User login
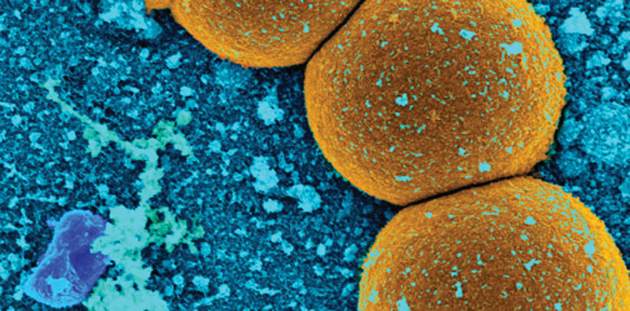
MRSA Prevalence in Asymptomatic Athletes Comparable to Dialysis, HIV Patients
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
FROM CLINICAL INFECTIOUS DISEASES
MRSA prevalence in asymptomatic athletes comparable to dialysis, HIV patients
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is comparable to that among individuals with chronic illnesses.
Major finding: The prevalence of MRSA colonization was 8% among U.S. athletes and 13% among U.S. collegiate athletes. The prevalence of MRSA in the total athletic population was comparable to MRSA in patients with illnesses such as kidney disease and HIV.
Data source: A PubMed and EMBASE search yielded 382 studies and was narrowed to 15 analyses.
Disclosures: The investigators declared no conflicts of interest.
Cognitive behavioral therapy alternative helps depressed teens
Depressed teens who initially declined antidepressants and received brief cognitive behavioral therapy (CBT) in a primary care setting were more likely to recover, and to recover faster, compared with similar young people who received usual care but not CBT, according to a randomized study of 212 adolescents.
From 10% to 15% of adolescents experience depression each year, and many refuse to take antidepressants or stop them before they have a chance to work. One alternative is a referral to a mental health specialty clinic; however, less than 30% of teens and their parents follow up on these referrals, according to Greg Clarke, Ph.D., of Kaiser Permanente Center for Health Research, and his colleagues.
Brief CBT offered small to moderate clinical benefit that persisted for at least 1 year. On average, teens in the CBT program recovered 7 weeks faster (22.6 weeks vs. 30 weeks) and in higher numbers (33% more recovery) compared with teens who didn’t receive CBT. After 6 months, 70% of teens in the CBT program had recovered, compared with 43% of teens not in the program.
By the end of the 2-year study, 89% who received CBT counseling and 79% in the standard care group had recovered (Pediatrics 2016 May. doi: 10.1542/peds.2015-1851).
But the youth in the CBT group were 10 times less likely to be hospitalized. “We were not surprised that CBT helped improve depression, but the much lower rates of psychiatric hospitalization was a welcome surprise. Offering brief CBT in primary care is an effective alternative with good results,” Dr. Clarke said in an interview.
Study participants had a diagnosis of major depression obtained via the Children’s Schedule for Affective Disorders and Schizophrenia (KSADS). Youth were randomized to either self-selected treatment (i.e., outpatient mental health, medication, school counseling, treatment for alcohol or drug abuse) or to self-selected treatment plus a 5- to 9-week CBT program within their primary care clinics. Counselors used traditional CBT techniques to help teens challenge depressive thoughts and replace those beliefs with more realistic, positive approaches.
Randomization was stratified by baseline depression severity, gender, Hispanic ethnicity, and age (12-15 years vs. 16-18 years). Researchers assessed these young people at baseline and followed them for 2 years, having them fill out follow-up surveys at 6, 12, 26, 52, 78, and 104 weeks. Those who assessed the surveys did not know which teens received CBT.
The acute-phase CBT program consisted of two four-session modules: cognitive therapy to address unrealistic thinking, and increasing pleasant activities (behavioral activation). Of those attending any sessions, 66% of 102 received at least one session of cognitive therapy, 62% received at least one session of behavioral activation, and 45% received both.
The National Institutes of Health funded the study. The researchers had no relevant disclosures.
Depressed teens who initially declined antidepressants and received brief cognitive behavioral therapy (CBT) in a primary care setting were more likely to recover, and to recover faster, compared with similar young people who received usual care but not CBT, according to a randomized study of 212 adolescents.
From 10% to 15% of adolescents experience depression each year, and many refuse to take antidepressants or stop them before they have a chance to work. One alternative is a referral to a mental health specialty clinic; however, less than 30% of teens and their parents follow up on these referrals, according to Greg Clarke, Ph.D., of Kaiser Permanente Center for Health Research, and his colleagues.
Brief CBT offered small to moderate clinical benefit that persisted for at least 1 year. On average, teens in the CBT program recovered 7 weeks faster (22.6 weeks vs. 30 weeks) and in higher numbers (33% more recovery) compared with teens who didn’t receive CBT. After 6 months, 70% of teens in the CBT program had recovered, compared with 43% of teens not in the program.
By the end of the 2-year study, 89% who received CBT counseling and 79% in the standard care group had recovered (Pediatrics 2016 May. doi: 10.1542/peds.2015-1851).
But the youth in the CBT group were 10 times less likely to be hospitalized. “We were not surprised that CBT helped improve depression, but the much lower rates of psychiatric hospitalization was a welcome surprise. Offering brief CBT in primary care is an effective alternative with good results,” Dr. Clarke said in an interview.
Study participants had a diagnosis of major depression obtained via the Children’s Schedule for Affective Disorders and Schizophrenia (KSADS). Youth were randomized to either self-selected treatment (i.e., outpatient mental health, medication, school counseling, treatment for alcohol or drug abuse) or to self-selected treatment plus a 5- to 9-week CBT program within their primary care clinics. Counselors used traditional CBT techniques to help teens challenge depressive thoughts and replace those beliefs with more realistic, positive approaches.
Randomization was stratified by baseline depression severity, gender, Hispanic ethnicity, and age (12-15 years vs. 16-18 years). Researchers assessed these young people at baseline and followed them for 2 years, having them fill out follow-up surveys at 6, 12, 26, 52, 78, and 104 weeks. Those who assessed the surveys did not know which teens received CBT.
The acute-phase CBT program consisted of two four-session modules: cognitive therapy to address unrealistic thinking, and increasing pleasant activities (behavioral activation). Of those attending any sessions, 66% of 102 received at least one session of cognitive therapy, 62% received at least one session of behavioral activation, and 45% received both.
The National Institutes of Health funded the study. The researchers had no relevant disclosures.
Depressed teens who initially declined antidepressants and received brief cognitive behavioral therapy (CBT) in a primary care setting were more likely to recover, and to recover faster, compared with similar young people who received usual care but not CBT, according to a randomized study of 212 adolescents.
From 10% to 15% of adolescents experience depression each year, and many refuse to take antidepressants or stop them before they have a chance to work. One alternative is a referral to a mental health specialty clinic; however, less than 30% of teens and their parents follow up on these referrals, according to Greg Clarke, Ph.D., of Kaiser Permanente Center for Health Research, and his colleagues.
Brief CBT offered small to moderate clinical benefit that persisted for at least 1 year. On average, teens in the CBT program recovered 7 weeks faster (22.6 weeks vs. 30 weeks) and in higher numbers (33% more recovery) compared with teens who didn’t receive CBT. After 6 months, 70% of teens in the CBT program had recovered, compared with 43% of teens not in the program.
By the end of the 2-year study, 89% who received CBT counseling and 79% in the standard care group had recovered (Pediatrics 2016 May. doi: 10.1542/peds.2015-1851).
But the youth in the CBT group were 10 times less likely to be hospitalized. “We were not surprised that CBT helped improve depression, but the much lower rates of psychiatric hospitalization was a welcome surprise. Offering brief CBT in primary care is an effective alternative with good results,” Dr. Clarke said in an interview.
Study participants had a diagnosis of major depression obtained via the Children’s Schedule for Affective Disorders and Schizophrenia (KSADS). Youth were randomized to either self-selected treatment (i.e., outpatient mental health, medication, school counseling, treatment for alcohol or drug abuse) or to self-selected treatment plus a 5- to 9-week CBT program within their primary care clinics. Counselors used traditional CBT techniques to help teens challenge depressive thoughts and replace those beliefs with more realistic, positive approaches.
Randomization was stratified by baseline depression severity, gender, Hispanic ethnicity, and age (12-15 years vs. 16-18 years). Researchers assessed these young people at baseline and followed them for 2 years, having them fill out follow-up surveys at 6, 12, 26, 52, 78, and 104 weeks. Those who assessed the surveys did not know which teens received CBT.
The acute-phase CBT program consisted of two four-session modules: cognitive therapy to address unrealistic thinking, and increasing pleasant activities (behavioral activation). Of those attending any sessions, 66% of 102 received at least one session of cognitive therapy, 62% received at least one session of behavioral activation, and 45% received both.
The National Institutes of Health funded the study. The researchers had no relevant disclosures.
FROM PEDIATRICS
Key clinical point: Cognitive behavioral therapy can be used in primary care for teens who have major depression and refuse antidepressants.
Major finding: On average, teens in the CBT program recovered 7 weeks faster (22.6 weeks vs. 30 weeks) and in higher numbers (33% more recovery) compared with teens who didn’t receive CBT.
Data source: Researchers enrolled 212 adolescents aged 12-18 years who were diagnosed with depression and refused or stopped taking their antidepressants.
Disclosures: The National Institutes of Health funded the study. The researchers had no relevant disclosures.
Rosacea linked to several autoimmune diseases in women
Rosacea in women is linked with an increased risk for a wide variety of autoimmune disorders including type 1 diabetes, celiac disease, multiple sclerosis, and rheumatoid arthritis, according to a large population-based case-control study.
The finding expands the association of rosacea and autoimmune diseases beyond the previously reported associations with type 1 diabetes and celiac disease, reported Dr. Alexander Egeberg of Herlev and Gentofte Hospital, University of Copenhagen, and colleagues (J Am Acad Dermatol. 2016;74:667-72.)
“Remember that the absolute risk is still low; having rosacea does not guarantee that patients will develop other autoimmune diseases, and vice versa,” Dr. Egeberg said in an interview. “The links may provide insight into the pathogenesis of these diseases, and it will be interesting to see if systemic treatment of rosacea also affects the autoimmune diseases and the other way around.”
Using Danish registered health records, the researchers found 6,759 patients with rosacea, and matched them by age and sex to 33,795 control subjects. About two-thirds of the patients were women.
Compared with their matched controls, people with rosacea were at least twice as likely to have type 1 diabetes, celiac disease, and rheumatoid arthritis (odds ratio 2.6 for type 1 diabetes, 2.0 for celiac disease, and 2.1 for rheumatoid arthritis) and 1.65 times as likely to have multiple sclerosis. The differences, with the exception of rheumatoid arthritis, were statistically significant only in women.
The researchers said the broader association with autoimmune comorbidities is “intriguing” and suggests the genetic component of rosacea could be stronger than previously assumed with autoimmune inflammatory pathways contributing to the disease course. Because distinct rosacea subtypes (erythematotelangiectatic, papulopustular, phymatous, and ocular) could be associated with specific comorbidities, future association studies should attempt to stratify for clinical subtypes of rosacea, they noted.
Rosacea in women is linked with an increased risk for a wide variety of autoimmune disorders including type 1 diabetes, celiac disease, multiple sclerosis, and rheumatoid arthritis, according to a large population-based case-control study.
The finding expands the association of rosacea and autoimmune diseases beyond the previously reported associations with type 1 diabetes and celiac disease, reported Dr. Alexander Egeberg of Herlev and Gentofte Hospital, University of Copenhagen, and colleagues (J Am Acad Dermatol. 2016;74:667-72.)
“Remember that the absolute risk is still low; having rosacea does not guarantee that patients will develop other autoimmune diseases, and vice versa,” Dr. Egeberg said in an interview. “The links may provide insight into the pathogenesis of these diseases, and it will be interesting to see if systemic treatment of rosacea also affects the autoimmune diseases and the other way around.”
Using Danish registered health records, the researchers found 6,759 patients with rosacea, and matched them by age and sex to 33,795 control subjects. About two-thirds of the patients were women.
Compared with their matched controls, people with rosacea were at least twice as likely to have type 1 diabetes, celiac disease, and rheumatoid arthritis (odds ratio 2.6 for type 1 diabetes, 2.0 for celiac disease, and 2.1 for rheumatoid arthritis) and 1.65 times as likely to have multiple sclerosis. The differences, with the exception of rheumatoid arthritis, were statistically significant only in women.
The researchers said the broader association with autoimmune comorbidities is “intriguing” and suggests the genetic component of rosacea could be stronger than previously assumed with autoimmune inflammatory pathways contributing to the disease course. Because distinct rosacea subtypes (erythematotelangiectatic, papulopustular, phymatous, and ocular) could be associated with specific comorbidities, future association studies should attempt to stratify for clinical subtypes of rosacea, they noted.
Rosacea in women is linked with an increased risk for a wide variety of autoimmune disorders including type 1 diabetes, celiac disease, multiple sclerosis, and rheumatoid arthritis, according to a large population-based case-control study.
The finding expands the association of rosacea and autoimmune diseases beyond the previously reported associations with type 1 diabetes and celiac disease, reported Dr. Alexander Egeberg of Herlev and Gentofte Hospital, University of Copenhagen, and colleagues (J Am Acad Dermatol. 2016;74:667-72.)
“Remember that the absolute risk is still low; having rosacea does not guarantee that patients will develop other autoimmune diseases, and vice versa,” Dr. Egeberg said in an interview. “The links may provide insight into the pathogenesis of these diseases, and it will be interesting to see if systemic treatment of rosacea also affects the autoimmune diseases and the other way around.”
Using Danish registered health records, the researchers found 6,759 patients with rosacea, and matched them by age and sex to 33,795 control subjects. About two-thirds of the patients were women.
Compared with their matched controls, people with rosacea were at least twice as likely to have type 1 diabetes, celiac disease, and rheumatoid arthritis (odds ratio 2.6 for type 1 diabetes, 2.0 for celiac disease, and 2.1 for rheumatoid arthritis) and 1.65 times as likely to have multiple sclerosis. The differences, with the exception of rheumatoid arthritis, were statistically significant only in women.
The researchers said the broader association with autoimmune comorbidities is “intriguing” and suggests the genetic component of rosacea could be stronger than previously assumed with autoimmune inflammatory pathways contributing to the disease course. Because distinct rosacea subtypes (erythematotelangiectatic, papulopustular, phymatous, and ocular) could be associated with specific comorbidities, future association studies should attempt to stratify for clinical subtypes of rosacea, they noted.
FROM JAAD
Key clinical point: Rosacea is linked with a broader spectrum of autoimmune diseases than previously recognized.
Major finding: Women with rosacea were more likely than were other women to have type 1 diabetes, celiac disease, multiple sclerosis, and rheumatoid arthritis.
Data source: A population-based case-control study of 6,759 patients with rosacea who were matched with 33,795 control subjects for age, sex, and calendar time.
Disclosures: Dr. Egeberg is employed by Pfizer. This research was performed independently through the authors’ academic university.