivity means growing engagement of health systems, health plans, patients, and families in all aspects of health care. For health-care providers, these technologies will mean an acceleration of the requirement to generate data in clinical settings and utilize data for clinical decision making. Easily available data on outcomes and, most importantly, cost of treatment will be expected at point of service.3
Access to information will continue to empower consumers to take an active role in their own health care. More patients will be comfortable with delivery of some health care via digital devices, apps, and virtual access to treatment. The market will respond with technology that helps consumers navigate health-care systems, explore options, and communicate directly with providers. The use of apps and virtual encounters is expected to transform the role of primary care providers: patients will increasingly utilize nonphysician resources in outpatient settings, bypassing primary care physicians and reaching out to specialty care as needed.4
David A. Schulman, MD, FCCP, Professor of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine, Atlanta, and Editor in Chief of CHEST Physician, has seen the transformation of patient behavior and attitudes in his own practice.
“In general, they have done far more research about their health problems before seeking my counsel than patients did previously. Many use the internet not just to read about their symptoms and diseases, but also to connect with others having similar issues, sharing experiences, treatments, outcomes, and emotions; in some ways, this is the new ‘crowdsourcing’ of medicine.”
Patients who do their own “research” can present a challenge for physicians. Dr. Schulman noted, “I am often surprised about the misconceptions about disease that derive from information gleaned from a web-based source. One need not look any farther than the groundswell of misinformation being spread about vaccinations to see the potential downside of the pervasive availability of medical ‘facts’ online. Since we are unlikely to convince our patients to avoid the online milieu entirely, our role as health-care providers is to help our patients process and appropriately weigh the information that they receive, potentially partnering with our national societies to help curate such information.”
Dr. Schulman’s approach to the potential of patient misinformation is to initiate almost all discussions with patients with the question “Have your read or seen anything about this condition?” He said, “It is rare for patients to answer negatively. And listening to them speak about their understanding of their disease provides me with invaluable information about how the remainder of our visit should be spent. Do we need to correct misunderstandings? Are there gaps in the explanation that I can fill? Can we move directly into a conversation about treatment options? Can I provide you with some additional resources that might help to further your knowledge about the condition?”
Generational factors will play a big role in health-care demand and delivery. Health-care companies are already building lower cost delivery models to capture the millennial market.4 Cost-saving digital tools and virtual contacts are currently most commonly used by younger patients.5 Physicians need to understand and be a part of this trend, Dr. Schulman argued. “We should embrace telemedicine and mobile applications to collect data from the patients in their day-to-day lives. While insurance coverage of telemedicine is far from universal at the moment, and the reliability of mobile applications is highly variable, we know that a growing number of our patients are already relying on their digital devices to manage their health. In much the same way that we will need to help patient evaluate online information, we should work with our national societies to support the creation of tools that will allow us to collect data in the home environment in a more robust and reliable fashion.”
The proportion of the US population over the age of 65 is increasing yearly.6 Six out of 10 Americans live with a chronic illness, such as heart disease or diabetes. These and other chronic diseases are the leading drivers of the $3.3 billion annual health-care costs.7 Cost containment for these older patients and those with chronic illness will involve a focus on quality and outcomes data, a drive to deliver treatment in lower cost outpatient settings, and an acceleration of the adoption of value-based models currently underway.8
Taken together, these trends will mean a growing digital interface between physician and patient, a more active consumer-patient, and the availability of a vast array of new tools to access and manage health-care data.
- Delivery of procedures and services will trend from physicians to other members of the health-care team and to lower cost, outpatient settings.9
- Health-care systems will ramp up investment in products and services that improve outcomes and cost effectiveness.10
- Increased regulatory requirements and new payment models mean an ever-growing utilization of information technology by providers to fulfill data imperatives.11
- Physicians will have an increased need for tools that prioritize costs and outcomes data at the point of care.12
- Integration of data from new technologies will touch every aspect of health-care delivery with the objective of improving outcomes and, in turn, reducing costs.13
- Changing consumer attitudes toward delivery of care will be based on a growing familiarity of patients with a digital or virtual interface with providers, facility with health-care apps, and preference for a menu of options for health-care delivery.14
Dr. Schulman concluded, “We can no more expect our patients to ignore the full panoply of medical information on the internet and digital tools on their mobile devices than we can tell the tide not to come in. The die is cast; this is the world within which we must ply our trade. By identifying best practices and sharing our successes, we can come through this revolution better for the experience.”
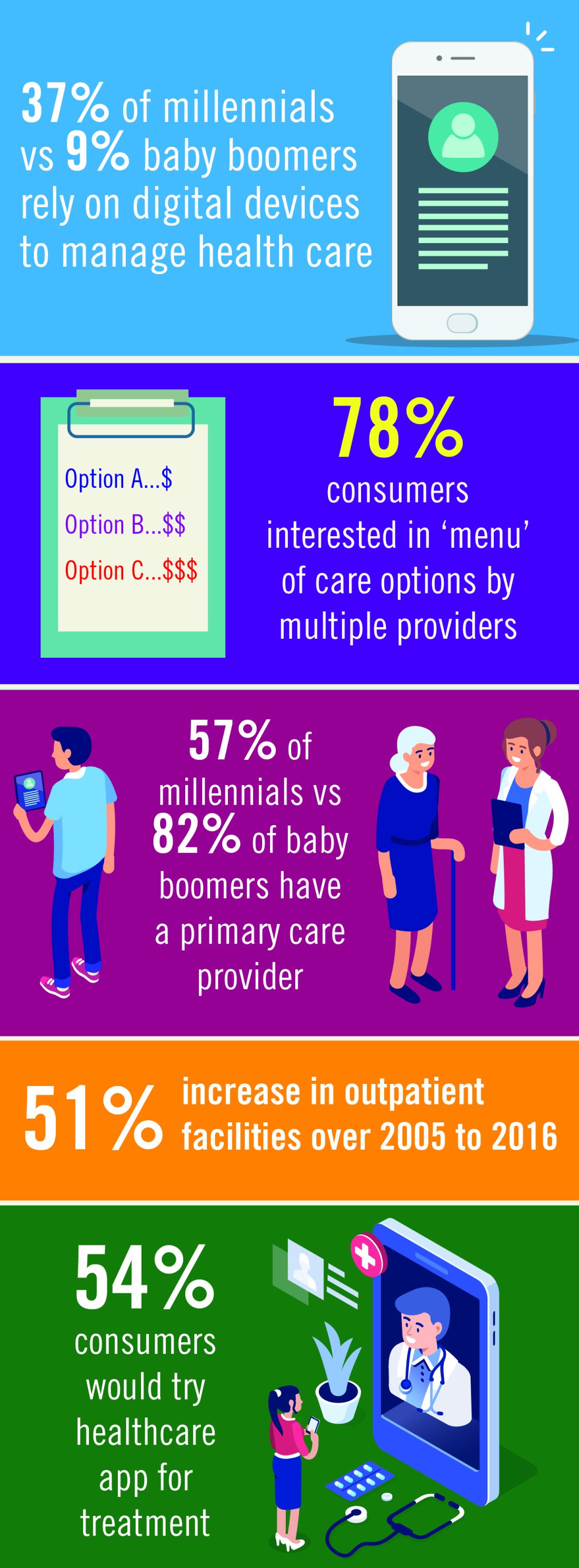
References
1. https://www.modernhealthcare.com/article/20181220/NEWS/181229992/number-of-outpatient-facilities-surges-as-industry-values-more
2. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
3. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
4. PcW Health Research Institute: Top health industry issues of 2019
5. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
6. https://www.census.gov/newsroom/press-releases/2017/cb17-100.html
7. https://www.cdc.gov/chronicdisease/index.htm
8. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/health-care-current-december4-2018.html
9. PcW Health Research Institute Top health industry issues of 2019: The New Health Economy comes of age
10. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
11. https://www2.deloitte.com/insights/us/en/industry/life-sciences/medtech-research-and-development-innovation.html
12. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
13. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
14. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: the CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Chest physicians are witnessing a revolution within the environment in which they practice. Information technology, changing consumer behavior, and the social imperative to contain costs are coming together to transform health care.
Innovation in the prevention, diagnosis, and treatment of health-related issues is being fueled by the emergence of accessible and affordable technology-based solutions and changes in patient approaches to health care. Consumers and employers are increasingly motivated to look for cost-effective options for health in care delivery and for economical access to innovations.1 Organizations will need to respond with a strategy that aligns with the changing environment and position physicians to lead these trends in the direction of improved patient care.2
Enabling technologies like electronic health records, blockchain, and artificial intelligence will increase connectivity among all the stakeholders in the health-care system. The exponential increase in connectivity means growing engagement of health systems, health plans, patients, and families in all aspects of health care. For health-care providers, these technologies will mean an acceleration of the requirement to generate data in clinical settings and utilize data for clinical decision making. Easily available data on outcomes and, most importantly, cost of treatment will be expected at point of service.3
Access to information will continue to empower consumers to take an active role in their own health care. More patients will be comfortable with delivery of some health care via digital devices, apps, and virtual access to treatment. The market will respond with technology that helps consumers navigate health-care systems, explore options, and communicate directly with providers. The use of apps and virtual encounters is expected to transform the role of primary care providers: patients will increasingly utilize nonphysician resources in outpatient settings, bypassing primary care physicians and reaching out to specialty care as needed.4
David A. Schulman, MD, FCCP, Professor of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine, Atlanta, and Editor in Chief of CHEST Physician, has seen the transformation of patient behavior and attitudes in his own practice.
“In general, they have done far more research about their health problems before seeking my counsel than patients did previously. Many use the internet not just to read about their symptoms and diseases, but also to connect with others having similar issues, sharing experiences, treatments, outcomes, and emotions; in some ways, this is the new ‘crowdsourcing’ of medicine.”
Patients who do their own “research” can present a challenge for physicians. Dr. Schulman noted, “I am often surprised about the misconceptions about disease that derive from information gleaned from a web-based source. One need not look any farther than the groundswell of misinformation being spread about vaccinations to see the potential downside of the pervasive availability of medical ‘facts’ online. Since we are unlikely to convince our patients to avoid the online milieu entirely, our role as health-care providers is to help our patients process and appropriately weigh the information that they receive, potentially partnering with our national societies to help curate such information.”
Dr. Schulman’s approach to the potential of patient misinformation is to initiate almost all discussions with patients with the question “Have your read or seen anything about this condition?” He said, “It is rare for patients to answer negatively. And listening to them speak about their understanding of their disease provides me with invaluable information about how the remainder of our visit should be spent. Do we need to correct misunderstandings? Are there gaps in the explanation that I can fill? Can we move directly into a conversation about treatment options? Can I provide you with some additional resources that might help to further your knowledge about the condition?”
Generational factors will play a big role in health-care demand and delivery. Health-care companies are already building lower cost delivery models to capture the millennial market.4 Cost-saving digital tools and virtual contacts are currently most commonly used by younger patients.5 Physicians need to understand and be a part of this trend, Dr. Schulman argued. “We should embrace telemedicine and mobile applications to collect data from the patients in their day-to-day lives. While insurance coverage of telemedicine is far from universal at the moment, and the reliability of mobile applications is highly variable, we know that a growing number of our patients are already relying on their digital devices to manage their health. In much the same way that we will need to help patient evaluate online information, we should work with our national societies to support the creation of tools that will allow us to collect data in the home environment in a more robust and reliable fashion.”
The proportion of the US population over the age of 65 is increasing yearly.6 Six out of 10 Americans live with a chronic illness, such as heart disease or diabetes. These and other chronic diseases are the leading drivers of the $3.3 billion annual health-care costs.7 Cost containment for these older patients and those with chronic illness will involve a focus on quality and outcomes data, a drive to deliver treatment in lower cost outpatient settings, and an acceleration of the adoption of value-based models currently underway.8
Taken together, these trends will mean a growing digital interface between physician and patient, a more active consumer-patient, and the availability of a vast array of new tools to access and manage health-care data.
- Delivery of procedures and services will trend from physicians to other members of the health-care team and to lower cost, outpatient settings.9
- Health-care systems will ramp up investment in products and services that improve outcomes and cost effectiveness.10
- Increased regulatory requirements and new payment models mean an ever-growing utilization of information technology by providers to fulfill data imperatives.11
- Physicians will have an increased need for tools that prioritize costs and outcomes data at the point of care.12
- Integration of data from new technologies will touch every aspect of health-care delivery with the objective of improving outcomes and, in turn, reducing costs.13
- Changing consumer attitudes toward delivery of care will be based on a growing familiarity of patients with a digital or virtual interface with providers, facility with health-care apps, and preference for a menu of options for health-care delivery.14
Dr. Schulman concluded, “We can no more expect our patients to ignore the full panoply of medical information on the internet and digital tools on their mobile devices than we can tell the tide not to come in. The die is cast; this is the world within which we must ply our trade. By identifying best practices and sharing our successes, we can come through this revolution better for the experience.”
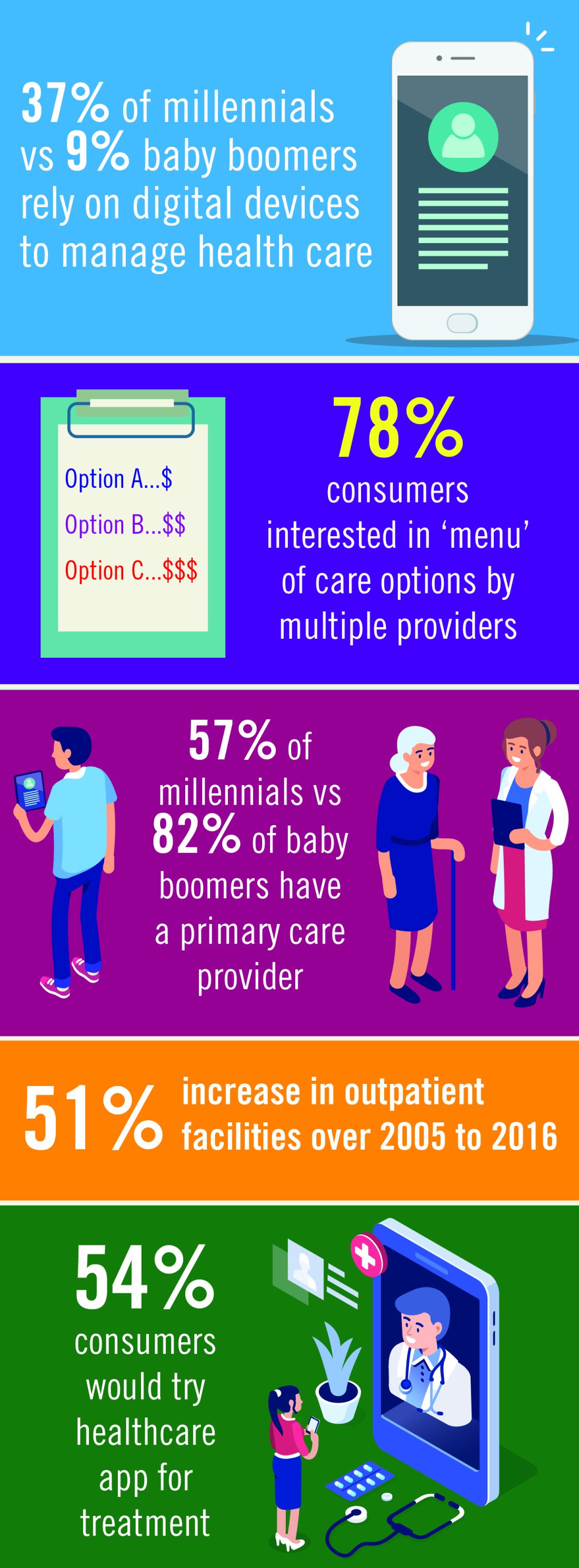
References
1. https://www.modernhealthcare.com/article/20181220/NEWS/181229992/number-of-outpatient-facilities-surges-as-industry-values-more
2. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
3. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
4. PcW Health Research Institute: Top health industry issues of 2019
5. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
6. https://www.census.gov/newsroom/press-releases/2017/cb17-100.html
7. https://www.cdc.gov/chronicdisease/index.htm
8. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/health-care-current-december4-2018.html
9. PcW Health Research Institute Top health industry issues of 2019: The New Health Economy comes of age
10. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
11. https://www2.deloitte.com/insights/us/en/industry/life-sciences/medtech-research-and-development-innovation.html
12. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
13. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
14. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: the CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Chest physicians are witnessing a revolution within the environment in which they practice. Information technology, changing consumer behavior, and the social imperative to contain costs are coming together to transform health care.
Innovation in the prevention, diagnosis, and treatment of health-related issues is being fueled by the emergence of accessible and affordable technology-based solutions and changes in patient approaches to health care. Consumers and employers are increasingly motivated to look for cost-effective options for health in care delivery and for economical access to innovations.1 Organizations will need to respond with a strategy that aligns with the changing environment and position physicians to lead these trends in the direction of improved patient care.2
Enabling technologies like electronic health records, blockchain, and artificial intelligence will increase connectivity among all the stakeholders in the health-care system. The exponential increase in connectivity means growing engagement of health systems, health plans, patients, and families in all aspects of health care. For health-care providers, these technologies will mean an acceleration of the requirement to generate data in clinical settings and utilize data for clinical decision making. Easily available data on outcomes and, most importantly, cost of treatment will be expected at point of service.3
Access to information will continue to empower consumers to take an active role in their own health care. More patients will be comfortable with delivery of some health care via digital devices, apps, and virtual access to treatment. The market will respond with technology that helps consumers navigate health-care systems, explore options, and communicate directly with providers. The use of apps and virtual encounters is expected to transform the role of primary care providers: patients will increasingly utilize nonphysician resources in outpatient settings, bypassing primary care physicians and reaching out to specialty care as needed.4
David A. Schulman, MD, FCCP, Professor of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine, Atlanta, and Editor in Chief of CHEST Physician, has seen the transformation of patient behavior and attitudes in his own practice.
“In general, they have done far more research about their health problems before seeking my counsel than patients did previously. Many use the internet not just to read about their symptoms and diseases, but also to connect with others having similar issues, sharing experiences, treatments, outcomes, and emotions; in some ways, this is the new ‘crowdsourcing’ of medicine.”
Patients who do their own “research” can present a challenge for physicians. Dr. Schulman noted, “I am often surprised about the misconceptions about disease that derive from information gleaned from a web-based source. One need not look any farther than the groundswell of misinformation being spread about vaccinations to see the potential downside of the pervasive availability of medical ‘facts’ online. Since we are unlikely to convince our patients to avoid the online milieu entirely, our role as health-care providers is to help our patients process and appropriately weigh the information that they receive, potentially partnering with our national societies to help curate such information.”
Dr. Schulman’s approach to the potential of patient misinformation is to initiate almost all discussions with patients with the question “Have your read or seen anything about this condition?” He said, “It is rare for patients to answer negatively. And listening to them speak about their understanding of their disease provides me with invaluable information about how the remainder of our visit should be spent. Do we need to correct misunderstandings? Are there gaps in the explanation that I can fill? Can we move directly into a conversation about treatment options? Can I provide you with some additional resources that might help to further your knowledge about the condition?”
Generational factors will play a big role in health-care demand and delivery. Health-care companies are already building lower cost delivery models to capture the millennial market.4 Cost-saving digital tools and virtual contacts are currently most commonly used by younger patients.5 Physicians need to understand and be a part of this trend, Dr. Schulman argued. “We should embrace telemedicine and mobile applications to collect data from the patients in their day-to-day lives. While insurance coverage of telemedicine is far from universal at the moment, and the reliability of mobile applications is highly variable, we know that a growing number of our patients are already relying on their digital devices to manage their health. In much the same way that we will need to help patient evaluate online information, we should work with our national societies to support the creation of tools that will allow us to collect data in the home environment in a more robust and reliable fashion.”
The proportion of the US population over the age of 65 is increasing yearly.6 Six out of 10 Americans live with a chronic illness, such as heart disease or diabetes. These and other chronic diseases are the leading drivers of the $3.3 billion annual health-care costs.7 Cost containment for these older patients and those with chronic illness will involve a focus on quality and outcomes data, a drive to deliver treatment in lower cost outpatient settings, and an acceleration of the adoption of value-based models currently underway.8
Taken together, these trends will mean a growing digital interface between physician and patient, a more active consumer-patient, and the availability of a vast array of new tools to access and manage health-care data.
- Delivery of procedures and services will trend from physicians to other members of the health-care team and to lower cost, outpatient settings.9
- Health-care systems will ramp up investment in products and services that improve outcomes and cost effectiveness.10
- Increased regulatory requirements and new payment models mean an ever-growing utilization of information technology by providers to fulfill data imperatives.11
- Physicians will have an increased need for tools that prioritize costs and outcomes data at the point of care.12
- Integration of data from new technologies will touch every aspect of health-care delivery with the objective of improving outcomes and, in turn, reducing costs.13
- Changing consumer attitudes toward delivery of care will be based on a growing familiarity of patients with a digital or virtual interface with providers, facility with health-care apps, and preference for a menu of options for health-care delivery.14
Dr. Schulman concluded, “We can no more expect our patients to ignore the full panoply of medical information on the internet and digital tools on their mobile devices than we can tell the tide not to come in. The die is cast; this is the world within which we must ply our trade. By identifying best practices and sharing our successes, we can come through this revolution better for the experience.”
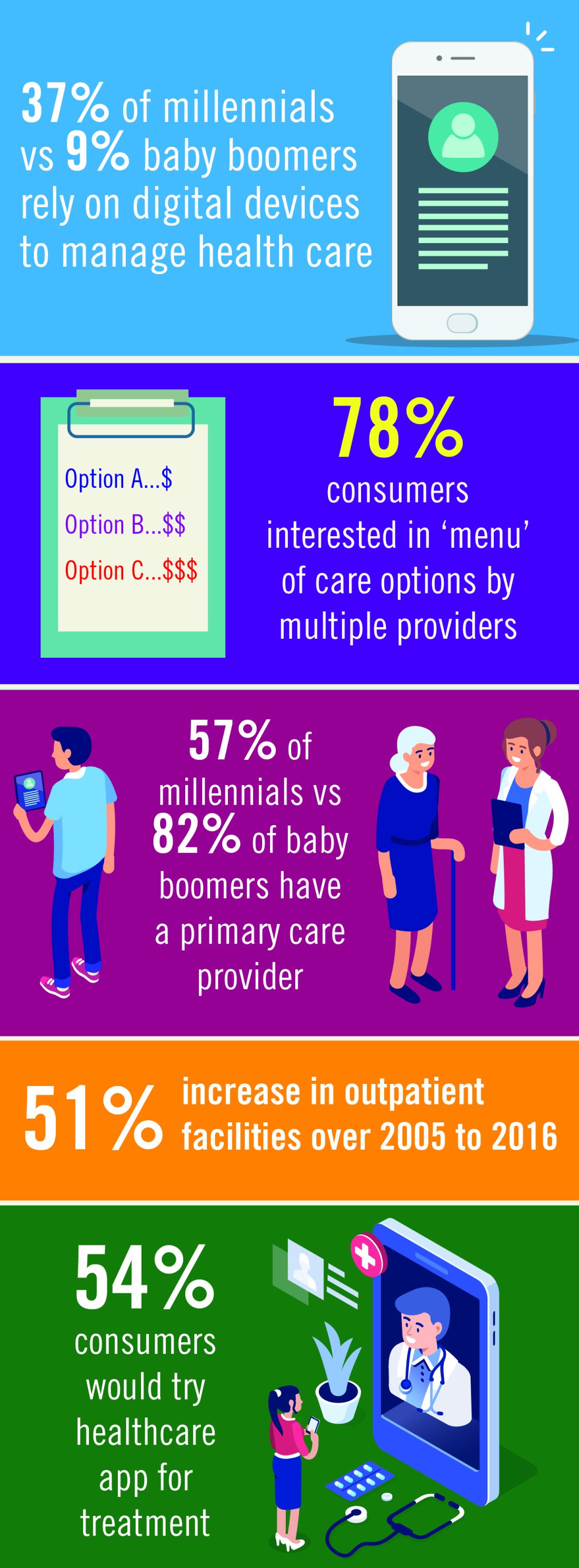
References
1. https://www.modernhealthcare.com/article/20181220/NEWS/181229992/number-of-outpatient-facilities-surges-as-industry-values-more
2. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
3. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
4. PcW Health Research Institute: Top health industry issues of 2019
5. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
6. https://www.census.gov/newsroom/press-releases/2017/cb17-100.html
7. https://www.cdc.gov/chronicdisease/index.htm
8. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/health-care-current-december4-2018.html
9. PcW Health Research Institute Top health industry issues of 2019: The New Health Economy comes of age
10. https://www.accenture.com/us-en/insights/health/digital-health-tech-vision-2018
11. https://www2.deloitte.com/insights/us/en/industry/life-sciences/medtech-research-and-development-innovation.html
12. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
13. https://www2.deloitte.com/insights/us/en/industry/health-care/volume-to-value-based-care.html
14. https://www.accenture.com/us-en/insights/health/digital-health-primary-care
FDA approves drug to treat low sexual desire in women
The .
“There are women who, for no known reason, have reduced sexual desire that causes marked distress, and who can benefit from safe and effective pharmacologic treatment,” Hylton V. Joffe, MD, director of the Center for Drug Evaluation and Research’s Division of Bone, Reproductive, and Urologic Products, stated in a press release. “Today’s approval provides women with another treatment option for this condition.”
HSDD is characterized by low sexual desire that causes marked distress or interpersonal difficulty and is not caused by a medical or psychiatric condition. Acquired HSDD develops in a patient who previously experienced no problems with sexual desire, and generalized HSDD is a lack of desire that occurs regardless of the type of sexual activity, situation, or partner.
Vyleesi was studied in two 24-week, randomized, double-blind, placebo-controlled trials in 1,247 premenopausal women with acquired, generalized HSDD. The women used Vyleesi two or three times per month and no more than once a week. About one-quarter of patients treated with Vyleesi had an increase of 1.2 or more in their sexual desire score (scored on a range of 1.2 to 6.0, with higher scores indicating greater sexual desire), compared with about 17% of those who took placebo. About 35% of the patients treated with Vyleesi had a decrease of one or more in their distress score (scored on a range of 0-4, with higher scores indicating greater distress from low sexual desire) compared with about 31% of those who took placebo.
The drug is injected under the skin of the abdomen or thigh at least 45 minutes before anticipated sexual activity. Patients may decide the optimal time to use Vyleesi based on the duration of benefit and any side effects, such as nausea. Patients should not take more than one dose of Vyleesi within 24 hours, or more than eight doses per month. Patients should discontinue treatment after 8 weeks if they do not report an improvement in sexual desire and associated distress.
Vyleesi works by activating melanocortin receptors but the exact mechanism for improving sexual desire is unknown. Some side effects were reported. “The most common side effects of Vyleesi are nausea and vomiting, flushing, injection site reactions, and headache. About 40% of patients in the clinical trials experienced nausea, most commonly with the first Vyleesi injection, and 13% needed medications for the treatment of nausea. About 1% of patients treated with Vyleesi in the clinical trials reported darkening of the gums and parts of the skin, including the face and breasts, which did not go away in about half the patients after stopping treatment. Patients with dark skin were more likely to develop this side effect,” according to the press release.
A temporary increase in blood pressure in patients after dosing with Vyleesi was observed during the clinical trials and therefore the drug is not recommended in patients at high risk for cardiovascular disease. In addition, patients who take a naltrexone-containing medication by mouth to treat alcohol or opioid dependence should not use Vyleesi because it may significantly decrease the levels of naltrexone in the blood and could lead to naltrexone treatment failure.
The full press release can be found on the FDA website.
The .
“There are women who, for no known reason, have reduced sexual desire that causes marked distress, and who can benefit from safe and effective pharmacologic treatment,” Hylton V. Joffe, MD, director of the Center for Drug Evaluation and Research’s Division of Bone, Reproductive, and Urologic Products, stated in a press release. “Today’s approval provides women with another treatment option for this condition.”
HSDD is characterized by low sexual desire that causes marked distress or interpersonal difficulty and is not caused by a medical or psychiatric condition. Acquired HSDD develops in a patient who previously experienced no problems with sexual desire, and generalized HSDD is a lack of desire that occurs regardless of the type of sexual activity, situation, or partner.
Vyleesi was studied in two 24-week, randomized, double-blind, placebo-controlled trials in 1,247 premenopausal women with acquired, generalized HSDD. The women used Vyleesi two or three times per month and no more than once a week. About one-quarter of patients treated with Vyleesi had an increase of 1.2 or more in their sexual desire score (scored on a range of 1.2 to 6.0, with higher scores indicating greater sexual desire), compared with about 17% of those who took placebo. About 35% of the patients treated with Vyleesi had a decrease of one or more in their distress score (scored on a range of 0-4, with higher scores indicating greater distress from low sexual desire) compared with about 31% of those who took placebo.
The drug is injected under the skin of the abdomen or thigh at least 45 minutes before anticipated sexual activity. Patients may decide the optimal time to use Vyleesi based on the duration of benefit and any side effects, such as nausea. Patients should not take more than one dose of Vyleesi within 24 hours, or more than eight doses per month. Patients should discontinue treatment after 8 weeks if they do not report an improvement in sexual desire and associated distress.
Vyleesi works by activating melanocortin receptors but the exact mechanism for improving sexual desire is unknown. Some side effects were reported. “The most common side effects of Vyleesi are nausea and vomiting, flushing, injection site reactions, and headache. About 40% of patients in the clinical trials experienced nausea, most commonly with the first Vyleesi injection, and 13% needed medications for the treatment of nausea. About 1% of patients treated with Vyleesi in the clinical trials reported darkening of the gums and parts of the skin, including the face and breasts, which did not go away in about half the patients after stopping treatment. Patients with dark skin were more likely to develop this side effect,” according to the press release.
A temporary increase in blood pressure in patients after dosing with Vyleesi was observed during the clinical trials and therefore the drug is not recommended in patients at high risk for cardiovascular disease. In addition, patients who take a naltrexone-containing medication by mouth to treat alcohol or opioid dependence should not use Vyleesi because it may significantly decrease the levels of naltrexone in the blood and could lead to naltrexone treatment failure.
The full press release can be found on the FDA website.
The .
“There are women who, for no known reason, have reduced sexual desire that causes marked distress, and who can benefit from safe and effective pharmacologic treatment,” Hylton V. Joffe, MD, director of the Center for Drug Evaluation and Research’s Division of Bone, Reproductive, and Urologic Products, stated in a press release. “Today’s approval provides women with another treatment option for this condition.”
HSDD is characterized by low sexual desire that causes marked distress or interpersonal difficulty and is not caused by a medical or psychiatric condition. Acquired HSDD develops in a patient who previously experienced no problems with sexual desire, and generalized HSDD is a lack of desire that occurs regardless of the type of sexual activity, situation, or partner.
Vyleesi was studied in two 24-week, randomized, double-blind, placebo-controlled trials in 1,247 premenopausal women with acquired, generalized HSDD. The women used Vyleesi two or three times per month and no more than once a week. About one-quarter of patients treated with Vyleesi had an increase of 1.2 or more in their sexual desire score (scored on a range of 1.2 to 6.0, with higher scores indicating greater sexual desire), compared with about 17% of those who took placebo. About 35% of the patients treated with Vyleesi had a decrease of one or more in their distress score (scored on a range of 0-4, with higher scores indicating greater distress from low sexual desire) compared with about 31% of those who took placebo.
The drug is injected under the skin of the abdomen or thigh at least 45 minutes before anticipated sexual activity. Patients may decide the optimal time to use Vyleesi based on the duration of benefit and any side effects, such as nausea. Patients should not take more than one dose of Vyleesi within 24 hours, or more than eight doses per month. Patients should discontinue treatment after 8 weeks if they do not report an improvement in sexual desire and associated distress.
Vyleesi works by activating melanocortin receptors but the exact mechanism for improving sexual desire is unknown. Some side effects were reported. “The most common side effects of Vyleesi are nausea and vomiting, flushing, injection site reactions, and headache. About 40% of patients in the clinical trials experienced nausea, most commonly with the first Vyleesi injection, and 13% needed medications for the treatment of nausea. About 1% of patients treated with Vyleesi in the clinical trials reported darkening of the gums and parts of the skin, including the face and breasts, which did not go away in about half the patients after stopping treatment. Patients with dark skin were more likely to develop this side effect,” according to the press release.
A temporary increase in blood pressure in patients after dosing with Vyleesi was observed during the clinical trials and therefore the drug is not recommended in patients at high risk for cardiovascular disease. In addition, patients who take a naltrexone-containing medication by mouth to treat alcohol or opioid dependence should not use Vyleesi because it may significantly decrease the levels of naltrexone in the blood and could lead to naltrexone treatment failure.
The full press release can be found on the FDA website.
FDA warns of possible temporary shortage of trach tube
manufactured by Smiths Medical caused by the closure of a large ethylene oxide sterilization facilities in Willowbrook, Ill., and the future planned closure of a similar facility.
The shortage may affect pediatric use because, although tubes are used for both adults and children, there are fewer alternative products on the market for pediatric patients. Parents and caregivers of children who use the Bivona tube are encouraged to check with Smiths Medical about available inventory and with their health care providers about alternative products.
Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in a press release, “I want to assure you that the FDA is working closely with the company to quickly resolve their sterilization challenges and bring these critical devices to the patients who need them as quickly as possible, which we anticipate will be made available again beginning the week of April 22.”
For patients currently using the Bivona tubes, Dr. Shuren noted, “The closure of the Willowbrook facility does not impact tubes already in use by patients at home or in health care settings. The company is communicating with patients about the tubes and how patients and caregivers can mitigate any potential impact, including reusing and cleaning tubes in accordance with the manufacturer’s instructions for use.”
Read the entire announcement at the FDA website.
manufactured by Smiths Medical caused by the closure of a large ethylene oxide sterilization facilities in Willowbrook, Ill., and the future planned closure of a similar facility.
The shortage may affect pediatric use because, although tubes are used for both adults and children, there are fewer alternative products on the market for pediatric patients. Parents and caregivers of children who use the Bivona tube are encouraged to check with Smiths Medical about available inventory and with their health care providers about alternative products.
Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in a press release, “I want to assure you that the FDA is working closely with the company to quickly resolve their sterilization challenges and bring these critical devices to the patients who need them as quickly as possible, which we anticipate will be made available again beginning the week of April 22.”
For patients currently using the Bivona tubes, Dr. Shuren noted, “The closure of the Willowbrook facility does not impact tubes already in use by patients at home or in health care settings. The company is communicating with patients about the tubes and how patients and caregivers can mitigate any potential impact, including reusing and cleaning tubes in accordance with the manufacturer’s instructions for use.”
Read the entire announcement at the FDA website.
manufactured by Smiths Medical caused by the closure of a large ethylene oxide sterilization facilities in Willowbrook, Ill., and the future planned closure of a similar facility.
The shortage may affect pediatric use because, although tubes are used for both adults and children, there are fewer alternative products on the market for pediatric patients. Parents and caregivers of children who use the Bivona tube are encouraged to check with Smiths Medical about available inventory and with their health care providers about alternative products.
Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in a press release, “I want to assure you that the FDA is working closely with the company to quickly resolve their sterilization challenges and bring these critical devices to the patients who need them as quickly as possible, which we anticipate will be made available again beginning the week of April 22.”
For patients currently using the Bivona tubes, Dr. Shuren noted, “The closure of the Willowbrook facility does not impact tubes already in use by patients at home or in health care settings. The company is communicating with patients about the tubes and how patients and caregivers can mitigate any potential impact, including reusing and cleaning tubes in accordance with the manufacturer’s instructions for use.”
Read the entire announcement at the FDA website.