User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Injustice can lead to treatment
In his editorial “New Year’s resolutions to help our patients” (From the Editor, Current Psychiatry, January 2010) Dr. Nasrallah decried criminalization of mentally ill individuals, which I agree, but I find that I can provide better treatment in the medium-security prison where I work part-time than in our community mental health clinic, which has been downsized. At the prison, we have a multidisciplinary staff, including primary care physicians. Patients keep their appointments and medication intake is monitored. We have enough time to see patients and adequate reimbursement for services. In fact, some patients do not want to leave because in prison they have a roof over their heads, adequate food, and competent health care.
Prisons are the only place in this country where people have the right to treatment. If only health care reform could replicate this outside of prison.
H. Steven Moffic, MD
Professor of psychiatry
Medical College of Wisconsin
Milwaukee, WI
In his editorial “New Year’s resolutions to help our patients” (From the Editor, Current Psychiatry, January 2010) Dr. Nasrallah decried criminalization of mentally ill individuals, which I agree, but I find that I can provide better treatment in the medium-security prison where I work part-time than in our community mental health clinic, which has been downsized. At the prison, we have a multidisciplinary staff, including primary care physicians. Patients keep their appointments and medication intake is monitored. We have enough time to see patients and adequate reimbursement for services. In fact, some patients do not want to leave because in prison they have a roof over their heads, adequate food, and competent health care.
Prisons are the only place in this country where people have the right to treatment. If only health care reform could replicate this outside of prison.
H. Steven Moffic, MD
Professor of psychiatry
Medical College of Wisconsin
Milwaukee, WI
In his editorial “New Year’s resolutions to help our patients” (From the Editor, Current Psychiatry, January 2010) Dr. Nasrallah decried criminalization of mentally ill individuals, which I agree, but I find that I can provide better treatment in the medium-security prison where I work part-time than in our community mental health clinic, which has been downsized. At the prison, we have a multidisciplinary staff, including primary care physicians. Patients keep their appointments and medication intake is monitored. We have enough time to see patients and adequate reimbursement for services. In fact, some patients do not want to leave because in prison they have a roof over their heads, adequate food, and competent health care.
Prisons are the only place in this country where people have the right to treatment. If only health care reform could replicate this outside of prison.
H. Steven Moffic, MD
Professor of psychiatry
Medical College of Wisconsin
Milwaukee, WI
Connecting the dots: Psychiatrists are virtuosos
“Connecting the dots” has emerged as a buzzword in our media and popular culture. This expression is a picturesque way to denote competence and implies an uncanny ability to recognize and integrate what appear to be multiple unrelated data points into an important, actionable pattern. An incisive decision or intervention often follows.
When I hear this expression, I contemplate the centrality of connecting the dots in psychiatric practice. In fact, it is a ubiquitous and indispensable approach to diagnosing and treating our patients. Psychiatrists are trained to be highly skilled at connecting not only one set of dots, but often a bewildering array of complex and disparate sets of dots related to each patient we evaluate and manage. It is impossible to arrive at an accurate psychiatric diagnosis and construct an appropriate and comprehensive treatment plan without connecting countless overt and covert dots related to interconnected pathologies across a patient’s brain, mind, and body. As part of the assessment, psychiatrists often presage the existence of dots that are not yet on their clinical radar and inquire about them with the patient and multiple corroborative sources. That’s what a good psychiatric interview and history taking usually entails.
Painting a diagnostic profile
The effective pursuit of connecting clinically relevant biologic, psychological, and social clinically relevant “dots” is an elegant mix of the art and science of psychiatry. By integrating a vast universe of clinical “dots,” (like an astronomer recognizing a galaxy in star-studded sky) psychiatrists can then identify their patients’ emotional topography, cognitive architecture, behavioral landscape, and psychodynamic geology. This enables us to formulate the patient’s clinical disorder across a matrix of biopsychosocial domains and paint a mosaic of “dots” representing predisposing, precipitating, perpetuating, and protective factors underpinning the patient’s psychopathology and illness course.
The emerging diagnostic profile of a patient leads to the next task of connecting another universe of dots related to launching a multifaceted treatment plan. An enormous number of dots have to be connected to determine a safe and effective treatment consistent with the patient’s demographics, lifestyle, social background, attitudes, beliefs, past and current medical history, family history, comorbidities, and laboratory data. Once those dots are connected and treatment begins, another phase of connecting the dots follows to monitor efficacy, safety, tolerability, and various clinical and functional outcomes related to treatment. Unless this phase is done expertly and meticulously, a patient’s remission, recovery, and return to wellness may be elusive and relapse or complications may develop.
We psychiatrists perform the Herculean task of connecting the dots many times a day on a heterogeneous group of patients with various psychopathologies, and we appear to do it effortlessly. This is a gratifying testimonial to the extensive and arduous years of training it takes to become skillful psychiatric physicians.
We always assume that other professionals also are connecting dots effectively in their respective areas of responsibility. Failure to connect the dots could result in a minor setback, or, in some cases, a catastrophic event. Aristotle defined “virtue” as excelling in one’s job. When we do our job well—diagnosing and healing mental, emotional, and behavioral brain disorders, preventing harm to self and others, and restoring wellness to ailing individuals—we psychiatrists are accomplishing “virtuous” acts and thus earn the privilege to be called “virtuosos.”
“Connecting the dots” has emerged as a buzzword in our media and popular culture. This expression is a picturesque way to denote competence and implies an uncanny ability to recognize and integrate what appear to be multiple unrelated data points into an important, actionable pattern. An incisive decision or intervention often follows.
When I hear this expression, I contemplate the centrality of connecting the dots in psychiatric practice. In fact, it is a ubiquitous and indispensable approach to diagnosing and treating our patients. Psychiatrists are trained to be highly skilled at connecting not only one set of dots, but often a bewildering array of complex and disparate sets of dots related to each patient we evaluate and manage. It is impossible to arrive at an accurate psychiatric diagnosis and construct an appropriate and comprehensive treatment plan without connecting countless overt and covert dots related to interconnected pathologies across a patient’s brain, mind, and body. As part of the assessment, psychiatrists often presage the existence of dots that are not yet on their clinical radar and inquire about them with the patient and multiple corroborative sources. That’s what a good psychiatric interview and history taking usually entails.
Painting a diagnostic profile
The effective pursuit of connecting clinically relevant biologic, psychological, and social clinically relevant “dots” is an elegant mix of the art and science of psychiatry. By integrating a vast universe of clinical “dots,” (like an astronomer recognizing a galaxy in star-studded sky) psychiatrists can then identify their patients’ emotional topography, cognitive architecture, behavioral landscape, and psychodynamic geology. This enables us to formulate the patient’s clinical disorder across a matrix of biopsychosocial domains and paint a mosaic of “dots” representing predisposing, precipitating, perpetuating, and protective factors underpinning the patient’s psychopathology and illness course.
The emerging diagnostic profile of a patient leads to the next task of connecting another universe of dots related to launching a multifaceted treatment plan. An enormous number of dots have to be connected to determine a safe and effective treatment consistent with the patient’s demographics, lifestyle, social background, attitudes, beliefs, past and current medical history, family history, comorbidities, and laboratory data. Once those dots are connected and treatment begins, another phase of connecting the dots follows to monitor efficacy, safety, tolerability, and various clinical and functional outcomes related to treatment. Unless this phase is done expertly and meticulously, a patient’s remission, recovery, and return to wellness may be elusive and relapse or complications may develop.
We psychiatrists perform the Herculean task of connecting the dots many times a day on a heterogeneous group of patients with various psychopathologies, and we appear to do it effortlessly. This is a gratifying testimonial to the extensive and arduous years of training it takes to become skillful psychiatric physicians.
We always assume that other professionals also are connecting dots effectively in their respective areas of responsibility. Failure to connect the dots could result in a minor setback, or, in some cases, a catastrophic event. Aristotle defined “virtue” as excelling in one’s job. When we do our job well—diagnosing and healing mental, emotional, and behavioral brain disorders, preventing harm to self and others, and restoring wellness to ailing individuals—we psychiatrists are accomplishing “virtuous” acts and thus earn the privilege to be called “virtuosos.”
“Connecting the dots” has emerged as a buzzword in our media and popular culture. This expression is a picturesque way to denote competence and implies an uncanny ability to recognize and integrate what appear to be multiple unrelated data points into an important, actionable pattern. An incisive decision or intervention often follows.
When I hear this expression, I contemplate the centrality of connecting the dots in psychiatric practice. In fact, it is a ubiquitous and indispensable approach to diagnosing and treating our patients. Psychiatrists are trained to be highly skilled at connecting not only one set of dots, but often a bewildering array of complex and disparate sets of dots related to each patient we evaluate and manage. It is impossible to arrive at an accurate psychiatric diagnosis and construct an appropriate and comprehensive treatment plan without connecting countless overt and covert dots related to interconnected pathologies across a patient’s brain, mind, and body. As part of the assessment, psychiatrists often presage the existence of dots that are not yet on their clinical radar and inquire about them with the patient and multiple corroborative sources. That’s what a good psychiatric interview and history taking usually entails.
Painting a diagnostic profile
The effective pursuit of connecting clinically relevant biologic, psychological, and social clinically relevant “dots” is an elegant mix of the art and science of psychiatry. By integrating a vast universe of clinical “dots,” (like an astronomer recognizing a galaxy in star-studded sky) psychiatrists can then identify their patients’ emotional topography, cognitive architecture, behavioral landscape, and psychodynamic geology. This enables us to formulate the patient’s clinical disorder across a matrix of biopsychosocial domains and paint a mosaic of “dots” representing predisposing, precipitating, perpetuating, and protective factors underpinning the patient’s psychopathology and illness course.
The emerging diagnostic profile of a patient leads to the next task of connecting another universe of dots related to launching a multifaceted treatment plan. An enormous number of dots have to be connected to determine a safe and effective treatment consistent with the patient’s demographics, lifestyle, social background, attitudes, beliefs, past and current medical history, family history, comorbidities, and laboratory data. Once those dots are connected and treatment begins, another phase of connecting the dots follows to monitor efficacy, safety, tolerability, and various clinical and functional outcomes related to treatment. Unless this phase is done expertly and meticulously, a patient’s remission, recovery, and return to wellness may be elusive and relapse or complications may develop.
We psychiatrists perform the Herculean task of connecting the dots many times a day on a heterogeneous group of patients with various psychopathologies, and we appear to do it effortlessly. This is a gratifying testimonial to the extensive and arduous years of training it takes to become skillful psychiatric physicians.
We always assume that other professionals also are connecting dots effectively in their respective areas of responsibility. Failure to connect the dots could result in a minor setback, or, in some cases, a catastrophic event. Aristotle defined “virtue” as excelling in one’s job. When we do our job well—diagnosing and healing mental, emotional, and behavioral brain disorders, preventing harm to self and others, and restoring wellness to ailing individuals—we psychiatrists are accomplishing “virtuous” acts and thus earn the privilege to be called “virtuosos.”
Psychosis in women: Consider midlife medical and psychological triggers
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
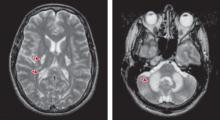
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
How to talk to older patients about medication and alcohol misuse
Serotonin syndrome or NMS? Clues to diagnosis
Symptoms of serotonin syndrome and neuroleptic malignant syndrome (NMS) are similar—mental status changes, autonomic dysfunction, and neuromuscular abnormalities—making the syndromes difficult to differentiate. However, therapeutic interventions and the mortality rates associated with these syndromes are widely divergent.
Because many medication regimens for treatment-resistant mood disorders modulate both serotonin and dopamine systems, psychiatrists must be prepared at any time to recognize either syndrome and quickly initiate appropriate treatment. For this, we rely on disease course, lab findings and vital signs, and the physical exam.
Clinical course
Serotonin syndrome symptoms can develop within minutes to hours after the administration of an agent that increases central serotonergic tone, such as a selective serotonin reuptake inhibitor. After rapid onset, serotonin syndrome symptoms may improve or even resolve within <24 hours. NMS, on the other hand, can develop days to weeks after the administration of a dopamine antagonist—such as an antipsychotic—and may take 3 to 14 days to resolve.
Labs and vital signs
The triad of fever, leukocytosis, and increased creatine kinase (CK) are associated with NMS. Hyperthermia is present in at least 90% of cases,1 although, some definitions of NMS list fever as a sine qua non. Leukocytosis and elevated hepatic transaminases are reported in at least 75% of NMS cases and increased CK in >90% of cases.1,2 These signs may be present in serotonin syndrome but are less common.
Although the pathophysiology of NMS is unclear and literature is limited, some case series report iron deficiency in >95% of cases.3 If this finding were replicated on a larger scale, iron deficiency might be a sensitive, rapid, and inexpensive test to help diagnose atypical NMS presentations. Larger studies are needed before clinicians can rely on this laboratory finding to diagnose NMS.
Physical exam findings
Neuromuscular manifestations also can help distinguish serotonin syndrome from NMS. Physicians often and rightly associate muscle rigidity with NMS. This finding also is present in approximately one-half of serotonin syndrome cases, however. Hyperreflexia and myoclonus, if present, may suggest serotonin syndrome.
1. Mills KC. Serotonin syndrome. A clinical update. Crit Care Clin. 1997;12(4):763-783.
2. Rosebush P, Stewart T. A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry. 1989;146:717-725.
3. Rosebush P, Mazurek M. Serum iron and neuroleptic malignant syndrome. Lancet. 1991;338(8760):149-151.
Symptoms of serotonin syndrome and neuroleptic malignant syndrome (NMS) are similar—mental status changes, autonomic dysfunction, and neuromuscular abnormalities—making the syndromes difficult to differentiate. However, therapeutic interventions and the mortality rates associated with these syndromes are widely divergent.
Because many medication regimens for treatment-resistant mood disorders modulate both serotonin and dopamine systems, psychiatrists must be prepared at any time to recognize either syndrome and quickly initiate appropriate treatment. For this, we rely on disease course, lab findings and vital signs, and the physical exam.
Clinical course
Serotonin syndrome symptoms can develop within minutes to hours after the administration of an agent that increases central serotonergic tone, such as a selective serotonin reuptake inhibitor. After rapid onset, serotonin syndrome symptoms may improve or even resolve within <24 hours. NMS, on the other hand, can develop days to weeks after the administration of a dopamine antagonist—such as an antipsychotic—and may take 3 to 14 days to resolve.
Labs and vital signs
The triad of fever, leukocytosis, and increased creatine kinase (CK) are associated with NMS. Hyperthermia is present in at least 90% of cases,1 although, some definitions of NMS list fever as a sine qua non. Leukocytosis and elevated hepatic transaminases are reported in at least 75% of NMS cases and increased CK in >90% of cases.1,2 These signs may be present in serotonin syndrome but are less common.
Although the pathophysiology of NMS is unclear and literature is limited, some case series report iron deficiency in >95% of cases.3 If this finding were replicated on a larger scale, iron deficiency might be a sensitive, rapid, and inexpensive test to help diagnose atypical NMS presentations. Larger studies are needed before clinicians can rely on this laboratory finding to diagnose NMS.
Physical exam findings
Neuromuscular manifestations also can help distinguish serotonin syndrome from NMS. Physicians often and rightly associate muscle rigidity with NMS. This finding also is present in approximately one-half of serotonin syndrome cases, however. Hyperreflexia and myoclonus, if present, may suggest serotonin syndrome.
Symptoms of serotonin syndrome and neuroleptic malignant syndrome (NMS) are similar—mental status changes, autonomic dysfunction, and neuromuscular abnormalities—making the syndromes difficult to differentiate. However, therapeutic interventions and the mortality rates associated with these syndromes are widely divergent.
Because many medication regimens for treatment-resistant mood disorders modulate both serotonin and dopamine systems, psychiatrists must be prepared at any time to recognize either syndrome and quickly initiate appropriate treatment. For this, we rely on disease course, lab findings and vital signs, and the physical exam.
Clinical course
Serotonin syndrome symptoms can develop within minutes to hours after the administration of an agent that increases central serotonergic tone, such as a selective serotonin reuptake inhibitor. After rapid onset, serotonin syndrome symptoms may improve or even resolve within <24 hours. NMS, on the other hand, can develop days to weeks after the administration of a dopamine antagonist—such as an antipsychotic—and may take 3 to 14 days to resolve.
Labs and vital signs
The triad of fever, leukocytosis, and increased creatine kinase (CK) are associated with NMS. Hyperthermia is present in at least 90% of cases,1 although, some definitions of NMS list fever as a sine qua non. Leukocytosis and elevated hepatic transaminases are reported in at least 75% of NMS cases and increased CK in >90% of cases.1,2 These signs may be present in serotonin syndrome but are less common.
Although the pathophysiology of NMS is unclear and literature is limited, some case series report iron deficiency in >95% of cases.3 If this finding were replicated on a larger scale, iron deficiency might be a sensitive, rapid, and inexpensive test to help diagnose atypical NMS presentations. Larger studies are needed before clinicians can rely on this laboratory finding to diagnose NMS.
Physical exam findings
Neuromuscular manifestations also can help distinguish serotonin syndrome from NMS. Physicians often and rightly associate muscle rigidity with NMS. This finding also is present in approximately one-half of serotonin syndrome cases, however. Hyperreflexia and myoclonus, if present, may suggest serotonin syndrome.
1. Mills KC. Serotonin syndrome. A clinical update. Crit Care Clin. 1997;12(4):763-783.
2. Rosebush P, Stewart T. A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry. 1989;146:717-725.
3. Rosebush P, Mazurek M. Serum iron and neuroleptic malignant syndrome. Lancet. 1991;338(8760):149-151.
1. Mills KC. Serotonin syndrome. A clinical update. Crit Care Clin. 1997;12(4):763-783.
2. Rosebush P, Stewart T. A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry. 1989;146:717-725.
3. Rosebush P, Mazurek M. Serum iron and neuroleptic malignant syndrome. Lancet. 1991;338(8760):149-151.
Aspirin to prevent cardiovascular events: Weighing risks and benefits
Dr. Xiong is assistant clinical professor, departments of internal medicine and psychiatry and behavioral sciences, University of California, Davis. Dr. Kenedi is an adjunct professor of psychiatry at Duke University Medical Center in Durham, NC, and a consultant (attending physician) in internal medicine and liaison psychiatry, Auckland City Hospital, Auckland, New Zealand.
Principal Source: U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;150:396-404.
- Consider discussing or recommending daily aspirin for men age 45 to 79 and women age 55 to 79 who are at risk for CVD, such as those who smoke or have diabetes.
- Psychiatric patients are at higher risk of CVD and often face systemic barriers to medical care. Collaborate with primary care physicians to determine which patients are good candidates for daily aspirin therapy.
- In psychiatric patients, watch for a potential drug-drug interaction between aspirin and valproate and increased risk of bleeding with selective serotonin reuptake inhibitors.
- Aspirin is associated with increased risk of serious gastrointestinal (GI) bleeding, hematuria, easy bruising, and epistaxis. Risk factors for GI bleeding include upper GI pain, history of GI ulcers, nonsteroidal anti-inflammatory drug (NSAID) use, alcohol dependence, and other anticoagulant use.
Cardiovascular disease (CVD) is the leading cause of death in the United States, accounting for >50% of all deaths. In persons age >40, the lifetime risk of death from CVD is 2 in 3 for men and more than 1 in 2 for women.1 Persons with severe mental illness have nearly twice the risk of death from CVD compared with the general population, which may be attributed to:
- lifestyle factors, including poor diet, lack of exercise, and tobacco dependence2
- antipsychotic medications, which have been shown to increase the risk of CVD3
- lower likelihood of undergoing cardiovascular procedures—including percutaneous transluminal coronary angioplasty and coronary artery bypass graft surgery—after myocardial infarction (MI).4
Psychiatrists are often the primary contact for patients with mental illness, giving us an opportunity to collaborate with primary care physicians and apply preventative measures that can reduce illness and improve patients’ morbidity and mortality. In addition to evaluating patients for possible hypercholesterolemia and diabetes, adding daily aspirin for primary prevention of heart attacks and strokes is an easily implementable option that could make a real difference in their health and quality of life.
New aspirin recommendations
The U.S. Preventive Services Task Force (USPSTF) found evidence that daily aspirin decreases the incidence of MI in men and ischemic strokes in women.1 However, total mortality for either gender was not significantly reduced.5 The USPSTF’s updated recommendations reflect results of the Women’s Health Study6 with different guidelines for men and women.
The USPSTF recommends daily aspirin for men age 45 to 79 and for women age 55 to 79 when the benefits of decreased MI for men and ischemic strokes for women outweigh the risks of increased GI bleeding ( Table 1 ).1 This grade A recommendation means there is high certainty of substantial net benefit.
Aspirin is not recommended for patients age ≥80 because of insufficient evidence of harm or benefit. The risks of MI in men age <45 and stroke in women age <55 are low, and daily aspirin generally is not indicated.
Optimal aspirin dose is unclear. The USPSTF recommends approximately 75 mg/d (effectively 81 mg/d or 1 “baby aspirin” in most U.S. settings). Higher aspirin doses might not be more effective for primary prevention and could increase the risk of GI bleeding. Note that some patients with a history of cardiovascular or cerebrovascular events might receive higher aspirin doses for secondary prevention of additional injury.
Risk assessment. In addition to age, other risk factors for CVD include:
- diabetes
- high total cholesterol (>240 mg/dL)
- low high-density lipoprotein cholesterol or so-called “good cholesterol” (<40 mg/dL for men, <50 mg/dL for women)
- hypertension
- smoking
- family history.
Several online tools—based on data from the Framingham Heart Study and other cohorts—can help estimate a patient’s CVD risk ( see Related Resources ), or consult with your patient’s primary care physician.
Potential harm of aspirin. USPSTF considers age and gender the most important risk factors for GI bleeding. GI bleeding is defined as serious hemorrhage, perforation, or other complications that could lead to hospitalization or death. Other risk factors include:
- upper GI pain
- history of gastric or duodenal ulcers
- NSAID use
- heavy, regular alcohol consumption.
In general, men have twice the risk of GI bleeding compared with women.1 The baseline number of GI bleeding events for individuals without a history of GI pain or bleeds taking daily aspirin is 4 per 10,000 person-years for women and 8 per 10,000 for men.1 Patients with preexisting GI ulcers who receive daily aspirin have more than 2 to 3 times the baseline risk of serious GI bleeding.7 NSAIDs taken with daily aspirin can quadruple the risk of GI bleeding compared with aspirin use alone, although antacid therapy can reduce this risk.8 Co-administered anticoagulants (eg, warfarin) also significantly increase the risk—especially when compliance with medication and monitoring is poor. Aspirin also increases the risk of hematuria, easy bruising, and epistaxis.
Because consuming >3 standard drinks a day also increases the risk of GI bleeding by up to 6 fold, patients with untreated chronic alcohol abuse or dependence might not be good candidates for daily aspirin therapy.9 Contrary to popular belief and pharmaceutical marketing, enteric-coated tablets do not seem to reduce the risk of bleeding because aspirin impacts platelet function, not the lining of the stomach.
Table 1
USPSTF recommendations for daily aspirin use
in primary prevention of cardiovascular disease
| Population | Recommendation |
|---|---|
| Men age 45 to 79 | Encourage aspirin use when potential benefit due to a reduction in myocardial infarctions outweighs potential increased risk of GI bleeding |
| Women age 55 to 79 | Encourage aspirin use when potential benefit of a reduction in ischemic strokes outweighs potential increased risk of GI bleeding |
| Men age <45 | Do not recommend aspirin use for cardiovascular prevention |
| Women age <55 | Do not recommend aspirin use for cardiovascular prevention |
| Men and women age ≥80 years | Insufficient evidence to make recommendations |
| GI: gastrointestinal; USPSTF: U.S. Preventive Services Task Force | |
| Source: Reference 1 | |
Aspirin for psychiatric patients
Patients who have serious mental illness are at increased risk for CVD and often experience systemic barriers to receiving appropriate medical care.10 Psychiatrists can provide and advocate for primary care services for our patients, including daily aspirin use to prevent CVD when appropriate, and encourage a closer relationship with a primary care physician before an adverse event occurs. Aspirin use in psychiatric patients is associated with:
- potential drug-drug interaction with valproate11
- mildly increased risk of bleeding as a result of reduced platelet function with the use of selective serotonin reuptake inhibitors.12
Balancing benefits vs risks. The USPSTF recommendation assumes that the value of preventing 1 MI or stroke is roughly equivalent to (or slightly less than) the cost of 1 GI bleeding event caused by aspirin. For example, among 1,000 men age 45 to 79 who have a ≥4% risk of MI over 10 years, 12.8 MIs would be prevented for every 8 GI bleeds caused by aspirin by following the current recommendations.1
The USPSTF guidelines are based on average levels of risk for age and gender. Some men age <45 may decide that it is more important to avoid a cardiovascular event rather than an episode of GI bleeding and might choose to begin daily aspirin. Aspirin use should be discouraged in most patients at high risk for GI bleeding. The point where the potential benefits outweigh the risks must be determined on an individual basis ( Table 2 ).
Table 2
Aspirin to prevent cardiovascular disease and stroke:
When benefits outweigh risks
| Men | Women | ||
|---|---|---|---|
| Age | 10-year CVD risk* | Age | 10-year stroke risk* |
| 45 to 59 | ≥4% | 55 to 59 | ≥3% |
| 60 to 69 | ≥9% | 60 to 69 | ≥8% |
| 70 to 79 | ≥12% | 70 to 79 | ≥11% |
| *Risk thresholds where aspirin should be started. Estimate risk using an online calculator based on the Framingham Heart Study at www.framinghamheartstudy.org/risk/coronary.html or consult with your patient’s primary care physician | |||
| CVD: cardiovascular disease | |||
| Source: Reference 1 | |||
- National Cholesterol Education Program. Online heart attack risk assessment tool. http://hp2010.nhlbihin.net/atpiii/calculator.asp.
- Framingham Heart study calculator. www.framinghamheartstudy.org/risk/coronary.html.
- National Cholesterol Education Program. www.nhlbi.nih.gov/health/public/heart/chol/wyntk.htm#risk.
- Colorado Neurological Institute. Online stroke risk assessment tool. www.thecni.org/Public/CNICenters/StrokeCenter/StrokeRiskCalculator/index.cfm.
- Agency for Healthcare Research and Quality. Fact sheet on aspirin to prevent cardiovascular disease. www.ahrq.gov/clinic/cvd/aspprovider.htm.
Drug brand names
- Valproate • Depacon
- Warfarin • Coumadin
Disclosures
Dr. Xiong reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Kenedi receives grant/research support from Duke University Medical Center and Auckland University.
1. U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;150:396-404.
2. Hert MD, Schreurs V, Vancampfort D, et al. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8:15-22.
3. Prevalence of metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III Schizophr Res. 2005;80:19-32.
4. Druss B, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;26:506-511.
5. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
6. Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293-1304.
7. Serrano P, Lanas A, Arroyo MT, et al. Risk of upper gastrointestinal bleeding in patients taking low-dose aspirin for the prevention of cardiovascular diseases. Aliment Pharmacol Ther. 2002;16:1945-1953.
8. Lanas A, Garcia-Rodriguez LA, Arroyo MT, et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut. 2006;55:1731-1738.
9. Kelly JP, Kaufman DW, Koff RS, et al. Alcohol consumption and the risk of major upper gastrointestinal bleeding. Am J Gastroenterol. 1995;90:1058-1064.
10. Druss BG, Marcu SC, Campbell J, et al. Medical services for clients in community mental health centers: results from a national survey. Psych Serv. 2008;59:917-920.
11. Sandson NB, Marcucci C, Bourke DL, et al. An interaction between aspirin and valproate: the relevance of plasma protein displacement drug-drug interactions. Am J Psychiatry. 2006;163:1891-1896.
12. de Abajo FJ, Rodriguez LA, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319:1106-1109.
Dr. Xiong is assistant clinical professor, departments of internal medicine and psychiatry and behavioral sciences, University of California, Davis. Dr. Kenedi is an adjunct professor of psychiatry at Duke University Medical Center in Durham, NC, and a consultant (attending physician) in internal medicine and liaison psychiatry, Auckland City Hospital, Auckland, New Zealand.
Principal Source: U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;150:396-404.
- Consider discussing or recommending daily aspirin for men age 45 to 79 and women age 55 to 79 who are at risk for CVD, such as those who smoke or have diabetes.
- Psychiatric patients are at higher risk of CVD and often face systemic barriers to medical care. Collaborate with primary care physicians to determine which patients are good candidates for daily aspirin therapy.
- In psychiatric patients, watch for a potential drug-drug interaction between aspirin and valproate and increased risk of bleeding with selective serotonin reuptake inhibitors.
- Aspirin is associated with increased risk of serious gastrointestinal (GI) bleeding, hematuria, easy bruising, and epistaxis. Risk factors for GI bleeding include upper GI pain, history of GI ulcers, nonsteroidal anti-inflammatory drug (NSAID) use, alcohol dependence, and other anticoagulant use.
Cardiovascular disease (CVD) is the leading cause of death in the United States, accounting for >50% of all deaths. In persons age >40, the lifetime risk of death from CVD is 2 in 3 for men and more than 1 in 2 for women.1 Persons with severe mental illness have nearly twice the risk of death from CVD compared with the general population, which may be attributed to:
- lifestyle factors, including poor diet, lack of exercise, and tobacco dependence2
- antipsychotic medications, which have been shown to increase the risk of CVD3
- lower likelihood of undergoing cardiovascular procedures—including percutaneous transluminal coronary angioplasty and coronary artery bypass graft surgery—after myocardial infarction (MI).4
Psychiatrists are often the primary contact for patients with mental illness, giving us an opportunity to collaborate with primary care physicians and apply preventative measures that can reduce illness and improve patients’ morbidity and mortality. In addition to evaluating patients for possible hypercholesterolemia and diabetes, adding daily aspirin for primary prevention of heart attacks and strokes is an easily implementable option that could make a real difference in their health and quality of life.
New aspirin recommendations
The U.S. Preventive Services Task Force (USPSTF) found evidence that daily aspirin decreases the incidence of MI in men and ischemic strokes in women.1 However, total mortality for either gender was not significantly reduced.5 The USPSTF’s updated recommendations reflect results of the Women’s Health Study6 with different guidelines for men and women.
The USPSTF recommends daily aspirin for men age 45 to 79 and for women age 55 to 79 when the benefits of decreased MI for men and ischemic strokes for women outweigh the risks of increased GI bleeding ( Table 1 ).1 This grade A recommendation means there is high certainty of substantial net benefit.
Aspirin is not recommended for patients age ≥80 because of insufficient evidence of harm or benefit. The risks of MI in men age <45 and stroke in women age <55 are low, and daily aspirin generally is not indicated.
Optimal aspirin dose is unclear. The USPSTF recommends approximately 75 mg/d (effectively 81 mg/d or 1 “baby aspirin” in most U.S. settings). Higher aspirin doses might not be more effective for primary prevention and could increase the risk of GI bleeding. Note that some patients with a history of cardiovascular or cerebrovascular events might receive higher aspirin doses for secondary prevention of additional injury.
Risk assessment. In addition to age, other risk factors for CVD include:
- diabetes
- high total cholesterol (>240 mg/dL)
- low high-density lipoprotein cholesterol or so-called “good cholesterol” (<40 mg/dL for men, <50 mg/dL for women)
- hypertension
- smoking
- family history.
Several online tools—based on data from the Framingham Heart Study and other cohorts—can help estimate a patient’s CVD risk ( see Related Resources ), or consult with your patient’s primary care physician.
Potential harm of aspirin. USPSTF considers age and gender the most important risk factors for GI bleeding. GI bleeding is defined as serious hemorrhage, perforation, or other complications that could lead to hospitalization or death. Other risk factors include:
- upper GI pain
- history of gastric or duodenal ulcers
- NSAID use
- heavy, regular alcohol consumption.
In general, men have twice the risk of GI bleeding compared with women.1 The baseline number of GI bleeding events for individuals without a history of GI pain or bleeds taking daily aspirin is 4 per 10,000 person-years for women and 8 per 10,000 for men.1 Patients with preexisting GI ulcers who receive daily aspirin have more than 2 to 3 times the baseline risk of serious GI bleeding.7 NSAIDs taken with daily aspirin can quadruple the risk of GI bleeding compared with aspirin use alone, although antacid therapy can reduce this risk.8 Co-administered anticoagulants (eg, warfarin) also significantly increase the risk—especially when compliance with medication and monitoring is poor. Aspirin also increases the risk of hematuria, easy bruising, and epistaxis.
Because consuming >3 standard drinks a day also increases the risk of GI bleeding by up to 6 fold, patients with untreated chronic alcohol abuse or dependence might not be good candidates for daily aspirin therapy.9 Contrary to popular belief and pharmaceutical marketing, enteric-coated tablets do not seem to reduce the risk of bleeding because aspirin impacts platelet function, not the lining of the stomach.
Table 1
USPSTF recommendations for daily aspirin use
in primary prevention of cardiovascular disease
| Population | Recommendation |
|---|---|
| Men age 45 to 79 | Encourage aspirin use when potential benefit due to a reduction in myocardial infarctions outweighs potential increased risk of GI bleeding |
| Women age 55 to 79 | Encourage aspirin use when potential benefit of a reduction in ischemic strokes outweighs potential increased risk of GI bleeding |
| Men age <45 | Do not recommend aspirin use for cardiovascular prevention |
| Women age <55 | Do not recommend aspirin use for cardiovascular prevention |
| Men and women age ≥80 years | Insufficient evidence to make recommendations |
| GI: gastrointestinal; USPSTF: U.S. Preventive Services Task Force | |
| Source: Reference 1 | |
Aspirin for psychiatric patients
Patients who have serious mental illness are at increased risk for CVD and often experience systemic barriers to receiving appropriate medical care.10 Psychiatrists can provide and advocate for primary care services for our patients, including daily aspirin use to prevent CVD when appropriate, and encourage a closer relationship with a primary care physician before an adverse event occurs. Aspirin use in psychiatric patients is associated with:
- potential drug-drug interaction with valproate11
- mildly increased risk of bleeding as a result of reduced platelet function with the use of selective serotonin reuptake inhibitors.12
Balancing benefits vs risks. The USPSTF recommendation assumes that the value of preventing 1 MI or stroke is roughly equivalent to (or slightly less than) the cost of 1 GI bleeding event caused by aspirin. For example, among 1,000 men age 45 to 79 who have a ≥4% risk of MI over 10 years, 12.8 MIs would be prevented for every 8 GI bleeds caused by aspirin by following the current recommendations.1
The USPSTF guidelines are based on average levels of risk for age and gender. Some men age <45 may decide that it is more important to avoid a cardiovascular event rather than an episode of GI bleeding and might choose to begin daily aspirin. Aspirin use should be discouraged in most patients at high risk for GI bleeding. The point where the potential benefits outweigh the risks must be determined on an individual basis ( Table 2 ).
Table 2
Aspirin to prevent cardiovascular disease and stroke:
When benefits outweigh risks
| Men | Women | ||
|---|---|---|---|
| Age | 10-year CVD risk* | Age | 10-year stroke risk* |
| 45 to 59 | ≥4% | 55 to 59 | ≥3% |
| 60 to 69 | ≥9% | 60 to 69 | ≥8% |
| 70 to 79 | ≥12% | 70 to 79 | ≥11% |
| *Risk thresholds where aspirin should be started. Estimate risk using an online calculator based on the Framingham Heart Study at www.framinghamheartstudy.org/risk/coronary.html or consult with your patient’s primary care physician | |||
| CVD: cardiovascular disease | |||
| Source: Reference 1 | |||
- National Cholesterol Education Program. Online heart attack risk assessment tool. http://hp2010.nhlbihin.net/atpiii/calculator.asp.
- Framingham Heart study calculator. www.framinghamheartstudy.org/risk/coronary.html.
- National Cholesterol Education Program. www.nhlbi.nih.gov/health/public/heart/chol/wyntk.htm#risk.
- Colorado Neurological Institute. Online stroke risk assessment tool. www.thecni.org/Public/CNICenters/StrokeCenter/StrokeRiskCalculator/index.cfm.
- Agency for Healthcare Research and Quality. Fact sheet on aspirin to prevent cardiovascular disease. www.ahrq.gov/clinic/cvd/aspprovider.htm.
Drug brand names
- Valproate • Depacon
- Warfarin • Coumadin
Disclosures
Dr. Xiong reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Kenedi receives grant/research support from Duke University Medical Center and Auckland University.
Dr. Xiong is assistant clinical professor, departments of internal medicine and psychiatry and behavioral sciences, University of California, Davis. Dr. Kenedi is an adjunct professor of psychiatry at Duke University Medical Center in Durham, NC, and a consultant (attending physician) in internal medicine and liaison psychiatry, Auckland City Hospital, Auckland, New Zealand.
Principal Source: U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;150:396-404.
- Consider discussing or recommending daily aspirin for men age 45 to 79 and women age 55 to 79 who are at risk for CVD, such as those who smoke or have diabetes.
- Psychiatric patients are at higher risk of CVD and often face systemic barriers to medical care. Collaborate with primary care physicians to determine which patients are good candidates for daily aspirin therapy.
- In psychiatric patients, watch for a potential drug-drug interaction between aspirin and valproate and increased risk of bleeding with selective serotonin reuptake inhibitors.
- Aspirin is associated with increased risk of serious gastrointestinal (GI) bleeding, hematuria, easy bruising, and epistaxis. Risk factors for GI bleeding include upper GI pain, history of GI ulcers, nonsteroidal anti-inflammatory drug (NSAID) use, alcohol dependence, and other anticoagulant use.
Cardiovascular disease (CVD) is the leading cause of death in the United States, accounting for >50% of all deaths. In persons age >40, the lifetime risk of death from CVD is 2 in 3 for men and more than 1 in 2 for women.1 Persons with severe mental illness have nearly twice the risk of death from CVD compared with the general population, which may be attributed to:
- lifestyle factors, including poor diet, lack of exercise, and tobacco dependence2
- antipsychotic medications, which have been shown to increase the risk of CVD3
- lower likelihood of undergoing cardiovascular procedures—including percutaneous transluminal coronary angioplasty and coronary artery bypass graft surgery—after myocardial infarction (MI).4
Psychiatrists are often the primary contact for patients with mental illness, giving us an opportunity to collaborate with primary care physicians and apply preventative measures that can reduce illness and improve patients’ morbidity and mortality. In addition to evaluating patients for possible hypercholesterolemia and diabetes, adding daily aspirin for primary prevention of heart attacks and strokes is an easily implementable option that could make a real difference in their health and quality of life.
New aspirin recommendations
The U.S. Preventive Services Task Force (USPSTF) found evidence that daily aspirin decreases the incidence of MI in men and ischemic strokes in women.1 However, total mortality for either gender was not significantly reduced.5 The USPSTF’s updated recommendations reflect results of the Women’s Health Study6 with different guidelines for men and women.
The USPSTF recommends daily aspirin for men age 45 to 79 and for women age 55 to 79 when the benefits of decreased MI for men and ischemic strokes for women outweigh the risks of increased GI bleeding ( Table 1 ).1 This grade A recommendation means there is high certainty of substantial net benefit.
Aspirin is not recommended for patients age ≥80 because of insufficient evidence of harm or benefit. The risks of MI in men age <45 and stroke in women age <55 are low, and daily aspirin generally is not indicated.
Optimal aspirin dose is unclear. The USPSTF recommends approximately 75 mg/d (effectively 81 mg/d or 1 “baby aspirin” in most U.S. settings). Higher aspirin doses might not be more effective for primary prevention and could increase the risk of GI bleeding. Note that some patients with a history of cardiovascular or cerebrovascular events might receive higher aspirin doses for secondary prevention of additional injury.
Risk assessment. In addition to age, other risk factors for CVD include:
- diabetes
- high total cholesterol (>240 mg/dL)
- low high-density lipoprotein cholesterol or so-called “good cholesterol” (<40 mg/dL for men, <50 mg/dL for women)
- hypertension
- smoking
- family history.
Several online tools—based on data from the Framingham Heart Study and other cohorts—can help estimate a patient’s CVD risk ( see Related Resources ), or consult with your patient’s primary care physician.
Potential harm of aspirin. USPSTF considers age and gender the most important risk factors for GI bleeding. GI bleeding is defined as serious hemorrhage, perforation, or other complications that could lead to hospitalization or death. Other risk factors include:
- upper GI pain
- history of gastric or duodenal ulcers
- NSAID use
- heavy, regular alcohol consumption.
In general, men have twice the risk of GI bleeding compared with women.1 The baseline number of GI bleeding events for individuals without a history of GI pain or bleeds taking daily aspirin is 4 per 10,000 person-years for women and 8 per 10,000 for men.1 Patients with preexisting GI ulcers who receive daily aspirin have more than 2 to 3 times the baseline risk of serious GI bleeding.7 NSAIDs taken with daily aspirin can quadruple the risk of GI bleeding compared with aspirin use alone, although antacid therapy can reduce this risk.8 Co-administered anticoagulants (eg, warfarin) also significantly increase the risk—especially when compliance with medication and monitoring is poor. Aspirin also increases the risk of hematuria, easy bruising, and epistaxis.
Because consuming >3 standard drinks a day also increases the risk of GI bleeding by up to 6 fold, patients with untreated chronic alcohol abuse or dependence might not be good candidates for daily aspirin therapy.9 Contrary to popular belief and pharmaceutical marketing, enteric-coated tablets do not seem to reduce the risk of bleeding because aspirin impacts platelet function, not the lining of the stomach.
Table 1
USPSTF recommendations for daily aspirin use
in primary prevention of cardiovascular disease
| Population | Recommendation |
|---|---|
| Men age 45 to 79 | Encourage aspirin use when potential benefit due to a reduction in myocardial infarctions outweighs potential increased risk of GI bleeding |
| Women age 55 to 79 | Encourage aspirin use when potential benefit of a reduction in ischemic strokes outweighs potential increased risk of GI bleeding |
| Men age <45 | Do not recommend aspirin use for cardiovascular prevention |
| Women age <55 | Do not recommend aspirin use for cardiovascular prevention |
| Men and women age ≥80 years | Insufficient evidence to make recommendations |
| GI: gastrointestinal; USPSTF: U.S. Preventive Services Task Force | |
| Source: Reference 1 | |
Aspirin for psychiatric patients
Patients who have serious mental illness are at increased risk for CVD and often experience systemic barriers to receiving appropriate medical care.10 Psychiatrists can provide and advocate for primary care services for our patients, including daily aspirin use to prevent CVD when appropriate, and encourage a closer relationship with a primary care physician before an adverse event occurs. Aspirin use in psychiatric patients is associated with:
- potential drug-drug interaction with valproate11
- mildly increased risk of bleeding as a result of reduced platelet function with the use of selective serotonin reuptake inhibitors.12
Balancing benefits vs risks. The USPSTF recommendation assumes that the value of preventing 1 MI or stroke is roughly equivalent to (or slightly less than) the cost of 1 GI bleeding event caused by aspirin. For example, among 1,000 men age 45 to 79 who have a ≥4% risk of MI over 10 years, 12.8 MIs would be prevented for every 8 GI bleeds caused by aspirin by following the current recommendations.1
The USPSTF guidelines are based on average levels of risk for age and gender. Some men age <45 may decide that it is more important to avoid a cardiovascular event rather than an episode of GI bleeding and might choose to begin daily aspirin. Aspirin use should be discouraged in most patients at high risk for GI bleeding. The point where the potential benefits outweigh the risks must be determined on an individual basis ( Table 2 ).
Table 2
Aspirin to prevent cardiovascular disease and stroke:
When benefits outweigh risks
| Men | Women | ||
|---|---|---|---|
| Age | 10-year CVD risk* | Age | 10-year stroke risk* |
| 45 to 59 | ≥4% | 55 to 59 | ≥3% |
| 60 to 69 | ≥9% | 60 to 69 | ≥8% |
| 70 to 79 | ≥12% | 70 to 79 | ≥11% |
| *Risk thresholds where aspirin should be started. Estimate risk using an online calculator based on the Framingham Heart Study at www.framinghamheartstudy.org/risk/coronary.html or consult with your patient’s primary care physician | |||
| CVD: cardiovascular disease | |||
| Source: Reference 1 | |||
- National Cholesterol Education Program. Online heart attack risk assessment tool. http://hp2010.nhlbihin.net/atpiii/calculator.asp.
- Framingham Heart study calculator. www.framinghamheartstudy.org/risk/coronary.html.
- National Cholesterol Education Program. www.nhlbi.nih.gov/health/public/heart/chol/wyntk.htm#risk.
- Colorado Neurological Institute. Online stroke risk assessment tool. www.thecni.org/Public/CNICenters/StrokeCenter/StrokeRiskCalculator/index.cfm.
- Agency for Healthcare Research and Quality. Fact sheet on aspirin to prevent cardiovascular disease. www.ahrq.gov/clinic/cvd/aspprovider.htm.
Drug brand names
- Valproate • Depacon
- Warfarin • Coumadin
Disclosures
Dr. Xiong reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Kenedi receives grant/research support from Duke University Medical Center and Auckland University.
1. U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;150:396-404.
2. Hert MD, Schreurs V, Vancampfort D, et al. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8:15-22.
3. Prevalence of metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III Schizophr Res. 2005;80:19-32.
4. Druss B, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;26:506-511.
5. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
6. Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293-1304.
7. Serrano P, Lanas A, Arroyo MT, et al. Risk of upper gastrointestinal bleeding in patients taking low-dose aspirin for the prevention of cardiovascular diseases. Aliment Pharmacol Ther. 2002;16:1945-1953.
8. Lanas A, Garcia-Rodriguez LA, Arroyo MT, et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut. 2006;55:1731-1738.
9. Kelly JP, Kaufman DW, Koff RS, et al. Alcohol consumption and the risk of major upper gastrointestinal bleeding. Am J Gastroenterol. 1995;90:1058-1064.
10. Druss BG, Marcu SC, Campbell J, et al. Medical services for clients in community mental health centers: results from a national survey. Psych Serv. 2008;59:917-920.
11. Sandson NB, Marcucci C, Bourke DL, et al. An interaction between aspirin and valproate: the relevance of plasma protein displacement drug-drug interactions. Am J Psychiatry. 2006;163:1891-1896.
12. de Abajo FJ, Rodriguez LA, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319:1106-1109.
1. U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;150:396-404.
2. Hert MD, Schreurs V, Vancampfort D, et al. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8:15-22.
3. Prevalence of metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III Schizophr Res. 2005;80:19-32.
4. Druss B, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;26:506-511.
5. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
6. Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293-1304.
7. Serrano P, Lanas A, Arroyo MT, et al. Risk of upper gastrointestinal bleeding in patients taking low-dose aspirin for the prevention of cardiovascular diseases. Aliment Pharmacol Ther. 2002;16:1945-1953.
8. Lanas A, Garcia-Rodriguez LA, Arroyo MT, et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut. 2006;55:1731-1738.
9. Kelly JP, Kaufman DW, Koff RS, et al. Alcohol consumption and the risk of major upper gastrointestinal bleeding. Am J Gastroenterol. 1995;90:1058-1064.
10. Druss BG, Marcu SC, Campbell J, et al. Medical services for clients in community mental health centers: results from a national survey. Psych Serv. 2008;59:917-920.
11. Sandson NB, Marcucci C, Bourke DL, et al. An interaction between aspirin and valproate: the relevance of plasma protein displacement drug-drug interactions. Am J Psychiatry. 2006;163:1891-1896.
12. de Abajo FJ, Rodriguez LA, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319:1106-1109.
Chasing the dragon
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
SAD: Is seasonal affective disorder a bipolar variant?
Ms. S, age 24, is referred to our team in early December by her primary care physician for “fatigue.” The patient describes going to bed and falling asleep before 9:30 these winter evenings, whereas in summer she went to bed at 11 PM. She craves bread, pasta, and sweets and reports increased appetite in winter compared with summer. Her mood is low, and she misses warm-weather activities of gardening and walking. Fatigue and difficulty concentrating are causing her problems at work and school.
Her history reveals mood elevation in spring as days become longer, with a clear change at approximately March 10 to 20. She reports “spring fever” and feeling “great” last year as soon as daylight saving time began. She slept only 3 hours a night and had a burst of ideas to expand her small business. She threw herself into her work, feeling she was making up for lost time and productivity. She also admits to making a large, misguided business investment during that time.
Upon questioning, she recalls that the previous spring she argued with her father and threw a cup of hot tea at him. When interviewed, Ms. S’s mother describes her daughter at that time as having “a very short fuse,” speaking loud and fast, staying up late at night, and looking as though she was not herself.
Seasonal affective disorder (SAD) is an umbrella term for mood disorders that follow a seasonal pattern of recurrence. Bipolar I disorder (BD I) or bipolar II disorder (BD II) with seasonal pattern (BD SP) is the DSM-IV-TR diagnosis for persons with depressive episodes in the fall or winter and mania (BD I) or hypomania (BD II) in spring or summer ( Table 1 ).1
This article compares BD SP with major depressive disorder with seasonal pattern (MDD SP), in which depressive episodes usually occur in fall or winter and fully remit in spring or summer.1 Rather than being categorically distinct from each other, BD SP and MDD SP may represent extreme variants on a seasonal depression continuum from unipolar to bipolar.
Table 1
DSM-IV-TR criteria for seasonal pattern specifier*
| A | A regular pattern of major depressive episodes (MDEs) at a particular time of year (such as fall and/or winter) |
| B | Full remission or change to mania or hypomania at a particular time of year (such as spring or summer) |
| C | 2 seasonal MDEs that followed the pattern described in (A) and (B) occurred in the past 2 years (and no nonseasonal MDEs) |
| D | Seasonal MDEs substantially outnumber nonseasonal MDEs across the lifespan |
Cases do not meet criteria if:
| |
| *Can be applied to a pattern of major depressive episodes in bipolar I disorder, bipolar II disorder, or major depressive disorder | |
| Source: Adapted from reference 1 | |
Overlap of MDD SP and BD SP
The seasonal pattern specifier can be applied to a diagnosis of MDD, BD I, or BD II.1 Seasonality-focused assessments, described below, can help characterize seasonal patterns that do not meet full SP criteria but may deserve clinical attention.
Symptom presentation. MDD SP and BD SP share similar atypical depressive symptom presentations and seasonal recurrence patterns ( Box 1 ). Hypersomnia, hyperphagia, and psychomotor retardation are more prevalent in major depressive episodes of bipolar disorders and SAD than in unipolar or nonseasonal mood disorders.2-4 Individuals with SAD also report fatigue and decreased physical activity,3 both of which are characteristic of bipolar depressive episodes.5
Although psychosis and psychiatric hospitalizations are more common in BD I than unipolar disorders,6 individuals with BD SP are less likely to report psychosis than those with nonseasonal BD.7 Another study found that BD SP patients reported a higher rate of psychiatric hospitalizations than MDD SP patients (28% vs 9.4%).6
Recurrence pattern. Major depressive episodes are highly recurrent in both MDD and BD, with or without a seasonal pattern. Approximately 75% of individuals with MDD experience ≥1 recurrence (mean, 10.8 episodes);8 MDD SP patients report a mean of 13.4 episodes.9 The mean lifetime episodes in BD SP is 20.74, compared with 11.67 in nonseasonal BD.7
Cassidy and Carroll10 measured the frequency of mood episodes in 304 BD patients not assessed for seasonality. Manic episodes peaked in early spring, mixed episodes peaked in late summer or fall, and depressive episodes peaked in fall-winter.
Irregular rhythm. Both BD and MDD SP involve irregularities in daily or circadian rhythms, such as changes in the timing of sleep, melatonin release, and body temperature.3,5,11 Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BD12 and are implicated in the core pathology of BD13 ( Box 2 ). In BD, life events that change social rhythms may disrupt circadian rhythms, triggering mood episodes.5
Etiologic hypotheses for both BD and SAD propose that an external event (life stress in BD; decreased photoperiod in SAD) leads to circadian dysregulation and, in turn, mood episodes. Circadian-related hypotheses for SAD and BD are supported by evidence showing efficacy of treatments that manipulate behavioral and circadian rhythms.
from unipolar to bipolar?
Seasonality refers to the degree of seasonal changes in behavior and mood within an individual. Seasonality scores are normally distributed,a suggesting that seasonality may be continuous in the general population—with some individuals meeting criteria for a seasonal mood disorder:
- A seasonal pattern is reported by approximately 10% to 20% of depressed outpatients with recurrent mood disorders and an estimated 15% to 22% of individuals with bipolar disorder (BD).b
- Persons with BD—seasonal or not—report greater seasonality compared with those with major depressive disorder (MDD).c
Among individuals with seasonal affective disorder, the course is bipolar in an estimated 12% to 22% and unipolar in 78% to 88%.d These estimates may reflect underdiagnosis of BD with seasonal pattern because hypomania is difficult to diagnose retrospectively.e
The bipolar-unipolar continuum includes (in order): BD I, BD II, bipolar disorder not otherwise specified, cyclothymia, bipolar spectrum disorder, and MDD.f In examining the validity of the bipolar spectrum model, Phelps et alg noted:
- At least 3 studies found that all symptoms reported by individuals with unipolar and bipolar diagnoses approach a normal distribution, rather than a bimodal distribution separating unipolar from bipolar symptom profiles.
- Data from 2 population-based studies indicate that subthreshold hypomanic symptoms are more common than and cause as much impairment as symptoms meeting criteria for BD II or I.
Some individuals who meet criteria for MDD with seasonal pattern have summertime periods of transient hypomania and hyperthymia (hypomanic-like periods without clinically significant impairment).h This suggests that the bipolar continuum also may exist among individuals with seasonal pattern mood disorders.
Source: Access reference citations here
Etiologic hypotheses of seasonal affective disorder (SAD) include:
- photoperiodic hypothesis (shorter winter days cause SAD,a perhaps mediated by a summer vs winter difference in duration of nightly melatonin release)b
- phase shift hypothesis (less available light in winter may lead to an inability to synchronize circadian rhythms with sleep/wake rhythms).c
Some case studies of rapid-cycling bipolar disorder (BD) suggest that mood is correlated with daily hours of sunshine and light therapy is antidepressant. Rapid-cycling patients may be hypersensitive to day-to-day changes in photoperiod, analogous to mood changes in response to changes in photoperiod across the seasons in SAD.d
Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BDe and are implicated in the core pathology of BD.f Phase delays also are present in some individuals with SAD and are associated with severity and treatment response.g Preliminary evidence suggests that variation in circadian clock genes is related to both BDf,h and SAD.i
Source: Access reference citations here
CASE CONTINUED: Seasonal pattern revealed
Ms. S was aware that she is vulnerable to depressive episodes in fall and winter but unaware of a pattern of hypomanic/manic episodes in spring and summer. Her family psychiatric history includes a sister diagnosed with BD I (with no seasonal specifier), and a maternal aunt who has attempted suicide several times.
Ms. S agrees to an assessment plan including a diagnostic interview, interviews measuring symptom severity and pattern of recurrence, routine laboratory examination, and self-report questionnaires. These show that she meets DSM-IV-TR criteria for BD I, depressed, moderate, with seasonal pattern.
Her assessment scores are 28 on the Structured Interview Guide for HDRS-seasonal affective disorder version (SIGH-SAD), 17 on the Hamilton Depression Rating Scale (HDRS), and 11 on the atypical subscale. The HDRS and atypical subscale are components of the SIGH-SAD reflecting typical (eg, insomnia, loss of appetite, etc.) and atypical (eg, hypersomnia, increased appetite, etc.) depression symptoms, respectively. Ms. S’s scores exceed the threshold scores defining a BD SP episode (>20 SIGH-SAD + >10 HDRS + >5 atypical subscale14 ). Data from self-report questionnaires corroborate this assessment.
We plan to administer the Hypomania Interview Guide (including Hyperthymia) for Seasonal Affective Disorder (HIGH-SAD) during treatment and the following spring to monitor prospectively for hypomanic symptoms.
Assessment tools
After complete assessment for mood episodes and mood disorders based on DSM-IV-TR, an additional assessment for bipolarity and seasonality may be helpful.1
Screen for bipolarity in patients with SAD to avoid triggering mania or hypomania during treatment. Useful tools include:
- HIGH-SAD15
- the National Institutes of Health Life Chart Method to establish a recurrent pattern of mood episodes and track treatment efficacy16
- assessments that characterize sub-threshold bipolar symptoms, such as the Bipolar Spectrum Diagnostic Scale17 ( see Box 3 ) and the Bipolarity Index.18
Also obtain collateral reports from significant others, review patient records, and use the same mania and hypomania scales for prospective assessment as the next spring approaches.6
Assess seasonality in patients with BD to improve diagnosis and treatment. Characterizing a seasonal pattern may allow you and your patient to predict episodes and treat proactively. Commonly used assessments include the SIGH-SAD and the Structured Clinical Interview for DSM Disorders (SCID) seasonal pattern specifier module.19
The SIGH-SAD measures symptom severity and provides recovery criteria based on changes in scores during treatment. Response is defined as a 50% reduction in symptoms; remission is >50% improvement in SIGH-SAD + HDRS <7 + atypical <7 or HDRS <2 + atypical <10.14
CASE CONTINUED: Treatment begins
Considering Ms. S’s diagnosis of BD I SP and the risk of precipitating mania with light treatment, we recommend starting treatment with a mood stabilizer. We narrow our options to those that have a direct antidepressant effect, with the hope that this may reduce the need for future antidepressant medications. For patients diagnosed with BD II SP, we could consider a regimen without mood stabilizers.
We offer Ms. S lithium, a first-line mood stabilizer with evidence of usefulness in treatment before chronotherapeutic interventions and in preventing suicidal behavior. However, Ms. S prefers our second option, lamotrigine, because she is concerned about lithium’s side effects and required blood draws to check drug levels as well as thyroid and kidney status.
Despite causing some initial drowsiness, her lamotrigine dosage is successfully titrated after 2 weeks of treatment to 300 mg/d, without side effects. Only then do we initiate light treatment, which Ms. S wishes to try before antidepressant medications. She also begins sessions with a therapist trained in cognitive-behavioral therapy (CBT) for SAD. (For details of this comprehensive treatment, see Box 4 )
Treating bipolar variant of SAD
Significant differences exist in the clinical management of BD SP and MDD SP, despite their commonalities ( Table 2 ). BD SP treatment remains distinct because of the risk of switching with the use of light therapy or antidepressants and the importance of mood stabilizers, especially in BD I.
Consensus guidelines for treating SAD recommend mood stabilizers and close monitoring during light therapy for patients with BD SP ( Table 3 ).2 Therapeutic sleep deprivation can quickly reverse depression during hospitalization but is not used often or recommended for outpatient treatment.20
Light therapy. A small body of evidence suggests that depressive symptoms in BD SP improve with bright light therapy, a treatment with demonstrated efficacy in MDD SP.21 No differences in response have been reported between light therapy for winter depressive episodes among individuals with BD SP or MDD SP.22-24 Light therapy may increase the risk of switching to mania/hypomania in patients with BD SP, however. Clinical supervision is imperative, even for patients thought to have MDD SP, because of the risk of undiagnosed BD.
Regular monitoring by a physician is indicated for individuals taking medications or remedies with photosensitizing effects (such as lithium, thioridazine, or St. John’s wort). An ophthalmologist consultation and monitoring is necessary for patients with preexisting eye problems, those taking photosensitizing medications, and those who develop eye problems during light treatment.2,6
The recommended starting dose for light therapy in MDD SP is 30 minutes daily in the early morning, but this dose may be too high for individuals with BD SP.25 To minimize the risk of switching, begin light therapy at 5 to 10 minutes daily and slowly increase while monitoring the clinical effect (see Related Resources , for more information about light therapy for affective disorders).
Pharmacotherapy. Pharmacologic treatments have not been studied for effectiveness in BD SP, and we hesitate to provide specific recommendations. Effective treatments may include those used for nonseasonal MDD, nonseasonal BD, and MDD SP. When using any medication for BD SP, weigh the risk of switching states against the potential beneficial effects.2
Year-round mood-stabilizer treatment is indicated to minimize the risk of mood episodes in BD SP, especially in patients with BD I. When treating SAD, mood stabilizers with antidepressant effects—such as lamotrigine or lithium (for maintenance), and quetiapine or aripiprazole (for acute treatment)—are preferable to agents without an antidepressant effect in monotherapy. More-sedating mood stabilizers (such as valproate or carbamazepine) likely would not be as beneficial as less-sedating agents, considering that patients with SAD frequently experience fatigue.
Because of the lack of adequate clinical trials of treatments for BD SP, we suggest that clinicians choose medications and follow algorithms relevant to BD without a seasonal specifier. Use similar schedules and dosages, with individual tailoring.5,26
Antidepressants that have shown efficacy in MDD SP include fluoxetine, bupropion, citalopram, and sertraline.6,9,27-29 For patients with BD SP, we initiate antidepressants when:
- light treatment fails
- the patient is unable to travel to the south
- light treatment is not available (often because patients cannot afford the cost, which is not covered by insurance)
- patient lacks time for light treatment.
An additional important consideration is history of response (such as a patient who did not respond well to light therapy in the past but responded very well to a particular antidepressant).
No studies have compared antidepressant classes or individual medications for MDD SP. Clinical wisdom is to base the antidepressant choice, dosages, decision points of when to switch, and schedule of switching (cross-tapering) on individual patients’ symptom clusters and comorbid conditions as well as the medication’s side effects.
Prophylactic treatment with bupropion would seem an appropriate initial choice for a prototypical SAD patient, considering this medication’s more activating effects and FDA approval for SAD treatment.9 For the minority of patients with SAD who present with agitation and increased sleepiness, a slightly sedating selective serotonin reuptake inhibitor such as citalopram would make more sense as a first-line treatment. Finally, we would recommend sertraline for patients with marked anxiety—especially panic attacks or obsessive-compulsive symptoms—but without insomnia.
For specific dosages, rely on the literature of treating nonseasonal depression (unipolar or bipolar). It is important to define decision-making points for dosage increases, augmentation, switching to another antidepressant, and cross-tapering, similar to how you would address a nonseasonal depression, typical or atypical.
In our view, treating a patient with BD I SP with an antidepressant alone—without a mood stabilizer—is almost always wrong. For BD II SP we leave it to the clinician to decide, based on individual patients, clinical experience, and ideally in consultation with a peer.
Seasonal dosages. You may wish to seasonally vary medications and dosages for patients with BD SP. Although no strong evidence exists, we recommend 2 options:
- Consider increasing mood-stabilizing medication in spring and summer, with a reduction (but no tapering for BD I) in fall and winter.
- Consider a complete antidepressant taper 2 weeks after daylight saving time begins in spring; taper under increased observation and not faster than 6 weeks, with close attention to emerging symptoms of depression or antidepressant withdrawal.
We do not taper antidepressants before daylight saving time, and we always consider additional stressors, losses, and challenges in our patients’ lives before tapering antidepressants in spring or summer. We also assess and monitor compliance.
Psychotherapy. Referral can be made to clinicians trained in CBT for patients with a seasonal pattern and interpersonal and social rhythm therapy (IPSRT) for BD. Integrative models for SAD and BD propose that psychological and biologic vulnerability factors interact with environmental events (such as winter season or disruption of daily routine) to trigger mood episodes.
CBT adapted for SAD targets mal-adaptive thinking and behavioral disengagement through cognitive therapy and behavioral activation to counteract SAD symptoms.30,31 Preliminary trials by our group suggest that CBT for MDD SP is an effective acute treatment30 and may prevent future episodes.32
IPSRT is an adaptation of interpersonal psychotherapy that aims to stabilize social relationships and rhythms in BD.33 IPSRT posits that irregularity in daily routines leads to circadian dysregulation, precipitating mood episodes in persons vulnerable to BD.34 The degree of regularity in social rhythms achieved in IPSRT is associated with reduced likelihood of recurrence post-treatment.34 If stabilizing social rhythms has a similar effect of regulating circadian rhythms in SAD, IPSRT may be effective in treating BD SP.
Table 2
Physiopathologic findings and clinical management for SAD vs BD
| SAD | BD | |
|---|---|---|
| Differences | May be unipolar or bipolar Defined by seasonality Light therapy and antidepressants indicated | Increased risk of psychosis and psychiatric hospitalization Most BD is not seasonal Mood stabilizers indicated Risk of switching states with light therapy and antidepressants |
| Similarities | Atypical depressive symptom presentation Highly recurrent Predictable season of recurrence allows proactive treatment Assess for mania and hypomania in both disorders Light therapy requires clinical supervision Psychotherapy may be beneficial | |
| BD: bipolar disorder; SAD: seasonal affective disorder | ||
Table 3
Recommended treatment for bipolar disorder with seasonal pattern
| Treatment | Recommendation |
|---|---|
| Mood-stabilizing medications | Maintain year-round, especially in patients with BP I |
| Antidepressants | Consider those with efficacy in unipolar SAD or nonseasonal bipolar depression |
| Light therapy | Initiate for 5 to 10 min/day for bipolar depressive episodes in patients receiving mood stabilizers or atypical antipsychotics; slowly increase duration while monitoring mood, sleep, and side effects to manage risk of hypomanic or manic switch |
| Psychotherapy | Consider CBT or interpersonal and social rhythm therapy to help manage symptoms and reduce episode recurrence |
| BP I: bipolar disorder type I; CBT: cognitive-behavioral therapy; SAD: seasonal affective disorder | |
CASE CONCLUSION: Ongoing treatment required
After several months of light therapy, Ms. S begins to feel better and reports having more energy. We taper her light therapy to 10 minutes daily in the morning from late February until 1 week after daylight saving time begins in mid-March. Weekly phone calls during this transition screen for signs of hypomania or mania. Lamotrigine is effective in preventing switches in spring.
Future plans include monitoring for hypomania through summer and possibly reinitiating light therapy in fall or winter. Because approximately one-half of individuals who undergo CBT for SAD do not experience another episode the winter after treatment, light therapy will be initiated only if depressive symptoms emerge. A booster session is scheduled with Ms. S’s CBT therapist in early fall to reinforce relapse prevention skills.
Antidepressant therapy will be recommended if full treatment response is not maintained with light therapy and continued use of CBT skills for SAD. During sessions, we emphasize compliance with lamotrigine. On several occasions Ms. S questions the need for ongoing therapy, but with education about the potential effects of mania she agrees to continue treatment as indicated.
Seasonality screening tools
- Seasonal Pattern module of the Structured Clinical Interview for DSM Disorders (SCID). www.scid4.org/faq/clinician_version.html.
- Hypomania Interview Guide for Seasonal Affective Disorder (HIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
- National Institutes of Health Life Chart Method. www.bipolarnews.org/Clinician%20Life%20Charting.htm.
- Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
Bipolarity screening tools
- Bipolar Spectrum Diagnostic Scale. Click here to download.
- Bipolarity Index. http://psycheducation.org/depression/STEPBipolarityIndex.htm.
Light therapy
- Wirz-Justice A, Benedetti F, Terman M. Chronotherapeutics for affective disorders: a clinician’s manual for light and wake therapy. Basel, Switzerland: S. Karger AG; 2009.
- Wirz-Justice A, Benedetti F, Berger M, et al. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
Psychotherapy
- Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder (therapist guide). New York, NY: Oxford University Press; 2008.
- Frank E. Treating bipolar disorder: a clinician’s guide to interpersonal and social rhythm therapy. New York, NY: Guilford Press, Inc.; 2005.
Drug brand names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin XL
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Valproate • Depakote
Disclosures
Drs. Roecklein and Rohan report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Postolache received an investigator-initiated award from The LiteBook Company (Vancouver, Canada) via the Society for Light Treatment and Biological Rhythms, as well as research support from Apollo Health (Salt Lake City, UT).
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Lam RW, Levitt AJ. eds. Clinical guidelines for the treatment of seasonal affective disorder. Vancouver, BC: Clinical and Academic Publishing; 1999.
3. Rosenthal NE, Sack DA, Gillin JC, et al. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry. 1984;41(1):72-80.
4. Michalak EE, Wilkinson C, Hood K, et al. Seasonal and nonseasonal depression: how do they differ? Symptom profile, clinical and family history in a general population sample. J Affect Disord. 2002;69(1-3):185-192.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
6. Sohn CH, Lam RW. Treatment of seasonal affective disorder: unipolar versus bipolar differences. Curr Psychiatry Rep. 2004;6(6):478-485.
7. Goikolea JM, Colom F, Martinez-Aran A, et al. Clinical and prognostic implications of seasonal pattern in bipolar disorder: a 10-year follow-up of 302 patients. Psychol Med. 2007;37:1595-1599.
8. Kessler RC, Zhao S, Blazer DG, et al. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45(1-2):19-30.
9. Modell JG, Rosenthal NE, Harriett AE, et al. Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL. Biol Psychiatry. 2005;58:658-667.
10. Cassidy F, Carroll BJ. Seasonal variation of mixed and pure episodes of bipolar disorder. J Affect Disord. 2002;68:25-31.
11. Shin K, Schaffer A, Levitt AJ, et al. Seasonality in a community sample of bipolar, unipolar and control subjects. J Affect Disord. 2005;86:19-25.
12. Wood J, Birmaher B, Axelson D, et al. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166(2-3):201-209.
13. Soreca I, Frank E, Kupfer DJ. The phenomenology of bipolar disorder: what drives the high rate of medical burden and determines long-term prognosis? Depress Anxiety. 2009;26(1):73-82.
14. Terman M, Terman J, Rafferty B. Experimental design and measures of success in the treatment of winter depression by bright light. Psychopharmacol Bull. 1990;26(4):505-510.
15. Goel N, Terman M, Terman JS, et al. Summer mood in winter depressives: validation of a structured interview. Depress Anxiety. 1999;9:83-91.
16. Denicoff KD, Leverich GS, Nolen WA, et al. Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med. 2000;30:1391-1397.
17. Ghaemi SN, Miller CJ, Berv DA, et al. Sensitivity and specificity of a new Bipolar Spectrum Diagnostic Scale. J Affect Disord. 2005;84:273-277.
18. Phelps J, Angst J, Katzow J, et al. Validity and utility of bipolar spectrum models. Bipolar Disord. 2008;10:179-193.
19. Williams JB, Link MJ, Rosenthal NE, et al. Structured Interview Guide for the Hamilton Depression Rating Scale - Seasonal Affective Disorder Version (SIGH-SAD). New York, NY: New York State Psychiatric Institute; 1992.
20. Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009;66(3):298-301.
21. Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162(4):656-662.
22. Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry. 1998;55(10):875-882.
23. Eastman CI, Young MA, Fogg LF, et al. Bright light treatment of winter depression: a placebo-controlled trial. Arch Gen Psychiatry. 1998;55(10):883-889.
24. Lewy AJ, Bauer VK, Cutler NL, et al. Morning vs evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55(10):890-896.
25. Sit D, Wisner KL, Hanusa BH, et al. Light therapy for bipolar disorder: a case series in women. Bipolar Disord. 2007;9:918-927.
26. Goodwin GM. Evidence-based guidelines for treating bipolar disorder: revised second edition—recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2009;23(4):346-388.
27. Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry. 2006;163:805-812.
28. Pjrek E, Konstantinidis A, Assem-Hilger E, et al. Therapeutic effects of escitalopram and reboxetine in seasonal affective disorder: a pooled analysis. J Psychiatr Res. 2009;43(8):792-797.
29. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology (Berl). 2004;171(4):390-397.
30. Rohan KJ, Roecklein KA, Tierney Lindsey K, et al. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. J Consult Clin Psychol. 2007;75(3):489-500.
31. Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder. Therapist guide. New York, NY: Oxford University Press; 2008.
32. Rohan KJ, Roecklein KA, Lacy TJ, et al. Winter depression recurrence one year after cognitive-behavioral therapy, light therapy, or combination treatment. Behav Ther. 2009;40(3):225-238.
33. Frank E, Kupfer DJ, Ehlers CL, et al. Interpersonal and social rhythm therapy for bipolar disorder: integrating interpersonal and behavioral approaches. Behavior Therapist. 1994;17:143-149.
34. Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62(9):996-1004.
Ms. S, age 24, is referred to our team in early December by her primary care physician for “fatigue.” The patient describes going to bed and falling asleep before 9:30 these winter evenings, whereas in summer she went to bed at 11 PM. She craves bread, pasta, and sweets and reports increased appetite in winter compared with summer. Her mood is low, and she misses warm-weather activities of gardening and walking. Fatigue and difficulty concentrating are causing her problems at work and school.
Her history reveals mood elevation in spring as days become longer, with a clear change at approximately March 10 to 20. She reports “spring fever” and feeling “great” last year as soon as daylight saving time began. She slept only 3 hours a night and had a burst of ideas to expand her small business. She threw herself into her work, feeling she was making up for lost time and productivity. She also admits to making a large, misguided business investment during that time.
Upon questioning, she recalls that the previous spring she argued with her father and threw a cup of hot tea at him. When interviewed, Ms. S’s mother describes her daughter at that time as having “a very short fuse,” speaking loud and fast, staying up late at night, and looking as though she was not herself.
Seasonal affective disorder (SAD) is an umbrella term for mood disorders that follow a seasonal pattern of recurrence. Bipolar I disorder (BD I) or bipolar II disorder (BD II) with seasonal pattern (BD SP) is the DSM-IV-TR diagnosis for persons with depressive episodes in the fall or winter and mania (BD I) or hypomania (BD II) in spring or summer ( Table 1 ).1
This article compares BD SP with major depressive disorder with seasonal pattern (MDD SP), in which depressive episodes usually occur in fall or winter and fully remit in spring or summer.1 Rather than being categorically distinct from each other, BD SP and MDD SP may represent extreme variants on a seasonal depression continuum from unipolar to bipolar.
Table 1
DSM-IV-TR criteria for seasonal pattern specifier*
| A | A regular pattern of major depressive episodes (MDEs) at a particular time of year (such as fall and/or winter) |
| B | Full remission or change to mania or hypomania at a particular time of year (such as spring or summer) |
| C | 2 seasonal MDEs that followed the pattern described in (A) and (B) occurred in the past 2 years (and no nonseasonal MDEs) |
| D | Seasonal MDEs substantially outnumber nonseasonal MDEs across the lifespan |
Cases do not meet criteria if:
| |
| *Can be applied to a pattern of major depressive episodes in bipolar I disorder, bipolar II disorder, or major depressive disorder | |
| Source: Adapted from reference 1 | |
Overlap of MDD SP and BD SP
The seasonal pattern specifier can be applied to a diagnosis of MDD, BD I, or BD II.1 Seasonality-focused assessments, described below, can help characterize seasonal patterns that do not meet full SP criteria but may deserve clinical attention.
Symptom presentation. MDD SP and BD SP share similar atypical depressive symptom presentations and seasonal recurrence patterns ( Box 1 ). Hypersomnia, hyperphagia, and psychomotor retardation are more prevalent in major depressive episodes of bipolar disorders and SAD than in unipolar or nonseasonal mood disorders.2-4 Individuals with SAD also report fatigue and decreased physical activity,3 both of which are characteristic of bipolar depressive episodes.5
Although psychosis and psychiatric hospitalizations are more common in BD I than unipolar disorders,6 individuals with BD SP are less likely to report psychosis than those with nonseasonal BD.7 Another study found that BD SP patients reported a higher rate of psychiatric hospitalizations than MDD SP patients (28% vs 9.4%).6
Recurrence pattern. Major depressive episodes are highly recurrent in both MDD and BD, with or without a seasonal pattern. Approximately 75% of individuals with MDD experience ≥1 recurrence (mean, 10.8 episodes);8 MDD SP patients report a mean of 13.4 episodes.9 The mean lifetime episodes in BD SP is 20.74, compared with 11.67 in nonseasonal BD.7
Cassidy and Carroll10 measured the frequency of mood episodes in 304 BD patients not assessed for seasonality. Manic episodes peaked in early spring, mixed episodes peaked in late summer or fall, and depressive episodes peaked in fall-winter.
Irregular rhythm. Both BD and MDD SP involve irregularities in daily or circadian rhythms, such as changes in the timing of sleep, melatonin release, and body temperature.3,5,11 Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BD12 and are implicated in the core pathology of BD13 ( Box 2 ). In BD, life events that change social rhythms may disrupt circadian rhythms, triggering mood episodes.5
Etiologic hypotheses for both BD and SAD propose that an external event (life stress in BD; decreased photoperiod in SAD) leads to circadian dysregulation and, in turn, mood episodes. Circadian-related hypotheses for SAD and BD are supported by evidence showing efficacy of treatments that manipulate behavioral and circadian rhythms.
from unipolar to bipolar?
Seasonality refers to the degree of seasonal changes in behavior and mood within an individual. Seasonality scores are normally distributed,a suggesting that seasonality may be continuous in the general population—with some individuals meeting criteria for a seasonal mood disorder:
- A seasonal pattern is reported by approximately 10% to 20% of depressed outpatients with recurrent mood disorders and an estimated 15% to 22% of individuals with bipolar disorder (BD).b
- Persons with BD—seasonal or not—report greater seasonality compared with those with major depressive disorder (MDD).c
Among individuals with seasonal affective disorder, the course is bipolar in an estimated 12% to 22% and unipolar in 78% to 88%.d These estimates may reflect underdiagnosis of BD with seasonal pattern because hypomania is difficult to diagnose retrospectively.e
The bipolar-unipolar continuum includes (in order): BD I, BD II, bipolar disorder not otherwise specified, cyclothymia, bipolar spectrum disorder, and MDD.f In examining the validity of the bipolar spectrum model, Phelps et alg noted:
- At least 3 studies found that all symptoms reported by individuals with unipolar and bipolar diagnoses approach a normal distribution, rather than a bimodal distribution separating unipolar from bipolar symptom profiles.
- Data from 2 population-based studies indicate that subthreshold hypomanic symptoms are more common than and cause as much impairment as symptoms meeting criteria for BD II or I.
Some individuals who meet criteria for MDD with seasonal pattern have summertime periods of transient hypomania and hyperthymia (hypomanic-like periods without clinically significant impairment).h This suggests that the bipolar continuum also may exist among individuals with seasonal pattern mood disorders.
Source: Access reference citations here
Etiologic hypotheses of seasonal affective disorder (SAD) include:
- photoperiodic hypothesis (shorter winter days cause SAD,a perhaps mediated by a summer vs winter difference in duration of nightly melatonin release)b
- phase shift hypothesis (less available light in winter may lead to an inability to synchronize circadian rhythms with sleep/wake rhythms).c
Some case studies of rapid-cycling bipolar disorder (BD) suggest that mood is correlated with daily hours of sunshine and light therapy is antidepressant. Rapid-cycling patients may be hypersensitive to day-to-day changes in photoperiod, analogous to mood changes in response to changes in photoperiod across the seasons in SAD.d
Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BDe and are implicated in the core pathology of BD.f Phase delays also are present in some individuals with SAD and are associated with severity and treatment response.g Preliminary evidence suggests that variation in circadian clock genes is related to both BDf,h and SAD.i
Source: Access reference citations here
CASE CONTINUED: Seasonal pattern revealed
Ms. S was aware that she is vulnerable to depressive episodes in fall and winter but unaware of a pattern of hypomanic/manic episodes in spring and summer. Her family psychiatric history includes a sister diagnosed with BD I (with no seasonal specifier), and a maternal aunt who has attempted suicide several times.
Ms. S agrees to an assessment plan including a diagnostic interview, interviews measuring symptom severity and pattern of recurrence, routine laboratory examination, and self-report questionnaires. These show that she meets DSM-IV-TR criteria for BD I, depressed, moderate, with seasonal pattern.
Her assessment scores are 28 on the Structured Interview Guide for HDRS-seasonal affective disorder version (SIGH-SAD), 17 on the Hamilton Depression Rating Scale (HDRS), and 11 on the atypical subscale. The HDRS and atypical subscale are components of the SIGH-SAD reflecting typical (eg, insomnia, loss of appetite, etc.) and atypical (eg, hypersomnia, increased appetite, etc.) depression symptoms, respectively. Ms. S’s scores exceed the threshold scores defining a BD SP episode (>20 SIGH-SAD + >10 HDRS + >5 atypical subscale14 ). Data from self-report questionnaires corroborate this assessment.
We plan to administer the Hypomania Interview Guide (including Hyperthymia) for Seasonal Affective Disorder (HIGH-SAD) during treatment and the following spring to monitor prospectively for hypomanic symptoms.
Assessment tools
After complete assessment for mood episodes and mood disorders based on DSM-IV-TR, an additional assessment for bipolarity and seasonality may be helpful.1
Screen for bipolarity in patients with SAD to avoid triggering mania or hypomania during treatment. Useful tools include:
- HIGH-SAD15
- the National Institutes of Health Life Chart Method to establish a recurrent pattern of mood episodes and track treatment efficacy16
- assessments that characterize sub-threshold bipolar symptoms, such as the Bipolar Spectrum Diagnostic Scale17 ( see Box 3 ) and the Bipolarity Index.18
Also obtain collateral reports from significant others, review patient records, and use the same mania and hypomania scales for prospective assessment as the next spring approaches.6
Assess seasonality in patients with BD to improve diagnosis and treatment. Characterizing a seasonal pattern may allow you and your patient to predict episodes and treat proactively. Commonly used assessments include the SIGH-SAD and the Structured Clinical Interview for DSM Disorders (SCID) seasonal pattern specifier module.19
The SIGH-SAD measures symptom severity and provides recovery criteria based on changes in scores during treatment. Response is defined as a 50% reduction in symptoms; remission is >50% improvement in SIGH-SAD + HDRS <7 + atypical <7 or HDRS <2 + atypical <10.14
CASE CONTINUED: Treatment begins
Considering Ms. S’s diagnosis of BD I SP and the risk of precipitating mania with light treatment, we recommend starting treatment with a mood stabilizer. We narrow our options to those that have a direct antidepressant effect, with the hope that this may reduce the need for future antidepressant medications. For patients diagnosed with BD II SP, we could consider a regimen without mood stabilizers.
We offer Ms. S lithium, a first-line mood stabilizer with evidence of usefulness in treatment before chronotherapeutic interventions and in preventing suicidal behavior. However, Ms. S prefers our second option, lamotrigine, because she is concerned about lithium’s side effects and required blood draws to check drug levels as well as thyroid and kidney status.
Despite causing some initial drowsiness, her lamotrigine dosage is successfully titrated after 2 weeks of treatment to 300 mg/d, without side effects. Only then do we initiate light treatment, which Ms. S wishes to try before antidepressant medications. She also begins sessions with a therapist trained in cognitive-behavioral therapy (CBT) for SAD. (For details of this comprehensive treatment, see Box 4 )
Treating bipolar variant of SAD
Significant differences exist in the clinical management of BD SP and MDD SP, despite their commonalities ( Table 2 ). BD SP treatment remains distinct because of the risk of switching with the use of light therapy or antidepressants and the importance of mood stabilizers, especially in BD I.
Consensus guidelines for treating SAD recommend mood stabilizers and close monitoring during light therapy for patients with BD SP ( Table 3 ).2 Therapeutic sleep deprivation can quickly reverse depression during hospitalization but is not used often or recommended for outpatient treatment.20
Light therapy. A small body of evidence suggests that depressive symptoms in BD SP improve with bright light therapy, a treatment with demonstrated efficacy in MDD SP.21 No differences in response have been reported between light therapy for winter depressive episodes among individuals with BD SP or MDD SP.22-24 Light therapy may increase the risk of switching to mania/hypomania in patients with BD SP, however. Clinical supervision is imperative, even for patients thought to have MDD SP, because of the risk of undiagnosed BD.
Regular monitoring by a physician is indicated for individuals taking medications or remedies with photosensitizing effects (such as lithium, thioridazine, or St. John’s wort). An ophthalmologist consultation and monitoring is necessary for patients with preexisting eye problems, those taking photosensitizing medications, and those who develop eye problems during light treatment.2,6
The recommended starting dose for light therapy in MDD SP is 30 minutes daily in the early morning, but this dose may be too high for individuals with BD SP.25 To minimize the risk of switching, begin light therapy at 5 to 10 minutes daily and slowly increase while monitoring the clinical effect (see Related Resources , for more information about light therapy for affective disorders).
Pharmacotherapy. Pharmacologic treatments have not been studied for effectiveness in BD SP, and we hesitate to provide specific recommendations. Effective treatments may include those used for nonseasonal MDD, nonseasonal BD, and MDD SP. When using any medication for BD SP, weigh the risk of switching states against the potential beneficial effects.2
Year-round mood-stabilizer treatment is indicated to minimize the risk of mood episodes in BD SP, especially in patients with BD I. When treating SAD, mood stabilizers with antidepressant effects—such as lamotrigine or lithium (for maintenance), and quetiapine or aripiprazole (for acute treatment)—are preferable to agents without an antidepressant effect in monotherapy. More-sedating mood stabilizers (such as valproate or carbamazepine) likely would not be as beneficial as less-sedating agents, considering that patients with SAD frequently experience fatigue.
Because of the lack of adequate clinical trials of treatments for BD SP, we suggest that clinicians choose medications and follow algorithms relevant to BD without a seasonal specifier. Use similar schedules and dosages, with individual tailoring.5,26
Antidepressants that have shown efficacy in MDD SP include fluoxetine, bupropion, citalopram, and sertraline.6,9,27-29 For patients with BD SP, we initiate antidepressants when:
- light treatment fails
- the patient is unable to travel to the south
- light treatment is not available (often because patients cannot afford the cost, which is not covered by insurance)
- patient lacks time for light treatment.
An additional important consideration is history of response (such as a patient who did not respond well to light therapy in the past but responded very well to a particular antidepressant).
No studies have compared antidepressant classes or individual medications for MDD SP. Clinical wisdom is to base the antidepressant choice, dosages, decision points of when to switch, and schedule of switching (cross-tapering) on individual patients’ symptom clusters and comorbid conditions as well as the medication’s side effects.
Prophylactic treatment with bupropion would seem an appropriate initial choice for a prototypical SAD patient, considering this medication’s more activating effects and FDA approval for SAD treatment.9 For the minority of patients with SAD who present with agitation and increased sleepiness, a slightly sedating selective serotonin reuptake inhibitor such as citalopram would make more sense as a first-line treatment. Finally, we would recommend sertraline for patients with marked anxiety—especially panic attacks or obsessive-compulsive symptoms—but without insomnia.
For specific dosages, rely on the literature of treating nonseasonal depression (unipolar or bipolar). It is important to define decision-making points for dosage increases, augmentation, switching to another antidepressant, and cross-tapering, similar to how you would address a nonseasonal depression, typical or atypical.
In our view, treating a patient with BD I SP with an antidepressant alone—without a mood stabilizer—is almost always wrong. For BD II SP we leave it to the clinician to decide, based on individual patients, clinical experience, and ideally in consultation with a peer.
Seasonal dosages. You may wish to seasonally vary medications and dosages for patients with BD SP. Although no strong evidence exists, we recommend 2 options:
- Consider increasing mood-stabilizing medication in spring and summer, with a reduction (but no tapering for BD I) in fall and winter.
- Consider a complete antidepressant taper 2 weeks after daylight saving time begins in spring; taper under increased observation and not faster than 6 weeks, with close attention to emerging symptoms of depression or antidepressant withdrawal.
We do not taper antidepressants before daylight saving time, and we always consider additional stressors, losses, and challenges in our patients’ lives before tapering antidepressants in spring or summer. We also assess and monitor compliance.
Psychotherapy. Referral can be made to clinicians trained in CBT for patients with a seasonal pattern and interpersonal and social rhythm therapy (IPSRT) for BD. Integrative models for SAD and BD propose that psychological and biologic vulnerability factors interact with environmental events (such as winter season or disruption of daily routine) to trigger mood episodes.
CBT adapted for SAD targets mal-adaptive thinking and behavioral disengagement through cognitive therapy and behavioral activation to counteract SAD symptoms.30,31 Preliminary trials by our group suggest that CBT for MDD SP is an effective acute treatment30 and may prevent future episodes.32
IPSRT is an adaptation of interpersonal psychotherapy that aims to stabilize social relationships and rhythms in BD.33 IPSRT posits that irregularity in daily routines leads to circadian dysregulation, precipitating mood episodes in persons vulnerable to BD.34 The degree of regularity in social rhythms achieved in IPSRT is associated with reduced likelihood of recurrence post-treatment.34 If stabilizing social rhythms has a similar effect of regulating circadian rhythms in SAD, IPSRT may be effective in treating BD SP.
Table 2
Physiopathologic findings and clinical management for SAD vs BD
| SAD | BD | |
|---|---|---|
| Differences | May be unipolar or bipolar Defined by seasonality Light therapy and antidepressants indicated | Increased risk of psychosis and psychiatric hospitalization Most BD is not seasonal Mood stabilizers indicated Risk of switching states with light therapy and antidepressants |
| Similarities | Atypical depressive symptom presentation Highly recurrent Predictable season of recurrence allows proactive treatment Assess for mania and hypomania in both disorders Light therapy requires clinical supervision Psychotherapy may be beneficial | |
| BD: bipolar disorder; SAD: seasonal affective disorder | ||
Table 3
Recommended treatment for bipolar disorder with seasonal pattern
| Treatment | Recommendation |
|---|---|
| Mood-stabilizing medications | Maintain year-round, especially in patients with BP I |
| Antidepressants | Consider those with efficacy in unipolar SAD or nonseasonal bipolar depression |
| Light therapy | Initiate for 5 to 10 min/day for bipolar depressive episodes in patients receiving mood stabilizers or atypical antipsychotics; slowly increase duration while monitoring mood, sleep, and side effects to manage risk of hypomanic or manic switch |
| Psychotherapy | Consider CBT or interpersonal and social rhythm therapy to help manage symptoms and reduce episode recurrence |
| BP I: bipolar disorder type I; CBT: cognitive-behavioral therapy; SAD: seasonal affective disorder | |
CASE CONCLUSION: Ongoing treatment required
After several months of light therapy, Ms. S begins to feel better and reports having more energy. We taper her light therapy to 10 minutes daily in the morning from late February until 1 week after daylight saving time begins in mid-March. Weekly phone calls during this transition screen for signs of hypomania or mania. Lamotrigine is effective in preventing switches in spring.
Future plans include monitoring for hypomania through summer and possibly reinitiating light therapy in fall or winter. Because approximately one-half of individuals who undergo CBT for SAD do not experience another episode the winter after treatment, light therapy will be initiated only if depressive symptoms emerge. A booster session is scheduled with Ms. S’s CBT therapist in early fall to reinforce relapse prevention skills.
Antidepressant therapy will be recommended if full treatment response is not maintained with light therapy and continued use of CBT skills for SAD. During sessions, we emphasize compliance with lamotrigine. On several occasions Ms. S questions the need for ongoing therapy, but with education about the potential effects of mania she agrees to continue treatment as indicated.
Seasonality screening tools
- Seasonal Pattern module of the Structured Clinical Interview for DSM Disorders (SCID). www.scid4.org/faq/clinician_version.html.
- Hypomania Interview Guide for Seasonal Affective Disorder (HIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
- National Institutes of Health Life Chart Method. www.bipolarnews.org/Clinician%20Life%20Charting.htm.
- Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
Bipolarity screening tools
- Bipolar Spectrum Diagnostic Scale. Click here to download.
- Bipolarity Index. http://psycheducation.org/depression/STEPBipolarityIndex.htm.
Light therapy
- Wirz-Justice A, Benedetti F, Terman M. Chronotherapeutics for affective disorders: a clinician’s manual for light and wake therapy. Basel, Switzerland: S. Karger AG; 2009.
- Wirz-Justice A, Benedetti F, Berger M, et al. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
Psychotherapy
- Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder (therapist guide). New York, NY: Oxford University Press; 2008.
- Frank E. Treating bipolar disorder: a clinician’s guide to interpersonal and social rhythm therapy. New York, NY: Guilford Press, Inc.; 2005.
Drug brand names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin XL
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Valproate • Depakote
Disclosures
Drs. Roecklein and Rohan report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Postolache received an investigator-initiated award from The LiteBook Company (Vancouver, Canada) via the Society for Light Treatment and Biological Rhythms, as well as research support from Apollo Health (Salt Lake City, UT).
Ms. S, age 24, is referred to our team in early December by her primary care physician for “fatigue.” The patient describes going to bed and falling asleep before 9:30 these winter evenings, whereas in summer she went to bed at 11 PM. She craves bread, pasta, and sweets and reports increased appetite in winter compared with summer. Her mood is low, and she misses warm-weather activities of gardening and walking. Fatigue and difficulty concentrating are causing her problems at work and school.
Her history reveals mood elevation in spring as days become longer, with a clear change at approximately March 10 to 20. She reports “spring fever” and feeling “great” last year as soon as daylight saving time began. She slept only 3 hours a night and had a burst of ideas to expand her small business. She threw herself into her work, feeling she was making up for lost time and productivity. She also admits to making a large, misguided business investment during that time.
Upon questioning, she recalls that the previous spring she argued with her father and threw a cup of hot tea at him. When interviewed, Ms. S’s mother describes her daughter at that time as having “a very short fuse,” speaking loud and fast, staying up late at night, and looking as though she was not herself.
Seasonal affective disorder (SAD) is an umbrella term for mood disorders that follow a seasonal pattern of recurrence. Bipolar I disorder (BD I) or bipolar II disorder (BD II) with seasonal pattern (BD SP) is the DSM-IV-TR diagnosis for persons with depressive episodes in the fall or winter and mania (BD I) or hypomania (BD II) in spring or summer ( Table 1 ).1
This article compares BD SP with major depressive disorder with seasonal pattern (MDD SP), in which depressive episodes usually occur in fall or winter and fully remit in spring or summer.1 Rather than being categorically distinct from each other, BD SP and MDD SP may represent extreme variants on a seasonal depression continuum from unipolar to bipolar.
Table 1
DSM-IV-TR criteria for seasonal pattern specifier*
| A | A regular pattern of major depressive episodes (MDEs) at a particular time of year (such as fall and/or winter) |
| B | Full remission or change to mania or hypomania at a particular time of year (such as spring or summer) |
| C | 2 seasonal MDEs that followed the pattern described in (A) and (B) occurred in the past 2 years (and no nonseasonal MDEs) |
| D | Seasonal MDEs substantially outnumber nonseasonal MDEs across the lifespan |
Cases do not meet criteria if:
| |
| *Can be applied to a pattern of major depressive episodes in bipolar I disorder, bipolar II disorder, or major depressive disorder | |
| Source: Adapted from reference 1 | |
Overlap of MDD SP and BD SP
The seasonal pattern specifier can be applied to a diagnosis of MDD, BD I, or BD II.1 Seasonality-focused assessments, described below, can help characterize seasonal patterns that do not meet full SP criteria but may deserve clinical attention.
Symptom presentation. MDD SP and BD SP share similar atypical depressive symptom presentations and seasonal recurrence patterns ( Box 1 ). Hypersomnia, hyperphagia, and psychomotor retardation are more prevalent in major depressive episodes of bipolar disorders and SAD than in unipolar or nonseasonal mood disorders.2-4 Individuals with SAD also report fatigue and decreased physical activity,3 both of which are characteristic of bipolar depressive episodes.5
Although psychosis and psychiatric hospitalizations are more common in BD I than unipolar disorders,6 individuals with BD SP are less likely to report psychosis than those with nonseasonal BD.7 Another study found that BD SP patients reported a higher rate of psychiatric hospitalizations than MDD SP patients (28% vs 9.4%).6
Recurrence pattern. Major depressive episodes are highly recurrent in both MDD and BD, with or without a seasonal pattern. Approximately 75% of individuals with MDD experience ≥1 recurrence (mean, 10.8 episodes);8 MDD SP patients report a mean of 13.4 episodes.9 The mean lifetime episodes in BD SP is 20.74, compared with 11.67 in nonseasonal BD.7
Cassidy and Carroll10 measured the frequency of mood episodes in 304 BD patients not assessed for seasonality. Manic episodes peaked in early spring, mixed episodes peaked in late summer or fall, and depressive episodes peaked in fall-winter.
Irregular rhythm. Both BD and MDD SP involve irregularities in daily or circadian rhythms, such as changes in the timing of sleep, melatonin release, and body temperature.3,5,11 Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BD12 and are implicated in the core pathology of BD13 ( Box 2 ). In BD, life events that change social rhythms may disrupt circadian rhythms, triggering mood episodes.5
Etiologic hypotheses for both BD and SAD propose that an external event (life stress in BD; decreased photoperiod in SAD) leads to circadian dysregulation and, in turn, mood episodes. Circadian-related hypotheses for SAD and BD are supported by evidence showing efficacy of treatments that manipulate behavioral and circadian rhythms.
from unipolar to bipolar?
Seasonality refers to the degree of seasonal changes in behavior and mood within an individual. Seasonality scores are normally distributed,a suggesting that seasonality may be continuous in the general population—with some individuals meeting criteria for a seasonal mood disorder:
- A seasonal pattern is reported by approximately 10% to 20% of depressed outpatients with recurrent mood disorders and an estimated 15% to 22% of individuals with bipolar disorder (BD).b
- Persons with BD—seasonal or not—report greater seasonality compared with those with major depressive disorder (MDD).c
Among individuals with seasonal affective disorder, the course is bipolar in an estimated 12% to 22% and unipolar in 78% to 88%.d These estimates may reflect underdiagnosis of BD with seasonal pattern because hypomania is difficult to diagnose retrospectively.e
The bipolar-unipolar continuum includes (in order): BD I, BD II, bipolar disorder not otherwise specified, cyclothymia, bipolar spectrum disorder, and MDD.f In examining the validity of the bipolar spectrum model, Phelps et alg noted:
- At least 3 studies found that all symptoms reported by individuals with unipolar and bipolar diagnoses approach a normal distribution, rather than a bimodal distribution separating unipolar from bipolar symptom profiles.
- Data from 2 population-based studies indicate that subthreshold hypomanic symptoms are more common than and cause as much impairment as symptoms meeting criteria for BD II or I.
Some individuals who meet criteria for MDD with seasonal pattern have summertime periods of transient hypomania and hyperthymia (hypomanic-like periods without clinically significant impairment).h This suggests that the bipolar continuum also may exist among individuals with seasonal pattern mood disorders.
Source: Access reference citations here
Etiologic hypotheses of seasonal affective disorder (SAD) include:
- photoperiodic hypothesis (shorter winter days cause SAD,a perhaps mediated by a summer vs winter difference in duration of nightly melatonin release)b
- phase shift hypothesis (less available light in winter may lead to an inability to synchronize circadian rhythms with sleep/wake rhythms).c
Some case studies of rapid-cycling bipolar disorder (BD) suggest that mood is correlated with daily hours of sunshine and light therapy is antidepressant. Rapid-cycling patients may be hypersensitive to day-to-day changes in photoperiod, analogous to mood changes in response to changes in photoperiod across the seasons in SAD.d
Circadian phase delays—in which internal rhythms lag behind the sleep cycle—are correlated with symptom severity in BDe and are implicated in the core pathology of BD.f Phase delays also are present in some individuals with SAD and are associated with severity and treatment response.g Preliminary evidence suggests that variation in circadian clock genes is related to both BDf,h and SAD.i
Source: Access reference citations here
CASE CONTINUED: Seasonal pattern revealed
Ms. S was aware that she is vulnerable to depressive episodes in fall and winter but unaware of a pattern of hypomanic/manic episodes in spring and summer. Her family psychiatric history includes a sister diagnosed with BD I (with no seasonal specifier), and a maternal aunt who has attempted suicide several times.
Ms. S agrees to an assessment plan including a diagnostic interview, interviews measuring symptom severity and pattern of recurrence, routine laboratory examination, and self-report questionnaires. These show that she meets DSM-IV-TR criteria for BD I, depressed, moderate, with seasonal pattern.
Her assessment scores are 28 on the Structured Interview Guide for HDRS-seasonal affective disorder version (SIGH-SAD), 17 on the Hamilton Depression Rating Scale (HDRS), and 11 on the atypical subscale. The HDRS and atypical subscale are components of the SIGH-SAD reflecting typical (eg, insomnia, loss of appetite, etc.) and atypical (eg, hypersomnia, increased appetite, etc.) depression symptoms, respectively. Ms. S’s scores exceed the threshold scores defining a BD SP episode (>20 SIGH-SAD + >10 HDRS + >5 atypical subscale14 ). Data from self-report questionnaires corroborate this assessment.
We plan to administer the Hypomania Interview Guide (including Hyperthymia) for Seasonal Affective Disorder (HIGH-SAD) during treatment and the following spring to monitor prospectively for hypomanic symptoms.
Assessment tools
After complete assessment for mood episodes and mood disorders based on DSM-IV-TR, an additional assessment for bipolarity and seasonality may be helpful.1
Screen for bipolarity in patients with SAD to avoid triggering mania or hypomania during treatment. Useful tools include:
- HIGH-SAD15
- the National Institutes of Health Life Chart Method to establish a recurrent pattern of mood episodes and track treatment efficacy16
- assessments that characterize sub-threshold bipolar symptoms, such as the Bipolar Spectrum Diagnostic Scale17 ( see Box 3 ) and the Bipolarity Index.18
Also obtain collateral reports from significant others, review patient records, and use the same mania and hypomania scales for prospective assessment as the next spring approaches.6
Assess seasonality in patients with BD to improve diagnosis and treatment. Characterizing a seasonal pattern may allow you and your patient to predict episodes and treat proactively. Commonly used assessments include the SIGH-SAD and the Structured Clinical Interview for DSM Disorders (SCID) seasonal pattern specifier module.19
The SIGH-SAD measures symptom severity and provides recovery criteria based on changes in scores during treatment. Response is defined as a 50% reduction in symptoms; remission is >50% improvement in SIGH-SAD + HDRS <7 + atypical <7 or HDRS <2 + atypical <10.14
CASE CONTINUED: Treatment begins
Considering Ms. S’s diagnosis of BD I SP and the risk of precipitating mania with light treatment, we recommend starting treatment with a mood stabilizer. We narrow our options to those that have a direct antidepressant effect, with the hope that this may reduce the need for future antidepressant medications. For patients diagnosed with BD II SP, we could consider a regimen without mood stabilizers.
We offer Ms. S lithium, a first-line mood stabilizer with evidence of usefulness in treatment before chronotherapeutic interventions and in preventing suicidal behavior. However, Ms. S prefers our second option, lamotrigine, because she is concerned about lithium’s side effects and required blood draws to check drug levels as well as thyroid and kidney status.
Despite causing some initial drowsiness, her lamotrigine dosage is successfully titrated after 2 weeks of treatment to 300 mg/d, without side effects. Only then do we initiate light treatment, which Ms. S wishes to try before antidepressant medications. She also begins sessions with a therapist trained in cognitive-behavioral therapy (CBT) for SAD. (For details of this comprehensive treatment, see Box 4 )
Treating bipolar variant of SAD
Significant differences exist in the clinical management of BD SP and MDD SP, despite their commonalities ( Table 2 ). BD SP treatment remains distinct because of the risk of switching with the use of light therapy or antidepressants and the importance of mood stabilizers, especially in BD I.
Consensus guidelines for treating SAD recommend mood stabilizers and close monitoring during light therapy for patients with BD SP ( Table 3 ).2 Therapeutic sleep deprivation can quickly reverse depression during hospitalization but is not used often or recommended for outpatient treatment.20
Light therapy. A small body of evidence suggests that depressive symptoms in BD SP improve with bright light therapy, a treatment with demonstrated efficacy in MDD SP.21 No differences in response have been reported between light therapy for winter depressive episodes among individuals with BD SP or MDD SP.22-24 Light therapy may increase the risk of switching to mania/hypomania in patients with BD SP, however. Clinical supervision is imperative, even for patients thought to have MDD SP, because of the risk of undiagnosed BD.
Regular monitoring by a physician is indicated for individuals taking medications or remedies with photosensitizing effects (such as lithium, thioridazine, or St. John’s wort). An ophthalmologist consultation and monitoring is necessary for patients with preexisting eye problems, those taking photosensitizing medications, and those who develop eye problems during light treatment.2,6
The recommended starting dose for light therapy in MDD SP is 30 minutes daily in the early morning, but this dose may be too high for individuals with BD SP.25 To minimize the risk of switching, begin light therapy at 5 to 10 minutes daily and slowly increase while monitoring the clinical effect (see Related Resources , for more information about light therapy for affective disorders).
Pharmacotherapy. Pharmacologic treatments have not been studied for effectiveness in BD SP, and we hesitate to provide specific recommendations. Effective treatments may include those used for nonseasonal MDD, nonseasonal BD, and MDD SP. When using any medication for BD SP, weigh the risk of switching states against the potential beneficial effects.2
Year-round mood-stabilizer treatment is indicated to minimize the risk of mood episodes in BD SP, especially in patients with BD I. When treating SAD, mood stabilizers with antidepressant effects—such as lamotrigine or lithium (for maintenance), and quetiapine or aripiprazole (for acute treatment)—are preferable to agents without an antidepressant effect in monotherapy. More-sedating mood stabilizers (such as valproate or carbamazepine) likely would not be as beneficial as less-sedating agents, considering that patients with SAD frequently experience fatigue.
Because of the lack of adequate clinical trials of treatments for BD SP, we suggest that clinicians choose medications and follow algorithms relevant to BD without a seasonal specifier. Use similar schedules and dosages, with individual tailoring.5,26
Antidepressants that have shown efficacy in MDD SP include fluoxetine, bupropion, citalopram, and sertraline.6,9,27-29 For patients with BD SP, we initiate antidepressants when:
- light treatment fails
- the patient is unable to travel to the south
- light treatment is not available (often because patients cannot afford the cost, which is not covered by insurance)
- patient lacks time for light treatment.
An additional important consideration is history of response (such as a patient who did not respond well to light therapy in the past but responded very well to a particular antidepressant).
No studies have compared antidepressant classes or individual medications for MDD SP. Clinical wisdom is to base the antidepressant choice, dosages, decision points of when to switch, and schedule of switching (cross-tapering) on individual patients’ symptom clusters and comorbid conditions as well as the medication’s side effects.
Prophylactic treatment with bupropion would seem an appropriate initial choice for a prototypical SAD patient, considering this medication’s more activating effects and FDA approval for SAD treatment.9 For the minority of patients with SAD who present with agitation and increased sleepiness, a slightly sedating selective serotonin reuptake inhibitor such as citalopram would make more sense as a first-line treatment. Finally, we would recommend sertraline for patients with marked anxiety—especially panic attacks or obsessive-compulsive symptoms—but without insomnia.
For specific dosages, rely on the literature of treating nonseasonal depression (unipolar or bipolar). It is important to define decision-making points for dosage increases, augmentation, switching to another antidepressant, and cross-tapering, similar to how you would address a nonseasonal depression, typical or atypical.
In our view, treating a patient with BD I SP with an antidepressant alone—without a mood stabilizer—is almost always wrong. For BD II SP we leave it to the clinician to decide, based on individual patients, clinical experience, and ideally in consultation with a peer.
Seasonal dosages. You may wish to seasonally vary medications and dosages for patients with BD SP. Although no strong evidence exists, we recommend 2 options:
- Consider increasing mood-stabilizing medication in spring and summer, with a reduction (but no tapering for BD I) in fall and winter.
- Consider a complete antidepressant taper 2 weeks after daylight saving time begins in spring; taper under increased observation and not faster than 6 weeks, with close attention to emerging symptoms of depression or antidepressant withdrawal.
We do not taper antidepressants before daylight saving time, and we always consider additional stressors, losses, and challenges in our patients’ lives before tapering antidepressants in spring or summer. We also assess and monitor compliance.
Psychotherapy. Referral can be made to clinicians trained in CBT for patients with a seasonal pattern and interpersonal and social rhythm therapy (IPSRT) for BD. Integrative models for SAD and BD propose that psychological and biologic vulnerability factors interact with environmental events (such as winter season or disruption of daily routine) to trigger mood episodes.
CBT adapted for SAD targets mal-adaptive thinking and behavioral disengagement through cognitive therapy and behavioral activation to counteract SAD symptoms.30,31 Preliminary trials by our group suggest that CBT for MDD SP is an effective acute treatment30 and may prevent future episodes.32
IPSRT is an adaptation of interpersonal psychotherapy that aims to stabilize social relationships and rhythms in BD.33 IPSRT posits that irregularity in daily routines leads to circadian dysregulation, precipitating mood episodes in persons vulnerable to BD.34 The degree of regularity in social rhythms achieved in IPSRT is associated with reduced likelihood of recurrence post-treatment.34 If stabilizing social rhythms has a similar effect of regulating circadian rhythms in SAD, IPSRT may be effective in treating BD SP.
Table 2
Physiopathologic findings and clinical management for SAD vs BD
| SAD | BD | |
|---|---|---|
| Differences | May be unipolar or bipolar Defined by seasonality Light therapy and antidepressants indicated | Increased risk of psychosis and psychiatric hospitalization Most BD is not seasonal Mood stabilizers indicated Risk of switching states with light therapy and antidepressants |
| Similarities | Atypical depressive symptom presentation Highly recurrent Predictable season of recurrence allows proactive treatment Assess for mania and hypomania in both disorders Light therapy requires clinical supervision Psychotherapy may be beneficial | |
| BD: bipolar disorder; SAD: seasonal affective disorder | ||
Table 3
Recommended treatment for bipolar disorder with seasonal pattern
| Treatment | Recommendation |
|---|---|
| Mood-stabilizing medications | Maintain year-round, especially in patients with BP I |
| Antidepressants | Consider those with efficacy in unipolar SAD or nonseasonal bipolar depression |
| Light therapy | Initiate for 5 to 10 min/day for bipolar depressive episodes in patients receiving mood stabilizers or atypical antipsychotics; slowly increase duration while monitoring mood, sleep, and side effects to manage risk of hypomanic or manic switch |
| Psychotherapy | Consider CBT or interpersonal and social rhythm therapy to help manage symptoms and reduce episode recurrence |
| BP I: bipolar disorder type I; CBT: cognitive-behavioral therapy; SAD: seasonal affective disorder | |
CASE CONCLUSION: Ongoing treatment required
After several months of light therapy, Ms. S begins to feel better and reports having more energy. We taper her light therapy to 10 minutes daily in the morning from late February until 1 week after daylight saving time begins in mid-March. Weekly phone calls during this transition screen for signs of hypomania or mania. Lamotrigine is effective in preventing switches in spring.
Future plans include monitoring for hypomania through summer and possibly reinitiating light therapy in fall or winter. Because approximately one-half of individuals who undergo CBT for SAD do not experience another episode the winter after treatment, light therapy will be initiated only if depressive symptoms emerge. A booster session is scheduled with Ms. S’s CBT therapist in early fall to reinforce relapse prevention skills.
Antidepressant therapy will be recommended if full treatment response is not maintained with light therapy and continued use of CBT skills for SAD. During sessions, we emphasize compliance with lamotrigine. On several occasions Ms. S questions the need for ongoing therapy, but with education about the potential effects of mania she agrees to continue treatment as indicated.
Seasonality screening tools
- Seasonal Pattern module of the Structured Clinical Interview for DSM Disorders (SCID). www.scid4.org/faq/clinician_version.html.
- Hypomania Interview Guide for Seasonal Affective Disorder (HIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
- National Institutes of Health Life Chart Method. www.bipolarnews.org/Clinician%20Life%20Charting.htm.
- Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD). www.chronotherapeutics.org/Tools_ENG.html.
Bipolarity screening tools
- Bipolar Spectrum Diagnostic Scale. Click here to download.
- Bipolarity Index. http://psycheducation.org/depression/STEPBipolarityIndex.htm.
Light therapy
- Wirz-Justice A, Benedetti F, Terman M. Chronotherapeutics for affective disorders: a clinician’s manual for light and wake therapy. Basel, Switzerland: S. Karger AG; 2009.
- Wirz-Justice A, Benedetti F, Berger M, et al. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
Psychotherapy
- Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder (therapist guide). New York, NY: Oxford University Press; 2008.
- Frank E. Treating bipolar disorder: a clinician’s guide to interpersonal and social rhythm therapy. New York, NY: Guilford Press, Inc.; 2005.
Drug brand names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin XL
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Valproate • Depakote
Disclosures
Drs. Roecklein and Rohan report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Postolache received an investigator-initiated award from The LiteBook Company (Vancouver, Canada) via the Society for Light Treatment and Biological Rhythms, as well as research support from Apollo Health (Salt Lake City, UT).
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Lam RW, Levitt AJ. eds. Clinical guidelines for the treatment of seasonal affective disorder. Vancouver, BC: Clinical and Academic Publishing; 1999.
3. Rosenthal NE, Sack DA, Gillin JC, et al. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry. 1984;41(1):72-80.
4. Michalak EE, Wilkinson C, Hood K, et al. Seasonal and nonseasonal depression: how do they differ? Symptom profile, clinical and family history in a general population sample. J Affect Disord. 2002;69(1-3):185-192.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
6. Sohn CH, Lam RW. Treatment of seasonal affective disorder: unipolar versus bipolar differences. Curr Psychiatry Rep. 2004;6(6):478-485.
7. Goikolea JM, Colom F, Martinez-Aran A, et al. Clinical and prognostic implications of seasonal pattern in bipolar disorder: a 10-year follow-up of 302 patients. Psychol Med. 2007;37:1595-1599.
8. Kessler RC, Zhao S, Blazer DG, et al. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45(1-2):19-30.
9. Modell JG, Rosenthal NE, Harriett AE, et al. Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL. Biol Psychiatry. 2005;58:658-667.
10. Cassidy F, Carroll BJ. Seasonal variation of mixed and pure episodes of bipolar disorder. J Affect Disord. 2002;68:25-31.
11. Shin K, Schaffer A, Levitt AJ, et al. Seasonality in a community sample of bipolar, unipolar and control subjects. J Affect Disord. 2005;86:19-25.
12. Wood J, Birmaher B, Axelson D, et al. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166(2-3):201-209.
13. Soreca I, Frank E, Kupfer DJ. The phenomenology of bipolar disorder: what drives the high rate of medical burden and determines long-term prognosis? Depress Anxiety. 2009;26(1):73-82.
14. Terman M, Terman J, Rafferty B. Experimental design and measures of success in the treatment of winter depression by bright light. Psychopharmacol Bull. 1990;26(4):505-510.
15. Goel N, Terman M, Terman JS, et al. Summer mood in winter depressives: validation of a structured interview. Depress Anxiety. 1999;9:83-91.
16. Denicoff KD, Leverich GS, Nolen WA, et al. Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med. 2000;30:1391-1397.
17. Ghaemi SN, Miller CJ, Berv DA, et al. Sensitivity and specificity of a new Bipolar Spectrum Diagnostic Scale. J Affect Disord. 2005;84:273-277.
18. Phelps J, Angst J, Katzow J, et al. Validity and utility of bipolar spectrum models. Bipolar Disord. 2008;10:179-193.
19. Williams JB, Link MJ, Rosenthal NE, et al. Structured Interview Guide for the Hamilton Depression Rating Scale - Seasonal Affective Disorder Version (SIGH-SAD). New York, NY: New York State Psychiatric Institute; 1992.
20. Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009;66(3):298-301.
21. Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162(4):656-662.
22. Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry. 1998;55(10):875-882.
23. Eastman CI, Young MA, Fogg LF, et al. Bright light treatment of winter depression: a placebo-controlled trial. Arch Gen Psychiatry. 1998;55(10):883-889.
24. Lewy AJ, Bauer VK, Cutler NL, et al. Morning vs evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55(10):890-896.
25. Sit D, Wisner KL, Hanusa BH, et al. Light therapy for bipolar disorder: a case series in women. Bipolar Disord. 2007;9:918-927.
26. Goodwin GM. Evidence-based guidelines for treating bipolar disorder: revised second edition—recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2009;23(4):346-388.
27. Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry. 2006;163:805-812.
28. Pjrek E, Konstantinidis A, Assem-Hilger E, et al. Therapeutic effects of escitalopram and reboxetine in seasonal affective disorder: a pooled analysis. J Psychiatr Res. 2009;43(8):792-797.
29. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology (Berl). 2004;171(4):390-397.
30. Rohan KJ, Roecklein KA, Tierney Lindsey K, et al. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. J Consult Clin Psychol. 2007;75(3):489-500.
31. Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder. Therapist guide. New York, NY: Oxford University Press; 2008.
32. Rohan KJ, Roecklein KA, Lacy TJ, et al. Winter depression recurrence one year after cognitive-behavioral therapy, light therapy, or combination treatment. Behav Ther. 2009;40(3):225-238.
33. Frank E, Kupfer DJ, Ehlers CL, et al. Interpersonal and social rhythm therapy for bipolar disorder: integrating interpersonal and behavioral approaches. Behavior Therapist. 1994;17:143-149.
34. Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62(9):996-1004.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Lam RW, Levitt AJ. eds. Clinical guidelines for the treatment of seasonal affective disorder. Vancouver, BC: Clinical and Academic Publishing; 1999.
3. Rosenthal NE, Sack DA, Gillin JC, et al. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry. 1984;41(1):72-80.
4. Michalak EE, Wilkinson C, Hood K, et al. Seasonal and nonseasonal depression: how do they differ? Symptom profile, clinical and family history in a general population sample. J Affect Disord. 2002;69(1-3):185-192.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
6. Sohn CH, Lam RW. Treatment of seasonal affective disorder: unipolar versus bipolar differences. Curr Psychiatry Rep. 2004;6(6):478-485.
7. Goikolea JM, Colom F, Martinez-Aran A, et al. Clinical and prognostic implications of seasonal pattern in bipolar disorder: a 10-year follow-up of 302 patients. Psychol Med. 2007;37:1595-1599.
8. Kessler RC, Zhao S, Blazer DG, et al. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45(1-2):19-30.
9. Modell JG, Rosenthal NE, Harriett AE, et al. Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL. Biol Psychiatry. 2005;58:658-667.
10. Cassidy F, Carroll BJ. Seasonal variation of mixed and pure episodes of bipolar disorder. J Affect Disord. 2002;68:25-31.
11. Shin K, Schaffer A, Levitt AJ, et al. Seasonality in a community sample of bipolar, unipolar and control subjects. J Affect Disord. 2005;86:19-25.
12. Wood J, Birmaher B, Axelson D, et al. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166(2-3):201-209.
13. Soreca I, Frank E, Kupfer DJ. The phenomenology of bipolar disorder: what drives the high rate of medical burden and determines long-term prognosis? Depress Anxiety. 2009;26(1):73-82.
14. Terman M, Terman J, Rafferty B. Experimental design and measures of success in the treatment of winter depression by bright light. Psychopharmacol Bull. 1990;26(4):505-510.
15. Goel N, Terman M, Terman JS, et al. Summer mood in winter depressives: validation of a structured interview. Depress Anxiety. 1999;9:83-91.
16. Denicoff KD, Leverich GS, Nolen WA, et al. Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med. 2000;30:1391-1397.
17. Ghaemi SN, Miller CJ, Berv DA, et al. Sensitivity and specificity of a new Bipolar Spectrum Diagnostic Scale. J Affect Disord. 2005;84:273-277.
18. Phelps J, Angst J, Katzow J, et al. Validity and utility of bipolar spectrum models. Bipolar Disord. 2008;10:179-193.
19. Williams JB, Link MJ, Rosenthal NE, et al. Structured Interview Guide for the Hamilton Depression Rating Scale - Seasonal Affective Disorder Version (SIGH-SAD). New York, NY: New York State Psychiatric Institute; 1992.
20. Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009;66(3):298-301.
21. Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162(4):656-662.
22. Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry. 1998;55(10):875-882.
23. Eastman CI, Young MA, Fogg LF, et al. Bright light treatment of winter depression: a placebo-controlled trial. Arch Gen Psychiatry. 1998;55(10):883-889.
24. Lewy AJ, Bauer VK, Cutler NL, et al. Morning vs evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55(10):890-896.
25. Sit D, Wisner KL, Hanusa BH, et al. Light therapy for bipolar disorder: a case series in women. Bipolar Disord. 2007;9:918-927.
26. Goodwin GM. Evidence-based guidelines for treating bipolar disorder: revised second edition—recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2009;23(4):346-388.
27. Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Am J Psychiatry. 2006;163:805-812.
28. Pjrek E, Konstantinidis A, Assem-Hilger E, et al. Therapeutic effects of escitalopram and reboxetine in seasonal affective disorder: a pooled analysis. J Psychiatr Res. 2009;43(8):792-797.
29. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology (Berl). 2004;171(4):390-397.
30. Rohan KJ, Roecklein KA, Tierney Lindsey K, et al. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. J Consult Clin Psychol. 2007;75(3):489-500.
31. Rohan KJ. Coping with the seasons: a cognitive-behavioral approach to seasonal affective disorder. Therapist guide. New York, NY: Oxford University Press; 2008.
32. Rohan KJ, Roecklein KA, Lacy TJ, et al. Winter depression recurrence one year after cognitive-behavioral therapy, light therapy, or combination treatment. Behav Ther. 2009;40(3):225-238.
33. Frank E, Kupfer DJ, Ehlers CL, et al. Interpersonal and social rhythm therapy for bipolar disorder: integrating interpersonal and behavioral approaches. Behavior Therapist. 1994;17:143-149.
34. Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62(9):996-1004.
Managing medication and alcohol misuse by your older patients
As the eldest post-World War II “baby boomers” turn 64 this year, relaxed social attitudes about substance use during their lifetimes may predict an increasing risk for substance use disorders (SUDs) in older Americans.1 This presents challenges for psychiatric clinicians:
- Common screening tools used for younger patients might not adequately diagnose SUDs in patients clinically defined as elderly (age ≥65).
- DSM-IV-TR’s definition of substance use as causing clinically significant impairment or distress—such as occupational difficulties, legal problems, or decreased participation in social activities—might not apply to older patients, or these problems could be caused by other factors in older individuals.2
This article describes screening and treatment approaches shown to be most effective for identifying and managing primary SUDs in older patients. Our goal is to help you ask the right questions and provide appropriate care.
Phase-of-life issues
Most older adults have a primary care physician, but their SUDs often go unrecognized.3 Clinicians and family members might hesitate to ask about substance use or prescription medication misuse, and complications—such as falls or cognitive impairment—may be misattributed to normal aging. Thus, SUD screening of older individuals referred for psychiatric care is important.
Older adults respond with higher adherence rates when SUD treatment addresses age-specific issues—such as recent losses, medical problems, and challenges of keeping scheduled appointments or multiple providers/referrals. A combination of psychosocial and biologic treatments may be most beneficial. Although outcomes vary, some evidence indicates that age-specific programs for older alcoholics significantly improve abstinence rates at 6 and 12 months, compared with mixed-age programs4 ( see Related Resources ).
We recommend that you incorporate phase-of-life considerations at all stages of treatment. These include:
- education regarding lowered alcohol intake recommendations
- assessment tools that use criteria relevant to older adults
- treatment interventions that involve age-specific groups and programming.
Screening tools
In a routine office visit, a sensible approach is to screen for alcohol, tobacco, and prescription medication misuse. First-line screening tools for alcohol abuse include the AUDIT-5, CAGE, or MAST-G ( Table 1 ), accompanied by questions about medication side effects and observation of behavioral signs of medication misuse.
Alcohol use disorders. The spectrum of alcohol use disorders includes heavy drinking, hazardous use, harmful use, abuse, and dependence ( Table 2 ). Taking into account older adults’ physiology—these individuals have slower metabolism and smaller volume of distribution—National Institute on Alcohol Abuse and Alcoholism (NIAAA) alcohol consumption guidelines for the elderly differ from those for younger adults.
NIAAA guidelines for the elderly define hazardous use as >3 drinks in 1 sitting or >7 drinks in 1 week for both men and women. This is in comparison with guidelines for younger adults that define hazardous use as >5 drinks in 1 sitting (or >2 drinks/day) for men and >3 drinks in 1 sitting (or >1 drink/day) for women. The NIAAA recommendation considers a standard drink to be 12 oz of beer, 5 oz of wine, or 1.5 oz of distilled spirits, each drink containing approximately 0.5 oz of alcohol.5
Not all screening tools developed to assess alcohol use have been studied extensively in older cohorts,6 and some might not be useful in certain populations.7 The CAGE screening tool, for example—although easy to administer and widely studied—has low sensitivity in psychiatric populations, does not address past vs current drinking problems, and does not distinguish age-specific criteria for problem drinking.
Consider using instruments specific to an older individual’s comorbidities:
- the AUDIT-5 is appropriate for an older patient with psychiatric illness
- the ARPS (or the shorter shARPS) for an older individual with medical problems is likely to improve the rate of identifying problem drinkers.
Table 1
Comparing screening tools for alcohol use disorders in the elderly
| Screening tool | Characteristics | Clinical usefulness |
|---|---|---|
| CAGE | 4 items; self-report; most widely used/studied alcohol use screen; specificity > sensitivity | First-line; most useful if goal is to identify alcohol dependence; may miss misuse or hazardous use |
| AUDIT-5 | 5 items; self-report; specificity > sensitivity; a shortened version of the 10-item AUDIT | First-line; helpful for identifying hazardous use; sensitive for a broader spectrum of alcohol misuse than CAGE |
| MAST-G | 22-item yes/no self-report; questions specific to elderly | First-line; designed to identify a population that drinks less than heavy drinkers |
| SMAST-G | 10 items; shorter version of MAST-G with similar characteristics | Less sensitive and specific than MAST-G; may be useful when time is limited |
| Cyr-Wartman | 2-question screen (“Have you ever had a drinking problem?” “When was your last drink?”); specificity > sensitivity | Use for brief screening; follow up with more thorough screening in case of positive response |
| ARPS/shARPS | 18 items in ARPS (shARPS is shorter); self-report; classifies patients as nonhazardous, hazardous, or harmful drinkers; good sensitivity | Focuses on relationship of alcohol and medical problems, medication use, and functional status |
| ARPS/shARPS: Alcohol-Related Problems Survey/short version of ARPS; AUDIT-5: Alcohol Use Disorders Identification Test, 5-item version; CAGE: Cut down, Annoyed, Guilty, Eye opener; MAST-G: Michigan Alcoholism Screening Test—Geriatric version; SMAST-G: shorter version of MAST-G | ||
Table 2
Spectrum of alcohol use disorders: Heavy drinking to dependence
| Term | Definition | Recommended intervention for patients age ≥65 |
|---|---|---|
| Heavy drinking | >1 drink/day | Brief alcohol intervention |
| Hazardous use | >3 drinks in 1 sitting or >7 drinks/week; places patient at risk for adverse consequences | Brief alcohol intervention |
| Harmful use | Greater than hazardous use, with evidence of negative physical or psychological consequences | Brief alcohol intervention |
| Abuse | Signs of increasing use or decreasing functioning, including engaging in fewer activities, preoccupation with substance, continued use despite adverse consequences | Brief interventions (advise to cut down, educate regarding deleterious effects, and consider referral to substance abuse specialist for evaluation) |
| Dependence | Clear interference with daily function (such as increased falls, otherwise unexplained cognitive impairment); unsuccessful quit attempts; continued use despite adverse consequences | Refer to substance abuse specialist for treatment, including detoxification and age-specific rehabilitation program |
Drug abuse or medication misuse. Illegal drug use is relatively rare in the geriatric population,8 although the rates in patients age 50 to 59 increased from 2.7% in 2002 to 5.0% in 2007.9 In part this may reflect a higher lifetime use of illicit drugs by the baby boomers compared with previous generations.
Evidence also suggests an increasing risk for misuse and abuse of prescription drugs. One factor associated with this risk is medical exposure to prescription drugs with abuse potential. Among older adults in the United States:
- 10% are taking sedative-hypnotic medications
- 15% have been prescribed an opioid-analgesic medication.10
Other factors associated with prescription medication misuse and abuse by older adults include female sex, social isolation, history of substance use or psychiatric disorder, polypharmacy, and chronic medical problems.11
Very few screening instruments detect illicit drug use or prescription medication abuse. To screen older patients, ask about the drugs they are using (prescription and nonprescription), ask about side effects, and look for behavioral signs of medication misuse ( Table 3 ).12,13
Laboratory tests for alcohol’s metabolic effects can identify biologic markers of alcohol use disorders. An elevated mean corpuscular volume (MCV) or gamma-glutamyl transpeptidase (GGT) above the upper normal value can indicate possible problem drinking, even without considering total alcohol intake. Normal lab values are the same for older and younger adults.
Evidence suggests a poor association between findings of the CAGE questionnaire and MCV and GGT tests. Di Bari et al14 reported that biologic markers help identify older drinkers with compromised health status independent of a positive CAGE. This suggests that using a combination of tools to screen for psychosocial and biologic consequences could be more accurate than a single instrument in identifying older individuals with alcohol use disorders.14 We often use a GGT and MCV, along with the CAGE and the AUDIT-5 or SMAST-G.
Tobacco use. Smoking rates decrease with age, but this trend may reflect early mortality among tobacco users. Nicotine dependence remains a significant public health issue among the 7% to 9% of adults age ≥65 who smoke.15 An estimated 70% of all smokers want to quit, and 46% make an attempt each year.11
The single most important step in addressing tobacco use and dependence is screening. After asking about tobacco use and assessing the patient’s willingness to quit, you can provide appropriate interventions.16
Table 3
Behavioral signs of medication misuse by elderly patients
| Excessive worry about whether the medications are working |
| Strong attachment to a particular psychoactive medication |
| Resisting cessation or decreased doses of a prescribed psychoactive drug |
| Excessive anxiety about the supply and timing of medications |
| Decline in hygiene or grooming |
| Daytime sleeping |
| Medical symptoms such as fatigue, weight loss, or insomnia |
| Psychiatric symptoms such as irritability, memory problems, or depression |
| Source: References 12,13 |
Treatment options
General treatment options to consider for older patients with SUDs include a brief outpatient intervention, referral to a substance abuse specialist or inpatient treatment, and appropriate pharmacotherapy ( Table 4 ).
Brief interventions vary from relatively unstructured interactions in a physician’s office to more formal therapy. Components of these interventions include expression of concern, assessment and feedback, and direct advice. For older patients with SUDs, psychosocial approaches can improve treatment outcomes. One useful example—designed for alcohol use disorders—is the BRENDA model ( Table 5 ). Any trained health care staff member can administer this model, which is standardized with a comprehensive manual.17
Several brief intervention trials—including Project Guiding Older Adult Lifestyles (GOAL), the Health Profile Project, and the Staying Healthy Project—found that brief intervention results in significantly decreased alcohol consumption, sometimes even at 12-month follow-up.18 These trials were conducted in primary care settings, but brief interventions likely would be effective in psychiatric practice as well. Project GOAL included two 10- to 15-minute sessions with a physician scheduled 1 month apart and a follow-up phone call 2 weeks after each visit. The Health Profile Project consisted of a single motivational enhancement session.19
When to refer. Severe cases may require evaluation by a substance abuse specialist of the need for detoxification from alcohol, benzodiazepines, or opioids. Referral is appropriate if the patient has:
- a history of complicated withdrawal, including withdrawal seizures or delirium tremens
- complicated underlying medical conditions, such as severe coronary artery disease, uncontrolled hypertension, or uncontrolled diabetes.
Because of age-related physiologic changes, the older population is at risk for a more protracted withdrawal with more severe symptoms, compared with younger patients.20 Specialized care may include detoxification (outpatient or inpatient, depending on withdrawal symptom severity), day hospital program, or—in the case of a patient with a long history of substance use and multiple relapses—a longer-term residential program.
Table 4
Recommended treatments for substance use disorders in the elderly
| Disorder | Treatment |
|---|---|
| Hazardous use | Assess for withdrawal symptoms; brief intervention |
| Alcohol dependence | Assess for withdrawal symptoms; Alcoholics Anonymous; use of BRENDA model ( Table 5 ); pharmacotherapy (naltrexone, acamprosate); structured rehabilitation program with age-appropriate programming |
| Prescription medication misuse* | Assess for withdrawal symptoms; taper off medication (slowly and gradually); buprenorphine detoxification; brief intervention |
| Opioid dependence | Appropriate detoxification; drug-free trial; harm reduction approach with methadone or buprenorphine; age-appropriate psychosocial groups; Narcotics Anonymous |
| *Sedative-hypnotic and opioid pain medications (such as oxycodone HCl) | |
Table 5
The BRENDA model:
A brief psychosocial intervention for alcohol use disorders*
| Biopsychosocial evaluation |
| Reporting the assessment to the patient |
| Empathy |
| Needs identification |
| Direct advice |
| Assessment of patient reaction to the advice |
| *Any trained health care staff member can administer this model, which is standardized with a comprehensive manual |
| Source: Reference 17 |
Pharmacotherapy
Pharmacotherapy is an important component in the treatment of older adults with SUDs. Other elements include psychosocial interventions, brief interventions, cognitive-behavioral therapies, and supportive programs such as Alcoholics Anonymous or Narcotics Anonymous. Randomized controlled trials on the use of medications for SUDs in older patients are limited. As with any other medication trial in the elderly, start with the lowest possible dose and titrate slowly to treatment effect.
Alcohol use disorders. In our experience, naltrexone—an opioid antagonist—is the first-line agent to consider for alcohol dependence in older patients ( Table 4 ). Oslin et al21 found naltrexone, 50 mg/d, to be well-tolerated and effective in decreasing rates of relapse to heavy drinking in older adults.
Because of its potential hepatotoxic effects, use naltrexone with caution in patients with hepatic impairment. We recommend baseline liver function tests, with repeat testing in 3 to 6 months. Severe liver disease would be a contraindication for naltrexone, but consider risk vs benefit in individual patients.
Acamprosate—a glutamatergic medication—has been studied and approved for treating alcohol dependence in adults, although no study has specifically examined its use in elderly patients. Acamprosate may offer an alternative for patients with severe liver disease or those who can’t tolerate naltrexone.
Disulfiram is rarely used in the elderly because of potential risks of hypotension and cardiovascular adverse effects in a disulfiram-ethanol reaction. Topiramate—an anticonvulsant that potentiates gamma-aminobutyric acid—has shown benefit in treating initiation of abstinence from alcohol.22 It is an incompatible treatment for the elderly, however, because it may cause cognitive impairment.
Sedative-hypnotic misuse. The goal in treating patients who misuse sedatives or hypnotics is detoxification, which usually is addressed with a gradual and slow taper under controlled supervision in the outpatient setting.
Opioid dependence. Treatment options for opioid dependence are the same whether older patients are misusing prescription opioids or illicit ones such as heroin. Naltrexone, methadone, and buprenorphine/naloxone have been widely studied and used in younger adults but only minimally in the elderly.
Studies conducted in methadone maintenance clinics have found positive results when older patients are treated for opioid dependence:
- patients age ≥55 may have fewer problems and better outcomes with opioid treatment than younger patients23
- older age is 1 of only 2 variables (the other is no criminal justice involvement) found to be positively associated with longer duration in treatment.24
Older individuals are more sensitive than younger adults to the sedation and respiratory depression of opioids. Buprenorphine is the only opioid with a ceiling effect for respiratory depression, and it does not have an increased half-life in the elderly as do other opioids.25
Other potential side effects of these medications include urinary retention—particularly in elderly males with prostatic hyperplasia—constipation, and movement disorders.
Despite potential side effects, we find that opioid dependence is more successfully treated with agonist or partial agonist therapy than with blocking agents. Buprenorphine and methadone address urges and cravings to use opioids, resulting in greater treatment retention and longer abstinence. Buprenorphine treatment is available in office-based practices of physicians who have received training and certification.
Smoking cessation. Pharmacotherapy and brief treatment interventions can be effective and should be offered to the older smoker. Nicotine replacement therapy, bupropion, varenicline, and nortriptyline help improve quit rates in younger adults, but studies of these agents in older adults are limited.
If monotherapy fails, try combining shorter-acting nicotine replacement therapy with longer-acting agents such as bupropion or varenicline. To our knowledge no dosing adjustment is necessary for the elderly, although we recommend low starting doses with gradual titration.
Some literature suggests nortriptyline as a second-line smoking cessation agent in the elderly. We do not recommend nortriptyline for smoking cessation in this population, however, because of tricyclic antidepressants’ cardiac effects.
- Schultz SK, Arndt S, Liesved J. Locations of facilities with special programs for older substance abuse clients in the U.S. Int J Geriatr Psychiatry. 2003;18(9):839-843.
- National Association of Addiction Treatment Providers. www.naatp.org.
- National Association of State Alcohol/Drug Abuse Directors. www.nasadad.org.
- Substance Abuse and Mental Health Services Administration. www.samhsa.gov.
- American Academy of Addiction Psychiatry. www.aaap.org.
Drug brand names
- Acamprosate • Campral
- Buprenorphine/naloxone • Suboxone
- Bupropion • Zyban
- Disulfiram • Antabuse
- Methadone • Dolophine, Methadose
- Naltrexone • ReVia
- Nortriptyline • Aventyl, Pamelor
- Oxycodone • OxyContin, Roxicodone, others
- Topiramate • Topamax
- Varenicline • Chantix
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Patterson TL, Jeste DV. The potential impact of the baby boom generation on substance abuse among elderly persons. Psychiatr Serv. 1999;50(9):1184-1188.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Oslin D, Pettinati H, Volpicelli J. Alcoholism treatment adherence. Older age predicts better adherence and drinking outcomes. Am J Geriatr Psychiatry. 2002;10(6):740-747.
4. Kashner TM, Rodell DI, Ogden SR, et al. Outcomes and costs of two VA inpatient treatment programs for older alcoholic patients. Hosp Community Psychiatry. 1992;43:985-989.
5. Alcohol and aging. Alcohol Alert, issue 40; April 1998. National Institute on Alcohol Abuse and Alcoholism. National Institutes of Health. Available at: http://pubs.niaaa.nih.gov/publications/aa40.htm. Accessed November 19, 2009.
6. Cyr MG, Wartman SA. The effectiveness of routine screening questions in the detection of alcoholism. JAMA. 1988;259(1):51-54.
7. O’Connell H, Chin AV, Hamilton F, et al. A systematic review of the utility of self-report alcohol screening instruments in the elderly. Int J Geriatr Psychiatry. 2004;19:1074-1086.
8. Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4:380-394.
9. Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2008. DHHS Publication SMA08-4343, NSDUH Series H-34.
10. Simoni-Wastila L, Zuckerman IH, Singhal PK, et al. National estimates of exposure to prescription drugs with addiction potential in community-dwelling elders. Subst Abus. 2005;26:33-42.
11. Reducing tobacco use: a report of the Surgeon General. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. August 9, 2000. Available at: http://www.surgeongeneral.gov/library/tobacco_use. Accessed November 19, 2009.
12. Blow FC. Substance abuse among older adults. Treatment improvement protocol (TIP) series 26. Substance Abuse and Mental Health Services Administration. Public Health Service. U.S. Department of Health and Human Services. Rockville, MD: Center for Substance Abuse Treatment; June 1998. Available at: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=hssamhsatip&part=A48302. Accessed November 19, 2009.
13. Finfgeld-Connett DL. Treatment of substance misuse in older women: using a brief intervention model. J Gerontol Nurs. 2004;30(8):30-37.
14. Di Bari M, Silvestrini G, Chiarlone M, et al. Features of excessive alcohol drinking in older adults distinctively captured by behavioral and biological screening instruments. An epidemiological study. J Clin Epidemiol. 2002;55:41-47.
15. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007. MMWR. 2008;57(45):1221-1226.
16. Treating tobacco use and dependence: 2008 update. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. Available at: http://www.surgeongeneral.gov/tobacco. Accessed November 19, 2009.
17. Starosta A, Leeman R, Volpicelli J. The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract. 2006;12(2):80-89.
18. Fleming M, Manuwell L, Barry K, et al. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999;48(5):378-384.
19. Barry KL, Blow FC, Cullinane P, et al. The effectiveness of implementing a brief alcohol intervention with older adults in community settings. Washington, DC: National Council on Aging; 2006.
20. Oslin D. Evidence-based treatment of geriatric substance abuse. Psychiatr Clin North Am. 2005;28:897-911.
21. Oslin D, Liberto JG, O’Brien J, et al. Naltrexone as an adjunctive treatment for older patients with alcohol dependence. Am J Geriatr Psychiatry. 1997;5:324-332.
22. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for treatment of alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-1651.
23. Firoz S, Carlson G. Characteristics and treatment outcome of older methadone-maintenance patients. Am J Geriatr Psychiatry. 2004;12(5):539-541.
24. Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93(1):51-60.
25. Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8(4):287-313.
As the eldest post-World War II “baby boomers” turn 64 this year, relaxed social attitudes about substance use during their lifetimes may predict an increasing risk for substance use disorders (SUDs) in older Americans.1 This presents challenges for psychiatric clinicians:
- Common screening tools used for younger patients might not adequately diagnose SUDs in patients clinically defined as elderly (age ≥65).
- DSM-IV-TR’s definition of substance use as causing clinically significant impairment or distress—such as occupational difficulties, legal problems, or decreased participation in social activities—might not apply to older patients, or these problems could be caused by other factors in older individuals.2
This article describes screening and treatment approaches shown to be most effective for identifying and managing primary SUDs in older patients. Our goal is to help you ask the right questions and provide appropriate care.
Phase-of-life issues
Most older adults have a primary care physician, but their SUDs often go unrecognized.3 Clinicians and family members might hesitate to ask about substance use or prescription medication misuse, and complications—such as falls or cognitive impairment—may be misattributed to normal aging. Thus, SUD screening of older individuals referred for psychiatric care is important.
Older adults respond with higher adherence rates when SUD treatment addresses age-specific issues—such as recent losses, medical problems, and challenges of keeping scheduled appointments or multiple providers/referrals. A combination of psychosocial and biologic treatments may be most beneficial. Although outcomes vary, some evidence indicates that age-specific programs for older alcoholics significantly improve abstinence rates at 6 and 12 months, compared with mixed-age programs4 ( see Related Resources ).
We recommend that you incorporate phase-of-life considerations at all stages of treatment. These include:
- education regarding lowered alcohol intake recommendations
- assessment tools that use criteria relevant to older adults
- treatment interventions that involve age-specific groups and programming.
Screening tools
In a routine office visit, a sensible approach is to screen for alcohol, tobacco, and prescription medication misuse. First-line screening tools for alcohol abuse include the AUDIT-5, CAGE, or MAST-G ( Table 1 ), accompanied by questions about medication side effects and observation of behavioral signs of medication misuse.
Alcohol use disorders. The spectrum of alcohol use disorders includes heavy drinking, hazardous use, harmful use, abuse, and dependence ( Table 2 ). Taking into account older adults’ physiology—these individuals have slower metabolism and smaller volume of distribution—National Institute on Alcohol Abuse and Alcoholism (NIAAA) alcohol consumption guidelines for the elderly differ from those for younger adults.
NIAAA guidelines for the elderly define hazardous use as >3 drinks in 1 sitting or >7 drinks in 1 week for both men and women. This is in comparison with guidelines for younger adults that define hazardous use as >5 drinks in 1 sitting (or >2 drinks/day) for men and >3 drinks in 1 sitting (or >1 drink/day) for women. The NIAAA recommendation considers a standard drink to be 12 oz of beer, 5 oz of wine, or 1.5 oz of distilled spirits, each drink containing approximately 0.5 oz of alcohol.5
Not all screening tools developed to assess alcohol use have been studied extensively in older cohorts,6 and some might not be useful in certain populations.7 The CAGE screening tool, for example—although easy to administer and widely studied—has low sensitivity in psychiatric populations, does not address past vs current drinking problems, and does not distinguish age-specific criteria for problem drinking.
Consider using instruments specific to an older individual’s comorbidities:
- the AUDIT-5 is appropriate for an older patient with psychiatric illness
- the ARPS (or the shorter shARPS) for an older individual with medical problems is likely to improve the rate of identifying problem drinkers.
Table 1
Comparing screening tools for alcohol use disorders in the elderly
| Screening tool | Characteristics | Clinical usefulness |
|---|---|---|
| CAGE | 4 items; self-report; most widely used/studied alcohol use screen; specificity > sensitivity | First-line; most useful if goal is to identify alcohol dependence; may miss misuse or hazardous use |
| AUDIT-5 | 5 items; self-report; specificity > sensitivity; a shortened version of the 10-item AUDIT | First-line; helpful for identifying hazardous use; sensitive for a broader spectrum of alcohol misuse than CAGE |
| MAST-G | 22-item yes/no self-report; questions specific to elderly | First-line; designed to identify a population that drinks less than heavy drinkers |
| SMAST-G | 10 items; shorter version of MAST-G with similar characteristics | Less sensitive and specific than MAST-G; may be useful when time is limited |
| Cyr-Wartman | 2-question screen (“Have you ever had a drinking problem?” “When was your last drink?”); specificity > sensitivity | Use for brief screening; follow up with more thorough screening in case of positive response |
| ARPS/shARPS | 18 items in ARPS (shARPS is shorter); self-report; classifies patients as nonhazardous, hazardous, or harmful drinkers; good sensitivity | Focuses on relationship of alcohol and medical problems, medication use, and functional status |
| ARPS/shARPS: Alcohol-Related Problems Survey/short version of ARPS; AUDIT-5: Alcohol Use Disorders Identification Test, 5-item version; CAGE: Cut down, Annoyed, Guilty, Eye opener; MAST-G: Michigan Alcoholism Screening Test—Geriatric version; SMAST-G: shorter version of MAST-G | ||
Table 2
Spectrum of alcohol use disorders: Heavy drinking to dependence
| Term | Definition | Recommended intervention for patients age ≥65 |
|---|---|---|
| Heavy drinking | >1 drink/day | Brief alcohol intervention |
| Hazardous use | >3 drinks in 1 sitting or >7 drinks/week; places patient at risk for adverse consequences | Brief alcohol intervention |
| Harmful use | Greater than hazardous use, with evidence of negative physical or psychological consequences | Brief alcohol intervention |
| Abuse | Signs of increasing use or decreasing functioning, including engaging in fewer activities, preoccupation with substance, continued use despite adverse consequences | Brief interventions (advise to cut down, educate regarding deleterious effects, and consider referral to substance abuse specialist for evaluation) |
| Dependence | Clear interference with daily function (such as increased falls, otherwise unexplained cognitive impairment); unsuccessful quit attempts; continued use despite adverse consequences | Refer to substance abuse specialist for treatment, including detoxification and age-specific rehabilitation program |
Drug abuse or medication misuse. Illegal drug use is relatively rare in the geriatric population,8 although the rates in patients age 50 to 59 increased from 2.7% in 2002 to 5.0% in 2007.9 In part this may reflect a higher lifetime use of illicit drugs by the baby boomers compared with previous generations.
Evidence also suggests an increasing risk for misuse and abuse of prescription drugs. One factor associated with this risk is medical exposure to prescription drugs with abuse potential. Among older adults in the United States:
- 10% are taking sedative-hypnotic medications
- 15% have been prescribed an opioid-analgesic medication.10
Other factors associated with prescription medication misuse and abuse by older adults include female sex, social isolation, history of substance use or psychiatric disorder, polypharmacy, and chronic medical problems.11
Very few screening instruments detect illicit drug use or prescription medication abuse. To screen older patients, ask about the drugs they are using (prescription and nonprescription), ask about side effects, and look for behavioral signs of medication misuse ( Table 3 ).12,13
Laboratory tests for alcohol’s metabolic effects can identify biologic markers of alcohol use disorders. An elevated mean corpuscular volume (MCV) or gamma-glutamyl transpeptidase (GGT) above the upper normal value can indicate possible problem drinking, even without considering total alcohol intake. Normal lab values are the same for older and younger adults.
Evidence suggests a poor association between findings of the CAGE questionnaire and MCV and GGT tests. Di Bari et al14 reported that biologic markers help identify older drinkers with compromised health status independent of a positive CAGE. This suggests that using a combination of tools to screen for psychosocial and biologic consequences could be more accurate than a single instrument in identifying older individuals with alcohol use disorders.14 We often use a GGT and MCV, along with the CAGE and the AUDIT-5 or SMAST-G.
Tobacco use. Smoking rates decrease with age, but this trend may reflect early mortality among tobacco users. Nicotine dependence remains a significant public health issue among the 7% to 9% of adults age ≥65 who smoke.15 An estimated 70% of all smokers want to quit, and 46% make an attempt each year.11
The single most important step in addressing tobacco use and dependence is screening. After asking about tobacco use and assessing the patient’s willingness to quit, you can provide appropriate interventions.16
Table 3
Behavioral signs of medication misuse by elderly patients
| Excessive worry about whether the medications are working |
| Strong attachment to a particular psychoactive medication |
| Resisting cessation or decreased doses of a prescribed psychoactive drug |
| Excessive anxiety about the supply and timing of medications |
| Decline in hygiene or grooming |
| Daytime sleeping |
| Medical symptoms such as fatigue, weight loss, or insomnia |
| Psychiatric symptoms such as irritability, memory problems, or depression |
| Source: References 12,13 |
Treatment options
General treatment options to consider for older patients with SUDs include a brief outpatient intervention, referral to a substance abuse specialist or inpatient treatment, and appropriate pharmacotherapy ( Table 4 ).
Brief interventions vary from relatively unstructured interactions in a physician’s office to more formal therapy. Components of these interventions include expression of concern, assessment and feedback, and direct advice. For older patients with SUDs, psychosocial approaches can improve treatment outcomes. One useful example—designed for alcohol use disorders—is the BRENDA model ( Table 5 ). Any trained health care staff member can administer this model, which is standardized with a comprehensive manual.17
Several brief intervention trials—including Project Guiding Older Adult Lifestyles (GOAL), the Health Profile Project, and the Staying Healthy Project—found that brief intervention results in significantly decreased alcohol consumption, sometimes even at 12-month follow-up.18 These trials were conducted in primary care settings, but brief interventions likely would be effective in psychiatric practice as well. Project GOAL included two 10- to 15-minute sessions with a physician scheduled 1 month apart and a follow-up phone call 2 weeks after each visit. The Health Profile Project consisted of a single motivational enhancement session.19
When to refer. Severe cases may require evaluation by a substance abuse specialist of the need for detoxification from alcohol, benzodiazepines, or opioids. Referral is appropriate if the patient has:
- a history of complicated withdrawal, including withdrawal seizures or delirium tremens
- complicated underlying medical conditions, such as severe coronary artery disease, uncontrolled hypertension, or uncontrolled diabetes.
Because of age-related physiologic changes, the older population is at risk for a more protracted withdrawal with more severe symptoms, compared with younger patients.20 Specialized care may include detoxification (outpatient or inpatient, depending on withdrawal symptom severity), day hospital program, or—in the case of a patient with a long history of substance use and multiple relapses—a longer-term residential program.
Table 4
Recommended treatments for substance use disorders in the elderly
| Disorder | Treatment |
|---|---|
| Hazardous use | Assess for withdrawal symptoms; brief intervention |
| Alcohol dependence | Assess for withdrawal symptoms; Alcoholics Anonymous; use of BRENDA model ( Table 5 ); pharmacotherapy (naltrexone, acamprosate); structured rehabilitation program with age-appropriate programming |
| Prescription medication misuse* | Assess for withdrawal symptoms; taper off medication (slowly and gradually); buprenorphine detoxification; brief intervention |
| Opioid dependence | Appropriate detoxification; drug-free trial; harm reduction approach with methadone or buprenorphine; age-appropriate psychosocial groups; Narcotics Anonymous |
| *Sedative-hypnotic and opioid pain medications (such as oxycodone HCl) | |
Table 5
The BRENDA model:
A brief psychosocial intervention for alcohol use disorders*
| Biopsychosocial evaluation |
| Reporting the assessment to the patient |
| Empathy |
| Needs identification |
| Direct advice |
| Assessment of patient reaction to the advice |
| *Any trained health care staff member can administer this model, which is standardized with a comprehensive manual |
| Source: Reference 17 |
Pharmacotherapy
Pharmacotherapy is an important component in the treatment of older adults with SUDs. Other elements include psychosocial interventions, brief interventions, cognitive-behavioral therapies, and supportive programs such as Alcoholics Anonymous or Narcotics Anonymous. Randomized controlled trials on the use of medications for SUDs in older patients are limited. As with any other medication trial in the elderly, start with the lowest possible dose and titrate slowly to treatment effect.
Alcohol use disorders. In our experience, naltrexone—an opioid antagonist—is the first-line agent to consider for alcohol dependence in older patients ( Table 4 ). Oslin et al21 found naltrexone, 50 mg/d, to be well-tolerated and effective in decreasing rates of relapse to heavy drinking in older adults.
Because of its potential hepatotoxic effects, use naltrexone with caution in patients with hepatic impairment. We recommend baseline liver function tests, with repeat testing in 3 to 6 months. Severe liver disease would be a contraindication for naltrexone, but consider risk vs benefit in individual patients.
Acamprosate—a glutamatergic medication—has been studied and approved for treating alcohol dependence in adults, although no study has specifically examined its use in elderly patients. Acamprosate may offer an alternative for patients with severe liver disease or those who can’t tolerate naltrexone.
Disulfiram is rarely used in the elderly because of potential risks of hypotension and cardiovascular adverse effects in a disulfiram-ethanol reaction. Topiramate—an anticonvulsant that potentiates gamma-aminobutyric acid—has shown benefit in treating initiation of abstinence from alcohol.22 It is an incompatible treatment for the elderly, however, because it may cause cognitive impairment.
Sedative-hypnotic misuse. The goal in treating patients who misuse sedatives or hypnotics is detoxification, which usually is addressed with a gradual and slow taper under controlled supervision in the outpatient setting.
Opioid dependence. Treatment options for opioid dependence are the same whether older patients are misusing prescription opioids or illicit ones such as heroin. Naltrexone, methadone, and buprenorphine/naloxone have been widely studied and used in younger adults but only minimally in the elderly.
Studies conducted in methadone maintenance clinics have found positive results when older patients are treated for opioid dependence:
- patients age ≥55 may have fewer problems and better outcomes with opioid treatment than younger patients23
- older age is 1 of only 2 variables (the other is no criminal justice involvement) found to be positively associated with longer duration in treatment.24
Older individuals are more sensitive than younger adults to the sedation and respiratory depression of opioids. Buprenorphine is the only opioid with a ceiling effect for respiratory depression, and it does not have an increased half-life in the elderly as do other opioids.25
Other potential side effects of these medications include urinary retention—particularly in elderly males with prostatic hyperplasia—constipation, and movement disorders.
Despite potential side effects, we find that opioid dependence is more successfully treated with agonist or partial agonist therapy than with blocking agents. Buprenorphine and methadone address urges and cravings to use opioids, resulting in greater treatment retention and longer abstinence. Buprenorphine treatment is available in office-based practices of physicians who have received training and certification.
Smoking cessation. Pharmacotherapy and brief treatment interventions can be effective and should be offered to the older smoker. Nicotine replacement therapy, bupropion, varenicline, and nortriptyline help improve quit rates in younger adults, but studies of these agents in older adults are limited.
If monotherapy fails, try combining shorter-acting nicotine replacement therapy with longer-acting agents such as bupropion or varenicline. To our knowledge no dosing adjustment is necessary for the elderly, although we recommend low starting doses with gradual titration.
Some literature suggests nortriptyline as a second-line smoking cessation agent in the elderly. We do not recommend nortriptyline for smoking cessation in this population, however, because of tricyclic antidepressants’ cardiac effects.
- Schultz SK, Arndt S, Liesved J. Locations of facilities with special programs for older substance abuse clients in the U.S. Int J Geriatr Psychiatry. 2003;18(9):839-843.
- National Association of Addiction Treatment Providers. www.naatp.org.
- National Association of State Alcohol/Drug Abuse Directors. www.nasadad.org.
- Substance Abuse and Mental Health Services Administration. www.samhsa.gov.
- American Academy of Addiction Psychiatry. www.aaap.org.
Drug brand names
- Acamprosate • Campral
- Buprenorphine/naloxone • Suboxone
- Bupropion • Zyban
- Disulfiram • Antabuse
- Methadone • Dolophine, Methadose
- Naltrexone • ReVia
- Nortriptyline • Aventyl, Pamelor
- Oxycodone • OxyContin, Roxicodone, others
- Topiramate • Topamax
- Varenicline • Chantix
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
As the eldest post-World War II “baby boomers” turn 64 this year, relaxed social attitudes about substance use during their lifetimes may predict an increasing risk for substance use disorders (SUDs) in older Americans.1 This presents challenges for psychiatric clinicians:
- Common screening tools used for younger patients might not adequately diagnose SUDs in patients clinically defined as elderly (age ≥65).
- DSM-IV-TR’s definition of substance use as causing clinically significant impairment or distress—such as occupational difficulties, legal problems, or decreased participation in social activities—might not apply to older patients, or these problems could be caused by other factors in older individuals.2
This article describes screening and treatment approaches shown to be most effective for identifying and managing primary SUDs in older patients. Our goal is to help you ask the right questions and provide appropriate care.
Phase-of-life issues
Most older adults have a primary care physician, but their SUDs often go unrecognized.3 Clinicians and family members might hesitate to ask about substance use or prescription medication misuse, and complications—such as falls or cognitive impairment—may be misattributed to normal aging. Thus, SUD screening of older individuals referred for psychiatric care is important.
Older adults respond with higher adherence rates when SUD treatment addresses age-specific issues—such as recent losses, medical problems, and challenges of keeping scheduled appointments or multiple providers/referrals. A combination of psychosocial and biologic treatments may be most beneficial. Although outcomes vary, some evidence indicates that age-specific programs for older alcoholics significantly improve abstinence rates at 6 and 12 months, compared with mixed-age programs4 ( see Related Resources ).
We recommend that you incorporate phase-of-life considerations at all stages of treatment. These include:
- education regarding lowered alcohol intake recommendations
- assessment tools that use criteria relevant to older adults
- treatment interventions that involve age-specific groups and programming.
Screening tools
In a routine office visit, a sensible approach is to screen for alcohol, tobacco, and prescription medication misuse. First-line screening tools for alcohol abuse include the AUDIT-5, CAGE, or MAST-G ( Table 1 ), accompanied by questions about medication side effects and observation of behavioral signs of medication misuse.
Alcohol use disorders. The spectrum of alcohol use disorders includes heavy drinking, hazardous use, harmful use, abuse, and dependence ( Table 2 ). Taking into account older adults’ physiology—these individuals have slower metabolism and smaller volume of distribution—National Institute on Alcohol Abuse and Alcoholism (NIAAA) alcohol consumption guidelines for the elderly differ from those for younger adults.
NIAAA guidelines for the elderly define hazardous use as >3 drinks in 1 sitting or >7 drinks in 1 week for both men and women. This is in comparison with guidelines for younger adults that define hazardous use as >5 drinks in 1 sitting (or >2 drinks/day) for men and >3 drinks in 1 sitting (or >1 drink/day) for women. The NIAAA recommendation considers a standard drink to be 12 oz of beer, 5 oz of wine, or 1.5 oz of distilled spirits, each drink containing approximately 0.5 oz of alcohol.5
Not all screening tools developed to assess alcohol use have been studied extensively in older cohorts,6 and some might not be useful in certain populations.7 The CAGE screening tool, for example—although easy to administer and widely studied—has low sensitivity in psychiatric populations, does not address past vs current drinking problems, and does not distinguish age-specific criteria for problem drinking.
Consider using instruments specific to an older individual’s comorbidities:
- the AUDIT-5 is appropriate for an older patient with psychiatric illness
- the ARPS (or the shorter shARPS) for an older individual with medical problems is likely to improve the rate of identifying problem drinkers.
Table 1
Comparing screening tools for alcohol use disorders in the elderly
| Screening tool | Characteristics | Clinical usefulness |
|---|---|---|
| CAGE | 4 items; self-report; most widely used/studied alcohol use screen; specificity > sensitivity | First-line; most useful if goal is to identify alcohol dependence; may miss misuse or hazardous use |
| AUDIT-5 | 5 items; self-report; specificity > sensitivity; a shortened version of the 10-item AUDIT | First-line; helpful for identifying hazardous use; sensitive for a broader spectrum of alcohol misuse than CAGE |
| MAST-G | 22-item yes/no self-report; questions specific to elderly | First-line; designed to identify a population that drinks less than heavy drinkers |
| SMAST-G | 10 items; shorter version of MAST-G with similar characteristics | Less sensitive and specific than MAST-G; may be useful when time is limited |
| Cyr-Wartman | 2-question screen (“Have you ever had a drinking problem?” “When was your last drink?”); specificity > sensitivity | Use for brief screening; follow up with more thorough screening in case of positive response |
| ARPS/shARPS | 18 items in ARPS (shARPS is shorter); self-report; classifies patients as nonhazardous, hazardous, or harmful drinkers; good sensitivity | Focuses on relationship of alcohol and medical problems, medication use, and functional status |
| ARPS/shARPS: Alcohol-Related Problems Survey/short version of ARPS; AUDIT-5: Alcohol Use Disorders Identification Test, 5-item version; CAGE: Cut down, Annoyed, Guilty, Eye opener; MAST-G: Michigan Alcoholism Screening Test—Geriatric version; SMAST-G: shorter version of MAST-G | ||
Table 2
Spectrum of alcohol use disorders: Heavy drinking to dependence
| Term | Definition | Recommended intervention for patients age ≥65 |
|---|---|---|
| Heavy drinking | >1 drink/day | Brief alcohol intervention |
| Hazardous use | >3 drinks in 1 sitting or >7 drinks/week; places patient at risk for adverse consequences | Brief alcohol intervention |
| Harmful use | Greater than hazardous use, with evidence of negative physical or psychological consequences | Brief alcohol intervention |
| Abuse | Signs of increasing use or decreasing functioning, including engaging in fewer activities, preoccupation with substance, continued use despite adverse consequences | Brief interventions (advise to cut down, educate regarding deleterious effects, and consider referral to substance abuse specialist for evaluation) |
| Dependence | Clear interference with daily function (such as increased falls, otherwise unexplained cognitive impairment); unsuccessful quit attempts; continued use despite adverse consequences | Refer to substance abuse specialist for treatment, including detoxification and age-specific rehabilitation program |
Drug abuse or medication misuse. Illegal drug use is relatively rare in the geriatric population,8 although the rates in patients age 50 to 59 increased from 2.7% in 2002 to 5.0% in 2007.9 In part this may reflect a higher lifetime use of illicit drugs by the baby boomers compared with previous generations.
Evidence also suggests an increasing risk for misuse and abuse of prescription drugs. One factor associated with this risk is medical exposure to prescription drugs with abuse potential. Among older adults in the United States:
- 10% are taking sedative-hypnotic medications
- 15% have been prescribed an opioid-analgesic medication.10
Other factors associated with prescription medication misuse and abuse by older adults include female sex, social isolation, history of substance use or psychiatric disorder, polypharmacy, and chronic medical problems.11
Very few screening instruments detect illicit drug use or prescription medication abuse. To screen older patients, ask about the drugs they are using (prescription and nonprescription), ask about side effects, and look for behavioral signs of medication misuse ( Table 3 ).12,13
Laboratory tests for alcohol’s metabolic effects can identify biologic markers of alcohol use disorders. An elevated mean corpuscular volume (MCV) or gamma-glutamyl transpeptidase (GGT) above the upper normal value can indicate possible problem drinking, even without considering total alcohol intake. Normal lab values are the same for older and younger adults.
Evidence suggests a poor association between findings of the CAGE questionnaire and MCV and GGT tests. Di Bari et al14 reported that biologic markers help identify older drinkers with compromised health status independent of a positive CAGE. This suggests that using a combination of tools to screen for psychosocial and biologic consequences could be more accurate than a single instrument in identifying older individuals with alcohol use disorders.14 We often use a GGT and MCV, along with the CAGE and the AUDIT-5 or SMAST-G.
Tobacco use. Smoking rates decrease with age, but this trend may reflect early mortality among tobacco users. Nicotine dependence remains a significant public health issue among the 7% to 9% of adults age ≥65 who smoke.15 An estimated 70% of all smokers want to quit, and 46% make an attempt each year.11
The single most important step in addressing tobacco use and dependence is screening. After asking about tobacco use and assessing the patient’s willingness to quit, you can provide appropriate interventions.16
Table 3
Behavioral signs of medication misuse by elderly patients
| Excessive worry about whether the medications are working |
| Strong attachment to a particular psychoactive medication |
| Resisting cessation or decreased doses of a prescribed psychoactive drug |
| Excessive anxiety about the supply and timing of medications |
| Decline in hygiene or grooming |
| Daytime sleeping |
| Medical symptoms such as fatigue, weight loss, or insomnia |
| Psychiatric symptoms such as irritability, memory problems, or depression |
| Source: References 12,13 |
Treatment options
General treatment options to consider for older patients with SUDs include a brief outpatient intervention, referral to a substance abuse specialist or inpatient treatment, and appropriate pharmacotherapy ( Table 4 ).
Brief interventions vary from relatively unstructured interactions in a physician’s office to more formal therapy. Components of these interventions include expression of concern, assessment and feedback, and direct advice. For older patients with SUDs, psychosocial approaches can improve treatment outcomes. One useful example—designed for alcohol use disorders—is the BRENDA model ( Table 5 ). Any trained health care staff member can administer this model, which is standardized with a comprehensive manual.17
Several brief intervention trials—including Project Guiding Older Adult Lifestyles (GOAL), the Health Profile Project, and the Staying Healthy Project—found that brief intervention results in significantly decreased alcohol consumption, sometimes even at 12-month follow-up.18 These trials were conducted in primary care settings, but brief interventions likely would be effective in psychiatric practice as well. Project GOAL included two 10- to 15-minute sessions with a physician scheduled 1 month apart and a follow-up phone call 2 weeks after each visit. The Health Profile Project consisted of a single motivational enhancement session.19
When to refer. Severe cases may require evaluation by a substance abuse specialist of the need for detoxification from alcohol, benzodiazepines, or opioids. Referral is appropriate if the patient has:
- a history of complicated withdrawal, including withdrawal seizures or delirium tremens
- complicated underlying medical conditions, such as severe coronary artery disease, uncontrolled hypertension, or uncontrolled diabetes.
Because of age-related physiologic changes, the older population is at risk for a more protracted withdrawal with more severe symptoms, compared with younger patients.20 Specialized care may include detoxification (outpatient or inpatient, depending on withdrawal symptom severity), day hospital program, or—in the case of a patient with a long history of substance use and multiple relapses—a longer-term residential program.
Table 4
Recommended treatments for substance use disorders in the elderly
| Disorder | Treatment |
|---|---|
| Hazardous use | Assess for withdrawal symptoms; brief intervention |
| Alcohol dependence | Assess for withdrawal symptoms; Alcoholics Anonymous; use of BRENDA model ( Table 5 ); pharmacotherapy (naltrexone, acamprosate); structured rehabilitation program with age-appropriate programming |
| Prescription medication misuse* | Assess for withdrawal symptoms; taper off medication (slowly and gradually); buprenorphine detoxification; brief intervention |
| Opioid dependence | Appropriate detoxification; drug-free trial; harm reduction approach with methadone or buprenorphine; age-appropriate psychosocial groups; Narcotics Anonymous |
| *Sedative-hypnotic and opioid pain medications (such as oxycodone HCl) | |
Table 5
The BRENDA model:
A brief psychosocial intervention for alcohol use disorders*
| Biopsychosocial evaluation |
| Reporting the assessment to the patient |
| Empathy |
| Needs identification |
| Direct advice |
| Assessment of patient reaction to the advice |
| *Any trained health care staff member can administer this model, which is standardized with a comprehensive manual |
| Source: Reference 17 |
Pharmacotherapy
Pharmacotherapy is an important component in the treatment of older adults with SUDs. Other elements include psychosocial interventions, brief interventions, cognitive-behavioral therapies, and supportive programs such as Alcoholics Anonymous or Narcotics Anonymous. Randomized controlled trials on the use of medications for SUDs in older patients are limited. As with any other medication trial in the elderly, start with the lowest possible dose and titrate slowly to treatment effect.
Alcohol use disorders. In our experience, naltrexone—an opioid antagonist—is the first-line agent to consider for alcohol dependence in older patients ( Table 4 ). Oslin et al21 found naltrexone, 50 mg/d, to be well-tolerated and effective in decreasing rates of relapse to heavy drinking in older adults.
Because of its potential hepatotoxic effects, use naltrexone with caution in patients with hepatic impairment. We recommend baseline liver function tests, with repeat testing in 3 to 6 months. Severe liver disease would be a contraindication for naltrexone, but consider risk vs benefit in individual patients.
Acamprosate—a glutamatergic medication—has been studied and approved for treating alcohol dependence in adults, although no study has specifically examined its use in elderly patients. Acamprosate may offer an alternative for patients with severe liver disease or those who can’t tolerate naltrexone.
Disulfiram is rarely used in the elderly because of potential risks of hypotension and cardiovascular adverse effects in a disulfiram-ethanol reaction. Topiramate—an anticonvulsant that potentiates gamma-aminobutyric acid—has shown benefit in treating initiation of abstinence from alcohol.22 It is an incompatible treatment for the elderly, however, because it may cause cognitive impairment.
Sedative-hypnotic misuse. The goal in treating patients who misuse sedatives or hypnotics is detoxification, which usually is addressed with a gradual and slow taper under controlled supervision in the outpatient setting.
Opioid dependence. Treatment options for opioid dependence are the same whether older patients are misusing prescription opioids or illicit ones such as heroin. Naltrexone, methadone, and buprenorphine/naloxone have been widely studied and used in younger adults but only minimally in the elderly.
Studies conducted in methadone maintenance clinics have found positive results when older patients are treated for opioid dependence:
- patients age ≥55 may have fewer problems and better outcomes with opioid treatment than younger patients23
- older age is 1 of only 2 variables (the other is no criminal justice involvement) found to be positively associated with longer duration in treatment.24
Older individuals are more sensitive than younger adults to the sedation and respiratory depression of opioids. Buprenorphine is the only opioid with a ceiling effect for respiratory depression, and it does not have an increased half-life in the elderly as do other opioids.25
Other potential side effects of these medications include urinary retention—particularly in elderly males with prostatic hyperplasia—constipation, and movement disorders.
Despite potential side effects, we find that opioid dependence is more successfully treated with agonist or partial agonist therapy than with blocking agents. Buprenorphine and methadone address urges and cravings to use opioids, resulting in greater treatment retention and longer abstinence. Buprenorphine treatment is available in office-based practices of physicians who have received training and certification.
Smoking cessation. Pharmacotherapy and brief treatment interventions can be effective and should be offered to the older smoker. Nicotine replacement therapy, bupropion, varenicline, and nortriptyline help improve quit rates in younger adults, but studies of these agents in older adults are limited.
If monotherapy fails, try combining shorter-acting nicotine replacement therapy with longer-acting agents such as bupropion or varenicline. To our knowledge no dosing adjustment is necessary for the elderly, although we recommend low starting doses with gradual titration.
Some literature suggests nortriptyline as a second-line smoking cessation agent in the elderly. We do not recommend nortriptyline for smoking cessation in this population, however, because of tricyclic antidepressants’ cardiac effects.
- Schultz SK, Arndt S, Liesved J. Locations of facilities with special programs for older substance abuse clients in the U.S. Int J Geriatr Psychiatry. 2003;18(9):839-843.
- National Association of Addiction Treatment Providers. www.naatp.org.
- National Association of State Alcohol/Drug Abuse Directors. www.nasadad.org.
- Substance Abuse and Mental Health Services Administration. www.samhsa.gov.
- American Academy of Addiction Psychiatry. www.aaap.org.
Drug brand names
- Acamprosate • Campral
- Buprenorphine/naloxone • Suboxone
- Bupropion • Zyban
- Disulfiram • Antabuse
- Methadone • Dolophine, Methadose
- Naltrexone • ReVia
- Nortriptyline • Aventyl, Pamelor
- Oxycodone • OxyContin, Roxicodone, others
- Topiramate • Topamax
- Varenicline • Chantix
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Patterson TL, Jeste DV. The potential impact of the baby boom generation on substance abuse among elderly persons. Psychiatr Serv. 1999;50(9):1184-1188.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Oslin D, Pettinati H, Volpicelli J. Alcoholism treatment adherence. Older age predicts better adherence and drinking outcomes. Am J Geriatr Psychiatry. 2002;10(6):740-747.
4. Kashner TM, Rodell DI, Ogden SR, et al. Outcomes and costs of two VA inpatient treatment programs for older alcoholic patients. Hosp Community Psychiatry. 1992;43:985-989.
5. Alcohol and aging. Alcohol Alert, issue 40; April 1998. National Institute on Alcohol Abuse and Alcoholism. National Institutes of Health. Available at: http://pubs.niaaa.nih.gov/publications/aa40.htm. Accessed November 19, 2009.
6. Cyr MG, Wartman SA. The effectiveness of routine screening questions in the detection of alcoholism. JAMA. 1988;259(1):51-54.
7. O’Connell H, Chin AV, Hamilton F, et al. A systematic review of the utility of self-report alcohol screening instruments in the elderly. Int J Geriatr Psychiatry. 2004;19:1074-1086.
8. Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4:380-394.
9. Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2008. DHHS Publication SMA08-4343, NSDUH Series H-34.
10. Simoni-Wastila L, Zuckerman IH, Singhal PK, et al. National estimates of exposure to prescription drugs with addiction potential in community-dwelling elders. Subst Abus. 2005;26:33-42.
11. Reducing tobacco use: a report of the Surgeon General. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. August 9, 2000. Available at: http://www.surgeongeneral.gov/library/tobacco_use. Accessed November 19, 2009.
12. Blow FC. Substance abuse among older adults. Treatment improvement protocol (TIP) series 26. Substance Abuse and Mental Health Services Administration. Public Health Service. U.S. Department of Health and Human Services. Rockville, MD: Center for Substance Abuse Treatment; June 1998. Available at: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=hssamhsatip&part=A48302. Accessed November 19, 2009.
13. Finfgeld-Connett DL. Treatment of substance misuse in older women: using a brief intervention model. J Gerontol Nurs. 2004;30(8):30-37.
14. Di Bari M, Silvestrini G, Chiarlone M, et al. Features of excessive alcohol drinking in older adults distinctively captured by behavioral and biological screening instruments. An epidemiological study. J Clin Epidemiol. 2002;55:41-47.
15. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007. MMWR. 2008;57(45):1221-1226.
16. Treating tobacco use and dependence: 2008 update. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. Available at: http://www.surgeongeneral.gov/tobacco. Accessed November 19, 2009.
17. Starosta A, Leeman R, Volpicelli J. The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract. 2006;12(2):80-89.
18. Fleming M, Manuwell L, Barry K, et al. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999;48(5):378-384.
19. Barry KL, Blow FC, Cullinane P, et al. The effectiveness of implementing a brief alcohol intervention with older adults in community settings. Washington, DC: National Council on Aging; 2006.
20. Oslin D. Evidence-based treatment of geriatric substance abuse. Psychiatr Clin North Am. 2005;28:897-911.
21. Oslin D, Liberto JG, O’Brien J, et al. Naltrexone as an adjunctive treatment for older patients with alcohol dependence. Am J Geriatr Psychiatry. 1997;5:324-332.
22. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for treatment of alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-1651.
23. Firoz S, Carlson G. Characteristics and treatment outcome of older methadone-maintenance patients. Am J Geriatr Psychiatry. 2004;12(5):539-541.
24. Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93(1):51-60.
25. Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8(4):287-313.
1. Patterson TL, Jeste DV. The potential impact of the baby boom generation on substance abuse among elderly persons. Psychiatr Serv. 1999;50(9):1184-1188.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Oslin D, Pettinati H, Volpicelli J. Alcoholism treatment adherence. Older age predicts better adherence and drinking outcomes. Am J Geriatr Psychiatry. 2002;10(6):740-747.
4. Kashner TM, Rodell DI, Ogden SR, et al. Outcomes and costs of two VA inpatient treatment programs for older alcoholic patients. Hosp Community Psychiatry. 1992;43:985-989.
5. Alcohol and aging. Alcohol Alert, issue 40; April 1998. National Institute on Alcohol Abuse and Alcoholism. National Institutes of Health. Available at: http://pubs.niaaa.nih.gov/publications/aa40.htm. Accessed November 19, 2009.
6. Cyr MG, Wartman SA. The effectiveness of routine screening questions in the detection of alcoholism. JAMA. 1988;259(1):51-54.
7. O’Connell H, Chin AV, Hamilton F, et al. A systematic review of the utility of self-report alcohol screening instruments in the elderly. Int J Geriatr Psychiatry. 2004;19:1074-1086.
8. Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4:380-394.
9. Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2008. DHHS Publication SMA08-4343, NSDUH Series H-34.
10. Simoni-Wastila L, Zuckerman IH, Singhal PK, et al. National estimates of exposure to prescription drugs with addiction potential in community-dwelling elders. Subst Abus. 2005;26:33-42.
11. Reducing tobacco use: a report of the Surgeon General. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. August 9, 2000. Available at: http://www.surgeongeneral.gov/library/tobacco_use. Accessed November 19, 2009.
12. Blow FC. Substance abuse among older adults. Treatment improvement protocol (TIP) series 26. Substance Abuse and Mental Health Services Administration. Public Health Service. U.S. Department of Health and Human Services. Rockville, MD: Center for Substance Abuse Treatment; June 1998. Available at: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=hssamhsatip&part=A48302. Accessed November 19, 2009.
13. Finfgeld-Connett DL. Treatment of substance misuse in older women: using a brief intervention model. J Gerontol Nurs. 2004;30(8):30-37.
14. Di Bari M, Silvestrini G, Chiarlone M, et al. Features of excessive alcohol drinking in older adults distinctively captured by behavioral and biological screening instruments. An epidemiological study. J Clin Epidemiol. 2002;55:41-47.
15. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007. MMWR. 2008;57(45):1221-1226.
16. Treating tobacco use and dependence: 2008 update. Office of the Surgeon General. Public Health Service. U.S. Department of Health and Human Services. Available at: http://www.surgeongeneral.gov/tobacco. Accessed November 19, 2009.
17. Starosta A, Leeman R, Volpicelli J. The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract. 2006;12(2):80-89.
18. Fleming M, Manuwell L, Barry K, et al. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999;48(5):378-384.
19. Barry KL, Blow FC, Cullinane P, et al. The effectiveness of implementing a brief alcohol intervention with older adults in community settings. Washington, DC: National Council on Aging; 2006.
20. Oslin D. Evidence-based treatment of geriatric substance abuse. Psychiatr Clin North Am. 2005;28:897-911.
21. Oslin D, Liberto JG, O’Brien J, et al. Naltrexone as an adjunctive treatment for older patients with alcohol dependence. Am J Geriatr Psychiatry. 1997;5:324-332.
22. Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for treatment of alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641-1651.
23. Firoz S, Carlson G. Characteristics and treatment outcome of older methadone-maintenance patients. Am J Geriatr Psychiatry. 2004;12(5):539-541.
24. Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93(1):51-60.
25. Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8(4):287-313.
Evidence vs experience
Concerning the role of “evidence” in psychiatric practice (“Are psychiatrists more evidence-based than psychologists?” From the Editor, Current Psychiatry, December 2009,), my question is whether psychiatrists who consider themselves evidence-based achieve better clinical results than those who do not. I suspect there is no significant difference. Of course, this question will never be answered to Dr. Nasrallah’s standards. No pharmaceutical or insurance companies are interested enough because, with the mediation of psychiatric thought leaders, they have succeeded in redefining the nature of and criteria for evidence. They now own it. To what degree it strongly pertains to the real world is an open question.
As a psychiatrist with several decades of experience who works on the front lines, I am leery of the growing biomedical depersonalization and algorithmic regimentation of treatment. I am less optimistic about the kind of progress implied in Dr. Nasrallah’s editorial. I do not believe it is his place to tell colleagues how they should practice. Psychiatric treatment mostly occurs in the context of a one-to-one relationship, and evidence generated by the research industry must be scrutinized according to the individual patient’s exigencies and factors affecting the patient’s life and clinical condition. This is a process of clinical judgment, which integrates not only the narrowly defined, research-based evidence Dr. Nasrallah mentioned but also a psychiatrist’s experience, which there appears to be little place for in psychiatry’s brave new world. It may be that psychologists maintain a certain clinical advantage over psychiatrists in this regard.
Edmond Zeldin, MD
Pawtucket, RI
Dr. Nasrallah responds
I welcome Dr. Zeldin’s critical remarks. As a clinician, I too value my more than 3 decades of clinical experience, but as a researcher I also recognize that it is insufficient to provide optimal care. On the first page of Dr. Gregory Gray’s book Evidence-based psychiatry,1 the first heading states “Clinical practice is not always evidence-based.” Dr. Gray says that evidence-based medicine (EBM) is “the application of a knowledge of medical informatics and clinical epidemiology to the treatment of individual patients and involves the integration of the best research evidence with clinical expertise and patient values.”
The EBM concept was initiated by D.L. Sackett et al in 1996,2 not by pharmaceutical companies. However, all drug companies must conduct strictly evidence-based clinical trials (double-blind, placebo-controlled, and sufficiently powered sample size) on experimental drugs before these agents can be approved by the FDA. The large FDA studies conducted by industry are part of EBM that are adopted in clinical practice. However, some non-FDA drug company studies are self-serving and not evidence-based.3
I recently reviewed 237 meta-analytic studies in schizophrenia,4 and only 30 of those studies address pharmacology. Other meta-analyses included: genetics (58 studies), cognition (38), neuroimaging (23), psychopathology (22), psychosocial therapies (19), neurophysiology (13), epidemiology (12), neurochemistry (8), development (7), and post-mortem (3). Those meta-analytic studies sift through thousands of published papers and help provide part of the “evidence” in schizophrenia. Similar meta-analyses are conducted for all psychiatric disorders.
Finally, I did not instruct readers that they must practice in an evidence-based manner. However, I implied that many patients are not receiving effective evidence-based care in both psychotherapy (by psychologists) and psychopharmacology (by psychiatrists). Many clinicians practice “experience-based medicine” or “eminence-based medicine,” but I believe EBM should be the basic framework into which we integrate our clinical experience or expert opinions to provide optimal care for our patients.
Henry A. Nasrallah, MD
Editor-in-Chief
1. Gray GE. Concise guide to evidence-based psychiatry. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
2. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence-based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
3. Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics. Am J Psychiatry. 2006;163:185-194.
4. Nasrallah HA. Meta-analysis trends in schizophrenia over three decades. Schizophr Res. 2009;108:1-2.
Concerning the role of “evidence” in psychiatric practice (“Are psychiatrists more evidence-based than psychologists?” From the Editor, Current Psychiatry, December 2009,), my question is whether psychiatrists who consider themselves evidence-based achieve better clinical results than those who do not. I suspect there is no significant difference. Of course, this question will never be answered to Dr. Nasrallah’s standards. No pharmaceutical or insurance companies are interested enough because, with the mediation of psychiatric thought leaders, they have succeeded in redefining the nature of and criteria for evidence. They now own it. To what degree it strongly pertains to the real world is an open question.
As a psychiatrist with several decades of experience who works on the front lines, I am leery of the growing biomedical depersonalization and algorithmic regimentation of treatment. I am less optimistic about the kind of progress implied in Dr. Nasrallah’s editorial. I do not believe it is his place to tell colleagues how they should practice. Psychiatric treatment mostly occurs in the context of a one-to-one relationship, and evidence generated by the research industry must be scrutinized according to the individual patient’s exigencies and factors affecting the patient’s life and clinical condition. This is a process of clinical judgment, which integrates not only the narrowly defined, research-based evidence Dr. Nasrallah mentioned but also a psychiatrist’s experience, which there appears to be little place for in psychiatry’s brave new world. It may be that psychologists maintain a certain clinical advantage over psychiatrists in this regard.
Edmond Zeldin, MD
Pawtucket, RI
Dr. Nasrallah responds
I welcome Dr. Zeldin’s critical remarks. As a clinician, I too value my more than 3 decades of clinical experience, but as a researcher I also recognize that it is insufficient to provide optimal care. On the first page of Dr. Gregory Gray’s book Evidence-based psychiatry,1 the first heading states “Clinical practice is not always evidence-based.” Dr. Gray says that evidence-based medicine (EBM) is “the application of a knowledge of medical informatics and clinical epidemiology to the treatment of individual patients and involves the integration of the best research evidence with clinical expertise and patient values.”
The EBM concept was initiated by D.L. Sackett et al in 1996,2 not by pharmaceutical companies. However, all drug companies must conduct strictly evidence-based clinical trials (double-blind, placebo-controlled, and sufficiently powered sample size) on experimental drugs before these agents can be approved by the FDA. The large FDA studies conducted by industry are part of EBM that are adopted in clinical practice. However, some non-FDA drug company studies are self-serving and not evidence-based.3
I recently reviewed 237 meta-analytic studies in schizophrenia,4 and only 30 of those studies address pharmacology. Other meta-analyses included: genetics (58 studies), cognition (38), neuroimaging (23), psychopathology (22), psychosocial therapies (19), neurophysiology (13), epidemiology (12), neurochemistry (8), development (7), and post-mortem (3). Those meta-analytic studies sift through thousands of published papers and help provide part of the “evidence” in schizophrenia. Similar meta-analyses are conducted for all psychiatric disorders.
Finally, I did not instruct readers that they must practice in an evidence-based manner. However, I implied that many patients are not receiving effective evidence-based care in both psychotherapy (by psychologists) and psychopharmacology (by psychiatrists). Many clinicians practice “experience-based medicine” or “eminence-based medicine,” but I believe EBM should be the basic framework into which we integrate our clinical experience or expert opinions to provide optimal care for our patients.
Henry A. Nasrallah, MD
Editor-in-Chief
Concerning the role of “evidence” in psychiatric practice (“Are psychiatrists more evidence-based than psychologists?” From the Editor, Current Psychiatry, December 2009,), my question is whether psychiatrists who consider themselves evidence-based achieve better clinical results than those who do not. I suspect there is no significant difference. Of course, this question will never be answered to Dr. Nasrallah’s standards. No pharmaceutical or insurance companies are interested enough because, with the mediation of psychiatric thought leaders, they have succeeded in redefining the nature of and criteria for evidence. They now own it. To what degree it strongly pertains to the real world is an open question.
As a psychiatrist with several decades of experience who works on the front lines, I am leery of the growing biomedical depersonalization and algorithmic regimentation of treatment. I am less optimistic about the kind of progress implied in Dr. Nasrallah’s editorial. I do not believe it is his place to tell colleagues how they should practice. Psychiatric treatment mostly occurs in the context of a one-to-one relationship, and evidence generated by the research industry must be scrutinized according to the individual patient’s exigencies and factors affecting the patient’s life and clinical condition. This is a process of clinical judgment, which integrates not only the narrowly defined, research-based evidence Dr. Nasrallah mentioned but also a psychiatrist’s experience, which there appears to be little place for in psychiatry’s brave new world. It may be that psychologists maintain a certain clinical advantage over psychiatrists in this regard.
Edmond Zeldin, MD
Pawtucket, RI
Dr. Nasrallah responds
I welcome Dr. Zeldin’s critical remarks. As a clinician, I too value my more than 3 decades of clinical experience, but as a researcher I also recognize that it is insufficient to provide optimal care. On the first page of Dr. Gregory Gray’s book Evidence-based psychiatry,1 the first heading states “Clinical practice is not always evidence-based.” Dr. Gray says that evidence-based medicine (EBM) is “the application of a knowledge of medical informatics and clinical epidemiology to the treatment of individual patients and involves the integration of the best research evidence with clinical expertise and patient values.”
The EBM concept was initiated by D.L. Sackett et al in 1996,2 not by pharmaceutical companies. However, all drug companies must conduct strictly evidence-based clinical trials (double-blind, placebo-controlled, and sufficiently powered sample size) on experimental drugs before these agents can be approved by the FDA. The large FDA studies conducted by industry are part of EBM that are adopted in clinical practice. However, some non-FDA drug company studies are self-serving and not evidence-based.3
I recently reviewed 237 meta-analytic studies in schizophrenia,4 and only 30 of those studies address pharmacology. Other meta-analyses included: genetics (58 studies), cognition (38), neuroimaging (23), psychopathology (22), psychosocial therapies (19), neurophysiology (13), epidemiology (12), neurochemistry (8), development (7), and post-mortem (3). Those meta-analytic studies sift through thousands of published papers and help provide part of the “evidence” in schizophrenia. Similar meta-analyses are conducted for all psychiatric disorders.
Finally, I did not instruct readers that they must practice in an evidence-based manner. However, I implied that many patients are not receiving effective evidence-based care in both psychotherapy (by psychologists) and psychopharmacology (by psychiatrists). Many clinicians practice “experience-based medicine” or “eminence-based medicine,” but I believe EBM should be the basic framework into which we integrate our clinical experience or expert opinions to provide optimal care for our patients.
Henry A. Nasrallah, MD
Editor-in-Chief
1. Gray GE. Concise guide to evidence-based psychiatry. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
2. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence-based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
3. Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics. Am J Psychiatry. 2006;163:185-194.
4. Nasrallah HA. Meta-analysis trends in schizophrenia over three decades. Schizophr Res. 2009;108:1-2.
1. Gray GE. Concise guide to evidence-based psychiatry. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
2. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence-based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
3. Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics. Am J Psychiatry. 2006;163:185-194.
4. Nasrallah HA. Meta-analysis trends in schizophrenia over three decades. Schizophr Res. 2009;108:1-2.