User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Violent behavior in autism spectrum disorder: Is it a fact, or fiction?
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
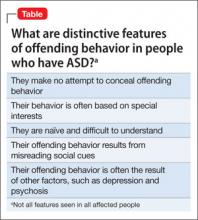
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
Problematic pruritus: Seeking a cure for psychogenic itch
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Managing geriatric bipolar disorder
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency room
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
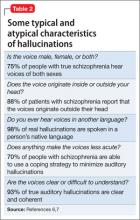
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
Lurasidone: classification and indications
The authors of “Atypical antipsychotics during pregnancy” (Current Psychiatry, July 2013, pp. 12-18) incorrectly state that all atypical antipsychotics are FDA Pregnancy Category C except for clozapine. In fact, lurasidone (Latuda) is FDA Pregnancy Category B. I was disappointed that the authors did not address this distinction; I find it puzzling why such a new medication, with such little data available, was able to obtain a FDA Pregnancy Category B label.
Laura Gilley, MD
Child and Adolescent Psychiatrist
Clinical Instructor
University of Utah
Salt Lake City, Utah
Drs. Robakis and Williams share clinically relevant information on an important issue in “Atypical antipsychotics during pregnancy.” For the most part, their information is current, but some facts need to be updated: Notably, olanzapine is now approved for use in the treatment of bipolar I disorder in children age 13 to 171 and paliperidone also is approved for the treatment of schizophrenia in children age 12 to 17.2
As we move forward with development of novel drugs, we will, I hope, create safer options for pregnant patients. Until then, clinically useful discussions of available evidence and risk/benefit analyses are greatly appreciated.
Deepak Prabhakar, MD, MPH
Attending Psychiatrist
Behavioral Health Services
Henry Ford Health System
Detroit, Michigan
References
1. Christian R, Saavedra L, Gaynes BN, et al. Future research needs for first- and second-generation antipsychotics for children and young adults. http://effectivehealthcare.ahrq.gov/ehc/products/147/835/CER39_Antipsychotics-Children-Young-Adults_20120221.pdf. Accessed August 13, 2012.
2. Invega {package insert}. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2013.
The authors of “Atypical antipsychotics during pregnancy” (Current Psychiatry, July 2013, pp. 12-18) incorrectly state that all atypical antipsychotics are FDA Pregnancy Category C except for clozapine. In fact, lurasidone (Latuda) is FDA Pregnancy Category B. I was disappointed that the authors did not address this distinction; I find it puzzling why such a new medication, with such little data available, was able to obtain a FDA Pregnancy Category B label.
Laura Gilley, MD
Child and Adolescent Psychiatrist
Clinical Instructor
University of Utah
Salt Lake City, Utah
Drs. Robakis and Williams share clinically relevant information on an important issue in “Atypical antipsychotics during pregnancy.” For the most part, their information is current, but some facts need to be updated: Notably, olanzapine is now approved for use in the treatment of bipolar I disorder in children age 13 to 171 and paliperidone also is approved for the treatment of schizophrenia in children age 12 to 17.2
As we move forward with development of novel drugs, we will, I hope, create safer options for pregnant patients. Until then, clinically useful discussions of available evidence and risk/benefit analyses are greatly appreciated.
Deepak Prabhakar, MD, MPH
Attending Psychiatrist
Behavioral Health Services
Henry Ford Health System
Detroit, Michigan
References
1. Christian R, Saavedra L, Gaynes BN, et al. Future research needs for first- and second-generation antipsychotics for children and young adults. http://effectivehealthcare.ahrq.gov/ehc/products/147/835/CER39_Antipsychotics-Children-Young-Adults_20120221.pdf. Accessed August 13, 2012.
2. Invega {package insert}. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2013.
The authors of “Atypical antipsychotics during pregnancy” (Current Psychiatry, July 2013, pp. 12-18) incorrectly state that all atypical antipsychotics are FDA Pregnancy Category C except for clozapine. In fact, lurasidone (Latuda) is FDA Pregnancy Category B. I was disappointed that the authors did not address this distinction; I find it puzzling why such a new medication, with such little data available, was able to obtain a FDA Pregnancy Category B label.
Laura Gilley, MD
Child and Adolescent Psychiatrist
Clinical Instructor
University of Utah
Salt Lake City, Utah
Drs. Robakis and Williams share clinically relevant information on an important issue in “Atypical antipsychotics during pregnancy.” For the most part, their information is current, but some facts need to be updated: Notably, olanzapine is now approved for use in the treatment of bipolar I disorder in children age 13 to 171 and paliperidone also is approved for the treatment of schizophrenia in children age 12 to 17.2
As we move forward with development of novel drugs, we will, I hope, create safer options for pregnant patients. Until then, clinically useful discussions of available evidence and risk/benefit analyses are greatly appreciated.
Deepak Prabhakar, MD, MPH
Attending Psychiatrist
Behavioral Health Services
Henry Ford Health System
Detroit, Michigan
References
1. Christian R, Saavedra L, Gaynes BN, et al. Future research needs for first- and second-generation antipsychotics for children and young adults. http://effectivehealthcare.ahrq.gov/ehc/products/147/835/CER39_Antipsychotics-Children-Young-Adults_20120221.pdf. Accessed August 13, 2012.
2. Invega {package insert}. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2013.
Should you report a patient who misuses a prescription?
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
A saga of psychiatric serendipities…
For a relatively young medical discipline like psychiatry, the history of discovery of biological therapeutics is replete with twists and turns, the pace of which will likely not abate. These discoveries can be initiated by both observant clinicians and dedicated researchers.
As I contemplated the scientific saga of developing somatic and pharmaceutical treatments for major psychiatric disorders, I recognized several interesting themes: serendipity, evolution, paradigm shifts, and radical breakthroughs. Consider the following examples of those themes.
Neuromodulation
Electroconvulsive therapy (ECT), the original neuromodulation therapy, was discovered (serendipity) when Meduna, mistakenly thinking that schizophrenia and epilepsy are “antagonistic,” used camphor and, later, metrazol, to induce seizures to treat schizophrenia. Later, Cerletti and Bini switched the seizure induction to electricity (evolution), and the use of ECT spread, like a seizure, around the world after their initial report. Later, unilateral ECT and pulse wave ECT were developed to reduce the incidence of side effects (further evolution).
In contemporary psychiatry, a paradigm shift in neuromodulation techniques has emerged over the past decade with the development of an array of novel neuromodulation techniques,1 some of which do not induce seizures or touch the scalp with electrodes—or even use electricity. These techniques include vagus nerve stimulation, repetitive transcranial magnetic stimulation, epidural cortical stimulation, focused ultrasound, low-field magnetic stimulation, transcranial direct current stimulation, and magnetic seizure therapy. Currently (pun intended!), radical breakthroughs with significant therapeutic promise are being developed, such as optogenetic stimulation and deep brain stimulation.
Antipsychotics
One of the most momentous serendipitous discoveries in psychiatry (one that should have won the Nobel Prize in Medicine or Physiology, like the discovery of penicillin) was the phenothiazine drug chlorpromazine, first used as an adjunct to surgical anesthesia in the late 1940s and early 1950s.2 Chlorpromazine eliminated psychotic symptoms in many patients (refuting centuries of dogma that madness is irreversible), led to
deinstitutionalization and community care of patients who suffer a serious psychiatric disorder, and reduced psychiatric beds from 50% of all hospital beds in the United States to about 5% today. Numerous phenothiazines were developed (evolution) followed by six non-phenothiazine classes (paradigm shift).
Another truly felicitous serendipity was the discovery of the first atypical antipsychotic, clozapine (synthesized in 1959, the same year that the antipsychotic thioridazine [Mellaril] was synthesized), which was initially shelved because it did not cause extrapyramidal symptoms (EPS); at the time, EPS were erroneously thought to be indispensable for antipsychotic efficacy! The discovery of clozapine led to the development of the nine atypical antipsychotics that have largely replaced the first-generation agents (paradigm shift) and that mimic clozapine’s far stronger binding of serotonin 5-HT2A receptors than binding of dopamine D2 receptors, thus reducing the occurrence of neurologic movement disorders (ie, EPS).
Clozapine led to a radical breakthrough when it proved to have efficacy in schizophrenia that is refractory to first-generation antipsychotics (the CATIE study showed the same efficacy for second-generation antipsychotics). A follow-up breakthrough was the
discovery of the efficacy of clozapine on suicidality, a significant cause of mortality in patients with schizophrenia.
A recently reported treatment for schizophrenia might be a potentially radical breakthrough. In a pilot study, researchers reported very rapid and significant improvement in positive and negative symptoms (and even anxiety and depressive symptoms, and within 4 hours and persisting for 4 weeks!3), using the antihypertensive sodium nitroprusside, administered IV. Here is another paradigm shift—in drug delivery, similar to what was seen with IV ketamine, which led to a radical breakthrough in treating drug-resistant depression.
Interestingly, the N-methyl-d-aspartate (NMDA) receptor is playing a key role in radical breakthroughs in schizophrenia and depression. A glycine transporter I inhibitor (which potentiates what is strongly suspected to be a hypofunctional NMDA receptor in schizophrenia) is undergoing further study for the treatment of negative and residual symptoms of schizophrenia, after a promising initial trial. This promises to be a radical breakthrough in addressing a major unmet need in psychiatry: treating negative symptoms of schizophrenia.
Antidepressants
Serendipity played a role in the discovery of the first antidepressant, iproniazid, a monoamine oxidase inhibitor (MAOI) that was used to treat tuberculosis in the 1940s and 1950s; medical staff in sanitariums noticed that the drug elevated the mood of depressed tuberculosis patients. Several other clinically useful MAOIs were then developed (evolution).
When the first tricyclic antidepressant (TCA), imipramine, was synthesized, it was intended to be an antipsychotic but—serendipitously—turned out to be a strong antidepressant. A paradigm shift from MAOIs to TCAs then occurred through the 1970s and 1980s, prompted by concerns over adverse effects caused by the interaction of MAOIs and foods that contain tyramine.
A mechanistic breakthrough occurred when the first selective serotonin reuptake inhibitor (SSRI), fluoxetine, was developed in the late 1980s, followed soon by several other SSRIs (evolution). This triggered another massive paradigm shift away from TCAs to SSRIs because of the low cardiotoxicity of SSRIs.
Evolution then led to the development of other heterocyclic antidepressants, such as nefazodone, mirtazapine, venlafaxine, and duloxetine.
The recent exciting (pun intended again!) discovery of the efficacy of the glutamate NMDA receptor-antagonist ketamine for severe, treatment-resistant depression represents a radical breakthrough in the rapidity of remission (within 1 or 2 hours of IV administration) of depression and suicidal impulses. Until now, such rapid response was believed unattainable.
The ketamine treatment model also rep- resents several paradigm shifts: from mono- amines to glutamate; from the oral route to the IV route; from gradual (6 to 8 weeks) to abrupt (1 or 2 hours) resolution of symptoms; and from neurochemistry (monoamine neurotransmitters) to neuroplasticity (mammalian target of rapapmycin [mTOR] and brain- derived neurotrophic factor [BDNF]).
The saga will go on
Explosive growth in molecular neuroscience and deeper understanding of the pathophysiology of major psychiatric disorders bode well for an accelerating pace of radical breakthroughs in psychiatric therapies. The new revelation that symptoms of chronic neuropsychiatric disorders such as depression, mania, and schizophrenia can be re- versed within a few hours, instead of weeks, months, or years, is jubilant news for our long-suffering patients.
But even as science-driven breakthroughs accelerate and prompt paradigm shifts in treatment, we should never under-estimate the importance and value of serendipity in generating new insights that lead to the same transformative paradigm shifts in therapeutics. Scientists are equipped to make discoveries that are breakthroughs, but observant clinicians can make serendipitous discoveries that may reinvent the care of psychotic disorders. The discovery of psychiatric therapies can begin in a clinical setting—not just in the ivory tower of academia.
1. Nasrallah HA, Tandon R. Classic antipsychotic medications. In: Schatzberg AI, Nemeroff CB, eds. Essentials of clinical psychopharmacology, 3rd ed. Arlington, VA: American Psychiatric Publishing Inc.; 2013:219-236.
2. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
3. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al: Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside. A randomized, double- blind, placebo-controlled trial. JAMA Psychiatry. 2013; 70(7):668-676.
For a relatively young medical discipline like psychiatry, the history of discovery of biological therapeutics is replete with twists and turns, the pace of which will likely not abate. These discoveries can be initiated by both observant clinicians and dedicated researchers.
As I contemplated the scientific saga of developing somatic and pharmaceutical treatments for major psychiatric disorders, I recognized several interesting themes: serendipity, evolution, paradigm shifts, and radical breakthroughs. Consider the following examples of those themes.
Neuromodulation
Electroconvulsive therapy (ECT), the original neuromodulation therapy, was discovered (serendipity) when Meduna, mistakenly thinking that schizophrenia and epilepsy are “antagonistic,” used camphor and, later, metrazol, to induce seizures to treat schizophrenia. Later, Cerletti and Bini switched the seizure induction to electricity (evolution), and the use of ECT spread, like a seizure, around the world after their initial report. Later, unilateral ECT and pulse wave ECT were developed to reduce the incidence of side effects (further evolution).
In contemporary psychiatry, a paradigm shift in neuromodulation techniques has emerged over the past decade with the development of an array of novel neuromodulation techniques,1 some of which do not induce seizures or touch the scalp with electrodes—or even use electricity. These techniques include vagus nerve stimulation, repetitive transcranial magnetic stimulation, epidural cortical stimulation, focused ultrasound, low-field magnetic stimulation, transcranial direct current stimulation, and magnetic seizure therapy. Currently (pun intended!), radical breakthroughs with significant therapeutic promise are being developed, such as optogenetic stimulation and deep brain stimulation.
Antipsychotics
One of the most momentous serendipitous discoveries in psychiatry (one that should have won the Nobel Prize in Medicine or Physiology, like the discovery of penicillin) was the phenothiazine drug chlorpromazine, first used as an adjunct to surgical anesthesia in the late 1940s and early 1950s.2 Chlorpromazine eliminated psychotic symptoms in many patients (refuting centuries of dogma that madness is irreversible), led to
deinstitutionalization and community care of patients who suffer a serious psychiatric disorder, and reduced psychiatric beds from 50% of all hospital beds in the United States to about 5% today. Numerous phenothiazines were developed (evolution) followed by six non-phenothiazine classes (paradigm shift).
Another truly felicitous serendipity was the discovery of the first atypical antipsychotic, clozapine (synthesized in 1959, the same year that the antipsychotic thioridazine [Mellaril] was synthesized), which was initially shelved because it did not cause extrapyramidal symptoms (EPS); at the time, EPS were erroneously thought to be indispensable for antipsychotic efficacy! The discovery of clozapine led to the development of the nine atypical antipsychotics that have largely replaced the first-generation agents (paradigm shift) and that mimic clozapine’s far stronger binding of serotonin 5-HT2A receptors than binding of dopamine D2 receptors, thus reducing the occurrence of neurologic movement disorders (ie, EPS).
Clozapine led to a radical breakthrough when it proved to have efficacy in schizophrenia that is refractory to first-generation antipsychotics (the CATIE study showed the same efficacy for second-generation antipsychotics). A follow-up breakthrough was the
discovery of the efficacy of clozapine on suicidality, a significant cause of mortality in patients with schizophrenia.
A recently reported treatment for schizophrenia might be a potentially radical breakthrough. In a pilot study, researchers reported very rapid and significant improvement in positive and negative symptoms (and even anxiety and depressive symptoms, and within 4 hours and persisting for 4 weeks!3), using the antihypertensive sodium nitroprusside, administered IV. Here is another paradigm shift—in drug delivery, similar to what was seen with IV ketamine, which led to a radical breakthrough in treating drug-resistant depression.
Interestingly, the N-methyl-d-aspartate (NMDA) receptor is playing a key role in radical breakthroughs in schizophrenia and depression. A glycine transporter I inhibitor (which potentiates what is strongly suspected to be a hypofunctional NMDA receptor in schizophrenia) is undergoing further study for the treatment of negative and residual symptoms of schizophrenia, after a promising initial trial. This promises to be a radical breakthrough in addressing a major unmet need in psychiatry: treating negative symptoms of schizophrenia.
Antidepressants
Serendipity played a role in the discovery of the first antidepressant, iproniazid, a monoamine oxidase inhibitor (MAOI) that was used to treat tuberculosis in the 1940s and 1950s; medical staff in sanitariums noticed that the drug elevated the mood of depressed tuberculosis patients. Several other clinically useful MAOIs were then developed (evolution).
When the first tricyclic antidepressant (TCA), imipramine, was synthesized, it was intended to be an antipsychotic but—serendipitously—turned out to be a strong antidepressant. A paradigm shift from MAOIs to TCAs then occurred through the 1970s and 1980s, prompted by concerns over adverse effects caused by the interaction of MAOIs and foods that contain tyramine.
A mechanistic breakthrough occurred when the first selective serotonin reuptake inhibitor (SSRI), fluoxetine, was developed in the late 1980s, followed soon by several other SSRIs (evolution). This triggered another massive paradigm shift away from TCAs to SSRIs because of the low cardiotoxicity of SSRIs.
Evolution then led to the development of other heterocyclic antidepressants, such as nefazodone, mirtazapine, venlafaxine, and duloxetine.
The recent exciting (pun intended again!) discovery of the efficacy of the glutamate NMDA receptor-antagonist ketamine for severe, treatment-resistant depression represents a radical breakthrough in the rapidity of remission (within 1 or 2 hours of IV administration) of depression and suicidal impulses. Until now, such rapid response was believed unattainable.
The ketamine treatment model also rep- resents several paradigm shifts: from mono- amines to glutamate; from the oral route to the IV route; from gradual (6 to 8 weeks) to abrupt (1 or 2 hours) resolution of symptoms; and from neurochemistry (monoamine neurotransmitters) to neuroplasticity (mammalian target of rapapmycin [mTOR] and brain- derived neurotrophic factor [BDNF]).
The saga will go on
Explosive growth in molecular neuroscience and deeper understanding of the pathophysiology of major psychiatric disorders bode well for an accelerating pace of radical breakthroughs in psychiatric therapies. The new revelation that symptoms of chronic neuropsychiatric disorders such as depression, mania, and schizophrenia can be re- versed within a few hours, instead of weeks, months, or years, is jubilant news for our long-suffering patients.
But even as science-driven breakthroughs accelerate and prompt paradigm shifts in treatment, we should never under-estimate the importance and value of serendipity in generating new insights that lead to the same transformative paradigm shifts in therapeutics. Scientists are equipped to make discoveries that are breakthroughs, but observant clinicians can make serendipitous discoveries that may reinvent the care of psychotic disorders. The discovery of psychiatric therapies can begin in a clinical setting—not just in the ivory tower of academia.
For a relatively young medical discipline like psychiatry, the history of discovery of biological therapeutics is replete with twists and turns, the pace of which will likely not abate. These discoveries can be initiated by both observant clinicians and dedicated researchers.
As I contemplated the scientific saga of developing somatic and pharmaceutical treatments for major psychiatric disorders, I recognized several interesting themes: serendipity, evolution, paradigm shifts, and radical breakthroughs. Consider the following examples of those themes.
Neuromodulation
Electroconvulsive therapy (ECT), the original neuromodulation therapy, was discovered (serendipity) when Meduna, mistakenly thinking that schizophrenia and epilepsy are “antagonistic,” used camphor and, later, metrazol, to induce seizures to treat schizophrenia. Later, Cerletti and Bini switched the seizure induction to electricity (evolution), and the use of ECT spread, like a seizure, around the world after their initial report. Later, unilateral ECT and pulse wave ECT were developed to reduce the incidence of side effects (further evolution).
In contemporary psychiatry, a paradigm shift in neuromodulation techniques has emerged over the past decade with the development of an array of novel neuromodulation techniques,1 some of which do not induce seizures or touch the scalp with electrodes—or even use electricity. These techniques include vagus nerve stimulation, repetitive transcranial magnetic stimulation, epidural cortical stimulation, focused ultrasound, low-field magnetic stimulation, transcranial direct current stimulation, and magnetic seizure therapy. Currently (pun intended!), radical breakthroughs with significant therapeutic promise are being developed, such as optogenetic stimulation and deep brain stimulation.
Antipsychotics
One of the most momentous serendipitous discoveries in psychiatry (one that should have won the Nobel Prize in Medicine or Physiology, like the discovery of penicillin) was the phenothiazine drug chlorpromazine, first used as an adjunct to surgical anesthesia in the late 1940s and early 1950s.2 Chlorpromazine eliminated psychotic symptoms in many patients (refuting centuries of dogma that madness is irreversible), led to
deinstitutionalization and community care of patients who suffer a serious psychiatric disorder, and reduced psychiatric beds from 50% of all hospital beds in the United States to about 5% today. Numerous phenothiazines were developed (evolution) followed by six non-phenothiazine classes (paradigm shift).
Another truly felicitous serendipity was the discovery of the first atypical antipsychotic, clozapine (synthesized in 1959, the same year that the antipsychotic thioridazine [Mellaril] was synthesized), which was initially shelved because it did not cause extrapyramidal symptoms (EPS); at the time, EPS were erroneously thought to be indispensable for antipsychotic efficacy! The discovery of clozapine led to the development of the nine atypical antipsychotics that have largely replaced the first-generation agents (paradigm shift) and that mimic clozapine’s far stronger binding of serotonin 5-HT2A receptors than binding of dopamine D2 receptors, thus reducing the occurrence of neurologic movement disorders (ie, EPS).
Clozapine led to a radical breakthrough when it proved to have efficacy in schizophrenia that is refractory to first-generation antipsychotics (the CATIE study showed the same efficacy for second-generation antipsychotics). A follow-up breakthrough was the
discovery of the efficacy of clozapine on suicidality, a significant cause of mortality in patients with schizophrenia.
A recently reported treatment for schizophrenia might be a potentially radical breakthrough. In a pilot study, researchers reported very rapid and significant improvement in positive and negative symptoms (and even anxiety and depressive symptoms, and within 4 hours and persisting for 4 weeks!3), using the antihypertensive sodium nitroprusside, administered IV. Here is another paradigm shift—in drug delivery, similar to what was seen with IV ketamine, which led to a radical breakthrough in treating drug-resistant depression.
Interestingly, the N-methyl-d-aspartate (NMDA) receptor is playing a key role in radical breakthroughs in schizophrenia and depression. A glycine transporter I inhibitor (which potentiates what is strongly suspected to be a hypofunctional NMDA receptor in schizophrenia) is undergoing further study for the treatment of negative and residual symptoms of schizophrenia, after a promising initial trial. This promises to be a radical breakthrough in addressing a major unmet need in psychiatry: treating negative symptoms of schizophrenia.
Antidepressants
Serendipity played a role in the discovery of the first antidepressant, iproniazid, a monoamine oxidase inhibitor (MAOI) that was used to treat tuberculosis in the 1940s and 1950s; medical staff in sanitariums noticed that the drug elevated the mood of depressed tuberculosis patients. Several other clinically useful MAOIs were then developed (evolution).
When the first tricyclic antidepressant (TCA), imipramine, was synthesized, it was intended to be an antipsychotic but—serendipitously—turned out to be a strong antidepressant. A paradigm shift from MAOIs to TCAs then occurred through the 1970s and 1980s, prompted by concerns over adverse effects caused by the interaction of MAOIs and foods that contain tyramine.
A mechanistic breakthrough occurred when the first selective serotonin reuptake inhibitor (SSRI), fluoxetine, was developed in the late 1980s, followed soon by several other SSRIs (evolution). This triggered another massive paradigm shift away from TCAs to SSRIs because of the low cardiotoxicity of SSRIs.
Evolution then led to the development of other heterocyclic antidepressants, such as nefazodone, mirtazapine, venlafaxine, and duloxetine.
The recent exciting (pun intended again!) discovery of the efficacy of the glutamate NMDA receptor-antagonist ketamine for severe, treatment-resistant depression represents a radical breakthrough in the rapidity of remission (within 1 or 2 hours of IV administration) of depression and suicidal impulses. Until now, such rapid response was believed unattainable.
The ketamine treatment model also rep- resents several paradigm shifts: from mono- amines to glutamate; from the oral route to the IV route; from gradual (6 to 8 weeks) to abrupt (1 or 2 hours) resolution of symptoms; and from neurochemistry (monoamine neurotransmitters) to neuroplasticity (mammalian target of rapapmycin [mTOR] and brain- derived neurotrophic factor [BDNF]).
The saga will go on
Explosive growth in molecular neuroscience and deeper understanding of the pathophysiology of major psychiatric disorders bode well for an accelerating pace of radical breakthroughs in psychiatric therapies. The new revelation that symptoms of chronic neuropsychiatric disorders such as depression, mania, and schizophrenia can be re- versed within a few hours, instead of weeks, months, or years, is jubilant news for our long-suffering patients.
But even as science-driven breakthroughs accelerate and prompt paradigm shifts in treatment, we should never under-estimate the importance and value of serendipity in generating new insights that lead to the same transformative paradigm shifts in therapeutics. Scientists are equipped to make discoveries that are breakthroughs, but observant clinicians can make serendipitous discoveries that may reinvent the care of psychotic disorders. The discovery of psychiatric therapies can begin in a clinical setting—not just in the ivory tower of academia.
1. Nasrallah HA, Tandon R. Classic antipsychotic medications. In: Schatzberg AI, Nemeroff CB, eds. Essentials of clinical psychopharmacology, 3rd ed. Arlington, VA: American Psychiatric Publishing Inc.; 2013:219-236.
2. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
3. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al: Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside. A randomized, double- blind, placebo-controlled trial. JAMA Psychiatry. 2013; 70(7):668-676.
1. Nasrallah HA, Tandon R. Classic antipsychotic medications. In: Schatzberg AI, Nemeroff CB, eds. Essentials of clinical psychopharmacology, 3rd ed. Arlington, VA: American Psychiatric Publishing Inc.; 2013:219-236.
2. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
3. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al: Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside. A randomized, double- blind, placebo-controlled trial. JAMA Psychiatry. 2013; 70(7):668-676.
How best to engage patients in their psychiatric care
Familiarizing yourself with Alcoholics Anonymous dictums
From “90 minutes in 90 days,” to “people, places, and things,” to “cucumbers and pickles,” Alcoholics Anonymous (AA) slogans have been influencing the public’s understanding of the addictive process for almost a century. Regrettably, these terms have, inadvertently, alienated the scientific community. The translation and subsequent use of AA slogans has been a valuable tool in engaging science experts with mutual-help fellowships such as AA.
Recent advances in the neurobiology and neurochemistry of addiction have validated several of the memorable sayings of AA.1 As a result, physicians and scientists are now more willing to explore AA’s mottos.
Here are five well-known AA slogans that we have translated into medical terms and then briefly assessed in terms of their validity and relevance in today’s treatment of alcohol addiction:
1. “90 meetings in 90 days”
TRUE! Clinically, the first three months of sobriety constitute the most severe part of prolonged withdrawal syndrome and pose the most dangerous opportunities for a relapse.
2. “Keep it simple”
NOT TRUE! Clinical research and everyday practice of addiction treatment show that combination approaches—with medications, group psychotherapy, individual psychotherapy, involvement in mutual-help groups, family therapy, primary care, and treatment of psychiatric comorbidities—typically result in better outcomes than singular approaches.2
3. “Denial is not just a river in Egypt”
NOT TRUE! Since motivational inter-viewing was introduced in the treatment of addiction, we have learned how to effectively work with patients who are in complete denial and have absolutely no interest in changing anything about their life.3
4. “Beware of people, places, and things”
TRUE! Otherwise known as “cues” in psychology literature, triggers of relapse have been implicated in both the basic understanding of the addictive process and its treatment. “Classical conditioning” and “operant conditioning” models of behavior incorporate triggers. Additionally, cognitive behavior therapy helps extensively with maintaining sobriety. Even the DSM-5 gives a nod to “people, places, and things” by introducing “cravings” as a bona fide criterion of a substance use disorder.
5. “A cucumber that has become a pickle cannot become a cucumber again”
EQUIVOCAL. It is not clear, and highly debatable, whether an alcoholic who has been sober for more than 20 years still has a heightened vulnerability to reverting to alcoholism after consumption of alcohol. What is evident is that, even if the neuroadaptations responsible for hijacking the pleasure-reward pathways of the brain one day return to a normal, pre-addiction state, this healing process takes a long time—probably measured in decades, not years.
Click here for another Pearl on alternatives to 12-step groups.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Volkow ND, Baler RD. Addiction science: Uncovering neurobiological complexity. Neuropharmacology. 2013; (13)217-7.
2. Nunes EV, Selzer J, Levounis P, et al. Substance dependence and co-occurring psychiatric disorders: Best practices for diagnosis and clinical treatment. New York, NY: Civic Research Institute, 2010.
3. Levounis, P, Arnaout B. Handbook of motivation and change: A practical guide for clinicians. Arlington, VA: American Psychiatric Publishing, Inc.; 2010.
From “90 minutes in 90 days,” to “people, places, and things,” to “cucumbers and pickles,” Alcoholics Anonymous (AA) slogans have been influencing the public’s understanding of the addictive process for almost a century. Regrettably, these terms have, inadvertently, alienated the scientific community. The translation and subsequent use of AA slogans has been a valuable tool in engaging science experts with mutual-help fellowships such as AA.
Recent advances in the neurobiology and neurochemistry of addiction have validated several of the memorable sayings of AA.1 As a result, physicians and scientists are now more willing to explore AA’s mottos.
Here are five well-known AA slogans that we have translated into medical terms and then briefly assessed in terms of their validity and relevance in today’s treatment of alcohol addiction:
1. “90 meetings in 90 days”
TRUE! Clinically, the first three months of sobriety constitute the most severe part of prolonged withdrawal syndrome and pose the most dangerous opportunities for a relapse.
2. “Keep it simple”
NOT TRUE! Clinical research and everyday practice of addiction treatment show that combination approaches—with medications, group psychotherapy, individual psychotherapy, involvement in mutual-help groups, family therapy, primary care, and treatment of psychiatric comorbidities—typically result in better outcomes than singular approaches.2
3. “Denial is not just a river in Egypt”
NOT TRUE! Since motivational inter-viewing was introduced in the treatment of addiction, we have learned how to effectively work with patients who are in complete denial and have absolutely no interest in changing anything about their life.3
4. “Beware of people, places, and things”
TRUE! Otherwise known as “cues” in psychology literature, triggers of relapse have been implicated in both the basic understanding of the addictive process and its treatment. “Classical conditioning” and “operant conditioning” models of behavior incorporate triggers. Additionally, cognitive behavior therapy helps extensively with maintaining sobriety. Even the DSM-5 gives a nod to “people, places, and things” by introducing “cravings” as a bona fide criterion of a substance use disorder.
5. “A cucumber that has become a pickle cannot become a cucumber again”
EQUIVOCAL. It is not clear, and highly debatable, whether an alcoholic who has been sober for more than 20 years still has a heightened vulnerability to reverting to alcoholism after consumption of alcohol. What is evident is that, even if the neuroadaptations responsible for hijacking the pleasure-reward pathways of the brain one day return to a normal, pre-addiction state, this healing process takes a long time—probably measured in decades, not years.
Click here for another Pearl on alternatives to 12-step groups.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
From “90 minutes in 90 days,” to “people, places, and things,” to “cucumbers and pickles,” Alcoholics Anonymous (AA) slogans have been influencing the public’s understanding of the addictive process for almost a century. Regrettably, these terms have, inadvertently, alienated the scientific community. The translation and subsequent use of AA slogans has been a valuable tool in engaging science experts with mutual-help fellowships such as AA.
Recent advances in the neurobiology and neurochemistry of addiction have validated several of the memorable sayings of AA.1 As a result, physicians and scientists are now more willing to explore AA’s mottos.
Here are five well-known AA slogans that we have translated into medical terms and then briefly assessed in terms of their validity and relevance in today’s treatment of alcohol addiction:
1. “90 meetings in 90 days”
TRUE! Clinically, the first three months of sobriety constitute the most severe part of prolonged withdrawal syndrome and pose the most dangerous opportunities for a relapse.
2. “Keep it simple”
NOT TRUE! Clinical research and everyday practice of addiction treatment show that combination approaches—with medications, group psychotherapy, individual psychotherapy, involvement in mutual-help groups, family therapy, primary care, and treatment of psychiatric comorbidities—typically result in better outcomes than singular approaches.2
3. “Denial is not just a river in Egypt”
NOT TRUE! Since motivational inter-viewing was introduced in the treatment of addiction, we have learned how to effectively work with patients who are in complete denial and have absolutely no interest in changing anything about their life.3
4. “Beware of people, places, and things”
TRUE! Otherwise known as “cues” in psychology literature, triggers of relapse have been implicated in both the basic understanding of the addictive process and its treatment. “Classical conditioning” and “operant conditioning” models of behavior incorporate triggers. Additionally, cognitive behavior therapy helps extensively with maintaining sobriety. Even the DSM-5 gives a nod to “people, places, and things” by introducing “cravings” as a bona fide criterion of a substance use disorder.
5. “A cucumber that has become a pickle cannot become a cucumber again”
EQUIVOCAL. It is not clear, and highly debatable, whether an alcoholic who has been sober for more than 20 years still has a heightened vulnerability to reverting to alcoholism after consumption of alcohol. What is evident is that, even if the neuroadaptations responsible for hijacking the pleasure-reward pathways of the brain one day return to a normal, pre-addiction state, this healing process takes a long time—probably measured in decades, not years.
Click here for another Pearl on alternatives to 12-step groups.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Volkow ND, Baler RD. Addiction science: Uncovering neurobiological complexity. Neuropharmacology. 2013; (13)217-7.
2. Nunes EV, Selzer J, Levounis P, et al. Substance dependence and co-occurring psychiatric disorders: Best practices for diagnosis and clinical treatment. New York, NY: Civic Research Institute, 2010.
3. Levounis, P, Arnaout B. Handbook of motivation and change: A practical guide for clinicians. Arlington, VA: American Psychiatric Publishing, Inc.; 2010.
1. Volkow ND, Baler RD. Addiction science: Uncovering neurobiological complexity. Neuropharmacology. 2013; (13)217-7.
2. Nunes EV, Selzer J, Levounis P, et al. Substance dependence and co-occurring psychiatric disorders: Best practices for diagnosis and clinical treatment. New York, NY: Civic Research Institute, 2010.
3. Levounis, P, Arnaout B. Handbook of motivation and change: A practical guide for clinicians. Arlington, VA: American Psychiatric Publishing, Inc.; 2010.
Investigational treatments for cognitive impairment in schizophrenia
Available treatments for schizophrenia (eg, antipsychotics) are primarily effective on positive symptoms (hallucinations, delusions, etc.). It is, however, increasingly clear that schizophrenia also is a severe neuropsychiatric illness associated with deficits in cognitive function. These deficits represent a core feature of the disorder, and are a major determinant of long-term disability.1 Cognitive dysfunction is among the earliest signs of illness that, typically, presents in the prodromal phase.
Since the formulation of the dopaminergic model of schizophrenia, cognitive studies of the disease primarily have examined dysfunction in dopaminergic-rich regions of the brain, such as the prefrontal cortex, and, therefore, have focused largely on executive functioning. But neurocognitive deficits in schizophrenia are not limited to executive functioning; comparable deficits have been observed across multiple areas of cognition.2
More recent formulations of cognitive dysfunction in schizophrenia divide deficits into multiple domains. These include verbal, visual, and working memory; attention and vigilance; speed of processing, reasoning, and problem solving; and social cognition (Table). Neurocognitive impairments often are closely associated with deficits in early sensory processing and basic neurophysiology.3
The prevalence of cognitive dysfunction also can be estimated using baseline data from the large-scale Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) trial.4 Although cognitive dysfunction was not one of the inclusion criteria in CATIE, most patients who were enrolled had profound cognitive deficits.5 Furthermore, meta-analyses6 suggest that composite neurocognitive measures can explain as much as 60% of the variance of overall functioning in schizophrenia.
Antipsychotics aren’t the answer
The cognitive-enhancing benefits of antipsychotic medications are minimal.7 As evidence of a direct relationship between cognitive dysfunction and long-term functional outcome in schizophrenia becomes established, the need for safe and effective treatment for these symptoms becomes more urgent. Given the mechanistic complexity of the potential cause of poor cognitive performance, the search for an effective treatment is ongoing—but that search has not been successful.
Despite mixed results for recent novel mechanism trials (http://newsroom.lilly.com/releasedetail.cfm?releaseid=703018) and a number of companies ceasing drug development, the work to develop safe and effective treatments for cognitive dysfunction in schizophrenia continues, as exemplified by National Institute of Mental Health-initiated programs to spur development of drugs that work by a novel mechanism. Rather than simply assessing novel compounds with paper-and-pencil cognitive scales, such programs seek to assess the ability of the compound to engage with the intended receptor (target),9 using imaging or electrophysiological tools. Without utilization of a target engagement biomarker, there is no way to know whether 1) the drug simply does not get into the brain in sufficient concentration to be effective in humans or 2) the overall mechanism is wrong.
In this article, we review several promising targets and techniques that are the subject of active research on the treatment of cognitive disorders in schizophrenia. This list isn’t exhaustive; our aim is to highlight a few of the promising treatments now being studied in clinical trials.
Acetylcholine receptors
Acetylcholine receptors comprise two major families, nicotinic and muscarinic receptors; evidence implicates deficits of both families in schizophrenia.10 Following up on epidemiological studies11 of the high percentage of schizophrenia patients who smoke tobacco (60% to 90%), the role of alpha-7 nicotinic acetylcholine receptors (á7 nAchR) has been explored. Nicotine itself might normalize some disrupted auditory processes, as measured by electroencephalography.12
Several clinical trials of partial á7 nAchR agonists have been conducted, with EVP-6124 and TC-5619 furthest along in development.
EVP-6124. Information is unavailable publicly on EVP-6124, except for an abstract presented in 2011 at the 51st Annual Meeting of the American College of Neuropsychopharmacology.13 In that study, 319 patients with schizophrenia were randomized to EVP-6124 (0.3 mg/d or 1 mg/d [n = 213]) or placebo (n = 106) adjunctive to at least 4 weeks of non-clozapine antipsychotics. Efficacy was shown up to 1 mg, in a dose-responsive manner. Modest, but significant, improvements in cognition, clinical function, and negative symptoms were seen. The most commonly reported side effects were headache (3.8%), nausea (3.2%), and nasopharyngitis (2.5%). Phase III studies are underway.
TC-5619. This partial á7 nAchR also showed positive results recently in a Phase II trial. Significant (P < .05) improvement was demonstrated in executive function in the Groton Maze Learning Task of the CogState Schizophrenia Battery and the Scale for Assessment of Negative Symptoms.14
Strong anatomic links also exist between muscarinic acetylcholine receptors and the brain dopaminergic system, especially muscarinic type-1 and type-4 (M1 and M4) receptors. The potential utility of an M1, M4, or combined M/M4 agonist is also supported by studies of M1 and M4 knockout mice, with particular evidence of cognitive enhancement with the use of M1 agonists.15
GSK1034702. Administration of the M1 allosteric agonist GSK1034702 to healthy human smokers, using the nicotine abstinence model of cognitive dysfunction, resulted in improvements in immediate recall.16
Xanomeline. In a small pilot study of 20 schizophrenia patients, xanomeline, a mixed M1/M4 agonist, demonstrated significant improvements in verbal learning, short-term memory, and overall symptoms.17
Dopamine receptors
All marketed antipsychotics block the dopamine type-2 (D2) receptor18; they are primarily effective on positive symptoms.4 In contrast, a role for the dopamine type-1 (D1) receptor in cognition is suggested by studies that demonstrate reduced D1 and N-methyl-d-aspartate (NMDA) glutamate receptor function in the prefrontal cortex.19-22
In a model of cognitive impairment in non-human primates, low-dose intermittent dosing of D1-receptor agonists produced improvements in cognitive function.23 This strategy aims to sensitize, rather than induce tolerance, to the effects of the D1-receptor agonist. Benefits were primarily seen in working memory. Phase II trials of a potent D1-receptor agonist, DAR-100A, the active enantiomer of dihydrexidine24 are ongoing (www.clinicaltrials.gov/ct2/show/NCT01519557).
Glutamatergic receptors
Intoxication with NMDA antagonists (such as phencyclidine and ketamine) yields a phenotype with similarity to schizophrenia.25 More than 20 years of research has provided evidence for the role of glutamatergic NMDA receptors in the pathophysiology of schizophrenia.26,27
NMDA receptors are distributed widely in the brain, but specific glutamatergic processes are localized to areas that are associated with cognition. This relative distribution provides a convenient framework from which to view the pattern of cognitive dysfunction associated with schizophrenia:
• NMDA receptors in the hippocampus are involved in learning and memory acquisition
• NMDA receptors in the visual cortex and auditory cortex are fundamental for auditory and visual sensory memory.
Previous reviews of ketamine administration have described cognitive deficits in healthy control subjects, comparable to what is seen in schizophrenia.28 The deficits are noted primarily in measures of executive functioning, attention/vigilance, verbal fluency, and visual and verbal working memory.
Most treatment studies of glutamatergic-based drugs have focused on positive and negative symptoms. Two recent comprehensive meta-analyses29,30 of NMDA-based treatments support small-to-moderate effect size improvement in total symptoms and in negative symptoms, in patients with chronic schizophrenia, when the drugs are used in combination with non-clozapine antipsychotics.
Bitopertin. A novel glycine-transport inhibitor, bitopertin, showed significant improvement in negative symptoms as an adjunctive treatment in a large Phase II trial.31,32 In the “per protocol” population (ie, patients who completed 8 weeks of treatment without any major protocol violations [n = 231]), negative symptoms diminished to a significantly (P < .05) greater degree from baseline in the 10 mg/d and 30 mg/d dosage groups, compared with placebo. Phase III studies of bitopertin are ongoing (www.clinicaltrials.gov/ct2/show/NCT01192906).
Direct evidence of a cognitive benefit of glutamatergic-based drugs is limited. In a recent large, multicenter study, low dosage D-serine (~30 mg/kg/d) did not separate from placebo,33 but an open-label study suggests increased efficacy with dosages >30 mg/kg/d.34 In addition to symptomatic improvements, a highly significant, large effect-size improvement was seen for overall cognition for dosages ≥60 mg/kg/d, leading to a significant dose-by-time interaction (P < .01).
Combination approaches. The value of combining glutamatergic medication and a cognitive training program is supported by the role of NMDA receptors in learning. For example, D-cycloserine, a glycine-site partial agonist, has been shown in several studies to enhance learning and behavioral therapies in anxiety disorders.35 Although an initial study in schizophrenia was negative for the effectiveness of D-serine (a glycine-site full agonist) and combined cognitive training,36 further research is ongoing to evaluate a role for such combined therapy.37,38
Brain stimulation
Two nonpharmacotherapeutic brain stimulation techniques, repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), have been applied in the study of schizophrenia symptoms, particularly for enhancing cognition.39 Both techniques use electric stimulation to influence activity of underlying brain regions: rTMS utilizes a magnetic coil and electromagnetic induction; tDCS, in contrast, utilizes constant low (<2 mA) direct current to specific regions of the scalp.
Cortical neuronal excitability is increased by anodal tDCS and high-frequency rTMS and reduced by cathodal tDCS and low-frequency rTMS. Both tDCS and rTMS appear to be NMDA receptor-dependent. tDCS is relatively inexpensive and requires less expertise to administer than rTMS does.
Both techniques might be efficacious for treating resistant auditory hallucinations.40,41 Applying rTMS over the left dorsolateral prefrontal cortex has led to improvement in verbal learning and visuomotor tracking in patients with schizophrenia.39 Stimulation of both sides of the prefrontal cortex with rTMS has brought improvement in visual memory, executive function, spatial working memory, and attention. Few papers have been published so far regarding enhancement of cognition with tDCS in schizophrenia,42 but beneficial effects of this technique have been seen across several disorders.43
Cognitive remediation techniques
A fundamental starting point for cognitive remediation is the idea that there is plasticity in the brain and that repetitive practice can lead to cognitive improvement. Cognitive remediation therapy often adopts computerized programs and exercises that attempt to improve psychosocial function by targeting structures of the brain that are involved in cognitive function, such as attention, working memory, executive functioning, planning, and cognitive flexibility.
In schizophrenia, cognitive remediation studies have traditionally targeted higher-order processes, such as attention and higher level processes, that might lead to improvement in overall cognition and function.44 Cognitive remediation typically is utilized complementary to pharmacotherapy, with some studies supporting the use of combined use of cognition-enhancing drugs and remediation programs.
A 2007 meta-analysis showed a medium-size but significant improvement in cognition through the use of cognitive remediation therapy45—especially when it is combined with psychiatric rehabilitation. More recent studies utilizing techniques that focus on bottom-up (auditory and visual processing) techniques has shown significant improvements.46-48 Several multicenter studies utilizing Posit Science programs combined with antipsychotic medication are ongoing (www.clinicaltrials.gov/ct2/show/NCT01173874 and www.clinicaltrials.gov/ct2/show/NCT01422902).
Bottom Line
Although cognitive dysfunction is a leading cause of disability in schizophrenia, no treatments are approved for this condition. Numerous novel-mechanism and nonpharmaceutical modalities are actively being studied for this difficult-to-treat problem, however—offering hope to patients.
Related Resources
Javitt DC, Zukin SR, Heresco-Levy U, et al. Etiological and therapeutic implications of the PCP/NMDA model of schizophrenia. Has an angel shown the way? Schizophr Bull. 2012; 38(5):958-966.
Keefe RS, Harvey PD. Cognitive impairment in schizophrenia. Handb Exp Pharmacol. 2012;(213):11-37.
Millan MJ, Agid Y, Brune M, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012; 11(2):141-168.
Drug Brand Names
D-cycloserine • Seromycin Ketamine • Ketalar
Xanomeline • Lumeron, Memcor
Disclosures
Dr. Kantrowitz receives grant or research support from EnVivo, the National Institute of Mental Health, Novartis, Pfizer, Roche-Genentech, the Stanley Foundation, and Sunovion; is a consultant to Health Advances, LLC, the Healthcare Advisory Board, Otsuka Pharmaceuticals, Strategic Edge Communications, and Vindico Medical Education; and owns a small number of shares of common stock in GlaxoSmithKline. Ms. Levy and Dr. Ballon report no financial relationships with manufacturers of any products mentioned in this article or with manufacturers of competing products.
1. Bowie CR, Reichenberg A, Patterson TL, et al. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418-425.
2. Kern RS, Gold JM, Dickinson D, et al. The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res. 2011;126(1-3):124-131.
3. Javitt DC, Spencer KM, Thaker GK, et al. Neurophysiological biomarkers for drug development in schizophrenia. Nat Rev Drug Discov. 2008;7(1):68-83.
4. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1253.
5. Keefe RS, Bilder RM, Harvey PD, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology. 2006;31(9):2033-2046.
6. Green MF, Kern RS, Braff DL, et al. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26(1):119-136.
7. Keefe RS, Bilder RM, Davis SM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64(6):633-647.
8. Yan J. NIMH tries to jumpstart drug innovations. Psychiatric News. 2013;48(1):8-10.
9. Javitt DC, Schoepp D, Kalivas PW, et al. Translating glutamate: from pathophysiology to treatment. Sci Transl Med. 2011;3(102):102mr2.
10. Foster DJ, Jones CK, Conn PJ. Emerging approaches for treatment of schizophrenia: modulation of cholinergic signaling. Discov Med. 2012;14(79):413-420.
11. D’Souza MS, Markou A. Schizophrenia and tobacco smoking comorbidity: nAChR agonists in the treatment of schizophrenia-associated cognitive deficits. Neuropharmacology. 2012;62(3):1564-1573.
12. Adler LE, Olincy A, Waldo M, et al. Schizophrenia, sensory gating, and nicotinic receptors. Schizophr Bull. 1998; 24(2):189-202.
13. Meltzer HY, Gawryl M, Ward S, et al. EVP-6124, an alpha-7 nicotinic partial agonist, reduces positive effects on cognition, clinical function, and negative symptoms in patients with chronic schizophrenia on stable antipsychotic therapy. Neuropsychopharmacology. 2011;36:S170-S171.
14. Lieberman JA, Dunbar G, Segreti AC, et al. A randomized exploratory trial of an alpha-7 nicotinic receptor agonist (TC-5619) for cognitive enhancement in schizophrenia. Neuropsychopharmacology. 2013;38(6):968-975.
15. Digby GJ, Noetzel MJ, Bubser M, et al. Novel allosteric agonists of M1 muscarinic acetylcholine receptors induce brain region-specific responses that correspond with behavioral effects in animal models. J Neurosci. 2012;32(25):8532-8544.
16. Nathan PJ, Watson J, Lund J, et al. The potent M1 receptor allosteric agonist GSK1034702 improves episodic memory in humans in the nicotine abstinence model of cognitive dysfunction. Int J Neuropsychopharmacol. 2013;16(4):721-731.
17. Shekhar A, Potter WZ, Lightfoot J, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165(8):1033-1039.
18. Di Forti M, Lappin LM, Murray RM. Risk factors for schizophrenia—all roads lead to dopamine. Eur Neuropsychopharmacol. 2007;17(suppl 2):S101-S107.
19. Krystal JH, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology (Berl). 2003;169(3-4): 215-233.
20. Abi-Dargham A, Moore H. Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist. 2003;9(5):404-416.
21. Abi-Dargham A, Mawlawi O, Lombardo I, et al. Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci. 2002;22(9):3708-3719.
22. Martinez A, Ramanathan DS, Foxe JJ, et al. The role of spatial attention in the selection of real and illusory objects. J Neurosci. 2007;27(30):7963-7973.
23. Castner SA, Williams GV, Goldman-Rakic PS. Reversal of antipsychotic-induced working memory deficits by short-term dopamine D1 receptor stimulation. Science. 2000;287(5460):2020-2022.
24. Slifstein M, Suckow RF, Javitch JA, et al. Characterization of in vivo pharmacokinetic properties of the dopamine D1 receptor agonist DAR-0100A in nonhuman primates using PET with [11C] NNC112 and [11C] raclopride. J Cereb Blood Flow Metab. 2011;31(1):293-304.
25. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
26. Kantrowitz JT, Javitt DC. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4):108-121.
27. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
28. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Javitt DC, Kantrowitz JT, eds. Handbook of neurochemistry and molecular neurobiology. New York, NY: Springer; 2009:3-36.
29. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
30. Singh SP, Singh V. Meta-analysis of the efficacy of adjunctive NMDA receptor modulators in chronic schizophrenia. CNS Drugs. 2011;25(10):859-868.
31. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropharmacology. 2010;35:S320-S321.
32. Pinard E, Alanine A, Alberati D, et al. Selective GlyT1 inhibitors: discovery of [4-(3-fluoro-5-trifluoromethylpyridin-2-yl)piperazin-1-yl][5-methanesulfonyl-2-(( S)-2,2,2-trifluoro-1-methylethoxy)phenyl]methanone (RG1678), a promising novel medicine to treat schizophrenia. J Med Chem. 2010;53(12):4603-4614.
33. Weiser M, Heresco-Levy U, Davidson M, et al. A multicenter, add-on randomized controlled trial of low-dose d-serine for negative and cognitive symptoms of schizophrenia. J Clin Psychiatry. 2012;73(6):e728-e734.
34. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
35. Norberg MM, Krystal JH, Tolin DF. A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry. 2008;63(12):1118-1126.
36. D’Souza DC, Radhakrishnan R, Perry E, et al. Feasibility, safety, and efficacy of the combination of D-serine and computerized cognitive retraining in schizophrenia: an international collaborative pilot study. Neuropsychopharmacology. 2013;38(3):492-503.
37. Gottlieb JD, Cather C, Shanahan M, et al. D-cycloserine facilitation of cognitive behavioral therapy for delusions in schizophrenia. Schizophr Res. 2011;131(1-3):69-74.
38. Kantrowitz J, Sehatpour P, Oakman E, et al. D-Serine and NMDA based sensory modulation. Poster presented at: 3rd Biennial Schizophrenia International Research Conference; April 14-18, 2012; Florence, Italy.
39. Demirtas-Tatlidede, A, Vahabzadeh-Hagh AM, Pascual-Leone A. Can noninvasive brain stimulation enhance cognition in neuropsychiatric disorders? Neuropharmacology. 2013;64:566-578.
40. Brunelin J, Mondino M, Gassab L, et al. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169(7):719-724.
41. Matheson SL, Green MJ, Loo C, et al. Quality assessment and comparison of evidence for electroconvulsive therapy and repetitive transcranial magnetic stimulation for schizophrenia: a systematic meta-review. Schizophr Res. 2012;118(1-3):201-210.
42. Vercammen A, Rushby JA, Loo C, et al. Transcranial direct current stimulation influences probabilistic association learning in schizophrenia. Schizophr Res. 2011;131(1-3):198-205.
43. Nitsche MA, Paulus W. Transcranial direct current stimulation--update 2011. Restor Neurol Neurosci. 2011; 29(6):463-492.
44. Keefe RS, Vinogradov S, Medalia A, et al. Report from the working group conference on multisite trial design for cognitive remediation in schizophrenia. Schizophr Bull. 2011;37(5):1057-1065.
45. McGurk SR, Twamley EW, Sitzer DI, et al. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164(12):1791-1802.
46. Fisher M, Holland C, Merzenich MM, et al. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry. 2009;166(7):805-811.
47. Norton DJ, McBain RK, Ongür D, et al. Perceptual training strongly improves visual motion perception in schizophrenia. Brain Cogn. 2011;77(2):248-256.
48. Kantrowitz JT, Revheim N, Pasternak R, et al. It’s all in the cards: effect of stimulus manipulation on Wisconsin Card Sorting Test performance in schizophrenia. Psychiatry Res. 2009;168(3):198-204.
Available treatments for schizophrenia (eg, antipsychotics) are primarily effective on positive symptoms (hallucinations, delusions, etc.). It is, however, increasingly clear that schizophrenia also is a severe neuropsychiatric illness associated with deficits in cognitive function. These deficits represent a core feature of the disorder, and are a major determinant of long-term disability.1 Cognitive dysfunction is among the earliest signs of illness that, typically, presents in the prodromal phase.
Since the formulation of the dopaminergic model of schizophrenia, cognitive studies of the disease primarily have examined dysfunction in dopaminergic-rich regions of the brain, such as the prefrontal cortex, and, therefore, have focused largely on executive functioning. But neurocognitive deficits in schizophrenia are not limited to executive functioning; comparable deficits have been observed across multiple areas of cognition.2
More recent formulations of cognitive dysfunction in schizophrenia divide deficits into multiple domains. These include verbal, visual, and working memory; attention and vigilance; speed of processing, reasoning, and problem solving; and social cognition (Table). Neurocognitive impairments often are closely associated with deficits in early sensory processing and basic neurophysiology.3
The prevalence of cognitive dysfunction also can be estimated using baseline data from the large-scale Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) trial.4 Although cognitive dysfunction was not one of the inclusion criteria in CATIE, most patients who were enrolled had profound cognitive deficits.5 Furthermore, meta-analyses6 suggest that composite neurocognitive measures can explain as much as 60% of the variance of overall functioning in schizophrenia.
Antipsychotics aren’t the answer
The cognitive-enhancing benefits of antipsychotic medications are minimal.7 As evidence of a direct relationship between cognitive dysfunction and long-term functional outcome in schizophrenia becomes established, the need for safe and effective treatment for these symptoms becomes more urgent. Given the mechanistic complexity of the potential cause of poor cognitive performance, the search for an effective treatment is ongoing—but that search has not been successful.
Despite mixed results for recent novel mechanism trials (http://newsroom.lilly.com/releasedetail.cfm?releaseid=703018) and a number of companies ceasing drug development, the work to develop safe and effective treatments for cognitive dysfunction in schizophrenia continues, as exemplified by National Institute of Mental Health-initiated programs to spur development of drugs that work by a novel mechanism. Rather than simply assessing novel compounds with paper-and-pencil cognitive scales, such programs seek to assess the ability of the compound to engage with the intended receptor (target),9 using imaging or electrophysiological tools. Without utilization of a target engagement biomarker, there is no way to know whether 1) the drug simply does not get into the brain in sufficient concentration to be effective in humans or 2) the overall mechanism is wrong.
In this article, we review several promising targets and techniques that are the subject of active research on the treatment of cognitive disorders in schizophrenia. This list isn’t exhaustive; our aim is to highlight a few of the promising treatments now being studied in clinical trials.
Acetylcholine receptors
Acetylcholine receptors comprise two major families, nicotinic and muscarinic receptors; evidence implicates deficits of both families in schizophrenia.10 Following up on epidemiological studies11 of the high percentage of schizophrenia patients who smoke tobacco (60% to 90%), the role of alpha-7 nicotinic acetylcholine receptors (á7 nAchR) has been explored. Nicotine itself might normalize some disrupted auditory processes, as measured by electroencephalography.12
Several clinical trials of partial á7 nAchR agonists have been conducted, with EVP-6124 and TC-5619 furthest along in development.
EVP-6124. Information is unavailable publicly on EVP-6124, except for an abstract presented in 2011 at the 51st Annual Meeting of the American College of Neuropsychopharmacology.13 In that study, 319 patients with schizophrenia were randomized to EVP-6124 (0.3 mg/d or 1 mg/d [n = 213]) or placebo (n = 106) adjunctive to at least 4 weeks of non-clozapine antipsychotics. Efficacy was shown up to 1 mg, in a dose-responsive manner. Modest, but significant, improvements in cognition, clinical function, and negative symptoms were seen. The most commonly reported side effects were headache (3.8%), nausea (3.2%), and nasopharyngitis (2.5%). Phase III studies are underway.
TC-5619. This partial á7 nAchR also showed positive results recently in a Phase II trial. Significant (P < .05) improvement was demonstrated in executive function in the Groton Maze Learning Task of the CogState Schizophrenia Battery and the Scale for Assessment of Negative Symptoms.14
Strong anatomic links also exist between muscarinic acetylcholine receptors and the brain dopaminergic system, especially muscarinic type-1 and type-4 (M1 and M4) receptors. The potential utility of an M1, M4, or combined M/M4 agonist is also supported by studies of M1 and M4 knockout mice, with particular evidence of cognitive enhancement with the use of M1 agonists.15
GSK1034702. Administration of the M1 allosteric agonist GSK1034702 to healthy human smokers, using the nicotine abstinence model of cognitive dysfunction, resulted in improvements in immediate recall.16
Xanomeline. In a small pilot study of 20 schizophrenia patients, xanomeline, a mixed M1/M4 agonist, demonstrated significant improvements in verbal learning, short-term memory, and overall symptoms.17
Dopamine receptors
All marketed antipsychotics block the dopamine type-2 (D2) receptor18; they are primarily effective on positive symptoms.4 In contrast, a role for the dopamine type-1 (D1) receptor in cognition is suggested by studies that demonstrate reduced D1 and N-methyl-d-aspartate (NMDA) glutamate receptor function in the prefrontal cortex.19-22
In a model of cognitive impairment in non-human primates, low-dose intermittent dosing of D1-receptor agonists produced improvements in cognitive function.23 This strategy aims to sensitize, rather than induce tolerance, to the effects of the D1-receptor agonist. Benefits were primarily seen in working memory. Phase II trials of a potent D1-receptor agonist, DAR-100A, the active enantiomer of dihydrexidine24 are ongoing (www.clinicaltrials.gov/ct2/show/NCT01519557).
Glutamatergic receptors
Intoxication with NMDA antagonists (such as phencyclidine and ketamine) yields a phenotype with similarity to schizophrenia.25 More than 20 years of research has provided evidence for the role of glutamatergic NMDA receptors in the pathophysiology of schizophrenia.26,27
NMDA receptors are distributed widely in the brain, but specific glutamatergic processes are localized to areas that are associated with cognition. This relative distribution provides a convenient framework from which to view the pattern of cognitive dysfunction associated with schizophrenia:
• NMDA receptors in the hippocampus are involved in learning and memory acquisition
• NMDA receptors in the visual cortex and auditory cortex are fundamental for auditory and visual sensory memory.
Previous reviews of ketamine administration have described cognitive deficits in healthy control subjects, comparable to what is seen in schizophrenia.28 The deficits are noted primarily in measures of executive functioning, attention/vigilance, verbal fluency, and visual and verbal working memory.
Most treatment studies of glutamatergic-based drugs have focused on positive and negative symptoms. Two recent comprehensive meta-analyses29,30 of NMDA-based treatments support small-to-moderate effect size improvement in total symptoms and in negative symptoms, in patients with chronic schizophrenia, when the drugs are used in combination with non-clozapine antipsychotics.
Bitopertin. A novel glycine-transport inhibitor, bitopertin, showed significant improvement in negative symptoms as an adjunctive treatment in a large Phase II trial.31,32 In the “per protocol” population (ie, patients who completed 8 weeks of treatment without any major protocol violations [n = 231]), negative symptoms diminished to a significantly (P < .05) greater degree from baseline in the 10 mg/d and 30 mg/d dosage groups, compared with placebo. Phase III studies of bitopertin are ongoing (www.clinicaltrials.gov/ct2/show/NCT01192906).
Direct evidence of a cognitive benefit of glutamatergic-based drugs is limited. In a recent large, multicenter study, low dosage D-serine (~30 mg/kg/d) did not separate from placebo,33 but an open-label study suggests increased efficacy with dosages >30 mg/kg/d.34 In addition to symptomatic improvements, a highly significant, large effect-size improvement was seen for overall cognition for dosages ≥60 mg/kg/d, leading to a significant dose-by-time interaction (P < .01).
Combination approaches. The value of combining glutamatergic medication and a cognitive training program is supported by the role of NMDA receptors in learning. For example, D-cycloserine, a glycine-site partial agonist, has been shown in several studies to enhance learning and behavioral therapies in anxiety disorders.35 Although an initial study in schizophrenia was negative for the effectiveness of D-serine (a glycine-site full agonist) and combined cognitive training,36 further research is ongoing to evaluate a role for such combined therapy.37,38
Brain stimulation
Two nonpharmacotherapeutic brain stimulation techniques, repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), have been applied in the study of schizophrenia symptoms, particularly for enhancing cognition.39 Both techniques use electric stimulation to influence activity of underlying brain regions: rTMS utilizes a magnetic coil and electromagnetic induction; tDCS, in contrast, utilizes constant low (<2 mA) direct current to specific regions of the scalp.
Cortical neuronal excitability is increased by anodal tDCS and high-frequency rTMS and reduced by cathodal tDCS and low-frequency rTMS. Both tDCS and rTMS appear to be NMDA receptor-dependent. tDCS is relatively inexpensive and requires less expertise to administer than rTMS does.
Both techniques might be efficacious for treating resistant auditory hallucinations.40,41 Applying rTMS over the left dorsolateral prefrontal cortex has led to improvement in verbal learning and visuomotor tracking in patients with schizophrenia.39 Stimulation of both sides of the prefrontal cortex with rTMS has brought improvement in visual memory, executive function, spatial working memory, and attention. Few papers have been published so far regarding enhancement of cognition with tDCS in schizophrenia,42 but beneficial effects of this technique have been seen across several disorders.43
Cognitive remediation techniques
A fundamental starting point for cognitive remediation is the idea that there is plasticity in the brain and that repetitive practice can lead to cognitive improvement. Cognitive remediation therapy often adopts computerized programs and exercises that attempt to improve psychosocial function by targeting structures of the brain that are involved in cognitive function, such as attention, working memory, executive functioning, planning, and cognitive flexibility.
In schizophrenia, cognitive remediation studies have traditionally targeted higher-order processes, such as attention and higher level processes, that might lead to improvement in overall cognition and function.44 Cognitive remediation typically is utilized complementary to pharmacotherapy, with some studies supporting the use of combined use of cognition-enhancing drugs and remediation programs.
A 2007 meta-analysis showed a medium-size but significant improvement in cognition through the use of cognitive remediation therapy45—especially when it is combined with psychiatric rehabilitation. More recent studies utilizing techniques that focus on bottom-up (auditory and visual processing) techniques has shown significant improvements.46-48 Several multicenter studies utilizing Posit Science programs combined with antipsychotic medication are ongoing (www.clinicaltrials.gov/ct2/show/NCT01173874 and www.clinicaltrials.gov/ct2/show/NCT01422902).
Bottom Line
Although cognitive dysfunction is a leading cause of disability in schizophrenia, no treatments are approved for this condition. Numerous novel-mechanism and nonpharmaceutical modalities are actively being studied for this difficult-to-treat problem, however—offering hope to patients.
Related Resources
Javitt DC, Zukin SR, Heresco-Levy U, et al. Etiological and therapeutic implications of the PCP/NMDA model of schizophrenia. Has an angel shown the way? Schizophr Bull. 2012; 38(5):958-966.
Keefe RS, Harvey PD. Cognitive impairment in schizophrenia. Handb Exp Pharmacol. 2012;(213):11-37.
Millan MJ, Agid Y, Brune M, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012; 11(2):141-168.
Drug Brand Names
D-cycloserine • Seromycin Ketamine • Ketalar
Xanomeline • Lumeron, Memcor
Disclosures
Dr. Kantrowitz receives grant or research support from EnVivo, the National Institute of Mental Health, Novartis, Pfizer, Roche-Genentech, the Stanley Foundation, and Sunovion; is a consultant to Health Advances, LLC, the Healthcare Advisory Board, Otsuka Pharmaceuticals, Strategic Edge Communications, and Vindico Medical Education; and owns a small number of shares of common stock in GlaxoSmithKline. Ms. Levy and Dr. Ballon report no financial relationships with manufacturers of any products mentioned in this article or with manufacturers of competing products.
Available treatments for schizophrenia (eg, antipsychotics) are primarily effective on positive symptoms (hallucinations, delusions, etc.). It is, however, increasingly clear that schizophrenia also is a severe neuropsychiatric illness associated with deficits in cognitive function. These deficits represent a core feature of the disorder, and are a major determinant of long-term disability.1 Cognitive dysfunction is among the earliest signs of illness that, typically, presents in the prodromal phase.
Since the formulation of the dopaminergic model of schizophrenia, cognitive studies of the disease primarily have examined dysfunction in dopaminergic-rich regions of the brain, such as the prefrontal cortex, and, therefore, have focused largely on executive functioning. But neurocognitive deficits in schizophrenia are not limited to executive functioning; comparable deficits have been observed across multiple areas of cognition.2
More recent formulations of cognitive dysfunction in schizophrenia divide deficits into multiple domains. These include verbal, visual, and working memory; attention and vigilance; speed of processing, reasoning, and problem solving; and social cognition (Table). Neurocognitive impairments often are closely associated with deficits in early sensory processing and basic neurophysiology.3
The prevalence of cognitive dysfunction also can be estimated using baseline data from the large-scale Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) trial.4 Although cognitive dysfunction was not one of the inclusion criteria in CATIE, most patients who were enrolled had profound cognitive deficits.5 Furthermore, meta-analyses6 suggest that composite neurocognitive measures can explain as much as 60% of the variance of overall functioning in schizophrenia.
Antipsychotics aren’t the answer
The cognitive-enhancing benefits of antipsychotic medications are minimal.7 As evidence of a direct relationship between cognitive dysfunction and long-term functional outcome in schizophrenia becomes established, the need for safe and effective treatment for these symptoms becomes more urgent. Given the mechanistic complexity of the potential cause of poor cognitive performance, the search for an effective treatment is ongoing—but that search has not been successful.
Despite mixed results for recent novel mechanism trials (http://newsroom.lilly.com/releasedetail.cfm?releaseid=703018) and a number of companies ceasing drug development, the work to develop safe and effective treatments for cognitive dysfunction in schizophrenia continues, as exemplified by National Institute of Mental Health-initiated programs to spur development of drugs that work by a novel mechanism. Rather than simply assessing novel compounds with paper-and-pencil cognitive scales, such programs seek to assess the ability of the compound to engage with the intended receptor (target),9 using imaging or electrophysiological tools. Without utilization of a target engagement biomarker, there is no way to know whether 1) the drug simply does not get into the brain in sufficient concentration to be effective in humans or 2) the overall mechanism is wrong.
In this article, we review several promising targets and techniques that are the subject of active research on the treatment of cognitive disorders in schizophrenia. This list isn’t exhaustive; our aim is to highlight a few of the promising treatments now being studied in clinical trials.
Acetylcholine receptors
Acetylcholine receptors comprise two major families, nicotinic and muscarinic receptors; evidence implicates deficits of both families in schizophrenia.10 Following up on epidemiological studies11 of the high percentage of schizophrenia patients who smoke tobacco (60% to 90%), the role of alpha-7 nicotinic acetylcholine receptors (á7 nAchR) has been explored. Nicotine itself might normalize some disrupted auditory processes, as measured by electroencephalography.12
Several clinical trials of partial á7 nAchR agonists have been conducted, with EVP-6124 and TC-5619 furthest along in development.
EVP-6124. Information is unavailable publicly on EVP-6124, except for an abstract presented in 2011 at the 51st Annual Meeting of the American College of Neuropsychopharmacology.13 In that study, 319 patients with schizophrenia were randomized to EVP-6124 (0.3 mg/d or 1 mg/d [n = 213]) or placebo (n = 106) adjunctive to at least 4 weeks of non-clozapine antipsychotics. Efficacy was shown up to 1 mg, in a dose-responsive manner. Modest, but significant, improvements in cognition, clinical function, and negative symptoms were seen. The most commonly reported side effects were headache (3.8%), nausea (3.2%), and nasopharyngitis (2.5%). Phase III studies are underway.
TC-5619. This partial á7 nAchR also showed positive results recently in a Phase II trial. Significant (P < .05) improvement was demonstrated in executive function in the Groton Maze Learning Task of the CogState Schizophrenia Battery and the Scale for Assessment of Negative Symptoms.14
Strong anatomic links also exist between muscarinic acetylcholine receptors and the brain dopaminergic system, especially muscarinic type-1 and type-4 (M1 and M4) receptors. The potential utility of an M1, M4, or combined M/M4 agonist is also supported by studies of M1 and M4 knockout mice, with particular evidence of cognitive enhancement with the use of M1 agonists.15
GSK1034702. Administration of the M1 allosteric agonist GSK1034702 to healthy human smokers, using the nicotine abstinence model of cognitive dysfunction, resulted in improvements in immediate recall.16
Xanomeline. In a small pilot study of 20 schizophrenia patients, xanomeline, a mixed M1/M4 agonist, demonstrated significant improvements in verbal learning, short-term memory, and overall symptoms.17
Dopamine receptors
All marketed antipsychotics block the dopamine type-2 (D2) receptor18; they are primarily effective on positive symptoms.4 In contrast, a role for the dopamine type-1 (D1) receptor in cognition is suggested by studies that demonstrate reduced D1 and N-methyl-d-aspartate (NMDA) glutamate receptor function in the prefrontal cortex.19-22
In a model of cognitive impairment in non-human primates, low-dose intermittent dosing of D1-receptor agonists produced improvements in cognitive function.23 This strategy aims to sensitize, rather than induce tolerance, to the effects of the D1-receptor agonist. Benefits were primarily seen in working memory. Phase II trials of a potent D1-receptor agonist, DAR-100A, the active enantiomer of dihydrexidine24 are ongoing (www.clinicaltrials.gov/ct2/show/NCT01519557).
Glutamatergic receptors
Intoxication with NMDA antagonists (such as phencyclidine and ketamine) yields a phenotype with similarity to schizophrenia.25 More than 20 years of research has provided evidence for the role of glutamatergic NMDA receptors in the pathophysiology of schizophrenia.26,27
NMDA receptors are distributed widely in the brain, but specific glutamatergic processes are localized to areas that are associated with cognition. This relative distribution provides a convenient framework from which to view the pattern of cognitive dysfunction associated with schizophrenia:
• NMDA receptors in the hippocampus are involved in learning and memory acquisition
• NMDA receptors in the visual cortex and auditory cortex are fundamental for auditory and visual sensory memory.
Previous reviews of ketamine administration have described cognitive deficits in healthy control subjects, comparable to what is seen in schizophrenia.28 The deficits are noted primarily in measures of executive functioning, attention/vigilance, verbal fluency, and visual and verbal working memory.
Most treatment studies of glutamatergic-based drugs have focused on positive and negative symptoms. Two recent comprehensive meta-analyses29,30 of NMDA-based treatments support small-to-moderate effect size improvement in total symptoms and in negative symptoms, in patients with chronic schizophrenia, when the drugs are used in combination with non-clozapine antipsychotics.
Bitopertin. A novel glycine-transport inhibitor, bitopertin, showed significant improvement in negative symptoms as an adjunctive treatment in a large Phase II trial.31,32 In the “per protocol” population (ie, patients who completed 8 weeks of treatment without any major protocol violations [n = 231]), negative symptoms diminished to a significantly (P < .05) greater degree from baseline in the 10 mg/d and 30 mg/d dosage groups, compared with placebo. Phase III studies of bitopertin are ongoing (www.clinicaltrials.gov/ct2/show/NCT01192906).
Direct evidence of a cognitive benefit of glutamatergic-based drugs is limited. In a recent large, multicenter study, low dosage D-serine (~30 mg/kg/d) did not separate from placebo,33 but an open-label study suggests increased efficacy with dosages >30 mg/kg/d.34 In addition to symptomatic improvements, a highly significant, large effect-size improvement was seen for overall cognition for dosages ≥60 mg/kg/d, leading to a significant dose-by-time interaction (P < .01).
Combination approaches. The value of combining glutamatergic medication and a cognitive training program is supported by the role of NMDA receptors in learning. For example, D-cycloserine, a glycine-site partial agonist, has been shown in several studies to enhance learning and behavioral therapies in anxiety disorders.35 Although an initial study in schizophrenia was negative for the effectiveness of D-serine (a glycine-site full agonist) and combined cognitive training,36 further research is ongoing to evaluate a role for such combined therapy.37,38
Brain stimulation
Two nonpharmacotherapeutic brain stimulation techniques, repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), have been applied in the study of schizophrenia symptoms, particularly for enhancing cognition.39 Both techniques use electric stimulation to influence activity of underlying brain regions: rTMS utilizes a magnetic coil and electromagnetic induction; tDCS, in contrast, utilizes constant low (<2 mA) direct current to specific regions of the scalp.
Cortical neuronal excitability is increased by anodal tDCS and high-frequency rTMS and reduced by cathodal tDCS and low-frequency rTMS. Both tDCS and rTMS appear to be NMDA receptor-dependent. tDCS is relatively inexpensive and requires less expertise to administer than rTMS does.
Both techniques might be efficacious for treating resistant auditory hallucinations.40,41 Applying rTMS over the left dorsolateral prefrontal cortex has led to improvement in verbal learning and visuomotor tracking in patients with schizophrenia.39 Stimulation of both sides of the prefrontal cortex with rTMS has brought improvement in visual memory, executive function, spatial working memory, and attention. Few papers have been published so far regarding enhancement of cognition with tDCS in schizophrenia,42 but beneficial effects of this technique have been seen across several disorders.43
Cognitive remediation techniques
A fundamental starting point for cognitive remediation is the idea that there is plasticity in the brain and that repetitive practice can lead to cognitive improvement. Cognitive remediation therapy often adopts computerized programs and exercises that attempt to improve psychosocial function by targeting structures of the brain that are involved in cognitive function, such as attention, working memory, executive functioning, planning, and cognitive flexibility.
In schizophrenia, cognitive remediation studies have traditionally targeted higher-order processes, such as attention and higher level processes, that might lead to improvement in overall cognition and function.44 Cognitive remediation typically is utilized complementary to pharmacotherapy, with some studies supporting the use of combined use of cognition-enhancing drugs and remediation programs.
A 2007 meta-analysis showed a medium-size but significant improvement in cognition through the use of cognitive remediation therapy45—especially when it is combined with psychiatric rehabilitation. More recent studies utilizing techniques that focus on bottom-up (auditory and visual processing) techniques has shown significant improvements.46-48 Several multicenter studies utilizing Posit Science programs combined with antipsychotic medication are ongoing (www.clinicaltrials.gov/ct2/show/NCT01173874 and www.clinicaltrials.gov/ct2/show/NCT01422902).
Bottom Line
Although cognitive dysfunction is a leading cause of disability in schizophrenia, no treatments are approved for this condition. Numerous novel-mechanism and nonpharmaceutical modalities are actively being studied for this difficult-to-treat problem, however—offering hope to patients.
Related Resources
Javitt DC, Zukin SR, Heresco-Levy U, et al. Etiological and therapeutic implications of the PCP/NMDA model of schizophrenia. Has an angel shown the way? Schizophr Bull. 2012; 38(5):958-966.
Keefe RS, Harvey PD. Cognitive impairment in schizophrenia. Handb Exp Pharmacol. 2012;(213):11-37.
Millan MJ, Agid Y, Brune M, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012; 11(2):141-168.
Drug Brand Names
D-cycloserine • Seromycin Ketamine • Ketalar
Xanomeline • Lumeron, Memcor
Disclosures
Dr. Kantrowitz receives grant or research support from EnVivo, the National Institute of Mental Health, Novartis, Pfizer, Roche-Genentech, the Stanley Foundation, and Sunovion; is a consultant to Health Advances, LLC, the Healthcare Advisory Board, Otsuka Pharmaceuticals, Strategic Edge Communications, and Vindico Medical Education; and owns a small number of shares of common stock in GlaxoSmithKline. Ms. Levy and Dr. Ballon report no financial relationships with manufacturers of any products mentioned in this article or with manufacturers of competing products.
1. Bowie CR, Reichenberg A, Patterson TL, et al. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418-425.
2. Kern RS, Gold JM, Dickinson D, et al. The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res. 2011;126(1-3):124-131.
3. Javitt DC, Spencer KM, Thaker GK, et al. Neurophysiological biomarkers for drug development in schizophrenia. Nat Rev Drug Discov. 2008;7(1):68-83.
4. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1253.
5. Keefe RS, Bilder RM, Harvey PD, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology. 2006;31(9):2033-2046.
6. Green MF, Kern RS, Braff DL, et al. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26(1):119-136.
7. Keefe RS, Bilder RM, Davis SM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64(6):633-647.
8. Yan J. NIMH tries to jumpstart drug innovations. Psychiatric News. 2013;48(1):8-10.
9. Javitt DC, Schoepp D, Kalivas PW, et al. Translating glutamate: from pathophysiology to treatment. Sci Transl Med. 2011;3(102):102mr2.
10. Foster DJ, Jones CK, Conn PJ. Emerging approaches for treatment of schizophrenia: modulation of cholinergic signaling. Discov Med. 2012;14(79):413-420.
11. D’Souza MS, Markou A. Schizophrenia and tobacco smoking comorbidity: nAChR agonists in the treatment of schizophrenia-associated cognitive deficits. Neuropharmacology. 2012;62(3):1564-1573.
12. Adler LE, Olincy A, Waldo M, et al. Schizophrenia, sensory gating, and nicotinic receptors. Schizophr Bull. 1998; 24(2):189-202.
13. Meltzer HY, Gawryl M, Ward S, et al. EVP-6124, an alpha-7 nicotinic partial agonist, reduces positive effects on cognition, clinical function, and negative symptoms in patients with chronic schizophrenia on stable antipsychotic therapy. Neuropsychopharmacology. 2011;36:S170-S171.
14. Lieberman JA, Dunbar G, Segreti AC, et al. A randomized exploratory trial of an alpha-7 nicotinic receptor agonist (TC-5619) for cognitive enhancement in schizophrenia. Neuropsychopharmacology. 2013;38(6):968-975.
15. Digby GJ, Noetzel MJ, Bubser M, et al. Novel allosteric agonists of M1 muscarinic acetylcholine receptors induce brain region-specific responses that correspond with behavioral effects in animal models. J Neurosci. 2012;32(25):8532-8544.
16. Nathan PJ, Watson J, Lund J, et al. The potent M1 receptor allosteric agonist GSK1034702 improves episodic memory in humans in the nicotine abstinence model of cognitive dysfunction. Int J Neuropsychopharmacol. 2013;16(4):721-731.
17. Shekhar A, Potter WZ, Lightfoot J, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165(8):1033-1039.
18. Di Forti M, Lappin LM, Murray RM. Risk factors for schizophrenia—all roads lead to dopamine. Eur Neuropsychopharmacol. 2007;17(suppl 2):S101-S107.
19. Krystal JH, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology (Berl). 2003;169(3-4): 215-233.
20. Abi-Dargham A, Moore H. Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist. 2003;9(5):404-416.
21. Abi-Dargham A, Mawlawi O, Lombardo I, et al. Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci. 2002;22(9):3708-3719.
22. Martinez A, Ramanathan DS, Foxe JJ, et al. The role of spatial attention in the selection of real and illusory objects. J Neurosci. 2007;27(30):7963-7973.
23. Castner SA, Williams GV, Goldman-Rakic PS. Reversal of antipsychotic-induced working memory deficits by short-term dopamine D1 receptor stimulation. Science. 2000;287(5460):2020-2022.
24. Slifstein M, Suckow RF, Javitch JA, et al. Characterization of in vivo pharmacokinetic properties of the dopamine D1 receptor agonist DAR-0100A in nonhuman primates using PET with [11C] NNC112 and [11C] raclopride. J Cereb Blood Flow Metab. 2011;31(1):293-304.
25. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
26. Kantrowitz JT, Javitt DC. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4):108-121.
27. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
28. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Javitt DC, Kantrowitz JT, eds. Handbook of neurochemistry and molecular neurobiology. New York, NY: Springer; 2009:3-36.
29. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
30. Singh SP, Singh V. Meta-analysis of the efficacy of adjunctive NMDA receptor modulators in chronic schizophrenia. CNS Drugs. 2011;25(10):859-868.
31. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropharmacology. 2010;35:S320-S321.
32. Pinard E, Alanine A, Alberati D, et al. Selective GlyT1 inhibitors: discovery of [4-(3-fluoro-5-trifluoromethylpyridin-2-yl)piperazin-1-yl][5-methanesulfonyl-2-(( S)-2,2,2-trifluoro-1-methylethoxy)phenyl]methanone (RG1678), a promising novel medicine to treat schizophrenia. J Med Chem. 2010;53(12):4603-4614.
33. Weiser M, Heresco-Levy U, Davidson M, et al. A multicenter, add-on randomized controlled trial of low-dose d-serine for negative and cognitive symptoms of schizophrenia. J Clin Psychiatry. 2012;73(6):e728-e734.
34. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
35. Norberg MM, Krystal JH, Tolin DF. A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry. 2008;63(12):1118-1126.
36. D’Souza DC, Radhakrishnan R, Perry E, et al. Feasibility, safety, and efficacy of the combination of D-serine and computerized cognitive retraining in schizophrenia: an international collaborative pilot study. Neuropsychopharmacology. 2013;38(3):492-503.
37. Gottlieb JD, Cather C, Shanahan M, et al. D-cycloserine facilitation of cognitive behavioral therapy for delusions in schizophrenia. Schizophr Res. 2011;131(1-3):69-74.
38. Kantrowitz J, Sehatpour P, Oakman E, et al. D-Serine and NMDA based sensory modulation. Poster presented at: 3rd Biennial Schizophrenia International Research Conference; April 14-18, 2012; Florence, Italy.
39. Demirtas-Tatlidede, A, Vahabzadeh-Hagh AM, Pascual-Leone A. Can noninvasive brain stimulation enhance cognition in neuropsychiatric disorders? Neuropharmacology. 2013;64:566-578.
40. Brunelin J, Mondino M, Gassab L, et al. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169(7):719-724.
41. Matheson SL, Green MJ, Loo C, et al. Quality assessment and comparison of evidence for electroconvulsive therapy and repetitive transcranial magnetic stimulation for schizophrenia: a systematic meta-review. Schizophr Res. 2012;118(1-3):201-210.
42. Vercammen A, Rushby JA, Loo C, et al. Transcranial direct current stimulation influences probabilistic association learning in schizophrenia. Schizophr Res. 2011;131(1-3):198-205.
43. Nitsche MA, Paulus W. Transcranial direct current stimulation--update 2011. Restor Neurol Neurosci. 2011; 29(6):463-492.
44. Keefe RS, Vinogradov S, Medalia A, et al. Report from the working group conference on multisite trial design for cognitive remediation in schizophrenia. Schizophr Bull. 2011;37(5):1057-1065.
45. McGurk SR, Twamley EW, Sitzer DI, et al. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164(12):1791-1802.
46. Fisher M, Holland C, Merzenich MM, et al. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry. 2009;166(7):805-811.
47. Norton DJ, McBain RK, Ongür D, et al. Perceptual training strongly improves visual motion perception in schizophrenia. Brain Cogn. 2011;77(2):248-256.
48. Kantrowitz JT, Revheim N, Pasternak R, et al. It’s all in the cards: effect of stimulus manipulation on Wisconsin Card Sorting Test performance in schizophrenia. Psychiatry Res. 2009;168(3):198-204.
1. Bowie CR, Reichenberg A, Patterson TL, et al. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418-425.
2. Kern RS, Gold JM, Dickinson D, et al. The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res. 2011;126(1-3):124-131.
3. Javitt DC, Spencer KM, Thaker GK, et al. Neurophysiological biomarkers for drug development in schizophrenia. Nat Rev Drug Discov. 2008;7(1):68-83.
4. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1253.
5. Keefe RS, Bilder RM, Harvey PD, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology. 2006;31(9):2033-2046.
6. Green MF, Kern RS, Braff DL, et al. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26(1):119-136.
7. Keefe RS, Bilder RM, Davis SM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64(6):633-647.
8. Yan J. NIMH tries to jumpstart drug innovations. Psychiatric News. 2013;48(1):8-10.
9. Javitt DC, Schoepp D, Kalivas PW, et al. Translating glutamate: from pathophysiology to treatment. Sci Transl Med. 2011;3(102):102mr2.
10. Foster DJ, Jones CK, Conn PJ. Emerging approaches for treatment of schizophrenia: modulation of cholinergic signaling. Discov Med. 2012;14(79):413-420.
11. D’Souza MS, Markou A. Schizophrenia and tobacco smoking comorbidity: nAChR agonists in the treatment of schizophrenia-associated cognitive deficits. Neuropharmacology. 2012;62(3):1564-1573.
12. Adler LE, Olincy A, Waldo M, et al. Schizophrenia, sensory gating, and nicotinic receptors. Schizophr Bull. 1998; 24(2):189-202.
13. Meltzer HY, Gawryl M, Ward S, et al. EVP-6124, an alpha-7 nicotinic partial agonist, reduces positive effects on cognition, clinical function, and negative symptoms in patients with chronic schizophrenia on stable antipsychotic therapy. Neuropsychopharmacology. 2011;36:S170-S171.
14. Lieberman JA, Dunbar G, Segreti AC, et al. A randomized exploratory trial of an alpha-7 nicotinic receptor agonist (TC-5619) for cognitive enhancement in schizophrenia. Neuropsychopharmacology. 2013;38(6):968-975.
15. Digby GJ, Noetzel MJ, Bubser M, et al. Novel allosteric agonists of M1 muscarinic acetylcholine receptors induce brain region-specific responses that correspond with behavioral effects in animal models. J Neurosci. 2012;32(25):8532-8544.
16. Nathan PJ, Watson J, Lund J, et al. The potent M1 receptor allosteric agonist GSK1034702 improves episodic memory in humans in the nicotine abstinence model of cognitive dysfunction. Int J Neuropsychopharmacol. 2013;16(4):721-731.
17. Shekhar A, Potter WZ, Lightfoot J, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165(8):1033-1039.
18. Di Forti M, Lappin LM, Murray RM. Risk factors for schizophrenia—all roads lead to dopamine. Eur Neuropsychopharmacol. 2007;17(suppl 2):S101-S107.
19. Krystal JH, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology (Berl). 2003;169(3-4): 215-233.
20. Abi-Dargham A, Moore H. Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist. 2003;9(5):404-416.
21. Abi-Dargham A, Mawlawi O, Lombardo I, et al. Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci. 2002;22(9):3708-3719.
22. Martinez A, Ramanathan DS, Foxe JJ, et al. The role of spatial attention in the selection of real and illusory objects. J Neurosci. 2007;27(30):7963-7973.
23. Castner SA, Williams GV, Goldman-Rakic PS. Reversal of antipsychotic-induced working memory deficits by short-term dopamine D1 receptor stimulation. Science. 2000;287(5460):2020-2022.
24. Slifstein M, Suckow RF, Javitch JA, et al. Characterization of in vivo pharmacokinetic properties of the dopamine D1 receptor agonist DAR-0100A in nonhuman primates using PET with [11C] NNC112 and [11C] raclopride. J Cereb Blood Flow Metab. 2011;31(1):293-304.
25. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
26. Kantrowitz JT, Javitt DC. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4):108-121.
27. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
28. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Javitt DC, Kantrowitz JT, eds. Handbook of neurochemistry and molecular neurobiology. New York, NY: Springer; 2009:3-36.
29. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
30. Singh SP, Singh V. Meta-analysis of the efficacy of adjunctive NMDA receptor modulators in chronic schizophrenia. CNS Drugs. 2011;25(10):859-868.
31. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropharmacology. 2010;35:S320-S321.
32. Pinard E, Alanine A, Alberati D, et al. Selective GlyT1 inhibitors: discovery of [4-(3-fluoro-5-trifluoromethylpyridin-2-yl)piperazin-1-yl][5-methanesulfonyl-2-(( S)-2,2,2-trifluoro-1-methylethoxy)phenyl]methanone (RG1678), a promising novel medicine to treat schizophrenia. J Med Chem. 2010;53(12):4603-4614.
33. Weiser M, Heresco-Levy U, Davidson M, et al. A multicenter, add-on randomized controlled trial of low-dose d-serine for negative and cognitive symptoms of schizophrenia. J Clin Psychiatry. 2012;73(6):e728-e734.
34. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
35. Norberg MM, Krystal JH, Tolin DF. A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry. 2008;63(12):1118-1126.
36. D’Souza DC, Radhakrishnan R, Perry E, et al. Feasibility, safety, and efficacy of the combination of D-serine and computerized cognitive retraining in schizophrenia: an international collaborative pilot study. Neuropsychopharmacology. 2013;38(3):492-503.
37. Gottlieb JD, Cather C, Shanahan M, et al. D-cycloserine facilitation of cognitive behavioral therapy for delusions in schizophrenia. Schizophr Res. 2011;131(1-3):69-74.
38. Kantrowitz J, Sehatpour P, Oakman E, et al. D-Serine and NMDA based sensory modulation. Poster presented at: 3rd Biennial Schizophrenia International Research Conference; April 14-18, 2012; Florence, Italy.
39. Demirtas-Tatlidede, A, Vahabzadeh-Hagh AM, Pascual-Leone A. Can noninvasive brain stimulation enhance cognition in neuropsychiatric disorders? Neuropharmacology. 2013;64:566-578.
40. Brunelin J, Mondino M, Gassab L, et al. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169(7):719-724.
41. Matheson SL, Green MJ, Loo C, et al. Quality assessment and comparison of evidence for electroconvulsive therapy and repetitive transcranial magnetic stimulation for schizophrenia: a systematic meta-review. Schizophr Res. 2012;118(1-3):201-210.
42. Vercammen A, Rushby JA, Loo C, et al. Transcranial direct current stimulation influences probabilistic association learning in schizophrenia. Schizophr Res. 2011;131(1-3):198-205.
43. Nitsche MA, Paulus W. Transcranial direct current stimulation--update 2011. Restor Neurol Neurosci. 2011; 29(6):463-492.
44. Keefe RS, Vinogradov S, Medalia A, et al. Report from the working group conference on multisite trial design for cognitive remediation in schizophrenia. Schizophr Bull. 2011;37(5):1057-1065.
45. McGurk SR, Twamley EW, Sitzer DI, et al. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164(12):1791-1802.
46. Fisher M, Holland C, Merzenich MM, et al. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry. 2009;166(7):805-811.
47. Norton DJ, McBain RK, Ongür D, et al. Perceptual training strongly improves visual motion perception in schizophrenia. Brain Cogn. 2011;77(2):248-256.
48. Kantrowitz JT, Revheim N, Pasternak R, et al. It’s all in the cards: effect of stimulus manipulation on Wisconsin Card Sorting Test performance in schizophrenia. Psychiatry Res. 2009;168(3):198-204.