User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Bleeding arm lesion

Pyogenic granulomas (PGs), also called lobular capillary hemangiomas, manifest as friable, moist or glistening, papules. PGs are a benign vascular proliferation. They often have a collarette, which is subtle in this lesion, and they bleed with minimal trauma. They are commonly seen on the gingiva during pregnancy, the umbilical area in newborns, or at sites of trauma.
Since PGs often occur during pregnancy, it’s been suggested that their development is related to hormonal changes.1 It’s also been suggested that PGs are the result of an abnormal hypertrophic healing response, as they can occur in men, infants (at the umbilical stump), and even within blood vessels.1
Although benign and painless, PGs are usually hard to ignore due to their raised appearance, tendency to bleed, and the low likelihood that they will resolve on their own. There are multiple physical treatment options available, including excision with primary closure, curettage followed by electrodessication, laser treatment, and cryosurgery. Topical therapies include timolol (a beta-blocker that has been used successfully with congenital hemangiomas), imiquimod, and trichloroacetic acid.1 These topical medications do not require any anesthetic, which may make them an appealing option for children. Unfortunately, topical medications require multiple applications over a period of 2 or more weeks.
In this case, the lesion was shaved off and sent out to pathology to rule out amelanotic melanoma. The pathology for this patient confirmed PG. Immediately following the lesion’s removal, the physician performed 2 cycles of curettage and electrodessication. Thus, the patient’s treatment was completed on the same day as her evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. Int J Dermatol. 2019;58:642-648. doi: 10.1111/ijd.14268

Pyogenic granulomas (PGs), also called lobular capillary hemangiomas, manifest as friable, moist or glistening, papules. PGs are a benign vascular proliferation. They often have a collarette, which is subtle in this lesion, and they bleed with minimal trauma. They are commonly seen on the gingiva during pregnancy, the umbilical area in newborns, or at sites of trauma.
Since PGs often occur during pregnancy, it’s been suggested that their development is related to hormonal changes.1 It’s also been suggested that PGs are the result of an abnormal hypertrophic healing response, as they can occur in men, infants (at the umbilical stump), and even within blood vessels.1
Although benign and painless, PGs are usually hard to ignore due to their raised appearance, tendency to bleed, and the low likelihood that they will resolve on their own. There are multiple physical treatment options available, including excision with primary closure, curettage followed by electrodessication, laser treatment, and cryosurgery. Topical therapies include timolol (a beta-blocker that has been used successfully with congenital hemangiomas), imiquimod, and trichloroacetic acid.1 These topical medications do not require any anesthetic, which may make them an appealing option for children. Unfortunately, topical medications require multiple applications over a period of 2 or more weeks.
In this case, the lesion was shaved off and sent out to pathology to rule out amelanotic melanoma. The pathology for this patient confirmed PG. Immediately following the lesion’s removal, the physician performed 2 cycles of curettage and electrodessication. Thus, the patient’s treatment was completed on the same day as her evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.

Pyogenic granulomas (PGs), also called lobular capillary hemangiomas, manifest as friable, moist or glistening, papules. PGs are a benign vascular proliferation. They often have a collarette, which is subtle in this lesion, and they bleed with minimal trauma. They are commonly seen on the gingiva during pregnancy, the umbilical area in newborns, or at sites of trauma.
Since PGs often occur during pregnancy, it’s been suggested that their development is related to hormonal changes.1 It’s also been suggested that PGs are the result of an abnormal hypertrophic healing response, as they can occur in men, infants (at the umbilical stump), and even within blood vessels.1
Although benign and painless, PGs are usually hard to ignore due to their raised appearance, tendency to bleed, and the low likelihood that they will resolve on their own. There are multiple physical treatment options available, including excision with primary closure, curettage followed by electrodessication, laser treatment, and cryosurgery. Topical therapies include timolol (a beta-blocker that has been used successfully with congenital hemangiomas), imiquimod, and trichloroacetic acid.1 These topical medications do not require any anesthetic, which may make them an appealing option for children. Unfortunately, topical medications require multiple applications over a period of 2 or more weeks.
In this case, the lesion was shaved off and sent out to pathology to rule out amelanotic melanoma. The pathology for this patient confirmed PG. Immediately following the lesion’s removal, the physician performed 2 cycles of curettage and electrodessication. Thus, the patient’s treatment was completed on the same day as her evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. Int J Dermatol. 2019;58:642-648. doi: 10.1111/ijd.14268
1. Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. Int J Dermatol. 2019;58:642-648. doi: 10.1111/ijd.14268
Pediatric obesity disparities widen
Lower levels of household income and education in the United States are associated with higher rates of adolescent obesity. These socioeconomic disparities “have widened during the last two decades,” new research shows.
Because obesity in adolescence has immediate and long-term health consequences, this phenomenon “may exacerbate socioeconomic disparities in chronic diseases into adulthood,” study author Ryunosuke Goto, MD, of University of Tokyo Hospital, and colleagues reported in JAMA Pediatrics.
Groups with higher rates of obesity may also be less likely to access treatment, said Kyung E. Rhee, MD, professor of pediatrics at University of California, San Diego School of Medicine, who was not involved in the new analysis.
“These are the families who have a harder time getting to the doctor’s office or getting to programs because they are working multiple jobs, or they don’t have as much flexibility,” Dr. Rhee told this news organization.
20 years of data
A recent study showed a relationship between socioeconomic status (SES) and weight in adults. Research examining current trends in adolescents has been limited, however, according to the authors of the new study.
To address this gap, Dr. Goto and colleagues looked at obesity trends among approximately 20,000 U.S. children aged 10-19 years using cross-sectional data from the 1999-2018 National Health and Nutrition Examination Surveys.
They compared the prevalence of obesity among participants whose household income was 138% of the federal poverty level or less versus those with higher levels of household income. They also examined obesity prevalence according to whether the head of household had graduated college.
Relative to higher-income households, adolescents from lower-income households were more likely to be non-Hispanic Black (21.7% vs. 10.4%) or Hispanic (30.6% vs. 13.4%) and to have an unmarried parent (54.5% vs. 23%). They were also more likely to have obesity (22.8% vs. 17.3%).
The prevalence of obesity likewise was higher among adolescents whose head of household did not have a college degree (21.8% vs. 11.6%).
In an analysis that adjusted for race, ethnicity, height, and marital status of the head of household, the prevalence of obesity increased over 20 years, particularly among adolescents from lower-income homes, the researchers reported.
Lower income was associated with an increase in obesity prevalence of 4.2 percentage points, and less education was associated with an increase in obesity prevalence of 9 percentage points.
By 2015-2018, the gap in obesity prevalence between low-income households and higher-income households was 6.4 percentage points more than it had been during 1999-2002 (95% confidence interval, 1.5-11.4). “When we assessed linear trends, the gap in obesity prevalence by income and education increased by an average of 1.5 (95% CI, 0.4-2.6) and 1.1 (95% CI, 0.0-2.3) percentage points every 4 years, respectively,” according to the researchers.
How to treat
Separately, researchers are studying ways to help treat patients with obesity and increase access to treatment. To that end, Dr. Rhee and colleagues developed a new program called Guided Self-Help Obesity Treatment in the Doctor’s Office (GOT Doc).
The guided self-help program was designed to provide similar resources as a leading treatment approach – family-based treatment – but in a less intensive, more accessible way.
Results from a randomized trial comparing this guided self-help approach with family-based treatment were published in Pediatrics.
The trial included 159 children and their parents. The children had an average age of 9.6 years and body mass index z-score of 2.1. Participants were primarily Latinx and from lower income neighborhoods.
Whereas family-based treatment included hour-long sessions at an academic center, the guided self-help program featured a 20-minute session in the office where patients typically see their primary care physician.
Both programs covered how to self-monitor food intake, set healthy goals, and modify the home environment to promote behavioral change. They also discussed body image, bullying, and emotional health. The program is framed around developing a healthy lifestyle rather than weight loss itself, Dr. Rhee said.
Children in both groups had significant reductions in their body mass index percentiles after the 6-month treatment programs. The reductions were largely maintained at 6-month follow-up.
Families in the guided self-help program, however, had a 67% lower risk of dropping out of the study and reported greater satisfaction and convenience. They attended more than half of the treatment sessions, whereas participants assigned to family-based treatment attended 1 in 5 sessions, on average.
The trial was conducted before the COVID-19 pandemic. Next, the researchers plan to test delivery of a guided self-help program via video calls, Dr. Rhee said.
Having options readily available for families who are interested in treatment for obesity proved valuable to clinicians, Dr. Rhee said. “They could then just refer them down the hall to the interventionist who was there, who was going to then work with the family to make these changes,” she said.
The study by Dr. Goto and colleagues was supported by grants from the Japan Society for the Promotion of Science. The trial by Dr. Rhee et al. was supported by a grant from the Health Resources and Services Administration. Neither research team had conflict of interest disclosures.
A version of this article first appeared on Medscape.com.
Lower levels of household income and education in the United States are associated with higher rates of adolescent obesity. These socioeconomic disparities “have widened during the last two decades,” new research shows.
Because obesity in adolescence has immediate and long-term health consequences, this phenomenon “may exacerbate socioeconomic disparities in chronic diseases into adulthood,” study author Ryunosuke Goto, MD, of University of Tokyo Hospital, and colleagues reported in JAMA Pediatrics.
Groups with higher rates of obesity may also be less likely to access treatment, said Kyung E. Rhee, MD, professor of pediatrics at University of California, San Diego School of Medicine, who was not involved in the new analysis.
“These are the families who have a harder time getting to the doctor’s office or getting to programs because they are working multiple jobs, or they don’t have as much flexibility,” Dr. Rhee told this news organization.
20 years of data
A recent study showed a relationship between socioeconomic status (SES) and weight in adults. Research examining current trends in adolescents has been limited, however, according to the authors of the new study.
To address this gap, Dr. Goto and colleagues looked at obesity trends among approximately 20,000 U.S. children aged 10-19 years using cross-sectional data from the 1999-2018 National Health and Nutrition Examination Surveys.
They compared the prevalence of obesity among participants whose household income was 138% of the federal poverty level or less versus those with higher levels of household income. They also examined obesity prevalence according to whether the head of household had graduated college.
Relative to higher-income households, adolescents from lower-income households were more likely to be non-Hispanic Black (21.7% vs. 10.4%) or Hispanic (30.6% vs. 13.4%) and to have an unmarried parent (54.5% vs. 23%). They were also more likely to have obesity (22.8% vs. 17.3%).
The prevalence of obesity likewise was higher among adolescents whose head of household did not have a college degree (21.8% vs. 11.6%).
In an analysis that adjusted for race, ethnicity, height, and marital status of the head of household, the prevalence of obesity increased over 20 years, particularly among adolescents from lower-income homes, the researchers reported.
Lower income was associated with an increase in obesity prevalence of 4.2 percentage points, and less education was associated with an increase in obesity prevalence of 9 percentage points.
By 2015-2018, the gap in obesity prevalence between low-income households and higher-income households was 6.4 percentage points more than it had been during 1999-2002 (95% confidence interval, 1.5-11.4). “When we assessed linear trends, the gap in obesity prevalence by income and education increased by an average of 1.5 (95% CI, 0.4-2.6) and 1.1 (95% CI, 0.0-2.3) percentage points every 4 years, respectively,” according to the researchers.
How to treat
Separately, researchers are studying ways to help treat patients with obesity and increase access to treatment. To that end, Dr. Rhee and colleagues developed a new program called Guided Self-Help Obesity Treatment in the Doctor’s Office (GOT Doc).
The guided self-help program was designed to provide similar resources as a leading treatment approach – family-based treatment – but in a less intensive, more accessible way.
Results from a randomized trial comparing this guided self-help approach with family-based treatment were published in Pediatrics.
The trial included 159 children and their parents. The children had an average age of 9.6 years and body mass index z-score of 2.1. Participants were primarily Latinx and from lower income neighborhoods.
Whereas family-based treatment included hour-long sessions at an academic center, the guided self-help program featured a 20-minute session in the office where patients typically see their primary care physician.
Both programs covered how to self-monitor food intake, set healthy goals, and modify the home environment to promote behavioral change. They also discussed body image, bullying, and emotional health. The program is framed around developing a healthy lifestyle rather than weight loss itself, Dr. Rhee said.
Children in both groups had significant reductions in their body mass index percentiles after the 6-month treatment programs. The reductions were largely maintained at 6-month follow-up.
Families in the guided self-help program, however, had a 67% lower risk of dropping out of the study and reported greater satisfaction and convenience. They attended more than half of the treatment sessions, whereas participants assigned to family-based treatment attended 1 in 5 sessions, on average.
The trial was conducted before the COVID-19 pandemic. Next, the researchers plan to test delivery of a guided self-help program via video calls, Dr. Rhee said.
Having options readily available for families who are interested in treatment for obesity proved valuable to clinicians, Dr. Rhee said. “They could then just refer them down the hall to the interventionist who was there, who was going to then work with the family to make these changes,” she said.
The study by Dr. Goto and colleagues was supported by grants from the Japan Society for the Promotion of Science. The trial by Dr. Rhee et al. was supported by a grant from the Health Resources and Services Administration. Neither research team had conflict of interest disclosures.
A version of this article first appeared on Medscape.com.
Lower levels of household income and education in the United States are associated with higher rates of adolescent obesity. These socioeconomic disparities “have widened during the last two decades,” new research shows.
Because obesity in adolescence has immediate and long-term health consequences, this phenomenon “may exacerbate socioeconomic disparities in chronic diseases into adulthood,” study author Ryunosuke Goto, MD, of University of Tokyo Hospital, and colleagues reported in JAMA Pediatrics.
Groups with higher rates of obesity may also be less likely to access treatment, said Kyung E. Rhee, MD, professor of pediatrics at University of California, San Diego School of Medicine, who was not involved in the new analysis.
“These are the families who have a harder time getting to the doctor’s office or getting to programs because they are working multiple jobs, or they don’t have as much flexibility,” Dr. Rhee told this news organization.
20 years of data
A recent study showed a relationship between socioeconomic status (SES) and weight in adults. Research examining current trends in adolescents has been limited, however, according to the authors of the new study.
To address this gap, Dr. Goto and colleagues looked at obesity trends among approximately 20,000 U.S. children aged 10-19 years using cross-sectional data from the 1999-2018 National Health and Nutrition Examination Surveys.
They compared the prevalence of obesity among participants whose household income was 138% of the federal poverty level or less versus those with higher levels of household income. They also examined obesity prevalence according to whether the head of household had graduated college.
Relative to higher-income households, adolescents from lower-income households were more likely to be non-Hispanic Black (21.7% vs. 10.4%) or Hispanic (30.6% vs. 13.4%) and to have an unmarried parent (54.5% vs. 23%). They were also more likely to have obesity (22.8% vs. 17.3%).
The prevalence of obesity likewise was higher among adolescents whose head of household did not have a college degree (21.8% vs. 11.6%).
In an analysis that adjusted for race, ethnicity, height, and marital status of the head of household, the prevalence of obesity increased over 20 years, particularly among adolescents from lower-income homes, the researchers reported.
Lower income was associated with an increase in obesity prevalence of 4.2 percentage points, and less education was associated with an increase in obesity prevalence of 9 percentage points.
By 2015-2018, the gap in obesity prevalence between low-income households and higher-income households was 6.4 percentage points more than it had been during 1999-2002 (95% confidence interval, 1.5-11.4). “When we assessed linear trends, the gap in obesity prevalence by income and education increased by an average of 1.5 (95% CI, 0.4-2.6) and 1.1 (95% CI, 0.0-2.3) percentage points every 4 years, respectively,” according to the researchers.
How to treat
Separately, researchers are studying ways to help treat patients with obesity and increase access to treatment. To that end, Dr. Rhee and colleagues developed a new program called Guided Self-Help Obesity Treatment in the Doctor’s Office (GOT Doc).
The guided self-help program was designed to provide similar resources as a leading treatment approach – family-based treatment – but in a less intensive, more accessible way.
Results from a randomized trial comparing this guided self-help approach with family-based treatment were published in Pediatrics.
The trial included 159 children and their parents. The children had an average age of 9.6 years and body mass index z-score of 2.1. Participants were primarily Latinx and from lower income neighborhoods.
Whereas family-based treatment included hour-long sessions at an academic center, the guided self-help program featured a 20-minute session in the office where patients typically see their primary care physician.
Both programs covered how to self-monitor food intake, set healthy goals, and modify the home environment to promote behavioral change. They also discussed body image, bullying, and emotional health. The program is framed around developing a healthy lifestyle rather than weight loss itself, Dr. Rhee said.
Children in both groups had significant reductions in their body mass index percentiles after the 6-month treatment programs. The reductions were largely maintained at 6-month follow-up.
Families in the guided self-help program, however, had a 67% lower risk of dropping out of the study and reported greater satisfaction and convenience. They attended more than half of the treatment sessions, whereas participants assigned to family-based treatment attended 1 in 5 sessions, on average.
The trial was conducted before the COVID-19 pandemic. Next, the researchers plan to test delivery of a guided self-help program via video calls, Dr. Rhee said.
Having options readily available for families who are interested in treatment for obesity proved valuable to clinicians, Dr. Rhee said. “They could then just refer them down the hall to the interventionist who was there, who was going to then work with the family to make these changes,” she said.
The study by Dr. Goto and colleagues was supported by grants from the Japan Society for the Promotion of Science. The trial by Dr. Rhee et al. was supported by a grant from the Health Resources and Services Administration. Neither research team had conflict of interest disclosures.
A version of this article first appeared on Medscape.com.
iLet system simplifies insulin delivery for type 1 diabetes
This transcript has been edited for clarity.
Today, I’m going to discuss the results of a new automated insulin delivery system that I think can really help many people with type 1 diabetes.
Dr. Steven Russell presented the results at the Advanced Technologies & Treatments for Diabetes meeting. The study focused on the iLet system, which is made by Beta Bionics and has been under development for a while. This was the single-hormone study, so it just looked at their algorithm using insulin alone. Eventually they’re going to study this, looking at the use of insulin plus glucagon together to see if that further improves outcomes.
One of the main reasons I think this study was so cool is because it included over 25% minority individuals who aren’t routinely studied in these insulin device trials. The study also included people who had a wide range of hemoglobin A1c levels; there was no high cut-point here. Over 30% of participants had an A1c greater than 8%. They also studied both children and adults and combined the results together.
Before I talk about the results, let me tell you about the pump. This is a tubed pump that has a sensor that it communicates with – it’s the Dexcom sensor – and it has an algorithm so it does automated insulin delivery. Instead of having to enter all sorts of information into the system, this thing requires that you put in only the patient’s weight. That’s it. From there, the system begins to figure out what the patient needs in terms of automated insulin delivery.
There are several different target settings that can be entered, and they can differ by time of day. There’s basically the time of day that one is eating a meal, so breakfast, lunch, or dinner, and there is the meal size, basically small, medium, and large. The individual enters this in real time so the system knows they’re eating, but other than that, the system just works.
It does this in a way that doesn’t allow for the individual using the pump to fidget with it. They can’t override the system and they can’t put in other insulin doses. The system is just there to take care of their diabetes.
They compared this system with people on any other system, including other automated insulin delivery systems, and put them into this trial. People were randomized to this system vs. whatever they’d been on (that was the control group) and they followed them for 13 weeks, which is not all that long.
There was a 0.5% reduction in A1c between the two groups. There was also an increase in the time in range, and this improvement in time in range happened almost immediately – within the first day or two of people being on the system. In terms of actual numbers, the adult patients started out with a time in range of 56% and this increased to 69% by the end of the study. The biggest improvement was time in range overnight, as is seen with other automated insulin delivery systems.
There was no reduction in time below a glucose level of 54 and there was an increase in the number of episodes of severe hypoglycemia in the group treated with the iLet system, but this was not statistically significant between the two groups.
I think these results are hard to compare with other pivotal trials investigating automated insulin delivery systems. The Tandem pivotal trial was a randomized controlled trial similar to this one, but the Medtronic and Omnipod studies were single-arm trials where patients were compared before and after they used the device.
More than anything, I think what’s important about this system is that it may allow for greater use of automated insulin delivery systems. It may allow primary care providers to use these systems without needing all sorts of support, and patients may be able to use these devices more simply than a device where they have to do carb counting and adjusting in ways that I think tend to be pretty complicated and require higher numeracy and literacy skills.
I couldn’t be happier. I love what they’re doing at Beta Bionics, and I look forward to more results, and in particular, to see if these results improve further when they do a study of insulin and glucagon in their dual-hormone pump system.
Thank you very much. This has been Dr Anne Peters for Medscape.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She disclosed ties with Abbott Diabetes Care, AstraZeneca, Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Today, I’m going to discuss the results of a new automated insulin delivery system that I think can really help many people with type 1 diabetes.
Dr. Steven Russell presented the results at the Advanced Technologies & Treatments for Diabetes meeting. The study focused on the iLet system, which is made by Beta Bionics and has been under development for a while. This was the single-hormone study, so it just looked at their algorithm using insulin alone. Eventually they’re going to study this, looking at the use of insulin plus glucagon together to see if that further improves outcomes.
One of the main reasons I think this study was so cool is because it included over 25% minority individuals who aren’t routinely studied in these insulin device trials. The study also included people who had a wide range of hemoglobin A1c levels; there was no high cut-point here. Over 30% of participants had an A1c greater than 8%. They also studied both children and adults and combined the results together.
Before I talk about the results, let me tell you about the pump. This is a tubed pump that has a sensor that it communicates with – it’s the Dexcom sensor – and it has an algorithm so it does automated insulin delivery. Instead of having to enter all sorts of information into the system, this thing requires that you put in only the patient’s weight. That’s it. From there, the system begins to figure out what the patient needs in terms of automated insulin delivery.
There are several different target settings that can be entered, and they can differ by time of day. There’s basically the time of day that one is eating a meal, so breakfast, lunch, or dinner, and there is the meal size, basically small, medium, and large. The individual enters this in real time so the system knows they’re eating, but other than that, the system just works.
It does this in a way that doesn’t allow for the individual using the pump to fidget with it. They can’t override the system and they can’t put in other insulin doses. The system is just there to take care of their diabetes.
They compared this system with people on any other system, including other automated insulin delivery systems, and put them into this trial. People were randomized to this system vs. whatever they’d been on (that was the control group) and they followed them for 13 weeks, which is not all that long.
There was a 0.5% reduction in A1c between the two groups. There was also an increase in the time in range, and this improvement in time in range happened almost immediately – within the first day or two of people being on the system. In terms of actual numbers, the adult patients started out with a time in range of 56% and this increased to 69% by the end of the study. The biggest improvement was time in range overnight, as is seen with other automated insulin delivery systems.
There was no reduction in time below a glucose level of 54 and there was an increase in the number of episodes of severe hypoglycemia in the group treated with the iLet system, but this was not statistically significant between the two groups.
I think these results are hard to compare with other pivotal trials investigating automated insulin delivery systems. The Tandem pivotal trial was a randomized controlled trial similar to this one, but the Medtronic and Omnipod studies were single-arm trials where patients were compared before and after they used the device.
More than anything, I think what’s important about this system is that it may allow for greater use of automated insulin delivery systems. It may allow primary care providers to use these systems without needing all sorts of support, and patients may be able to use these devices more simply than a device where they have to do carb counting and adjusting in ways that I think tend to be pretty complicated and require higher numeracy and literacy skills.
I couldn’t be happier. I love what they’re doing at Beta Bionics, and I look forward to more results, and in particular, to see if these results improve further when they do a study of insulin and glucagon in their dual-hormone pump system.
Thank you very much. This has been Dr Anne Peters for Medscape.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She disclosed ties with Abbott Diabetes Care, AstraZeneca, Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Today, I’m going to discuss the results of a new automated insulin delivery system that I think can really help many people with type 1 diabetes.
Dr. Steven Russell presented the results at the Advanced Technologies & Treatments for Diabetes meeting. The study focused on the iLet system, which is made by Beta Bionics and has been under development for a while. This was the single-hormone study, so it just looked at their algorithm using insulin alone. Eventually they’re going to study this, looking at the use of insulin plus glucagon together to see if that further improves outcomes.
One of the main reasons I think this study was so cool is because it included over 25% minority individuals who aren’t routinely studied in these insulin device trials. The study also included people who had a wide range of hemoglobin A1c levels; there was no high cut-point here. Over 30% of participants had an A1c greater than 8%. They also studied both children and adults and combined the results together.
Before I talk about the results, let me tell you about the pump. This is a tubed pump that has a sensor that it communicates with – it’s the Dexcom sensor – and it has an algorithm so it does automated insulin delivery. Instead of having to enter all sorts of information into the system, this thing requires that you put in only the patient’s weight. That’s it. From there, the system begins to figure out what the patient needs in terms of automated insulin delivery.
There are several different target settings that can be entered, and they can differ by time of day. There’s basically the time of day that one is eating a meal, so breakfast, lunch, or dinner, and there is the meal size, basically small, medium, and large. The individual enters this in real time so the system knows they’re eating, but other than that, the system just works.
It does this in a way that doesn’t allow for the individual using the pump to fidget with it. They can’t override the system and they can’t put in other insulin doses. The system is just there to take care of their diabetes.
They compared this system with people on any other system, including other automated insulin delivery systems, and put them into this trial. People were randomized to this system vs. whatever they’d been on (that was the control group) and they followed them for 13 weeks, which is not all that long.
There was a 0.5% reduction in A1c between the two groups. There was also an increase in the time in range, and this improvement in time in range happened almost immediately – within the first day or two of people being on the system. In terms of actual numbers, the adult patients started out with a time in range of 56% and this increased to 69% by the end of the study. The biggest improvement was time in range overnight, as is seen with other automated insulin delivery systems.
There was no reduction in time below a glucose level of 54 and there was an increase in the number of episodes of severe hypoglycemia in the group treated with the iLet system, but this was not statistically significant between the two groups.
I think these results are hard to compare with other pivotal trials investigating automated insulin delivery systems. The Tandem pivotal trial was a randomized controlled trial similar to this one, but the Medtronic and Omnipod studies were single-arm trials where patients were compared before and after they used the device.
More than anything, I think what’s important about this system is that it may allow for greater use of automated insulin delivery systems. It may allow primary care providers to use these systems without needing all sorts of support, and patients may be able to use these devices more simply than a device where they have to do carb counting and adjusting in ways that I think tend to be pretty complicated and require higher numeracy and literacy skills.
I couldn’t be happier. I love what they’re doing at Beta Bionics, and I look forward to more results, and in particular, to see if these results improve further when they do a study of insulin and glucagon in their dual-hormone pump system.
Thank you very much. This has been Dr Anne Peters for Medscape.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She disclosed ties with Abbott Diabetes Care, AstraZeneca, Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen.
A version of this article first appeared on Medscape.com.
Children and COVID: Vaccines now available to all ages
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.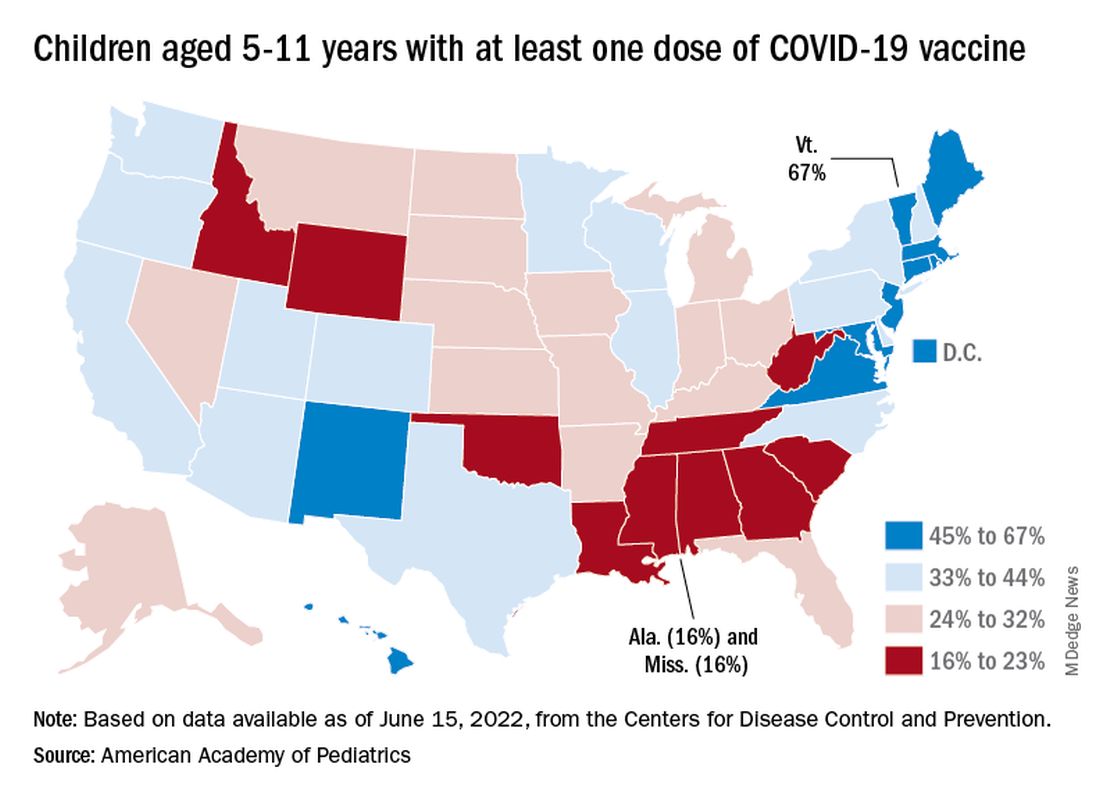
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.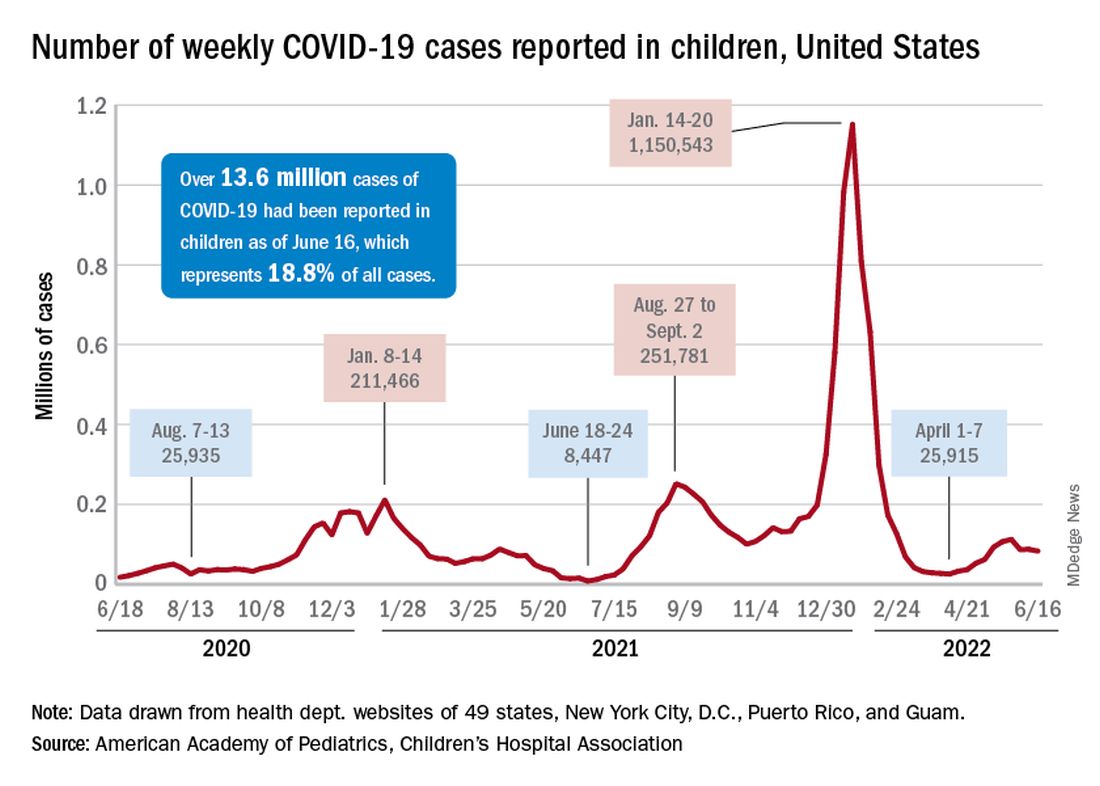
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.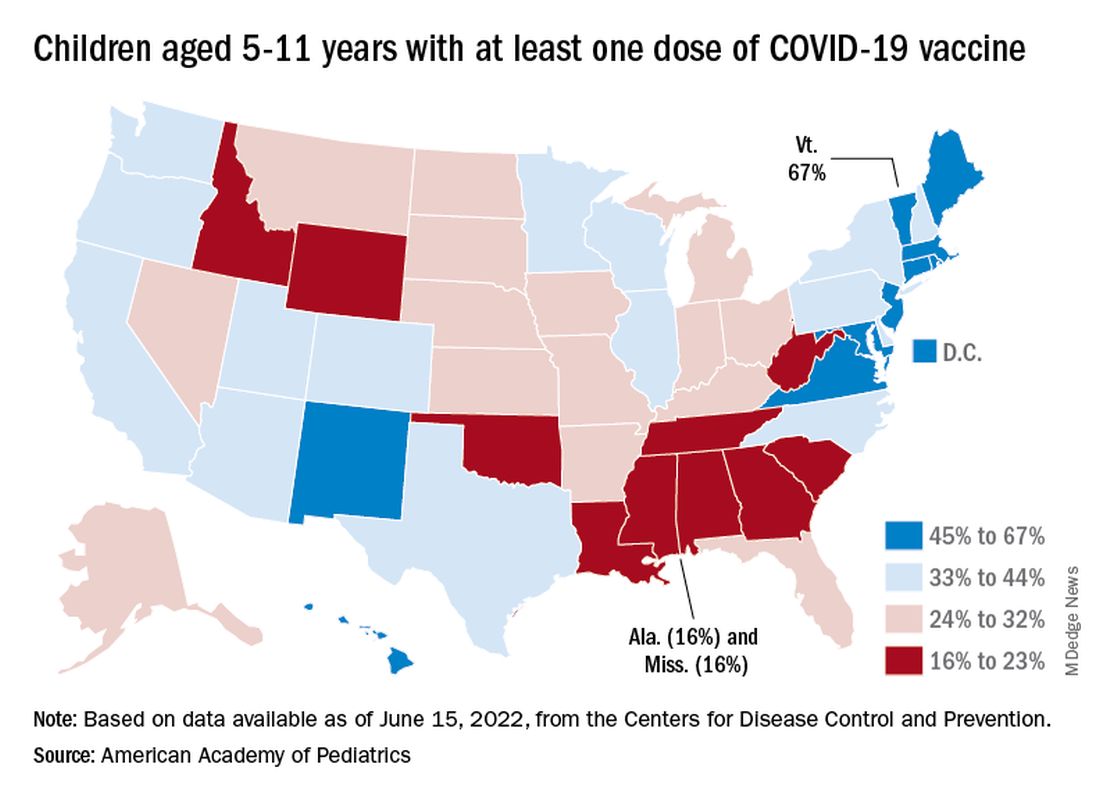
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.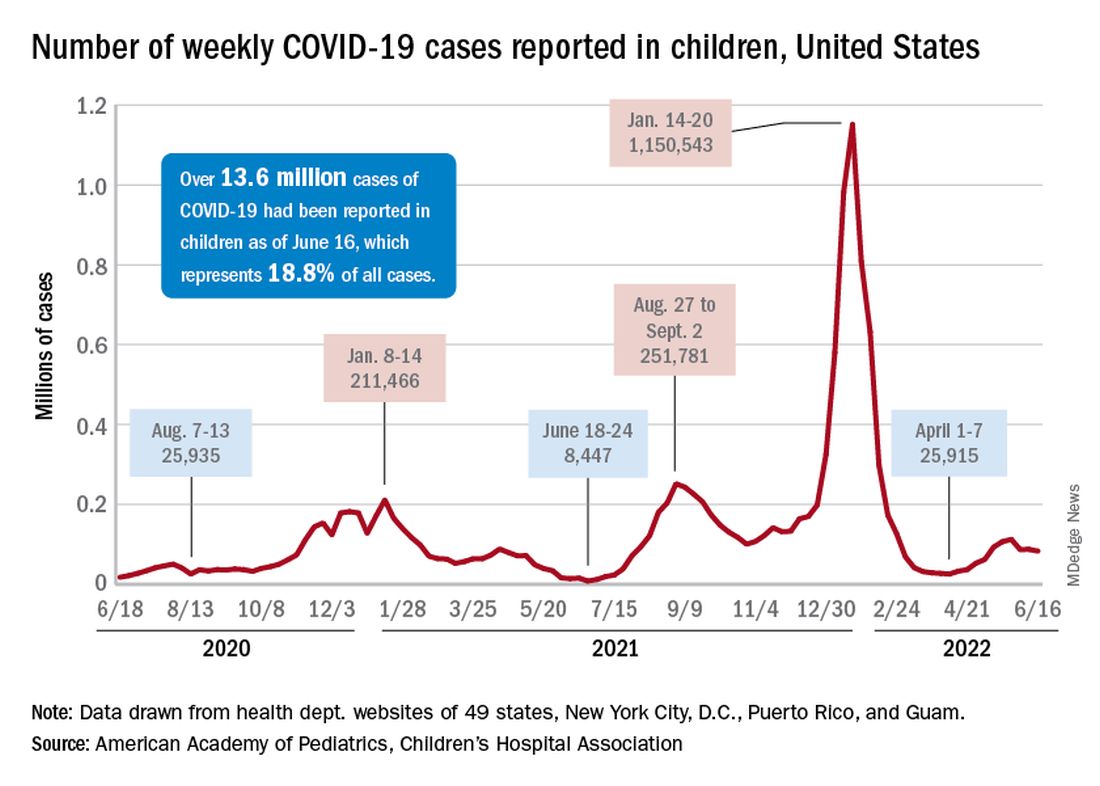
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.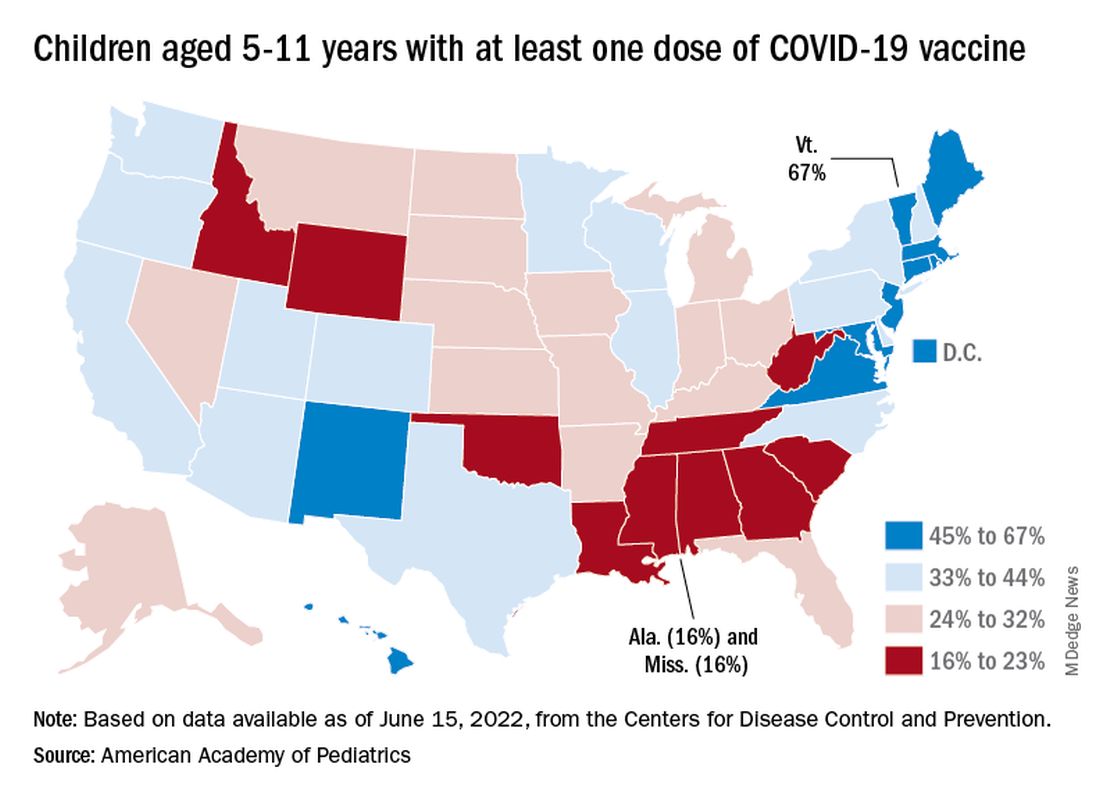
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.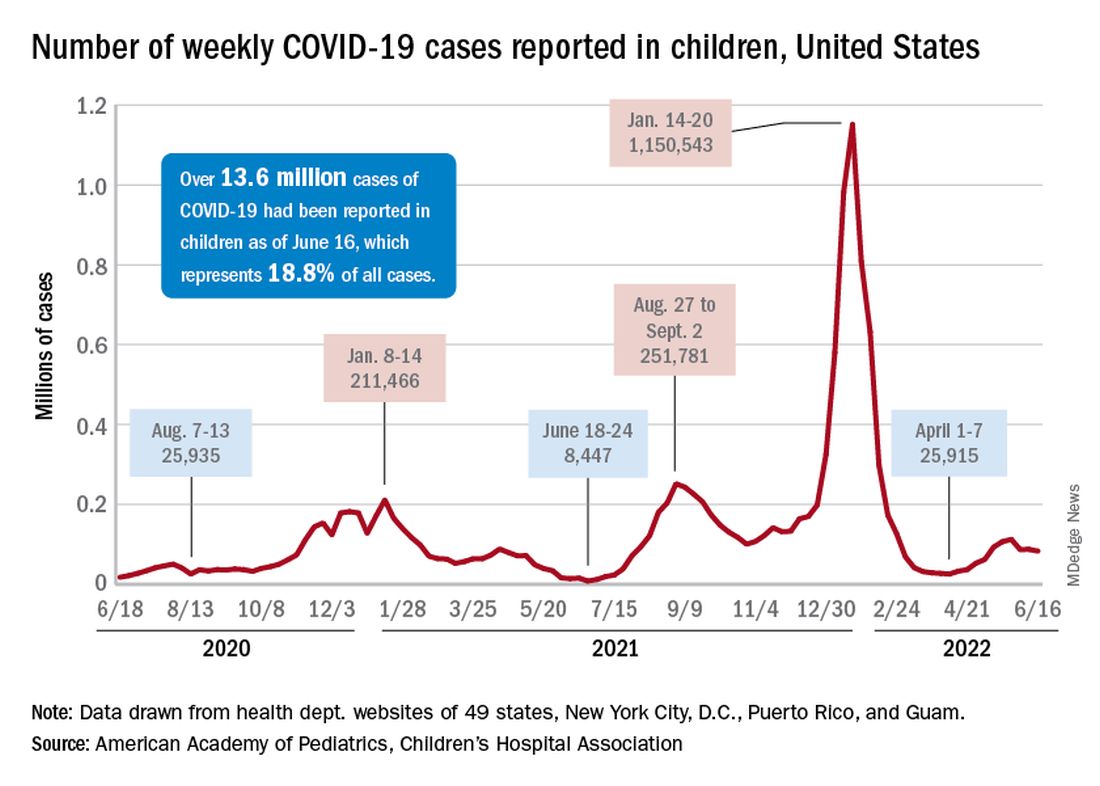
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
Postherpetic Pink, Smooth, Annular Convalescing Plaques
The Diagnosis: Granuloma Annulare
A biopsy of a lesion on the right flank demonstrated granulomatous inflammation and interstitial mucin (Figure), characteristic of granuloma annulare (GA).1,2 Granuloma annulare is a relatively common skin disorder with an unknown etiology. It typically presents as smooth, annular, erythematous plaques.1 The most common variants of GA are localized, generalized, and subcutaneous. Our case demonstrated Wolf isotopic response, an unrelated skin disease that forms at the same location as a previously healed skin lesion.2 It is important to be aware of this phenomenon so that it is not confused with a recurrence of herpes zoster virus (HZV).
Although relatively infrequent, GA is the most common isotopic response following HZV infections.3-5 Other postherpetic isotopic eruptions include cutaneous malignancies, lichen planus, sarcoidosis, morphea, reactive perforating collagenosis, psoriasis, and infections, among others.3,5,6 The time between HZV infection and GA can be variable, ranging from a few weeks to many years apart.3
Oftentimes GA will spontaneously resolve within 2 years; however, recurrence is common.7-9 There currently are no standard treatment guidelines. The most promising treatment options include intralesional or topical glucocorticoids for localized GA as well as phototherapy or hydroxychloroquine for widespread disease.8,10

Annular elastolytic giant cell granuloma (also called actinic granuloma) is a rare idiopathic inflammatory skin disease. It is characterized by erythematous annular papules or plaques mainly found on sun-exposed skin, such as the backs of the hands, forearms, or face.11,12 Therefore, based on the distribution of our patient’s lesions, annular elastolytic giant cell granuloma was an unlikely diagnosis. Furthermore, it is not a known postherpetic isotopic reaction. Annular elastolytic giant cell granuloma can appear histologically similar to GA. Differentiating histologic features include a nonpalisading granuloma as well as the absence of mucin and necrobiosis.12
Annular lichen planus is a long-recognized but uncommon clinical variant of lichen planus that typically presents as pruritic, purple, annular plaques on the penis, scrotum, or intertriginous areas.13 The violaceous coloring is more characteristic of lichen planus. Histology is helpful in differentiating from GA.
Nummular eczema presents as scattered, welldefined, pruritic, erythematous, coin-shaped, coin-sized plaques in patients with diffusely dry skin.14 The scaling and serous crusting as well as more prominent pruritus help distinguish it from GA. The appearance of nummular eczema is quite characteristic; therefore, a biopsy typically is unnecessary for diagnosis. However, a potassium hydroxide wet mount examination of a skin scraping should be performed if tinea corporis also is suspected.
Superficial erythema annulare centrifugum classically presents as an annular or arciform pruritic lesion with an advancing outer erythematous edge with an inner rim of scale that most commonly occurs on the lower extremities. 15 The presence of pruritus and trailing scale helps distinguish this lesion from GA. Histologically, there are epidermal changes of hyperplasia, spongiosis, and parakeratosis, as well as lymphohistiocytic infiltrate surrounding the superficial dermal vessels.16
We report this case to highlight GA as the most common postherpetic isotopic response. It should be on the differential diagnosis when a patient presents with erythematous, smooth, annular plaques occurring in the distribution of a resolved case of HZV.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- . Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Kapoor R, Piris A, Saavedra AP, et al. Wolf isotopic response manifesting as postherpetic granuloma annulare: a case series. Arch Pathol Lab Med. 2013;137:255-258.
- Ezra N, Ahdout J, Haley JC, et al. Granuloma annulare in a zoster scar of a patient with multiple myeloma. Cutis. 2011;87:240-244.
- Noh TW, Park SH, Kang YS, et al. Morphea developing at the site of healed herpes zoster. Ann Dermatol. 2011;23:242-245.
- Ruocco V, Ruocco E, Ghersetich I, et al. Isotopic response after herpesvirus infection: an update. J Am Acad Dermatol. 2002;46:90-94.
- Sparrow G, Abell E. Granuloma annulare and necrobiosis lipoidica treated by jet injector. Br J Dermatol. 1975;93:85-89.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Thornsberry LA, English JC. Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. Am J Clin Dermatol. 2013;14:279-290.
- Rubin CB, Rosenbach M. Granuloma annulare: a retrospective series of 133 patients. Cutis. 2019;103:102-106.
- Stein JA, Fangman B, Strober B. Actinic granuloma. Dermatol Online J. 2007;13:19.
- Mistry AM, Patel R, Mistry M, et al. Annular elastolytic giant cell granuloma. Cureus. 2020;12:E11456.
- Reich HL, Nguyen JT, James WD. Annular lichen planus: a case series of 20 patients. J Am Acad Dermatol. 2004;50:595-599.
- Leung AKC, Lam JM, Leong KF, et al. Nummular eczema: an updated review. Recent Pat Inflamm Allergy Drug Discov. 2020;14:146-155.
- Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462.
- Coronel-Pérez IM, Morillo-Andújar M. Erythema annulare centrifugum responding to natural ultraviolet light [in Spanish]. Actas Dermosifiliogr. 2010;101:177-178.
The Diagnosis: Granuloma Annulare
A biopsy of a lesion on the right flank demonstrated granulomatous inflammation and interstitial mucin (Figure), characteristic of granuloma annulare (GA).1,2 Granuloma annulare is a relatively common skin disorder with an unknown etiology. It typically presents as smooth, annular, erythematous plaques.1 The most common variants of GA are localized, generalized, and subcutaneous. Our case demonstrated Wolf isotopic response, an unrelated skin disease that forms at the same location as a previously healed skin lesion.2 It is important to be aware of this phenomenon so that it is not confused with a recurrence of herpes zoster virus (HZV).
Although relatively infrequent, GA is the most common isotopic response following HZV infections.3-5 Other postherpetic isotopic eruptions include cutaneous malignancies, lichen planus, sarcoidosis, morphea, reactive perforating collagenosis, psoriasis, and infections, among others.3,5,6 The time between HZV infection and GA can be variable, ranging from a few weeks to many years apart.3
Oftentimes GA will spontaneously resolve within 2 years; however, recurrence is common.7-9 There currently are no standard treatment guidelines. The most promising treatment options include intralesional or topical glucocorticoids for localized GA as well as phototherapy or hydroxychloroquine for widespread disease.8,10

Annular elastolytic giant cell granuloma (also called actinic granuloma) is a rare idiopathic inflammatory skin disease. It is characterized by erythematous annular papules or plaques mainly found on sun-exposed skin, such as the backs of the hands, forearms, or face.11,12 Therefore, based on the distribution of our patient’s lesions, annular elastolytic giant cell granuloma was an unlikely diagnosis. Furthermore, it is not a known postherpetic isotopic reaction. Annular elastolytic giant cell granuloma can appear histologically similar to GA. Differentiating histologic features include a nonpalisading granuloma as well as the absence of mucin and necrobiosis.12
Annular lichen planus is a long-recognized but uncommon clinical variant of lichen planus that typically presents as pruritic, purple, annular plaques on the penis, scrotum, or intertriginous areas.13 The violaceous coloring is more characteristic of lichen planus. Histology is helpful in differentiating from GA.
Nummular eczema presents as scattered, welldefined, pruritic, erythematous, coin-shaped, coin-sized plaques in patients with diffusely dry skin.14 The scaling and serous crusting as well as more prominent pruritus help distinguish it from GA. The appearance of nummular eczema is quite characteristic; therefore, a biopsy typically is unnecessary for diagnosis. However, a potassium hydroxide wet mount examination of a skin scraping should be performed if tinea corporis also is suspected.
Superficial erythema annulare centrifugum classically presents as an annular or arciform pruritic lesion with an advancing outer erythematous edge with an inner rim of scale that most commonly occurs on the lower extremities. 15 The presence of pruritus and trailing scale helps distinguish this lesion from GA. Histologically, there are epidermal changes of hyperplasia, spongiosis, and parakeratosis, as well as lymphohistiocytic infiltrate surrounding the superficial dermal vessels.16
We report this case to highlight GA as the most common postherpetic isotopic response. It should be on the differential diagnosis when a patient presents with erythematous, smooth, annular plaques occurring in the distribution of a resolved case of HZV.
The Diagnosis: Granuloma Annulare
A biopsy of a lesion on the right flank demonstrated granulomatous inflammation and interstitial mucin (Figure), characteristic of granuloma annulare (GA).1,2 Granuloma annulare is a relatively common skin disorder with an unknown etiology. It typically presents as smooth, annular, erythematous plaques.1 The most common variants of GA are localized, generalized, and subcutaneous. Our case demonstrated Wolf isotopic response, an unrelated skin disease that forms at the same location as a previously healed skin lesion.2 It is important to be aware of this phenomenon so that it is not confused with a recurrence of herpes zoster virus (HZV).
Although relatively infrequent, GA is the most common isotopic response following HZV infections.3-5 Other postherpetic isotopic eruptions include cutaneous malignancies, lichen planus, sarcoidosis, morphea, reactive perforating collagenosis, psoriasis, and infections, among others.3,5,6 The time between HZV infection and GA can be variable, ranging from a few weeks to many years apart.3
Oftentimes GA will spontaneously resolve within 2 years; however, recurrence is common.7-9 There currently are no standard treatment guidelines. The most promising treatment options include intralesional or topical glucocorticoids for localized GA as well as phototherapy or hydroxychloroquine for widespread disease.8,10

Annular elastolytic giant cell granuloma (also called actinic granuloma) is a rare idiopathic inflammatory skin disease. It is characterized by erythematous annular papules or plaques mainly found on sun-exposed skin, such as the backs of the hands, forearms, or face.11,12 Therefore, based on the distribution of our patient’s lesions, annular elastolytic giant cell granuloma was an unlikely diagnosis. Furthermore, it is not a known postherpetic isotopic reaction. Annular elastolytic giant cell granuloma can appear histologically similar to GA. Differentiating histologic features include a nonpalisading granuloma as well as the absence of mucin and necrobiosis.12
Annular lichen planus is a long-recognized but uncommon clinical variant of lichen planus that typically presents as pruritic, purple, annular plaques on the penis, scrotum, or intertriginous areas.13 The violaceous coloring is more characteristic of lichen planus. Histology is helpful in differentiating from GA.
Nummular eczema presents as scattered, welldefined, pruritic, erythematous, coin-shaped, coin-sized plaques in patients with diffusely dry skin.14 The scaling and serous crusting as well as more prominent pruritus help distinguish it from GA. The appearance of nummular eczema is quite characteristic; therefore, a biopsy typically is unnecessary for diagnosis. However, a potassium hydroxide wet mount examination of a skin scraping should be performed if tinea corporis also is suspected.
Superficial erythema annulare centrifugum classically presents as an annular or arciform pruritic lesion with an advancing outer erythematous edge with an inner rim of scale that most commonly occurs on the lower extremities. 15 The presence of pruritus and trailing scale helps distinguish this lesion from GA. Histologically, there are epidermal changes of hyperplasia, spongiosis, and parakeratosis, as well as lymphohistiocytic infiltrate surrounding the superficial dermal vessels.16
We report this case to highlight GA as the most common postherpetic isotopic response. It should be on the differential diagnosis when a patient presents with erythematous, smooth, annular plaques occurring in the distribution of a resolved case of HZV.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- . Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Kapoor R, Piris A, Saavedra AP, et al. Wolf isotopic response manifesting as postherpetic granuloma annulare: a case series. Arch Pathol Lab Med. 2013;137:255-258.
- Ezra N, Ahdout J, Haley JC, et al. Granuloma annulare in a zoster scar of a patient with multiple myeloma. Cutis. 2011;87:240-244.
- Noh TW, Park SH, Kang YS, et al. Morphea developing at the site of healed herpes zoster. Ann Dermatol. 2011;23:242-245.
- Ruocco V, Ruocco E, Ghersetich I, et al. Isotopic response after herpesvirus infection: an update. J Am Acad Dermatol. 2002;46:90-94.
- Sparrow G, Abell E. Granuloma annulare and necrobiosis lipoidica treated by jet injector. Br J Dermatol. 1975;93:85-89.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Thornsberry LA, English JC. Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. Am J Clin Dermatol. 2013;14:279-290.
- Rubin CB, Rosenbach M. Granuloma annulare: a retrospective series of 133 patients. Cutis. 2019;103:102-106.
- Stein JA, Fangman B, Strober B. Actinic granuloma. Dermatol Online J. 2007;13:19.
- Mistry AM, Patel R, Mistry M, et al. Annular elastolytic giant cell granuloma. Cureus. 2020;12:E11456.
- Reich HL, Nguyen JT, James WD. Annular lichen planus: a case series of 20 patients. J Am Acad Dermatol. 2004;50:595-599.
- Leung AKC, Lam JM, Leong KF, et al. Nummular eczema: an updated review. Recent Pat Inflamm Allergy Drug Discov. 2020;14:146-155.
- Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462.
- Coronel-Pérez IM, Morillo-Andújar M. Erythema annulare centrifugum responding to natural ultraviolet light [in Spanish]. Actas Dermosifiliogr. 2010;101:177-178.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- . Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Kapoor R, Piris A, Saavedra AP, et al. Wolf isotopic response manifesting as postherpetic granuloma annulare: a case series. Arch Pathol Lab Med. 2013;137:255-258.
- Ezra N, Ahdout J, Haley JC, et al. Granuloma annulare in a zoster scar of a patient with multiple myeloma. Cutis. 2011;87:240-244.
- Noh TW, Park SH, Kang YS, et al. Morphea developing at the site of healed herpes zoster. Ann Dermatol. 2011;23:242-245.
- Ruocco V, Ruocco E, Ghersetich I, et al. Isotopic response after herpesvirus infection: an update. J Am Acad Dermatol. 2002;46:90-94.
- Sparrow G, Abell E. Granuloma annulare and necrobiosis lipoidica treated by jet injector. Br J Dermatol. 1975;93:85-89.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Thornsberry LA, English JC. Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. Am J Clin Dermatol. 2013;14:279-290.
- Rubin CB, Rosenbach M. Granuloma annulare: a retrospective series of 133 patients. Cutis. 2019;103:102-106.
- Stein JA, Fangman B, Strober B. Actinic granuloma. Dermatol Online J. 2007;13:19.
- Mistry AM, Patel R, Mistry M, et al. Annular elastolytic giant cell granuloma. Cureus. 2020;12:E11456.
- Reich HL, Nguyen JT, James WD. Annular lichen planus: a case series of 20 patients. J Am Acad Dermatol. 2004;50:595-599.
- Leung AKC, Lam JM, Leong KF, et al. Nummular eczema: an updated review. Recent Pat Inflamm Allergy Drug Discov. 2020;14:146-155.
- Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462.
- Coronel-Pérez IM, Morillo-Andújar M. Erythema annulare centrifugum responding to natural ultraviolet light [in Spanish]. Actas Dermosifiliogr. 2010;101:177-178.
An 82-year-old man presented with painful, pink, smooth, annular convalescing plaques on the right back, flank, and abdomen in a zosteriform distribution involving the T10/11 dermatome. He had a history of hypertension and type 2 diabetes mellitus, and 12 months prior to presentation he had an outbreak of herpes zoster virus in the same distribution that was treated with valacyclovir 1000 mg 3 times daily for 7 days. Over the following month he noticed a resolution of blisters and crusting as they morphed into the current lesions.

New saliva-based COVID-19 test provides rapid results
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
Bone density loss in lean male runners parallels similar issue in women
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
FROM ENDO 2022
Biden moves to limit nicotine levels in cigarettes
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
Vaping safety views shifted following lung injury reports
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
COVID-19 Pandemic stress affected ovulation, not menstruation
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ENDO 2022







