User login
ABSTRACT
Purpose The purpose of this study was to determine the frequency of patients seen at a single institution who were diagnosed with a cervical vessel dissection related to chiropractic neck manipulation.
Methods We identified cases through a retrospective chart review of patients seen between April 2008 and March 2012 who had a diagnosis of cervical artery dissection following a recent chiropractic manipulation. Relevant imaging studies were reviewed by a board-certified neuroradiologist to confirm the findings of a cervical artery dissection and stroke. We conducted telephone interviews to ascertain the presence of residual symptoms in the affected patients.
Results Of the 141 patients with cervical artery dissection, 12 had documented chiropractic neck manipulation prior to the onset of the symptoms that led to medical presentation. The 12 patients had a total of 16 cervical artery dissections. All 12 patients developed symptoms of acute stroke. All strokes were confirmed with magnetic resonance imaging or computerized tomography. We obtained follow-up information on 9 patients, 8 of whom had residual symptoms and one of whom died as a result of his injury.
Conclusions In this case series, 12 patients with newly diagnosed cervical artery dissection(s) had recent chiropractic neck manipulation. Patients who are considering chiropractic cervical manipulation should be informed of the potential risk and be advised to seek immediate medical attention should they develop symptoms.
A prospective randomized controlled study published in 2012 showed chiropractic manipulation is beneficial in the treatment of neck pain compared with medical treatment, but it showed no significant difference between chiropractic manipulation and physical therapy exercises.1 Although chiropractic manipulation of the cervical spine may be effective, it may also cause harm.
Cerebellar and spinal cord injuries related to cervical chiropractic manipulation were first reported in 1947.2 By 1974, there were 12 reported cases.3 Noninvasive imaging has since greatly improved the diagnosis of cervical artery dissection and of stroke,4 and cervical artery dissection is now recognized as pathogenic of strokes occurring in association with chiropractic manipulation.5
A prospective series published in 2011 reported that, over 4 years, 13 patients were treated at a single institution for cervical arterial dissection following chiropractic treatment.6 That so many patients might be seen for this condition in that time frame at a single institution suggests the risk for such injury may be greater than thought. To explore that possibility, we performed a 4-year retrospective review to determine the experience at OSF Saint Francis Medical Center, which is affiliated with the University of Illinois College of Medicine, Peoria.
METHODS
Data sources. After receiving approval by the local institutional review board, we obtained data from the electronic medical records of OSF Saint Francis Medical Center, Peoria, Ill., using Epic (Epic Systems Corporation, Verona, Wis.) and IDX (General Electric Corporation, Fairfield, Conn.) systems. The records were queried using ICD-9 codes 443.21 and 443.24 to identify patients from April 2008 through March 2012 who had primary or secondary diagnoses of vertebral artery dissection (VAD) or carotid artery dissection (CAD). We reviewed all records of VAD and CAD to identify those that may have been associated with chiropractic manipulation.
Data collection. We abstracted data from 12 patients’ charts. Two patients were unavailable for direct contact: one was involved in ongoing litigation, and one had died (although we were able to speak with his wife). We attempted telephone contact with the 10 remaining patients and reached 8.
Data included the symptoms leading to chiropractic manipulation, symptoms following manipulation, timing of onset of symptoms relative to chiropractic manipulation, identifying information for the treating chiropractor, and residual patient symptoms. We also recorded patients’ ages, sex, locations of dissection, and locations of stroke. All dissections and strokes had been diagnosed during the patient’s initial hospitalization.
A board-certified radiologist (JRD) with a Certificate of Added Qualification in Neuroradiology (American Board of Medical Specialties) reviewed all pertinent imaging to confirm all dissections and strokes.
RESULTS
The medical record query yielded 141 patients with VAD or CAD, 15 of whom had undergone chiropractic manipulation prior to their presentation. The temporal association between chiropractic manipulation and arterial dissection was equivocal for 3 patients. In 12 patients, there was a verifiable temporal association between chiropractic manipulation and the arterial dissection. Three of the 12 patients were men and 9 were women. Ages ranged from 22 to 46 years, with a mean of 35.3 years.
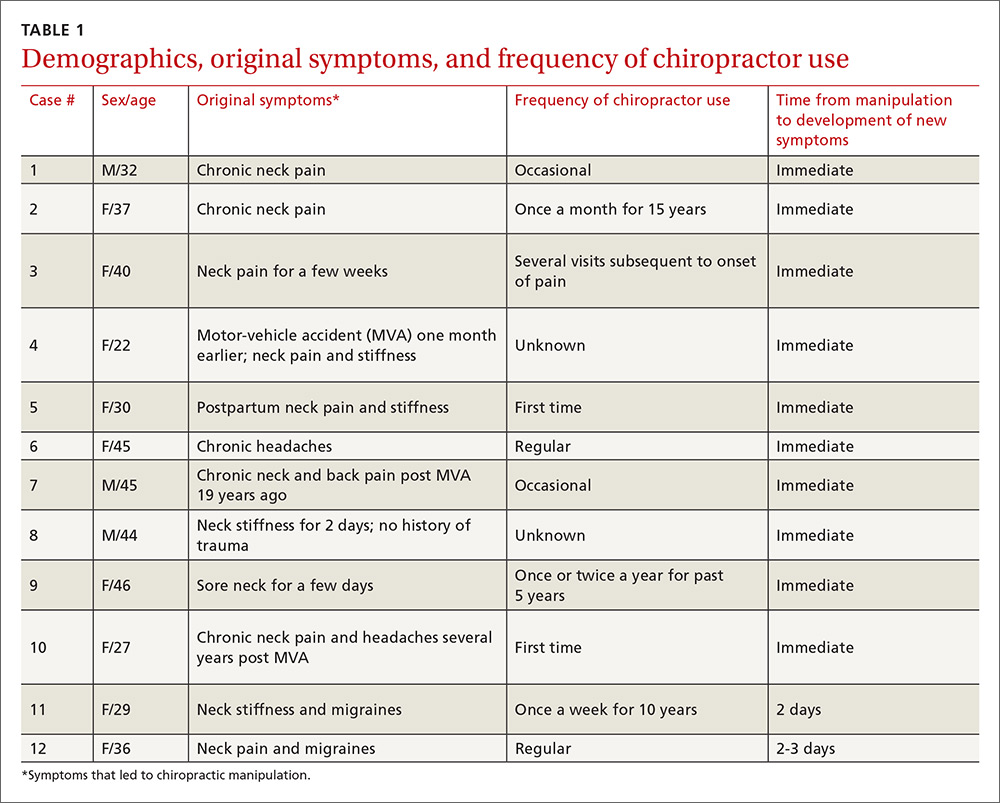
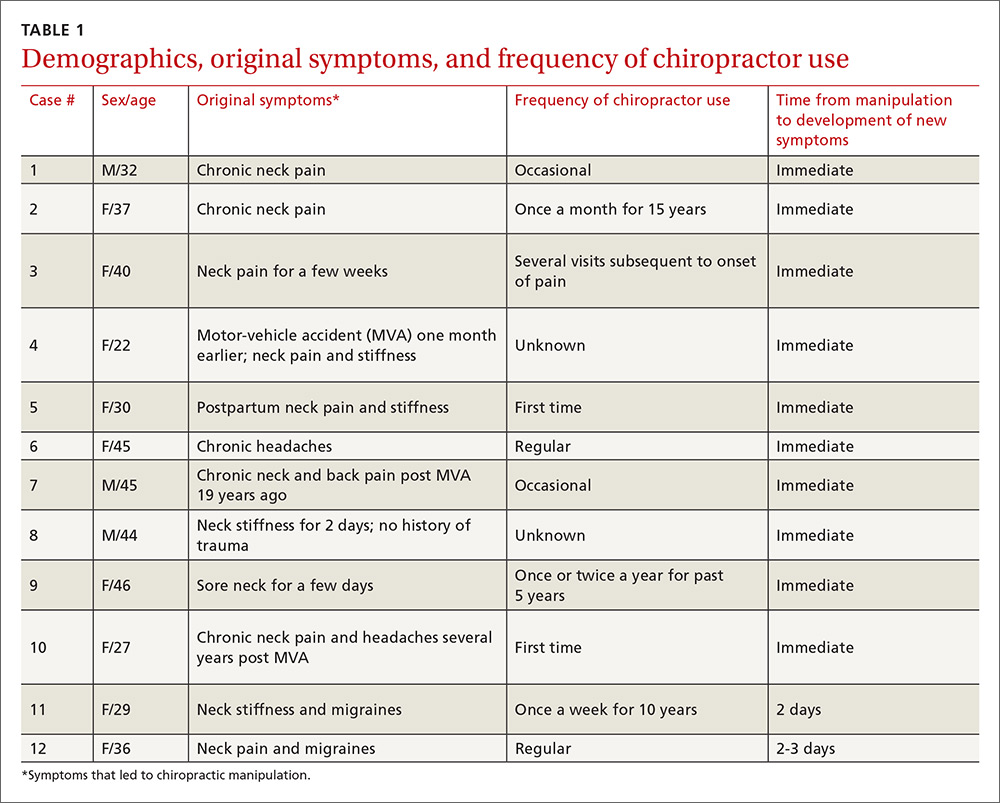
Acute or chronic neck pain was the most common reason for seeking chiropractic care (TABLE 1). Immediately upon performance of cervical manipulation, 10 of the 12 developed acute symptoms different than those that caused them to seek chiropractic care. Two patients developed symptoms 2 to 3 days post-manipulation. Neither of the 2 had a history of neck trauma within the preceding year. Ten of the 12 patients sought immediate medical attention. Two of the 12 patients sought care when their symptoms became more severe, ranging from 2 days to several weeks later (TABLE 2). The treating chiropractor was identified in 7 cases and was different in each of the 7 cases.
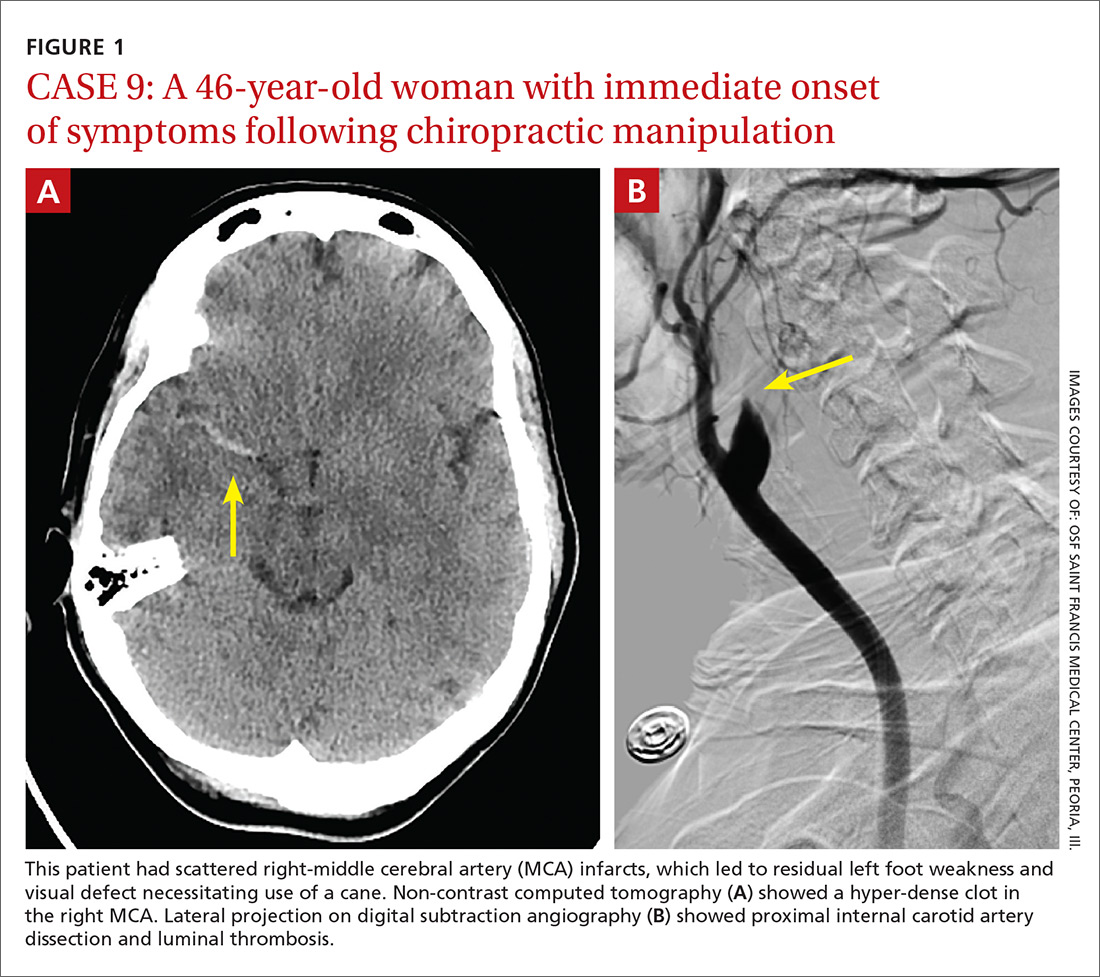
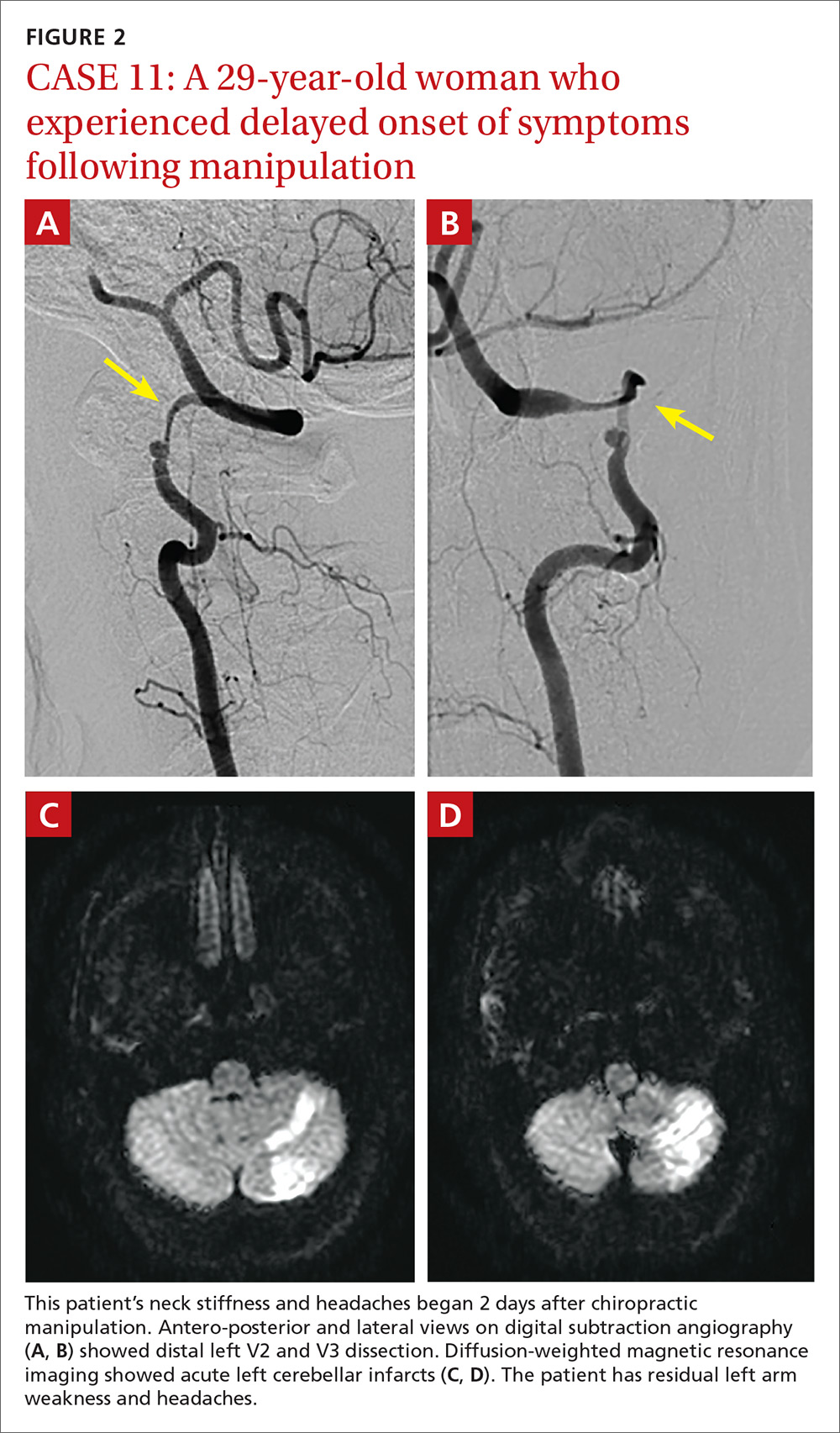
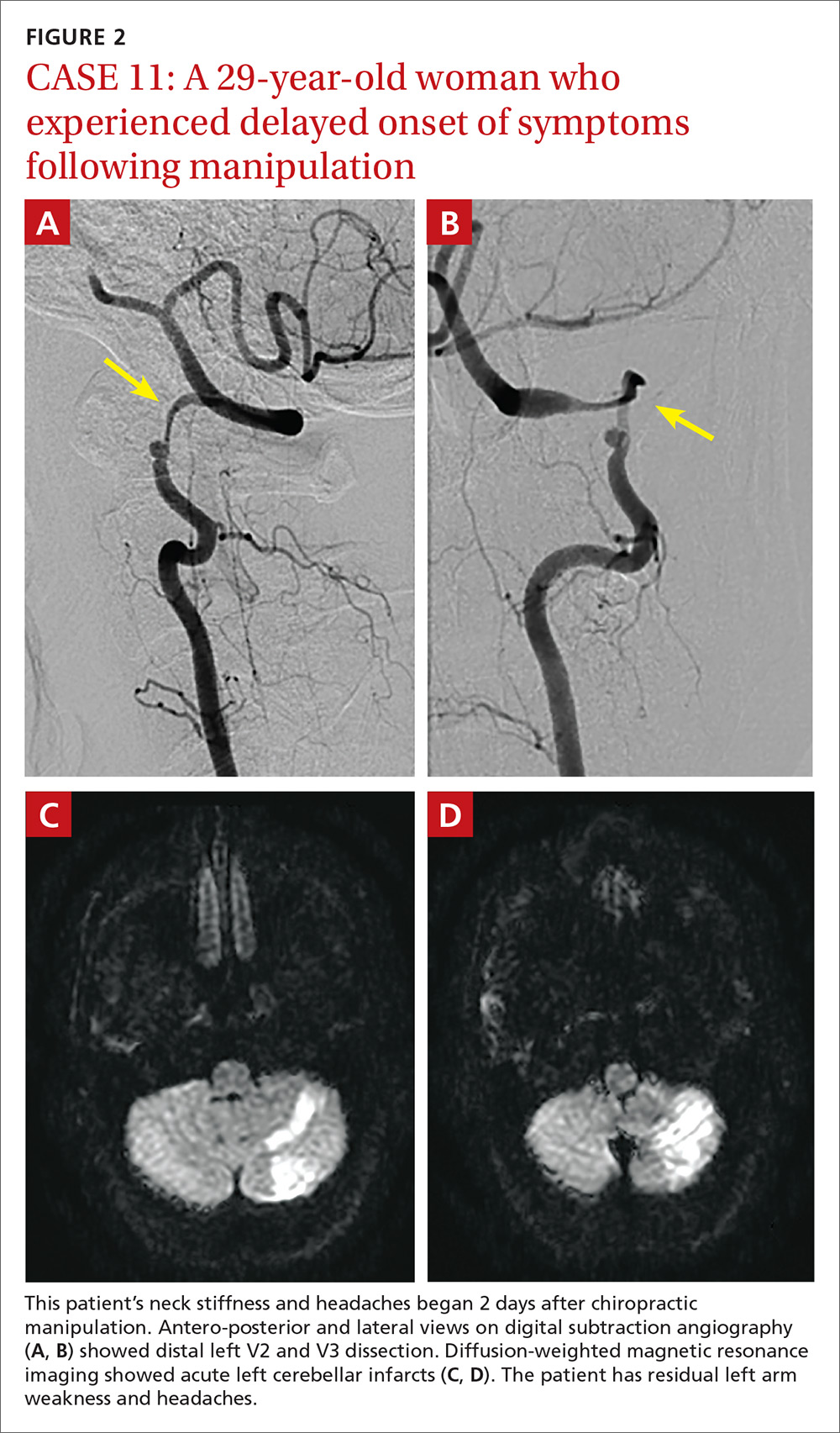
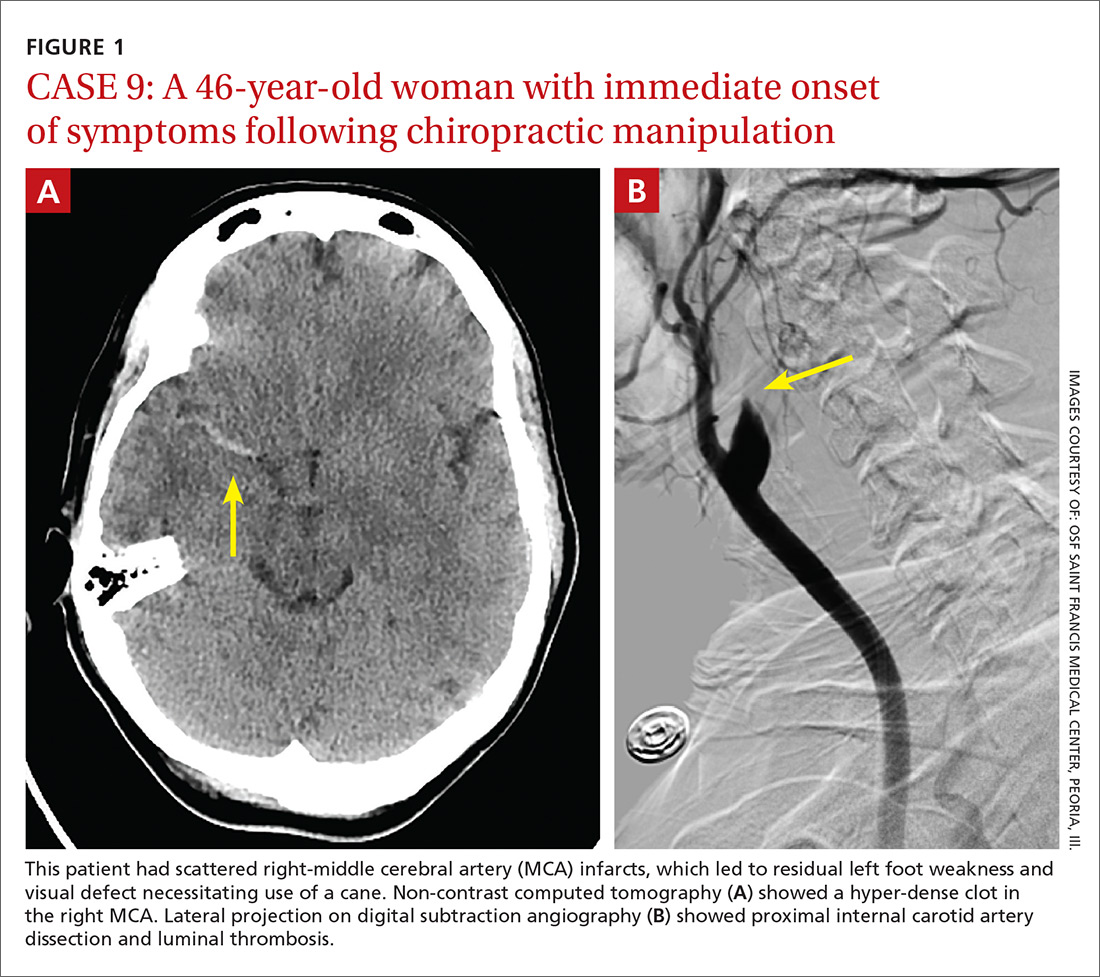
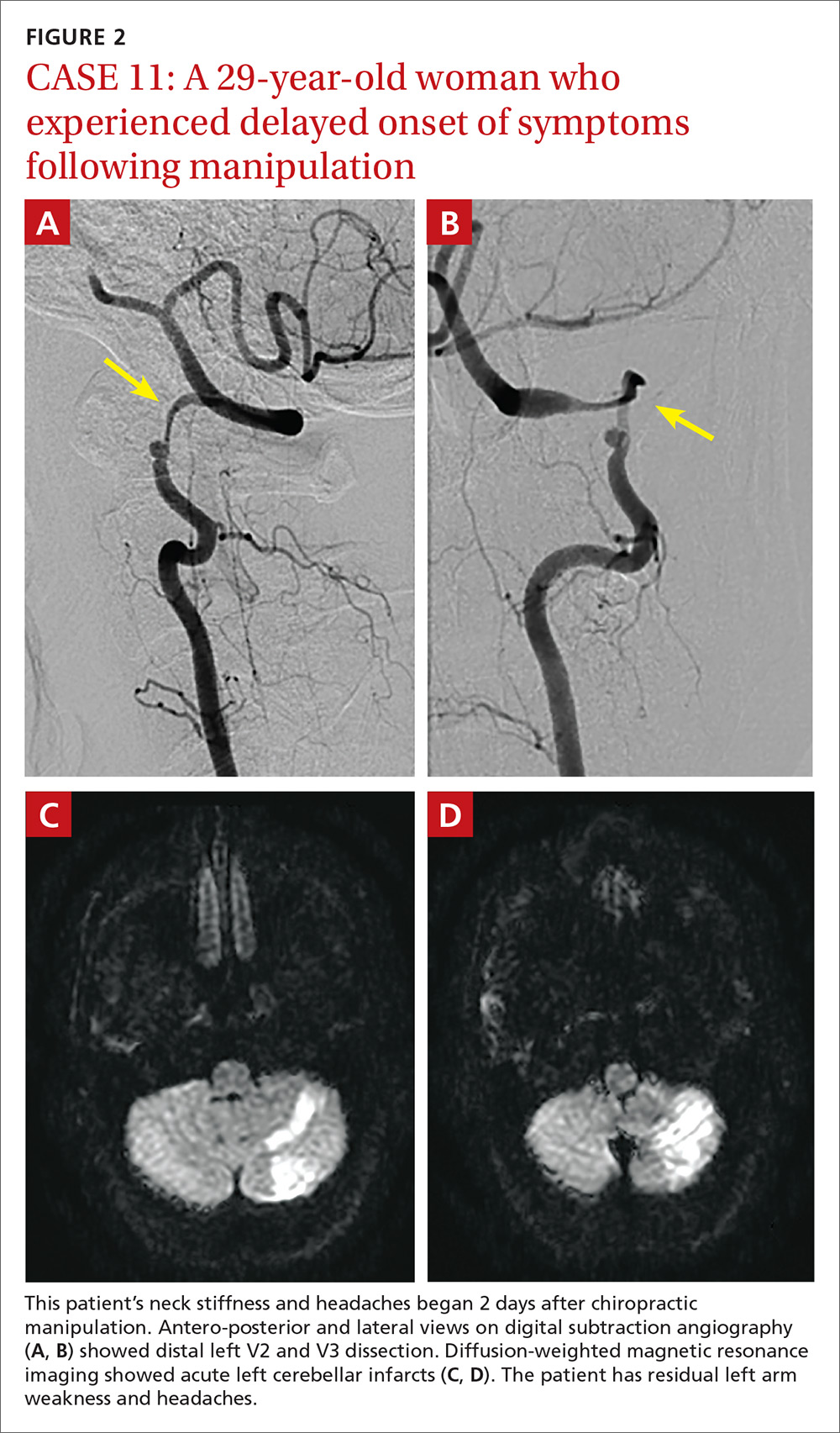
A total of 16 cervical artery dissections, 14 VAD and 2 CAD, were confirmed by computed tomography angiography (CTA), magnetic resonance angiography (MRA), or catheter angiography (FIGURE 1). All 12 patients had acute strokes confirmed by MRA or CTA, including 9 in the cerebellum (FIGURE 2), 4 in the cerebrum, 2 in the medulla, and one in the pons.
Long-term outcomes were determined for 9 patients (TABLE 2). One patient’s symptoms resolved. Three patients had dizziness, clumsiness, or balance problems; 3 had persistent headaches; 2 had bilateral visual field abnormalities; and one patient walked with a cane, was no longer driving a car, and was on disability. One patient died as a result of his injury. One of the 12 cases was previously described in a case report.7

DISCUSSION
Dissection of the cervical arteries is more common than dissection in other arteries of comparable size. This increased risk in the cervical arteries is believed to be due to their relative mobility and proximity to bony structures.4
Sudden neck movement, a feature of chiropractic treatment, is one of several known risk factors for ‘spontaneous’ cervical artery dissection.8,9 Symptom onset and stroke may be delayed after a spontaneous cervical artery dissection.10 Spontaneous dissection more commonly involves the carotid arteries;4 however, the vertebral arteries appear more prone to dissection as a consequence of chiropractic manipulation,11 likely due to their relation to the cervical spine.
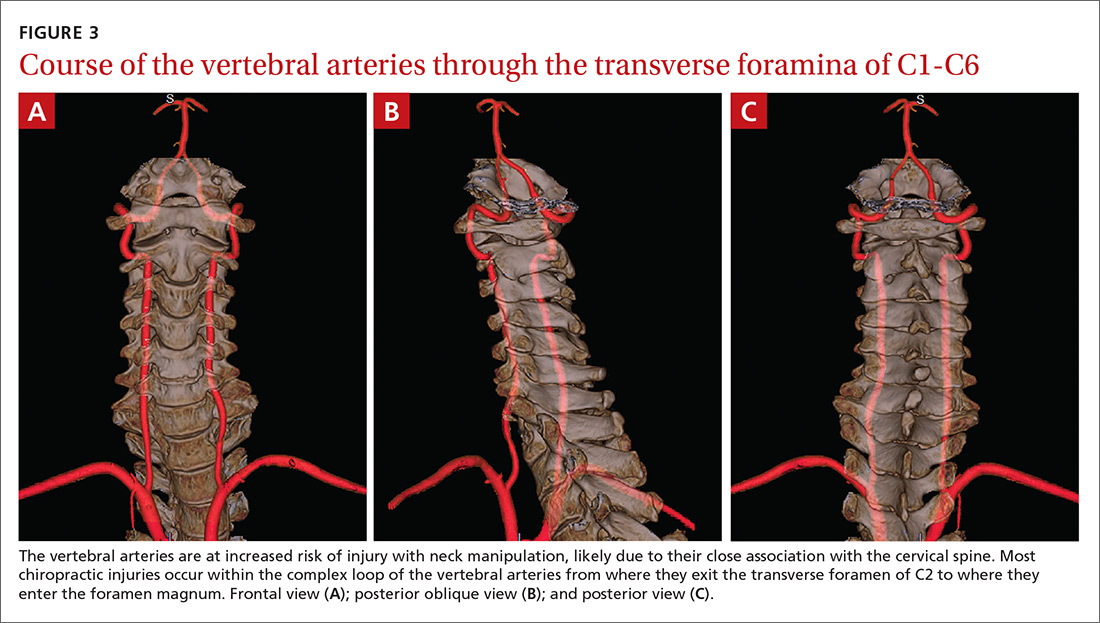
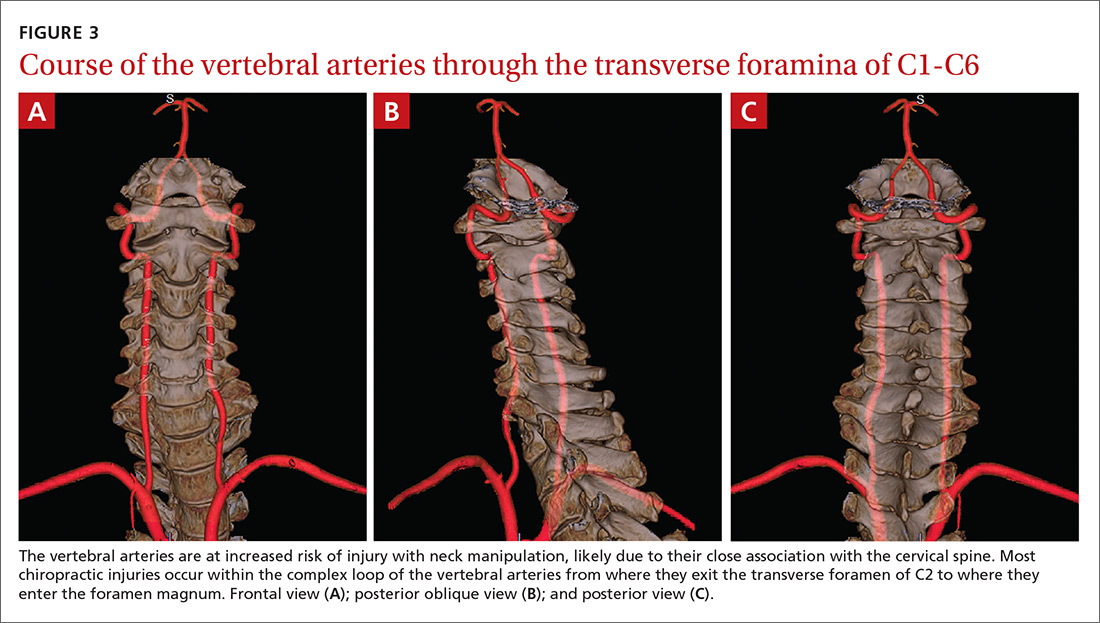
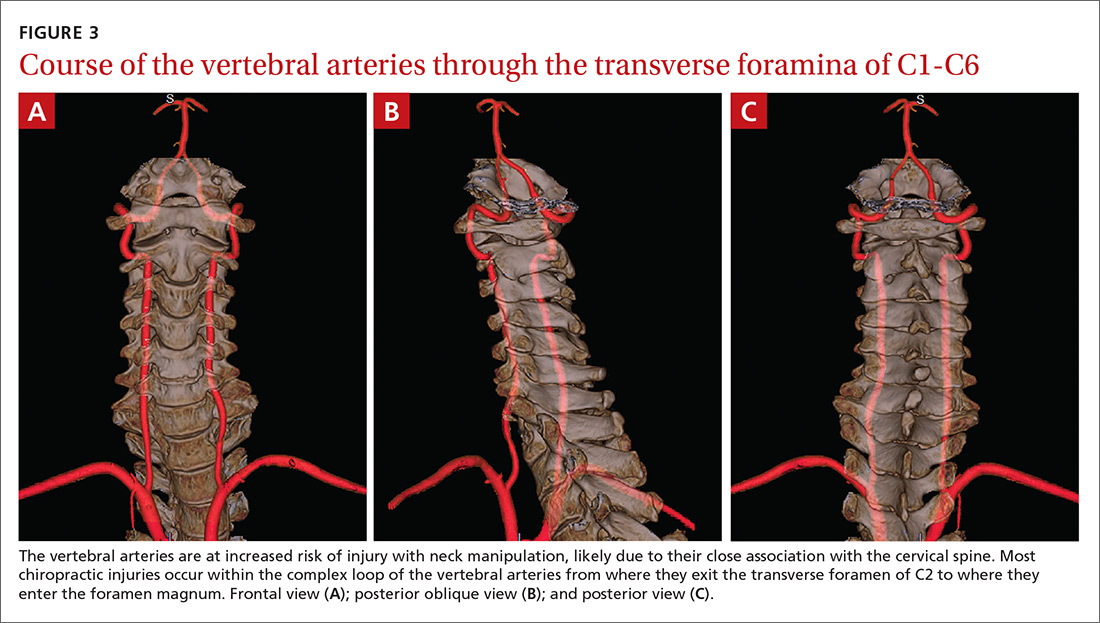
The vertebral artery runs through foramina in the transverse processes of vertebral bodies C1 through C6 (FIGURE 3). On exiting the C2 transverse process, the vertebral artery has a tortuous course, making several turns over and through adjacent bony structures.12 The artery is most prone to injury between the entrance to the transverse foramen of C6 and the foramen magnum (V2 and V3 segments).13 (The area of highest vulnerability is the tortuous segment from the transverse foramen of C2 to the foramen magnum.)
Sudden movements of the cervical spine may cause arterial dissection, whether the maneuvers are performed by a physician, a chiropractor, or a physical therapist.14 Injuries reported in the literature, however, most commonly follow chiropractic manipulation. In our series of 141 dissections, we found no cases associated with manipulation by other health professionals.
A 2003 study revealed cervical spine manipulation to be an independent and strong risk factor for vertebral artery dissection. The authors believed the relationship was likely causal.5 Data from the Canadian Stroke Consortium showed a 28% incidence of chiropractic manipulation in cases of cervical artery dissection.10
A 2008 study showed an association between vertebrobasilar stroke and chiropractic visits within one month of the vascular event.15 However, the study also showed an association of similar magnitude between vertebrobasilar stroke and visits to primary care physicians within the prior month. This suggests that cervical manipulation by chiropractors poses no more risk for cervical artery dissection than visits to primary care physicians. However, it is hard to reconcile such a conclusion with other studies, including our own, in which 10 patients developed new symptoms immediately with chiropractic manipulation of their cervical spines.
Perhaps the one-month observation period of Cassidy et al was excessive. Many post-manipulation events occur within hours or at most a few days, as would be expected given the hypothesized pathogenic mechanism. Perhaps if they had shortened their interval of study to the preceding 3 days, their findings may have been different.
A recent systematic review and meta-analysis demonstrated a slight association between chiropractic neck manipulation and cervical artery dissection. It stated that the quality of the published literature was very low, and it concluded there was no convincing evidence of causation.16 The fact that 10 of the 12 patients in our case series demonstrated acute symptoms immediately upon receiving spinal manipulation suggests a possible causal link; however, we agree with the authors of the meta-analysis that the quality of the literature is low.
A recent statement from the American Heart Association/American Stroke Association (and endorsed by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons) has recommended that chiropractors inform patients of the statistical association between cervical artery dissection and cervical manipulation.17 In addition, it is important for chiropractors to be aware of the signs and symptoms of cervical artery dissection and stroke and to assess for these symptoms before performing neck manipulation, as illustrated in a recent case report.18 Due to the risk of death, patients who experience symptoms consistent with cervical artery dissection after chiropractic manipulation of the cervical spine should be advised to seek medical care immediately.
Our case series has several limitations. The study was retrospective. Existing documentation of associated chiropractic care was often sparse, necessitating phone calls to supplement the information. We believe it is possible that cases may have been missed because of inaccurate medical record documentation, deficits in the interview process concerning chiropractic care at the time of hospitalization, or because information concerning chiropractic care was not recorded in the chart.
A significant portion of our information came through phone contact with several of the patients. In some cases, we relied heavily on their recollection of events that had occurred anytime from a few days to a few years earlier. The accuracy and completeness of the information supplied by patients was not verified, allowing for potential recall bias.
We do not know whether our experience is consistent with that of other areas of the United States. However, the fact that a similar-size hospital in Phoenix reported similar findings suggests the experience may be more widespread.6
IMPLICATIONS OF OUR FINDINGS
Over a 4-year period at our institution, 12 patients experienced cervical vessel dissection related to chiropractic neck manipulation. A similar institution in another part of the country had previously described 13 such cases. The patients at both institutions were relatively young and incurred substantial residual morbidity. A single patient at each institution died. If these findings are representative of other institutions across the United States, the incidence of stroke secondary to chiropractic manipulation may be higher than supposed.
To assess this problem further, a randomized prospective cohort study could establish the relative risk of chiropractic manipulation of the cervical spine resulting in a cervical artery dissection. But such a study may be methodologically prohibitive. More feasible would be a case-control study similar to one carried out by Smith et al5 in which patients who had experienced cervical artery dissection were matched with subjects who had not incurred such injuries. Comparing the groups’ odds of having received chiropractic manipulation demonstrated that spinal manipulative therapy is an independent risk factor for vertebral artery dissection and is highly suggestive of a causal association. Replicating this study in a different population would be valuable.
Based on our findings, all patients who visit chiropractors for cervical spine manipulation should be informed of the potential risks and of the need to seek immediate medical assistance should symptoms suggestive of dissection or stroke occur during or after manipulation. Until the actual level of risk from chiropractic manipulation is known, patients with neck pain may be better served by equally effective passive physical therapy exercises.1
CORRESPONDENCE
Raymond E. Bertino, MD, 427 West Crestwood Drive, Peoria, IL 61614; [email protected].
ACKNOWLEDGEMENTS
We thank Deepak Nair, MD, for his assistance in reviewing the stroke neurology aspects of this study; Katie Groesch, MD, for her assistance in drafting portions of the Methods and Results sections; Rita Hermacinski for the generation of 3D images; and Stephanie Arthalony for her assistance in gathering information through patient telephone interviews.
1.
2. Pratt-Thomas HR, Knute EB. Cerebellar and spinal injuries after chiropractic manipulation. JAMA. 1947;133:600-603.
3. Miller RG, Burton R. Stroke following chiropractic manipulation of the spine. JAMA. 1974;229:189-190.
4. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Eng J Med. 2001;344:898-906.
5. Smith WS, Johnston SC, Skalabrin EJ, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology. 2003;60:1424-1428.
6. Albuquerque FC, Hu YC, Dashti SR, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011;115:1197-1205.
7. Bertino RE, Talkad AV, DeSanto JR, et al. Chiropractic manipulation of the neck and cervical artery dissection. Ann Intern Med. 2012;157:150-152.
8. Dittrich R, Rohsbach D, Heidbreder A, et al. Mild mechanical traumas are possible risk factors for cervical artery dissection. Cerebrovasc Dis. 2006;23:275-281.
9. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668-678.
10. Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian Stroke Consortium. CMAJ. 2000;163:38-40.
11. Stevinson C, Ernst E. Risks associated with spinal manipulation. Am J Med. 2002;112:566–571.
12. Doshi AH, Aggarwal A, Patel AB. Normal vascular anatomy. In Naidich TP, Castillo M, Cha S, Smirniotopoulos JG, eds. Imaging of the Brain. Philadelphia, Pa: Saunders;
13. Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke. 2006;37:2499-2503.
14. Reuter U, Hämling M, Kavuk I, et al. Vertebral artery dissections after chiropractic neck manipulation in Germany over three years. J Neurol. 2006;253:724-730.
15. Cassidy JD, Boyle E, Cote P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008;17(Suppl 1):S176-S183.
16. Church EW, Sieg EP, Zalatima O, et al. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: No evidence for causation. Cureus. 2016;8:e498.
17. Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3155-3174.
18. Tarola G, Phillips RB. Chiropractic response to a spontaneous vertebral artery dissection. J Chiropr Med. 2015;14:183-190.
ABSTRACT
Purpose The purpose of this study was to determine the frequency of patients seen at a single institution who were diagnosed with a cervical vessel dissection related to chiropractic neck manipulation.
Methods We identified cases through a retrospective chart review of patients seen between April 2008 and March 2012 who had a diagnosis of cervical artery dissection following a recent chiropractic manipulation. Relevant imaging studies were reviewed by a board-certified neuroradiologist to confirm the findings of a cervical artery dissection and stroke. We conducted telephone interviews to ascertain the presence of residual symptoms in the affected patients.
Results Of the 141 patients with cervical artery dissection, 12 had documented chiropractic neck manipulation prior to the onset of the symptoms that led to medical presentation. The 12 patients had a total of 16 cervical artery dissections. All 12 patients developed symptoms of acute stroke. All strokes were confirmed with magnetic resonance imaging or computerized tomography. We obtained follow-up information on 9 patients, 8 of whom had residual symptoms and one of whom died as a result of his injury.
Conclusions In this case series, 12 patients with newly diagnosed cervical artery dissection(s) had recent chiropractic neck manipulation. Patients who are considering chiropractic cervical manipulation should be informed of the potential risk and be advised to seek immediate medical attention should they develop symptoms.
A prospective randomized controlled study published in 2012 showed chiropractic manipulation is beneficial in the treatment of neck pain compared with medical treatment, but it showed no significant difference between chiropractic manipulation and physical therapy exercises.1 Although chiropractic manipulation of the cervical spine may be effective, it may also cause harm.
Cerebellar and spinal cord injuries related to cervical chiropractic manipulation were first reported in 1947.2 By 1974, there were 12 reported cases.3 Noninvasive imaging has since greatly improved the diagnosis of cervical artery dissection and of stroke,4 and cervical artery dissection is now recognized as pathogenic of strokes occurring in association with chiropractic manipulation.5
A prospective series published in 2011 reported that, over 4 years, 13 patients were treated at a single institution for cervical arterial dissection following chiropractic treatment.6 That so many patients might be seen for this condition in that time frame at a single institution suggests the risk for such injury may be greater than thought. To explore that possibility, we performed a 4-year retrospective review to determine the experience at OSF Saint Francis Medical Center, which is affiliated with the University of Illinois College of Medicine, Peoria.
METHODS
Data sources. After receiving approval by the local institutional review board, we obtained data from the electronic medical records of OSF Saint Francis Medical Center, Peoria, Ill., using Epic (Epic Systems Corporation, Verona, Wis.) and IDX (General Electric Corporation, Fairfield, Conn.) systems. The records were queried using ICD-9 codes 443.21 and 443.24 to identify patients from April 2008 through March 2012 who had primary or secondary diagnoses of vertebral artery dissection (VAD) or carotid artery dissection (CAD). We reviewed all records of VAD and CAD to identify those that may have been associated with chiropractic manipulation.
Data collection. We abstracted data from 12 patients’ charts. Two patients were unavailable for direct contact: one was involved in ongoing litigation, and one had died (although we were able to speak with his wife). We attempted telephone contact with the 10 remaining patients and reached 8.
Data included the symptoms leading to chiropractic manipulation, symptoms following manipulation, timing of onset of symptoms relative to chiropractic manipulation, identifying information for the treating chiropractor, and residual patient symptoms. We also recorded patients’ ages, sex, locations of dissection, and locations of stroke. All dissections and strokes had been diagnosed during the patient’s initial hospitalization.
A board-certified radiologist (JRD) with a Certificate of Added Qualification in Neuroradiology (American Board of Medical Specialties) reviewed all pertinent imaging to confirm all dissections and strokes.
RESULTS
The medical record query yielded 141 patients with VAD or CAD, 15 of whom had undergone chiropractic manipulation prior to their presentation. The temporal association between chiropractic manipulation and arterial dissection was equivocal for 3 patients. In 12 patients, there was a verifiable temporal association between chiropractic manipulation and the arterial dissection. Three of the 12 patients were men and 9 were women. Ages ranged from 22 to 46 years, with a mean of 35.3 years.
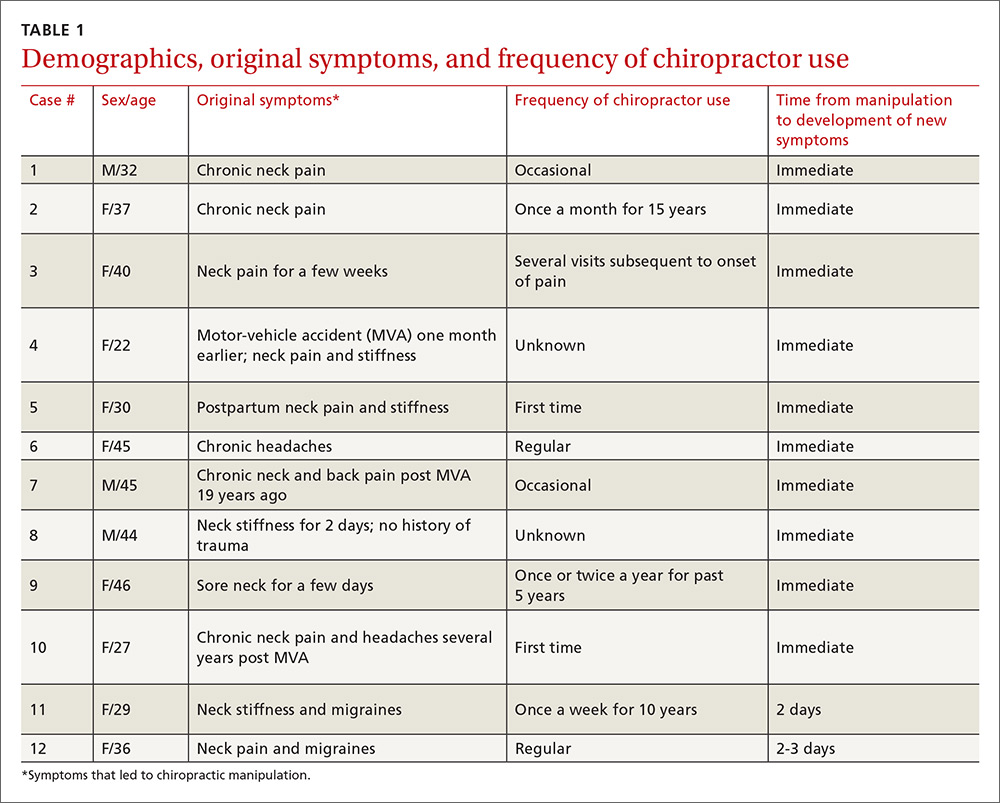
Acute or chronic neck pain was the most common reason for seeking chiropractic care (TABLE 1). Immediately upon performance of cervical manipulation, 10 of the 12 developed acute symptoms different than those that caused them to seek chiropractic care. Two patients developed symptoms 2 to 3 days post-manipulation. Neither of the 2 had a history of neck trauma within the preceding year. Ten of the 12 patients sought immediate medical attention. Two of the 12 patients sought care when their symptoms became more severe, ranging from 2 days to several weeks later (TABLE 2). The treating chiropractor was identified in 7 cases and was different in each of the 7 cases.
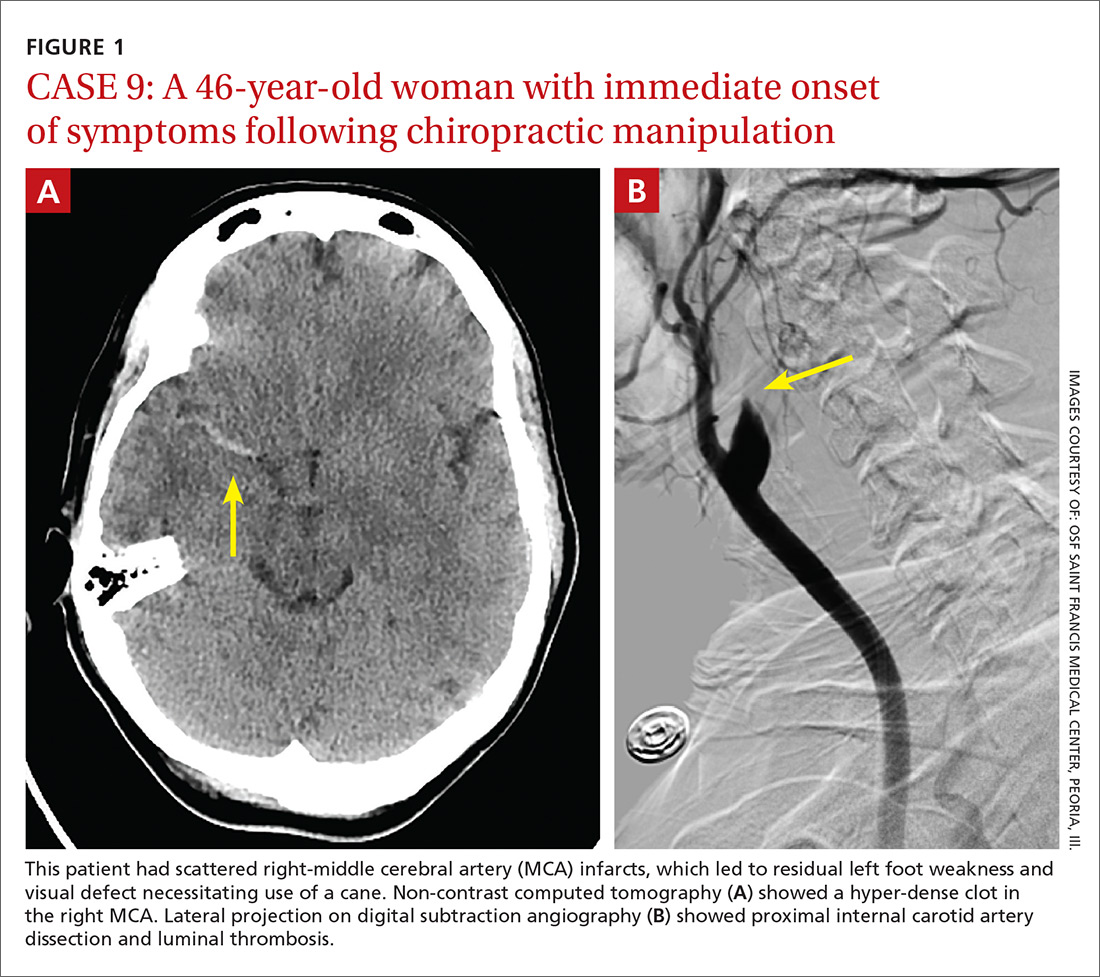
A total of 16 cervical artery dissections, 14 VAD and 2 CAD, were confirmed by computed tomography angiography (CTA), magnetic resonance angiography (MRA), or catheter angiography (FIGURE 1). All 12 patients had acute strokes confirmed by MRA or CTA, including 9 in the cerebellum (FIGURE 2), 4 in the cerebrum, 2 in the medulla, and one in the pons.
Long-term outcomes were determined for 9 patients (TABLE 2). One patient’s symptoms resolved. Three patients had dizziness, clumsiness, or balance problems; 3 had persistent headaches; 2 had bilateral visual field abnormalities; and one patient walked with a cane, was no longer driving a car, and was on disability. One patient died as a result of his injury. One of the 12 cases was previously described in a case report.7

DISCUSSION
Dissection of the cervical arteries is more common than dissection in other arteries of comparable size. This increased risk in the cervical arteries is believed to be due to their relative mobility and proximity to bony structures.4
Sudden neck movement, a feature of chiropractic treatment, is one of several known risk factors for ‘spontaneous’ cervical artery dissection.8,9 Symptom onset and stroke may be delayed after a spontaneous cervical artery dissection.10 Spontaneous dissection more commonly involves the carotid arteries;4 however, the vertebral arteries appear more prone to dissection as a consequence of chiropractic manipulation,11 likely due to their relation to the cervical spine.
The vertebral artery runs through foramina in the transverse processes of vertebral bodies C1 through C6 (FIGURE 3). On exiting the C2 transverse process, the vertebral artery has a tortuous course, making several turns over and through adjacent bony structures.12 The artery is most prone to injury between the entrance to the transverse foramen of C6 and the foramen magnum (V2 and V3 segments).13 (The area of highest vulnerability is the tortuous segment from the transverse foramen of C2 to the foramen magnum.)
Sudden movements of the cervical spine may cause arterial dissection, whether the maneuvers are performed by a physician, a chiropractor, or a physical therapist.14 Injuries reported in the literature, however, most commonly follow chiropractic manipulation. In our series of 141 dissections, we found no cases associated with manipulation by other health professionals.
A 2003 study revealed cervical spine manipulation to be an independent and strong risk factor for vertebral artery dissection. The authors believed the relationship was likely causal.5 Data from the Canadian Stroke Consortium showed a 28% incidence of chiropractic manipulation in cases of cervical artery dissection.10
A 2008 study showed an association between vertebrobasilar stroke and chiropractic visits within one month of the vascular event.15 However, the study also showed an association of similar magnitude between vertebrobasilar stroke and visits to primary care physicians within the prior month. This suggests that cervical manipulation by chiropractors poses no more risk for cervical artery dissection than visits to primary care physicians. However, it is hard to reconcile such a conclusion with other studies, including our own, in which 10 patients developed new symptoms immediately with chiropractic manipulation of their cervical spines.
Perhaps the one-month observation period of Cassidy et al was excessive. Many post-manipulation events occur within hours or at most a few days, as would be expected given the hypothesized pathogenic mechanism. Perhaps if they had shortened their interval of study to the preceding 3 days, their findings may have been different.
A recent systematic review and meta-analysis demonstrated a slight association between chiropractic neck manipulation and cervical artery dissection. It stated that the quality of the published literature was very low, and it concluded there was no convincing evidence of causation.16 The fact that 10 of the 12 patients in our case series demonstrated acute symptoms immediately upon receiving spinal manipulation suggests a possible causal link; however, we agree with the authors of the meta-analysis that the quality of the literature is low.
A recent statement from the American Heart Association/American Stroke Association (and endorsed by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons) has recommended that chiropractors inform patients of the statistical association between cervical artery dissection and cervical manipulation.17 In addition, it is important for chiropractors to be aware of the signs and symptoms of cervical artery dissection and stroke and to assess for these symptoms before performing neck manipulation, as illustrated in a recent case report.18 Due to the risk of death, patients who experience symptoms consistent with cervical artery dissection after chiropractic manipulation of the cervical spine should be advised to seek medical care immediately.
Our case series has several limitations. The study was retrospective. Existing documentation of associated chiropractic care was often sparse, necessitating phone calls to supplement the information. We believe it is possible that cases may have been missed because of inaccurate medical record documentation, deficits in the interview process concerning chiropractic care at the time of hospitalization, or because information concerning chiropractic care was not recorded in the chart.
A significant portion of our information came through phone contact with several of the patients. In some cases, we relied heavily on their recollection of events that had occurred anytime from a few days to a few years earlier. The accuracy and completeness of the information supplied by patients was not verified, allowing for potential recall bias.
We do not know whether our experience is consistent with that of other areas of the United States. However, the fact that a similar-size hospital in Phoenix reported similar findings suggests the experience may be more widespread.6
IMPLICATIONS OF OUR FINDINGS
Over a 4-year period at our institution, 12 patients experienced cervical vessel dissection related to chiropractic neck manipulation. A similar institution in another part of the country had previously described 13 such cases. The patients at both institutions were relatively young and incurred substantial residual morbidity. A single patient at each institution died. If these findings are representative of other institutions across the United States, the incidence of stroke secondary to chiropractic manipulation may be higher than supposed.
To assess this problem further, a randomized prospective cohort study could establish the relative risk of chiropractic manipulation of the cervical spine resulting in a cervical artery dissection. But such a study may be methodologically prohibitive. More feasible would be a case-control study similar to one carried out by Smith et al5 in which patients who had experienced cervical artery dissection were matched with subjects who had not incurred such injuries. Comparing the groups’ odds of having received chiropractic manipulation demonstrated that spinal manipulative therapy is an independent risk factor for vertebral artery dissection and is highly suggestive of a causal association. Replicating this study in a different population would be valuable.
Based on our findings, all patients who visit chiropractors for cervical spine manipulation should be informed of the potential risks and of the need to seek immediate medical assistance should symptoms suggestive of dissection or stroke occur during or after manipulation. Until the actual level of risk from chiropractic manipulation is known, patients with neck pain may be better served by equally effective passive physical therapy exercises.1
CORRESPONDENCE
Raymond E. Bertino, MD, 427 West Crestwood Drive, Peoria, IL 61614; [email protected].
ACKNOWLEDGEMENTS
We thank Deepak Nair, MD, for his assistance in reviewing the stroke neurology aspects of this study; Katie Groesch, MD, for her assistance in drafting portions of the Methods and Results sections; Rita Hermacinski for the generation of 3D images; and Stephanie Arthalony for her assistance in gathering information through patient telephone interviews.
ABSTRACT
Purpose The purpose of this study was to determine the frequency of patients seen at a single institution who were diagnosed with a cervical vessel dissection related to chiropractic neck manipulation.
Methods We identified cases through a retrospective chart review of patients seen between April 2008 and March 2012 who had a diagnosis of cervical artery dissection following a recent chiropractic manipulation. Relevant imaging studies were reviewed by a board-certified neuroradiologist to confirm the findings of a cervical artery dissection and stroke. We conducted telephone interviews to ascertain the presence of residual symptoms in the affected patients.
Results Of the 141 patients with cervical artery dissection, 12 had documented chiropractic neck manipulation prior to the onset of the symptoms that led to medical presentation. The 12 patients had a total of 16 cervical artery dissections. All 12 patients developed symptoms of acute stroke. All strokes were confirmed with magnetic resonance imaging or computerized tomography. We obtained follow-up information on 9 patients, 8 of whom had residual symptoms and one of whom died as a result of his injury.
Conclusions In this case series, 12 patients with newly diagnosed cervical artery dissection(s) had recent chiropractic neck manipulation. Patients who are considering chiropractic cervical manipulation should be informed of the potential risk and be advised to seek immediate medical attention should they develop symptoms.
A prospective randomized controlled study published in 2012 showed chiropractic manipulation is beneficial in the treatment of neck pain compared with medical treatment, but it showed no significant difference between chiropractic manipulation and physical therapy exercises.1 Although chiropractic manipulation of the cervical spine may be effective, it may also cause harm.
Cerebellar and spinal cord injuries related to cervical chiropractic manipulation were first reported in 1947.2 By 1974, there were 12 reported cases.3 Noninvasive imaging has since greatly improved the diagnosis of cervical artery dissection and of stroke,4 and cervical artery dissection is now recognized as pathogenic of strokes occurring in association with chiropractic manipulation.5
A prospective series published in 2011 reported that, over 4 years, 13 patients were treated at a single institution for cervical arterial dissection following chiropractic treatment.6 That so many patients might be seen for this condition in that time frame at a single institution suggests the risk for such injury may be greater than thought. To explore that possibility, we performed a 4-year retrospective review to determine the experience at OSF Saint Francis Medical Center, which is affiliated with the University of Illinois College of Medicine, Peoria.
METHODS
Data sources. After receiving approval by the local institutional review board, we obtained data from the electronic medical records of OSF Saint Francis Medical Center, Peoria, Ill., using Epic (Epic Systems Corporation, Verona, Wis.) and IDX (General Electric Corporation, Fairfield, Conn.) systems. The records were queried using ICD-9 codes 443.21 and 443.24 to identify patients from April 2008 through March 2012 who had primary or secondary diagnoses of vertebral artery dissection (VAD) or carotid artery dissection (CAD). We reviewed all records of VAD and CAD to identify those that may have been associated with chiropractic manipulation.
Data collection. We abstracted data from 12 patients’ charts. Two patients were unavailable for direct contact: one was involved in ongoing litigation, and one had died (although we were able to speak with his wife). We attempted telephone contact with the 10 remaining patients and reached 8.
Data included the symptoms leading to chiropractic manipulation, symptoms following manipulation, timing of onset of symptoms relative to chiropractic manipulation, identifying information for the treating chiropractor, and residual patient symptoms. We also recorded patients’ ages, sex, locations of dissection, and locations of stroke. All dissections and strokes had been diagnosed during the patient’s initial hospitalization.
A board-certified radiologist (JRD) with a Certificate of Added Qualification in Neuroradiology (American Board of Medical Specialties) reviewed all pertinent imaging to confirm all dissections and strokes.
RESULTS
The medical record query yielded 141 patients with VAD or CAD, 15 of whom had undergone chiropractic manipulation prior to their presentation. The temporal association between chiropractic manipulation and arterial dissection was equivocal for 3 patients. In 12 patients, there was a verifiable temporal association between chiropractic manipulation and the arterial dissection. Three of the 12 patients were men and 9 were women. Ages ranged from 22 to 46 years, with a mean of 35.3 years.
Acute or chronic neck pain was the most common reason for seeking chiropractic care (TABLE 1). Immediately upon performance of cervical manipulation, 10 of the 12 developed acute symptoms different than those that caused them to seek chiropractic care. Two patients developed symptoms 2 to 3 days post-manipulation. Neither of the 2 had a history of neck trauma within the preceding year. Ten of the 12 patients sought immediate medical attention. Two of the 12 patients sought care when their symptoms became more severe, ranging from 2 days to several weeks later (TABLE 2). The treating chiropractor was identified in 7 cases and was different in each of the 7 cases.
A total of 16 cervical artery dissections, 14 VAD and 2 CAD, were confirmed by computed tomography angiography (CTA), magnetic resonance angiography (MRA), or catheter angiography (FIGURE 1). All 12 patients had acute strokes confirmed by MRA or CTA, including 9 in the cerebellum (FIGURE 2), 4 in the cerebrum, 2 in the medulla, and one in the pons.
Long-term outcomes were determined for 9 patients (TABLE 2). One patient’s symptoms resolved. Three patients had dizziness, clumsiness, or balance problems; 3 had persistent headaches; 2 had bilateral visual field abnormalities; and one patient walked with a cane, was no longer driving a car, and was on disability. One patient died as a result of his injury. One of the 12 cases was previously described in a case report.7

DISCUSSION
Dissection of the cervical arteries is more common than dissection in other arteries of comparable size. This increased risk in the cervical arteries is believed to be due to their relative mobility and proximity to bony structures.4
Sudden neck movement, a feature of chiropractic treatment, is one of several known risk factors for ‘spontaneous’ cervical artery dissection.8,9 Symptom onset and stroke may be delayed after a spontaneous cervical artery dissection.10 Spontaneous dissection more commonly involves the carotid arteries;4 however, the vertebral arteries appear more prone to dissection as a consequence of chiropractic manipulation,11 likely due to their relation to the cervical spine.
The vertebral artery runs through foramina in the transverse processes of vertebral bodies C1 through C6 (FIGURE 3). On exiting the C2 transverse process, the vertebral artery has a tortuous course, making several turns over and through adjacent bony structures.12 The artery is most prone to injury between the entrance to the transverse foramen of C6 and the foramen magnum (V2 and V3 segments).13 (The area of highest vulnerability is the tortuous segment from the transverse foramen of C2 to the foramen magnum.)
Sudden movements of the cervical spine may cause arterial dissection, whether the maneuvers are performed by a physician, a chiropractor, or a physical therapist.14 Injuries reported in the literature, however, most commonly follow chiropractic manipulation. In our series of 141 dissections, we found no cases associated with manipulation by other health professionals.
A 2003 study revealed cervical spine manipulation to be an independent and strong risk factor for vertebral artery dissection. The authors believed the relationship was likely causal.5 Data from the Canadian Stroke Consortium showed a 28% incidence of chiropractic manipulation in cases of cervical artery dissection.10
A 2008 study showed an association between vertebrobasilar stroke and chiropractic visits within one month of the vascular event.15 However, the study also showed an association of similar magnitude between vertebrobasilar stroke and visits to primary care physicians within the prior month. This suggests that cervical manipulation by chiropractors poses no more risk for cervical artery dissection than visits to primary care physicians. However, it is hard to reconcile such a conclusion with other studies, including our own, in which 10 patients developed new symptoms immediately with chiropractic manipulation of their cervical spines.
Perhaps the one-month observation period of Cassidy et al was excessive. Many post-manipulation events occur within hours or at most a few days, as would be expected given the hypothesized pathogenic mechanism. Perhaps if they had shortened their interval of study to the preceding 3 days, their findings may have been different.
A recent systematic review and meta-analysis demonstrated a slight association between chiropractic neck manipulation and cervical artery dissection. It stated that the quality of the published literature was very low, and it concluded there was no convincing evidence of causation.16 The fact that 10 of the 12 patients in our case series demonstrated acute symptoms immediately upon receiving spinal manipulation suggests a possible causal link; however, we agree with the authors of the meta-analysis that the quality of the literature is low.
A recent statement from the American Heart Association/American Stroke Association (and endorsed by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons) has recommended that chiropractors inform patients of the statistical association between cervical artery dissection and cervical manipulation.17 In addition, it is important for chiropractors to be aware of the signs and symptoms of cervical artery dissection and stroke and to assess for these symptoms before performing neck manipulation, as illustrated in a recent case report.18 Due to the risk of death, patients who experience symptoms consistent with cervical artery dissection after chiropractic manipulation of the cervical spine should be advised to seek medical care immediately.
Our case series has several limitations. The study was retrospective. Existing documentation of associated chiropractic care was often sparse, necessitating phone calls to supplement the information. We believe it is possible that cases may have been missed because of inaccurate medical record documentation, deficits in the interview process concerning chiropractic care at the time of hospitalization, or because information concerning chiropractic care was not recorded in the chart.
A significant portion of our information came through phone contact with several of the patients. In some cases, we relied heavily on their recollection of events that had occurred anytime from a few days to a few years earlier. The accuracy and completeness of the information supplied by patients was not verified, allowing for potential recall bias.
We do not know whether our experience is consistent with that of other areas of the United States. However, the fact that a similar-size hospital in Phoenix reported similar findings suggests the experience may be more widespread.6
IMPLICATIONS OF OUR FINDINGS
Over a 4-year period at our institution, 12 patients experienced cervical vessel dissection related to chiropractic neck manipulation. A similar institution in another part of the country had previously described 13 such cases. The patients at both institutions were relatively young and incurred substantial residual morbidity. A single patient at each institution died. If these findings are representative of other institutions across the United States, the incidence of stroke secondary to chiropractic manipulation may be higher than supposed.
To assess this problem further, a randomized prospective cohort study could establish the relative risk of chiropractic manipulation of the cervical spine resulting in a cervical artery dissection. But such a study may be methodologically prohibitive. More feasible would be a case-control study similar to one carried out by Smith et al5 in which patients who had experienced cervical artery dissection were matched with subjects who had not incurred such injuries. Comparing the groups’ odds of having received chiropractic manipulation demonstrated that spinal manipulative therapy is an independent risk factor for vertebral artery dissection and is highly suggestive of a causal association. Replicating this study in a different population would be valuable.
Based on our findings, all patients who visit chiropractors for cervical spine manipulation should be informed of the potential risks and of the need to seek immediate medical assistance should symptoms suggestive of dissection or stroke occur during or after manipulation. Until the actual level of risk from chiropractic manipulation is known, patients with neck pain may be better served by equally effective passive physical therapy exercises.1
CORRESPONDENCE
Raymond E. Bertino, MD, 427 West Crestwood Drive, Peoria, IL 61614; [email protected].
ACKNOWLEDGEMENTS
We thank Deepak Nair, MD, for his assistance in reviewing the stroke neurology aspects of this study; Katie Groesch, MD, for her assistance in drafting portions of the Methods and Results sections; Rita Hermacinski for the generation of 3D images; and Stephanie Arthalony for her assistance in gathering information through patient telephone interviews.
1.
2. Pratt-Thomas HR, Knute EB. Cerebellar and spinal injuries after chiropractic manipulation. JAMA. 1947;133:600-603.
3. Miller RG, Burton R. Stroke following chiropractic manipulation of the spine. JAMA. 1974;229:189-190.
4. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Eng J Med. 2001;344:898-906.
5. Smith WS, Johnston SC, Skalabrin EJ, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology. 2003;60:1424-1428.
6. Albuquerque FC, Hu YC, Dashti SR, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011;115:1197-1205.
7. Bertino RE, Talkad AV, DeSanto JR, et al. Chiropractic manipulation of the neck and cervical artery dissection. Ann Intern Med. 2012;157:150-152.
8. Dittrich R, Rohsbach D, Heidbreder A, et al. Mild mechanical traumas are possible risk factors for cervical artery dissection. Cerebrovasc Dis. 2006;23:275-281.
9. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668-678.
10. Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian Stroke Consortium. CMAJ. 2000;163:38-40.
11. Stevinson C, Ernst E. Risks associated with spinal manipulation. Am J Med. 2002;112:566–571.
12. Doshi AH, Aggarwal A, Patel AB. Normal vascular anatomy. In Naidich TP, Castillo M, Cha S, Smirniotopoulos JG, eds. Imaging of the Brain. Philadelphia, Pa: Saunders;
13. Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke. 2006;37:2499-2503.
14. Reuter U, Hämling M, Kavuk I, et al. Vertebral artery dissections after chiropractic neck manipulation in Germany over three years. J Neurol. 2006;253:724-730.
15. Cassidy JD, Boyle E, Cote P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008;17(Suppl 1):S176-S183.
16. Church EW, Sieg EP, Zalatima O, et al. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: No evidence for causation. Cureus. 2016;8:e498.
17. Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3155-3174.
18. Tarola G, Phillips RB. Chiropractic response to a spontaneous vertebral artery dissection. J Chiropr Med. 2015;14:183-190.
1.
2. Pratt-Thomas HR, Knute EB. Cerebellar and spinal injuries after chiropractic manipulation. JAMA. 1947;133:600-603.
3. Miller RG, Burton R. Stroke following chiropractic manipulation of the spine. JAMA. 1974;229:189-190.
4. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Eng J Med. 2001;344:898-906.
5. Smith WS, Johnston SC, Skalabrin EJ, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology. 2003;60:1424-1428.
6. Albuquerque FC, Hu YC, Dashti SR, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011;115:1197-1205.
7. Bertino RE, Talkad AV, DeSanto JR, et al. Chiropractic manipulation of the neck and cervical artery dissection. Ann Intern Med. 2012;157:150-152.
8. Dittrich R, Rohsbach D, Heidbreder A, et al. Mild mechanical traumas are possible risk factors for cervical artery dissection. Cerebrovasc Dis. 2006;23:275-281.
9. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668-678.
10. Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian Stroke Consortium. CMAJ. 2000;163:38-40.
11. Stevinson C, Ernst E. Risks associated with spinal manipulation. Am J Med. 2002;112:566–571.
12. Doshi AH, Aggarwal A, Patel AB. Normal vascular anatomy. In Naidich TP, Castillo M, Cha S, Smirniotopoulos JG, eds. Imaging of the Brain. Philadelphia, Pa: Saunders;
13. Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke. 2006;37:2499-2503.
14. Reuter U, Hämling M, Kavuk I, et al. Vertebral artery dissections after chiropractic neck manipulation in Germany over three years. J Neurol. 2006;253:724-730.
15. Cassidy JD, Boyle E, Cote P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008;17(Suppl 1):S176-S183.
16. Church EW, Sieg EP, Zalatima O, et al. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: No evidence for causation. Cureus. 2016;8:e498.
17. Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3155-3174.
18. Tarola G, Phillips RB. Chiropractic response to a spontaneous vertebral artery dissection. J Chiropr Med. 2015;14:183-190.
