User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Osteoporosis risk rises with air pollution levels
COPENHAGEN – Chronic exposure to high levels of particulate matter (PM) air pollution 2.5 mcm (PM2.5) or larger, and 10 mcm (PM10) or larger, in size is associated with a significantly higher likelihood of having osteoporosis, according to research presented at the annual European Congress of Rheumatology.
The results of the 7-year longitudinal study carried out across Italy from 2013 to 2019 dovetail with other recent published accounts from the same team of Italian researchers, led by Giovanni Adami, MD, of the rheumatology unit at the University of Verona (Italy). In addition to the current report presented at EULAR 2022, Dr. Adami and associates have reported an increased risk of flares of both rheumatoid arthritis and psoriasis following periods of elevated pollution, as well as an overall elevated risk for autoimmune diseases with higher concentrations of PM2.5 and PM10.
The pathogenesis of osteoporosis is thought to involve both genetic and environmental input, such as smoking, which is itself environmental air pollution, Dr. Adami said. The biological rationale for why air pollution might contribute to risk for osteoporosis comes from studies showing that exposure to indoor air pollution from biomass combustion raises serum levels of RANKL (receptor activator of nuclear factor-kappa ligand 1) but lowers serum osteoprotegerin – suggesting an increased risk of bone resorption – and that toxic metals such as lead, cadmium, mercury, and aluminum accumulate in the skeleton and negatively affect bone health.
In their study, Dr. Adami and colleagues found that, overall, the average exposure during the period 2013-2019 across Italy was 16.0 mcg/m3 for PM2.5 and 25.0 mcg/m3 for PM10.
“I can tell you that [25.0 mcg/m3 for PM10] is a very high exposure. It’s not very good for your health,” Dr. Adami said.
Data on more than 59,000 Italian women
Dr. Adami and colleagues used clinical characteristics and densitometric data from Italy’s osteoporosis fracture risk and osteoporosis screening reimbursement tool known as DeFRAcalc79, which has amassed variables from more than 59,000 women across the country. They used long-term average PM concentrations across Italy during 2013-2019 that were obtained from the Italian Institute for Environmental Protection and Research’s 617 air quality stations in 110 Italian provinces. The researchers linked individuals to a PM exposure value determined from the average concentration of urban, rural, and near-traffic stations in each person’s province of residence.
For 59,950 women across Italy who were at high risk for fracture, the researchers found 64.5% with bone mineral density that was defined as osteoporotic. At PM10 concentrations of 30 mcg/m3 or greater, there was a significantly higher likelihood of osteoporosis at both the femoral neck (odds ratio, 1.15) and lumbar spine (OR, 1.17).
The likelihood of osteoporosis was slightly greater with PM2.5 at concentrations of 25 mcg/m3 or more at the femoral neck (OR, 1.22) and lumbar spine (OR, 1.18). These comparisons were adjusted for age, body mass index (BMI), presence of prevalent fragility fractures, family history of osteoporosis, menopause, glucocorticoid use, comorbidities, and for residency in northern, central, or southern Italy.
Both thresholds of PM10 > 30 mcg/m3 and PM2.5 > 25 mcg/m3 “are considered safe … by the World Health Organization,” Dr. Adami pointed out.
“If you live in a place where the chronic exposure is less than 30 mcg/m3, you probably have slightly lower risk of osteoporosis as compared to those who live in a highly industrialized, polluted zone,” he explained.
“The cortical bone – femoral neck – seemed to be more susceptible, compared to trabecular bone, which is the lumbar spine. We have no idea why this is true, but we might speculate that somehow chronic inflammation like the [kind] seen in rheumatoid arthritis might be responsible for cortical bone impairment and not trabecular bone impairment,” Dr. Adami said.
One audience member, Kenneth Poole, BM, PhD, senior lecturer and honorary consultant in Metabolic Bone Disease and Rheumatology at the University of Cambridge (England), asked whether it was possible to account for the possibility of confounding caused by areas with dense housing in places where the particulate matter would be highest, and where residents may be less active and use stairs less often.
Dr. Adami noted that confounding is indeed a possibility, but he said Italy is unique in that its most polluted area – the Po River valley – is also its most wealthy area and in general has less crowded living situations with a healthier population, which could have attenuated, rather than reinforced, the results.
Does air pollution have an immunologic effect?
In interviews with this news organization, session comoderators Filipe Araújo, MD, and Irene Bultink, MD, PhD, said that the growth in evidence for the impact of air pollution on risk for, and severity of, various diseases suggests air pollution might have an immunologic effect.
“I think it’s very important to point this out. I also think it’s very hard to rule out confounding, because when you’re living in a city with crowded housing you may not walk or ride your bike but instead go by car or metro, and [the lifestyle is different],” said Dr. Bultink of Amsterdam University Medical Centers.
“It stresses that these diseases [that are associated with air pollution] although they are different in their pathophysiology, it points toward the systemic nature of rheumatic diseases, including osteoporosis,” said Dr. Araújo of Hospital Cuf Cascais (Portugal) and Hospital Ortopédico de Sant’Ana, Parede, Portugal.
The study was independently supported.Dr. Adami disclosed being a shareholder of Galapagos and Theramex.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Chronic exposure to high levels of particulate matter (PM) air pollution 2.5 mcm (PM2.5) or larger, and 10 mcm (PM10) or larger, in size is associated with a significantly higher likelihood of having osteoporosis, according to research presented at the annual European Congress of Rheumatology.
The results of the 7-year longitudinal study carried out across Italy from 2013 to 2019 dovetail with other recent published accounts from the same team of Italian researchers, led by Giovanni Adami, MD, of the rheumatology unit at the University of Verona (Italy). In addition to the current report presented at EULAR 2022, Dr. Adami and associates have reported an increased risk of flares of both rheumatoid arthritis and psoriasis following periods of elevated pollution, as well as an overall elevated risk for autoimmune diseases with higher concentrations of PM2.5 and PM10.
The pathogenesis of osteoporosis is thought to involve both genetic and environmental input, such as smoking, which is itself environmental air pollution, Dr. Adami said. The biological rationale for why air pollution might contribute to risk for osteoporosis comes from studies showing that exposure to indoor air pollution from biomass combustion raises serum levels of RANKL (receptor activator of nuclear factor-kappa ligand 1) but lowers serum osteoprotegerin – suggesting an increased risk of bone resorption – and that toxic metals such as lead, cadmium, mercury, and aluminum accumulate in the skeleton and negatively affect bone health.
In their study, Dr. Adami and colleagues found that, overall, the average exposure during the period 2013-2019 across Italy was 16.0 mcg/m3 for PM2.5 and 25.0 mcg/m3 for PM10.
“I can tell you that [25.0 mcg/m3 for PM10] is a very high exposure. It’s not very good for your health,” Dr. Adami said.
Data on more than 59,000 Italian women
Dr. Adami and colleagues used clinical characteristics and densitometric data from Italy’s osteoporosis fracture risk and osteoporosis screening reimbursement tool known as DeFRAcalc79, which has amassed variables from more than 59,000 women across the country. They used long-term average PM concentrations across Italy during 2013-2019 that were obtained from the Italian Institute for Environmental Protection and Research’s 617 air quality stations in 110 Italian provinces. The researchers linked individuals to a PM exposure value determined from the average concentration of urban, rural, and near-traffic stations in each person’s province of residence.
For 59,950 women across Italy who were at high risk for fracture, the researchers found 64.5% with bone mineral density that was defined as osteoporotic. At PM10 concentrations of 30 mcg/m3 or greater, there was a significantly higher likelihood of osteoporosis at both the femoral neck (odds ratio, 1.15) and lumbar spine (OR, 1.17).
The likelihood of osteoporosis was slightly greater with PM2.5 at concentrations of 25 mcg/m3 or more at the femoral neck (OR, 1.22) and lumbar spine (OR, 1.18). These comparisons were adjusted for age, body mass index (BMI), presence of prevalent fragility fractures, family history of osteoporosis, menopause, glucocorticoid use, comorbidities, and for residency in northern, central, or southern Italy.
Both thresholds of PM10 > 30 mcg/m3 and PM2.5 > 25 mcg/m3 “are considered safe … by the World Health Organization,” Dr. Adami pointed out.
“If you live in a place where the chronic exposure is less than 30 mcg/m3, you probably have slightly lower risk of osteoporosis as compared to those who live in a highly industrialized, polluted zone,” he explained.
“The cortical bone – femoral neck – seemed to be more susceptible, compared to trabecular bone, which is the lumbar spine. We have no idea why this is true, but we might speculate that somehow chronic inflammation like the [kind] seen in rheumatoid arthritis might be responsible for cortical bone impairment and not trabecular bone impairment,” Dr. Adami said.
One audience member, Kenneth Poole, BM, PhD, senior lecturer and honorary consultant in Metabolic Bone Disease and Rheumatology at the University of Cambridge (England), asked whether it was possible to account for the possibility of confounding caused by areas with dense housing in places where the particulate matter would be highest, and where residents may be less active and use stairs less often.
Dr. Adami noted that confounding is indeed a possibility, but he said Italy is unique in that its most polluted area – the Po River valley – is also its most wealthy area and in general has less crowded living situations with a healthier population, which could have attenuated, rather than reinforced, the results.
Does air pollution have an immunologic effect?
In interviews with this news organization, session comoderators Filipe Araújo, MD, and Irene Bultink, MD, PhD, said that the growth in evidence for the impact of air pollution on risk for, and severity of, various diseases suggests air pollution might have an immunologic effect.
“I think it’s very important to point this out. I also think it’s very hard to rule out confounding, because when you’re living in a city with crowded housing you may not walk or ride your bike but instead go by car or metro, and [the lifestyle is different],” said Dr. Bultink of Amsterdam University Medical Centers.
“It stresses that these diseases [that are associated with air pollution] although they are different in their pathophysiology, it points toward the systemic nature of rheumatic diseases, including osteoporosis,” said Dr. Araújo of Hospital Cuf Cascais (Portugal) and Hospital Ortopédico de Sant’Ana, Parede, Portugal.
The study was independently supported.Dr. Adami disclosed being a shareholder of Galapagos and Theramex.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Chronic exposure to high levels of particulate matter (PM) air pollution 2.5 mcm (PM2.5) or larger, and 10 mcm (PM10) or larger, in size is associated with a significantly higher likelihood of having osteoporosis, according to research presented at the annual European Congress of Rheumatology.
The results of the 7-year longitudinal study carried out across Italy from 2013 to 2019 dovetail with other recent published accounts from the same team of Italian researchers, led by Giovanni Adami, MD, of the rheumatology unit at the University of Verona (Italy). In addition to the current report presented at EULAR 2022, Dr. Adami and associates have reported an increased risk of flares of both rheumatoid arthritis and psoriasis following periods of elevated pollution, as well as an overall elevated risk for autoimmune diseases with higher concentrations of PM2.5 and PM10.
The pathogenesis of osteoporosis is thought to involve both genetic and environmental input, such as smoking, which is itself environmental air pollution, Dr. Adami said. The biological rationale for why air pollution might contribute to risk for osteoporosis comes from studies showing that exposure to indoor air pollution from biomass combustion raises serum levels of RANKL (receptor activator of nuclear factor-kappa ligand 1) but lowers serum osteoprotegerin – suggesting an increased risk of bone resorption – and that toxic metals such as lead, cadmium, mercury, and aluminum accumulate in the skeleton and negatively affect bone health.
In their study, Dr. Adami and colleagues found that, overall, the average exposure during the period 2013-2019 across Italy was 16.0 mcg/m3 for PM2.5 and 25.0 mcg/m3 for PM10.
“I can tell you that [25.0 mcg/m3 for PM10] is a very high exposure. It’s not very good for your health,” Dr. Adami said.
Data on more than 59,000 Italian women
Dr. Adami and colleagues used clinical characteristics and densitometric data from Italy’s osteoporosis fracture risk and osteoporosis screening reimbursement tool known as DeFRAcalc79, which has amassed variables from more than 59,000 women across the country. They used long-term average PM concentrations across Italy during 2013-2019 that were obtained from the Italian Institute for Environmental Protection and Research’s 617 air quality stations in 110 Italian provinces. The researchers linked individuals to a PM exposure value determined from the average concentration of urban, rural, and near-traffic stations in each person’s province of residence.
For 59,950 women across Italy who were at high risk for fracture, the researchers found 64.5% with bone mineral density that was defined as osteoporotic. At PM10 concentrations of 30 mcg/m3 or greater, there was a significantly higher likelihood of osteoporosis at both the femoral neck (odds ratio, 1.15) and lumbar spine (OR, 1.17).
The likelihood of osteoporosis was slightly greater with PM2.5 at concentrations of 25 mcg/m3 or more at the femoral neck (OR, 1.22) and lumbar spine (OR, 1.18). These comparisons were adjusted for age, body mass index (BMI), presence of prevalent fragility fractures, family history of osteoporosis, menopause, glucocorticoid use, comorbidities, and for residency in northern, central, or southern Italy.
Both thresholds of PM10 > 30 mcg/m3 and PM2.5 > 25 mcg/m3 “are considered safe … by the World Health Organization,” Dr. Adami pointed out.
“If you live in a place where the chronic exposure is less than 30 mcg/m3, you probably have slightly lower risk of osteoporosis as compared to those who live in a highly industrialized, polluted zone,” he explained.
“The cortical bone – femoral neck – seemed to be more susceptible, compared to trabecular bone, which is the lumbar spine. We have no idea why this is true, but we might speculate that somehow chronic inflammation like the [kind] seen in rheumatoid arthritis might be responsible for cortical bone impairment and not trabecular bone impairment,” Dr. Adami said.
One audience member, Kenneth Poole, BM, PhD, senior lecturer and honorary consultant in Metabolic Bone Disease and Rheumatology at the University of Cambridge (England), asked whether it was possible to account for the possibility of confounding caused by areas with dense housing in places where the particulate matter would be highest, and where residents may be less active and use stairs less often.
Dr. Adami noted that confounding is indeed a possibility, but he said Italy is unique in that its most polluted area – the Po River valley – is also its most wealthy area and in general has less crowded living situations with a healthier population, which could have attenuated, rather than reinforced, the results.
Does air pollution have an immunologic effect?
In interviews with this news organization, session comoderators Filipe Araújo, MD, and Irene Bultink, MD, PhD, said that the growth in evidence for the impact of air pollution on risk for, and severity of, various diseases suggests air pollution might have an immunologic effect.
“I think it’s very important to point this out. I also think it’s very hard to rule out confounding, because when you’re living in a city with crowded housing you may not walk or ride your bike but instead go by car or metro, and [the lifestyle is different],” said Dr. Bultink of Amsterdam University Medical Centers.
“It stresses that these diseases [that are associated with air pollution] although they are different in their pathophysiology, it points toward the systemic nature of rheumatic diseases, including osteoporosis,” said Dr. Araújo of Hospital Cuf Cascais (Portugal) and Hospital Ortopédico de Sant’Ana, Parede, Portugal.
The study was independently supported.Dr. Adami disclosed being a shareholder of Galapagos and Theramex.
A version of this article first appeared on Medscape.com.
AT THE EULAR 2022 CONGRESS
What are the signs of post–acute infection syndromes?
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
HPV vaccination with Cervarix ‘unmasks’ cervical lesions from non-vax strains
Vaccines against human papillomavirus have been hailed as a success: they have been shown to decrease the incidence of cervical lesions associated with the HPV types that are in the vaccine.
However,
An expert not involved in the research said the new data “tell us to be a little bit careful.” Although the HPV types not included in the vaccine are rarer and less aggressive, they can still cause cancer.
The data come from the Costa Rica HPV Vaccine Trial, which involved more than 10,000 women aged 18-25 years. The HPV vaccine used in the trial was Cervarix, from GlaxoSmithKline. It covers the two leading causes of cervical cancer, HPV-16 and -18, and provides partial protection against three other genotypes.
After a follow-up of 11 years, among vaccinated women, there was an excess of precancerous cervical lesions caused by genotypes not included in the vaccine, resulting in negative vaccine efficacy for those HPV variants.
The increase wasn’t enough to offset the overall benefit of vaccination when all genotypes were considered, said the researchers, led by Jaimie Shing, PhD, a postdoctoral research fellow at the National Cancer Institute in Bethesda, Md.
Vaccinated women “still had long-term absolute reductions in high-grade lesions,” they pointed out.
The net protection “remained considerable, emphasizing the importance of HPV vaccination for cervical cancer prevention,” the team concluded.
The findings were published online in The Lancet Oncology.
The results are likely the first evidence to date of “clinical unmasking” with HPV vaccination, meaning that protection against the strains covered by the vaccine leaves women more prone to attack from other carcinogenic HPV variants.
This phenomenon “could attenuate long-term reductions in high-grade disease following successful implementation of HPV vaccination programs,” the investigators commented.
Highlighting a need for caution
The take-home message from the trial is that “we have to be careful,” said Marc Steben, MD, co-President of HPV Global Action and a professor at the University of Montreal.
He noted that the Cervarix HPV vaccine used in the trial is not the vaccine that is used now in developed nations.
The current standard HPV vaccine is Gardasil 9 (Merck), which offers broader coverage against nine HPV types (types 6, 11, 16, 18, 31, 33, 45, 52, and 58).
There are 12 main carcinogenic HPV genotypes, so unmasking of other strains is still possible with Gardasil 9, he said.
There is another issue, Dr. Steben added. The success of HPV vaccinations - a nearly 90% reduction in invasive cervical cancer in women who are vaccinated at a young age – has led to questions about the future role of routine cervical cancer screening.
“Some people are saying that if we achieve 90% coverage, we might” eliminate community transmission and no longer need to screen, he said.
These trial results “tell us to be a little bit careful,” Dr. Steben continued. Those HPV types that are less aggressive and rarer than HPV-16 and -18 “can still cause cancer and might be there and surprise us. It could take more time than we thought” to get to the point where screening can be eliminated.
“There might be a little problem if we stop too early,” he said.
Study details
During the period 2004-2005, the investigators randomly assigned 3,727 women aged 18-25 years to receive Cervarix and 3,739 to a control group that received the hepatitis A vaccine; after 4 years, the control group also received Cervarix and exited the study. They were replaced by an unvaccinated control group of 2,836 women. The new control group and the original HPV vaccine group were followed for an additional 7 years.
In years 7-11 of the trial, the investigators found 9.2 additional cervical intraepithelial neoplasias of grade 2 or worse (CIN2+) from HPV types not covered by Cervarix per 1,000 vaccinated women in comparison with unvaccinated participants. This corresponds to –71.2% negative vaccine efficacy against CIN2+ lesions of HPV types not covered by the vaccine.
There were 8.3 additional CIN3+ lesions from nontargeted HPV strains per 1,000 vaccinated women in comparison with unvaccinated participants, which corresponds to –135% negative vaccine efficacy.
Overall, however, there was a net benefit of vaccination, with 27 fewer CIN2+ lesions when all HPV genotypes – vaccine covered or not – were considered per 1,000 vaccinated women over the entire 11 years of follow-up.
There were also 8.7 fewer CIN3+ lesions across all genotypes per 1,000 vaccinated women, but the benefit was not statistically significant.
Among the study limits, the team was unable to evaluate the effect of clinical unmasking on cervical cancer, because women were treated for high-grade cervical lesions before cases could progress to cervical cancer.
The trial was funded by the National Cancer Institute and the National Institutes of Health Office of Research on Women’s Health. GlaxoSmithKline provided the Cervarix vaccine and supported aspects of the trial. Two authors are named inventors on U.S. government–owned HPV vaccine patents with expired licenses to GlaxoSmithKline and Merck. Dr. Steben is an adviser/speaker for many companies, including GlaxoSmithKline and Merck.
A version of this article first appeared on Medscape.com.
Vaccines against human papillomavirus have been hailed as a success: they have been shown to decrease the incidence of cervical lesions associated with the HPV types that are in the vaccine.
However,
An expert not involved in the research said the new data “tell us to be a little bit careful.” Although the HPV types not included in the vaccine are rarer and less aggressive, they can still cause cancer.
The data come from the Costa Rica HPV Vaccine Trial, which involved more than 10,000 women aged 18-25 years. The HPV vaccine used in the trial was Cervarix, from GlaxoSmithKline. It covers the two leading causes of cervical cancer, HPV-16 and -18, and provides partial protection against three other genotypes.
After a follow-up of 11 years, among vaccinated women, there was an excess of precancerous cervical lesions caused by genotypes not included in the vaccine, resulting in negative vaccine efficacy for those HPV variants.
The increase wasn’t enough to offset the overall benefit of vaccination when all genotypes were considered, said the researchers, led by Jaimie Shing, PhD, a postdoctoral research fellow at the National Cancer Institute in Bethesda, Md.
Vaccinated women “still had long-term absolute reductions in high-grade lesions,” they pointed out.
The net protection “remained considerable, emphasizing the importance of HPV vaccination for cervical cancer prevention,” the team concluded.
The findings were published online in The Lancet Oncology.
The results are likely the first evidence to date of “clinical unmasking” with HPV vaccination, meaning that protection against the strains covered by the vaccine leaves women more prone to attack from other carcinogenic HPV variants.
This phenomenon “could attenuate long-term reductions in high-grade disease following successful implementation of HPV vaccination programs,” the investigators commented.
Highlighting a need for caution
The take-home message from the trial is that “we have to be careful,” said Marc Steben, MD, co-President of HPV Global Action and a professor at the University of Montreal.
He noted that the Cervarix HPV vaccine used in the trial is not the vaccine that is used now in developed nations.
The current standard HPV vaccine is Gardasil 9 (Merck), which offers broader coverage against nine HPV types (types 6, 11, 16, 18, 31, 33, 45, 52, and 58).
There are 12 main carcinogenic HPV genotypes, so unmasking of other strains is still possible with Gardasil 9, he said.
There is another issue, Dr. Steben added. The success of HPV vaccinations - a nearly 90% reduction in invasive cervical cancer in women who are vaccinated at a young age – has led to questions about the future role of routine cervical cancer screening.
“Some people are saying that if we achieve 90% coverage, we might” eliminate community transmission and no longer need to screen, he said.
These trial results “tell us to be a little bit careful,” Dr. Steben continued. Those HPV types that are less aggressive and rarer than HPV-16 and -18 “can still cause cancer and might be there and surprise us. It could take more time than we thought” to get to the point where screening can be eliminated.
“There might be a little problem if we stop too early,” he said.
Study details
During the period 2004-2005, the investigators randomly assigned 3,727 women aged 18-25 years to receive Cervarix and 3,739 to a control group that received the hepatitis A vaccine; after 4 years, the control group also received Cervarix and exited the study. They were replaced by an unvaccinated control group of 2,836 women. The new control group and the original HPV vaccine group were followed for an additional 7 years.
In years 7-11 of the trial, the investigators found 9.2 additional cervical intraepithelial neoplasias of grade 2 or worse (CIN2+) from HPV types not covered by Cervarix per 1,000 vaccinated women in comparison with unvaccinated participants. This corresponds to –71.2% negative vaccine efficacy against CIN2+ lesions of HPV types not covered by the vaccine.
There were 8.3 additional CIN3+ lesions from nontargeted HPV strains per 1,000 vaccinated women in comparison with unvaccinated participants, which corresponds to –135% negative vaccine efficacy.
Overall, however, there was a net benefit of vaccination, with 27 fewer CIN2+ lesions when all HPV genotypes – vaccine covered or not – were considered per 1,000 vaccinated women over the entire 11 years of follow-up.
There were also 8.7 fewer CIN3+ lesions across all genotypes per 1,000 vaccinated women, but the benefit was not statistically significant.
Among the study limits, the team was unable to evaluate the effect of clinical unmasking on cervical cancer, because women were treated for high-grade cervical lesions before cases could progress to cervical cancer.
The trial was funded by the National Cancer Institute and the National Institutes of Health Office of Research on Women’s Health. GlaxoSmithKline provided the Cervarix vaccine and supported aspects of the trial. Two authors are named inventors on U.S. government–owned HPV vaccine patents with expired licenses to GlaxoSmithKline and Merck. Dr. Steben is an adviser/speaker for many companies, including GlaxoSmithKline and Merck.
A version of this article first appeared on Medscape.com.
Vaccines against human papillomavirus have been hailed as a success: they have been shown to decrease the incidence of cervical lesions associated with the HPV types that are in the vaccine.
However,
An expert not involved in the research said the new data “tell us to be a little bit careful.” Although the HPV types not included in the vaccine are rarer and less aggressive, they can still cause cancer.
The data come from the Costa Rica HPV Vaccine Trial, which involved more than 10,000 women aged 18-25 years. The HPV vaccine used in the trial was Cervarix, from GlaxoSmithKline. It covers the two leading causes of cervical cancer, HPV-16 and -18, and provides partial protection against three other genotypes.
After a follow-up of 11 years, among vaccinated women, there was an excess of precancerous cervical lesions caused by genotypes not included in the vaccine, resulting in negative vaccine efficacy for those HPV variants.
The increase wasn’t enough to offset the overall benefit of vaccination when all genotypes were considered, said the researchers, led by Jaimie Shing, PhD, a postdoctoral research fellow at the National Cancer Institute in Bethesda, Md.
Vaccinated women “still had long-term absolute reductions in high-grade lesions,” they pointed out.
The net protection “remained considerable, emphasizing the importance of HPV vaccination for cervical cancer prevention,” the team concluded.
The findings were published online in The Lancet Oncology.
The results are likely the first evidence to date of “clinical unmasking” with HPV vaccination, meaning that protection against the strains covered by the vaccine leaves women more prone to attack from other carcinogenic HPV variants.
This phenomenon “could attenuate long-term reductions in high-grade disease following successful implementation of HPV vaccination programs,” the investigators commented.
Highlighting a need for caution
The take-home message from the trial is that “we have to be careful,” said Marc Steben, MD, co-President of HPV Global Action and a professor at the University of Montreal.
He noted that the Cervarix HPV vaccine used in the trial is not the vaccine that is used now in developed nations.
The current standard HPV vaccine is Gardasil 9 (Merck), which offers broader coverage against nine HPV types (types 6, 11, 16, 18, 31, 33, 45, 52, and 58).
There are 12 main carcinogenic HPV genotypes, so unmasking of other strains is still possible with Gardasil 9, he said.
There is another issue, Dr. Steben added. The success of HPV vaccinations - a nearly 90% reduction in invasive cervical cancer in women who are vaccinated at a young age – has led to questions about the future role of routine cervical cancer screening.
“Some people are saying that if we achieve 90% coverage, we might” eliminate community transmission and no longer need to screen, he said.
These trial results “tell us to be a little bit careful,” Dr. Steben continued. Those HPV types that are less aggressive and rarer than HPV-16 and -18 “can still cause cancer and might be there and surprise us. It could take more time than we thought” to get to the point where screening can be eliminated.
“There might be a little problem if we stop too early,” he said.
Study details
During the period 2004-2005, the investigators randomly assigned 3,727 women aged 18-25 years to receive Cervarix and 3,739 to a control group that received the hepatitis A vaccine; after 4 years, the control group also received Cervarix and exited the study. They were replaced by an unvaccinated control group of 2,836 women. The new control group and the original HPV vaccine group were followed for an additional 7 years.
In years 7-11 of the trial, the investigators found 9.2 additional cervical intraepithelial neoplasias of grade 2 or worse (CIN2+) from HPV types not covered by Cervarix per 1,000 vaccinated women in comparison with unvaccinated participants. This corresponds to –71.2% negative vaccine efficacy against CIN2+ lesions of HPV types not covered by the vaccine.
There were 8.3 additional CIN3+ lesions from nontargeted HPV strains per 1,000 vaccinated women in comparison with unvaccinated participants, which corresponds to –135% negative vaccine efficacy.
Overall, however, there was a net benefit of vaccination, with 27 fewer CIN2+ lesions when all HPV genotypes – vaccine covered or not – were considered per 1,000 vaccinated women over the entire 11 years of follow-up.
There were also 8.7 fewer CIN3+ lesions across all genotypes per 1,000 vaccinated women, but the benefit was not statistically significant.
Among the study limits, the team was unable to evaluate the effect of clinical unmasking on cervical cancer, because women were treated for high-grade cervical lesions before cases could progress to cervical cancer.
The trial was funded by the National Cancer Institute and the National Institutes of Health Office of Research on Women’s Health. GlaxoSmithKline provided the Cervarix vaccine and supported aspects of the trial. Two authors are named inventors on U.S. government–owned HPV vaccine patents with expired licenses to GlaxoSmithKline and Merck. Dr. Steben is an adviser/speaker for many companies, including GlaxoSmithKline and Merck.
A version of this article first appeared on Medscape.com.
FROM THE LANCET ONCOLOGY
Could a type 2 diabetes drug tackle kidney stones?
than patients who received placebo during a median 1.5 years of treatment.
These findings are from an analysis of pooled data from phase 1-4 clinical trials of empagliflozin for blood glucose control in 15,081 patients with type 2 diabetes.
Priyadarshini Balasubramanian, MD, presented the study as a poster at the annual meeting of the Endocrine Society; the study also was published online in the Journal of Clinical Endocrinology & Metabolism.
The researchers acknowledge this was a retrospective, post-hoc analysis and that urolithiasis – a stone in the urinary tract, which includes nephrolithiasis, a kidney stone – was an adverse event, not a primary or secondary outcome.
Also, the stone composition, which might help explain how the drug may affect stone formation, is unknown.
Therefore, “dedicated randomized prospective clinical trials are needed to confirm these initial observations in patients both with and without type 2 diabetes,” said Dr. Balasubramanian, a clinical fellow in the section of endocrinology & metabolism, department of internal medicine at Yale University, New Haven, Conn.
However, “if this association is proven, empagliflozin may be used to decrease the risk of kidney stones at least in those with type 2 diabetes, but maybe also in those without diabetes,” Dr. Balasubramanian said in an interview.
Further trials are also needed to determine if this is a class effect, which is likely, she speculated, and to unravel the potential mechanism.
This is important because of the prevalence of kidney stones, which affect up to 15% of the general population and 15%-20% of patients with diabetes, she explained.
‘Provocative’ earlier findings
The current study was prompted by a recent observational study by Kasper B. Kristensen, MD, PhD, and colleagues.
Because SGLT2 inhibitors increase urinary glucose excretion through reduced renal reabsorption of glucose leading to osmotic diuresis and increased urinary flow, they hypothesized that these therapies “may reduce the risk of upper urinary tract stones (nephrolithiasis) by reducing the concentration of lithogenic substances in urine.”
Using data from Danish Health registries, they matched 12,325 individuals newly prescribed an SGLT2 inhibitor 1:1 with patients newly prescribed a glucagonlike peptide-1 (GLP1) agonist, another new class of drugs for treating type 2 diabetes.
They found a hazard ratio of 0.51 (95% confidence interval, 0.37-0.71) for incident nephrolithiasis and a hazard ratio of 0.68 (95% CI, 0.48-0.97) for recurrent nephrolithiasis for patients taking SGLT2 inhibitors versus GLP-1 agonists.
These findings are “striking,” according to Dr. Balasubramanian and colleagues. However, “these data, while provocative, were entirely retrospective and therefore possibly prone to bias,” they add.
Pooled data from 20 trials
The current study analyzed data from 20 randomized controlled trials of glycemic control in type 2 diabetes, in which 10,177 patients had received empagliflozin 10 mg or 25 mg and 4,904 patients had received placebo.
Most patients (46.5%) had participated in the EMPA-REG OUTCOMES trial, which also had the longest follow-up (2.6 years).
The researchers identified patients with a new stone from the urinary tract (including the kidney, ureter, and urethra). Patients had received either the study drug for a median of 543 days or placebo for a median of 549 days.
During treatment, 104 of 10,177 patients in the pooled empagliflozin groups and 79 of 4,904 patients in the pooled placebo groups developed a stone in the urinary tract.
This was equivalent to 0.63 new urinary-tract stones per 100 patient-years in the pooled empagliflozin groups versus 1.01 new urinary-tract stones per 100 patient-years in the pooled placebo groups.
The incidence rate ratio was 0.64 (95% CI, 0.48-0.86), in favor of empagliflozin.
When the analysis was restricted to new kidney stones, the results were similar: 75 of 10,177 patients in the pooled empagliflozin groups and 57 of 4,904 patients in the pooled placebo groups developed a kidney stone.
This was equivalent to 0.45 new kidney stones per 100 patient-years in the pooled empagliflozin groups versus 0.72 new kidney stones per 100 patient-years in the pooled placebo groups.
The IRR was 0.65 (95% CI, 0.46-0.92), in favor of empagliflozin.
Upcoming small RCT in adults without diabetes
Invited to comment on the new study, Dr. Kristensen said: “The reduced risk of SGLT2 inhibitors towards nephrolithiasis is now reported in at least two studies with different methodology, different populations, and different exposure and outcome definitions.”
“I agree that randomized clinical trials designed specifically to confirm these findings appear warranted,” added Dr. Kristensen, from the Institute of Public Health, Clinical Pharmacology, Pharmacy, and Environmental Medicine, University of Southern Denmark in Odense.
There is a need for studies in patients with and without diabetes, he added, especially ones that focus on prevention of nephrolithiasis in patients with kidney stone disease.
A new trial should shed further light on this.
Results are expected by the end of 2022 for SWEETSTONE (Impact of the SGLT2 Inhibitor Empagliflozin on Urinary Supersaturations in Kidney Stone Formers), a randomized, double-blind crossover exploratory study in 46 patients without diabetes.
This should provide preliminary data to “establish the relevance for larger trials assessing the prophylactic potential of empagliflozin in kidney stone disease,” according to an article on the trial protocol recently published in BMJ.
The trials included in the pooled dataset were funded by Boehringer Ingelheim or the Boehringer Ingelheim and Eli Lilly Diabetes Alliance. Dr. Balasubramanian has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
than patients who received placebo during a median 1.5 years of treatment.
These findings are from an analysis of pooled data from phase 1-4 clinical trials of empagliflozin for blood glucose control in 15,081 patients with type 2 diabetes.
Priyadarshini Balasubramanian, MD, presented the study as a poster at the annual meeting of the Endocrine Society; the study also was published online in the Journal of Clinical Endocrinology & Metabolism.
The researchers acknowledge this was a retrospective, post-hoc analysis and that urolithiasis – a stone in the urinary tract, which includes nephrolithiasis, a kidney stone – was an adverse event, not a primary or secondary outcome.
Also, the stone composition, which might help explain how the drug may affect stone formation, is unknown.
Therefore, “dedicated randomized prospective clinical trials are needed to confirm these initial observations in patients both with and without type 2 diabetes,” said Dr. Balasubramanian, a clinical fellow in the section of endocrinology & metabolism, department of internal medicine at Yale University, New Haven, Conn.
However, “if this association is proven, empagliflozin may be used to decrease the risk of kidney stones at least in those with type 2 diabetes, but maybe also in those without diabetes,” Dr. Balasubramanian said in an interview.
Further trials are also needed to determine if this is a class effect, which is likely, she speculated, and to unravel the potential mechanism.
This is important because of the prevalence of kidney stones, which affect up to 15% of the general population and 15%-20% of patients with diabetes, she explained.
‘Provocative’ earlier findings
The current study was prompted by a recent observational study by Kasper B. Kristensen, MD, PhD, and colleagues.
Because SGLT2 inhibitors increase urinary glucose excretion through reduced renal reabsorption of glucose leading to osmotic diuresis and increased urinary flow, they hypothesized that these therapies “may reduce the risk of upper urinary tract stones (nephrolithiasis) by reducing the concentration of lithogenic substances in urine.”
Using data from Danish Health registries, they matched 12,325 individuals newly prescribed an SGLT2 inhibitor 1:1 with patients newly prescribed a glucagonlike peptide-1 (GLP1) agonist, another new class of drugs for treating type 2 diabetes.
They found a hazard ratio of 0.51 (95% confidence interval, 0.37-0.71) for incident nephrolithiasis and a hazard ratio of 0.68 (95% CI, 0.48-0.97) for recurrent nephrolithiasis for patients taking SGLT2 inhibitors versus GLP-1 agonists.
These findings are “striking,” according to Dr. Balasubramanian and colleagues. However, “these data, while provocative, were entirely retrospective and therefore possibly prone to bias,” they add.
Pooled data from 20 trials
The current study analyzed data from 20 randomized controlled trials of glycemic control in type 2 diabetes, in which 10,177 patients had received empagliflozin 10 mg or 25 mg and 4,904 patients had received placebo.
Most patients (46.5%) had participated in the EMPA-REG OUTCOMES trial, which also had the longest follow-up (2.6 years).
The researchers identified patients with a new stone from the urinary tract (including the kidney, ureter, and urethra). Patients had received either the study drug for a median of 543 days or placebo for a median of 549 days.
During treatment, 104 of 10,177 patients in the pooled empagliflozin groups and 79 of 4,904 patients in the pooled placebo groups developed a stone in the urinary tract.
This was equivalent to 0.63 new urinary-tract stones per 100 patient-years in the pooled empagliflozin groups versus 1.01 new urinary-tract stones per 100 patient-years in the pooled placebo groups.
The incidence rate ratio was 0.64 (95% CI, 0.48-0.86), in favor of empagliflozin.
When the analysis was restricted to new kidney stones, the results were similar: 75 of 10,177 patients in the pooled empagliflozin groups and 57 of 4,904 patients in the pooled placebo groups developed a kidney stone.
This was equivalent to 0.45 new kidney stones per 100 patient-years in the pooled empagliflozin groups versus 0.72 new kidney stones per 100 patient-years in the pooled placebo groups.
The IRR was 0.65 (95% CI, 0.46-0.92), in favor of empagliflozin.
Upcoming small RCT in adults without diabetes
Invited to comment on the new study, Dr. Kristensen said: “The reduced risk of SGLT2 inhibitors towards nephrolithiasis is now reported in at least two studies with different methodology, different populations, and different exposure and outcome definitions.”
“I agree that randomized clinical trials designed specifically to confirm these findings appear warranted,” added Dr. Kristensen, from the Institute of Public Health, Clinical Pharmacology, Pharmacy, and Environmental Medicine, University of Southern Denmark in Odense.
There is a need for studies in patients with and without diabetes, he added, especially ones that focus on prevention of nephrolithiasis in patients with kidney stone disease.
A new trial should shed further light on this.
Results are expected by the end of 2022 for SWEETSTONE (Impact of the SGLT2 Inhibitor Empagliflozin on Urinary Supersaturations in Kidney Stone Formers), a randomized, double-blind crossover exploratory study in 46 patients without diabetes.
This should provide preliminary data to “establish the relevance for larger trials assessing the prophylactic potential of empagliflozin in kidney stone disease,” according to an article on the trial protocol recently published in BMJ.
The trials included in the pooled dataset were funded by Boehringer Ingelheim or the Boehringer Ingelheim and Eli Lilly Diabetes Alliance. Dr. Balasubramanian has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
than patients who received placebo during a median 1.5 years of treatment.
These findings are from an analysis of pooled data from phase 1-4 clinical trials of empagliflozin for blood glucose control in 15,081 patients with type 2 diabetes.
Priyadarshini Balasubramanian, MD, presented the study as a poster at the annual meeting of the Endocrine Society; the study also was published online in the Journal of Clinical Endocrinology & Metabolism.
The researchers acknowledge this was a retrospective, post-hoc analysis and that urolithiasis – a stone in the urinary tract, which includes nephrolithiasis, a kidney stone – was an adverse event, not a primary or secondary outcome.
Also, the stone composition, which might help explain how the drug may affect stone formation, is unknown.
Therefore, “dedicated randomized prospective clinical trials are needed to confirm these initial observations in patients both with and without type 2 diabetes,” said Dr. Balasubramanian, a clinical fellow in the section of endocrinology & metabolism, department of internal medicine at Yale University, New Haven, Conn.
However, “if this association is proven, empagliflozin may be used to decrease the risk of kidney stones at least in those with type 2 diabetes, but maybe also in those without diabetes,” Dr. Balasubramanian said in an interview.
Further trials are also needed to determine if this is a class effect, which is likely, she speculated, and to unravel the potential mechanism.
This is important because of the prevalence of kidney stones, which affect up to 15% of the general population and 15%-20% of patients with diabetes, she explained.
‘Provocative’ earlier findings
The current study was prompted by a recent observational study by Kasper B. Kristensen, MD, PhD, and colleagues.
Because SGLT2 inhibitors increase urinary glucose excretion through reduced renal reabsorption of glucose leading to osmotic diuresis and increased urinary flow, they hypothesized that these therapies “may reduce the risk of upper urinary tract stones (nephrolithiasis) by reducing the concentration of lithogenic substances in urine.”
Using data from Danish Health registries, they matched 12,325 individuals newly prescribed an SGLT2 inhibitor 1:1 with patients newly prescribed a glucagonlike peptide-1 (GLP1) agonist, another new class of drugs for treating type 2 diabetes.
They found a hazard ratio of 0.51 (95% confidence interval, 0.37-0.71) for incident nephrolithiasis and a hazard ratio of 0.68 (95% CI, 0.48-0.97) for recurrent nephrolithiasis for patients taking SGLT2 inhibitors versus GLP-1 agonists.
These findings are “striking,” according to Dr. Balasubramanian and colleagues. However, “these data, while provocative, were entirely retrospective and therefore possibly prone to bias,” they add.
Pooled data from 20 trials
The current study analyzed data from 20 randomized controlled trials of glycemic control in type 2 diabetes, in which 10,177 patients had received empagliflozin 10 mg or 25 mg and 4,904 patients had received placebo.
Most patients (46.5%) had participated in the EMPA-REG OUTCOMES trial, which also had the longest follow-up (2.6 years).
The researchers identified patients with a new stone from the urinary tract (including the kidney, ureter, and urethra). Patients had received either the study drug for a median of 543 days or placebo for a median of 549 days.
During treatment, 104 of 10,177 patients in the pooled empagliflozin groups and 79 of 4,904 patients in the pooled placebo groups developed a stone in the urinary tract.
This was equivalent to 0.63 new urinary-tract stones per 100 patient-years in the pooled empagliflozin groups versus 1.01 new urinary-tract stones per 100 patient-years in the pooled placebo groups.
The incidence rate ratio was 0.64 (95% CI, 0.48-0.86), in favor of empagliflozin.
When the analysis was restricted to new kidney stones, the results were similar: 75 of 10,177 patients in the pooled empagliflozin groups and 57 of 4,904 patients in the pooled placebo groups developed a kidney stone.
This was equivalent to 0.45 new kidney stones per 100 patient-years in the pooled empagliflozin groups versus 0.72 new kidney stones per 100 patient-years in the pooled placebo groups.
The IRR was 0.65 (95% CI, 0.46-0.92), in favor of empagliflozin.
Upcoming small RCT in adults without diabetes
Invited to comment on the new study, Dr. Kristensen said: “The reduced risk of SGLT2 inhibitors towards nephrolithiasis is now reported in at least two studies with different methodology, different populations, and different exposure and outcome definitions.”
“I agree that randomized clinical trials designed specifically to confirm these findings appear warranted,” added Dr. Kristensen, from the Institute of Public Health, Clinical Pharmacology, Pharmacy, and Environmental Medicine, University of Southern Denmark in Odense.
There is a need for studies in patients with and without diabetes, he added, especially ones that focus on prevention of nephrolithiasis in patients with kidney stone disease.
A new trial should shed further light on this.
Results are expected by the end of 2022 for SWEETSTONE (Impact of the SGLT2 Inhibitor Empagliflozin on Urinary Supersaturations in Kidney Stone Formers), a randomized, double-blind crossover exploratory study in 46 patients without diabetes.
This should provide preliminary data to “establish the relevance for larger trials assessing the prophylactic potential of empagliflozin in kidney stone disease,” according to an article on the trial protocol recently published in BMJ.
The trials included in the pooled dataset were funded by Boehringer Ingelheim or the Boehringer Ingelheim and Eli Lilly Diabetes Alliance. Dr. Balasubramanian has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ENDO 2022
What’s the best time of day to exercise? It depends on your goals
For most of us, the “best” time of day to work out is simple: When we can.
Maybe that’s before or after work. Or when the gym offers free daycare. Or when our favorite instructor teaches our favorite class.
That’s why we call it a “routine.” And if the results are the same, it’s hard to imagine changing it up.
But what if the results aren’t the same?
They may not be, according to a new study from a research team at Skidmore College in Saratoga Springs, N.Y.
Women who worked out in the morning lost more fat, while those who trained in the evening gained more upper-body strength and power. As for men, the performance improvements were similar no matter when they exercised. But those who did so in the evening had a significant drop in blood pressure, among other benefits.
The study is part of a growing body of research showing different results for different times of day among different populations. As it turns out, when you exercise can ultimately have a big effect, not just on strength and fat loss, but also heart health, mood, and quality of sleep.
An accidental discovery
The original goal of the Skidmore study was to test a unique fitness program with a group of healthy, fit, and extremely active adults in early middle age.
The program includes four workouts a week, each with a different focus: strength, steady-pace endurance, high-intensity intervals, and flexibility (traditional stretching combined with yoga and Pilates exercises).
But because the group was so large – 27 women and 20 men completed the 3-month program – they had to split them into morning and evening workout groups.
It wasn’t until researchers looked at the results that they saw the differences between morning and evening exercise, says lead author Paul Arciero, PhD.
Dr. Arciero stressed that participants in every group got leaner and stronger. But the women who worked out in the morning got much bigger reductions in body fat and body-fat percentage than the evening group. Meanwhile, women in the evening group got much bigger gains in upper-body strength, power, and muscular endurance than their morning counterparts.
Among the men, the evening group had significantly larger improvements in blood pressure, cholesterol levels, and the percentage of fat they burned for energy, along with a bigger drop in feelings of fatigue.
Strategic timing for powerful results
Some of these findings are consistent with previous research. For example, a study published in 2021 showed that the ability to exert high effort and express strength and power peaks in the late afternoon, about the same time that your core body temperature is at its highest point.
On the other hand, you’ll probably perform better in the morning when the activity requires a lot of skill and coordination or depends on strategic decision-making.
The findings apply to both men and women.
Performance aside, exercise timing might offer strong health benefits for men with type 2 diabetes, or at high risk for it.
A study showed that men who exercised between 3 p.m. and 6 p.m. saw dramatic improvements in blood sugar management and insulin sensitivity, compared to a group that worked out between 8 a.m. and 10 a.m.
They also lost more fat during the 12-week program, even though they were doing the exact same workouts.
Train consistently, sleep well
When you exercise can affect your sleep quality in many ways, said neuroscientist Jennifer Heisz, PhD, of McMaster University, Hamilton, Ont.
First, she said, “exercise helps you fall asleep faster and sleep deeper at night.” (The only exception is if you exercise so intensely or so close to bedtime that your heart rate is still elevated.)
Second, “exercising at a consistent time every day helps regulate the body’s circadian rhythms.” It doesn’t matter if the exercise is in the morning, evening, or anywhere in between. As long as it’s predictable, it will help you fall asleep and wake up at the same times.
Outdoor exercise is even better, she said. The sun is the most powerful regulator of the circadian clock and works in tandem with physical activity.
Third, exercising at specific times can help you overcome jet lag or adjust to an earlier or later shift at work.
“Exercising at 7 a.m. or between 1 and 4 p.m. helps your circadian clock to ‘fall back’ in time, making it easier to wake up earlier,” Dr. Heisz said. If you need to train your body to wake up later in the morning, try working out between 7 p.m. and 10 p.m.
All exercise is good, but the right timing can make it even better
“The best time to exercise is when you can fit it in,” Dr. Arciero said. “You’ve got to choose the time that fits your lifestyle best.”
But context matters, he noted.
“For someone needing to achieve an improvement in their risk for cardiometabolic disease,” his study shows an advantage to working out later in the day, especially for men. If you’re more focused on building upper-body strength and power, you’ll probably get better results from training in the afternoon or evening.
And for fat loss, the Skidmore study shows better results for women who did morning workouts.
And if you’re still not sure? Try sleeping on it – preferably after your workout.
A version of this article first appeared on WebMD.com.
For most of us, the “best” time of day to work out is simple: When we can.
Maybe that’s before or after work. Or when the gym offers free daycare. Or when our favorite instructor teaches our favorite class.
That’s why we call it a “routine.” And if the results are the same, it’s hard to imagine changing it up.
But what if the results aren’t the same?
They may not be, according to a new study from a research team at Skidmore College in Saratoga Springs, N.Y.
Women who worked out in the morning lost more fat, while those who trained in the evening gained more upper-body strength and power. As for men, the performance improvements were similar no matter when they exercised. But those who did so in the evening had a significant drop in blood pressure, among other benefits.
The study is part of a growing body of research showing different results for different times of day among different populations. As it turns out, when you exercise can ultimately have a big effect, not just on strength and fat loss, but also heart health, mood, and quality of sleep.
An accidental discovery
The original goal of the Skidmore study was to test a unique fitness program with a group of healthy, fit, and extremely active adults in early middle age.
The program includes four workouts a week, each with a different focus: strength, steady-pace endurance, high-intensity intervals, and flexibility (traditional stretching combined with yoga and Pilates exercises).
But because the group was so large – 27 women and 20 men completed the 3-month program – they had to split them into morning and evening workout groups.
It wasn’t until researchers looked at the results that they saw the differences between morning and evening exercise, says lead author Paul Arciero, PhD.
Dr. Arciero stressed that participants in every group got leaner and stronger. But the women who worked out in the morning got much bigger reductions in body fat and body-fat percentage than the evening group. Meanwhile, women in the evening group got much bigger gains in upper-body strength, power, and muscular endurance than their morning counterparts.
Among the men, the evening group had significantly larger improvements in blood pressure, cholesterol levels, and the percentage of fat they burned for energy, along with a bigger drop in feelings of fatigue.
Strategic timing for powerful results
Some of these findings are consistent with previous research. For example, a study published in 2021 showed that the ability to exert high effort and express strength and power peaks in the late afternoon, about the same time that your core body temperature is at its highest point.
On the other hand, you’ll probably perform better in the morning when the activity requires a lot of skill and coordination or depends on strategic decision-making.
The findings apply to both men and women.
Performance aside, exercise timing might offer strong health benefits for men with type 2 diabetes, or at high risk for it.
A study showed that men who exercised between 3 p.m. and 6 p.m. saw dramatic improvements in blood sugar management and insulin sensitivity, compared to a group that worked out between 8 a.m. and 10 a.m.
They also lost more fat during the 12-week program, even though they were doing the exact same workouts.
Train consistently, sleep well
When you exercise can affect your sleep quality in many ways, said neuroscientist Jennifer Heisz, PhD, of McMaster University, Hamilton, Ont.
First, she said, “exercise helps you fall asleep faster and sleep deeper at night.” (The only exception is if you exercise so intensely or so close to bedtime that your heart rate is still elevated.)
Second, “exercising at a consistent time every day helps regulate the body’s circadian rhythms.” It doesn’t matter if the exercise is in the morning, evening, or anywhere in between. As long as it’s predictable, it will help you fall asleep and wake up at the same times.
Outdoor exercise is even better, she said. The sun is the most powerful regulator of the circadian clock and works in tandem with physical activity.
Third, exercising at specific times can help you overcome jet lag or adjust to an earlier or later shift at work.
“Exercising at 7 a.m. or between 1 and 4 p.m. helps your circadian clock to ‘fall back’ in time, making it easier to wake up earlier,” Dr. Heisz said. If you need to train your body to wake up later in the morning, try working out between 7 p.m. and 10 p.m.
All exercise is good, but the right timing can make it even better
“The best time to exercise is when you can fit it in,” Dr. Arciero said. “You’ve got to choose the time that fits your lifestyle best.”
But context matters, he noted.
“For someone needing to achieve an improvement in their risk for cardiometabolic disease,” his study shows an advantage to working out later in the day, especially for men. If you’re more focused on building upper-body strength and power, you’ll probably get better results from training in the afternoon or evening.
And for fat loss, the Skidmore study shows better results for women who did morning workouts.
And if you’re still not sure? Try sleeping on it – preferably after your workout.
A version of this article first appeared on WebMD.com.
For most of us, the “best” time of day to work out is simple: When we can.
Maybe that’s before or after work. Or when the gym offers free daycare. Or when our favorite instructor teaches our favorite class.
That’s why we call it a “routine.” And if the results are the same, it’s hard to imagine changing it up.
But what if the results aren’t the same?
They may not be, according to a new study from a research team at Skidmore College in Saratoga Springs, N.Y.
Women who worked out in the morning lost more fat, while those who trained in the evening gained more upper-body strength and power. As for men, the performance improvements were similar no matter when they exercised. But those who did so in the evening had a significant drop in blood pressure, among other benefits.
The study is part of a growing body of research showing different results for different times of day among different populations. As it turns out, when you exercise can ultimately have a big effect, not just on strength and fat loss, but also heart health, mood, and quality of sleep.
An accidental discovery
The original goal of the Skidmore study was to test a unique fitness program with a group of healthy, fit, and extremely active adults in early middle age.
The program includes four workouts a week, each with a different focus: strength, steady-pace endurance, high-intensity intervals, and flexibility (traditional stretching combined with yoga and Pilates exercises).
But because the group was so large – 27 women and 20 men completed the 3-month program – they had to split them into morning and evening workout groups.
It wasn’t until researchers looked at the results that they saw the differences between morning and evening exercise, says lead author Paul Arciero, PhD.
Dr. Arciero stressed that participants in every group got leaner and stronger. But the women who worked out in the morning got much bigger reductions in body fat and body-fat percentage than the evening group. Meanwhile, women in the evening group got much bigger gains in upper-body strength, power, and muscular endurance than their morning counterparts.
Among the men, the evening group had significantly larger improvements in blood pressure, cholesterol levels, and the percentage of fat they burned for energy, along with a bigger drop in feelings of fatigue.
Strategic timing for powerful results
Some of these findings are consistent with previous research. For example, a study published in 2021 showed that the ability to exert high effort and express strength and power peaks in the late afternoon, about the same time that your core body temperature is at its highest point.
On the other hand, you’ll probably perform better in the morning when the activity requires a lot of skill and coordination or depends on strategic decision-making.
The findings apply to both men and women.
Performance aside, exercise timing might offer strong health benefits for men with type 2 diabetes, or at high risk for it.
A study showed that men who exercised between 3 p.m. and 6 p.m. saw dramatic improvements in blood sugar management and insulin sensitivity, compared to a group that worked out between 8 a.m. and 10 a.m.
They also lost more fat during the 12-week program, even though they were doing the exact same workouts.
Train consistently, sleep well
When you exercise can affect your sleep quality in many ways, said neuroscientist Jennifer Heisz, PhD, of McMaster University, Hamilton, Ont.
First, she said, “exercise helps you fall asleep faster and sleep deeper at night.” (The only exception is if you exercise so intensely or so close to bedtime that your heart rate is still elevated.)
Second, “exercising at a consistent time every day helps regulate the body’s circadian rhythms.” It doesn’t matter if the exercise is in the morning, evening, or anywhere in between. As long as it’s predictable, it will help you fall asleep and wake up at the same times.
Outdoor exercise is even better, she said. The sun is the most powerful regulator of the circadian clock and works in tandem with physical activity.
Third, exercising at specific times can help you overcome jet lag or adjust to an earlier or later shift at work.
“Exercising at 7 a.m. or between 1 and 4 p.m. helps your circadian clock to ‘fall back’ in time, making it easier to wake up earlier,” Dr. Heisz said. If you need to train your body to wake up later in the morning, try working out between 7 p.m. and 10 p.m.
All exercise is good, but the right timing can make it even better
“The best time to exercise is when you can fit it in,” Dr. Arciero said. “You’ve got to choose the time that fits your lifestyle best.”
But context matters, he noted.
“For someone needing to achieve an improvement in their risk for cardiometabolic disease,” his study shows an advantage to working out later in the day, especially for men. If you’re more focused on building upper-body strength and power, you’ll probably get better results from training in the afternoon or evening.
And for fat loss, the Skidmore study shows better results for women who did morning workouts.
And if you’re still not sure? Try sleeping on it – preferably after your workout.
A version of this article first appeared on WebMD.com.
FROM FRONTIERS IN PHYSIOLOGY
To predict mortality, you need a leg to stand on
Storks everywhere, rejoice.
According to the findings, people in middle age and older who couldn’t perform the 10-second standing test were nearly four times as likely to die of any cause – heart attacks, strokes, cancer, and more – in the coming years than those who could, well, stand the test of time.
Claudio Gil Araújo, MD, PhD, research director of the Exercise Medicine Clinic-CLINIMEX in Rio de Janeiro, who led the study, called the results “awesome!”
“As a physician who has worked with cardiac patients for over 4 decades, I was very impressed in finding out that, for those between 51 and 75 years of age, it is riskier for survival to not complete the 10-second one-leg standing test than to have been diagnosed as having coronary artery disease or in being hypertensive” or having abnormal cholesterol, Dr. Araújo said in an interview.
The findings appeared in the British Journal of Sports Medicine.
Researchers have known for at least a half century that balance and mortality are connected. One reason is falls: Worldwide, nearly 700,000 people each year die as a result of a fall, according to the World Health Organization, and more than 37 million falls annually require medical attention. But as the new study indicates, falls aren’t the only problem.
Dr. Araújo and colleagues have been working on ways to improve balance and strength as people age. In addition to the one-legged standing test, they have previously shown that the ability to rise from a sitting position on the floor is also a strong predictor of longevity.
For the new study, the researchers assessed 1,702 people in Brazil (68% men) aged 51-75 years who had been participating in an ongoing exercise study that began there in 1994.
Three tries to succeed
Starting in 2008, the team introduced the standing test, which involves balancing on one leg and placing the other foot at the back weight-bearing limb for support. People get three tries to maintain that posture for at least 10 seconds.
Not surprisingly, the ability to perform the test dropped with age. Although 20% of people in the study overall were unable to stand on one leg for 10 seconds, that figure rose to about 70% for those aged 76-80 years, and nearly 90% for those aged 81-85, according to the researchers. Of the two dozen 85-year-olds in the study, only two were able to complete the standing test, Dr. Araújo told this news organization.
At roughly age 70, half of people could not complete the 10-second test.
Over an average of 7 years of follow-up, 17.5% of people who could not manage the 10-second stand had died, compared with 4.5% of those who could last that long, the study found.
After accounting for age and many other risk factors, such as diabetes, body mass index, and a history of heart disease, people who were unable to complete the standing test were 84% more likely to die from any cause over the study period than their peers with better one-legged static balance (95% confidence interval, 1.23-2.78; P < .001).
The researchers said their study was limited by its lack of diversity – all the participants were relatively affluent Brazilians – and the inability to control for a history of falls and physical activity. But they said the size of the cohort, the long follow-up period, and their use of sophistical statistical methods helped mitigate the shortcomings.
Although low aerobic fitness is a marker of poor health, much less attention has been paid to nonaerobic fitness – things like balance, flexibility, and muscle strength and power, Dr. Araújo said.
“We are accumulating evidence that these three components of nonaerobic physical fitness are potentially relevant for good health and even more relevant for survival in older subjects,” Dr. Araújo said. Poor nonaerobic fitness, which is normally but not always associated with a sedentary lifestyle, “is the background of most cases of frailty, and being frail is strongly associated with a poor quality of life, less physical activity and exercise, and so on. It’s a bad circle.”
Dr. Araújo’s group has been using the standing test in their clinic for more than a dozen years and have seen gains in their patients. “Patients are often unaware that they are unable to sustain 10 seconds standing one legged. After this simple evaluation, they are much more prone to engage in balance training,” he said.
For now, the researchers don’t have data to show that improving static balance or performance on the standing test can affect survival, a “quite attractive” possibility, he added. But balance can be substantially improved through training.
“After only a few sessions, an improvement can be perceived, and this influences quality of life,” Dr. Araújo said. “And this is exactly what we do with the patients that we evaluated and for those that are attending our medically supervised exercise program.”
George A. Kuchel, MD, CM, FRCP, professor and Travelers Chair in Geriatrics and Gerontology at the University of Connecticut, Farmington, called the research “well done” and said the results “make perfect sense, since we have known for a long time that muscle strength is an important determinant of health, independence, and survival.”
Identifying frail patients quickly, simply, and reliably in the clinical setting is a pressing need, Dr. Kuchel, director of the UConn Center on Aging, said in an interview. The 10-second test “has considerable appeal” for this purpose.
“This could be, or rather should be, of great interest to all busy clinicians who see older adults in primary care or consultative capacities,” Dr. Kuchel added. “I hate to be nihilistic as regards what is possible in the context of really busy clinical practices, but even the minute or so that this takes to do may very well be too much for busy clinicians to do.”
Dr. Araújo and Dr. Kuchel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Storks everywhere, rejoice.
According to the findings, people in middle age and older who couldn’t perform the 10-second standing test were nearly four times as likely to die of any cause – heart attacks, strokes, cancer, and more – in the coming years than those who could, well, stand the test of time.
Claudio Gil Araújo, MD, PhD, research director of the Exercise Medicine Clinic-CLINIMEX in Rio de Janeiro, who led the study, called the results “awesome!”
“As a physician who has worked with cardiac patients for over 4 decades, I was very impressed in finding out that, for those between 51 and 75 years of age, it is riskier for survival to not complete the 10-second one-leg standing test than to have been diagnosed as having coronary artery disease or in being hypertensive” or having abnormal cholesterol, Dr. Araújo said in an interview.
The findings appeared in the British Journal of Sports Medicine.
Researchers have known for at least a half century that balance and mortality are connected. One reason is falls: Worldwide, nearly 700,000 people each year die as a result of a fall, according to the World Health Organization, and more than 37 million falls annually require medical attention. But as the new study indicates, falls aren’t the only problem.
Dr. Araújo and colleagues have been working on ways to improve balance and strength as people age. In addition to the one-legged standing test, they have previously shown that the ability to rise from a sitting position on the floor is also a strong predictor of longevity.
For the new study, the researchers assessed 1,702 people in Brazil (68% men) aged 51-75 years who had been participating in an ongoing exercise study that began there in 1994.
Three tries to succeed
Starting in 2008, the team introduced the standing test, which involves balancing on one leg and placing the other foot at the back weight-bearing limb for support. People get three tries to maintain that posture for at least 10 seconds.
Not surprisingly, the ability to perform the test dropped with age. Although 20% of people in the study overall were unable to stand on one leg for 10 seconds, that figure rose to about 70% for those aged 76-80 years, and nearly 90% for those aged 81-85, according to the researchers. Of the two dozen 85-year-olds in the study, only two were able to complete the standing test, Dr. Araújo told this news organization.
At roughly age 70, half of people could not complete the 10-second test.
Over an average of 7 years of follow-up, 17.5% of people who could not manage the 10-second stand had died, compared with 4.5% of those who could last that long, the study found.
After accounting for age and many other risk factors, such as diabetes, body mass index, and a history of heart disease, people who were unable to complete the standing test were 84% more likely to die from any cause over the study period than their peers with better one-legged static balance (95% confidence interval, 1.23-2.78; P < .001).
The researchers said their study was limited by its lack of diversity – all the participants were relatively affluent Brazilians – and the inability to control for a history of falls and physical activity. But they said the size of the cohort, the long follow-up period, and their use of sophistical statistical methods helped mitigate the shortcomings.
Although low aerobic fitness is a marker of poor health, much less attention has been paid to nonaerobic fitness – things like balance, flexibility, and muscle strength and power, Dr. Araújo said.
“We are accumulating evidence that these three components of nonaerobic physical fitness are potentially relevant for good health and even more relevant for survival in older subjects,” Dr. Araújo said. Poor nonaerobic fitness, which is normally but not always associated with a sedentary lifestyle, “is the background of most cases of frailty, and being frail is strongly associated with a poor quality of life, less physical activity and exercise, and so on. It’s a bad circle.”
Dr. Araújo’s group has been using the standing test in their clinic for more than a dozen years and have seen gains in their patients. “Patients are often unaware that they are unable to sustain 10 seconds standing one legged. After this simple evaluation, they are much more prone to engage in balance training,” he said.
For now, the researchers don’t have data to show that improving static balance or performance on the standing test can affect survival, a “quite attractive” possibility, he added. But balance can be substantially improved through training.
“After only a few sessions, an improvement can be perceived, and this influences quality of life,” Dr. Araújo said. “And this is exactly what we do with the patients that we evaluated and for those that are attending our medically supervised exercise program.”
George A. Kuchel, MD, CM, FRCP, professor and Travelers Chair in Geriatrics and Gerontology at the University of Connecticut, Farmington, called the research “well done” and said the results “make perfect sense, since we have known for a long time that muscle strength is an important determinant of health, independence, and survival.”
Identifying frail patients quickly, simply, and reliably in the clinical setting is a pressing need, Dr. Kuchel, director of the UConn Center on Aging, said in an interview. The 10-second test “has considerable appeal” for this purpose.
“This could be, or rather should be, of great interest to all busy clinicians who see older adults in primary care or consultative capacities,” Dr. Kuchel added. “I hate to be nihilistic as regards what is possible in the context of really busy clinical practices, but even the minute or so that this takes to do may very well be too much for busy clinicians to do.”
Dr. Araújo and Dr. Kuchel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Storks everywhere, rejoice.
According to the findings, people in middle age and older who couldn’t perform the 10-second standing test were nearly four times as likely to die of any cause – heart attacks, strokes, cancer, and more – in the coming years than those who could, well, stand the test of time.
Claudio Gil Araújo, MD, PhD, research director of the Exercise Medicine Clinic-CLINIMEX in Rio de Janeiro, who led the study, called the results “awesome!”
“As a physician who has worked with cardiac patients for over 4 decades, I was very impressed in finding out that, for those between 51 and 75 years of age, it is riskier for survival to not complete the 10-second one-leg standing test than to have been diagnosed as having coronary artery disease or in being hypertensive” or having abnormal cholesterol, Dr. Araújo said in an interview.
The findings appeared in the British Journal of Sports Medicine.
Researchers have known for at least a half century that balance and mortality are connected. One reason is falls: Worldwide, nearly 700,000 people each year die as a result of a fall, according to the World Health Organization, and more than 37 million falls annually require medical attention. But as the new study indicates, falls aren’t the only problem.
Dr. Araújo and colleagues have been working on ways to improve balance and strength as people age. In addition to the one-legged standing test, they have previously shown that the ability to rise from a sitting position on the floor is also a strong predictor of longevity.
For the new study, the researchers assessed 1,702 people in Brazil (68% men) aged 51-75 years who had been participating in an ongoing exercise study that began there in 1994.
Three tries to succeed
Starting in 2008, the team introduced the standing test, which involves balancing on one leg and placing the other foot at the back weight-bearing limb for support. People get three tries to maintain that posture for at least 10 seconds.
Not surprisingly, the ability to perform the test dropped with age. Although 20% of people in the study overall were unable to stand on one leg for 10 seconds, that figure rose to about 70% for those aged 76-80 years, and nearly 90% for those aged 81-85, according to the researchers. Of the two dozen 85-year-olds in the study, only two were able to complete the standing test, Dr. Araújo told this news organization.
At roughly age 70, half of people could not complete the 10-second test.
Over an average of 7 years of follow-up, 17.5% of people who could not manage the 10-second stand had died, compared with 4.5% of those who could last that long, the study found.
After accounting for age and many other risk factors, such as diabetes, body mass index, and a history of heart disease, people who were unable to complete the standing test were 84% more likely to die from any cause over the study period than their peers with better one-legged static balance (95% confidence interval, 1.23-2.78; P < .001).
The researchers said their study was limited by its lack of diversity – all the participants were relatively affluent Brazilians – and the inability to control for a history of falls and physical activity. But they said the size of the cohort, the long follow-up period, and their use of sophistical statistical methods helped mitigate the shortcomings.
Although low aerobic fitness is a marker of poor health, much less attention has been paid to nonaerobic fitness – things like balance, flexibility, and muscle strength and power, Dr. Araújo said.
“We are accumulating evidence that these three components of nonaerobic physical fitness are potentially relevant for good health and even more relevant for survival in older subjects,” Dr. Araújo said. Poor nonaerobic fitness, which is normally but not always associated with a sedentary lifestyle, “is the background of most cases of frailty, and being frail is strongly associated with a poor quality of life, less physical activity and exercise, and so on. It’s a bad circle.”
Dr. Araújo’s group has been using the standing test in their clinic for more than a dozen years and have seen gains in their patients. “Patients are often unaware that they are unable to sustain 10 seconds standing one legged. After this simple evaluation, they are much more prone to engage in balance training,” he said.
For now, the researchers don’t have data to show that improving static balance or performance on the standing test can affect survival, a “quite attractive” possibility, he added. But balance can be substantially improved through training.
“After only a few sessions, an improvement can be perceived, and this influences quality of life,” Dr. Araújo said. “And this is exactly what we do with the patients that we evaluated and for those that are attending our medically supervised exercise program.”
George A. Kuchel, MD, CM, FRCP, professor and Travelers Chair in Geriatrics and Gerontology at the University of Connecticut, Farmington, called the research “well done” and said the results “make perfect sense, since we have known for a long time that muscle strength is an important determinant of health, independence, and survival.”
Identifying frail patients quickly, simply, and reliably in the clinical setting is a pressing need, Dr. Kuchel, director of the UConn Center on Aging, said in an interview. The 10-second test “has considerable appeal” for this purpose.
“This could be, or rather should be, of great interest to all busy clinicians who see older adults in primary care or consultative capacities,” Dr. Kuchel added. “I hate to be nihilistic as regards what is possible in the context of really busy clinical practices, but even the minute or so that this takes to do may very well be too much for busy clinicians to do.”
Dr. Araújo and Dr. Kuchel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF SPORTS MEDICINE
Pandemic public health measures may have mitigated Kawasaki disease
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Heart failure: Medicare cost sharing may put quadruple therapy out of reach
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.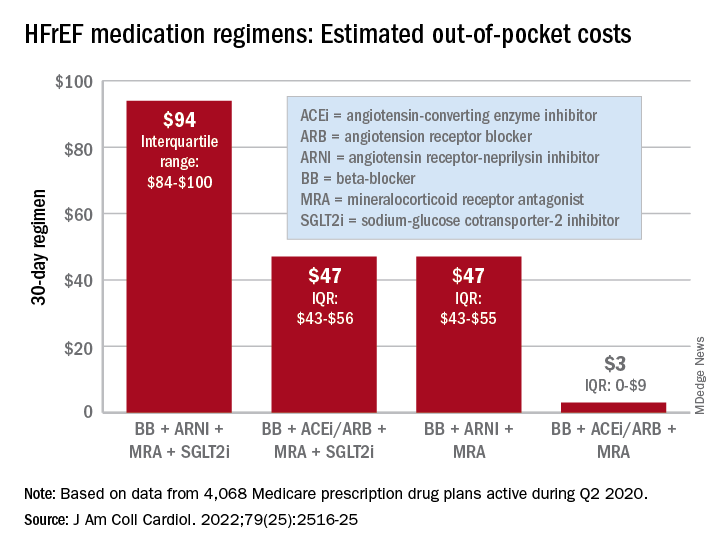
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.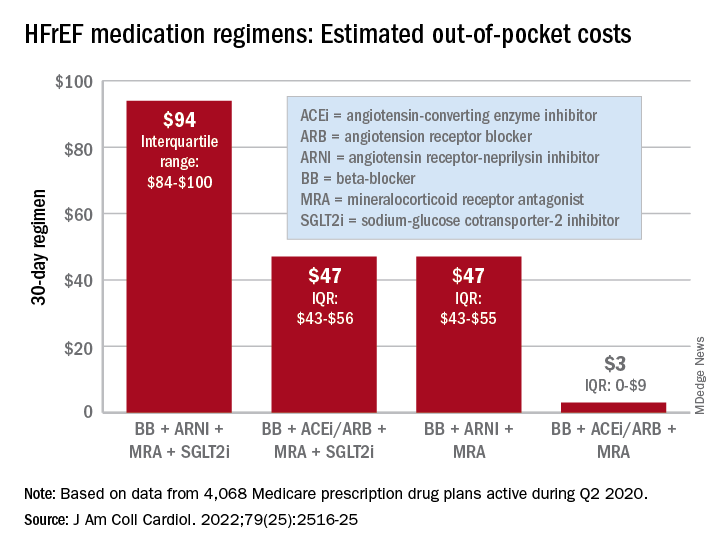
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.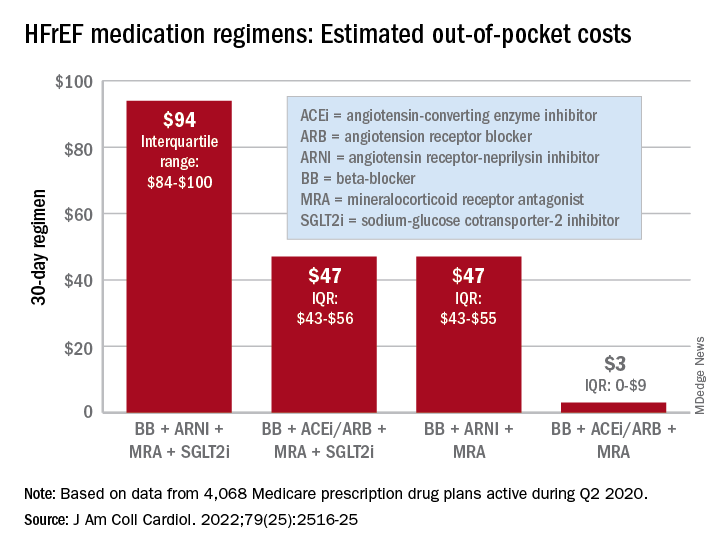
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
FROM THE JOURNAL Of the AMERICAN COLLEGE OF CARDIOLOGY
Can the ketogenic diet treat polycystic ovary syndrome?
MADRID – During the International Scientific Symposium “New Frontiers in Scientific Research” that recently took place in Barcelona, specialists analyzed the role of the very-low-calorie ketogenic diet. This analysis was in relation to three comorbidities that have a higher incidence among overweight and obese patients: polycystic ovary syndrome, nonalcoholic fatty liver disease, and type 2 diabetes. The experts’ aim? To analyze and update the latest evidence on the benefits of this dietary choice.
Polycystic ovary syndrome
Alessandra Gambineri, MD, PhD, associate professor at the department of medicine and surgery (DIMEC) at the University of Bologna, Italy, addressed the link between obesity and polycystic ovary syndrome, which she described as a chronic disease that affects about 10% of women of childbearing age and that presents diverse phenotypes with different characteristics.
“The pathophysiology of this syndrome is characterized by the interaction of three factors: androgen excess, adipose tissue dysfunction, and insulin resistance. These factors interact with each other and are expressed differently in each phenotype,” said Dr. Gambineri.
She indicated that adipose tissue dysfunction is central to this pathology. This centrality results from its association with secretions, such as free fatty acids, proinflammatory cytokines, certain adipokines that promote insulin resistance, glucocorticosteroids, androgens, and oxidative stress.
“Similarly, the oxidative stress that characterizes this syndrome is increasingly present in obese individuals,” said Dr. Gambineri. “This oxidative stress also produces ovary hypotoxicity that aggravates ovulatory function. In this context, the very-low-calorie ketogenic diet can be useful in several ways: weight reduction; promoting the loss of mainly visceral/abdominal fat; decreasing lipotoxicity; and improving inflammation, hyperinsulinemia, and insulin resistance.”
This was the path followed to carry out a study that aimed to analyze the effects of the very-low-calorie ketogenic diet on manifestations of polycystic ovary syndrome in the obesity phenotype. Dr. Gambineri presented its results.
“The objective was to compare the effects of a very-low-calorie ketogenic diet and the standard low-calorie (hypocaloric) diet as a control group,” she said. “The effects studied include body weight, insulin resistance, menstrual cycle, ovulation, ovarian morphology, and hyperandrogenism in a population of 30 obese women with polycystic ovary syndrome and insulin resistance.”
Study participants had a diagnosis of polycystic ovary syndrome as defined by the National Institutes of Health criteria and were aged 18-45 years. These women were randomly assigned to two groups of equal size: experimental (very-low-calorie ketogenic diet) and control (hypocaloric diet). “The women assigned to the experimental group followed the ketogenic stage for eight weeks and then moved to the second, low-calorie diet phase for an additional eight weeks, while those in the control group (hypocaloric diet) followed the low-calorie diet for all 16 weeks.”
The primary outcomes were changes in weight and body composition, specifically fat mass and lean mass, measured by bioimpedance. “The changes observed in the following aspects were considered secondary outcomes: abdominal fat distribution, metabolic parameters, ovulation, ovarian morphology, hirsutism, hyperandrogenism, psychological well-being, and psychological distress,” said Dr. Gambineri. “Any reduction in the ovarian stroma, the area where androgens are synthesized, was also analyzed.”
The study authors found that although BMI decreased in both groups, this reduction was greater in the group that followed the very-low-calorie ketogenic diet. Significant weight loss was observed in both groups, 12.4 kg versus 4.7 kg. Significant differences were also observed in waist circumference (−8.1% in the experimental group vs. −2.2% in the control group), fat mass (−15.1% vs. −8.5%), and free testosterone (−30.3% vs. +10.6%). Only the experimental group saw a reduction in insulin.
“A key point regarding hyperandrogenism, especially regarding what’s referred to as free testosterone, there was only a significant reduction in the very-low-calorie ketogenic diet group,” said Dr. Gambineri. “This reduction was especially evident in the first part of the study, coinciding with the ketogenic period. The reason for this effect lies in the significant increase in the concentration of sex hormone-binding globulins, SHB6. Said globulins bind to the testosterone present in female blood, producing a reduction in free testosterone, a very important effect considering that this syndrome is an androgenic disorder. Furthermore, current treatments for polycystic ovary syndrome do not reduce free testosterone as much as this dietary approach does.”
For the specialist, among all these positive effects in these patients, perhaps most important is the notable improvement that occurs in ovulation. “At the beginning of the study, only 38.5% of the participants in the experimental group and 14.3% of those in the control group had ovulatory cycles. After the intervention, 84.6% managed to ovulate, compared to 35.7% who achieved this goal in the other group.”
Dr. Gambineri suggested that this method is “valid for reducing fat mass and rapidly improving hyperandrogenism and ovulatory dysfunction in women with obesity and polycystic ovary syndrome.”
Reversing type 2 diabetes?
Daniela Sofrà, MD, an endocrinologist specializing in diabetology at La Source Clinic, Lausanne, Switzerland, reviewed the current evidence on the role of the very-low-calorie ketogenic diet in the management of type 2 diabetes.
“It’s time to rethink diabetes treatment and focus efforts on managing obesity as an associated factor,” she said. “One of the hypotheses being examined in this regard is the twin cycle, which postulates that type 2 diabetes is the result of excess fat in the liver. This in turn is associated with insulin resistance with pancreas dysfunction.”
Dr. Sofrà added that there is a study documenting for the first time the reversibility of the morphology of the diabetic pancreas after caloric restriction with the very-low-calorie ketogenic diet. “The reason for this effect is the use of visceral and intrahepatic fat, which can lead to the remission of the clinical manifestation of type 2 diabetes, understanding as such the definition made by the American Diabetes Association: glycosylated hemoglobin < 6.5% without pharmacological therapy.”
Specifically, the results of this research showed that after following the very-low-calorie ketogenic diet and achieving a 15% weight loss (mean weight loss of the participants), liver glucose levels returned to normal levels within 7 days. Beta cell function returned to near normal within 8 weeks.
“Subsequent studies have shown the durability of remission of type 2 diabetes, thanks to the reactivation of the insulin-secreting function of beta cells that had become dedifferentiated in the face of chronic nutrient excess. Specifically, 6 out of 10 patients maintained glycosylated hemoglobin < 6% after 6 months without the need for pharmacological therapy,” Dr. Sofrà added.
Likewise, she highlighted that the probability of achieving remission is mainly determined by the duration of the disease. “The years with diabetes are one of the main predictors of the response that the patient will have with this dietary intervention. Studies have shown that remission is possible in patients with diabetes for less than 6 years, although there are other projects that indicate that it can be achieved with up to 10 years’ duration.”
Based on these data, Dr. Sofrà emphasized the pleiotropic effects of the very-low-calorie ketogenic diet on glycemic control, favoring the possible remission of diabetes or the reduction of drugs, as well as the reduction of the HOMA-IR index (insulin resistance) and waist circumference in people with type 2 diabetes.
Nonalcoholic fatty liver disease
The third comorbidity of obesity that may benefit from the very-low-calorie ketogenic diet is hepatic steatosis, or nonalcoholic fatty liver disease, said Hardy Walle, MD, an internal medicine specialist and director/founder of the Bodymed center, Kirkel, Germany, and one of the authors of this research.
“Recent research shows that ectopic fat and nonalcoholic fatty liver disease could be considered a cause, or at least one of the causes, of most of the diseases that affect the population as a consequence of overweight and obesity,” said Dr. Walle. “Some authors have stated that without fatty liver, there is no type 2 diabetes.”
Dr. Walle pointed out that between 30% and 40% of the adult population has nonalcoholic fatty liver disease, a percentage that increases considerably in people with obesity, reaching 70% prevalence and increasing, in the case of type 2 diabetes, to almost 90%. “Even normal weight does not rule out fatty liver; in fact, about 15% of people with nonalcoholic fatty liver disease are not overweight.”
In a setting where there are no approved drugs for the treatment of fatty liver (the current standard approach focuses on lifestyle interventions), a short-term hypocaloric diet (or liver fasting) is considered an effective method for management of this pathology. This principle was demonstrated by a study by the Saarland University, Saarbrücken, Germany, that Dr. Walle used to illustrate this statement.
“The participants (60 patients with hepatic steatosis) followed a hypocaloric diet (less than 1,000 kcal/day) for 14 days with a formula rich in protein and fiber specially developed for the treatment of nonalcoholic fatty liver disease. A fibroscan was then performed with controlled attenuation parameter measurement to quantify fatty liver disease. The results showed not only a significant improvement in nonalcoholic fatty liver disease parameters but also a marked improvement in all relevant metabolic parameters (serum lipids, liver enzymes),” explained Dr. Walle.
“This evidence leads us to affirm that the concept of hepatic fasting (by means of a hypocaloric diet) marks a point of reference for a future treatment approach for nonalcoholic fatty liver disease,” he concluded.
The study that Dr. Gambineri presented was carried out with the collaboration of the Pronokal Group (Nestlé Health Science). Dr. Gambineri, Dr. Sofrà, and Dr. Walle disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MADRID – During the International Scientific Symposium “New Frontiers in Scientific Research” that recently took place in Barcelona, specialists analyzed the role of the very-low-calorie ketogenic diet. This analysis was in relation to three comorbidities that have a higher incidence among overweight and obese patients: polycystic ovary syndrome, nonalcoholic fatty liver disease, and type 2 diabetes. The experts’ aim? To analyze and update the latest evidence on the benefits of this dietary choice.
Polycystic ovary syndrome
Alessandra Gambineri, MD, PhD, associate professor at the department of medicine and surgery (DIMEC) at the University of Bologna, Italy, addressed the link between obesity and polycystic ovary syndrome, which she described as a chronic disease that affects about 10% of women of childbearing age and that presents diverse phenotypes with different characteristics.
“The pathophysiology of this syndrome is characterized by the interaction of three factors: androgen excess, adipose tissue dysfunction, and insulin resistance. These factors interact with each other and are expressed differently in each phenotype,” said Dr. Gambineri.
She indicated that adipose tissue dysfunction is central to this pathology. This centrality results from its association with secretions, such as free fatty acids, proinflammatory cytokines, certain adipokines that promote insulin resistance, glucocorticosteroids, androgens, and oxidative stress.
“Similarly, the oxidative stress that characterizes this syndrome is increasingly present in obese individuals,” said Dr. Gambineri. “This oxidative stress also produces ovary hypotoxicity that aggravates ovulatory function. In this context, the very-low-calorie ketogenic diet can be useful in several ways: weight reduction; promoting the loss of mainly visceral/abdominal fat; decreasing lipotoxicity; and improving inflammation, hyperinsulinemia, and insulin resistance.”
This was the path followed to carry out a study that aimed to analyze the effects of the very-low-calorie ketogenic diet on manifestations of polycystic ovary syndrome in the obesity phenotype. Dr. Gambineri presented its results.
“The objective was to compare the effects of a very-low-calorie ketogenic diet and the standard low-calorie (hypocaloric) diet as a control group,” she said. “The effects studied include body weight, insulin resistance, menstrual cycle, ovulation, ovarian morphology, and hyperandrogenism in a population of 30 obese women with polycystic ovary syndrome and insulin resistance.”
Study participants had a diagnosis of polycystic ovary syndrome as defined by the National Institutes of Health criteria and were aged 18-45 years. These women were randomly assigned to two groups of equal size: experimental (very-low-calorie ketogenic diet) and control (hypocaloric diet). “The women assigned to the experimental group followed the ketogenic stage for eight weeks and then moved to the second, low-calorie diet phase for an additional eight weeks, while those in the control group (hypocaloric diet) followed the low-calorie diet for all 16 weeks.”
The primary outcomes were changes in weight and body composition, specifically fat mass and lean mass, measured by bioimpedance. “The changes observed in the following aspects were considered secondary outcomes: abdominal fat distribution, metabolic parameters, ovulation, ovarian morphology, hirsutism, hyperandrogenism, psychological well-being, and psychological distress,” said Dr. Gambineri. “Any reduction in the ovarian stroma, the area where androgens are synthesized, was also analyzed.”
The study authors found that although BMI decreased in both groups, this reduction was greater in the group that followed the very-low-calorie ketogenic diet. Significant weight loss was observed in both groups, 12.4 kg versus 4.7 kg. Significant differences were also observed in waist circumference (−8.1% in the experimental group vs. −2.2% in the control group), fat mass (−15.1% vs. −8.5%), and free testosterone (−30.3% vs. +10.6%). Only the experimental group saw a reduction in insulin.
“A key point regarding hyperandrogenism, especially regarding what’s referred to as free testosterone, there was only a significant reduction in the very-low-calorie ketogenic diet group,” said Dr. Gambineri. “This reduction was especially evident in the first part of the study, coinciding with the ketogenic period. The reason for this effect lies in the significant increase in the concentration of sex hormone-binding globulins, SHB6. Said globulins bind to the testosterone present in female blood, producing a reduction in free testosterone, a very important effect considering that this syndrome is an androgenic disorder. Furthermore, current treatments for polycystic ovary syndrome do not reduce free testosterone as much as this dietary approach does.”
For the specialist, among all these positive effects in these patients, perhaps most important is the notable improvement that occurs in ovulation. “At the beginning of the study, only 38.5% of the participants in the experimental group and 14.3% of those in the control group had ovulatory cycles. After the intervention, 84.6% managed to ovulate, compared to 35.7% who achieved this goal in the other group.”
Dr. Gambineri suggested that this method is “valid for reducing fat mass and rapidly improving hyperandrogenism and ovulatory dysfunction in women with obesity and polycystic ovary syndrome.”
Reversing type 2 diabetes?
Daniela Sofrà, MD, an endocrinologist specializing in diabetology at La Source Clinic, Lausanne, Switzerland, reviewed the current evidence on the role of the very-low-calorie ketogenic diet in the management of type 2 diabetes.
“It’s time to rethink diabetes treatment and focus efforts on managing obesity as an associated factor,” she said. “One of the hypotheses being examined in this regard is the twin cycle, which postulates that type 2 diabetes is the result of excess fat in the liver. This in turn is associated with insulin resistance with pancreas dysfunction.”
Dr. Sofrà added that there is a study documenting for the first time the reversibility of the morphology of the diabetic pancreas after caloric restriction with the very-low-calorie ketogenic diet. “The reason for this effect is the use of visceral and intrahepatic fat, which can lead to the remission of the clinical manifestation of type 2 diabetes, understanding as such the definition made by the American Diabetes Association: glycosylated hemoglobin < 6.5% without pharmacological therapy.”
Specifically, the results of this research showed that after following the very-low-calorie ketogenic diet and achieving a 15% weight loss (mean weight loss of the participants), liver glucose levels returned to normal levels within 7 days. Beta cell function returned to near normal within 8 weeks.
“Subsequent studies have shown the durability of remission of type 2 diabetes, thanks to the reactivation of the insulin-secreting function of beta cells that had become dedifferentiated in the face of chronic nutrient excess. Specifically, 6 out of 10 patients maintained glycosylated hemoglobin < 6% after 6 months without the need for pharmacological therapy,” Dr. Sofrà added.
Likewise, she highlighted that the probability of achieving remission is mainly determined by the duration of the disease. “The years with diabetes are one of the main predictors of the response that the patient will have with this dietary intervention. Studies have shown that remission is possible in patients with diabetes for less than 6 years, although there are other projects that indicate that it can be achieved with up to 10 years’ duration.”
Based on these data, Dr. Sofrà emphasized the pleiotropic effects of the very-low-calorie ketogenic diet on glycemic control, favoring the possible remission of diabetes or the reduction of drugs, as well as the reduction of the HOMA-IR index (insulin resistance) and waist circumference in people with type 2 diabetes.
Nonalcoholic fatty liver disease
The third comorbidity of obesity that may benefit from the very-low-calorie ketogenic diet is hepatic steatosis, or nonalcoholic fatty liver disease, said Hardy Walle, MD, an internal medicine specialist and director/founder of the Bodymed center, Kirkel, Germany, and one of the authors of this research.
“Recent research shows that ectopic fat and nonalcoholic fatty liver disease could be considered a cause, or at least one of the causes, of most of the diseases that affect the population as a consequence of overweight and obesity,” said Dr. Walle. “Some authors have stated that without fatty liver, there is no type 2 diabetes.”
Dr. Walle pointed out that between 30% and 40% of the adult population has nonalcoholic fatty liver disease, a percentage that increases considerably in people with obesity, reaching 70% prevalence and increasing, in the case of type 2 diabetes, to almost 90%. “Even normal weight does not rule out fatty liver; in fact, about 15% of people with nonalcoholic fatty liver disease are not overweight.”
In a setting where there are no approved drugs for the treatment of fatty liver (the current standard approach focuses on lifestyle interventions), a short-term hypocaloric diet (or liver fasting) is considered an effective method for management of this pathology. This principle was demonstrated by a study by the Saarland University, Saarbrücken, Germany, that Dr. Walle used to illustrate this statement.
“The participants (60 patients with hepatic steatosis) followed a hypocaloric diet (less than 1,000 kcal/day) for 14 days with a formula rich in protein and fiber specially developed for the treatment of nonalcoholic fatty liver disease. A fibroscan was then performed with controlled attenuation parameter measurement to quantify fatty liver disease. The results showed not only a significant improvement in nonalcoholic fatty liver disease parameters but also a marked improvement in all relevant metabolic parameters (serum lipids, liver enzymes),” explained Dr. Walle.
“This evidence leads us to affirm that the concept of hepatic fasting (by means of a hypocaloric diet) marks a point of reference for a future treatment approach for nonalcoholic fatty liver disease,” he concluded.
The study that Dr. Gambineri presented was carried out with the collaboration of the Pronokal Group (Nestlé Health Science). Dr. Gambineri, Dr. Sofrà, and Dr. Walle disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MADRID – During the International Scientific Symposium “New Frontiers in Scientific Research” that recently took place in Barcelona, specialists analyzed the role of the very-low-calorie ketogenic diet. This analysis was in relation to three comorbidities that have a higher incidence among overweight and obese patients: polycystic ovary syndrome, nonalcoholic fatty liver disease, and type 2 diabetes. The experts’ aim? To analyze and update the latest evidence on the benefits of this dietary choice.
Polycystic ovary syndrome
Alessandra Gambineri, MD, PhD, associate professor at the department of medicine and surgery (DIMEC) at the University of Bologna, Italy, addressed the link between obesity and polycystic ovary syndrome, which she described as a chronic disease that affects about 10% of women of childbearing age and that presents diverse phenotypes with different characteristics.
“The pathophysiology of this syndrome is characterized by the interaction of three factors: androgen excess, adipose tissue dysfunction, and insulin resistance. These factors interact with each other and are expressed differently in each phenotype,” said Dr. Gambineri.
She indicated that adipose tissue dysfunction is central to this pathology. This centrality results from its association with secretions, such as free fatty acids, proinflammatory cytokines, certain adipokines that promote insulin resistance, glucocorticosteroids, androgens, and oxidative stress.
“Similarly, the oxidative stress that characterizes this syndrome is increasingly present in obese individuals,” said Dr. Gambineri. “This oxidative stress also produces ovary hypotoxicity that aggravates ovulatory function. In this context, the very-low-calorie ketogenic diet can be useful in several ways: weight reduction; promoting the loss of mainly visceral/abdominal fat; decreasing lipotoxicity; and improving inflammation, hyperinsulinemia, and insulin resistance.”
This was the path followed to carry out a study that aimed to analyze the effects of the very-low-calorie ketogenic diet on manifestations of polycystic ovary syndrome in the obesity phenotype. Dr. Gambineri presented its results.
“The objective was to compare the effects of a very-low-calorie ketogenic diet and the standard low-calorie (hypocaloric) diet as a control group,” she said. “The effects studied include body weight, insulin resistance, menstrual cycle, ovulation, ovarian morphology, and hyperandrogenism in a population of 30 obese women with polycystic ovary syndrome and insulin resistance.”
Study participants had a diagnosis of polycystic ovary syndrome as defined by the National Institutes of Health criteria and were aged 18-45 years. These women were randomly assigned to two groups of equal size: experimental (very-low-calorie ketogenic diet) and control (hypocaloric diet). “The women assigned to the experimental group followed the ketogenic stage for eight weeks and then moved to the second, low-calorie diet phase for an additional eight weeks, while those in the control group (hypocaloric diet) followed the low-calorie diet for all 16 weeks.”
The primary outcomes were changes in weight and body composition, specifically fat mass and lean mass, measured by bioimpedance. “The changes observed in the following aspects were considered secondary outcomes: abdominal fat distribution, metabolic parameters, ovulation, ovarian morphology, hirsutism, hyperandrogenism, psychological well-being, and psychological distress,” said Dr. Gambineri. “Any reduction in the ovarian stroma, the area where androgens are synthesized, was also analyzed.”
The study authors found that although BMI decreased in both groups, this reduction was greater in the group that followed the very-low-calorie ketogenic diet. Significant weight loss was observed in both groups, 12.4 kg versus 4.7 kg. Significant differences were also observed in waist circumference (−8.1% in the experimental group vs. −2.2% in the control group), fat mass (−15.1% vs. −8.5%), and free testosterone (−30.3% vs. +10.6%). Only the experimental group saw a reduction in insulin.
“A key point regarding hyperandrogenism, especially regarding what’s referred to as free testosterone, there was only a significant reduction in the very-low-calorie ketogenic diet group,” said Dr. Gambineri. “This reduction was especially evident in the first part of the study, coinciding with the ketogenic period. The reason for this effect lies in the significant increase in the concentration of sex hormone-binding globulins, SHB6. Said globulins bind to the testosterone present in female blood, producing a reduction in free testosterone, a very important effect considering that this syndrome is an androgenic disorder. Furthermore, current treatments for polycystic ovary syndrome do not reduce free testosterone as much as this dietary approach does.”
For the specialist, among all these positive effects in these patients, perhaps most important is the notable improvement that occurs in ovulation. “At the beginning of the study, only 38.5% of the participants in the experimental group and 14.3% of those in the control group had ovulatory cycles. After the intervention, 84.6% managed to ovulate, compared to 35.7% who achieved this goal in the other group.”
Dr. Gambineri suggested that this method is “valid for reducing fat mass and rapidly improving hyperandrogenism and ovulatory dysfunction in women with obesity and polycystic ovary syndrome.”
Reversing type 2 diabetes?
Daniela Sofrà, MD, an endocrinologist specializing in diabetology at La Source Clinic, Lausanne, Switzerland, reviewed the current evidence on the role of the very-low-calorie ketogenic diet in the management of type 2 diabetes.
“It’s time to rethink diabetes treatment and focus efforts on managing obesity as an associated factor,” she said. “One of the hypotheses being examined in this regard is the twin cycle, which postulates that type 2 diabetes is the result of excess fat in the liver. This in turn is associated with insulin resistance with pancreas dysfunction.”
Dr. Sofrà added that there is a study documenting for the first time the reversibility of the morphology of the diabetic pancreas after caloric restriction with the very-low-calorie ketogenic diet. “The reason for this effect is the use of visceral and intrahepatic fat, which can lead to the remission of the clinical manifestation of type 2 diabetes, understanding as such the definition made by the American Diabetes Association: glycosylated hemoglobin < 6.5% without pharmacological therapy.”
Specifically, the results of this research showed that after following the very-low-calorie ketogenic diet and achieving a 15% weight loss (mean weight loss of the participants), liver glucose levels returned to normal levels within 7 days. Beta cell function returned to near normal within 8 weeks.
“Subsequent studies have shown the durability of remission of type 2 diabetes, thanks to the reactivation of the insulin-secreting function of beta cells that had become dedifferentiated in the face of chronic nutrient excess. Specifically, 6 out of 10 patients maintained glycosylated hemoglobin < 6% after 6 months without the need for pharmacological therapy,” Dr. Sofrà added.
Likewise, she highlighted that the probability of achieving remission is mainly determined by the duration of the disease. “The years with diabetes are one of the main predictors of the response that the patient will have with this dietary intervention. Studies have shown that remission is possible in patients with diabetes for less than 6 years, although there are other projects that indicate that it can be achieved with up to 10 years’ duration.”
Based on these data, Dr. Sofrà emphasized the pleiotropic effects of the very-low-calorie ketogenic diet on glycemic control, favoring the possible remission of diabetes or the reduction of drugs, as well as the reduction of the HOMA-IR index (insulin resistance) and waist circumference in people with type 2 diabetes.
Nonalcoholic fatty liver disease
The third comorbidity of obesity that may benefit from the very-low-calorie ketogenic diet is hepatic steatosis, or nonalcoholic fatty liver disease, said Hardy Walle, MD, an internal medicine specialist and director/founder of the Bodymed center, Kirkel, Germany, and one of the authors of this research.
“Recent research shows that ectopic fat and nonalcoholic fatty liver disease could be considered a cause, or at least one of the causes, of most of the diseases that affect the population as a consequence of overweight and obesity,” said Dr. Walle. “Some authors have stated that without fatty liver, there is no type 2 diabetes.”
Dr. Walle pointed out that between 30% and 40% of the adult population has nonalcoholic fatty liver disease, a percentage that increases considerably in people with obesity, reaching 70% prevalence and increasing, in the case of type 2 diabetes, to almost 90%. “Even normal weight does not rule out fatty liver; in fact, about 15% of people with nonalcoholic fatty liver disease are not overweight.”
In a setting where there are no approved drugs for the treatment of fatty liver (the current standard approach focuses on lifestyle interventions), a short-term hypocaloric diet (or liver fasting) is considered an effective method for management of this pathology. This principle was demonstrated by a study by the Saarland University, Saarbrücken, Germany, that Dr. Walle used to illustrate this statement.
“The participants (60 patients with hepatic steatosis) followed a hypocaloric diet (less than 1,000 kcal/day) for 14 days with a formula rich in protein and fiber specially developed for the treatment of nonalcoholic fatty liver disease. A fibroscan was then performed with controlled attenuation parameter measurement to quantify fatty liver disease. The results showed not only a significant improvement in nonalcoholic fatty liver disease parameters but also a marked improvement in all relevant metabolic parameters (serum lipids, liver enzymes),” explained Dr. Walle.
“This evidence leads us to affirm that the concept of hepatic fasting (by means of a hypocaloric diet) marks a point of reference for a future treatment approach for nonalcoholic fatty liver disease,” he concluded.
The study that Dr. Gambineri presented was carried out with the collaboration of the Pronokal Group (Nestlé Health Science). Dr. Gambineri, Dr. Sofrà, and Dr. Walle disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Disturbed sleep drives poor PrEP adherence in young Black sexual-minority men
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.



