User login
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
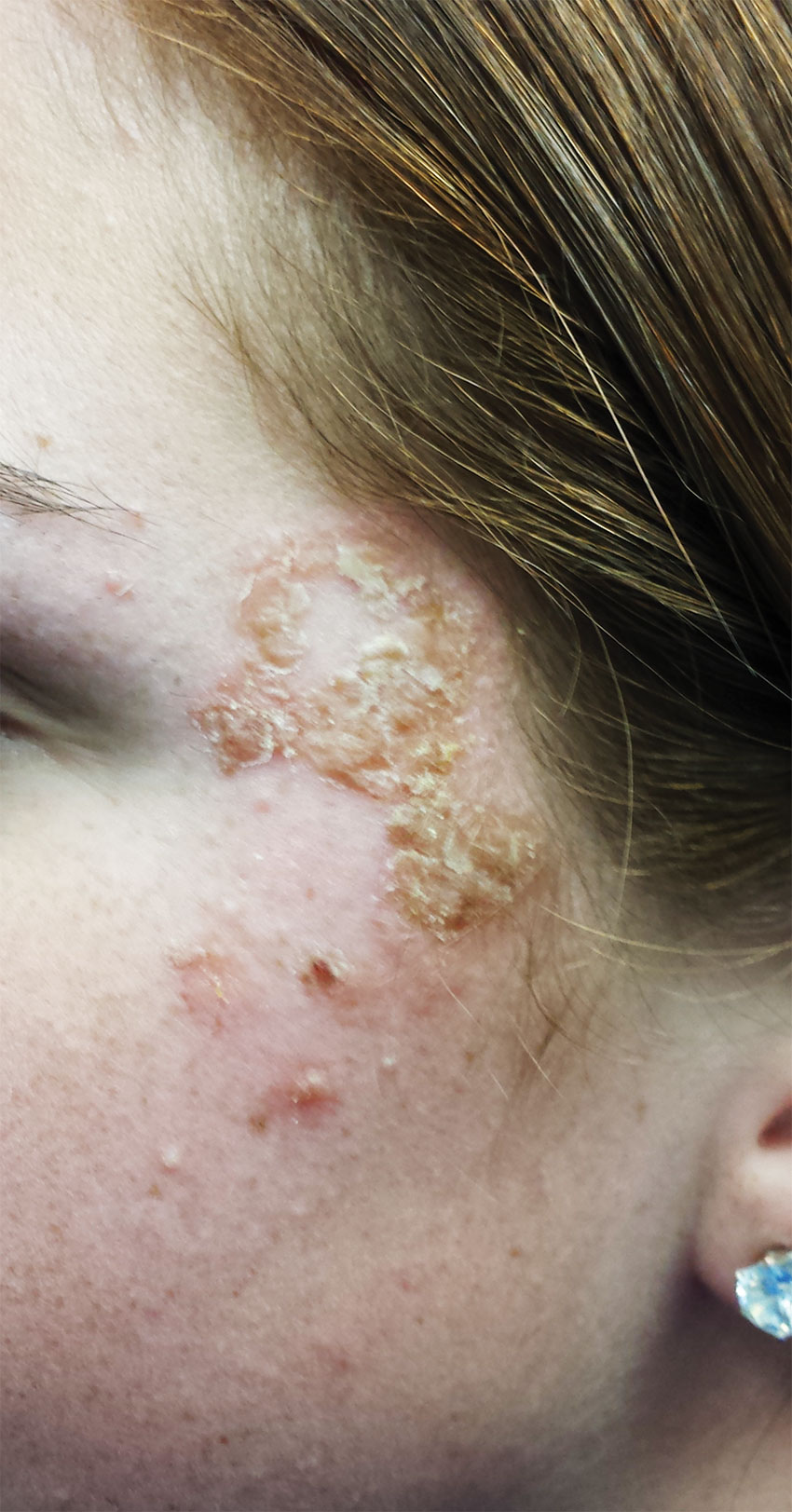
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
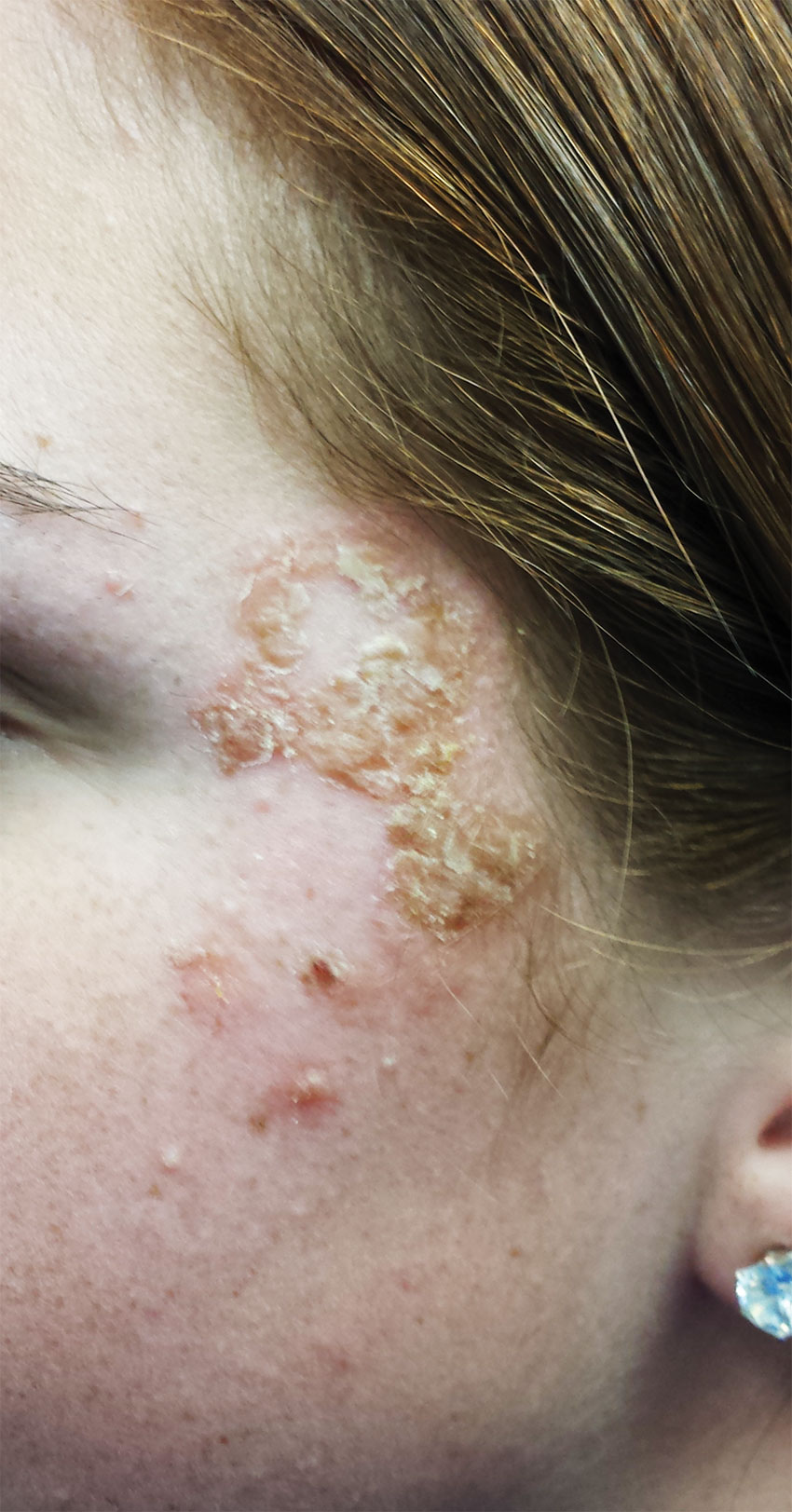
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
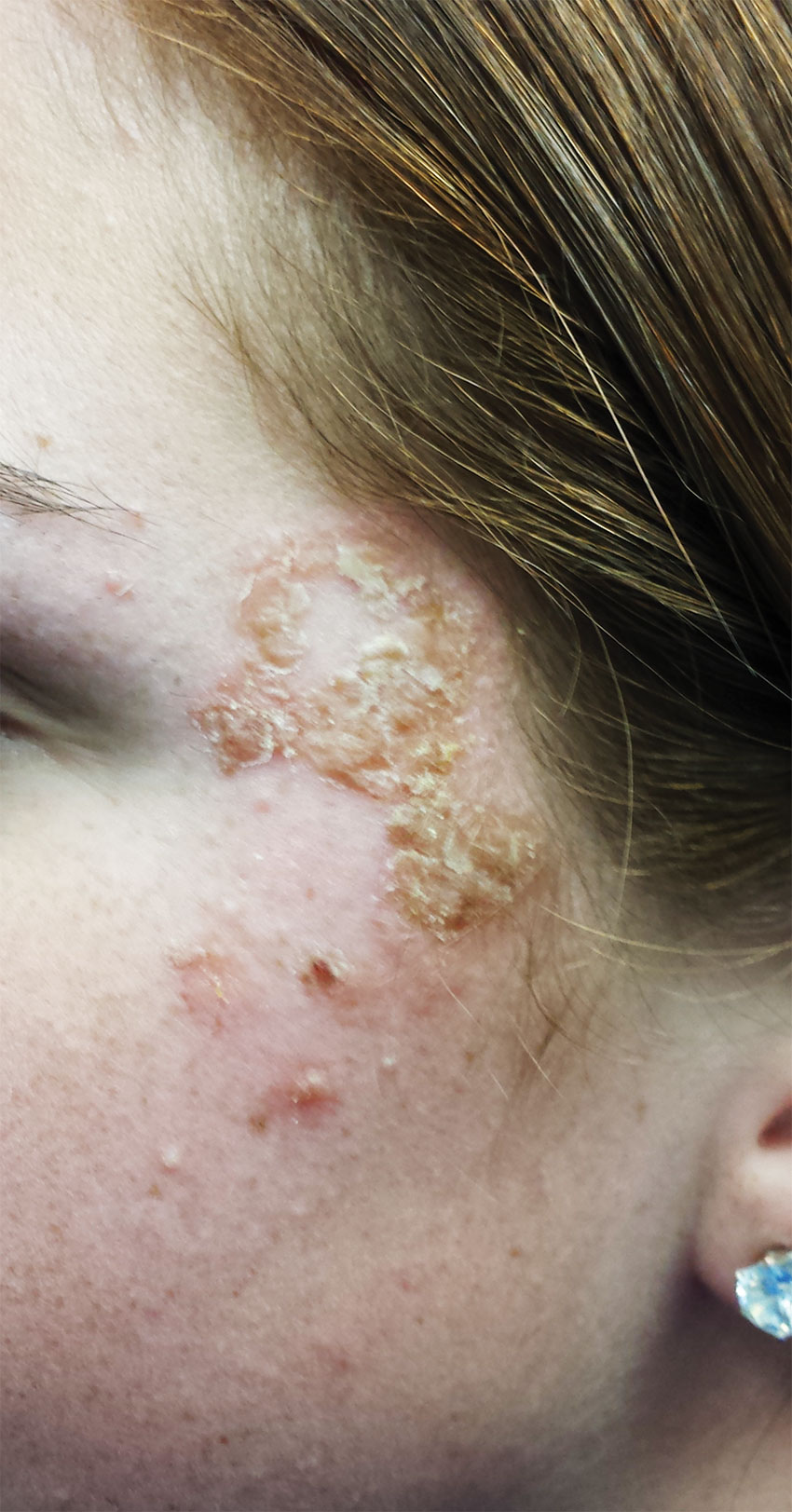
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.