User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
A depressed adolescent who won’t eat and reacts slowly
CASE A fainting spell
Ms. A, age 13, is admitted to a pediatric unit after fainting and losing consciousness for 5 minutes in the shower, during which time she was non-responsive. She reports feeling nauseated and having blurry vision before dropping to the floor.
Ms. A reports intentional self-restriction of calories, self-induced vomiting, and other purging behaviors, such as laxative abuse and excessive exercising.
During the mental status examination, Ms. A is lying in bed wearing hospital clothes, legs flexed at the knee, hands on her side, and a fixed gaze at the ceiling with poor eye contact. She is of slender stature and tall, seems slightly older than her stated age, and is poorly groomed.
Throughout the interview, Ms. A has significant psychomotor retardation, reports her mood as tired, and has a blunted affect. She speaks at a low volume and has poverty of speech; she takes deep sighs before answering questions. Her thought process is linear and she cooperates with the interview. She has poor recall, including delayed 3-minute recall and poor sustained attention. Her abstraction capacity is fair and her intellect is average and comparable with her age group. Ms. A is preoccupied that eating will cause weight gain. She denies hallucinations but reports passive death wishes with self-harm by scratching.
What is the differential diagnosis to explain Ms. A’s presentation?
a) syncope
b) seizures
c) dehydration
d) hypotension
HISTORY Preoccupied with weight
Ms. A reports vomiting twice a day, while showering and at night when no one is around, every day for 2 months. She stopped eating and taking in fluids 3 days before admission to the medical unit. Also, she reports restricting her diet to 700 to 1,000 calories a day, skipping lunch at school, and eating minimally at night. Ms. A uses raspberry ketones and green coffee beans, which are advertised to aid weight loss, and laxative pills from her mother’s medicine cabinet once or twice a week when her throat is sore from vomiting. She reports exercising excessively, which includes running, crunches, and lifting weights. She has lost approximately 30 lb in the last 2 months.
Ms. A says she fears gaining weight and feels increased guilt after eating a meal. She said that looking at food induced “anxiety attack” symptoms of increased heart rate, sweaty palms, feeling of choking, nervousness, and shakiness. She adds that she does not want to be “bigger” than her classmates. Her understanding of the consequences of not eating is, “It will get worse, I will shut down and die. I do not fear death, I only fear getting bigger than others.”
She reports that her fixation on avoiding food started when she realized that she was the tallest girl in her class and the only girl in her class running on the track team, after which she quit athletics. She reports that depression symptoms pre-dated her eating disorder symptoms; onset of significant depression likely was precipitated by her grandfather’s death a year earlier, and then exacerbated by the recent death of a family pet.
Ms. A’s depressive symptoms are described as anhedonia (avoiding being outside and not enjoying drawing anymore), decreased energy, tearfulness, sadness, decreased concentration, and passive suicidal thoughts. Her mother is supportive and motivates her daughter to “get better.” Ms. A denies any symptoms of psychosis, other anxiety symptoms, other mood disorder symptoms, substance abuse, or homicidality.
Ms. A’s mother says she felt that, recently, her daughter has been having some difficulty with confused thoughts and significantly delayed responses. However, the mother reports that her daughter always had somewhat delayed responses from what she felt is typical. Her mother adds that Ms. A’s suicidal thoughts have worsened since her daughter started restricting her diet.
Which diagnosis likely accounts for Ms. A’s presentation?
a) major depressive disorder (MDD)
b) eating disorder, not otherwise specified (NOS)
c) anorexia nervosa, purging type
d) catatonia, unspecified
e) anxiety disorder NOS
f) cognitive disorder
g) psychosis NOS
The authors’ observations
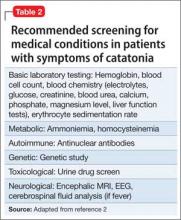
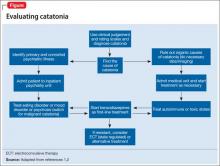
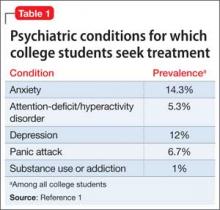
There are many reported causes of catatonia in children and adolescents, including those that are psychiatric, medical, or neurological, as well as drugs (Table 1).1,2 Affective disorders have been associated with catatonia in adults, but has not been widely reported in children and adolescents.1,3 Organic and neurologic causes, such as neurological tumors and cerebral hemorrhage, should be ruled out first because, although rare, they can be fatal (Table 2).2 If the cause of catatonia is not recognized quickly (Figure,1,2) effective treatment could be delayed.4
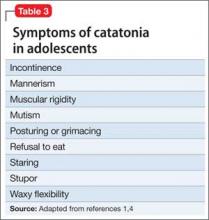
Catatonia involves psychomotor abnormalities, which are listed in Table 3.1,4
Presentation in adults and adolescents is similar.
An eating disorder could be comorbid with another psychiatric disorder, such as MDD, dysthymia, or panic disorder.5 Ms. A’s report of depression before she began restricting food favored a primary diagnosis of MDD. Her depressive symptoms of low appetite or low self-worth could have led to her preoccupation with body image.
There has been evidence that negative self-image and eating disorders are associated, but data are limited and the connection remains unclear.6 Ms. A’s self-esteem was very low. Her fixation on restricting food could have been perpetuated by her self-criticism and by being excluded from her peer group in school. Her weight loss could have brought anxiety symptoms to the forefront because of physiologic changes that accompany extreme weight loss.
The treatment team was concerned about her delayed responses, which could be explained by the catatonic features that reflected the severity of her depression. She had no obvious symptoms of psychosis, but her intrusive thoughts and obsessions with avoiding food did not completely rule out psychosis.
Childhood-onset schizophrenia, although rare, has been associated with catatonia; following up with a catatonia rating scale, such as the Catatonia Rating Scale or the Bush- Francis Catatonia Rating Scale (BFCRS), would be useful for tracking symptom progress. In Ms. A’s case, her mood disorder was primary, but did not rule out psychosis-like prodromal symptoms.7
Ms. A is diagnosed with MDD, single episode, severe, with catatonic features, and without psychosis, and eating disorder, NOS.
EVALUATION Mostly normal
Ms. A does not have a history of mental illness and was not seeing a psychiatrist or therapist, nor did she have any prior psychiatric admissions. She denies suicide attempts, but reports self-injurious behavior involving scratching her skin, which started during the current mood episode. She has never taken any psychotropic medications. Ms. A lives at home with her biological mother and father and 17-year-old brother. She attends middle school with average grades and has no history of disciplinary actions. She has no history of bullying or teasing, although she did report some previous difficulty with relational aggression toward her peers in the 5th grade. Her mother has a history of anorexia nervosa that began when she was a teenager, but these symptoms are stable and under control. There is additionally a family history of bipolar disorder.
Ms. A has a family history of coronary artery disease and diabetes in the mother and maternal relatives. Her grandfather died from liver cancer. She was allergic to sulfa drugs and was taking a multivitamin and minocycline for acne.
Physical examination reveals some superficial scratches but otherwise was within normal limits. Initial lab results reveal a normal complete blood count and differential. Thyroid-stimulating hormone is 1.29 mIU/L and free T4 is 0.96 mg/dL, both within normal limits. Urinalysis is within normal limits and urine pregnancy test is negative. A comprehensive metabolic panel shows mild elevation in aspartate aminotransferase (AST) at 60 U/L and alanine aminotransferase (ALT) at 92 U/L, respectively. Phosphorus level is within normal limits. Prealbumin level is slightly low at 15.1 mg/dL.
Which treatment plan would you recommend for Ms. A?
a) discharge with outpatient psychiatric treatment
b) recommend medical stabilization with follow-up from the psychosomatic team and then outpatient psychiatric follow-up
c) admit her to the psychiatric acute inpatient hospital with psychiatric outpatient discharge follow-up plan
d) discharge her home with follow-up with her primary care physician
e) recommend follow-up from the psychosomatic team while on medical floor with acute inpatient admission and psychiatric outpatient follow-up at discharge
The authors’ observations
Scarcity of data and reporting of cases of adolescent catatonia limits guidance for diagnosis and treatment.8 There are several rating scales with variability in definition, but that overall provide a guiding tool for detecting catatonia. The Brief Cognitive Rating Scale is considered the most versatile because it is more valid, reliable, and requires less time to complete than other rating scales.9
Ms. A’s symptoms were a combination of depressive symptoms with severity defined by catatonic features, eating disorder with worsening course, anxiety symptoms, and genetic loading of eating disorder in her mother. The challenge of this case was making an accurate diagnosis and treating Ms. A, which required continuous observation following an eating disorder protocol, resolution of her catatonia, resuming a normal diet, and decreasing her suicidality. Retrospectively, her scores on the BFCRS were high on screening items 1 to 14, which measure presence or absence and severity of symptoms.
The best option was to admit Ms. A to an inpatient psychiatric facility after she is cleared medically with outpatient services to follow up.
How would you treat Ms. A’s symptoms?
a) aggressively treat catatonia
b) address her eating disorder
c) work to resolve her depression
The authors’ observations
The challenge was to choose the psychotropic medication that would target her depression, obsessive, rigid thoughts, and catatonia. Administering an antidepressant with an antipsychotic would have relieved her depressive and obsessive symptoms but would not have improved her catatonia. The psychosomatic medicine team recommended starting a selective serotonin reuptake inhibitor and a benzodiazepine to target both the depression and the catatonic symptoms. Ms. A received sertraline, 12.5 mg/d, which was increased to 25 mg/d on the third day. IV lorazepam, 1 mg, 3 times a day, was recommended but the pediatric team prescribed an oral formulation. The hospital’s eating disorder protocol was instituted on the day of admission.
Treatment options for catatonia
Benzodiazepines are the first line of treatment for catatonia and other neuroleptics, specifically antipsychotics, have been considered dangerous.10 Benzodiazepine-resistant catatonia, which is sometimes seen in patients with autism, might respond to electroconvulsive therapy (ECT),11 although in some states it cannot be administered to children age <18.12 Benzodiazepines have shown dramatic improvement within hours, as has ECT.8,13 Additionally, if patients do not respond to a benzodiazepine or ECT, consider other options such as zolpidem, olanzapine,14 or sensory integration system (in adolescents with autism).15
Ms. A did not need ECT or an alternative treatment because she responded well to 3 doses of oral lorazepam. Her amotivation, negativism, and rigidity with prolonged posturing improved. Her psychomotor retardation improved overall, although she reported some dizziness and had some postural hypotension, which was attributed to her eating issues and dehydration.
OUTCOME Feeling motivated
Ms. A is transferred to psychiatric inpatient unit. She tolerates sertraline, which is titrated to 50 mg/d. She is placed on the hospital’s standard eating disorder protocol. She continues to eat well with adequate intake of solids and liquid and exhibits only some anxiety associated with meals. During the course of hospitalization, she attends group therapy and her catatonic symptoms completely resolve. She says she thinks that her thoughts are improving and that she is not longer feeling confused. She reports being motivated to continue to improve her eating disorder symptoms.
The treatment team holds a family session during which family dynamic issues that are stressful to Ms. A are discussed, such as some conflict with her parents as well as some negative interactions between Ms. A and her father. Repeat comprehensive metabolic panel on admission to the inpatient psychiatric hospital reveals persistent elevation of AST at 92 U/L and ALT at 143 U/L. Ms. A is discharged home with follow-up with a psychiatrist and a therapist. The treatment team also recommends that she follow up in a program that specializes in eating disorders.
4-month follow-up. Ms. A returns to inpatient psychiatric hospital after overdose of sertraline and aripiprazole, which were started by an outpatient psychiatrist. She reports severe depressive symptoms because of school stressors. She denies any problems eating and did not show any symptoms of catatonia. In her chart, there is a mention of “cloudy thoughts” and quietness. At this admission, her ALT is 17 U/L and AST is 19 U/L. Sertraline is increased to 150 mg/d and aripiprazole is reduced to 2 mg/d and then later increased to 5 mg/d, after which she is discharged home with an outpatient psychiatric follow-up.
1-year follow-up. Ms. A has been following up with an outpatient psychiatrist and is receiving sertraline, 150 mg/d, aripiprazole, 2.5 mg/d, and extended-release methylphenidate, 36 mg/d, along with L-methylfolate, multivitamins, and omega-3 fish oil as adjuvants for her depressive symptoms. Ms. A does not show symptoms of an eating disorder or catatonia, and her depression and psychomotor activity have improved, with better overall functionality, after adding the stimulant and adjunctives to the antidepressant.
The authors’ observations
The importance of including catatonia NOS with its various specifiers, such as medical, metabolic, toxic, affective, etc., has been discussed.16,17 In Ms. A’s case, instead of treating the specific symptoms—affective or eating disorder or obsessive quality of thought content, mimicking psychotic-like symptoms—addressing the catatonia initially had a better outcome. More studies related to chronic and acute catatonia in adolescents are needed because of the risk of increased morbidity and premature death.18 Early recognition of catatonia is needed19 because it often is underdiagnosed.20
Eating disorders often become worse over the first 5 years, and close monitoring and assessment is needed for adolescents.21 Also, prodromal psychotic symptoms require follow-up because techniques for early detection and intervention for children and adolescents are still in their infancy.22
Bottom Line
Catatonia in adolescents should be addressed early, when it is treatable and the outcome is favorable. It is important to recognize catatonia in an emergency department or inpatient medical unit setting in a hospital because it is often underdiagnosed or misdiagnosed. The presentation of catatonia is similar in adolescents and adults. Benzodiazepines are first-line treatment for catatonia; consider electroconvulsive therapy if patients do not respond to drug therapy.
Related Resources
• Roberto AJ, Pinnaka S, Mohan A, et al. Adolescent catatonia successfully treated with lorazepam and aripiprazole. Case Rep Psychiatry. 2014;2014:309517. doi: 10.1155/2014/309517.
• Raffin M, Zugaj-Bensaou L, Bodeau N, et al. Treatment use in a prospective naturalistic cohort of children and adolescents with catatonia. Eur Child Adolesc Psychiatry. 2015;24(4):441-449.
Drug Brand Names
Aripiprazole • Abilify Minocycline • Minocin
L-methylfolate • Deplin Olanzapine • Zyprexa
Lorazepam • Ativan Sertraline • Zoloft
Methylphenidate • Ritalin, Concerta Zolpidem • Ambien, Intermezzo
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Dhossche D, Wilson C, Wachtel LE. Catatonia in childhood and adolescence: implications for the DSM-5. Primary Psychiatry. http://primarypsychiatry.com/catatonia-in-childhood-and-adolescence-implications-for-the-dsm-5. Published May 21, 2013. Accessed July 2, 2015.
2. Lahutte B, Cornic F, Bonnot O, et al. Multidisciplinary approach of organic catatonia in children and adolescents may improve treatment decision making. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1393-1398.
3. Brake JA, Abidi S. A case of adolescent catatonia. J Can Acad Child Adolesc Psychiatry. 2010;19(2):138-140.
4. Consoli A, Raffin M, Laurent C, et al. Medical and developmental risk factors of catatonia in children and adolescents: a prospective case-control study. Schizophr Res. 2012;137(1-3):151-158.
5. Zaider TI, Johnson JG, Cockell SJ. Psychiatric comorbidity associated with eating disorder symptomatology among adolescents in the community. Int J Eat Disord. 2000;28(1):58-67.
6. Forsén Mantilla E, Bergsten K, Birgegård A. Self-image and eating disorder symptoms in normal and clinical adolescents. Eat Behav. 2014;15(1):125-131.
7. Bonnot O, Tanguy ML, Consoli A, et al. Does catatonia influence the phenomenology of childhood onset schizophrenia beyond motor symptoms? Psychiatry Res. 2008;158(3):356-362.
8. Singh LK, Praharaj SK. Immediate response to lorazepam in a patient with 17 years of chronic catatonia. J Neuropsychiatry Clin Neurosci. 2013;25(3):E47-E48.
9. Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord. 2011;135(1-3):1-9.
10. Cottencin O, Warembourg F, de Chouly de Lenclave MB, et al. Catatonia and consultation-liaison psychiatry study of 12 cases. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(6):1170-1176.
11. Wachtel LE, Hermida A, Dhossche DM. Maintenance electroconvulsive therapy in autistic catatonia: a case series review. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(4):581-587.
12. Wachtel LE, Dhossche DM, Kellner CH. When is electroconvulsive therapy appropriate for children and adolescents? Med Hypotheses. 2011;76(3):395-399.
13. Takaoka K, Takata T. Catatonia in childhood and adolescence. Psychiatry Clin Neurosci. 2003;57(2):129-137.
14. Ceylan MF, Kul M, Kultur SE, et al. Major depression with catatonic features in a child remitted with olanzapine. J Child Adolesc Psychopharmacol. 2010;20(3):225-227.
15. Consoli A, Gheorghiev C, Jutard C, et al. Lorazepam, fluoxetine and packing therapy in an adolescent with pervasive developmental disorder and catatonia. J Physiol Paris. 2010;104(6):309-314.
16. Dhossche D, Cohen D, Ghaziuddin N, et al. The study of pediatric catatonia supports a home of its own for catatonia in DSM-5. Med Hypotheses. 2010;75(6):558-560.
17. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
18. Cornic F, Consoli A, Tanguy ML, et al. Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res. 2009;113(2-3):233-240.
19. Quigley J, Lommel KM, Coffey B. Catatonia in an adolescent with Asperger’s disorder. J Child Adolesc Psychopharmacol. 2009;19(1):93-96.
20. Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. 2012;125(1):33-38.
21. Ackard DM, Fulkerson JA, Neumark-Sztainer D. Stability of eating disorder diagnostic classifications in adolescents: five-year longitudinal findings from a population-based study. Eat Disord. 2011;19(4):308-322.
22. Schimmelmann BG, Schultze-Lutter F. Early detection and intervention of psychosis in children and adolescents: urgent need for studies. Eur Child Adolesc Psychiatry. 2012;21(5):239-241.
CASE A fainting spell
Ms. A, age 13, is admitted to a pediatric unit after fainting and losing consciousness for 5 minutes in the shower, during which time she was non-responsive. She reports feeling nauseated and having blurry vision before dropping to the floor.
Ms. A reports intentional self-restriction of calories, self-induced vomiting, and other purging behaviors, such as laxative abuse and excessive exercising.
During the mental status examination, Ms. A is lying in bed wearing hospital clothes, legs flexed at the knee, hands on her side, and a fixed gaze at the ceiling with poor eye contact. She is of slender stature and tall, seems slightly older than her stated age, and is poorly groomed.
Throughout the interview, Ms. A has significant psychomotor retardation, reports her mood as tired, and has a blunted affect. She speaks at a low volume and has poverty of speech; she takes deep sighs before answering questions. Her thought process is linear and she cooperates with the interview. She has poor recall, including delayed 3-minute recall and poor sustained attention. Her abstraction capacity is fair and her intellect is average and comparable with her age group. Ms. A is preoccupied that eating will cause weight gain. She denies hallucinations but reports passive death wishes with self-harm by scratching.
What is the differential diagnosis to explain Ms. A’s presentation?
a) syncope
b) seizures
c) dehydration
d) hypotension
HISTORY Preoccupied with weight
Ms. A reports vomiting twice a day, while showering and at night when no one is around, every day for 2 months. She stopped eating and taking in fluids 3 days before admission to the medical unit. Also, she reports restricting her diet to 700 to 1,000 calories a day, skipping lunch at school, and eating minimally at night. Ms. A uses raspberry ketones and green coffee beans, which are advertised to aid weight loss, and laxative pills from her mother’s medicine cabinet once or twice a week when her throat is sore from vomiting. She reports exercising excessively, which includes running, crunches, and lifting weights. She has lost approximately 30 lb in the last 2 months.
Ms. A says she fears gaining weight and feels increased guilt after eating a meal. She said that looking at food induced “anxiety attack” symptoms of increased heart rate, sweaty palms, feeling of choking, nervousness, and shakiness. She adds that she does not want to be “bigger” than her classmates. Her understanding of the consequences of not eating is, “It will get worse, I will shut down and die. I do not fear death, I only fear getting bigger than others.”
She reports that her fixation on avoiding food started when she realized that she was the tallest girl in her class and the only girl in her class running on the track team, after which she quit athletics. She reports that depression symptoms pre-dated her eating disorder symptoms; onset of significant depression likely was precipitated by her grandfather’s death a year earlier, and then exacerbated by the recent death of a family pet.
Ms. A’s depressive symptoms are described as anhedonia (avoiding being outside and not enjoying drawing anymore), decreased energy, tearfulness, sadness, decreased concentration, and passive suicidal thoughts. Her mother is supportive and motivates her daughter to “get better.” Ms. A denies any symptoms of psychosis, other anxiety symptoms, other mood disorder symptoms, substance abuse, or homicidality.
Ms. A’s mother says she felt that, recently, her daughter has been having some difficulty with confused thoughts and significantly delayed responses. However, the mother reports that her daughter always had somewhat delayed responses from what she felt is typical. Her mother adds that Ms. A’s suicidal thoughts have worsened since her daughter started restricting her diet.
Which diagnosis likely accounts for Ms. A’s presentation?
a) major depressive disorder (MDD)
b) eating disorder, not otherwise specified (NOS)
c) anorexia nervosa, purging type
d) catatonia, unspecified
e) anxiety disorder NOS
f) cognitive disorder
g) psychosis NOS
The authors’ observations
There are many reported causes of catatonia in children and adolescents, including those that are psychiatric, medical, or neurological, as well as drugs (Table 1).1,2 Affective disorders have been associated with catatonia in adults, but has not been widely reported in children and adolescents.1,3 Organic and neurologic causes, such as neurological tumors and cerebral hemorrhage, should be ruled out first because, although rare, they can be fatal (Table 2).2 If the cause of catatonia is not recognized quickly (Figure,1,2) effective treatment could be delayed.4
Catatonia involves psychomotor abnormalities, which are listed in Table 3.1,4
Presentation in adults and adolescents is similar.
An eating disorder could be comorbid with another psychiatric disorder, such as MDD, dysthymia, or panic disorder.5 Ms. A’s report of depression before she began restricting food favored a primary diagnosis of MDD. Her depressive symptoms of low appetite or low self-worth could have led to her preoccupation with body image.
There has been evidence that negative self-image and eating disorders are associated, but data are limited and the connection remains unclear.6 Ms. A’s self-esteem was very low. Her fixation on restricting food could have been perpetuated by her self-criticism and by being excluded from her peer group in school. Her weight loss could have brought anxiety symptoms to the forefront because of physiologic changes that accompany extreme weight loss.
The treatment team was concerned about her delayed responses, which could be explained by the catatonic features that reflected the severity of her depression. She had no obvious symptoms of psychosis, but her intrusive thoughts and obsessions with avoiding food did not completely rule out psychosis.
Childhood-onset schizophrenia, although rare, has been associated with catatonia; following up with a catatonia rating scale, such as the Catatonia Rating Scale or the Bush- Francis Catatonia Rating Scale (BFCRS), would be useful for tracking symptom progress. In Ms. A’s case, her mood disorder was primary, but did not rule out psychosis-like prodromal symptoms.7
Ms. A is diagnosed with MDD, single episode, severe, with catatonic features, and without psychosis, and eating disorder, NOS.
EVALUATION Mostly normal
Ms. A does not have a history of mental illness and was not seeing a psychiatrist or therapist, nor did she have any prior psychiatric admissions. She denies suicide attempts, but reports self-injurious behavior involving scratching her skin, which started during the current mood episode. She has never taken any psychotropic medications. Ms. A lives at home with her biological mother and father and 17-year-old brother. She attends middle school with average grades and has no history of disciplinary actions. She has no history of bullying or teasing, although she did report some previous difficulty with relational aggression toward her peers in the 5th grade. Her mother has a history of anorexia nervosa that began when she was a teenager, but these symptoms are stable and under control. There is additionally a family history of bipolar disorder.
Ms. A has a family history of coronary artery disease and diabetes in the mother and maternal relatives. Her grandfather died from liver cancer. She was allergic to sulfa drugs and was taking a multivitamin and minocycline for acne.
Physical examination reveals some superficial scratches but otherwise was within normal limits. Initial lab results reveal a normal complete blood count and differential. Thyroid-stimulating hormone is 1.29 mIU/L and free T4 is 0.96 mg/dL, both within normal limits. Urinalysis is within normal limits and urine pregnancy test is negative. A comprehensive metabolic panel shows mild elevation in aspartate aminotransferase (AST) at 60 U/L and alanine aminotransferase (ALT) at 92 U/L, respectively. Phosphorus level is within normal limits. Prealbumin level is slightly low at 15.1 mg/dL.
Which treatment plan would you recommend for Ms. A?
a) discharge with outpatient psychiatric treatment
b) recommend medical stabilization with follow-up from the psychosomatic team and then outpatient psychiatric follow-up
c) admit her to the psychiatric acute inpatient hospital with psychiatric outpatient discharge follow-up plan
d) discharge her home with follow-up with her primary care physician
e) recommend follow-up from the psychosomatic team while on medical floor with acute inpatient admission and psychiatric outpatient follow-up at discharge
The authors’ observations
Scarcity of data and reporting of cases of adolescent catatonia limits guidance for diagnosis and treatment.8 There are several rating scales with variability in definition, but that overall provide a guiding tool for detecting catatonia. The Brief Cognitive Rating Scale is considered the most versatile because it is more valid, reliable, and requires less time to complete than other rating scales.9
Ms. A’s symptoms were a combination of depressive symptoms with severity defined by catatonic features, eating disorder with worsening course, anxiety symptoms, and genetic loading of eating disorder in her mother. The challenge of this case was making an accurate diagnosis and treating Ms. A, which required continuous observation following an eating disorder protocol, resolution of her catatonia, resuming a normal diet, and decreasing her suicidality. Retrospectively, her scores on the BFCRS were high on screening items 1 to 14, which measure presence or absence and severity of symptoms.
The best option was to admit Ms. A to an inpatient psychiatric facility after she is cleared medically with outpatient services to follow up.
How would you treat Ms. A’s symptoms?
a) aggressively treat catatonia
b) address her eating disorder
c) work to resolve her depression
The authors’ observations
The challenge was to choose the psychotropic medication that would target her depression, obsessive, rigid thoughts, and catatonia. Administering an antidepressant with an antipsychotic would have relieved her depressive and obsessive symptoms but would not have improved her catatonia. The psychosomatic medicine team recommended starting a selective serotonin reuptake inhibitor and a benzodiazepine to target both the depression and the catatonic symptoms. Ms. A received sertraline, 12.5 mg/d, which was increased to 25 mg/d on the third day. IV lorazepam, 1 mg, 3 times a day, was recommended but the pediatric team prescribed an oral formulation. The hospital’s eating disorder protocol was instituted on the day of admission.
Treatment options for catatonia
Benzodiazepines are the first line of treatment for catatonia and other neuroleptics, specifically antipsychotics, have been considered dangerous.10 Benzodiazepine-resistant catatonia, which is sometimes seen in patients with autism, might respond to electroconvulsive therapy (ECT),11 although in some states it cannot be administered to children age <18.12 Benzodiazepines have shown dramatic improvement within hours, as has ECT.8,13 Additionally, if patients do not respond to a benzodiazepine or ECT, consider other options such as zolpidem, olanzapine,14 or sensory integration system (in adolescents with autism).15
Ms. A did not need ECT or an alternative treatment because she responded well to 3 doses of oral lorazepam. Her amotivation, negativism, and rigidity with prolonged posturing improved. Her psychomotor retardation improved overall, although she reported some dizziness and had some postural hypotension, which was attributed to her eating issues and dehydration.
OUTCOME Feeling motivated
Ms. A is transferred to psychiatric inpatient unit. She tolerates sertraline, which is titrated to 50 mg/d. She is placed on the hospital’s standard eating disorder protocol. She continues to eat well with adequate intake of solids and liquid and exhibits only some anxiety associated with meals. During the course of hospitalization, she attends group therapy and her catatonic symptoms completely resolve. She says she thinks that her thoughts are improving and that she is not longer feeling confused. She reports being motivated to continue to improve her eating disorder symptoms.
The treatment team holds a family session during which family dynamic issues that are stressful to Ms. A are discussed, such as some conflict with her parents as well as some negative interactions between Ms. A and her father. Repeat comprehensive metabolic panel on admission to the inpatient psychiatric hospital reveals persistent elevation of AST at 92 U/L and ALT at 143 U/L. Ms. A is discharged home with follow-up with a psychiatrist and a therapist. The treatment team also recommends that she follow up in a program that specializes in eating disorders.
4-month follow-up. Ms. A returns to inpatient psychiatric hospital after overdose of sertraline and aripiprazole, which were started by an outpatient psychiatrist. She reports severe depressive symptoms because of school stressors. She denies any problems eating and did not show any symptoms of catatonia. In her chart, there is a mention of “cloudy thoughts” and quietness. At this admission, her ALT is 17 U/L and AST is 19 U/L. Sertraline is increased to 150 mg/d and aripiprazole is reduced to 2 mg/d and then later increased to 5 mg/d, after which she is discharged home with an outpatient psychiatric follow-up.
1-year follow-up. Ms. A has been following up with an outpatient psychiatrist and is receiving sertraline, 150 mg/d, aripiprazole, 2.5 mg/d, and extended-release methylphenidate, 36 mg/d, along with L-methylfolate, multivitamins, and omega-3 fish oil as adjuvants for her depressive symptoms. Ms. A does not show symptoms of an eating disorder or catatonia, and her depression and psychomotor activity have improved, with better overall functionality, after adding the stimulant and adjunctives to the antidepressant.
The authors’ observations
The importance of including catatonia NOS with its various specifiers, such as medical, metabolic, toxic, affective, etc., has been discussed.16,17 In Ms. A’s case, instead of treating the specific symptoms—affective or eating disorder or obsessive quality of thought content, mimicking psychotic-like symptoms—addressing the catatonia initially had a better outcome. More studies related to chronic and acute catatonia in adolescents are needed because of the risk of increased morbidity and premature death.18 Early recognition of catatonia is needed19 because it often is underdiagnosed.20
Eating disorders often become worse over the first 5 years, and close monitoring and assessment is needed for adolescents.21 Also, prodromal psychotic symptoms require follow-up because techniques for early detection and intervention for children and adolescents are still in their infancy.22
Bottom Line
Catatonia in adolescents should be addressed early, when it is treatable and the outcome is favorable. It is important to recognize catatonia in an emergency department or inpatient medical unit setting in a hospital because it is often underdiagnosed or misdiagnosed. The presentation of catatonia is similar in adolescents and adults. Benzodiazepines are first-line treatment for catatonia; consider electroconvulsive therapy if patients do not respond to drug therapy.
Related Resources
• Roberto AJ, Pinnaka S, Mohan A, et al. Adolescent catatonia successfully treated with lorazepam and aripiprazole. Case Rep Psychiatry. 2014;2014:309517. doi: 10.1155/2014/309517.
• Raffin M, Zugaj-Bensaou L, Bodeau N, et al. Treatment use in a prospective naturalistic cohort of children and adolescents with catatonia. Eur Child Adolesc Psychiatry. 2015;24(4):441-449.
Drug Brand Names
Aripiprazole • Abilify Minocycline • Minocin
L-methylfolate • Deplin Olanzapine • Zyprexa
Lorazepam • Ativan Sertraline • Zoloft
Methylphenidate • Ritalin, Concerta Zolpidem • Ambien, Intermezzo
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE A fainting spell
Ms. A, age 13, is admitted to a pediatric unit after fainting and losing consciousness for 5 minutes in the shower, during which time she was non-responsive. She reports feeling nauseated and having blurry vision before dropping to the floor.
Ms. A reports intentional self-restriction of calories, self-induced vomiting, and other purging behaviors, such as laxative abuse and excessive exercising.
During the mental status examination, Ms. A is lying in bed wearing hospital clothes, legs flexed at the knee, hands on her side, and a fixed gaze at the ceiling with poor eye contact. She is of slender stature and tall, seems slightly older than her stated age, and is poorly groomed.
Throughout the interview, Ms. A has significant psychomotor retardation, reports her mood as tired, and has a blunted affect. She speaks at a low volume and has poverty of speech; she takes deep sighs before answering questions. Her thought process is linear and she cooperates with the interview. She has poor recall, including delayed 3-minute recall and poor sustained attention. Her abstraction capacity is fair and her intellect is average and comparable with her age group. Ms. A is preoccupied that eating will cause weight gain. She denies hallucinations but reports passive death wishes with self-harm by scratching.
What is the differential diagnosis to explain Ms. A’s presentation?
a) syncope
b) seizures
c) dehydration
d) hypotension
HISTORY Preoccupied with weight
Ms. A reports vomiting twice a day, while showering and at night when no one is around, every day for 2 months. She stopped eating and taking in fluids 3 days before admission to the medical unit. Also, she reports restricting her diet to 700 to 1,000 calories a day, skipping lunch at school, and eating minimally at night. Ms. A uses raspberry ketones and green coffee beans, which are advertised to aid weight loss, and laxative pills from her mother’s medicine cabinet once or twice a week when her throat is sore from vomiting. She reports exercising excessively, which includes running, crunches, and lifting weights. She has lost approximately 30 lb in the last 2 months.
Ms. A says she fears gaining weight and feels increased guilt after eating a meal. She said that looking at food induced “anxiety attack” symptoms of increased heart rate, sweaty palms, feeling of choking, nervousness, and shakiness. She adds that she does not want to be “bigger” than her classmates. Her understanding of the consequences of not eating is, “It will get worse, I will shut down and die. I do not fear death, I only fear getting bigger than others.”
She reports that her fixation on avoiding food started when she realized that she was the tallest girl in her class and the only girl in her class running on the track team, after which she quit athletics. She reports that depression symptoms pre-dated her eating disorder symptoms; onset of significant depression likely was precipitated by her grandfather’s death a year earlier, and then exacerbated by the recent death of a family pet.
Ms. A’s depressive symptoms are described as anhedonia (avoiding being outside and not enjoying drawing anymore), decreased energy, tearfulness, sadness, decreased concentration, and passive suicidal thoughts. Her mother is supportive and motivates her daughter to “get better.” Ms. A denies any symptoms of psychosis, other anxiety symptoms, other mood disorder symptoms, substance abuse, or homicidality.
Ms. A’s mother says she felt that, recently, her daughter has been having some difficulty with confused thoughts and significantly delayed responses. However, the mother reports that her daughter always had somewhat delayed responses from what she felt is typical. Her mother adds that Ms. A’s suicidal thoughts have worsened since her daughter started restricting her diet.
Which diagnosis likely accounts for Ms. A’s presentation?
a) major depressive disorder (MDD)
b) eating disorder, not otherwise specified (NOS)
c) anorexia nervosa, purging type
d) catatonia, unspecified
e) anxiety disorder NOS
f) cognitive disorder
g) psychosis NOS
The authors’ observations
There are many reported causes of catatonia in children and adolescents, including those that are psychiatric, medical, or neurological, as well as drugs (Table 1).1,2 Affective disorders have been associated with catatonia in adults, but has not been widely reported in children and adolescents.1,3 Organic and neurologic causes, such as neurological tumors and cerebral hemorrhage, should be ruled out first because, although rare, they can be fatal (Table 2).2 If the cause of catatonia is not recognized quickly (Figure,1,2) effective treatment could be delayed.4
Catatonia involves psychomotor abnormalities, which are listed in Table 3.1,4
Presentation in adults and adolescents is similar.
An eating disorder could be comorbid with another psychiatric disorder, such as MDD, dysthymia, or panic disorder.5 Ms. A’s report of depression before she began restricting food favored a primary diagnosis of MDD. Her depressive symptoms of low appetite or low self-worth could have led to her preoccupation with body image.
There has been evidence that negative self-image and eating disorders are associated, but data are limited and the connection remains unclear.6 Ms. A’s self-esteem was very low. Her fixation on restricting food could have been perpetuated by her self-criticism and by being excluded from her peer group in school. Her weight loss could have brought anxiety symptoms to the forefront because of physiologic changes that accompany extreme weight loss.
The treatment team was concerned about her delayed responses, which could be explained by the catatonic features that reflected the severity of her depression. She had no obvious symptoms of psychosis, but her intrusive thoughts and obsessions with avoiding food did not completely rule out psychosis.
Childhood-onset schizophrenia, although rare, has been associated with catatonia; following up with a catatonia rating scale, such as the Catatonia Rating Scale or the Bush- Francis Catatonia Rating Scale (BFCRS), would be useful for tracking symptom progress. In Ms. A’s case, her mood disorder was primary, but did not rule out psychosis-like prodromal symptoms.7
Ms. A is diagnosed with MDD, single episode, severe, with catatonic features, and without psychosis, and eating disorder, NOS.
EVALUATION Mostly normal
Ms. A does not have a history of mental illness and was not seeing a psychiatrist or therapist, nor did she have any prior psychiatric admissions. She denies suicide attempts, but reports self-injurious behavior involving scratching her skin, which started during the current mood episode. She has never taken any psychotropic medications. Ms. A lives at home with her biological mother and father and 17-year-old brother. She attends middle school with average grades and has no history of disciplinary actions. She has no history of bullying or teasing, although she did report some previous difficulty with relational aggression toward her peers in the 5th grade. Her mother has a history of anorexia nervosa that began when she was a teenager, but these symptoms are stable and under control. There is additionally a family history of bipolar disorder.
Ms. A has a family history of coronary artery disease and diabetes in the mother and maternal relatives. Her grandfather died from liver cancer. She was allergic to sulfa drugs and was taking a multivitamin and minocycline for acne.
Physical examination reveals some superficial scratches but otherwise was within normal limits. Initial lab results reveal a normal complete blood count and differential. Thyroid-stimulating hormone is 1.29 mIU/L and free T4 is 0.96 mg/dL, both within normal limits. Urinalysis is within normal limits and urine pregnancy test is negative. A comprehensive metabolic panel shows mild elevation in aspartate aminotransferase (AST) at 60 U/L and alanine aminotransferase (ALT) at 92 U/L, respectively. Phosphorus level is within normal limits. Prealbumin level is slightly low at 15.1 mg/dL.
Which treatment plan would you recommend for Ms. A?
a) discharge with outpatient psychiatric treatment
b) recommend medical stabilization with follow-up from the psychosomatic team and then outpatient psychiatric follow-up
c) admit her to the psychiatric acute inpatient hospital with psychiatric outpatient discharge follow-up plan
d) discharge her home with follow-up with her primary care physician
e) recommend follow-up from the psychosomatic team while on medical floor with acute inpatient admission and psychiatric outpatient follow-up at discharge
The authors’ observations
Scarcity of data and reporting of cases of adolescent catatonia limits guidance for diagnosis and treatment.8 There are several rating scales with variability in definition, but that overall provide a guiding tool for detecting catatonia. The Brief Cognitive Rating Scale is considered the most versatile because it is more valid, reliable, and requires less time to complete than other rating scales.9
Ms. A’s symptoms were a combination of depressive symptoms with severity defined by catatonic features, eating disorder with worsening course, anxiety symptoms, and genetic loading of eating disorder in her mother. The challenge of this case was making an accurate diagnosis and treating Ms. A, which required continuous observation following an eating disorder protocol, resolution of her catatonia, resuming a normal diet, and decreasing her suicidality. Retrospectively, her scores on the BFCRS were high on screening items 1 to 14, which measure presence or absence and severity of symptoms.
The best option was to admit Ms. A to an inpatient psychiatric facility after she is cleared medically with outpatient services to follow up.
How would you treat Ms. A’s symptoms?
a) aggressively treat catatonia
b) address her eating disorder
c) work to resolve her depression
The authors’ observations
The challenge was to choose the psychotropic medication that would target her depression, obsessive, rigid thoughts, and catatonia. Administering an antidepressant with an antipsychotic would have relieved her depressive and obsessive symptoms but would not have improved her catatonia. The psychosomatic medicine team recommended starting a selective serotonin reuptake inhibitor and a benzodiazepine to target both the depression and the catatonic symptoms. Ms. A received sertraline, 12.5 mg/d, which was increased to 25 mg/d on the third day. IV lorazepam, 1 mg, 3 times a day, was recommended but the pediatric team prescribed an oral formulation. The hospital’s eating disorder protocol was instituted on the day of admission.
Treatment options for catatonia
Benzodiazepines are the first line of treatment for catatonia and other neuroleptics, specifically antipsychotics, have been considered dangerous.10 Benzodiazepine-resistant catatonia, which is sometimes seen in patients with autism, might respond to electroconvulsive therapy (ECT),11 although in some states it cannot be administered to children age <18.12 Benzodiazepines have shown dramatic improvement within hours, as has ECT.8,13 Additionally, if patients do not respond to a benzodiazepine or ECT, consider other options such as zolpidem, olanzapine,14 or sensory integration system (in adolescents with autism).15
Ms. A did not need ECT or an alternative treatment because she responded well to 3 doses of oral lorazepam. Her amotivation, negativism, and rigidity with prolonged posturing improved. Her psychomotor retardation improved overall, although she reported some dizziness and had some postural hypotension, which was attributed to her eating issues and dehydration.
OUTCOME Feeling motivated
Ms. A is transferred to psychiatric inpatient unit. She tolerates sertraline, which is titrated to 50 mg/d. She is placed on the hospital’s standard eating disorder protocol. She continues to eat well with adequate intake of solids and liquid and exhibits only some anxiety associated with meals. During the course of hospitalization, she attends group therapy and her catatonic symptoms completely resolve. She says she thinks that her thoughts are improving and that she is not longer feeling confused. She reports being motivated to continue to improve her eating disorder symptoms.
The treatment team holds a family session during which family dynamic issues that are stressful to Ms. A are discussed, such as some conflict with her parents as well as some negative interactions between Ms. A and her father. Repeat comprehensive metabolic panel on admission to the inpatient psychiatric hospital reveals persistent elevation of AST at 92 U/L and ALT at 143 U/L. Ms. A is discharged home with follow-up with a psychiatrist and a therapist. The treatment team also recommends that she follow up in a program that specializes in eating disorders.
4-month follow-up. Ms. A returns to inpatient psychiatric hospital after overdose of sertraline and aripiprazole, which were started by an outpatient psychiatrist. She reports severe depressive symptoms because of school stressors. She denies any problems eating and did not show any symptoms of catatonia. In her chart, there is a mention of “cloudy thoughts” and quietness. At this admission, her ALT is 17 U/L and AST is 19 U/L. Sertraline is increased to 150 mg/d and aripiprazole is reduced to 2 mg/d and then later increased to 5 mg/d, after which she is discharged home with an outpatient psychiatric follow-up.
1-year follow-up. Ms. A has been following up with an outpatient psychiatrist and is receiving sertraline, 150 mg/d, aripiprazole, 2.5 mg/d, and extended-release methylphenidate, 36 mg/d, along with L-methylfolate, multivitamins, and omega-3 fish oil as adjuvants for her depressive symptoms. Ms. A does not show symptoms of an eating disorder or catatonia, and her depression and psychomotor activity have improved, with better overall functionality, after adding the stimulant and adjunctives to the antidepressant.
The authors’ observations
The importance of including catatonia NOS with its various specifiers, such as medical, metabolic, toxic, affective, etc., has been discussed.16,17 In Ms. A’s case, instead of treating the specific symptoms—affective or eating disorder or obsessive quality of thought content, mimicking psychotic-like symptoms—addressing the catatonia initially had a better outcome. More studies related to chronic and acute catatonia in adolescents are needed because of the risk of increased morbidity and premature death.18 Early recognition of catatonia is needed19 because it often is underdiagnosed.20
Eating disorders often become worse over the first 5 years, and close monitoring and assessment is needed for adolescents.21 Also, prodromal psychotic symptoms require follow-up because techniques for early detection and intervention for children and adolescents are still in their infancy.22
Bottom Line
Catatonia in adolescents should be addressed early, when it is treatable and the outcome is favorable. It is important to recognize catatonia in an emergency department or inpatient medical unit setting in a hospital because it is often underdiagnosed or misdiagnosed. The presentation of catatonia is similar in adolescents and adults. Benzodiazepines are first-line treatment for catatonia; consider electroconvulsive therapy if patients do not respond to drug therapy.
Related Resources
• Roberto AJ, Pinnaka S, Mohan A, et al. Adolescent catatonia successfully treated with lorazepam and aripiprazole. Case Rep Psychiatry. 2014;2014:309517. doi: 10.1155/2014/309517.
• Raffin M, Zugaj-Bensaou L, Bodeau N, et al. Treatment use in a prospective naturalistic cohort of children and adolescents with catatonia. Eur Child Adolesc Psychiatry. 2015;24(4):441-449.
Drug Brand Names
Aripiprazole • Abilify Minocycline • Minocin
L-methylfolate • Deplin Olanzapine • Zyprexa
Lorazepam • Ativan Sertraline • Zoloft
Methylphenidate • Ritalin, Concerta Zolpidem • Ambien, Intermezzo
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Dhossche D, Wilson C, Wachtel LE. Catatonia in childhood and adolescence: implications for the DSM-5. Primary Psychiatry. http://primarypsychiatry.com/catatonia-in-childhood-and-adolescence-implications-for-the-dsm-5. Published May 21, 2013. Accessed July 2, 2015.
2. Lahutte B, Cornic F, Bonnot O, et al. Multidisciplinary approach of organic catatonia in children and adolescents may improve treatment decision making. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1393-1398.
3. Brake JA, Abidi S. A case of adolescent catatonia. J Can Acad Child Adolesc Psychiatry. 2010;19(2):138-140.
4. Consoli A, Raffin M, Laurent C, et al. Medical and developmental risk factors of catatonia in children and adolescents: a prospective case-control study. Schizophr Res. 2012;137(1-3):151-158.
5. Zaider TI, Johnson JG, Cockell SJ. Psychiatric comorbidity associated with eating disorder symptomatology among adolescents in the community. Int J Eat Disord. 2000;28(1):58-67.
6. Forsén Mantilla E, Bergsten K, Birgegård A. Self-image and eating disorder symptoms in normal and clinical adolescents. Eat Behav. 2014;15(1):125-131.
7. Bonnot O, Tanguy ML, Consoli A, et al. Does catatonia influence the phenomenology of childhood onset schizophrenia beyond motor symptoms? Psychiatry Res. 2008;158(3):356-362.
8. Singh LK, Praharaj SK. Immediate response to lorazepam in a patient with 17 years of chronic catatonia. J Neuropsychiatry Clin Neurosci. 2013;25(3):E47-E48.
9. Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord. 2011;135(1-3):1-9.
10. Cottencin O, Warembourg F, de Chouly de Lenclave MB, et al. Catatonia and consultation-liaison psychiatry study of 12 cases. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(6):1170-1176.
11. Wachtel LE, Hermida A, Dhossche DM. Maintenance electroconvulsive therapy in autistic catatonia: a case series review. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(4):581-587.
12. Wachtel LE, Dhossche DM, Kellner CH. When is electroconvulsive therapy appropriate for children and adolescents? Med Hypotheses. 2011;76(3):395-399.
13. Takaoka K, Takata T. Catatonia in childhood and adolescence. Psychiatry Clin Neurosci. 2003;57(2):129-137.
14. Ceylan MF, Kul M, Kultur SE, et al. Major depression with catatonic features in a child remitted with olanzapine. J Child Adolesc Psychopharmacol. 2010;20(3):225-227.
15. Consoli A, Gheorghiev C, Jutard C, et al. Lorazepam, fluoxetine and packing therapy in an adolescent with pervasive developmental disorder and catatonia. J Physiol Paris. 2010;104(6):309-314.
16. Dhossche D, Cohen D, Ghaziuddin N, et al. The study of pediatric catatonia supports a home of its own for catatonia in DSM-5. Med Hypotheses. 2010;75(6):558-560.
17. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
18. Cornic F, Consoli A, Tanguy ML, et al. Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res. 2009;113(2-3):233-240.
19. Quigley J, Lommel KM, Coffey B. Catatonia in an adolescent with Asperger’s disorder. J Child Adolesc Psychopharmacol. 2009;19(1):93-96.
20. Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. 2012;125(1):33-38.
21. Ackard DM, Fulkerson JA, Neumark-Sztainer D. Stability of eating disorder diagnostic classifications in adolescents: five-year longitudinal findings from a population-based study. Eat Disord. 2011;19(4):308-322.
22. Schimmelmann BG, Schultze-Lutter F. Early detection and intervention of psychosis in children and adolescents: urgent need for studies. Eur Child Adolesc Psychiatry. 2012;21(5):239-241.
1. Dhossche D, Wilson C, Wachtel LE. Catatonia in childhood and adolescence: implications for the DSM-5. Primary Psychiatry. http://primarypsychiatry.com/catatonia-in-childhood-and-adolescence-implications-for-the-dsm-5. Published May 21, 2013. Accessed July 2, 2015.
2. Lahutte B, Cornic F, Bonnot O, et al. Multidisciplinary approach of organic catatonia in children and adolescents may improve treatment decision making. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1393-1398.
3. Brake JA, Abidi S. A case of adolescent catatonia. J Can Acad Child Adolesc Psychiatry. 2010;19(2):138-140.
4. Consoli A, Raffin M, Laurent C, et al. Medical and developmental risk factors of catatonia in children and adolescents: a prospective case-control study. Schizophr Res. 2012;137(1-3):151-158.
5. Zaider TI, Johnson JG, Cockell SJ. Psychiatric comorbidity associated with eating disorder symptomatology among adolescents in the community. Int J Eat Disord. 2000;28(1):58-67.
6. Forsén Mantilla E, Bergsten K, Birgegård A. Self-image and eating disorder symptoms in normal and clinical adolescents. Eat Behav. 2014;15(1):125-131.
7. Bonnot O, Tanguy ML, Consoli A, et al. Does catatonia influence the phenomenology of childhood onset schizophrenia beyond motor symptoms? Psychiatry Res. 2008;158(3):356-362.
8. Singh LK, Praharaj SK. Immediate response to lorazepam in a patient with 17 years of chronic catatonia. J Neuropsychiatry Clin Neurosci. 2013;25(3):E47-E48.
9. Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord. 2011;135(1-3):1-9.
10. Cottencin O, Warembourg F, de Chouly de Lenclave MB, et al. Catatonia and consultation-liaison psychiatry study of 12 cases. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(6):1170-1176.
11. Wachtel LE, Hermida A, Dhossche DM. Maintenance electroconvulsive therapy in autistic catatonia: a case series review. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(4):581-587.
12. Wachtel LE, Dhossche DM, Kellner CH. When is electroconvulsive therapy appropriate for children and adolescents? Med Hypotheses. 2011;76(3):395-399.
13. Takaoka K, Takata T. Catatonia in childhood and adolescence. Psychiatry Clin Neurosci. 2003;57(2):129-137.
14. Ceylan MF, Kul M, Kultur SE, et al. Major depression with catatonic features in a child remitted with olanzapine. J Child Adolesc Psychopharmacol. 2010;20(3):225-227.
15. Consoli A, Gheorghiev C, Jutard C, et al. Lorazepam, fluoxetine and packing therapy in an adolescent with pervasive developmental disorder and catatonia. J Physiol Paris. 2010;104(6):309-314.
16. Dhossche D, Cohen D, Ghaziuddin N, et al. The study of pediatric catatonia supports a home of its own for catatonia in DSM-5. Med Hypotheses. 2010;75(6):558-560.
17. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
18. Cornic F, Consoli A, Tanguy ML, et al. Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res. 2009;113(2-3):233-240.
19. Quigley J, Lommel KM, Coffey B. Catatonia in an adolescent with Asperger’s disorder. J Child Adolesc Psychopharmacol. 2009;19(1):93-96.
20. Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. 2012;125(1):33-38.
21. Ackard DM, Fulkerson JA, Neumark-Sztainer D. Stability of eating disorder diagnostic classifications in adolescents: five-year longitudinal findings from a population-based study. Eat Disord. 2011;19(4):308-322.
22. Schimmelmann BG, Schultze-Lutter F. Early detection and intervention of psychosis in children and adolescents: urgent need for studies. Eur Child Adolesc Psychiatry. 2012;21(5):239-241.
How to tame the big time wasters in your practice
Pulling up charts. Phone tag. Prior authorizations. Rinse, repeat.
Reminiscent of the movie Groundhog Day, the daily grind in running a practice rarely gives way. Some days there are more faxes to process or paperwork to push than other days but, on the whole, there’s no escaping the tedium and time sink that these gloomy chores engender. In some practices, an assistant is hired to absorb the barrage; if not, it is left to the clinician to handle at the expense of time for patient care or life outside practice.
Compounding matters, creating new systems to assuage these tasks can feel like a sisyphean endeavor, because the energy required to start likely will be more than what is already being expended. For example, switching from paper-based to electronic systems is tantalizing but incurs its own learning curve and has a financial cost. Likewise, hiring administrative help demands a significant investment in training and, if patient contact is part of the job description, even more preparation is necessary because she (he) becomes the public face of the practice. Fortunately, both of these options pay dividends in the long run.
Yet, even with some basic strategies, what seems like the inevitability of inertia can be reshaped into a more efficient, less quotidian experience. Consider the following ways to streamline processes and eliminate time wasted and not spent on providing care.
Patient-specific tasks
Prior authorizations. The typical process is to have to call the insurance company to have the paperwork faxed, burning 5 to 15 minutes by being placed on hold or being transferred between departments. Instead, ask the patient to call the insurance company (she [he] should get the phone number from the pharmacist and have your fax number handy) and request the paperwork, with her (his) demographic information pre-filled in, be faxed to your office. If she is told by the insurance company that the doctor has to call, instruct the patient to explain it is merely a request to have forms faxed and to call again and speak with a different agent if necessary. If the patient pushes back, explaining that this helps keeps your rates lower or from having to bill for this specific time usually smooths things over.
Voicemails. Listening (and re-listening) to a long voicemail takes time. Although using a professional transcription service might be costly, it may be less expensive than your time if you get lots of long voicemails. Or, consider using a service that provides computer-generated transcriptions. Although less accurate, it often allows you to skim and is more affordable.
Scheduling. Booking follow-up appointments during a session uses valuable clinical care time, but booking them outside of session can be laborious. As an alternative, offer online scheduling through your electronic medical record (EMR) or a stand-alone service that allows you to retain control over what times you are available and how soon and far out patients can book. Be sure that only your current patients and, perhaps, colleagues (for scheduling phone calls) have access to your calendar, and make your cancellation policy explicitly clear.
Refill requests. Patients routinely opt-in for automatic prescription refill requests at their pharmacy, believing it is a no-brainer for convenience’s sake. However, for psychiatrists who prescribe only enough refills to last until the patient’s next appointment, these requests can become a burden because they can’t be ignored, but shouldn’t necessarily be acted upon either. Often, time is spent clarifying with the patient if a refill is really needed, and sometimes—consciously or unconsciously— patients use automatic requests to bypass having to come in for an appointment. As an alternative, ask your patients to opt-out of auto-refill programs and to contact you directly if they are about to run out of medication.
Prescreening. An inordinate amount of time can be spent ensuring that a prospective patient is a good fit from a clinical, scheduling, and payment perspective. Save time by having a simple prescreening process that conveys that you care, yet want to make sure certain criteria are met before you accept a patient into the practice. This is where having a trained assistant or an electronic prescreening option can be useful.
Practice at large
Electronic charts. Common complaints about EMRs among users are they are clunky, convoluted, and slow, and the EMR “flow” does not match the provider’s. Although each extra click might only take a few seconds, the loss of rhythm is draining and leads to a dissatisfying, tired feeling. Be sure when selecting an EMR that the user experience is considered as important as functionality.
Billing statements. Write or print, fold, place in an envelope, put a stamp on the envelope, address the envelope, take it to the mailbox. Need more be said about how inefficient this is? Use your EMR, a biller, or billing software to send statements automatically.
Of course, make sure that any method that employs technology or outsourcing to a service has appropriate Health Insurance Portability and Accountability Act safeguards.
Nothing to lose but your chains
Although running a practice gives you some freedom in your schedule, with that comes the shackles of processing administrative tasks that accompany clinical care. Finding ways to handle them more efficiently leads to improved job satisfaction and more time for patient care. You and your patients will both benefit.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Pulling up charts. Phone tag. Prior authorizations. Rinse, repeat.
Reminiscent of the movie Groundhog Day, the daily grind in running a practice rarely gives way. Some days there are more faxes to process or paperwork to push than other days but, on the whole, there’s no escaping the tedium and time sink that these gloomy chores engender. In some practices, an assistant is hired to absorb the barrage; if not, it is left to the clinician to handle at the expense of time for patient care or life outside practice.
Compounding matters, creating new systems to assuage these tasks can feel like a sisyphean endeavor, because the energy required to start likely will be more than what is already being expended. For example, switching from paper-based to electronic systems is tantalizing but incurs its own learning curve and has a financial cost. Likewise, hiring administrative help demands a significant investment in training and, if patient contact is part of the job description, even more preparation is necessary because she (he) becomes the public face of the practice. Fortunately, both of these options pay dividends in the long run.
Yet, even with some basic strategies, what seems like the inevitability of inertia can be reshaped into a more efficient, less quotidian experience. Consider the following ways to streamline processes and eliminate time wasted and not spent on providing care.
Patient-specific tasks
Prior authorizations. The typical process is to have to call the insurance company to have the paperwork faxed, burning 5 to 15 minutes by being placed on hold or being transferred between departments. Instead, ask the patient to call the insurance company (she [he] should get the phone number from the pharmacist and have your fax number handy) and request the paperwork, with her (his) demographic information pre-filled in, be faxed to your office. If she is told by the insurance company that the doctor has to call, instruct the patient to explain it is merely a request to have forms faxed and to call again and speak with a different agent if necessary. If the patient pushes back, explaining that this helps keeps your rates lower or from having to bill for this specific time usually smooths things over.
Voicemails. Listening (and re-listening) to a long voicemail takes time. Although using a professional transcription service might be costly, it may be less expensive than your time if you get lots of long voicemails. Or, consider using a service that provides computer-generated transcriptions. Although less accurate, it often allows you to skim and is more affordable.
Scheduling. Booking follow-up appointments during a session uses valuable clinical care time, but booking them outside of session can be laborious. As an alternative, offer online scheduling through your electronic medical record (EMR) or a stand-alone service that allows you to retain control over what times you are available and how soon and far out patients can book. Be sure that only your current patients and, perhaps, colleagues (for scheduling phone calls) have access to your calendar, and make your cancellation policy explicitly clear.
Refill requests. Patients routinely opt-in for automatic prescription refill requests at their pharmacy, believing it is a no-brainer for convenience’s sake. However, for psychiatrists who prescribe only enough refills to last until the patient’s next appointment, these requests can become a burden because they can’t be ignored, but shouldn’t necessarily be acted upon either. Often, time is spent clarifying with the patient if a refill is really needed, and sometimes—consciously or unconsciously— patients use automatic requests to bypass having to come in for an appointment. As an alternative, ask your patients to opt-out of auto-refill programs and to contact you directly if they are about to run out of medication.
Prescreening. An inordinate amount of time can be spent ensuring that a prospective patient is a good fit from a clinical, scheduling, and payment perspective. Save time by having a simple prescreening process that conveys that you care, yet want to make sure certain criteria are met before you accept a patient into the practice. This is where having a trained assistant or an electronic prescreening option can be useful.
Practice at large
Electronic charts. Common complaints about EMRs among users are they are clunky, convoluted, and slow, and the EMR “flow” does not match the provider’s. Although each extra click might only take a few seconds, the loss of rhythm is draining and leads to a dissatisfying, tired feeling. Be sure when selecting an EMR that the user experience is considered as important as functionality.
Billing statements. Write or print, fold, place in an envelope, put a stamp on the envelope, address the envelope, take it to the mailbox. Need more be said about how inefficient this is? Use your EMR, a biller, or billing software to send statements automatically.
Of course, make sure that any method that employs technology or outsourcing to a service has appropriate Health Insurance Portability and Accountability Act safeguards.
Nothing to lose but your chains
Although running a practice gives you some freedom in your schedule, with that comes the shackles of processing administrative tasks that accompany clinical care. Finding ways to handle them more efficiently leads to improved job satisfaction and more time for patient care. You and your patients will both benefit.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Pulling up charts. Phone tag. Prior authorizations. Rinse, repeat.
Reminiscent of the movie Groundhog Day, the daily grind in running a practice rarely gives way. Some days there are more faxes to process or paperwork to push than other days but, on the whole, there’s no escaping the tedium and time sink that these gloomy chores engender. In some practices, an assistant is hired to absorb the barrage; if not, it is left to the clinician to handle at the expense of time for patient care or life outside practice.
Compounding matters, creating new systems to assuage these tasks can feel like a sisyphean endeavor, because the energy required to start likely will be more than what is already being expended. For example, switching from paper-based to electronic systems is tantalizing but incurs its own learning curve and has a financial cost. Likewise, hiring administrative help demands a significant investment in training and, if patient contact is part of the job description, even more preparation is necessary because she (he) becomes the public face of the practice. Fortunately, both of these options pay dividends in the long run.
Yet, even with some basic strategies, what seems like the inevitability of inertia can be reshaped into a more efficient, less quotidian experience. Consider the following ways to streamline processes and eliminate time wasted and not spent on providing care.
Patient-specific tasks
Prior authorizations. The typical process is to have to call the insurance company to have the paperwork faxed, burning 5 to 15 minutes by being placed on hold or being transferred between departments. Instead, ask the patient to call the insurance company (she [he] should get the phone number from the pharmacist and have your fax number handy) and request the paperwork, with her (his) demographic information pre-filled in, be faxed to your office. If she is told by the insurance company that the doctor has to call, instruct the patient to explain it is merely a request to have forms faxed and to call again and speak with a different agent if necessary. If the patient pushes back, explaining that this helps keeps your rates lower or from having to bill for this specific time usually smooths things over.
Voicemails. Listening (and re-listening) to a long voicemail takes time. Although using a professional transcription service might be costly, it may be less expensive than your time if you get lots of long voicemails. Or, consider using a service that provides computer-generated transcriptions. Although less accurate, it often allows you to skim and is more affordable.
Scheduling. Booking follow-up appointments during a session uses valuable clinical care time, but booking them outside of session can be laborious. As an alternative, offer online scheduling through your electronic medical record (EMR) or a stand-alone service that allows you to retain control over what times you are available and how soon and far out patients can book. Be sure that only your current patients and, perhaps, colleagues (for scheduling phone calls) have access to your calendar, and make your cancellation policy explicitly clear.
Refill requests. Patients routinely opt-in for automatic prescription refill requests at their pharmacy, believing it is a no-brainer for convenience’s sake. However, for psychiatrists who prescribe only enough refills to last until the patient’s next appointment, these requests can become a burden because they can’t be ignored, but shouldn’t necessarily be acted upon either. Often, time is spent clarifying with the patient if a refill is really needed, and sometimes—consciously or unconsciously— patients use automatic requests to bypass having to come in for an appointment. As an alternative, ask your patients to opt-out of auto-refill programs and to contact you directly if they are about to run out of medication.
Prescreening. An inordinate amount of time can be spent ensuring that a prospective patient is a good fit from a clinical, scheduling, and payment perspective. Save time by having a simple prescreening process that conveys that you care, yet want to make sure certain criteria are met before you accept a patient into the practice. This is where having a trained assistant or an electronic prescreening option can be useful.
Practice at large
Electronic charts. Common complaints about EMRs among users are they are clunky, convoluted, and slow, and the EMR “flow” does not match the provider’s. Although each extra click might only take a few seconds, the loss of rhythm is draining and leads to a dissatisfying, tired feeling. Be sure when selecting an EMR that the user experience is considered as important as functionality.
Billing statements. Write or print, fold, place in an envelope, put a stamp on the envelope, address the envelope, take it to the mailbox. Need more be said about how inefficient this is? Use your EMR, a biller, or billing software to send statements automatically.
Of course, make sure that any method that employs technology or outsourcing to a service has appropriate Health Insurance Portability and Accountability Act safeguards.
Nothing to lose but your chains
Although running a practice gives you some freedom in your schedule, with that comes the shackles of processing administrative tasks that accompany clinical care. Finding ways to handle them more efficiently leads to improved job satisfaction and more time for patient care. You and your patients will both benefit.
Disclosure
Dr. Braslow is the founder of Luminello.com.
How to prevent misuse of psychotropics among college students
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
What do >700 letters to a mass murderer tell us about the people who wrote them?
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
Do you practice sophisticated psychiatry? 10 Proposed foundations of advanced care
Some psychiatrists are rapid adopters of the latest discoveries. Others wait before they adopt new modalities and change their practice accordingly. Then, there are some—admittedly, a minority—who stubbornly persist in practicing exactly as they did 30 or 40 years ago when they completed residency.
What are the foundations of exemplary, advanced, brain-based psychiatric care?
Here are my 10 proposed tenets of excellence in psychiatric practice. They reflect superior assessment and management of patients as well as personal growth and contributions to the specialty.
Provide a complete medical assessment for every patient at the first lifetime psychiatric contact, whether inpatient or outpatient. This includes routine physical and neurologic examinations and a panel of basic laboratory tests (complete blood count, liver and kidney functions, urine screen, thyroid-stimulating hormone, electrolytes, fasting glucose, and fasting lipids). All vital signs are measured and recorded. Referrals to other medical specialists are made as needed.
This medical assessment must, of course, include a comprehensive psychiatric evaluation: personal history, social history, medical history, family history, and a complete neuropsychiatric mental status examination.
Create a thorough 3-generation pedigree of all relatives, indicating not only psychopathology, addiction, and legal problems but also medical (especially neurologic) disorders and cause of death.
Perform basic assessment of brain structure and function (a MRI scan, a neurocognitive battery, and tests of neurologic soft signs).
Measure biomarkers that reflect potential harm to the brain according to emerging research—eg, pro-inflammatory markers (such as C-reactive protein [CRP], interleukin-6, and tumor necrosis factor alpha [TNF-α]) and oxidative stress biomarkers of increased free radical activity (superoxide dismutase [SOD], glutathione, thiobarbituric acid [GSH] reactive substances [TBARS], and catalase).
Maintain measurement-based practice, in which:
• severity of illness is measured by a specific, appropriate rating scale (eg, Positive and Negative Syndrome Scale for schizophrenia [PANSS], Young Mania Rating Scale [YMRS], Montgomery-Åsberg Depression Rating Scale [MADRS] for depression, Hamilton Anxiety Rating Scale [HAM-A] for anxiety, Yale-Brown Obsessive Compulsive Scale [Y-BOCS] for obsessions and compulsions)
• degree of response to treatment is measured as a reflection of the extent of drop in the total score of those rating scales, which are administered at every visit
• severity of common side effects is measured by the Simpson-Angus Scale (SAS) for parkinsonism, the Barnes Akathisia Rating Scale (BARS), the Abnormal Involuntary Movement Scale (AIMS) for tardive dyskinesia, the Glasgow Antipsychotic Side-effect Scale (GASS), etc.
Use tier-1 evidence-based psychiatry (that is, findings from large, placebo-controlled, double-blind studies) to select best treatments. This includes being familiar with:
• principles of meta-analysis
• the meaning of low, medium, and large effect sizes
• for every medication used, the calculation and clinical implications of number needed to treat (NNT) and number needed to harm (NNH).
Always combine the dual management approaches of pharmacotherapy plus psychotherapy/psychosocial therapy.
Share knowledge and experience gleaned from practice with the community of psychiatrists, including:
• writing letters to the editor about a clinical matter
• submitting case reports or case series for publication
• teaching students or residents at the local medical school (after obtaining adjunct faculty status).
In addition, psychiatrists should educate the public to eliminate misperceptions and erase stigma about mental illness.
Participate in creating new psychiatric knowledge by developing skills to become a clinical trialist, so that you can participate as an investigator in multicenter clinical trials of new medications, or, at least, refer patients for possible participation in ongoing clinical trials conducted at local academic centers.
Engage in effective and continuous life-learning, by:
• attending weekly Grand Rounds at the nearest academic department of psychiatry
• attending national continuing medical education conferences annually
• scanning PubMed regularly (at least 3 times a week, if not daily) for the latest research related to one’s patients or to read about advances in one’s clinical subspecialty; read the abstracts and download several PDFs a week for subsequent reading.
Some readers will agree with part, but not all, of these proposed components of advanced psychiatric practice. That’s to be expected; I welcome your letters rebutting some tenets, or proposing additional ones, of a sophisticated psychiatric practice. After all, sophistication is a journey, not a destination.
Some psychiatrists are rapid adopters of the latest discoveries. Others wait before they adopt new modalities and change their practice accordingly. Then, there are some—admittedly, a minority—who stubbornly persist in practicing exactly as they did 30 or 40 years ago when they completed residency.
What are the foundations of exemplary, advanced, brain-based psychiatric care?
Here are my 10 proposed tenets of excellence in psychiatric practice. They reflect superior assessment and management of patients as well as personal growth and contributions to the specialty.
Provide a complete medical assessment for every patient at the first lifetime psychiatric contact, whether inpatient or outpatient. This includes routine physical and neurologic examinations and a panel of basic laboratory tests (complete blood count, liver and kidney functions, urine screen, thyroid-stimulating hormone, electrolytes, fasting glucose, and fasting lipids). All vital signs are measured and recorded. Referrals to other medical specialists are made as needed.
This medical assessment must, of course, include a comprehensive psychiatric evaluation: personal history, social history, medical history, family history, and a complete neuropsychiatric mental status examination.
Create a thorough 3-generation pedigree of all relatives, indicating not only psychopathology, addiction, and legal problems but also medical (especially neurologic) disorders and cause of death.
Perform basic assessment of brain structure and function (a MRI scan, a neurocognitive battery, and tests of neurologic soft signs).
Measure biomarkers that reflect potential harm to the brain according to emerging research—eg, pro-inflammatory markers (such as C-reactive protein [CRP], interleukin-6, and tumor necrosis factor alpha [TNF-α]) and oxidative stress biomarkers of increased free radical activity (superoxide dismutase [SOD], glutathione, thiobarbituric acid [GSH] reactive substances [TBARS], and catalase).
Maintain measurement-based practice, in which:
• severity of illness is measured by a specific, appropriate rating scale (eg, Positive and Negative Syndrome Scale for schizophrenia [PANSS], Young Mania Rating Scale [YMRS], Montgomery-Åsberg Depression Rating Scale [MADRS] for depression, Hamilton Anxiety Rating Scale [HAM-A] for anxiety, Yale-Brown Obsessive Compulsive Scale [Y-BOCS] for obsessions and compulsions)
• degree of response to treatment is measured as a reflection of the extent of drop in the total score of those rating scales, which are administered at every visit
• severity of common side effects is measured by the Simpson-Angus Scale (SAS) for parkinsonism, the Barnes Akathisia Rating Scale (BARS), the Abnormal Involuntary Movement Scale (AIMS) for tardive dyskinesia, the Glasgow Antipsychotic Side-effect Scale (GASS), etc.
Use tier-1 evidence-based psychiatry (that is, findings from large, placebo-controlled, double-blind studies) to select best treatments. This includes being familiar with:
• principles of meta-analysis
• the meaning of low, medium, and large effect sizes
• for every medication used, the calculation and clinical implications of number needed to treat (NNT) and number needed to harm (NNH).
Always combine the dual management approaches of pharmacotherapy plus psychotherapy/psychosocial therapy.
Share knowledge and experience gleaned from practice with the community of psychiatrists, including:
• writing letters to the editor about a clinical matter
• submitting case reports or case series for publication
• teaching students or residents at the local medical school (after obtaining adjunct faculty status).
In addition, psychiatrists should educate the public to eliminate misperceptions and erase stigma about mental illness.
Participate in creating new psychiatric knowledge by developing skills to become a clinical trialist, so that you can participate as an investigator in multicenter clinical trials of new medications, or, at least, refer patients for possible participation in ongoing clinical trials conducted at local academic centers.
Engage in effective and continuous life-learning, by:
• attending weekly Grand Rounds at the nearest academic department of psychiatry
• attending national continuing medical education conferences annually
• scanning PubMed regularly (at least 3 times a week, if not daily) for the latest research related to one’s patients or to read about advances in one’s clinical subspecialty; read the abstracts and download several PDFs a week for subsequent reading.
Some readers will agree with part, but not all, of these proposed components of advanced psychiatric practice. That’s to be expected; I welcome your letters rebutting some tenets, or proposing additional ones, of a sophisticated psychiatric practice. After all, sophistication is a journey, not a destination.
Some psychiatrists are rapid adopters of the latest discoveries. Others wait before they adopt new modalities and change their practice accordingly. Then, there are some—admittedly, a minority—who stubbornly persist in practicing exactly as they did 30 or 40 years ago when they completed residency.
What are the foundations of exemplary, advanced, brain-based psychiatric care?
Here are my 10 proposed tenets of excellence in psychiatric practice. They reflect superior assessment and management of patients as well as personal growth and contributions to the specialty.
Provide a complete medical assessment for every patient at the first lifetime psychiatric contact, whether inpatient or outpatient. This includes routine physical and neurologic examinations and a panel of basic laboratory tests (complete blood count, liver and kidney functions, urine screen, thyroid-stimulating hormone, electrolytes, fasting glucose, and fasting lipids). All vital signs are measured and recorded. Referrals to other medical specialists are made as needed.
This medical assessment must, of course, include a comprehensive psychiatric evaluation: personal history, social history, medical history, family history, and a complete neuropsychiatric mental status examination.
Create a thorough 3-generation pedigree of all relatives, indicating not only psychopathology, addiction, and legal problems but also medical (especially neurologic) disorders and cause of death.
Perform basic assessment of brain structure and function (a MRI scan, a neurocognitive battery, and tests of neurologic soft signs).
Measure biomarkers that reflect potential harm to the brain according to emerging research—eg, pro-inflammatory markers (such as C-reactive protein [CRP], interleukin-6, and tumor necrosis factor alpha [TNF-α]) and oxidative stress biomarkers of increased free radical activity (superoxide dismutase [SOD], glutathione, thiobarbituric acid [GSH] reactive substances [TBARS], and catalase).
Maintain measurement-based practice, in which:
• severity of illness is measured by a specific, appropriate rating scale (eg, Positive and Negative Syndrome Scale for schizophrenia [PANSS], Young Mania Rating Scale [YMRS], Montgomery-Åsberg Depression Rating Scale [MADRS] for depression, Hamilton Anxiety Rating Scale [HAM-A] for anxiety, Yale-Brown Obsessive Compulsive Scale [Y-BOCS] for obsessions and compulsions)
• degree of response to treatment is measured as a reflection of the extent of drop in the total score of those rating scales, which are administered at every visit
• severity of common side effects is measured by the Simpson-Angus Scale (SAS) for parkinsonism, the Barnes Akathisia Rating Scale (BARS), the Abnormal Involuntary Movement Scale (AIMS) for tardive dyskinesia, the Glasgow Antipsychotic Side-effect Scale (GASS), etc.
Use tier-1 evidence-based psychiatry (that is, findings from large, placebo-controlled, double-blind studies) to select best treatments. This includes being familiar with:
• principles of meta-analysis
• the meaning of low, medium, and large effect sizes
• for every medication used, the calculation and clinical implications of number needed to treat (NNT) and number needed to harm (NNH).
Always combine the dual management approaches of pharmacotherapy plus psychotherapy/psychosocial therapy.
Share knowledge and experience gleaned from practice with the community of psychiatrists, including:
• writing letters to the editor about a clinical matter
• submitting case reports or case series for publication
• teaching students or residents at the local medical school (after obtaining adjunct faculty status).
In addition, psychiatrists should educate the public to eliminate misperceptions and erase stigma about mental illness.
Participate in creating new psychiatric knowledge by developing skills to become a clinical trialist, so that you can participate as an investigator in multicenter clinical trials of new medications, or, at least, refer patients for possible participation in ongoing clinical trials conducted at local academic centers.
Engage in effective and continuous life-learning, by:
• attending weekly Grand Rounds at the nearest academic department of psychiatry
• attending national continuing medical education conferences annually
• scanning PubMed regularly (at least 3 times a week, if not daily) for the latest research related to one’s patients or to read about advances in one’s clinical subspecialty; read the abstracts and download several PDFs a week for subsequent reading.
Some readers will agree with part, but not all, of these proposed components of advanced psychiatric practice. That’s to be expected; I welcome your letters rebutting some tenets, or proposing additional ones, of a sophisticated psychiatric practice. After all, sophistication is a journey, not a destination.
For residents, technology can put professionalism and reputation at risk
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
Reducing the duration of untreated psychosis
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Collaborative care
Consider telehealth technology to perform reliable and valid cognitive screening
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.
Provide your patients with a DEFENSE against age-related cognitive decline
Psychiatric providers often encounter older adult patients who report difficulty with memory and express the fear they are “developing dementia.” Often, after a thorough evaluation of the reported deficits and history, we find that a serious or progressive neurocognitive disorder is unlikely. However, such occasions are an opportunity to discuss lifestyle changes that may help prevent, or at least slow, development of later-life cognitive decline.
Although I inform my patients that the body of evidence supporting many of these preventive measures still is evolving, I suggest the following approach that may provide a DEFENSE against future cognitive disability.
Diet options that are “heart healthy” seem to be “brain healthy” as well. This may be due, in part, to the antioxidant and anti-inflammatory effects of particular foods.1 Therefore, I suggest patients try to implement a Mediterranean-type diet that emphasizes fish (especially those rich in omega-3 fats, such as salmon and tuna), poultry, fresh fruit, and vegetables, as well as legumes.
ETOH has been shown, in a moderate amount (eg, 1 drink a day for women and 1 to 2 drinks for men), to be brain protective because of the antioxidants found in the alcohol or the direct relaxation effects that are produced—or both. Although red wine often is recommended, recent studies have shown that those who enjoyed an active life into their 70s and 80s had consumed a moderate amount of alcohol over their lifetime regardless of the type of spirit (eg, 12 oz of beer, 4 oz of wine, 1 oz of hard liquor).2
Friends contribute to an active, stimulating, and emotionally supported life. Having a strong social network, an antidote to loneliness and depression, has been shown to reduce the risk of “turning on” specific genes that stimulate an inflammatory process that can lead to brain cell death and neural damage.3
Exercise might be the most important ingredient for a longer, healthier, and more cognitively intact life. Moderate exercise, several times a week, increases blood flow to the brain and, subsequently, stimulates neuronal synapses and the hippocampus.4 The forms of exercise include walking, biking, swimming, resistance training, and even gardening.
No tobacco! It is known that smoking leads to accelerated aging for the heart and brain, so it is our responsibility to remain vigilant in promoting smoking cessation strategies.
Sleep has received increased attention, with recent studies providing evidence that the brain uses that time to “flush out” neurotoxic by-products of cognitive activity that have accumulated throughout the day.5 As evidence continues to be examined on this process, it is reasonable to recommend adequate sleep and a consistent sleep pattern as possible defenses against brain cell insult.
Engagement in tasks that are cognitively stimulating has been promoted as potential “brain exercises” to stave off future memory loss. For example, computer games that are mentally challenging; lively and frequent conversations; and learning a language all appear to increase neural activation and communication throughout the brain.6
As brain research continues to expand, providers will become more knowledgeable and aware of the steps our patients can take when they discuss concerns about their risk of progressive cognitive disability and memory loss. For now, however, it is important to describe what we do know based on current research and help our patients develop the best defense they can against age-related cognitive decline.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Gu Y, Nieves JW, Stern Y, et al. Food combination and Alzheimer disease risk: a protective diet. Arch Neurol. 2010;67(6):699-706.
2. Paganini-Hill A, Kawas CH, Corrada MM. Type of alcohol consumed, changes in intake over time, and mortality: the Leisure World Cohort Study. Age Ageing. 2007;36(2):203-209.
3. Cole SW, Hawkley LC, Arevelo JM, et al. Transcript origin analysis identifies antigen-presenting cells as primary targets of socially regulated gene expression in leukocytes. Proc Natl Acad Sci U S A. 2011;108(7):3080-3085.
4. Small G, Vorgan G. The Alzheimer’s Prevention Program: keep your brain healthy for the rest of your life. New York, NY: Workman Publishing Company, Inc; 2011:71.
5. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
6. Hall CB, Liptor RB, Sliwinski M, et al. Cognitive activities delay onset of memory decline in persons who develop dementia. Neurology. 2009;73(5):356-361.
Psychiatric providers often encounter older adult patients who report difficulty with memory and express the fear they are “developing dementia.” Often, after a thorough evaluation of the reported deficits and history, we find that a serious or progressive neurocognitive disorder is unlikely. However, such occasions are an opportunity to discuss lifestyle changes that may help prevent, or at least slow, development of later-life cognitive decline.
Although I inform my patients that the body of evidence supporting many of these preventive measures still is evolving, I suggest the following approach that may provide a DEFENSE against future cognitive disability.
Diet options that are “heart healthy” seem to be “brain healthy” as well. This may be due, in part, to the antioxidant and anti-inflammatory effects of particular foods.1 Therefore, I suggest patients try to implement a Mediterranean-type diet that emphasizes fish (especially those rich in omega-3 fats, such as salmon and tuna), poultry, fresh fruit, and vegetables, as well as legumes.
ETOH has been shown, in a moderate amount (eg, 1 drink a day for women and 1 to 2 drinks for men), to be brain protective because of the antioxidants found in the alcohol or the direct relaxation effects that are produced—or both. Although red wine often is recommended, recent studies have shown that those who enjoyed an active life into their 70s and 80s had consumed a moderate amount of alcohol over their lifetime regardless of the type of spirit (eg, 12 oz of beer, 4 oz of wine, 1 oz of hard liquor).2
Friends contribute to an active, stimulating, and emotionally supported life. Having a strong social network, an antidote to loneliness and depression, has been shown to reduce the risk of “turning on” specific genes that stimulate an inflammatory process that can lead to brain cell death and neural damage.3
Exercise might be the most important ingredient for a longer, healthier, and more cognitively intact life. Moderate exercise, several times a week, increases blood flow to the brain and, subsequently, stimulates neuronal synapses and the hippocampus.4 The forms of exercise include walking, biking, swimming, resistance training, and even gardening.
No tobacco! It is known that smoking leads to accelerated aging for the heart and brain, so it is our responsibility to remain vigilant in promoting smoking cessation strategies.
Sleep has received increased attention, with recent studies providing evidence that the brain uses that time to “flush out” neurotoxic by-products of cognitive activity that have accumulated throughout the day.5 As evidence continues to be examined on this process, it is reasonable to recommend adequate sleep and a consistent sleep pattern as possible defenses against brain cell insult.
Engagement in tasks that are cognitively stimulating has been promoted as potential “brain exercises” to stave off future memory loss. For example, computer games that are mentally challenging; lively and frequent conversations; and learning a language all appear to increase neural activation and communication throughout the brain.6
As brain research continues to expand, providers will become more knowledgeable and aware of the steps our patients can take when they discuss concerns about their risk of progressive cognitive disability and memory loss. For now, however, it is important to describe what we do know based on current research and help our patients develop the best defense they can against age-related cognitive decline.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychiatric providers often encounter older adult patients who report difficulty with memory and express the fear they are “developing dementia.” Often, after a thorough evaluation of the reported deficits and history, we find that a serious or progressive neurocognitive disorder is unlikely. However, such occasions are an opportunity to discuss lifestyle changes that may help prevent, or at least slow, development of later-life cognitive decline.
Although I inform my patients that the body of evidence supporting many of these preventive measures still is evolving, I suggest the following approach that may provide a DEFENSE against future cognitive disability.
Diet options that are “heart healthy” seem to be “brain healthy” as well. This may be due, in part, to the antioxidant and anti-inflammatory effects of particular foods.1 Therefore, I suggest patients try to implement a Mediterranean-type diet that emphasizes fish (especially those rich in omega-3 fats, such as salmon and tuna), poultry, fresh fruit, and vegetables, as well as legumes.
ETOH has been shown, in a moderate amount (eg, 1 drink a day for women and 1 to 2 drinks for men), to be brain protective because of the antioxidants found in the alcohol or the direct relaxation effects that are produced—or both. Although red wine often is recommended, recent studies have shown that those who enjoyed an active life into their 70s and 80s had consumed a moderate amount of alcohol over their lifetime regardless of the type of spirit (eg, 12 oz of beer, 4 oz of wine, 1 oz of hard liquor).2
Friends contribute to an active, stimulating, and emotionally supported life. Having a strong social network, an antidote to loneliness and depression, has been shown to reduce the risk of “turning on” specific genes that stimulate an inflammatory process that can lead to brain cell death and neural damage.3
Exercise might be the most important ingredient for a longer, healthier, and more cognitively intact life. Moderate exercise, several times a week, increases blood flow to the brain and, subsequently, stimulates neuronal synapses and the hippocampus.4 The forms of exercise include walking, biking, swimming, resistance training, and even gardening.
No tobacco! It is known that smoking leads to accelerated aging for the heart and brain, so it is our responsibility to remain vigilant in promoting smoking cessation strategies.
Sleep has received increased attention, with recent studies providing evidence that the brain uses that time to “flush out” neurotoxic by-products of cognitive activity that have accumulated throughout the day.5 As evidence continues to be examined on this process, it is reasonable to recommend adequate sleep and a consistent sleep pattern as possible defenses against brain cell insult.
Engagement in tasks that are cognitively stimulating has been promoted as potential “brain exercises” to stave off future memory loss. For example, computer games that are mentally challenging; lively and frequent conversations; and learning a language all appear to increase neural activation and communication throughout the brain.6
As brain research continues to expand, providers will become more knowledgeable and aware of the steps our patients can take when they discuss concerns about their risk of progressive cognitive disability and memory loss. For now, however, it is important to describe what we do know based on current research and help our patients develop the best defense they can against age-related cognitive decline.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Gu Y, Nieves JW, Stern Y, et al. Food combination and Alzheimer disease risk: a protective diet. Arch Neurol. 2010;67(6):699-706.
2. Paganini-Hill A, Kawas CH, Corrada MM. Type of alcohol consumed, changes in intake over time, and mortality: the Leisure World Cohort Study. Age Ageing. 2007;36(2):203-209.
3. Cole SW, Hawkley LC, Arevelo JM, et al. Transcript origin analysis identifies antigen-presenting cells as primary targets of socially regulated gene expression in leukocytes. Proc Natl Acad Sci U S A. 2011;108(7):3080-3085.
4. Small G, Vorgan G. The Alzheimer’s Prevention Program: keep your brain healthy for the rest of your life. New York, NY: Workman Publishing Company, Inc; 2011:71.
5. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
6. Hall CB, Liptor RB, Sliwinski M, et al. Cognitive activities delay onset of memory decline in persons who develop dementia. Neurology. 2009;73(5):356-361.
1. Gu Y, Nieves JW, Stern Y, et al. Food combination and Alzheimer disease risk: a protective diet. Arch Neurol. 2010;67(6):699-706.
2. Paganini-Hill A, Kawas CH, Corrada MM. Type of alcohol consumed, changes in intake over time, and mortality: the Leisure World Cohort Study. Age Ageing. 2007;36(2):203-209.
3. Cole SW, Hawkley LC, Arevelo JM, et al. Transcript origin analysis identifies antigen-presenting cells as primary targets of socially regulated gene expression in leukocytes. Proc Natl Acad Sci U S A. 2011;108(7):3080-3085.
4. Small G, Vorgan G. The Alzheimer’s Prevention Program: keep your brain healthy for the rest of your life. New York, NY: Workman Publishing Company, Inc; 2011:71.
5. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
6. Hall CB, Liptor RB, Sliwinski M, et al. Cognitive activities delay onset of memory decline in persons who develop dementia. Neurology. 2009;73(5):356-361.